Plasma Cell Dyscrasias Miten R Patel MD Cancer




- Slides: 41
Plasma Cell Dyscrasias Miten R. Patel, MD Cancer Specialists of North Florida

Disclosures • None
Objectives • • • Review types of Plasma cell dyscrasias Epidemiology and definitions Presenting signs and symptoms Myeloma staging Couple of cases Treatment overview
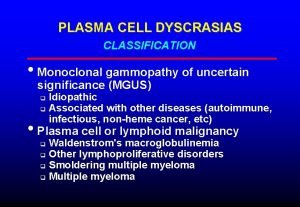
Plasma Cell Dyscrasias • Monoclonal Gammopathy of Unknown Significance (MGUS) • Smoldering Myeloma (SMM) • Multiple Myeloma (MM) • Waldenstroms Macroglobulinemia (WM) • Amyloidosis • Solitary plasmacytoma • POEMS syndrome
MGUS • Mean age at diagnosis – 70 yo • M>F, incidence increases with age, found in 1 -2% of adults • African Americans 2 -3 x > Caucasians • Present in 3% of persons >50 and 5% of persons over the age of 70 • Most cases sporadic but relatives of patients with MGUS/myeloma have an increased risk (RR 2 -3)
MGUS • Definition – Serum monoclonal protein <3 g/d. L, bone marrow plasma cells <10%, and absence of end organ damage • • Hypercalcemia Renal Failure Anemia/Thrombocytopenia Lytic bone lesions
