HOSPITAL INFECTIONS HCAI Meral SNMEZOLU MD Yeditepe University















- Slides: 96
HOSPITAL INFECTIONS (HCAI) Meral SÖNMEZOĞLU, MD Yeditepe University Hospital Associate Professor of Department of Infectious Diseases and Clinical Microbiology
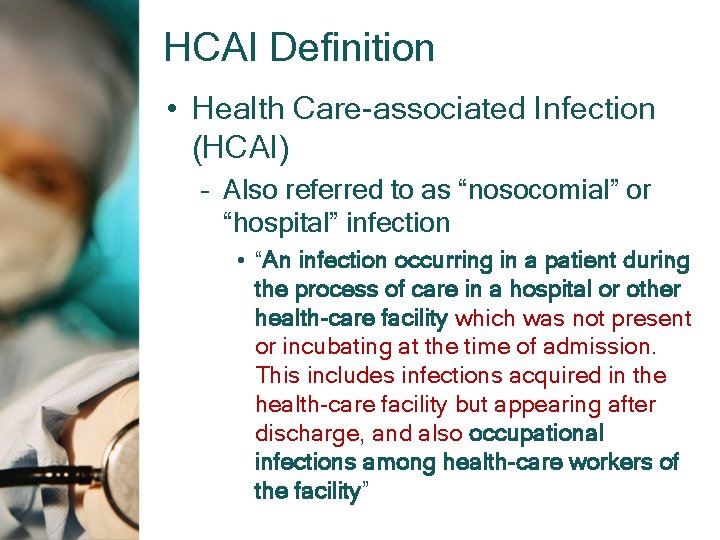
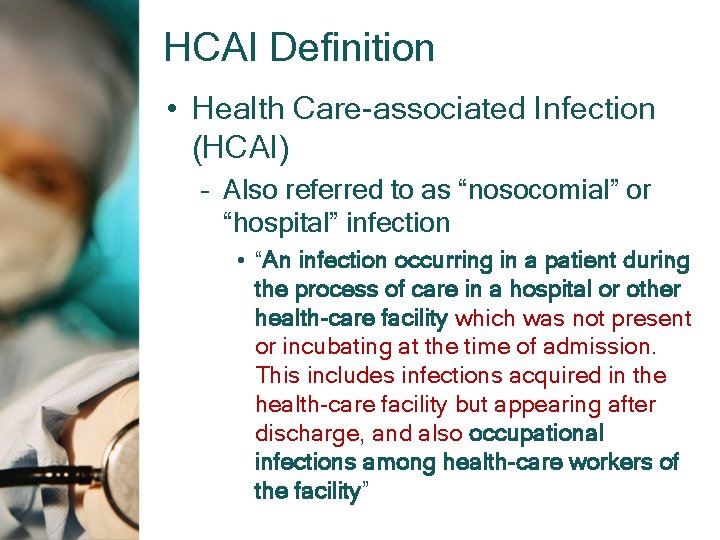
HCAI Definition • Health Care-associated Infection (HCAI) – Also referred to as “nosocomial” or “hospital” infection • “An infection occurring in a patient during the process of care in a hospital or other health-care facility which was not present or incubating at the time of admission. This includes infections acquired in the health-care facility but appearing after discharge, and also occupational infections among health-care workers of the facility”

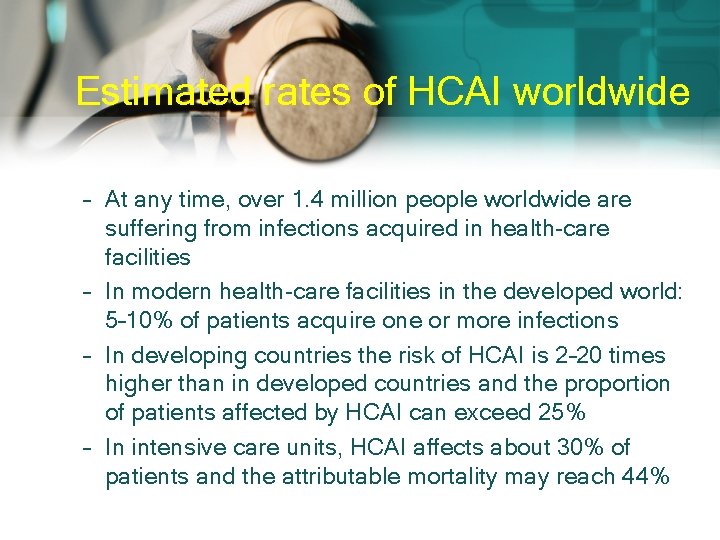
HCAI • The World Health Organization has reported that, at any given time, approximately 1. 4 million people have an HAI; • in developing countries, the risk can be up to 20 times greater than in developed countries. • In addition, the emergence of HAIs caused by multidrug-resistant microorganisms is an increasing concern.

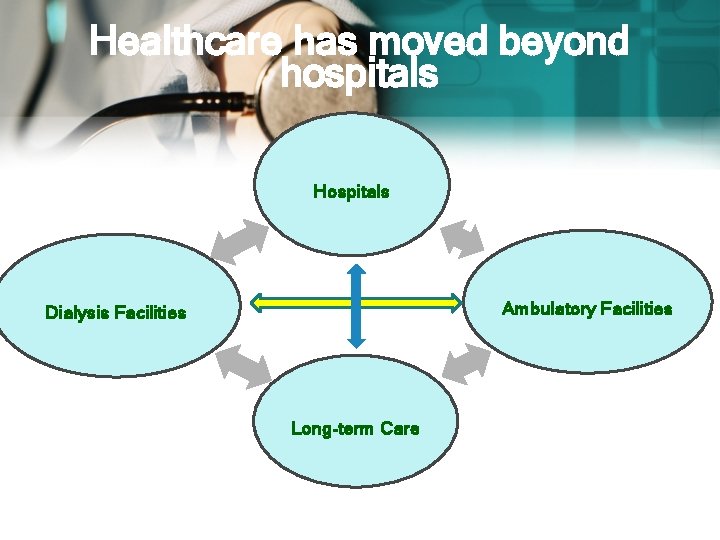
Healthcare-Associated Infections (HAIs) q q 1 out of 20 hospitalized patients affected Associated with increased mortality Attributed costs: $26 -33 billion annually HAIs occur in all types of facilities, including: • • Long-term care facilities Dialysis facilities Ambulatory surgical centers Hospitals
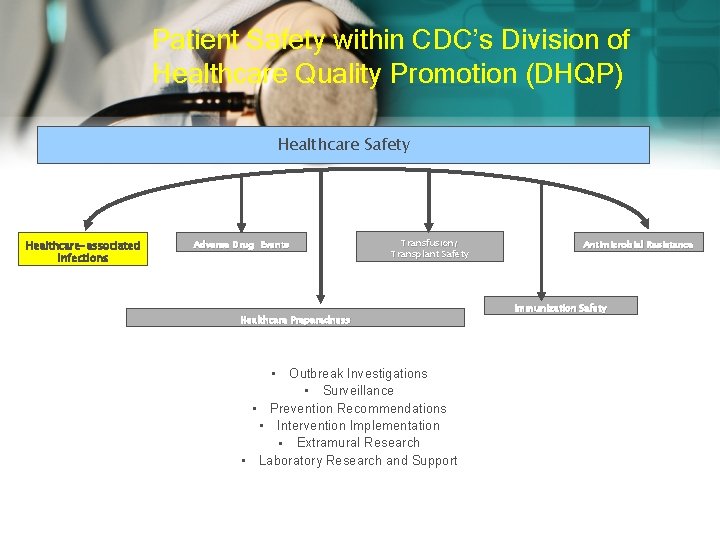
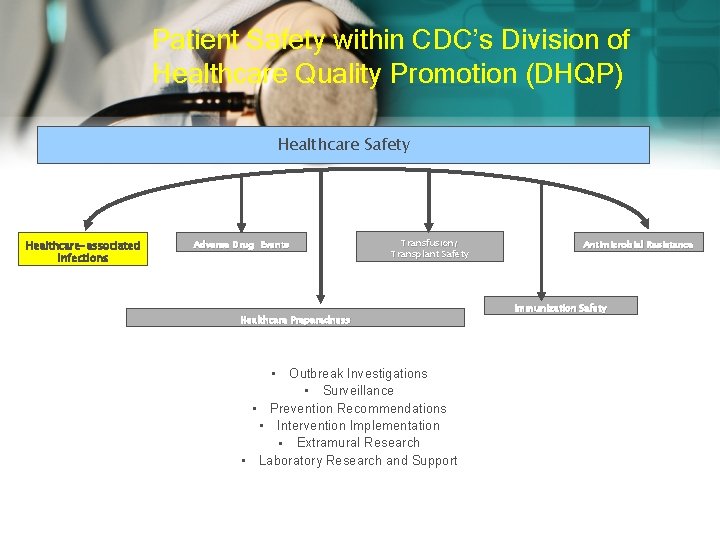
Patient Safety within CDC’s Division of Healthcare Quality Promotion (DHQP) Healthcare Safety Healthcare-associated Infections Adverse Drug Events Transfusion/ Transplant Safety Healthcare Preparedness Outbreak Investigations § Surveillance § Prevention Recommendations § Intervention Implementation § Extramural Research § Laboratory Research and Support § Antimicrobial Resistance Immunization Safety
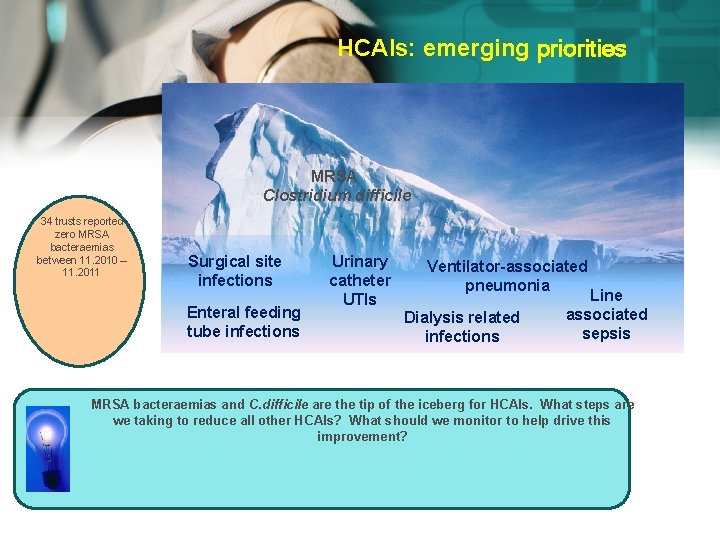
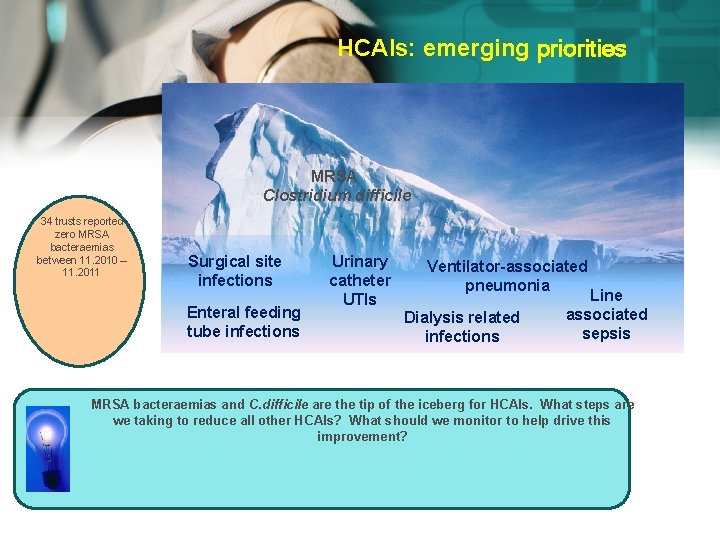
HCAIs: emerging priorities MRSA Clostridium difficile 34 trusts reported zero MRSA bacteraemias between 11. 2010 – 11. 2011 Surgical site infections Enteral feeding tube infections Urinary catheter UTIs Ventilator-associated pneumonia Dialysis related infections Line associated sepsis MRSA bacteraemias and C. difficile are the tip of the iceberg for HCAIs. What steps are we taking to reduce all other HCAIs? What should we monitor to help drive this improvement?
