PEDIATRIC FACIAL SWELLING A GUIDE TO RADIOLOGIC DIAGNOSIS
- Slides: 35
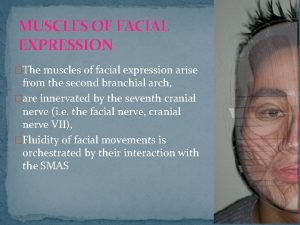
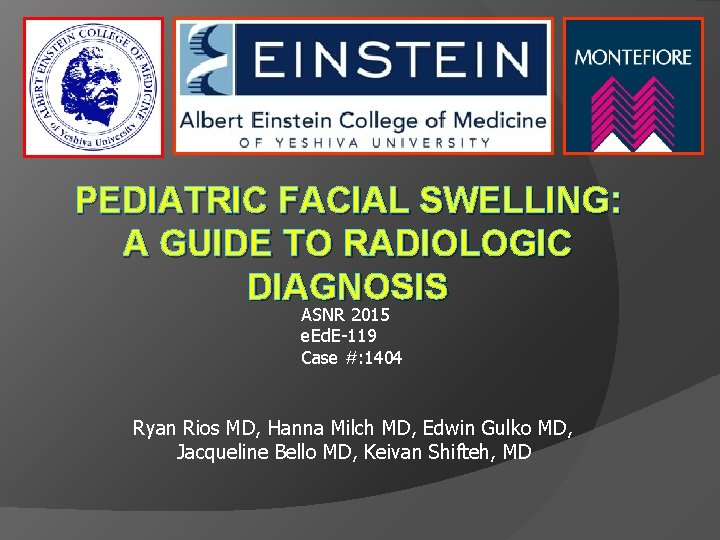
PEDIATRIC FACIAL SWELLING: A GUIDE TO RADIOLOGIC DIAGNOSIS ASNR 2015 e. Ed. E-119 Case #: 1404 Ryan Rios MD, Hanna Milch MD, Edwin Gulko MD, Jacqueline Bello MD, Keivan Shifteh, MD
Introduction Facial swelling is a common clinical problem in the pediatric population. The origins of facial swelling can vary from congenital to acquired conditions such as infection / inflammatory, benign or malignant conditions involving the soft tissue and/or bone. Clinical history and physical manifestations are the most important factors in the evaluation of facial swelling and deciding whether imaging is indicated. Recent advances in imaging have led to the increasing use of CT and MRI for evaluation of the underlying causes of facial swelling and the extent of disease, leading to more effective treatment.
Purpose This presentation will focus on reviewing the differential diagnosis of facial and neck swelling in children. Explain how CT and MR are used to distinguish causes of facial swelling in children. Provide a pictorial review of common and rare causes of pediatric facial swelling.
Purpose Etiologies are separated into the following categories: Infectious: Orbital cellulitis, Pot puffy tumor, Cat scratch disease, Parotitis, Tuberculosis adenitis, Sialoadenitis, Abscesses , Infected masses (Ranula, Thyroglossal duct cyst, Type I brachial cleft cyst). Inflammatory: Eosinophilic granuloma, ALPS, Rosi dorfman disease, Pseudotumor. Vascular: Facial AVM, Hemangioma, Lymphangioma Benign tumor: Gardner syndrome, Cemento osseous dysplasia, Plexiform neurofibromatosis, Non-ossifying fibroma, Ranula, Fibrous dysplasia. Neoplastic: Lymph node metastasis resembling a type II brachial cleft cyst, Primitive neuroectodermal tumor (PNET), Orbital lymphoma, Rhabdomyosarcoma. Trauma: Facial soft tissue emphysema, Carotid cavernous fistula.
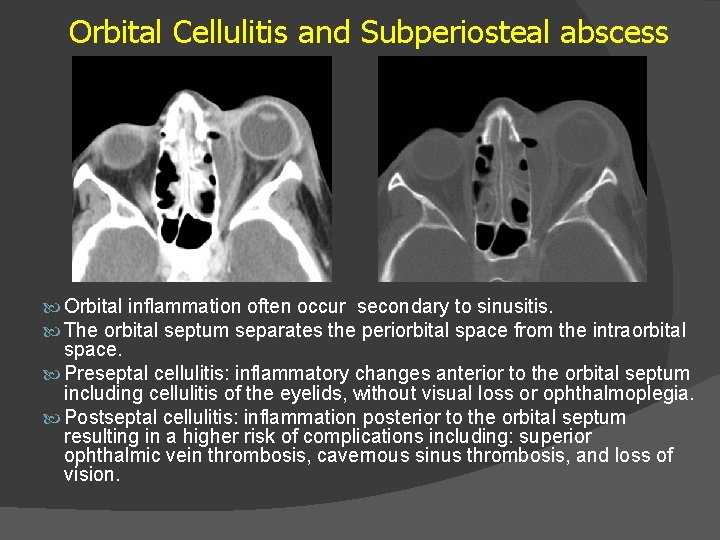
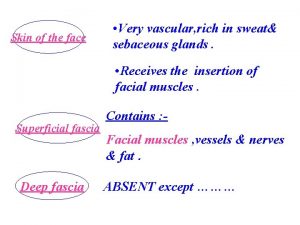
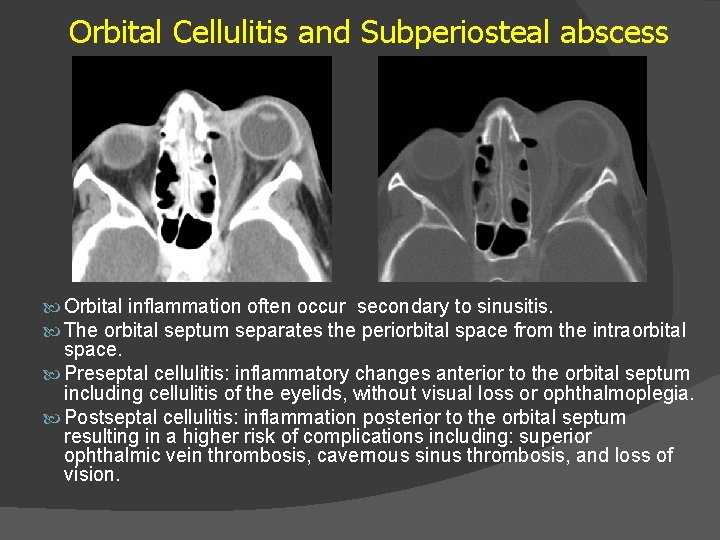
Orbital Cellulitis and Subperiosteal abscess Orbital inflammation often occur secondary to sinusitis. The orbital septum separates the periorbital space from the intraorbital space. Preseptal cellulitis: inflammatory changes anterior to the orbital septum including cellulitis of the eyelids, without visual loss or ophthalmoplegia. Postseptal cellulitis: inflammation posterior to the orbital septum resulting in a higher risk of complications including: superior ophthalmic vein thrombosis, cavernous sinus thrombosis, and loss of vision.
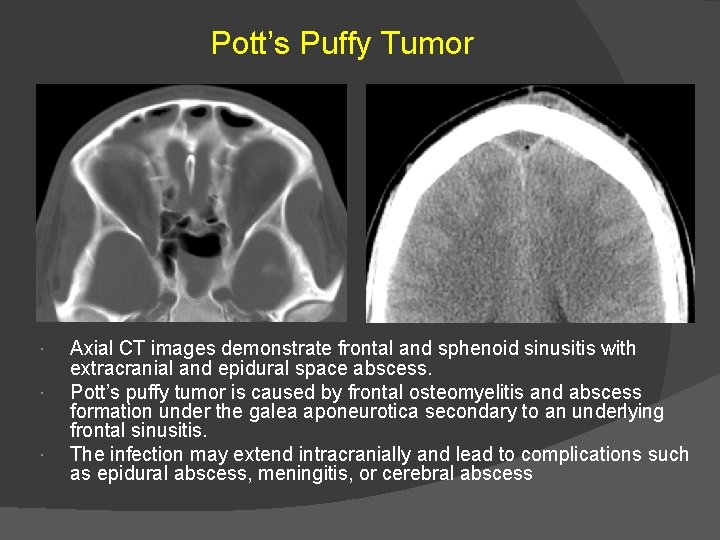
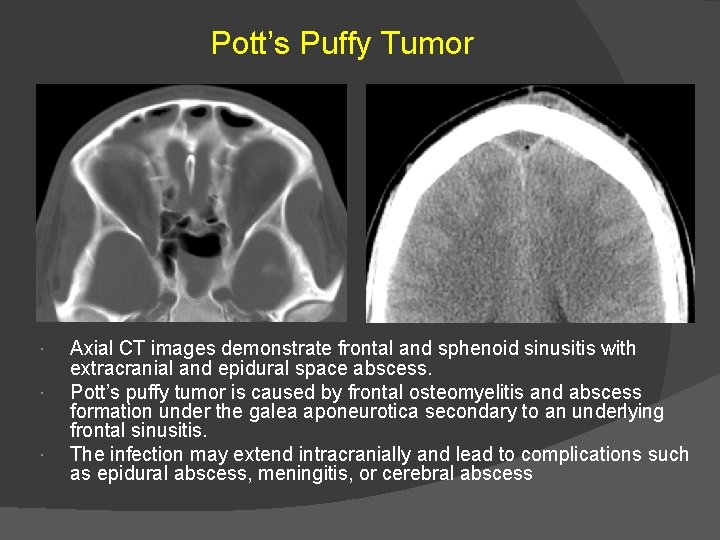
Pott’s Puffy Tumor Axial CT images demonstrate frontal and sphenoid sinusitis with extracranial and epidural space abscess. Pott’s puffy tumor is caused by frontal osteomyelitis and abscess formation under the galea aponeurotica secondary to an underlying frontal sinusitis. The infection may extend intracranially and lead to complications such as epidural abscess, meningitis, or cerebral abscess
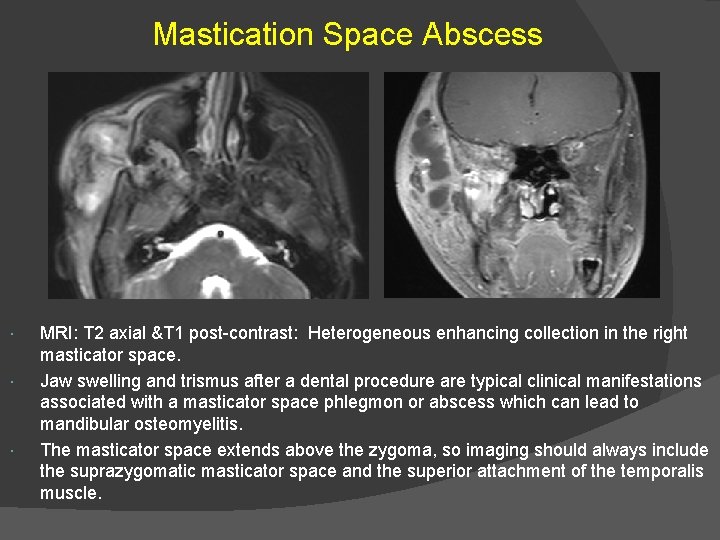
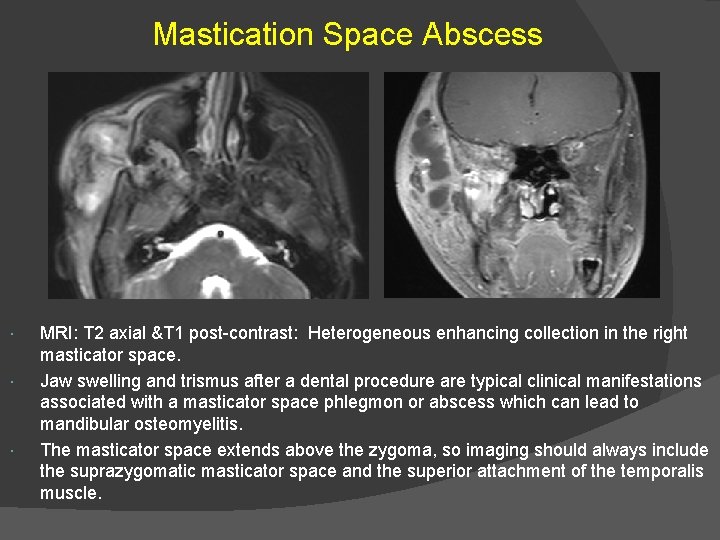
Mastication Space Abscess MRI: T 2 axial &T 1 post-contrast: Heterogeneous enhancing collection in the right masticator space. Jaw swelling and trismus after a dental procedure are typical clinical manifestations associated with a masticator space phlegmon or abscess which can lead to mandibular osteomyelitis. The masticator space extends above the zygoma, so imaging should always include the suprazygomatic masticator space and the superior attachment of the temporalis muscle.
