Multiple Myeloma Multiple Myeloma Definition Malignant proliferation of











- Slides: 46
Multiple Myeloma
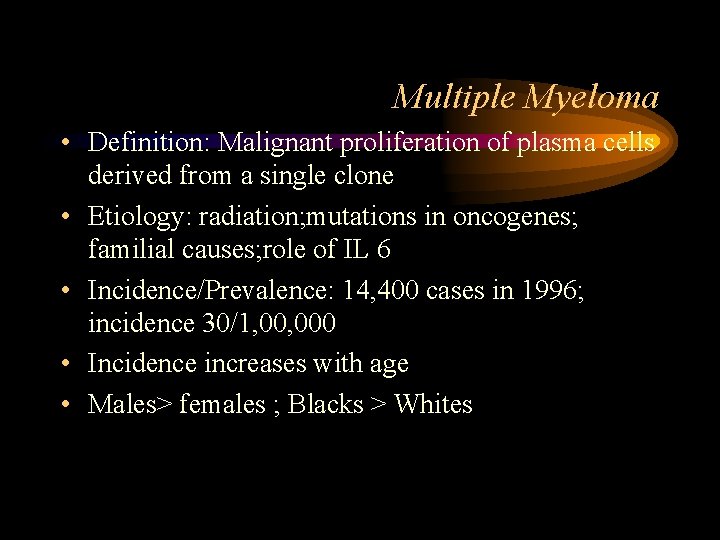
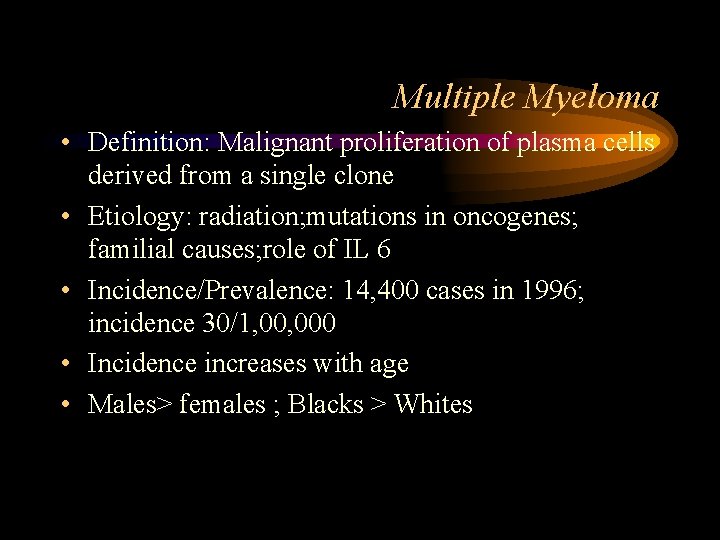
Multiple Myeloma • Definition: Malignant proliferation of plasma cells derived from a single clone • Etiology: radiation; mutations in oncogenes; familial causes; role of IL 6 • Incidence/Prevalence: 14, 400 cases in 1996; incidence 30/1, 000 • Incidence increases with age • Males> females ; Blacks > Whites
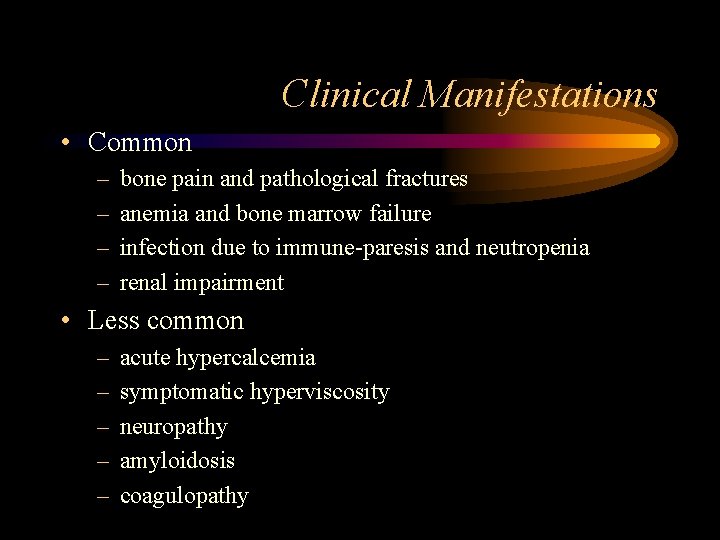
Clinical Manifestations • Common – – bone pain and pathological fractures anemia and bone marrow failure infection due to immune-paresis and neutropenia renal impairment • Less common – – – acute hypercalcemia symptomatic hyperviscosity neuropathy amyloidosis coagulopathy
Clinical Manifestations • Bone Pain: – 70%, Precipitated by movement – Pathological fractures – Activation of Osteoclasts by OAF produced by myeloma cells • Susceptibility to infections: – Diffuse hypogammaglob. If the M spike is excluded – Poor Antibody responses , Neutrophil dysfunction – Pneumococcus, S. aureus, GN aerobes. Pneumonia, Pyelonephrits

Clinical Manifestations • Renal failure: 25% – – Multiple contributory factors Hypercalcemia, Hyperuricemia, recuurent Infections Tubular damage produced by Light chains type 2 proximal RTA, Non selective proteinuria • Anemia: 80% – Normochromic/Normocytic – Myelophthisis; Inhibition by cytokines produced by plasma cells. – Leukopenia/thrombocytopenia only in advanced cases.
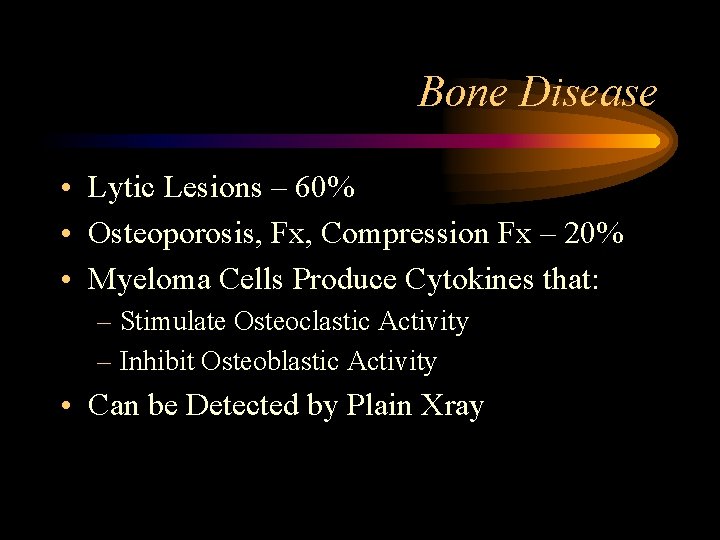
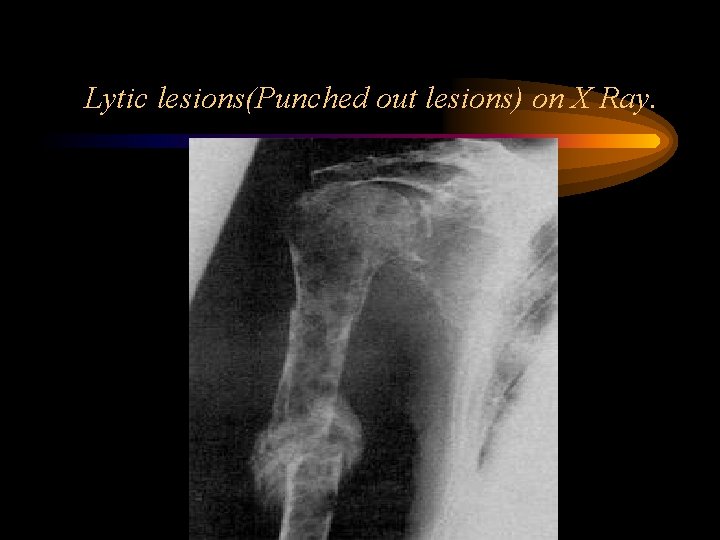
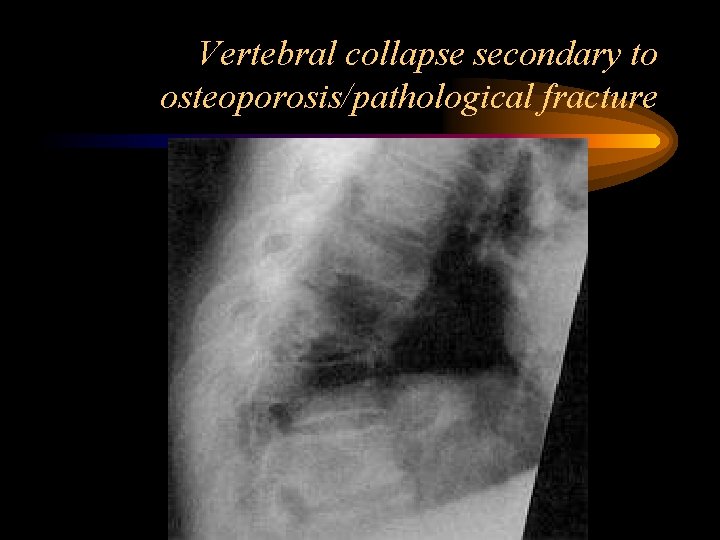
Bone Disease • Lytic Lesions – 60% • Osteoporosis, Fx, Compression Fx – 20% • Myeloma Cells Produce Cytokines that: – Stimulate Osteoclastic Activity – Inhibit Osteoblastic Activity • Can be Detected by Plain Xray
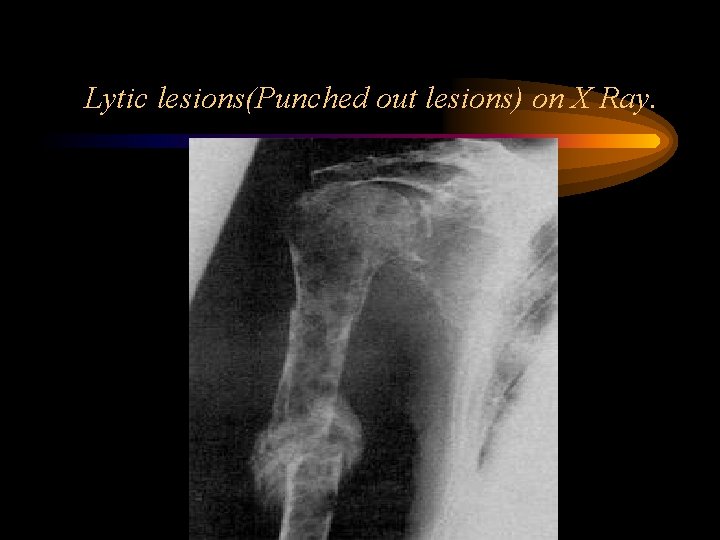
Lytic lesions(Punched out lesions) on X Ray.