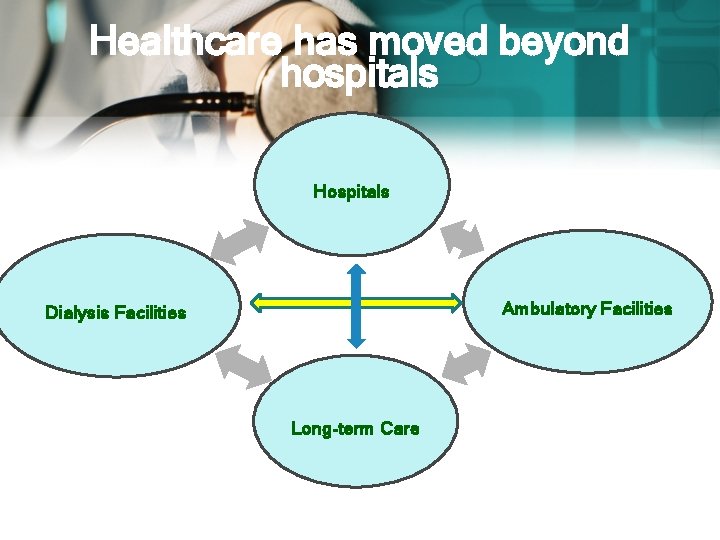
Healthcare has moved beyond hospitals Hospitals Ambulatory Facilities Dialysis Facilities Long-term Care
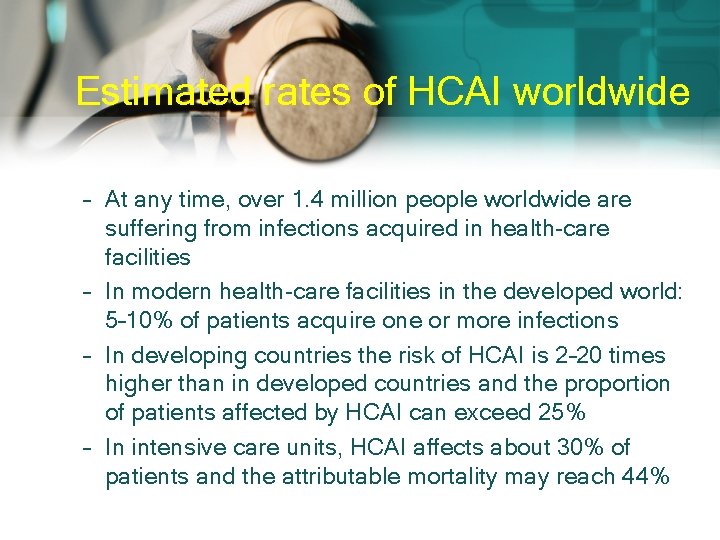
Estimated rates of HCAI worldwide – At any time, over 1. 4 million people worldwide are suffering from infections acquired in health-care facilities – In modern health-care facilities in the developed world: 5– 10% of patients acquire one or more infections – In developing countries the risk of HCAI is 2– 20 times higher than in developed countries and the proportion of patients affected by HCAI can exceed 25% – In intensive care units, HCAI affects about 30% of patients and the attributable mortality may reach 44%
The impact of HCAI • HCAI can cause: – – – more serious illness prolongation of stay in a health-care facility long-term disability excess deaths high additional financial burden high personal costs on patients and their families
Outbreaks vs. Endemic Problems Endemic problems represent the majority of HAIs q q Device-associated infections • • Catheter-associated urinary tract infections (CAUTI) • Ventilator-associated Pneumonia (VAP) Procedure-associated infections • q Central line-associated Blood stream infections (CLABSI) Surgical site infections (SSI) Adherence problems • Antimicrobial stewardship, hand hygiene

Most frequent sites of infection and their risk factors URINARY TRACT INFECTIONS Urinary catheter Urinary invasive procedures 34% 13% Advanced age Severe underlying disease Urolitiasis Pregnancy Diabetes SURGICAL SITE INFECTIONS Inadequate antibiotic prophylaxis Incorrect surgical skin preparation Inappropriate wound care Most common sites of health. OF care. LACK associated infection HAND and the risk factors underlying the HYGIENE occurrence of infections Surgical intervention duration Type of wound Poor surgical asepsis Diabetes Nutritional state Immunodeficiency Lack of training and supervision LOWER RESPIRATORY TRACT INFECTIONS Mechanical ventilation Aspiration Nasogastric tube Central nervous system depressants Antibiotics and anti-acids Prolonged health-care facilities stay Malnutrition Advanced age Surgery Immunodeficiency BLOOD INFECTIONS Vascular catheter Neonatal age Critical care Severe underlying disease Neutropenia Immunodeficiency New invasive technologies Lack of training and supervision 17% 14%
Patients Most Likely to Develop Nosocomial Infections 1. 2. 3. 4. 5. 6. Elderly patients. Women in labor and delivery. Premature infants and newborns. Surgical and burn patients. Diabetic and cancer patients. Patients receiving treatment with steroids, anticancer drugs, antilymphocyte serum, and radiation.
Patients Most Likely to Develop Nosocomial Infections (Cont’d) 7. 8. Immunosupressed patients (I. e. , patients whose immune systems are not functioning properly) Patients who are paralyzed or are undergoing renal dialysis or catheterization; quite often, these patient’s normal defence mechanisms are not functioning properly) Nabeel Al-Mawajdeh RN. MCS
Major Factors Contributing to Nosocomial Infections 1. 2. 3. 4. 5. An ever- increasing number of drug-resistant pathogens. Lack of awareness of routine infection control measures. Neglect of aseptic techniques and safety precautions. Lengthy complicated surgeries. Overcrowding of hospitals. Nabeel Al-Mawajdeh RN. MCS

Major Factors Contributing to Nosocomial Infections (Cont’d) 6. 7. 8. Shortage of hospital staff. An increased number of Immunosupressed patients. The overuse and improper use of indwelling medical devices. Nabeel Al-Mawajdeh RN. MCS
SURGICAL SITE INFECTIONS
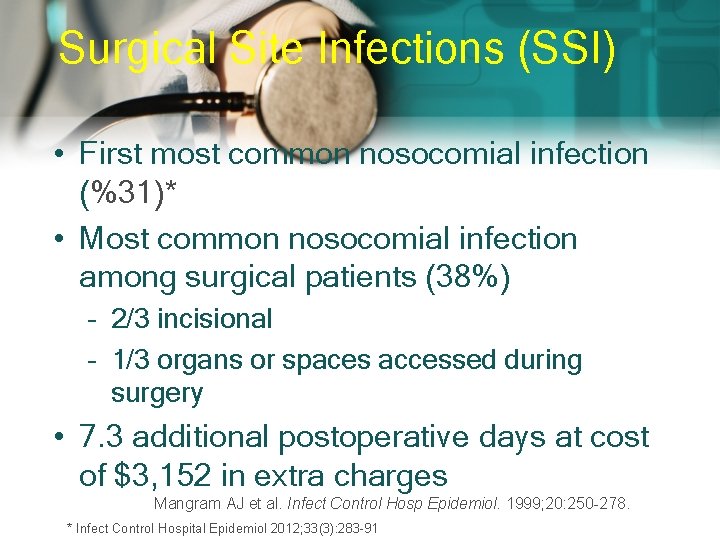
Surgical Site Infections (SSI) • First most common nosocomial infection (%31)* • Most common nosocomial infection among surgical patients (38%) – 2/3 incisional – 1/3 organs or spaces accessed during surgery • 7. 3 additional postoperative days at cost of $3, 152 in extra charges Mangram AJ et al. Infect Control Hosp Epidemiol. 1999; 20: 250 -278. * Infect Control Hospital Epidemiol 2012; 33(3): 283 -91
Colonization vs Contamination – Definitions • Colonization – Bacteria present in a wound with no signs or symptoms of systemic inflammation – Usually less than 105 cfu/m. L • Contamination – – Transient exposure of a wound to bacteria Varying concentrations of bacteria possible Time of exposure suggested to be < 6 hours SSI prophylaxis best strategy
SSI – Definitions • Infection – – – Systemic and local signs of inflammation Bacterial counts ≥ 105 cfu/m. L Purulent versus nonpurulent LOS effect Economic effect • Surgical wound infection is SSI LOS=length of stay.
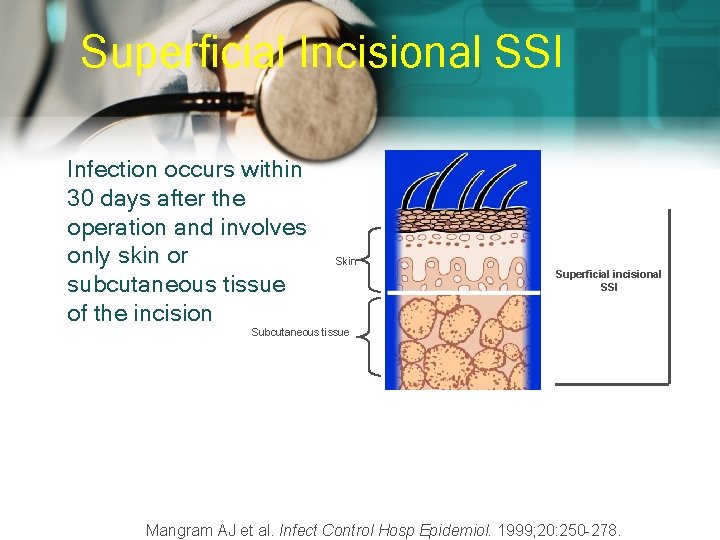
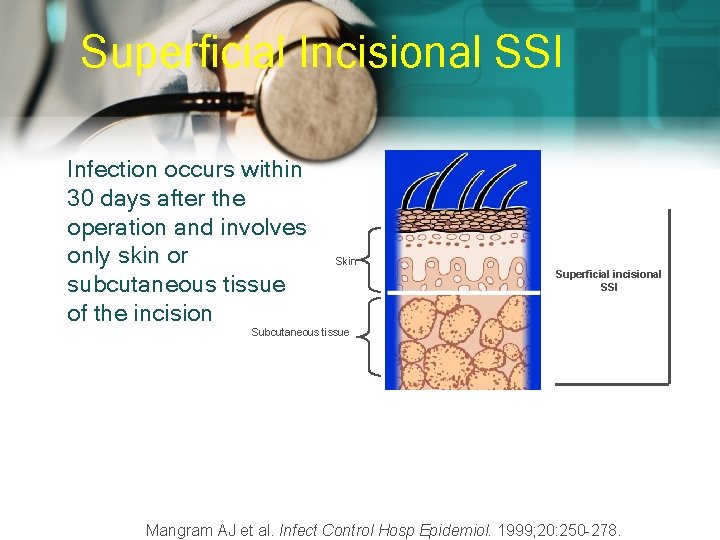
Superficial Incisional SSI Infection occurs within 30 days after the operation and involves only skin or subcutaneous tissue of the incision Skin Superficial incisional SSI Subcutaneous tissue Mangram AJ et al. Infect Control Hosp Epidemiol. 1999; 20: 250 -278.
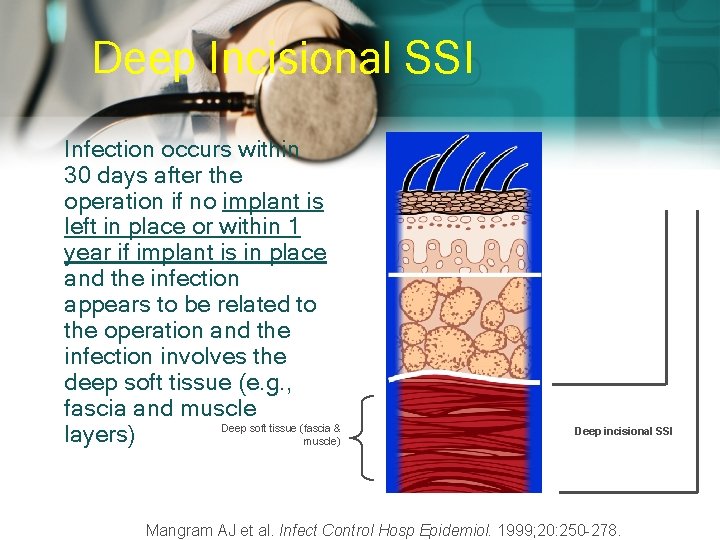
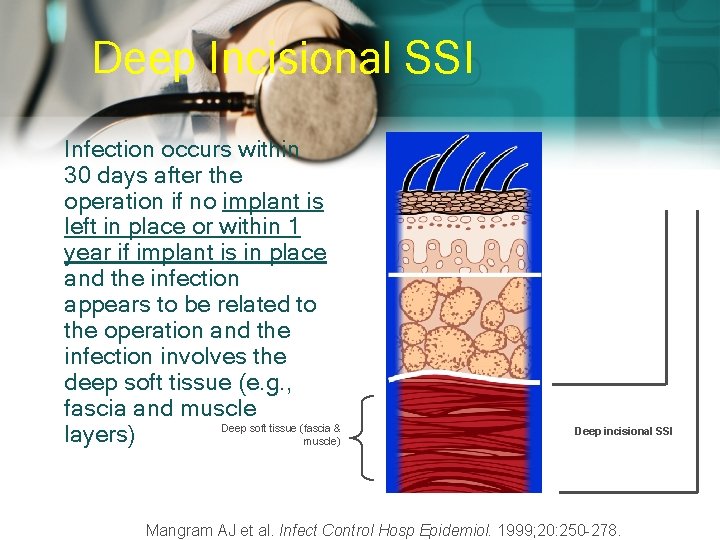
Deep Incisional SSI Infection occurs within 30 days after the operation if no implant is left in place or within 1 year if implant is in place and the infection appears to be related to the operation and the infection involves the deep soft tissue (e. g. , fascia and muscle Deep soft tissue (fascia & layers) muscle) Superficial incisional SSI Deep incisional SSI Mangram AJ et al. Infect Control Hosp Epidemiol. 1999; 20: 250 -278.
