Paediatrics and Child Health The child with developmental



















- Slides: 60
Paediatrics and Child Health The child with developmental delay / learning difficulties

Learning outcomes you should be able to … 1. Recognise the key stages of normal childhood development 2. Make an outline assessment of a child with developmental delay 3. Use playtime to assess the nature and degree of delay 4. Recognise major differences between global and isolated areas of delay
… more learning outcomes 5. Identify major categories of developmental delay in patients 6. Initiate appropriate investigations for the cause of developmental delay 7. Work with the multidisciplinary team in the assessment and care of patients with developmental delay 8. Assess the impact of delay and / or complex needs on the child and the family 9. Recognise multiple factors impacting on a child’s ability to learn
1. Recognise the key stages of normal childhood development

Typically developing children l l l Sequence of acquired skills Areas of development in young children Quality of skills
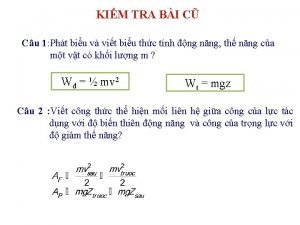
Four Domains of Development 1. 2. 3. 4. Gross motor skills Fine motor and visual skills Hearing, speech and language skills Social, emotional and behavioural skills Cognitive development refers to higher mental function
Developmental surveillance Reviews l Newborn examination l 6 -8 weeks l 6 -9 month l 18 -24 months l 3 -3 ½ years l Preschool review
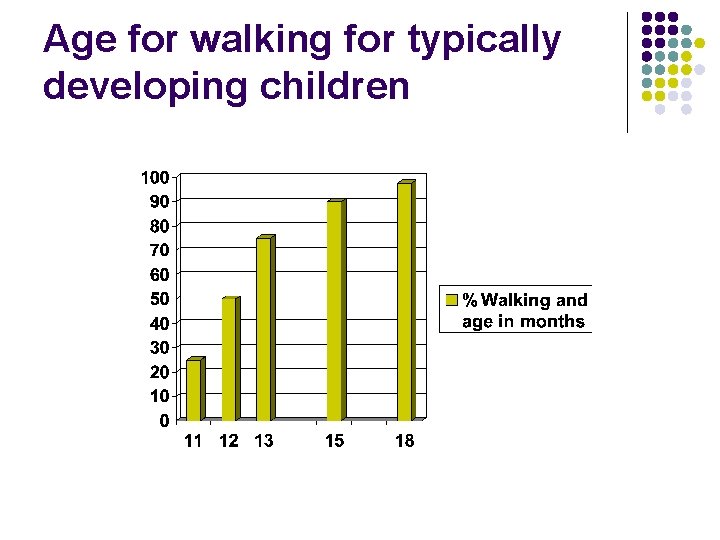
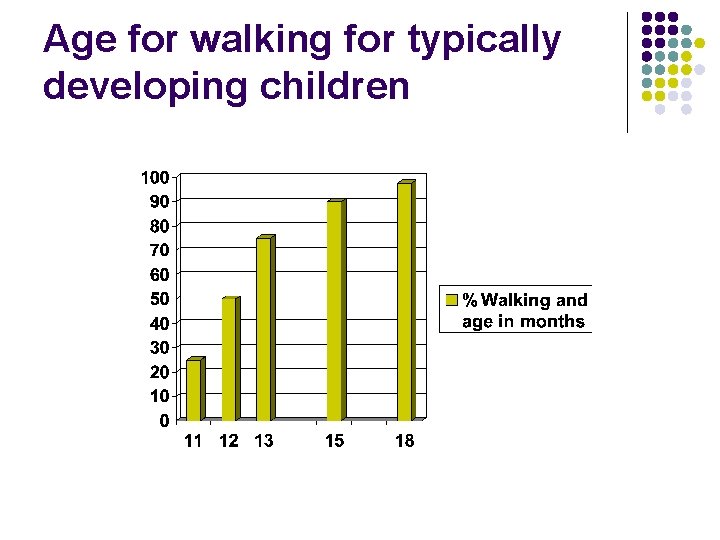
Age for walking for typically developing children
‘Normal’ l Median age for walking is 12 months l Limit age (2 standard deviations above average) is 18 months
Typically Developing Child: Gross motor Newborn examination: limbs flexed, marked head lag 6 -8 weeks: Lying prone, lifts head to 45 degree 6 -9 month: little or no head control on pull-to-sit (3 m), rolls back to front (6 m), sits without support (8 m)
Gross motor (12 -18 months): crawls (10 m) stands independently (11 m) walks independently (12 m)

