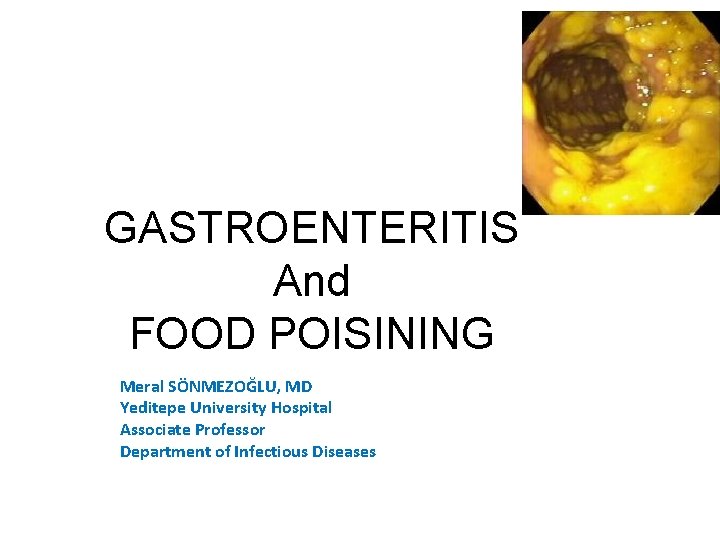
GASTROENTERITIS And FOOD POISINING Meral SNMEZOLU MD Yeditepe































- Slides: 143
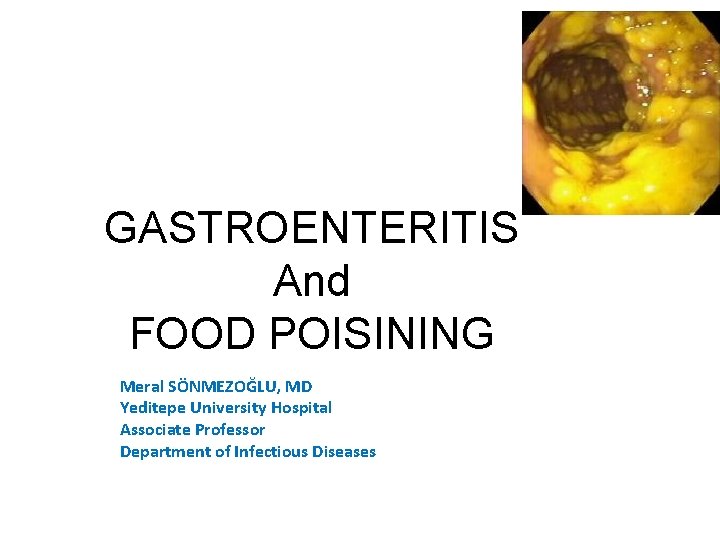
GASTROENTERITIS And FOOD POISINING Meral SÖNMEZOĞLU, MD Yeditepe University Hospital Associate Professor Department of Infectious Diseases and Microbiology
Learning Objectives – Describe and classify of gastroenteritis and food poisoning – Explain the epidemiology of gastroenteritis and possible etiologic agents in various clinical settings – Know the pathophysiology of gastroenteritis – Develop an information on diagnosis and management plan for gastroenteritis
• With the exception of Helicobacter pylori gastritis, the term gastroenteritis is applied to syndromes of diarrhea or vomiting that tend to involve noninflammatory infection in the upper small bowel or inflammatory infection in the colon
• Risk of acquiring a gastrointestinal infection varies greatly with age, living conditions, personal and cultural habits, and group exposures • The second epidemiologic determinant of risk for enteric infection is where you are • The third determinant of risk is when you are there. The majority of enteric illnesses in temperate climates occur during winter months. The opposite is true in tropical countries, where distinct summer peaks of illnesses are common. The role of rainfall is uncertain, and some adjacent areas with similar monsoon climates have opposite seasons of major diarrheal illnesses, as illustrated by the peak seasons for cholera
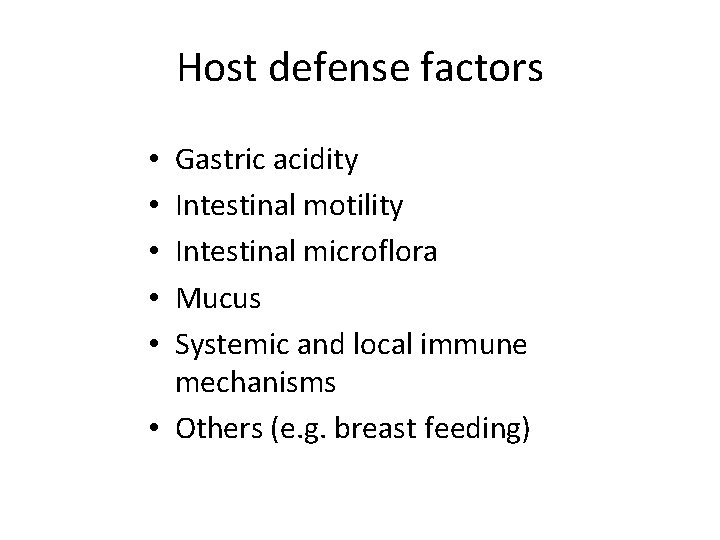
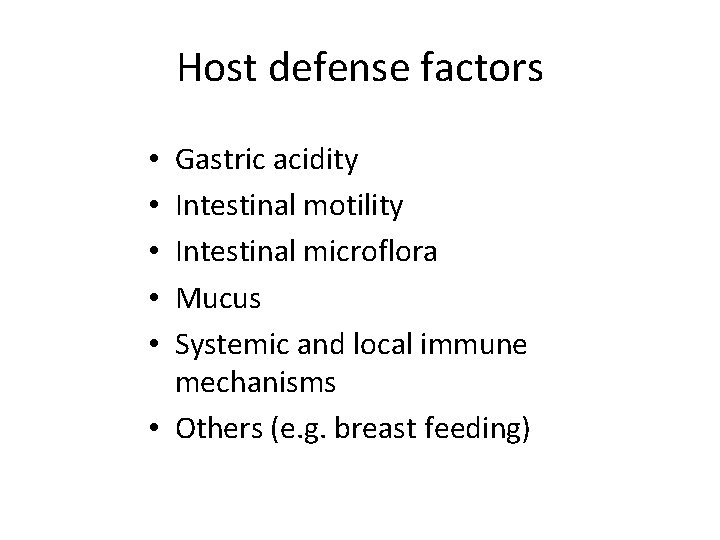
Host defense factors Gastric acidity Intestinal motility Intestinal microflora Mucus Systemic and local immune mechanisms • Others (e. g. breast feeding) • • •
