CENTRAL NERVOUS SYSTEM INFECTIONS Dr Meral SNMEZOLU Infectous
















- Slides: 104
CENTRAL NERVOUS SYSTEM INFECTIONS Dr. Meral SÖNMEZOĞLU Infectous Diseases Department YEDİTEPE UNIVERSITY HOSPITAL
Learning objectives – Classify central nervous system infections – Understand the pathophysiology of central nervous – – – system infections Know the possible etiologic agents at certain ages Know the symptoms, signs and diagnosis of central nervous system infections Know treatment modalities of central nervous system infections Understand prognosis and know complications Be alert to the clinical presentation of acute central nervous system infections
CNS Infections l Meningitis – Bacterial, viral, fungal, chemical, carcinomatous l Encephalitis – Bacterial, viral l Meningoencephalitis l Abscess – Parenchymal, subdural, epidural

CNS Infections l Signs and symptoms – Fever – Headache – Altered mental status -lethargy to coma – Neck stiffness – meningismus – flex/ext – Increased intracranial pressure – papilledema, nausea/vomiting, abducens palsies, bulging fontanelle in infants

Meningitis l Bacterial l Viral ( aseptic) l TB l Fungal l Chemical l Parasitic l? Carcinomatous
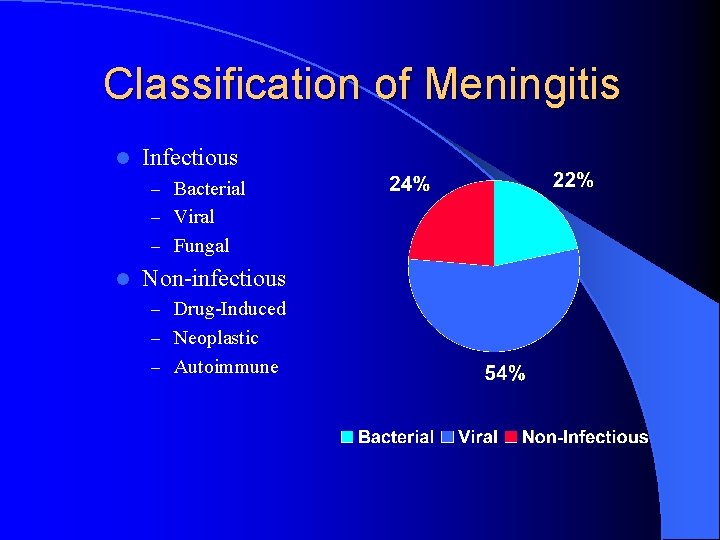
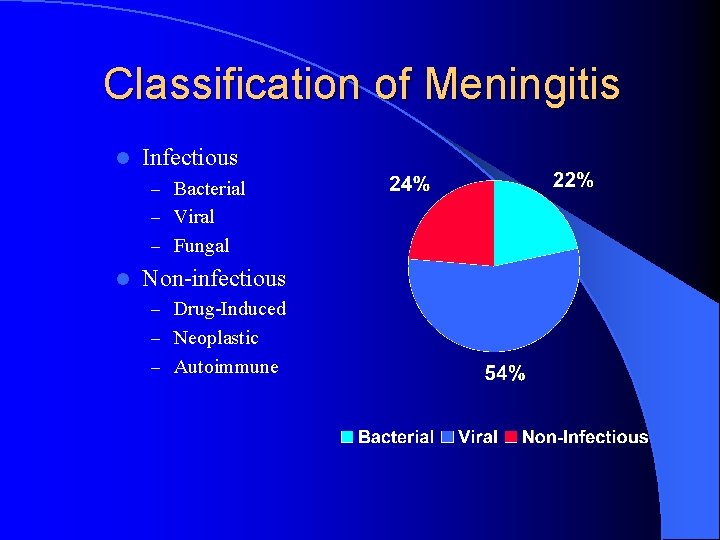
Classification of Meningitis l Infectious – Bacterial – Viral – Fungal l Non-infectious – Drug-Induced – Neoplastic – Autoimmune
Viral Meningitis
Noninfectious. . l l l l l Metabolic Mitochondrial (Reye’s, MELAS) NMS (Neuroleptic malignant syndrome) Nutritional deficiency (Wernicke’s) Paraneoplastic PRES or Malignant hypertension Seizures – (non-convulsive status) TBI Toxic Vascular
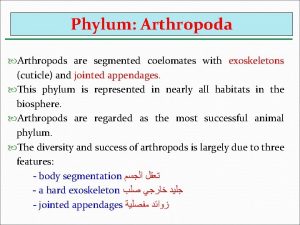
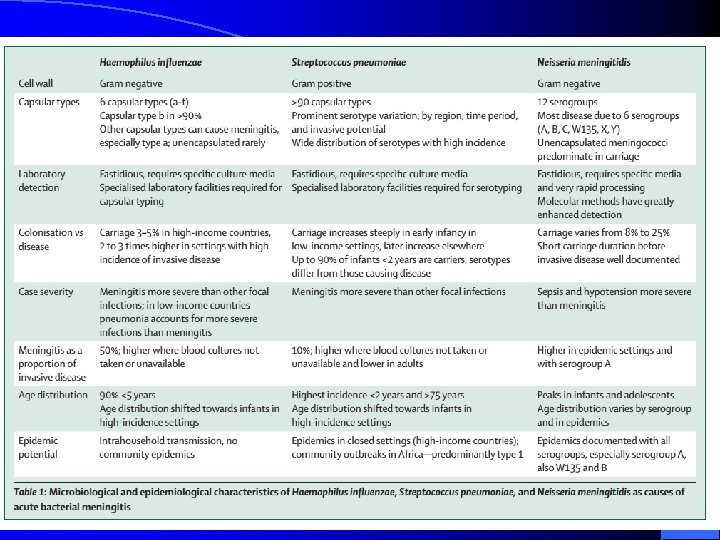
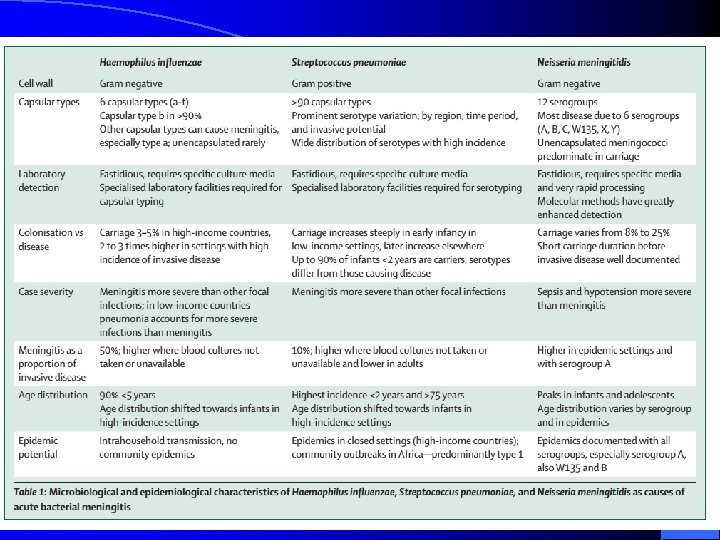
Bacterial Meningitis l Definition – Bacterial meningitis is an inflammatory response to bacterial infection of the piaarachnoid and CSF of the subarachnoid space l Epidemiology – Incidence is between 3 -5 per 100, 000 – More than 2, 000 deaths annually in the U. S. – Relative frequency of bacterial species varies with age.

Routes of Entry – Hematogenous – Neighboring focus – Anatomic defect l congenital l traumatic l surgical – Intraneural pathways
Bacterial Meningitis l Streptococcus pneumoniae l Hemophilus influenzae l Listeria moncytogenes l Group B streptococcus l Niesseria meningitidis

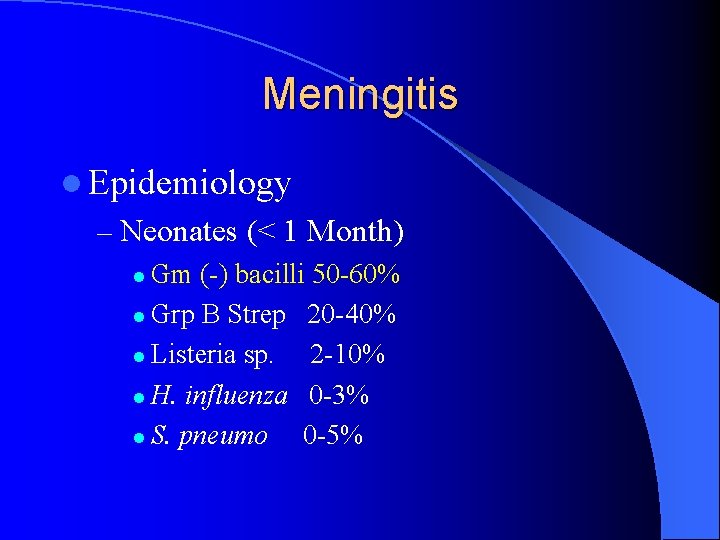
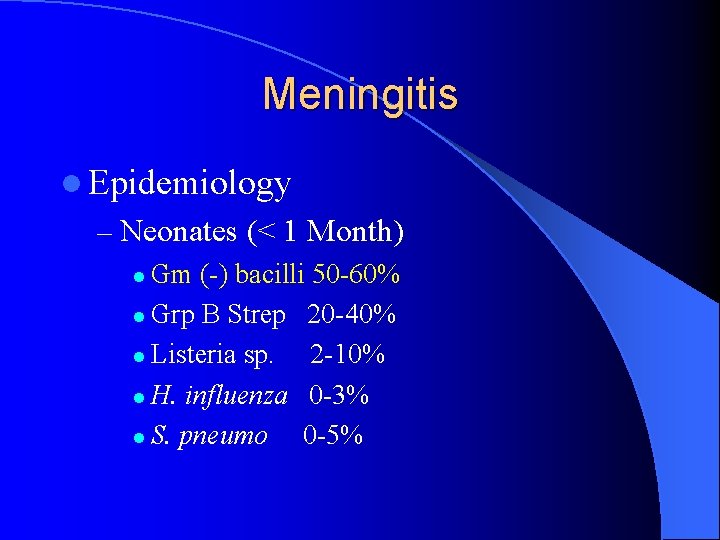
Meningitis l Epidemiology – Neonates (< 1 Month) l Gm (-) bacilli 50 -60% l Grp B Strep 20 -40% l Listeria sp. 2 -10% l H. influenza 0 -3% l S. pneumo 0 -5%
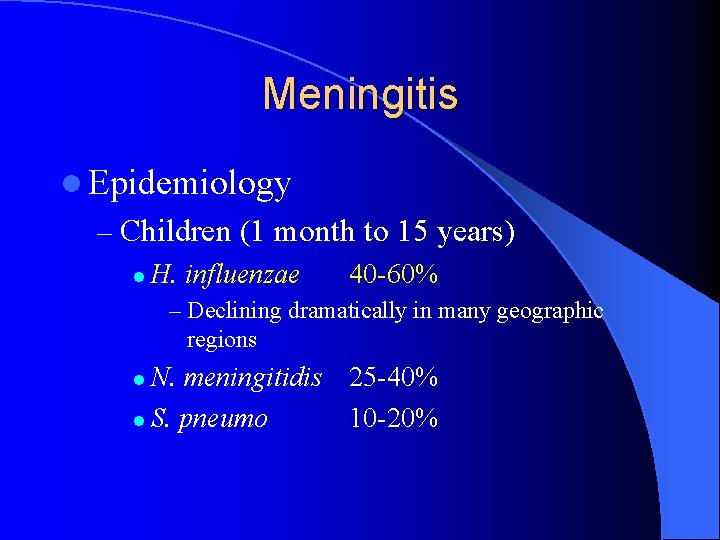
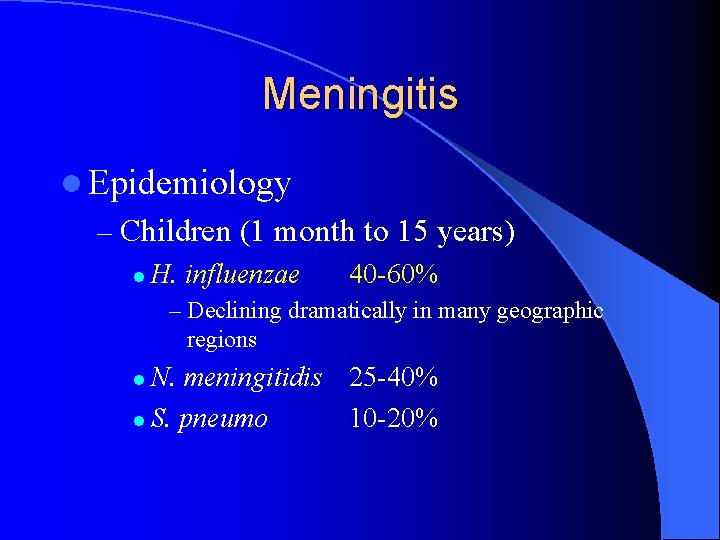
Meningitis l Epidemiology – Children (1 month to 15 years) l H. influenzae 40 -60% – Declining dramatically in many geographic regions N. meningitidis 25 -40% l S. pneumo 10 -20% l
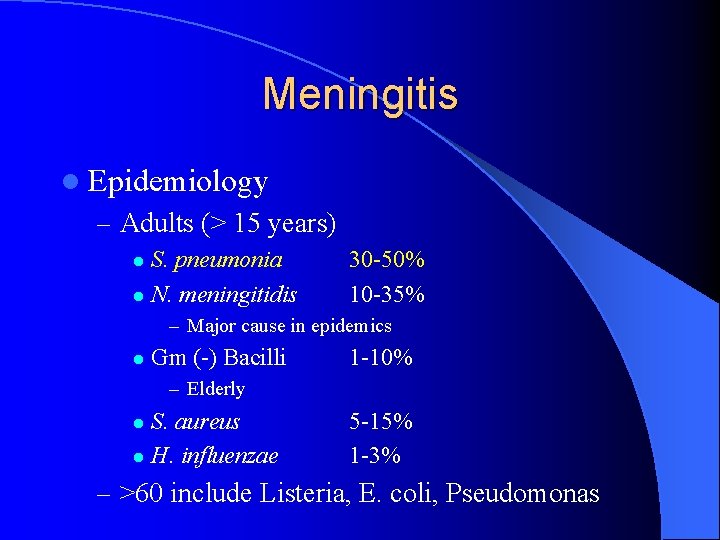
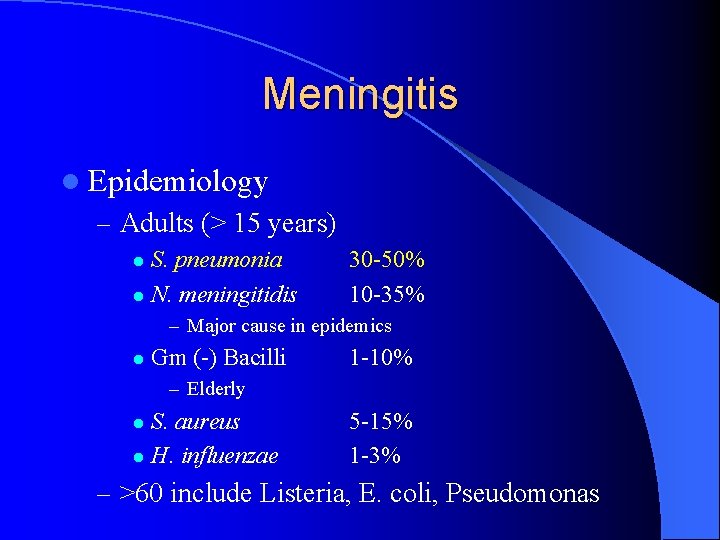
Meningitis l Epidemiology – Adults (> 15 years) S. pneumonia l N. meningitidis l 30 -50% 10 -35% – Major cause in epidemics l Gm (-) Bacilli 1 -10% – Elderly S. aureus l H. influenzae l 5 -15% 1 -3% – >60 include Listeria, E. coli, Pseudomonas
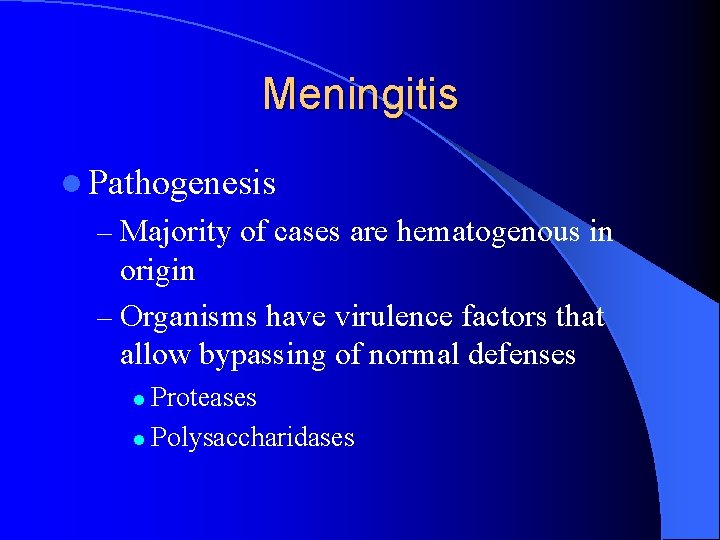
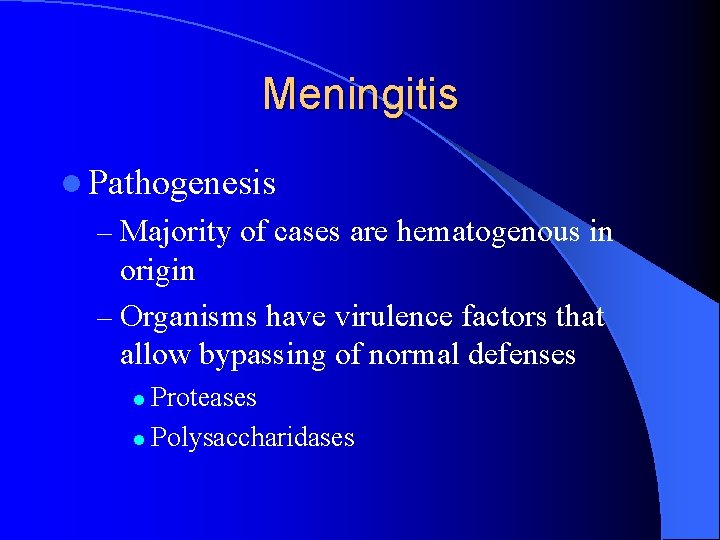
Meningitis l Pathogenesis – Majority of cases are hematogenous in origin – Organisms have virulence factors that allow bypassing of normal defenses Proteases l Polysaccharidases l
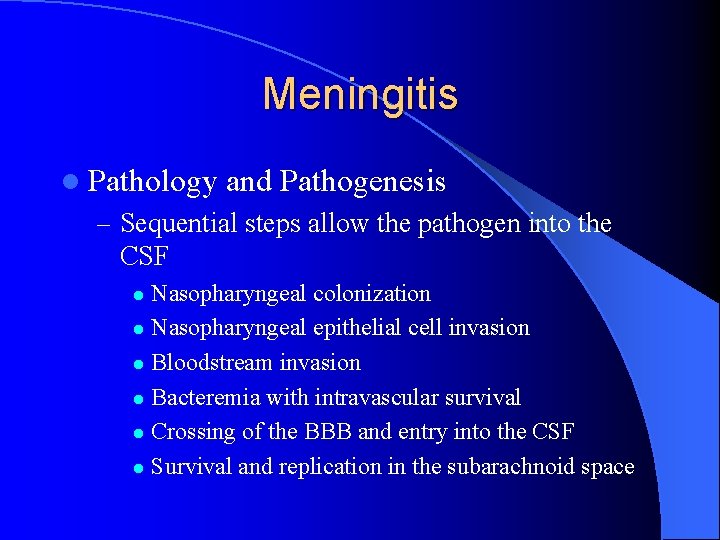
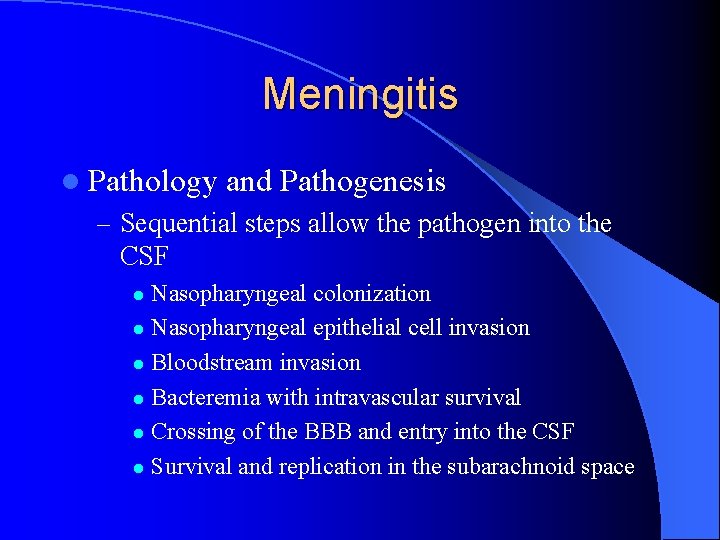
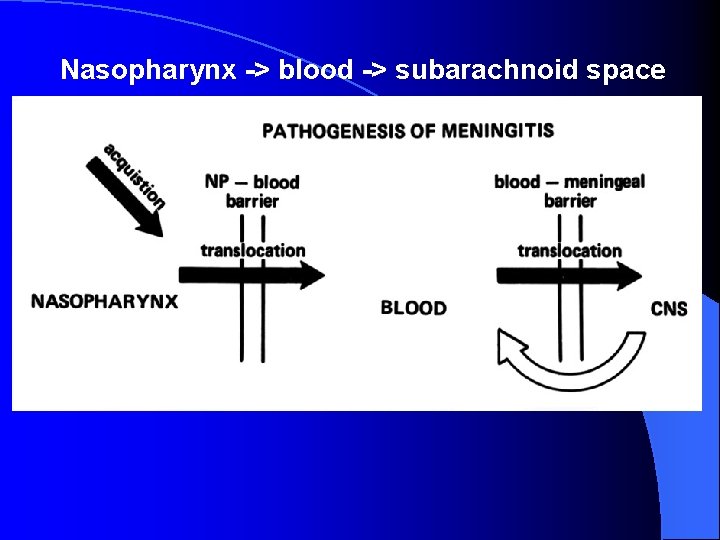
Meningitis l Pathology and Pathogenesis – Sequential steps allow the pathogen into the CSF Nasopharyngeal colonization l Nasopharyngeal epithelial cell invasion l Bloodstream invasion l Bacteremia with intravascular survival l Crossing of the BBB and entry into the CSF l Survival and replication in the subarachnoid space l
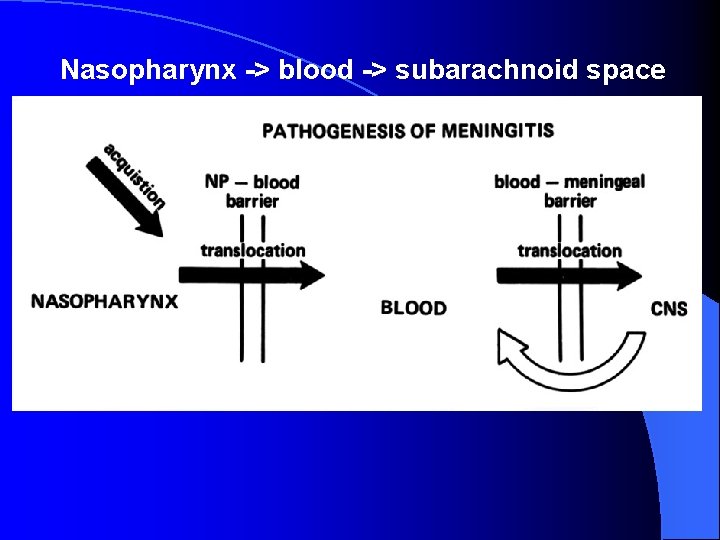
Nasopharynx -> blood -> subarachnoid space

