MATERNAL CHILD HEALTH MCH Maternal and Child Health




- Slides: 31
MATERNAL CHILD HEALTH

MCH (Maternal and Child Health) • MCH is a promotive, preventive curative and rehabilitative health care to mother and children. • Health care to a special and vulnerable group • Children of < 5 yrs of age • Female of reproductive age group (15 -45 yrs ) • MCH care includes all the activities which promotes health and prevent health problem of mother and child.
Why women and children? ? • Forms priority group in any community • Forms 60 -70% of population in developing countries • In India • Women (15 -45) – 19% • Children (<5 yrs) – 40% • Vulnerable to disease, disability and death • Women – Child bearing • Children – Growth Development Survival

OBJECTIVES OF MCH CARE • Reduction of morbidity and mortality rates for mother and child. • Promotion of reproductive health. • Promotion of physical and psychological development of children.
Components of MCH care (Sub areas) • • • Maternal health Family planning Child health School health Handicapped children Care of children in special settings like day Care centers
• The content of MCH care will very according to the demography, social and economical pattern • The MCH services should always be flexible and base on and adapted to the local needs and resources of the community it serves • MCH conceived all activities which promote health and prevent or solve the health problems of mother and children 6
RECENT TRENDS IN MCH • Integration of Care: • Earlier the services is fragmented, the various components were dealt with separately by different staff or departments • This approach has changed • An integrated approach implies to all those involve in maternity care • This approach help to promote the continuity of care 7
• The improving the efficiency and effectiveness of MCH care • Risk approach: • The managerial tools for better use of scares resources • Early detection of mother and children with risk factors • And given additional and more skilled care including hospitalization 8
• Manpower Changes: • Provision of professional specialist, field workers (MPHW, HG, AWW, ASHA) and voluntary workers • • • Primary Health care: MCH care Family planning Control of infection Health education 9
Why - Mother and child combined ? • Considered as one unit – • During ante-natal period child is a part of mother only and obtain all his building material and oxygen from mother. • Child health depends on health of mother • Healthy mother provides healthy child • Certain diseases of mother during pregnancy have effects on foetus • Even after birth child is dependant on mother for nutrition up to 6 – 9 months of life. • Mother and child un-seperable – post-natal care. • Mother is first teacher of child
Who provide MCH care • In past MCH services were fragmented • Current trend is to provide MCH services and Family planning services through Family Welfare services. • MCH services should be flexible based on local community needs which are based on • • Social and economical status Local customs and traditions Status of women Level of urbanization and migration • An Obstratisian and Pediatrician joins hands and link themselves with PSM
Common MCH problems • • Malnutrition Infection Consequences of unregulated fertility Malnutrition • Pregnant female • LBW, Anemia, PPH, • Nursing women • Children • Two most important period are intrauterine life and weaning period
Common MCH problems • Infection • Maternal infection cause • • Growth retardation Abortion LBW Puerperal sepsis • Infection of children • Diarrhoea • RTI • Chronic infection like Malaria, Tb • Consequences of Uncotrolled Fertility • • Increase prevalence of LBW Anemia Abortion APH
Maternal Health • Each year in India, 30 million women experience pregnancy and 27 million have a live birth • Of these, over 100, 000 maternal deaths and one million newborn deaths occur annually. • Despite a series of programmatic initiatives, there is little evidence that maternity has become significantly safer over the last 20 years. • Current MMR is 212/100000 live births.