Bacterial virulence factors • • Adherence Enterotoxin production Cytotoxin production Mucosal invasion
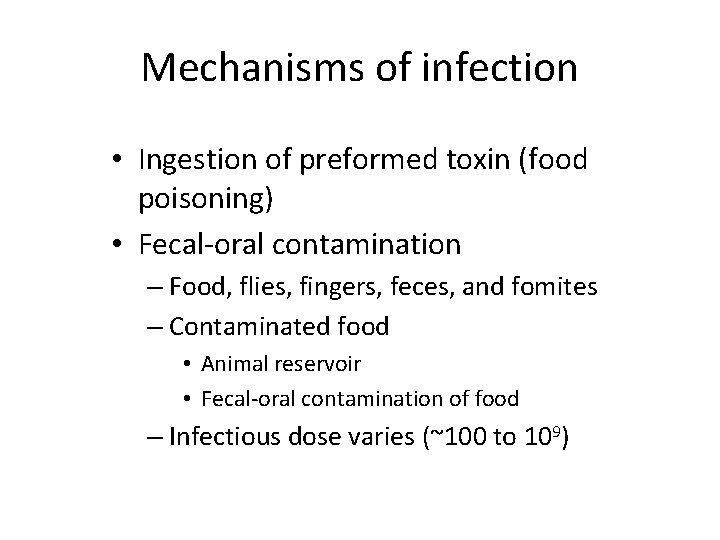
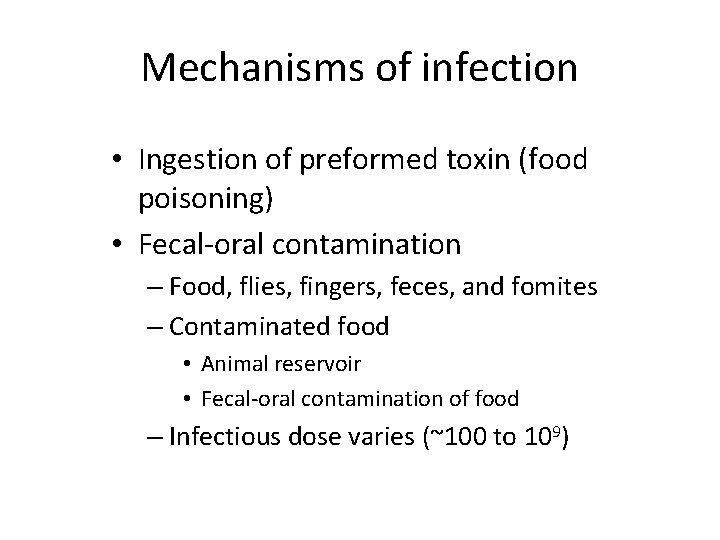
Mechanisms of infection • Ingestion of preformed toxin (food poisoning) • Fecal-oral contamination – Food, flies, fingers, feces, and fomites – Contaminated food • Animal reservoir • Fecal-oral contamination of food – Infectious dose varies (~100 to 109)
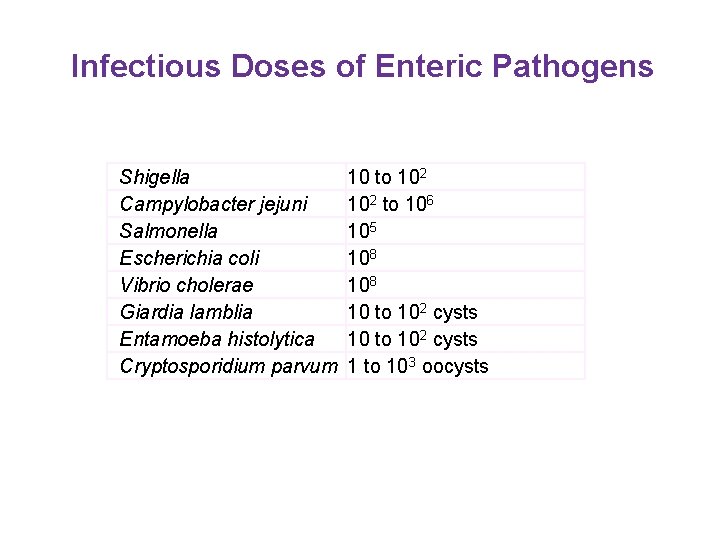
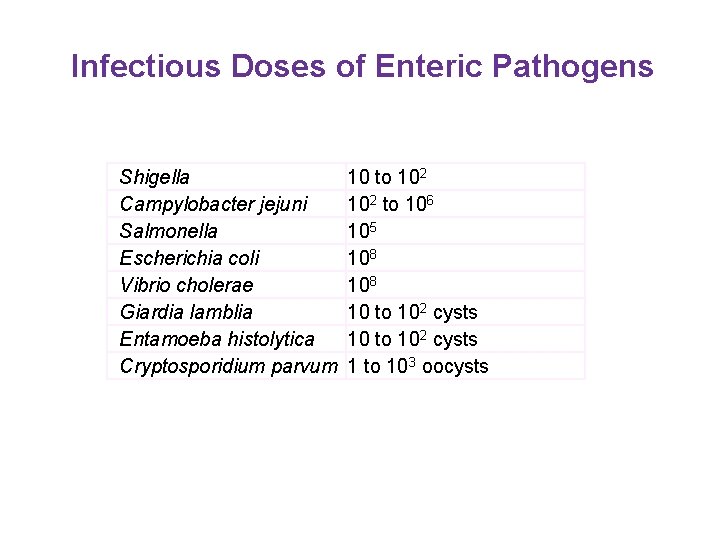
Infectious Doses of Enteric Pathogens Shigella Campylobacter jejuni Salmonella Escherichia coli Vibrio cholerae Giardia lamblia Entamoeba histolytica Cryptosporidium parvum 10 to 102 to 106 105 108 10 to 102 cysts 1 to 103 oocysts
DIARRHEA • Alteration in a normal bowel movement • Characterized by an increased in the water content, volume, or frequency of stools • >3 or more stools and at least 200 gr • Decrease in consistency (soft or liquid) and an increase in frequency of bowel movement to >3 stools per day
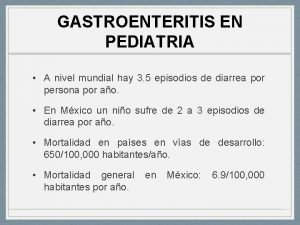
INFECTIOUS DIARRHEA • 3 -5 billion episodes yearly • Major cause of worldwide morbidity and mortality • 5 million deaths yearly, 80% < 1 year of age • Major cause of work/school absenteeism • Major economic burden, especially in developing countries
INFECTIOUS DIARRHEA • Due to an infectious etiology • Accompanied by symptoms of nausea, vomiting, or abdominal cramps. • Acute diarrhea is an episode of diarrhea of <14 days in duration • Persistent diarrhea is of >14 days in duration • Chronic diarrhea lasts >30 days