Gross motor 18 -24 months: squats to pick up an object (18 m) Runs (2 y) runs (2 y) walks upstairs holding on and two feet to a step (2 y), 3 -3 ½ years: walks alone upstairs with alternating feet per step (3 y) pedals tricycle (3 y) 4 years: Hops (4 y)
Limits ages: Gross motor skills Still has head lag at 4 months (not in line with spine on pull to sit) l Persistent primitive reflexes 34 months l Unable to sit unsupported at 9 m l Not walking independently at 18 m l Nb asymmetry at any age l
Fine motor and visual skills Newborn examination: hands closed 6 -8 weeks: Does your baby watch your face and follow with his/her eyes? Fixes and follows briefly 6 -9 month: Have you noticed a squint? Palmar grasp (5 m) Passes toy from hand to hand (6 m) Inferior (raking) pincer grasp (9 m) Looking for falling toys: object prmanence (9 m).
Fine motor 12 -18 months: Refined pincer (10 ½ m) Tower of two bricks (15 m) Scribbles spontaneously (15 m) Imitates stroke (18 m)

Fine motor 18 -24 months: Tower 3 bricks (18 m) Tower 6 or 7 bricks (2 years)

Fine motor 3 – 4 years: Copies (pre-drawn) circle (3 y) Draws person: head and one other part (3 y) Copies (pre-drawn) cross (4 y) Draws person: head, legs and arms (4 y) Copies pre-drawn square (4 ½ y) Draws person: face, trunk, legs, arms (5 y)

Limits ages: Fine motor skills l l l Not fixing and following visually at 3 m Not reaches for objects at 6 m Not transferring objects at 8 m Not developed pincer grasp at 12 m Not turning pages 24 m Inability to stack graded cups 24 m

Hearing, speech and language Newborn: startles to loud noises 6 - 8 weeks: vocalises when pleased 6 ½ weeks 6 – 9 months: Turns to sounds (7 m) Babbbles (6 ½ m) monosyllabic then polysyllabic
Hearing and language 12 – 18 months: Knows and turns to own name (12 m) Shows undersatnding of familiar objects and people (12 m) Points to show interest (15 m) Can point to two named body parts (on self) (15 m) on doll (18 m) Uses 2 to 6 recognisable words (15 m)
Hearing and language 18 – 24 months: l l Follow a two-step command (2 y). Put the brick in the cup. Puts 2 or more words together to form simple sentences (2 y) e. g. ‘Daddy car’ (Do Not count phrases that are heard together e. g. Thank you) 3 – 3 ½ years: l l Understands commands with three key words (3 y) Understand negatives (3 y) Uses ‘what’ and ‘how’ (3 y) Uses personal pronouns (me/ you) (3 ½ y)
Hearing and language 4 years: Asks why? When? how. ? (4 y) Able to tell long stories (4 y) Counts (by rote) to 20 (4 y)

Limits ages: Hearing, speech and language l l l l No double syllable babble aged 12 m No words with meaning at 12 m Fewer than 6 words at 18 m Not responding to one word commands at 18 m No 2 – 3 words phrases at 2 ½ y Unintelligible/ repeating phrases without meaning at 3 y The child who appears not to understand Parental / professional concern
Social, emotional and behavioural skills 6 – 8 weeks: Smiles responsively 6 – 9 months: Takes everything to mouth (7 m): should disappear by 12 m Put hand up to bottle/ breast when feeding (6 m) Stranger awareness (9 m) Plays peek-a-boo (9 m)
Social, emotional and behavioural skills 18 – 24 months: Holds spoon and gets food to mouth (18 m) Plays alongside other children (2 y) 3 – 3 ½ years: Shares toys. (3 y)Simple make- believe play with peers (3 y) Eats with fork and spoon (3 y) Able to postpone urination during the day (3 y) Can pull pants up and down.
Social, emotional and behavioural development 4 years: Eats with knife and fork. Understands taking turns. Dress and undress excluding fastenings (3 ½ to 4 y)

Limits ages: Social, emotional and behavioural skills l l l Not smiling at 8 weeks Persistent mouthing at 12 m No symbolic play at 3. 5 years Not playing with peers at 3. 5 years Other concerns
Further reading: l l Illustrated Paediatrics From Birth to Five Years Children’s Developmental Progress, Mary D Sheridan
2. Make an outline assessment 3. Use playtime to assess delay Observe: Start with some typically developing children. Observe the child’s play History: Ask parents about developmental milestones Their baby’s gestation at birth and current age Do the parents have any concerns Examination: Use available toys: bricks, pencil paper, books, balls to test 4 domains of development: Gross motor, fine motor and vision, language and hearing, social Interpretation: Consider the 4 domains of development. Is the child achieving expected developmental progress in all areas?
Developmental Assessment Tools Standardised assessment tools you may see in use: q The “Schedule of Growing Skills” (Nelson) q The Denver charts q The Griffiths Scales During your training you should aim to: 1. Observe a developmental assessment in clinic 2. See a child at home with a health visitor 3. Carry out some outline assessments (start with a typically developing child)
Developmental assessment in clinic l History l l l Developmental assessment l l Antenatal history Birth history Medical History Developmental history Family and social history Fine motor, language and then gross motor (we start with tasks the child can do). Usually dependent on Hx for selfcare and interactive social skills. Qualitative observations Examination inc OFC, Ht, Wt