INDICATORS OF MCH CARE • Maternal and child health status is assessed through mortality, morbidity and growth and development. • Commonly used mortality indicators are : • Maternal mortality rate • Mortality in infancy and childhood: • Perinatal mortality rate • Neonatal mortality rate • Post neonatal mortality rate • Infant mortality rate • 1 -4 mortality rate • Under 5 mortality rate • Child survival rate
Maternal Death Watch • 380 women become Every Minute. . . pregnant • 190 women face unplanned or unwanted pregnancy • 110 women experience a pregnancy related complication • 40 women have an unsafe abortion • 1 woman dies from a pregnancy-related complication
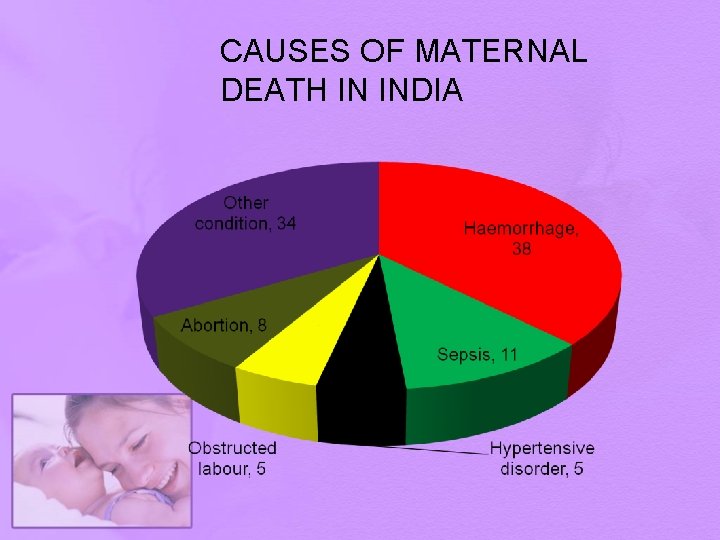