INFECTIOUS DIARRHEA • Second leading cause of morbidity and mortality worldwide • More than 2 million deaths annually • Some causes of infectious diarrhea result in serious long term sequelae (HUS-STEC, G-B Campylobacter)
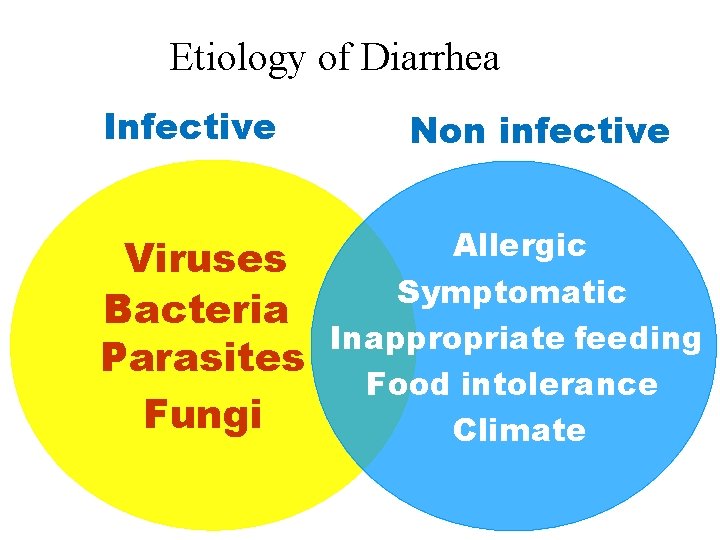
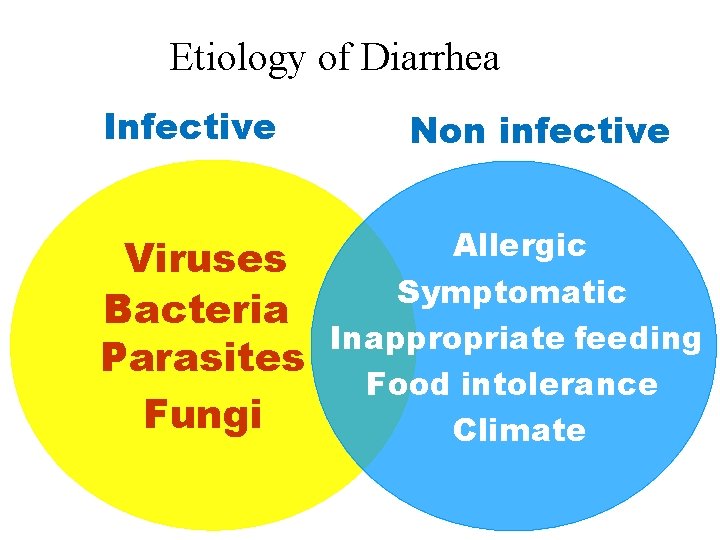
Etiology of Diarrhea Infective Non infective Viruses Bacteria Parasites Fungi Allergic Symptomatic Inappropriate feeding Food intolerance Climate
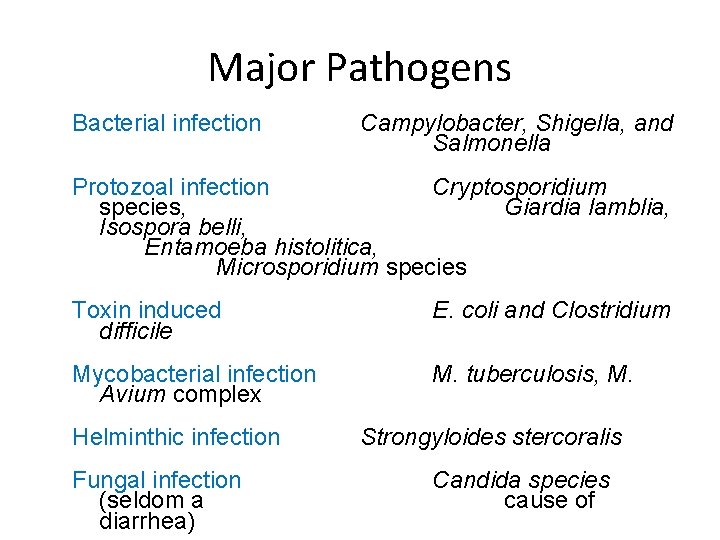
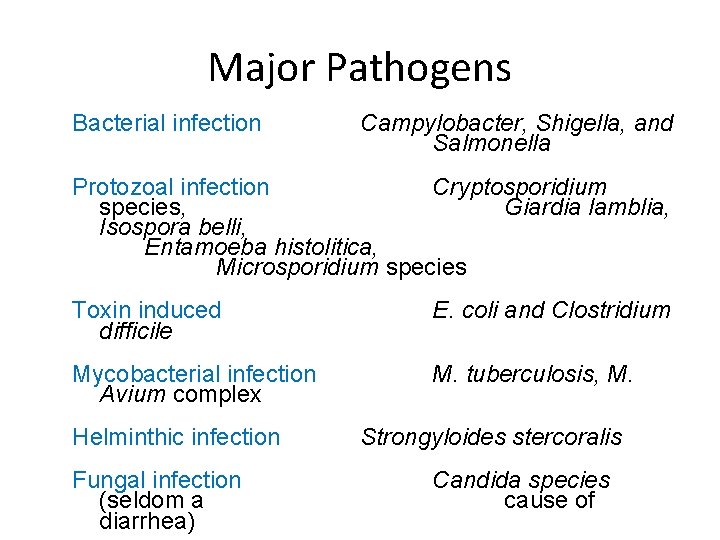
Major Pathogens Bacterial infection Campylobacter, Shigella, and Salmonella Protozoal infection Cryptosporidium species, Giardia lamblia, Isospora belli, Entamoeba histolitica, Microsporidium species Toxin induced difficile E. coli and Clostridium Mycobacterial infection Avium complex M. tuberculosis, M. Helminthic infection Fungal infection (seldom a diarrhea) Strongyloides stercoralis Candida species cause of
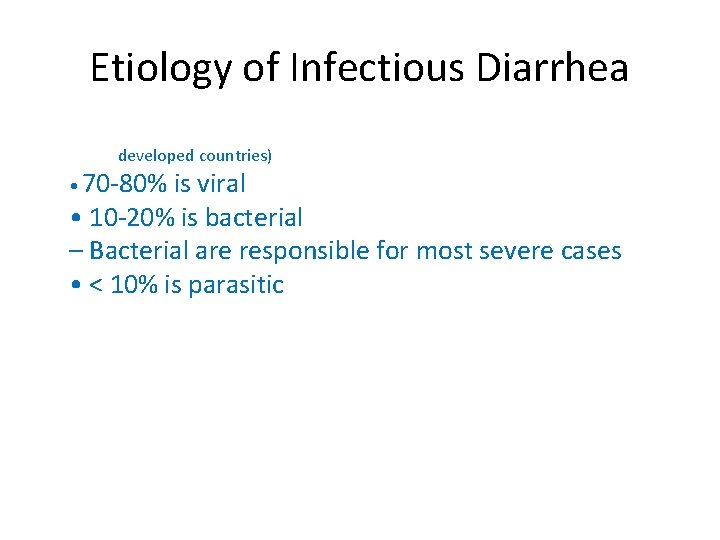
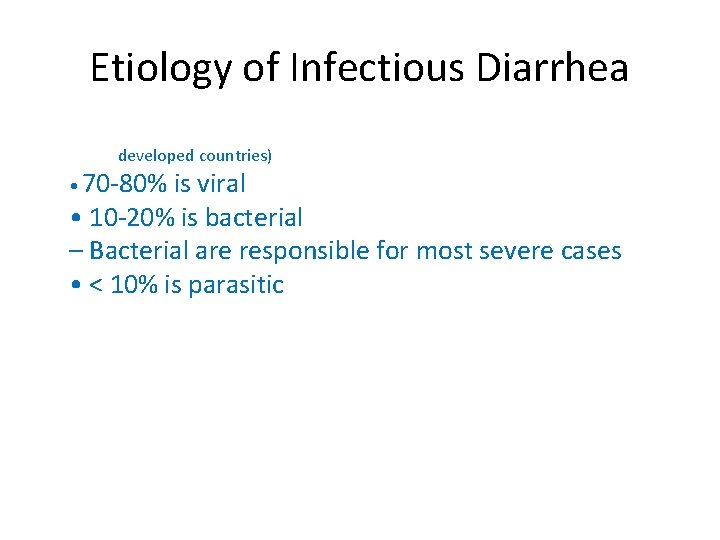
Etiology of Infectious Diarrhea (in (((8 developed countries) • 70 -80% is viral • 10 -20% is bacterial – Bacterial are responsible for most severe cases • < 10% is parasitic
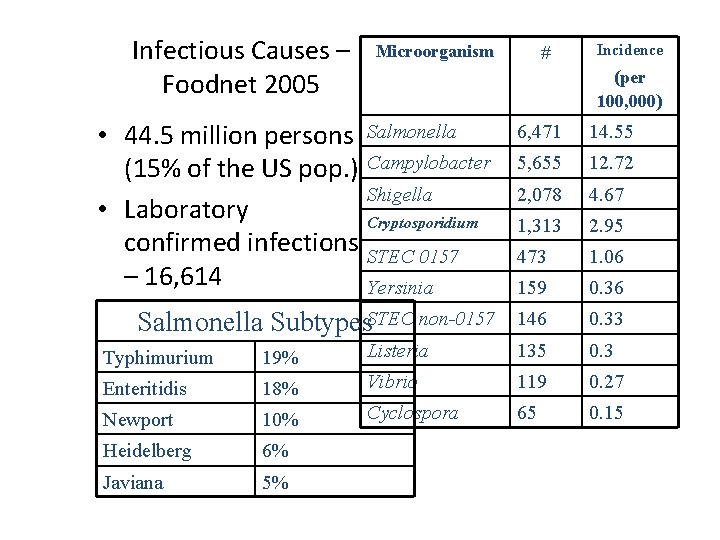
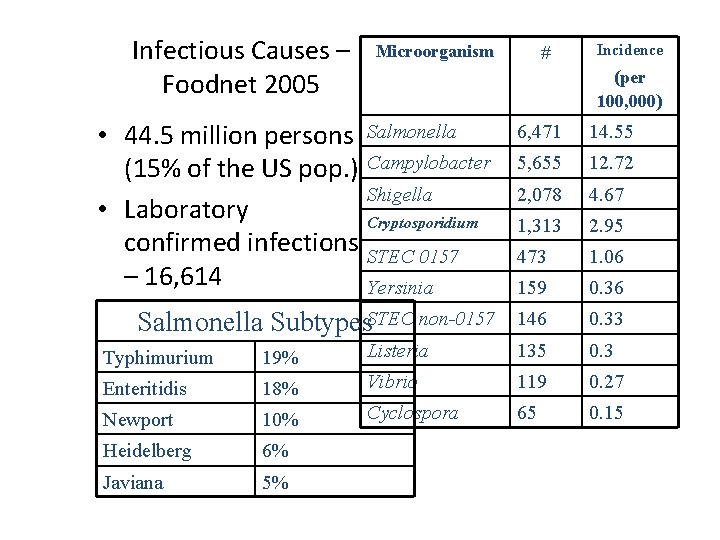
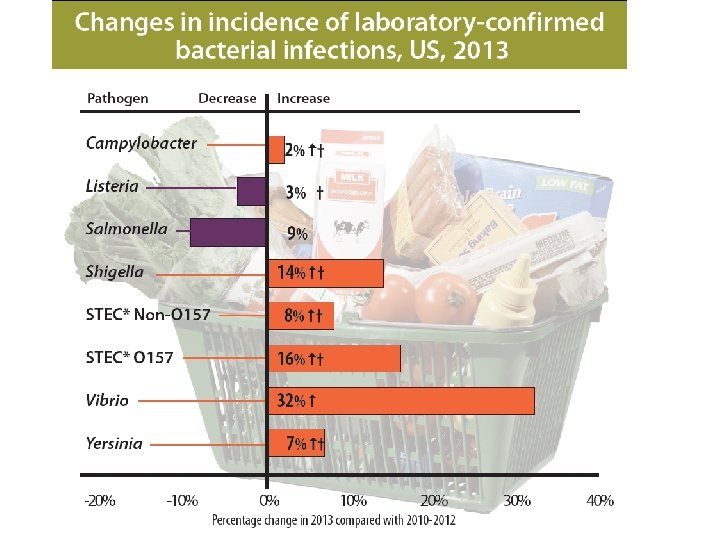
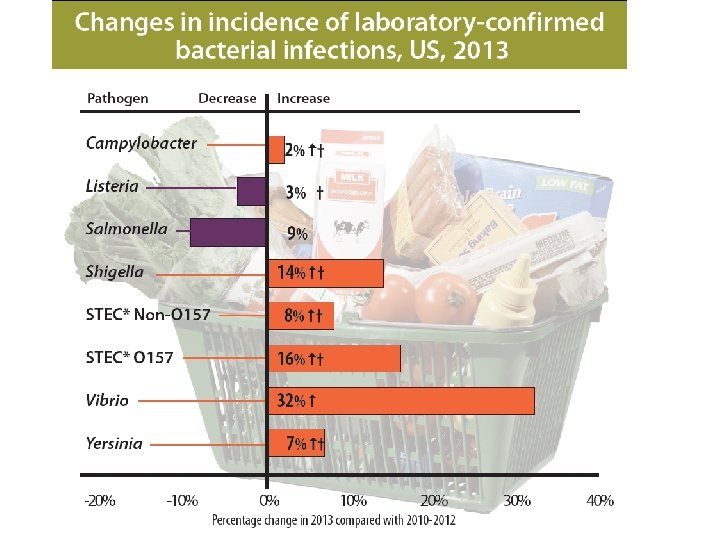
Infectious Causes – Foodnet 2005 Microorganism # Incidence (per 100, 000) • 44. 5 million persons Salmonella (15% of the US pop. ) Campylobacter Shigella • Laboratory Cryptosporidium confirmed infections STEC 0157 – 16, 614 Yersinia Salmonella Subtypes. STEC non-0157 6, 471 14. 55 5, 655 12. 72 2, 078 4. 67 1, 313 2. 95 473 1. 06 159 0. 36 146 0. 33 Typhimurium 19% Listeria 135 0. 3 Enteritidis 18% Vibrio 119 0. 27 Newport 10% Cyclospora 65 0. 15 Heidelberg 6% Javiana 5%