4. Difference between global and isolated delay John Smith, aged 3, was slow to walk … at what age would you expect most children to be walking independently? Adam Scott, aged 10 months, was slow to babble … when would you expect a baby to babble? …and what about first words, when do they emerge?
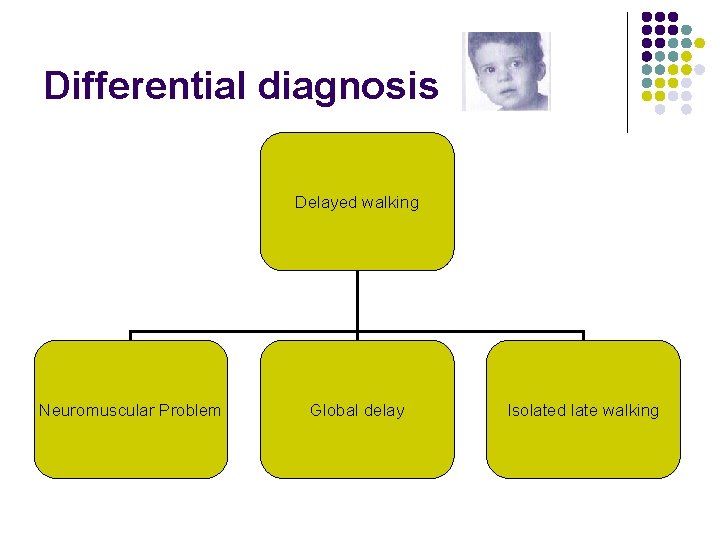
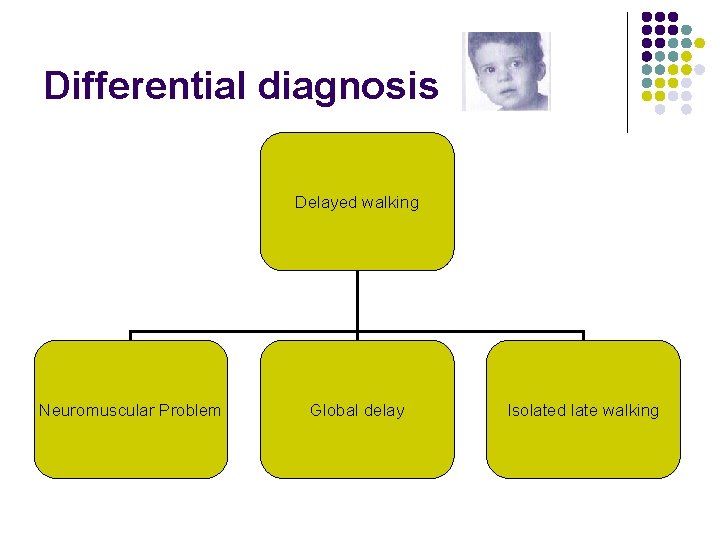
Differential diagnosis Delayed walking Neuromuscular Problem Global delay Isolated late walking
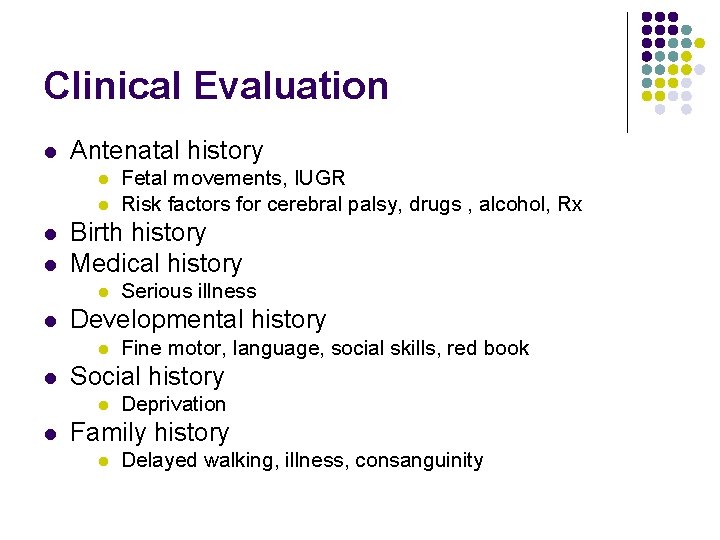
Clinical Evaluation l Antenatal history l l Birth history Medical history l l Fine motor, language, social skills, red book Social history l l Serious illness Developmental history l l Fetal movements, IUGR Risk factors for cerebral palsy, drugs , alcohol, Rx Deprivation Family history l Delayed walking, illness, consanguinity

