Northside Hospital Student Orientation Welcome We are so





- Slides: 163
Northside Hospital Student Orientation
Welcome!! We are so happy to have you as part of our team! We hope that your experience at Northside Hospital will be a valuable stepping stone in your career!
Purpose Of This Presentation • Introduce Northside Hospital services • Ensure accurate completion of required paperwork • Provide information regarding key policy & procedural issues
About Northside Hospital • Sandy Springs location opened in 1970, presently a 444 bed full service hospital • Forsyth location in Cumming, GA acquired 2002, presently a 78 bed hospital & growing • Cherokee location in Canton, GA licensed for 84 beds • All are not-for profit community hospitals • Named Atlanta’s “Most Preferred Hospital” since 1997 by the National Research Corporation
Proud To Serve. . . • Women’s Services--Obstetrics & GYN • Oncology Programs--Bone Marrow, Leukemia, Breast & GYN cancers • Surgical Services • Radiology Services • Emergency Services • Cardiology • Medical/Surgical • Critical Care • Pharmacy
Core Values At Northside • • • Dignity Respect Pride Warmth Caring
Forms • The forms on this website must be completed at the time of Orientation, signed, dated & returned to instructor before your arrival at any Northside Hospital campus – Acknowledgement and Release Form – Health History • All questions must be answered in #6 (TB skin test) & #7 (Rubella)
Name Badge • Our policy requires that you wear your name badge AT ALL TIMES while you are on the Northside Hospital Campus • Name badge--school issued, photo ID • You will also be issued a Northside Hospital name badge, identifying the unit/ department in which you will be doing your clinical experience
Dining At Northside • Two food services on main campus – Mc. Donald’s – Morrison’s • 30% discount with your name badge – Morrison’s: when open (6: 30 AM - 7 PM) – Mc. Donald’s: only when Morrison’s is closed • Northside Forsyth & Northside Cherokee cafeterias offer students a 20% discount
Parking At Northside Facilities • Parking at the main hospital is available in the Women’s Center Deck on Hollis Cobb Drive directly opposite the Women’s Center • Enter the deck using a code (provided to your faculty member) or by taking parking ticket; show your student ID at attendant exit or use code at keypad exits for free parking • At Forsyth & Cherokee, use designated employee parking areas--no code required
Confidentiality • Critical to maintain because: – Protect the trust patients have in their health care providers – Requirement of Code of Ethics of various professions – Required by regulatory & accrediting organizations
Health Insurance Portability and Accountability Act…. . . HIPAA Enacted to ensure that personal medical information (shared with doctors, hospitals and others who provide and pay for healthcare) is protected. Establishes restrictions on uses and disclosures of personal health information. Allows patients enhanced protection and greater access to their medical records.
Protected Health Information (PHI) • Any patient’s health or personal information transmitted through oral, recorded, paper, or electronic means. Such as: – Patient name and address. – Social Security Number. – Medical records. – Billing information
Minimum Reporting Necessary • PHI is to only be used or disclosed when it is necessary to carry out a specific function. • This standard does not apply when PHI is used or disclosed for treatment purposes
Our Role for Privacy Notice • We are required to inform patients of how we, as a facility, use and disclose their PHI. • Patients must receive this notice on the date the first service is rendered. • The right to access and control the PHI of minors is left to the parents - except when state law overrides parental control.
Patients Have Rights To: • Restrict use and disclosure. (Although the provider, NSH, is not required to agree). • Designate an alternate means for communication with the patient (i. e. work number vs home number) • Inspect and amend their medical record or “state their part of the story”. • Request a history of non-routine disclosures for as far back as 6 years. • Contact the designated NSH privacy official with questions and breech of privacy complaints.
Tips On Confidentiality • Avoid using waiting areas to interview or brief patients or family members • Be mindful that there are often patients & family members on employee elevators, in hallways & in the cafeteria
Confidentiality & Technology • Prior to sending a fax, check with the charge nurse in the department to which you are assigned • When using a copier, don’t leave material unattended • Don’t use someone else’s username to access a system for any reason • Don’t leave computer displays showing confidential information--log-off when finished
Questions About Confidentiality Practices • Ask your preceptor or the charge nurse of the unit to which you are assigned • If you see or suspect a possible HIPAA Security or Privacy violation, call Northside’s HIPAA hotline: – (404) 845 -5534
Respect and Courtesy At Northside Hospital • Knock before entering • Introduce yourself before observing or initiating care in any setting

PATIENT’S RIGHTS AND RESPONSIBILITIES PARTNERING WITH OUR PATIENTS AND FAMILIES
Patient Rights • Patients have the right to privacy, confidentiality, ethics consultation, refusal of treatment, safety, interpretation when needed, assessment & management of pain and more • Patients have the right to speak to a Patient Representative to have complaints and or suggestions for improvement heard and the right for assistance with special needs, including interpretation services • For a complete listing of patients rights, see “Your Rights and Responsibilities as a Patient” fact sheet
Patient Responsibilities • Patient responsibilities include asking questions, providing accurate information, following treatment plans and more • Listed on the reverse side of “Your Rights and Responsibilities as a Patient” fact sheet
Patient Rights & Responsibilities • Northside encourages patients and families to be active members of their healthcare team in order to provide the highest quality of care • In keeping with this “partnership” philosophy, every patient that is admitted to Northside Hospital receives a written copy of their rights and responsibilities along with ways to help prevent medical errors (available in English and Spanish)
Patient Rights & Responsibilities • Other patients rights reference materials: – Patient/Family/Visitors Guides located in all patient rooms and patient access areas – Mosby’s Multicultural Reference Guide • Located on patient care units and in Health Resource Library – Multi-Faith Informational Manual • Located on patient care units and in Health Resource Library • Information regarding Northside’s Ethical Code of Conduct can be found in policy A-018
Other Supportive Services Available • • Patient Relations Interpretation Services Pastoral Care Check with the charge nurse for more information on utilization or how to access

DIVERSITY

DIVERSITY • Defined as “any collective mixture characterized by similarities and differences” • NSH is committed to creating an environment in which our patients’ cultural differences, beliefs and practices are respected