MGUS • Non-Ig. M MGUS – Progresses to myeloma – Rarely, to AL amyloid, light chain disease or other lymphoproliferative disorder • Ig. M MGUS – Progresses to Waldenstroms macroglobulinemia – Rarely, to myeloma, AL amyloidosis or lymphoma
MGUS • Part of the spectrum of smoldering myeloma and multiple myeloma • Characterized by a monoclonal protein level of <30 g/L (m spike of 3. 0 g/d. L), <10% plasma cells in the bone marrow • Progression to MM or related disorder is about 1% per year. • Clinically asymptomatic premalignant condition
MGUS • No symptoms? – Pts. identified when undergoing testing for other conditions such as neuropathy, vasculitis, hemolytic anemia, rashes, hypercalcemia, elevated ESR, elevated total protein – Likely had existed for years before diagnosis – Finding on labs - usually elevated total protein, immunoglobulin, abnormal SPEP/UPEP, positive IFE, or abnormal light chain ratio
MGUS – Workup • Labs - CBC + diff, BMP (Cr, Ca), SPEP + IFE, Quant Igs, 24 urine IFE, B 2 microglobulin, albumin, serum free light chains • Imaging – Skeletal survey, Certain cases - MRI & PET scan • Bone Marrow biopsy & aspirate – Cytogenetics & FISH studies