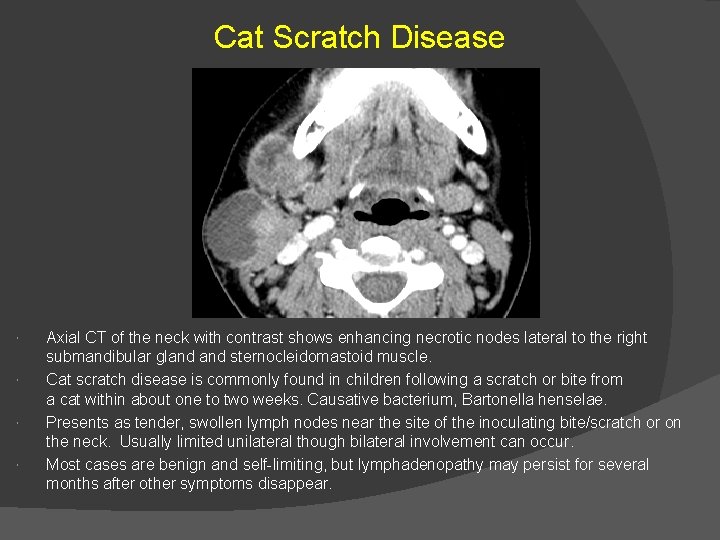
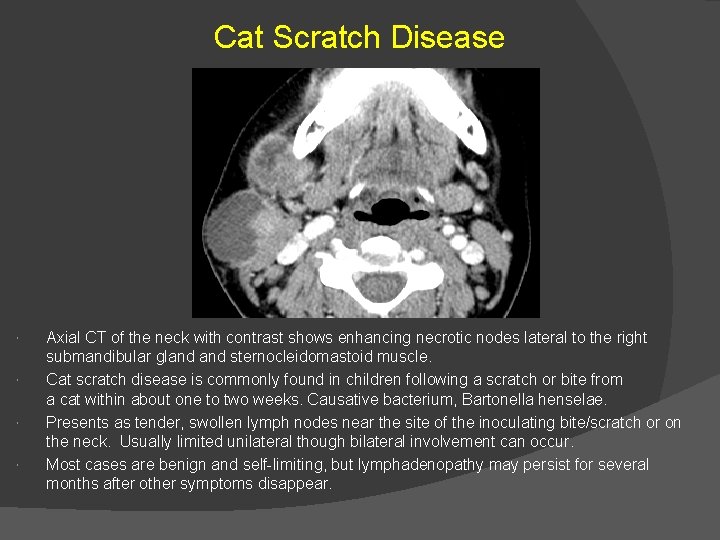
Cat Scratch Disease Axial CT of the neck with contrast shows enhancing necrotic nodes lateral to the right submandibular gland sternocleidomastoid muscle. Cat scratch disease is commonly found in children following a scratch or bite from a cat within about one to two weeks. Causative bacterium, Bartonella henselae. Presents as tender, swollen lymph nodes near the site of the inoculating bite/scratch or on the neck. Usually limited unilateral though bilateral involvement can occur. Most cases are benign and self-limiting, but lymphadenopathy may persist for several months after other symptoms disappear.
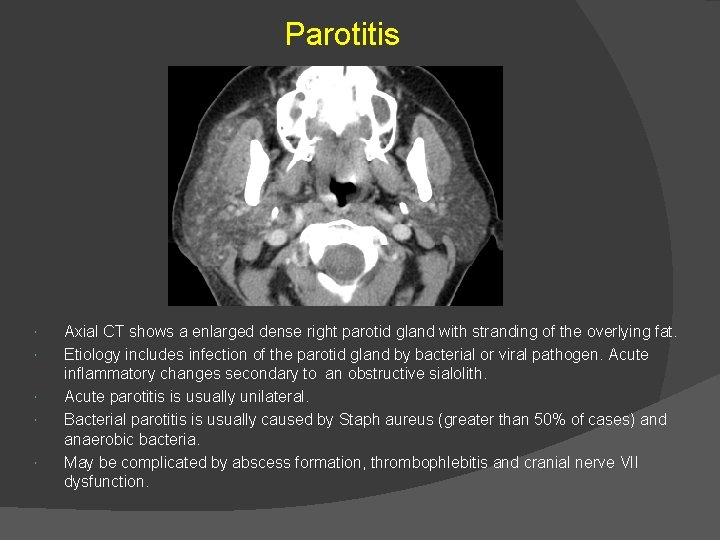
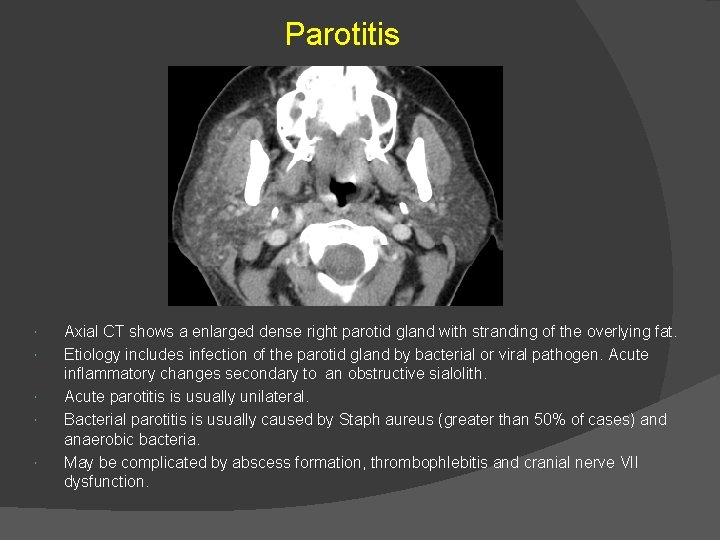
Parotitis Axial CT shows a enlarged dense right parotid gland with stranding of the overlying fat. Etiology includes infection of the parotid gland by bacterial or viral pathogen. Acute inflammatory changes secondary to an obstructive sialolith. Acute parotitis is usually unilateral. Bacterial parotitis is usually caused by Staph aureus (greater than 50% of cases) and anaerobic bacteria. May be complicated by abscess formation, thrombophlebitis and cranial nerve VII dysfunction.
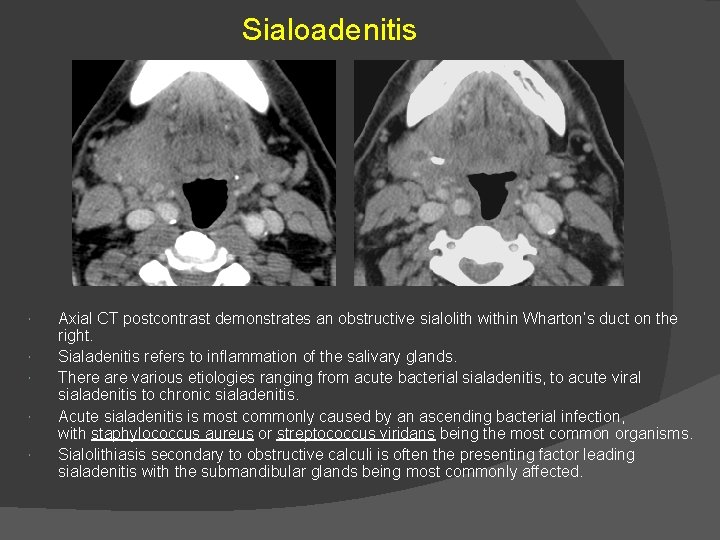
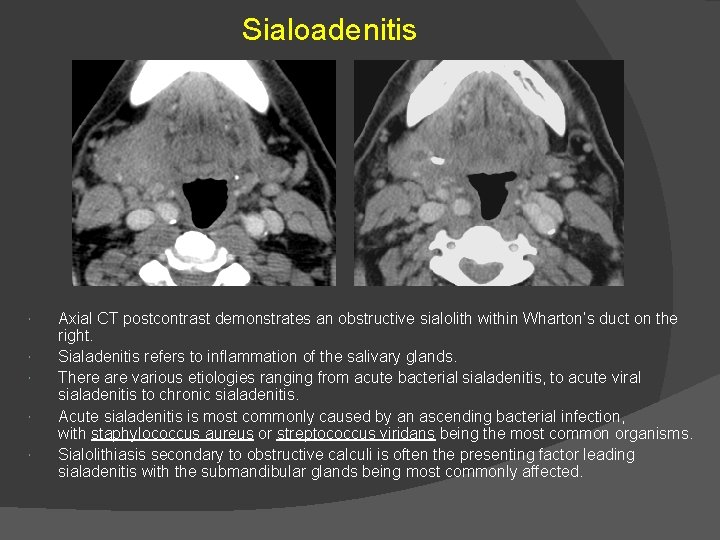
Sialoadenitis Axial CT postcontrast demonstrates an obstructive sialolith within Wharton’s duct on the right. Sialadenitis refers to inflammation of the salivary glands. There are various etiologies ranging from acute bacterial sialadenitis, to acute viral sialadenitis to chronic sialadenitis. Acute sialadenitis is most commonly caused by an ascending bacterial infection, with staphylococcus aureus or streptococcus viridans being the most common organisms. Sialolithiasis secondary to obstructive calculi is often the presenting factor leading sialadenitis with the submandibular glands being most commonly affected.
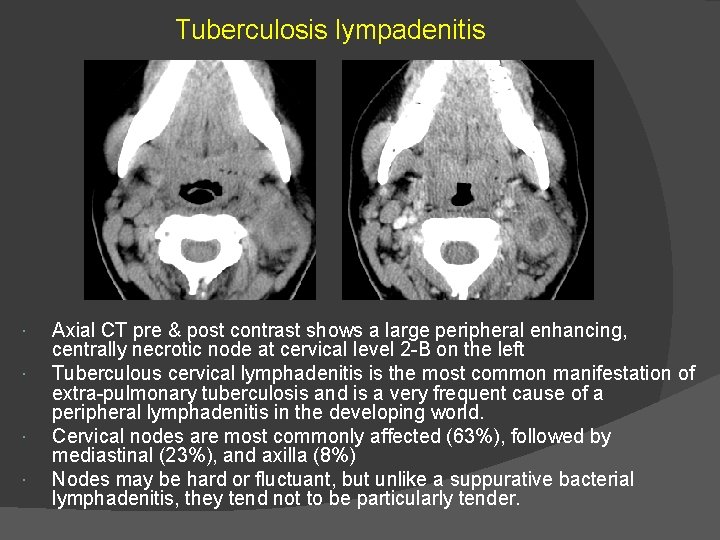
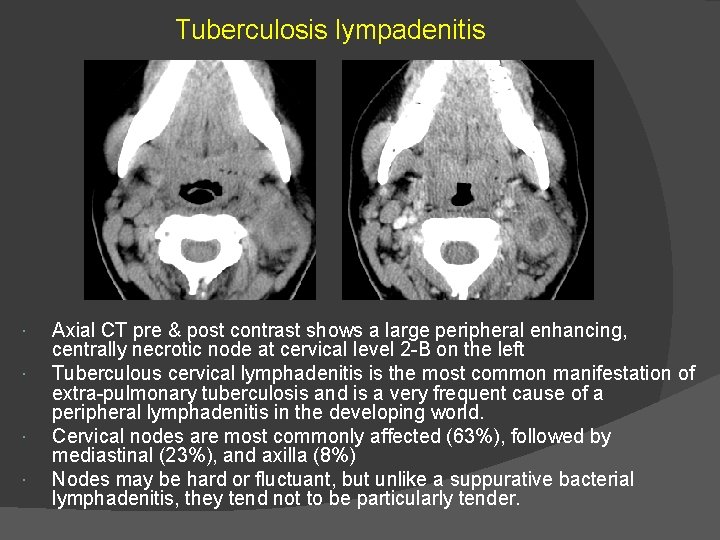
Tuberculosis lympadenitis Axial CT pre & post contrast shows a large peripheral enhancing, centrally necrotic node at cervical level 2 -B on the left Tuberculous cervical lymphadenitis is the most common manifestation of extra-pulmonary tuberculosis and is a very frequent cause of a peripheral lymphadenitis in the developing world. Cervical nodes are most commonly affected (63%), followed by mediastinal (23%), and axilla (8%) Nodes may be hard or fluctuant, but unlike a suppurative bacterial lymphadenitis, they tend not to be particularly tender.