Clinical examination l Neurological l l Movement and posture, muscle mass, power, tone, reflexes, sensation, bladder and bowel control ? muscle, neuromuscular, motor neuron, CNS OFC, vision, hearing, dysmorphism, skin Developmental l General developmental assessment ? global v. isolated Importance of follow up and monitoring progress
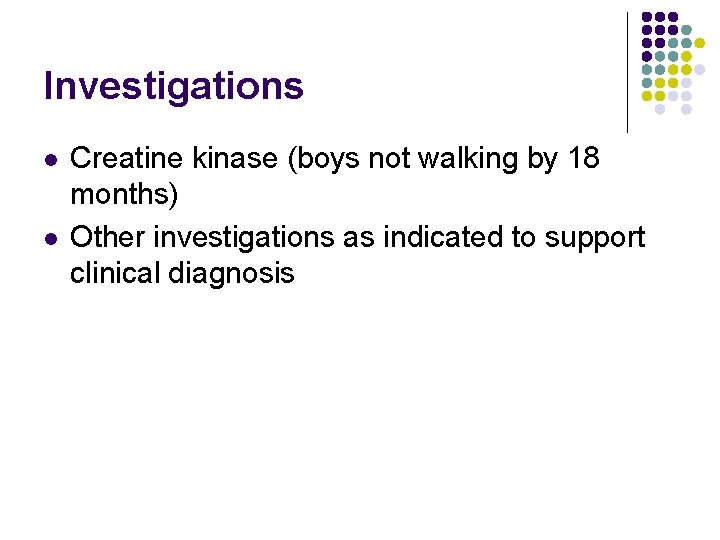
Investigations l l Creatine kinase (boys not walking by 18 months) Other investigations as indicated to support clinical diagnosis
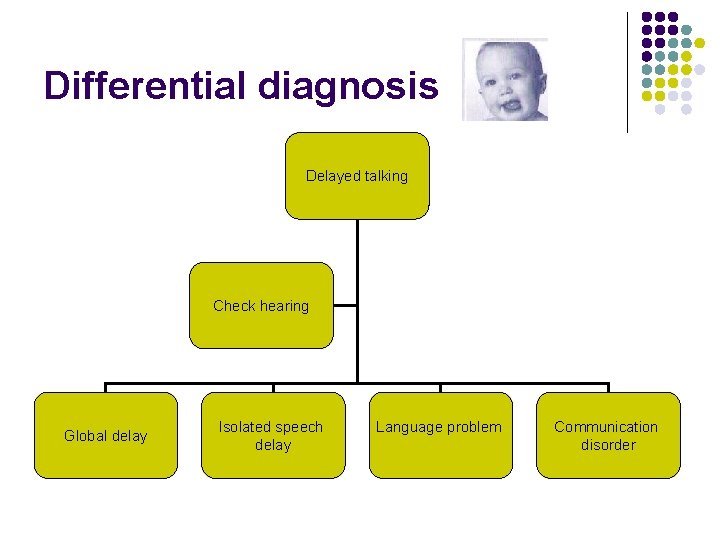
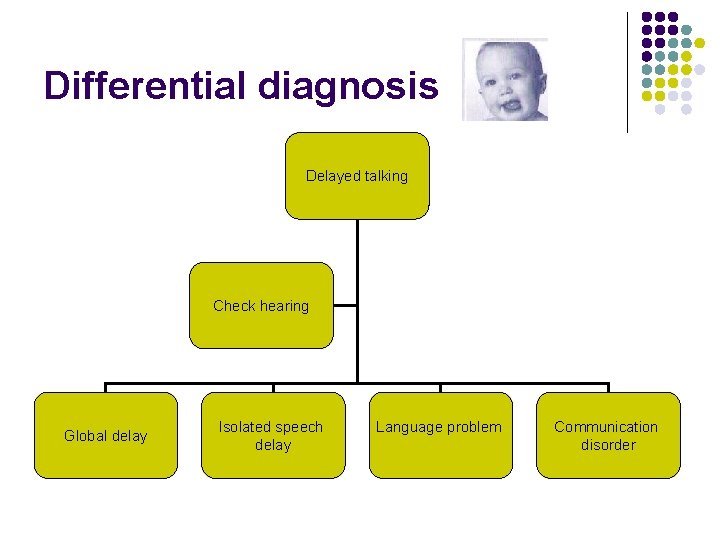
Differential diagnosis Delayed talking Check hearing Global delay Isolated speech delay Language problem Communication disorder