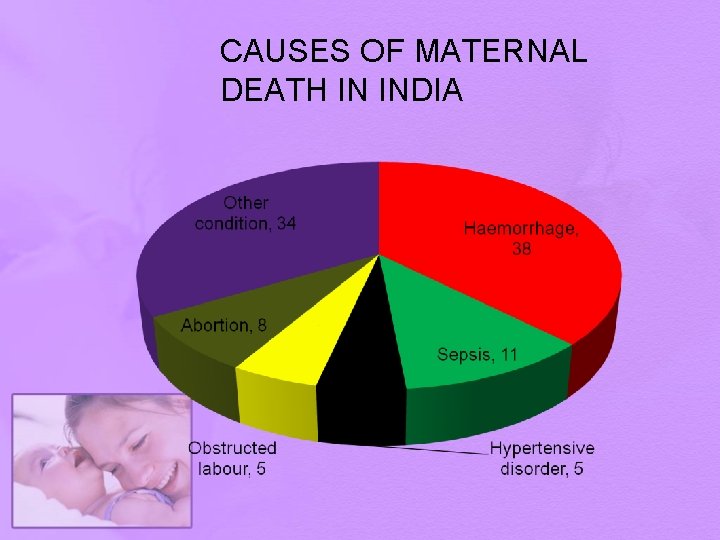
CAUSES OF MATERNAL DEATH IN INDIA
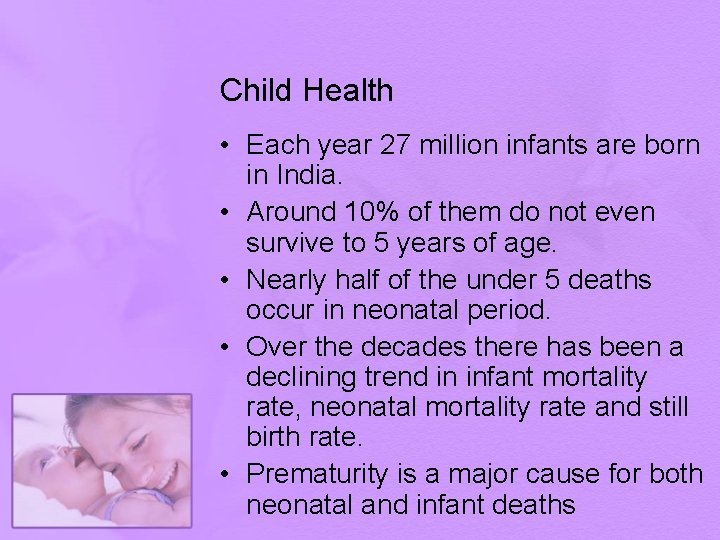
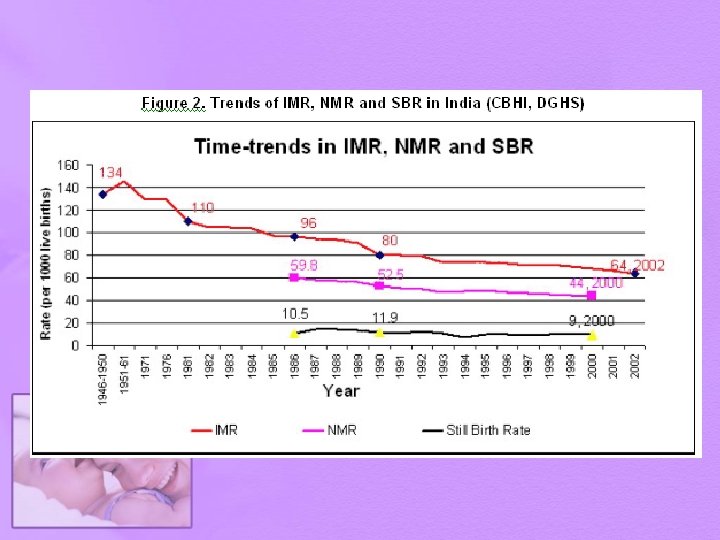
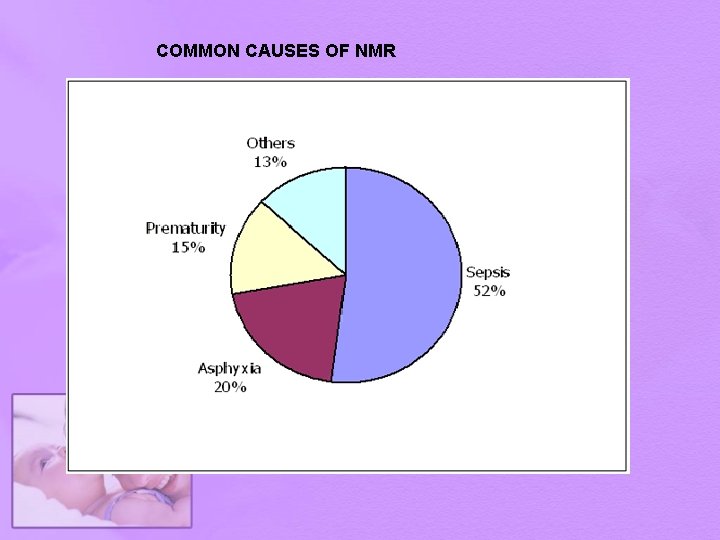
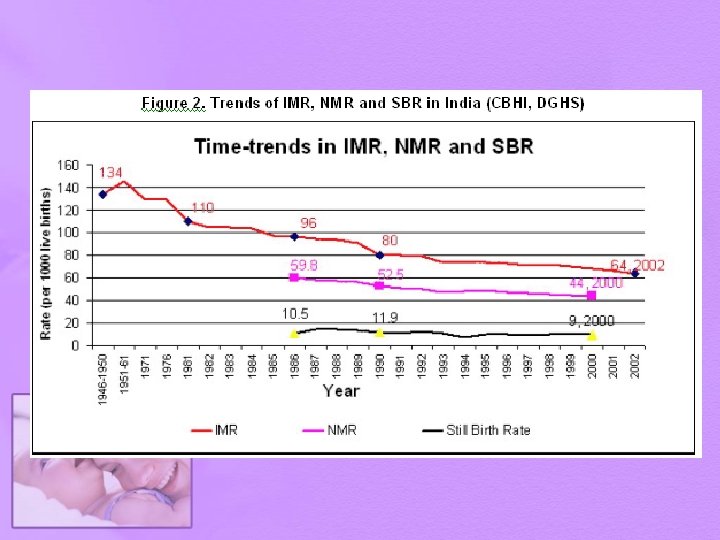
Child Health • Each year 27 million infants are born in India. • Around 10% of them do not even survive to 5 years of age. • Nearly half of the under 5 deaths occur in neonatal period. • Over the decades there has been a declining trend in infant mortality rate, neonatal mortality rate and still birth rate. • Prematurity is a major cause for both neonatal and infant deaths
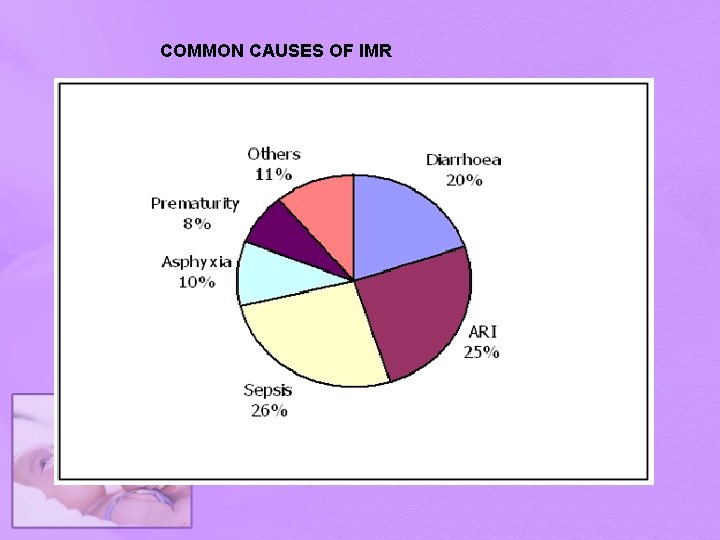
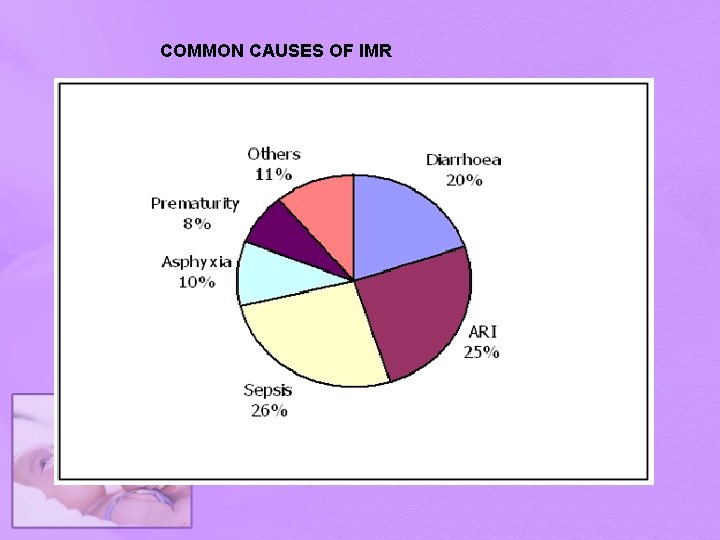
COMMON CAUSES OF IMR