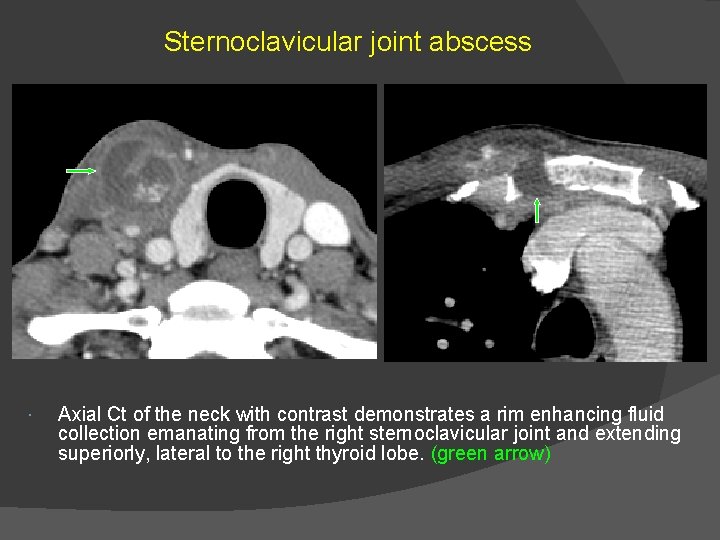
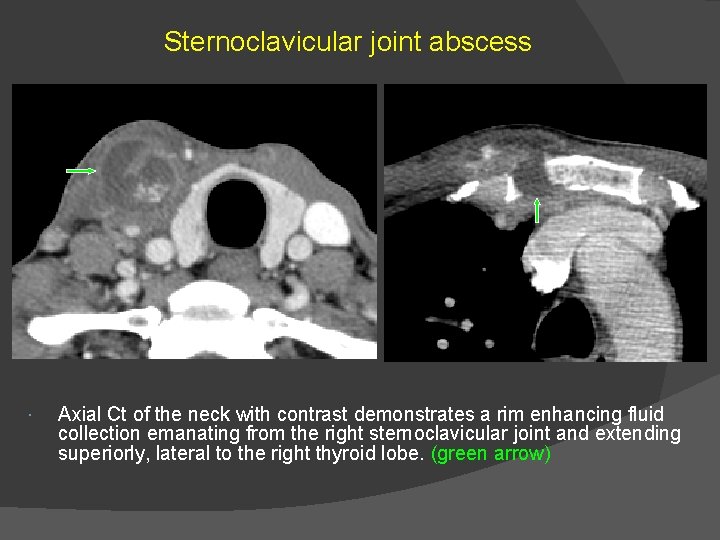
Sternoclavicular joint abscess Axial Ct of the neck with contrast demonstrates a rim enhancing fluid collection emanating from the right sternoclavicular joint and extending superiorly, lateral to the right thyroid lobe. (green arrow)
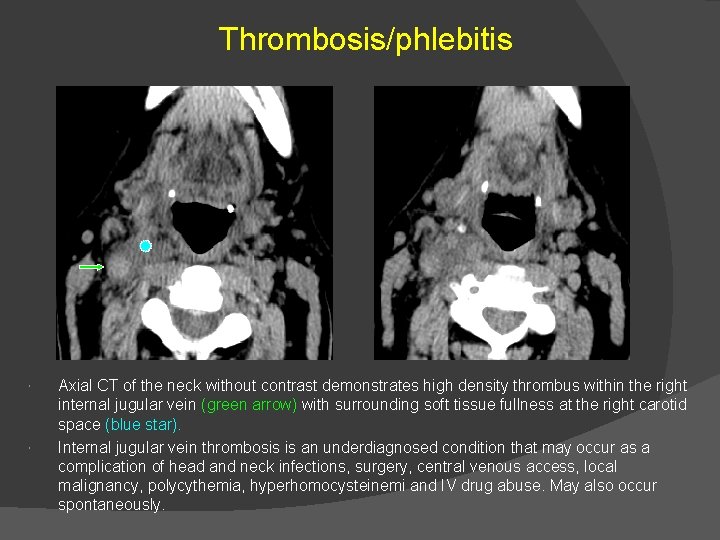
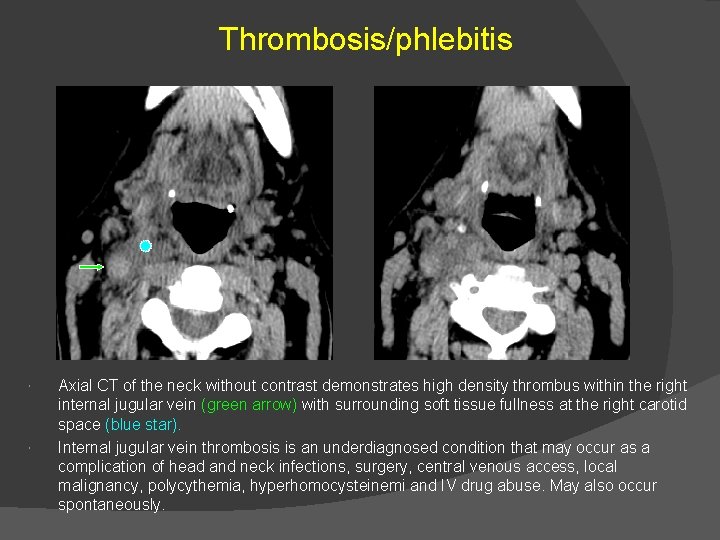
Thrombosis/phlebitis Axial CT of the neck without contrast demonstrates high density thrombus within the right internal jugular vein (green arrow) with surrounding soft tissue fullness at the right carotid space (blue star). Internal jugular vein thrombosis is an underdiagnosed condition that may occur as a complication of head and neck infections, surgery, central venous access, local malignancy, polycythemia, hyperhomocysteinemi and IV drug abuse. May also occur spontaneously.
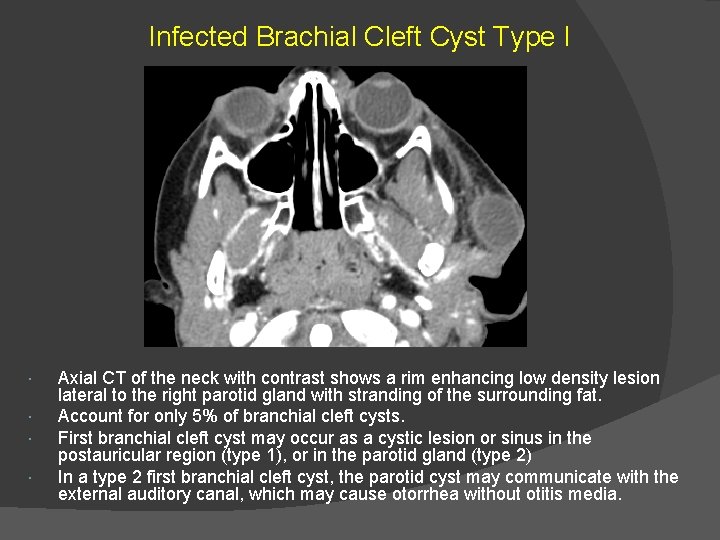
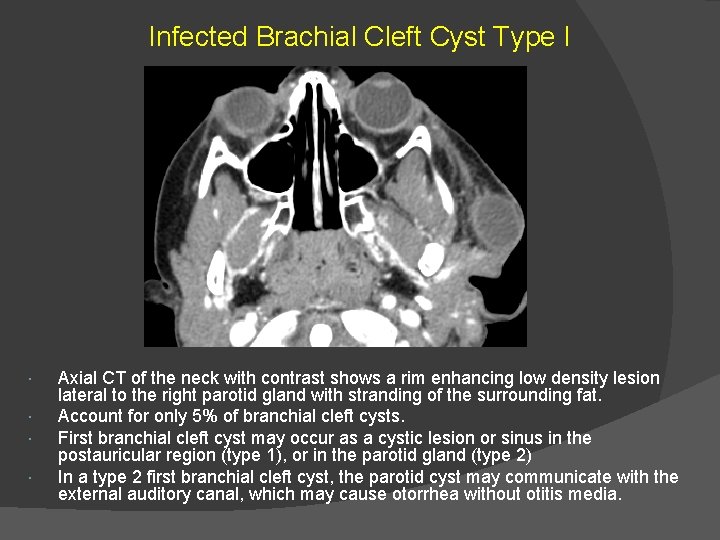
Infected Brachial Cleft Cyst Type I Axial CT of the neck with contrast shows a rim enhancing low density lesion lateral to the right parotid gland with stranding of the surrounding fat. Account for only 5% of branchial cleft cysts. First branchial cleft cyst may occur as a cystic lesion or sinus in the postauricular region (type 1), or in the parotid gland (type 2) In a type 2 first branchial cleft cyst, the parotid cyst may communicate with the external auditory canal, which may cause otorrhea without otitis media.
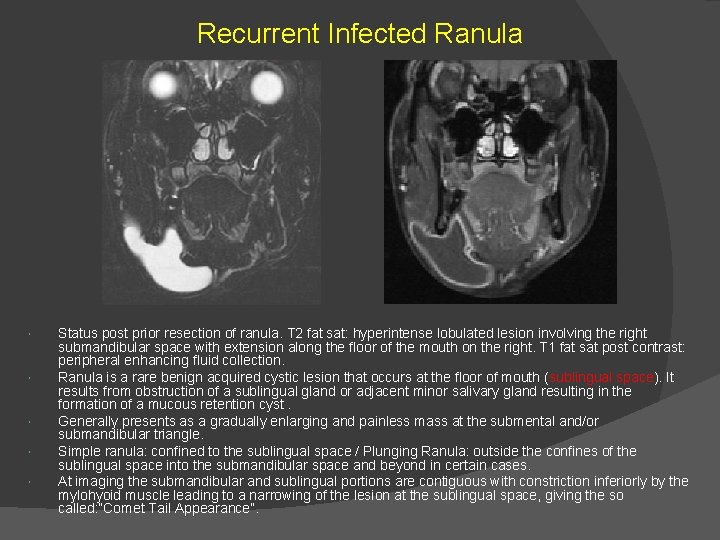
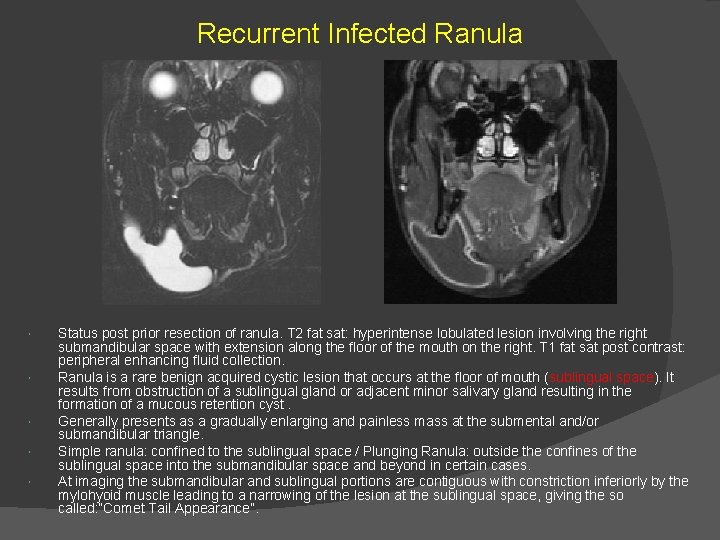
Recurrent Infected Ranula Status post prior resection of ranula. T 2 fat sat: hyperintense lobulated lesion involving the right submandibular space with extension along the floor of the mouth on the right. T 1 fat sat post contrast: peripheral enhancing fluid collection. Ranula is a rare benign acquired cystic lesion that occurs at the floor of mouth (sublingual space). It results from obstruction of a sublingual gland or adjacent minor salivary gland resulting in the formation of a mucous retention cyst. Generally presents as a gradually enlarging and painless mass at the submental and/or submandibular triangle. Simple ranula: confined to the sublingual space / Plunging Ranula: outside the confines of the sublingual space into the submandibular space and beyond in certain cases. At imaging the submandibular and sublingual portions are contiguous with constriction inferiorly by the mylohyoid muscle leading to a narrowing of the lesion at the sublingual space, giving the so called: “Comet Tail Appearance”.
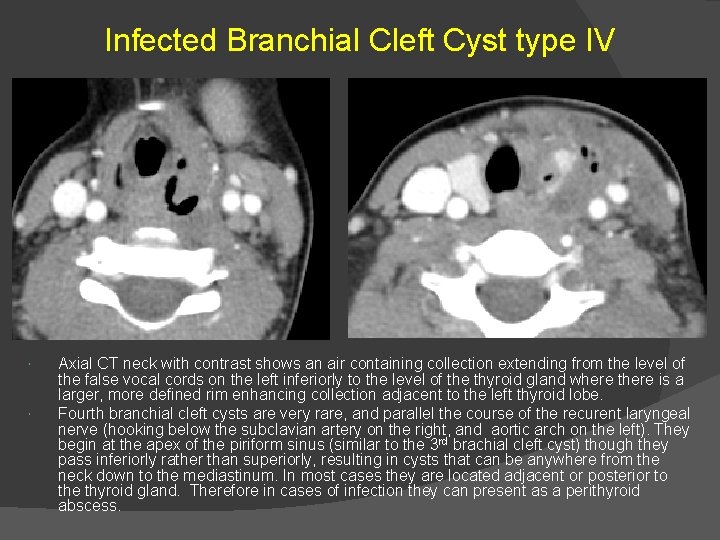
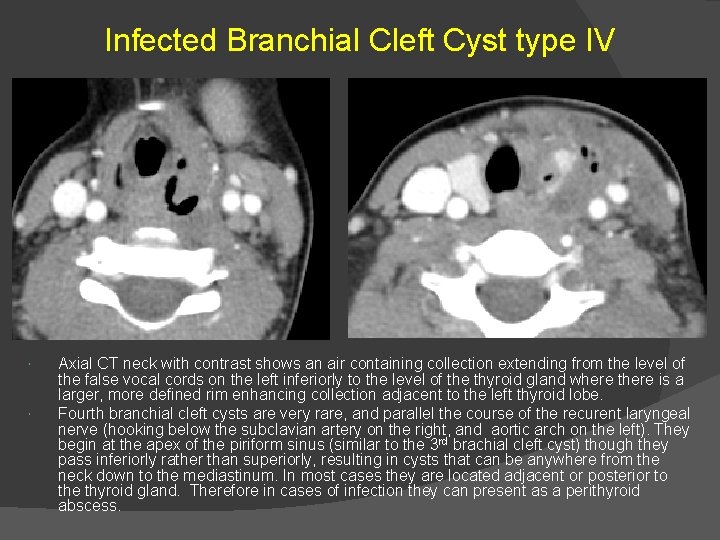
Infected Branchial Cleft Cyst type IV Axial CT neck with contrast shows an air containing collection extending from the level of the false vocal cords on the left inferiorly to the level of the thyroid gland where there is a larger, more defined rim enhancing collection adjacent to the left thyroid lobe. Fourth branchial cleft cysts are very rare, and parallel the course of the recurent laryngeal nerve (hooking below the subclavian artery on the right, and aortic arch on the left). They begin at the apex of the piriform sinus (similar to the 3 rd brachial cleft cyst) though they pass inferiorly rather than superiorly, resulting in cysts that can be anywhere from the neck down to the mediastinum. In most cases they are located adjacent or posterior to the thyroid gland. Therefore in cases of infection they can present as a perithyroid abscess.
