Neck Space Infections Dr Vishal Sharma Fascial layers


























- Slides: 99

Neck Space Infections Dr. Vishal Sharma
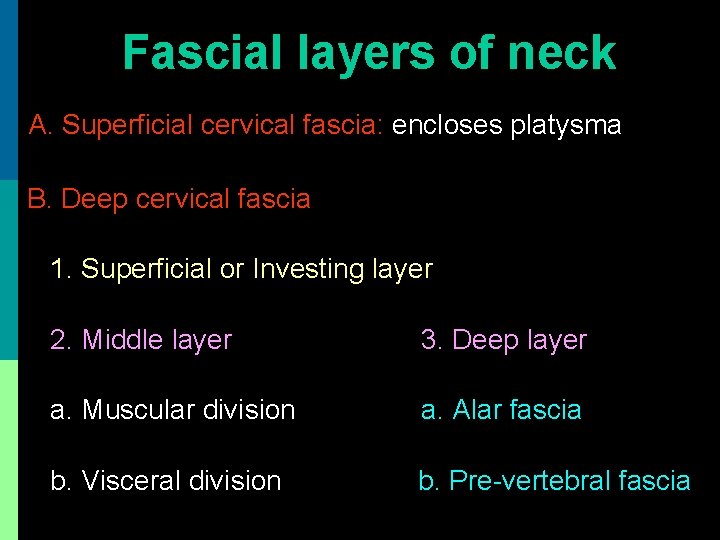
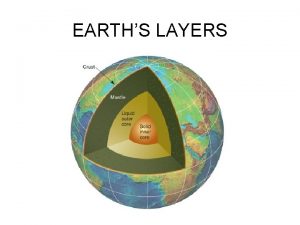
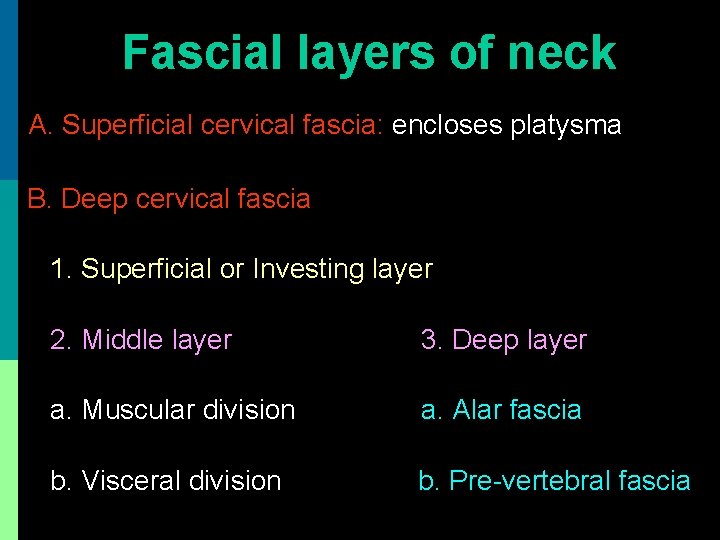
Fascial layers of neck A. Superficial cervical fascia: encloses platysma B. Deep cervical fascia 1. Superficial or Investing layer 2. Middle layer 3. Deep layer a. Muscular division a. Alar fascia b. Visceral division b. Pre-vertebral fascia
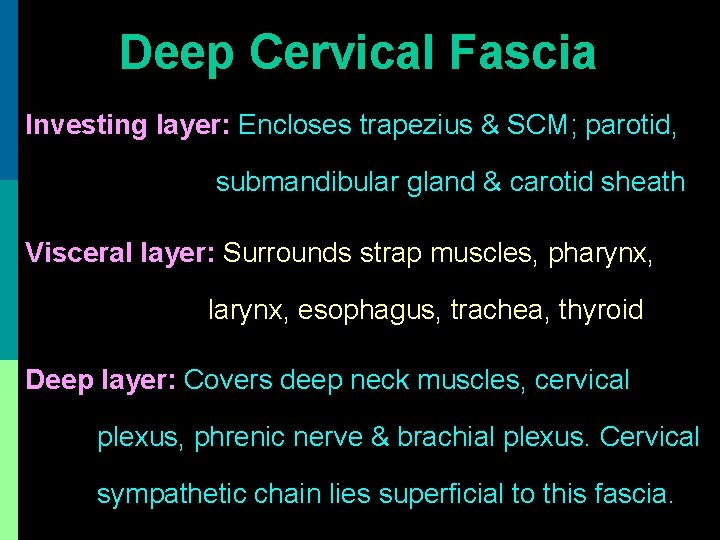
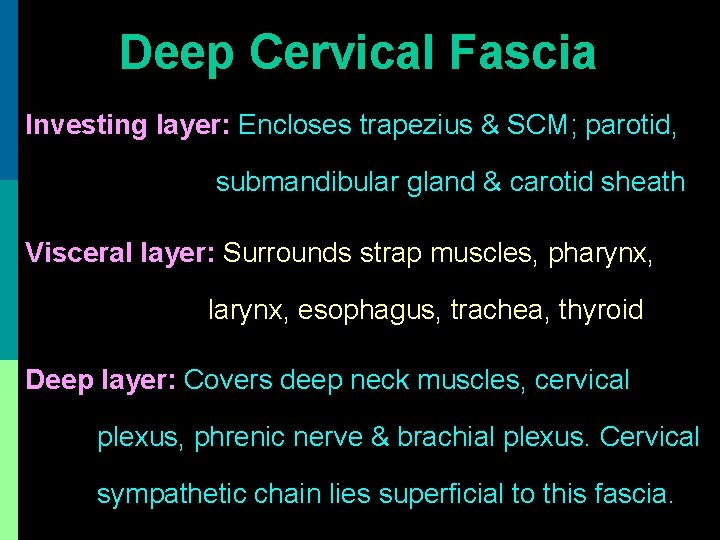
Deep Cervical Fascia Investing layer: Encloses trapezius & SCM; parotid, submandibular gland & carotid sheath Visceral layer: Surrounds strap muscles, pharynx, larynx, esophagus, trachea, thyroid Deep layer: Covers deep neck muscles, cervical plexus, phrenic nerve & brachial plexus. Cervical sympathetic chain lies superficial to this fascia.


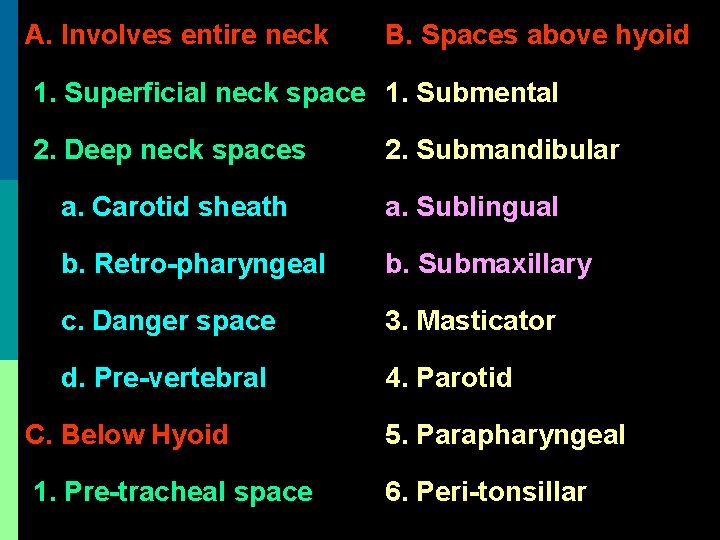
Classification of neck spaces
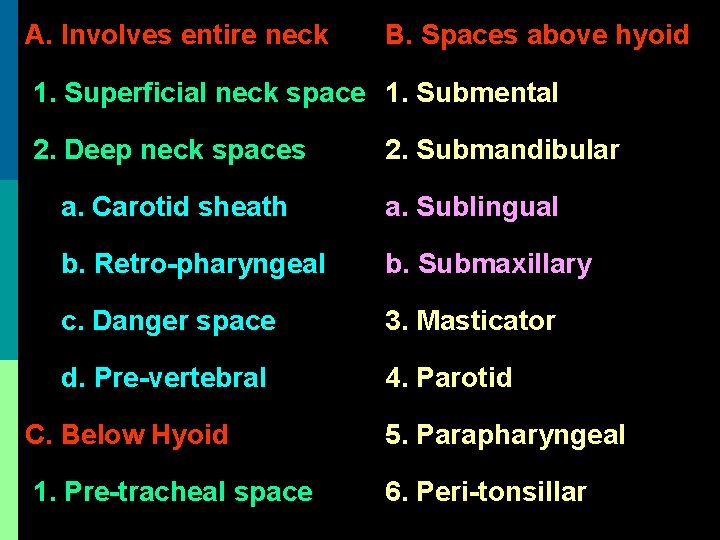
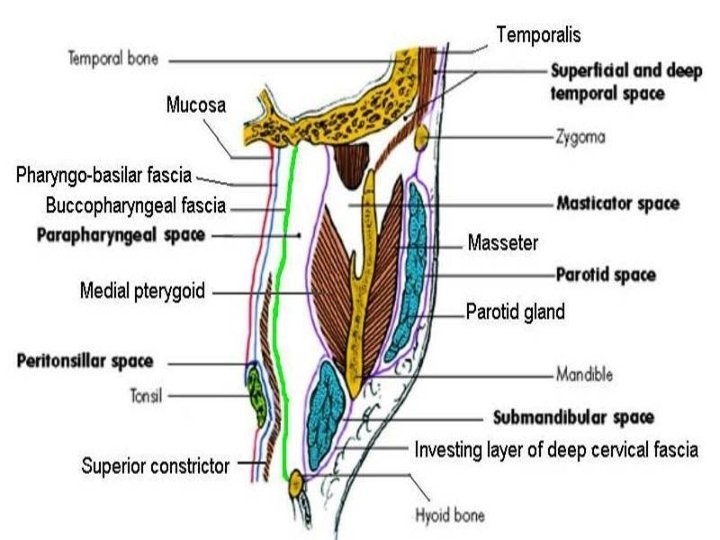
A. Involves entire neck B. Spaces above hyoid 1. Superficial neck space 1. Submental 2. Deep neck spaces 2. Submandibular a. Carotid sheath a. Sublingual b. Retro-pharyngeal b. Submaxillary c. Danger space 3. Masticator d. Pre-vertebral 4. Parotid C. Below Hyoid 5. Parapharyngeal 1. Pre-tracheal space 6. Peri-tonsillar



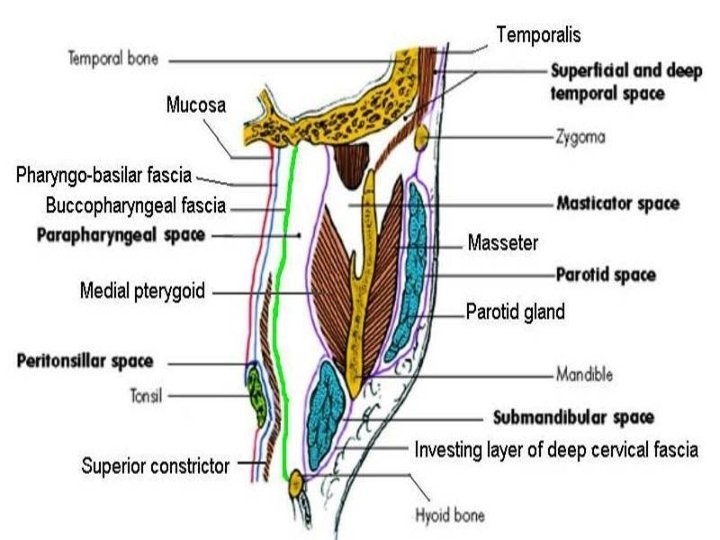
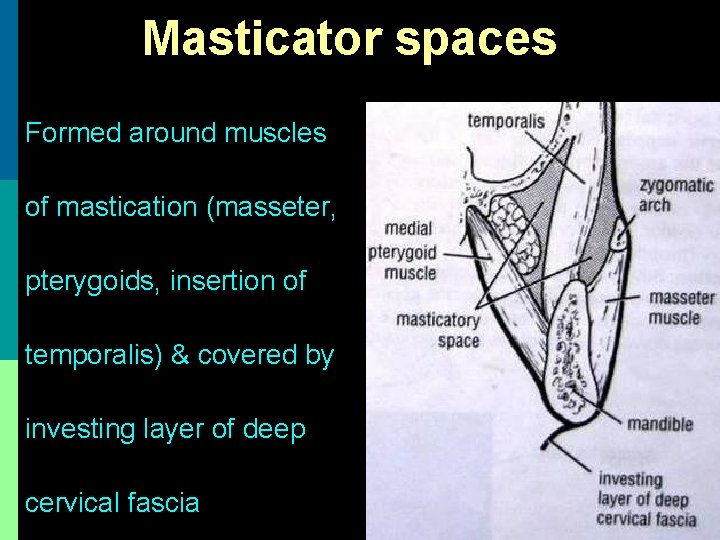
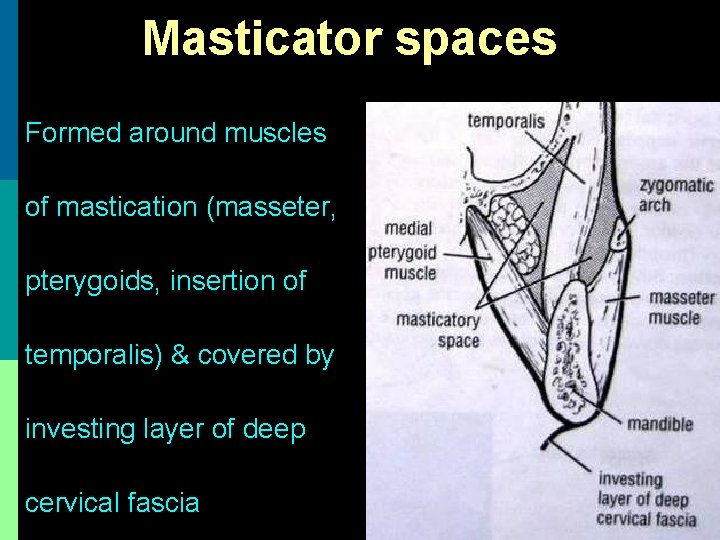
Masticator spaces Formed around muscles of mastication (masseter, pterygoids, insertion of temporalis) & covered by investing layer of deep cervical fascia
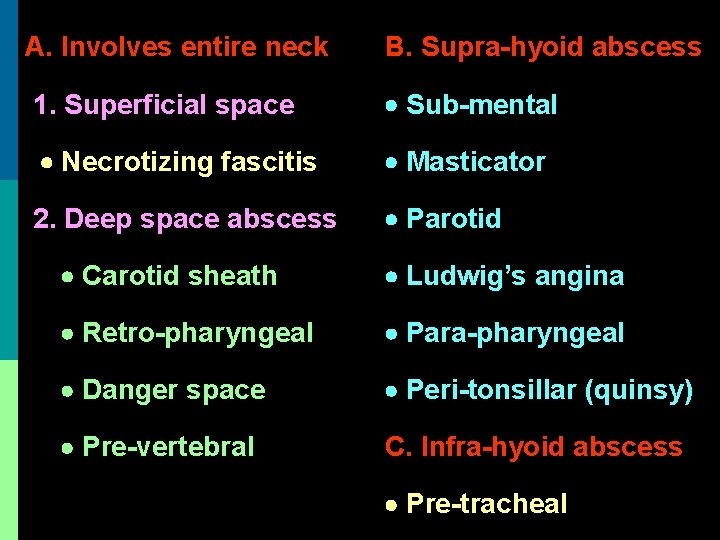
Classification of neck space infections
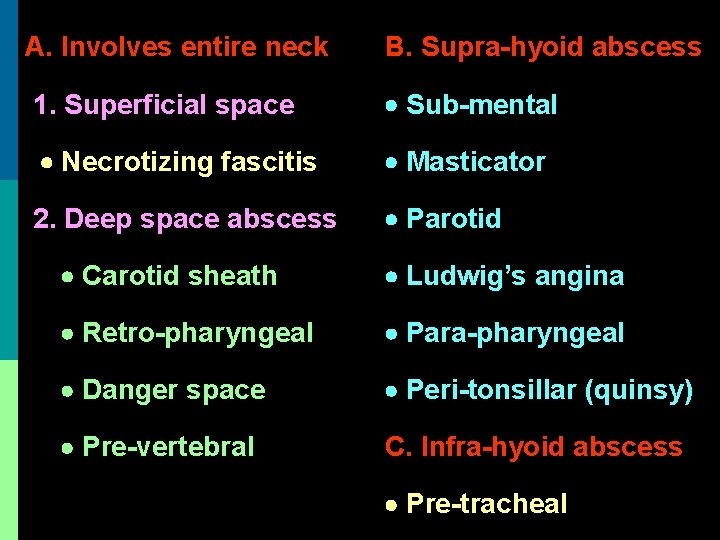
A. Involves entire neck B. Supra-hyoid abscess 1. Superficial space Sub-mental Necrotizing fascitis Masticator 2. Deep space abscess Parotid Carotid sheath Ludwig’s angina Retro-pharyngeal Para-pharyngeal Danger space Peri-tonsillar (quinsy) Pre-vertebral C. Infra-hyoid abscess Pre-tracheal
Necrotizing fasciitis
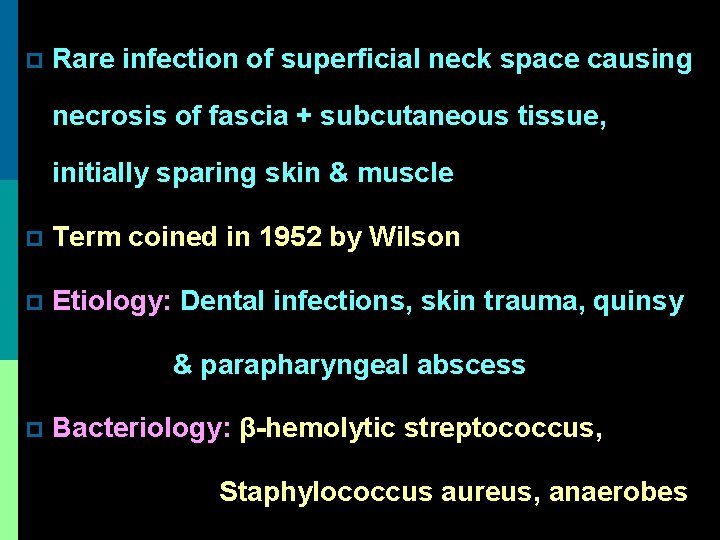
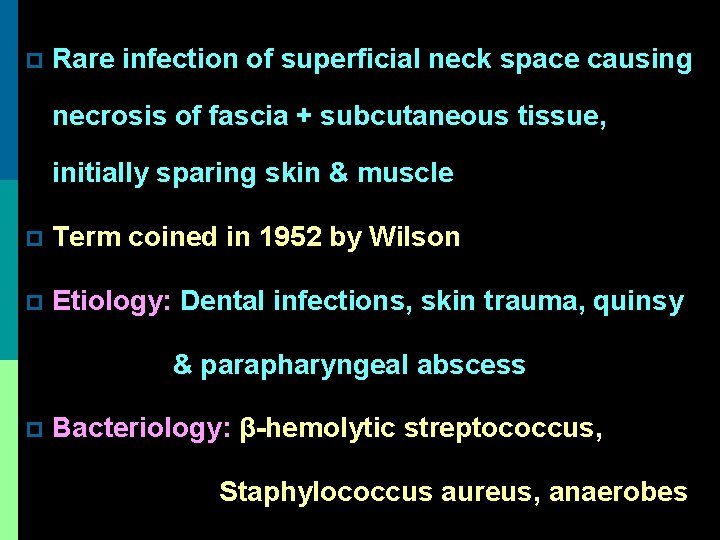
p Rare infection of superficial neck space causing necrosis of fascia + subcutaneous tissue, initially sparing skin & muscle p Term coined in 1952 by Wilson p Etiology: Dental infections, skin trauma, quinsy & parapharyngeal abscess p Bacteriology: β-hemolytic streptococcus, Staphylococcus aureus, anaerobes
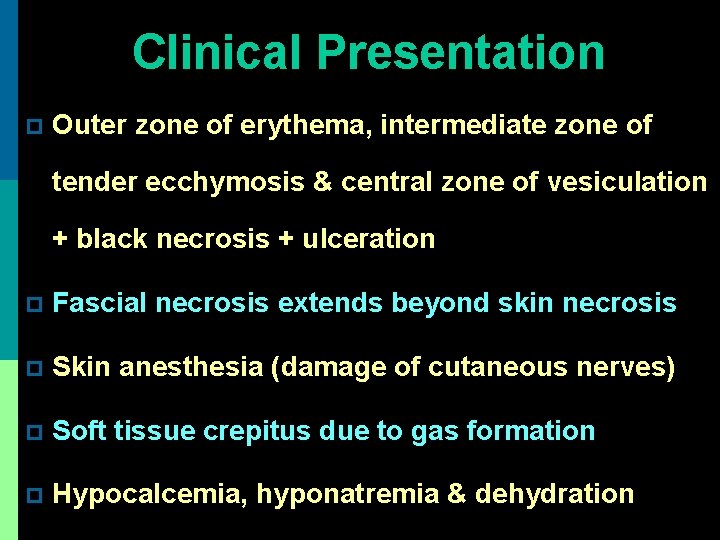
Clinical Presentation p Outer zone of erythema, intermediate zone of tender ecchymosis & central zone of vesiculation + black necrosis + ulceration p Fascial necrosis extends beyond skin necrosis p Skin anesthesia (damage of cutaneous nerves) p Soft tissue crepitus due to gas formation p Hypocalcemia, hyponatremia & dehydration

