TRANSFUSION INDICATIONS AND REACTIONS Dr Meral SNMEZOLU Yeditepe



















- Slides: 84

TRANSFUSION INDICATIONS AND REACTIONS Dr. Meral SÖNMEZOĞLU Yeditepe University Hospital Transfusion Center
Early History of Transfusion Ø Harvey’s theory of circulation, 1628 Ø Physick, Philadelphia, 1795 Ø Blundell, England, 1818 Ø Problems of sterility, coagulability, intravenous routes ignored
Karl Landsteiner (1868 -1943) Discovered ABO blood groups, 1900 Ø Nobel Prize, 1930 Ø

Classic Nine Blood Group Systems ABO, 1900 Ø MN and P, 1927 Ø Rh, 1940 Ø Lutheran, 1945 Ø Kell, 1946 Ø Lewis, 1946 Ø Duffy, 1950 Ø Kidd, 1951 Ø
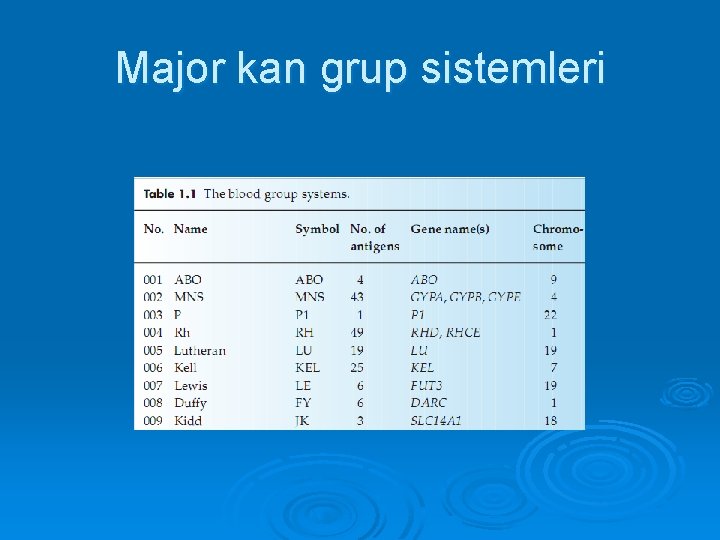
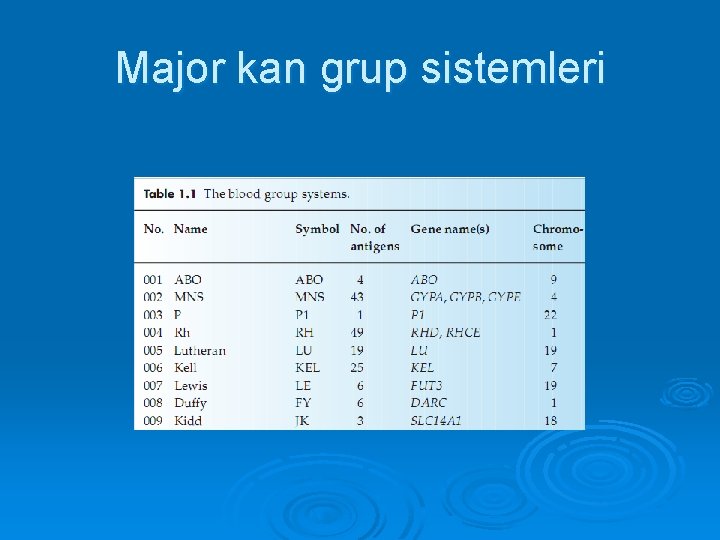
Major kan grup sistemleri

Diğer kan grup sistemleri
Compatibility Testing Ø Ig. M antibodies- direct agglutination; reactive in cold (room temp or below); either intra- or extravascular hemolysis Ø Ig. G antibodies- often require antiglobulin reagent to allow agglutination; reactive at body temp (37 C); usually extravascular hemolysis
Compatibility Testing (2) Ø Type- determine recipient’s ABO and Rh (D) type l l Forward type- Ag on RBCs Backward type- Corresponding Ab in serum Ø Screen- two/three RBC panel to detect unexpected antibodies Ø Antibody identification using extended panel
Compatibility Testing (3) Ø Immediate spin Ø Incubation at 37 C Ø Antiglobulin phase
Compatibility Testing (4) Ø Crossmatch- donor RBCs with recipient serum, look for agglutination Ø Screen- detect weak antibodies Ø Crossmatch- detect Ab against lowincidence Ag
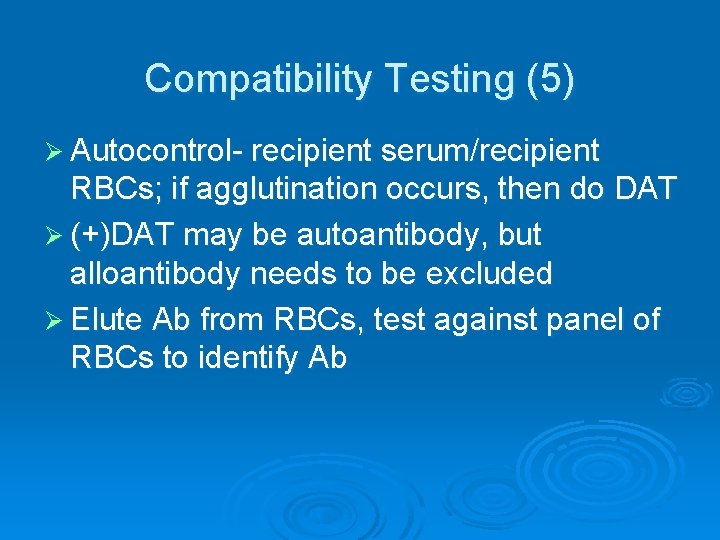
Compatibility Testing (5) Ø Autocontrol- recipient serum/recipient RBCs; if agglutination occurs, then do DAT Ø (+)DAT may be autoantibody, but alloantibody needs to be excluded Ø Elute Ab from RBCs, test against panel of RBCs to identify Ab
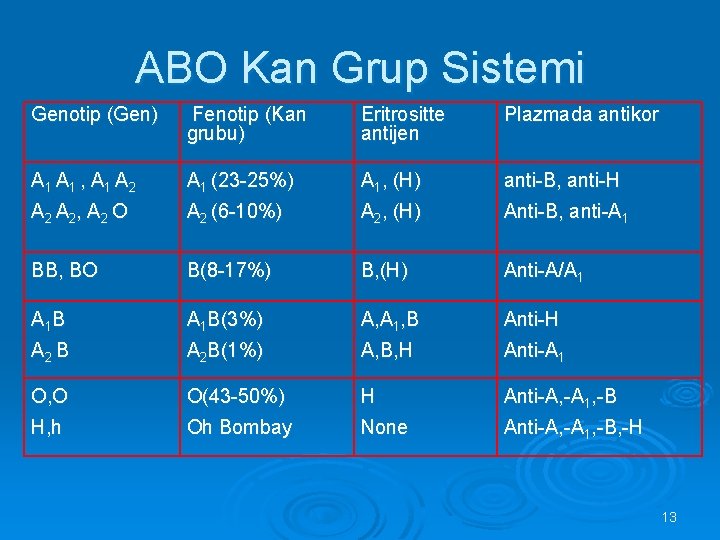
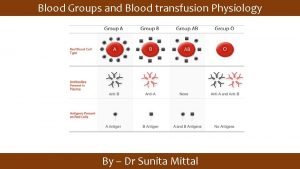
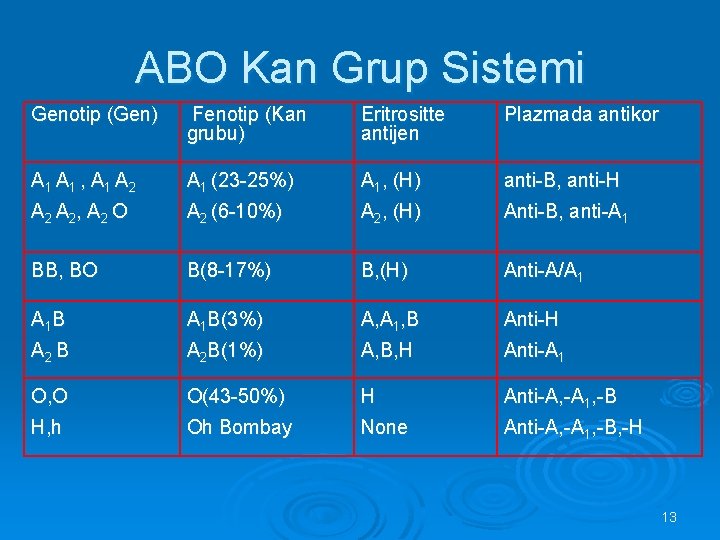
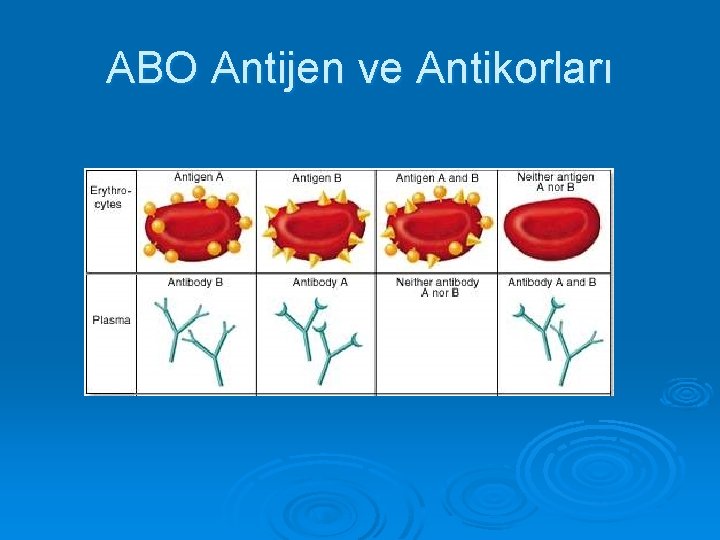
ABO Kan Grup Sistemi Genotip (Gen) Fenotip (Kan grubu) Eritrositte antijen Plazmada antikor A 1 , A 1 A 2 A 1 (23 -25%) A 1, (H) anti-B, anti-H A 2 , A 2 O A 2 (6 -10%) A 2, (H) Anti-B, anti-A 1 BB, BO B(8 -17%) B, (H) Anti-A/A 1 B A 1 B(3%) A, A 1, B Anti-H A 2 B A 2 B(1%) A, B, H Anti-A 1 O, O O(43 -50%) H Anti-A, -A 1, -B H, h Oh Bombay None Anti-A, -A 1, -B, -H 13
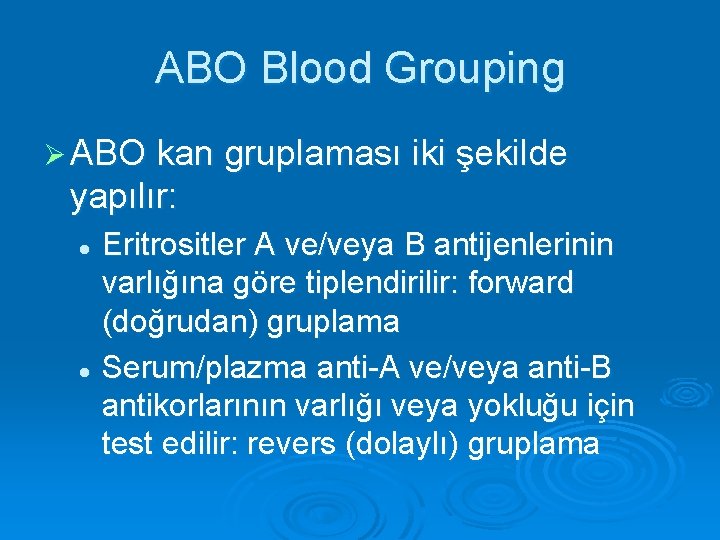
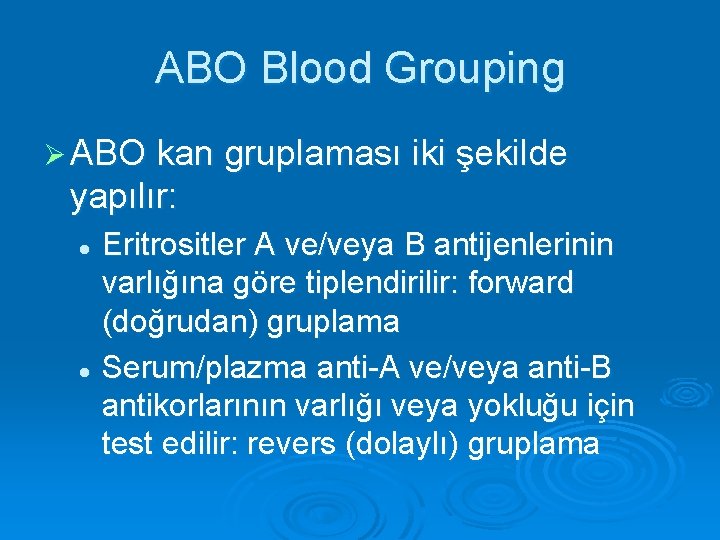
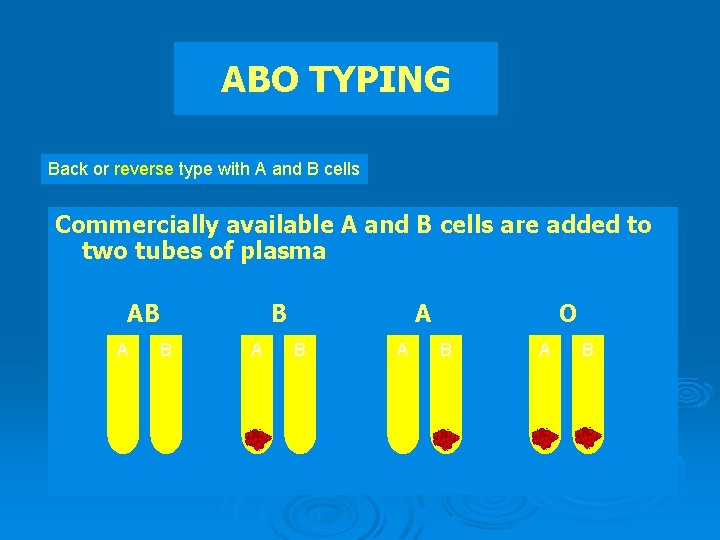
ABO Blood Grouping Ø ABO kan gruplaması iki şekilde yapılır: Eritrositler A ve/veya B antijenlerinin varlığına göre tiplendirilir: forward (doğrudan) gruplama l Serum/plazma anti-A ve/veya anti-B antikorlarının varlığı veya yokluğu için test edilir: revers (dolaylı) gruplama l
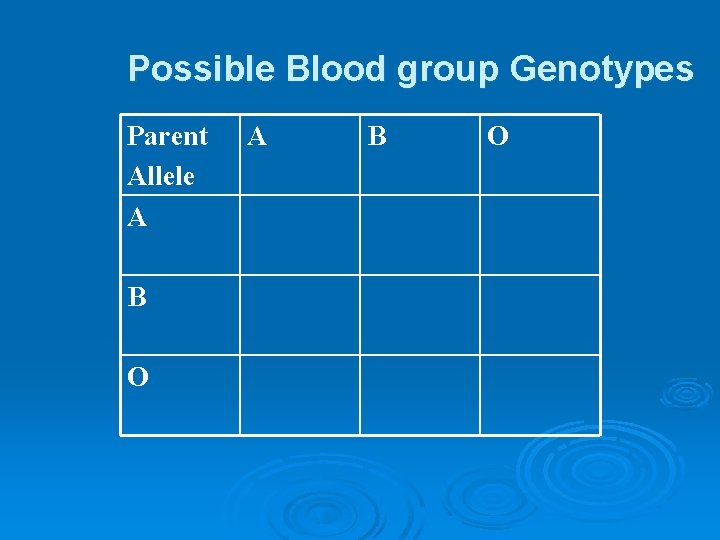
Possible Blood group Genotypes Parent Allele A B O
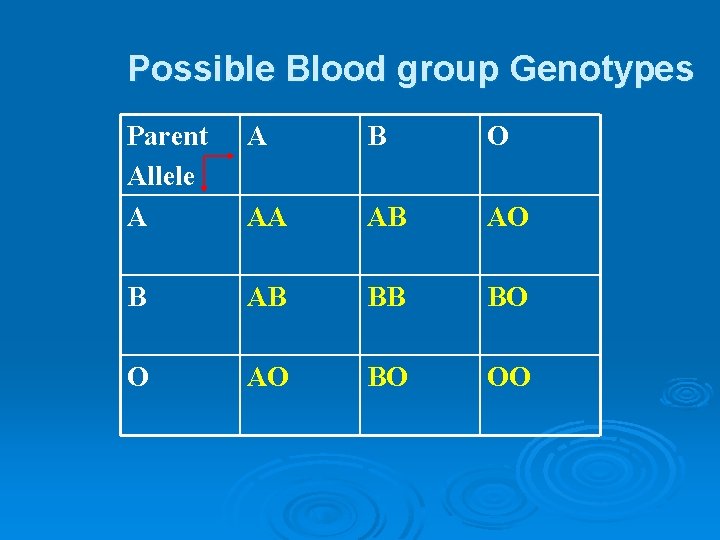
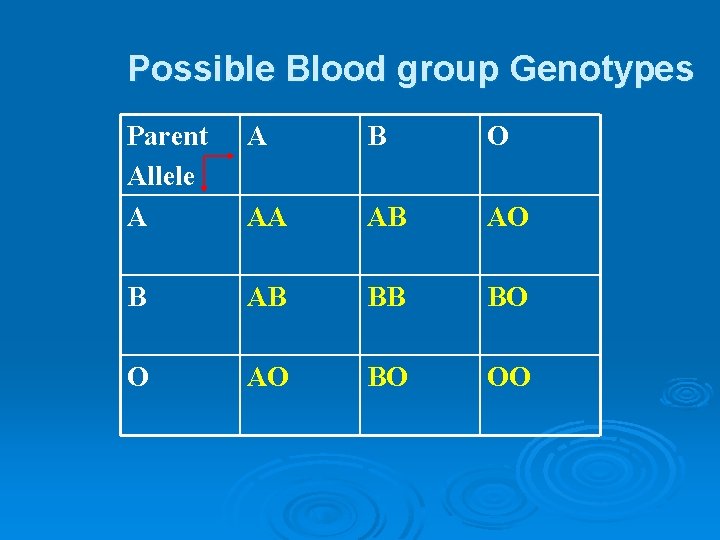
Possible Blood group Genotypes Parent Allele A A B O AA AB AO B AB BB BO O AO BO OO
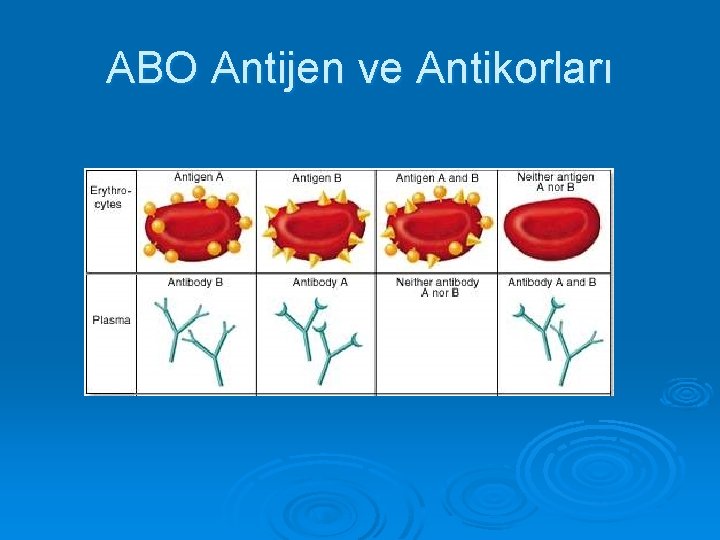
ABO Antijen ve Antikorları

