NECK 2 CLASS 11 22092015 ANATOMY OF NECK








- Slides: 33
NECK 2 CLASS 11 22/09/2015
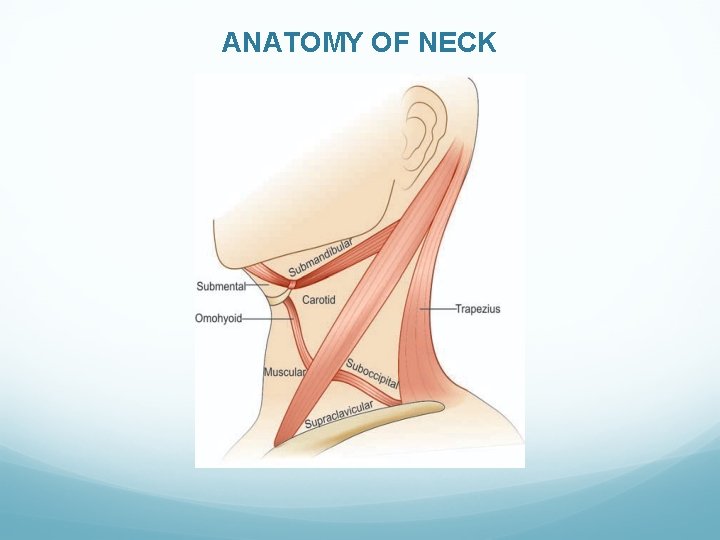
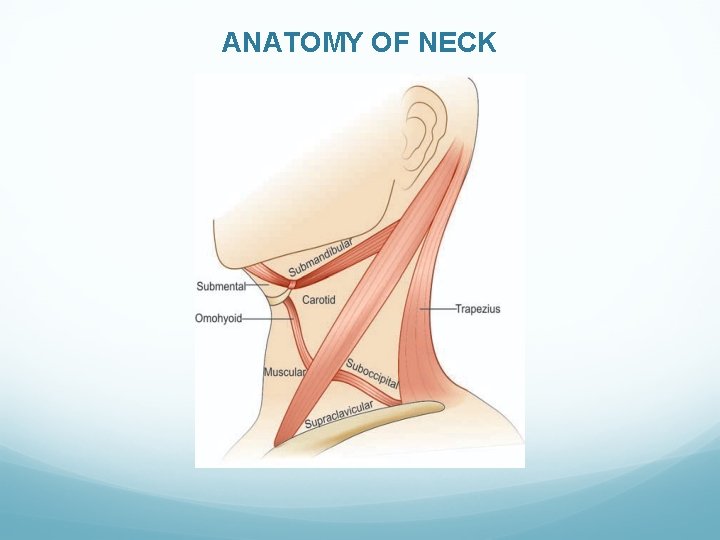
ANATOMY OF NECK

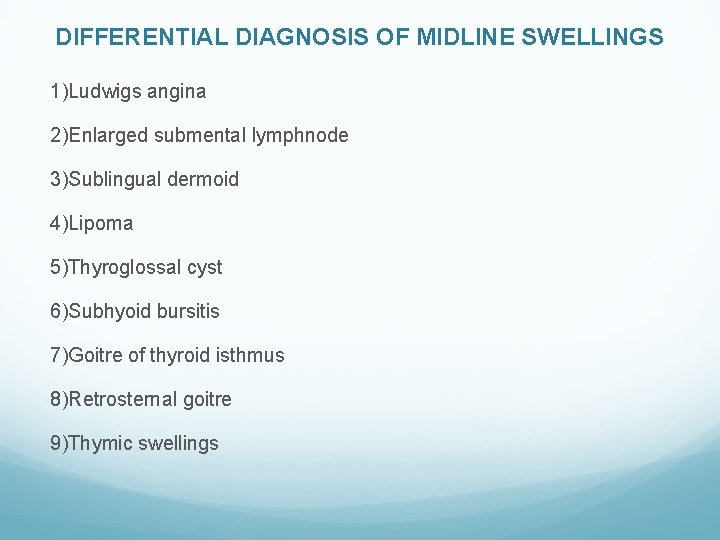
DIFFERENTIAL DIAGNOSIS OF MIDLINE SWELLINGS 1)Ludwigs angina 2)Enlarged submental lymphnode 3)Sublingual dermoid 4)Lipoma 5)Thyroglossal cyst 6)Subhyoid bursitis 7)Goitre of thyroid isthmus 8)Retrosternal goitre 9)Thymic swellings
LUDWIG’S ANGINA It is an inflammatory oedema of submandibular region and floor of the mouth. Streptococcal infection. It causes diffuse swelling and brawny oedema of the submandibular region. It is common in severely ill and in advanced malignancy, causing trismus, laryngeal oedema. Extension of infection into para-pharyngeal space may lead to dreaded internal jugular vein thrombosis.