MGUS • Once confirmed (Monoclonal protein <3 g/d. L, <10% plasma cells, no CRAB symptoms) – no treatment • Serial followup, every 3 -6 months, exam, assessment and labs, less often after 2 years. • Monitor for developing symptoms (bone pain, hypercalcemia, kidney dysfunction, anemia, etc) • SMM – every 3 months until progression • No treatment unless symptomatic MM
Smoldering Myeloma • Smoldering Myeloma (aka asymptomatic multiple myeloma) – Same as MM but without symptoms and • Hgb > 10. 5, • Monoclonal Ig Peak (usually > 3 g/d. L and/or >10 but <60% clonal plasma cells) • Normal serum Ca and Cr levels • No lytic bone lesions • REQUIRES NO TREATMENT • >60% plasma cells or FLC ratio >100 even without end organ damage, best classified as multiple myeloma
Multiple Myeloma • Presentation – Weakness, Fatigue, Pallor (32%) – Weight Loss (24%) – Radiculopathy, cord compression – Bone pain (58%), fractures – Recurrent infections (dysfunctional immunoglobulin) – Labs – Anemia (73%), hypercalcemia (28%), elevated total protein, kidney dysfunction (48%)
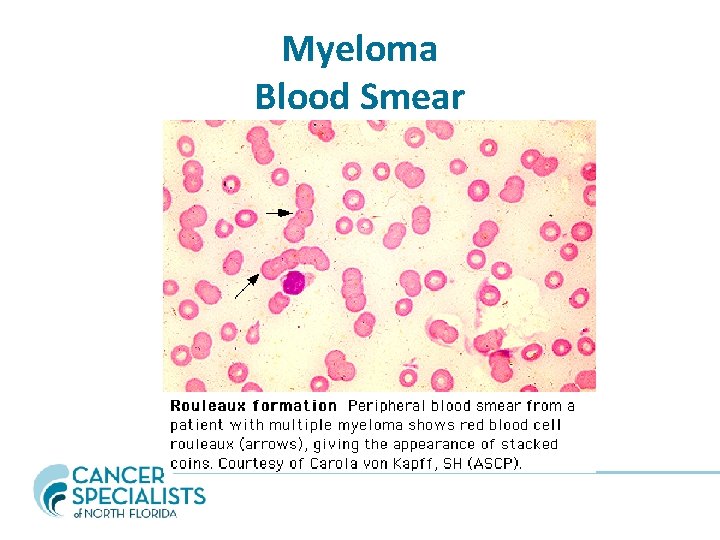