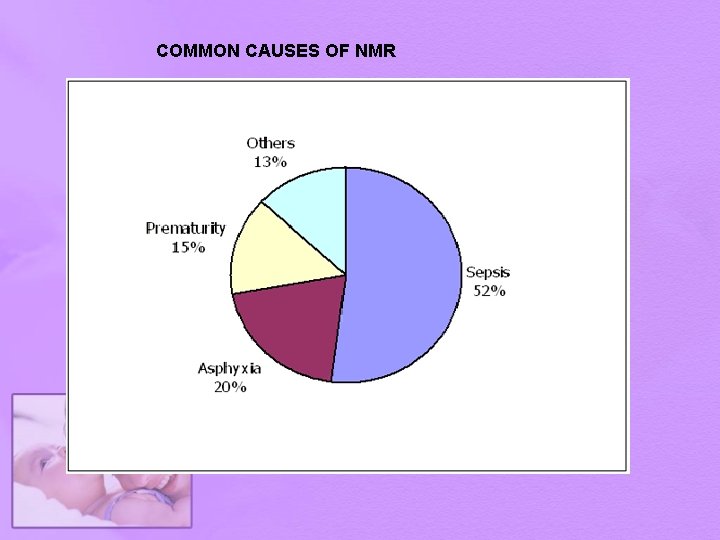
COMMON CAUSES OF NMR

Evolution of Maternal and Child health programmes in India Year Milestones 1952 Family Planning Programme adopted by Govt. of India (GOI) 1961 Dept. of Family Planning created in Ministry of Health 1971 Medical Termination of Pregnancy Act (MTP Act) 1971 1977 Renaming of Family Planning to Family Welfare 1978 Expanded Programme on Immunization (EPI) 1985 Universal Immunization Programme (UIP)+ National Oral Rehydration Therapy (ORT) Programme 1992 Child Survival and Safe Motherhood Programme (CSSM) 1996 Target-free approach 1997 Reproductive and Child Health Programme -1 (RCH-1) 2005 Reproductive and Child Health Programme -2 (RCH-2)
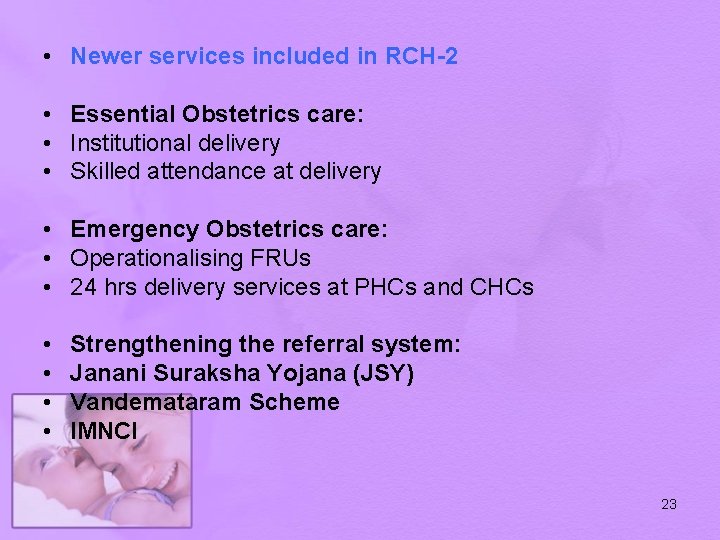