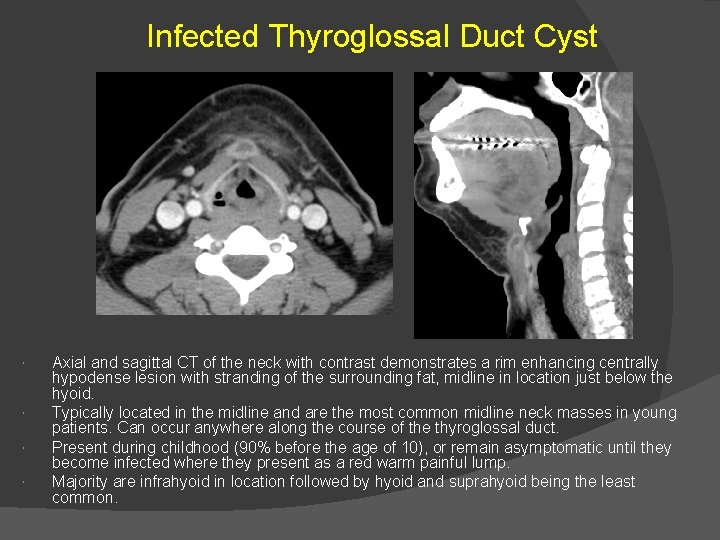
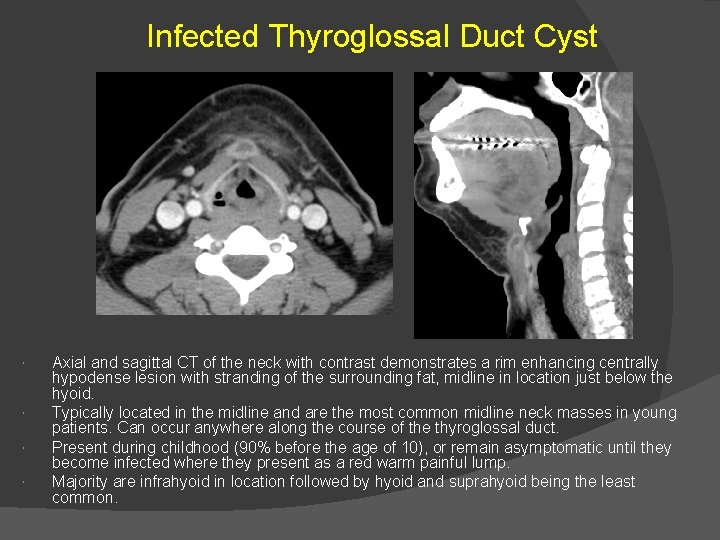
Infected Thyroglossal Duct Cyst Axial and sagittal CT of the neck with contrast demonstrates a rim enhancing centrally hypodense lesion with stranding of the surrounding fat, midline in location just below the hyoid. Typically located in the midline and are the most common midline neck masses in young patients. Can occur anywhere along the course of the thyroglossal duct. Present during childhood (90% before the age of 10), or remain asymptomatic until they become infected where they present as a red warm painful lump. Majority are infrahyoid in location followed by hyoid and suprahyoid being the least common.
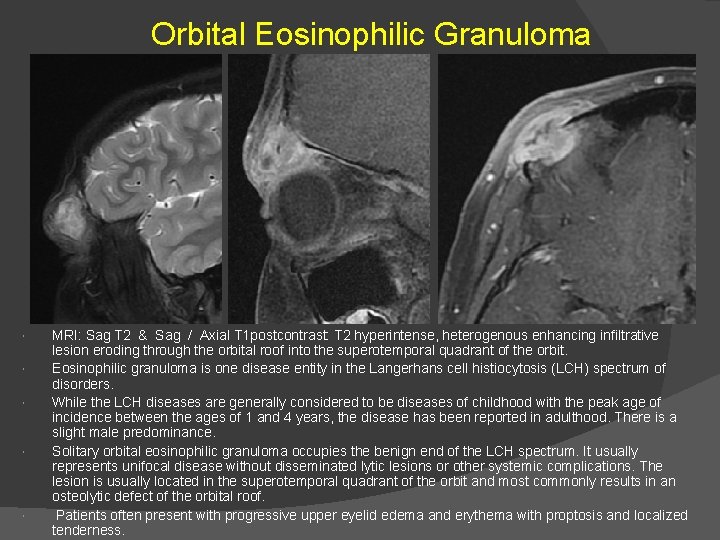
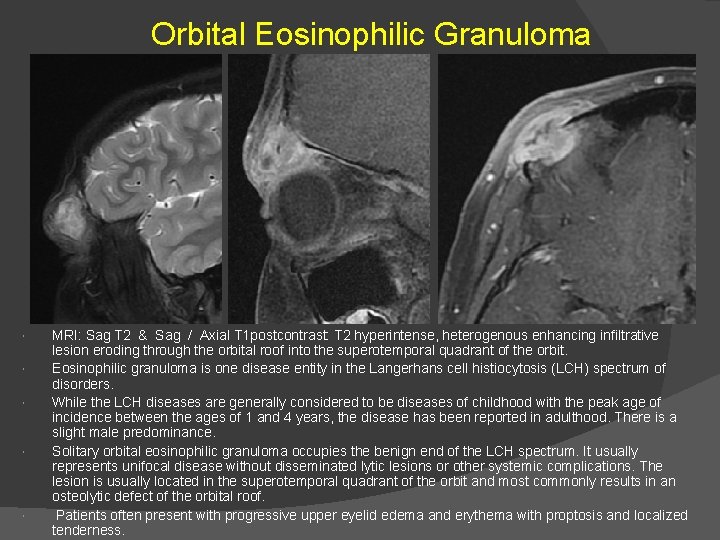
Orbital Eosinophilic Granuloma MRI: Sag T 2 & Sag / Axial T 1 postcontrast: T 2 hyperintense, heterogenous enhancing infiltrative lesion eroding through the orbital roof into the superotemporal quadrant of the orbit. Eosinophilic granuloma is one disease entity in the Langerhans cell histiocytosis (LCH) spectrum of disorders. While the LCH diseases are generally considered to be diseases of childhood with the peak age of incidence between the ages of 1 and 4 years, the disease has been reported in adulthood. There is a slight male predominance. Solitary orbital eosinophilic granuloma occupies the benign end of the LCH spectrum. It usually represents unifocal disease without disseminated lytic lesions or other systemic complications. The lesion is usually located in the superotemporal quadrant of the orbit and most commonly results in an osteolytic defect of the orbital roof. Patients often present with progressive upper eyelid edema and erythema with proptosis and localized tenderness.
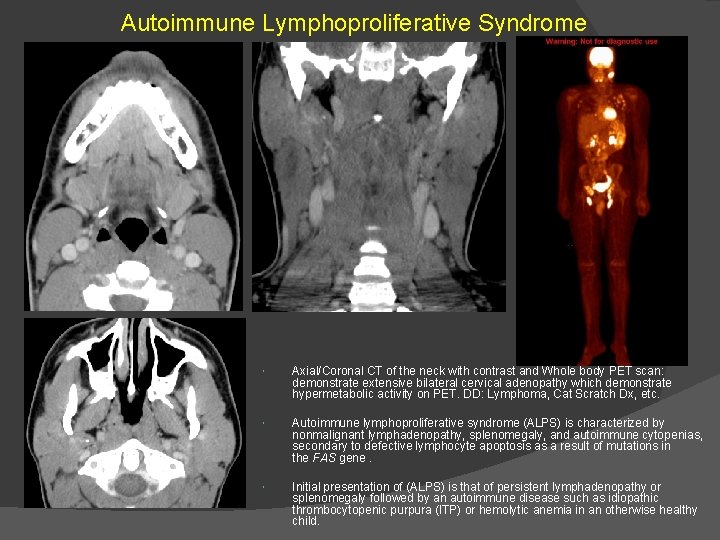
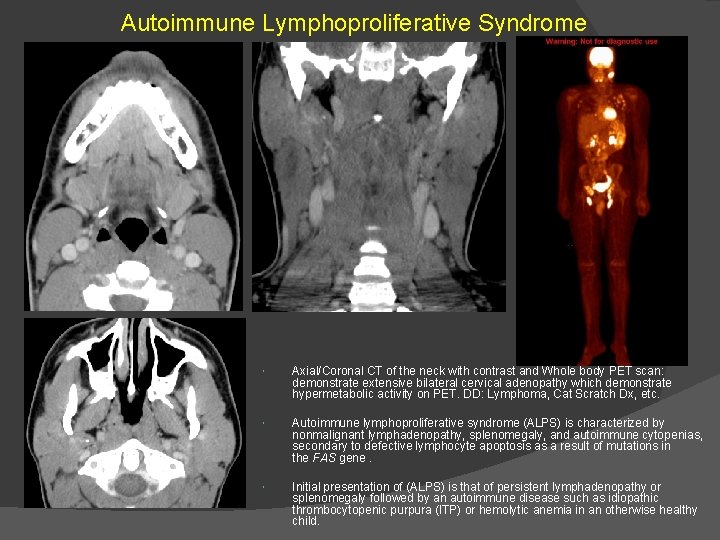
Autoimmune Lymphoproliferative Syndrome Axial/Coronal CT of the neck with contrast and Whole body PET scan: demonstrate extensive bilateral cervical adenopathy which demonstrate hypermetabolic activity on PET. DD: Lymphoma, Cat Scratch Dx, etc. Autoimmune lymphoproliferative syndrome (ALPS) is characterized by nonmalignant lymphadenopathy, splenomegaly, and autoimmune cytopenias, secondary to defective lymphocyte apoptosis as a result of mutations in the FAS gene. Initial presentation of (ALPS) is that of persistent lymphadenopathy or splenomegaly followed by an autoimmune disease such as idiopathic thrombocytopenic purpura (ITP) or hemolytic anemia in an otherwise healthy child.
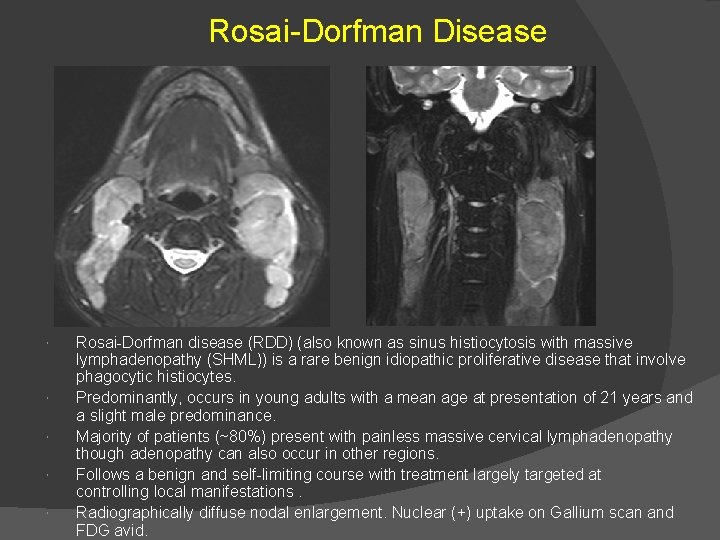
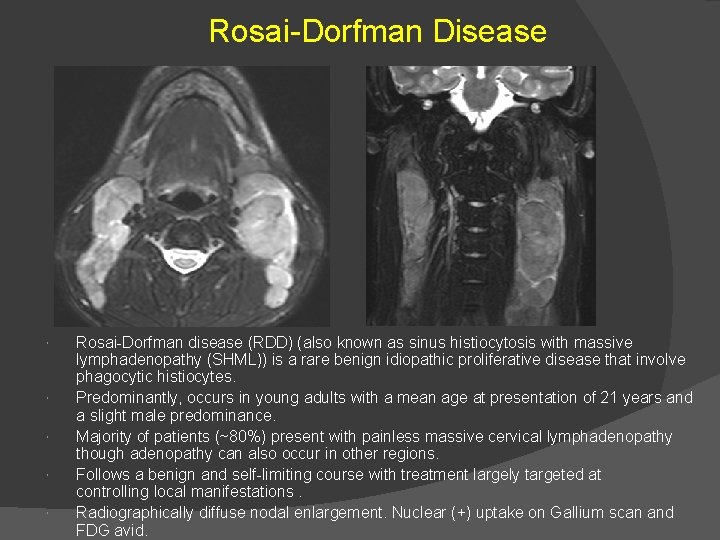
Rosai-Dorfman Disease Rosai-Dorfman disease (RDD) (also known as sinus histiocytosis with massive lymphadenopathy (SHML)) is a rare benign idiopathic proliferative disease that involve phagocytic histiocytes. Predominantly, occurs in young adults with a mean age at presentation of 21 years and a slight male predominance. Majority of patients (~80%) present with painless massive cervical lymphadenopathy though adenopathy can also occur in other regions. Follows a benign and self-limiting course with treatment largely targeted at controlling local manifestations. Radiographically diffuse nodal enlargement. Nuclear (+) uptake on Gallium scan and FDG avid.