Multiple Myeloma Rouleaux Formation Elevated Sed Rate Elevated C Reactive Protein Normocytic, normochromic anemia Renal Disease, Cr > 2 mg/d. L in 19% Renal insufficiency caused by cast nephropathy (myeloma kidney) or hypercalcemia • Altered mental status caused by hypercalcemia and hyperviscosity • • •
Multiple Myeloma • Monoclonal Ig – – Ig. G 60% Ig. A 20% Light chain only 18% (K>L) Ig. M, Ig. D, Ig. E, non-secretory < 1% • For nonsecretory myeloma (no M protein) or light chain only, diagnosis is often made with bony lesions and plasmacytosis by bone marrow
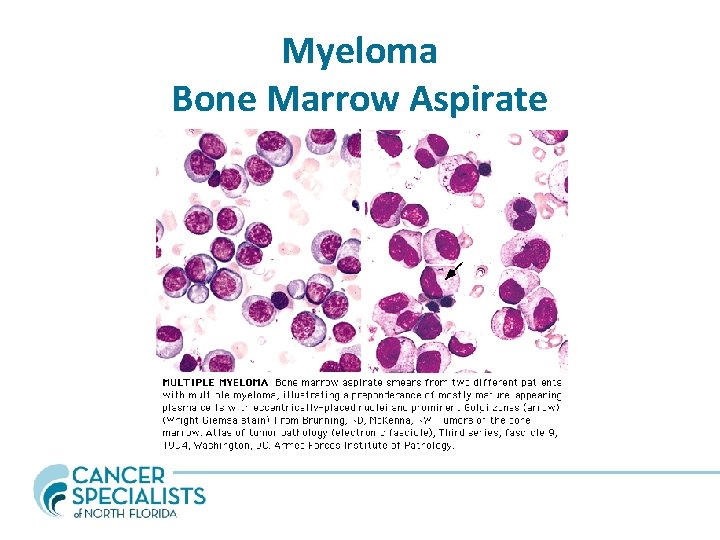
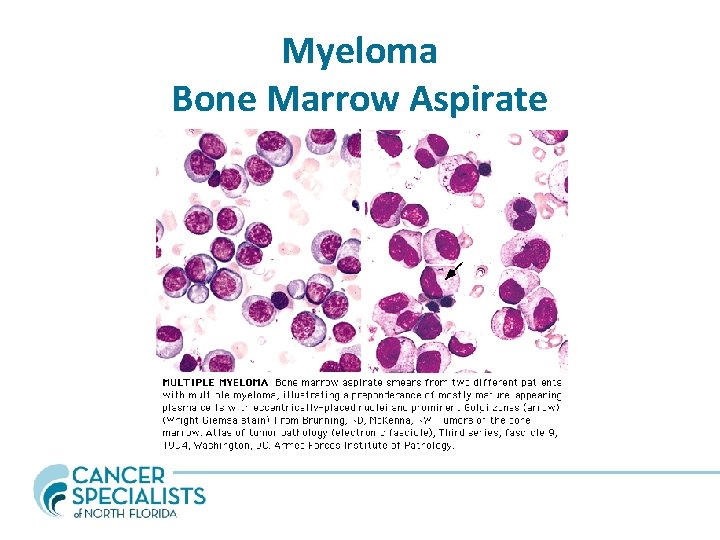
Myeloma Bone Marrow Aspirate
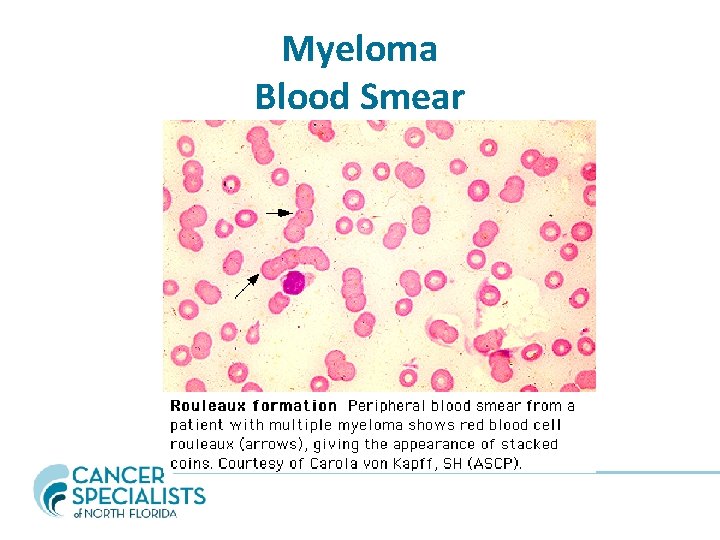
Myeloma Blood Smear
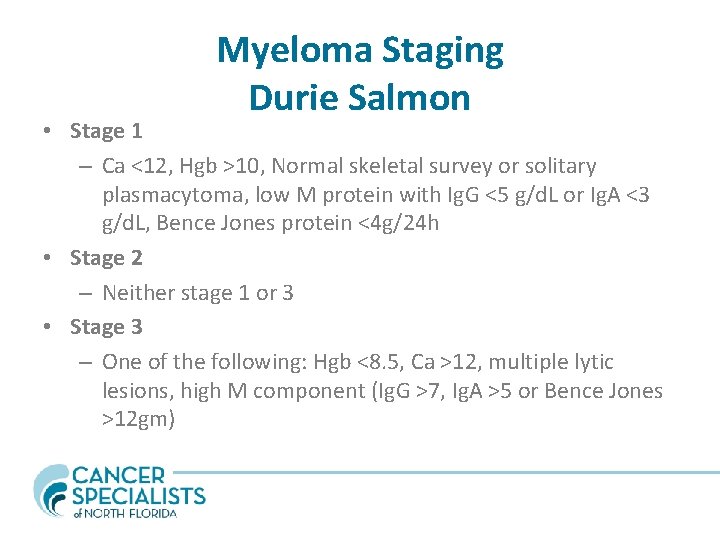
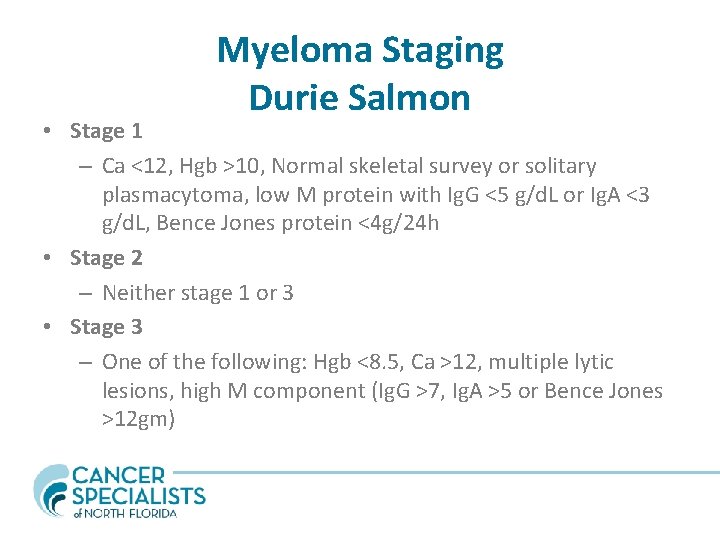
Myeloma Staging Durie Salmon • Stage 1 – Ca <12, Hgb >10, Normal skeletal survey or solitary plasmacytoma, low M protein with Ig. G <5 g/d. L or Ig. A <3 g/d. L, Bence Jones protein <4 g/24 h • Stage 2 – Neither stage 1 or 3 • Stage 3 – One of the following: Hgb <8. 5, Ca >12, multiple lytic lesions, high M component (Ig. G >7, Ig. A >5 or Bence Jones >12 gm)