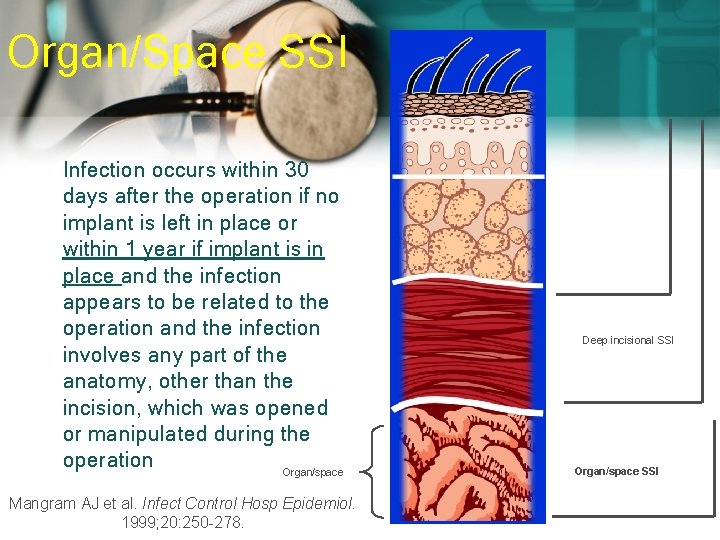
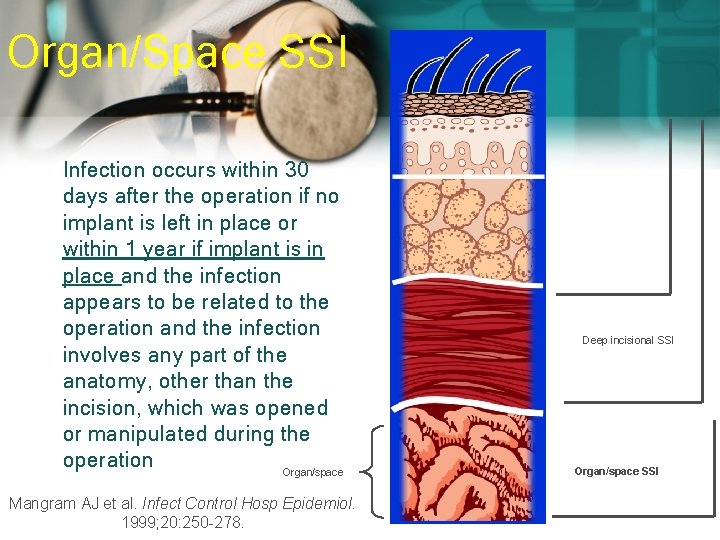
Organ/Space SSI Infection occurs within 30 days after the operation if no implant is left in place or within 1 year if implant is in place and the infection appears to be related to the operation and the infection involves any part of the anatomy, other than the incision, which was opened or manipulated during the operation Organ/space Mangram AJ et al. Infect Control Hosp Epidemiol. 1999; 20: 250 -278. Superficial incisional SSI Deep incisional SSI Organ/space SSI
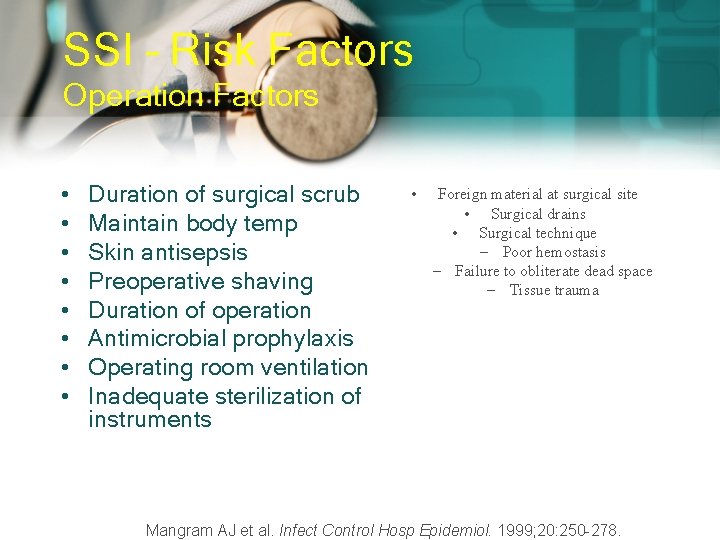
SSI – Risk Factors Operation Factors • • Duration of surgical scrub Maintain body temp Skin antisepsis Preoperative shaving Duration of operation Antimicrobial prophylaxis Operating room ventilation Inadequate sterilization of instruments • Foreign material at surgical site • Surgical drains • Surgical technique – Poor hemostasis – Failure to obliterate dead space – Tissue trauma Mangram AJ et al. Infect Control Hosp Epidemiol. 1999; 20: 250 -278.
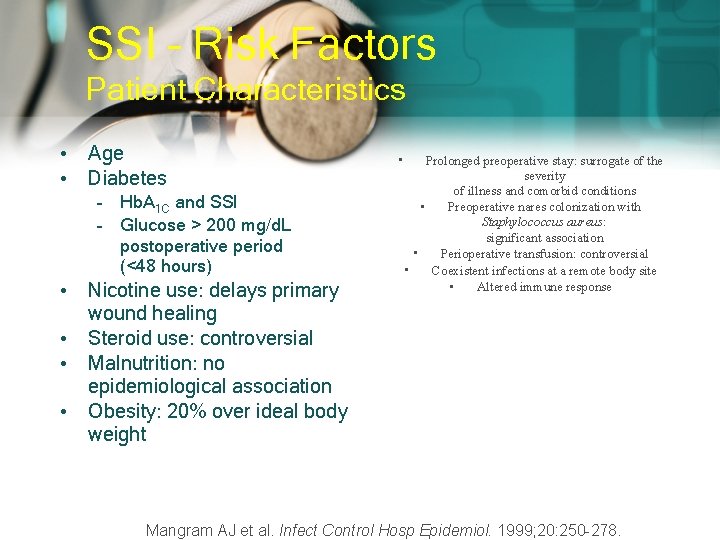
SSI – Risk Factors Patient Characteristics • Age • Diabetes – Hb. A 1 C and SSI – Glucose > 200 mg/d. L postoperative period (<48 hours) • Nicotine use: delays primary wound healing • Steroid use: controversial • Malnutrition: no epidemiological association • Obesity: 20% over ideal body weight • Prolonged preoperative stay: surrogate of the severity of illness and comorbid conditions Preoperative nares colonization with • Staphylococcus aureus: significant association Perioperative transfusion: controversial • Coexistent infections at a remote body site • Altered immune response • Mangram AJ et al. Infect Control Hosp Epidemiol. 1999; 20: 250 -278.
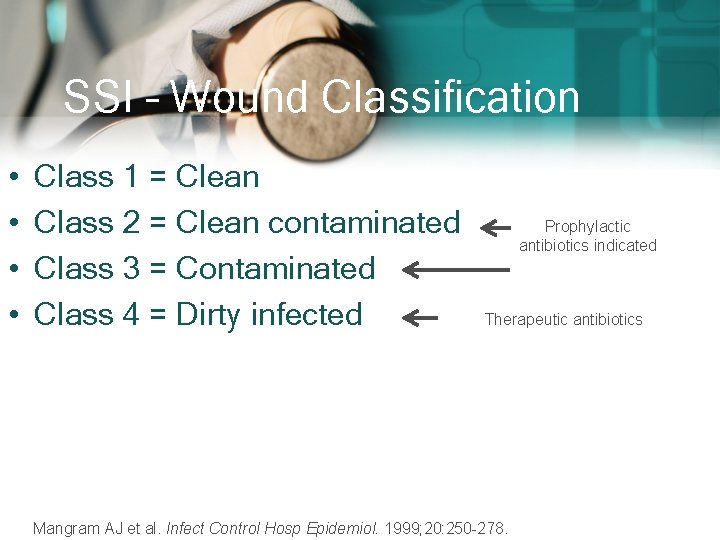
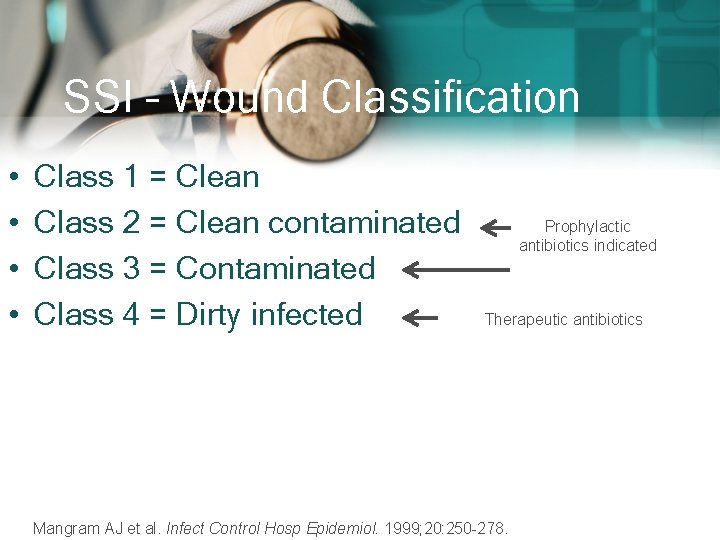
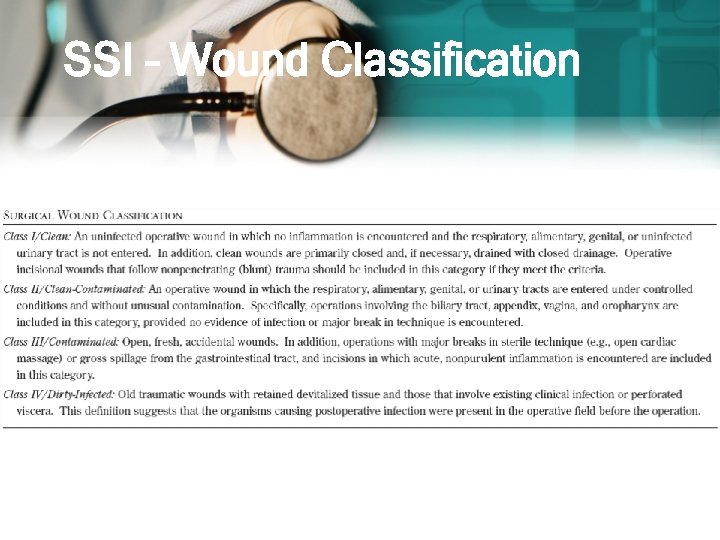
SSI – Wound Classification • • Class 1 = Clean Class 2 = Clean contaminated Class 3 = Contaminated Class 4 = Dirty infected Prophylactic antibiotics indicated Therapeutic antibiotics Mangram AJ et al. Infect Control Hosp Epidemiol. 1999; 20: 250 -278.
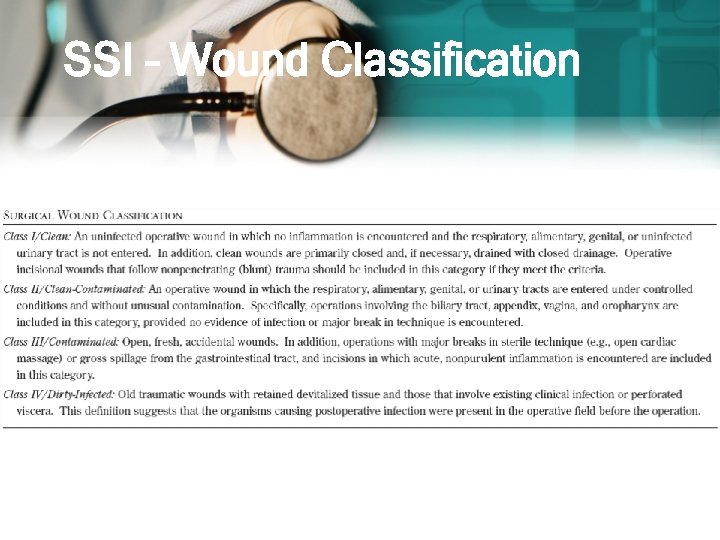
SSI – Wound Classification
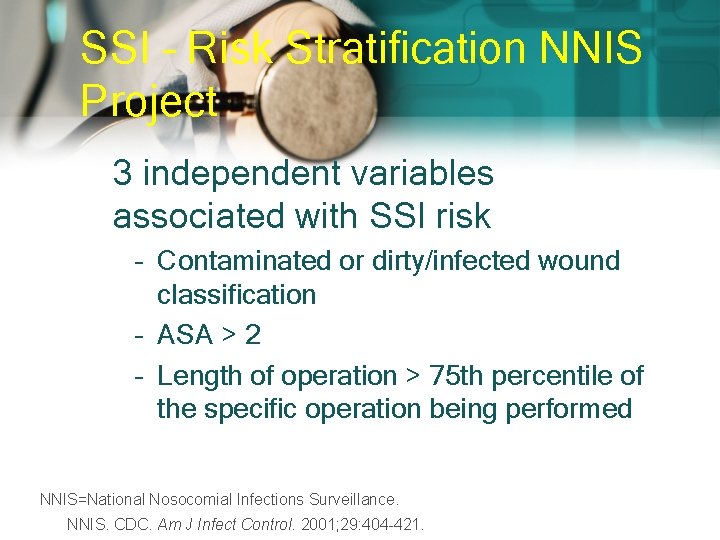
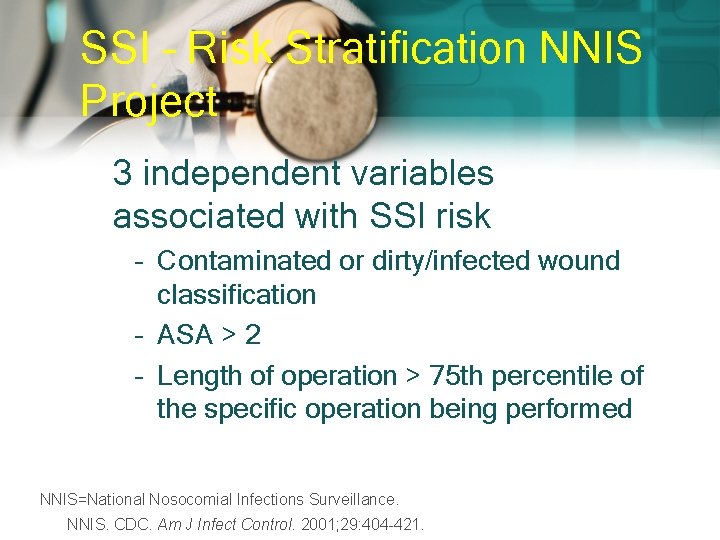
SSI – Risk Stratification NNIS Project 3 independent variables associated with SSI risk – Contaminated or dirty/infected wound classification – ASA > 2 – Length of operation > 75 th percentile of the specific operation being performed NNIS=National Nosocomial Infections Surveillance. NNIS. CDC. Am J Infect Control. 2001; 29: 404 -421.