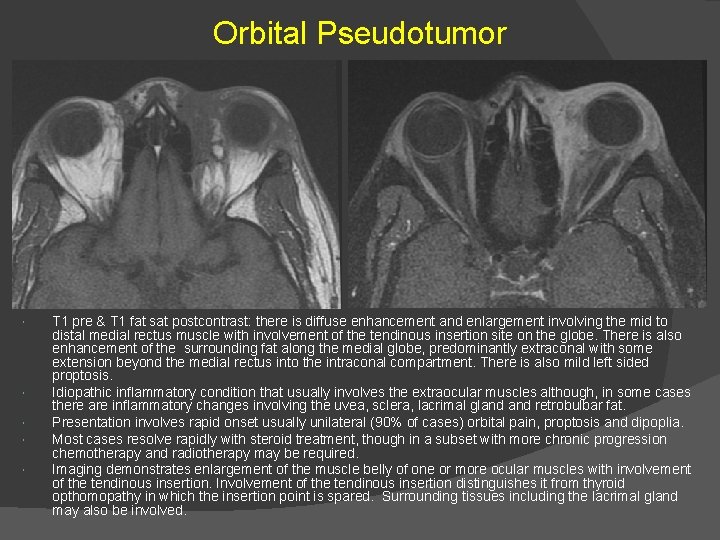
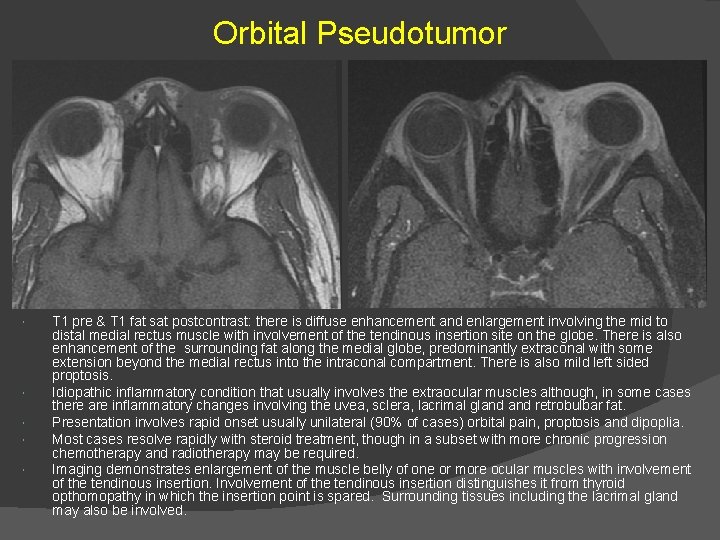
Orbital Pseudotumor T 1 pre & T 1 fat sat postcontrast: there is diffuse enhancement and enlargement involving the mid to distal medial rectus muscle with involvement of the tendinous insertion site on the globe. There is also enhancement of the surrounding fat along the medial globe, predominantly extraconal with some extension beyond the medial rectus into the intraconal compartment. There is also mild left sided proptosis. Idiopathic inflammatory condition that usually involves the extraocular muscles although, in some cases there are inflammatory changes involving the uvea, sclera, lacrimal gland retrobulbar fat. Presentation involves rapid onset usually unilateral (90% of cases) orbital pain, proptosis and dipoplia. Most cases resolve rapidly with steroid treatment, though in a subset with more chronic progression chemotherapy and radiotherapy may be required. Imaging demonstrates enlargement of the muscle belly of one or more ocular muscles with involvement of the tendinous insertion. Involvement of the tendinous insertion distinguishes it from thyroid opthomopathy in which the insertion point is spared. Surrounding tissues including the lacrimal gland may also be involved.
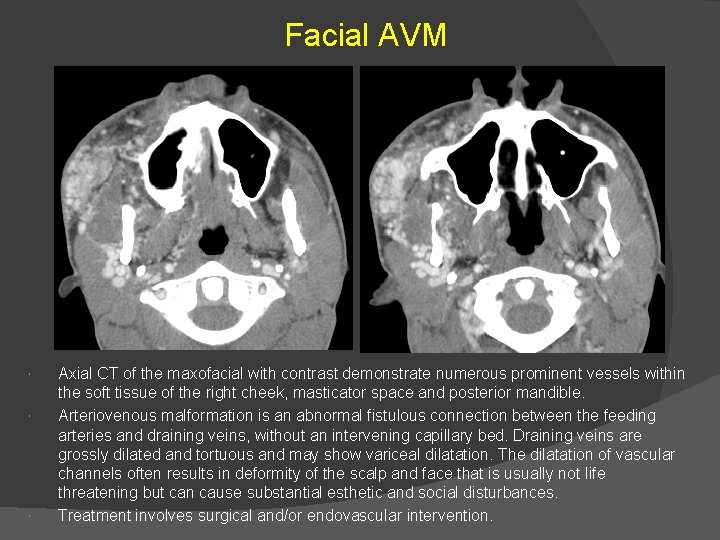
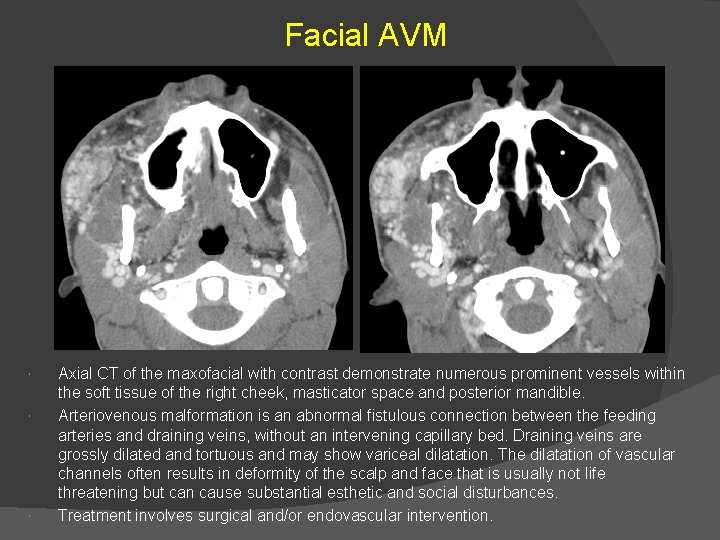
Facial AVM Axial CT of the maxofacial with contrast demonstrate numerous prominent vessels within the soft tissue of the right cheek, masticator space and posterior mandible. Arteriovenous malformation is an abnormal fistulous connection between the feeding arteries and draining veins, without an intervening capillary bed. Draining veins are grossly dilated and tortuous and may show variceal dilatation. The dilatation of vascular channels often results in deformity of the scalp and face that is usually not life threatening but can cause substantial esthetic and social disturbances. Treatment involves surgical and/or endovascular intervention.
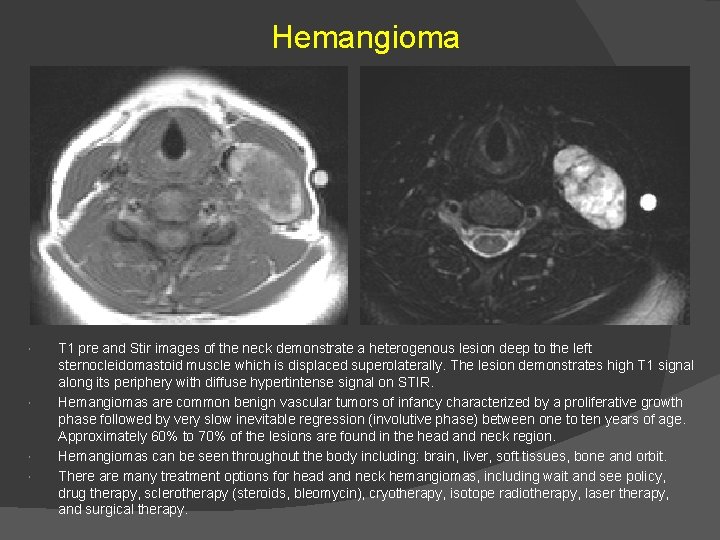
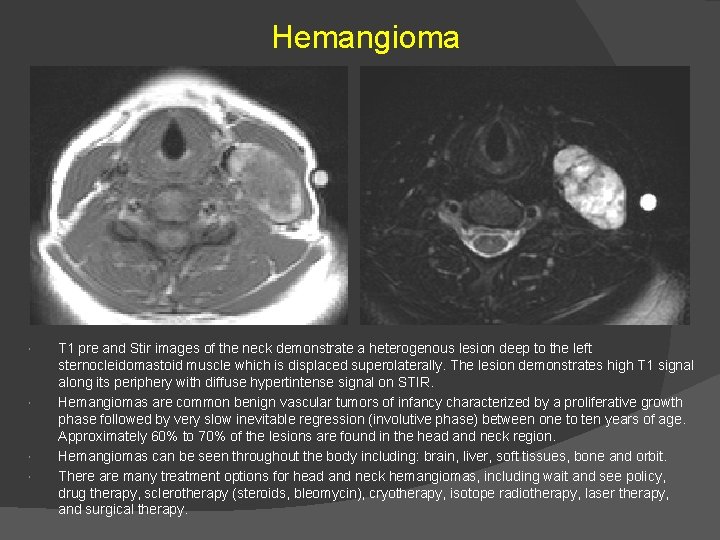
Hemangioma T 1 pre and Stir images of the neck demonstrate a heterogenous lesion deep to the left sternocleidomastoid muscle which is displaced superolaterally. The lesion demonstrates high T 1 signal along its periphery with diffuse hypertintense signal on STIR. Hemangiomas are common benign vascular tumors of infancy characterized by a proliferative growth phase followed by very slow inevitable regression (involutive phase) between one to ten years of age. Approximately 60% to 70% of the lesions are found in the head and neck region. Hemangiomas can be seen throughout the body including: brain, liver, soft tissues, bone and orbit. There are many treatment options for head and neck hemangiomas, including wait and see policy, drug therapy, sclerotherapy (steroids, bleomycin), cryotherapy, isotope radiotherapy, laser therapy, and surgical therapy.
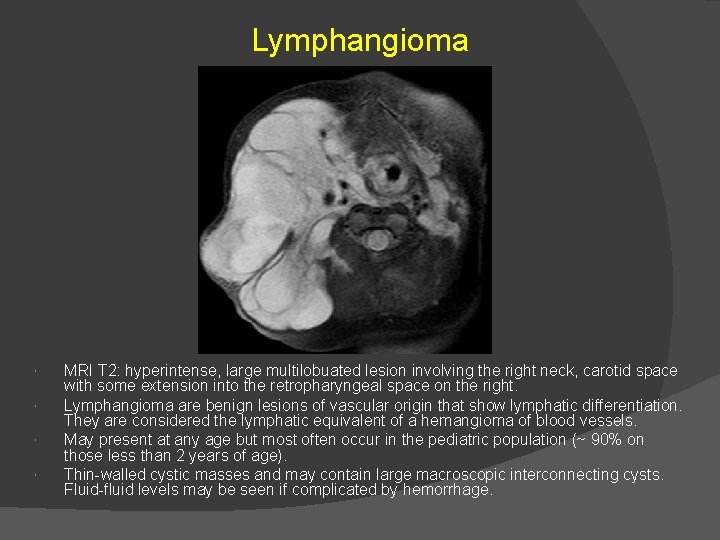
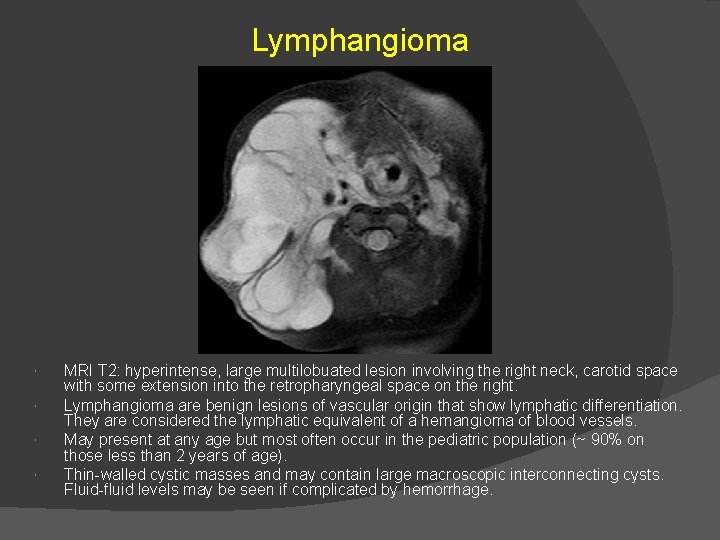
Lymphangioma MRI T 2: hyperintense, large multilobuated lesion involving the right neck, carotid space with some extension into the retropharyngeal space on the right. Lymphangioma are benign lesions of vascular origin that show lymphatic differentiation. They are considered the lymphatic equivalent of a hemangioma of blood vessels. May present at any age but most often occur in the pediatric population (~ 90% on those less than 2 years of age). Thin-walled cystic masses and may contain large macroscopic interconnecting cysts. Fluid-fluid levels may be seen if complicated by hemorrhage.