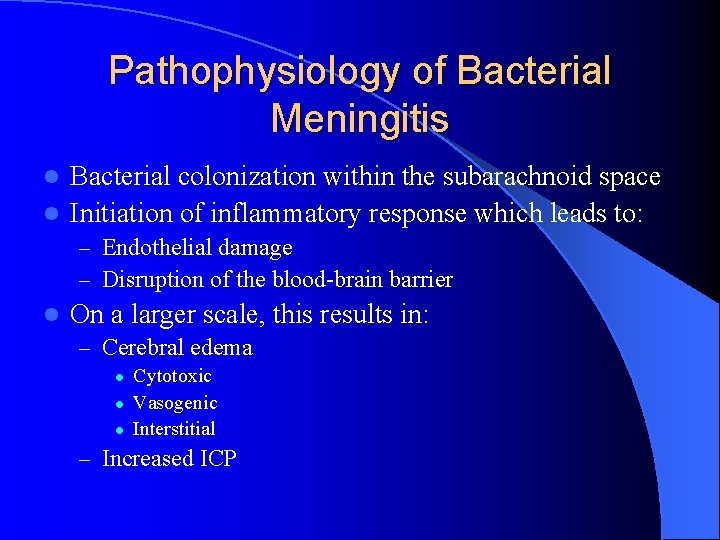
Pathophysiology of Bacterial Meningitis Bacterial colonization within the subarachnoid space l Initiation of inflammatory response which leads to: l – Endothelial damage – Disruption of the blood-brain barrier l On a larger scale, this results in: – Cerebral edema l l l Cytotoxic Vasogenic Interstitial – Increased ICP
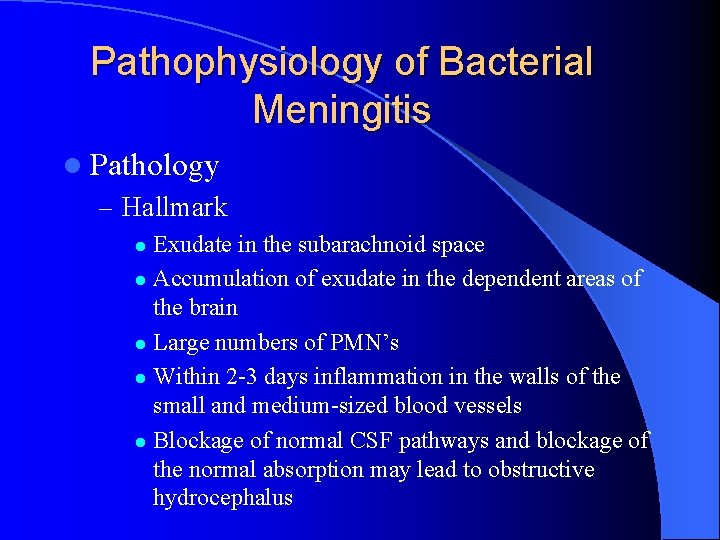
Pathophysiology of Bacterial Meningitis l Pathology – Hallmark Exudate in the subarachnoid space l Accumulation of exudate in the dependent areas of the brain l Large numbers of PMN’s l Within 2 -3 days inflammation in the walls of the small and medium-sized blood vessels l Blockage of normal CSF pathways and blockage of the normal absorption may lead to obstructive hydrocephalus l



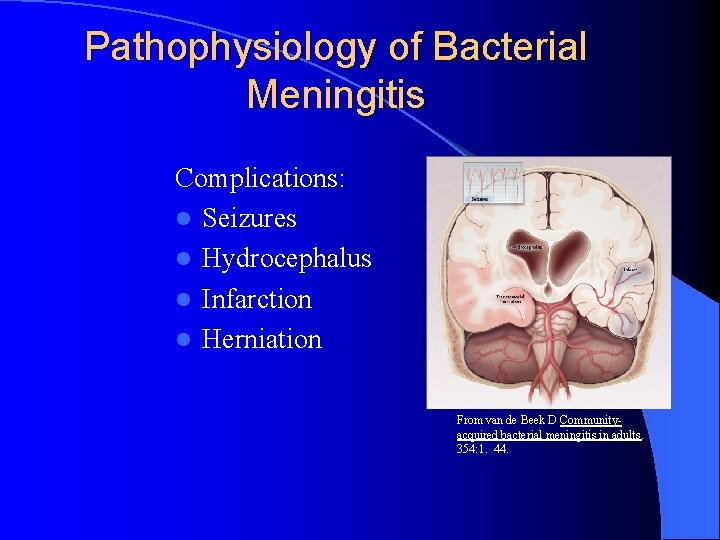
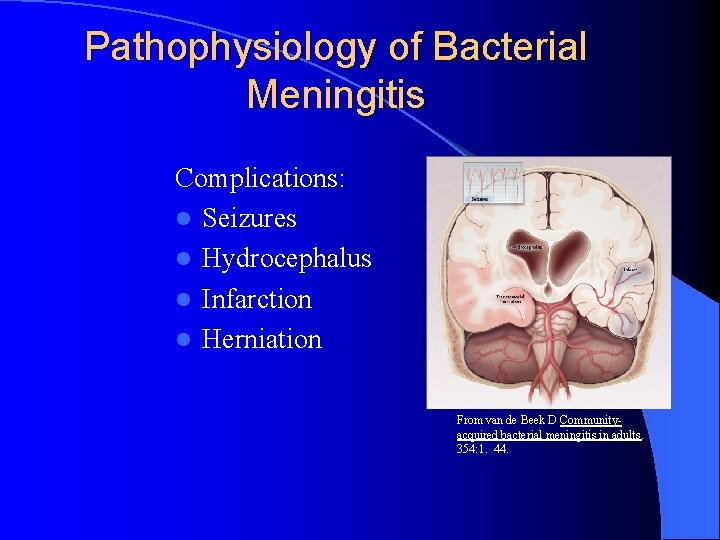
Pathophysiology of Bacterial Meningitis Complications: l Seizures l Hydrocephalus l Infarction l Herniation From van de Beek D Communityacquired bacterial meningitis in adults. 354: 1. 44.
Clinical Presentation of Meningitis Classic signs ; – fever, headache, neck stiffness, photophobia, nausea, vomiting, and signs of cerebral dysfunction (eg, lethargy, confusion, decreased level of consciousness coma). l The triad of fever, nuchal rigidity, and change in mental status is found in only two thirds of patients l Atypical presentation may be observed in certain groups (elderly, diabetic, neutropenic, immunocompromised hosts. . ). l
Clinical Presentation of Meningitis l Signs of cerebral dysfunction are common, including confusion, irritability, delirium, and coma. These are usually accompanied by fever and photophobia. l Signs of meningeal irritation are observed in only approximately 50% of patients with bacterial meningitis, and their absence certainly does not rule out meningitis