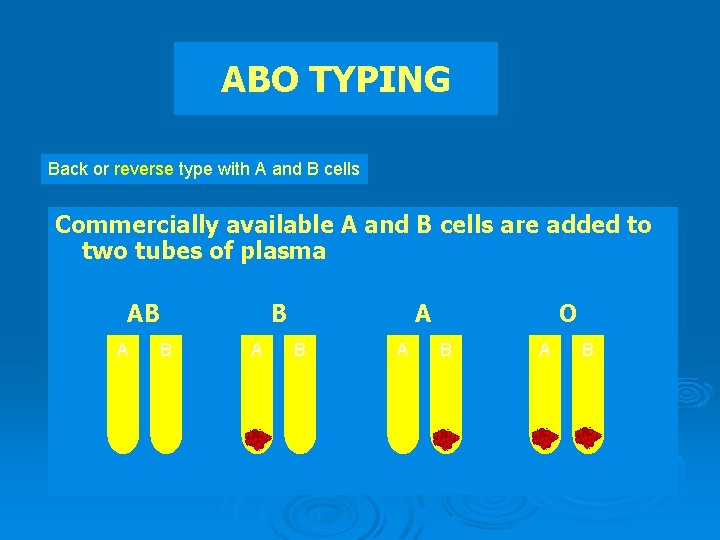
ABO TYPING Back or reverse type with A and B cells Commercially available A and B cells are added to two tubes of plasma AB A B B A A B A O B A B
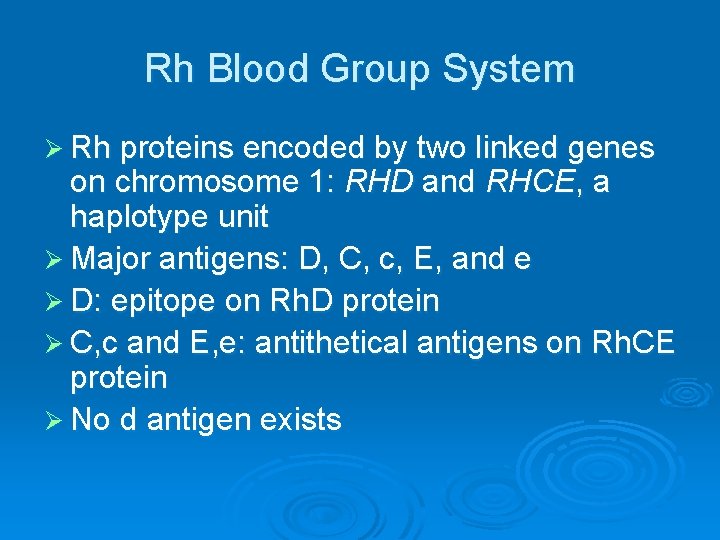
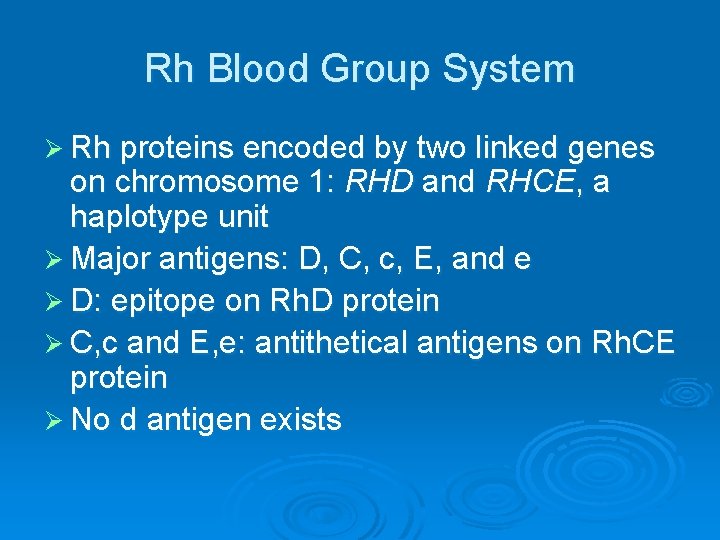
Rh Blood Group System Ø Rh proteins encoded by two linked genes on chromosome 1: RHD and RHCE, a haplotype unit Ø Major antigens: D, C, c, E, and e Ø D: epitope on Rh. D protein Ø C, c and E, e: antithetical antigens on Rh. CE protein Ø No d antigen exists
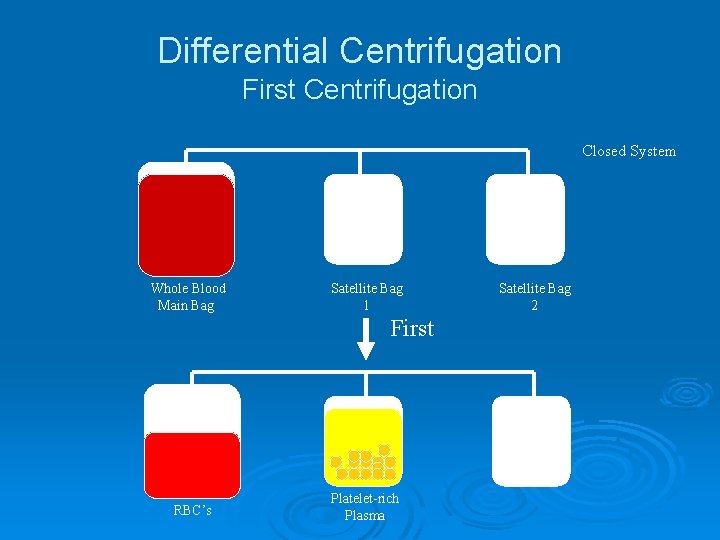
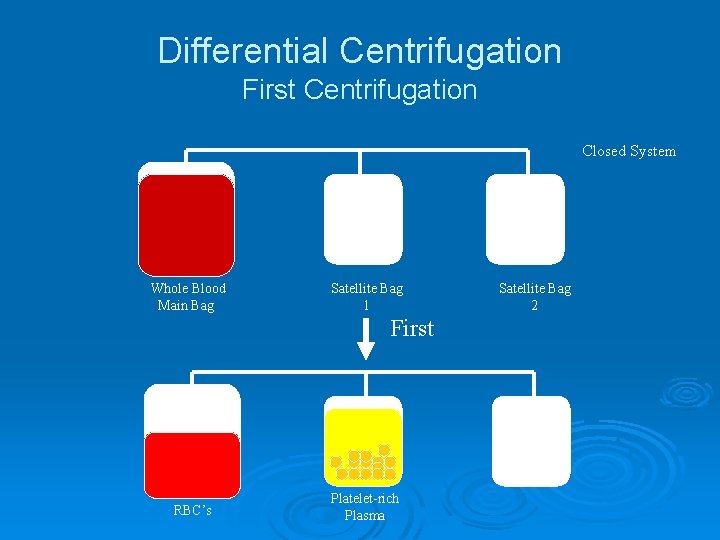
Differential Centrifugation First Centrifugation Closed System Whole Blood Main Bag Satellite Bag 1 First RBC’s Platelet-rich Plasma Satellite Bag 2
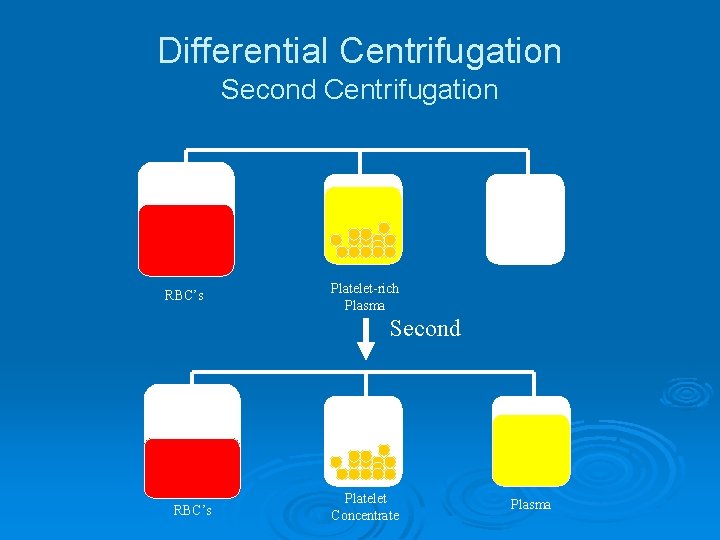
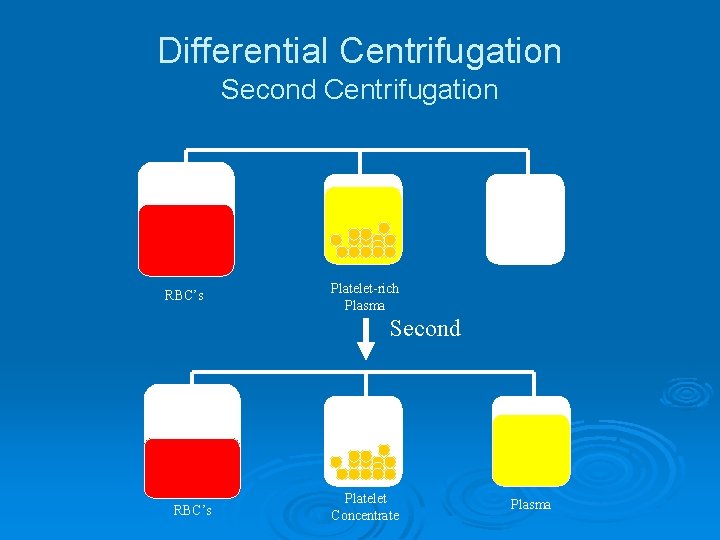
Differential Centrifugation Second Centrifugation RBC’s Platelet-rich Plasma Second RBC’s Platelet Concentrate Plasma
Whole Blood Ø Storage l Ø Indications l Ø 4° for up to 35 days Massive Blood Loss/Trauma/Exchange Transfusion Considerations l l Use filter as platelets and coagulation factors will not be active after 3 -5 days Donor and recipient must be ABO identical
RBC Concentrate Ø Storage l Ø Indications l Ø 4° for up to 42 days, can be frozen Many indications—ie anemia, hypoxia, etc. Considerations l l l Recipient must not have antibodies to donor RBC’s (note: patients can develop antibodies over time) Usual dose 10 cc/kg (will increase Hgb by 2. 5 gm/dl) Usually transfuse over 2 -4 hours (slower for chronic anemia
Function of RBCs Oxygen Transport Ø Delivery of oxygen from lungs to tissues Oxygen transport is dependent on Ø Hematocrit Ø Cardiac output Ø Oxygen extraction
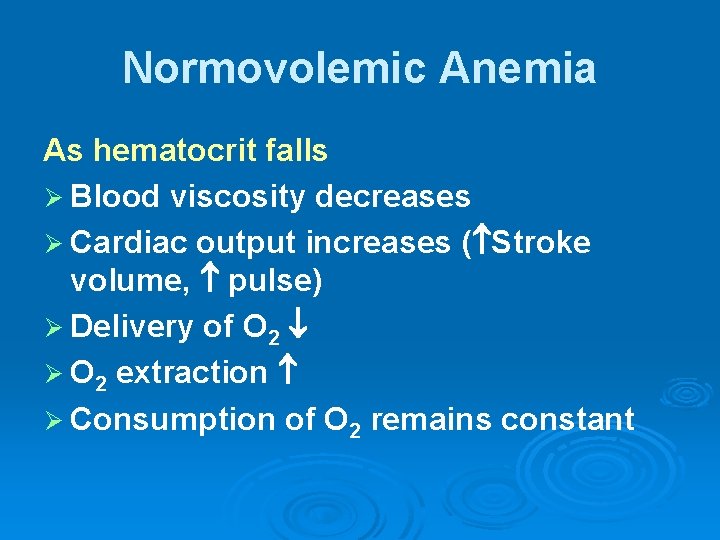
Normovolemic Anemia As hematocrit falls Ø Blood viscosity decreases Ø Cardiac output increases ( Stroke volume, pulse) Ø Delivery of O 2 Ø O 2 extraction Ø Consumption of O 2 remains constant