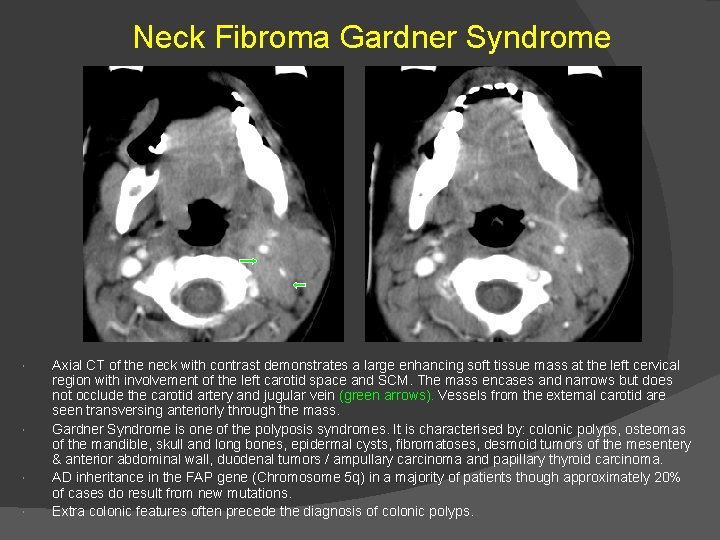
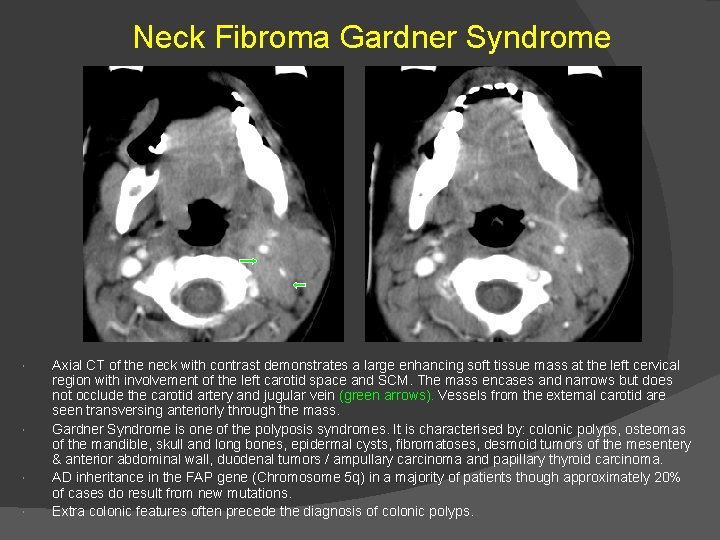
Neck Fibroma Gardner Syndrome Axial CT of the neck with contrast demonstrates a large enhancing soft tissue mass at the left cervical region with involvement of the left carotid space and SCM. The mass encases and narrows but does not occlude the carotid artery and jugular vein (green arrows). Vessels from the external carotid are seen transversing anteriorly through the mass. Gardner Syndrome is one of the polyposis syndromes. It is characterised by: colonic polyps, osteomas of the mandible, skull and long bones, epidermal cysts, fibromatoses, desmoid tumors of the mesentery & anterior abdominal wall, duodenal tumors / ampullary carcinoma and papillary thyroid carcinoma. AD inheritance in the FAP gene (Chromosome 5 q) in a majority of patients though approximately 20% of cases do result from new mutations. Extra colonic features often precede the diagnosis of colonic polyps.
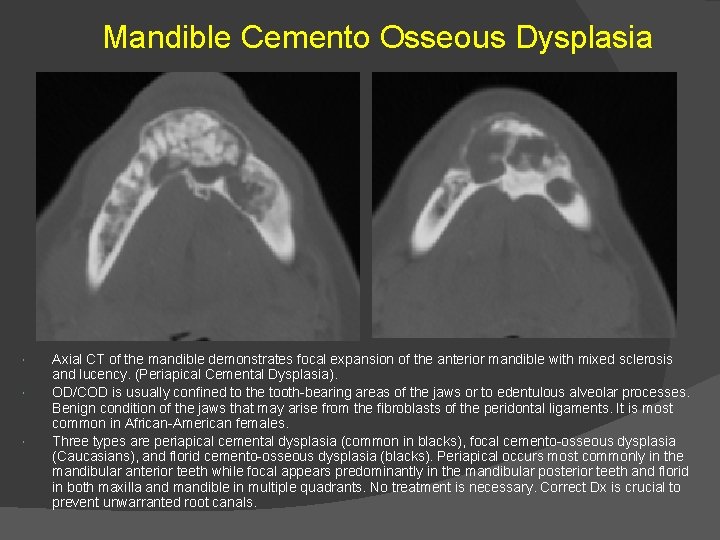
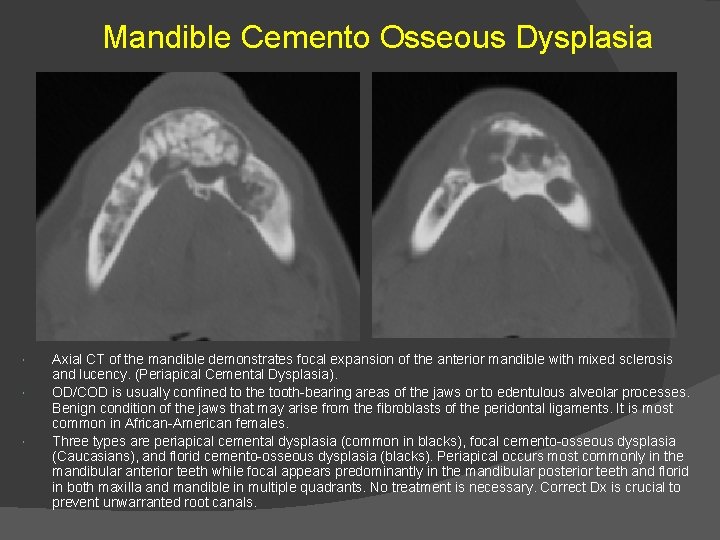
Mandible Cemento Osseous Dysplasia Axial CT of the mandible demonstrates focal expansion of the anterior mandible with mixed sclerosis and lucency. (Periapical Cemental Dysplasia). OD/COD is usually confined to the tooth-bearing areas of the jaws or to edentulous alveolar processes. Benign condition of the jaws that may arise from the fibroblasts of the peridontal ligaments. It is most common in African-American females. Three types are periapical cemental dysplasia (common in blacks), focal cemento-osseous dysplasia (Caucasians), and florid cemento-osseous dysplasia (blacks). Periapical occurs most commonly in the mandibular anterior teeth while focal appears predominantly in the mandibular posterior teeth and florid in both maxilla and mandible in multiple quadrants. No treatment is necessary. Correct Dx is crucial to prevent unwarranted root canals.
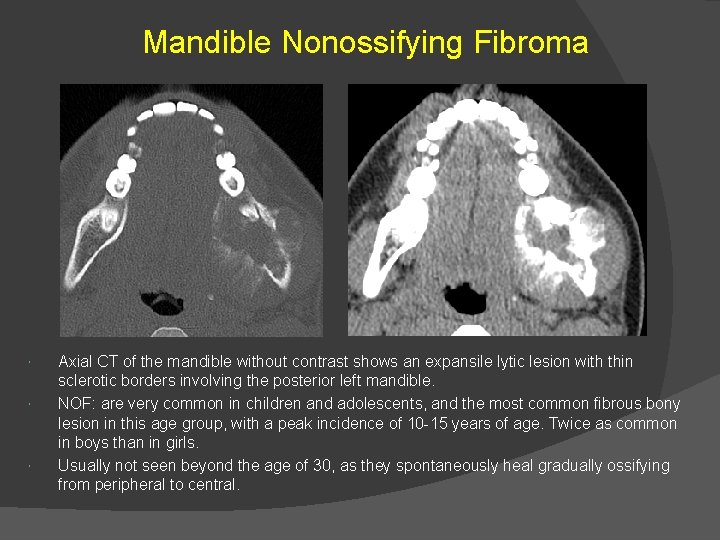
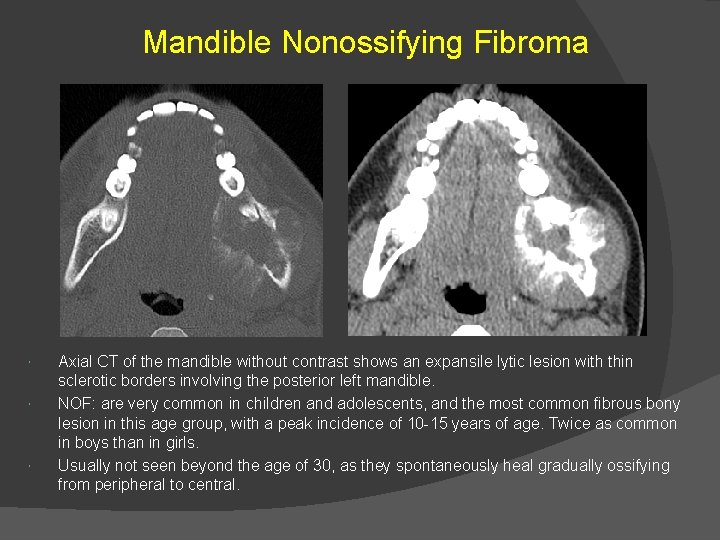
Mandible Nonossifying Fibroma Axial CT of the mandible without contrast shows an expansile lytic lesion with thin sclerotic borders involving the posterior left mandible. NOF: are very common in children and adolescents, and the most common fibrous bony lesion in this age group, with a peak incidence of 10 -15 years of age. Twice as common in boys than in girls. Usually not seen beyond the age of 30, as they spontaneously heal gradually ossifying from peripheral to central.