CULTURE • Defined as the dynamic pattern of learned behavior, values, beliefs and world view exhibited by groups that share history and geographic proximity • Transmitted through institutions of society (family, religion, educational systems, political systems, media) • Beliefs about the cause, prevention and treatment of illness vary among cultures
CULTURAL DIFFERENCES • • • Age Gender Educational background Experience Lifestyle Nationality Physical ability Race Religion
CULTURAL ASSESSMENT • Listen with sympathy & understanding to the patient’s perception of the problem • Explain your perceptions of the problem & your strategy for treatment • Acknowledge & discuss the differences & similarities between these perceptions • Recommend treatment while remembering the patient’s cultural parameters • Negotiate agreement
Avoid • Stereotyping: making broad statements/ assumptions based on membership in a group (“All _____ think this way”) • Ethnocentrism: belief in supremacy of one’s own ethnic group • Prejudice: biased or hostile attitudes or perceptions toward a person who belongs to a group simply because he/she belongs to that group
Culturally Sensitive Care • Become familiar with socioeconomic & demographic characteristics, belief systems & health behaviors of other culture • Apply cultural knowledge, behaviors & interpersonal & clinical skills that enhance your effectiveness in managing patient care
2005 NATIONAL PATIENT SAFETY GOALS
2005 NATIONAL PATIENT SAFETY GOALS • Goal I: Improve the accuracy of patient identification § Taking of Blood Samples or Other Specimens for Clinical Testing § Administration of Medications § Administration of Blood Products § Any Treatment or Procedure § NSH uses 2 identifiers--check with clinical resource to determine appropriate identifiers for procedure
2005 NATIONAL PATIENT SAFETY GOALS • Goal II: Improve the effectiveness of communication among caregivers – Do Not Use Abbreviations--refer to list on all charts & throughout departments – Verbal/Telephone Orders – Timeliness of reporting and receipt of critical test results and values
2005 NATIONAL PATIENT SAFETY GOALS • Goal III: Improve the safety of high-alert medications § Drug Concentration standardization § Removal of concentrated electrolytes from patient care areas § Annual review of look-alike/sound-alike drugs
2005 NATIONAL PATIENT SAFETY GOALS • Goal IV: Eliminate wrong site, wrong patient, wrong procedure surgery – Pre-operative Verification Process – Marking of site – Conduct a “time-out” immediately before starting the procedure • Goal V: Improve the safety of using infusion pumps § Ensure Free-flow protection
2005 NATIONAL PATIENT SAFETY GOALS • Goal VI: Improve the effectiveness of clinical alarm systems § Regular testing and maintenance is performed § Alarms are audible with respect to competing noises in unit • Goal VII: Reduce the risk of health careassociated infections – Comply with current CDC hand hygiene guidelines
2005 NATIONAL PATIENT SAFETY GOALS • Goal VIII: Accurately and completely reconcile medications across the continuum of care – Obtain and document complete list of patient’s medication upon admission – Communicate complete list of patient’s medications to next provider of service whether within or outside the organization
2005 NATIONAL PATIENT SAFETY GOALS • Goal IX: Reduce the risk of patient harm from falls – Assess and periodically reassess each patient’s risk for Falling, including the potential risk associated with Patient’s medication regimen
RISK MANAGEMENT
PURPOSE OF RISK MANAGEMENT • Identify, evaluate & reduce the risk of injury or loss to patients, staff members & the organization • Injury can be actual physical injury to a person or loss or damage to property, reputation or income • Early identification of injury or loss can prevent similar recurrences in the future
INCIDENT REPORTING • In your everyday contact with patients, you are in the best position to identify patient safety issues, unusual outcomes or injures • These are recorded on incident reports – Not to assign blame to to evaluate process involved – An opportunity to improve practice & quality of care
INCIDENT REPORTS • Factual statement • Gives account of what actually happened to a particular patient in a particular situation – Does not give opinions of what happened or why happened – Does not point fingers or assign blame – Is not part of Medical Record – Does not take the place of documentation in the Medical Record
IF YOU DISCOVER AN UNUSUAL OCCURRENCE • Report to charge nurse • Follow instructions for completion of Incident Report • Document incident in Medical Record in factual, concise way
IMPAIRED PROVIDERS
WHAT IS AN IMPAIRED PROVIDER? • A Physician or Affiliated Practitioner (CRNA, CNM, etc) whose ability or clinical judgment may be adversely altered because of § psychiatric or other medical conditions or § the use of alcohol or illegal drugs or § the use or abuse of prescribed drugs or OTC drugs § resulting in the inability to provide appropriate patient care, an immediate threat to the safety and welfare of patients and staff, or an inability to fulfill other duties or responsibilities.
TYPES OF HEALTH ISSUES THAT MAY RESULT IN IMPAIRMENT § Any disease that might impact manual dexterity, such as arthritis in a physician or other practitioner who performs procedures § Any situation that could slow response times or cloud decision making § Lack of sleep § Depression § Stress from divorce, problems with children, or family illness § Substance dependency or abuse
RECOGNIZING AN IMPAIRED PROVIDER--JOB PERFORMANCE § Agitation with questions regarding activities or care § Complaints from patients or families regarding care provided or unreasonable behavior during visits § Memory lapses or generalized forgetfulness, including forgotten verbal orders Alteration in clinical judgment (treatments/orders don’t fit the patient’s clinical situation) § Inappropriate medication orders or over prescribing medications § Decreased quality of medical record documentation § Delays in returning pages/calls or inappropriate response to calling § Making rounds in “off hours”
RECOGNIZING AN IMPAIRED PROVIDER--PHYSICAL APPEARANCE/BEHAVIOR § § § Personality changes, especially increased irritability Changes in personal grooming or mode of dress Slurred speech, tremors Reddened eyes, dilated or pinpoint pupils Frequent accidents with evidence of abrasions, hematoma, sprains or fractures § Alcohol on breath § Needle marks
PROTECTING PATIENTS • NSH requires that hospital staff report any “reasonable suspicion” of impairment • Anyone may report suspected impairment, including family, patients, staff or students • May be reported to: § Any manager, director, or VP § Any House Coordinator or designated House Coordinator/Supervisor § Medical staff leadership such as Chief of Staff, Vice Chief of Staff, Department Chairs, etc
IMMEDIATELY REPORT: • An immediate report of reasonable suspicion of impairment should be made to your supervisor if any of the following occur § The impaired provider is attempting to care for a patient § The impairment could contribute to a potential adverse outcome for a patient § Impairment has contributed to an accident or incident
SUMMARY OF APPROACH TO IMPAIRED PROVIDERS § The primary goal of reporting impairment is to offer assistance to the impaired provider and at the same time protect patients and hospital staff from harm • Northside Hospital and Medical Staff recognize that impaired providers are individuals who are dedicated to helping others, and are now in need of help themselves.