Speech delay l l Is there a hearing problem? Is there evidence of global delay? Is there a speech or language problem? Is this a pervasive communication problem?
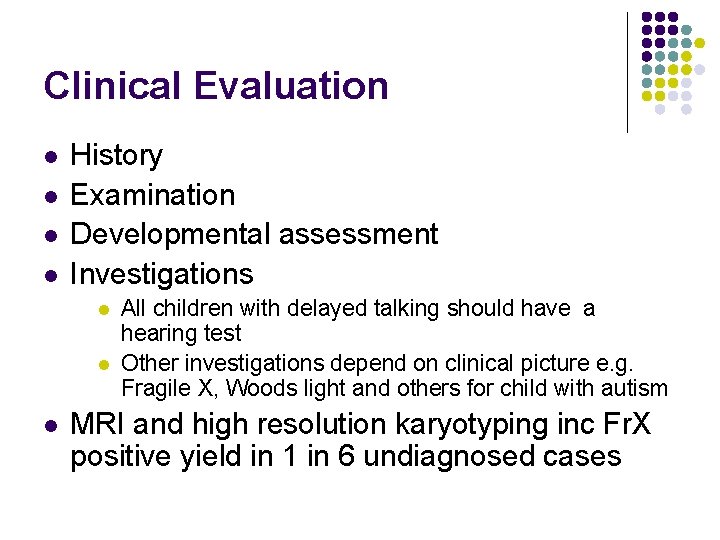
Clinical Evaluation l l History Examination Developmental assessment Investigations l l l All children with delayed talking should have a hearing test Other investigations depend on clinical picture e. g. Fragile X, Woods light and others for child with autism MRI and high resolution karyotyping inc Fr. X positive yield in 1 in 6 undiagnosed cases
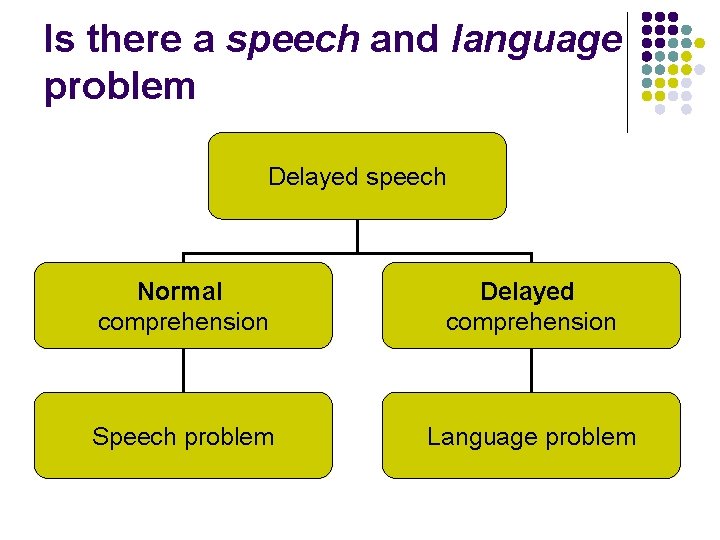
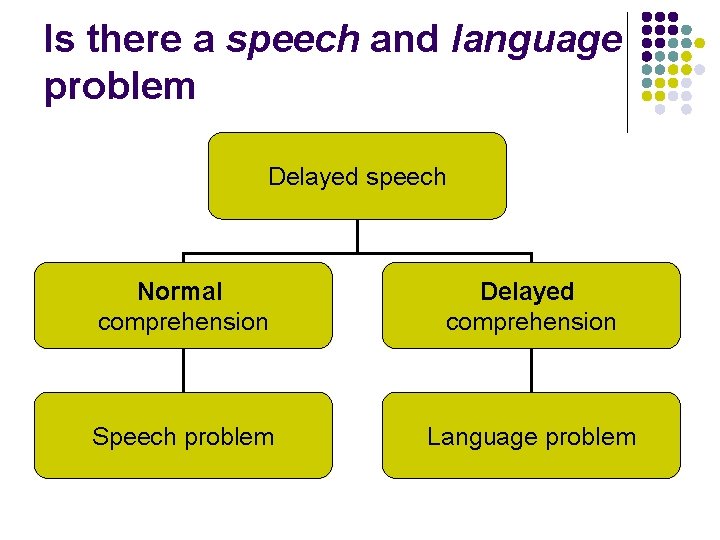
Is there a speech and language problem Delayed speech Normal comprehension Delayed comprehension Speech problem Language problem