• Newer services included in RCH-2 • Essential Obstetrics care: • Institutional delivery • Skilled attendance at delivery • Emergency Obstetrics care: • Operationalising FRUs • 24 hrs delivery services at PHCs and CHCs • • Strengthening the referral system: Janani Suraksha Yojana (JSY) Vandemataram Scheme IMNCI 23
Janani Suraksha Yojana Expectations of a mother from Society. .
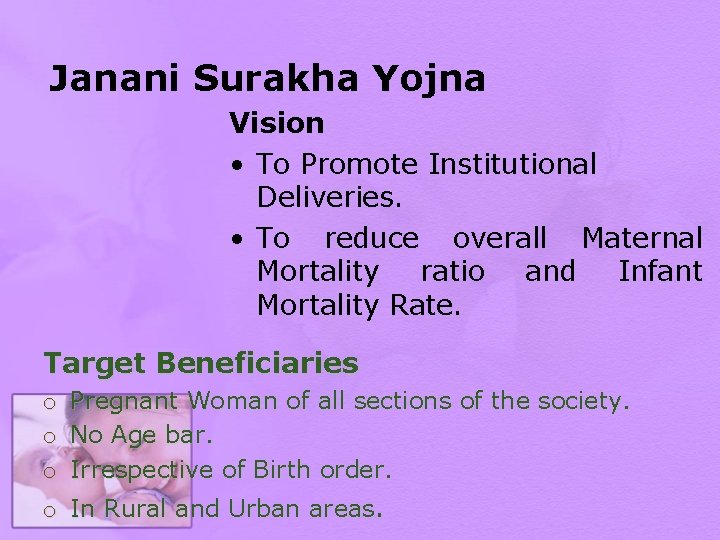
Janani Surakha Yojna Vision • To Promote Institutional Deliveries. • To reduce overall Maternal Mortality ratio and Infant Mortality Rate. Target Beneficiaries o o o Pregnant Woman of all sections of the society. No Age bar. Irrespective of Birth order. o In Rural and Urban areas.