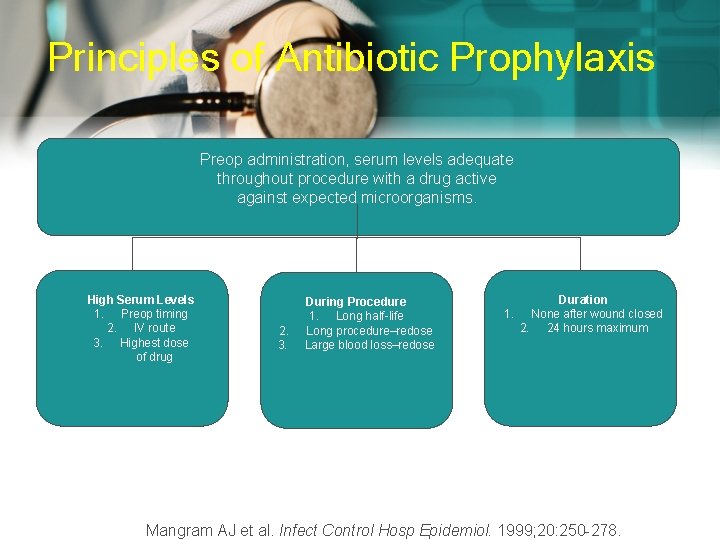
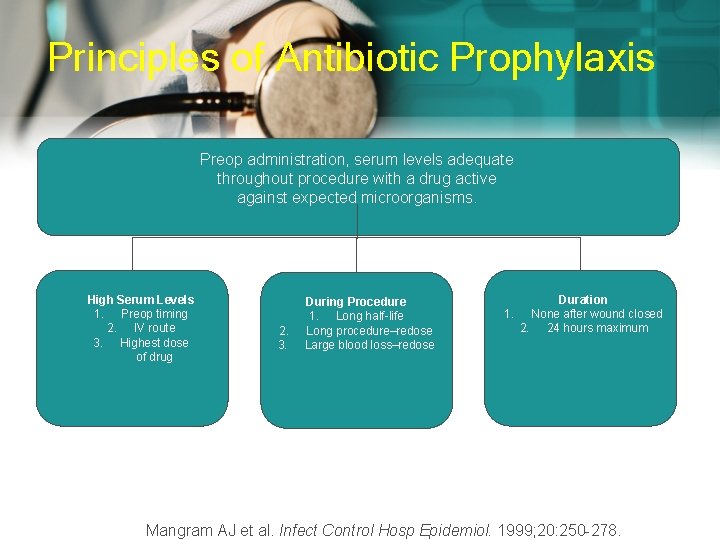
Principles of Antibiotic Prophylaxis Preop administration, serum levels adequate throughout procedure with a drug active against expected microorganisms. High Serum Levels 1. Preop timing 2. IV route 3. Highest dose of drug 2. 3. During Procedure 1. Long half-life Long procedure–redose Large blood loss–redose Duration 1. None after wound closed 2. 24 hours maximum Mangram AJ et al. Infect Control Hosp Epidemiol. 1999; 20: 250 -278.
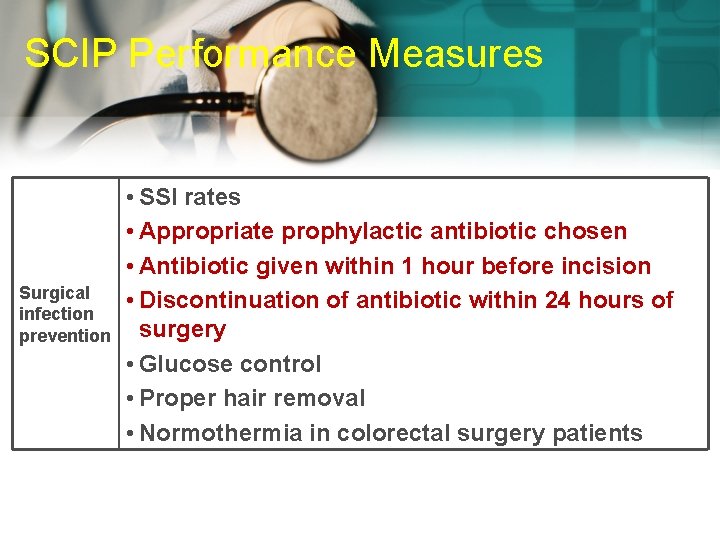
SCIP Performance Measures Surgical infection prevention • SSI rates • Appropriate prophylactic antibiotic chosen • Antibiotic given within 1 hour before incision • Discontinuation of antibiotic within 24 hours of surgery • Glucose control • Proper hair removal • Normothermia in colorectal surgery patients
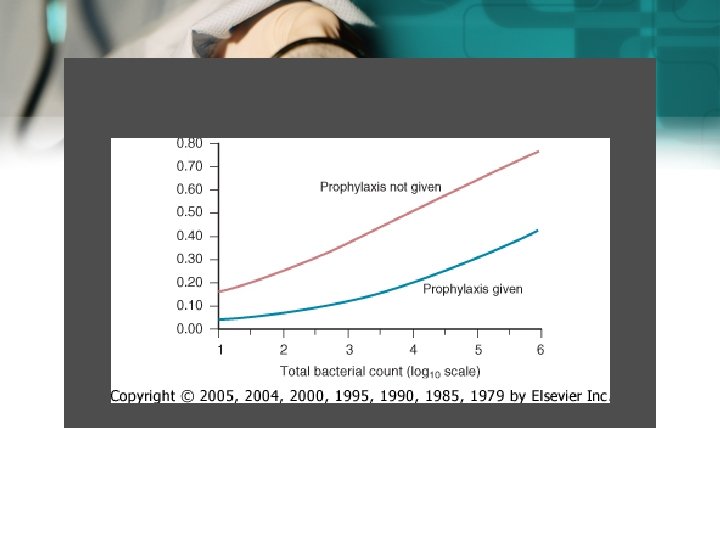
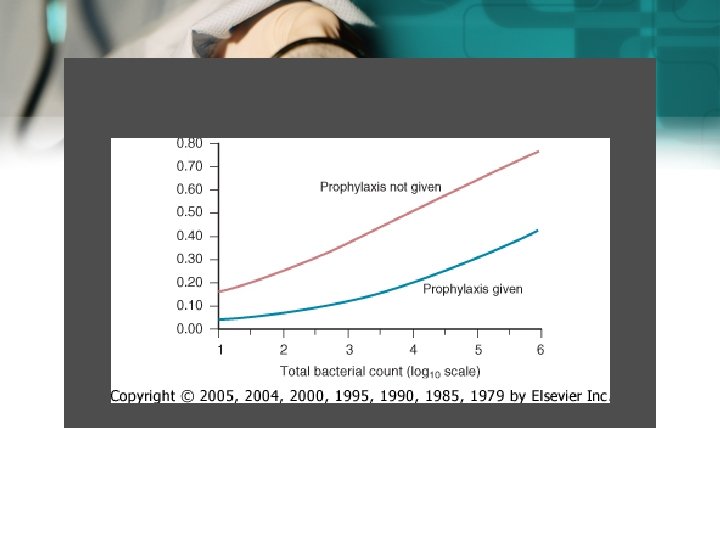
Infection Rate Downloaded from: Principles and Practice of Infectious Diseases
Process Indicators: Duration of Antimicrobial Prophylaxis Prophylactic antimicrobials should be discontinued within 24 hrs after the end of surgery Bratzler DW et al. Clin Infect Dis 2004; 38: 1706 -15.
Process Indicators: Timing of First Antibiotic Dose Infusion should begin within 60 minutes of the incision Bratzler DW et al. Clin Infect Dis 2004; 38: 1706 -15.

CATHETER ASSOCIATED UTI (CAUTI)
Importance • Catheter-associated (CA) bacteriuria is the most common health care– associated infection worldwide and • a result of the widespread use of urinary catheterization, much of which is inappropriate, in hospitals and longterm care facilities (LTCFs). 34
• The most effective way to reduce the incidence of CA-ASB and CA-UTI is to reduce the use of urinary catheterization by restricting its use to patients who have clear indications and by removing the catheter as soon as it is no longer needed 35
CAUTI • Patient has at least 2 of the following signs or symptoms with no other recognized cause: • fever (38. 8 C), • urgency, frequency, • dysuria, or suprapubic tenderness • and at least 1 of the following
CAUTI • • positive dipstick for leukocyte esterase and/ or nitrate pyuria (urine specimen with >10 white blood cell [WBC]/mm or >3 WBC/highpower field of unspun urine) • organisms seen on Gram’s stain of unspun urine • at least 2 urine cultures with repeated isolation of the same uropathogen (gram negative bacteria or Staphylococcus saprophyticus) with >10 colonies/m. L in non voided specimen
38
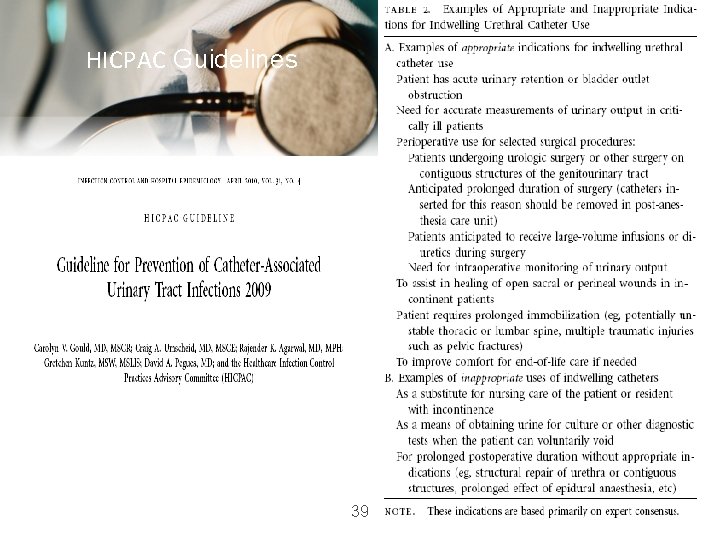
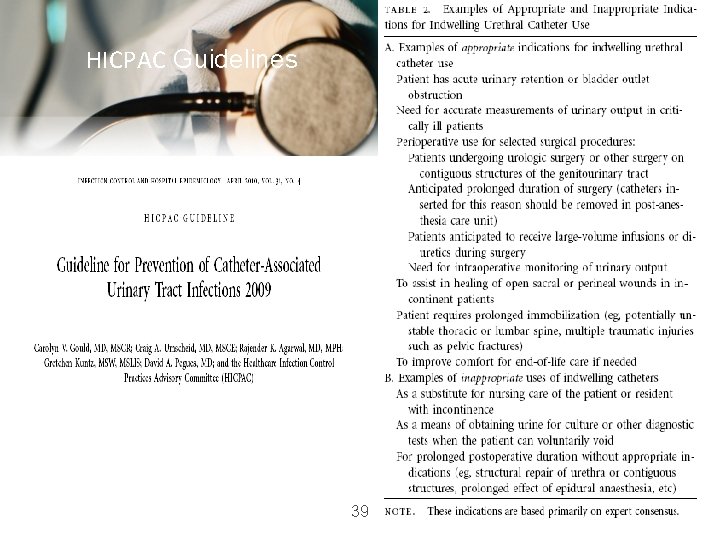
HICPAC Guidelines 39
40
41
42
43
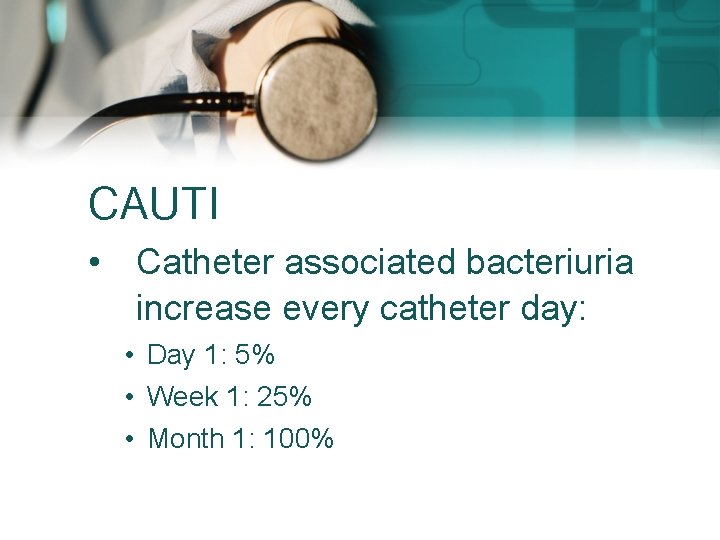
CAUTI • Catheter associated bacteriuria increase every catheter day: • Day 1: 5% • Week 1: 25% • Month 1: 100%
Prevention • removing the catheter as soon as it is no longer needed
Nosocomial Bloodstream Infections
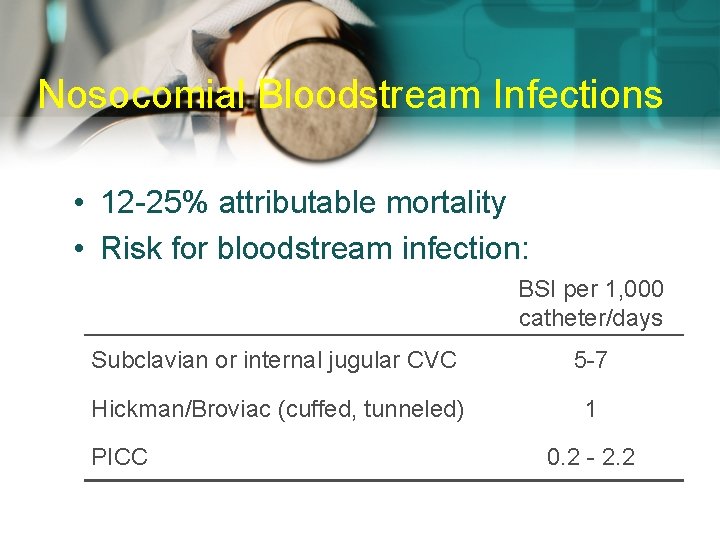
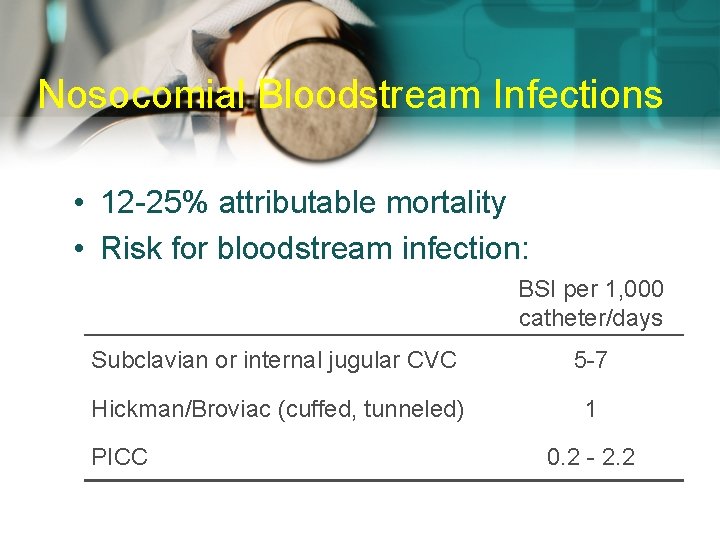