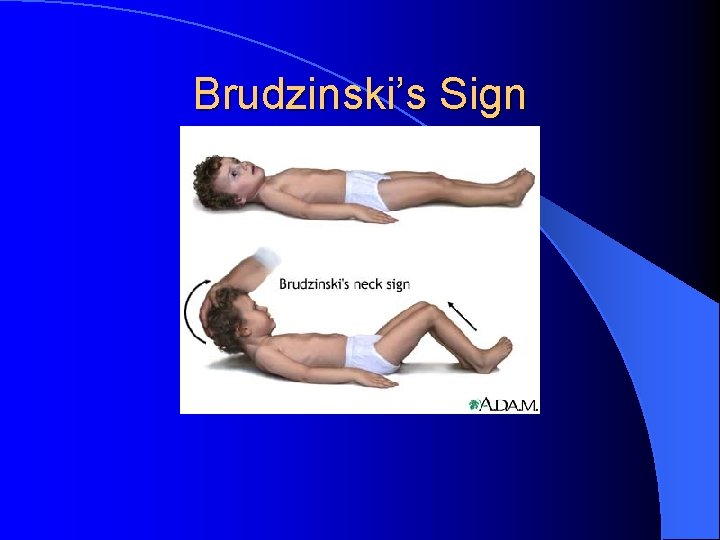
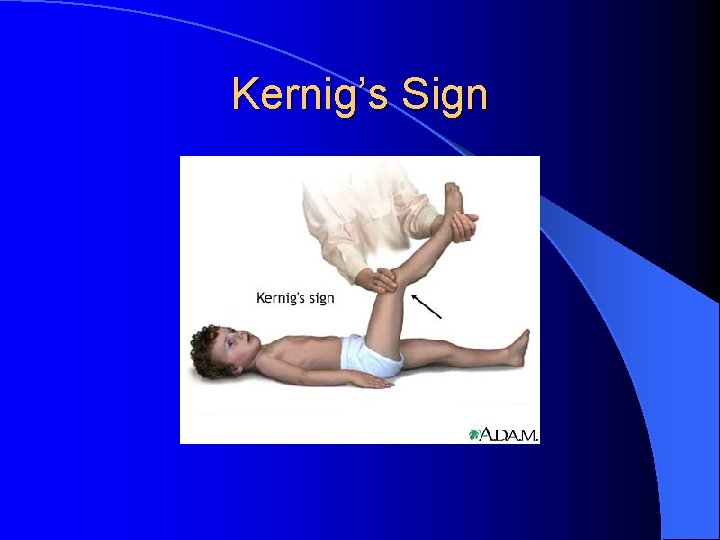
Meningitis l Clinical Manifestations – Nuchal rigidity – Kernig’s l Pt supine with flexed knee has increased pain with passive extension of the same leg – Brudzinski’s Supine pt with neck flexed will raise knees to take pressure off of the meninges l Present in 50% of acute bacterial meningitis cases l – Cranial Nerve Palsies l IV, VII – Seizures
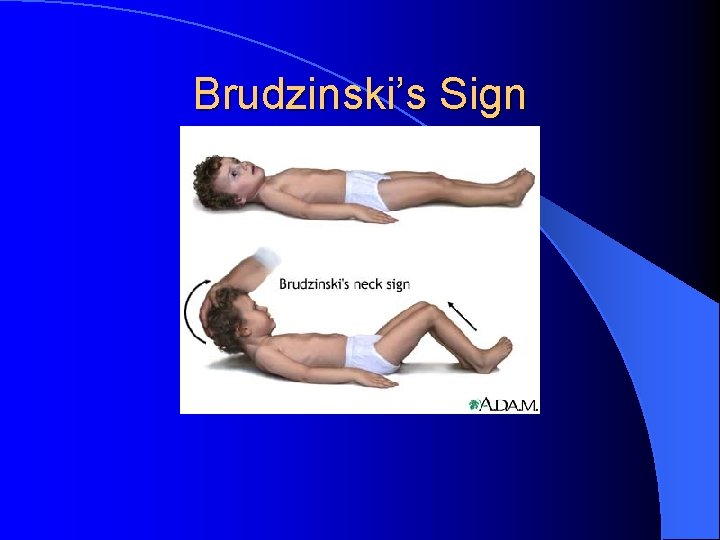
Brudzinski’s Sign
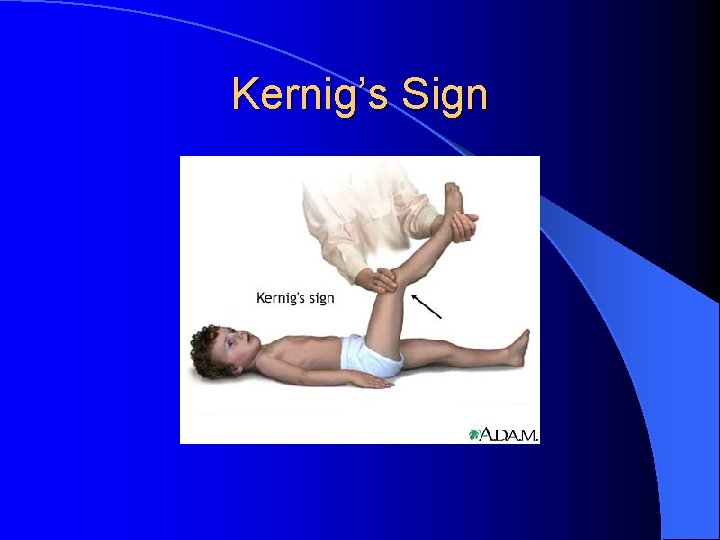
Kernig’s Sign
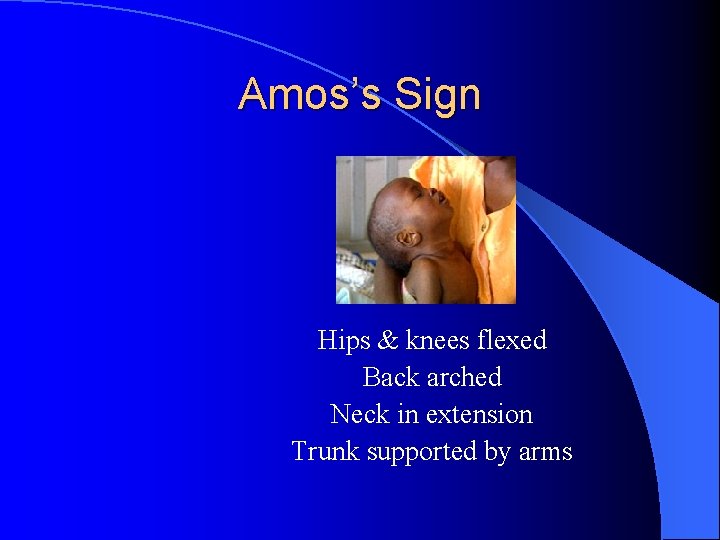
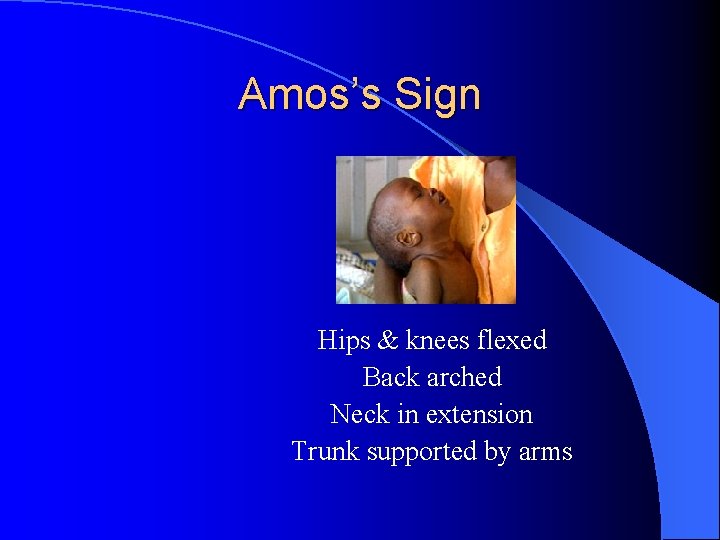
Amos’s Sign Hips & knees flexed Back arched Neck in extension Trunk supported by arms
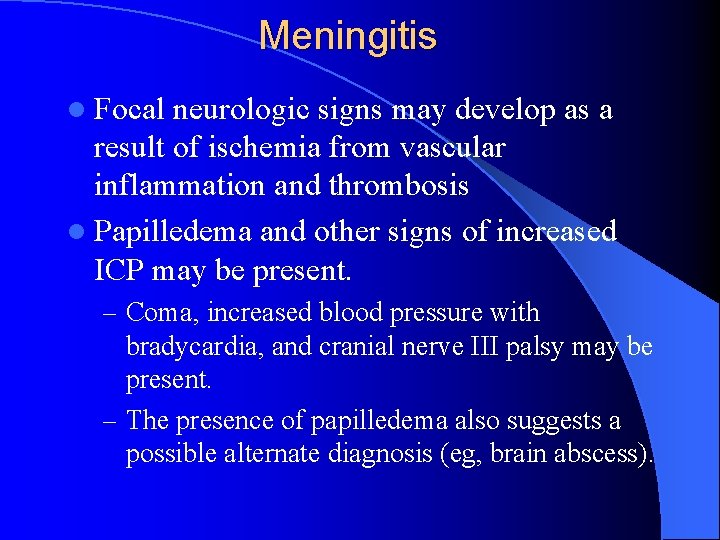
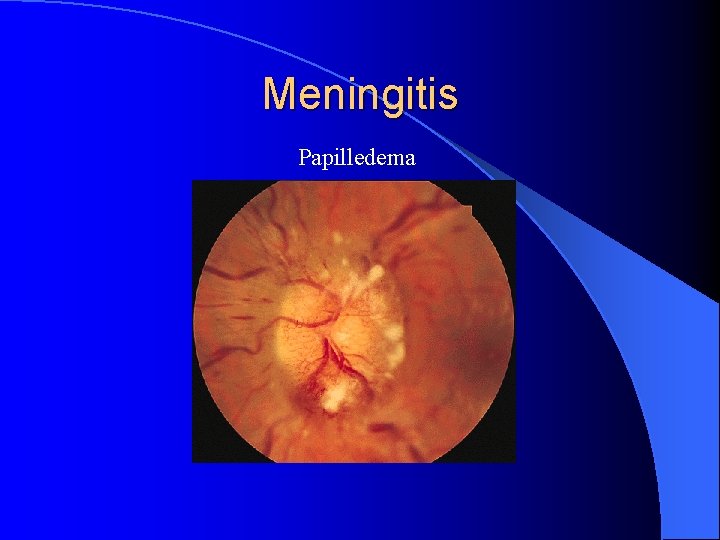
Meningitis l Focal neurologic signs may develop as a result of ischemia from vascular inflammation and thrombosis l Papilledema and other signs of increased ICP may be present. – Coma, increased blood pressure with bradycardia, and cranial nerve III palsy may be present. – The presence of papilledema also suggests a possible alternate diagnosis (eg, brain abscess).
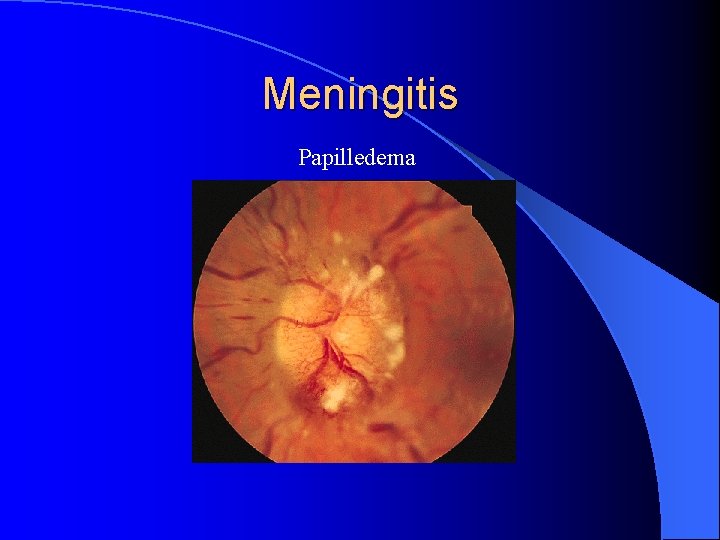
Meningitis Papilledema
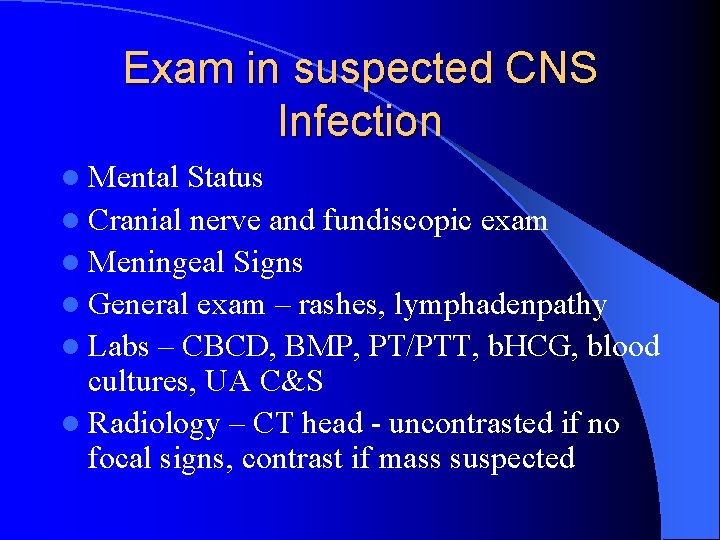
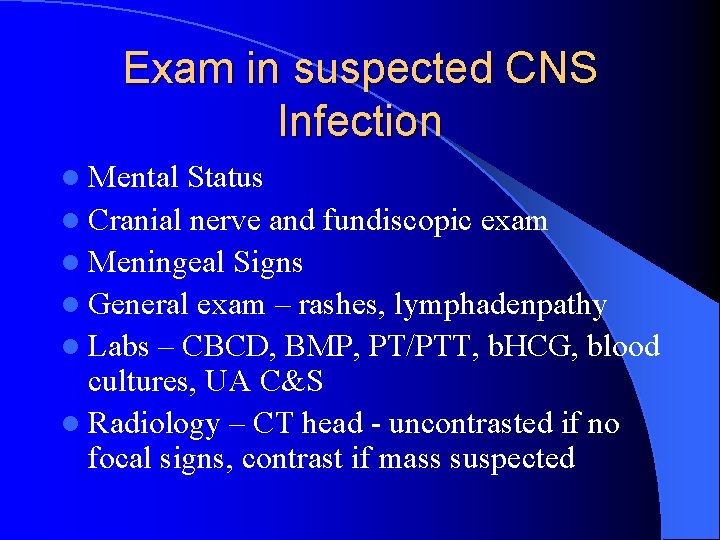
Exam in suspected CNS Infection l Mental Status l Cranial nerve and fundiscopic exam l Meningeal Signs l General exam – rashes, lymphadenpathy l Labs – CBCD, BMP, PT/PTT, b. HCG, blood cultures, UA C&S l Radiology – CT head - uncontrasted if no focal signs, contrast if mass suspected
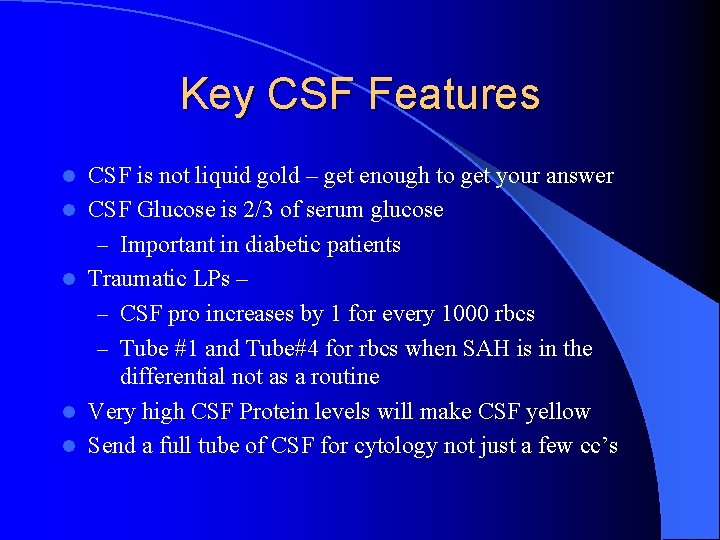
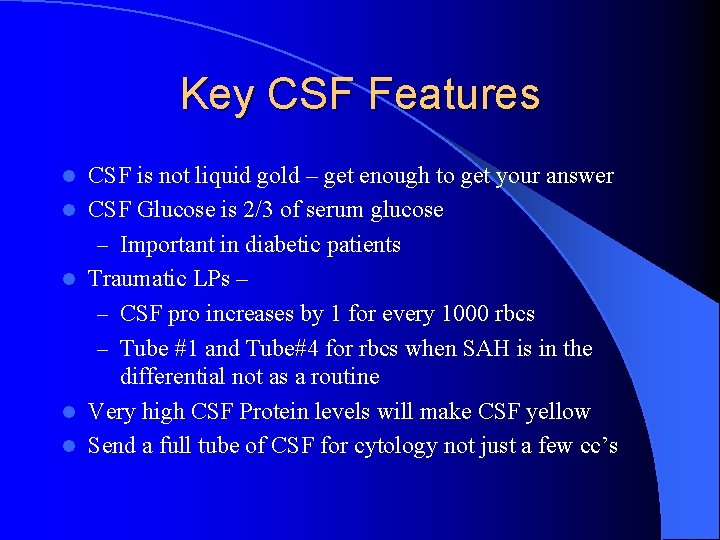
Key CSF Features l l l CSF is not liquid gold – get enough to get your answer CSF Glucose is 2/3 of serum glucose – Important in diabetic patients Traumatic LPs – – CSF pro increases by 1 for every 1000 rbcs – Tube #1 and Tube#4 for rbcs when SAH is in the differential not as a routine Very high CSF Protein levels will make CSF yellow Send a full tube of CSF for cytology not just a few cc’s
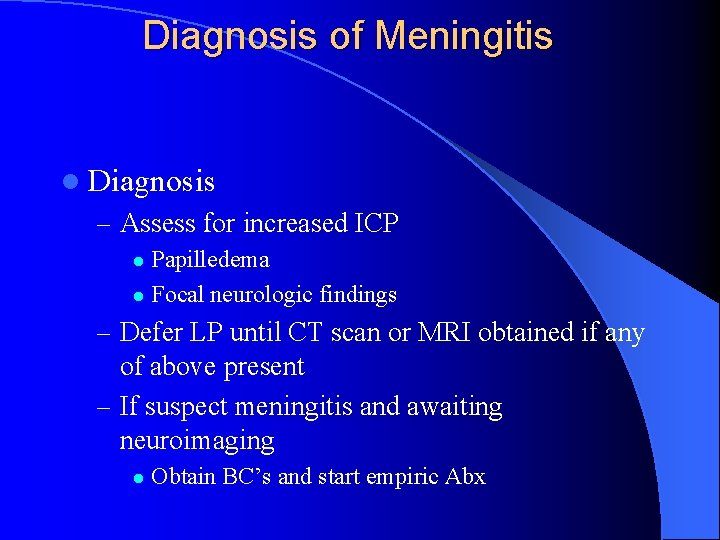
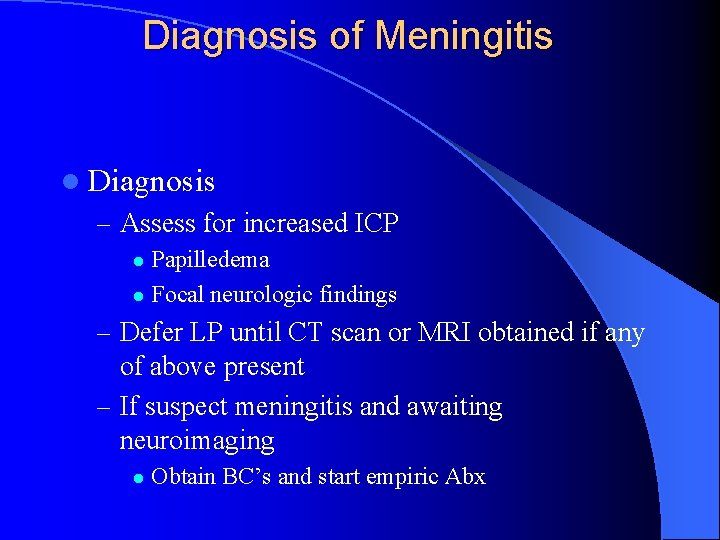
Diagnosis of Meningitis l Diagnosis – Assess for increased ICP Papilledema l Focal neurologic findings l – Defer LP until CT scan or MRI obtained if any of above present – If suspect meningitis and awaiting neuroimaging l Obtain BC’s and start empiric Abx
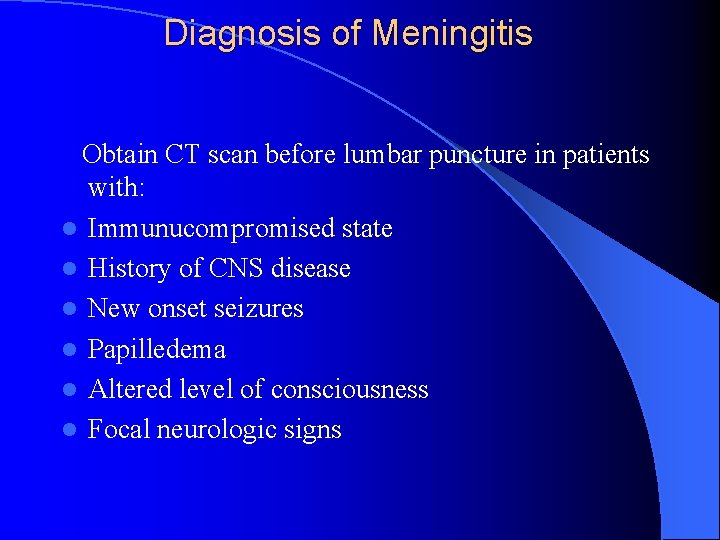
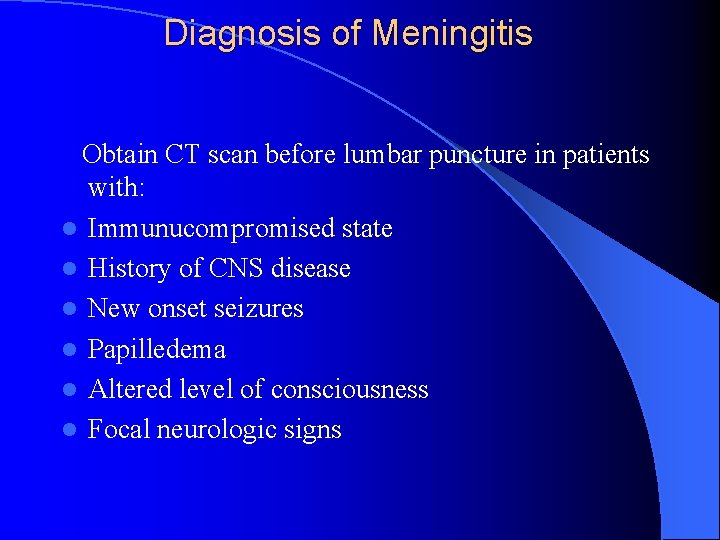
Diagnosis of Meningitis Obtain CT scan before lumbar puncture in patients with: l Immunucompromised state l History of CNS disease l New onset seizures l Papilledema l Altered level of consciousness l Focal neurologic signs
Diagnosis of Meningitis l Obtain blood cultures and give empiric antibiotics if LP is delayed
LP Increased intracranial pressure is expected – but LP contraindicated if a mass is present or if epidural spinal abscess is suspected Left lateral decubitus position L 3 -L 4 interspace or L 4 -L 5 interspace Think about your studies before the LP
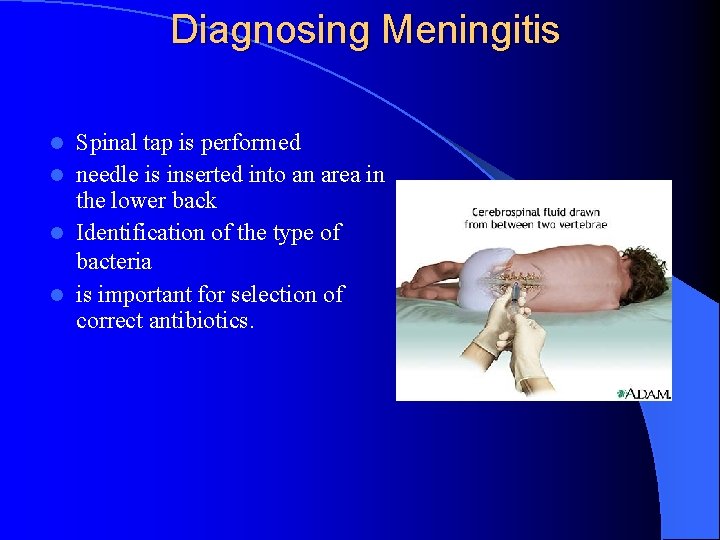
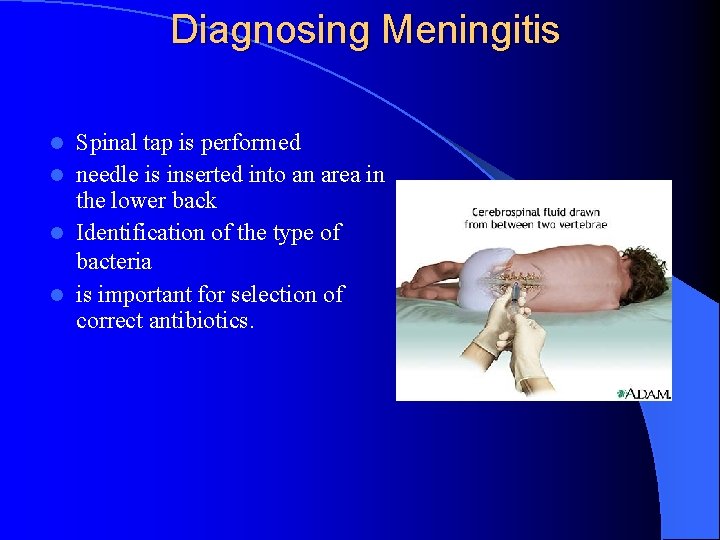
Diagnosing Meningitis Spinal tap is performed l needle is inserted into an area in the lower back l Identification of the type of bacteria l is important for selection of correct antibiotics. l
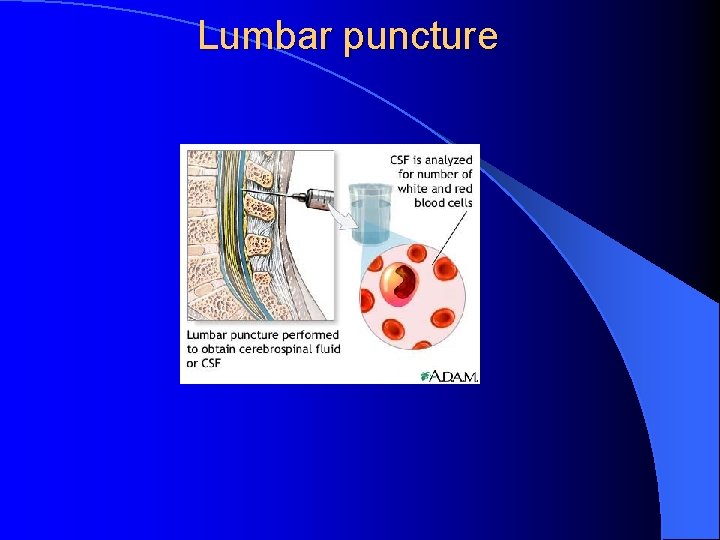
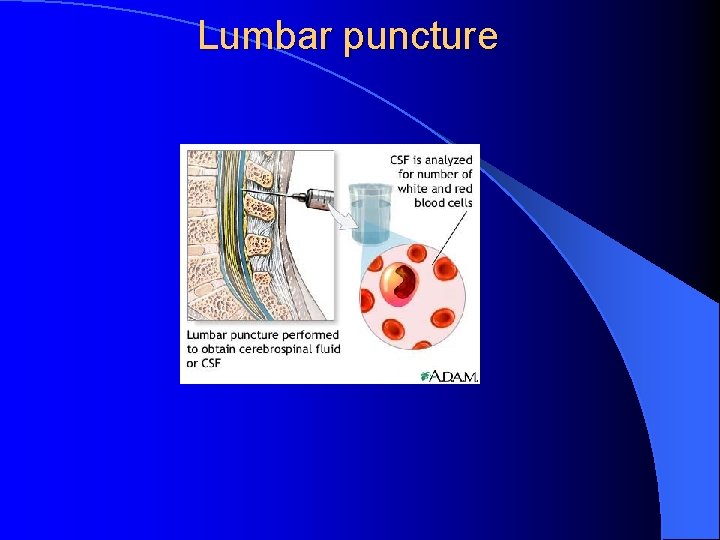
Lumbar puncture

