Lymphoma and Multiple Myeloma Terry Hayes M D














- Slides: 104
Lymphoma and Multiple Myeloma Terry Hayes, M. D. , Ph. D.
Topics to be Covered • Non-Hodgkin’s Lymphoma • Hodgkin’s Disease • Multiple Myeloma
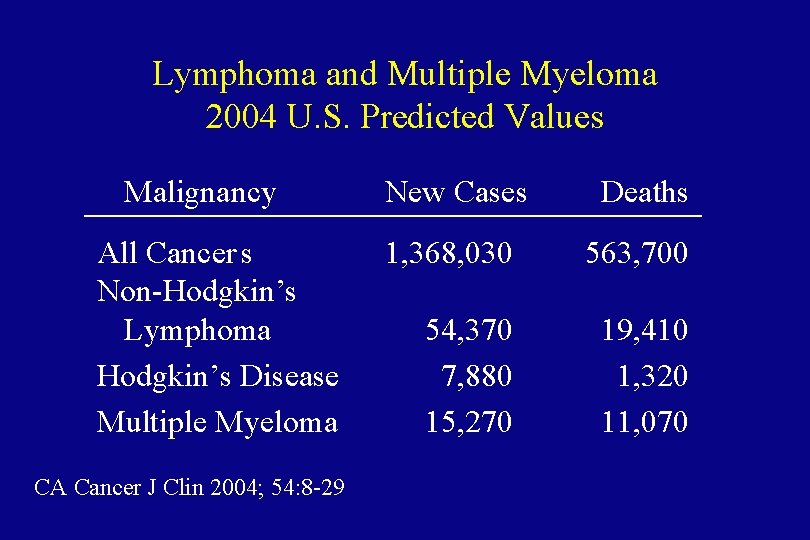
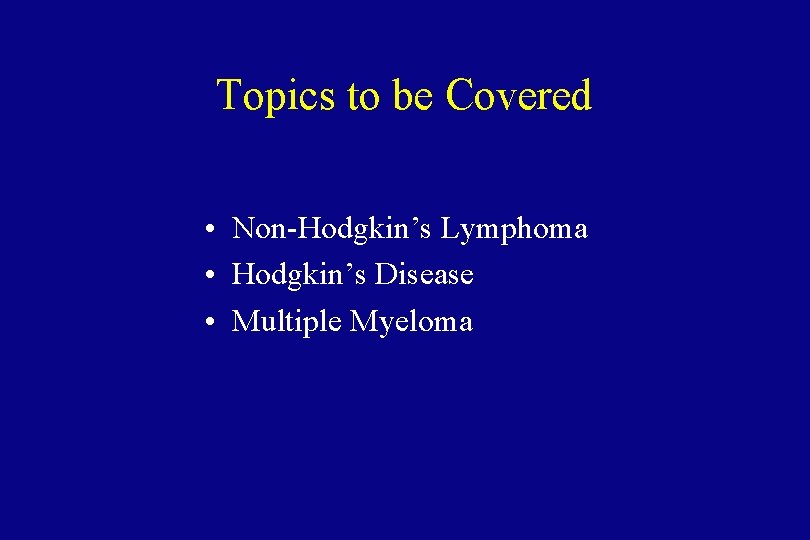
Lymphoma and Multiple Myeloma 2004 U. S. Predicted Values Malignancy All Cancer s Non-Hodgkin’s Lymphoma Hodgkin’s Disease Multiple Myeloma CA Cancer J Clin 2004; 54: 8 -29 New Cases Deaths 1, 368, 030 563, 700 54, 370 7, 880 15, 270 19, 410 1, 320 11, 070
Non-Hodgkin’s Lymphoma
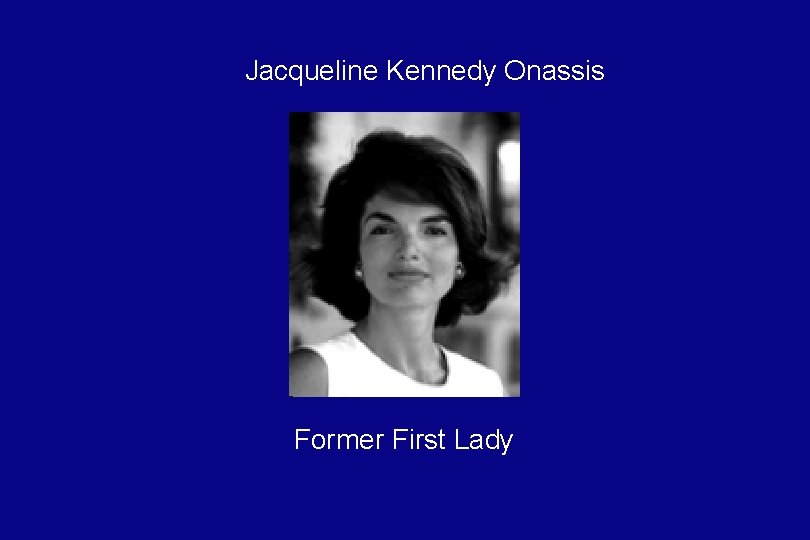
Jacqueline Kennedy Onassis Former First Lady
King Hussein of Jordan
“Mr. T” (Lawrence Tureaud) Television star, The A-Team. Sylvester Stallone's adversary in "Rocky III. ”
Non-Hodgkin’s Lymphoma • 6 th most common cause of cancer death in United States. • Increasing in incidence and mortality. • Since 1970, the incidence of lymphoma has almost doubled.
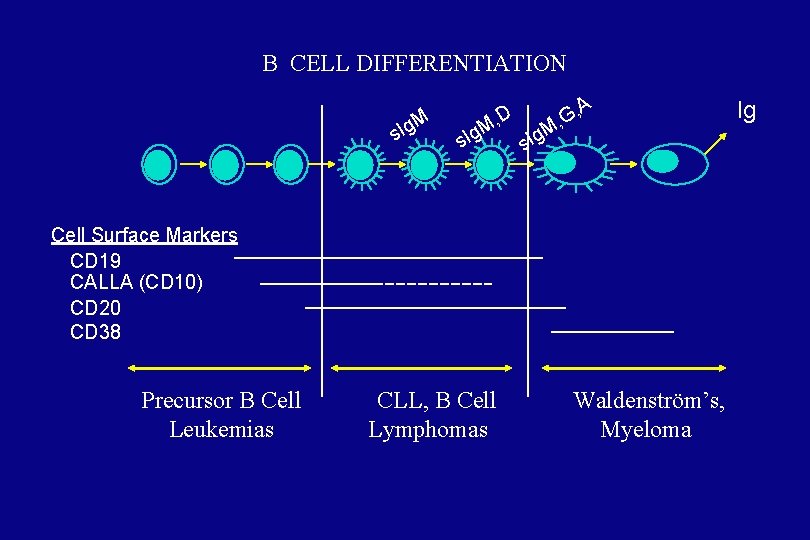
Overview • The types of non- Hodgkin’s lymphoma reflect the developmental stages of lymphocytes. • Each type of lymphoma can be viewed as a lymphocyte arrested at a certain stage of development and transformed into a malignant cell. • 85% B cell origin, the rest T or null cell.
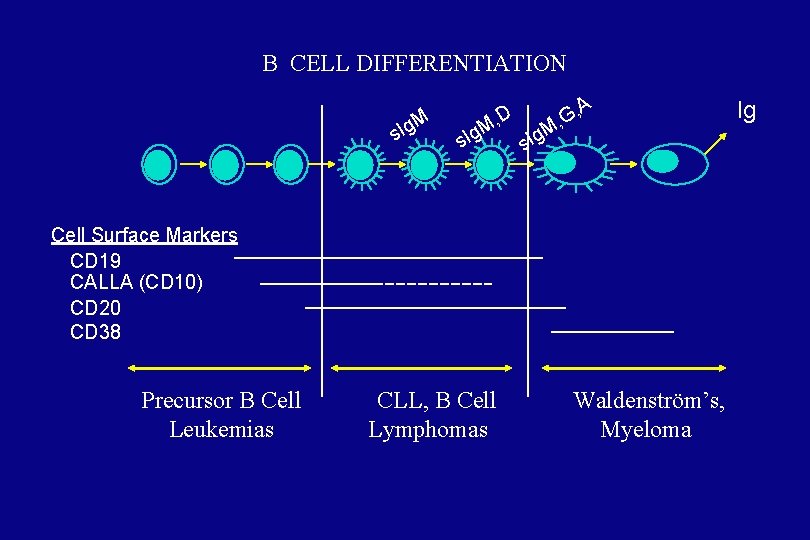
B CELL DIFFERENTIATION Ig. M s s. Ig D M, A G, , Ig. M s Cell Surface Markers CD 19 CALLA (CD 10) CD 20 CD 38 Precursor B Cell Leukemias CLL, B Cell Lymphomas Waldenström’s, Myeloma Ig
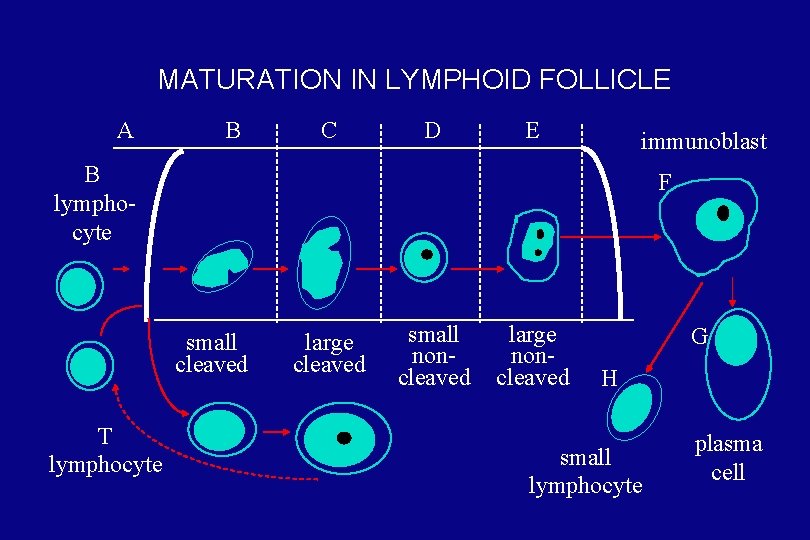
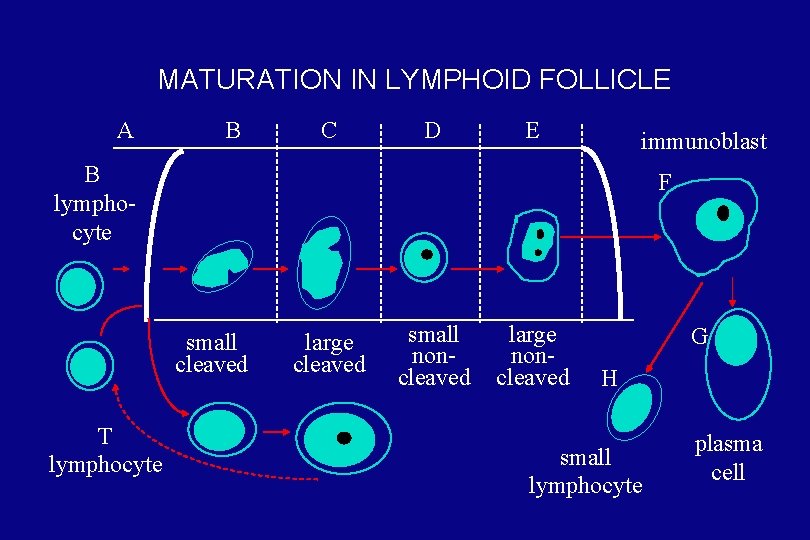
MATURATION IN LYMPHOID FOLLICLE A B C D E immunoblast B lymphocyte F small cleaved T lymphocyte large cleaved small noncleaved large noncleaved G H small lymphocyte plasma cell
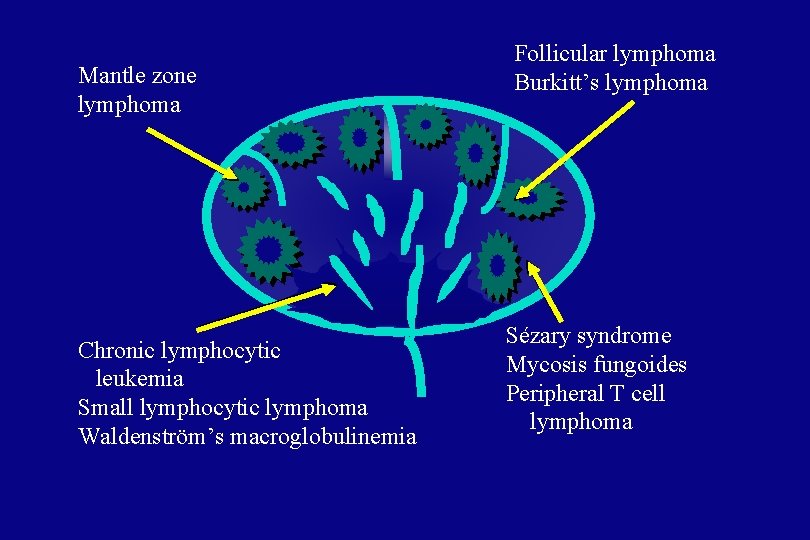
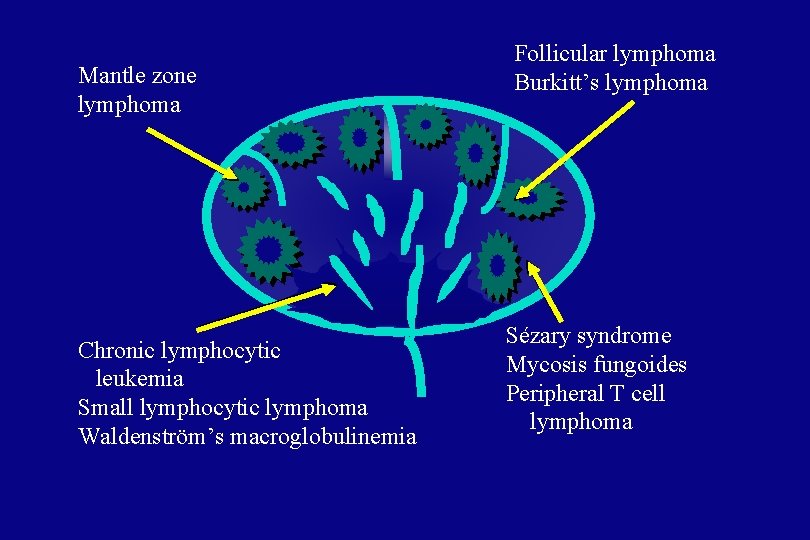
Mantle zone lymphoma Chronic lymphocytic leukemia Small lymphocytic lymphoma Waldenström’s macroglobulinemia Follicular lymphoma Burkitt’s lymphoma Sézary syndrome Mycosis fungoides Peripheral T cell lymphoma
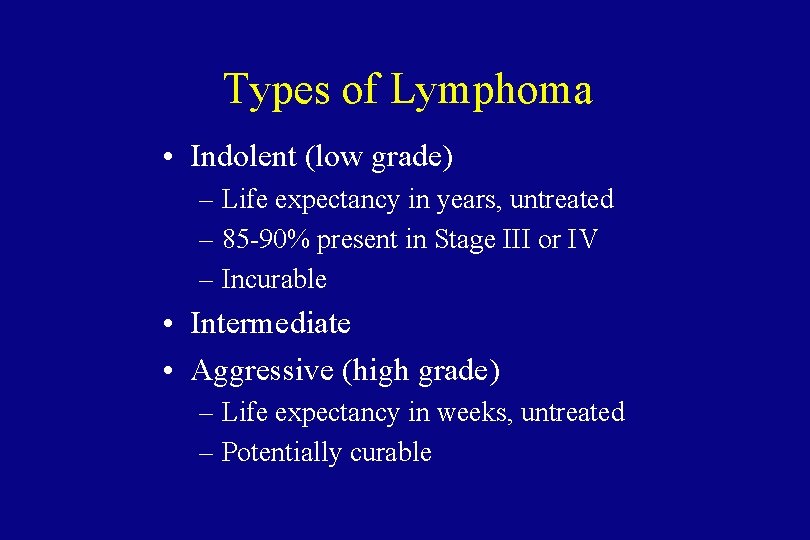
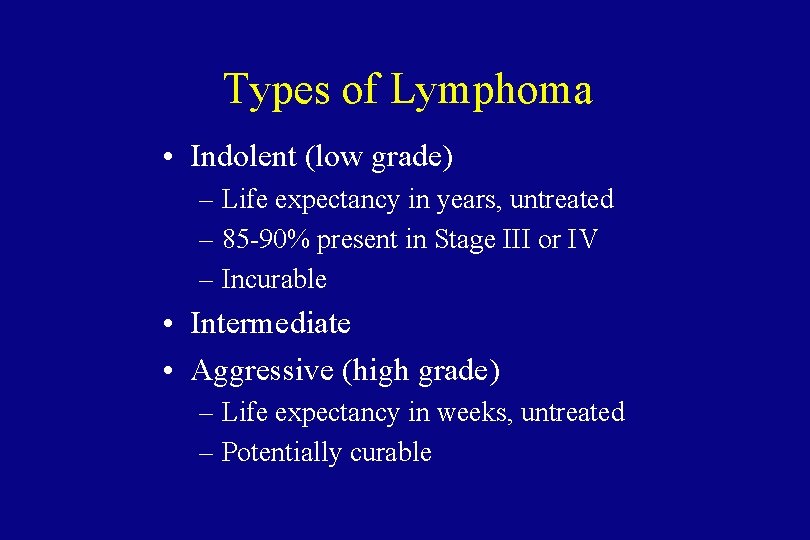
Types of Lymphoma • Indolent (low grade) – Life expectancy in years, untreated – 85 -90% present in Stage III or IV – Incurable • Intermediate • Aggressive (high grade) – Life expectancy in weeks, untreated – Potentially curable