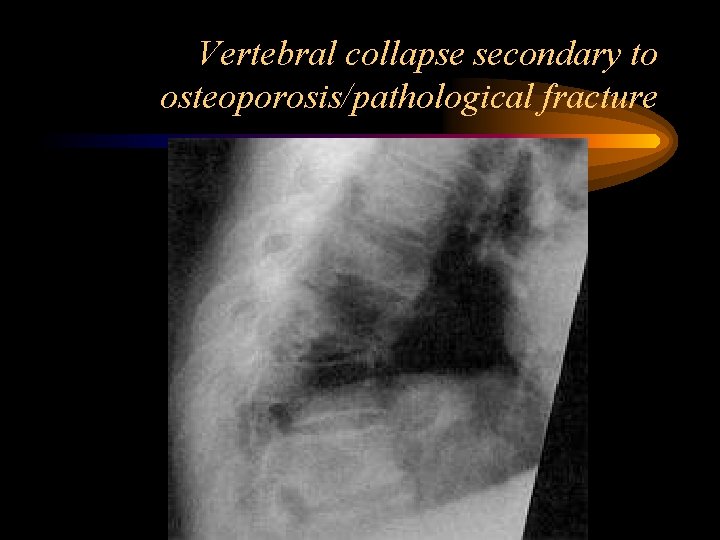
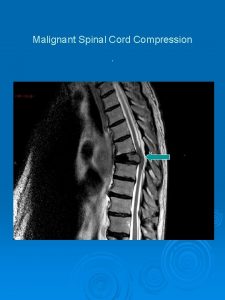
Vertebral collapse secondary to osteoporosis/pathological fracture

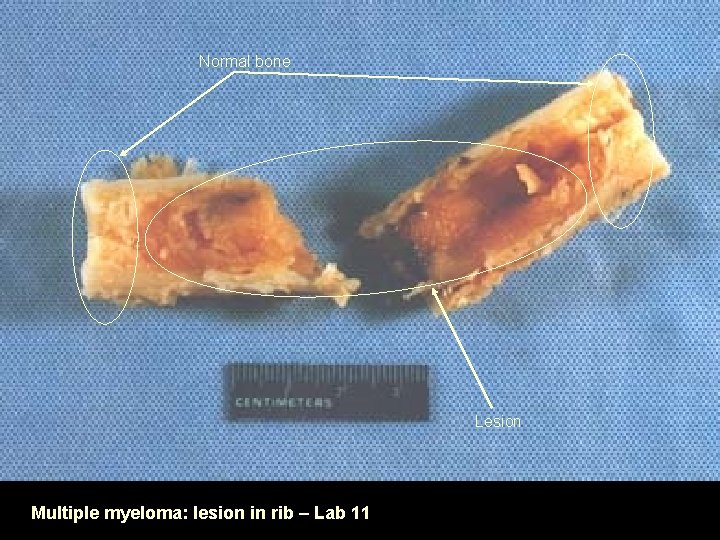
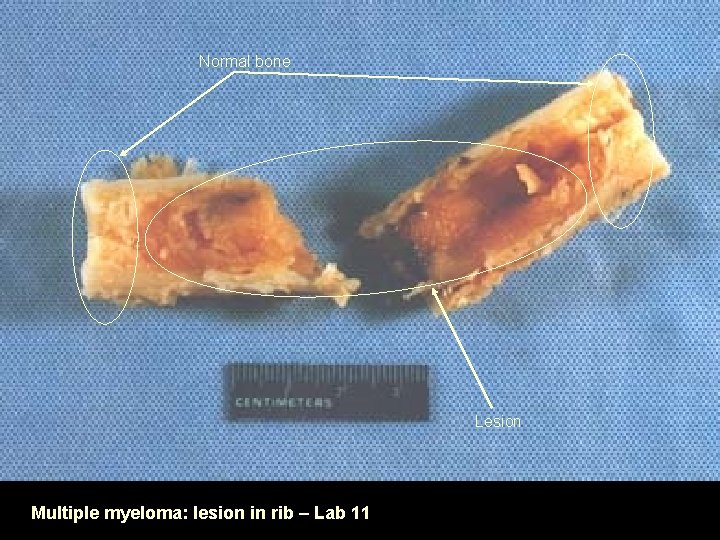
Normal bone Lesion Multiple myeloma: lesion in rib – Lab 11

Multiple myeloma: multiple lesions in skull – Lab 11
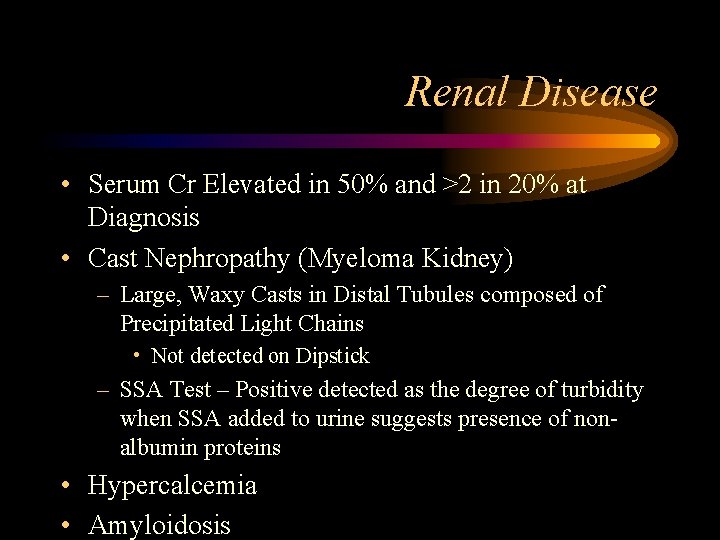
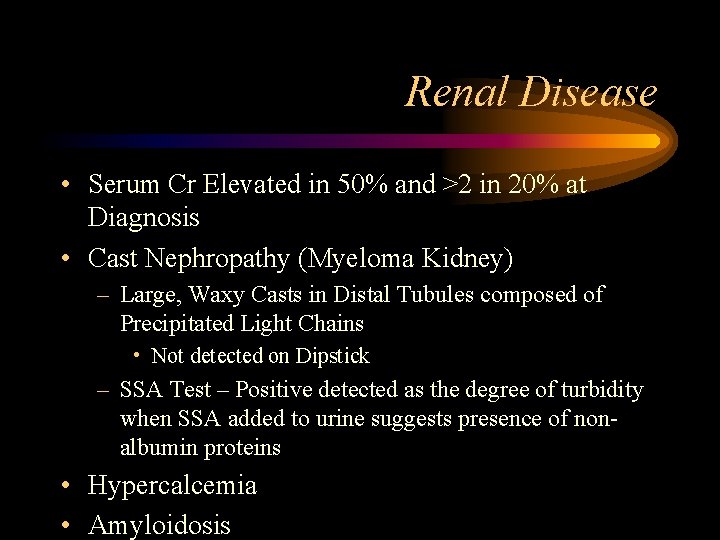
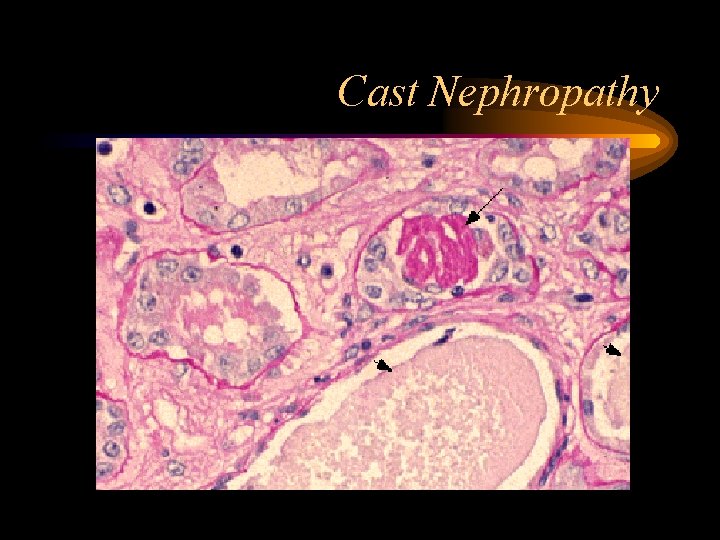
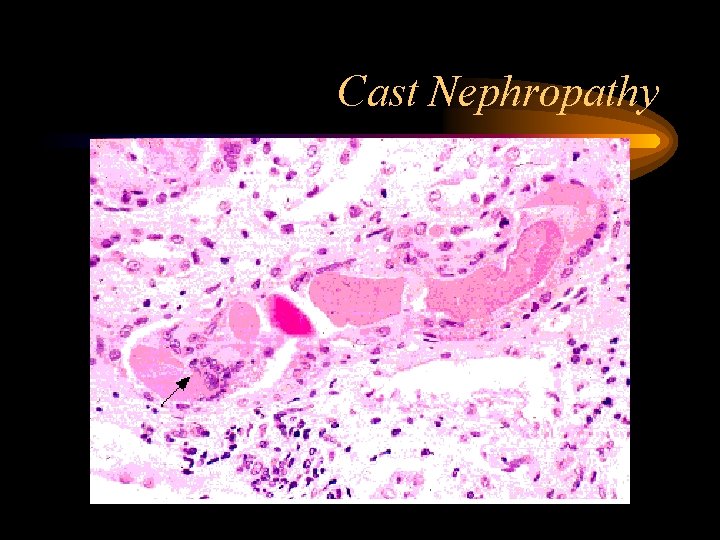
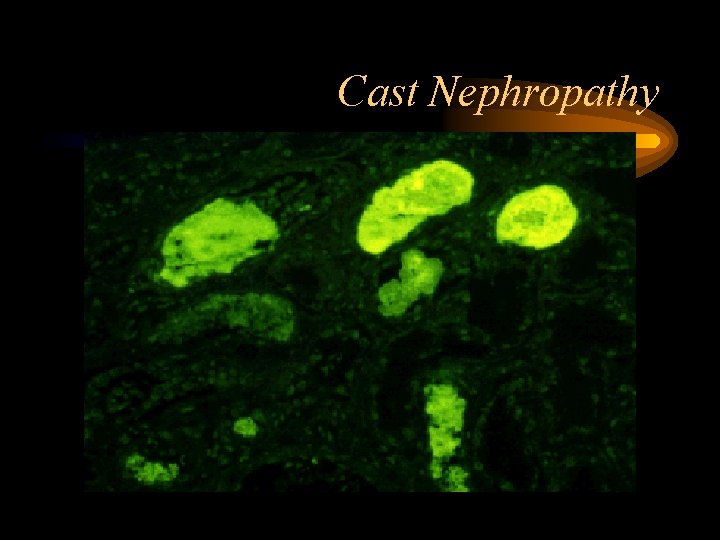
Renal Disease • Serum Cr Elevated in 50% and >2 in 20% at Diagnosis • Cast Nephropathy (Myeloma Kidney) – Large, Waxy Casts in Distal Tubules composed of Precipitated Light Chains • Not detected on Dipstick – SSA Test – Positive detected as the degree of turbidity when SSA added to urine suggests presence of nonalbumin proteins • Hypercalcemia • Amyloidosis
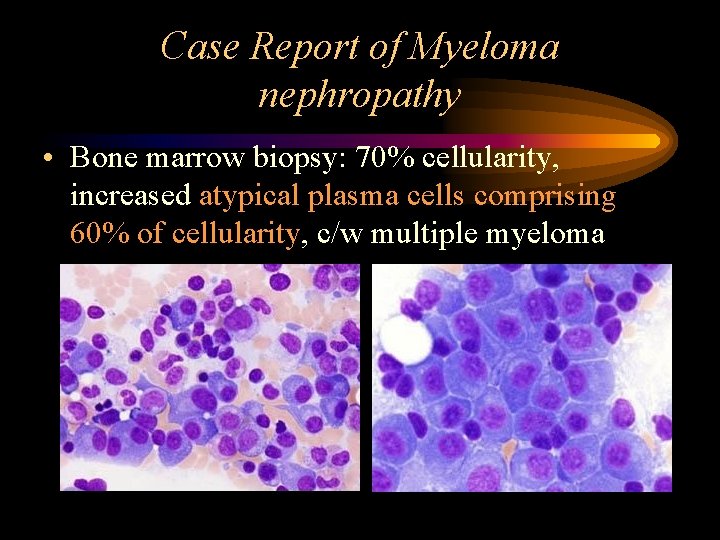
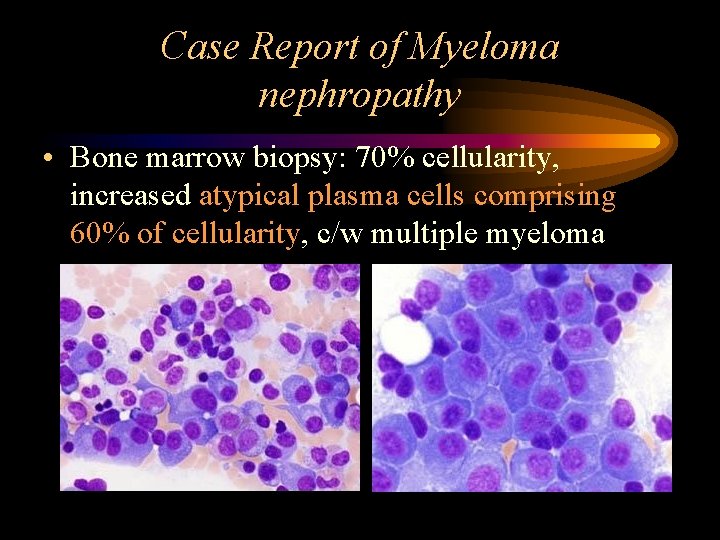
Case Report of Myeloma nephropathy • Bone marrow biopsy: 70% cellularity, increased atypical plasma cells comprising 60% of cellularity, c/w multiple myeloma
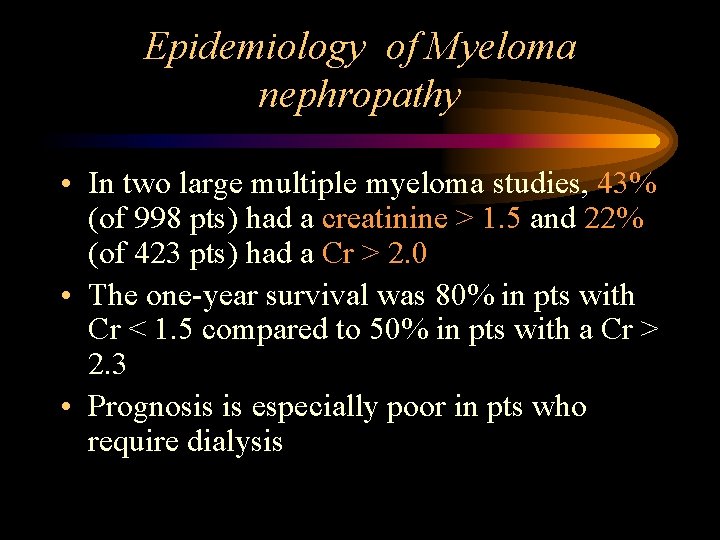