Mechanisms of infection • Ingestion of preformed toxin (food poisoning) • Fecal-oral contamination – Food, flies, fingers, feces, and fomites – Contaminated food • Animal reservoir • Fecal-oral contamination of food – Infectious dose varies (~100 to 109)

Host defense factors • • • Gastric acidity Intestinal motility Intestinal microflora Mucus Systemic and local immune mechanisms Others (e. g. breast feeding)

Defense Barriers of the Enterocytes 1 1. 3 Physical barrier: mucus 2. Bacteriological (flora) 3. Immunological: Secretory Ig. A 2

Morphology of Intestinal Mucosa Villi covered mainly (90%) by tall columnar absorptive cells (Enterocytes) having a micrevillar brush border Crypts of lieberkuhn Covered mainly by short columnar secretory cells Goblet cells without brush 23 border
Bacterial virulence factors • • Adherence Enterotoxin production Cytotoxin production Mucosal invasion
Diarrhea • Non-inflammatory – Watery diarrhea, no blood or mucus or pus in stool, no fever or systemic signs – Secretory or osmotic mechanism – Dehydration may occur – Generally self-limited and more benign – Therapy generally supportive • Inflammatory – Frequent lower volume stool, mucoid, bloody, or purulent. Often with fever or systemic signs, tenesmus, urgency – Exudative mechanism – Dehydration rare – Less benign
Osmotic Diarrhea Definition: Increased amounts of poorly absorbed, osmotically active solutes in gut lumen • Interferes with absorption of water • Solutes are ingested – Magnesium sulfate or citrate or magnesium containing antacids – Sorbitol – Malabsorption of food • Lactase deficiency • Celiac sprue • Variety of infectious organisms (particularly viruses)