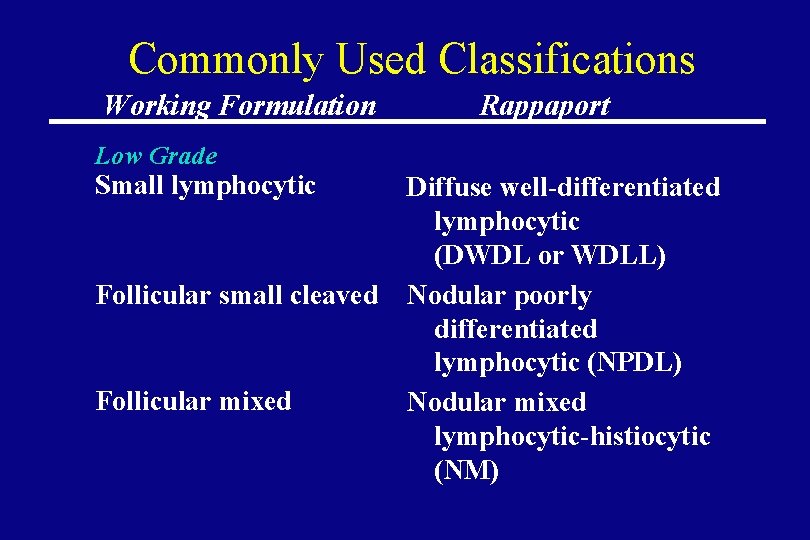
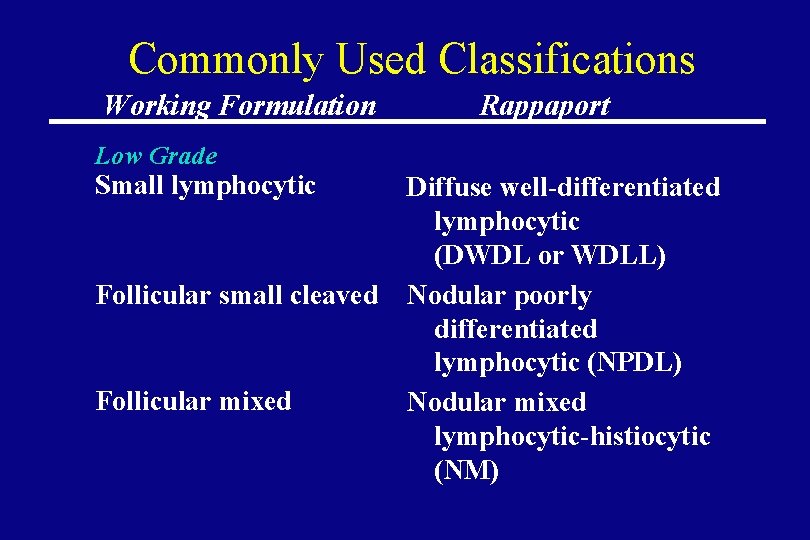
Commonly Used Classifications Working Formulation Rappaport Low Grade Small lymphocytic Follicular small cleaved Follicular mixed Diffuse well-differentiated lymphocytic (DWDL or WDLL) Nodular poorly differentiated lymphocytic (NPDL) Nodular mixed lymphocytic-histiocytic (NM)
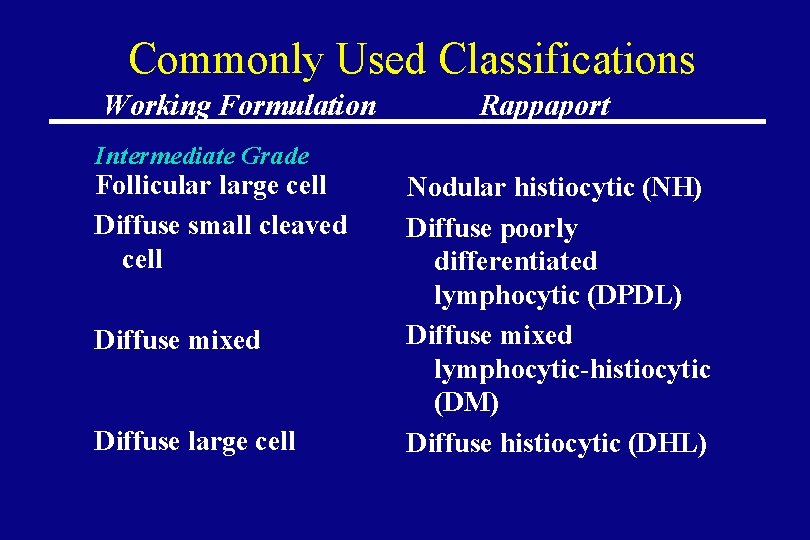
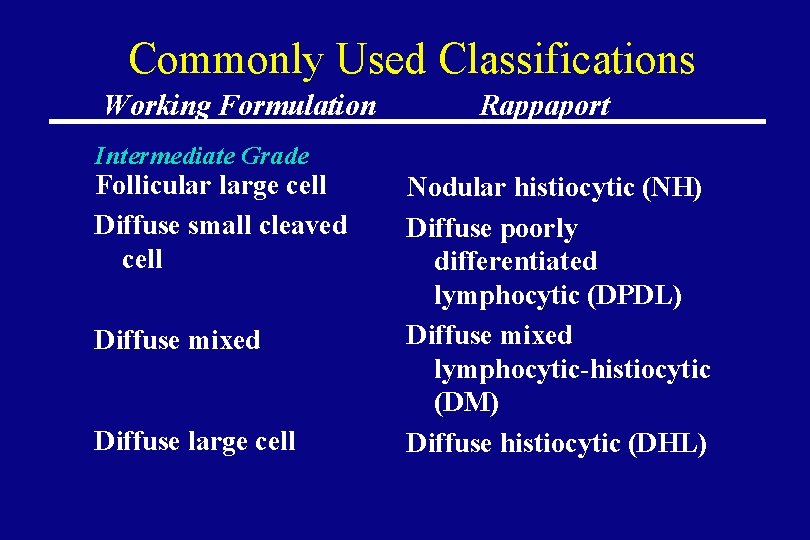
Commonly Used Classifications Working Formulation Rappaport Intermediate Grade Follicular large cell Diffuse small cleaved cell Diffuse mixed Diffuse large cell Nodular histiocytic (NH) Diffuse poorly differentiated lymphocytic (DPDL) Diffuse mixed lymphocytic-histiocytic (DM) Diffuse histiocytic (DHL)
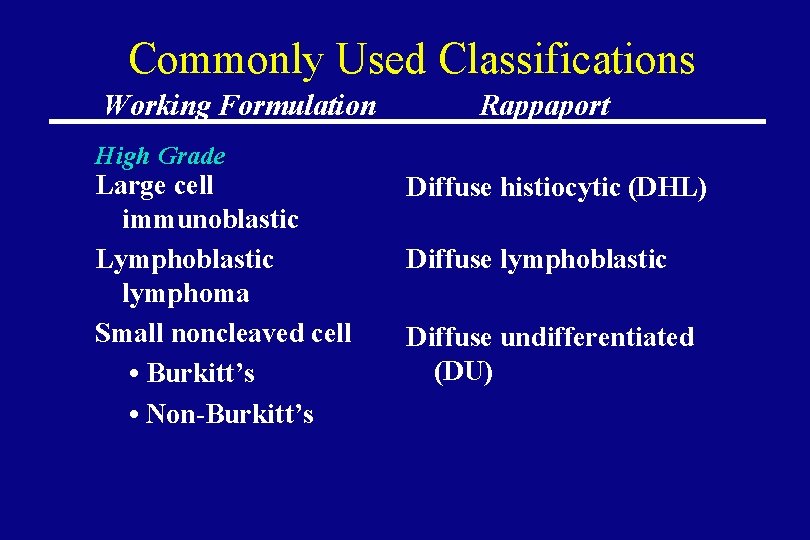
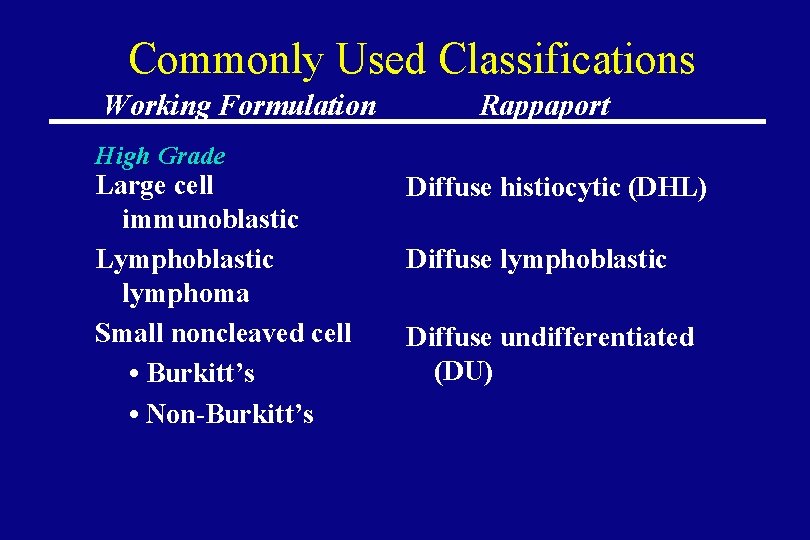
Commonly Used Classifications Working Formulation Rappaport High Grade Large cell immunoblastic Lymphoblastic lymphoma Small noncleaved cell • Burkitt’s • Non-Burkitt’s Diffuse histiocytic (DHL) Diffuse lymphoblastic Diffuse undifferentiated (DU)
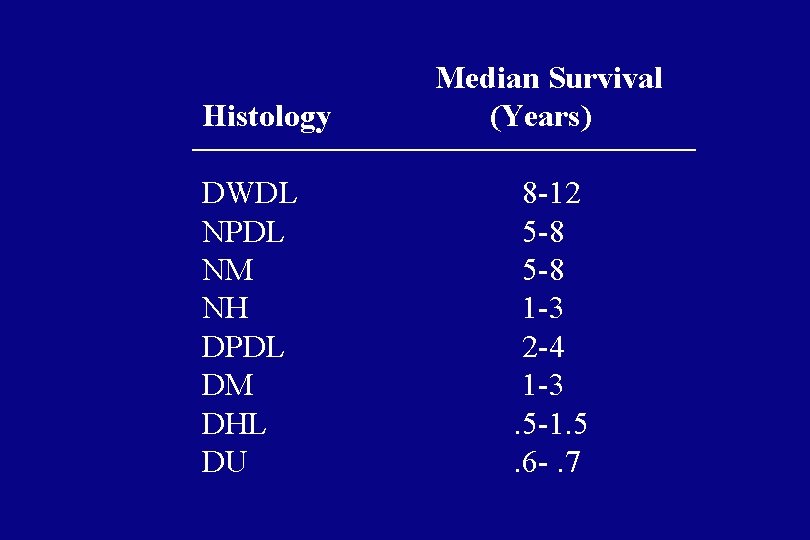
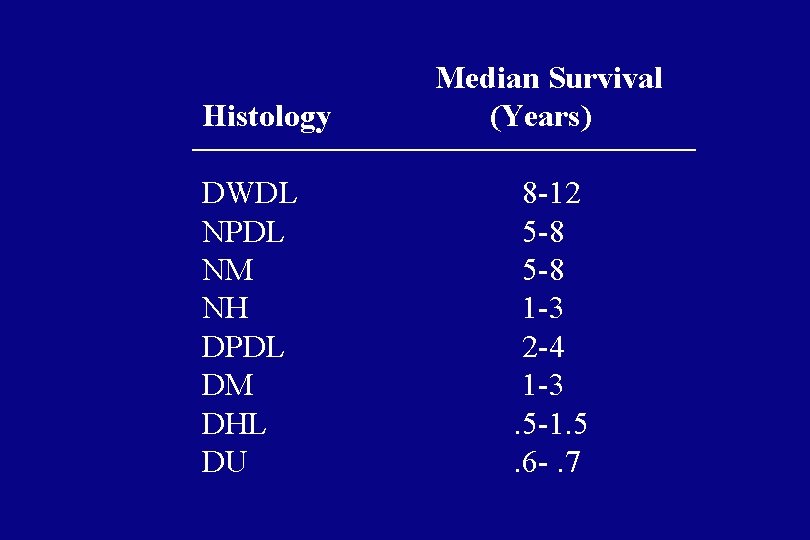
Histology DWDL NPDL NM NH DPDL DM DHL DU Median Survival (Years) 8 -12 5 -8 1 -3 2 -4 1 -3. 5 -1. 5. 6 -. 7
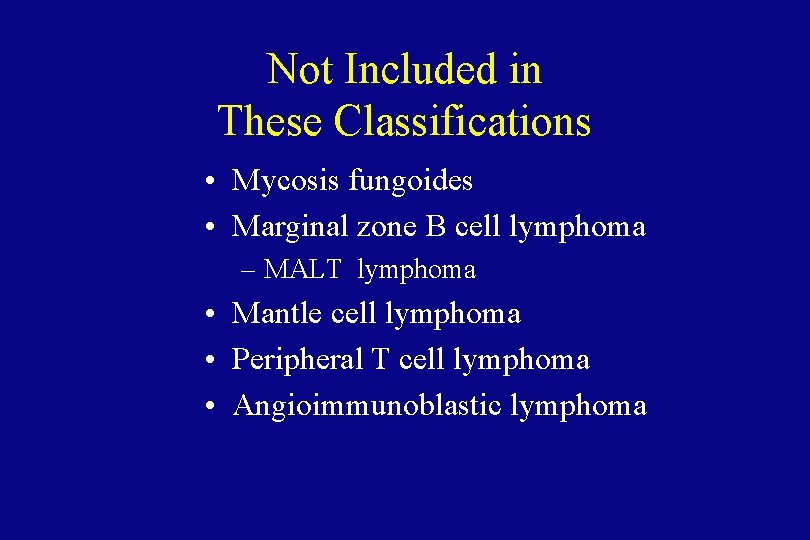
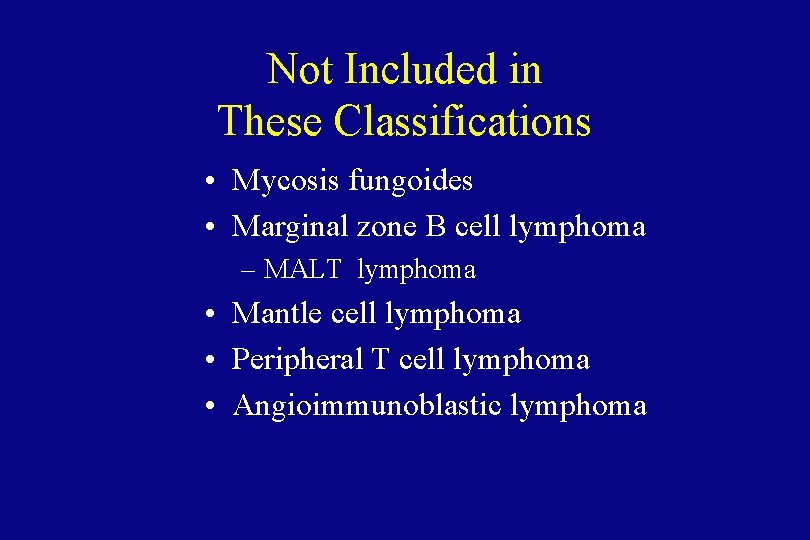
Not Included in These Classifications • Mycosis fungoides • Marginal zone B cell lymphoma – MALT lymphoma • Mantle cell lymphoma • Peripheral T cell lymphoma • Angioimmunoblastic lymphoma

The REAL Classification (Revised European-American Lymphoma Classification) September, 1994
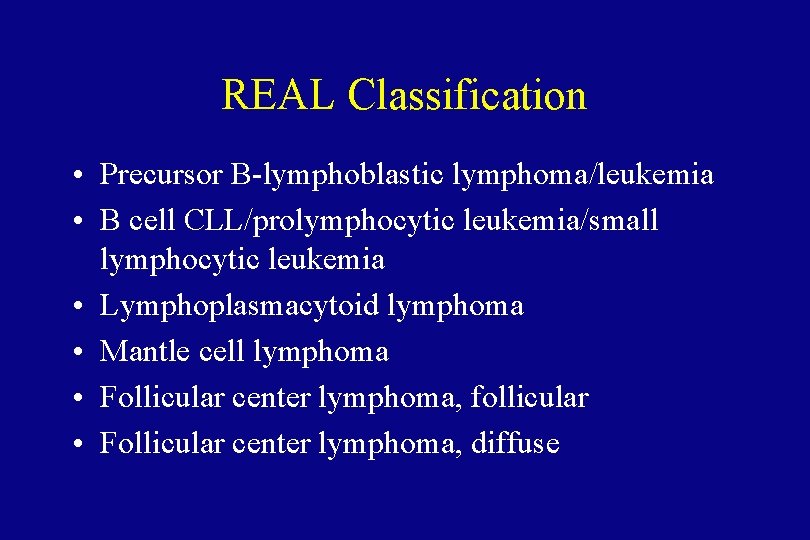
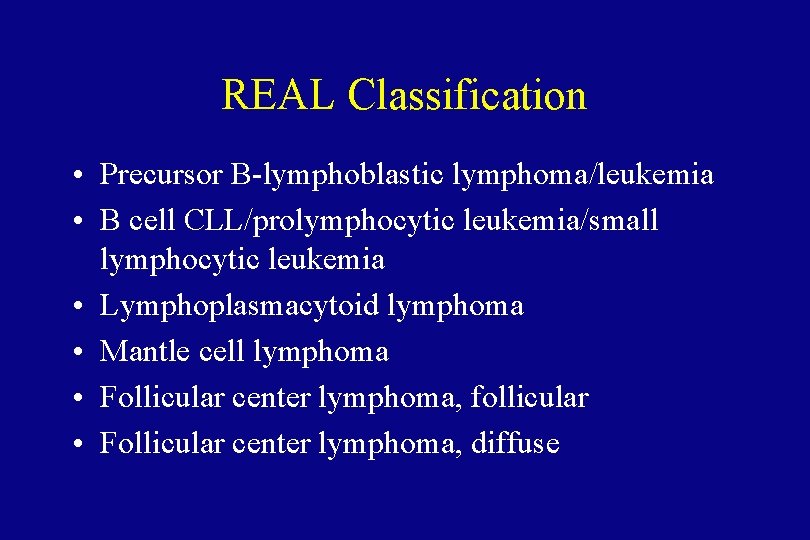
REAL Classification • Precursor B-lymphoblastic lymphoma/leukemia • B cell CLL/prolymphocytic leukemia/small lymphocytic leukemia • Lymphoplasmacytoid lymphoma • Mantle cell lymphoma • Follicular center lymphoma, follicular • Follicular center lymphoma, diffuse
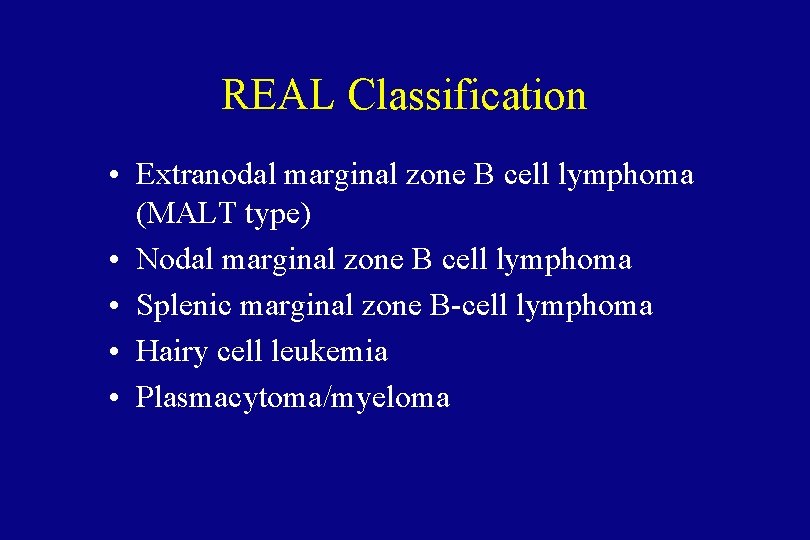
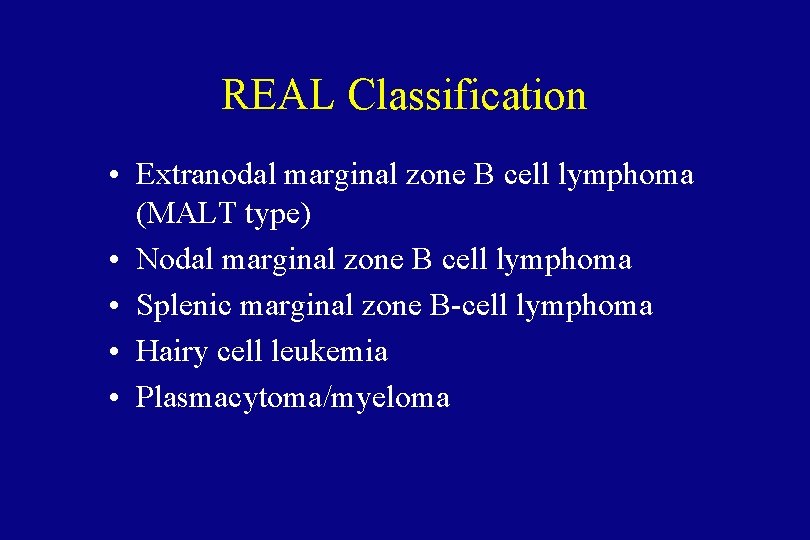
REAL Classification • Extranodal marginal zone B cell lymphoma (MALT type) • Nodal marginal zone B cell lymphoma • Splenic marginal zone B-cell lymphoma • Hairy cell leukemia • Plasmacytoma/myeloma
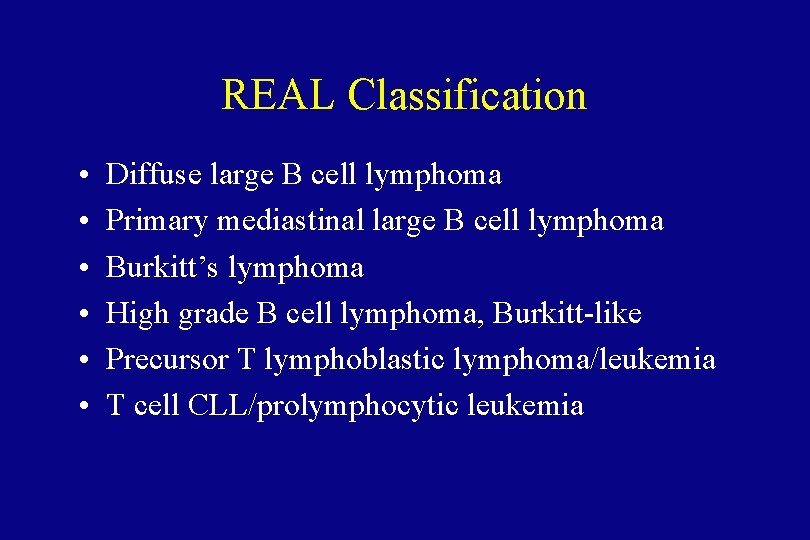