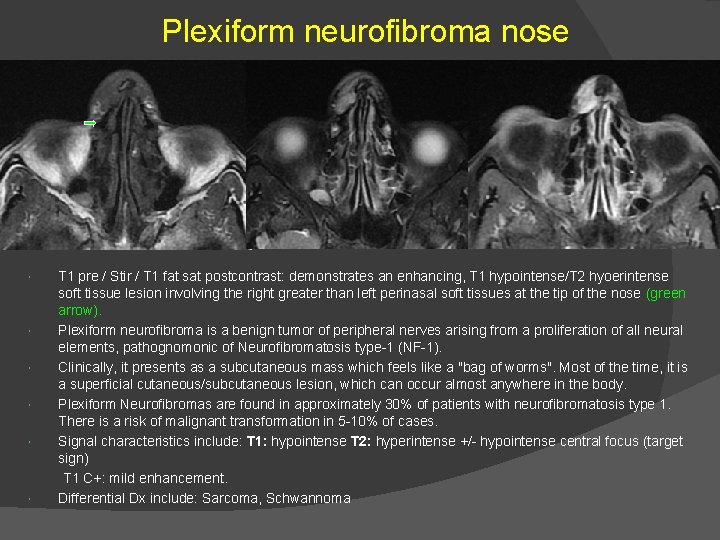
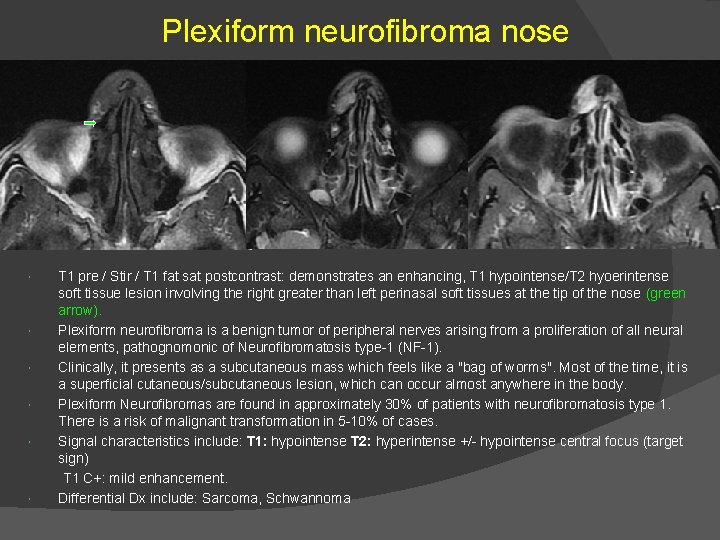
Plexiform neurofibroma nose T 1 pre / Stir / T 1 fat sat postcontrast: demonstrates an enhancing, T 1 hypointense/T 2 hyoerintense soft tissue lesion involving the right greater than left perinasal soft tissues at the tip of the nose (green arrow). Plexiform neurofibroma is a benign tumor of peripheral nerves arising from a proliferation of all neural elements, pathognomonic of Neurofibromatosis type-1 (NF-1). Clinically, it presents as a subcutaneous mass which feels like a "bag of worms". Most of the time, it is a superficial cutaneous/subcutaneous lesion, which can occur almost anywhere in the body. Plexiform Neurofibromas are found in approximately 30% of patients with neurofibromatosis type 1. There is a risk of malignant transformation in 5 -10% of cases. Signal characteristics include: T 1: hypointense T 2: hyperintense +/- hypointense central focus (target sign) T 1 C+: mild enhancement. Differential Dx include: Sarcoma, Schwannoma
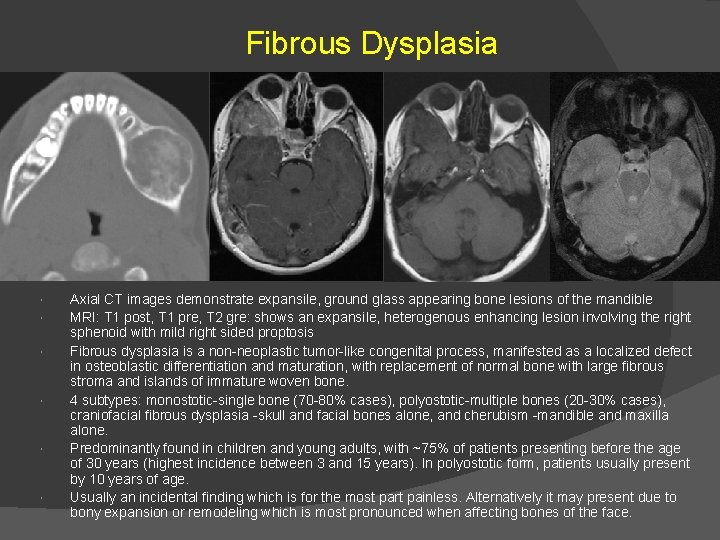
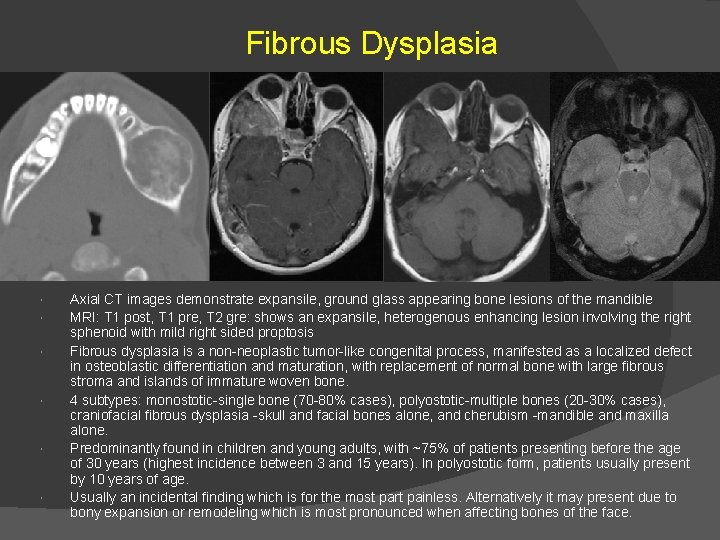
Fibrous Dysplasia Axial CT images demonstrate expansile, ground glass appearing bone lesions of the mandible MRI: T 1 post, T 1 pre, T 2 gre: shows an expansile, heterogenous enhancing lesion involving the right sphenoid with mild right sided proptosis Fibrous dysplasia is a non-neoplastic tumor-like congenital process, manifested as a localized defect in osteoblastic differentiation and maturation, with replacement of normal bone with large fibrous stroma and islands of immature woven bone. 4 subtypes: monostotic-single bone (70 -80% cases), polyostotic-multiple bones (20 -30% cases), craniofacial fibrous dysplasia -skull and facial bones alone, and cherubism -mandible and maxilla alone. Predominantly found in children and young adults, with ~75% of patients presenting before the age of 30 years (highest incidence between 3 and 15 years). In polyostotic form, patients usually present by 10 years of age. Usually an incidental finding which is for the most part painless. Alternatively it may present due to bony expansion or remodeling which is most pronounced when affecting bones of the face.
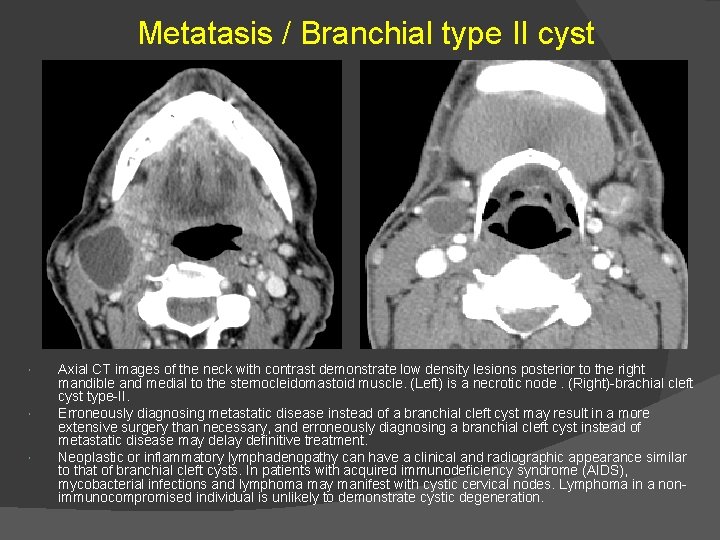
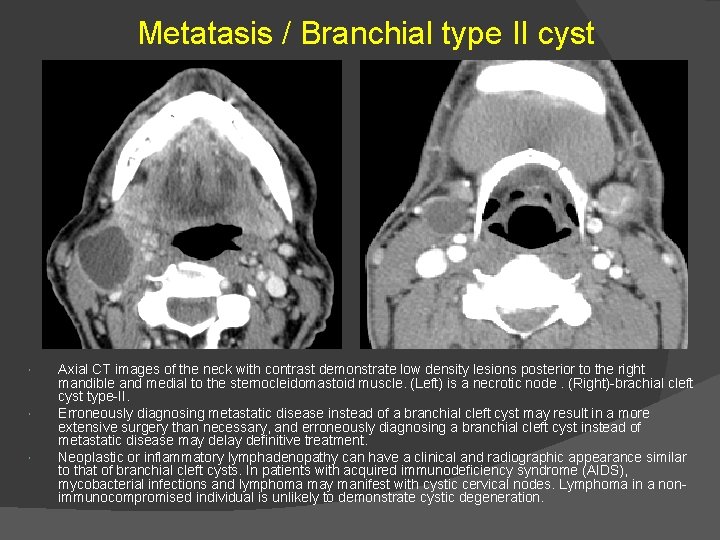
Metatasis / Branchial type II cyst Axial CT images of the neck with contrast demonstrate low density lesions posterior to the right mandible and medial to the sternocleidomastoid muscle. (Left) is a necrotic node. (Right)-brachial cleft cyst type-II. Erroneously diagnosing metastatic disease instead of a branchial cleft cyst may result in a more extensive surgery than necessary, and erroneously diagnosing a branchial cleft cyst instead of metastatic disease may delay definitive treatment. Neoplastic or inflammatory lymphadenopathy can have a clinical and radiographic appearance similar to that of branchial cleft cysts. In patients with acquired immunodeficiency syndrome (AIDS), mycobacterial infections and lymphoma may manifest with cystic cervical nodes. Lymphoma in a nonimmunocompromised individual is unlikely to demonstrate cystic degeneration.
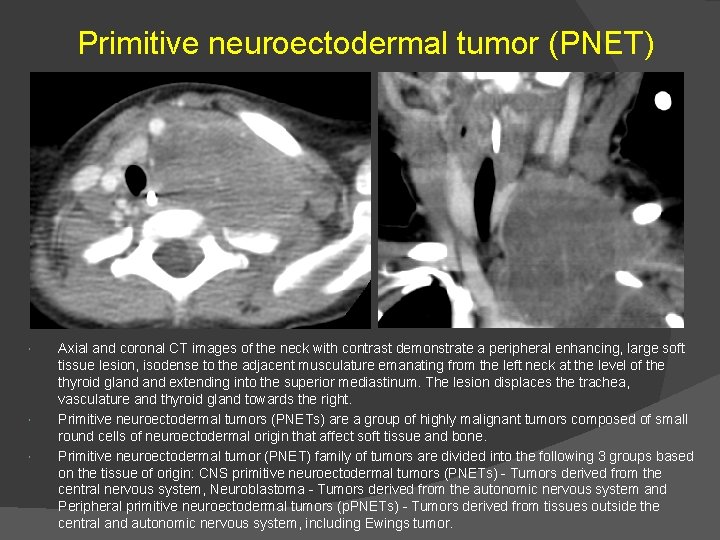
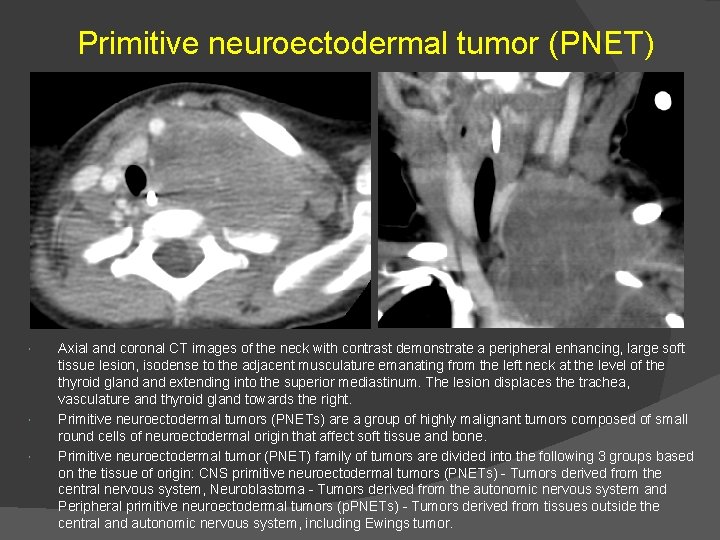
Primitive neuroectodermal tumor (PNET) Axial and coronal CT images of the neck with contrast demonstrate a peripheral enhancing, large soft tissue lesion, isodense to the adjacent musculature emanating from the left neck at the level of the thyroid gland extending into the superior mediastinum. The lesion displaces the trachea, vasculature and thyroid gland towards the right. Primitive neuroectodermal tumors (PNETs) are a group of highly malignant tumors composed of small round cells of neuroectodermal origin that affect soft tissue and bone. Primitive neuroectodermal tumor (PNET) family of tumors are divided into the following 3 groups based on the tissue of origin: CNS primitive neuroectodermal tumors (PNETs) - Tumors derived from the central nervous system, Neuroblastoma - Tumors derived from the autonomic nervous system and Peripheral primitive neuroectodermal tumors (p. PNETs) - Tumors derived from tissues outside the central and autonomic nervous system, including Ewings tumor.