As the infection is deep to the deep fascia in a closed fascial plane, it spreads very fast causing dangerous complications. Precipitating factors • Caries teeth • Oral or other malignancy • Submandibular salivary infection/calculi • Chemotherapy • Chronic diseases like diabetes mellitus • Cachexia of any cause

Clinical Features • Fever, toxicity, diffuse swelling, dysphagia, dyspnoea, trismus. • Intraoral oedema is common. • Brawny swelling in submandibular region. • Putrid halitosis.
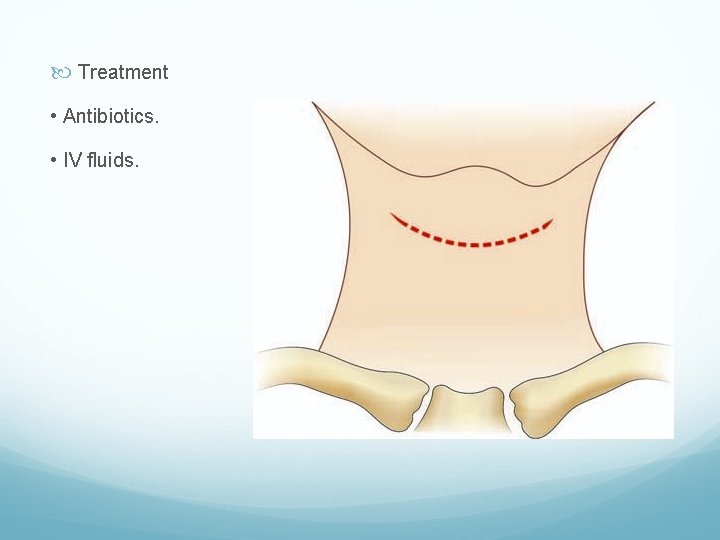
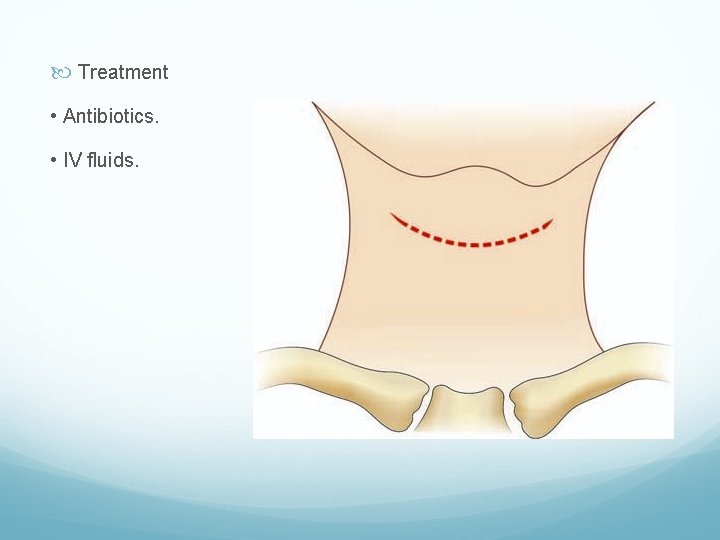
Treatment • Antibiotics. • IV fluids.
Decompression of the submandibular region is done, by making a deep incision extending into the deep fascia and also cutting both the mylohyoid muscles. Either it is left open and delayed suturing is done (better option) or it is loosely sutured. Complications 1. Laryngeal oedema and respiratory distress, may require tracheostomy 2. Septicaemia 3. Extension of infection into parapharyngeal space.
SUBHYOID BURSITIS Subhyoid bursa is space between posterior surface of the body of hyoid bone and thyrohyoid membrane. It lessens friction between these two structures during swallowing. Due to constant friction inflammatory fluid collects in the bursa leading to bursitis, which presents like a horizontally placed midline swelling between lower part of the hyoid bone and thyrohyoid membrane.