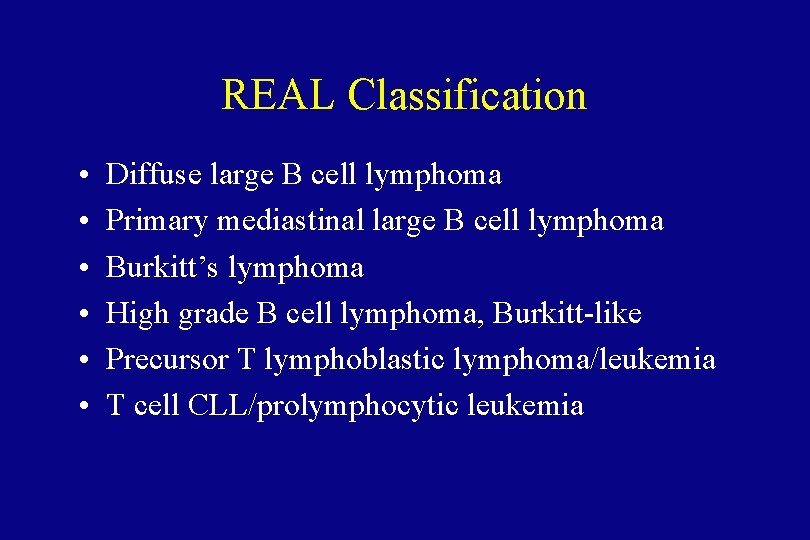
REAL Classification • • • Diffuse large B cell lymphoma Primary mediastinal large B cell lymphoma Burkitt’s lymphoma High grade B cell lymphoma, Burkitt-like Precursor T lymphoblastic lymphoma/leukemia T cell CLL/prolymphocytic leukemia
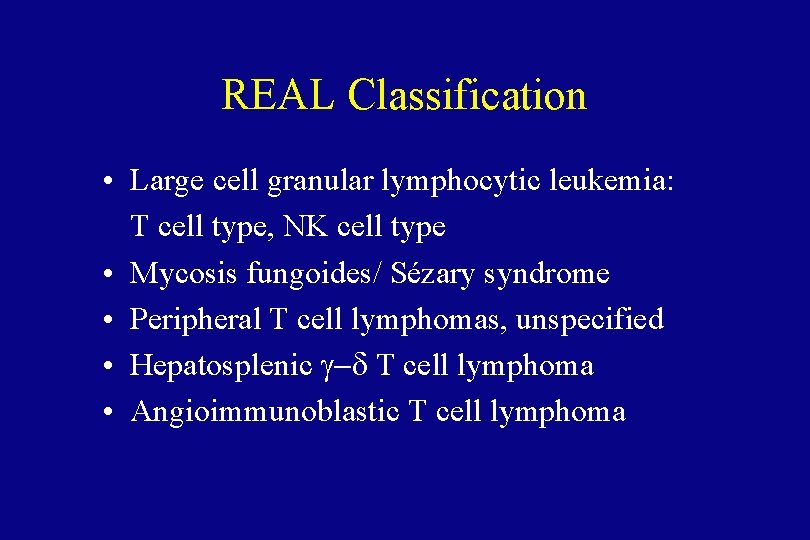
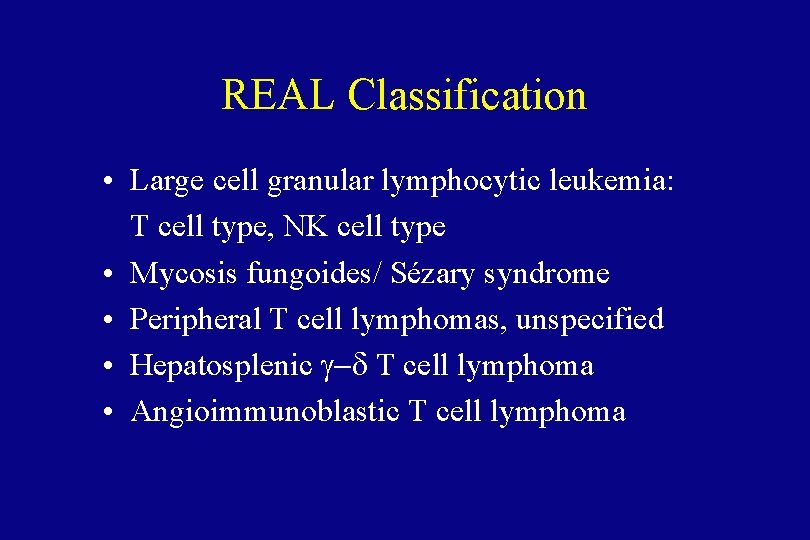
REAL Classification • Large cell granular lymphocytic leukemia: T cell type, NK cell type • Mycosis fungoides/ Sézary syndrome • Peripheral T cell lymphomas, unspecified • Hepatosplenic g-d T cell lymphoma • Angioimmunoblastic T cell lymphoma
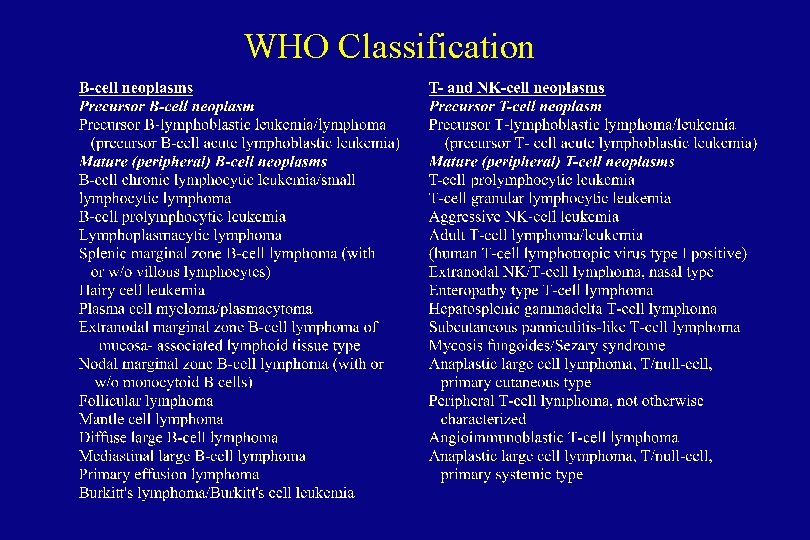
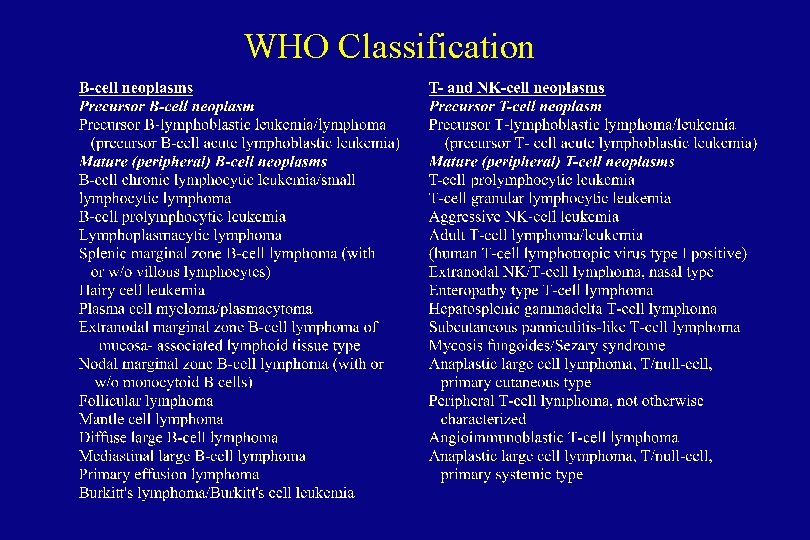
WHO Classification
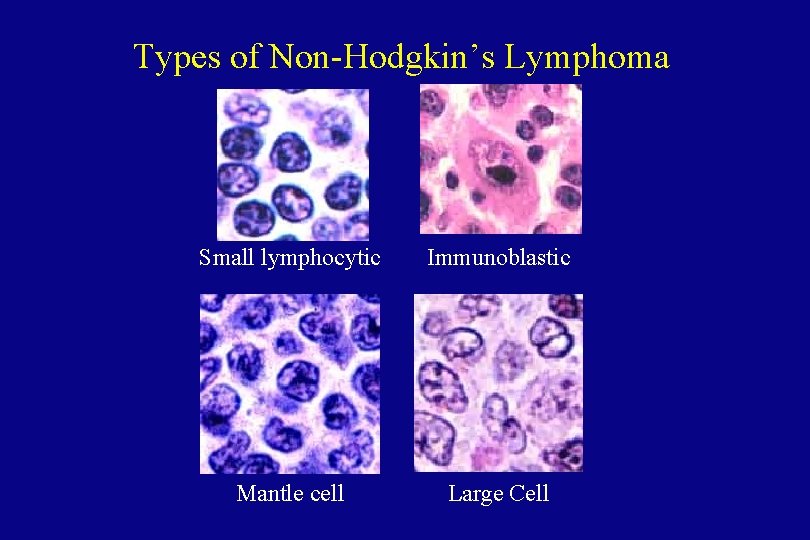
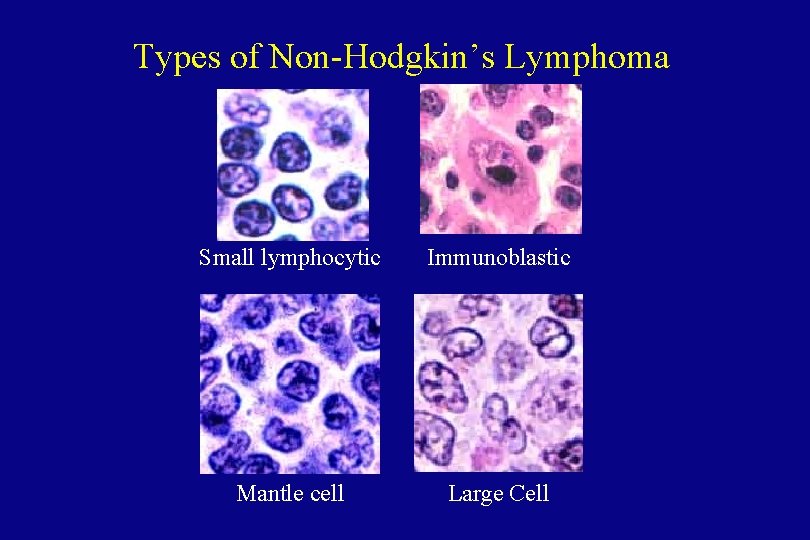
Types of Non-Hodgkin’s Lymphoma Small lymphocytic Immunoblastic Mantle cell Large Cell
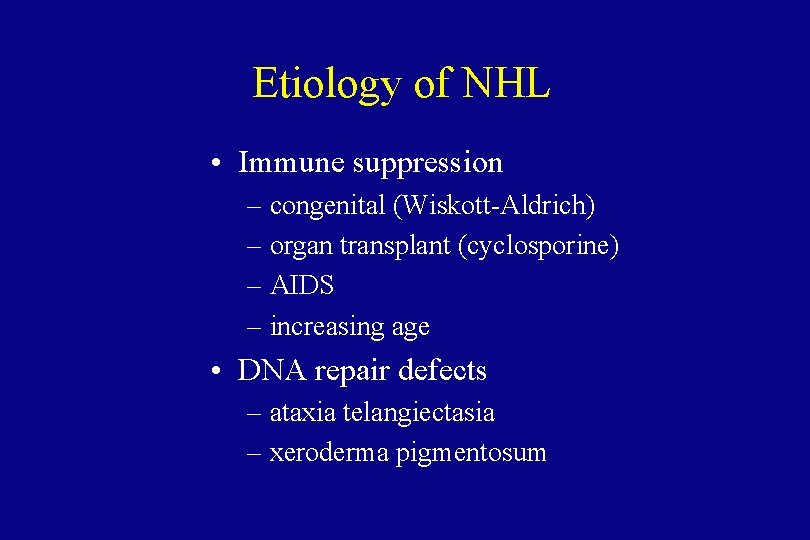
Etiology of NHL • Immune suppression – congenital (Wiskott-Aldrich) – organ transplant (cyclosporine) – AIDS – increasing age • DNA repair defects – ataxia telangiectasia – xeroderma pigmentosum

Etiology of NHL • Chronic inflammation and antigenic stimulation – Helicobacter pylori inflammation, stomach – Chlamydia psittaci inflammation, ocular adnexal tissues – Sjögren’s syndrome • Viral causes – EBV and Burkitt’s lymphoma – HTLV-I and T cell leukemia-lymphoma – HTLV-V and cutaneous T cell lymphoma – Hepatitis C
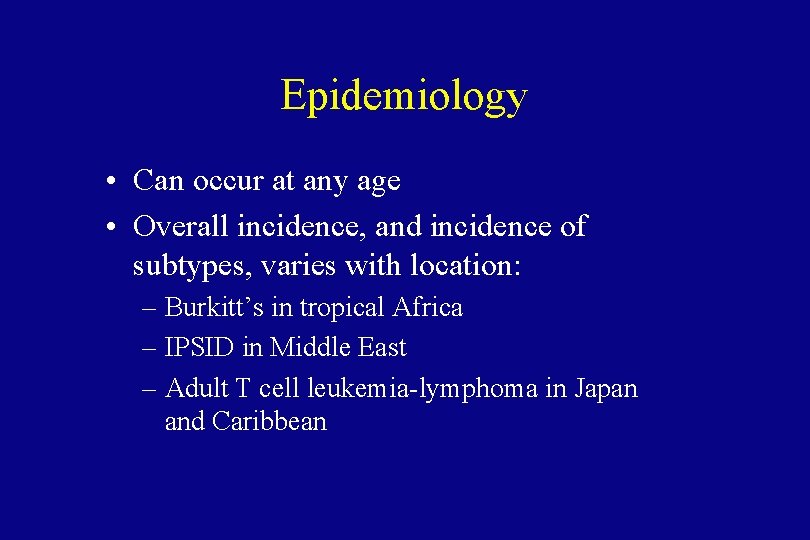
Epidemiology • Can occur at any age • Overall incidence, and incidence of subtypes, varies with location: – Burkitt’s in tropical Africa – IPSID in Middle East – Adult T cell leukemia-lymphoma in Japan and Caribbean
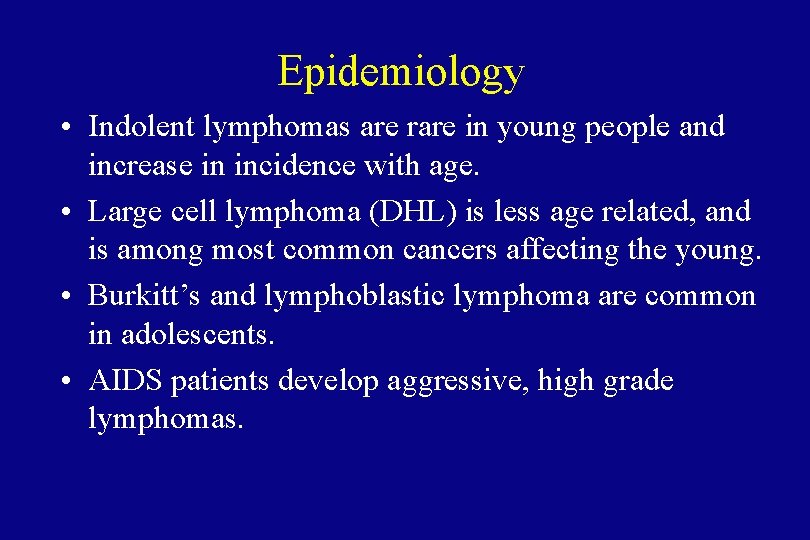
Epidemiology • Indolent lymphomas are rare in young people and increase in incidence with age. • Large cell lymphoma (DHL) is less age related, and is among most common cancers affecting the young. • Burkitt’s and lymphoblastic lymphoma are common in adolescents. • AIDS patients develop aggressive, high grade lymphomas.
Clinical Features • • • Lymphadenopathy Cytopenias Systemic symptoms Hepatosplenomegaly Fever Night sweats


Clinical Features • Lymphadenopathy may fluctuate or spontaneously remit, especially in low-grade lymphomas. • B symptoms more common in high-grade lymphomas. • Hematogenous spread of disease, with no predictable pattern.