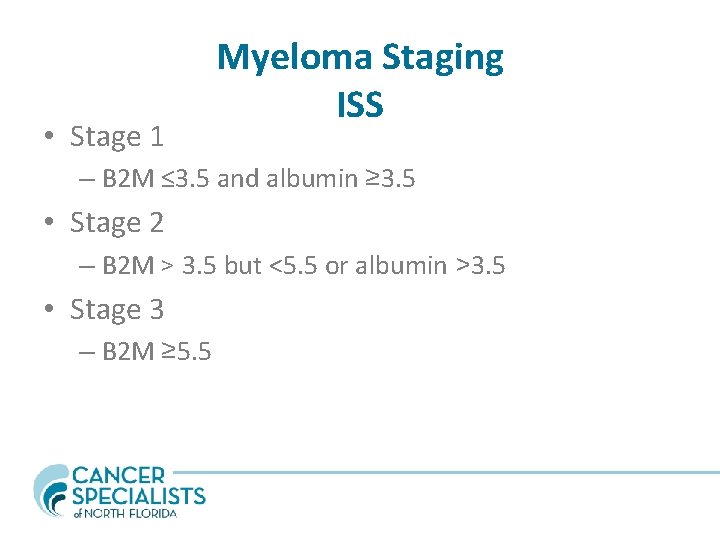
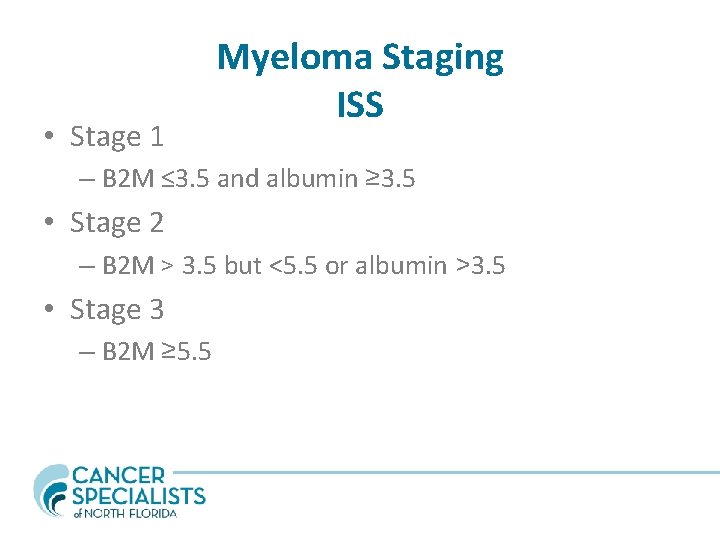
• Stage 1 Myeloma Staging ISS – B 2 M ≤ 3. 5 and albumin ≥ 3. 5 • Stage 2 – B 2 M > 3. 5 but <5. 5 or albumin >3. 5 • Stage 3 – B 2 M ≥ 5. 5
Case Presentation • 41 yo WF with no symptoms goes to annual physical at office based clinic. • No symptoms other than mild fatigue • Routine annual labs drawn
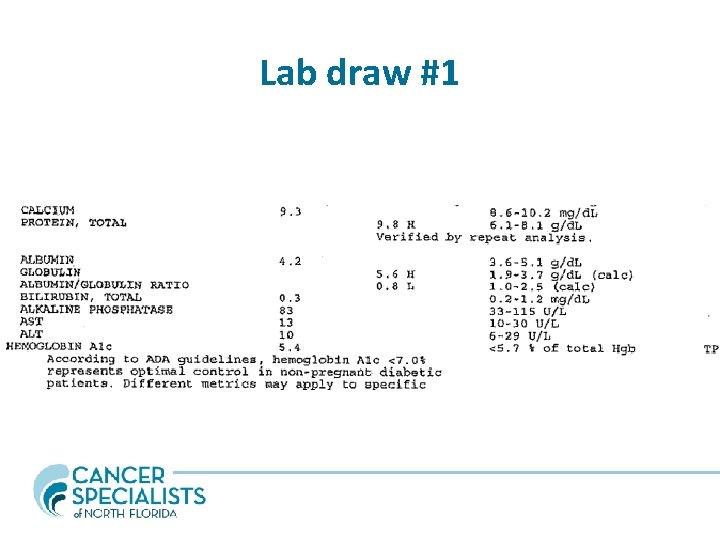
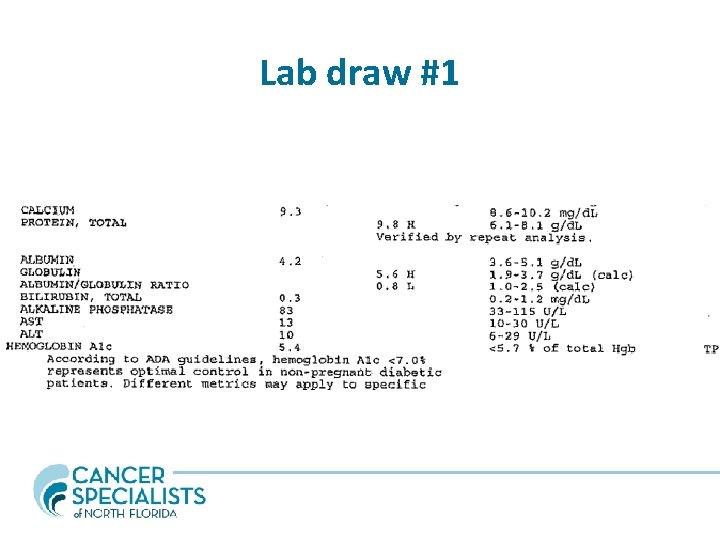
Lab draw #1
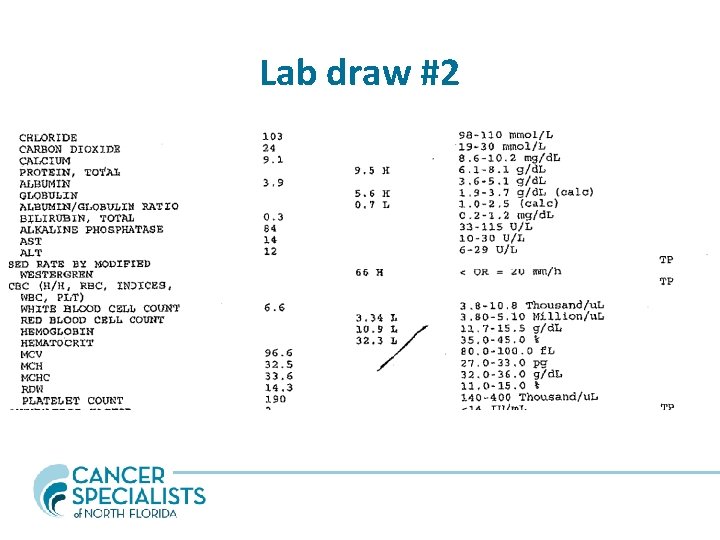
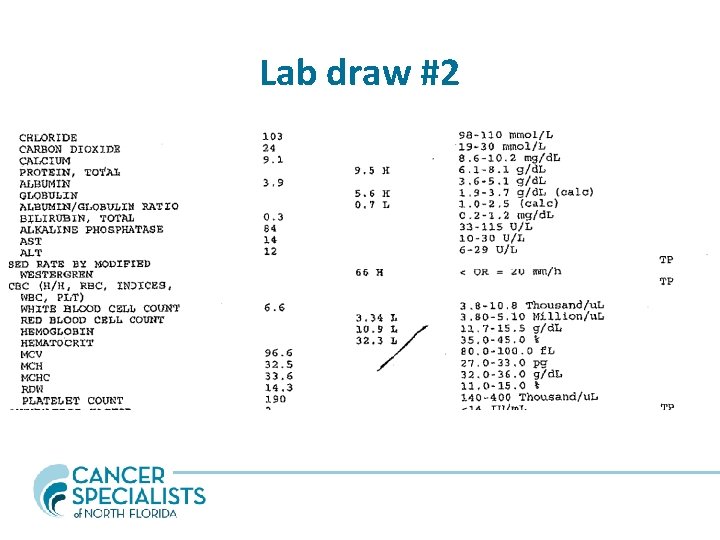
Lab draw #2
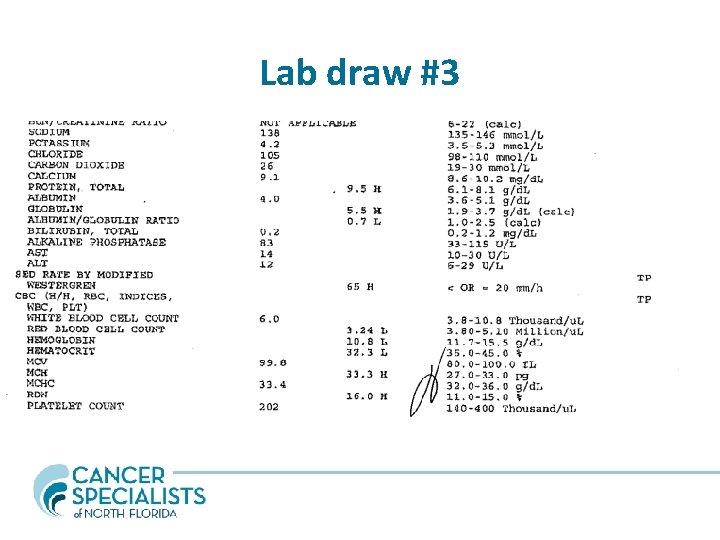
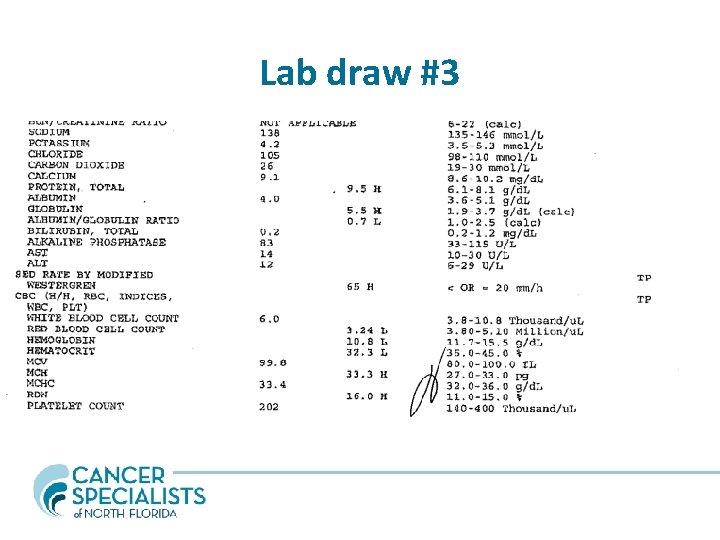
Lab draw #3
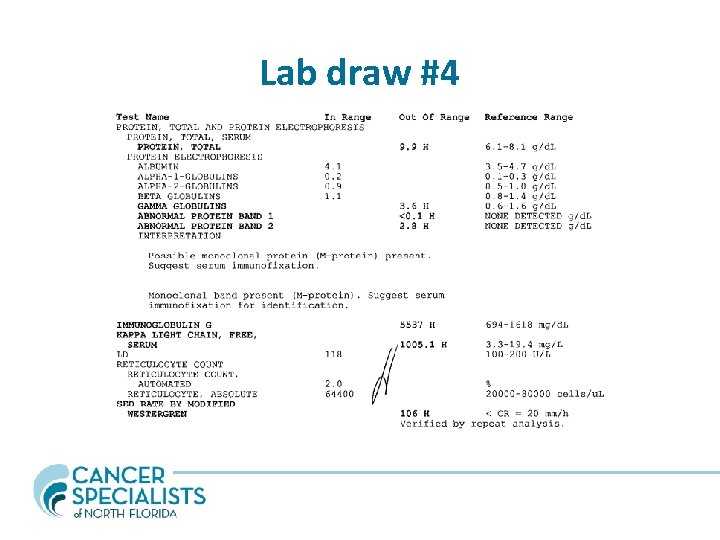
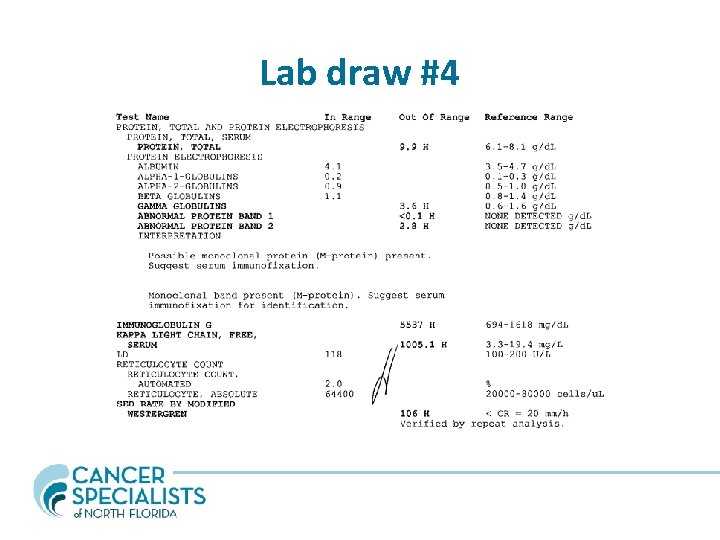
Lab draw #4
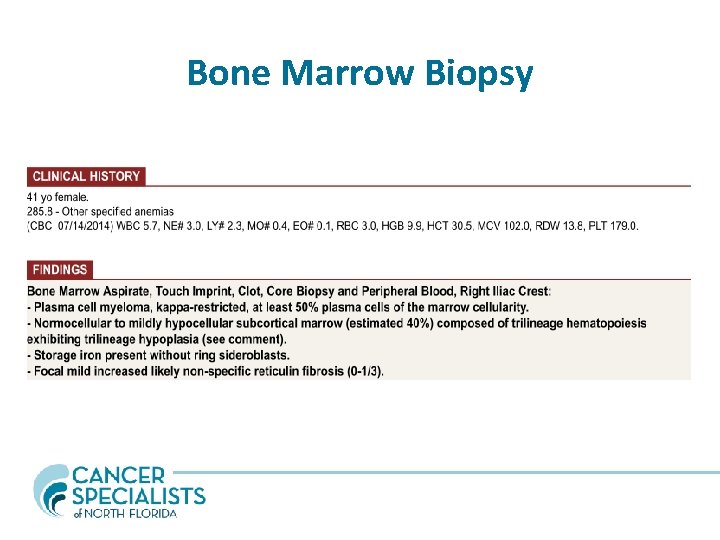
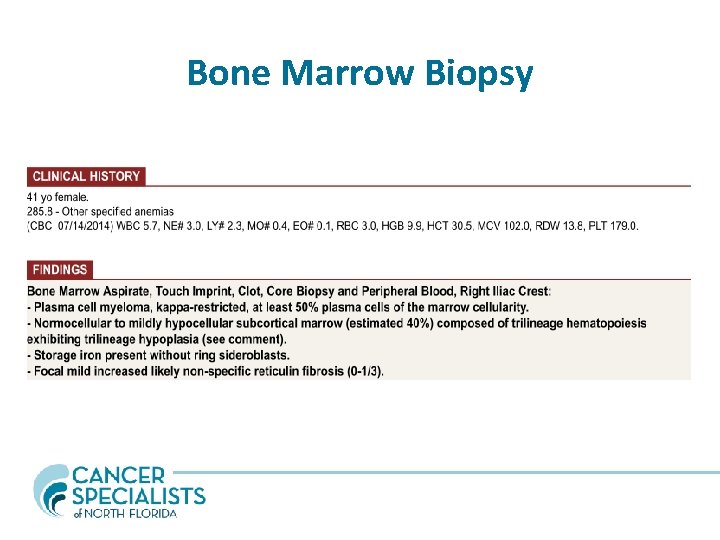
Bone Marrow Biopsy

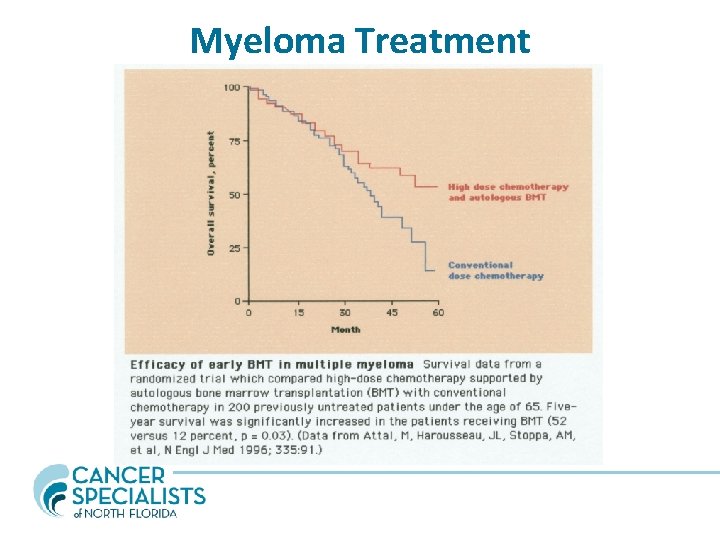
Myeloma Treatment • Determine eligibility for HDT and SCT – Age, overall health, psychological evaluation – Avoid alkylating agents (marrow toxic) – Chemotherapy to induce remission – Refer for stem cell collection and transplant – Maintenance therapy – Regular monitoring – ASCT improves median OS by >12 months