Limits of Compensation At very low hemoglobin levels (approximately 4 g/d. L) Ø O 2 delivery does not meet demand Ø Anerobic metabolism lactic acidosis cardiac arrest
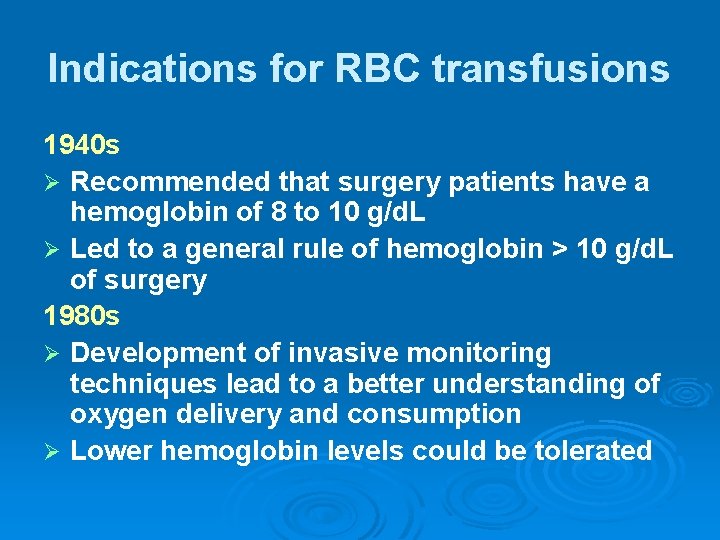
Indications for RBC transfusions 1940 s Ø Recommended that surgery patients have a hemoglobin of 8 to 10 g/d. L Ø Led to a general rule of hemoglobin > 10 g/d. L of surgery patients 1980 s Ø Development of invasive monitoring techniques lead to a better understanding of oxygen delivery and consumption Ø Lower hemoglobin levels could be tolerated
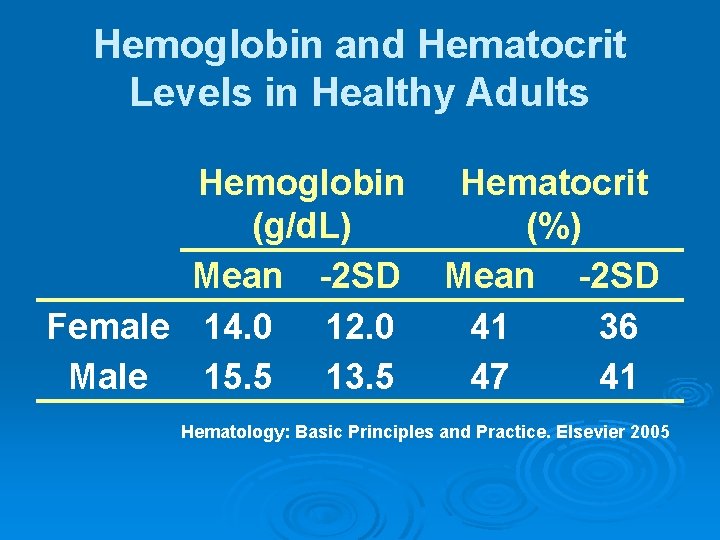
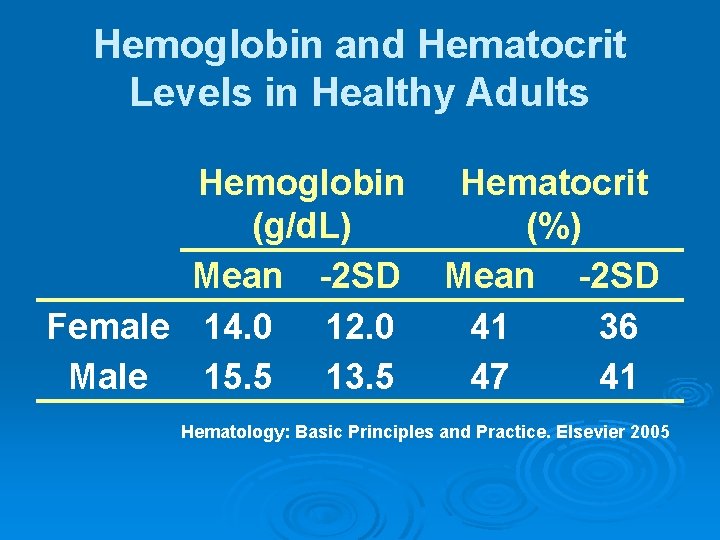
Hemoglobin and Hematocrit Levels in Healthy Adults Hemoglobin (g/d. L) Mean -2 SD Female 14. 0 12. 0 Male 15. 5 13. 5 Hematocrit (%) Mean -2 SD 41 36 47 41 Hematology: Basic Principles and Practice. Elsevier 2005
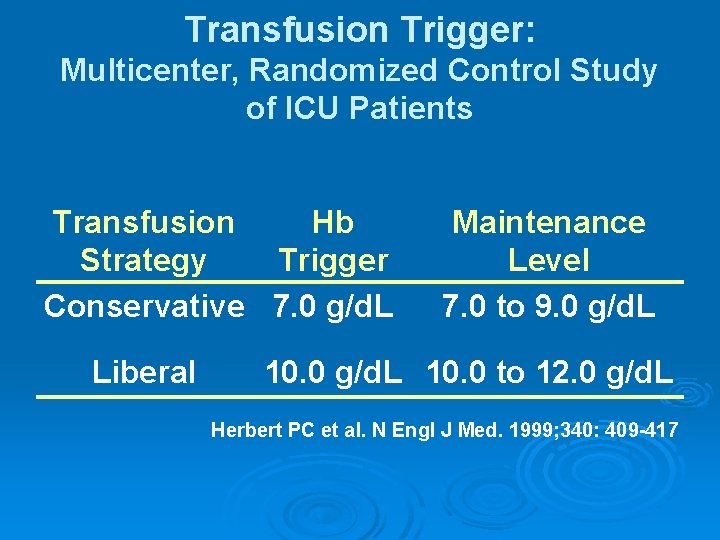
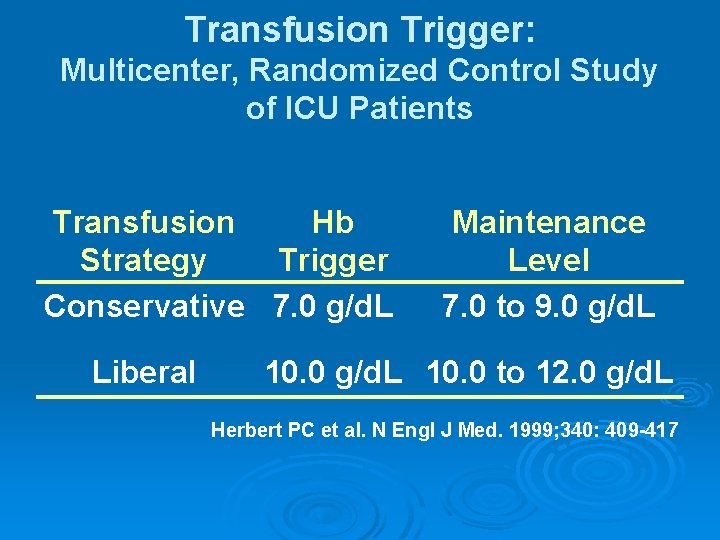
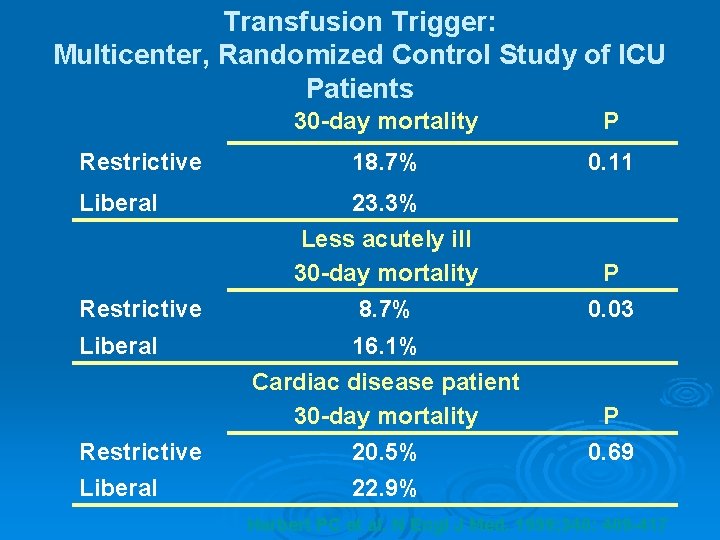
Transfusion Trigger: Multicenter, Randomized Control Study of ICU Patients Transfusion Hb Strategy Trigger Conservative 7. 0 g/d. L Liberal Maintenance Level 7. 0 to 9. 0 g/d. L 10. 0 to 12. 0 g/d. L Herbert PC et al. N Engl J Med. 1999; 340: 409 -417
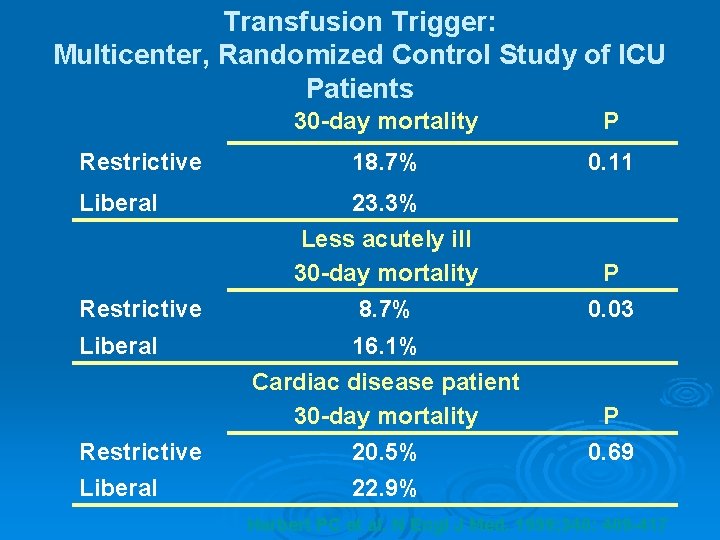
Transfusion Trigger: Multicenter, Randomized Control Study of ICU Patients 30 -day mortality P Restrictive 18. 7% 0. 11 Liberal 23. 3% Less acutely ill 30 -day mortality P Restrictive 8. 7% 0. 03 Liberal 16. 1% Cardiac disease patient 30 -day mortality P Restrictive 20. 5% 0. 69 Liberal 22. 9% Herbert PC et al. N Engl J Med. 1999; 340: 409 -417
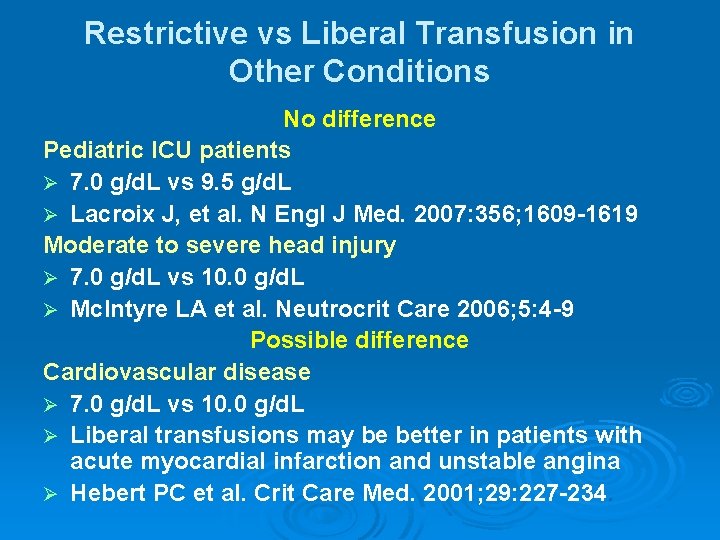
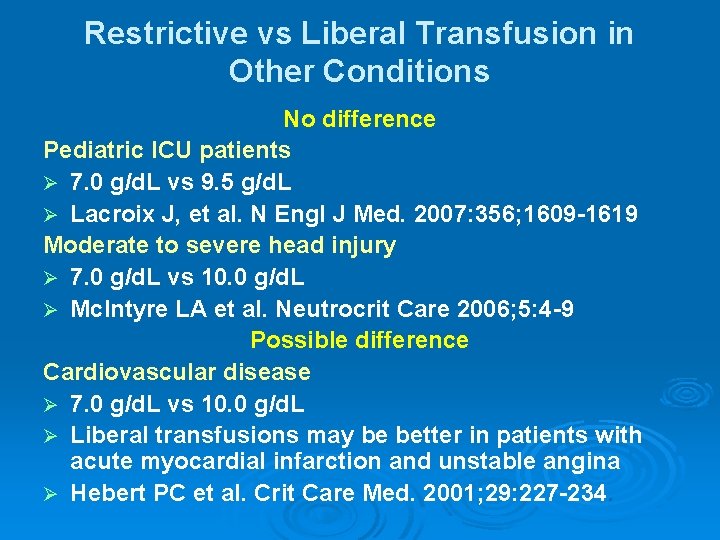
Restrictive vs Liberal Transfusion in Other Conditions No difference Pediatric ICU patients Ø 7. 0 g/d. L vs 9. 5 g/d. L Ø Lacroix J, et al. N Engl J Med. 2007: 356; 1609 -1619 Moderate to severe head injury Ø 7. 0 g/d. L vs 10. 0 g/d. L Ø Mc. Intyre LA et al. Neutrocrit Care 2006; 5: 4 -9 Possible difference Cardiovascular disease Ø 7. 0 g/d. L vs 10. 0 g/d. L Ø Liberal transfusions may be better in patients with acute myocardial infarction and unstable angina Ø Hebert PC et al. Crit Care Med. 2001; 29: 227 -234.
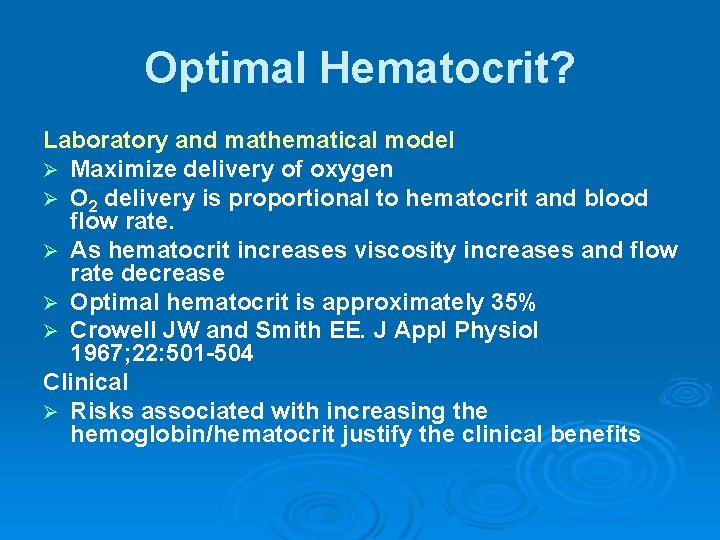
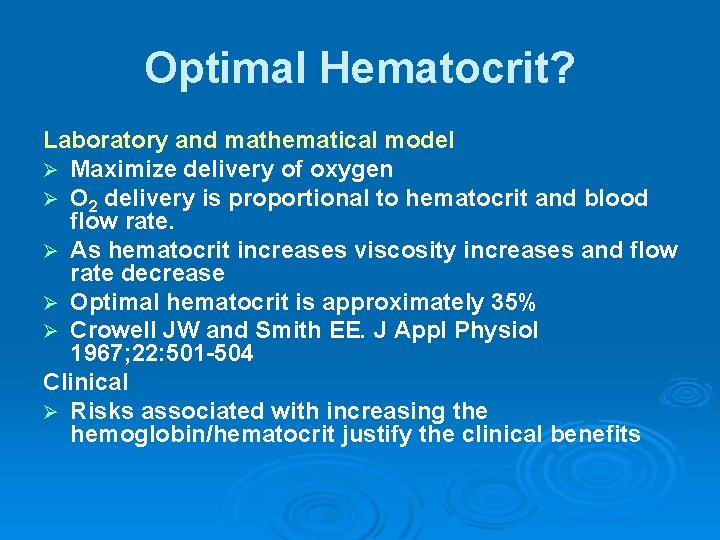
Optimal Hematocrit? Laboratory and mathematical model Ø Maximize delivery of oxygen Ø O 2 delivery is proportional to hematocrit and blood flow rate. Ø As hematocrit increases viscosity increases and flow rate decrease Ø Optimal hematocrit is approximately 35% Ø Crowell JW and Smith EE. J Appl Physiol 1967; 22: 501 -504 Clinical Ø Risks associated with increasing the hemoglobin/hematocrit justify the clinical benefits
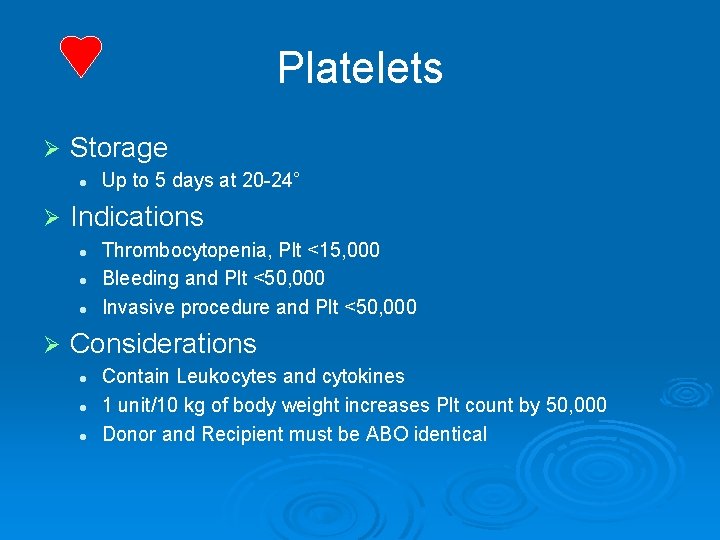
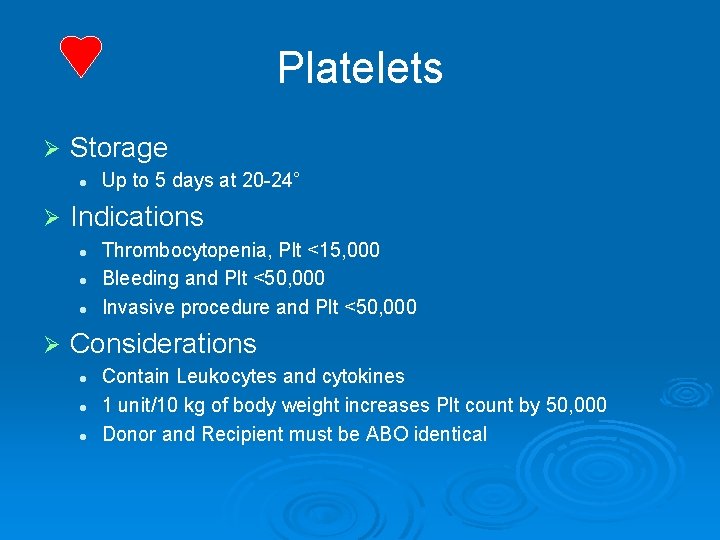
Platelets Ø Storage l Ø Indications l l l Ø Up to 5 days at 20 -24° Thrombocytopenia, Plt <15, 000 Bleeding and Plt <50, 000 Invasive procedure and Plt <50, 000 Considerations l l l Contain Leukocytes and cytokines 1 unit/10 kg of body weight increases Plt count by 50, 000 Donor and Recipient must be ABO identical
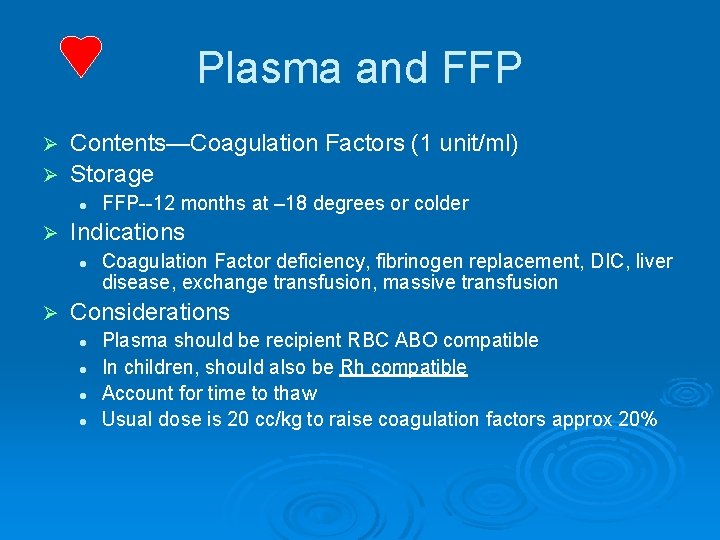
Plasma and FFP Contents—Coagulation Factors (1 unit/ml) Ø Storage Ø l Ø Indications l Ø FFP--12 months at – 18 degrees or colder Coagulation Factor deficiency, fibrinogen replacement, DIC, liver disease, exchange transfusion, massive transfusion Considerations l l Plasma should be recipient RBC ABO compatible In children, should also be Rh compatible Account for time to thaw Usual dose is 20 cc/kg to raise coagulation factors approx 20%