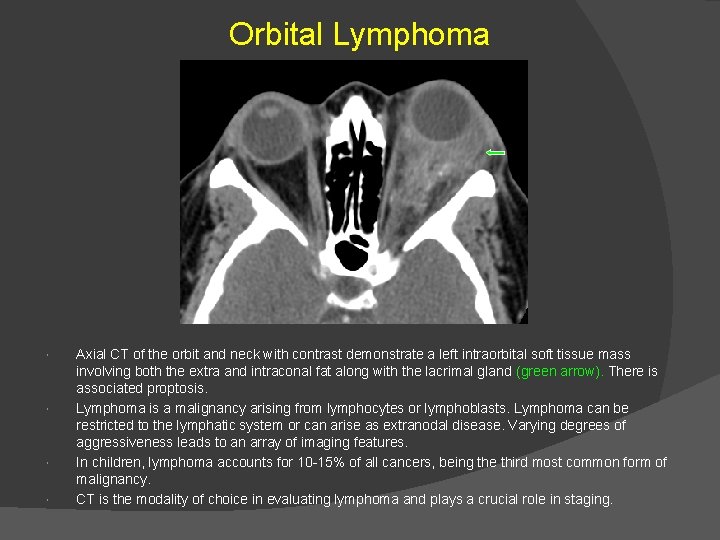
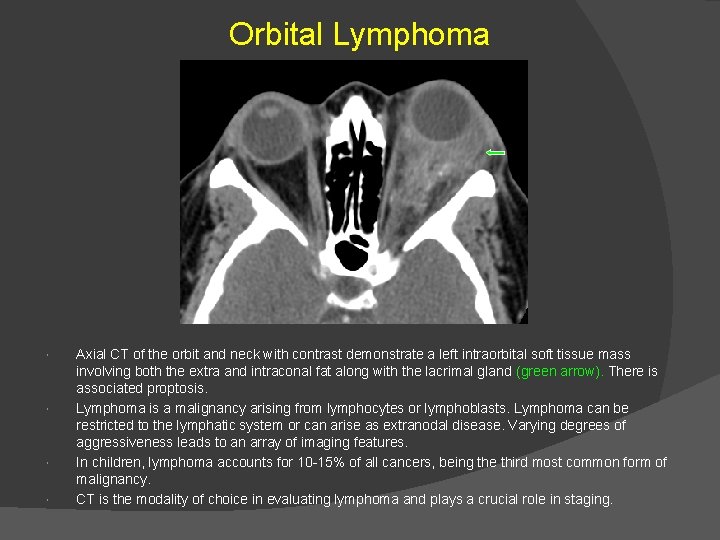
Orbital Lymphoma Axial CT of the orbit and neck with contrast demonstrate a left intraorbital soft tissue mass involving both the extra and intraconal fat along with the lacrimal gland (green arrow). There is associated proptosis. Lymphoma is a malignancy arising from lymphocytes or lymphoblasts. Lymphoma can be restricted to the lymphatic system or can arise as extranodal disease. Varying degrees of aggressiveness leads to an array of imaging features. In children, lymphoma accounts for 10 -15% of all cancers, being the third most common form of malignancy. CT is the modality of choice in evaluating lymphoma and plays a crucial role in staging.
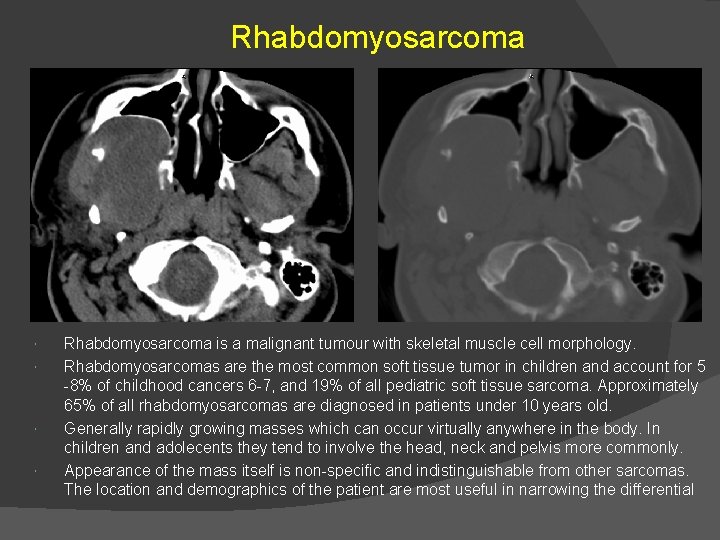
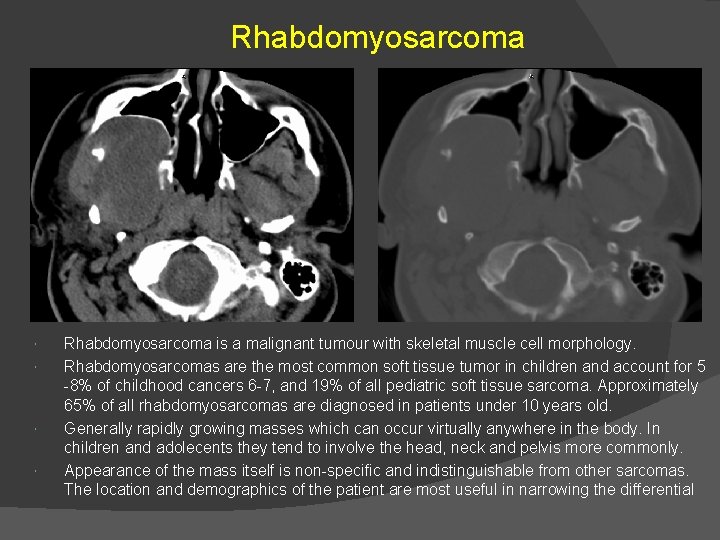
Rhabdomyosarcoma is a malignant tumour with skeletal muscle cell morphology. Rhabdomyosarcomas are the most common soft tissue tumor in children and account for 5 -8% of childhood cancers 6 -7, and 19% of all pediatric soft tissue sarcoma. Approximately 65% of all rhabdomyosarcomas are diagnosed in patients under 10 years old. Generally rapidly growing masses which can occur virtually anywhere in the body. In children and adolecents they tend to involve the head, neck and pelvis more commonly. Appearance of the mass itself is non-specific and indistinguishable from other sarcomas. The location and demographics of the patient are most useful in narrowing the differential
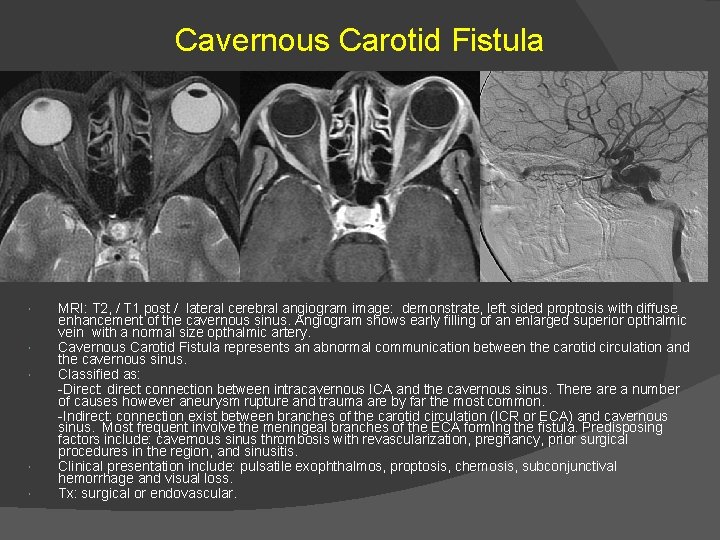
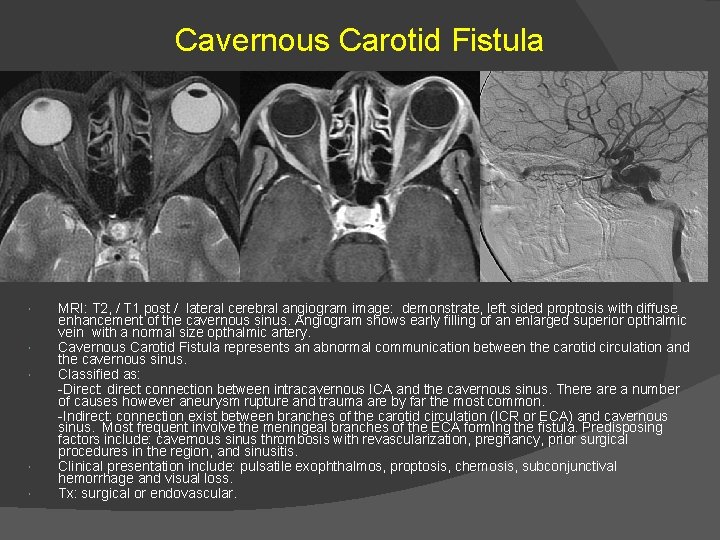
Cavernous Carotid Fistula MRI: T 2, / T 1 post / lateral cerebral angiogram image: demonstrate, left sided proptosis with diffuse enhancement of the cavernous sinus. Angiogram shows early filling of an enlarged superior opthalmic vein with a normal size opthalmic artery. Cavernous Carotid Fistula represents an abnormal communication between the carotid circulation and the cavernous sinus. Classified as: -Direct: direct connection between intracavernous ICA and the cavernous sinus. There a number of causes however aneurysm rupture and trauma are by far the most common. -Indirect: connection exist between branches of the carotid circulation (ICR or ECA) and cavernous sinus. Most frequent involve the meningeal branches of the ECA forming the fistula. Predisposing factors include: cavernous sinus thrombosis with revascularization, pregnancy, prior surgical procedures in the region, and sinusitis. Clinical presentation include: pulsatile exophthalmos, proptosis, chemosis, subconjunctival hemorrhage and visual loss. Tx: surgical or endovascular.
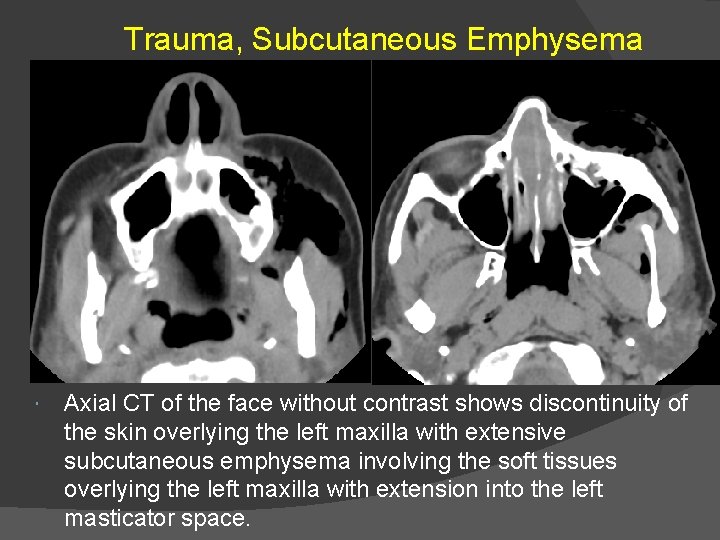
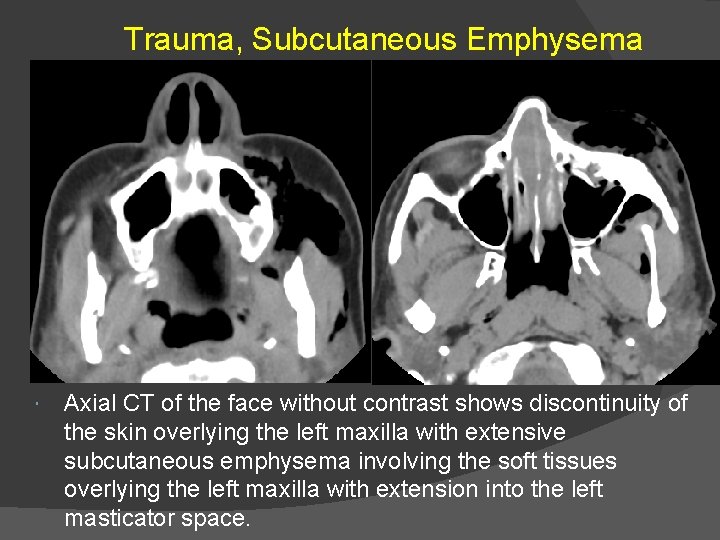
Trauma, Subcutaneous Emphysema Axial CT of the face without contrast shows discontinuity of the skin overlying the left maxilla with extensive subcutaneous emphysema involving the soft tissues overlying the left maxilla with extension into the left masticator space.
 Anterior neck swelling differential diagnosis
Anterior neck swelling differential diagnosis Scalp swelling differential diagnosis
Scalp swelling differential diagnosis Pharmacology and venipuncture in radiology pdf
Pharmacology and venipuncture in radiology pdf Apical pulmonar
Apical pulmonar El camino rad tech
El camino rad tech Facial vein and facial artery
Facial vein and facial artery Second phase of nursing process
Second phase of nursing process Nursing process and critical thinking
Nursing process and critical thinking Types of nursing diagnosis
Types of nursing diagnosis Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference What this
What this Leonardo da vinci face proportions
Leonardo da vinci face proportions Pediatric dysphagia goals
Pediatric dysphagia goals Nyhus classification
Nyhus classification Brilliantly translucent swelling
Brilliantly translucent swelling Mitochondrial swelling
Mitochondrial swelling Iv site pain and swelling
Iv site pain and swelling Cellulitis nose
Cellulitis nose Polimastia ascellare
Polimastia ascellare Salivary gland swelling
Salivary gland swelling Complication of iv infusion
Complication of iv infusion Lymph nodes swelling in stomach
Lymph nodes swelling in stomach Enophthalmos definition
Enophthalmos definition Potato tumor
Potato tumor What is a soliloquy?
What is a soliloquy? Fibrin cuff theory
Fibrin cuff theory Cross fluctuation swelling
Cross fluctuation swelling Liver cirrhosis
Liver cirrhosis Periarticular soft tissue swelling
Periarticular soft tissue swelling Level 3 electrical facial
Level 3 electrical facial Nervo auricular
Nervo auricular Hd clear kit
Hd clear kit Mesenchyme cells
Mesenchyme cells Foramen infraorbitalis
Foramen infraorbitalis Facial expression recognition
Facial expression recognition