Secretory Diarrhea • Excess secretion of electrolytes and water across mucosal surface • Usually coupled with inhibition of absorption • Clinical features – stools very watery – stool volume large – fasting does not stop diarrhea
Secretory Diarrhea • Bacterial or viral enterotoxins – Cholera, enterotoxigenic E. coli, B. cereus, S. aureus, Rotavirus, Norwalk virus • Hormonal secretagogues • Certain laxatives (castor oil, senna)
Exudative Diarrhea • Intestinal or colonic mucosa inflamed and ulcerated – Leakage of fluid, blood, pus – Impairment of absorption – Increased secretion (prostaglandins) • The extent of bowel involved determines – Severity of diarrhea – Systemic signs and symptoms (abdominal pain, fever, etc)
Exudative Diarrhea • Infectious, invasive organisms – Shigella, Campylobacter, Yersinia, E. histolytica, EHEC, C diff • Idiopathic inflammatory bowel disease – Crohns disease – Ulcerative Colitis • Ischemia
• • Associated Signs & Symptoms • Systemic illness/fever – invasive pathogen involvement • Vomiting as predominant symptom – likely viral organism or food poisoning • Abdominal pain – inflammatory process (Shigella, Campylobacter, EHEC) • Persistent abdominal pain and fever: Yersinia
When to Consider ABX Most cases of diarrhea resolve spontaneously and do not require treatment with antibiotics. Antibiotic therapy may be considered however, in the following circumstances: – When signs and symptoms include: • Fever • Bloody stools • Presence of fecal leukocytes or occult blood; – To reduce fecal excretion and environmental contamination by a highly infectious agent like Shigella; – For persistent or life-threatening diarrheal infections such as cholera; – For immunocompromised patients.