Cryoprecipitate Ø Description l Ø Storage l Ø After collection, refrozen and stored up to 1 year at -18° Indication l l Ø Precipitate formed/collected when FFP is thawed at 4° Fibrinogen deficiency or dysfibrinogenemia von. Willebrands Disease Factor VIII or XIII deficiency DIC (not used alone) Considerations l l ABO compatible preferred (but not limiting) Usual dose is 1 unit/5 -10 kg of recipient body weight
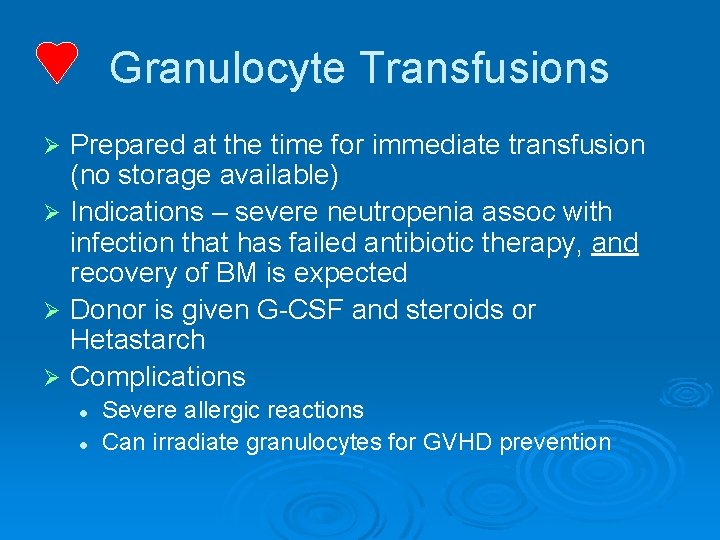
Granulocyte Transfusions Prepared at the time for immediate transfusion (no storage available) Ø Indications – severe neutropenia assoc with infection that has failed antibiotic therapy, and recovery of BM is expected Ø Donor is given G-CSF and steroids or Hetastarch Ø Complications Ø l l Severe allergic reactions Can irradiate granulocytes for GVHD prevention
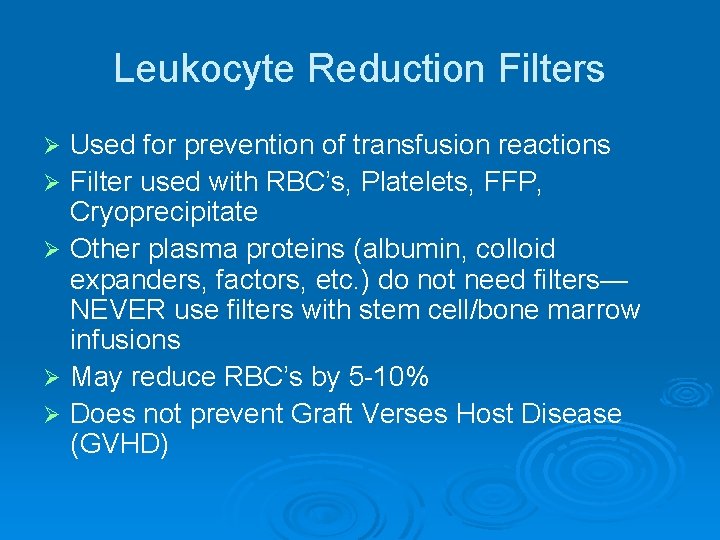
Leukocyte Reduction Filters Ø Ø Ø Used for prevention of transfusion reactions Filter used with RBC’s, Platelets, FFP, Cryoprecipitate Other plasma proteins (albumin, colloid expanders, factors, etc. ) do not need filters— NEVER use filters with stem cell/bone marrow infusions May reduce RBC’s by 5 -10% Does not prevent Graft Verses Host Disease (GVHD)
RBC Transfusions Preparations Ø Type l Ø Screen l l Ø Typing of RBC’s for ABO and Rh are determined for both donor and recipient Screen RBC’s for atypical antibodies Approx 1 -2% of patients have antibodies Crossmatch l Donor cells and recipient serum are mixed and evaluated for agglutination
RBC Transfusions Administration Ø Dose l l Ø Procedure l l Ø Usual dose of 10 cc/kg infused over 2 -4 hours Maximum dose 15 -20 cc/kg can be given to hemodynamically stable patient May need Premedication (Tylenol and/or Benadryl) Filter use—routinely leukodepleted Monitoring—VS q 15 minutes, clinical status Do NOT mix with medications Complications l l Rapid infusion may result in Pulmonary edema Transfusion Reaction