Strategy Early Registration at AWC/SC (MCHN days) Provision of 3 ANC & 2 PNC Early identification of complicated case Arrange Referral Transport & Escort her Role of ASHA.
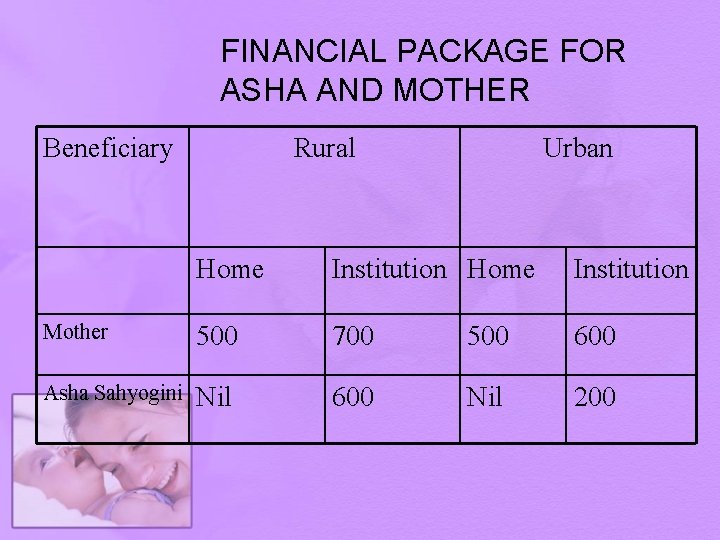
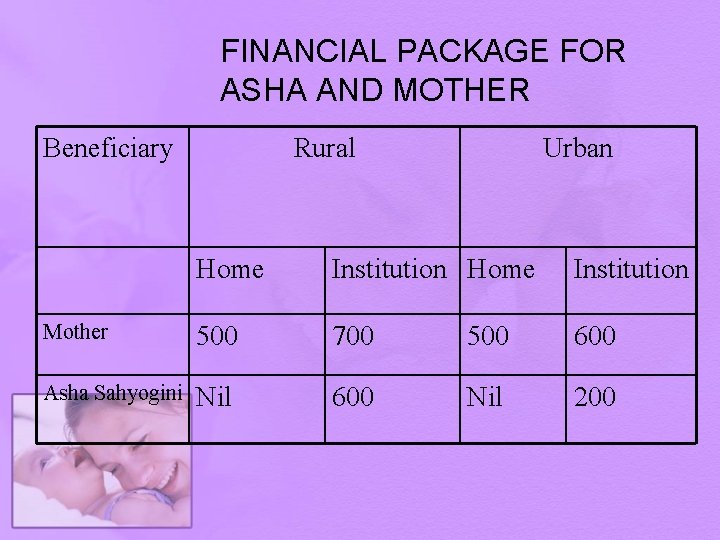
FINANCIAL PACKAGE FOR ASHA AND MOTHER Beneficiary Rural Urban Home Institution Mother 500 700 500 600 Asha Sahyogini Nil 600 Nil 200
IMCI – IMNCI • Focus on the young infant: Since a significant proportion of child mortality is centered in the first few months of life; • Inclusion of essential newborn care in the programme. • Development of a protocol for Home Visits by field functionaries like ANMs and anganwari workers for all newborns in the first week of life.