Peter Small, aged 7, was difficult to engage in conversation in clinic, what kind of conversation would you expect to have with a child of this age? Think of some reasons why a 7 year old child may have difficulty holding a conversation
Is this a pervasive communication problem? l Does the child have normal non-verbal communication skills? l l l Smiling, gaze fixation Turn taking Pointing Waving Showing and sharing

Is there ‘autistic’ behaviour? l Clinically l l Social interactions (‘avoidance’) Play skills (‘mechanical’ not ‘imaginative’) Obsessions (video, routes, routines) Standardised assessment l l l DSM IV / ICD 10 criteria Autism Diagnostic Interview Autism Diagnostic Observations Schedule

Normal Development

Severity of Developmental delay 20 5 0 % child population Developmental abilities and intelligence in the childhood population follow a normal distribution curve just like height or weight. 70 100 140 Developmental quotient Children whose attainments fall below the 2 nd centile have a significant delay. Intelligence quotient (DQ) <70 (Average DQ = 100) Delays are divided into: DQ §Mild 60 -70 §Moderate 50 -60 §Severe 40 -50 §Profound <40
Identifying developmental delay During the first year of life …. l the most dramatic changes seen in development are in the area of gross motor skills as the child learns to walk l Severe or moderate global developmental delay may be first noticed because the child is slow to sit, roll, crawl and walk – but the sequence of these events will follow the normal pattern l Detailed assessment will show if the delay is global or specific
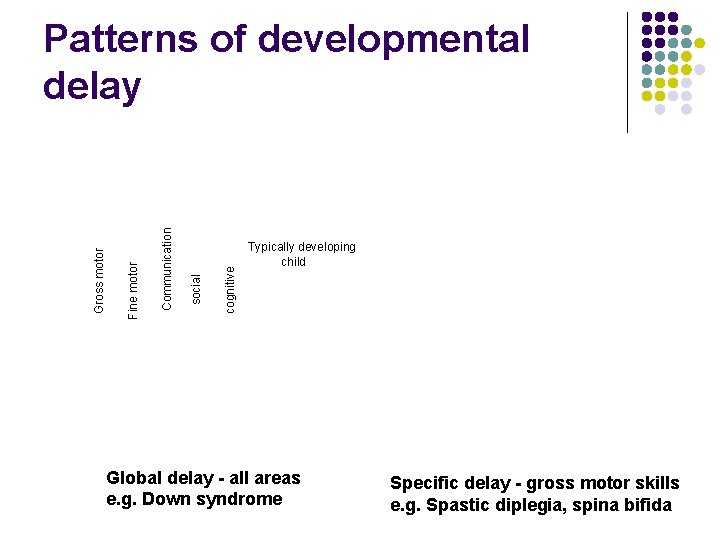