Epidemiology of Myeloma nephropathy • In two large multiple myeloma studies, 43% (of 998 pts) had a creatinine > 1. 5 and 22% (of 423 pts) had a Cr > 2. 0 • The one-year survival was 80% in pts with Cr < 1. 5 compared to 50% in pts with a Cr > 2. 3 • Prognosis is especially poor in pts who require dialysis
Causes of renal failure in MM • • Cast nephropathy Light chain deposition disease Primary amyloidosis Hypercalcemia Renal tubular dysfunction Volume depletion IV contrast dye, nephrotoxic meds
Myeloma Kidney • Two main pathogenetic mechanisms: – Intracellular cast formation – Direct tubular toxicity by light chains • Contributing factors to presence of renal failure due to multiple myeloma: – High rate of light chain excretion (tumor load) – Biochemical characteristics of light chain – Concurrent volume depletion
Cast Nephropathy • Most common pathological diagnosis on renal biopsy in multiple myeloma • Due to light chains binding with Tamm-Horsfall mucoprotein, which is secreted by tubular cells in ascending loop of Henle, forming casts • Multinucleated giant cells surround the casts • Dehydration worsens cast nephropathy due to decreased flow in tubules, increased concentration of light chains
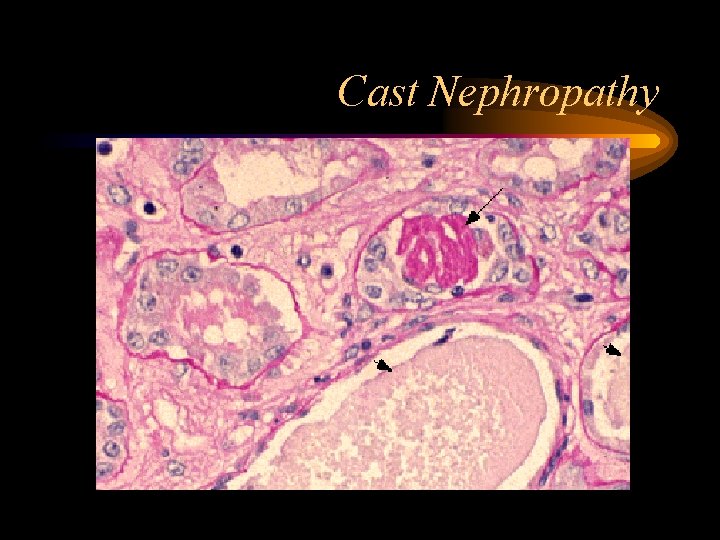
Cast Nephropathy
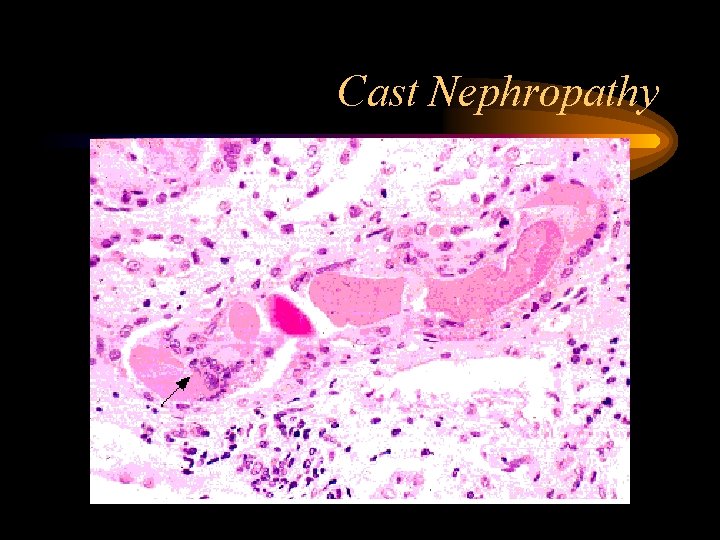
Cast Nephropathy
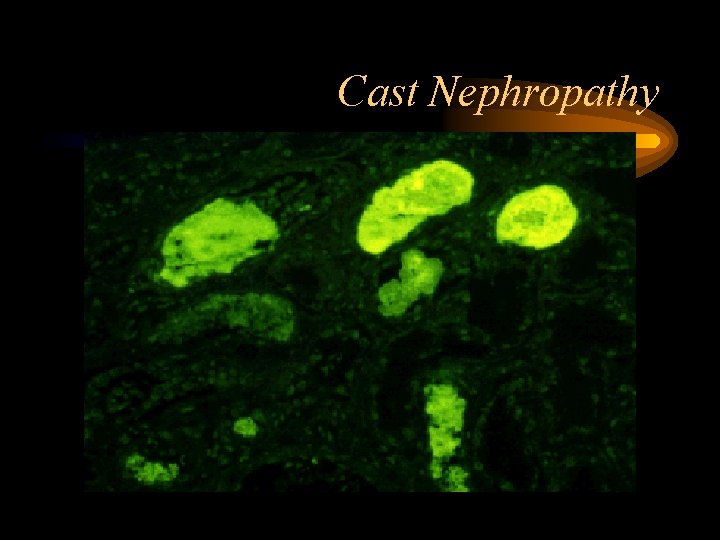
Cast Nephropathy

Minimal diagnostic criteria for myeloma • >10% Plasma cells in bone marrow or plasmacytoma on biopsy • Clinical features of myeloma • Plus at least one of: – – – Serum M band (Ig. G >30 g/l; Ig. A >20 g/l) Urine M band (Bence Jones proteinuria) Osteolytic lesions on skeletal survey

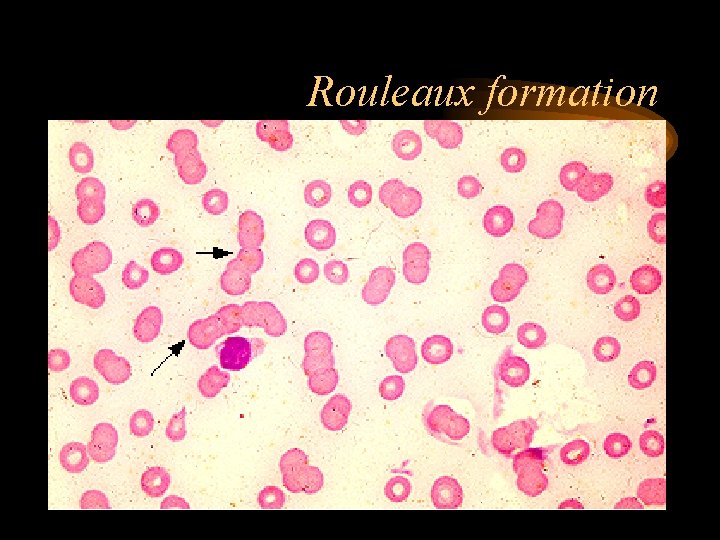
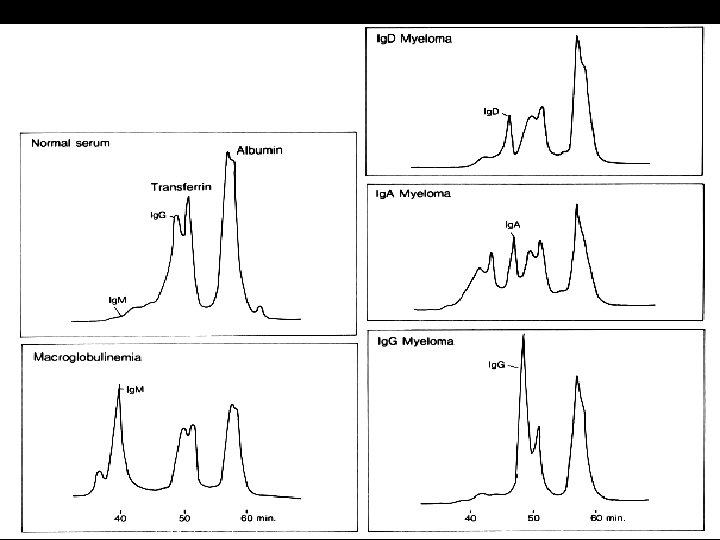
Initial Work-up • CBC w/diff – peripheral smear – Normocytic, Normochromic Anemia most common – Rouleaux Formation >50% of patients • Chemistry (ca, alb, cr, LD, CRP, B 2 M) • SPEP – Monoclonal Protein • Serum Viscosity (if M-protein conc. Is high, >5 g/d. L) or sx of hyperviscosity are present • UA and UPEP • Metastatic bone Survey • Bone Marrow Biopsy
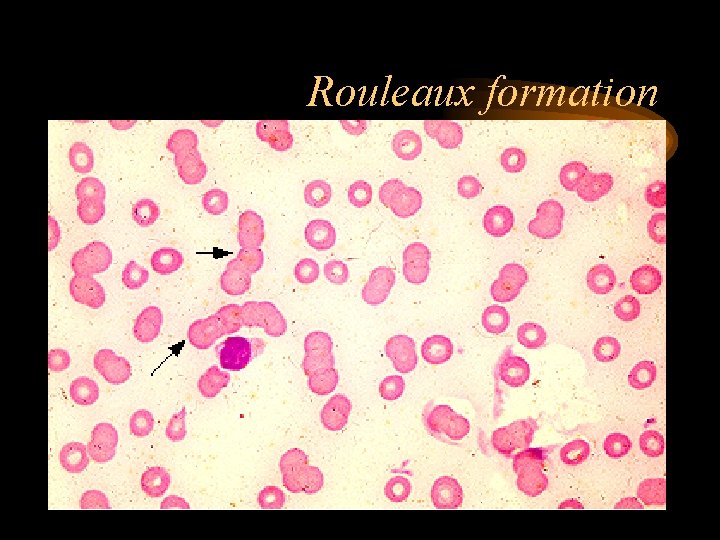
Rouleaux formation
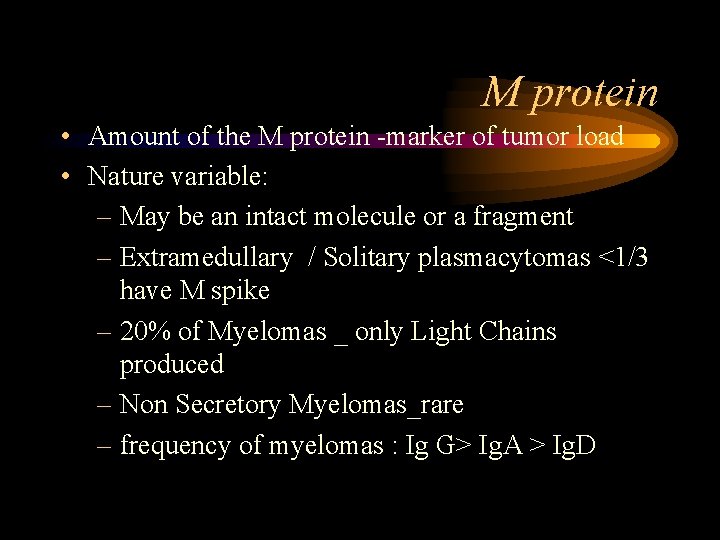
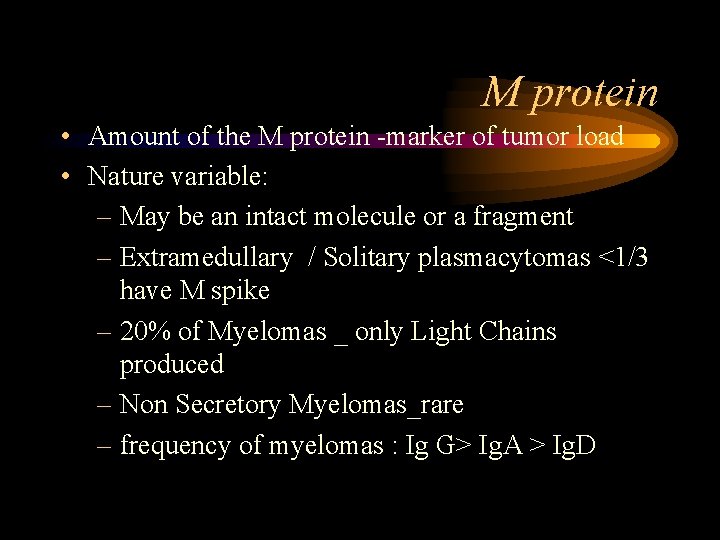
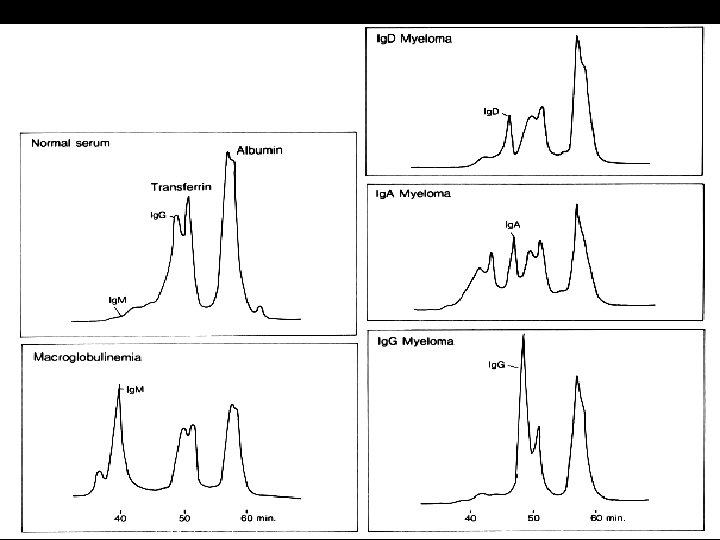