ENVIRONMENT OF CARE
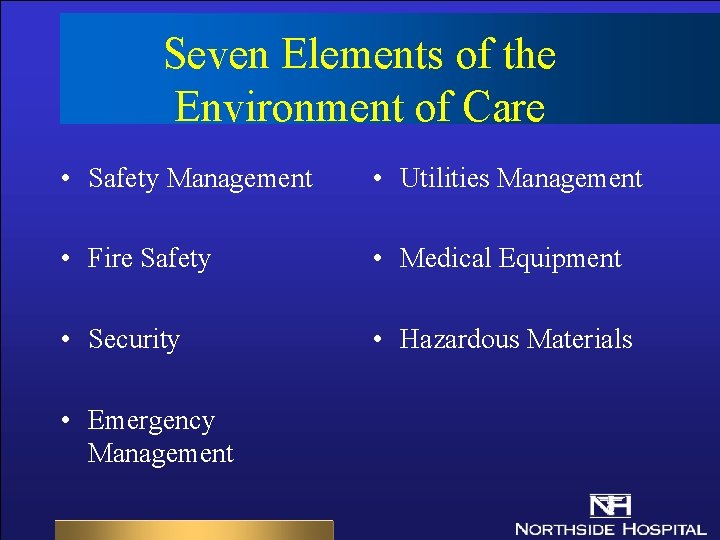
Seven Elements of the Environment of Care • Safety Management • Utilities Management • Fire Safety • Medical Equipment • Security • Hazardous Materials • Emergency Management
Safety Management • Safety Officer for NSH System – (404) 851 -8784 • Use the location- specific emergency number to report all Code Blue, Safety, Security and Medical Emergencies.
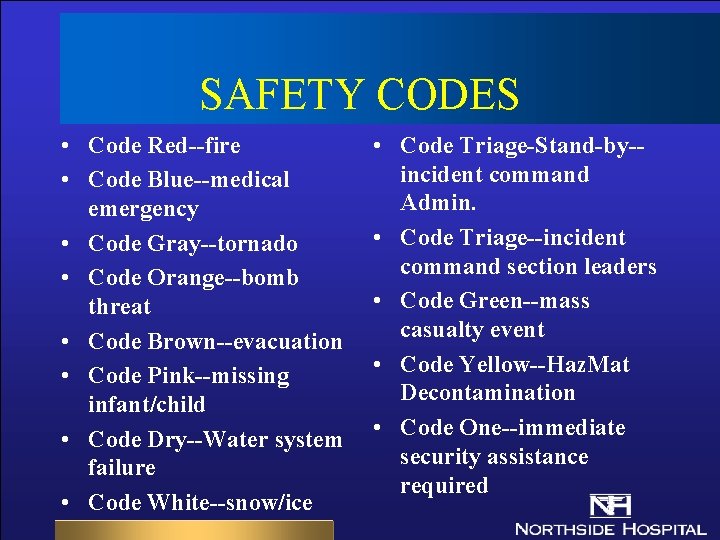
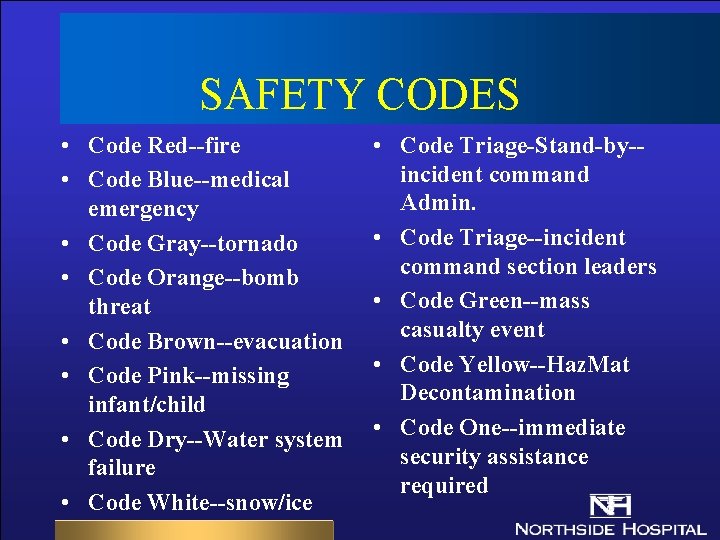
SAFETY CODES • Code Red--fire • Code Blue--medical emergency • Code Gray--tornado • Code Orange--bomb threat • Code Brown--evacuation • Code Pink--missing infant/child • Code Dry--Water system failure • Code White--snow/ice • Code Triage-Stand-by-incident command Admin. • Code Triage--incident command section leaders • Code Green--mass casualty event • Code Yellow--Haz. Mat Decontamination • Code One--immediate security assistance required
Safety Management • Report all Needle Sticks and Injuries to your Supervisor. • Use Standard Precautions when dealing with patient’s bodily secretions. • Personal Protective Equipment (PPE) will be provided at no cost.