Features • Smooth, soft, cystic, fluctuant, non-transilluminating swelling which moves upwards with deglutition but not while protruding the tongue out. • It should be differentiated from thyroglossal cyst and pretracheal lymph nodes. • It contains turbid fluid often may get infected to make the swelling tender or to form an abscess.
Treatment • Excision under general anaesthesia.
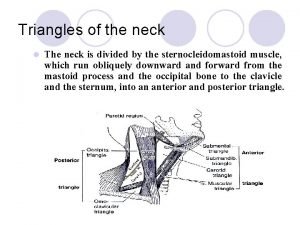
DIFFERENTIAL DIAGNOSIS OF ANTERIOR TRIANGLE SWELLINGS 1) Cold abscess 2) Branchial cyst 3) Carotid body tumor 4) Carotid aneurysm

CAROTID BODY TUMOUR Potato tumour/Chemodectoma/Non-chromaffin para-ganglioma. Carotid body– • Normal carotid body is 3 -5 mm sized flat brownish nodule in the adventitious of common carotid artery • It consists of chief cells (contains catecholamine granules) and supportive cells • It gets its nerve supply from glossopharyngeal nerve • These chemoreceptors are sensitive to changes in p. H and temperature in the body especially in hypoxia, help in autoregulation of respiration and circulation.
Carotid body hyperplasia can occur in people residing in high altitudes who are exposed to chronic hypoxia. • Other chemoreceptors in the body are – aortic bodies in the arch of aorta; glomus jugular in the bulb of the internal jugular vein; glomus intravagale in relation to ganglion nodosum of the vagus nerve and others like pulmonary (near pulmonary artery) and myocardial (near coronary artery origin) receptors.
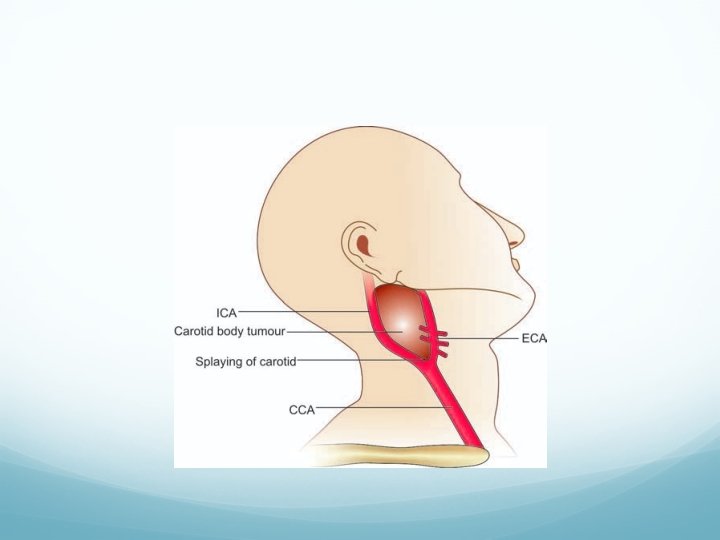
The tumour is situated in the adventitia of the artery. • They are benign or locally malignant tumours, but in 20% cases spread can occur to the regional lymph nodes and lungs. • Blood supply to the tumour is from external carotid artery. Tumour does not secrete epinephrine or any endocrine substances. • They can be familial. • Common in high altitude area, common in females. • Pathologically, it is well-encapsulated, hard creamy yellowish tumour with dense fibrous tissue. Carotid body tumour cells are not hormonally active.
Clinical Features (0. 5%–Incidence) 1. Usually unilateral. 2. More common in middle age. 3. Swelling in the carotid region of the neck which is smooth, firm, pulsatile (transmitted pulsation—due to pulsatile carotid vessel overlying its surface) and moves only side to side but not in vertical direction. 4. Features of transient ischaemic attacks due to compression over the carotids, “carotid body syncope. ”
5. Thrill may be felt and bruit may be heard. 6. It is located at the level of hyoid bone deep to anterior edge of the sternomastoid muscle in anterior triangle, vertically placed, round, firm ‘potato’ like swelling. Often tumour may extend into the cranial cavity along the internal carotid artery as dumbbell tumour.