M protein • Amount of the M protein -marker of tumor load • Nature variable: – May be an intact molecule or a fragment – Extramedullary / Solitary plasmacytomas <1/3 have M spike – 20% of Myelomas _ only Light Chains produced – Non Secretory Myelomas_rare – frequency of myelomas : Ig G> Ig. A > Ig. D
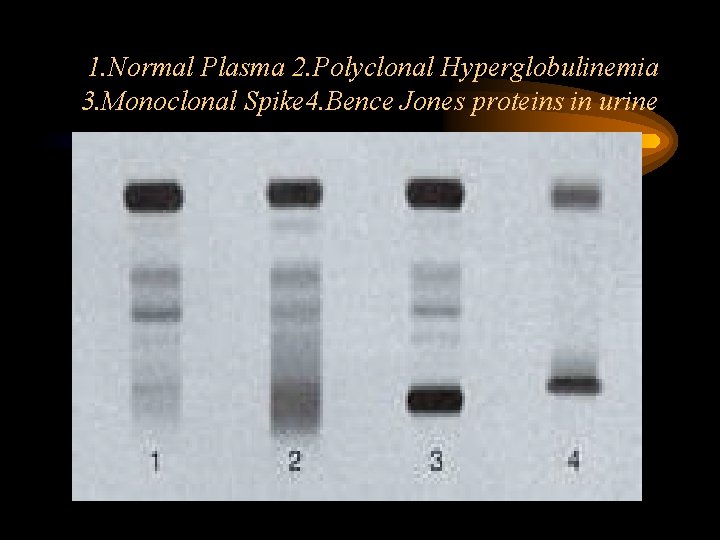
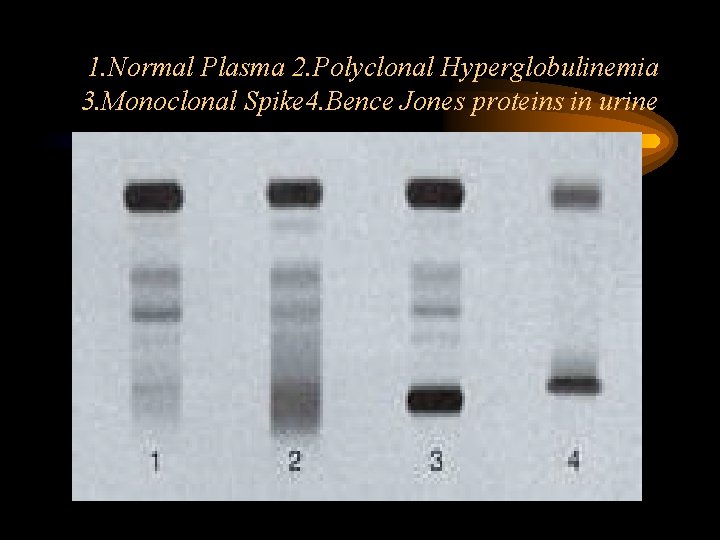
1. Normal Plasma 2. Polyclonal Hyperglobulinemia 3. Monoclonal Spike 4. Bence Jones proteins in urine
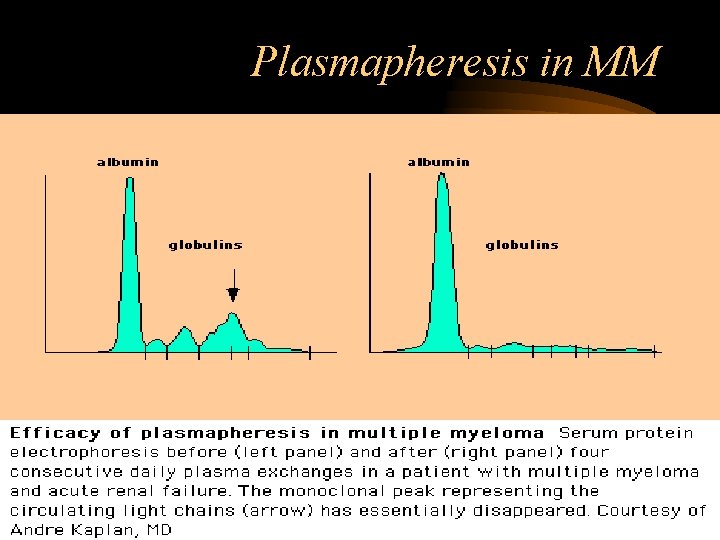
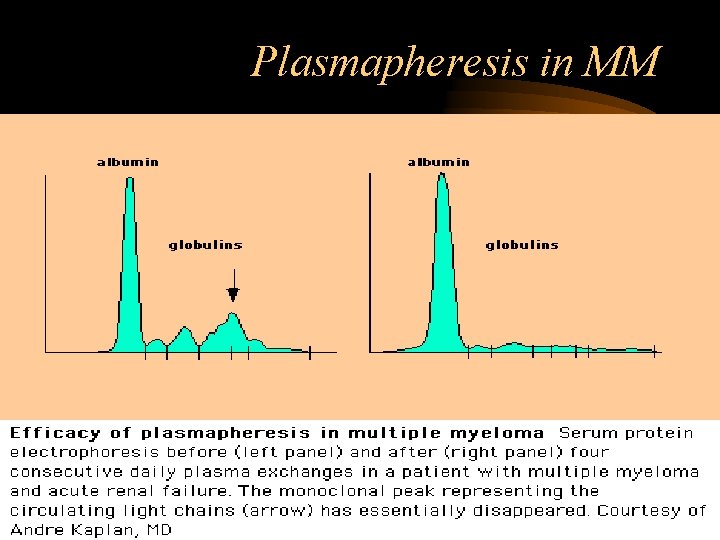
Plasmapheresis in MM
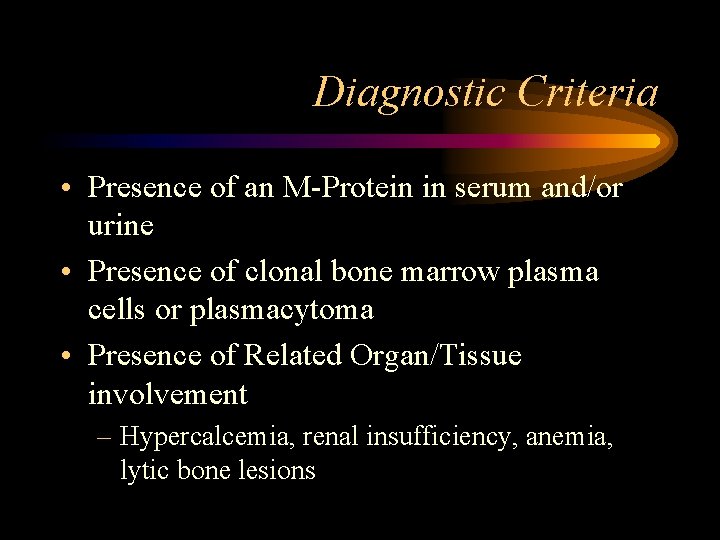
Diagnostic Criteria • Presence of an M-Protein in serum and/or urine • Presence of clonal bone marrow plasma cells or plasmacytoma • Presence of Related Organ/Tissue involvement – Hypercalcemia, renal insufficiency, anemia, lytic bone lesions
Screening and Diagnosis • • • Blood and urine tests X-rays Magnetic Resonance Imaging (MRI) Computerized Tomography (CT) Bone marrow examination
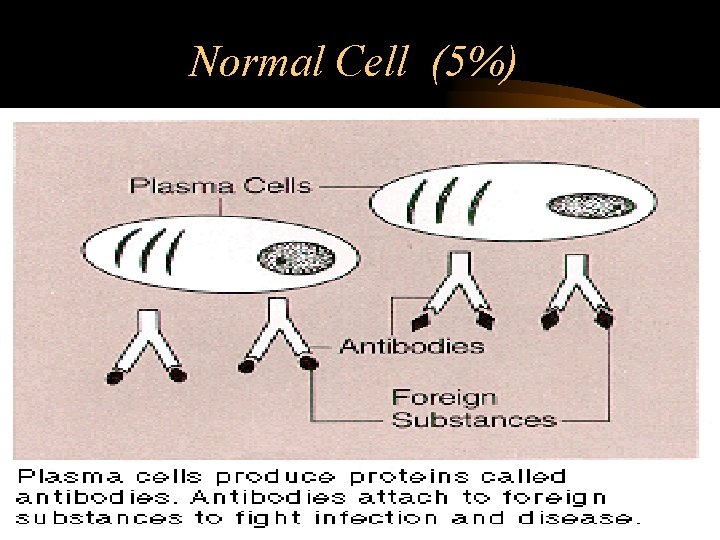
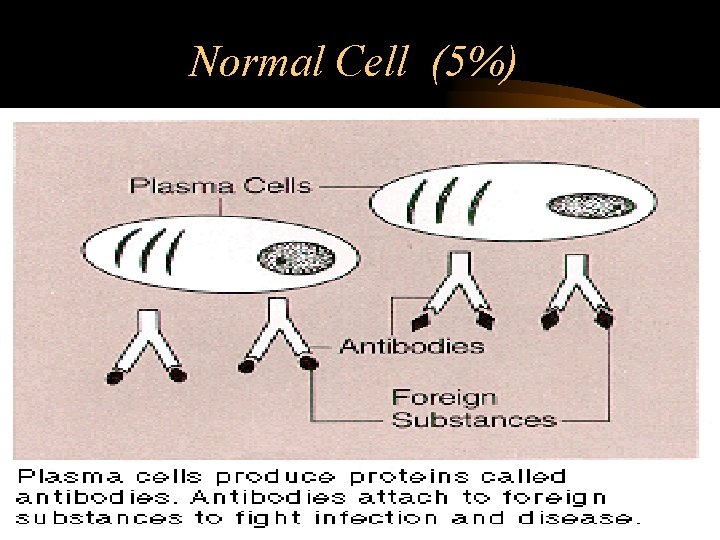
Normal Cell (5%)
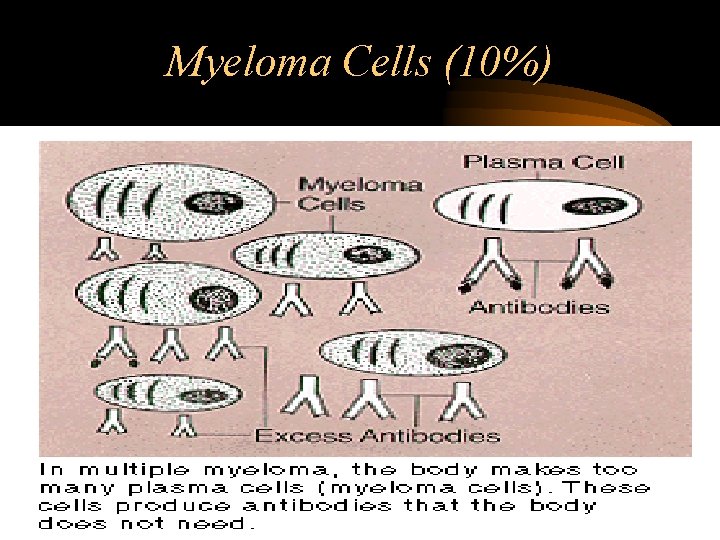
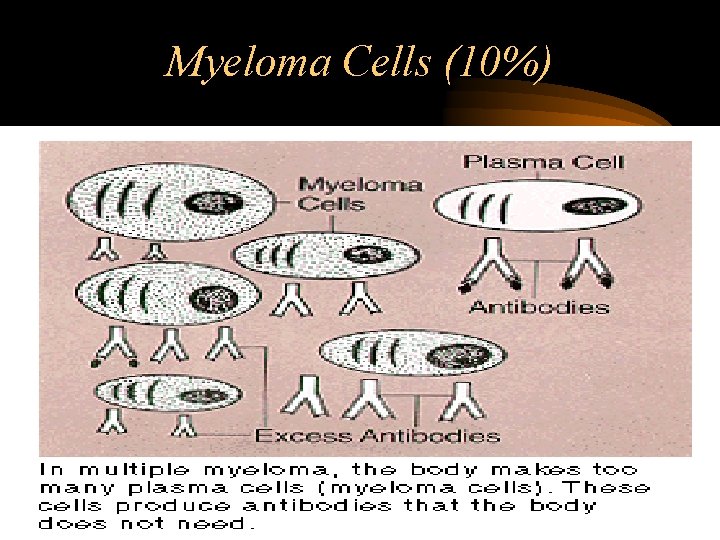
Myeloma Cells (10%)
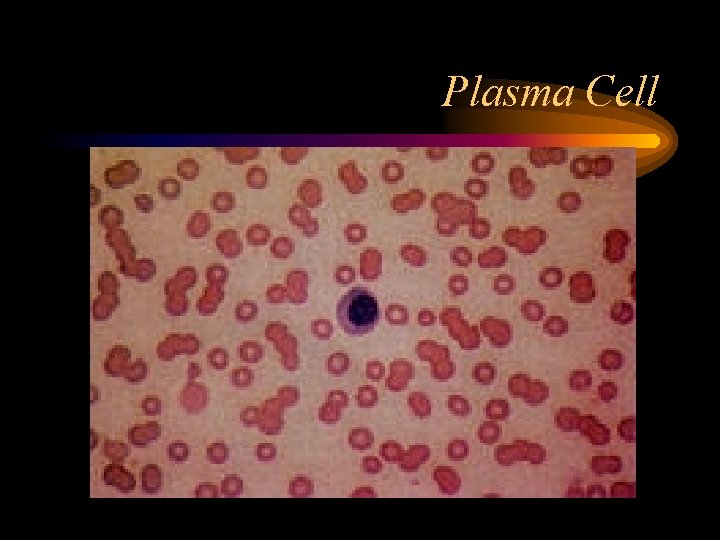