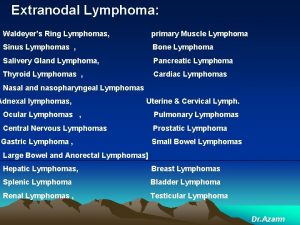
Clinical Features • Classic lymphoma: arises in lymph node or bone marrow. • Extranodal primary more common in high -grade lymphoma. • Waldeyer’s ring involvement frequent in GI lymphomas.
Diagnosis of NHL • Excisional biopsy is preferred to show nodal architecture (follicular vs diffuse). • Immunohistochemistry to confirm cells are lymphoid – LCA (leukocyte common antigen) – Monoclonal staining with Igk or Igl • Flow cytometry: – CD 19, CD 20 for B cell lymphomas – CD 3, CD 4, CD 8 for T cell lymphomas
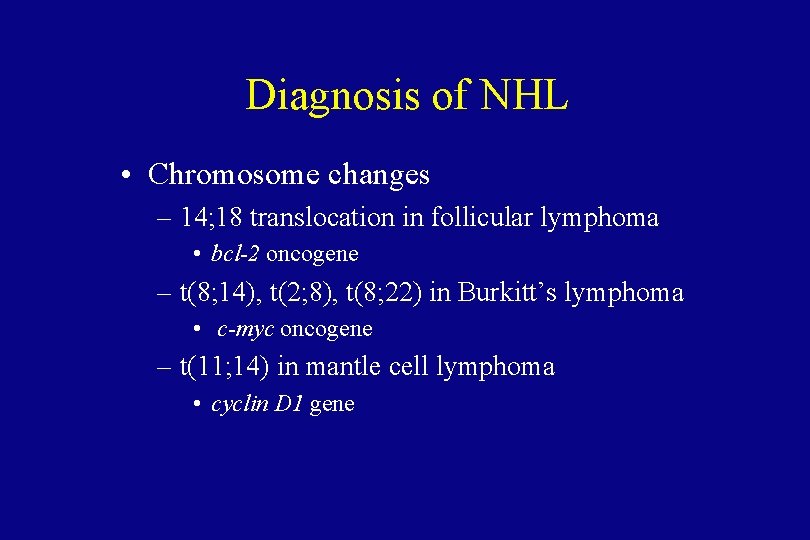
Diagnosis of NHL • Chromosome changes – 14; 18 translocation in follicular lymphoma • bcl-2 oncogene – t(8; 14), t(2; 8), t(8; 22) in Burkitt’s lymphoma • c-myc oncogene – t(11; 14) in mantle cell lymphoma • cyclin D 1 gene
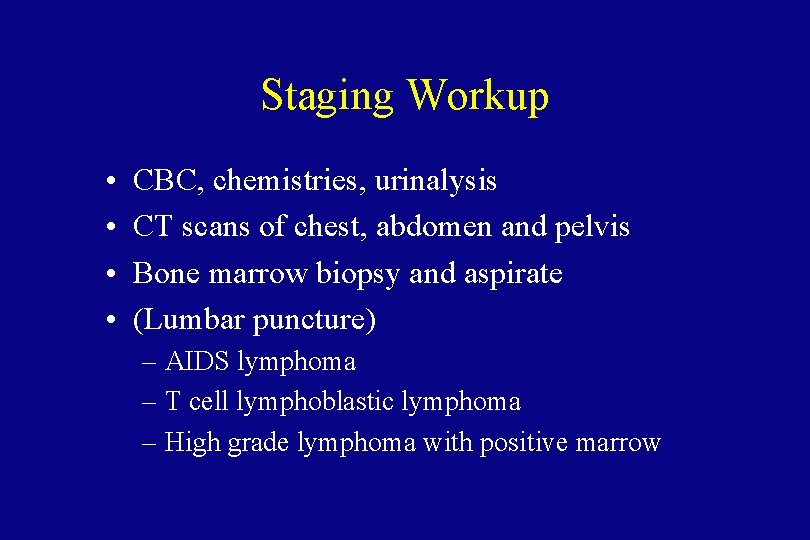
Staging Workup • • CBC, chemistries, urinalysis CT scans of chest, abdomen and pelvis Bone marrow biopsy and aspirate (Lumbar puncture) – AIDS lymphoma – T cell lymphoblastic lymphoma – High grade lymphoma with positive marrow
Staging laparotomy and lymphangiogram are not indicated in non-Hodgkin’s lymphoma.
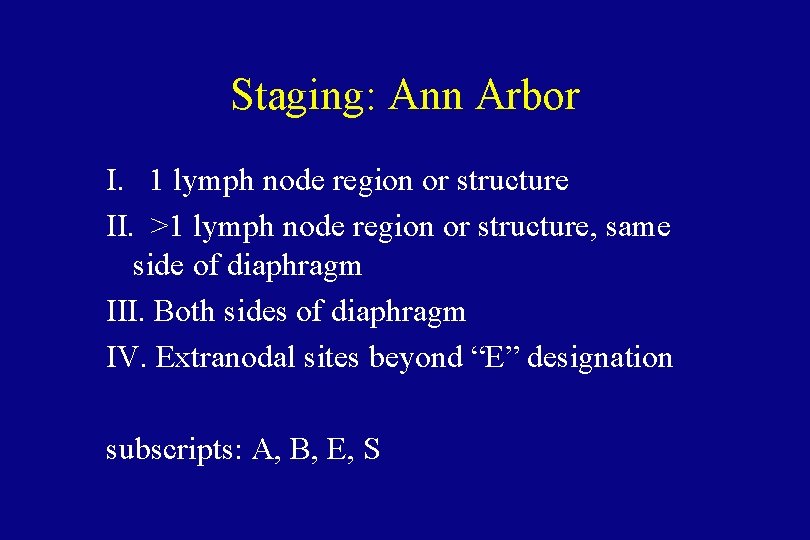
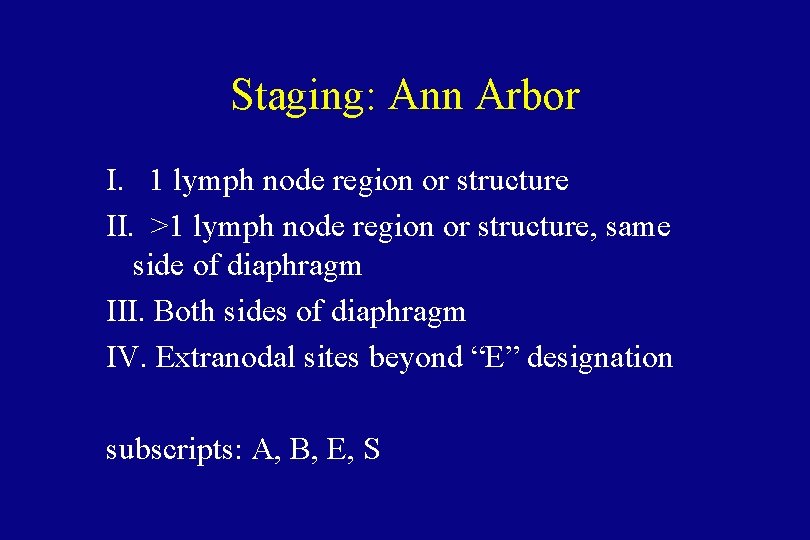
Staging: Ann Arbor I. 1 lymph node region or structure II. >1 lymph node region or structure, same side of diaphragm III. Both sides of diaphragm IV. Extranodal sites beyond “E” designation subscripts: A, B, E, S
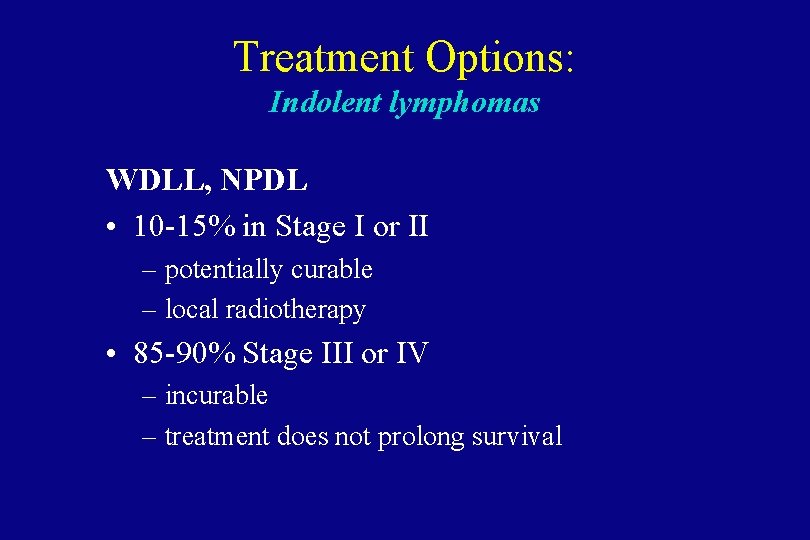
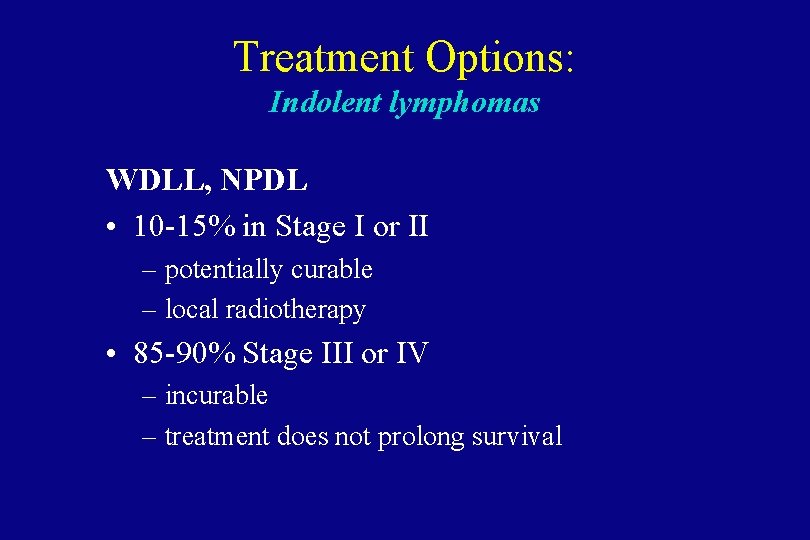
Treatment Options: Indolent lymphomas WDLL, NPDL • 10 -15% in Stage I or II – potentially curable – local radiotherapy • 85 -90% Stage III or IV – incurable – treatment does not prolong survival

Reasons to Treat in Advanced Indolent Lymphomas • • • Constitutional symptoms Anatomic obstruction Organ dysfunction Cosmetic considerations Painful lymph nodes Cytopenias
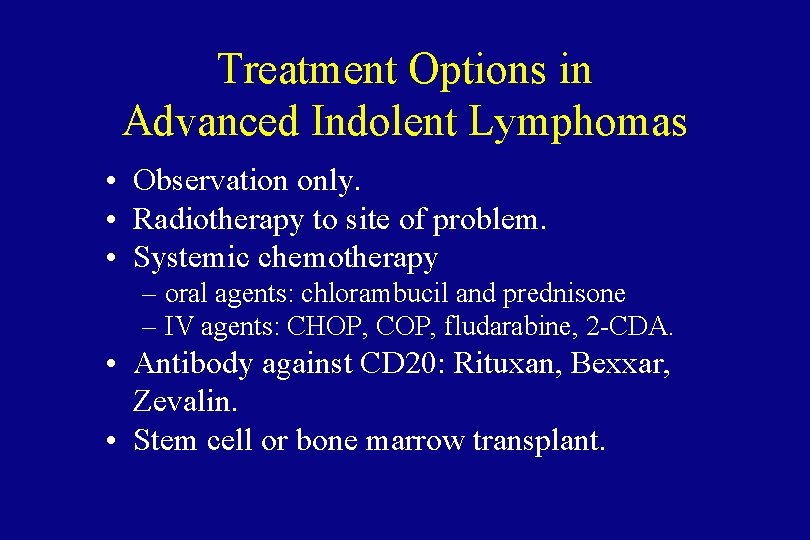
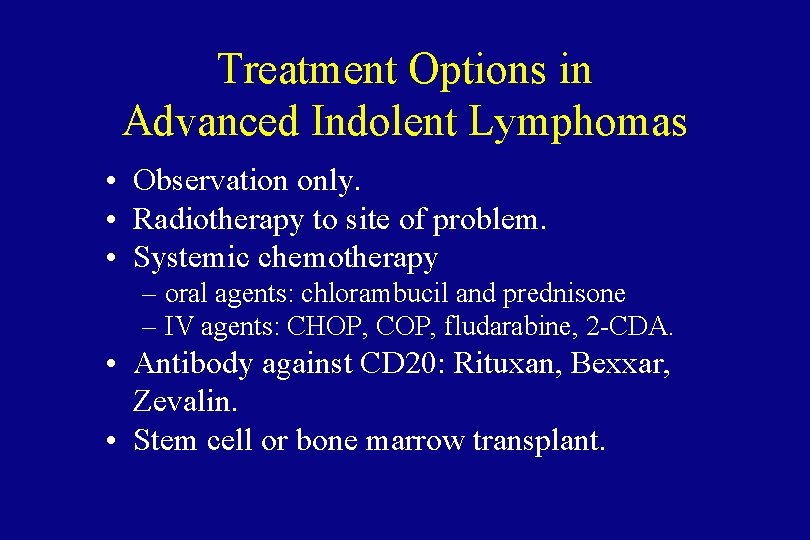
Treatment Options in Advanced Indolent Lymphomas • Observation only. • Radiotherapy to site of problem. • Systemic chemotherapy – oral agents: chlorambucil and prednisone – IV agents: CHOP, COP, fludarabine, 2 -CDA. • Antibody against CD 20: Rituxan, Bexxar, Zevalin. • Stem cell or bone marrow transplant.