Platelet Transfusions Preparations Ø ABO antigens are present on platelets l l Ø ABO compatible platelets are ideal This is not limiting if Platelets indicated and type specific not available Rh antigens are not present on platelets l Note: a few RBC’s in Platelet unit may sensitize the Rh- patient
Platelet Transfusions Administration Ø Dose l l l Ø Procedure l l l Ø May be given as single units or as apheresis units Usual dose is approx 4 units/m 2—in children using 1 -2 apheresis units is ideal 1 apheresis unit contains 6 -8 Plt units (packs) from a single donor Should be administered over 20 -40 minutes Filter use Premedicate if hx of Transfusion Reaction Complications—Transfusion Reaction
Conclusions Ø Although RBCs are much safer than 20 years ago, transfusion practices have become more restrictive Ø The transfusion threshold at most institutions is a hemoglobin of 7 to 8 g/d. L for most patients Ø Higher thresholds are used for specific patients

TRANSFUSION REACTIONS
Transfusion Reactions are… Adverse reactions associated with the transfusion of blood and its components
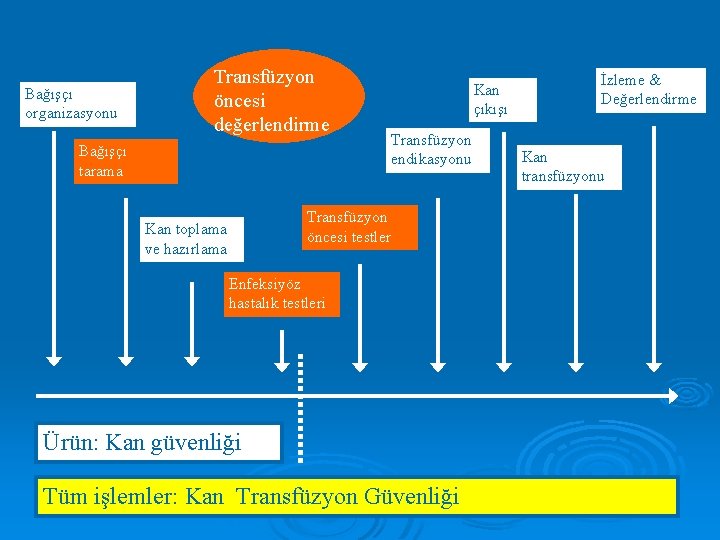
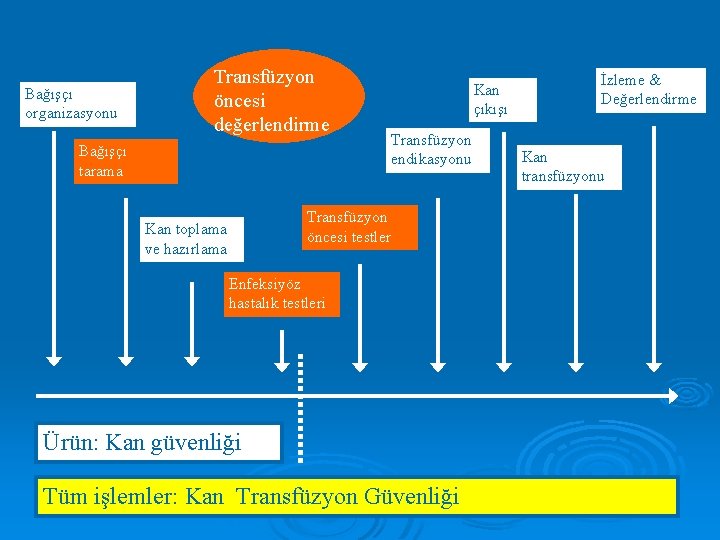
Bağışçı organizasyonu Transfüzyon öncesi değerlendirme Bağışçı tarama Kan çıkışı Transfüzyon endikasyonu Transfüzyon öncesi testler Kan toplama ve hazırlama Enfeksiyöz hastalık testleri Ürün: Kan güvenliği Tüm işlemler: Kan Transfüzyon Güvenliği İzleme & Değerlendirme Kan transfüzyonu
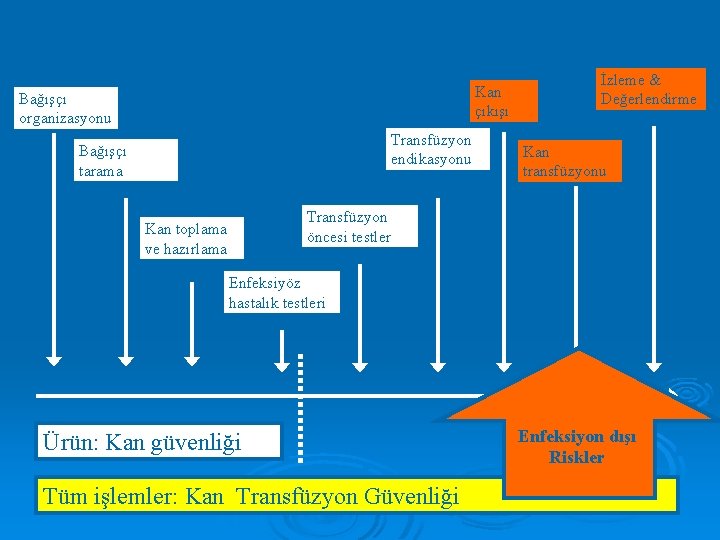
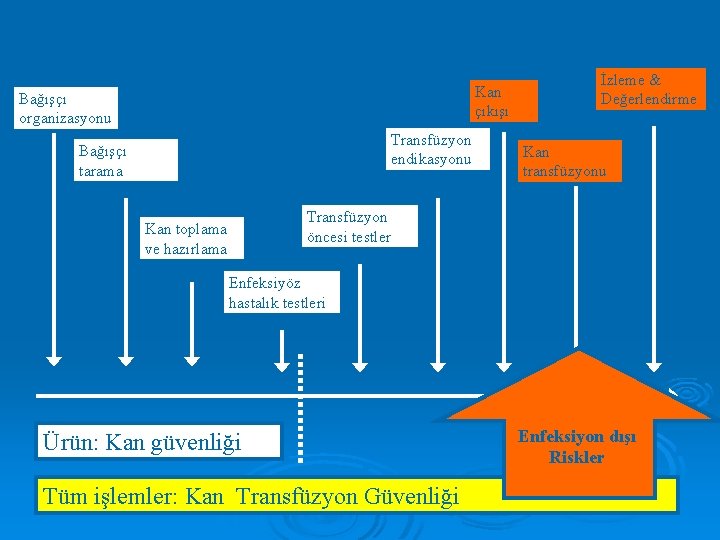
Kan çıkışı Bağışçı organizasyonu Transfüzyon endikasyonu Bağışçı tarama İzleme & Değerlendirme Kan transfüzyonu Transfüzyon öncesi testler Kan toplama ve hazırlama Enfeksiyöz hastalık testleri Ürün: Kan güvenliği Tüm işlemler: Kan Transfüzyon Güvenliği Enfeksiyon dışı Riskler
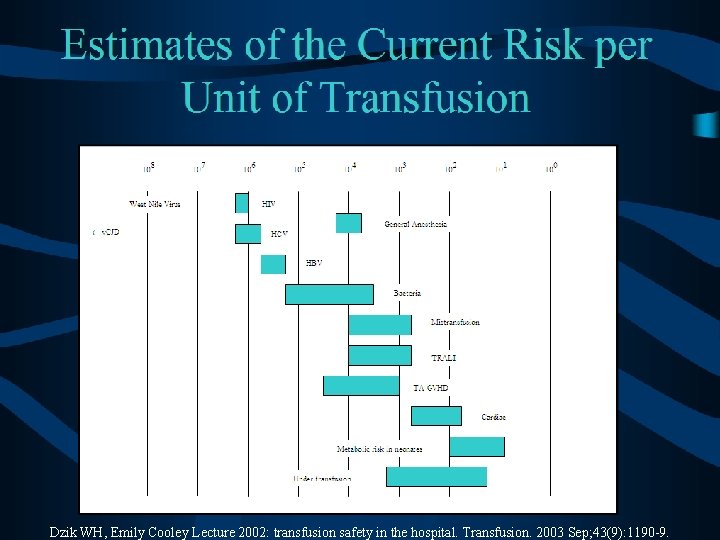
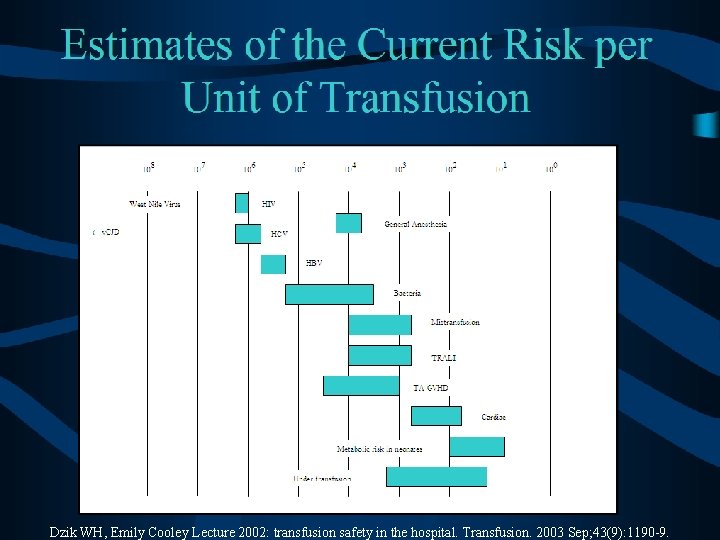
Dzik WH, Emily Cooley Lecture 2002: transfusion safety in the hospital. Transfusion. 2003 Sep; 43(9): 1190 -9.
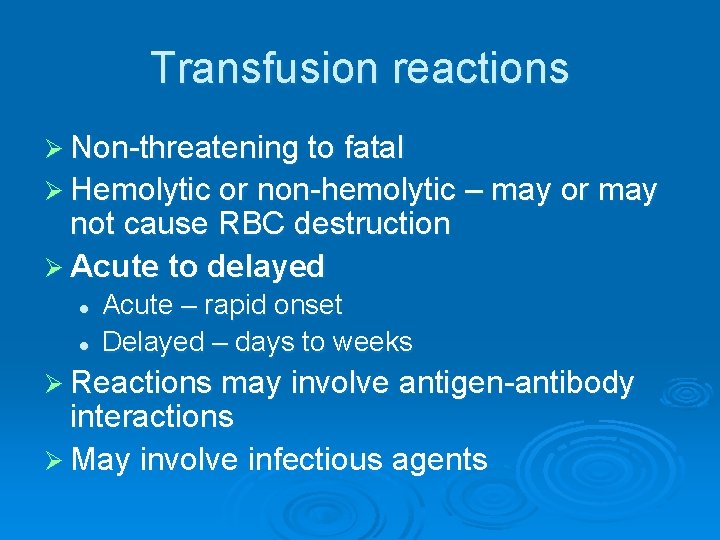
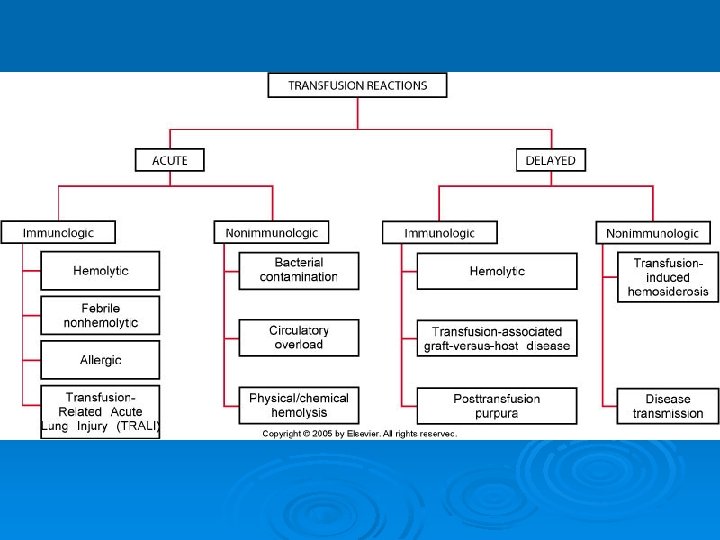
Transfusion reactions Ø Non-threatening to fatal Ø Hemolytic or non-hemolytic – may or may not cause RBC destruction Ø Acute to delayed l l Acute – rapid onset Delayed – days to weeks Ø Reactions may involve antigen-antibody interactions Ø May involve infectious agents
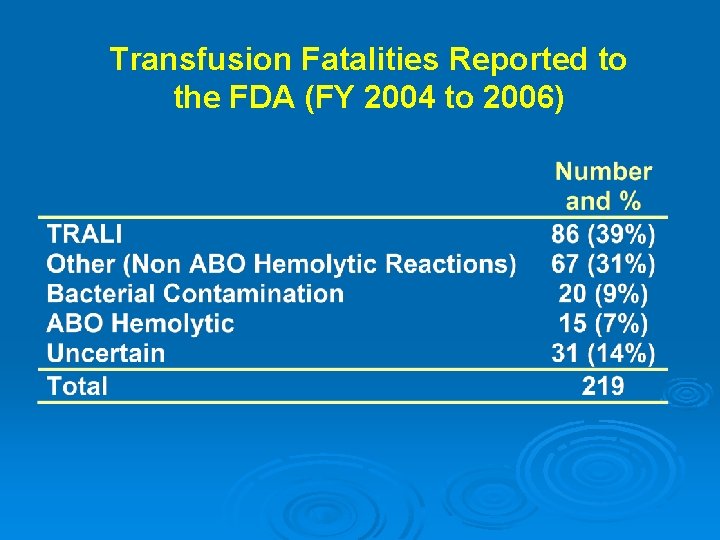
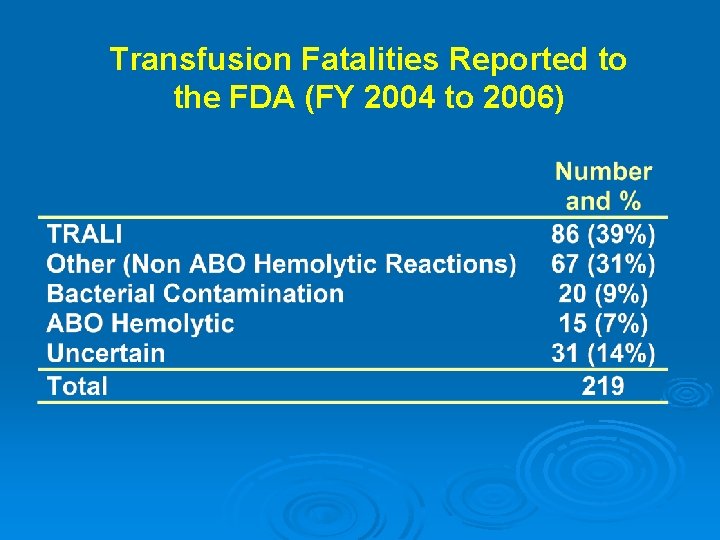
Transfusion Fatalities Reported to the FDA (FY 2004 to 2006)