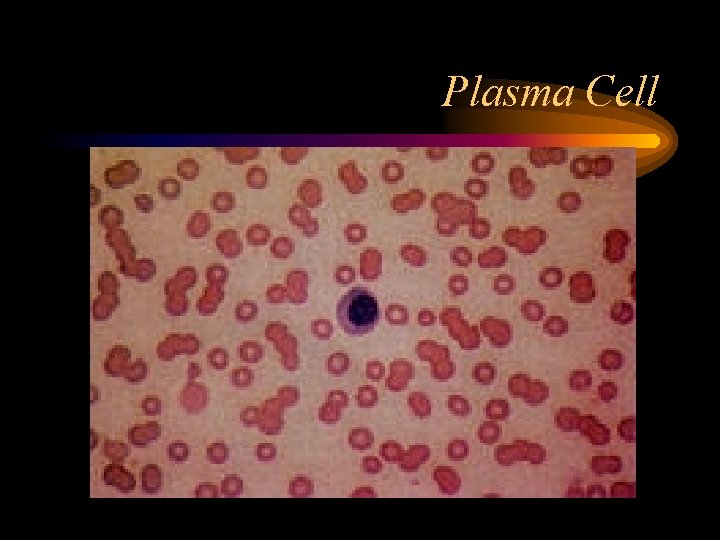
Plasma Cell

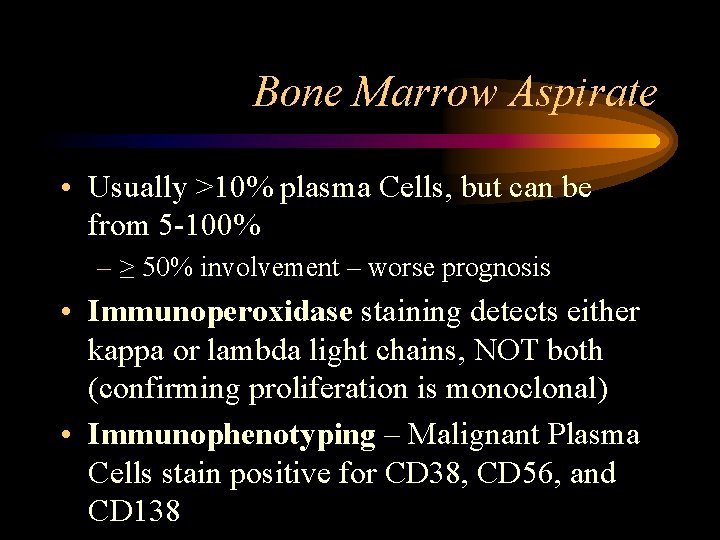
Bone Marrow Aspirate
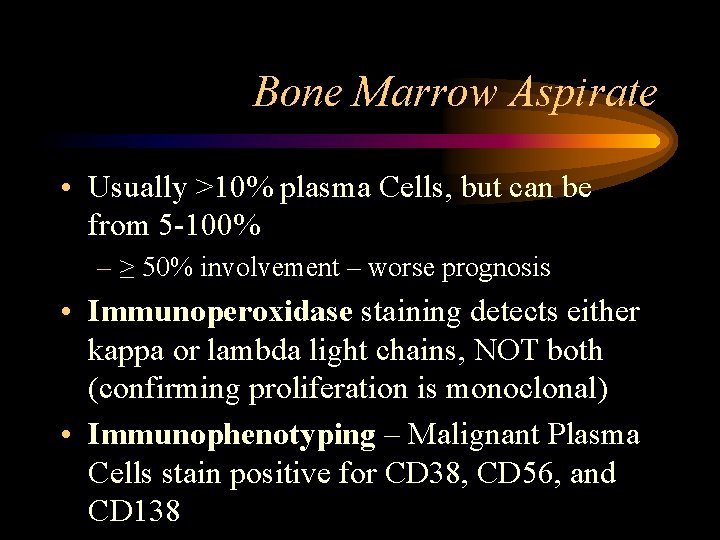
Bone Marrow Aspirate • Usually >10% plasma Cells, but can be from 5 -100% – ≥ 50% involvement – worse prognosis • Immunoperoxidase staining detects either kappa or lambda light chains, NOT both (confirming proliferation is monoclonal) • Immunophenotyping – Malignant Plasma Cells stain positive for CD 38, CD 56, and CD 138

Bone Marrow Biopsy

Staging • Stage 1 – Low amount of myeloma • Stage 2 – Medium amount of myeloma • Stage 3 – High amount of myeloma • A – Normal kidney function • B – Abnormal kidney function
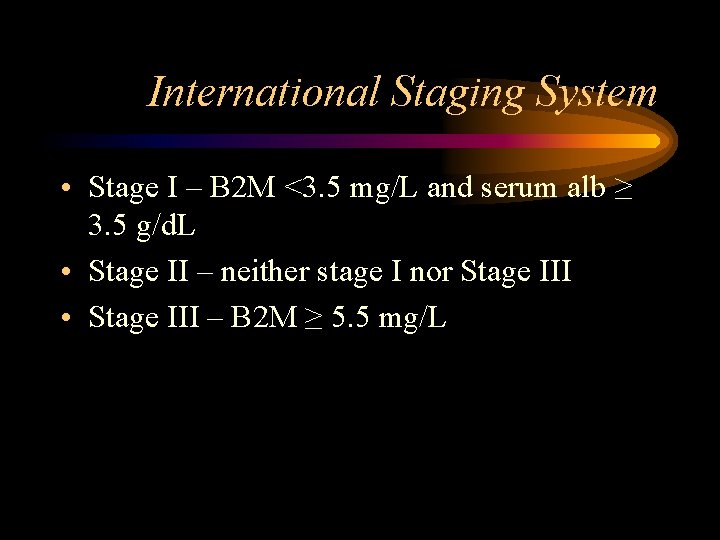
International Staging System • Stage I – B 2 M <3. 5 mg/L and serum alb ≥ 3. 5 g/d. L • Stage II – neither stage I nor Stage III • Stage III – B 2 M ≥ 5. 5 mg/L
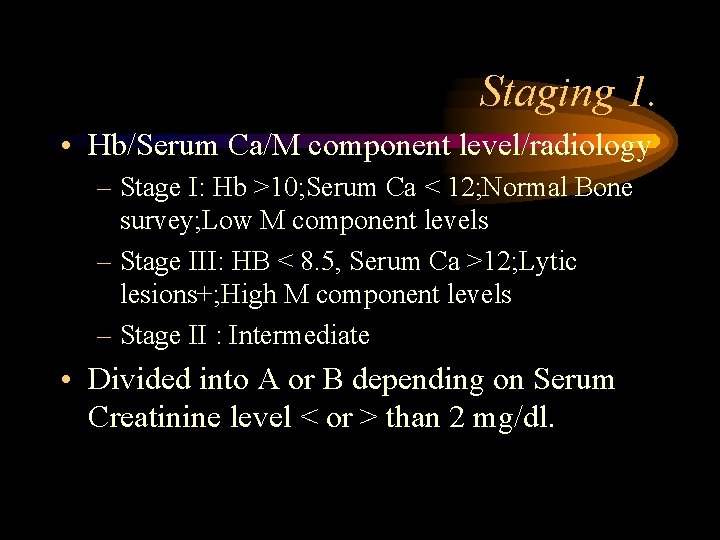
Staging 1. • Hb/Serum Ca/M component level/radiology – Stage I: Hb >10; Serum Ca < 12; Normal Bone survey; Low M component levels – Stage III: HB < 8. 5, Serum Ca >12; Lytic lesions+; High M component levels – Stage II : Intermediate • Divided into A or B depending on Serum Creatinine level < or > than 2 mg/dl.