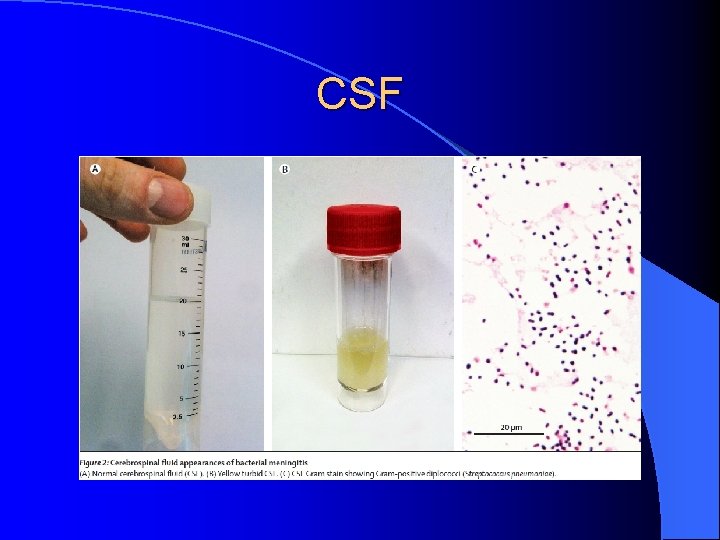
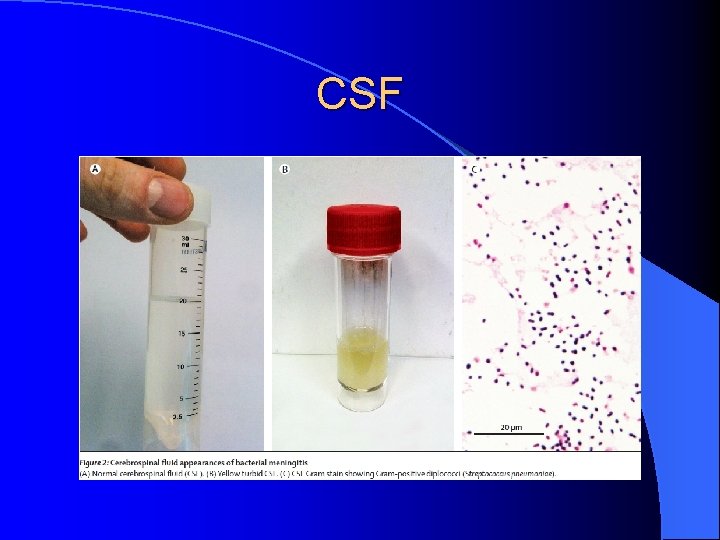
CSF
LP-CSF l Tube # 1 Protein & Glucose l Tube # 2 Gram stain & Culture l Tube # 3 Cell count & differential l Tube # 4 Store ( PCR, viral studies etc)
Diagnosis of Meningitis l Diagnosis – CSF Findings : Opening pressure Appearance Cell count & differential Glucose Protein Gram stain & culture
Bacterial Meningitis l Opening pressure: high, > 200 mm. H 20 l Cloudy l 1000 -5000 cells/mm 3 with a neutrophil predominance of about 80 -95% l <40 mg/dl and less than 2/3 of the serum glucose l Protein elevated
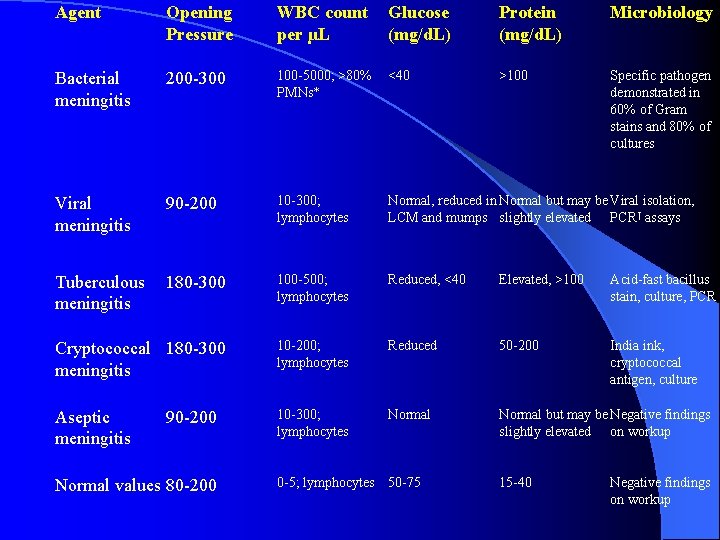
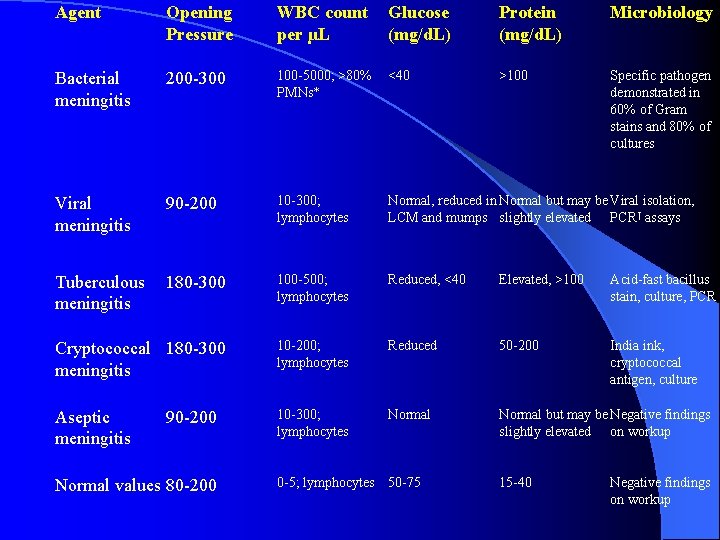
Agent Opening Pressure WBC count per µL Glucose (mg/d. L) Protein (mg/d. L) Microbiology Bacterial meningitis 200 -300 100 -5000; >80% PMNs* <40 >100 Specific pathogen demonstrated in 60% of Gram stains and 80% of cultures Viral meningitis 90 -200 10 -300; lymphocytes Normal, reduced in Normal but may be Viral isolation, LCM and mumps slightly elevated PCR† assays Tuberculous meningitis 180 -300 100 -500; lymphocytes Reduced, <40 Elevated, >100 Acid-fast bacillus stain, culture, PCR Cryptococcal 180 -300 meningitis 10 -200; lymphocytes Reduced 50 -200 India ink, cryptococcal antigen, culture Aseptic meningitis 10 -300; lymphocytes Normal but may be Negative findings slightly elevated on workup 90 -200 Normal values 80 -200 0 -5; lymphocytes 50 -75 15 -40 Negative findings on workup
Treatment l Early recognition of acute communityacquired bacterial meningitis is essential to improve the prognosis of the disease. l Clinical assessment alone is insufficient to exclude acute bacterial meningitis, l Lumbar puncture with CSF analysis is needed in all patients with suspected acute bacterial meningitis. l
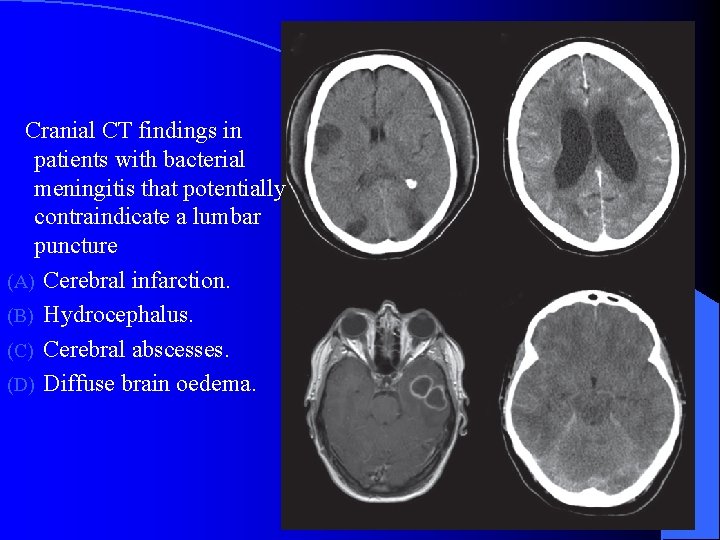
Treatment l In some cases, cranial imaging is needed before lumbar puncture to detect brain shift; in these patients, empirical antibiotic treatment should be given before imaging
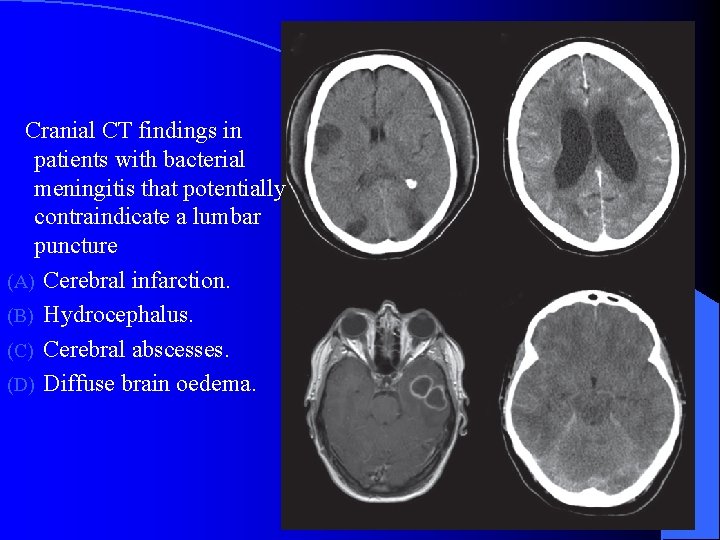
Cranial CT findings in patients with bacterial meningitis that potentially contraindicate a lumbar puncture (A) Cerebral infarction. (B) Hydrocephalus. (C) Cerebral abscesses. (D) Diffuse brain oedema.
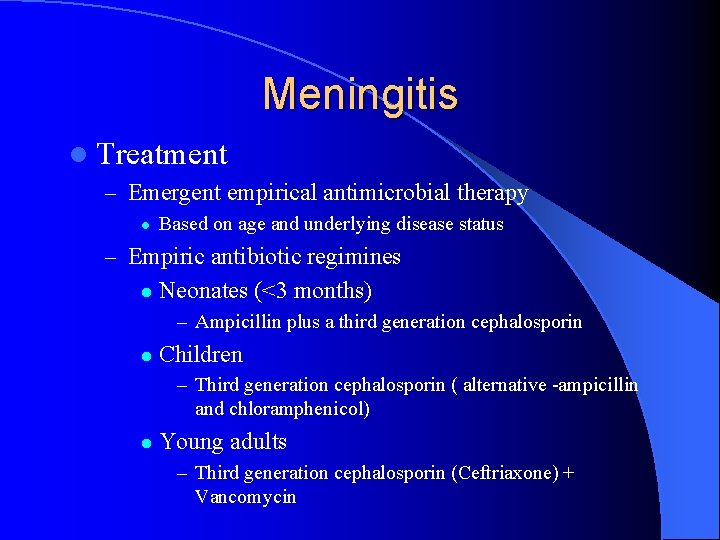
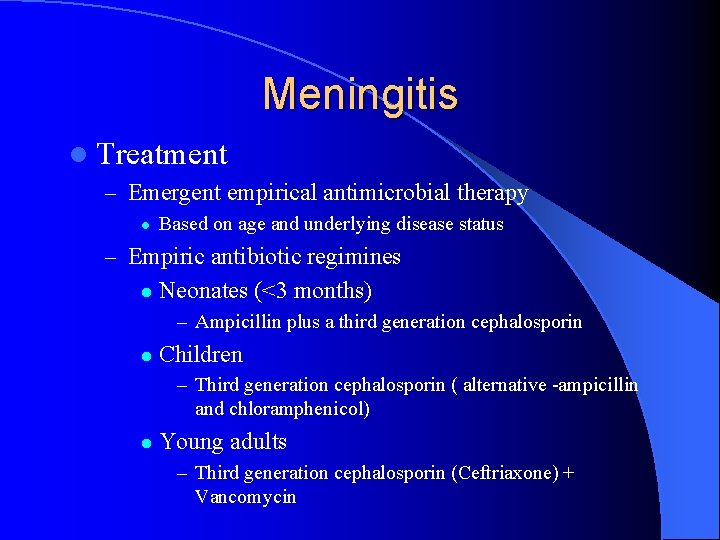
Meningitis l Treatment – Emergent empirical antimicrobial therapy l Based on age and underlying disease status – Empiric antibiotic regimines l Neonates (<3 months) – Ampicillin plus a third generation cephalosporin l Children – Third generation cephalosporin ( alternative -ampicillin and chloramphenicol) l Young adults – Third generation cephalosporin (Ceftriaxone) + Vancomycin

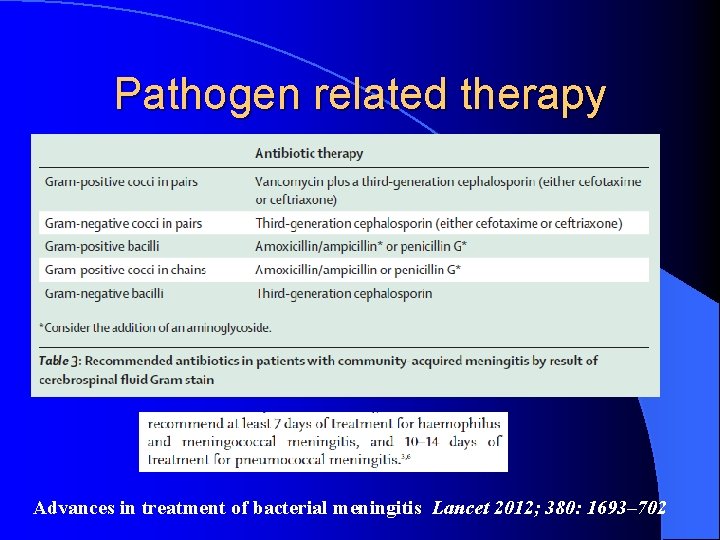
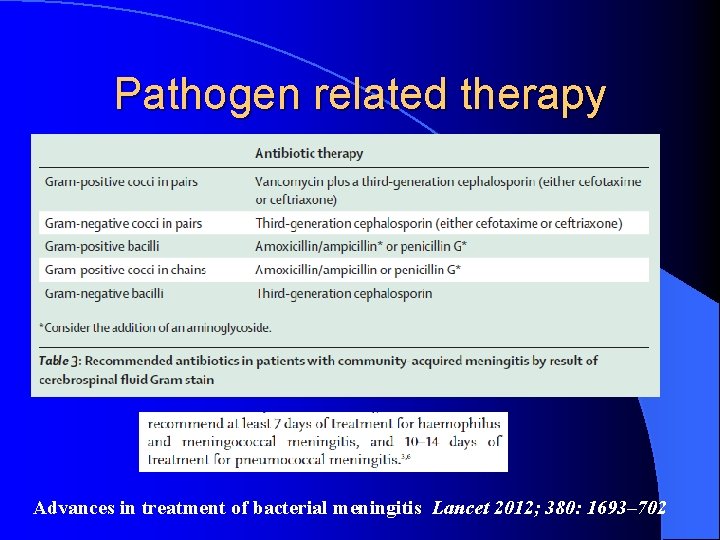
Pathogen related therapy Advances in treatment of bacterial meningitis Lancet 2012; 380: 1693– 702

Adjunctive Treatment of Bacterial Meningitis l Steroids – Dexamethasone IV q 6 for 4 days
Complications l The long-term neurologic sequelae can be grouped into 3 categories as follows: – Hearing impairment – Obstructive hydrocephalus – Brain parenchymal damage: Most important feared complication of bacterial meningitis. It could lead to sensory and motor deficits, cerebral palsy, learning disabilities, mental retardation, cortical blindness, and seizures.
Mortality of meningitis l Overall mortality rate from bacterial meningitis has decreased but remains alarmingly high. It is reported to be approximately 25%. l Among the common causes of acute bacterial meningitis, the highest mortality rate is observed with pneumococcus. l 19 -26% for S pneumoniae meningitis, l 3 -6% for H influenzae meningitis, l 3 -13% for N meningitidis meningitis, l 15 -29% for L monocytogenes meningitis.
Meningitis l Prognosis – Pneumococcal Meningitis l Associated with the highest mortality rate – 19 -26% l Permanent neurologic sequelae – 1/3 of pts – Hearing loss – Mental retardation – Seizures – Cerebral Palsy

PREVENTION
S. Pneumoniae l Polysaccaride vaccine l Conjugated vaccine
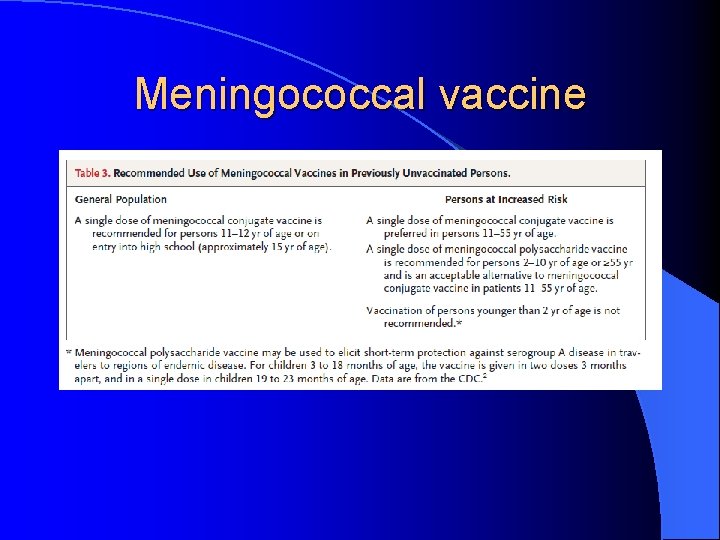
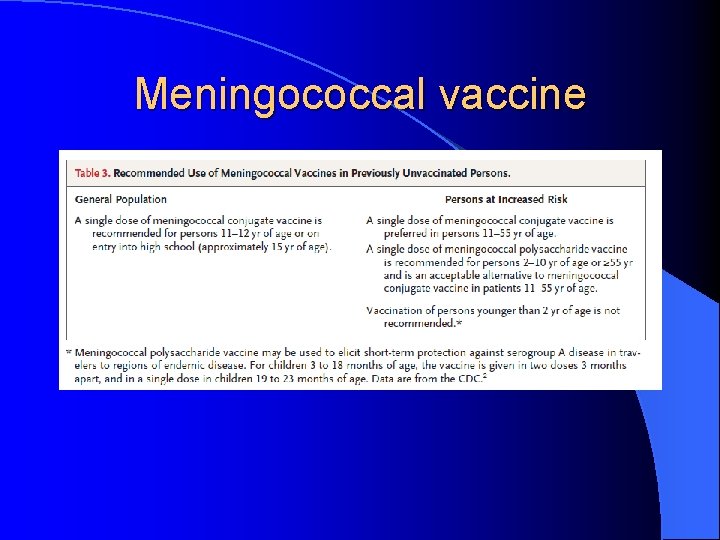
Meningococcal vaccine

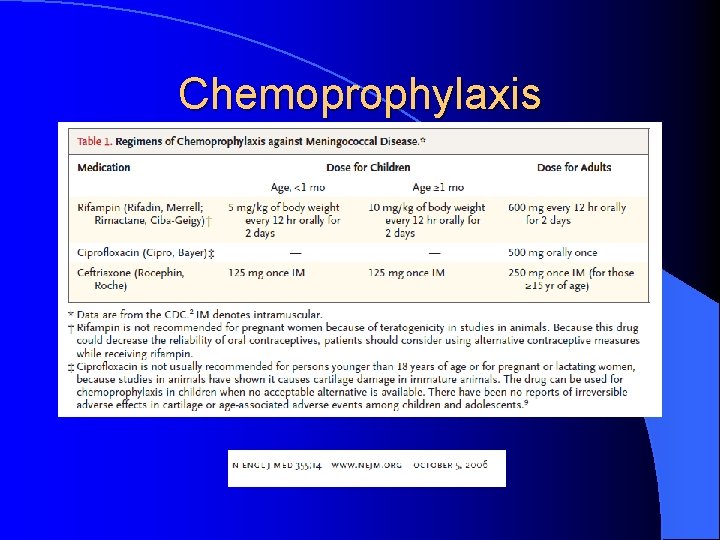
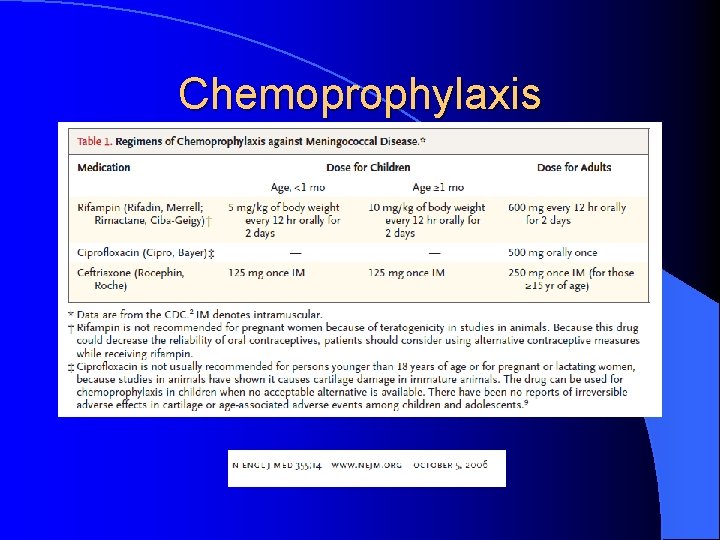
Chemoprophylaxis