Necrotizing fasciitis of chest
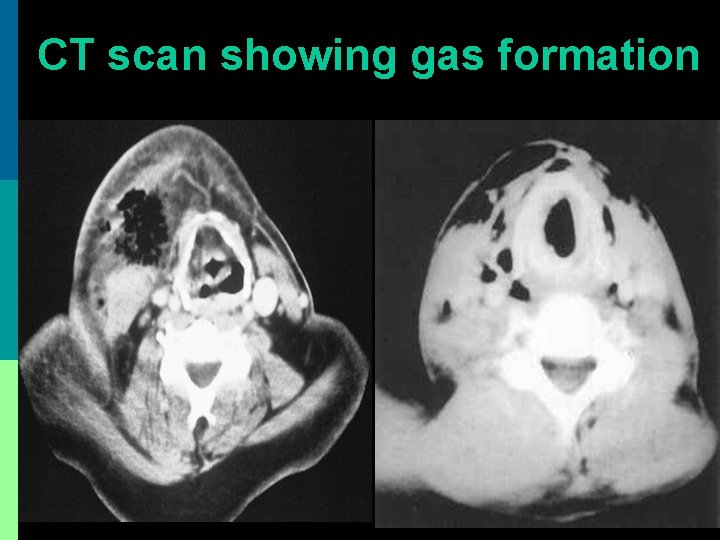
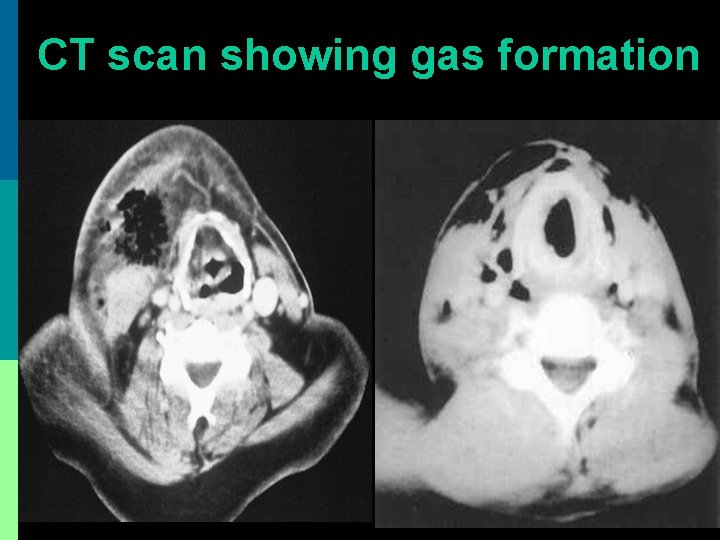
CT scan showing gas formation
Treatment p Early correction of fluid & electrolyte imbalance p I. V. Ampicillin + Gentamicin + Clindamycin p Immediate radical debridement of necrotic tissue (in presence of subcutaneous air, progressive infection despite 48 hours of medical therapy, obvious fluctuation or skin necrosis) p Skin grafting after debridement

Wound debridement

Skin grafting

Healed wound
p Poor prognostic factors: Diabetes mellitus, atherosclerosis, chronic renal failure, obesity, immuno-suppression, malnutrition p Complications: necrosis of chest wall fascia, mediastinitis, pleural effusion, pericardial effusion, empyema, airway obstruction, arterial erosion, jugular vein thrombophlebitis, septic shock, lung abscess, carotid artery thrombosis
Ludwig’s Angina
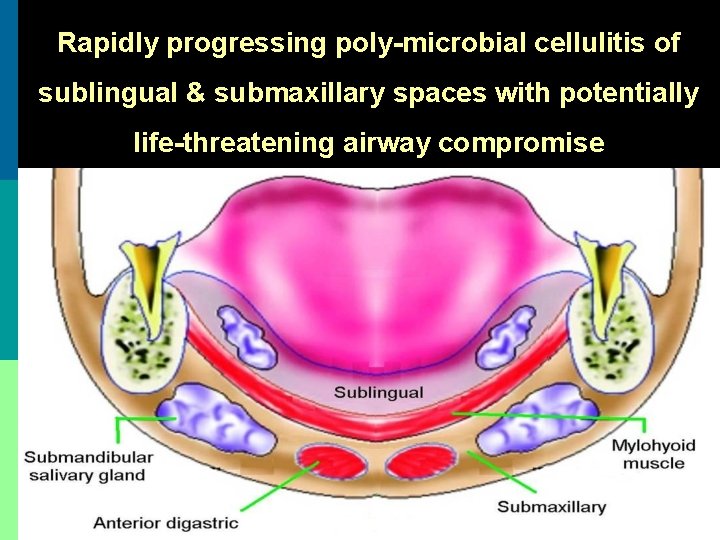
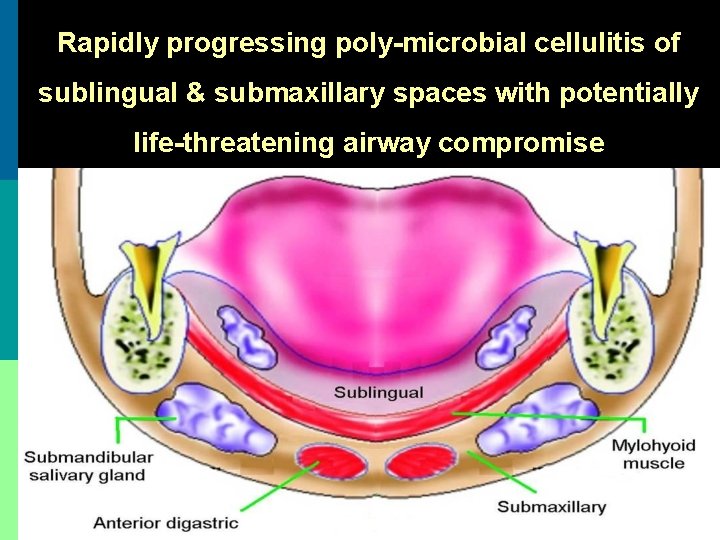
Rapidly progressing poly-microbial cellulitis of sublingual & submaxillary spaces with potentially life-threatening airway compromise
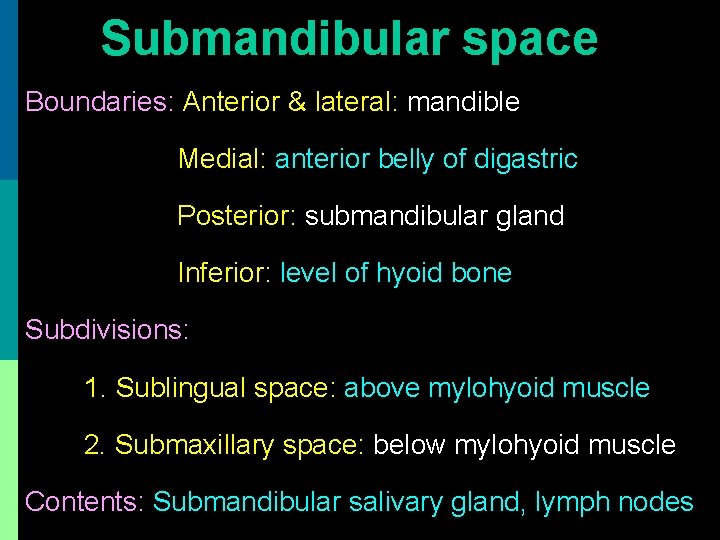
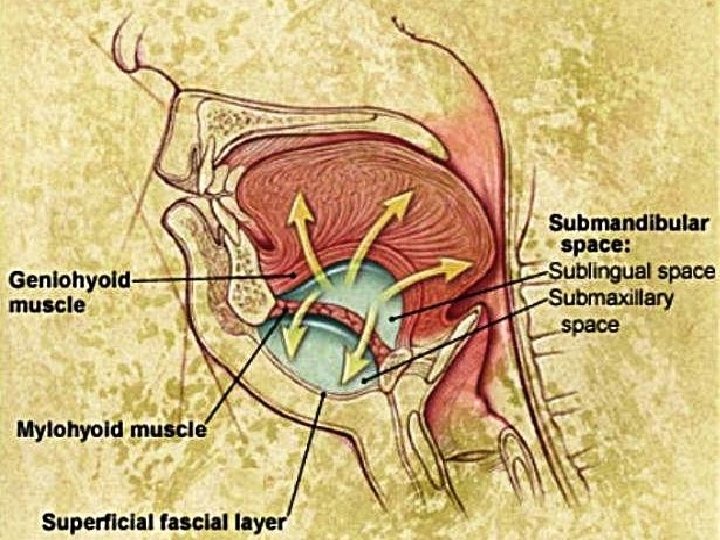
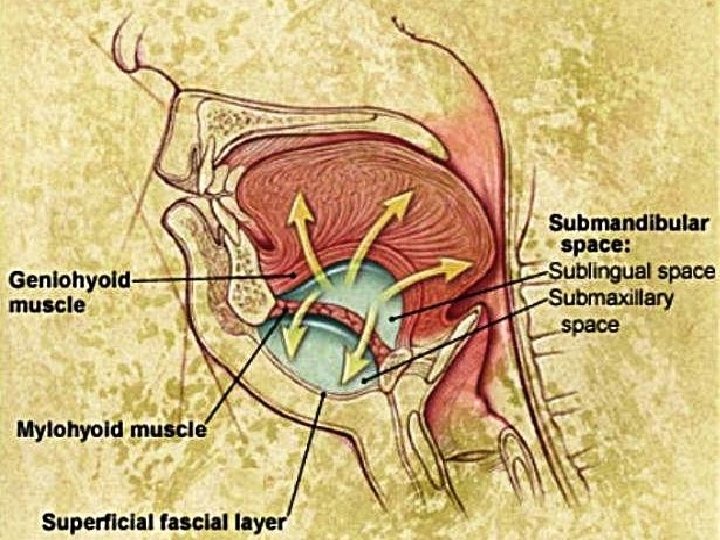
Submandibular space Boundaries: Anterior & lateral: mandible Medial: anterior belly of digastric Posterior: submandibular gland Inferior: level of hyoid bone Subdivisions: 1. Sublingual space: above mylohyoid muscle 2. Submaxillary space: below mylohyoid muscle Contents: Submandibular salivary gland, lymph nodes
Etiology of Ludwig’s angina
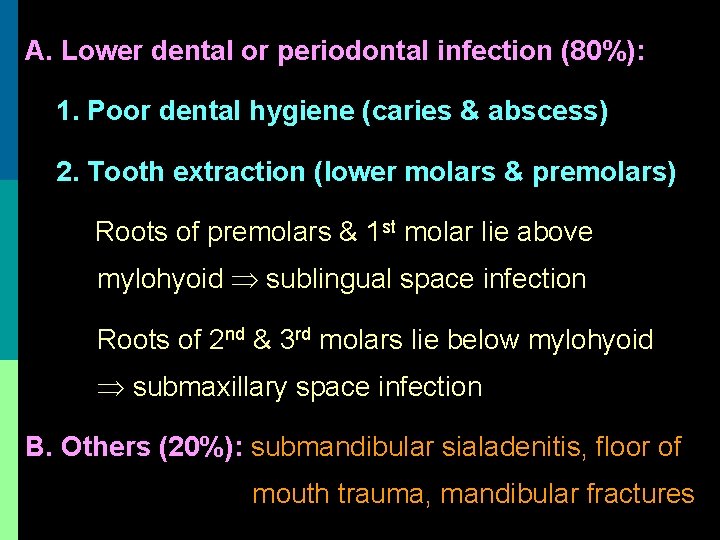
A. Lower dental or periodontal infection (80%): 1. Poor dental hygiene (caries & abscess) 2. Tooth extraction (lower molars & premolars) Roots of premolars & 1 st molar lie above mylohyoid sublingual space infection Roots of 2 nd & 3 rd molars lie below mylohyoid submaxillary space infection B. Others (20%): submandibular sialadenitis, floor of mouth trauma, mandibular fractures