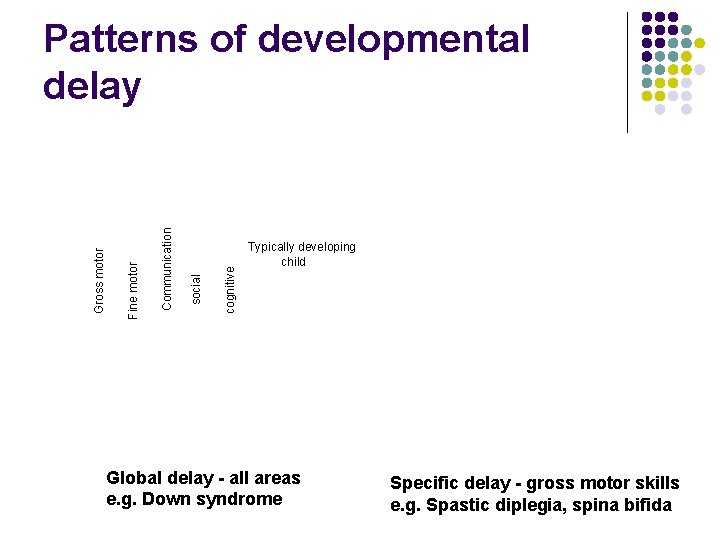
cognitive social Communication Fine motor Gross motor Patterns of developmental delay Typically developing child Global delay - all areas e. g. Down syndrome Specific delay - gross motor skills e. g. Spastic diplegia, spina bifida
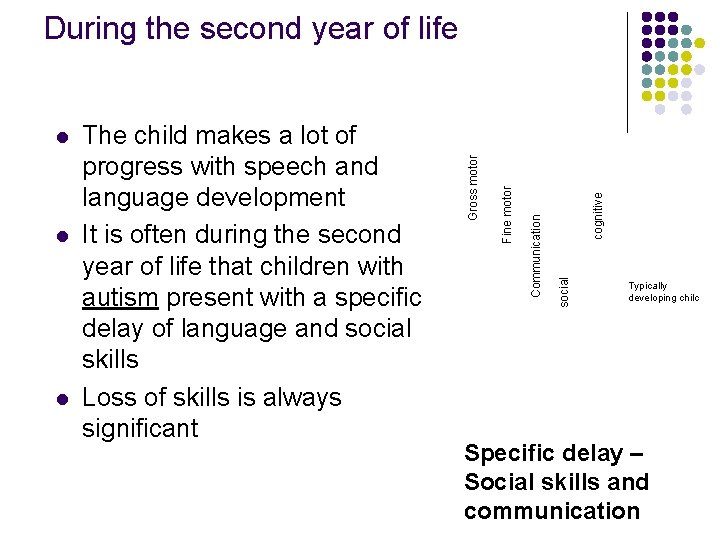
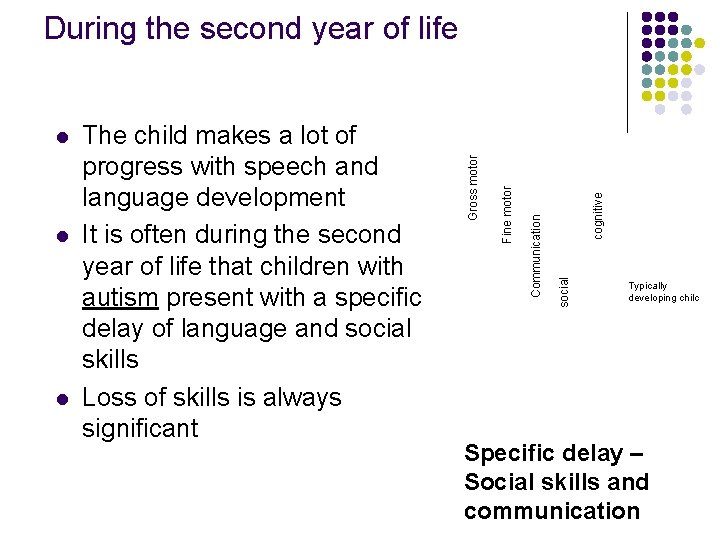
l cognitive social Communication l The child makes a lot of progress with speech and language development It is often during the second year of life that children with autism present with a specific delay of language and social skills Loss of skills is always significant Fine motor l Gross motor During the second year of life Typically developing chilc Specific delay – Social skills and communication
During the fourth year of life l l Cognitive abilities become more apparent with increasing age. As children approach school age mild or moderate learning difficulties may be noticed for the first time by pre-school teachers who will refer to the educational psychologist and paediatrician.
Case Study l Amy is a 7 year old school girl. She was healthy at birth. Her 7 month health visitor developmental screen suggested that her development was within satisfactory limits l What does this mean in terms of the four areas of development discussed earlier?
Thinking time ….
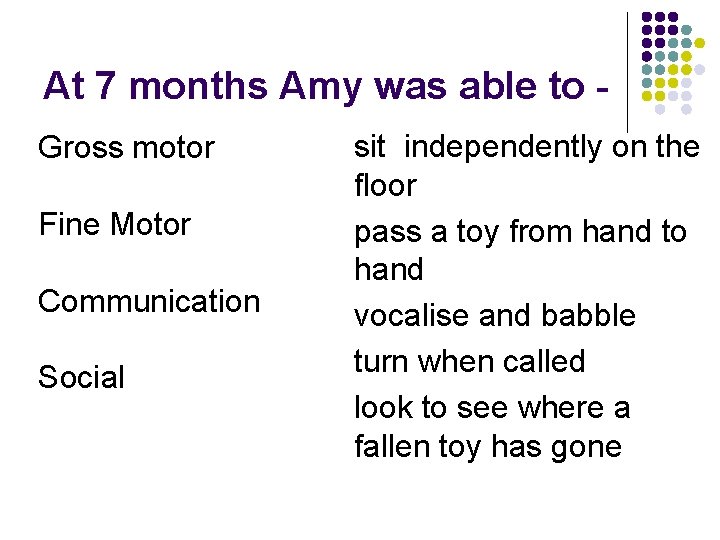
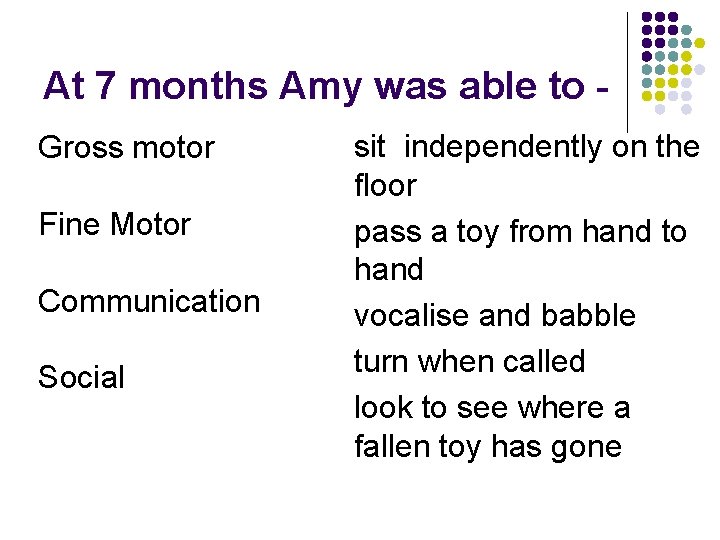
At 7 months Amy was able to Gross motor Fine Motor Communication Social sit independently on the floor pass a toy from hand to hand vocalise and babble turn when called look to see where a fallen toy has gone