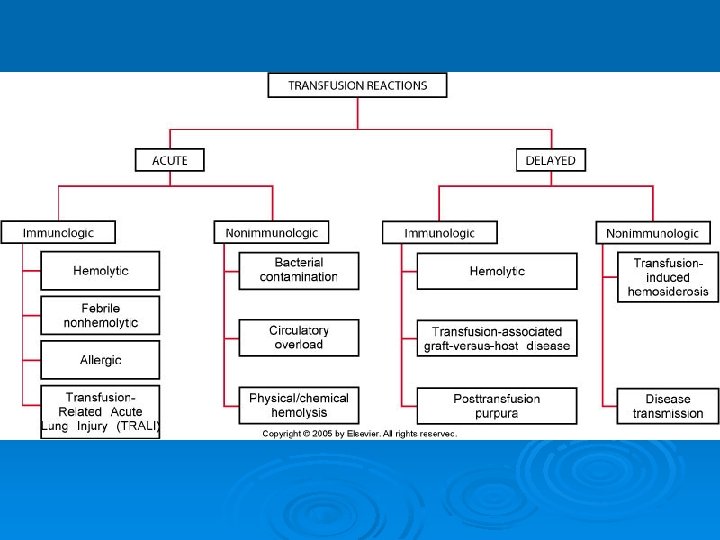
Acute Immunologic Reactions
Hemolytic Transfusion Reactions (HTR) Ø Most common cause is ABO incompatibility (clerical error) Ø Red cell destruction due to complement activation by Ig. M (within 24 hours) Ø As little as 10 -15 m. L can trigger a reaction
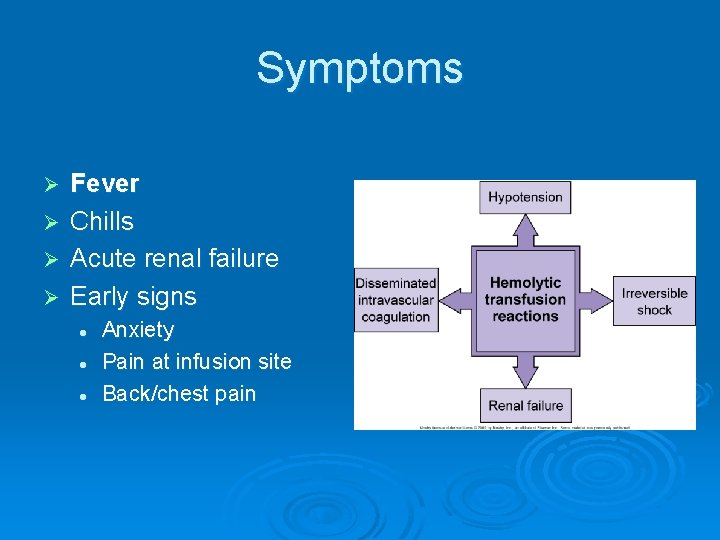
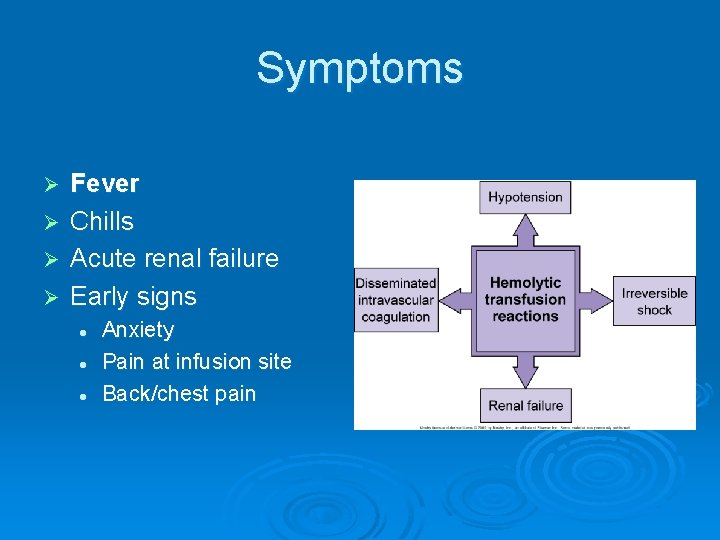
Symptoms Ø Ø Fever Chills Acute renal failure Early signs l l l Anxiety Pain at infusion site Back/chest pain
HTR maintenance Ø To prevent renal failure, fluids (saline) are infused along with diuretics (furosemide) to increase urine output Ø How do you prevent HTR? l l Follow the standard operating procedures (SOPs) to avoid errors Perform pretransfusion compatibility testing
Febrile Nonhemolytic Reactions Ø Ø Ø Caused from HLAs or leukocyte antigens on the WBCs of the donor that react with the recipient antibody Any component that contains WBCs could cause FNHTRs Raises temperature >1°C (fever) Antipyretics are used to treat fever or are given as a preventive measure Aspirin not used because of its effect on platelet function Leukocyte reduced units may also be given
Allergic Transfusion Reactions May be caused by antibodies (recipient) to plasma proteins (donor) Ø A mild transfusion reaction that causes: Ø l l l Urticaria: hives Erythema: redness of the skin Dyspnea: shortness of breath An antihistamine can be given prior to transfusion or during transfusion Ø Not life threatening Ø
Anaphylactic Reactions May be associated with Ig. A antibodies Ø Very severe & life threatening reaction although rare Ø Symptoms: Ø l l Ø NO fever Skin flushing Nausea Diarrhea Hypotension Cardiac arrhythmia Cardiac arrest Laryngeal edema Treated with epinephrine (vasoconstrictor & bronchiole dilator)
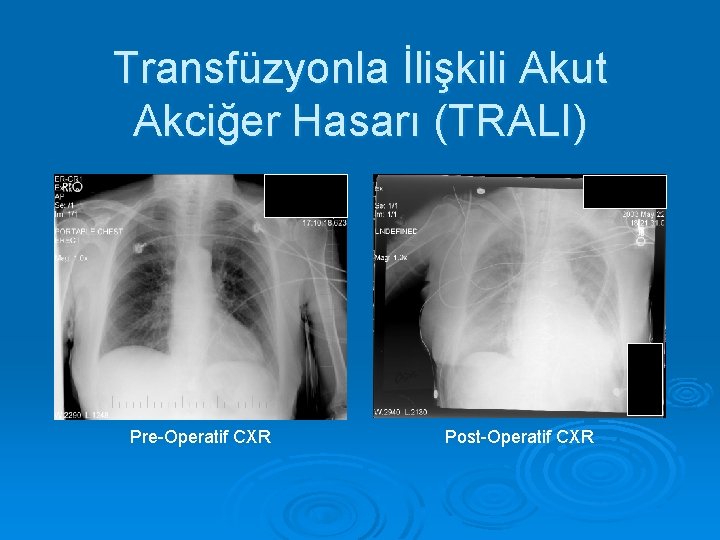
Transfusion Related Lung Injury Ø Ø Ø TRALI Caused by donor antibodies that react with the recipient’s granulocytes or vice versa The lungs fill with a high-protein fluid Patient displays acute respiratory insufficiency with x-ray showing bilateral symmetric pulmonary edema Dyspnea, cyanosis, tachycardia, and hypoxemia
TRALI Ø 1 in 5, 000 transfusions Ø Symptoms occur within 2 hours and may end in 2 -4 days if treated Ø Treated with IV steroids, although they may not work well Ø Prevention: l Avoid donations from multiparous women and those who have received multiple transfusions
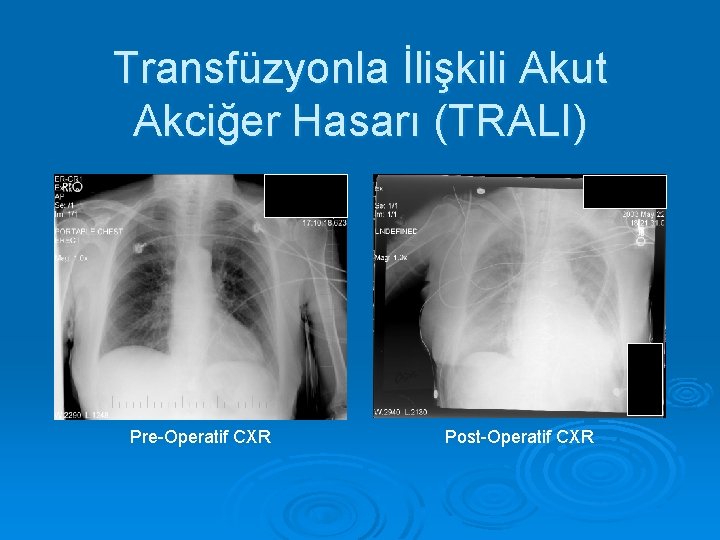
Transfüzyonla İlişkili Akut Akciğer Hasarı (TRALI) Pre-Operatif CXR Post-Operatif CXR