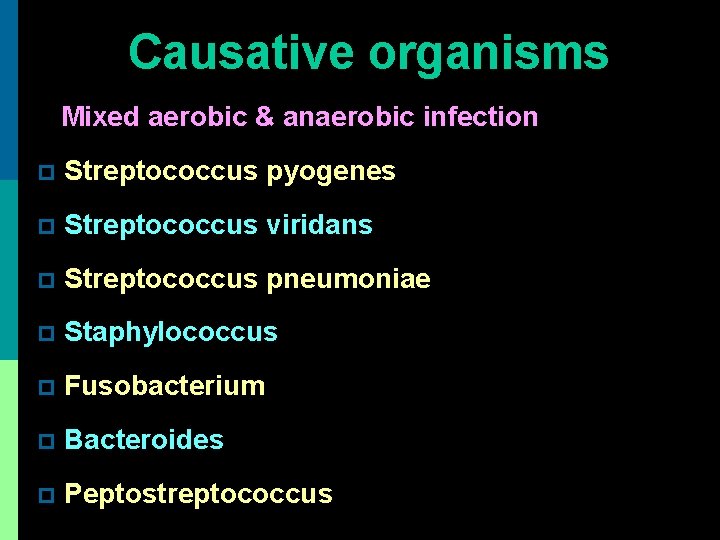
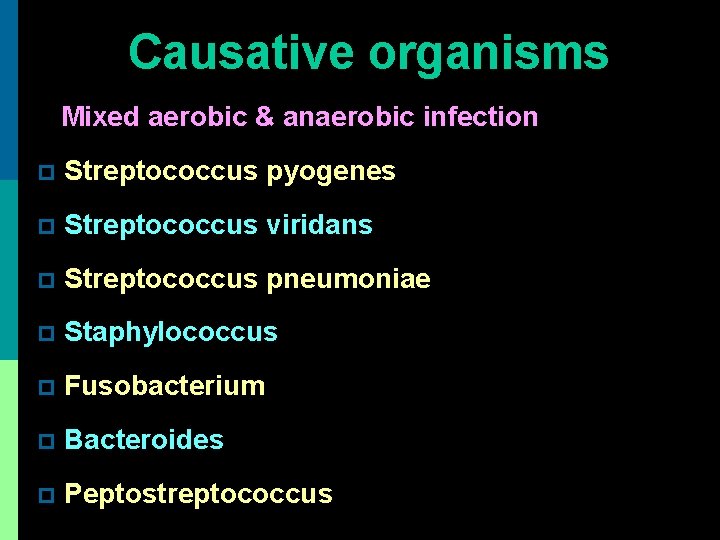
Causative organisms Mixed aerobic & anaerobic infection p Streptococcus pyogenes p Streptococcus viridans p Streptococcus pneumoniae p Staphylococcus p Fusobacterium p Bacteroides p Peptostreptococcus
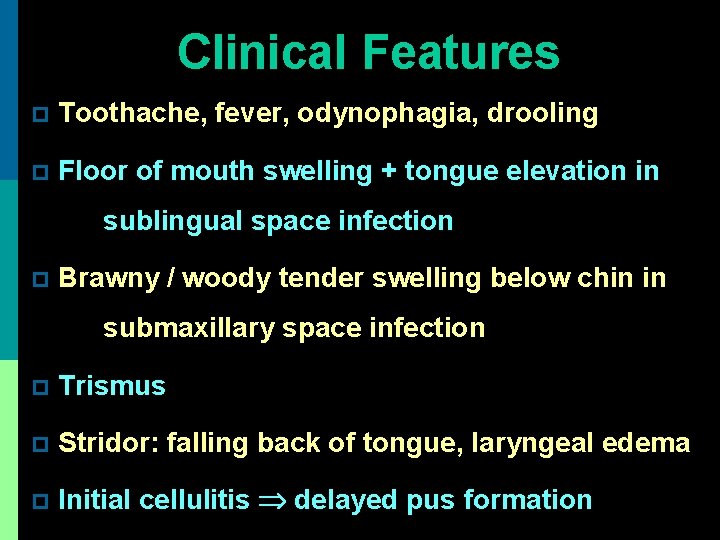
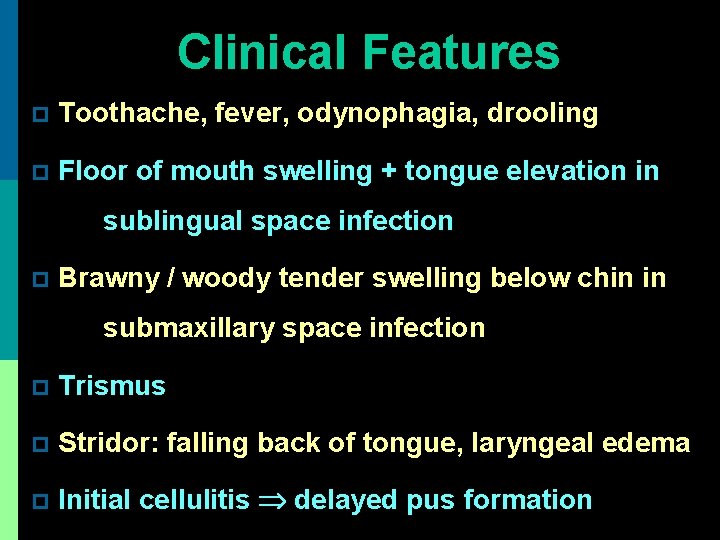
Clinical Features p Toothache, fever, odynophagia, drooling p Floor of mouth swelling + tongue elevation in sublingual space infection p Brawny / woody tender swelling below chin in submaxillary space infection p Trismus p Stridor: falling back of tongue, laryngeal edema p Initial cellulitis delayed pus formation
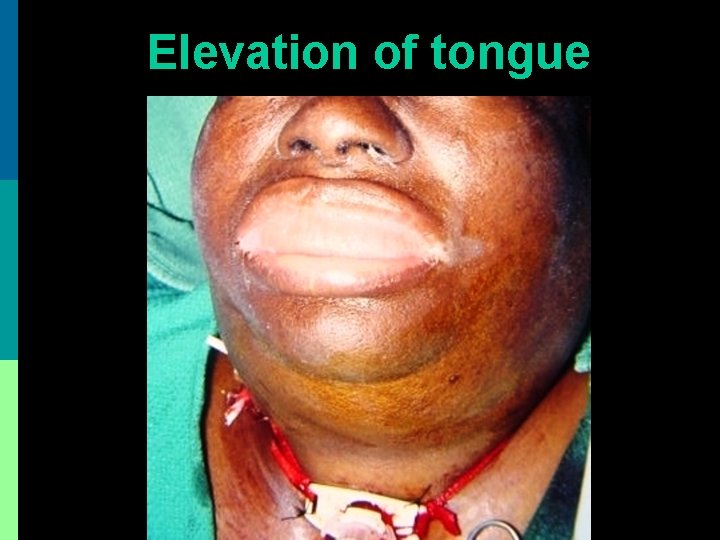
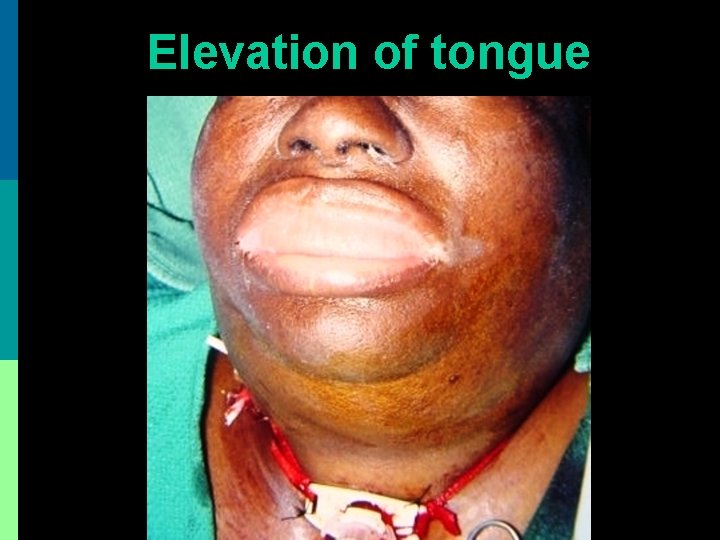
Elevation of tongue

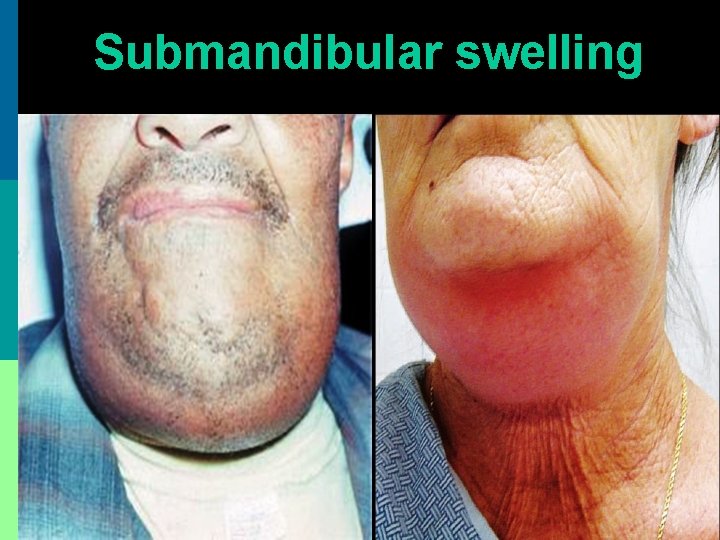
Submandibular swelling
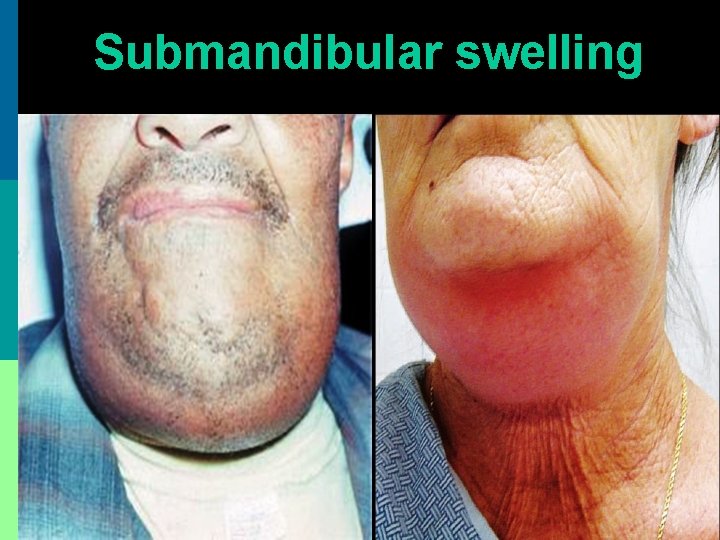
Submandibular swelling
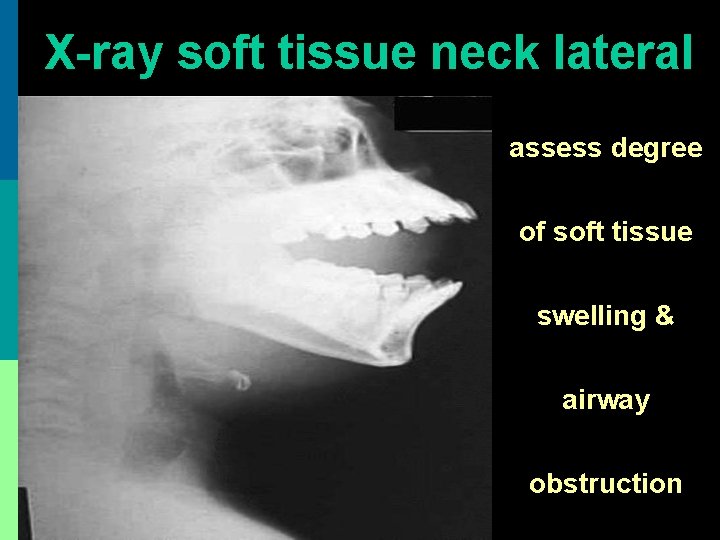
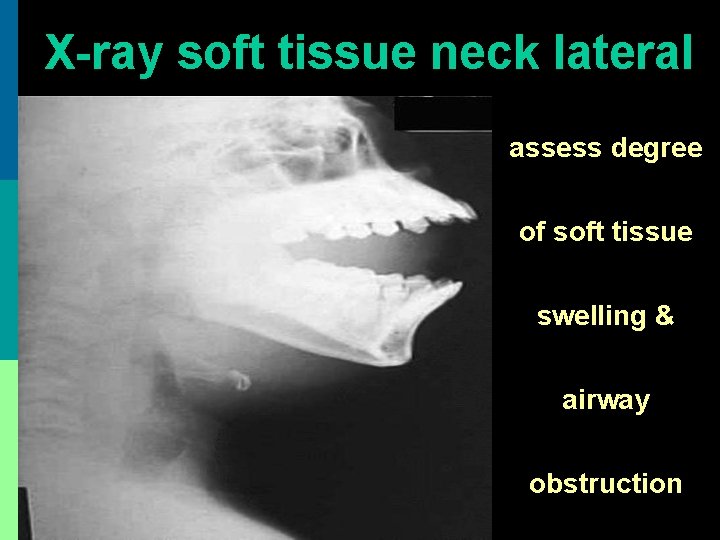
X-ray soft tissue neck lateral assess degree of soft tissue swelling & airway obstruction
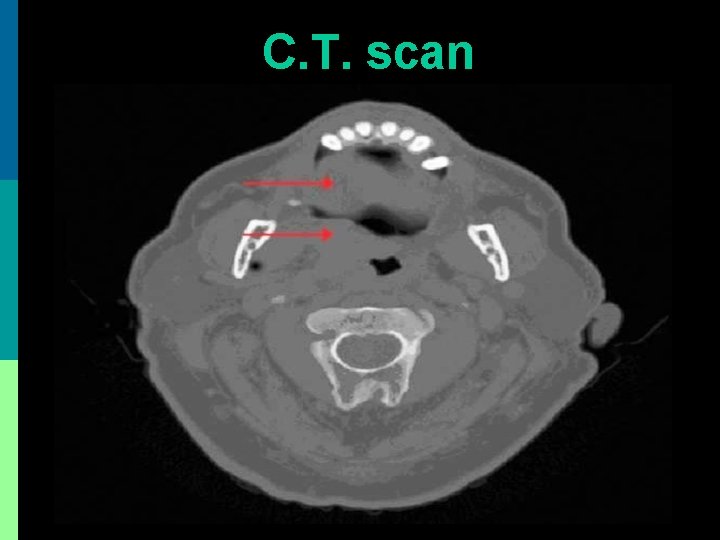
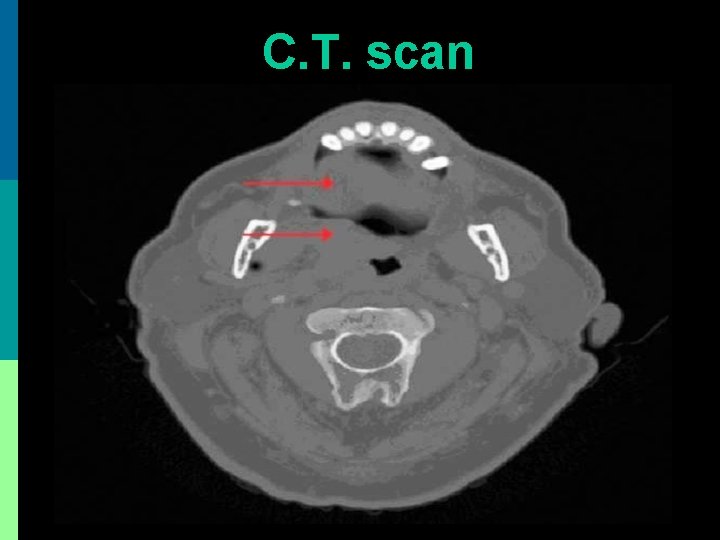
C. T. scan