Other meningitis
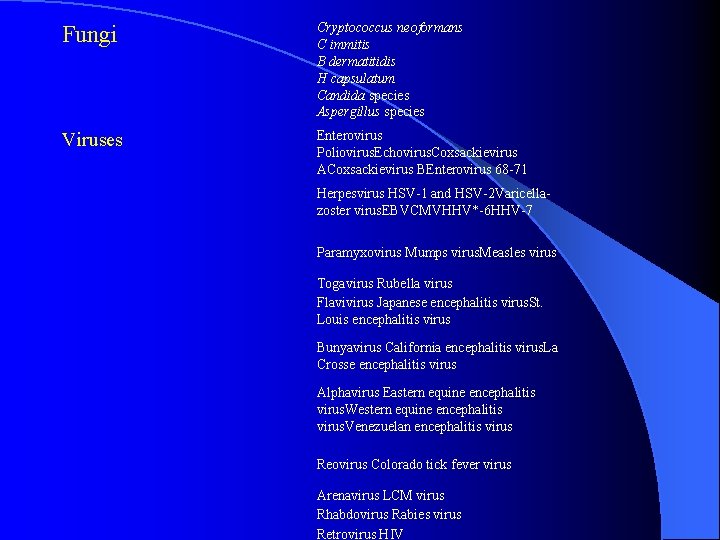
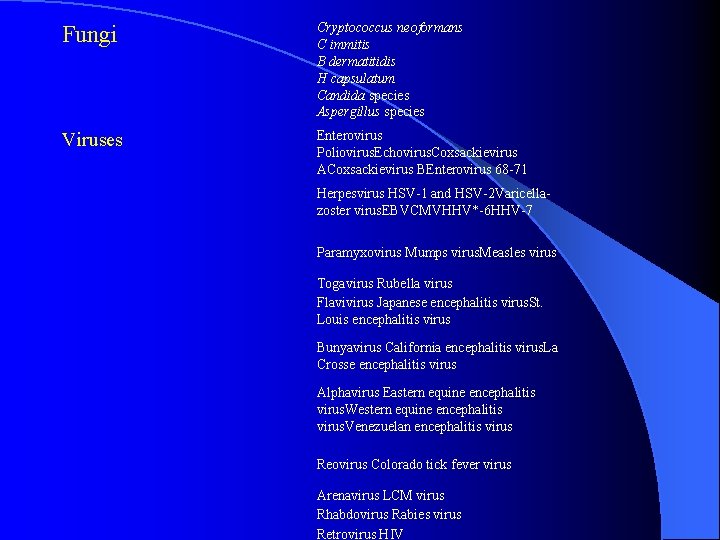
Fungi Cryptococcus neoformans C immitis B dermatitidis H capsulatum Candida species Aspergillus species Viruses Enterovirus Poliovirus. Echovirus. Coxsackievirus ACoxsackievirus BEnterovirus 68 -71 Herpesvirus HSV-1 and HSV-2 Varicellazoster virus. EBVCMVHHV*-6 HHV-7 Paramyxovirus Mumps virus. Measles virus Togavirus Rubella virus Flavivirus Japanese encephalitis virus. St. Louis encephalitis virus Bunyavirus California encephalitis virus. La Crosse encephalitis virus Alphavirus Eastern equine encephalitis virus. Western equine encephalitis virus. Venezuelan encephalitis virus Reovirus Colorado tick fever virus Arenavirus LCM virus Rhabdovirus Rabies virus Retrovirus HIV
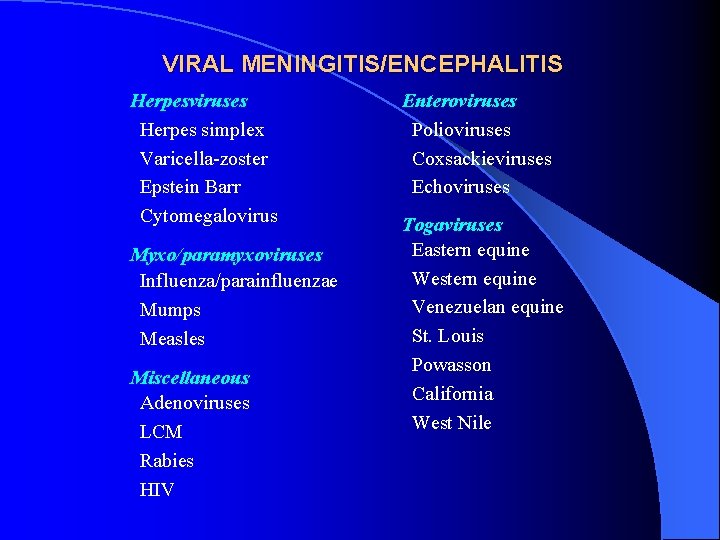
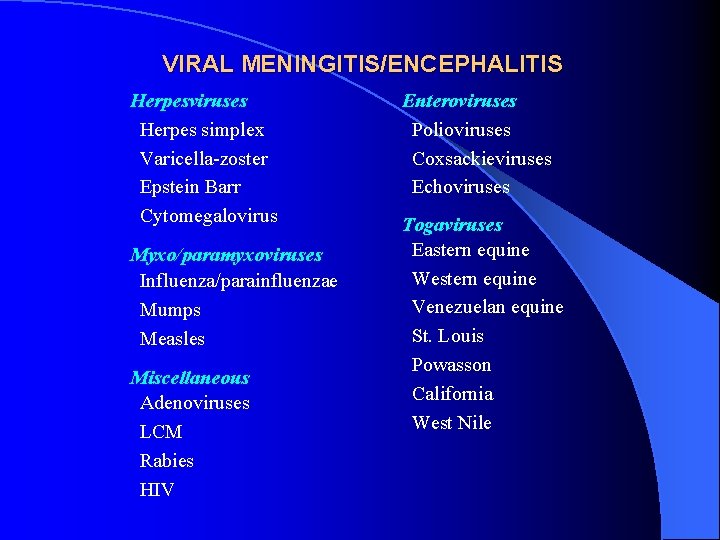
VIRAL MENINGITIS/ENCEPHALITIS Herpesviruses Herpes simplex Varicella-zoster Epstein Barr Cytomegalovirus Myxo/paramyxoviruses Influenza/parainfluenzae Mumps Measles Miscellaneous Adenoviruses LCM Rabies HIV Enteroviruses Polioviruses Coxsackieviruses Echoviruses Togaviruses Eastern equine Western equine Venezuelan equine St. Louis Powasson California West Nile
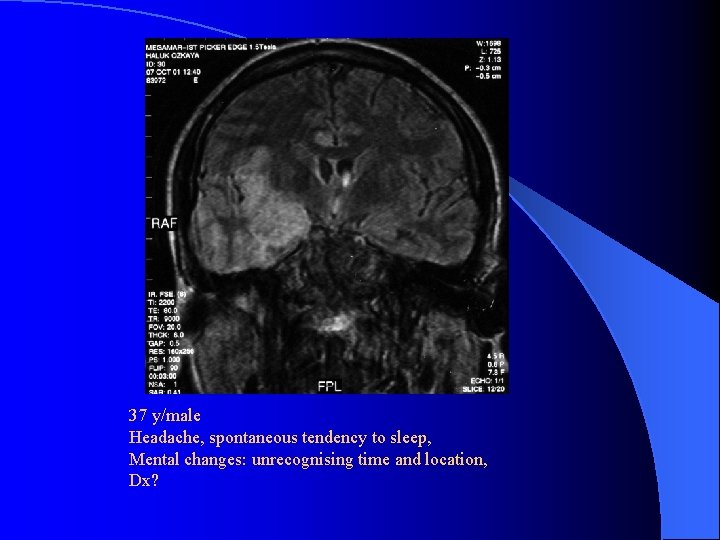
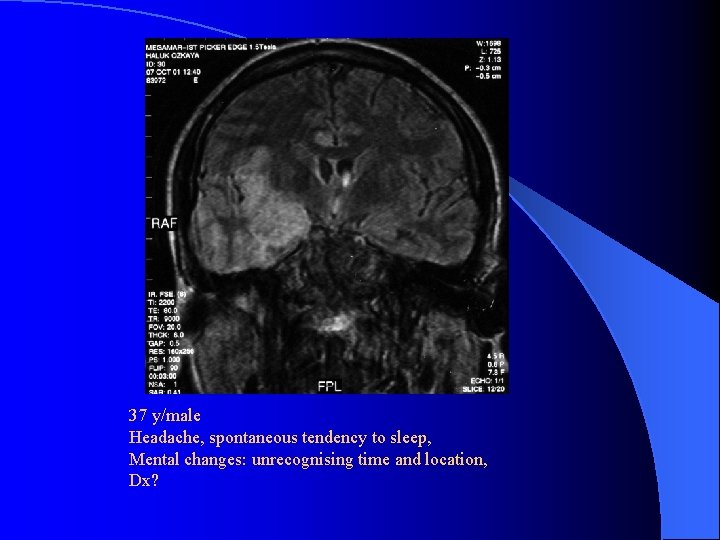
37 y/male Headache, spontaneous tendency to sleep, Mental changes: unrecognising time and location, Dx?
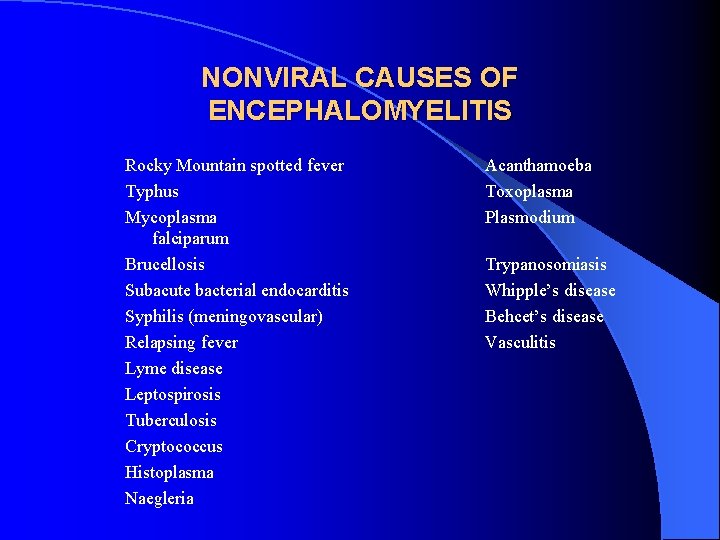
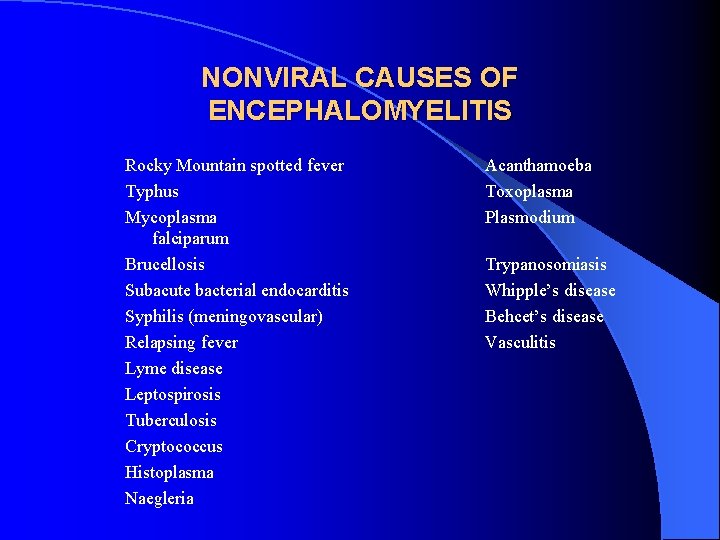
NONVIRAL CAUSES OF ENCEPHALOMYELITIS Rocky Mountain spotted fever Typhus Mycoplasma falciparum Brucellosis Subacute bacterial endocarditis Syphilis (meningovascular) Relapsing fever Lyme disease Leptospirosis Tuberculosis Cryptococcus Histoplasma Naegleria Acanthamoeba Toxoplasma Plasmodium Trypanosomiasis Whipple’s disease Behcet’s disease Vasculitis
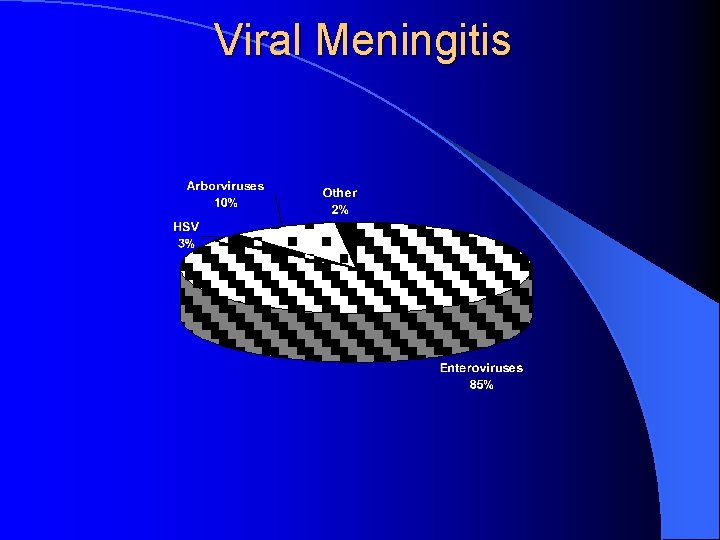
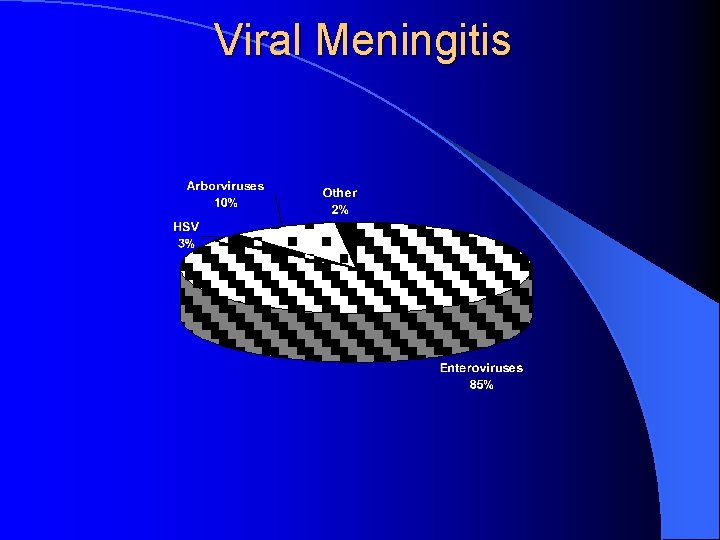
Viral Meningitis Very common Often caused by enteroviruses Treatment is supportive
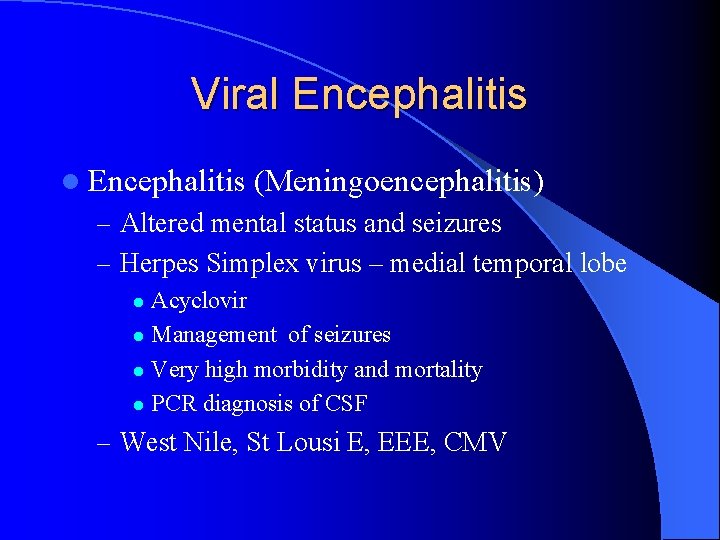
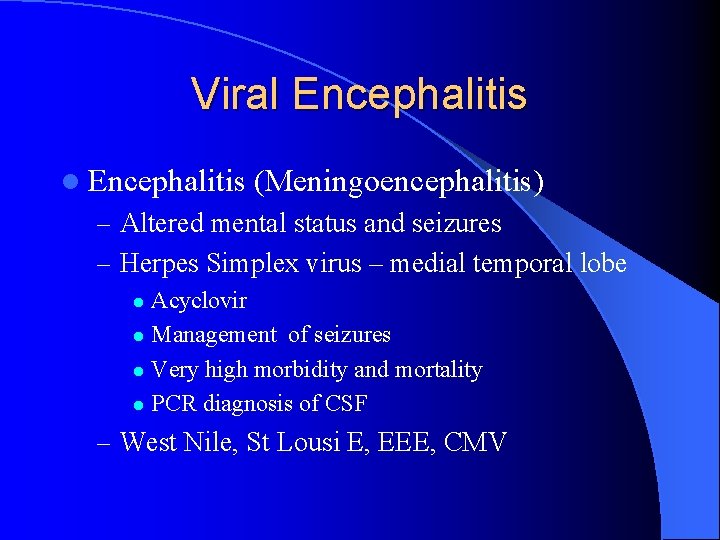
Viral Encephalitis (Meningoencephalitis) – Altered mental status and seizures – Herpes Simplex virus – medial temporal lobe Acyclovir l Management of seizures l Very high morbidity and mortality l PCR diagnosis of CSF l – West Nile, St Lousi E, EEE, CMV
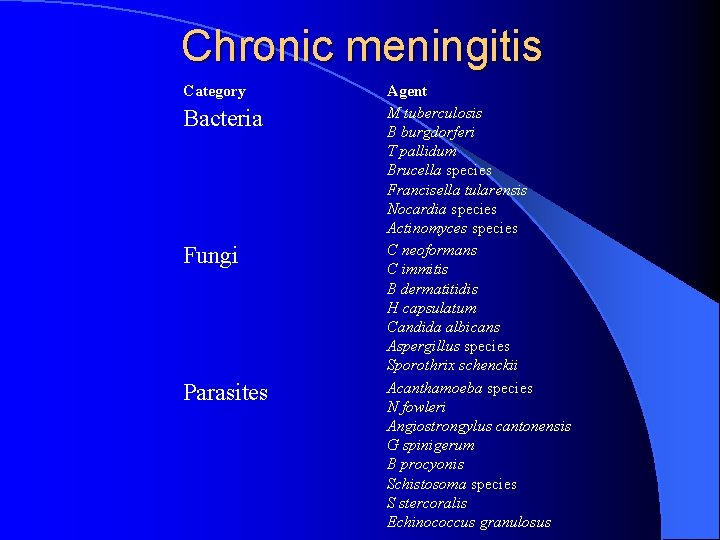
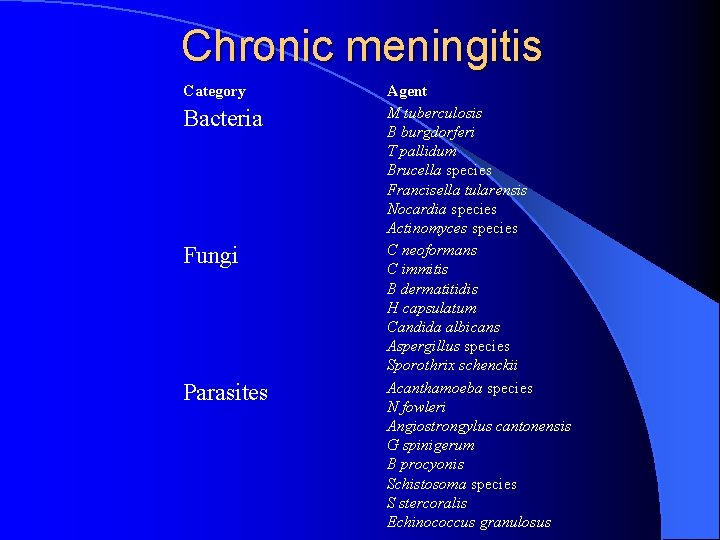
Chronic meningitis Category Bacteria Fungi Parasites Agent M tuberculosis B burgdorferi T pallidum Brucella species Francisella tularensis Nocardia species Actinomyces species C neoformans C immitis B dermatitidis H capsulatum Candida albicans Aspergillus species Sporothrix schenckii Acanthamoeba species N fowleri Angiostrongylus cantonensis G spinigerum B procyonis Schistosoma species S stercoralis Echinococcus granulosus
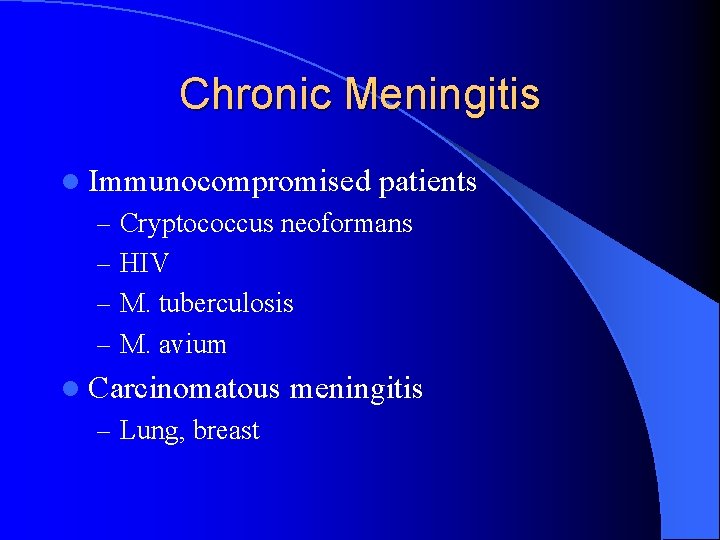
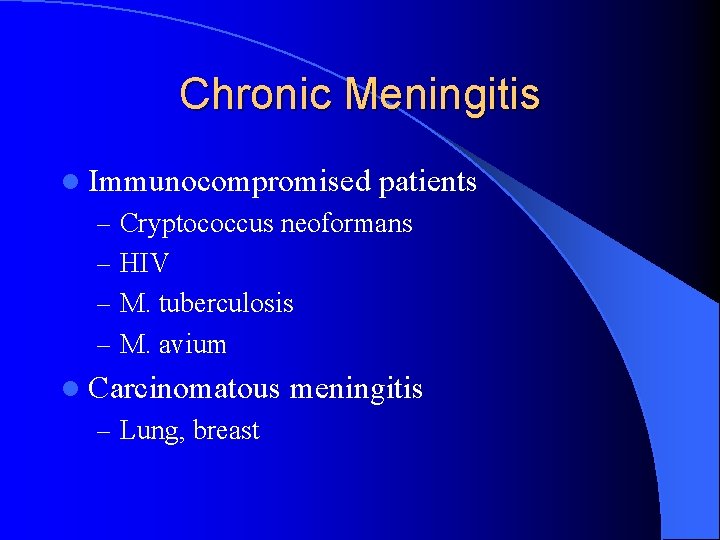
Chronic Meningitis l Immunocompromised patients – Cryptococcus neoformans – HIV – M. tuberculosis – M. avium l Carcinomatous – Lung, breast meningitis
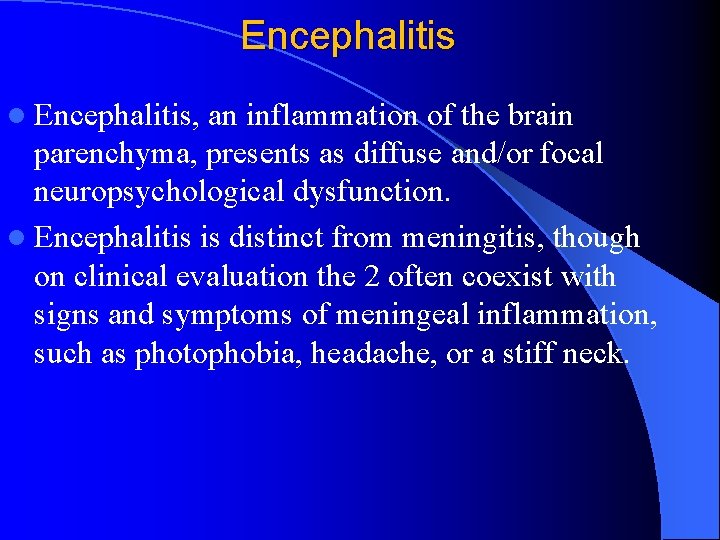
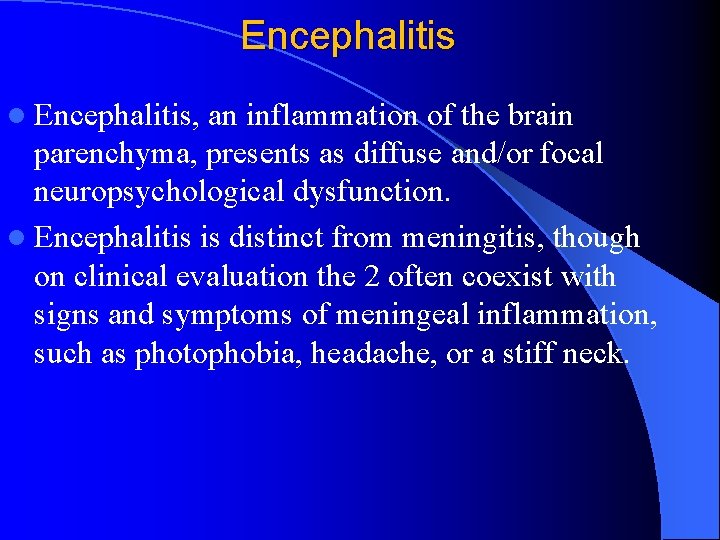