What is IMNCI • Standardized case management of sick newborns and children • Focus on the most common causes of mortality • Nutrition assessment and counselling for all sick infants and children • Home care for newborns to • promote exclusive breastfeeding • prevent hypothermia • improve illness recognition & timely care seeking
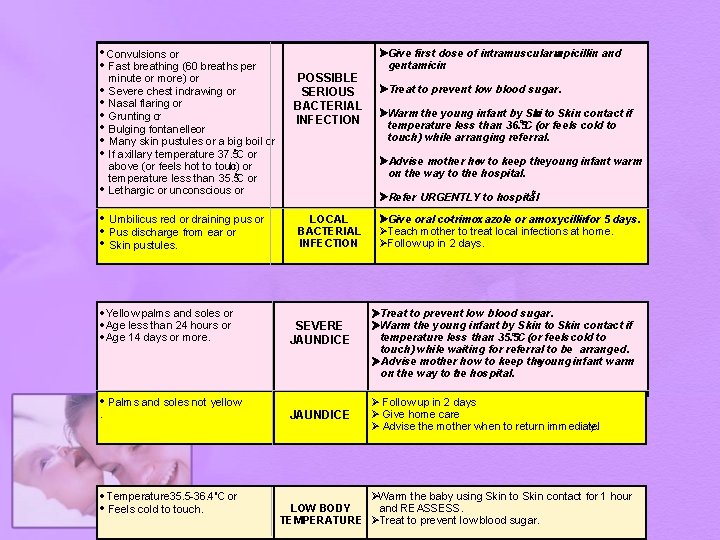
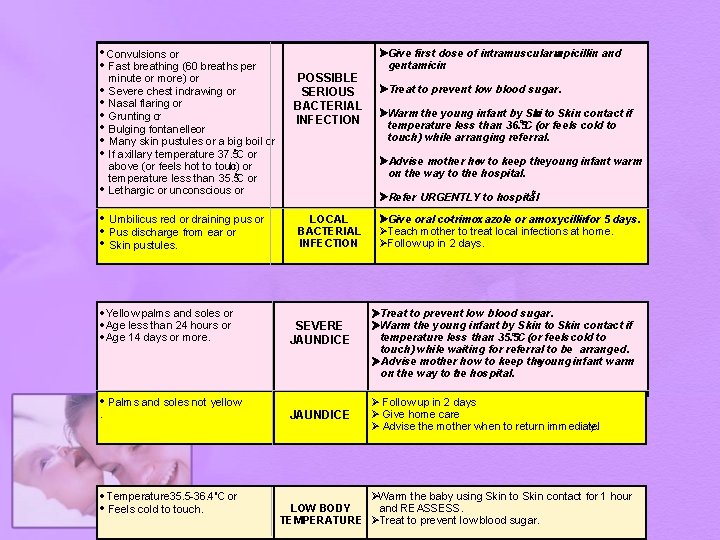
· Convulsions or · Fast breathing (60 breaths per minute or more) or · Severe chest indrawing or · Nasal flaring or · Grunting or · Bulging fontanelle or · Many skin pustules or a big boil or o · If axillary temperature 37. 5 C or above (or feels hot to touc h) or o temperature less than 35. 5 C or · Lethargic or unconscious or · Umbilicus red or draining pus or · Pus discharge from ear or · Skin pustules. · Yellow palms and soles or · Age less than 24 hours or · Age 14 days or more. POSSIBLE SERIOUS BACTERIAL INFECTION · Temperature 35. 5 -36. 4 o. C or · Feels cold to touch. Ø Treat to prevent low blood sugar. ØWarm the young infant by Ski n to Skin contact if o temperature less than 36. 5 C (or feels cold to touch) while arranging referral. Ø Advise mother how to keep theyoung infant warm on the way to the hospital. # Ø Refer URGENTLY to hospital LOCAL BACTERIAL INFECTION SEVERE JAUNDICE · Palms and soles not yellow . ØGive first dose of intramuscular mpicillin a and gentamicin. JAUNDICE ØGive oral co-trimoxazole or amoxycillinfor 5 days. ØTeach mother to treat local infections at home. ØFollow up in 2 days. ØTreat to prevent low blood sugar. ØWarm the young infant by Skin to Skin contact if o temperature less than 35. 5 C (or feels cold to touch) while waiting for referral to be arranged. Ø Advise mother how to keep theyoung infant warm on the way to h t e hospital. Ø Follow up in 2 days Ø Give home care Ø Advise the mother when to return immediatel y. ØWarm the baby using Skin to Skin contact for 1 hour LOW BODY and REASSESS. TEMPERATURE ØTreat to prevent low blood sugar.