Staging 2 • Serum b 2 microglobulin levels. • If < 0. 004 g/L : Stage 1; Median survival 43 months • If >0. 004 g/L: Stage II; Median survival 12 months
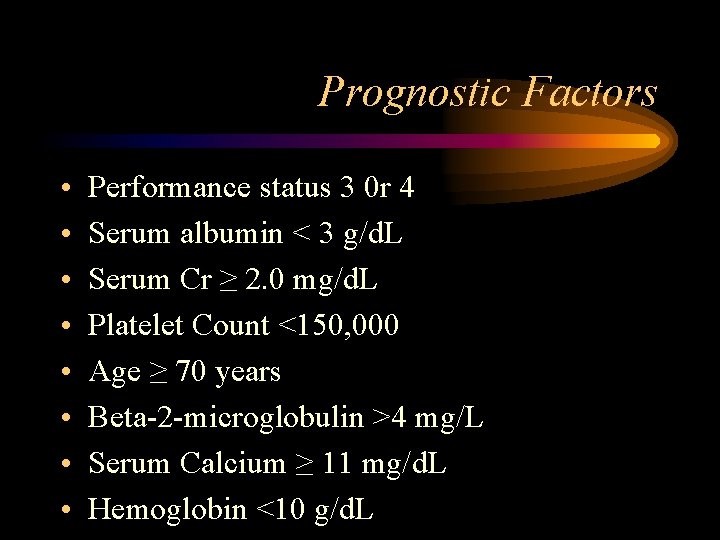
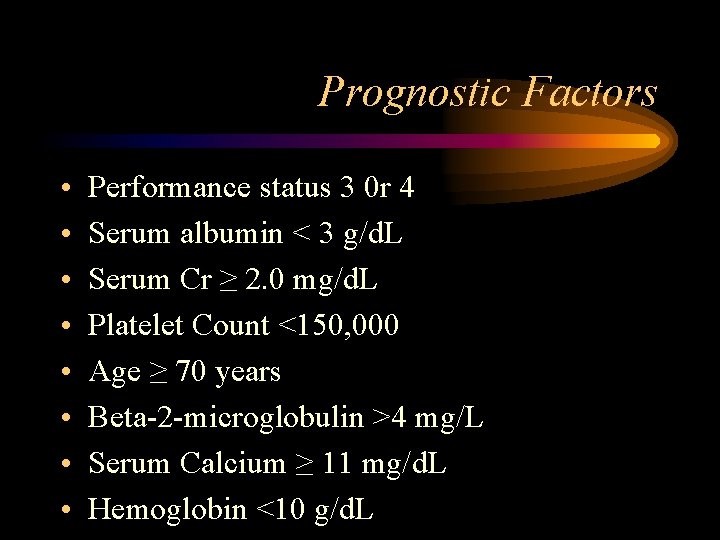
Prognostic Factors • • Performance status 3 0 r 4 Serum albumin < 3 g/d. L Serum Cr ≥ 2. 0 mg/d. L Platelet Count <150, 000 Age ≥ 70 years Beta-2 -microglobulin >4 mg/L Serum Calcium ≥ 11 mg/d. L Hemoglobin <10 g/d. L
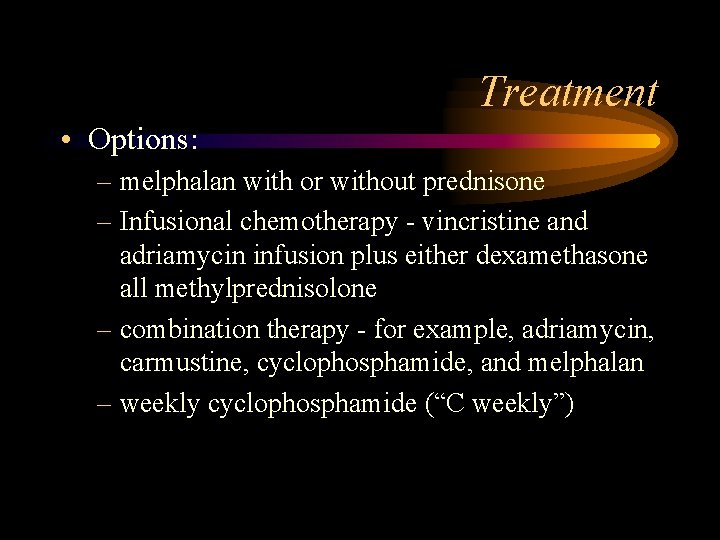
Treatment • Options: – melphalan with or without prednisone – Infusional chemotherapy - vincristine and adriamycin infusion plus either dexamethasone all methylprednisolone – combination therapy - for example, adriamycin, carmustine, cyclophosphamide, and melphalan – weekly cyclophosphamide (“C weekly”)
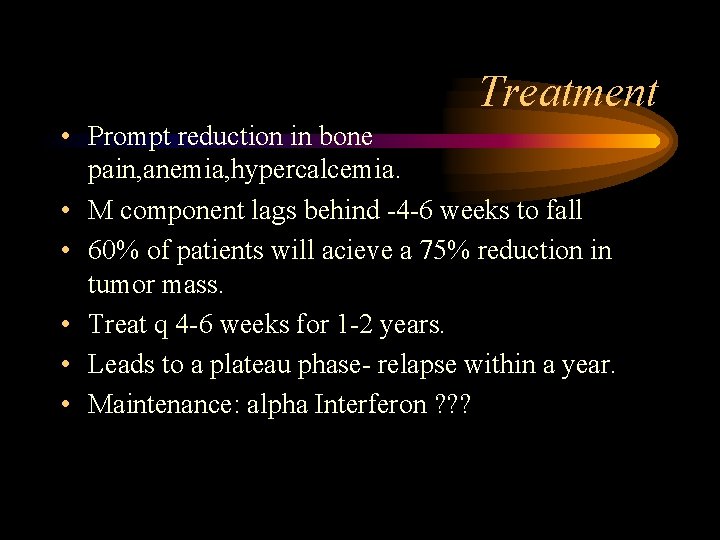
Treatment • Prompt reduction in bone pain, anemia, hypercalcemia. • M component lags behind -4 -6 weeks to fall • 60% of patients will acieve a 75% reduction in tumor mass. • Treat q 4 -6 weeks for 1 -2 years. • Leads to a plateau phase- relapse within a year. • Maintenance: alpha Interferon ? ? ?