Acute Non-immunologic Reactions

Bacterial Contamination Ø Ø Ø One of the more common reactions Does not involve antigen-antibody interactions Results from bacterial contamination of blood products l l Yersinia enterocolitica Serratia liquifaciens Symptoms include fever, shock, & renal dysfunction (due to endotoxins) Ø Stop immediately and treat with antibiotics Ø l Hypotension can be treated with vasopressors
Circulatory Overload Occurs when a patient is transfused too rapidly, overloading the cardiopulmonary system (too much fluid at one time) Ø Symptoms Ø l l Cyanosis Dyspnea Severe headache Congestive Heart Failure (CHF) Place patient in upright position Ø Give patients small aliquots of each unit over time to prevent reaction Ø

Delayed Immunologic Reactions
Delayed Hemolytic Transfusion Reactions Ø DHTRs occur at least 24 hrs after transfusion Ø Mediated by Ig. G antibodies l l Patient previously exposed to RBC antigen and has low antibody titer until exposed again Rh, Kidd, Duffy, and Kell Ø DAT negative at first, but becomes + Ø Elutions are performed to identify Ab
DHTRs Ø Symptoms include: l l l Fever Gradual Hemoglobin Fever Jaundice Hemoglobinuria Ø Must give antigen negative blood
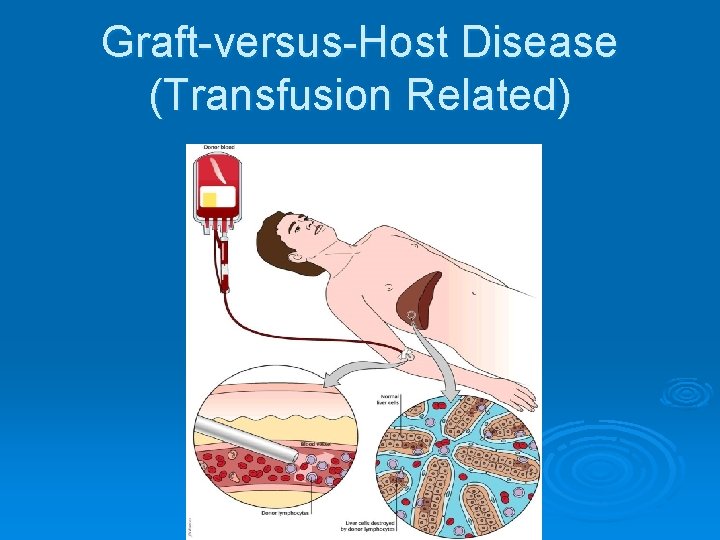
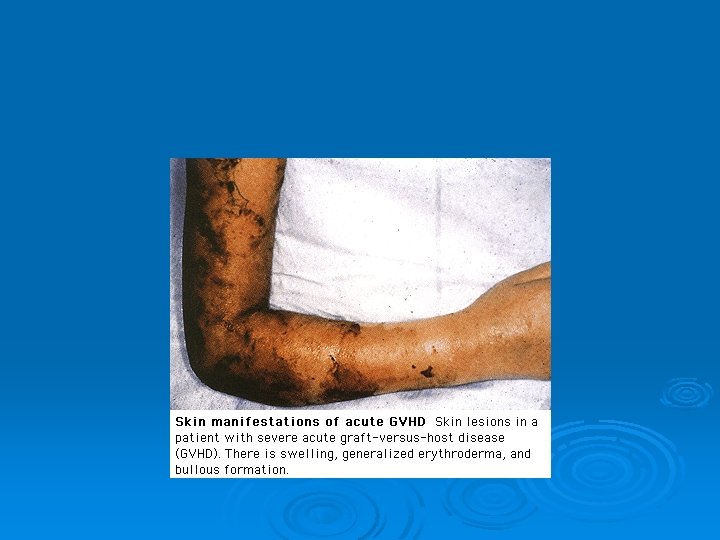
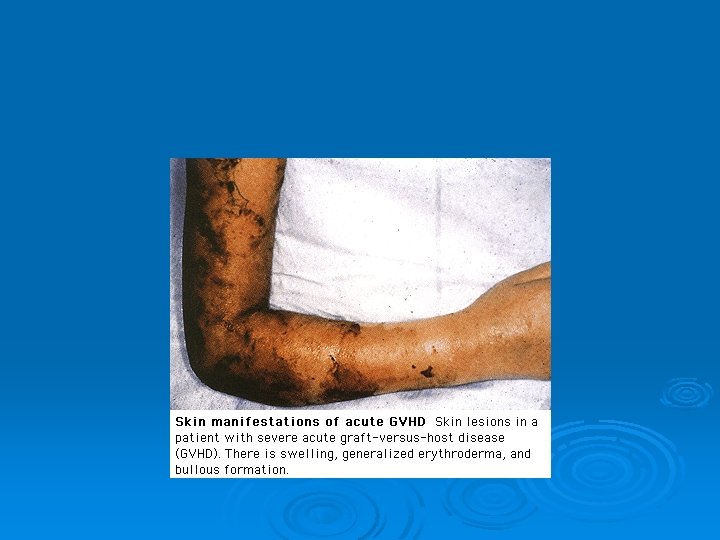
Graft-versus-Host Disease (Transfusion Related) Rare but fatal condition that has a 90% mortality rate Symptoms appear after about 12 days May be caused by donor lymphocytes transfused into an immunocompromised recipient Ø Pancytopenia occurs as a result of the immunologic response Ø Any components that contain T-lymphocytes should be irradiated to prevent GVHD Ø Ø Ø
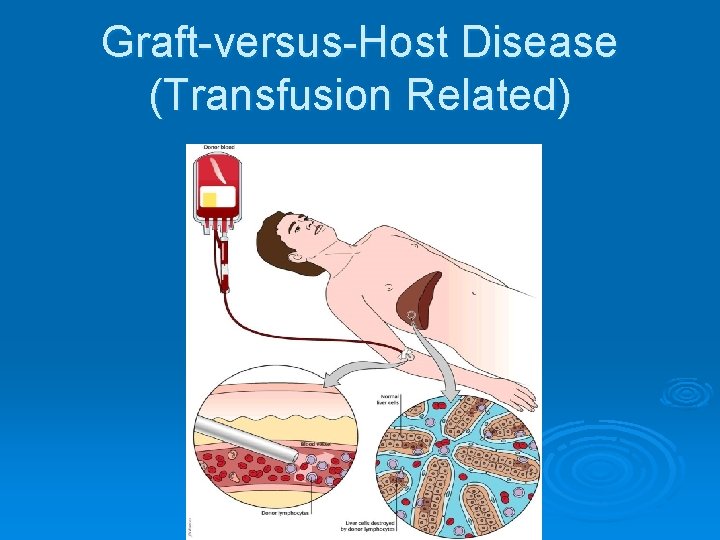
Graft-versus-Host Disease (Transfusion Related)
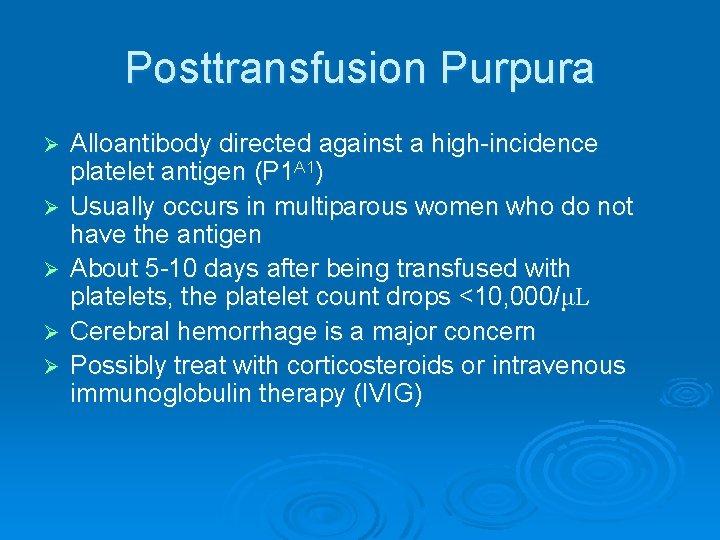
Posttransfusion Purpura Ø Ø Ø Alloantibody directed against a high-incidence platelet antigen (P 1 A 1) Usually occurs in multiparous women who do not have the antigen About 5 -10 days after being transfused with platelets, the platelet count drops <10, 000/μL Cerebral hemorrhage is a major concern Possibly treat with corticosteroids or intravenous immunoglobulin therapy (IVIG)