Nosocomial Bloodstream Infections • 12 -25% attributable mortality • Risk for bloodstream infection: BSI per 1, 000 catheter/days Subclavian or internal jugular CVC 5 -7 Hickman/Broviac (cuffed, tunneled) 1 PICC 0. 2 - 2. 2
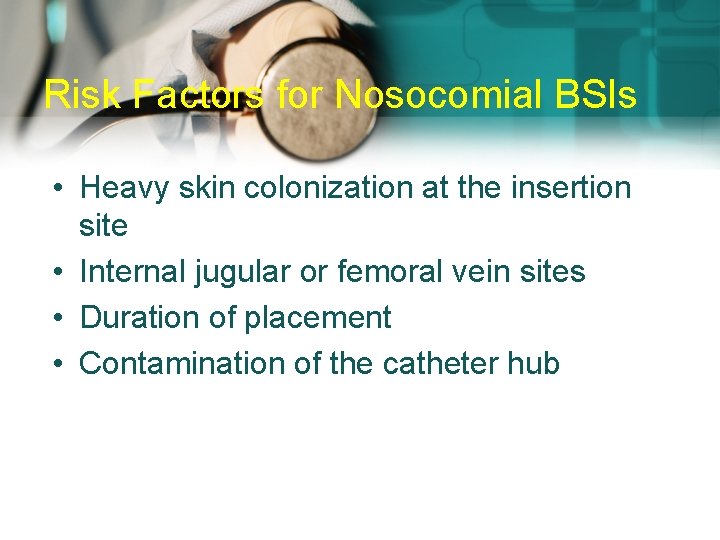
Risk Factors for Nosocomial BSIs • Heavy skin colonization at the insertion site • Internal jugular or femoral vein sites • Duration of placement • Contamination of the catheter hub
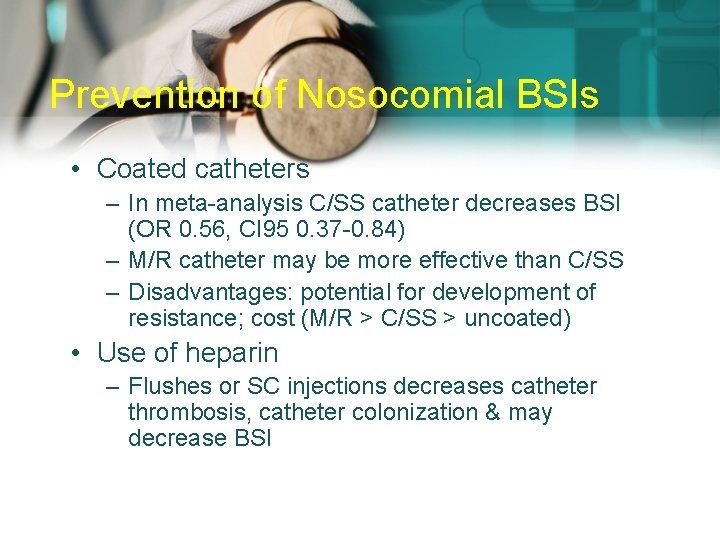
Prevention of Nosocomial BSIs • Coated catheters – In meta-analysis C/SS catheter decreases BSI (OR 0. 56, CI 95 0. 37 -0. 84) – M/R catheter may be more effective than C/SS – Disadvantages: potential for development of resistance; cost (M/R > C/SS > uncoated) • Use of heparin – Flushes or SC injections decreases catheter thrombosis, catheter colonization & may decrease BSI
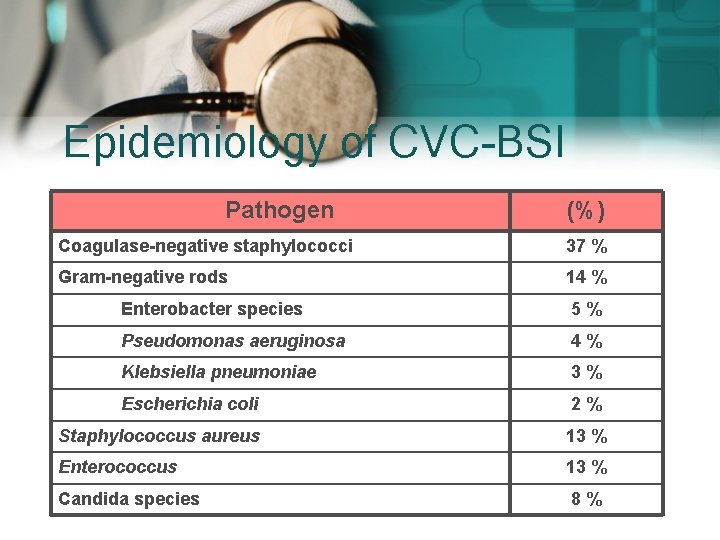
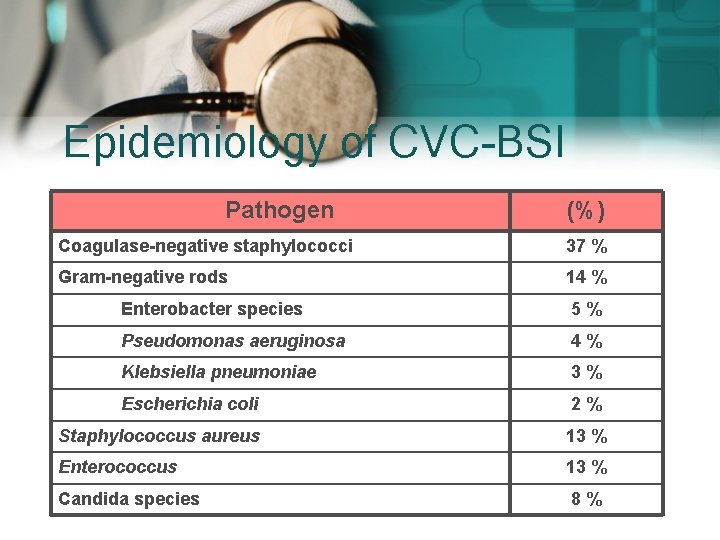
Epidemiology of CVC-BSI Pathogen (%) Coagulase-negative staphylococci 37 % Gram-negative rods 14 % Enterobacter species 5% Pseudomonas aeruginosa 4% Klebsiella pneumoniae 3% Escherichia coli 2% Staphylococcus aureus 13 % Enterococcus 13 % Candida species 8%
Prevention of Nosocomial BSIs • Limit duration of use of intravascular catheters – No advantage to changing catheters routinely • Change CVCs to PICCs when possible • Maximal barrier precautions for insertion – Sterile gloves, gown, mask, cap, full-size drape – Moderately strong supporting evidence • Chlorhexidine prep for catheter insertion
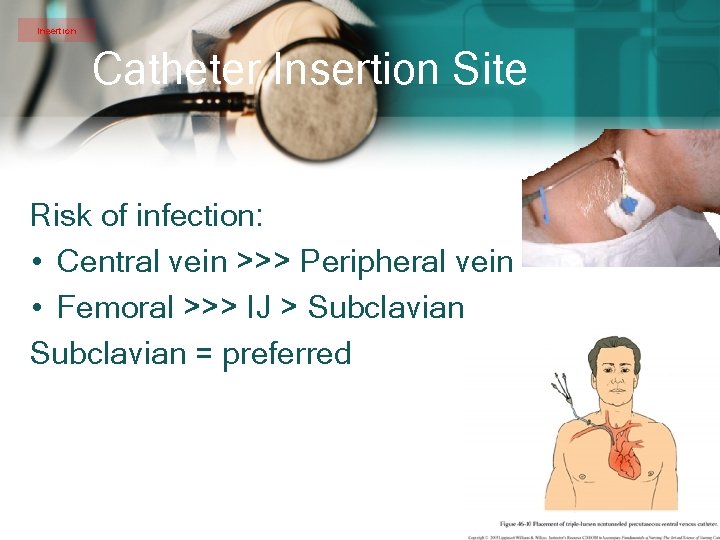
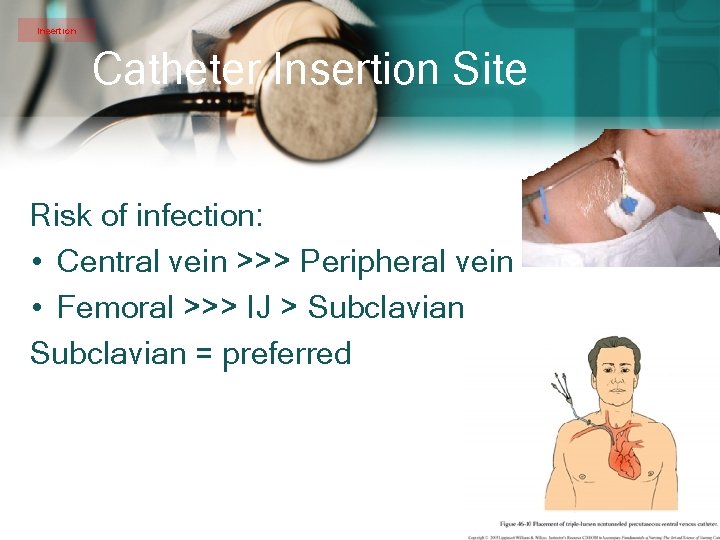
Insertion Catheter Insertion Site Risk of infection: • Central vein >>> Peripheral vein • Femoral >>> IJ > Subclavian = preferred
Components of IHI CR-BSI Prevention Bundle 1) 2) 3) 4) 5) Hand hygiene Maximal barrier precautions Chlorhexidine skin prep Optimal site selection Daily review of line necessity
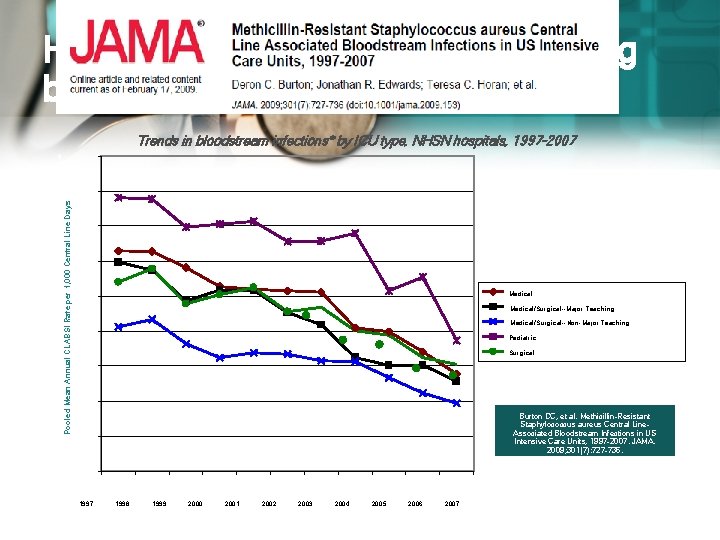
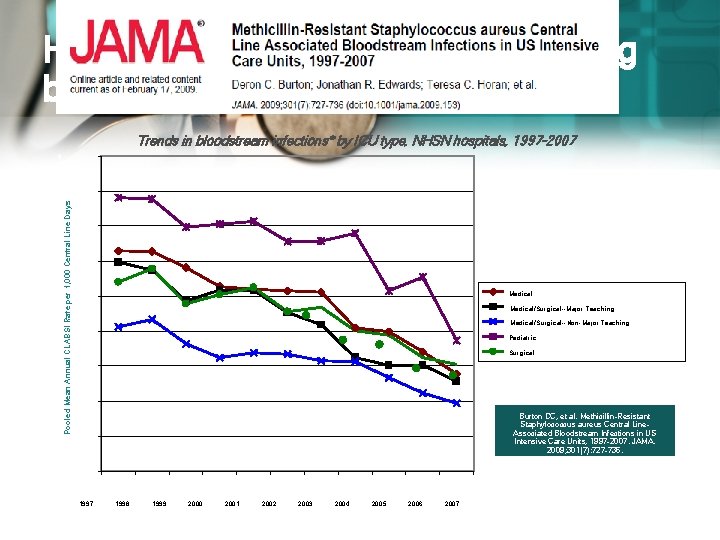
Hospitals using NHSN are preventing bloodstream infections Trends in bloodstream infections* by ICU type, NHSN hospitals, 1997 -2007 9 7 6 5 4 3 2 Pooled Mean Annual CLABSI Rate per 1, 000 Central Line Days 8 Medical/Surgical--Major Teaching Medical/Surgical--Non-Major Teaching Pediatric Surgical Burton DC, et al. Methicillin-Resistant Staphylococcus aureus Central Line. Associated Bloodstream Infections in US Intensive Care Units, 1997 -2007. JAMA. 2009; 301(7): 727 -736. 1 0 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 2007
Health-Care Associated (Nosocomial) Pneumonia
Definition Occurring at least 48 hours after admission and not incubating at the time of hospitalization
Introduction • Nosocomial pneumonia is the 2 nd most common hospital-acquired infections after UTI. Accounting for 31 % of all nosocomial infections • Nosocomial pneumonia is the leading cause of death from hospital-acquired infections. • The incidence of nosocomial pneumonia is highest in ICU.
