Improving Chronic Illness Care Chronic Care Model Family



- Slides: 12

Improving Chronic Illness Care: Chronic Care Model Family Medicine Introduction to Chronic Disease Care Selective Mary C. Spalding, MD 7/1/14 Copyright 1996 -2014 The Mac. Coll Center. The Improving Chronic Illness Care program is supported by The Robert Wood Johnson Foundation, with direction and technical assistance provided by Group Health's Mac. Coll Center for Health Care Innovation
Chronic Condition Any condition that requires ongoing adjustments by the affected person and interactions with the health care system. • Most recent data show that more than 145 million people are chronically ill • By 2030, an estimated chronically ill population of 171 million.

Current Management of Diseases Many deficiencies: • Rushed practitioners not following established practice guidelines • Lack of care coordination • Lack of active follow-up to ensure the best outcomes • Patients inadequately trained to manage their illnesses
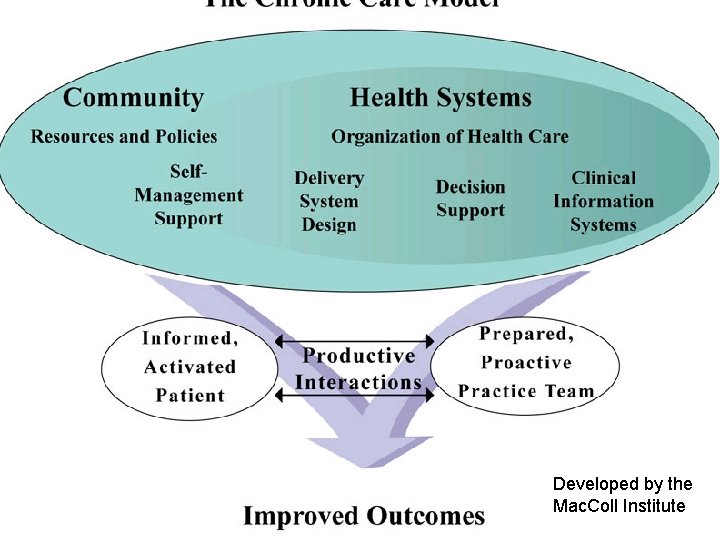
Chronic Care Model • Summarizes the basic elements for improving care in health systems at the community, organization, practice and patient levels. • Promotes effective change in provider groups to support evidence-based clinical and quality improvement across a wide variety of health care settings.
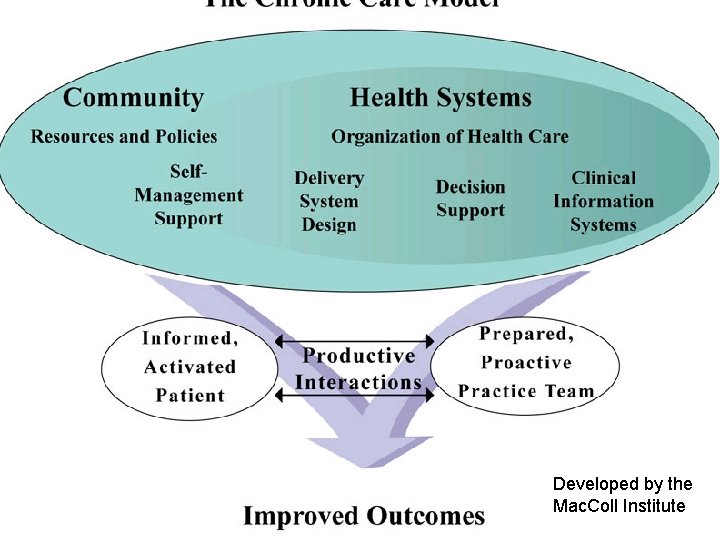
Developed by the Mac. Coll Institute
Health System Create a culture, organization and mechanisms that promote safe, high quality care • Visibly support improvement at all levels of the organization, beginning with the senior leader • Promote effective improvement strategies aimed at comprehensive system change • Encourage open and systematic handling of errors and quality problems to improve care • Provide incentives based on quality of care • Develop agreements that facilitate care coordination within and across organizations
Delivery System Design Assure the delivery of effective, efficient clinical care and self-management support • Define roles and distribute tasks among team members • Use planned interactions to support evidence-based care • Provide clinical case management services for complex patients • Ensure regular follow-up by the care team • Give care that patients understand that fits with their cultural background
Decision Support Promote clinical care that is consistent with scientific evidence and patient preferences • Embed evidence-based guidelines into daily clinical practice • Share evidence-based guidelines and information with patients to encourage their participation • Use proven provider education methods • Integrate specialist expertise and primary care

Clinical Information Systems Organize patient and population data to facilitate efficient and effective care Provide timely reminders for providers and patients Identify relevant subpopulations for proactive care Facilitate individual patient care planning Share information with patients and providers to coordinate care • Monitor performance of practice team and care system • •
Self-Management Support Empower and prepare patients to manage their health and health care • Emphasize the patient's central role in managing their health • Use effective self-management support strategies that include assessment, goal-setting, action planning, problem-solving and follow-up • Organize internal and community resources to provide ongoing self-management support to patients
The Community Mobilize community resources to meet needs of patients • Encourage patients to participate in effective community programs • Form partnerships with community organizations to support and develop interventions that fill gaps in needed services • Advocate for policies to improve patient care
The RAND Evaluation • Organizations were able to improve, making an average of 48 changes in 5. 8 out of the 6 CCM areas; • Patients with diabetes had significant decreases to their risk of cardiovascular disease; • CHF pilot patients more knowledgeable and more often on recommended therapy, had 35% fewer hospital days; • Asthma and diabetes pilot patients were more likely to receive appropriate therapy.
 Improving chronic illness care model
Improving chronic illness care model Accidents/illness of family members
Accidents/illness of family members Wagner's chronic care model
Wagner's chronic care model Chronic care model definition
Chronic care model definition Flinders model of chronic health disorders
Flinders model of chronic health disorders Wagner chronic care model 1998
Wagner chronic care model 1998 Nurses improving care for healthsystem elders
Nurses improving care for healthsystem elders Gap model of service quality with examples
Gap model of service quality with examples Gaps model for improving service quality
Gaps model for improving service quality Conclusion of mental health
Conclusion of mental health Chronic care solutions
Chronic care solutions Chronic care
Chronic care Hepatitis a incubation period
Hepatitis a incubation period