Shamblin classification of carotid body tumor • Type I– Localised, easily resectable (26%) • Type II– Adherent, partially surrounding the carotids (46%) • Type III– Adherent, encased carotids completely (27%)
Investigations • Doppler. • Angiogram to see the ‘tumour blush’—DSA. Widening/ splaying of the carotid artery with tumour blush in an angiogram is called as Lyre sign. • CT scan, MRI. No FNAC: No partial excision.
Treatment • If it is small, it can be excised easily as the tumour is situated in the adventitia. • When it is large, as commonly observed, complete excision has to be done followed by placing a vascular graft. • Carotid body tumour is not radiosensitive (controversial).
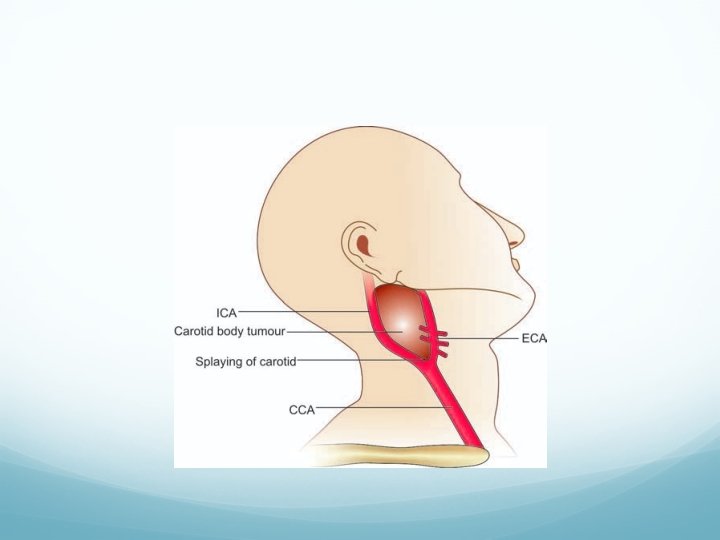
Complications of the Surgery • Bleeding. • Blockage of common carotid artery, leading to contralateral side hemiplegia. This can be prevented by stenting the common carotid artery towards internal carotid artery and is done during surgical excision of the tumour.
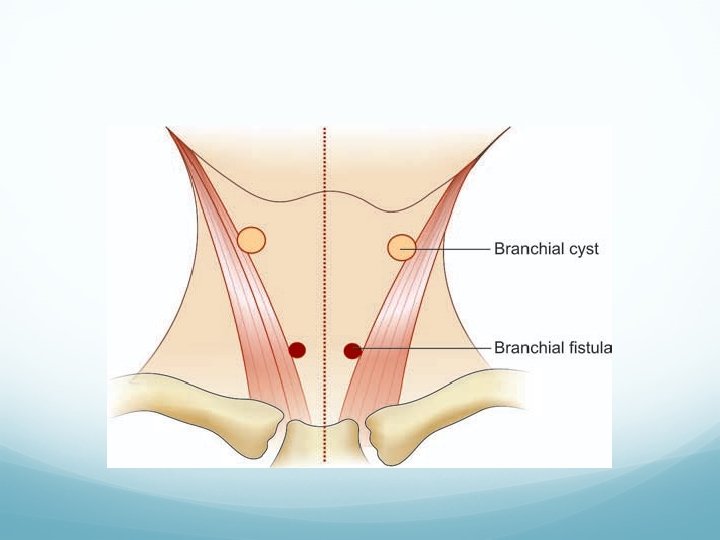
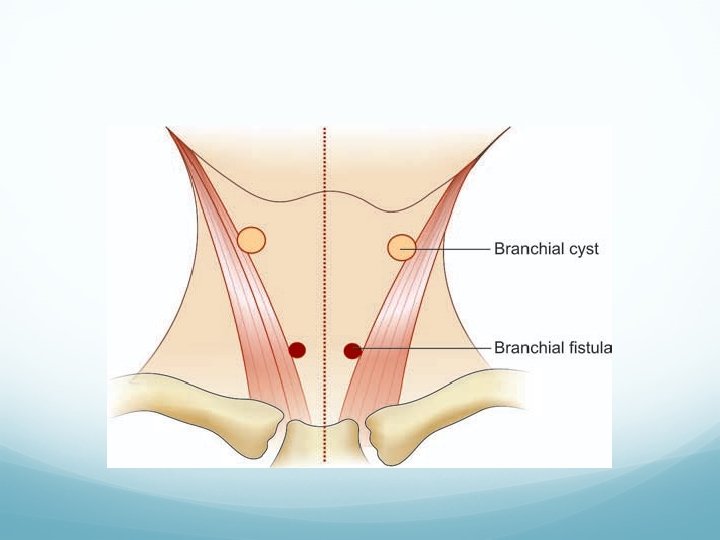
BRANCHIAL CYST It arises from the remnants of second branchial cleft. Normally 2 nd, 3 rd, 4 th clefts disappear to form a smooth neck. Persistent 2 nd cleft is called as cervical sinus which eventually gets sequestered to form branchial cyst. Features Swelling in the neck beneath the anterior border of upper third of the sternomastoid muscle. It is smooth, soft, fluctuant, often transilluminant with a sensation of ‘Half-filled double hot water bottle’.