Security Management • There is 24 hour Security on-site • Escorts are available by calling Security • Emergency Phones, Intercoms and Stairwell Alarms are available in Parking Decks • Report all Suspicious Persons to Security
Fire Safety • Code Red is the Code for Fire or Smoke. • Use R-A-C-E if you discover a fire or smoke condition. – Rescue: – Alarm: – Contain: – Extinguish: Your Patient and Yourself Pull the nearest Alarm Close all Doors. Use a Fire Extinguisher
Fire Safety • Report all Smells of Smoke to emergency number & Alert your Charge Person. • Use P-A-S-S with Fire Extinguishers. – Pull the pin. – Aim at the base of the fire. – Squeeze the handle. – Sweep the fire.
Medical Equipment • Notify Charge Person if Medical Equipment does not seem to be working correctly • All Electrical Patient Equipment MUST have a three prong plug and an up to date Safety Inspection Sticker.
Emergency Management • Code Orange is for Bomb Threats. Report suspicious items to Security. Do Not Touch or Move Suspicious Items. • Code Grey is for Tornadoes. Close & Latch all Windows. Relocate patients to Inner Hallways if able. If not, protect patients by moving them away from windows.
Emergency Management • Code Green is for External Mass Casualty. Continue in your present role and follow the instructions of your Charge Person. • Bio-Terrorism: Use Standard Precautions for all patients. smallpox patients will be placed on Air Control & Contact Precautions. Plague patients will be placed on Droplet Precautions.
Hazardous Materials • Material Safety Data Sheets (info on all chemicals used on unit/department)--ask the department supervisor on how to retrieve • Report all Chemical Spills to your Charge person. • Use Personal Protective Equipment
Utilities Management • Utility Systems include Elevators, Water, Electricity, Heating, Ventilation and Air Conditioning. • Report any problems with Utility Systems to your Charge Person or the Hospital Safety Officer.
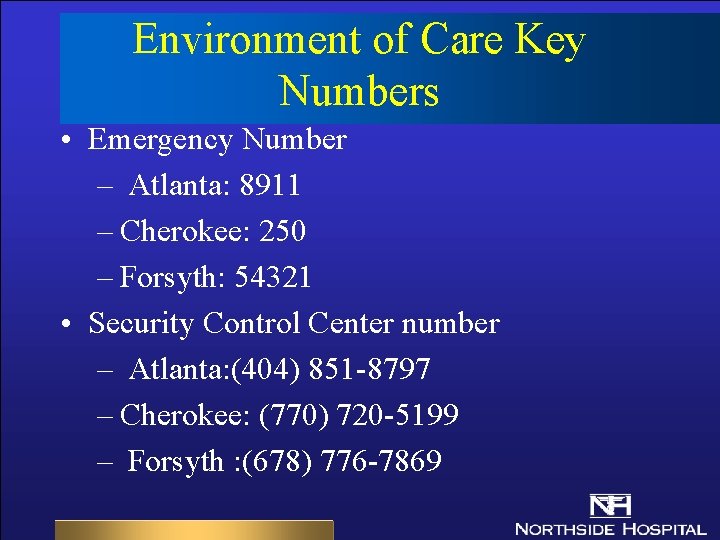
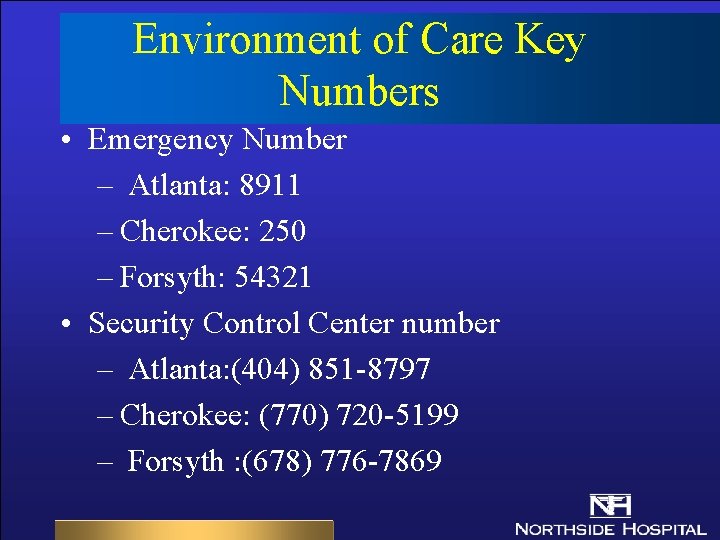
Environment of Care Key Numbers • Emergency Number – Atlanta: 8911 – Cherokee: 250 – Forsyth: 54321 • Security Control Center number – Atlanta: (404) 851 -8797 – Cherokee: (770) 720 -5199 – Forsyth : (678) 776 -7869
INFECTION CONTROL PRESENTS ISOLATION BIOTERRORISM CLEAN/STERILE TECHNIIQUE
The Isolation Guidelines Has Two Major Parts • Standard Precautions – Precautions for care of all patients regardless of diagnosis • Transmission Based Precautions – Precautions designed for care of specified patients
Unconfirmed Infectious Process • Isolate pending confirmation of diagnosis • Based on experience • “Educated guess”
Standard Precautions • • Used for all patients at all times Replaces Universal Precautions Barrier precautions the same Use common sense
Standard Precautions Barriers • • Handwashing Gloves Gowns/Aprons Masks Goggles Sharps containers Ventilation Devices
Standard Precautions Procedures • Handwashing (Most important prevention) – Consider waterless when no sinks – before patient care – after removing PPE – between tasks – after patient care completed
Standard Precautions • Gloves – for venipuncture, vascular access, when touching contaminated items – clean gloves for mucous membranes & change often • Gowns – to prevent soiling of uniform and skin contamination when pt. care requires contact with blood, body fluids or nonintact skin
Standard Precautions • Mask & Goggles – to protect mucous membranes of the eyes, nose and mouth from droplets of blood or body fluids – use anytime there is a potential risk • THIS MEANS SUCTIONING!!!