Antibiotics • Most helpful for: – Shigella, ETEC, ameobiasis, Giardia, cholera, S. typhi • May help for: – non-typhi Salmonella & Camplyobacter • Can prolong fecal shedding, use only if severe case • Not useful for viral, EIEC • Can be harmful in EHEC (O 157: H 7) • Multi-Drug resistance is a rapidly growing problem
Acute infectious diarrhea Bacterial infection Common nonbacterial infection HKO antigens Common among population – particular day care centers • Developing countries – serious health effects, fatal • In the U. S. , 1/3 due to contaminated food • • 34

HKO antigens • • H = flagellar antigen K= capsular antigen O= cell wall antigen Ex. E. coli O 157: H 7 35
Bacterial • • Salmonella Shiga-toxin producing Escherichia coli Non-shiga-toxin E. coli Campylobacter Yersinia Clostridium difficile Vibrio cholerae 36
Acute Diarrhea in Children The most important infective causes of acute diarrhea in developing countries in children are: • Rotavirus • Enterotoxigenic escherichia coli • Shigella • Campylobacter jejuni • Salmonella typhimurium 37
Salmonella • • Contaminated animal products Salmonellosis - mild Typhoid fever – severe Normal flora in animals 38
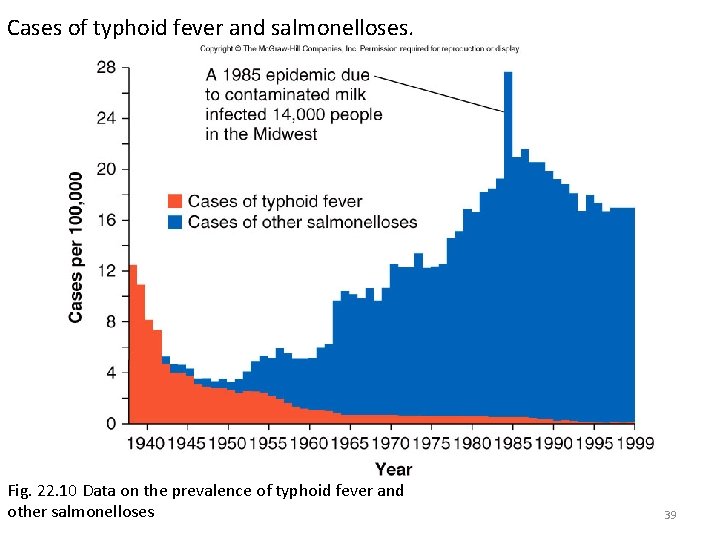
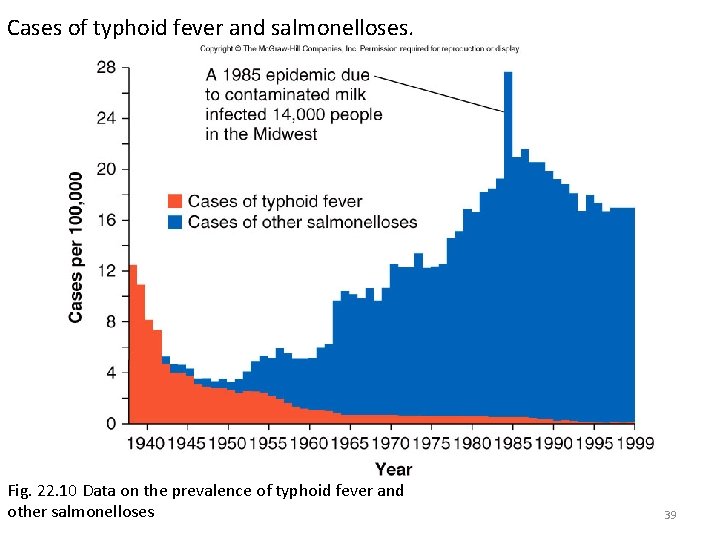
Cases of typhoid fever and salmonelloses. Fig. 22. 10 Data on the prevalence of typhoid fever and other salmonelloses 39
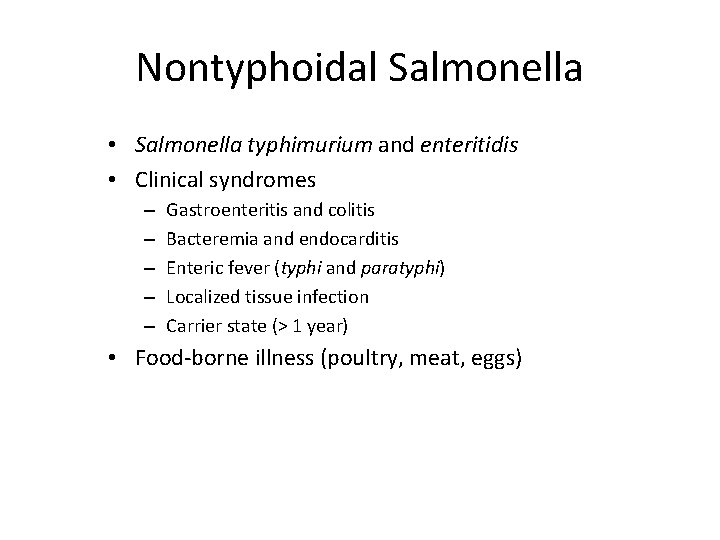
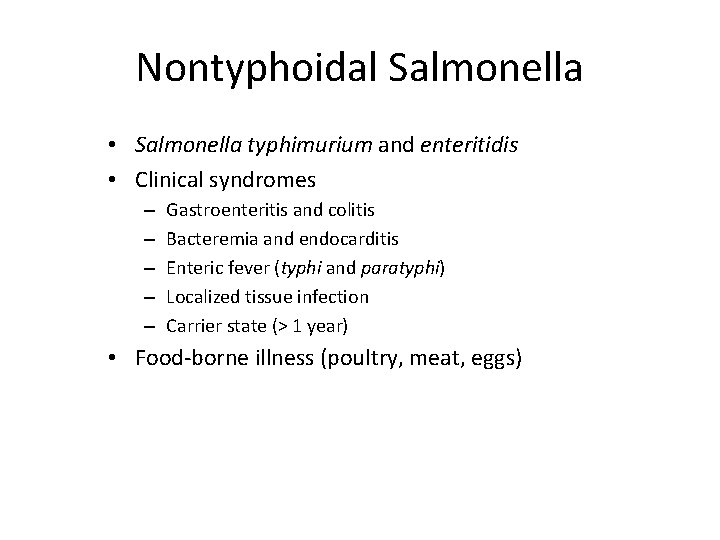
Nontyphoidal Salmonella • Salmonella typhimurium and enteritidis • Clinical syndromes – – – Gastroenteritis and colitis Bacteremia and endocarditis Enteric fever (typhi and paratyphi) Localized tissue infection Carrier state (> 1 year) • Food-borne illness (poultry, meat, eggs)
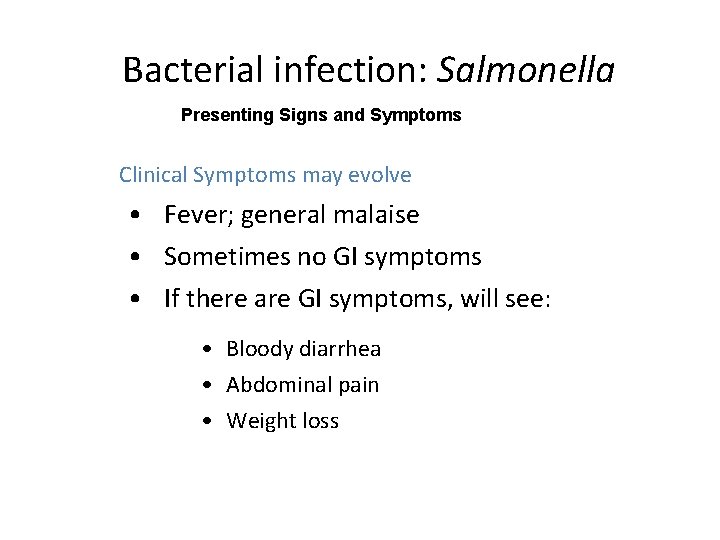