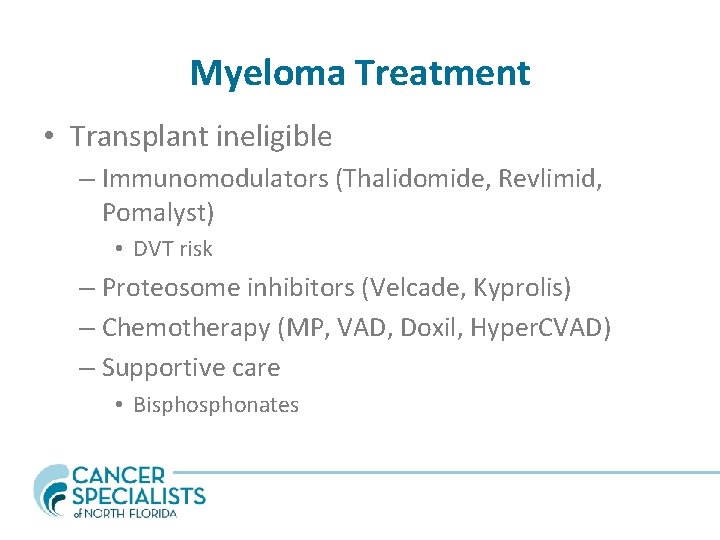
Myeloma Treatment • Transplant ineligible – Immunomodulators (Thalidomide, Revlimid, Pomalyst) • DVT risk – Proteosome inhibitors (Velcade, Kyprolis) – Chemotherapy (MP, VAD, Doxil, Hyper. CVAD) – Supportive care • Bisphonates
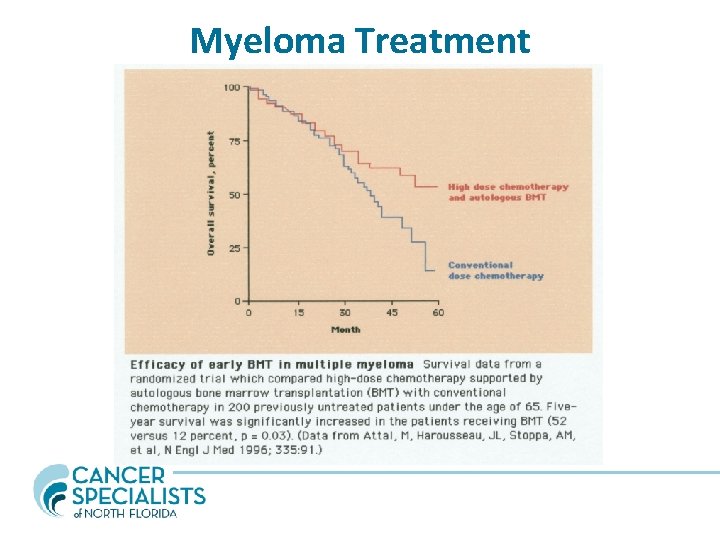
Myeloma Treatment
Solitary Plasmacytoma • Approx 3% of myeloma patients • No or very low myeloma protein in serum or urine • MR must be done to evaluate patient as it may detect other bone lesions (upstage the patient to myeloma) • Presence of monoclonal protein >1 yr after irradiation denotes progression to myeloma • Treat with XRT (at least 45 Gy). • MM manifests overtime, only 20% remain disease free at 10 yrs • Median time to progression is 2 yrs
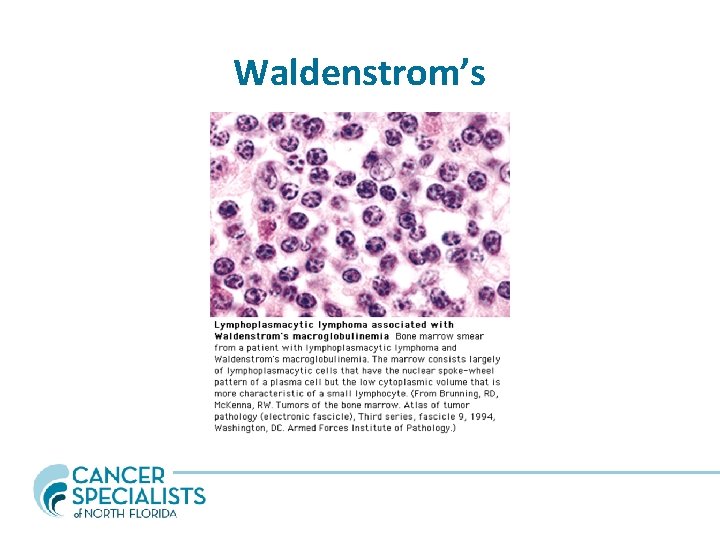
Waldenstrom’s • • • Lymphoplasmacytic bone marrow infiltration Malignant B lymphocytes producing monoclonal Ig. M Median age 65; Whites > Blacks; M>F 1500 cases in the US per year Hyperviscosity syndromes – neurologic complaints