Transmission Based Precautions • Designed for patients known or suspected to be infected or colonized with transmissible or epidemiologically important organisms
Transmission Based Precautions, con’t: • Three Types: – Airborne Precautions – Droplet Precautions – Contact Precautions • New precautions called STANDARD PLUS – Use Gloves to enter room & for all patient contact
Airborne Precautions Used For: • Airborne spread, tiny droplets • TB - Suspect or confirmed • Chicken Pox (Varicella) – or disseminated Zoster • • Measles - (Rubeola) Small Pox - (BT) SARS Hemorrhagic Fevers - (BT) – (Ebola, Lassa, Marburg
Airborne Precautions • Mask – use at all times – N 95 (must be fitted) for TB, SMALLPOX & SARS – surgical mask for CP & other • Isolation room needed – negative pressure – keep door closed
AIRBORNE • Add CONTACT PRECAUTIONS – for Chicken Pox , disseminated Zoster & Smallpox ( Use 2 signs) & SARS – Teach patient to cover nose & mouth when coughing
Droplet Precautions used for • Large Droplets • Acute respiratory infections • N. meningitides, pneumonia caused by : influenza, Mycoplasma, , parvovirus, pertussis, Plague (BT), SARS
Droplet Precautions Con’t • Mask – Surgical Mask is the primary barrier unless patient has large amounts of secretions or drainage – Wear mask when working within 3 feet of patient – Wear Mask when suctioning – Wear mask on patient when transporting
Contact Precautions Used For: • Drug Resistant Bacteria – MRSA, VRE &, Others Identified by ICC • • C. Difficile Major Drainage from wound infections Diarrhea if patient is incontinent Highly Contagious skin infections ie: scabies, lice, impetigo • SARS
Contact Precautions • Wear gloves and gowns when entering the room • Remove all PPE before leaving the room • Transmission by direct pt. contact or contact with items in the environment • Create a barrier ALL THE TIME • May use empirically
Northside Isolation For Resistance ( Orange Sign) • Use With Contact Isolation Sign • Important Points – Wear all PPE when entering room – Remove all PPE before leaving – Don’t touch doorknobs and surfaces after gloves are contaminated
New Precautions Called Standard Plus • Standard Precautions With Gloves – Wear gloves to enter room and for all contact with patient – designed for patients who have a hx of MRSA, VRE but who have no symptoms of infection, drainage, or an invasive device in place
Standard Precautions: Other Components • Linen - Clean Cover Or Store In Closet – Never toss on floor – Never shake – Consider used as contaminated • CPR - Masks Available--check with supervisor of unit for location
Standard Precautions: Other Components • All NSH facilities dispose of waste in strict compliance with Georgia Regs – Red Bagged • Fluid filled containers • Microbiological, pathological – Tissue • Blood Spills - clean up by using gloves, paper towels and disinfect area • Sharps - Empty 3/4 Full
Standard Precautions: Other Components • Exposures – First aid – Report ASAP to Employee Health in off hours your supervisor / ER/ school – Source testing – PEP prophylaxis/vaccine – Use safety devices
Standard Precautions • Exposure Control Plan (ECP) In The Infection Control Manual – Tuberculosis Plan – Vaccines
Bioterrorism • What Is Bioterrorism? – Bioterrorism is the intentional release of pathogenic organisms , (bacteria, viruses, fungi) or toxins into a community to cause disease and inflict terror – Primary Agents • • Anthrax Botulism Plague Smallpox
Bioterrorism • What Is Your Role? – NSH has a bioterrorism plan – Take directions from your supervisor – Apply appropriate isolation • Standard precautions for all. • Smallpox - place in airborne/contact precautions • Plague - droplet precautions
Appropriate Use Of Clean and Sterile Technique • Basic Principles – Microorganisms are capable of causing illness in humans – Microorganisms can be transmitted by direct or indirect contact – Illness can be prevented by interrupting transmission
Definition Of ASEPSIS • Clean technique - refers to practices that reduce the numbers of microorganisms to prevent or reduce transmission • Surgical technique- refers to practices designed to render and maintain objects and areas maximally free from microorganisms
Clean Technique • Reduce numbers of skin microorganisms by handwashing or cleaning – Use soap for routine care – Apply friction to increase amount of soil removed – Clean from areas of clean to areas of less clean
Clean Technique (Cont. ). • Barrier techniques reduce transmission from patient to personnel – Use no-touch dressing technique to avoid contaminating sterile supplies – Use sterile gloves for dressing application – Wear clean gloves or apron or gown to protect clothing – Wear clean gloves to avoid contact with infectious material – Room placement important (ie: neg pressure)
Surgical Technique • Provide maximum reduction of skin microorganisms without damaging tissue • Surgical Scrub – Cleanse with soap to remove soil – Use antimicrobial agent: may leave residue to continue suppression – Apply friction with scrub brush
Sterile Technique Provide Maximum Reduction • Patient Prep – Use antiseptic agent – Remove hair when necessary. • Note: When hair removal is necessary, it should be done with a depilatory or, less desirably , by clipping, rather than by shaving with a razor. It should be done immediately before the procedure,
Sterile Technique • Use barrier techniques to decrease transmission of microorganisms from personnel to patient – Maintain area of sterile field with sterile gloves, gowns and drapes – Wear appropriate attire as indicated by risk of procedure and area of hospital where the procedure is performed
Surgical Technique – Environmental Controls To Reduce Microorganisms During Surgical Procedures: Use special treatment rooms – Control activity to reduce airborne transmission • Keep doors closed during procedures • Exclude visitors and unnecessary personnel • Avoid cleaning activities in the area during surgical procedures
Reprocessing Equipment Between Patients – Discard disposables after each patient use. – Use mechanical cleaning or change cover of surfaces not in contact with abraded skin, mucous membranes, or infectious secretions/excretion (e. g. , exam. tables, stretchers, wheelchairs. ) – Use mechanical cleaning and disinfection of noninvasive equipment that may become contaminated with body fluids (e. g. , electrodes, ear speculums, stethoscopes, blood pressure cuffs, outside surfaces of equipment such as ventilators or intravenous pumps. )
CARING FOR PATIENTS
Assessment • Each department has a specific scope of assessment based on professional & regulatory standards • Consult with preceptor to determine expectations & requirements appropriate to your clinical assignment
Interdisciplinary Plan of Care • Shows collaboration and coordination of patient care among disciplines • Interdisciplinary Plan of Care is supported by: – Interdisciplinary Clinical Guidelines – Standards of practice – Protocols • Each discipline documents consultation visit-promotes communication about care of patient
Interdisciplinary Plan of Care Includes • Admission date, diagnosis • Problem identification and prioritization • Consultation visits • Nutrition • Diagnostics • Activity • Treatments/ Interventions • Psychosocial/Spiritual • Patient/Family Education • Discharge Plan • Goals/Outcomes
Patient Safety-Restraints • Definition: – Method of physically restricting a person's freedom of movement, physical activity, or normal access to his or her body, including medication. • Goal: – Limit use of restraints to situations where alternative measures have failed & only when the possible benefits clearly outweigh the risks
Patient Safety-Restraints • Your role: – Restraints always require an MD order prior to implementation • Restraints used as part of a procedure are not considered a restraint – Communicate with patient’s nurse prior to any treatment/procedure/interaction – Communicate assessment findings relevant to patient’s behavior to patient’s nurse – If restraints are removed prior to treatment/procedure, have patient’s nurse check re-application prior to leaving patient unattended
Patient Safety-Falls • DEFINITION: An uncontrolled or unintentional descent from a higher elevation to a lower elevation • CAUSE OF FALLS: Age; gait; impaired cognition, vision and mobility; medications; failure to call for assistance; elimination; environmental issues • Falls occur in all Service Areas! • Falls occur on all shifts! • Restraints do not prevent falls!