Case study 1 continued l Amy then had an episode of encephalitis of unknown cause. Her parents were devastated. She recovered and she is now a happy seven year old school girl, but she has an acquired cerebral palsy affecting all four limbs and severe learning difficulties. Amy is well supported at home and at school Write a list of people, whom you think will be involved in her care …

The support network includes. . 1. Parents and family 2. Professionals l Health l Social Services l Education Parents and professionals form the multi-agency team who together develop a “care plan” to meet all Amy’s needs The best way to find out more is to talk to parents and professionals and sit in on a multi -agency meeting

The support team - school Amy has a special seat at school and a special tricycle for playtime. She does daily physio with her teachers aid as well as school work, such as threading beads and posting shapes. She knows her shapes and colours, but her speech is difficult to understand, so she is learning to use Makaton signs and she has an Alphasmart to record her ideas. Her peers are reading, writing and running about at play time. They like to come and help Amy, but she can’t join in with all their games.
The support team - home At home Amy has a hoist to lift her onto her bed and into the bath. How do you think she gets up stairs? Who will advise her about her exercises and equipment needs? Who advises about extra help at school and at home? Are these people on your list? Consider the day to day reality for Amy’s parents as they care for her, helping her to stay healthy and learn new skills. Parents react in different ways. Find out from parents and young people what kind of help they need.
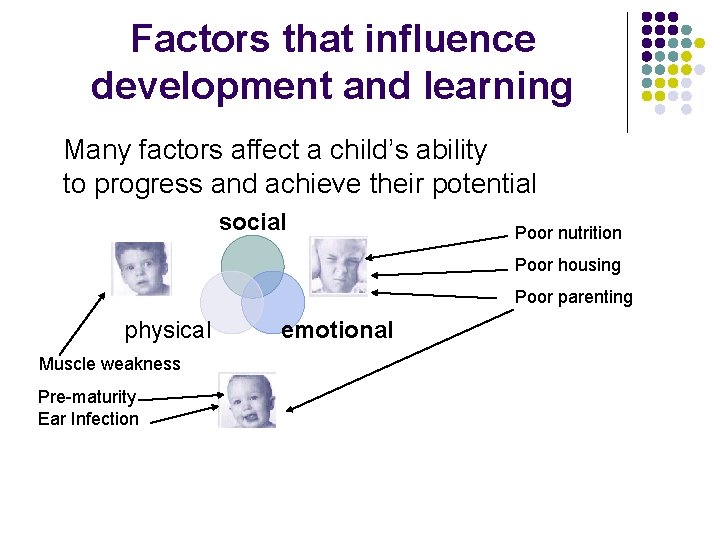
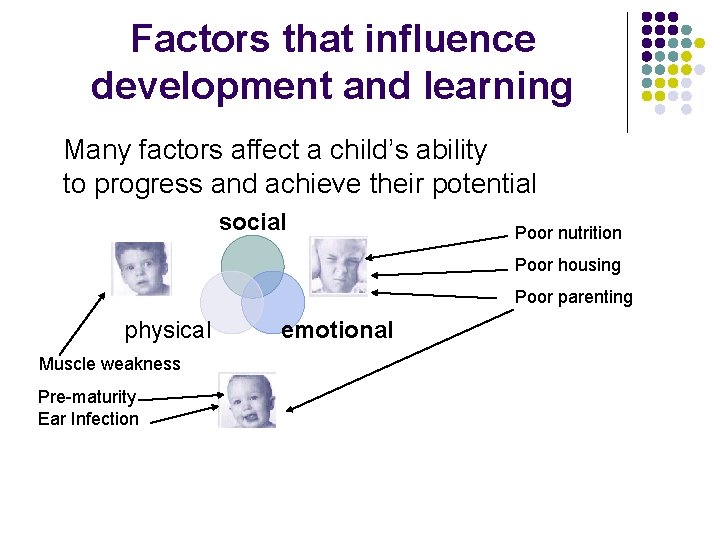
Factors that influence development and learning Many factors affect a child’s ability to progress and achieve their potential social Poor nutrition Poor housing Poor parenting physical Muscle weakness Pre-maturity Ear Infection emotional
More Resources 1. 2. 3. 4. 5. 6. The cerebral palsy website www. scope. org. uk The national autistic society website www. nas. org. uk Contact a family website www. cafamily. org. uk www. downs-syndrome. org. uk There is also a good site written by a parent/paediatrician of a child with down’s syndrome www. ds-health. com Paediatric information www. pier. org. uk

remember…. l Children learn through play and are continually gaining new skills l You can learn about children by watching them at play and playing with them l Understanding normal development helps you to recognise the child with developmental delay like all new skills this takes time l Parents know their child best – ask them what their child can do and if they have concerns
Specialty evaluation l l l Confirmation and categorisation of child’s developmental delay Identification of underlying aetiology Referral to, and assurance of, the provision of appropriate therapy services and resources Counselling of family regarding diagnosis. Aetiology and prognosis Identification of any possible co-existing conditions that may require medical intervention and ongoing management
 Royal college of paediatrics developmental milestones
Royal college of paediatrics developmental milestones History taking paediatrics
History taking paediatrics Paediatrics
Paediatrics Neonatology lectures
Neonatology lectures London school of paediatrics
London school of paediatrics Child's developmental needs triangle
Child's developmental needs triangle National programs related to child health and welfare
National programs related to child health and welfare Chapter 50 intellectual and developmental disabilities
Chapter 50 intellectual and developmental disabilities 14 lcp principles
14 lcp principles Health and social care component 3
Health and social care component 3 Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Glasgow thang điểm
Glasgow thang điểm Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Các môn thể thao bắt đầu bằng tiếng bóng
Các môn thể thao bắt đầu bằng tiếng bóng Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế
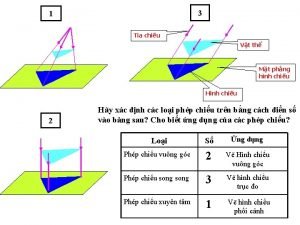
Cái miệng nó xinh thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Ví dụ giọng cùng tên
Ví dụ giọng cùng tên Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Tia chieu sa te
Tia chieu sa te Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot Số nguyên tố là
Số nguyên tố là Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Objective of child health
Objective of child health National policies related to child health and welfare
National policies related to child health and welfare History of maternal and child health
History of maternal and child health Maternal and child health services
Maternal and child health services Preventive health and safety in the child care setting
Preventive health and safety in the child care setting Reproductive and child health programme phase 1
Reproductive and child health programme phase 1 패자트리
패자트리 Initiative vs guilt
Initiative vs guilt Lawrence kohlberg developmental psychology
Lawrence kohlberg developmental psychology