Encephalitis l Encephalitis, an inflammation of the brain parenchyma, presents as diffuse and/or focal neuropsychological dysfunction. l Encephalitis is distinct from meningitis, though on clinical evaluation the 2 often coexist with signs and symptoms of meningeal inflammation, such as photophobia, headache, or a stiff neck.
Encephalitis l Acute encephalitis is most commonly a viral infection with parenchymal damage varying from mild to profound l Subacute and chronic encephalopathies, most likely toxoplasmosis in immunocompromised patients
Encephalitis l Individuals at the extremes of age are at highest risk, particularly for HSE
Encephalitis l The classic presentation is encephalopathy with diffuse or focal neurologic symptoms, including the following: – Behavioral and personality changes, decreased level – – of consciousness Stiff neck, photophobia, and lethargy Generalized or localized seizures (60% of children with California encephalitis [CE]) Acute confusion or amnestic states Flaccid paralysis (10% with WNE)
Infectious etiologies of Encephalitis l l l l Viral agents, such as HSV type 1 and 2 (almost exclusively in neonates), VZV, EBV, Measles virus (PIE and SSPE), mumps, and rubella are spread through person-to-person contact. Human herpesvirus 6 may also be a causative agent. Bacterial pathogens, such as Mycoplasma species, rickettsial or cat-scratch disease, Toxoplasma gondii West Nile virus can be transmitted by means of an organ transplant and via blood transfusions.
Encephalitis l Laboratory tests (biochemical). l Viral serology l CT scan l EEE l CSF analysis
Encephalitis l The goal of treatment for acutely ill patients is administration of the first dose or doses acyclovir with or without antibiotics or steroids as quickly as possible l Look for and treat systemic complications, particularly in HSE, EEE, JE, such as hypotension or shock, hypoxemia, hyponatremia (SIADH), and exacerbation of chronic diseases
BRAIN ABSCESS l l l l Infrequent but not uncommon; pathogenesis diverse with contiguous spread & blood-borne seeding most common Clinical features include headache (90%), fever (57%), MS changes (67%), hemiparesis (61%), & papilledema (56%) Dx often suggested by neuroimaging (CT or MRI) LP is contraindicated due to risk of herniation Infxns often polymicrobial (strep, enteric GNRs, &/or anaerobes); S. aureus may cause abscesses in association with IE Other less common etiologies include Nocardia, fungi, M. tuberculosis, T. gondii, & neurocysticercosis Drainage often a necessary component of management
BRAIN ABSCESS Empiric Therapy Penicillin G Metronidazole 18 -24 mu IV qd 500 mg IV q 6 h Add nafcillin 12 gm/d if staph suspected (use vanc if MRSA a concern) l Add cefotaxime, ceftriaxone, or ceftazidime if GNRs suspected l Substitute vanc 2 -4 gm IV/d for pen G if DRSP suspected l
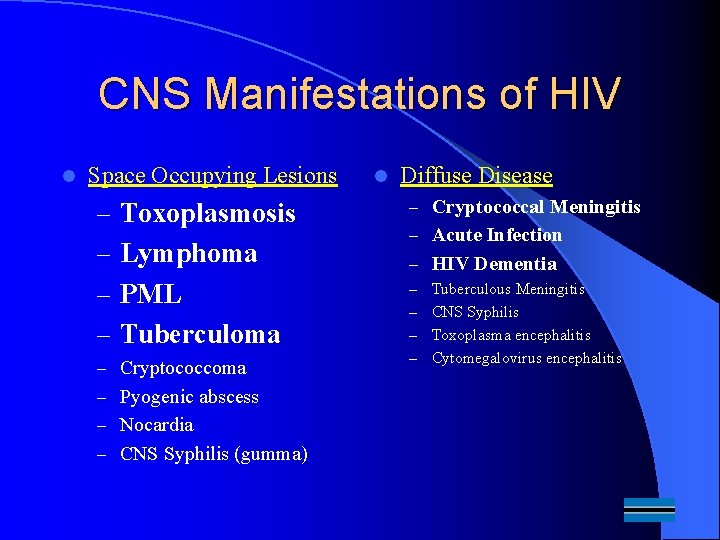
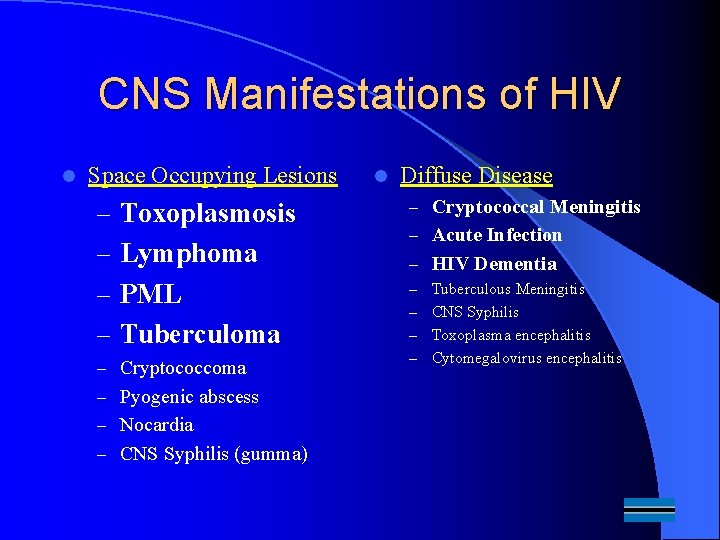
CNS Manifestations of HIV l Space Occupying Lesions – Toxoplasmosis – Lymphoma – PML – Tuberculoma – Cryptococcoma – Pyogenic abscess – Nocardia – CNS Syphilis (gumma) l Diffuse Disease – Cryptococcal Meningitis – Acute Infection – HIV Dementia Tuberculous Meningitis – CNS Syphilis – Toxoplasma encephalitis – Cytomegalovirus encephalitis –