Treatment • Supportive therapy – analgesia – rehydration – treatment and any hypercalcemia – treatment of any renal impairment – treatment of any infection – local radiotherapy if required – chemotherapy – prevention of further bone damage
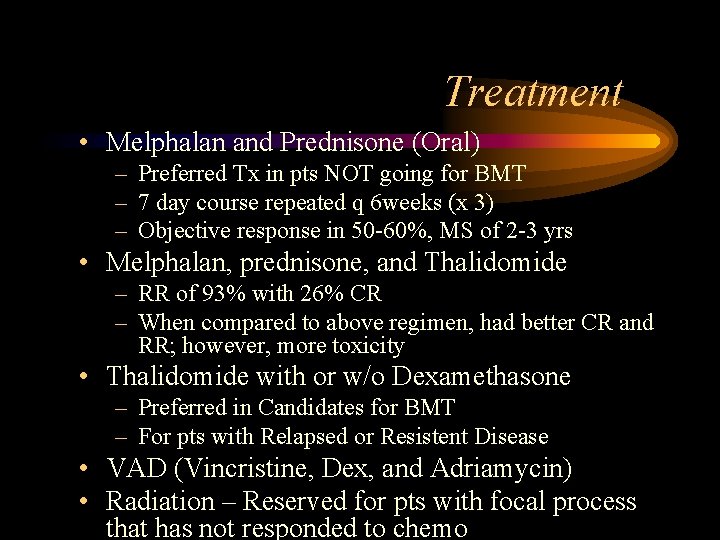
Treatment • Melphalan and Prednisone (Oral) – Preferred Tx in pts NOT going for BMT – 7 day course repeated q 6 weeks (x 3) – Objective response in 50 -60%, MS of 2 -3 yrs • Melphalan, prednisone, and Thalidomide – RR of 93% with 26% CR – When compared to above regimen, had better CR and RR; however, more toxicity • Thalidomide with or w/o Dexamethasone – Preferred in Candidates for BMT – For pts with Relapsed or Resistent Disease • VAD (Vincristine, Dex, and Adriamycin) • Radiation – Reserved for pts with focal process that has not responded to chemo

Treatment Outcomes • Cure – Not yet been Achieved • Molecular Complete Response – No evidence of Disease • Complete Response – No detectable M protein AND nml % of Plasma cells in Bone Marrow • Progressive Disease – >25% increase in M Protein, new bony lesions, or a new plasmacytoma
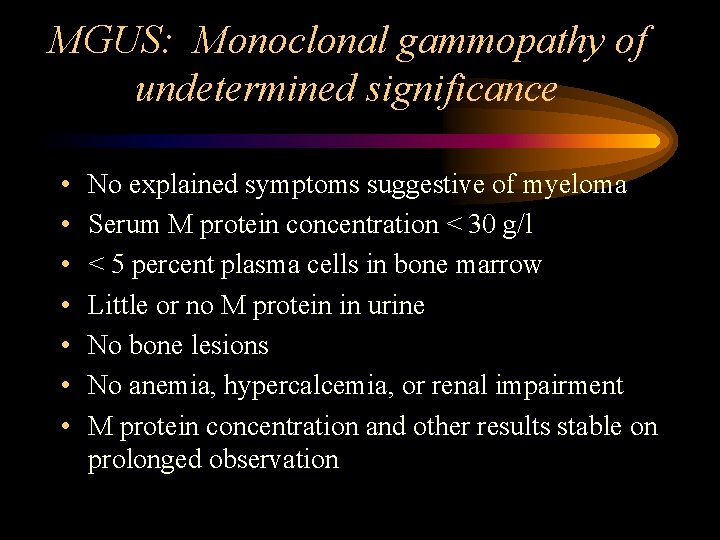
MGUS: Monoclonal gammopathy of undetermined significance • • No explained symptoms suggestive of myeloma Serum M protein concentration < 30 g/l < 5 percent plasma cells in bone marrow Little or no M protein in urine No bone lesions No anemia, hypercalcemia, or renal impairment M protein concentration and other results stable on prolonged observation
 Crab criteria multiple myeloma
Crab criteria multiple myeloma Crab criteria multiple myeloma
Crab criteria multiple myeloma Mielma
Mielma Waldenstrom's
Waldenstrom's Crab kriterleri
Crab kriterleri Waldenstrom macroglobulinemia vs multiple myeloma
Waldenstrom macroglobulinemia vs multiple myeloma Kpd myeloma
Kpd myeloma Mayo clinic multiple myeloma
Mayo clinic multiple myeloma Multiple myeloma cure
Multiple myeloma cure Neoplastic proliferation of white blood cells
Neoplastic proliferation of white blood cells Arahnoidalna cista
Arahnoidalna cista Intimal proliferation
Intimal proliferation Proliferation advertising
Proliferation advertising Proliferation of interest groups
Proliferation of interest groups Uncontrolled clonal proliferation
Uncontrolled clonal proliferation Industrial proliferation
Industrial proliferation Folliculocentric basaloid proliferation
Folliculocentric basaloid proliferation Prolyferation
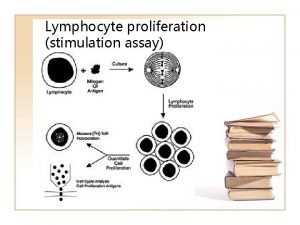
Prolyferation Lymphocyte proliferation
Lymphocyte proliferation Benign vs malignant
Benign vs malignant Malignant neuroleptic syndrome
Malignant neuroleptic syndrome Carotonemia
Carotonemia Malignant hypertension management
Malignant hypertension management Malignant and benign tumors
Malignant and benign tumors Kitwood's psychological needs
Kitwood's psychological needs Neuroleptic malignant syndrome
Neuroleptic malignant syndrome Hypokalemia
Hypokalemia Background
Background Malignant neoplasm of the blood-forming organs
Malignant neoplasm of the blood-forming organs Malignant mesothelioma
Malignant mesothelioma Perdida de polaridad celular
Perdida de polaridad celular Benign and malignant tumors
Benign and malignant tumors Malignant neoplasm
Malignant neoplasm Benign and malignant tumor difference
Benign and malignant tumor difference Catatonic behavior example
Catatonic behavior example Hypertensive urgency vs emergency
Hypertensive urgency vs emergency Histological features of malignant cells
Histological features of malignant cells Hematocrit
Hematocrit Hypertensive emergency vs urgency
Hypertensive emergency vs urgency Uk myeloma forum
Uk myeloma forum European myeloma network
European myeloma network Daratumumab macmillan
Daratumumab macmillan Myeloma
Myeloma Myeloma euronet
Myeloma euronet Multiple baseline vs multiple probe design
Multiple baseline vs multiple probe design Shared memory mimd architecture
Shared memory mimd architecture Suburban sprawl definition ap human geography
Suburban sprawl definition ap human geography