Introduction • The incidence of nosocomial pneumonia in ventilated patients was 10 -fold higher than non-ventilated patients • The reported crude mortality for HAP is 30% to greater than 70%. --- Medical Clinics of North America Therapy of Nosocomial pneumonia 2001 vol. 85 1583 -94
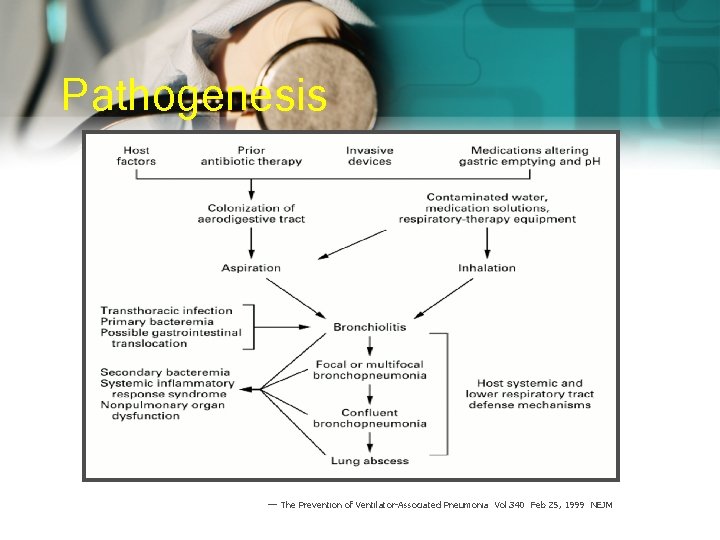
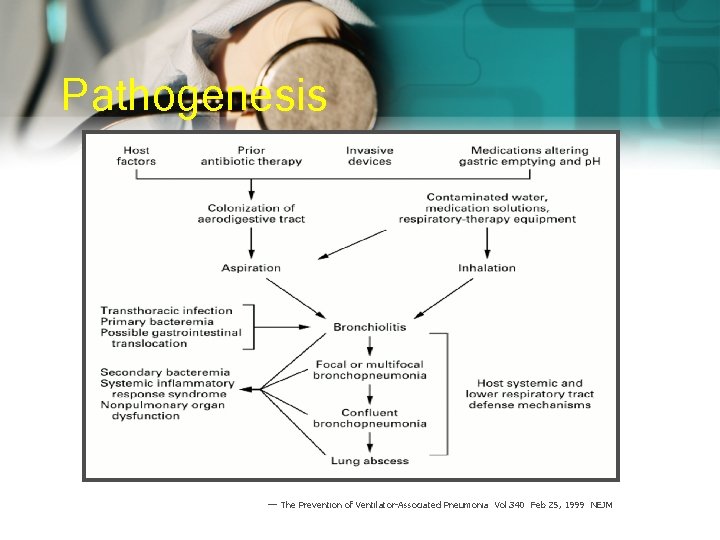
Pathogenesis --- The Prevention of Ventilator-Associated Pneumonia Vol. 340 Feb 25, 1999 NEJM
Classification • Early-onset nosocomial pneumonia: Occurs during the first 4 days Usually is due to S. pneumoniae, MSSA, H. Influenza, or anaerobes. • Late-onset nosocomial pneumonia: More than 4 days More commonly by G(-) organisms, esp. P. aeruginosa, Acinetobacter, Enterobacteriaceae (klebsiella, Enterobacter, Serratia) or MRSA.
Causative Agent • Enteric G(-) bacilli are isolated most frequently particularly in patients with lateonset disease and in patients with serious underlying disease often already on broadspectrum antibiotics. • Prior use of broad-spectrum antibiotics and an immunocompromised state make resistant gram-negative organisms more likely.
Causative Agent • P. aeruginosa and Acinetobacter are common causes of late-onset pneumonia, particularly in the ventilated patients.
Causative Agent • S. aureus is isolated in about 20~40% of cases and is particularly common in : 1. Ventilated patients after head trauma, neurosurgery, and wound infection 2. In patients who had received prior antibiotics or Prolonged care in ICU • MRSA is seen more commonly in patients Received corticosteroids Undergone mechanical ventilation >5 days Presented with chronic lung disease Had prior antibiotics therapy
Causative Agent • Anaerobes are common in patients predisposed to aspiration • VAP with anaerobes occurred more often with oropharyngeal intubation than nasopharyngeal intubation.
Causative Agent • Legionella pneumophilia occurs sporadically but may be endemic in hospitals with contaminated water systems. The incidence is underestimated because the test to identify Legionella are not performed routinely. • Because the incubation period of Legionella infection is 2 to 10 days. cases that occur more than 10 days after admission are considered to be nosocomial, and cases that develop between 4 and 10 days are considered as possible nosocomial. • Patients who are immunocompromised, critically ill, or on steroids are at highest risk for infection.
Prevention of health care-associated infection – Validated and standardized prevention strategies have been shown to reduce HCAI – At least 50% of HCAI could be prevented – Most solutions are simple and not resource-demanding and can be implemented in developed, as well as in transitional and developing countries
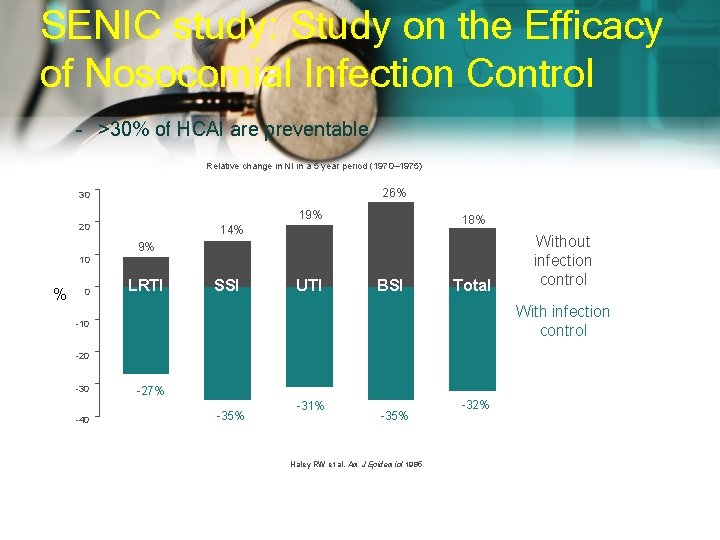
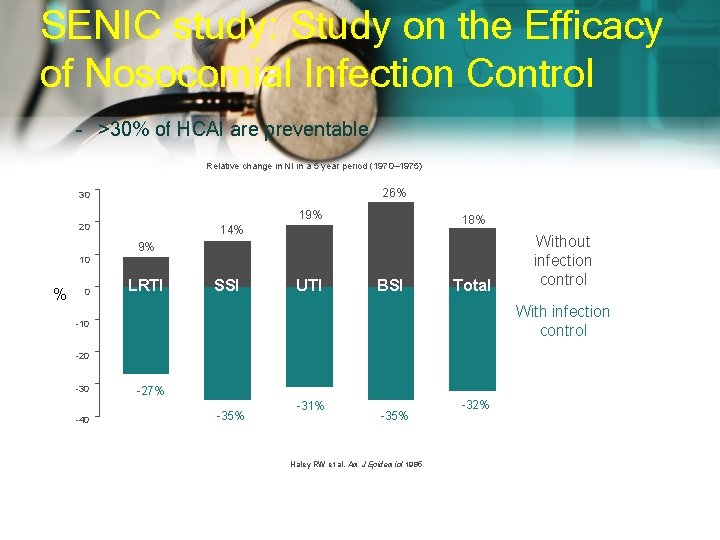
SENIC study: Study on the Efficacy of Nosocomial Infection Control – >30% of HCAI are preventable Relative change in NI in a 5 year period (1970– 1975) 26% 30 19% 20 18% 14% 9% 10 % 0 LRTI SSI UTI BSI Total With infection control -10 -20 -30 -40 Without infection control -27% -35% -31% -35% Haley RW et al. Am J Epidemiol 1985 -32%
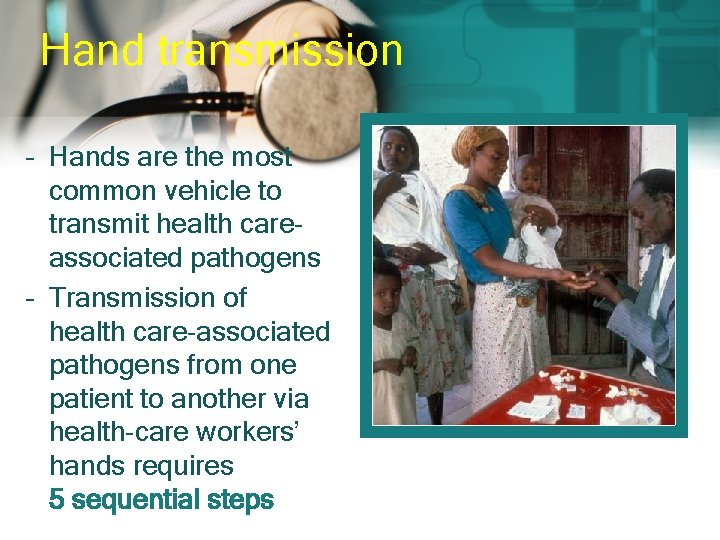
Hand transmission – Hands are the most common vehicle to transmit health careassociated pathogens – Transmission of health care-associated pathogens from one patient to another via health-care workers’ hands requires 5 sequential steps

one two three 5 stages of hand transmission Germs present on patient skin and immediate environment surfaces Germ transfer onto healthcare worker’s hands Germs survive on hands for several minutes four five Suboptimal or omitted hand cleansing results in hands remaining contaminated Contaminated hands transmit germs via direct contact with patient or patient’s immediate environment
Prevent Infection Bundles (sets of infection control recommendations) to prevent infection when inserting devices or performing procedures.