Patient Safety-Falls • Fall Prevention: – All patients are assessed on admission and each shift – “Risk to Fall” assigned to patients with the following criteria: • History of falls and/or • Combination of two or more factors: age>70, gait problems, fatigue/weakness, disorientation/confusion, medications affecting balance, judgement &/or level of consciousness
Patient Safety-Falls • ‘Risk to Fall Plan’ – Confidential ID with “Yellow Armband” – Frequent monitoring: toileting & ADLs every 2 hours or as indicated – Pt & Family Ed Plan - teaching tool – Environmental Safety precautions • Keep pathways clear • Provide assistance with mobility – Communicate concerns to RN coordinating patient’s care
Patient Safety-Falls • FALL EVENT – Notify patient’s nurse immediately – Assess patient for injury – Complete an Incident Report • Report is forwarded to unit manager and Risk Management • Fall data included on monthly unit report card • Unit leadership reviews fall data and addresses issues at staff meetings – Document factual details of event in medical record • Do not refer to incident report in medical record • Stick to observations & what the patient says • Do not make assumptions or judgments
Patient Safety-Armband Alerts • Yellow: Risk to Fall – Educate patient / family on Safety Tips to prevent falls – Check physical environment for safety measures • Pink: Lymphedema Precautions – Criteria applies to patients with history of Breast Cancer surgery where axillary nodes removed; dialysis arm shunt and upper extremity surgery • Orange: Do Not Resuscitate – Armband should list “No-Code” or “Limited Code” with limitations listed
DOCUMENTATION
General Guidelines • All medical record entries must be done in black ink & dated & timed • Times used are based on 24 hour clock (military time); e. g. , 7 AM = 0700 & 7 PM = 1900 • Errors are corrected by crossing through the error, writing “error” above the notation & initialing the error; do not erase or use correction fluid
General Guidelines (Cont. ) • Signature form is to be used by all members of the interdisciplinary healthcare team to sign on the chart initially; afterward, use initials for any chart entry • All categories of forms must be completed-do not leave blanks
General Guidelines (Cont. ) • Charting by exception: – A checkmark will be placed in the appropriate column if patient meets defined assessment criteria – If patient does not meet defined assessment criteria, place an asterisk in the appropriate time column & document abnormal findings using bolded letter or narrative note
NON-NURSING STUDENTS: STOP HERE!! • Nursing Students must continue to review this program
Nursing Process • “A” (assessment) documented by observations & narrative notes; documented by RN, LPN, PCT & other supportive personnel • RN analyzes data to identify problem & develop plan • “P” (plan) documented on Plan of Care; RN function to prioritize problems & coordinate care
Nursing Process (Cont. ) • “I” (intervention) documented on acuity tool, flow sheets, through narrative notes or checklists; completed by all who provide care • “E” (evaluation) documented at least once per shift; evaluates progress to goals & effectiveness of treatment; RN responsibility
Initial Patient Assessment • • Physical, psychological, and social status Nutritional, functional, and educational needs Department's specific content Determines the need for care or treatment, – H & P (done by MD) • Inpatient: on chart within 24 hrs • Outpatient: on chart prior to procedure – Nursing Assessment completion: • Inpatient: on chart within 24 hrs • Outpatient: on chart prior to procedure
Patient Reassessment • Done according to the department's specific policies and procedures on reassessing patients. • Done when – significant change in the patient's condition – when a significant change occurs in the patient's diagnosis. – According to department specific, patient specific guidelines
Plan of Care • Initiated within 24 hours of admission • Reviewed each shift to determine currency & priority of problem list
Implementation • Activities performed by all members of nursing team documented to demonstrate care provided to patient
Evaluation • Nursing evaluation should reflect patients progress toward goals/outcome criteria (achievement or non achievement of the goals/outcome criteria) • If a patient does not meet outcome criteria for identified problems prior to discharge, they should be referenced in the discharge education, follow-up, transfer note etc.