Treatment of Ludwig’s angina
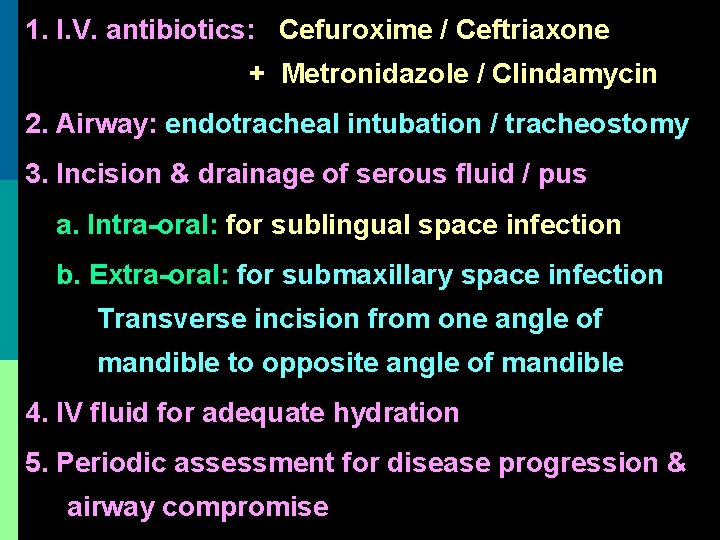
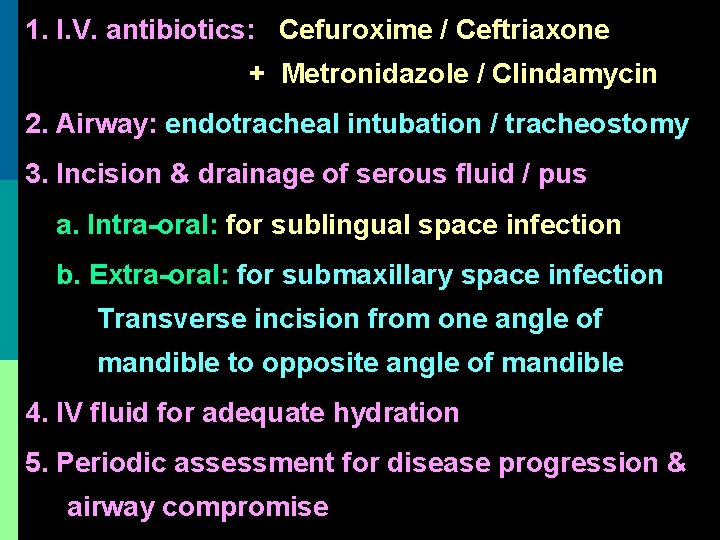
1. I. V. antibiotics: Cefuroxime / Ceftriaxone + Metronidazole / Clindamycin 2. Airway: endotracheal intubation / tracheostomy 3. Incision & drainage of serous fluid / pus a. Intra-oral: for sublingual space infection b. Extra-oral: for submaxillary space infection Transverse incision from one angle of mandible to opposite angle of mandible 4. IV fluid for adequate hydration 5. Periodic assessment for disease progression & airway compromise

Incision drainage + Tracheostomy

Incision drainage + Tracheostomy
Complications p Parapharyngeal abscess p Retropharyngeal abscess p Acute airway obstruction (within hours): due to pushing back of tongue, laryngeal edema p Aspiration pneumonia p Septicemia p Death
Retropharyngeal abscess
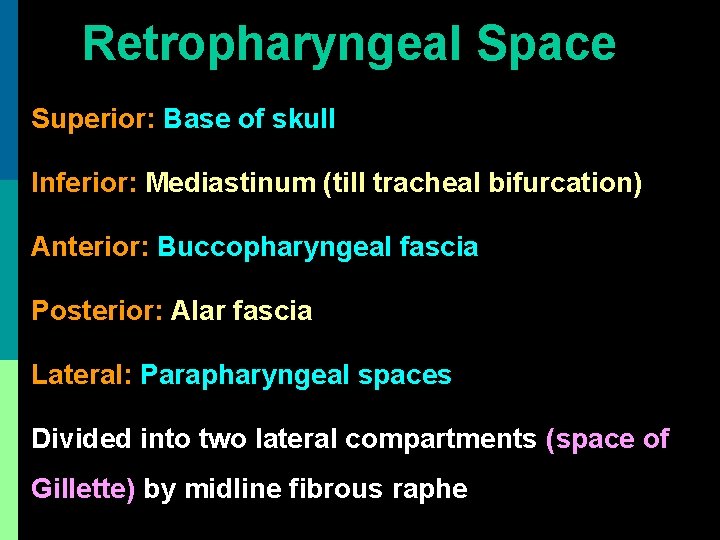
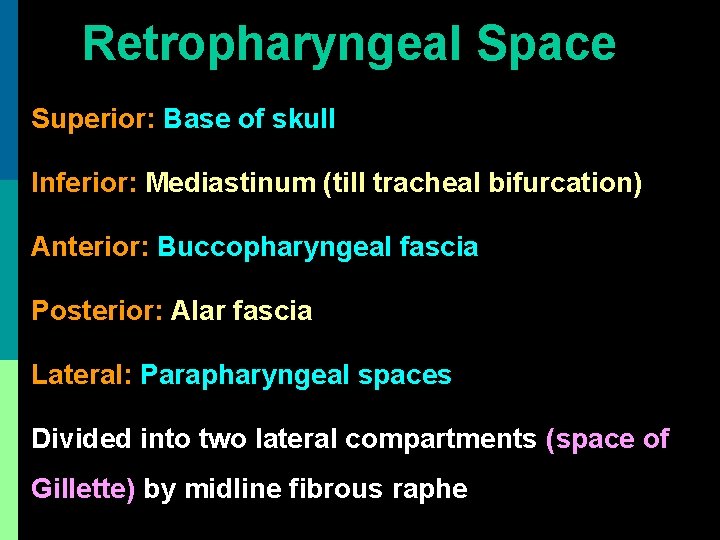
Retropharyngeal Space Superior: Base of skull Inferior: Mediastinum (till tracheal bifurcation) Anterior: Buccopharyngeal fascia Posterior: Alar fascia Lateral: Parapharyngeal spaces Divided into two lateral compartments (space of Gillette) by midline fibrous raphe

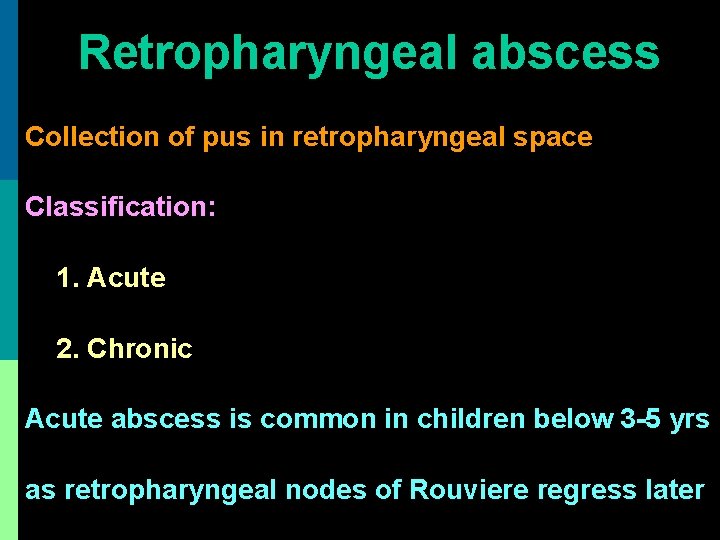
Retropharyngeal abscess Collection of pus in retropharyngeal space Classification: 1. Acute 2. Chronic Acute abscess is common in children below 3 -5 yrs as retropharyngeal nodes of Rouviere regress later

Acute Retropharyngeal Abscess
Etiology p Suppuration of retropharyngeal lymph node of Rouviere from upper respiratory tract infection p Penetrating injury of posterior pharyngeal wall (e. g. . fish bone, vertebral fracture) p Following endoscopic trauma to pharynx p Acute mastoitis: pus tracking under petrous bone
Symptoms p H/o upper respiratory tract infection p Dysphagia / odynophagia p Difficulty in breathing p Croupy cough p Hot potato voice p Neck stiffness