including vision change, headache, vertigo, nystagmus, dizziness, deafness, diplopia and ataxia • 10 -20% of pts. Have a cryoglobulin (Type I) which precipitates at high T >22 C on cold exposure may cause symptoms such as Raynauds phenomenon, urticaria, purpura and acral cyanosis. • Diarrhea and Steatorrhea (Ig. M infiltration into GI tract)
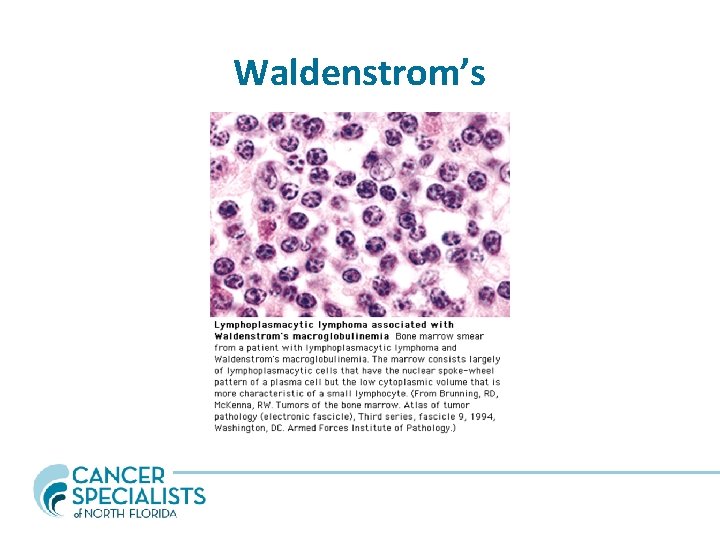
Waldenstrom’s
Waldenstrom’s Treatment • Goal to reduce hyperviscosity (Ig. M is a pentamer!) and lymphoproliferation – Pheresis if symptoms from the hyperviscosity causing severe neurologic deficits • Chemotherapy – Chlorambucil, other CCU, Cladribine and Fludarabine, Rituxan, IFN, Thalidomide, Ibrutinib, Velcade

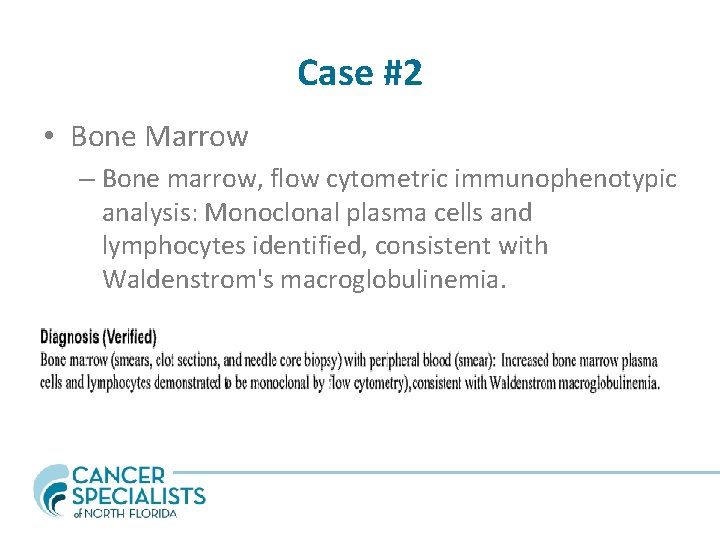
Case #2 • 73 yo WF presenting with neuropathy, dizziness, 40 lb weight loss, Ig. M 5454, immediately hospitalized due to neurologic symptoms, started plasma exchange
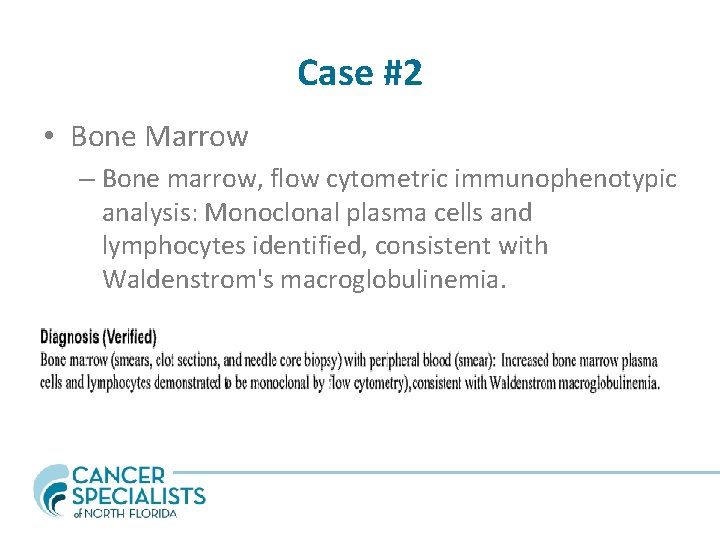
Case #2 • Bone Marrow – Bone marrow, flow cytometric immunophenotypic analysis: Monoclonal plasma cells and lymphocytes identified, consistent with Waldenstrom's macroglobulinemia.