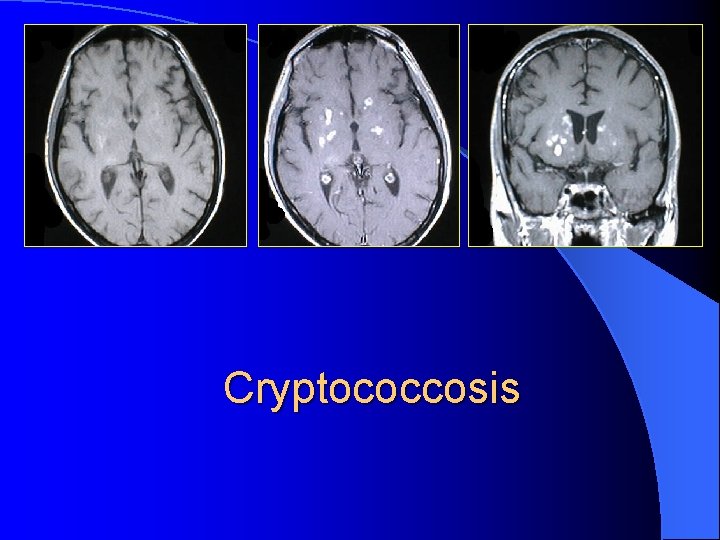
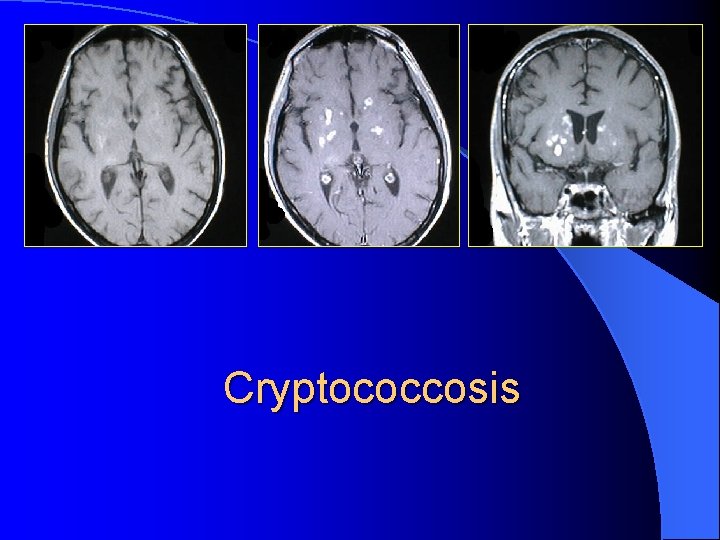
Cryptococcosis
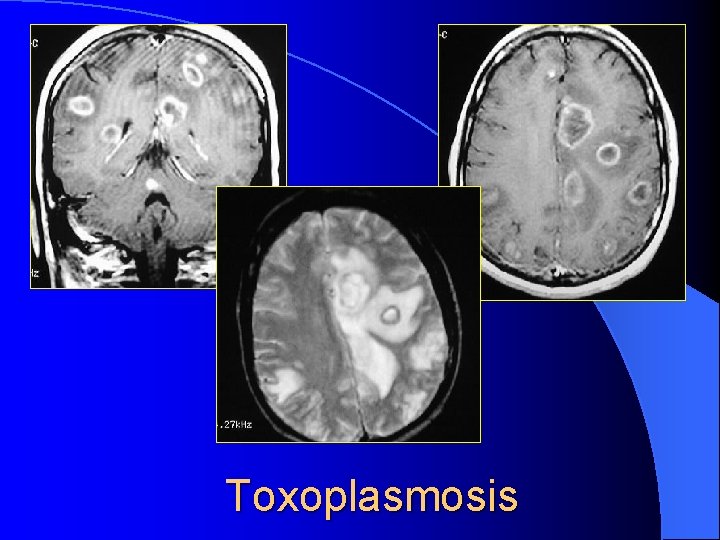
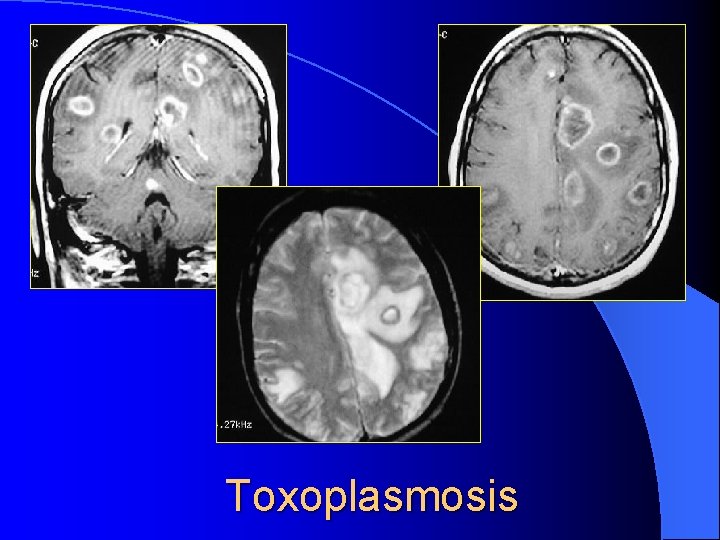
Toxoplasmosis
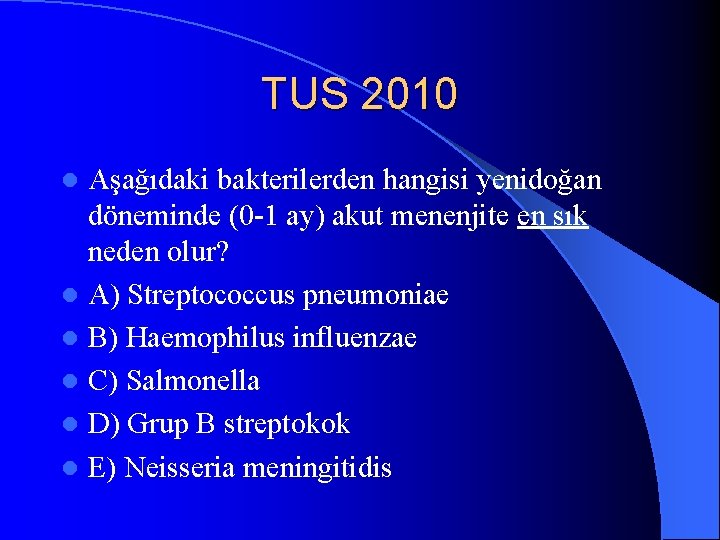
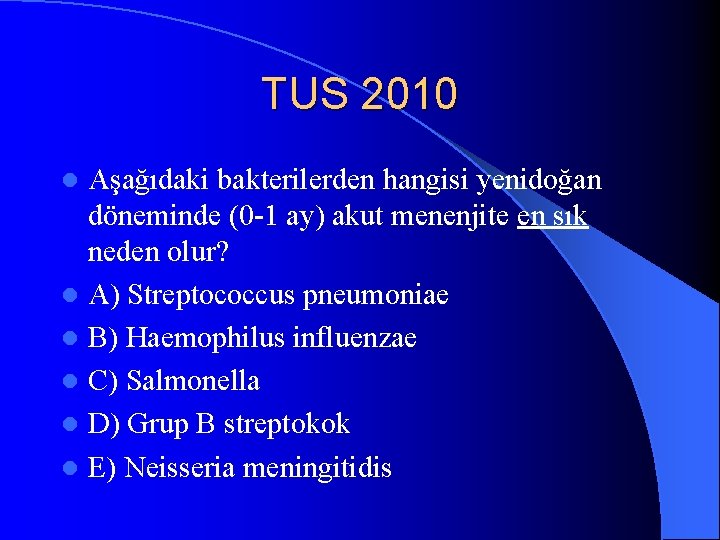
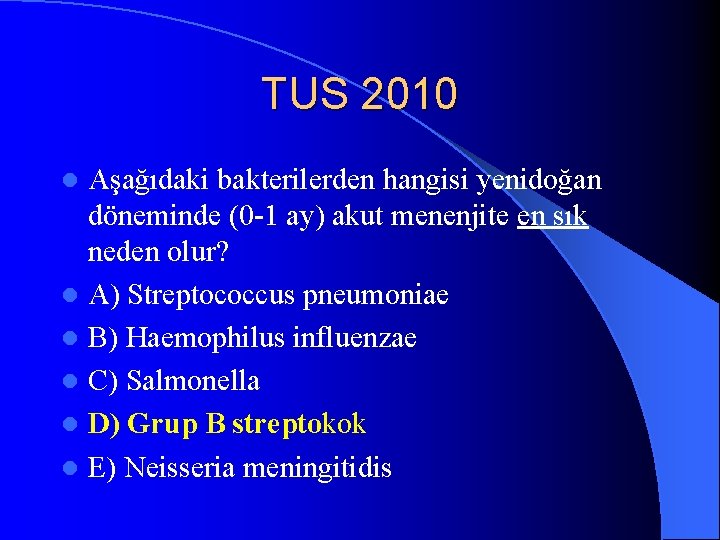
TUS 2010 Aşağıdaki bakterilerden hangisi yenidoğan döneminde (0 -1 ay) akut menenjite en sık neden olur? l A) Streptococcus pneumoniae l B) Haemophilus influenzae l C) Salmonella l D) Grup B streptokok l E) Neisseria meningitidis l
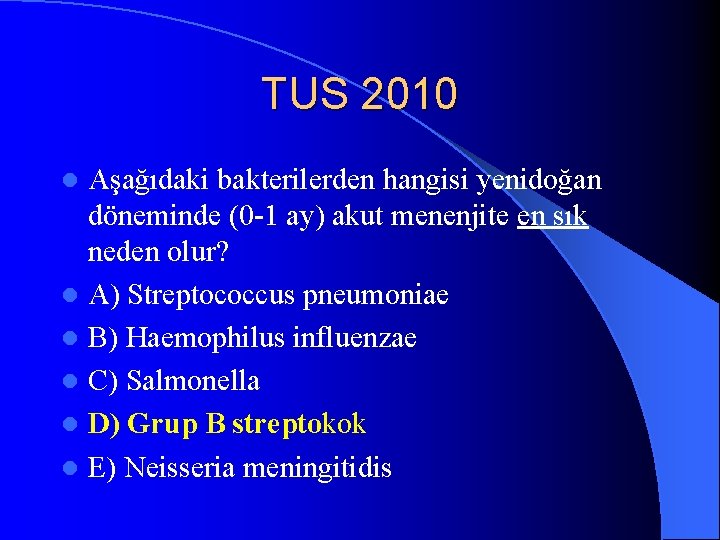
TUS 2010 Aşağıdaki bakterilerden hangisi yenidoğan döneminde (0 -1 ay) akut menenjite en sık neden olur? l A) Streptococcus pneumoniae l B) Haemophilus influenzae l C) Salmonella l D) Grup B streptokok l E) Neisseria meningitidis l
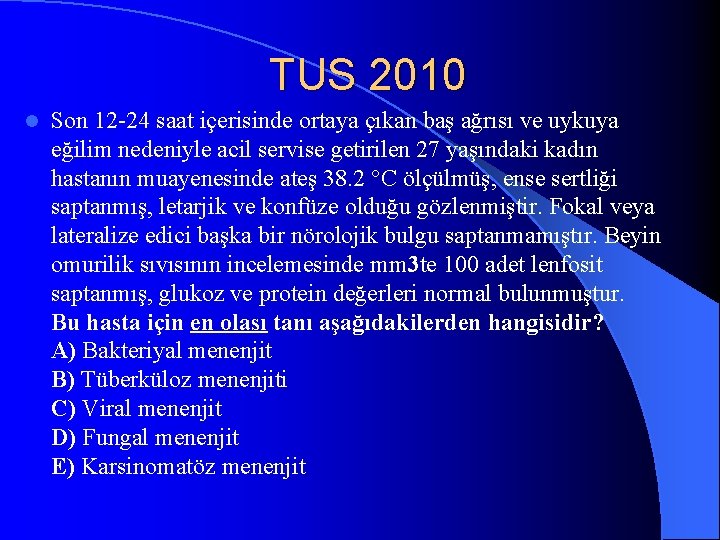
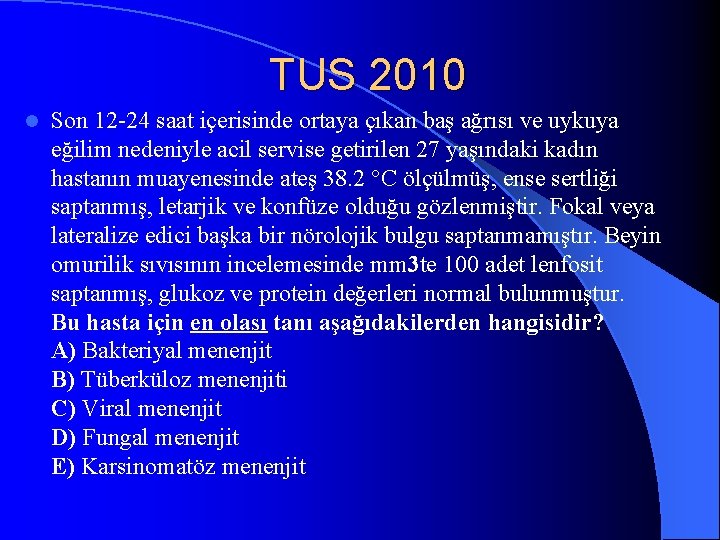
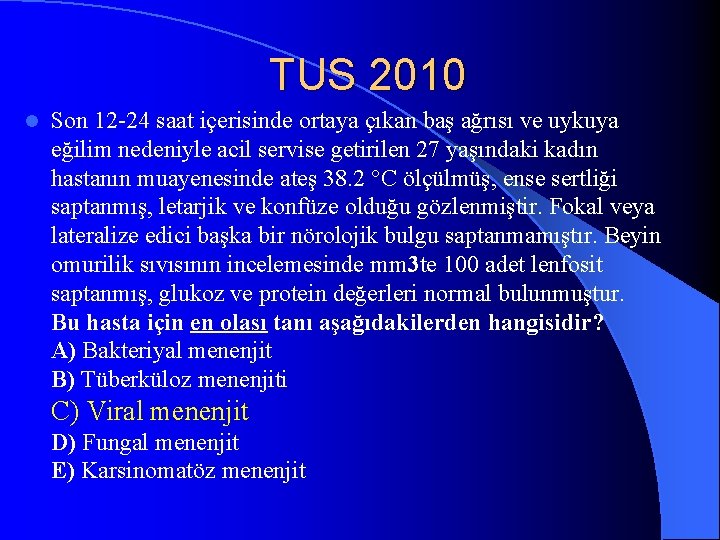
TUS 2010 l Son 12 -24 saat içerisinde ortaya çıkan baş ağrısı ve uykuya eğilim nedeniyle acil servise getirilen 27 yaşındaki kadın hastanın muayenesinde ateş 38. 2 °C ölçülmüş, ense sertliği saptanmış, letarjik ve konfüze olduğu gözlenmiştir. Fokal veya lateralize edici başka bir nörolojik bulgu saptanmamıştır. Beyin omurilik sıvısının incelemesinde mm 3 te 100 adet lenfosit saptanmış, glukoz ve protein değerleri normal bulunmuştur. Bu hasta için en olası tanı aşağıdakilerden hangisidir? A) Bakteriyal menenjit B) Tüberküloz menenjiti C) Viral menenjit D) Fungal menenjit E) Karsinomatöz menenjit
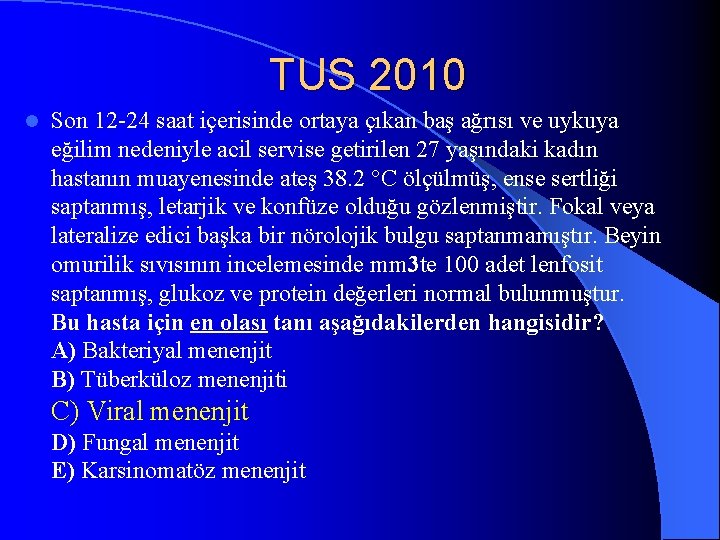
TUS 2010 l Son 12 -24 saat içerisinde ortaya çıkan baş ağrısı ve uykuya eğilim nedeniyle acil servise getirilen 27 yaşındaki kadın hastanın muayenesinde ateş 38. 2 °C ölçülmüş, ense sertliği saptanmış, letarjik ve konfüze olduğu gözlenmiştir. Fokal veya lateralize edici başka bir nörolojik bulgu saptanmamıştır. Beyin omurilik sıvısının incelemesinde mm 3 te 100 adet lenfosit saptanmış, glukoz ve protein değerleri normal bulunmuştur. Bu hasta için en olası tanı aşağıdakilerden hangisidir? A) Bakteriyal menenjit B) Tüberküloz menenjiti C) Viral menenjit D) Fungal menenjit E) Karsinomatöz menenjit
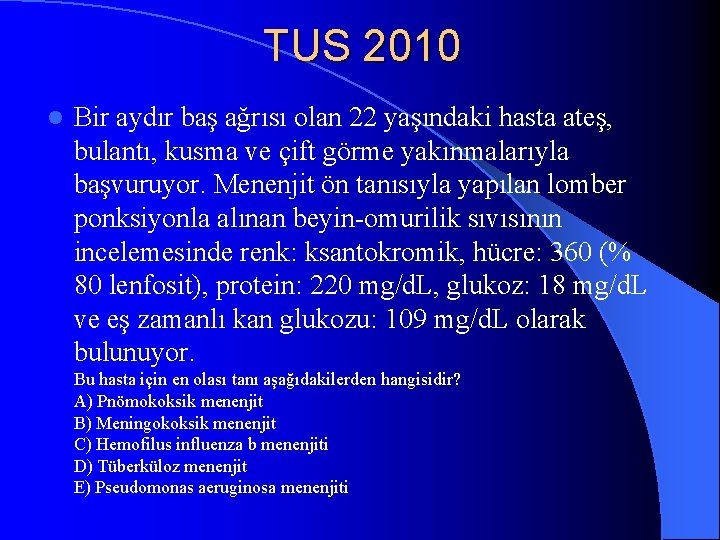
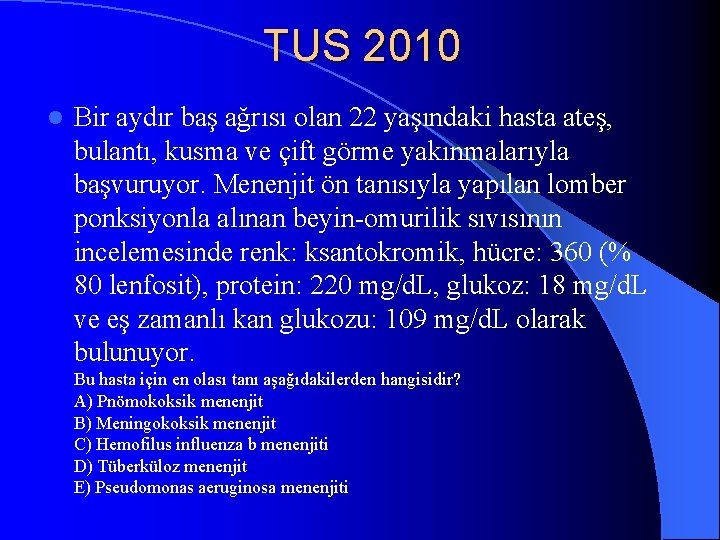
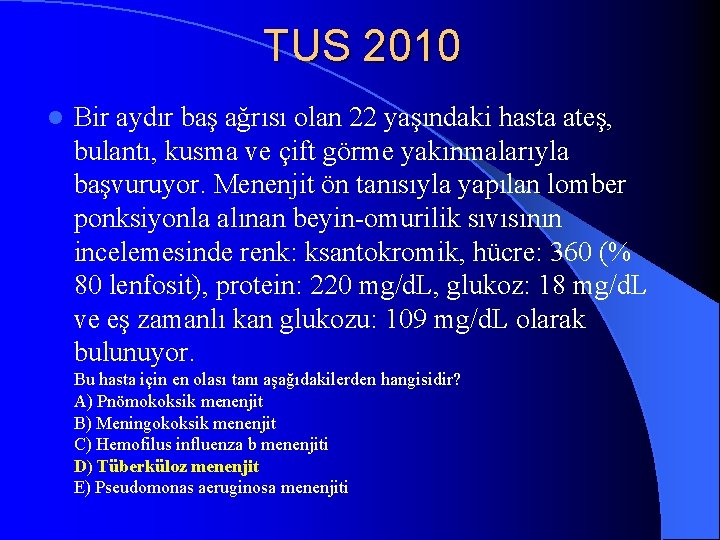
TUS 2010 l Bir aydır baş ağrısı olan 22 yaşındaki hasta ateş, bulantı, kusma ve çift görme yakınmalarıyla başvuruyor. Menenjit ön tanısıyla yapılan lomber ponksiyonla alınan beyin-omurilik sıvısının incelemesinde renk: ksantokromik, hücre: 360 (% 80 lenfosit), protein: 220 mg/d. L, glukoz: 18 mg/d. L ve eş zamanlı kan glukozu: 109 mg/d. L olarak bulunuyor. Bu hasta için en olası tanı aşağıdakilerden hangisidir? A) Pnömokoksik menenjit B) Meningokoksik menenjit C) Hemofilus influenza b menenjiti D) Tüberküloz menenjit E) Pseudomonas aeruginosa menenjiti
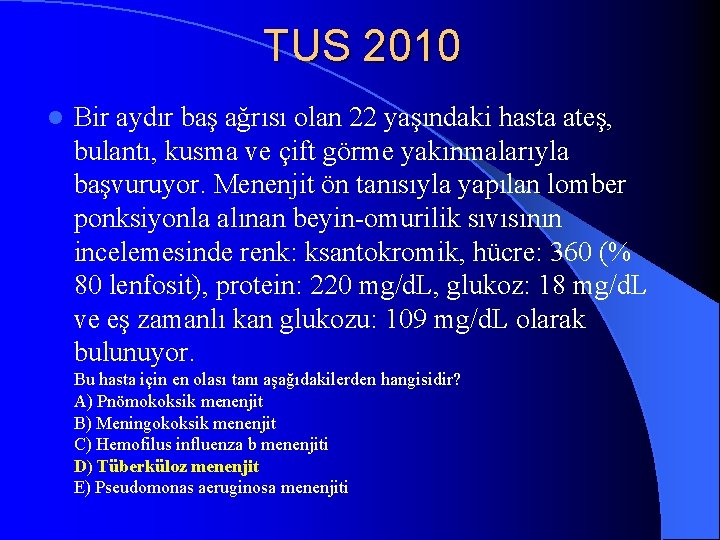
TUS 2010 l Bir aydır baş ağrısı olan 22 yaşındaki hasta ateş, bulantı, kusma ve çift görme yakınmalarıyla başvuruyor. Menenjit ön tanısıyla yapılan lomber ponksiyonla alınan beyin-omurilik sıvısının incelemesinde renk: ksantokromik, hücre: 360 (% 80 lenfosit), protein: 220 mg/d. L, glukoz: 18 mg/d. L ve eş zamanlı kan glukozu: 109 mg/d. L olarak bulunuyor. Bu hasta için en olası tanı aşağıdakilerden hangisidir? A) Pnömokoksik menenjit B) Meningokoksik menenjit C) Hemofilus influenza b menenjiti D) Tüberküloz menenjit E) Pseudomonas aeruginosa menenjiti
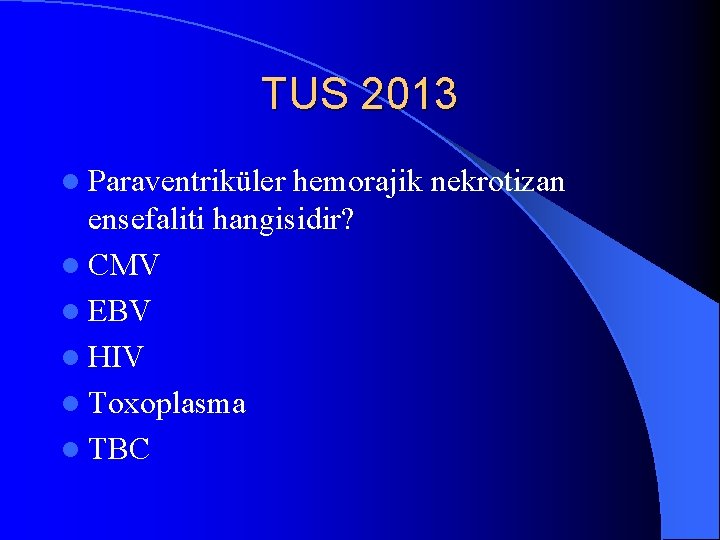
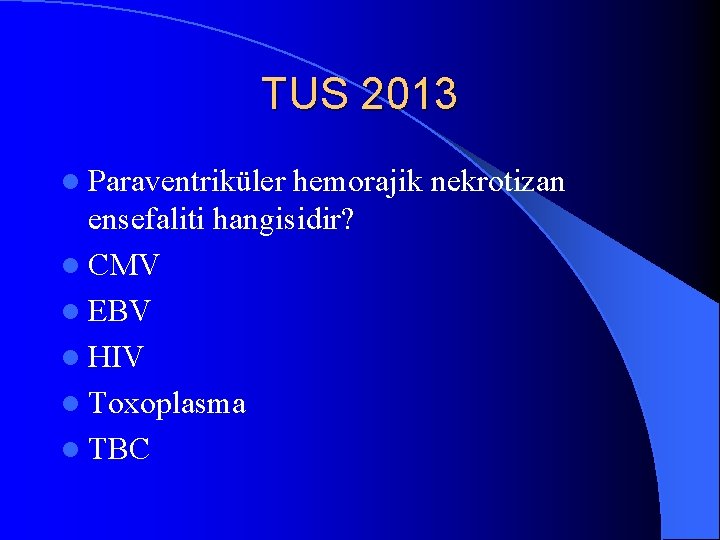
TUS 2013 l Paraventriküler hemorajik nekrotizan ensefaliti hangisidir? l CMV l EBV l HIV l Toxoplasma l TBC
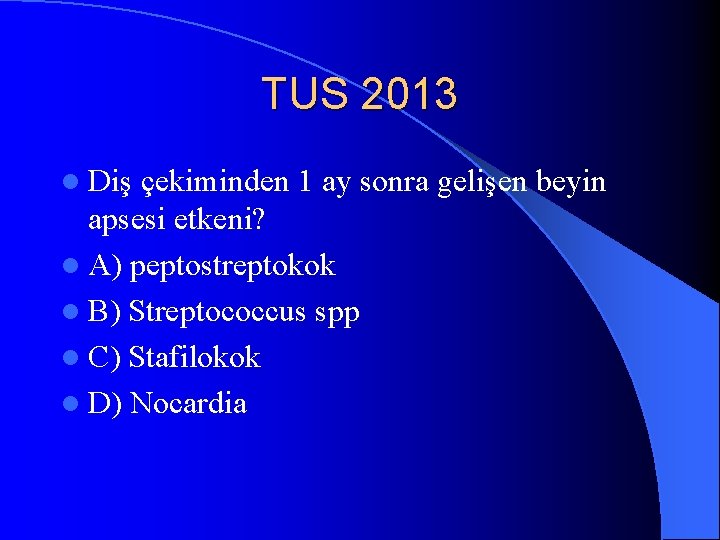
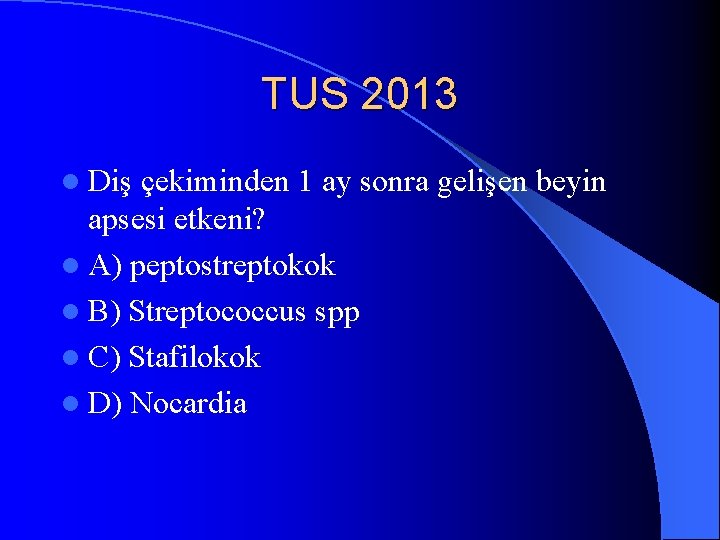
TUS 2013 l Diş çekiminden 1 ay sonra gelişen beyin apsesi etkeni? l A) peptostreptokok l B) Streptococcus spp l C) Stafilokok l D) Nocardia
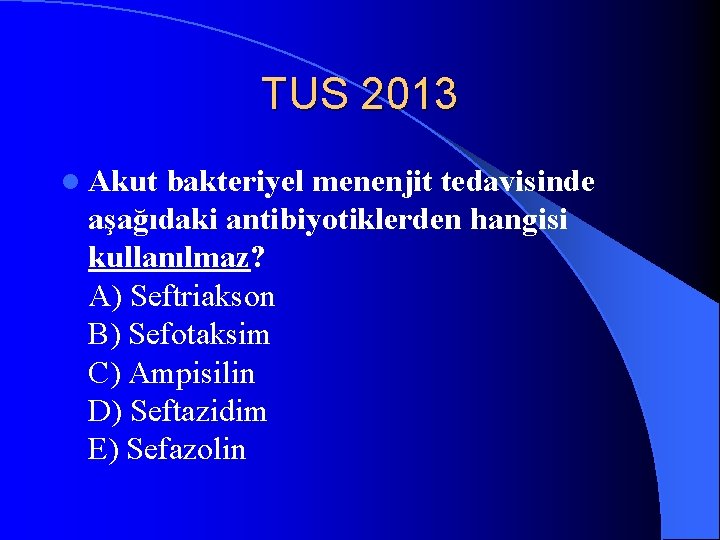
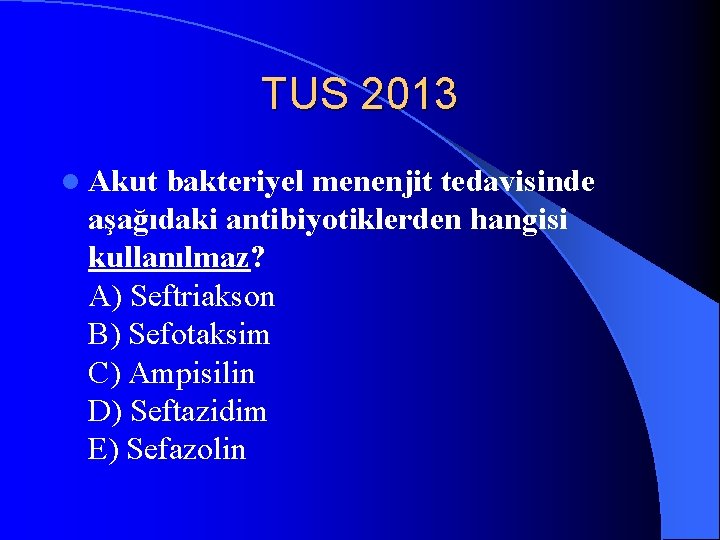
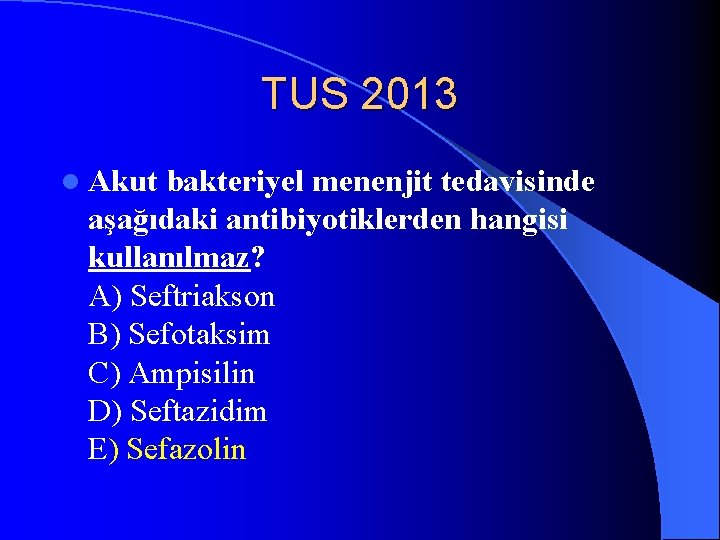
TUS 2013 l Akut bakteriyel menenjit tedavisinde aşağıdaki antibiyotiklerden hangisi kullanılmaz? A) Seftriakson B) Sefotaksim C) Ampisilin D) Seftazidim E) Sefazolin
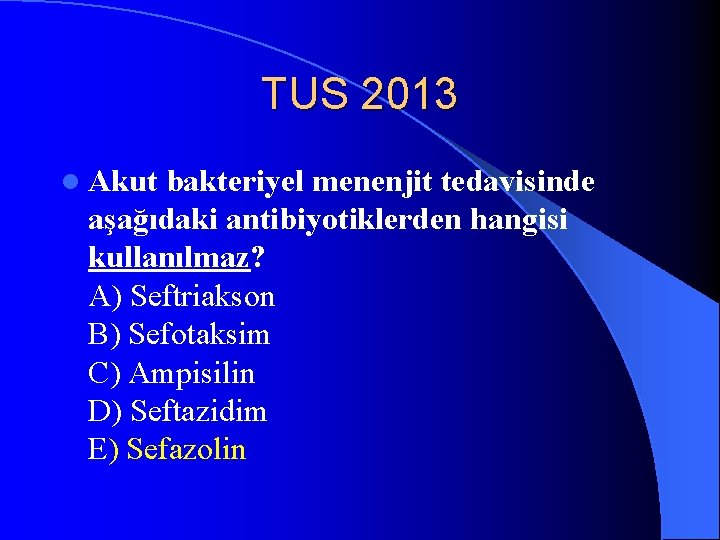
TUS 2013 l Akut bakteriyel menenjit tedavisinde aşağıdaki antibiyotiklerden hangisi kullanılmaz? A) Seftriakson B) Sefotaksim C) Ampisilin D) Seftazidim E) Sefazolin
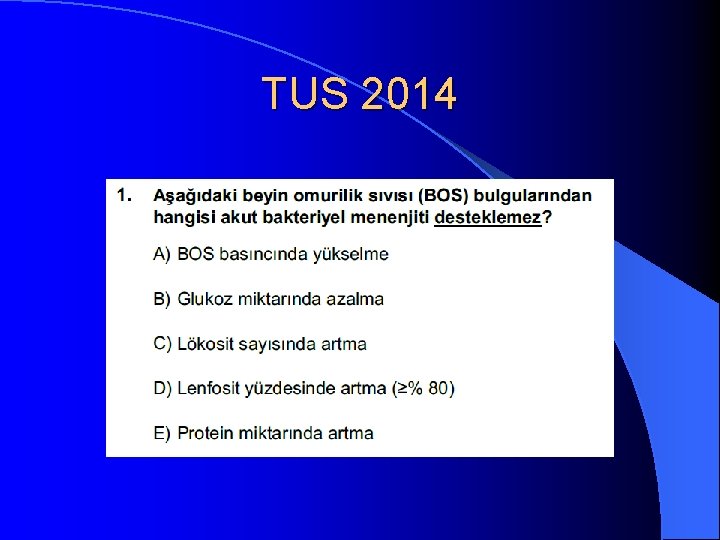
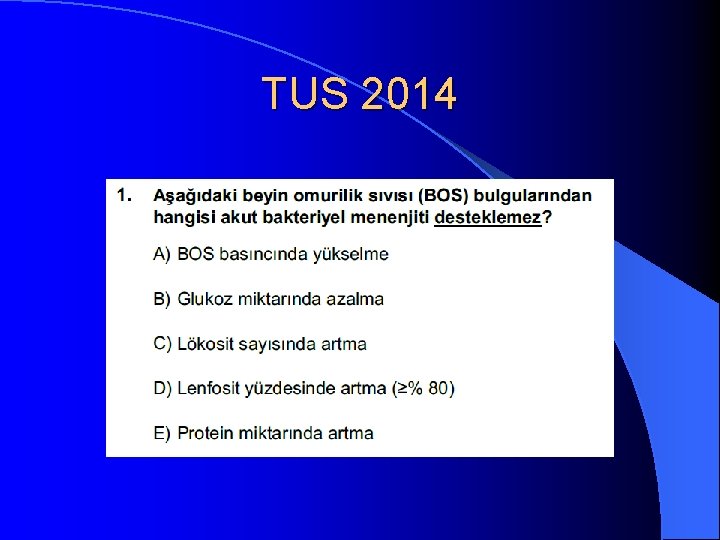
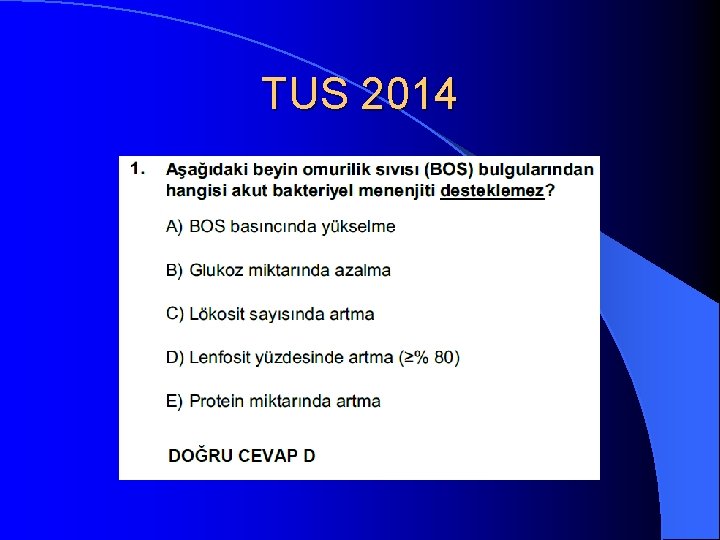
TUS 2014
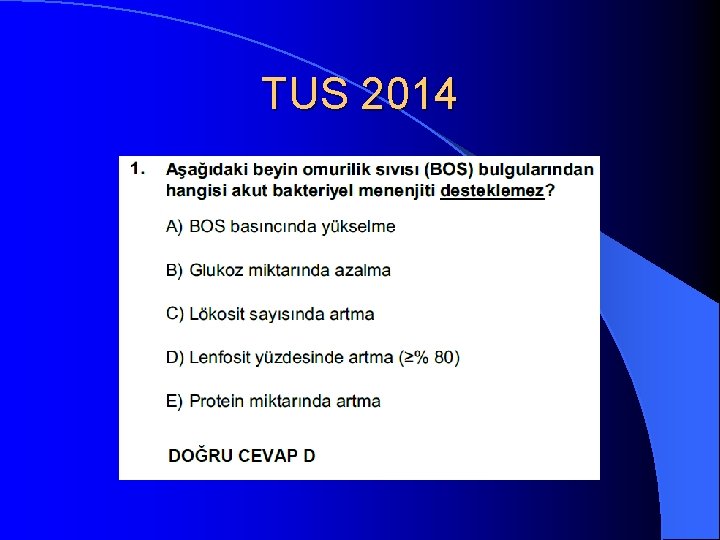
TUS 2014
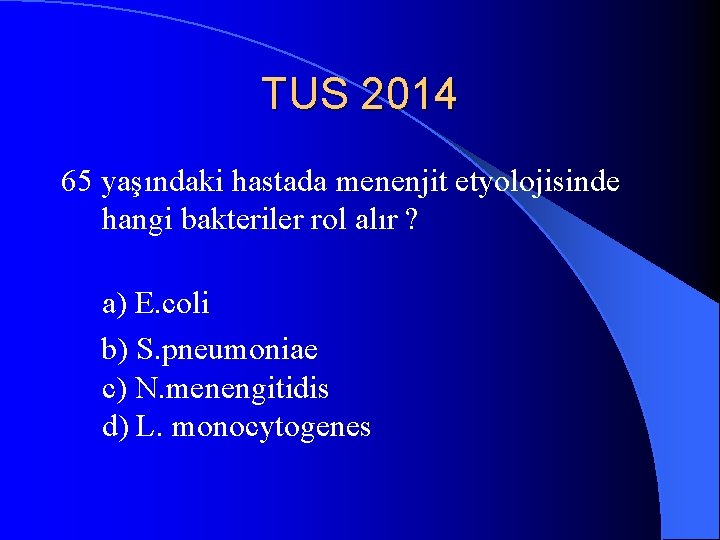
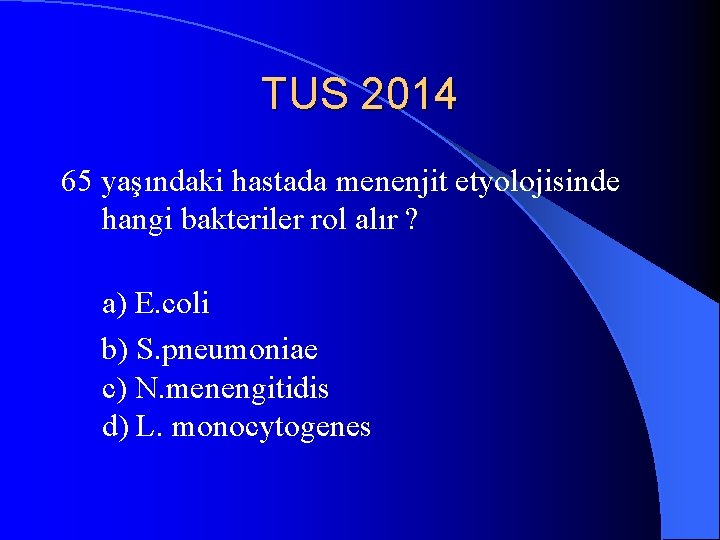
TUS 2014 65 yaşındaki hastada menenjit etyolojisinde hangi bakteriler rol alır ? a) E. coli b) S. pneumoniae c) N. menengitidis d) L. monocytogenes
 Infectous definition
Infectous definition Identify each type of neuronal pool
Identify each type of neuronal pool Nervous
Nervous Neuronal pools are collections of
Neuronal pools are collections of Meral yılmaz öğretmen
Meral yılmaz öğretmen Pınar seden meral
Pınar seden meral Meral nur ergin
Meral nur ergin Meral dogan
Meral dogan Büyükelçilik protokol sıra düzeni
Büyükelçilik protokol sıra düzeni Endocervix
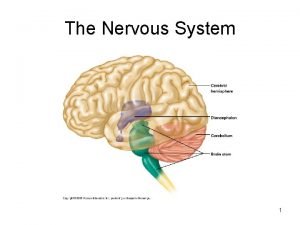
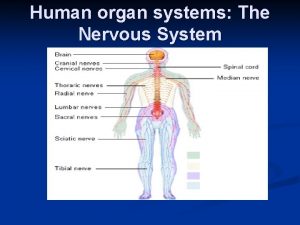
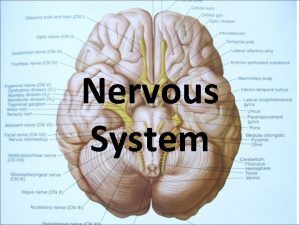
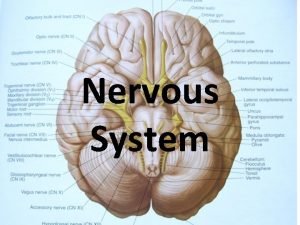
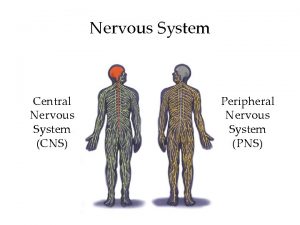
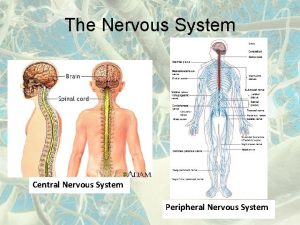
Endocervix Division of central nervous system
Division of central nervous system Central nervous system amusement park