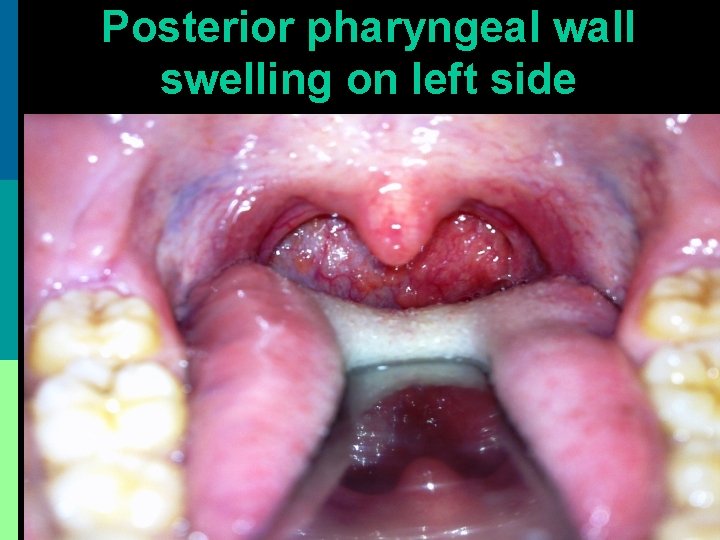
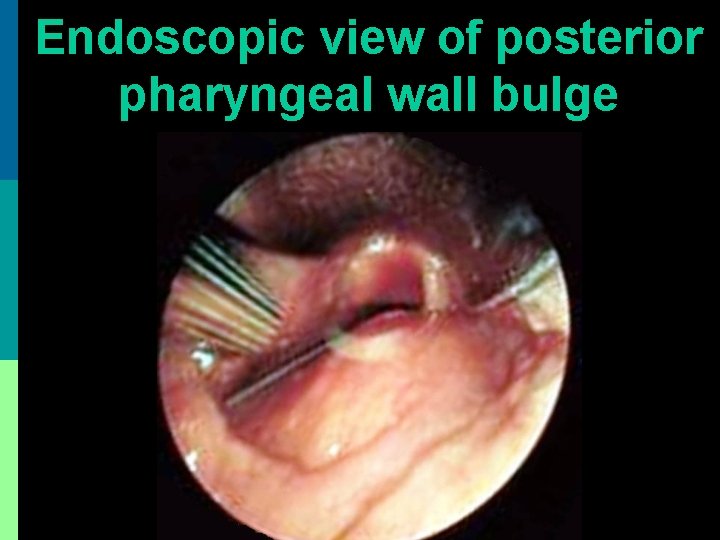
Signs p Febrile, ill-looking, child with drooling p Tender neck swelling + fistula p Torticollis (twisted neck) on side of abscess followed by hyperextension of neck p U/L bulge on posterior pharyngeal wall
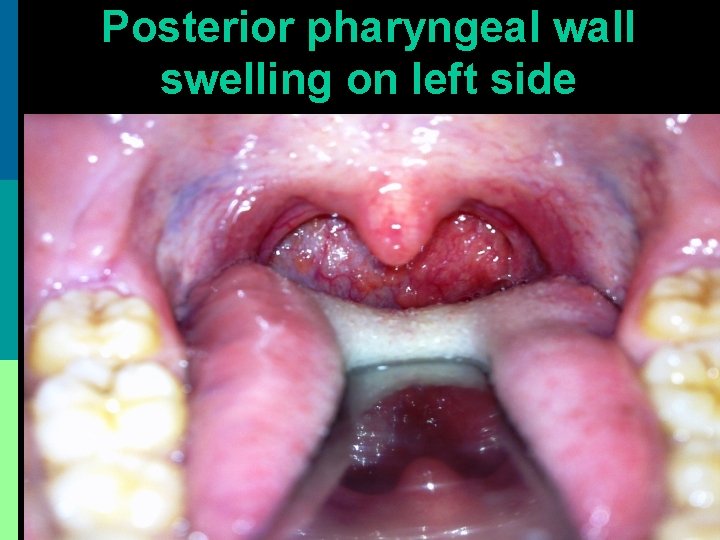
Posterior pharyngeal wall swelling on left side
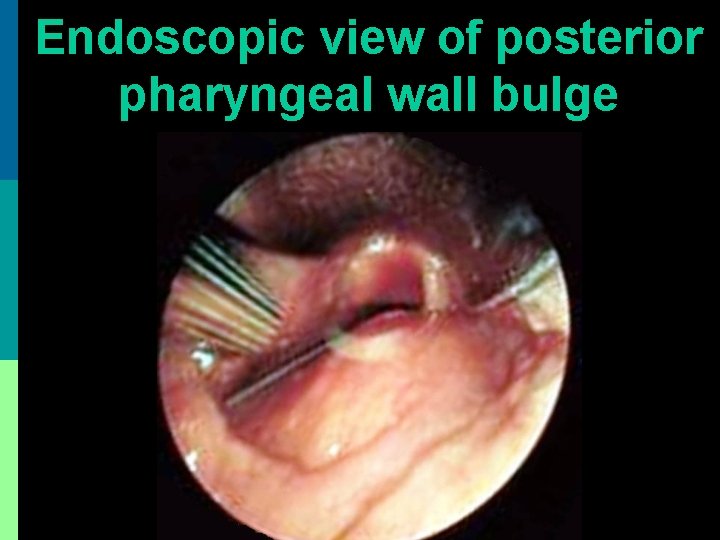
Endoscopic view of posterior pharyngeal wall bulge
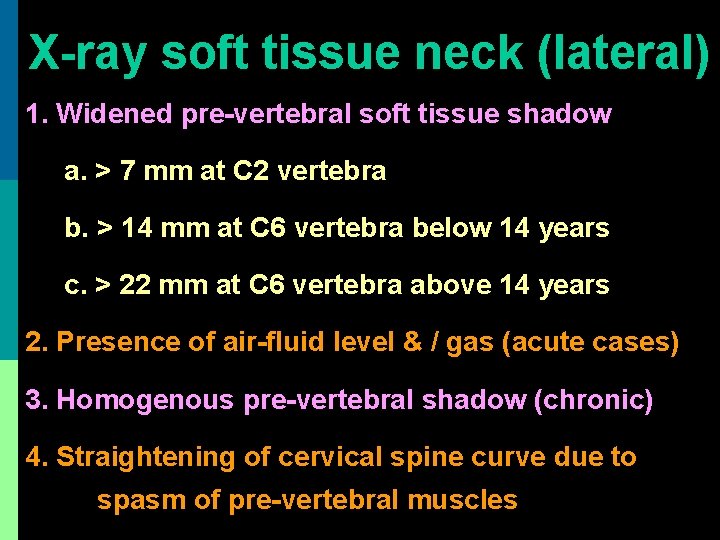
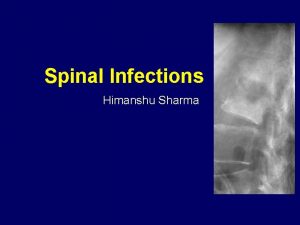
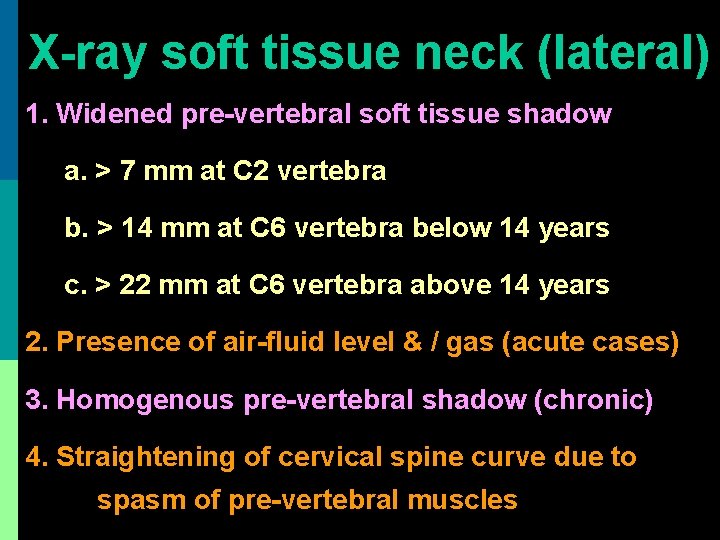
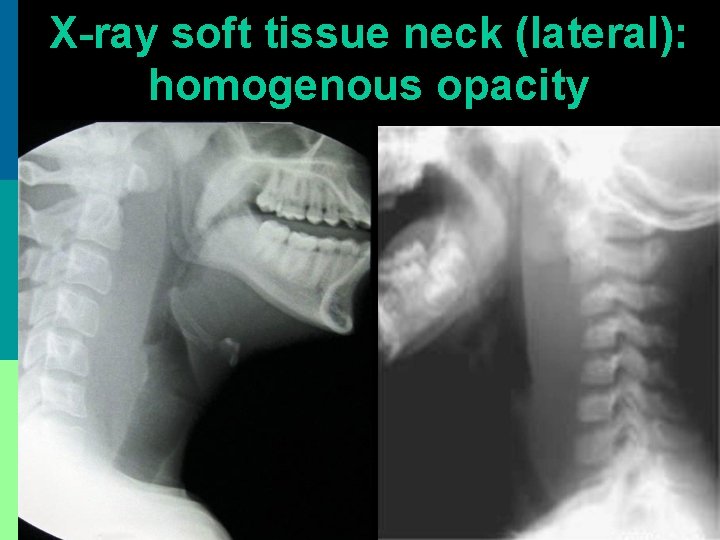
X-ray soft tissue neck (lateral) 1. Widened pre-vertebral soft tissue shadow a. > 7 mm at C 2 vertebra b. > 14 mm at C 6 vertebra below 14 years c. > 22 mm at C 6 vertebra above 14 years 2. Presence of air-fluid level & / gas (acute cases) 3. Homogenous pre-vertebral shadow (chronic) 4. Straightening of cervical spine curve due to spasm of pre-vertebral muscles
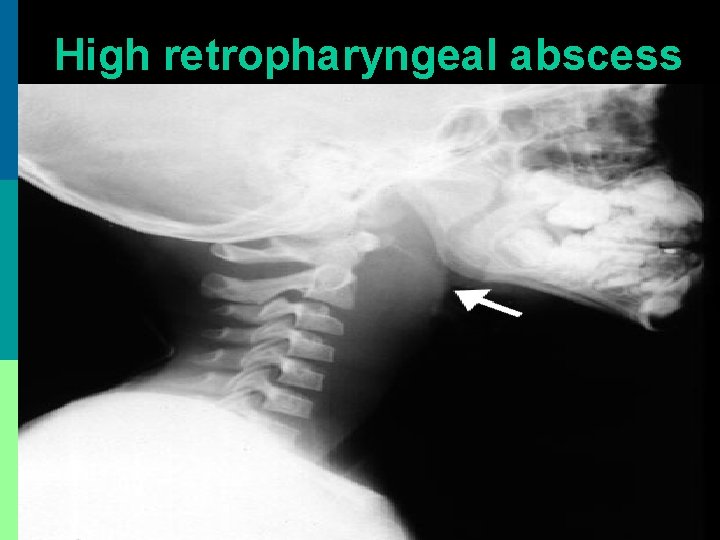
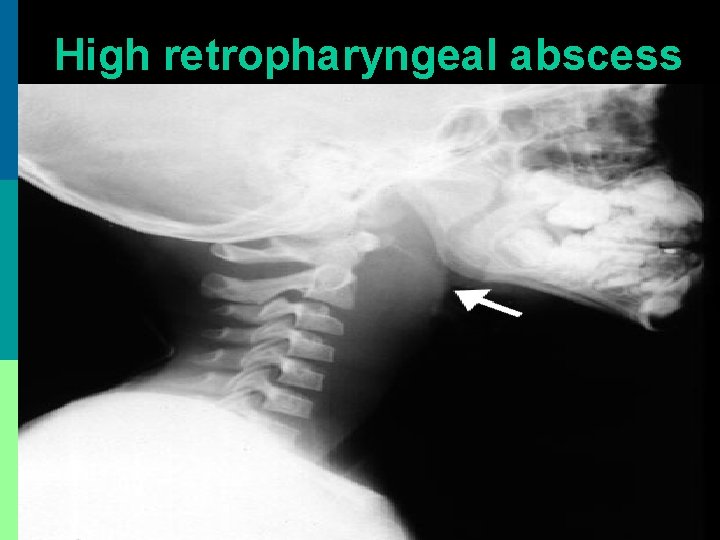
High retropharyngeal abscess
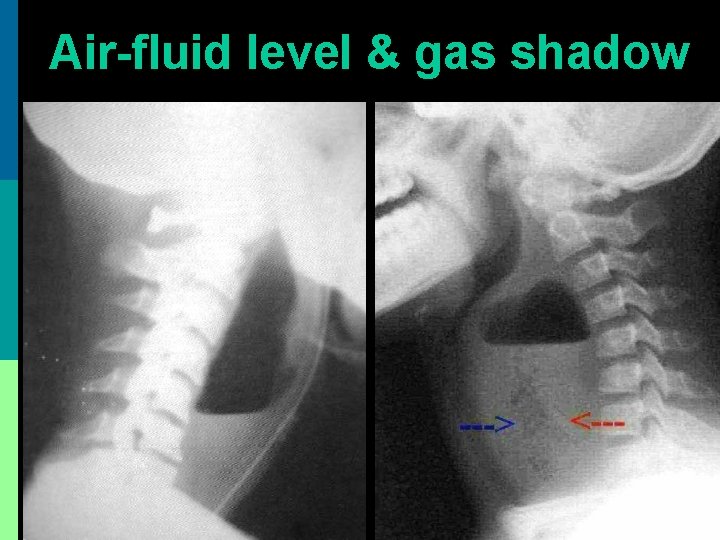
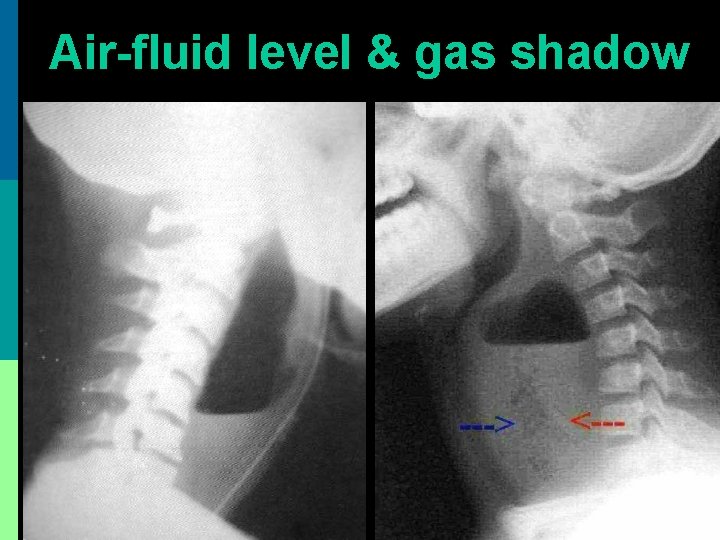
Air-fluid level & gas shadow
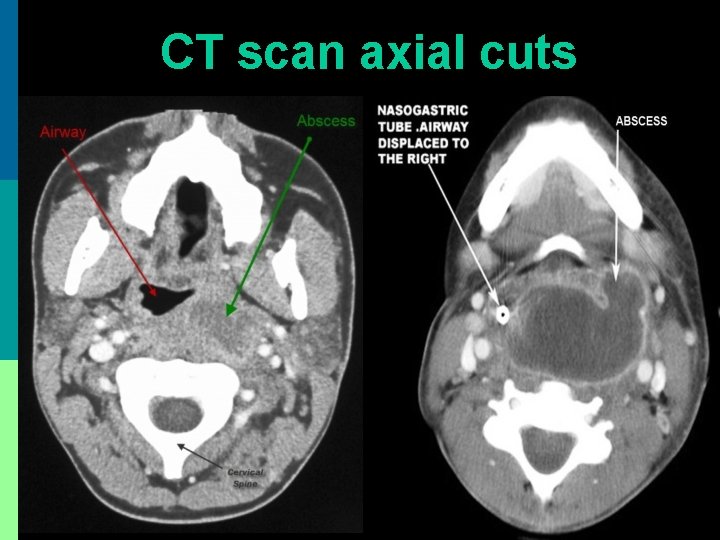
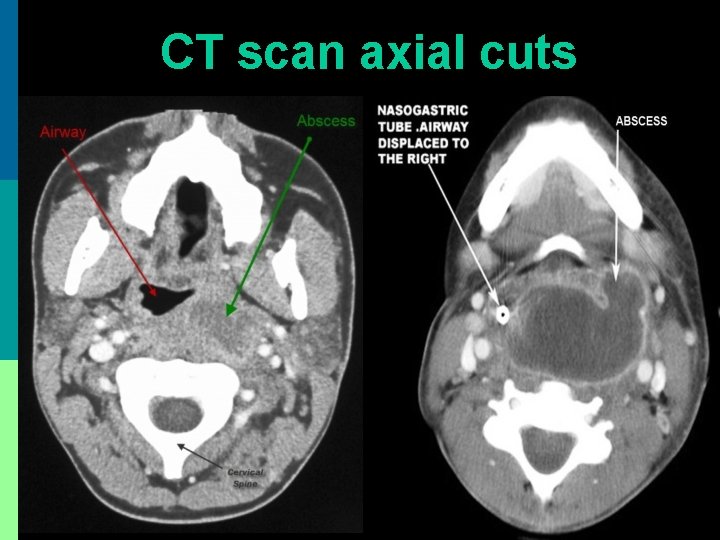
CT scan axial cuts
Treatment 1. IV antibiotics: Ceftriaxone + Metronidazole 2. Incision & drainage: p No anesthesia (as it may rupture abscess) or very careful endotracheal intubation p Supine with head hanging low from table p Vertical or horizontal incision on fluctuant area p Incision + immediate suction of pus 3. Tracheostomy for airway obstruction
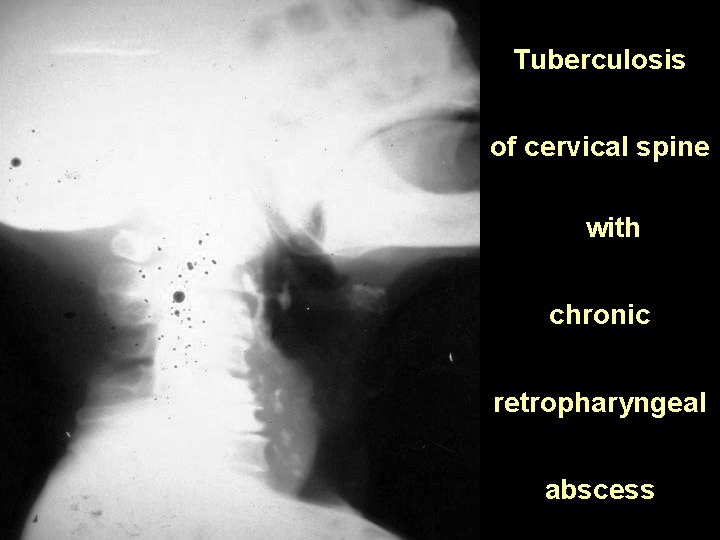
Chronic Retropharyngeal Abscess
Etiology p Caries of cervical spine: presents as central posterior pharyngeal wall swelling p Tubercular infection of retropharyngeal lymph nodes from infected deep cervical nodes: presents as lateral posterior pharyngeal wall swelling true retropharyngeal abscess p Post traumatic: vertebral fracture p Spread from parapharyngeal abscess
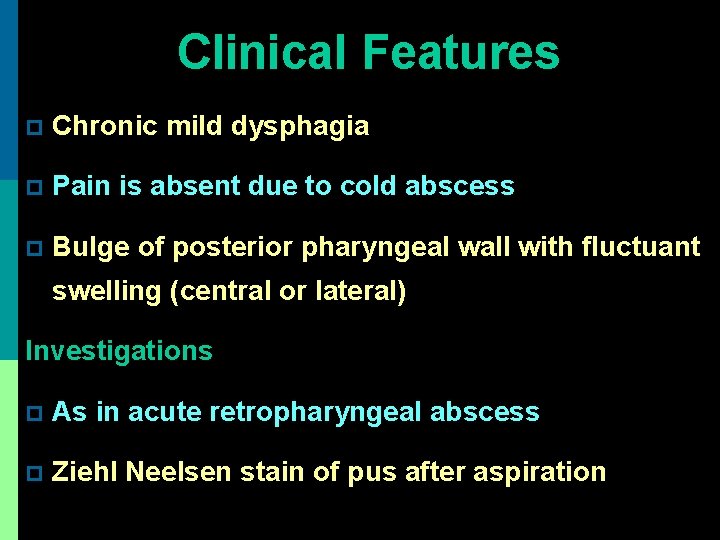
Clinical Features p Chronic mild dysphagia p Pain is absent due to cold abscess p Bulge of posterior pharyngeal wall with fluctuant swelling (central or lateral) Investigations p As in acute retropharyngeal abscess p Ziehl Neelsen stain of pus after aspiration
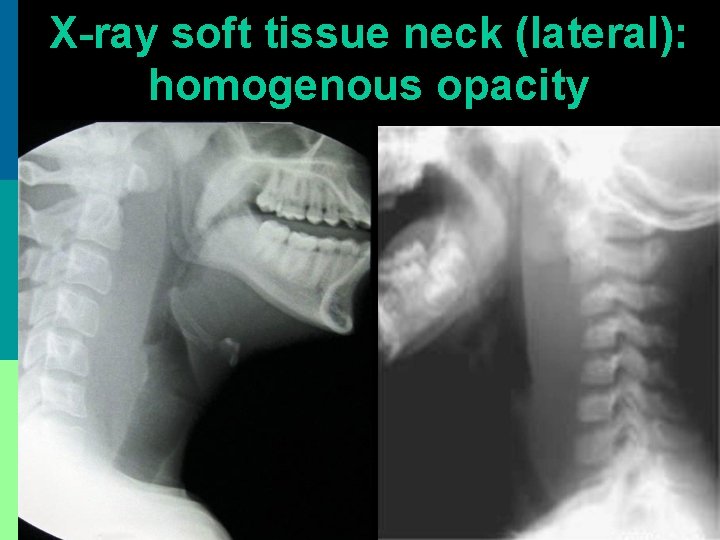
X-ray soft tissue neck (lateral): homogenous opacity
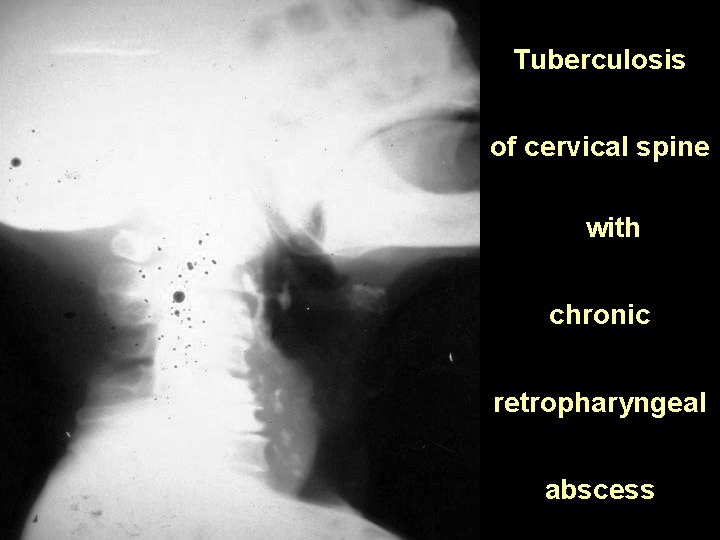
Tuberculosis of cervical spine with chronic retropharyngeal abscess
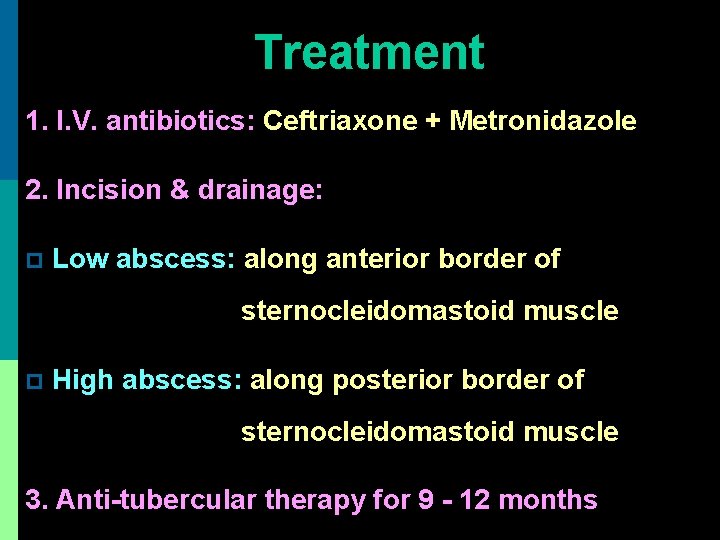
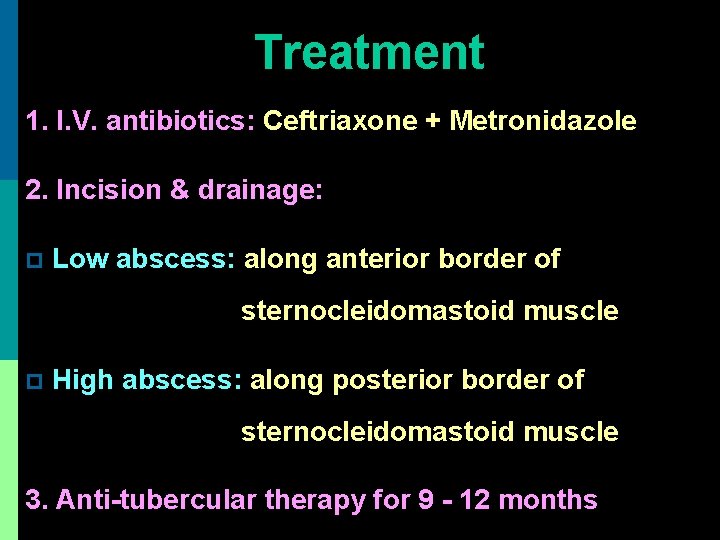
Treatment 1. I. V. antibiotics: Ceftriaxone + Metronidazole 2. Incision & drainage: p Low abscess: along anterior border of sternocleidomastoid muscle p High abscess: along posterior border of sternocleidomastoid muscle 3. Anti-tubercular therapy for 9 - 12 months
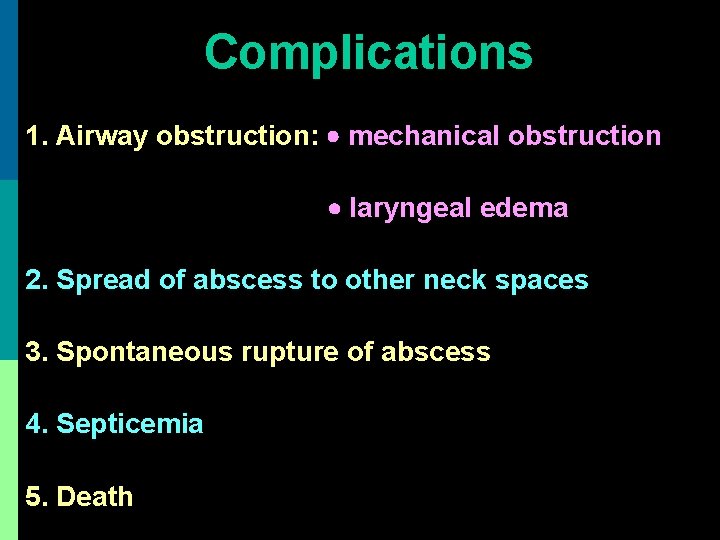
Complications 1. Airway obstruction: mechanical obstruction laryngeal edema 2. Spread of abscess to other neck spaces 3. Spontaneous rupture of abscess 4. Septicemia 5. Death
Parapharyngeal abscess
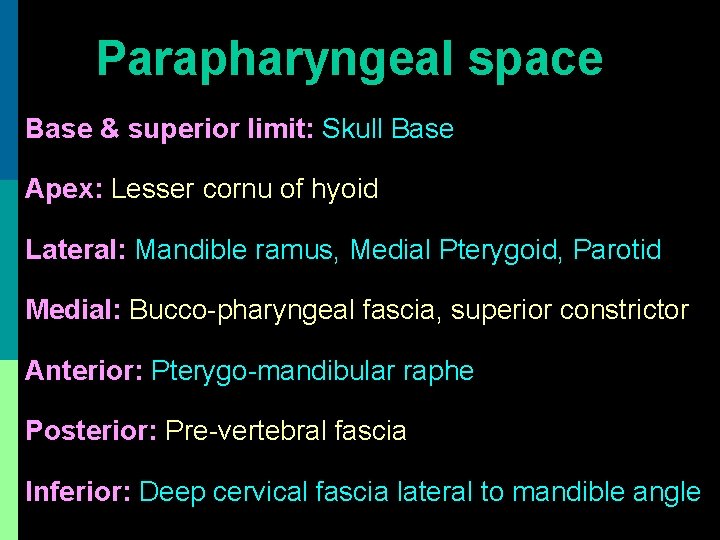
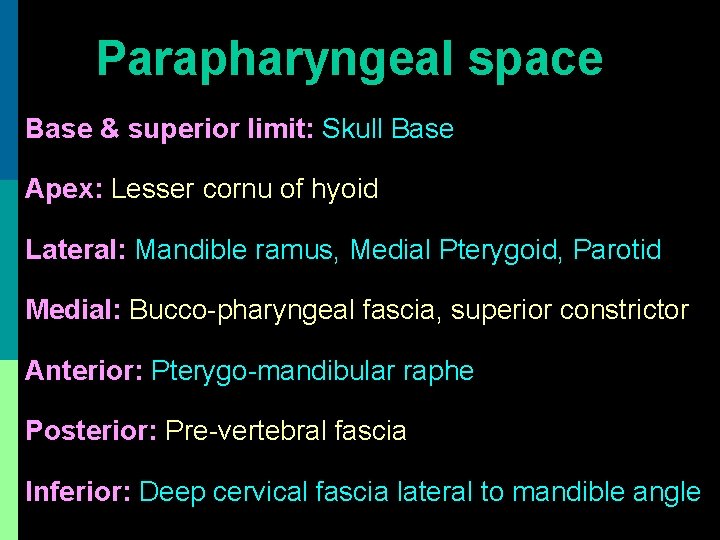
Parapharyngeal space Base & superior limit: Skull Base Apex: Lesser cornu of hyoid Lateral: Mandible ramus, Medial Pterygoid, Parotid Medial: Bucco-pharyngeal fascia, superior constrictor Anterior: Pterygo-mandibular raphe Posterior: Pre-vertebral fascia Inferior: Deep cervical fascia lateral to mandible angle