CHOP Chemotherapy • • Cyclophosphamide (Cytoxan) Hydroxydaunorubicin (Adriamycin) Oncovin (vincristine) Prednisone
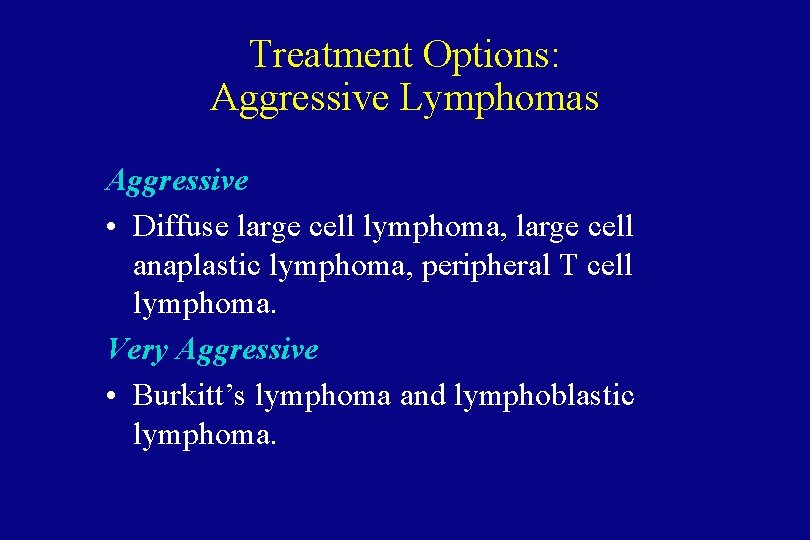
Treatment Options: Aggressive Lymphomas Aggressive • Diffuse large cell lymphoma, large cell anaplastic lymphoma, peripheral T cell lymphoma. Very Aggressive • Burkitt’s lymphoma and lymphoblastic lymphoma.
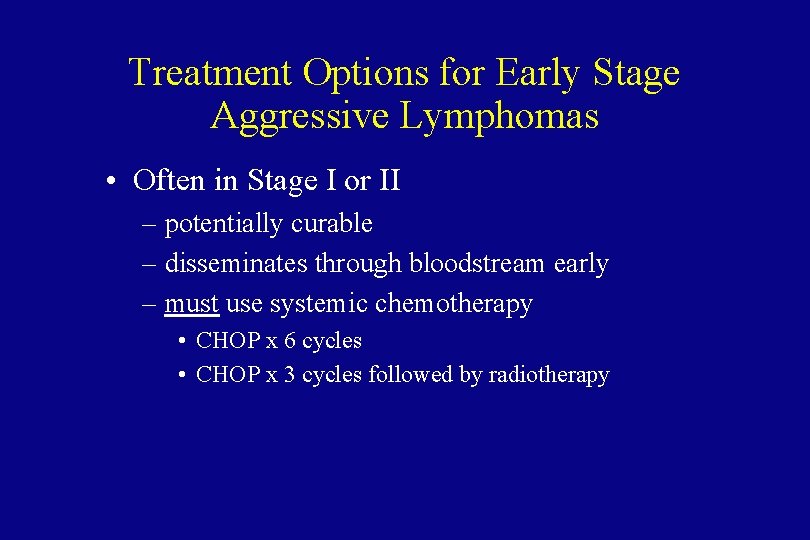
Treatment Options for Early Stage Aggressive Lymphomas • Often in Stage I or II – potentially curable – disseminates through bloodstream early – must use systemic chemotherapy • CHOP x 6 cycles • CHOP x 3 cycles followed by radiotherapy
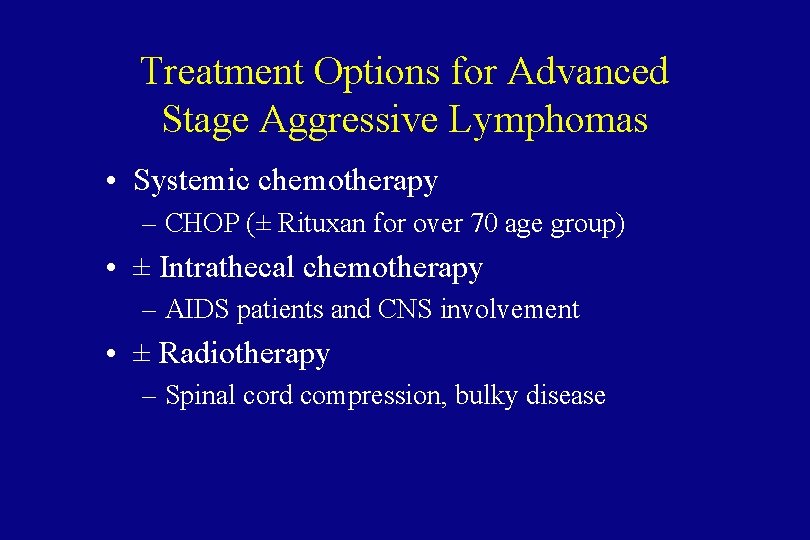
Treatment Options for Advanced Stage Aggressive Lymphomas • Systemic chemotherapy – CHOP (± Rituxan for over 70 age group) • ± Intrathecal chemotherapy – AIDS patients and CNS involvement • ± Radiotherapy – Spinal cord compression, bulky disease
Lymphoblastic Lymphoma • • T cell malignancy. Male adolescents. Mediastinal mass. T cell variant of T cell acute lymphoblastic leukemia. • Prognosis improving with intensive ALL regimens.

Burkitt’s Lymphoma • African variety: jaw tumor, strongly linked to Epstein-Barr Virus infection. • In U. S. , about 50% EBV infection. • May present as abdominal mass. • Most rapidly growing human tumor. • Typical chromosome abnormality: c-myc oncogene linked to one of the immunoglobulin genes.
Burkitt’s Lymphoma • Treated with multidrug regimen similar to pediatric leukemia/lymphoma regimens.
Notable Subtypes of Lymphoma
Mycosis Fungoides • Malignancy of helper T cells. • Affinity for skin. • Can be treated with electron beam radiation, ultraviolet light, or topical alkylating agents.

AIDS Lymphoma • Aggressive lymphomas of B cell origin. • Burkitt’s, Burkitt’s-like, and large cell immunoblastic. • Treatment often limited by immune compromise of the patient. • Prognosis improved with HAART therapy.
MALT Lymphoma • Mucosa-Associated Lymphoid Tissue • Chronic infection of the stomach by Helicobacter pylori. • Localized to the stomach, indolent course. • Can be cured in many cases by antibiotics against H. pylori.

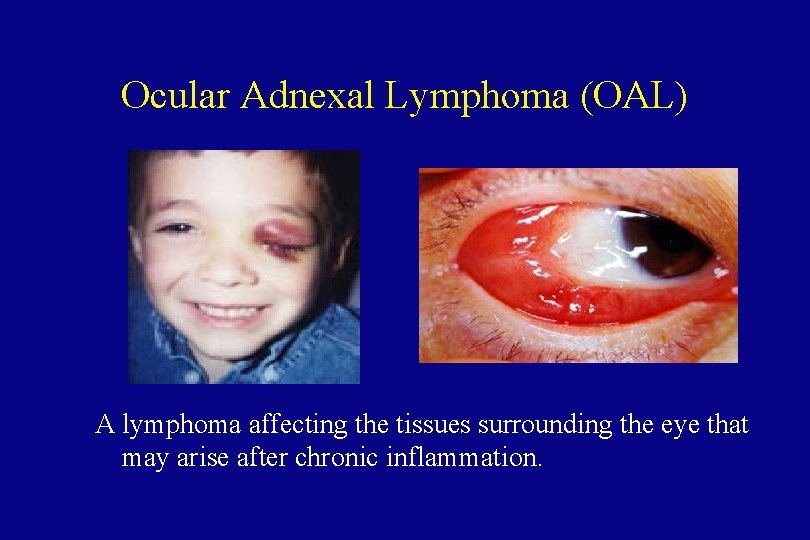
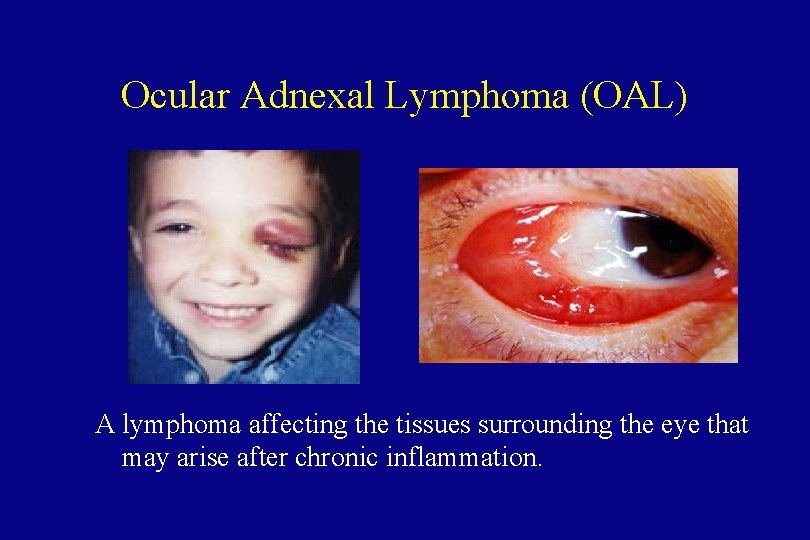
Ocular Adnexal Lymphoma (OAL) A lymphoma affecting the tissues surrounding the eye that may arise after chronic inflammation.
Treatment • May respond to antibiotic therapy against Chlamydia. • One patient treated with doxycycline (100 mg bid for 3 weeks) had complete remission for more than 12 months, and another patient had minimal remission for more than 18 months. ASCO 2003, Abstract 2273
Hodgkin’s Disease
Thomas Hodgkin English pathologist, described the disease that bears his name in 1832.

Paul Allen Cofounded Microsoft with Bill Gates
Mario Lemieux Top player in the US National Hockey League
Brandon Tartikoff Youngest US television network president (Cosby, Seinfeld)
Hodgkin’s Disease • One-seventh as common a snon-Hodgkin’s lymphoma. • Highly treatable and curable, even when disseminated. • Presence of Reed-Sternberg cell is necessary to make diagnosis.
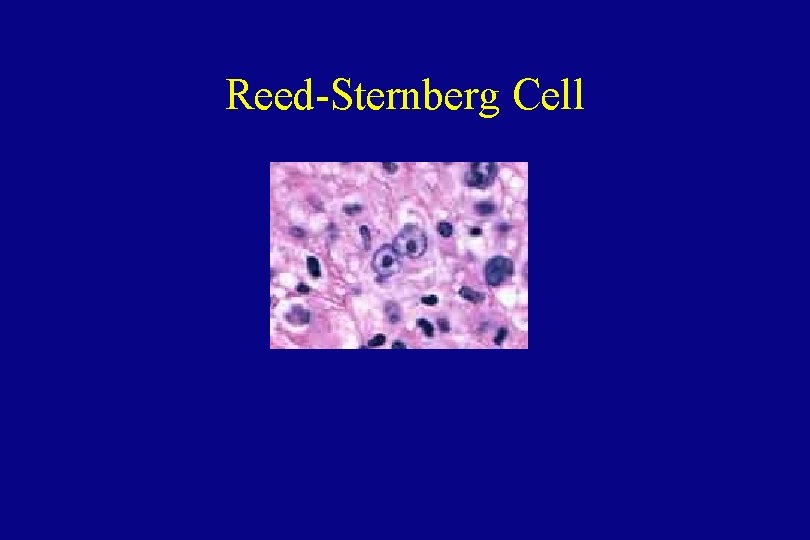
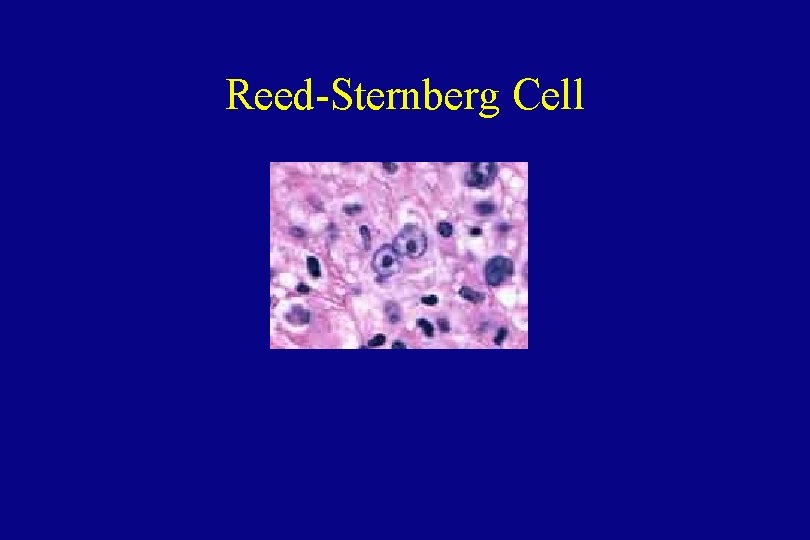
Reed-Sternberg Cell
Subtypes of Hodgkin’s Disease • • Lymphocyte predominant Nodular sclerosis Mixed cellularity Lymphocyte depleted Unlike non-Hodgkin’s lymphoma, in Hodgkin’s Disease the histologic subtype does not determine how the disease is treated.