Bacterial infection: Salmonella Presenting Signs and Symptoms • Clinical Symptoms may evolve • Fever; general malaise • Sometimes no GI symptoms • If there are GI symptoms, will see: • Bloody diarrhea • Abdominal pain • Weight loss
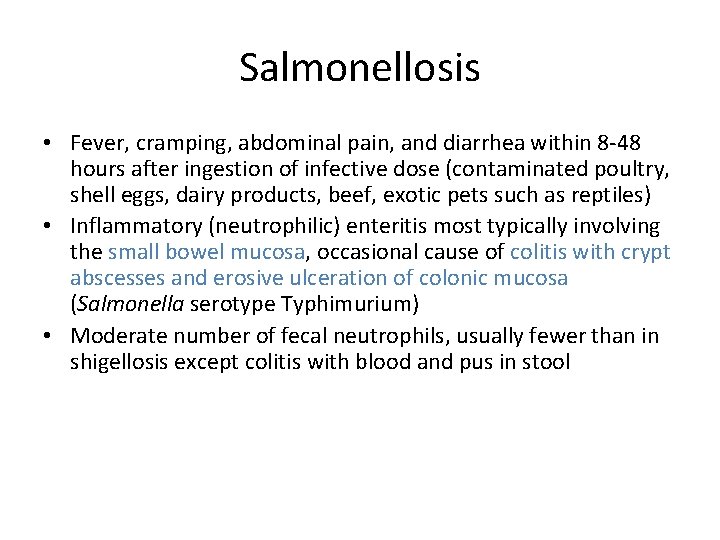
Salmonellosis • Fever, cramping, abdominal pain, and diarrhea within 8 -48 hours after ingestion of infective dose (contaminated poultry, shell eggs, dairy products, beef, exotic pets such as reptiles) • Inflammatory (neutrophilic) enteritis most typically involving the small bowel mucosa, occasional cause of colitis with crypt abscesses and erosive ulceration of colonic mucosa (Salmonella serotype Typhimurium) • Moderate number of fecal neutrophils, usually fewer than in shigellosis except colitis with blood and pus in stool
Complications of Salmonellosis • Diarrhea usually self-limited (3 -7 days), if persists >10 days another microbial etiology likely • Occasional dehydration requiring hospitalization • Bacteremia (1 -4% immunocompetent cases) (persistent bacteremia suggests endovascular infection site such as atherosclerotic plaques and aneurysms) • After resolution of diarrhea mean duration of carriage in stool is 4 -5 weeks

Bacterial infection: Salmonella Diagnostics • Stool culture • Salmonella bacilli may be found in stool/blood cultures • Serology: positive Widal test with increased titers
Management and Treatment • • • • TMP/SMX 960 mg bid or Chloramphenicol 250 mg qid for 3 weeks In case of sepsis, IV therapy is necessary Shorter regimens are: • ciprofloxacin 500 mg bid or ofloxacin 400 mg bid or ceftriaxone 2 g IV for 7 -10 days • Many patients often relapse after treatment and chronic maintenance therapy (TMP/SMX 1 DD daily) is sometimes necessary.