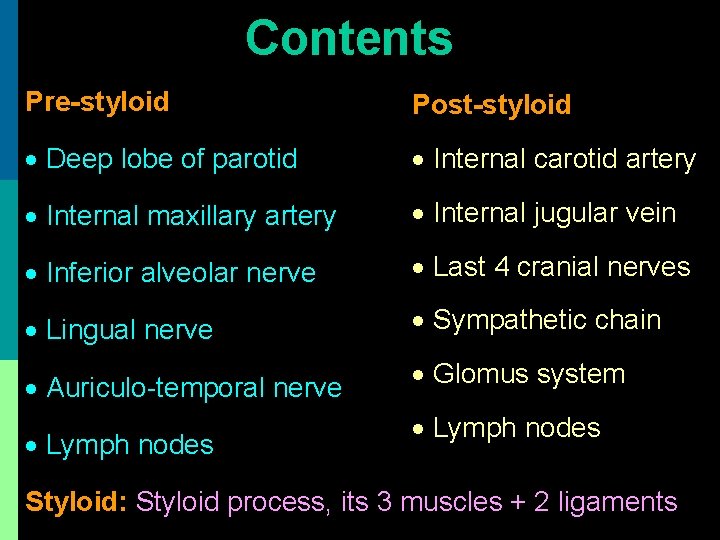
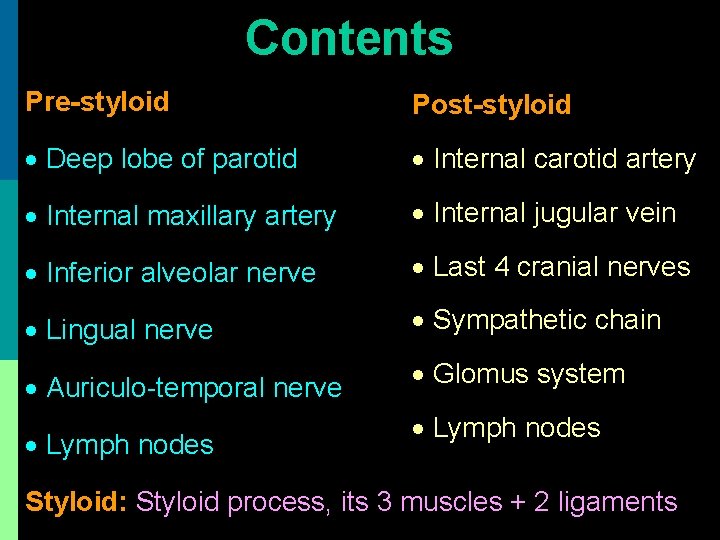
Contents Pre-styloid Post-styloid Deep lobe of parotid Internal carotid artery Internal maxillary artery Internal jugular vein Inferior alveolar nerve Last 4 cranial nerves Lingual nerve Sympathetic chain Auriculo-temporal nerve Glomus system Lymph nodes Styloid: Styloid process, its 3 muscles + 2 ligaments
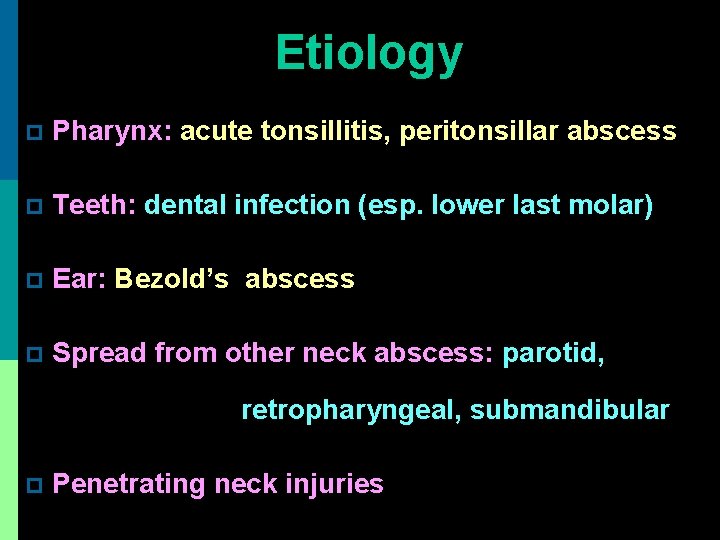
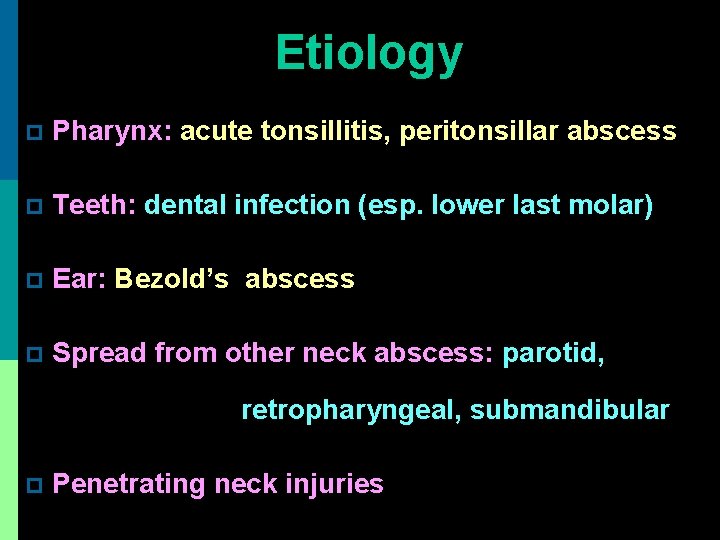
Etiology p Pharynx: acute tonsillitis, peritonsillar abscess p Teeth: dental infection (esp. lower last molar) p Ear: Bezold’s abscess p Spread from other neck abscess: parotid, retropharyngeal, submandibular p Penetrating neck injuries
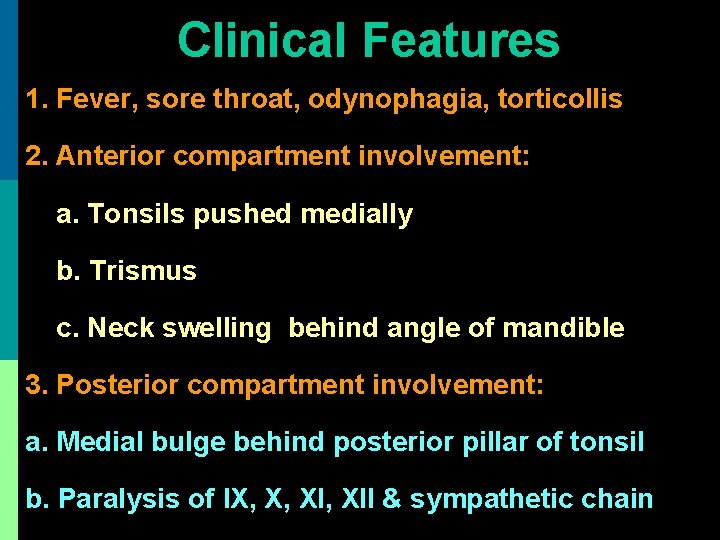
Clinical Features 1. Fever, sore throat, odynophagia, torticollis 2. Anterior compartment involvement: a. Tonsils pushed medially b. Trismus c. Neck swelling behind angle of mandible 3. Posterior compartment involvement: a. Medial bulge behind posterior pillar of tonsil b. Paralysis of IX, X, XII & sympathetic chain

CT scan neck: axial cuts
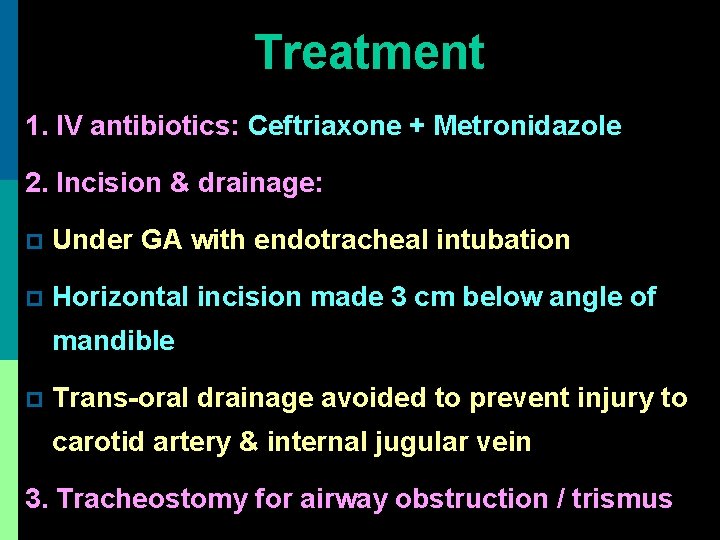
Treatment 1. IV antibiotics: Ceftriaxone + Metronidazole 2. Incision & drainage: p Under GA with endotracheal intubation p Horizontal incision made 3 cm below angle of mandible p Trans-oral drainage avoided to prevent injury to carotid artery & internal jugular vein 3. Tracheostomy for airway obstruction / trismus