Etiology of Hodgkin’s Disease • Reed-Sternberg cells are the malignant cells. • Minor population in the malignant tissues – many normal lymphocytes, eosinophils, other cells • Cell of origin is unknown: T, B, both, neither. • Some R-S cells contain EBV genomes.
Epidemiology • In developed countries, bimodal distribution of patients. – young adulthood – after age 50 • More common in affluent families with few siblings. • In developing countries, more common in young children.
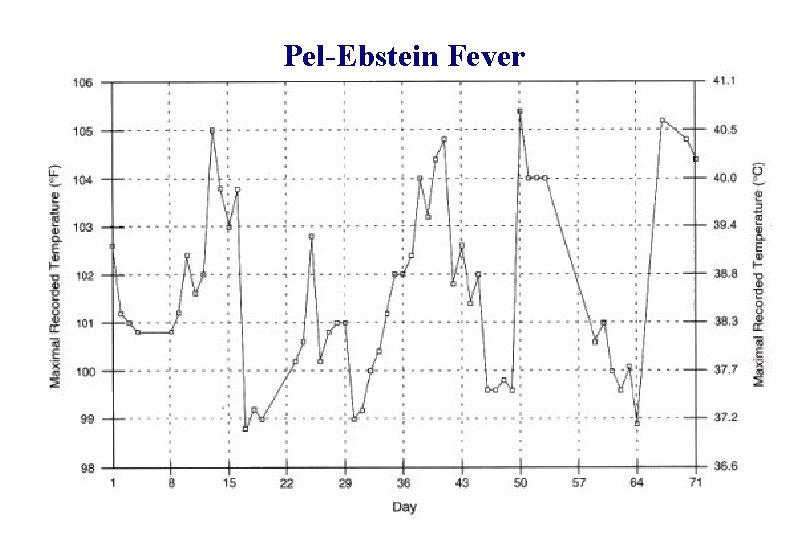
Signs and Symptoms • Lymph node enlargement, usually cervical or mediastinal. • Systemic “B” symptoms common. • Pel-Ebstein fever. – relapsing, high-grade fever that can reach 105106°F, periodicity of 7 -10 days. Fever spikes abrupt in onset and resolution • Pain on drinking alcohol.
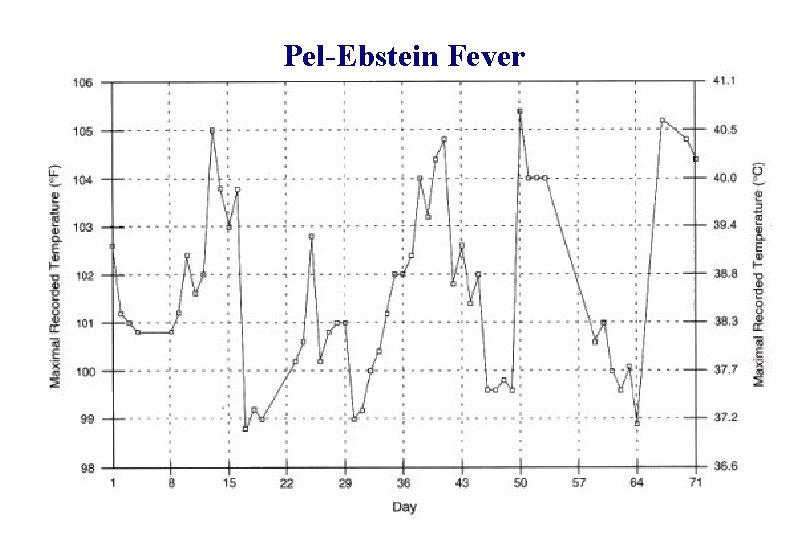
Pel-Ebstein Fever
Clinical Features • T cell mediated immune deficiency, even in early stage disease. Prone to infections: – Herpes zoster (“shingles”) in one fourth of patients – Fungal or mycobacterial infections • Immune defect may persist even after lymphoma is cured.
Clinical Features • Predictable contiguous spread of disease: – cervical nodes to mediastinum or axilla – mediastinum to periaortic nodes or spleen, etc. • Basis for staging and treatment decisions.
Diagnosis • Excisional biopsy of a lymph node. Fine needle aspirate is not sufficient to make the diagnosis of Hodgkin’s disease.
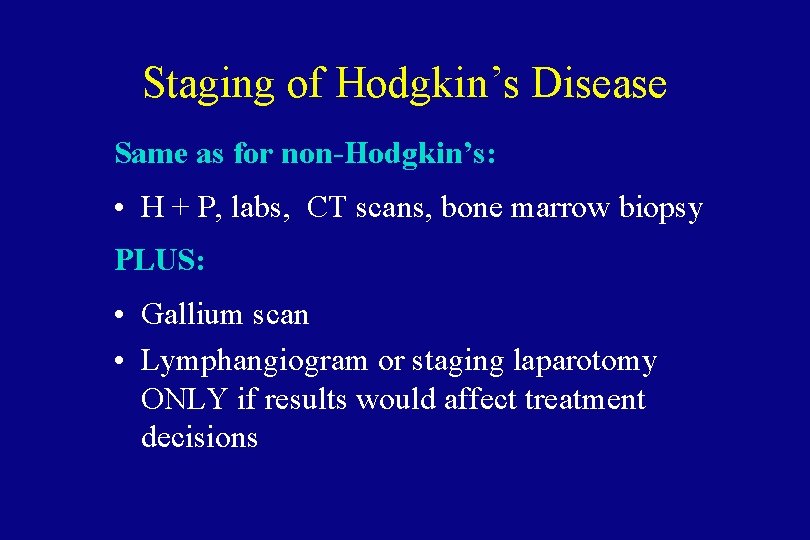
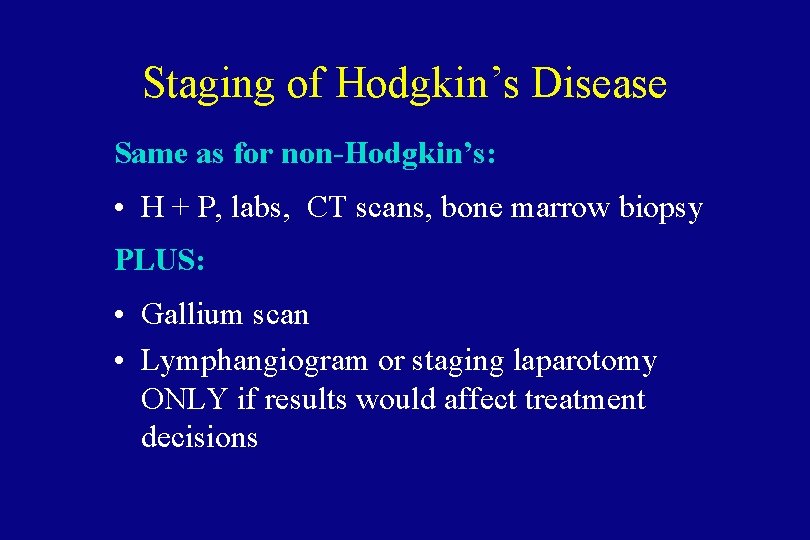
Staging of Hodgkin’s Disease Same as for non-Hodgkin’s: • H + P, labs, CT scans, bone marrow biopsy PLUS: • Gallium scan • Lymphangiogram or staging laparotomy ONLY if results would affect treatment decisions
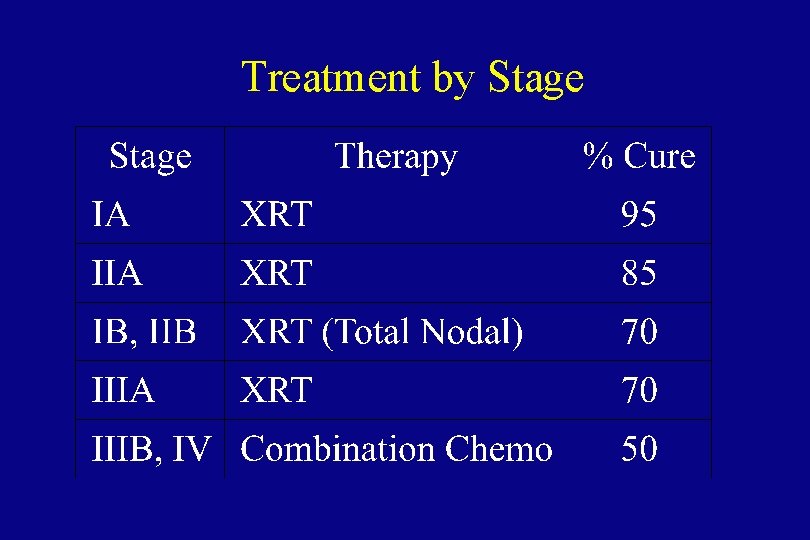
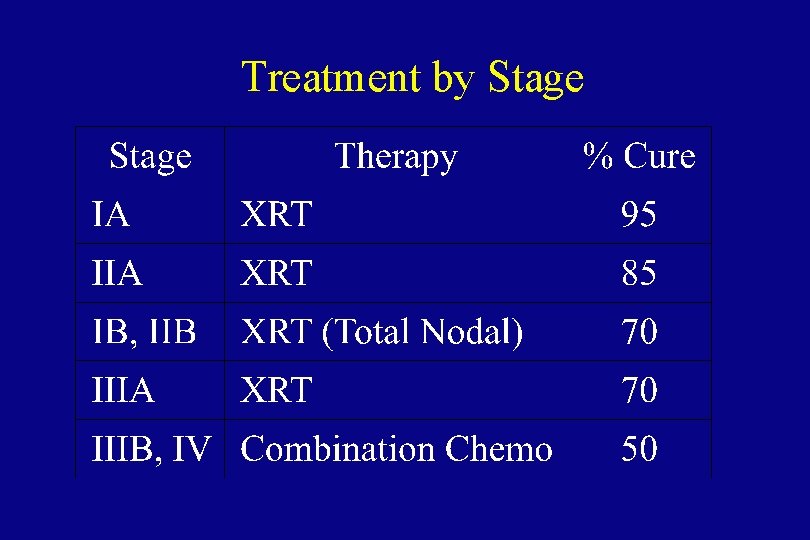
Treatment by Stage
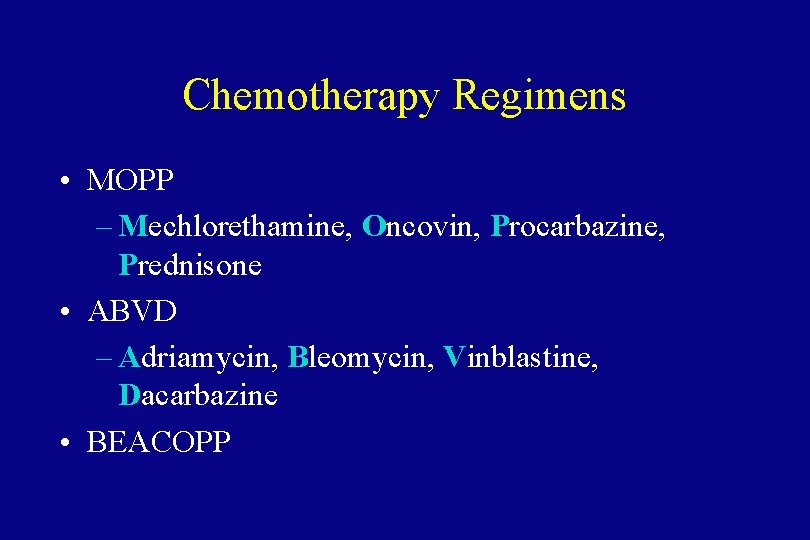
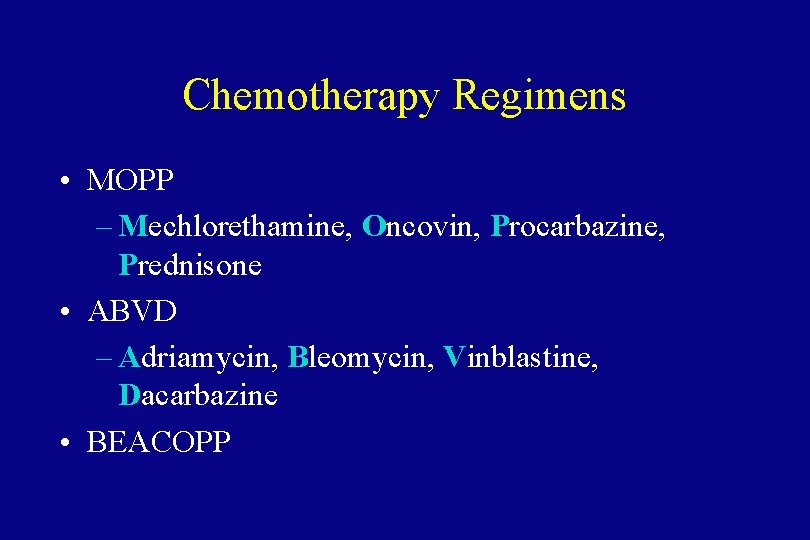
Chemotherapy Regimens • MOPP – Mechlorethamine, Oncovin, Procarbazine, Prednisone • ABVD – Adriamycin, Bleomycin, Vinblastine, Dacarbazine • BEACOPP
Treatment Options • Often, patients who relapse after radiotherapy can be cured by salvage chemotherapy. • Combined chemotherapy and radiotherapy is given for bulky mediastinal masses. • Chemotherapy now being tested for earlier stages of the disease.
Late Complications of Hodgkin’s Disease • High incidence of second malignancies – leukemia first 10 years, solid tumors over time. • Leukemia in patients receiving alkylating agents or combined chemo/XRT. • Lung cancer and breast cancer in patients receiving XRT to chest. Lung cancer especially high in smokers.
Late Complications of Hodgkin’s Disease • Hypothyroidism after irradiation of the neck. • Constrictive pericarditis after radiotherapy to the mediastinum. • Infertility after use of alkylating agents. • Heart failure after Adriamycin treatment.
Multiple Myeloma
Ann Landers Advice Columnist
Mark Lenard Sarek (Spock’s father) on Star Trek
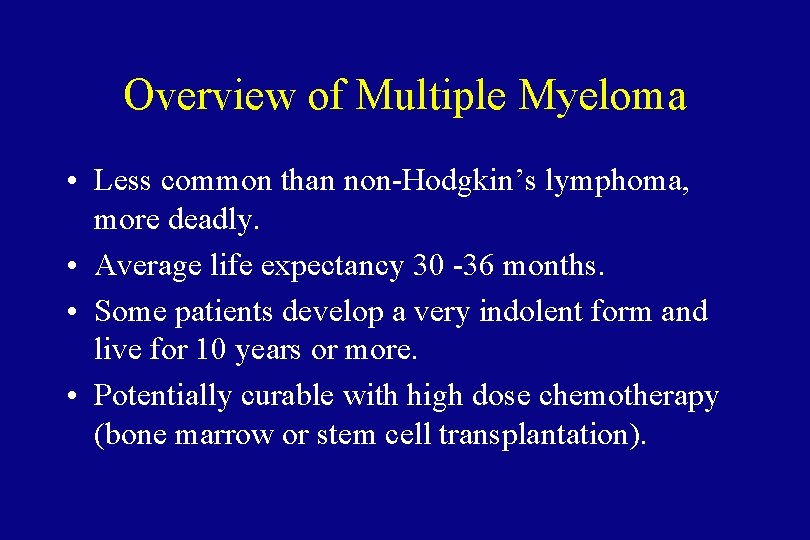
Overview of Multiple Myeloma • Less common than non-Hodgkin’s lymphoma, more deadly. • Average life expectancy 30 -36 months. • Some patients develop a very indolent form and live for 10 years or more. • Potentially curable with high dose chemotherapy (bone marrow or stem cell transplantation).