It contains cholesterol crystals which is from the lining of mucous membrane which contains sebaceous gland. Histologically, it is lined by squamous epithelium. It may get infected to form an abscess. FNAC shows cholesterol crystals.
Treatment: Excision under G/A. Cyst is in relation to carotids, hypoglossal nerve, glossopharyngeal nerve, spinal accessory nerve, posterior belly of digastric and pharyngeal wall. Medially it is close to the posterior pillar of tonsils. Complications of Surgery • Injury to major structures. • Infection. • Recurrence/fistula formation due to incomplete removal of the track.
BRANCHIAL FISTULA It is a persistent second branchial cleft with a communication outside to the exterior. It is commonly a congenital fistula. Occasionally, the condition is secondary to incised, infected branchial cyst. Often it is bilateral. External orifice of the fistula is situated in the lower third of the neck near the anterior border of the sternomastoid muscle. Internal orifice is located on the anterior aspect of the posterior pillar of the fauces, just behind the tonsils.



Sometimes fistula ends internally as blind end. Track is lined by ciliated columnar epithelium with patches of lymphoid tissues beneath it, causing recurrent inflammation. Discharge is mucoid or mucopurulent. Investigations: Discharge study, fistulogram. Treatment: Always surgery.
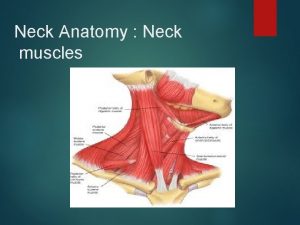
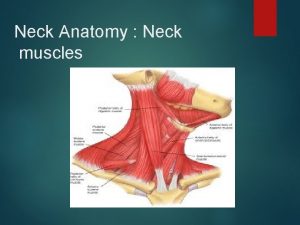
 Neck fascia
Neck fascia Midclavicular and midaxillary line
Midclavicular and midaxillary line Anatomy of the throat and neck
Anatomy of the throat and neck Fascia thoracolumbalis
Fascia thoracolumbalis Anatomy of a java class
Anatomy of a java class In today's class
In today's class Package mypackage class first class body
Package mypackage class first class body Introduction to ooad
Introduction to ooad Lower boundary of modal class
Lower boundary of modal class Class i vs class ii mhc
Class i vs class ii mhc Abstract concrete class relationship
Abstract concrete class relationship Frequency distribution table
Frequency distribution table Response class vs stimulus class
Response class vs stimulus class Stimulus class vs response class
Stimulus class vs response class Therapeutic class and pharmacologic class
Therapeutic class and pharmacologic class Class maths student student1 class student string name
Class maths student student1 class student string name Unordered stem and leaf plot
Unordered stem and leaf plot In greenfoot, you can cast an actor class to a world class?
In greenfoot, you can cast an actor class to a world class? Static and dynamic class loading in java
Static and dynamic class loading in java Class 0 esd
Class 0 esd Static uml diagrams
Static uml diagrams Class 2 class 3
Class 2 class 3 Public class test subject extends test class
Public class test subject extends test class Package mypackage class first class body
Package mypackage class first class body Class third class
Class third class Uml class diagram inner class
Uml class diagram inner class Component class has composite class as collaborator
Component class has composite class as collaborator Structural adaptations frilled neck lizard
Structural adaptations frilled neck lizard Neck anatomical term
Neck anatomical term L
L Naomi alexandra
Naomi alexandra “the american embassy” by chimamanda ngozi adichie
“the american embassy” by chimamanda ngozi adichie Stomach layers histology
Stomach layers histology Neck righting reflex
Neck righting reflex