Peritonsillar abscess (Quinsy)
Etio-pathogenesis Pus present between tonsillar capsule & superior constrictor muscle Pathology: aerobic + anaerobic organisms 1. Acute tonsillitis blockage of crypts intra tonsillar abscess peritonsillitis quinsy 2. Abscess of Weber's salivary gland in supra tonsillar fossa quinsy
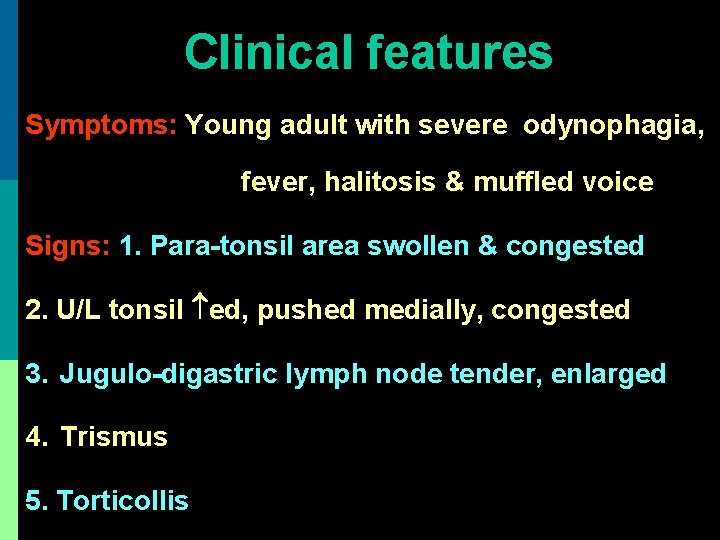
Clinical features Symptoms: Young adult with severe odynophagia, fever, halitosis & muffled voice Signs: 1. Para-tonsil area swollen & congested 2. U/L tonsil ed, pushed medially, congested 3. Jugulo-digastric lymph node tender, enlarged 4. Trismus 5. Torticollis
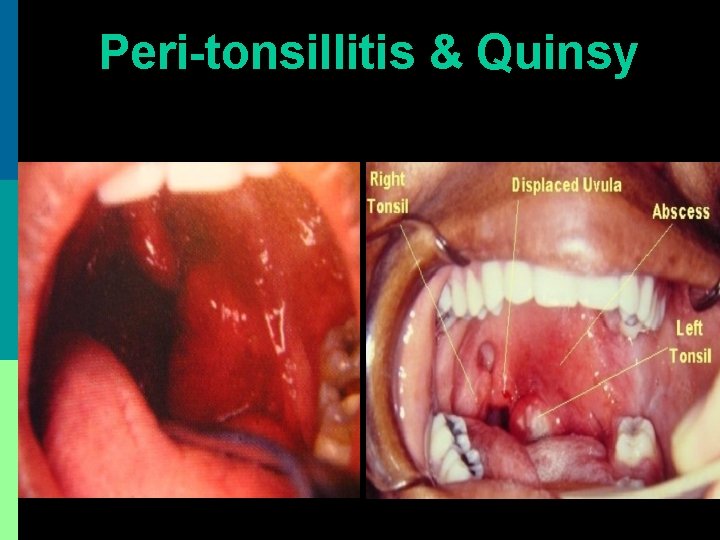
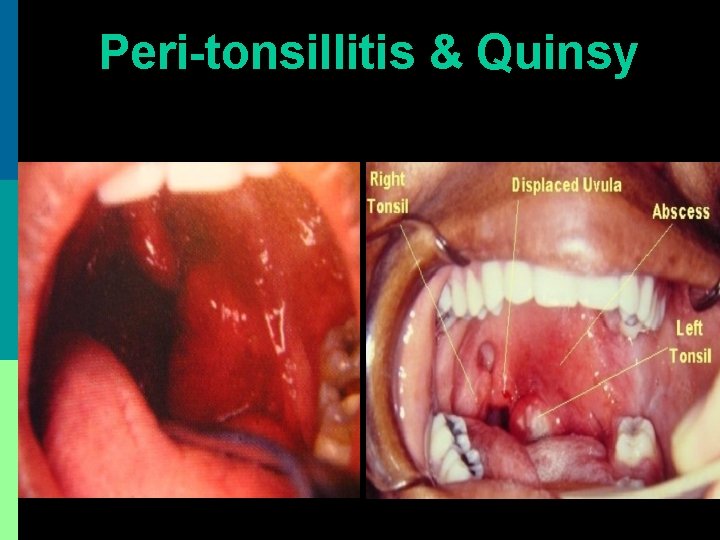
Peri-tonsillitis & Quinsy
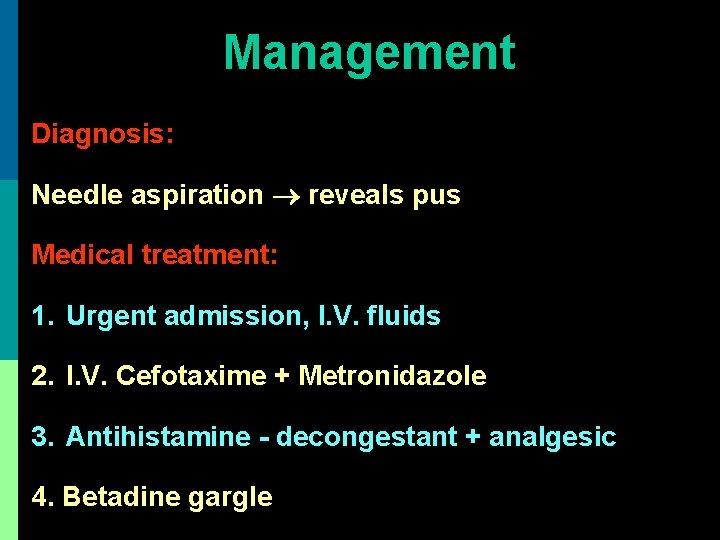
Management Diagnosis: Needle aspiration reveals pus Medical treatment: 1. Urgent admission, I. V. fluids 2. I. V. Cefotaxime + Metronidazole 3. Antihistamine - decongestant + analgesic 4. Betadine gargle
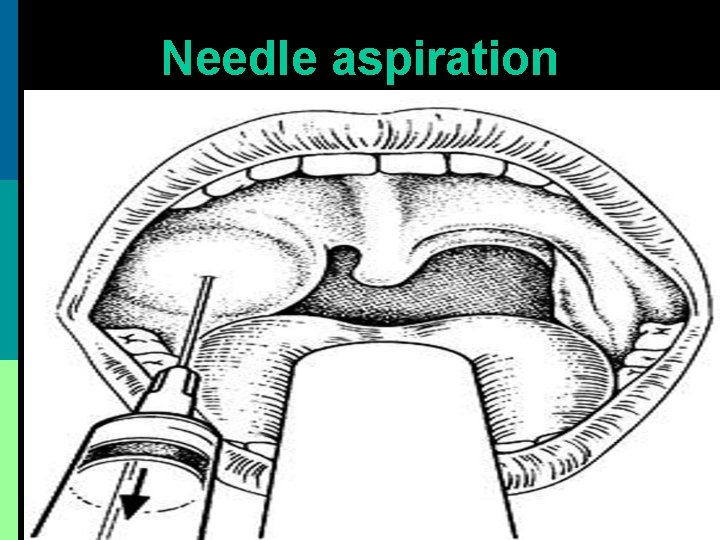
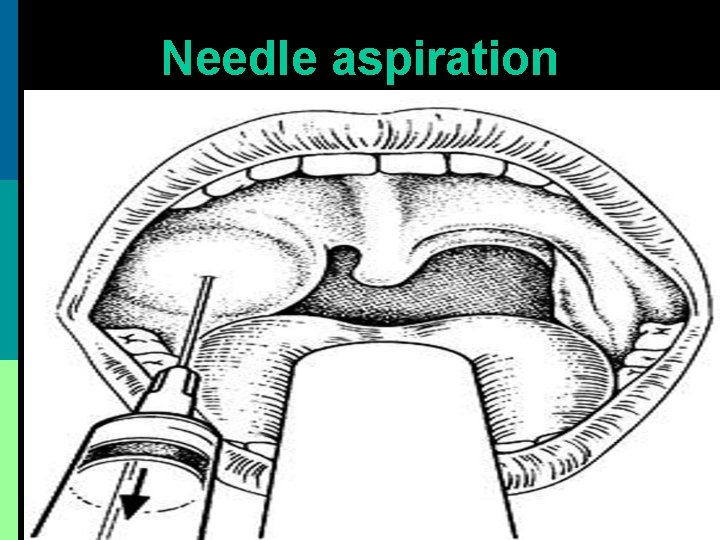
Needle aspiration
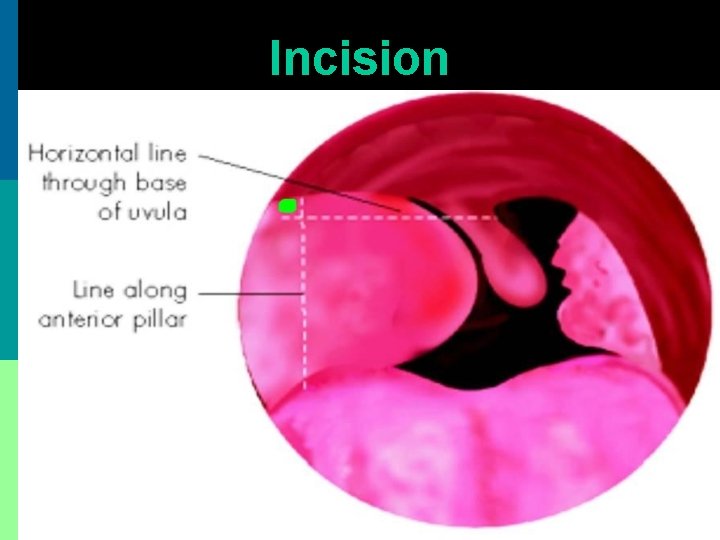
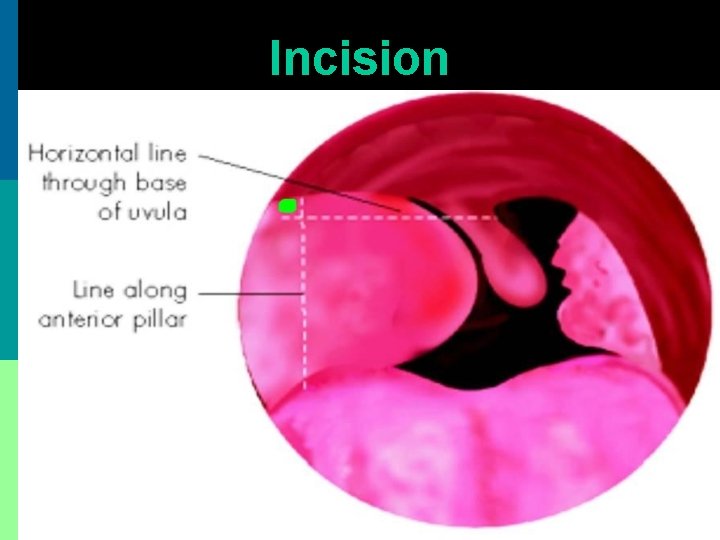
Incision
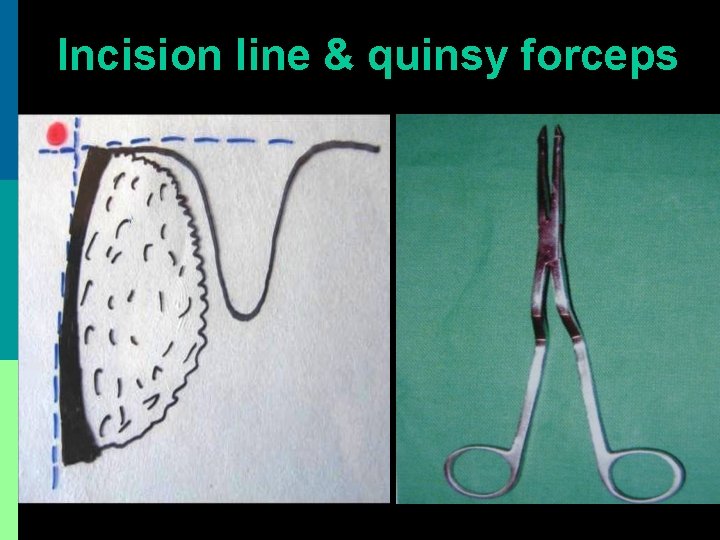
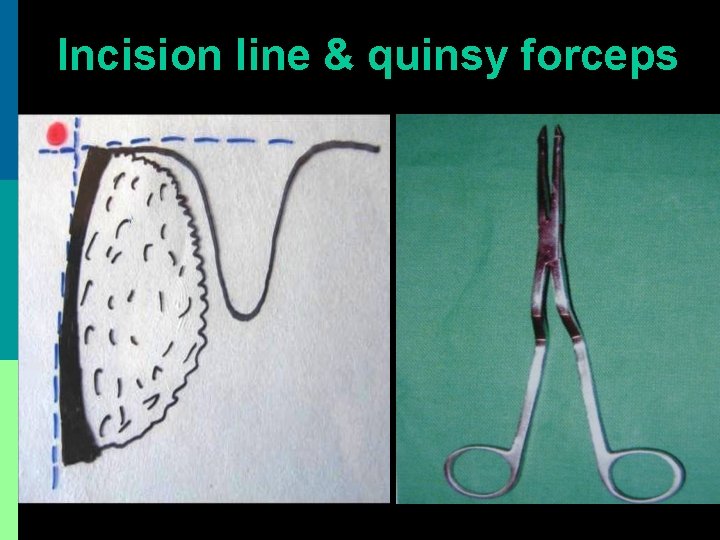
Incision line & quinsy forceps