MEDICATION ADMINISTRATION
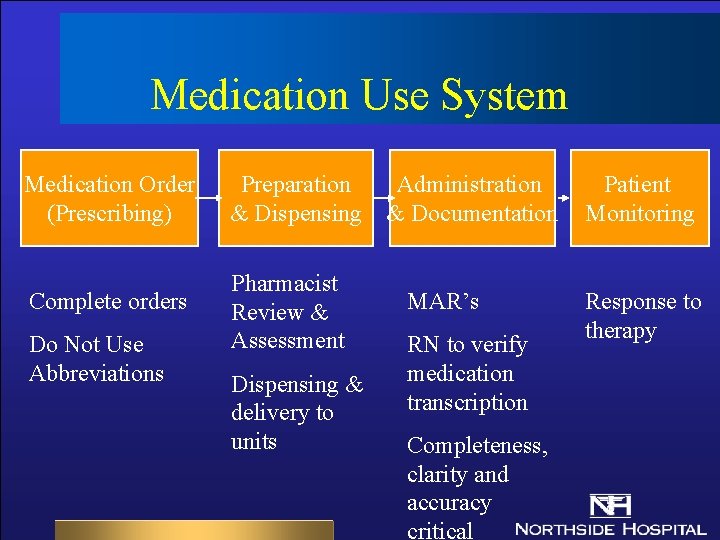
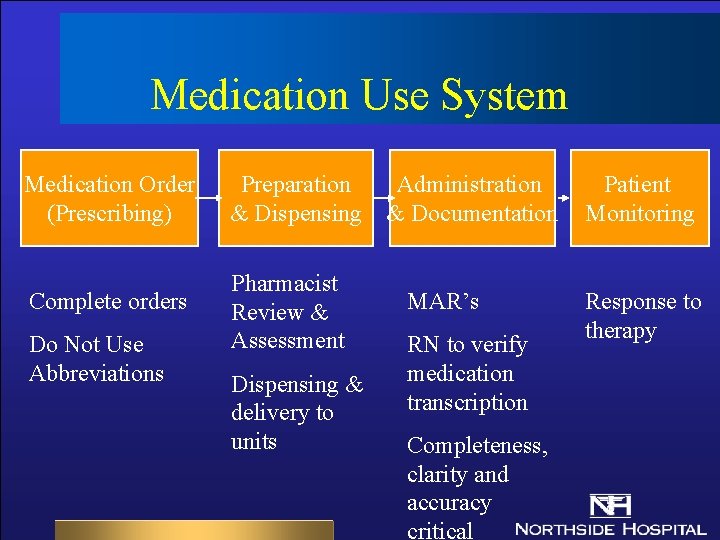
Medication Use System Medication Order (Prescribing) Preparation Administration & Dispensing & Documentation Patient Monitoring Complete orders Pharmacist Review & Assessment Response to therapy Do Not Use Abbreviations Dispensing & delivery to units MAR’s RN to verify medication transcription Completeness, clarity and accuracy critical
Five Rights • • • Right patient Right drug Right dose Right time Right route
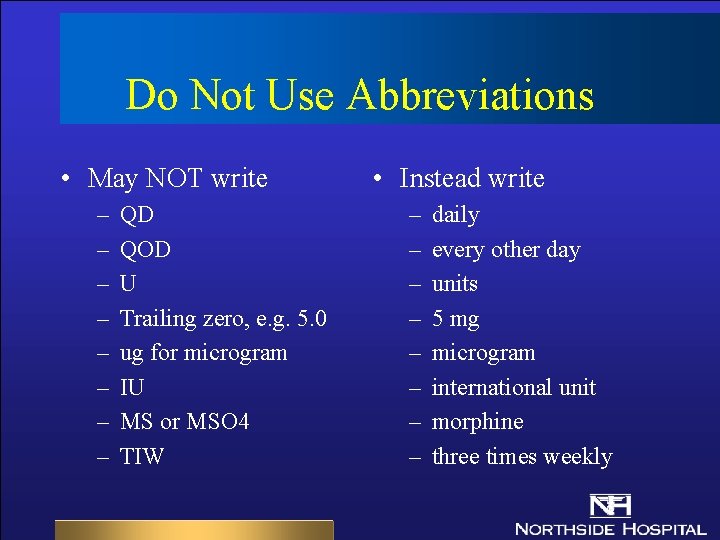
Do Not Use Abbreviations • May NOT write – – – – QD QOD U Trailing zero, e. g. 5. 0 ug for microgram IU MS or MSO 4 TIW • Instead write – – – – daily every other day units 5 mg microgram international unit morphine three times weekly
RN Responsibilities • Verifying medication order • Coordination of administration & documentation of all routine, PRN & STAT medications • Administration of all IV solutions, central line fluids & piggyback solutions
LPN RESPONSIBILITIES • Verify medication orders • Safe administration of all permitted medications (PO, IM, SQ, Routine IV infusions, Accepted IV piggybacks [antibiotics, antivirals, GI meds], select IV push medications following specific training) • Refrain from administering unauthorized medications (blood/blood products, titratable IV infusions, IV push medications, chemotherapeutic agents, PCA or epidural medications)
Respiratory Therapist’s Responsibilities • May accept & document telephone orders for respiratory/inhaled medications (e. g. , inhaled bronchodilators, sodium bicarb, etc) • May administer & document inhaled medications
Dietitian Responsibilities • May accept & document telephone orders for diets or nutritional supplements • May provide & document oral nutritional supplements to patient

PHARMACIST RESPONSIBILITIES • Managing Medication Use System – Order assessment & processing – Dispensing functions and drug distribution • Clinical Functions – Ensure appropriateness of orders – Identify and resolve drug related problems – Resources to MD’s, Nursing, Patients, etc.