Delayed Nonimmunologic Reactions
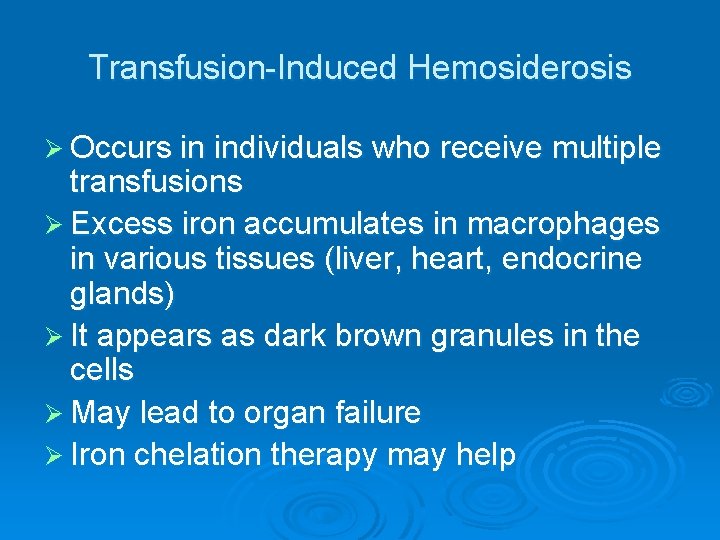
Transfusion-Induced Hemosiderosis Ø Occurs in individuals who receive multiple transfusions Ø Excess iron accumulates in macrophages in various tissues (liver, heart, endocrine glands) Ø It appears as dark brown granules in the cells Ø May lead to organ failure Ø Iron chelation therapy may help
Disease Transmission Ø Hepatitis Ø HIV Ø HTLV Ø Cytomegalovirus Ø Malaria Ø Babesiosis Ø Syphilis
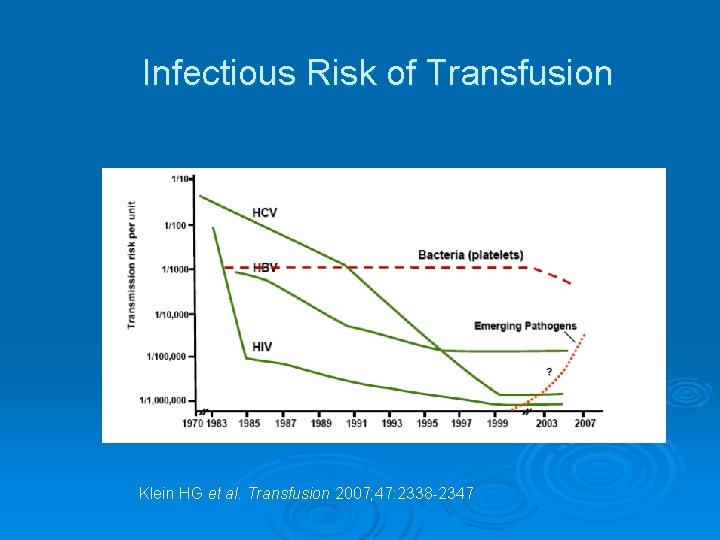
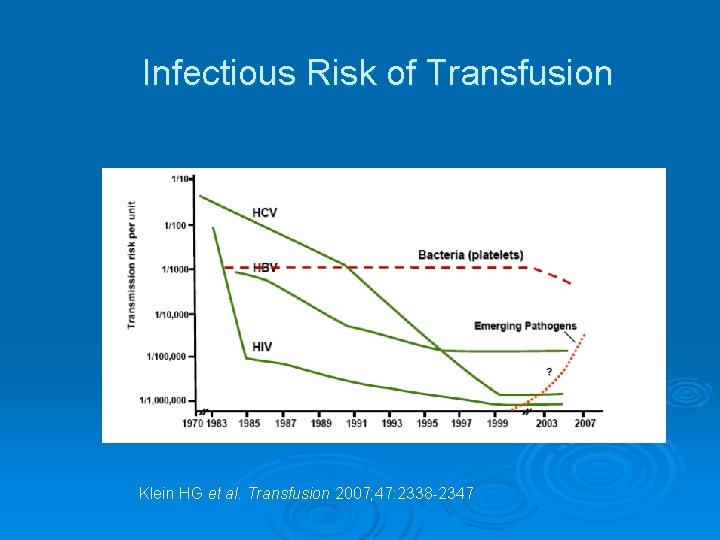
Infectious Risk of Transfusion Klein HG et al. Transfusion 2007; 47: 2338 -2347

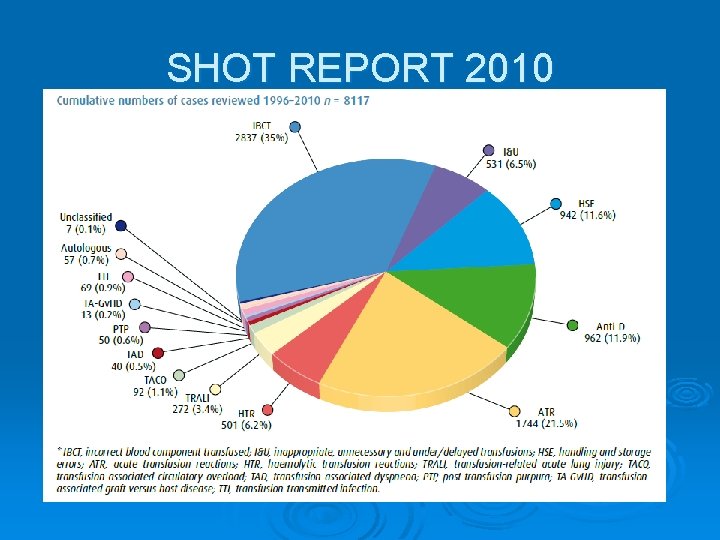
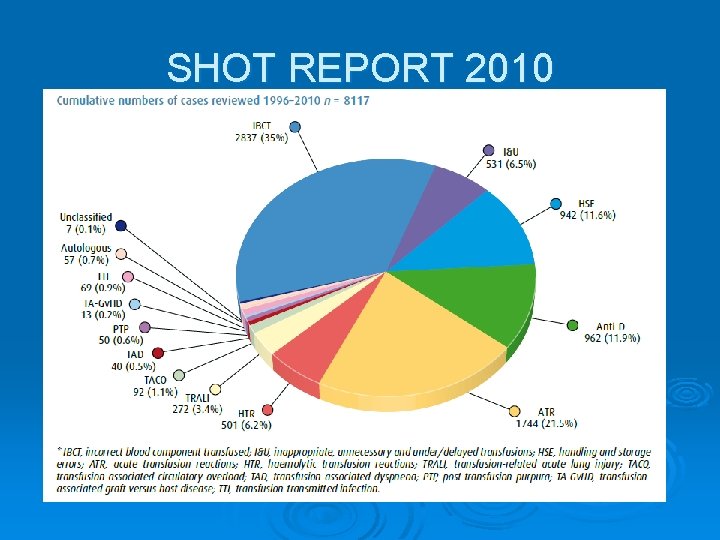
SHOT REPORT 2010

SHOT REPORT 2010

SHOT REPORT 2010 (definite)
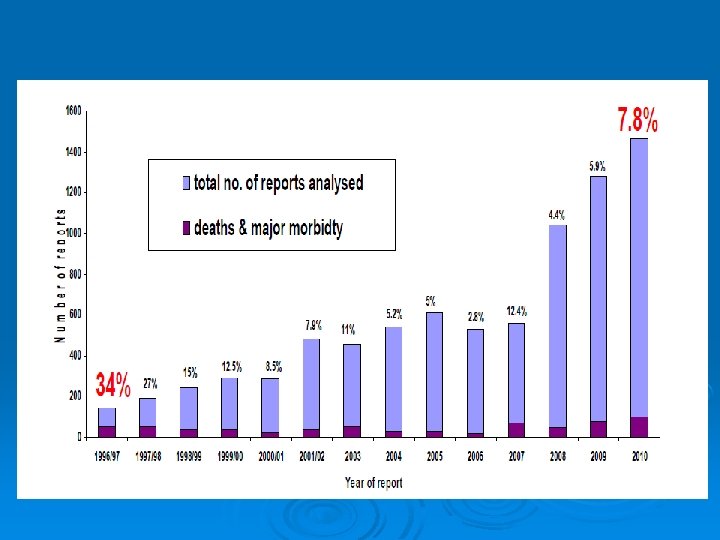
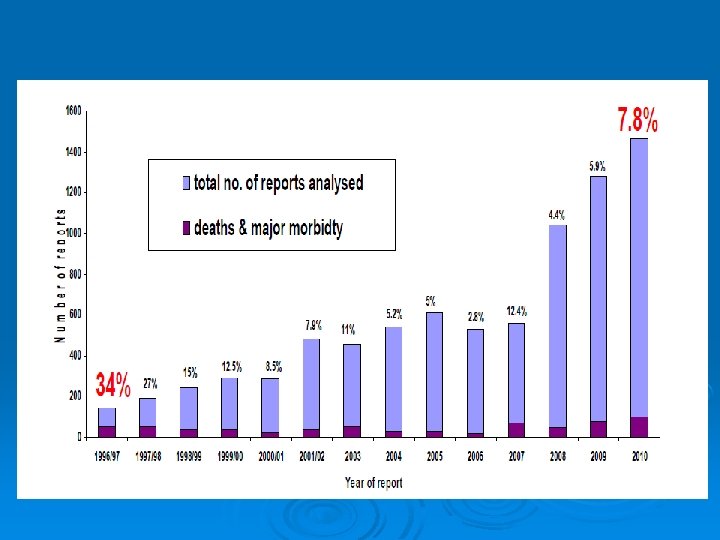
DEATHS AND MAJOR MORBIDITY

SHOT REPORT 2010



 Indication of transfusion
Indication of transfusion Platelet concentrate
Platelet concentrate Blood transfusion indications
Blood transfusion indications Blood transfusion indications
Blood transfusion indications Indications for blood transfusion
Indications for blood transfusion Cryoprecipetate
Cryoprecipetate Cryoprecipitate dose
Cryoprecipitate dose Platelets transfusion indication
Platelets transfusion indication When to transfuse blood
When to transfuse blood Filiz bakar ateş
Filiz bakar ateş Coadsys exam yeditepe
Coadsys exam yeditepe Coadsys exam
Coadsys exam Meral yılmaz öğretmen
Meral yılmaz öğretmen Pınar seden meral
Pınar seden meral Meral güneş ergin
Meral güneş ergin Meral dogan
Meral dogan Protokol sıralaması
Protokol sıralaması Lugol
Lugol Indications of a chemical reaction
Indications of a chemical reaction Indications of chemical reactions
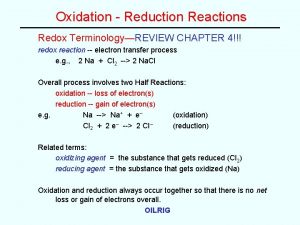
Indications of chemical reactions Chemical reactions section 2 classifying chemical reactions
Chemical reactions section 2 classifying chemical reactions Example of redox reaction
Example of redox reaction Section 2 classifying chemical reactions worksheet answers
Section 2 classifying chemical reactions worksheet answers Types of reactions
Types of reactions Chemistry unit 5 reactions balancing reactions worksheet
Chemistry unit 5 reactions balancing reactions worksheet Blood transfusion complications
Blood transfusion complications Complications of blood transfusion
Complications of blood transfusion Tpn and blood transfusion compatibility
Tpn and blood transfusion compatibility Hemolytic transfusion reaction
Hemolytic transfusion reaction Transfusion en urgence vitale immédiate
Transfusion en urgence vitale immédiate Rational use of blood
Rational use of blood Blood transfusion requirements
Blood transfusion requirements Chonicu
Chonicu Twin-twin transfusion syndrome
Twin-twin transfusion syndrome Double volume exchange transfusion
Double volume exchange transfusion Massive transfusion complication
Massive transfusion complication Transfusion plaquetas indicaciones
Transfusion plaquetas indicaciones Complication of blood transfusion
Complication of blood transfusion Blood transfusion requirements
Blood transfusion requirements Fresh frozen plasma transfusion time
Fresh frozen plasma transfusion time Iv gauge sizes
Iv gauge sizes What are the complications of blood transfusion
What are the complications of blood transfusion Abo system of blood grouping
Abo system of blood grouping Blood group percentage in india
Blood group percentage in india Fresh frozen plasma contents
Fresh frozen plasma contents Hemolytic transfusion reaction
Hemolytic transfusion reaction Compatibilité transfusion plaquettes
Compatibilité transfusion plaquettes Nursing responsibility in blood transfusion
Nursing responsibility in blood transfusion Blood transfusion in children
Blood transfusion in children Coconut water transfusion
Coconut water transfusion Mtp template
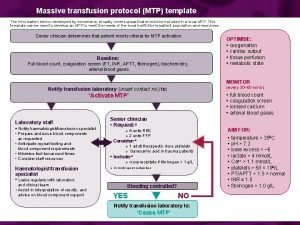
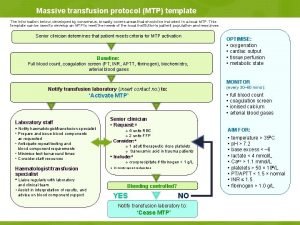
Mtp template Abo compatibility test
Abo compatibility test Blood transfusion
Blood transfusion Transfusion reaction
Transfusion reaction Blood transfusion
Blood transfusion Whats a platelet transfusion
Whats a platelet transfusion Factor goteo
Factor goteo Test de beth vincent interprétation
Test de beth vincent interprétation Trali symptoms
Trali symptoms Ffp
Ffp Super transfusion
Super transfusion Transfusion trigger
Transfusion trigger Specimen identification
Specimen identification Breast milk jaundice slideshare
Breast milk jaundice slideshare Haivn
Haivn Mtp template
Mtp template Faranoush
Faranoush Transfusion sanguine
Transfusion sanguine Responsabilité ide
Responsabilité ide Name that
Name that Blood transfusion steps nclex
Blood transfusion steps nclex Pit and fissure definition
Pit and fissure definition Classification of space maintainers
Classification of space maintainers Different types of position in nursing
Different types of position in nursing Transpalatal arch space maintainer
Transpalatal arch space maintainer Contraindications of removable partial denture
Contraindications of removable partial denture Lma indication
Lma indication Questionable abutments in fpd
Questionable abutments in fpd Colostomy care contraindication
Colostomy care contraindication Counter bevel onlay
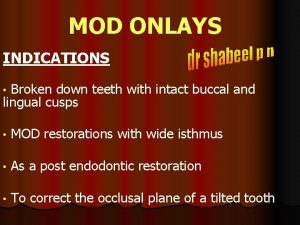
Counter bevel onlay Contraindications of tooth extraction
Contraindications of tooth extraction Absolute contraindications of tooth extraction
Absolute contraindications of tooth extraction Whats a cpm machine
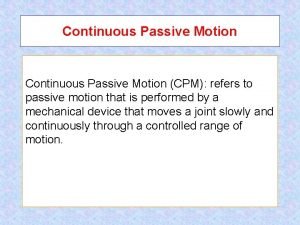
Whats a cpm machine Continuous passive motion indications and contraindications
Continuous passive motion indications and contraindications Indications and appellations of origin
Indications and appellations of origin