Alternate incision site at maximum bulge
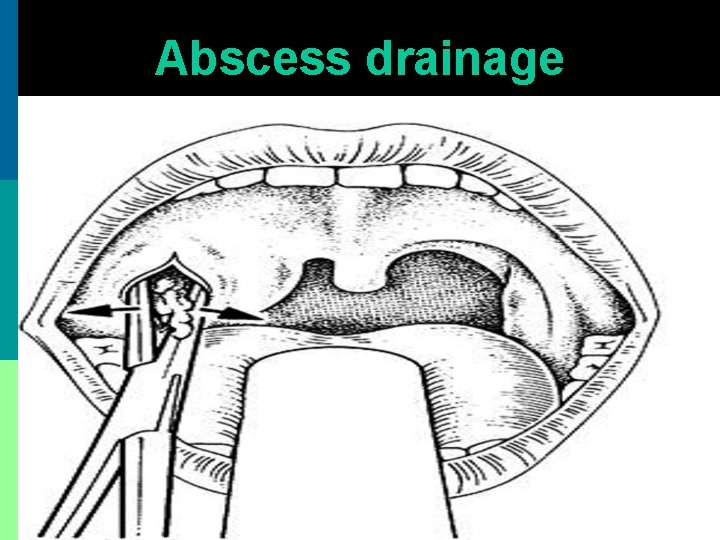
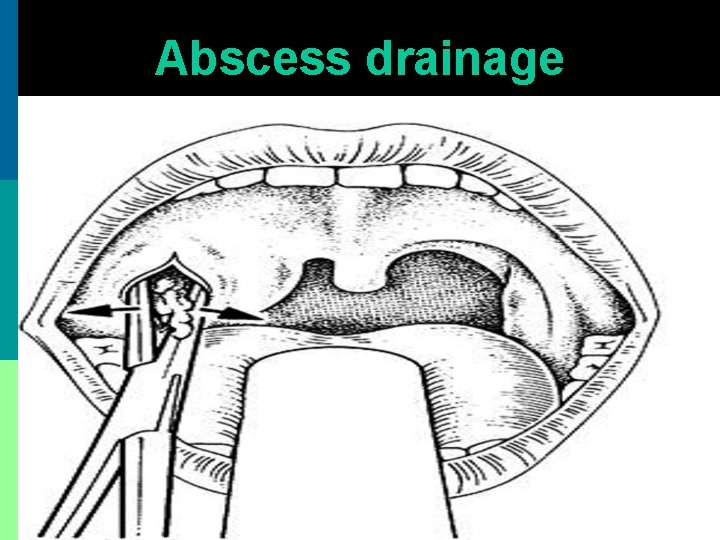
Abscess drainage
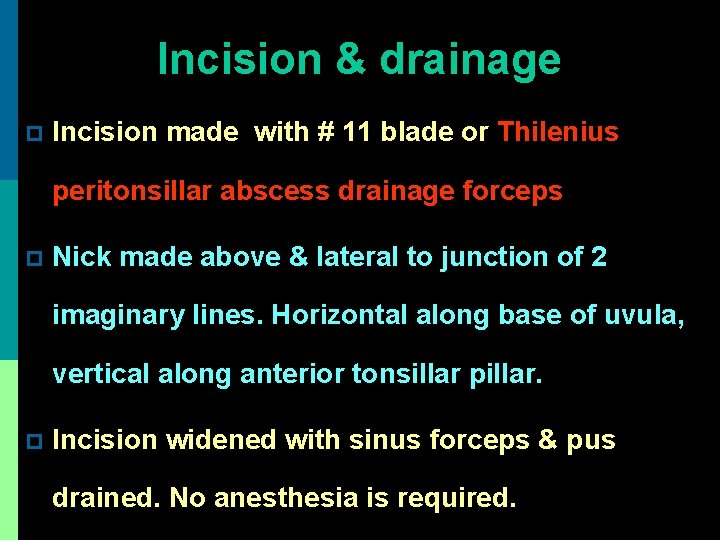
Incision & drainage p Incision made with # 11 blade or Thilenius peritonsillar abscess drainage forceps p Nick made above & lateral to junction of 2 imaginary lines. Horizontal along base of uvula, vertical along anterior tonsillar pillar. p Incision widened with sinus forceps & pus drained. No anesthesia is required.
Surgical treatment 1. Interval tonsillectomy after 4 – 6 wk. 2. Hot tonsillectomy or abscess tonsillectomy is avoided as it leads to: more bleeding septicemia
Complications of quinsy 1. Parapharyngeal abscess 2. Retropharyngeal abscess 3. Laryngitis & laryngeal edema 4. Lung abscess 5. Internal jugular vein thrombosis 6. Septicemia
Parotid abscess
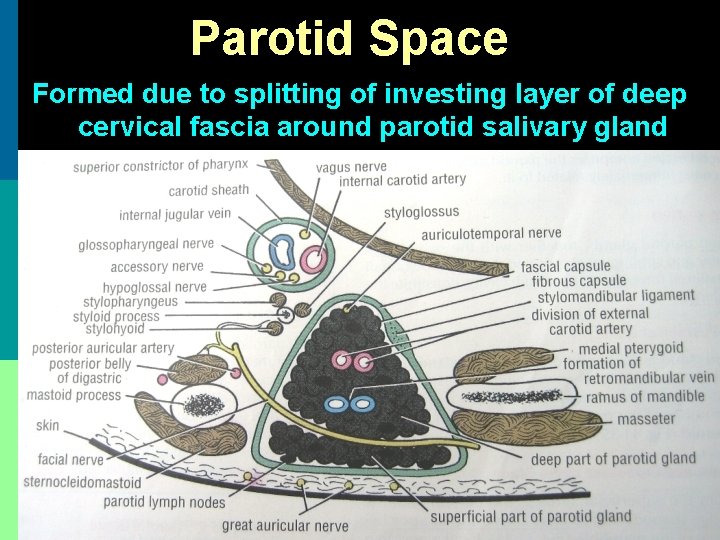
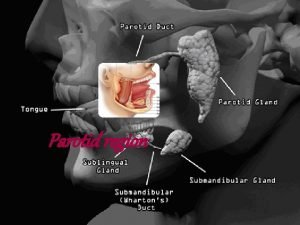
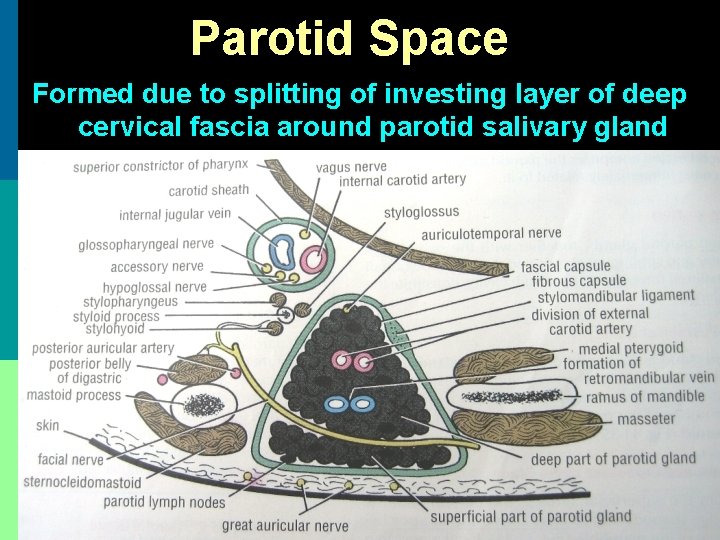
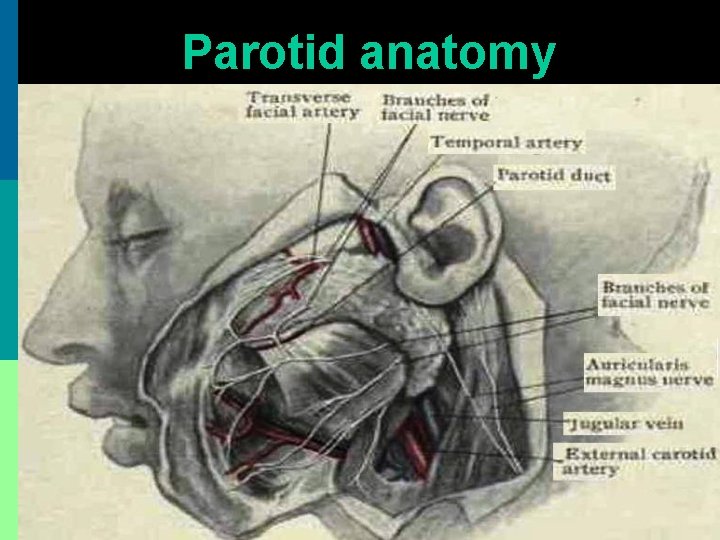
Parotid Space Formed due to splitting of investing layer of deep cervical fascia around parotid salivary gland
Etiology p Ascent of bacterial infection (Staphylococcus, Haemophillus, Streptococcus) to a dehydrated parotid gland along parotid duct from oral cavity p Suppuration of intra-parotid lymph nodes p Spread of infection from EAC via cartilaginous fissures of Santorini or bony foramen of Huschke
Causes of parotid dehydration 1. Post-operative patient (surgical mumps) 2. Medications that decrease salivary flow: p Antihistamines p Tricyclic antidepressants p Barbiturates p Diuretics p Parasympathomimetics
Parotid abscess p Pain + induration over parotid gland p Pitting edema of parotid area differentiates parotid abscess from simple parotitis p Parotid massage expresses pus from parotid duct into oral cavity (opposite upper 2 nd molar)
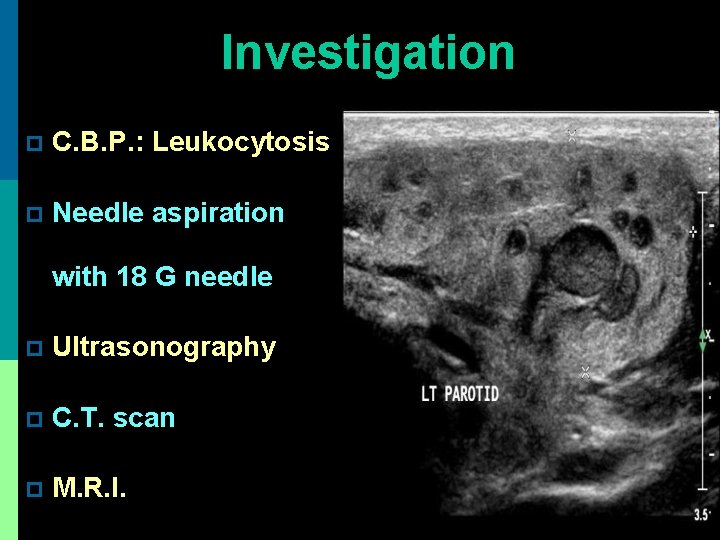
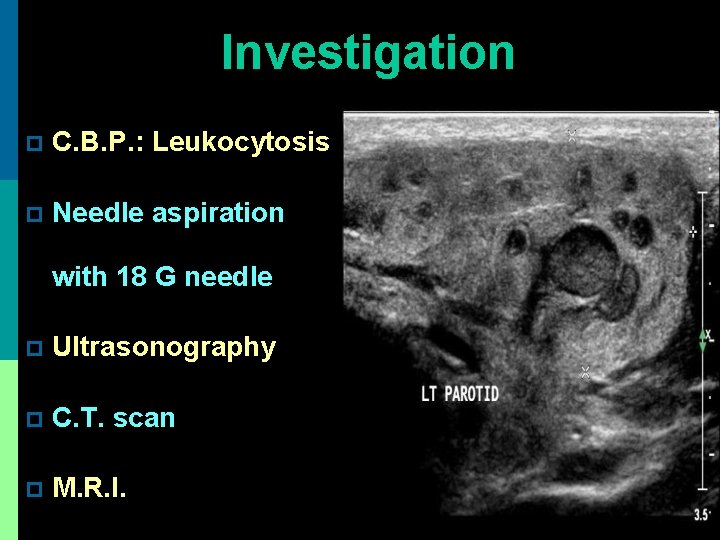
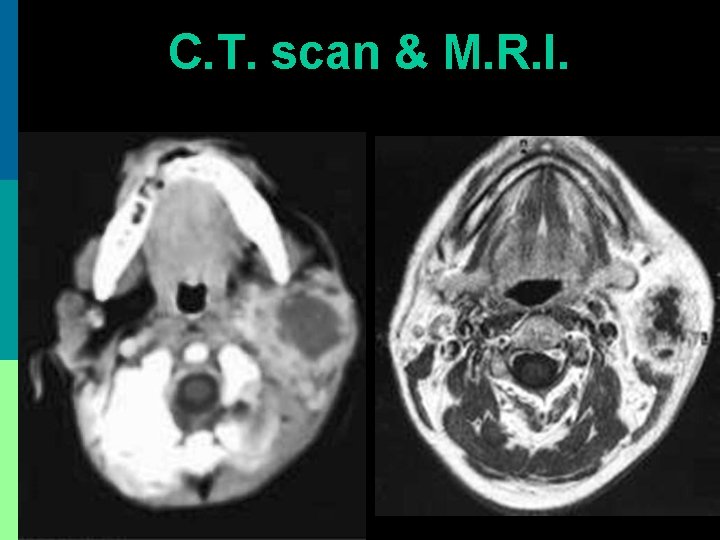
Investigation p C. B. P. : Leukocytosis p Needle aspiration with 18 G needle p Ultrasonography p C. T. scan p M. R. I.
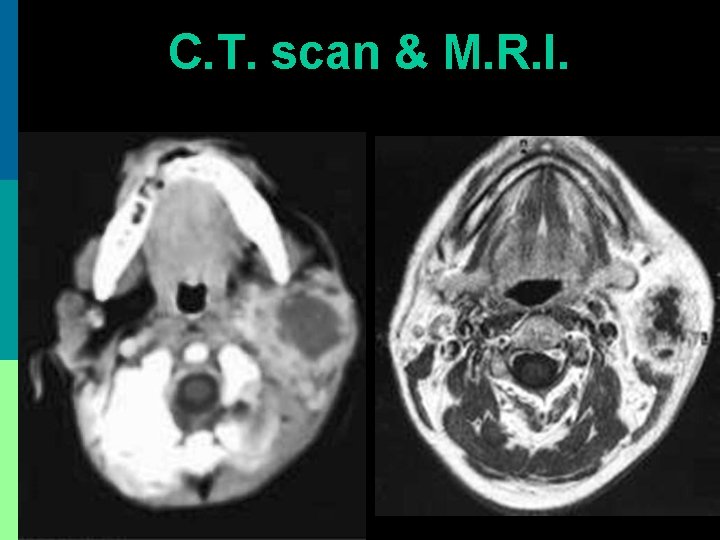
C. T. scan & M. R. I.
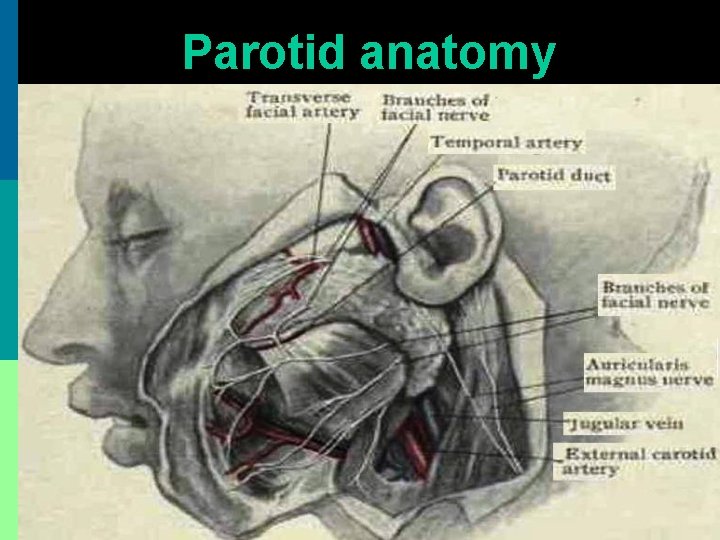
Parotid anatomy

Treatment 1. IV fluid for dehydration 2. IV Ampicillin + Gentamicin + Metronidazole 3. Incision drainage: a. Blair’s incision made b. Multiple incisions made through fascia, parallel to facial nerve branches c. Blunt dissection to evacuate pus. Drains placed.

Thank You
 Dr vishal sharma
Dr vishal sharma Potential spaces of the hand
Potential spaces of the hand Dangerous space of neck
Dangerous space of neck Spaces of the neck
Spaces of the neck Pharengyal
Pharengyal Simple alidade
Simple alidade Waldenstrom's disease
Waldenstrom's disease Vishal sundaram
Vishal sundaram Vishal thakkar nose
Vishal thakkar nose Vishal gupta bits pilani
Vishal gupta bits pilani Style
Style Dr vishal jaiswal
Dr vishal jaiswal Link tree vishal tiwari
Link tree vishal tiwari Principle of surveying
Principle of surveying Blake patel only connect
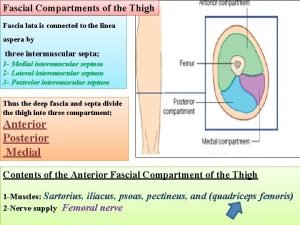
Blake patel only connect Musculo obturador
Musculo obturador Forearm space of parona boundaries
Forearm space of parona boundaries Storch infections
Storch infections Genital infections
Genital infections Postpartum infections
Postpartum infections Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Bone and joint infections
Bone and joint infections Opportunistic infections
Opportunistic infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Phagocytr
Phagocytr Johnson and johnson botnet infections
Johnson and johnson botnet infections Cryptosporidiose
Cryptosporidiose Can methotrexate cause yeast infections
Can methotrexate cause yeast infections Genital infections
Genital infections Acute gingival infections
Acute gingival infections Storch infections
Storch infections Eye infections
Eye infections Opportunistic infections
Opportunistic infections Facial nerve decompression surgery
Facial nerve decompression surgery Keerti sharma md
Keerti sharma md Dr vivek sharma
Dr vivek sharma Aditi sharma cmu
Aditi sharma cmu Riju sharma
Riju sharma Pushpa
Pushpa Pradeep sharma university of houston
Pradeep sharma university of houston Pushpa raj sharma
Pushpa raj sharma Dr pushpa raj sharma clinic
Dr pushpa raj sharma clinic Dr pushpa raj sharma pediatrician
Dr pushpa raj sharma pediatrician Ranipril
Ranipril Amrit sharma morgan stanley
Amrit sharma morgan stanley Pushpa raj sharma
Pushpa raj sharma Jag sharma
Jag sharma Dr madhurima sharma
Dr madhurima sharma Hina sharma architect
Hina sharma architect Dr pushpa raj sharma contact number
Dr pushpa raj sharma contact number Archana sharma psychologist
Archana sharma psychologist Ca umesh sharma
Ca umesh sharma Sankaran's card repertory
Sankaran's card repertory Adjacency matrix of multigraph
Adjacency matrix of multigraph Dr suman sharma
Dr suman sharma Lasert tag
Lasert tag Pushpa raj sharma
Pushpa raj sharma Umesh sharma md
Umesh sharma md Cs deepak sharma
Cs deepak sharma Pawan sharma bits pilani
Pawan sharma bits pilani Pushpa raj sharma
Pushpa raj sharma Dr pushpa raj sharma pediatrician
Dr pushpa raj sharma pediatrician Sumit sharma teri
Sumit sharma teri Dr bikas sharma
Dr bikas sharma Dr pk sharma
Dr pk sharma Gaurav sharma cisco
Gaurav sharma cisco Dr rakesh sharma
Dr rakesh sharma Modern concept of child care
Modern concept of child care Cartesian space trajectory planning
Cartesian space trajectory planning Ndc to screen space
Ndc to screen space Space junk the space age began
Space junk the space age began Camera space to world space
Camera space to world space Unscented trajectory chapter 5
Unscented trajectory chapter 5 Rash on upper chest and back
Rash on upper chest and back Zygomaticus major
Zygomaticus major Ct neck
Ct neck The five guildsmen canterbury tales
The five guildsmen canterbury tales What has a neck but no head
What has a neck but no head Neck injury zone
Neck injury zone Cdsa dam neck
Cdsa dam neck Regional write up head face and neck
Regional write up head face and neck Synotenovitis
Synotenovitis Popliteal angle test
Popliteal angle test Brush strum
Brush strum How are v shaped valleys formed
How are v shaped valleys formed Svaly hk
Svaly hk Stomach layers histology
Stomach layers histology Happy feet plastic around neck
Happy feet plastic around neck Posterior triangle
Posterior triangle This is home ukulele
This is home ukulele Sauropod neck posture
Sauropod neck posture Neck o flex
Neck o flex Tnm 8 head and neck
Tnm 8 head and neck Greater and lesser pelvis
Greater and lesser pelvis Moro reflex absent
Moro reflex absent Diphtheria
Diphtheria Face regions anatomy
Face regions anatomy Boutonniere and swan neck deformity
Boutonniere and swan neck deformity Pnf neck patterns
Pnf neck patterns Macfee incision
Macfee incision