Prevent Transmission Hand Hygiene, Isolation, Environmental Cleaning, etc

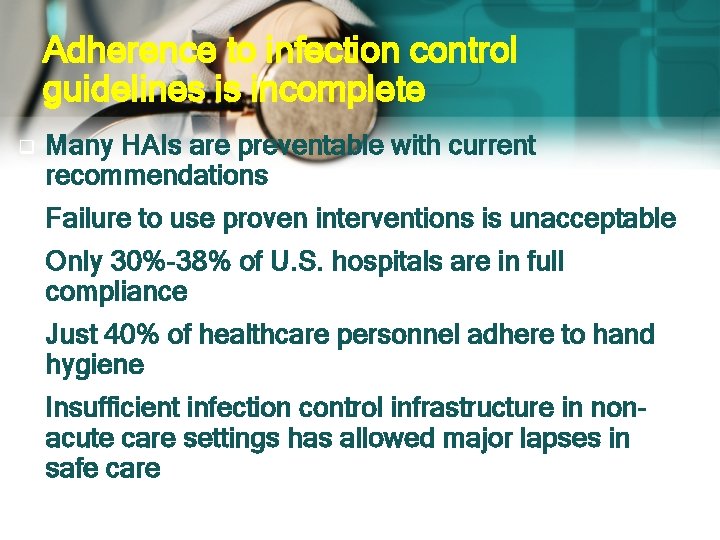
Adherence to infection control guidelines is incomplete q Many HAIs are preventable with current recommendations q Failure to use proven interventions is unacceptable q Only 30%-38% of U. S. hospitals are in full compliance q Just 40% of healthcare personnel adhere to hand hygiene q Insufficient infection control infrastructure in nonacute care settings has allowed major lapses in safe care
Why should you clean your hands? – Any health-care worker, caregiver or person involved in patient care needs to be concerned about hand hygiene – Therefore hand hygiene concerns you! – You must perform hand hygiene to: – protect the patient against harmful germs carried on your hands or present on his/her own skin – protect yourself and the health-care environment from harmful germs

The “My 5 Moments for Hand Hygiene” approach
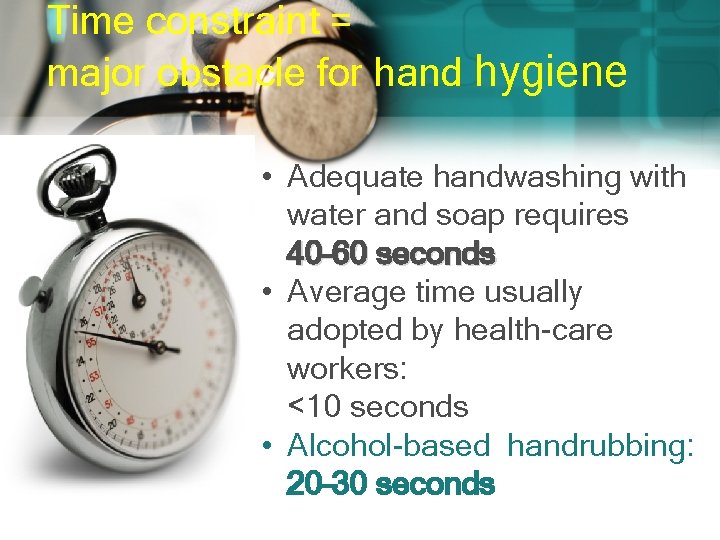
Time constraint = major obstacle for hand hygiene • Adequate handwashing with water and soap requires 40– 60 seconds • Average time usually adopted by health-care workers: <10 seconds • Alcohol-based handrubbing: 20– 30 seconds
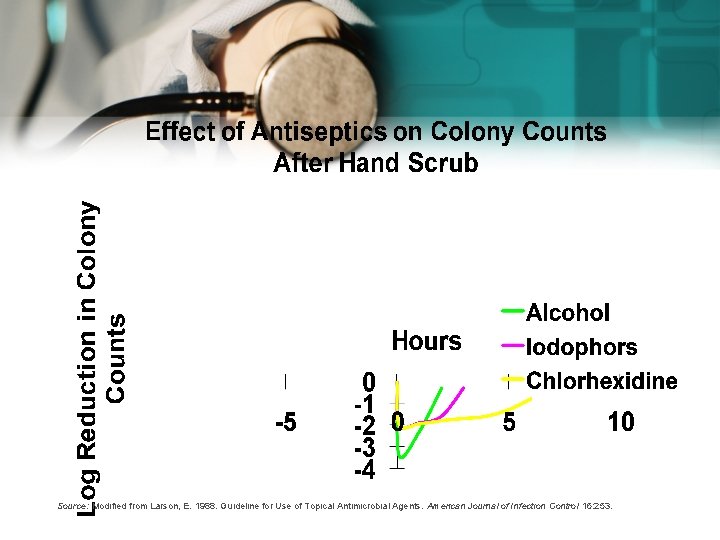
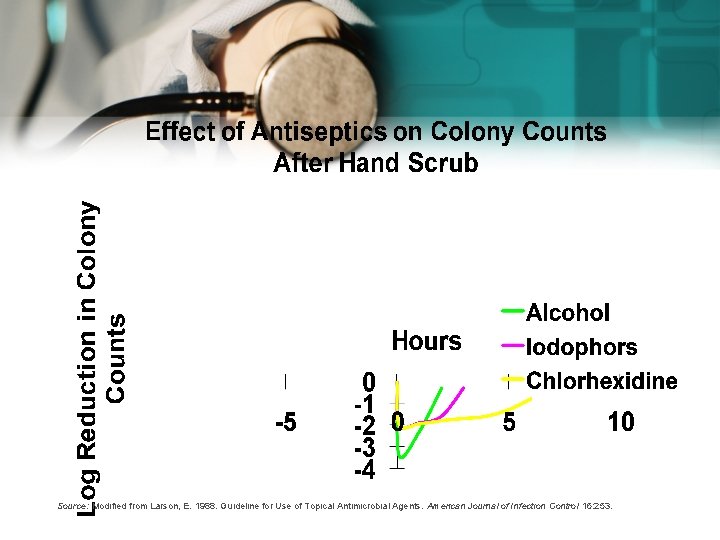
Source: Modified from Larson, E. 1988. Guideline for Use of Topical Antimicrobial Agents. American Journal of Infection Control 16: 253.
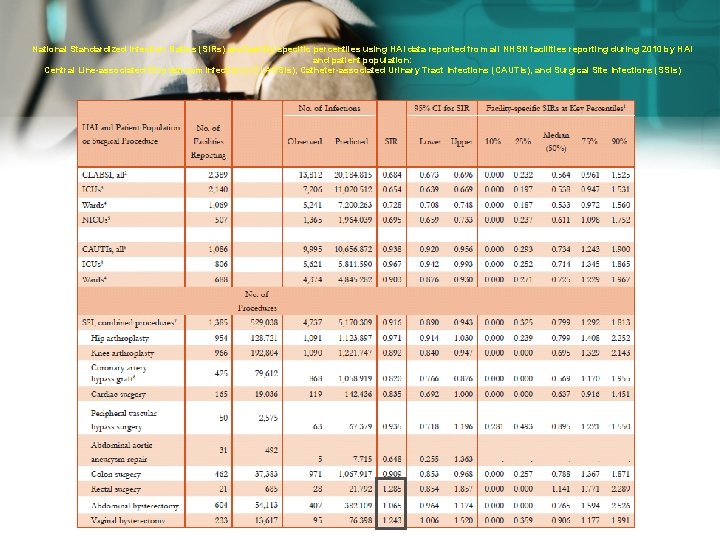
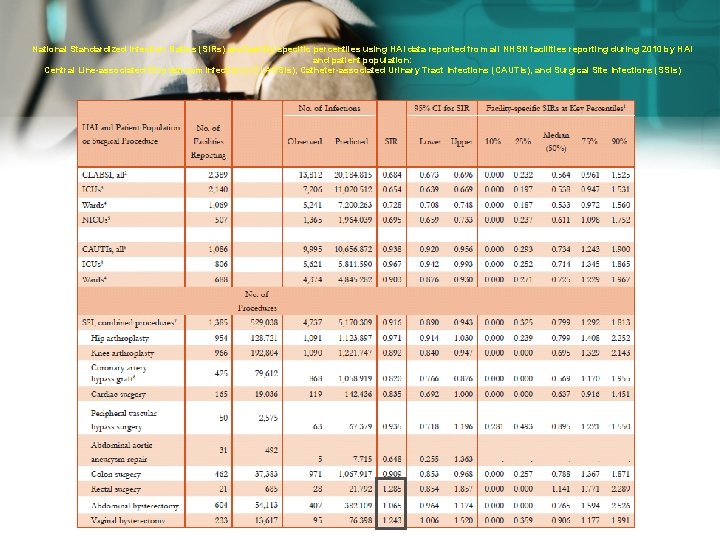
National Standardized Infection Ratios (SIRs) and facility-specific percentiles using HAI data reported from all NHSN facilities reporting during 2010 by HAI and patient population: Central Line-associated Bloodstream Infections (CLABSIs), Catheter-associated Urinary Tract Infections (CAUTIs), and Surgical Site Infections (SSIs)




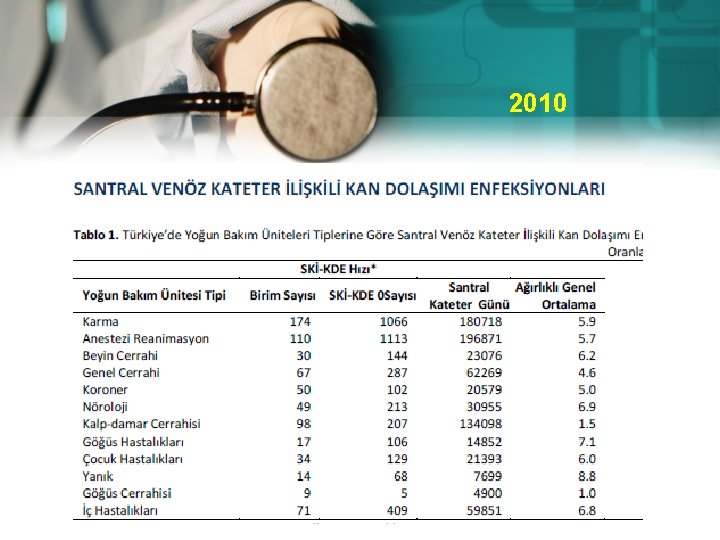
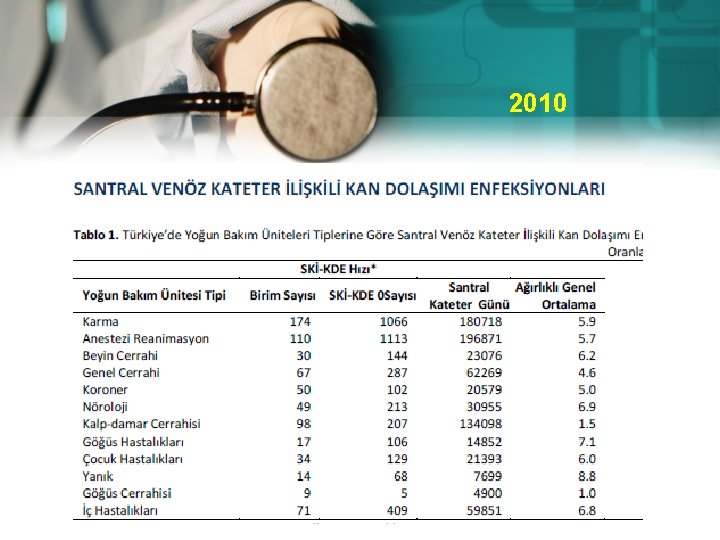
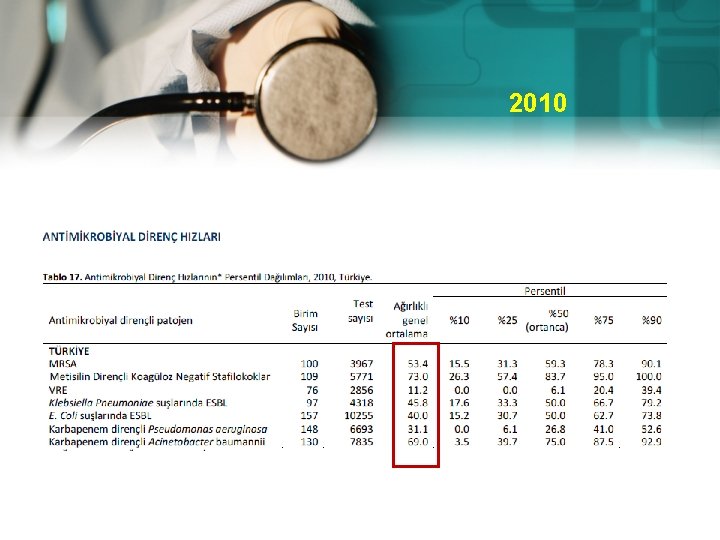
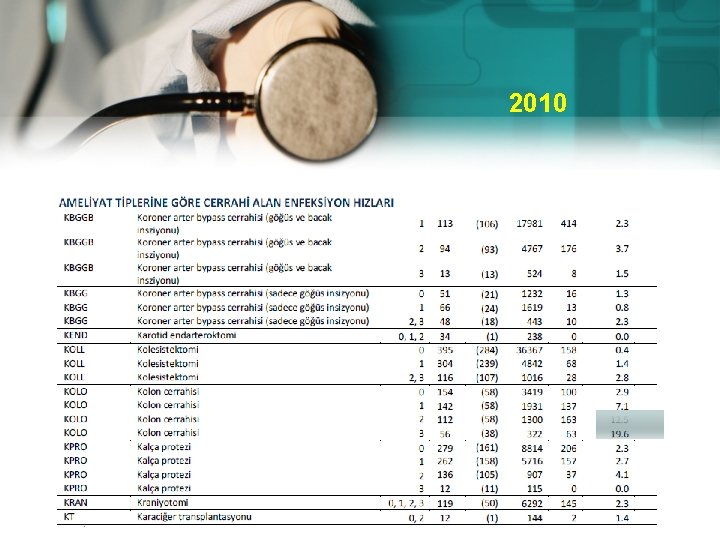
2010
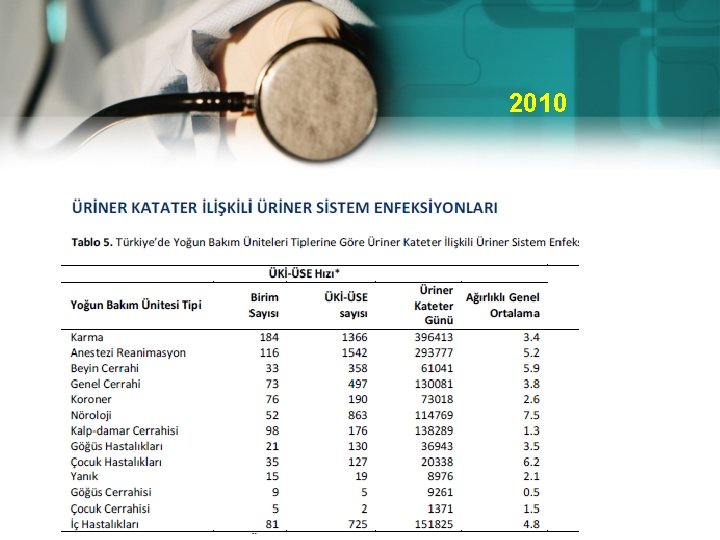
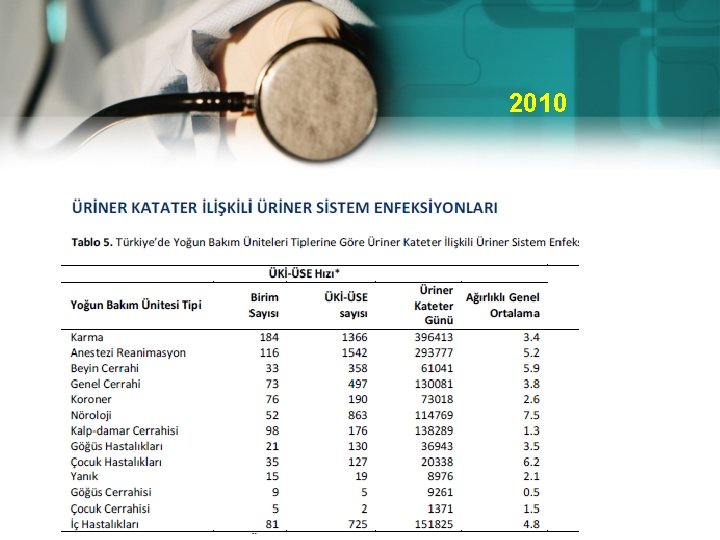
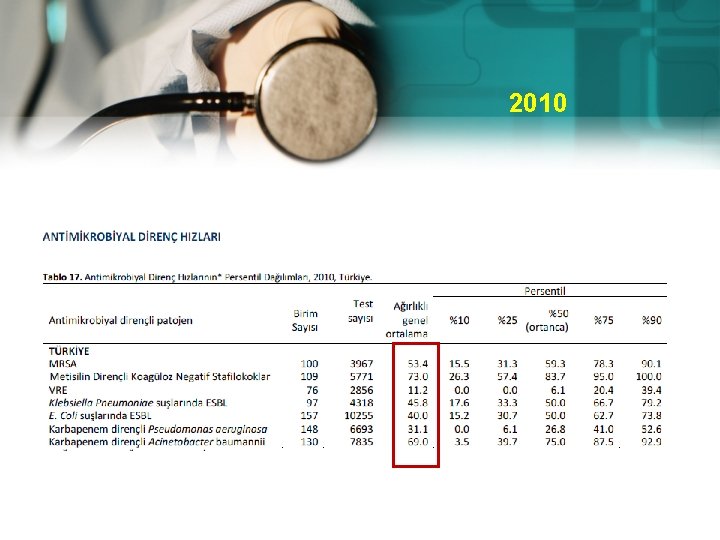
2010
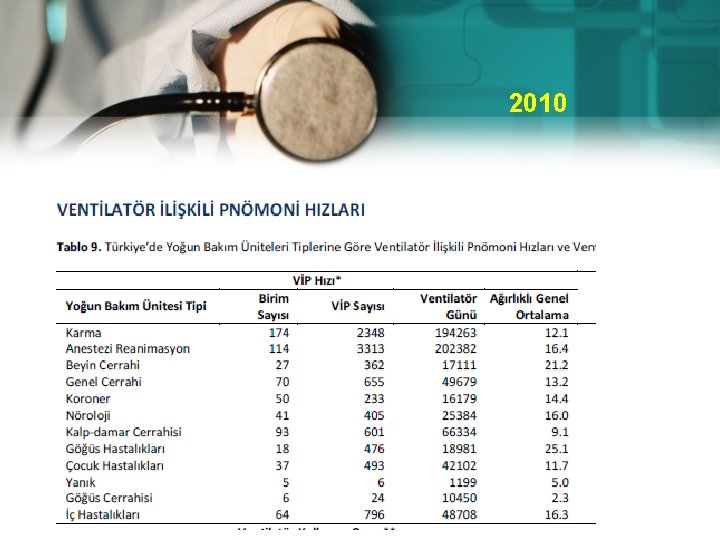
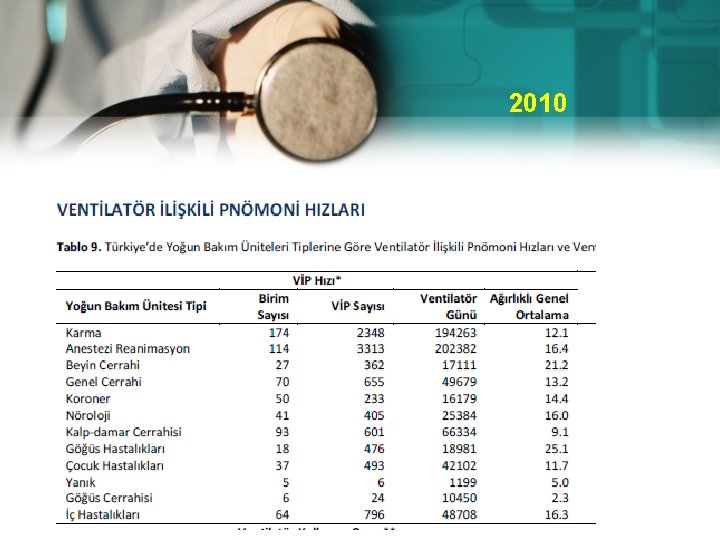
2010
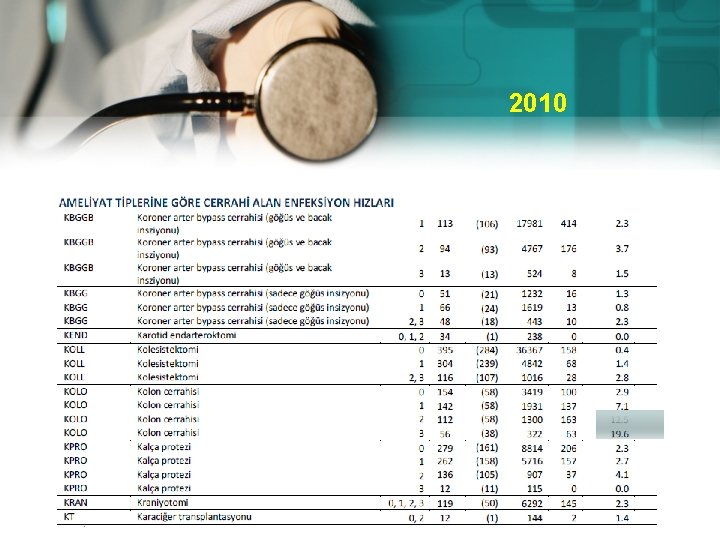
2010
2010



TUS 2012 • Aşağıdakilerden hangisi temiz-kontamine yaraya örnektir? A) Kolesistektomi B) Tiroidektomi C) İnguinal fıtık onarımı D) Mastektomi E) Perfore apandisit varlığında apendektomi
TUS 2012 • Aşağıdakilerden hangisi temiz-kontamine yaraya örnektir? A) Kolesistektomi B) Tiroidektomi C) İnguinal fıtık onarımı D) Mastektomi E) Perfore apandisit varlığında apendektomi
TUS 2012 • Protez, greft gibi implantların uygulandığı ameliyatlarda cerrahi alan enfeksiyonu tanısı koyabilmek için enfeksiyon en geç ne zaman ortaya çıkmalıdır? A) 1 ay B) 3 ay C) 6 ay D) 1 yıl E) 2 yıl
TUS 2012 • Protez, greft gibi implantların uygulandığı ameliyatlarda cerrahi alan enfeksiyonu tanısı koyabilmek için enfeksiyon en geç ne zaman ortaya çıkmalıdır? A) 1 ay B) 3 ay C) 6 ay D) 1 yıl E) 2 yıl
TUS 2010 Aşağıdaki ameliyat tiplerinin hangisinde cerrahi alan enfeksiyonu en fazla görülür? A) Kolesistektomi B) Tiroidektomi C) Memeden kitle eksizyonu D) Kolon rezeksiyonu E) İnguinal herni ameliyatı
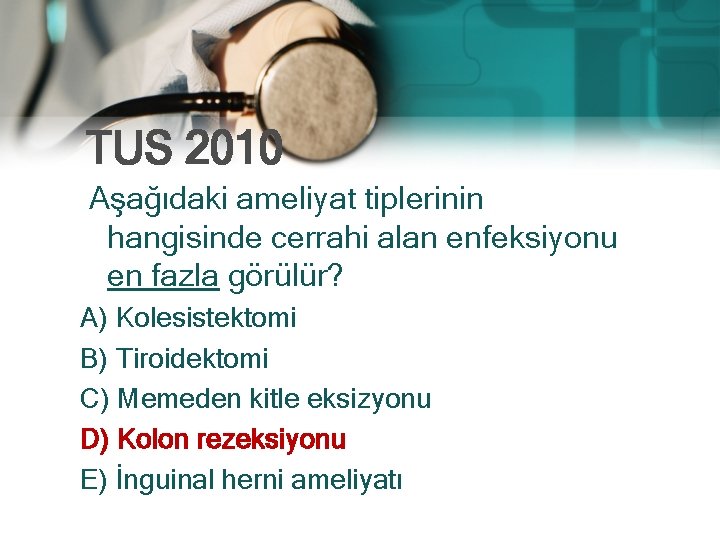
TUS 2010 Aşağıdaki ameliyat tiplerinin hangisinde cerrahi alan enfeksiyonu en fazla görülür? A) Kolesistektomi B) Tiroidektomi C) Memeden kitle eksizyonu D) Kolon rezeksiyonu E) İnguinal herni ameliyatı
 Pakigri
Pakigri Coadsys exam
Coadsys exam Coadsys exam
Coadsys exam Meral yılmaz öğretmen
Meral yılmaz öğretmen Pınar seden meral
Pınar seden meral Meral güneş ergin
Meral güneş ergin Meral dogan
Meral dogan Ankara protokol listesi
Ankara protokol listesi Colposcopy
Colposcopy Opportunistic infections
Opportunistic infections Methotrexate yeast infection
Methotrexate yeast infection Opportunistic infections
Opportunistic infections Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Johnson and johnson botnet infections
Johnson and johnson botnet infections Storch infections
Storch infections Storch infections
Storch infections Bone and joint infections
Bone and joint infections Neurosiphyllis