MEDICATION ORDERING PRACTICES • Telephone orders may be accepted at any time; individual accepting telephone orders must: – Write order – Read back written order – Document read back • Verbal orders may only be taken during emergencies or when MD is scrubbed in for sterile procedure
Prior To Administration. . . • Medications must be verified by an RN or LPN prior to administration • Identify patient appropriately: – Medication: Compare patient name & account number on armband & MAR – Blood: Compare patient name & medical record number on armband & blood
Medication Scheduling • First dose of routine doses should be given within 2 hours of order • Oral medication should be scheduled to maximize patient sleeping times
Cultures Before Antibiotics • When cultures are ordered prior to antibiotic administration, notify MD if cultures have not been obtained within 2 hours of written order • Physician is to specify how to proceed
Labeling Open Medications • Sterile saline IV flush bottles are intended as one use only; discard any unused portion after withdrawing desired amount • Other medications that are multi-use vials (e. g. , insulin) must be labeled with date & time opened, as well as initials of individual who opened the vial
Other Labeling Issues • If medication is drawn up into a syringe but there is a delay in administration, the syringe must be labeled with medication name, dose, date, time drawn up & initials; such medications should NOT be left lying on countertops, etc. , but should be secured appropriately
Other Labeling Issues (Cont. ) • Leave oral medications in wrappers until ready to administer; it is not acceptable to put pill into med cup in med drawer unlabeled
Checks & Balances • A double check with an RN is required for dosage calculation for specific drugs: – heparin – insulin – thrombolytics • Prior to administration, an independent double check of the dosage drawn up is required for: – heparin – insulin
Checks & Balances (Cont. ) • Those drips that require precise dosing and/or titration must be administered via an infusion pump • When programming changes in IV heparin or insulin, a second RN witness is required
Insulin Procedures • Rounding: if the dose is 0. 5 units or greater, round up to the nearest whole number; if the dose is less than 0. 5 units, round down to the nearest whole number • Only insulin syringes are to be used for insulin administration • Discard insulin vials 4 weeks after opening • Insulin may be stored at room temperature after opening
Hypoglycemia • If a hypoglycemic reaction occurs or the blood glucose is < or = 60, shut off insulin drip (if present) & treat the patient according to hypoglycemic guidelines
Irrigating Solutions • Label bottles with date & time when opened • Discard all irrigation solutions 24 hours after being opened
Controlled Drug Procedures • All narcotics are kept in PYXIS • Students/Faculty will be issued temporary PYXIS access numbers by the charge nurse as necessary • In the event of a drug discrepancy, personnel are expected to remain on the unit until all discrepancies are found or accounted for
Waste Procedures For Controlled Drugs • There should be no wasted narcotics except for partial doses • A controlled drug waste will be witnessed & electronically “co-signed” by an RN in PYXIS • If an entire dose of an oral or injectable drug is refused, broken or not used for any reason, it MUST be returned to the Pharmacy by PYXIS or manually by the RN, LPN or student
Waste By Broken Ampules • In the event of a broken ampule, the breakage should be witnessed by an RN & the broken glass returned to pharmacy with a discrepancy report
Medications From Home • A patient may not take medications from home unless the pharmacy does not have that particular drug • If the patient presents medications from home, they should be: – sent home with the patient’s family, or – locked up with the patient’s valuables if there is no one to take them home
Medications From Home (Cont. ) • If indicated & the physician writes the order that the patient is to take the home meds: – The medications must be sent to pharmacy for identification – The medication must be written on the MAR as a scheduled medication – Medication must be kept in Medication Cart on unit, not at bedside – Doses must be documented as per usual
DOCUMENTING MEDICATION ADMINISTRATION • Medications are documented on 3 types of Medication Administration Records (MAR) – Computer-generated Medication Administration Record (CMAR) : this is a 24 hour MAR (Atlanta & Forsyth) – Preprinted Medication Administration Record (MAR): this is a multi-day MAR (Atlanta) – Manually transcribed (hand-written) MAR (Cherokee)
DOCUMENTATION OF ROUTINE MEDS • Use 24 hour clock to document time • All routine medications will be charted on the Routine Medication Administration Record (MAR) • Dressing changes are scheduled & documented on the MAR
DOCUMENTATION OF ROUTINE MEDS (CONT) • Document the EXACT time (e. g. , 0842 instead of 0800) of administration of the following: – Aminoglycosides – Vancomycin – Antiarrhythmics – Theophyllines – Digoxin
Documenting PRN Meds • All PRN medications will be charted on the PRN MAR at the time they are administered • Documentation to include initials, dosage, route &/or site • Effectiveness of PRN medication must also be documented using the effectiveness codes
Special Documentation Requirements • All insulin will be charted on the diabetic flow sheet • All anticoagulants will be charted on the Routine MAR if they are regularly scheduled; Coumadin ordered on a daily basis is recorded on the “one time only” section of the Routine MAR

Documentation Of Single Dose Meds • All one time only medications will be charted on the Routine MAR in the “one dose medication” section in departments with preprinted MARs • All preop medications will be charted on the Routine MAR in the “one dose medication” section in departments with preprinted MARs • On units using CMARs, single dose & pre-op meds will be charted as a scheduled dose
General Med Documentation • If a generic drug is given, the generic drug name is automatically used on the CMAR • Each individual who transcribes or records medications will also identify herself/himself on the signature form • Allergies are automatically recorded on the CMAR; on units using pre-printed MARs, allergies must be recorded on the MAR in addition to the Master Allergy Sheet
Medications Not Given • When documenting a med not given on CMAR, the time of the dose is circled, the time is initialed & the appropriate code for reason is to be noted • When documenting a med not given on a preprinted MAR, initial the appropriate time slot, circle initials & place the appropriate code for meds not given beside circled initials • The physician must be informed if a patient refuses or misses a dose of medication
DISCONTINUATION OF MEDS ON PRE-PRINTED MARS • When a scheduled med is discontinued, it will be stamped or written “D/C” on the MAR • When a PRN medication is discontinued, it will be stamped or written “D/C” on the MAR • All D/C’d meds must be verified by an RN with initials & date
DISCONTINUATION OF MEDS ON CMARs • In the appropriate column, document the date & time the med is stopped • Place initials in the appropriate column • Draw a diagonal line through the medication, place stop date, time & initials in “Stop” column”, “X” out remaining shift boxes that will not be given • All D/C’d meds must be verified by an RN with initials & date
QUESTIONS? ? • Feel free to ask your charge nurse, preceptor or instructor
BEST WISHES! • We look forward to seeing you soon!