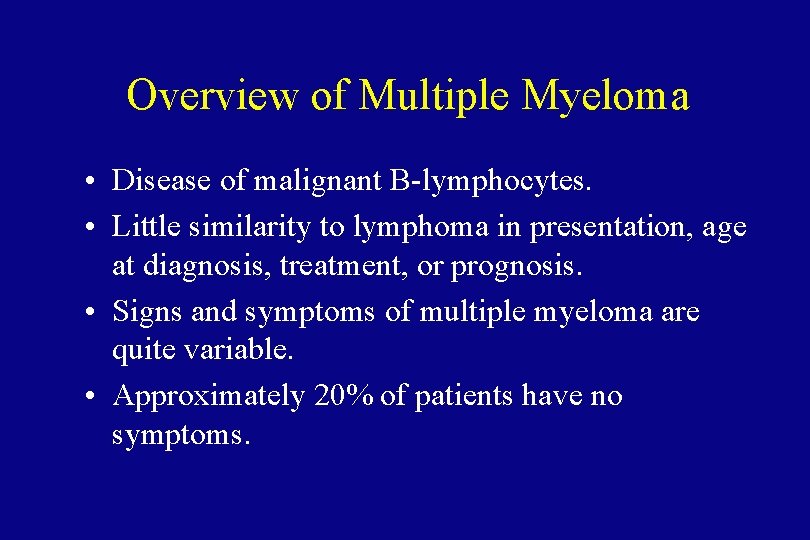
Overview of Multiple Myeloma • Disease of malignant B-lymphocytes. • Little similarity to lymphoma in presentation, age at diagnosis, treatment, or prognosis. • Signs and symptoms of multiple myeloma are quite variable. • Approximately 20% of patients have no symptoms.
Etiology of Multiple Myeloma • Unknown. Suggested predisposing factors include: – Viral infection with Human Herpesvirus 8 (HHV-8). – MGUS (monoclonal gammopathy of undetermined significance).

Epidemiology • • • Average at presentation is about 65. Males are affected more often than females. Incidence in blacks is twice that of whites. Five-year survival is approximately 25 -30%. Median survival 30 -36 months.

Multiple Myeloma • More than 15% plasma cells in the bone marrow. • Monoclonal immunoglobulin peak on SPEP – more than 3 gm/d. L. • Presence of Bence Jones protein in urine. • Decreased levels of normal immunoglobulins.
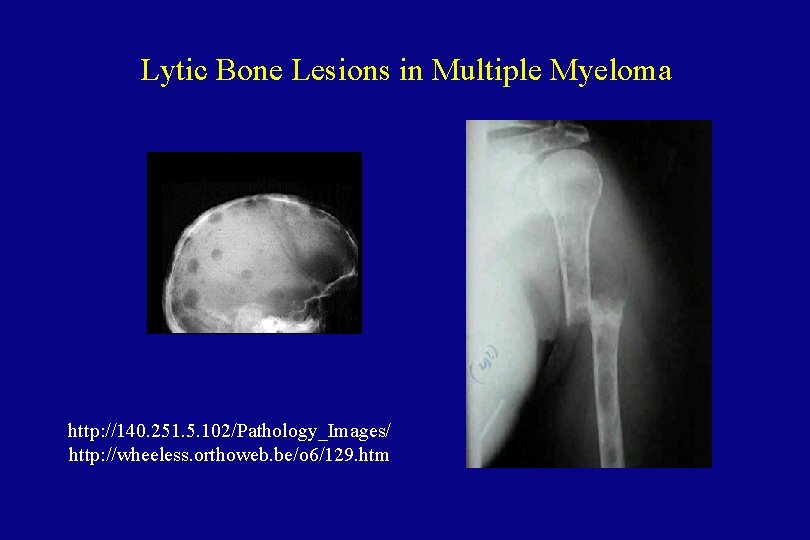
Clinical Features • Bone marrow failure - Anemia, thrombocytopenia, neutropenia • Renal failure • Bone disease with skeletal destruction – lytic lesions – generalized decrease in bone density • Hypercalcemia
Clinical Features • Hyperviscosity syndrome • Recurrent infections • Amyloidosis

Diagnosis and Staging Workup • Bone marrow biopsy and aspirate • Serum protein electrophoresis and immunofixation • Skeletal survey – Plain x-rays are better than bone scan. – Lytic lesions do not show up well on bone scan. • Quantitative immunoglobulins
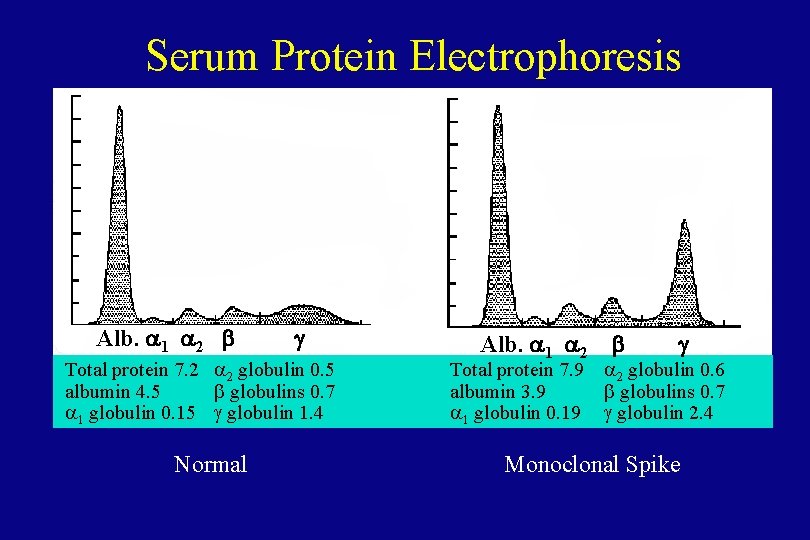
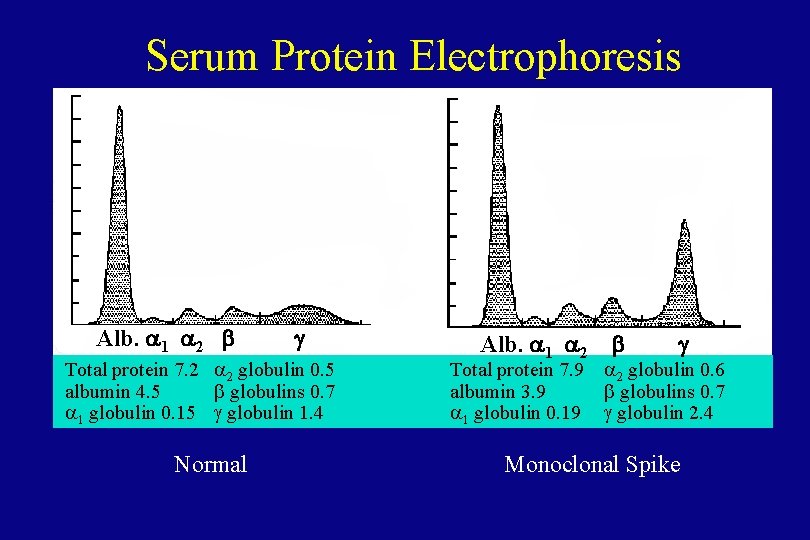
Serum Protein Electrophoresis Alb. a 1 a 2 b g Total protein 7. 2 a 2 globulin 0. 5 albumin 4. 5 b globulins 0. 7 a 1 globulin 0. 15 g globulin 1. 4 Normal Alb. a 1 a 2 Total protein 7. 9 albumin 3. 9 a 1 globulin 0. 19 b g a 2 globulin 0. 6 b globulins 0. 7 g globulin 2. 4 Monoclonal Spike
Monoclonal Immunoglobulin Spike on Serum Protein Electrophoresis (SPEP) • Multiple myeloma • Non-Hodgkin’s lymphoma • Monoclonal gammopathy of undetermined significance (MGUS). Not clinically significant unless present in high quantity (over 3 gm/d. L).
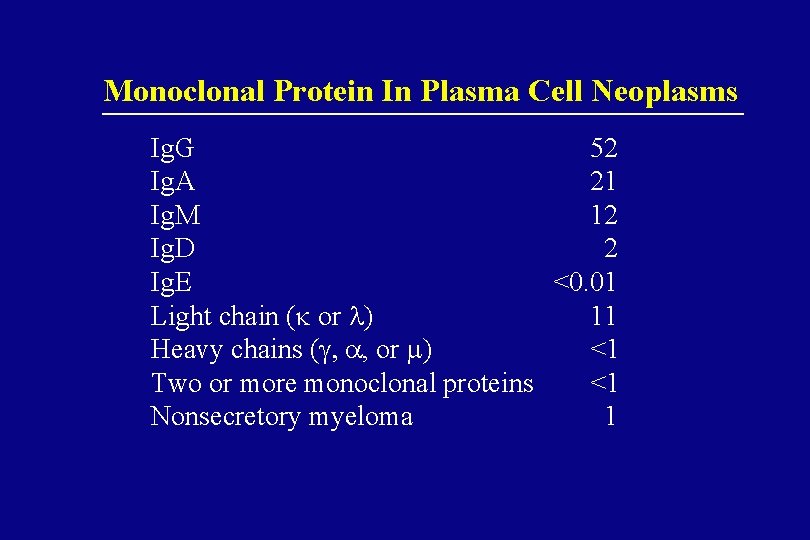
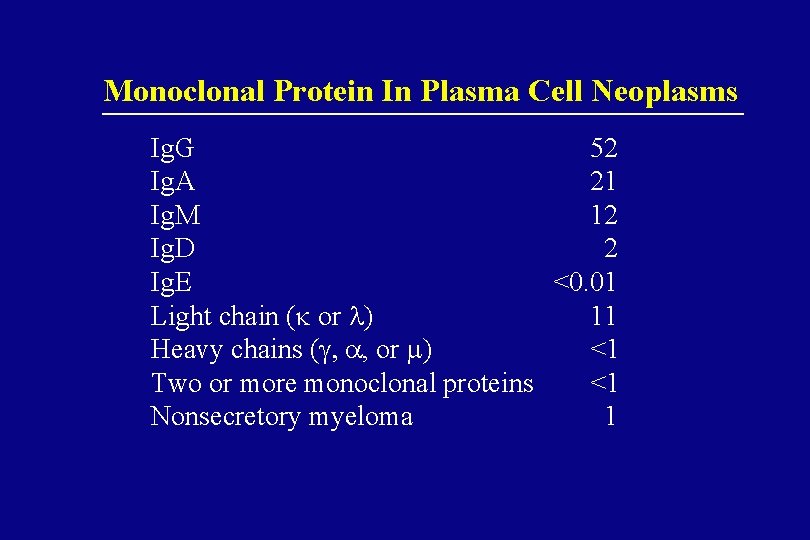
Monoclonal Protein In Plasma Cell Neoplasms Ig. G 52 Ig. A 21 Ig. M 12 Ig. D 2 Ig. E <0. 01 Light chain (k or l) 11 Heavy chains (g, a, or m) <1 Two or more monoclonal proteins <1 Nonsecretory myeloma 1
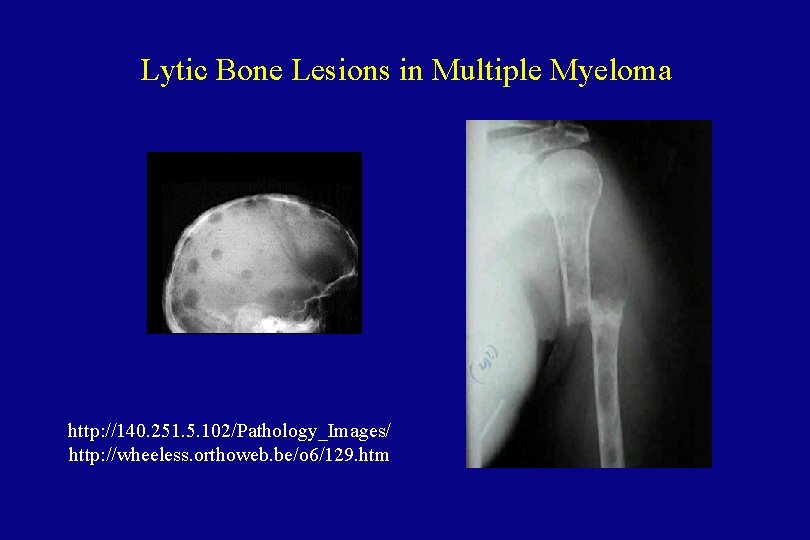
Lytic Bone Lesions in Multiple Myeloma http: //140. 251. 5. 102/Pathology_Images/ http: //wheeless. orthoweb. be/o 6/129. htm
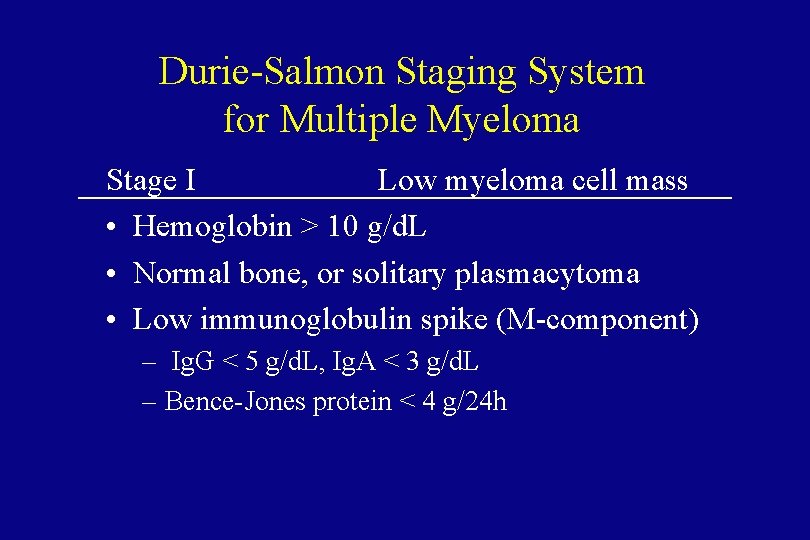
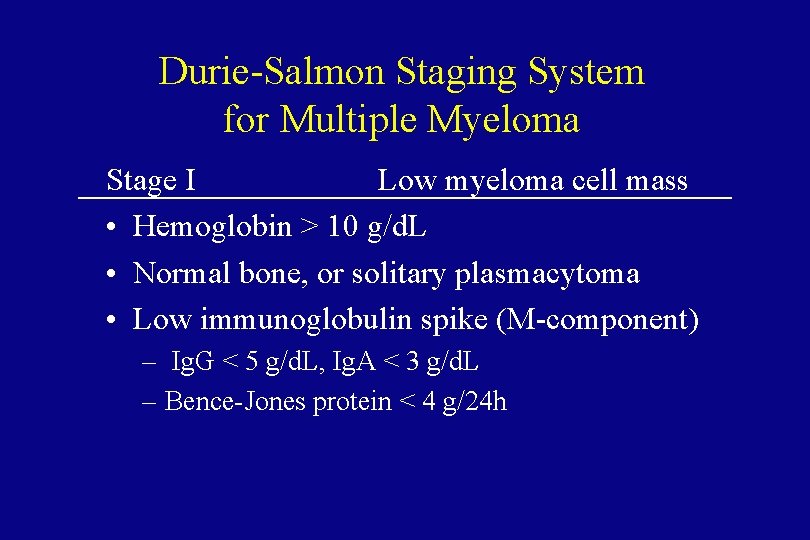
Durie-Salmon Staging System for Multiple Myeloma Stage I Low myeloma cell mass • Hemoglobin > 10 g/d. L • Normal bone, or solitary plasmacytoma • Low immunoglobulin spike (M-component) – Ig. G < 5 g/d. L, Ig. A < 3 g/d. L – Bence-Jones protein < 4 g/24 h
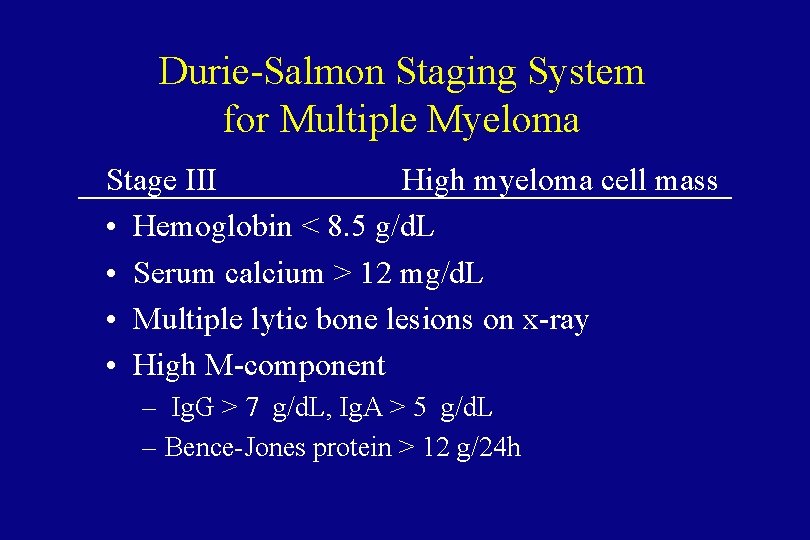
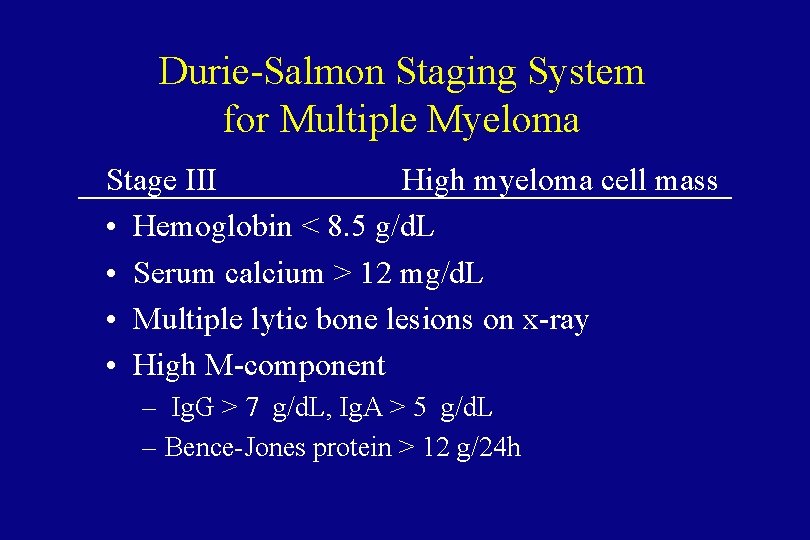
Durie-Salmon Staging System for Multiple Myeloma Stage III High myeloma cell mass • Hemoglobin < 8. 5 g/d. L • Serum calcium > 12 mg/d. L • Multiple lytic bone lesions on x-ray • High M-component – Ig. G > 7 g/d. L, Ig. A > 5 g/d. L – Bence-Jones protein > 12 g/24 h
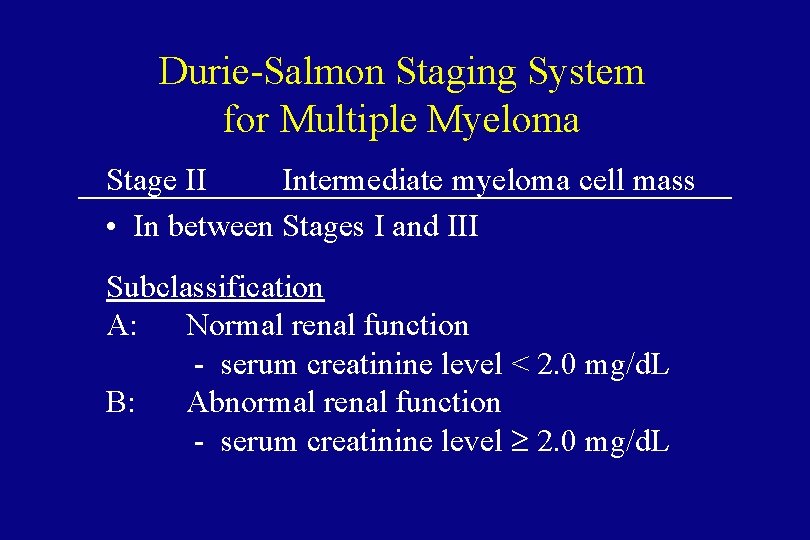
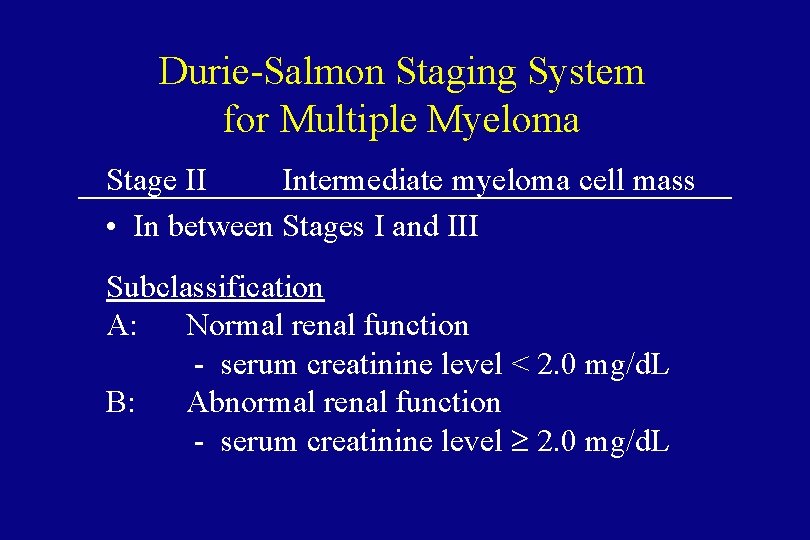
Durie-Salmon Staging System for Multiple Myeloma Stage II Intermediate myeloma cell mass • In between Stages I and III Subclassification A: Normal renal function - serum creatinine level < 2. 0 mg/d. L B: Abnormal renal function - serum creatinine level ³ 2. 0 mg/d. L
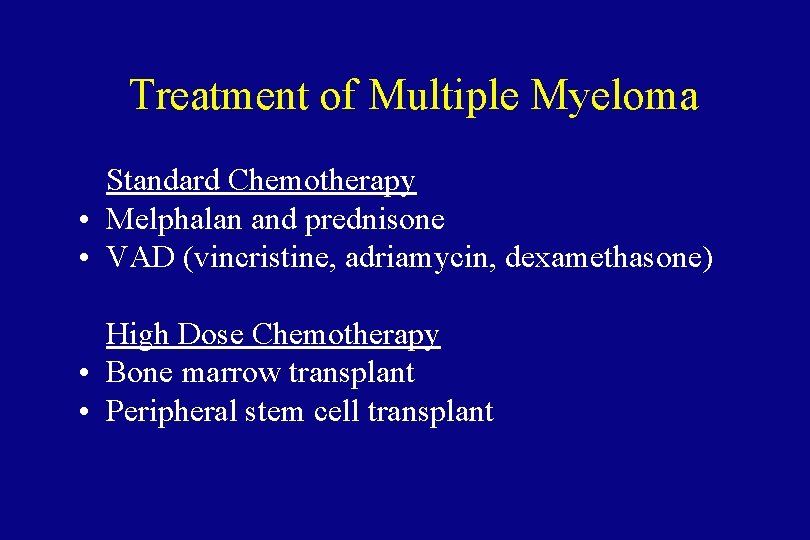
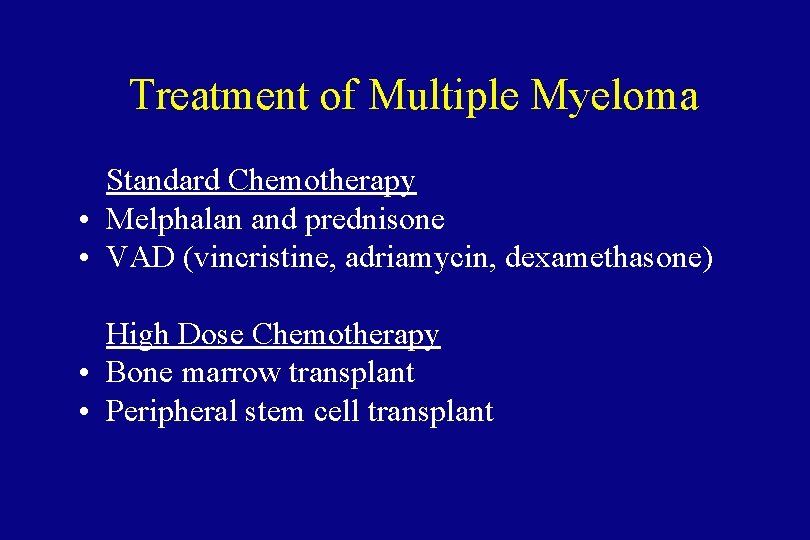
Treatment of Multiple Myeloma Standard Chemotherapy • Melphalan and prednisone • VAD (vincristine, adriamycin, dexamethasone) High Dose Chemotherapy • Bone marrow transplant • Peripheral stem cell transplant
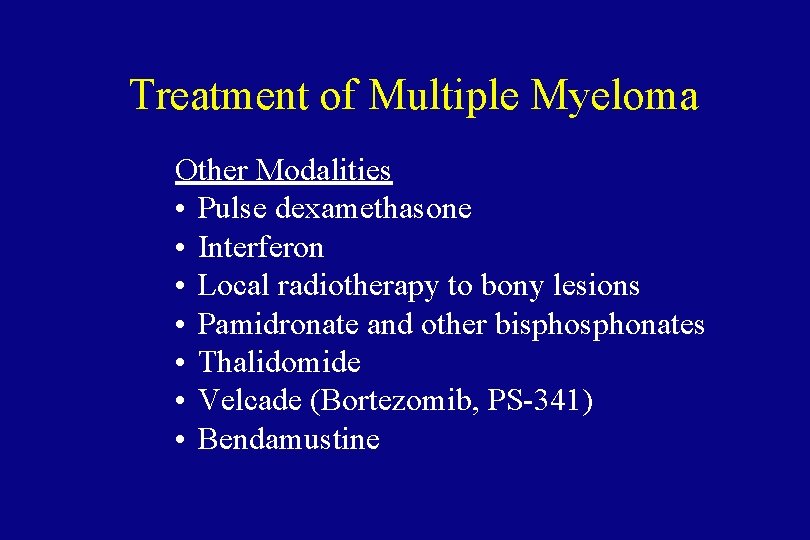
Treatment of Multiple Myeloma Other Modalities • Pulse dexamethasone • Interferon • Local radiotherapy to bony lesions • Pamidronate and other bisphonates • Thalidomide • Velcade (Bortezomib, PS-341) • Bendamustine

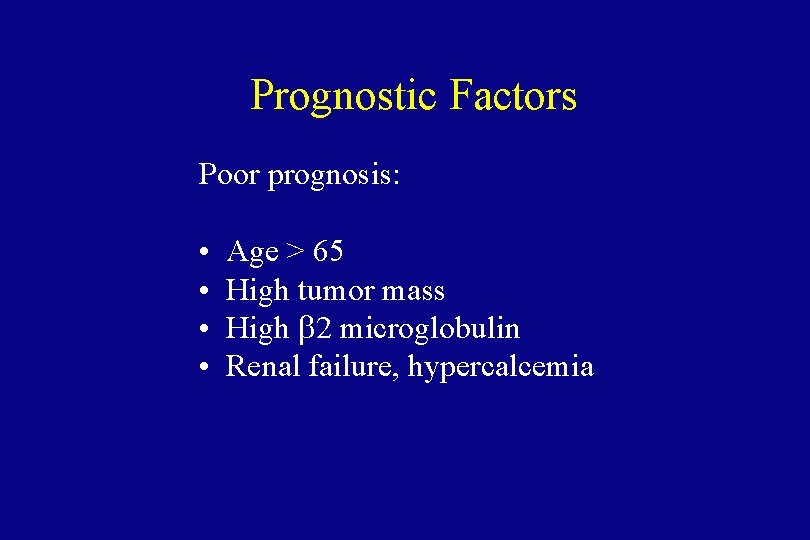
Prognostic Factors Poor prognosis: • • Age > 65 High tumor mass High b 2 microglobulin Renal failure, hypercalcemia
Conclusions: Lymphoma and Multiple Myeloma • • Malignancies of B cells. Sometimes preventable. Highly treatable and often curable. Study of these diseases have led to important advances in the understanding of the biology of lymphoid cells.
 Terry hayes md
Terry hayes md Smoldering lymphoma
Smoldering lymphoma Crab mm
Crab mm Vtd protocol multiple myeloma
Vtd protocol multiple myeloma Waldenstrom's disease
Waldenstrom's disease Multiple myelom tanı kriterleri