Central nervous system amusement park Label the parts of the central nervous system
Label the parts of the central nervous system Nervous tissue
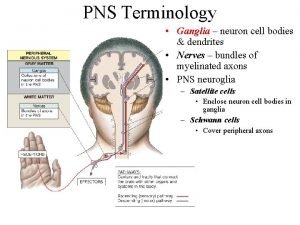
Nervous tissue Central and peripheral nervous system
Central and peripheral nervous system Bser aer
Bser aer What does this graph show
What does this graph show Central nervous system for kids
Central nervous system for kids Nervous system and digestive system
Nervous system and digestive system Endocrine system and nervous system
Endocrine system and nervous system General mechanism of hormone action
General mechanism of hormone action Endocrine system
Endocrine system Opportunistic infections
Opportunistic infections Can methotrexate cause yeast infections
Can methotrexate cause yeast infections Opportunistic infections
Opportunistic infections Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Johnson and johnson botnet infections
Johnson and johnson botnet infections Storch infections
Storch infections Storch infections
Storch infections Bone and joint infections
Bone and joint infections Infections opportunistes digestives
Infections opportunistes digestives Eye infections
Eye infections Postpartum infections
Postpartum infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Genital infections
Genital infections Amber blumling
Amber blumling Salmonella life cycle
Salmonella life cycle Classification of acute gingival infections
Classification of acute gingival infections Central nervous sysytem
Central nervous sysytem Chemical messengers of the nervous system
Chemical messengers of the nervous system Is flatworm asexual reproduction
Is flatworm asexual reproduction The nervous system is made up of
The nervous system is made up of Three basic functions of the nervous system
Three basic functions of the nervous system Learning objectives of nervous system
Learning objectives of nervous system Bipolar neuron function
Bipolar neuron function What is stimuli in nervous system
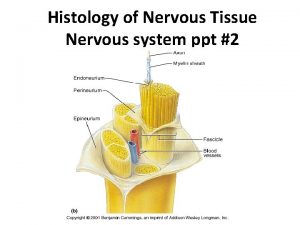
What is stimuli in nervous system Neuron bundle
Neuron bundle Visceral nervous system
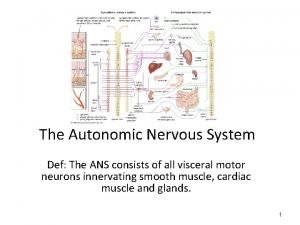
Visceral nervous system Ans
Ans Spinal nerve pairs
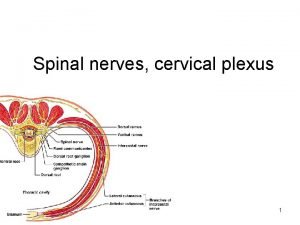
Spinal nerve pairs Sns somatic nervous system
Sns somatic nervous system Brain scienstructable
Brain scienstructable Skeletal muscle autonomic nervous system
Skeletal muscle autonomic nervous system Roundworms nervous system
Roundworms nervous system Arthropods respiratory system
Arthropods respiratory system Jointed foot phylum
Jointed foot phylum Nervous system of arthropods
Nervous system of arthropods Parasympathatic nervous system
Parasympathatic nervous system Nervous system in coelenterata
Nervous system in coelenterata Autonomic nervous system consists of
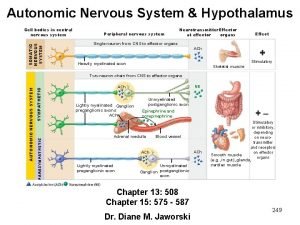
Autonomic nervous system consists of The body's speedy electrochemical communication network
The body's speedy electrochemical communication network Section 35-1 human body systems answer key
Section 35-1 human body systems answer key Autonomic nervous system pathway
Autonomic nervous system pathway L
L Basic unit of nervous system
Basic unit of nervous system What is a pathogen
What is a pathogen Histology of neuron ppt
Histology of neuron ppt Gray matter in the brain
Gray matter in the brain Comparison of endocrine and nervous system
Comparison of endocrine and nervous system 8 divisions of the nervous system
8 divisions of the nervous system How to take care of your nervous system
How to take care of your nervous system Effector cells in nervous system
Effector cells in nervous system Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Endocrine and nervous system comparison
Endocrine and nervous system comparison Beta-blockers for overactive sympathetic nervous system
Beta-blockers for overactive sympathetic nervous system Hypothalamus
Hypothalamus Ganglion on spine
Ganglion on spine Nervous system of silkworm
Nervous system of silkworm Section 35-3 divisions of the nervous system
Section 35-3 divisions of the nervous system Building block of the nervous system
Building block of the nervous system Structure of nervous system graphic organizer
Structure of nervous system graphic organizer Ganglion peripheral nervous system
Ganglion peripheral nervous system Classification of planaria
Classification of planaria Cnidae
Cnidae Rami ventralis
Rami ventralis Sympathetic and parasympathetic nervous system difference
Sympathetic and parasympathetic nervous system difference Learning objectives of nervous system
Learning objectives of nervous system Divisions of the nervous system
Divisions of the nervous system Limb apraxia
Limb apraxia Disorders of the nervous system
Disorders of the nervous system Sistem pencernaan osteichthyes
Sistem pencernaan osteichthyes How the nervous system works
How the nervous system works Nervous system of computer
Nervous system of computer Enteric plexus
Enteric plexus Pak pandani
Pak pandani Chapter 8 the nervous system
Chapter 8 the nervous system Nervous system
Nervous system Section 35-3 divisions of the nervous system
Section 35-3 divisions of the nervous system Autonomic nervous system
Autonomic nervous system Functional unit of nervous system
Functional unit of nervous system Digestive system theme park ideas
Digestive system theme park ideas The autonomic nervous system controls
The autonomic nervous system controls Why do animals need a nervous system
Why do animals need a nervous system The nervous system
The nervous system Nervous system function
Nervous system function