Case #2 • Dramatic decline in Ig. M (>5000 to <2000) after plasma exchange • Symptoms have improved • Treated with Rituxan and Velcade, Ig. M started rising again. • Changed to Ibrutinib, symptoms remain improved, Ig. M stabilized below 1500 • Ig. M stable for > 2 years now
Amyloidosis • Occurs in 10% of patients with MM • Infiltrative process resulting from amyloid fibril deposition in organs • Fibril is made from the terminal amino acid residue (NH 2) of the variable portion of the light chain Ig molecule • Produced by clonal plasma cells

Amyloidosis • Renal disease - asymptomatic proteinuria to nephrotic syndrome • Cardiomyopathy • Hepatomegaly • Neuropathy • Pseudohypertrophy of muscles • Bleeding problems (Factor X def, Liver dz) • Lung and Skin infiltration
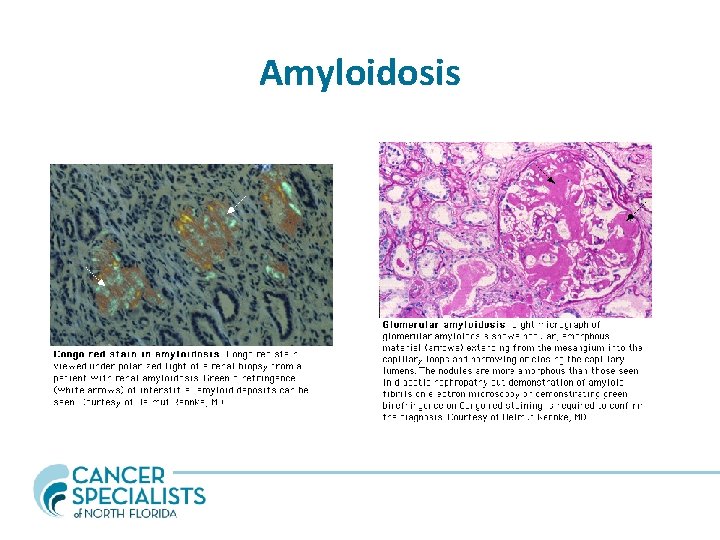
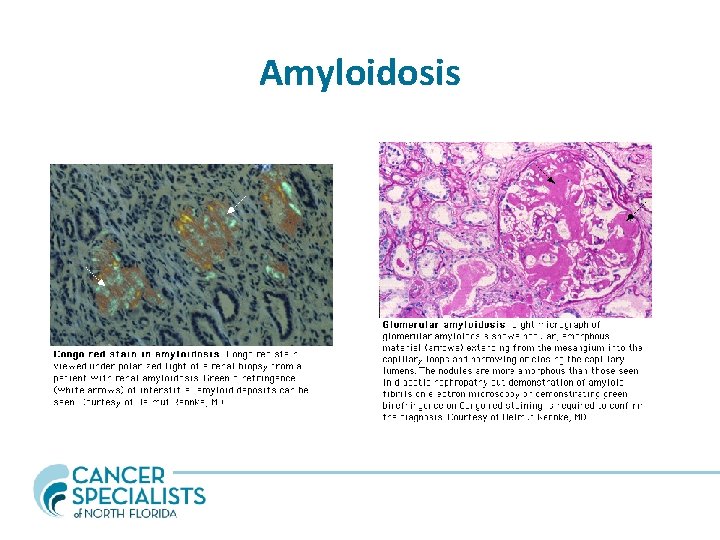
Amyloidosis
Amyloidosis • AL should be suspected in patients with plasma cell dyscrasia history • Biopsy results as shown • SPEP/UPEP - confirms monoclonal protein (plasma cell population) • Treatment - treat underlying plasma cell dyscrasia
Summary • MGUS, SMM and MM are a spectrum of the same disease process • MGUS and SMM patients need close observation • WM patients present with hyperviscosity symptoms and very high Ig. M, total protein • Amyloidosis (AL) is characterized by fibril deposition in organs with damage (most commonly heart/liver/kidney) • Treatment is dependant on the disease process
Questions Miten R. Patel, MD Office 904 -516 -3737 Cell phone 904 -451 -9820 miten. patel@csnf. us
 Waldenstrom macroglobulinemia mnemonic
Waldenstrom macroglobulinemia mnemonic Plasma cell neoplasm
Plasma cell neoplasm Plasma cell mastitis treatment
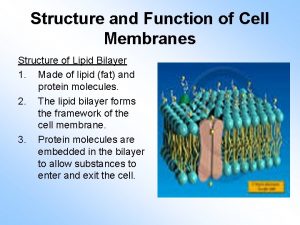
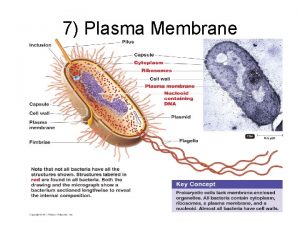
Plasma cell mastitis treatment Lipids cell membrane function
Lipids cell membrane function Smoldering multiple myeloma
Smoldering multiple myeloma Työturvallisuus tilaaja ja toimittaja
Työturvallisuus tilaaja ja toimittaja Järviekosysteemi
Järviekosysteemi Miten dekolonisaatio vaikutti kylmään sotaan?
Miten dekolonisaatio vaikutti kylmään sotaan? Logopedian kandiohjelma
Logopedian kandiohjelma Miten lattanat lisääntyvät
Miten lattanat lisääntyvät Mihin hauskuutta tarvitaan
Mihin hauskuutta tarvitaan Miten referoidaan
Miten referoidaan Nestelista tulostettava
Nestelista tulostettava Luetelma yo
Luetelma yo Arvoitusdekkari
Arvoitusdekkari Ympyrälieriön tilavuus
Ympyrälieriön tilavuus Mitä kappaleeseen jatkuvasti vaikuttava voima saa aikaan
Mitä kappaleeseen jatkuvasti vaikuttava voima saa aikaan Voittoprosentin laskeminen
Voittoprosentin laskeminen Hinnoittelualue
Hinnoittelualue Lukualueet
Lukualueet Itseisarvo matematiikka
Itseisarvo matematiikka Lemcba
Lemcba Tunnetuimmat tulivuoret
Tunnetuimmat tulivuoret Työ ja teho
Työ ja teho Miten magneettinen vuorovaikutus ilmenee
Miten magneettinen vuorovaikutus ilmenee Laktoosi operoni
Laktoosi operoni Lentokoneen aerodynamiikka
Lentokoneen aerodynamiikka Vaihto-opiskelu tanska
Vaihto-opiskelu tanska Laadullisen tutkimuksen luotettavuuden arviointi
Laadullisen tutkimuksen luotettavuuden arviointi Hygieniaosaamistodistus
Hygieniaosaamistodistus Pyramidien rakentaminen
Pyramidien rakentaminen Op mobiiliavain käyttöönotto
Op mobiiliavain käyttöönotto Millainen englanniksi
Millainen englanniksi Dr vikas patel
Dr vikas patel Dr vikas patel
Dr vikas patel Kanika kitchlu-connolly
Kanika kitchlu-connolly Dr niraj patel
Dr niraj patel Is it really
Is it really Jaydeep patel youtube income
Jaydeep patel youtube income Dr niraj patel
Dr niraj patel Dr megha patel
Dr megha patel Ushma patel uci
Ushma patel uci