Multiple myelom tanı kriterleri Waldenstrom macroglobulinemia vs multiple myeloma
Waldenstrom macroglobulinemia vs multiple myeloma Kpd multiple myeloma
Kpd multiple myeloma Mayo clinic multiple myeloma
Mayo clinic multiple myeloma Smoldering multiple myeloma
Smoldering multiple myeloma Exercise physiology mascot
Exercise physiology mascot European myeloma network
European myeloma network Myeloma cure on the horizon
Myeloma cure on the horizon Myeloma
Myeloma Anita waldmann
Anita waldmann Difference between hodgkin and non hodgkin lymphoma
Difference between hodgkin and non hodgkin lymphoma Leukemia vs lymphoma
Leukemia vs lymphoma Primary cutaneous gamma/delta t-cell lymphoma
Primary cutaneous gamma/delta t-cell lymphoma Adams hayes and hopson transition theory
Adams hayes and hopson transition theory Barbara douglas counselling psychologist
Barbara douglas counselling psychologist Hiv roga lakshana
Hiv roga lakshana Indolent non-hodgkin lymphoma quizlet
Indolent non-hodgkin lymphoma quizlet Lymphoma
Lymphoma Lymphoma classification ppt
Lymphoma classification ppt Hodgkin's lymphoma alcohol pain
Hodgkin's lymphoma alcohol pain Mark juckett
Mark juckett Ann arbor staging system
Ann arbor staging system Pleural space
Pleural space Rbac mantle cell lymphoma
Rbac mantle cell lymphoma Classification of hodgkin lymphoma
Classification of hodgkin lymphoma Burkitt lymphoma
Burkitt lymphoma Hodjkins disease
Hodjkins disease Burkitt lymphoma
Burkitt lymphoma Szóbajön
Szóbajön Non-hodgkin lymphoma
Non-hodgkin lymphoma Lymphoma case presentation
Lymphoma case presentation Maintenance rituximab mantle cell lymphoma
Maintenance rituximab mantle cell lymphoma Hepatosplenic t-cell lymphoma
Hepatosplenic t-cell lymphoma Neoplastic proliferation of white blood cells
Neoplastic proliferation of white blood cells Splenomegaly and hypersplenism
Splenomegaly and hypersplenism Hodgkin lymphoma classification
Hodgkin lymphoma classification Bcell lymphoma
Bcell lymphoma Gadolinium mrt
Gadolinium mrt Nonhodgkins lymphoma
Nonhodgkins lymphoma Sanjana bhagwat
Sanjana bhagwat Aspiration biopsy
Aspiration biopsy Multiple baseline across settings
Multiple baseline across settings Shared memory mimd architecture
Shared memory mimd architecture Adien ficci
Adien ficci Taylor hayes bio
Taylor hayes bio Hayes valley south
Hayes valley south Hallicarnasus
Hallicarnasus David hayes sheffield
David hayes sheffield Kelsey-hayes abs schematic
Kelsey-hayes abs schematic Rylie hayes
Rylie hayes Rutherford b hayes
Rutherford b hayes Swampfox mohawk
Swampfox mohawk Color 06062002
Color 06062002 Chapter 13 the catcher in the rye
Chapter 13 the catcher in the rye Bruce hayes ucla
Bruce hayes ucla Roth ira hamilton
Roth ira hamilton Van galen modeli nedir
Van galen modeli nedir Ivey hayes
Ivey hayes Niamh hayes
Niamh hayes Katelyn hayes
Katelyn hayes Wayne b. hayes
Wayne b. hayes Stephen hayes ericsson
Stephen hayes ericsson Brandi boyer interview
Brandi boyer interview Sally hayes catcher in the rye
Sally hayes catcher in the rye Alexander hayes
Alexander hayes Cardiac rehabilitation near south san francisco
Cardiac rehabilitation near south san francisco Dr niamh hayes
Dr niamh hayes Shana hayes
Shana hayes Hayes vle
Hayes vle The professor's appointment was shocking
The professor's appointment was shocking Intermediate math problems for students by m. colwell
Intermediate math problems for students by m. colwell Julie rae jennings
Julie rae jennings Terry goh
Terry goh Terry stop
Terry stop Terry richardson obama
Terry richardson obama Nazon maya
Nazon maya Terry fox elementary school
Terry fox elementary school Teori pengambilan keputusan
Teori pengambilan keputusan Terry laster
Terry laster Terry traffic tamer
Terry traffic tamer Terry eagleton what is a novel
Terry eagleton what is a novel Kaley jackson
Kaley jackson Michael fellows barrister
Michael fellows barrister Dr terry weaver
Dr terry weaver We finally arrived at your destination
We finally arrived at your destination Dr terry correll
Dr terry correll Terry tadlock
Terry tadlock Terry biddington
Terry biddington Name five pieces of equipment unique to pedicures
Name five pieces of equipment unique to pedicures Types of ergonomics
Types of ergonomics Marty strus stagg
Marty strus stagg Viessmann manufacturing company
Viessmann manufacturing company Terry fox paragraph
Terry fox paragraph The man behind the moon by shelton pacer genre
The man behind the moon by shelton pacer genre Terry hill framework operations strategy
Terry hill framework operations strategy Noman terry towel
Noman terry towel Terry gage
Terry gage Mary austin fecha de nacimiento
Mary austin fecha de nacimiento Ken wilber matrix
Ken wilber matrix Terry landscaping & lawn care
Terry landscaping & lawn care