Neurosiphyllis Eye infections
Eye infections Postpartum infections
Postpartum infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Genital infections
Genital infections Amber blumling
Amber blumling Phagocytr
Phagocytr Acute gingival infections
Acute gingival infections Pharmacist required for 250 beds
Pharmacist required for 250 beds University hospital of pisa
University hospital of pisa Bezmalem
Bezmalem Benha university hospital
Benha university hospital Kyorin university ranking
Kyorin university ranking University hospital tuebingen
University hospital tuebingen Pisa university hospital
Pisa university hospital Patras university hospital
Patras university hospital Pisa university hospital
Pisa university hospital Hanifin rajka atopic dermatitis
Hanifin rajka atopic dermatitis Portsmouth hospitals nhs trust values
Portsmouth hospitals nhs trust values Kyung hee university hospital at gangdong
Kyung hee university hospital at gangdong Kaohsiung medical university hospital
Kaohsiung medical university hospital University of iowa hospitals and clinics
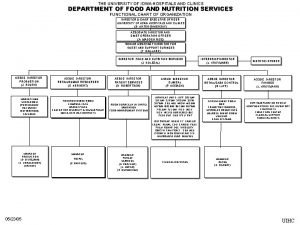
University of iowa hospitals and clinics King saud university hospital nurse salary
King saud university hospital nurse salary 沈榮麟
沈榮麟 York hospital entrance 2
York hospital entrance 2 Erpno
Erpno Ninewells hospital outpatients area 3
Ninewells hospital outpatients area 3 Wardaccreditationprogramme
Wardaccreditationprogramme Umd capital region health
Umd capital region health Evangelismos laboratory
Evangelismos laboratory Tung shin tcm
Tung shin tcm L hospital kuralı
L hospital kuralı X=a doğrusu
X=a doğrusu Royal surrey hospital buses
Royal surrey hospital buses Balfour ward cameron hospital
Balfour ward cameron hospital Dally and sodapop
Dally and sodapop Swatt warwick hospital
Swatt warwick hospital Decent hospital
Decent hospital Pink wristband meaning hospital
Pink wristband meaning hospital Code green hospital
Code green hospital Igawilo hospital
Igawilo hospital Caj rawatan warga asing 2020
Caj rawatan warga asing 2020 Swedish american heart hospital
Swedish american heart hospital Suvarna arogya suraksha trust hospital list
Suvarna arogya suraksha trust hospital list Code red hospital
Code red hospital Infrastructure of hospital pharmacy
Infrastructure of hospital pharmacy St john's episcopal ophthalmology residency
St john's episcopal ophthalmology residency St francis hospital escanaba mi
St francis hospital escanaba mi Srs hospital management system
Srs hospital management system Game use case diagram
Game use case diagram Sarvodaya hospital bidada
Sarvodaya hospital bidada Severance children's hospital
Severance children's hospital A sentinel event
A sentinel event Niveles de la salud
Niveles de la salud Aintree beds
Aintree beds Hospital heli moreno blanco
Hospital heli moreno blanco Adverse events in hospital
Adverse events in hospital Ir adverse event
Ir adverse event Puerperal endometritis
Puerperal endometritis Hospital straight elevator
Hospital straight elevator National orthopaedic hospital cappagh
National orthopaedic hospital cappagh Analise swot de um hospital
Analise swot de um hospital 405 field hospital
405 field hospital Cascade valley hospital
Cascade valley hospital Audifonos es una palabra aguda grave o esdrujula
Audifonos es una palabra aguda grave o esdrujula Mullinure hospital armagh
Mullinure hospital armagh Kaiser santa rosa medical records
Kaiser santa rosa medical records Nursing organizational chart in hospital
Nursing organizational chart in hospital Organizational structure of private hospital
Organizational structure of private hospital Marshall pickens hospital
Marshall pickens hospital Omd552
Omd552 Omd hospital
Omd hospital Northside hospital new hire orientation
Northside hospital new hire orientation Normas de higiene en un hospital
Normas de higiene en un hospital Ward 41 auckland hospital
Ward 41 auckland hospital Labana developers
Labana developers Mount auburn professional services
Mount auburn professional services Begoña huete neurologa
Begoña huete neurologa Hospital de basurto historia
Hospital de basurto historia Plano pabellones hospital basurto
Plano pabellones hospital basurto