Shigella • • • Primarily a human parasite Infects the large intestine No perforation of intestine Dysentery Exotoxin (shiga-toxin) Enterotoxin 46

Shigella Presenting Signs and Symptoms • Clinical Symptoms may evolve • High fever • Abdominal pain • Bloody diarrhea
Shigella • dysenteriae, flexneri, boydii, sonnei • Watery or bloody diarrhea • May be complicated by reactive arthritis and rarely HUS • Very infectious ( ~100 organisms cause disease)
Shigella- Diagnostics • Stool microscopy— fresh examination and after concentration • Multiple stool samples may be necessary • Shigella bacillus found in stool
Shigella Management and Treatment § TMP/SMX 960 mg bid x 5 days § or § amoxicillin 500 mg tid x 5 days • If resistant to the above, give • • • or norfloxacin 400 mg bid x 5 days or nalidixic acid 1 g qid x 10 days ciprofloxacin 500 mg bid
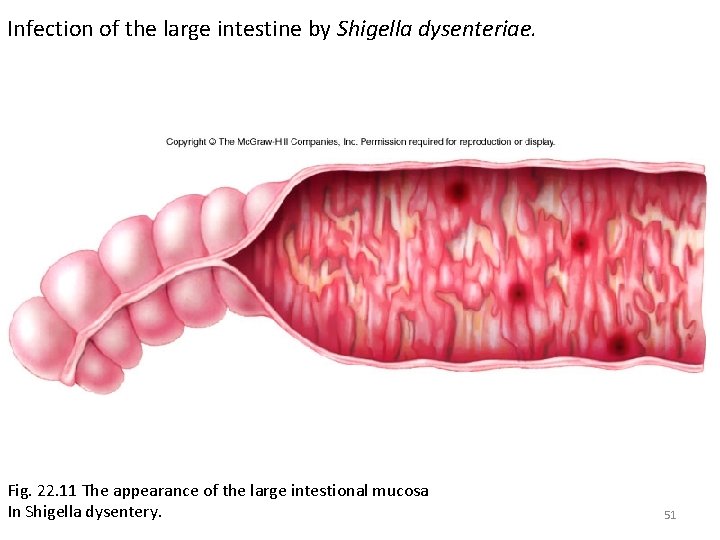
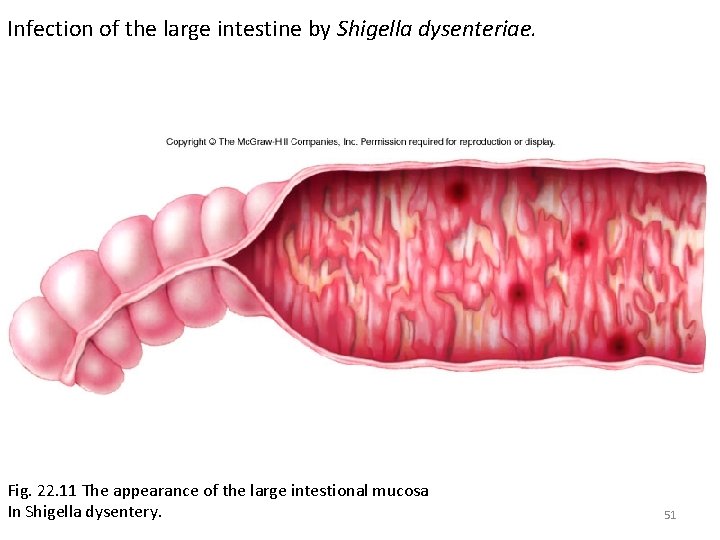
Infection of the large intestine by Shigella dysenteriae. Fig. 22. 11 The appearance of the large intestional mucosa In Shigella dysentery. 51

Shigella colitis (Campylobacter or Salmonella would look much the same. ) Salmonella would look much the same © University of Alabama at Birmingham, Dept. of Path.
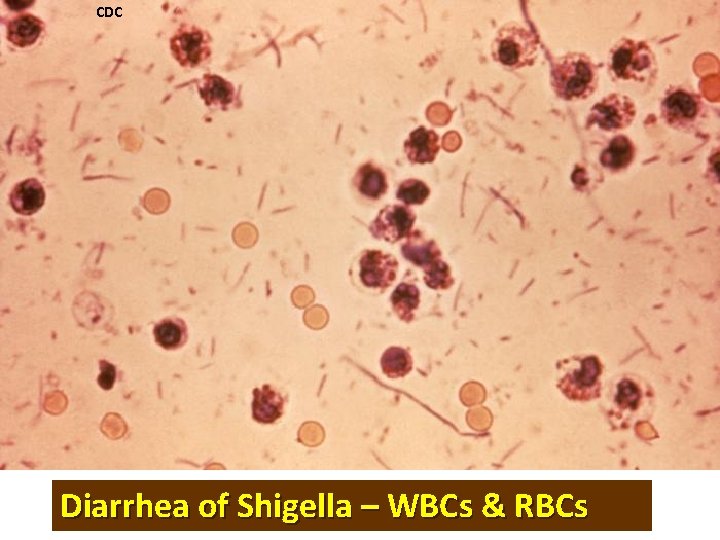
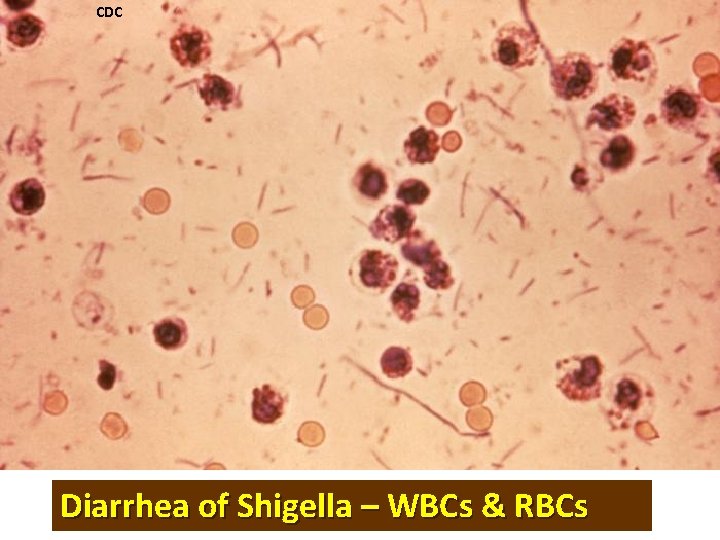
CDC Diarrhea of Shigella – WBCs & RBCs
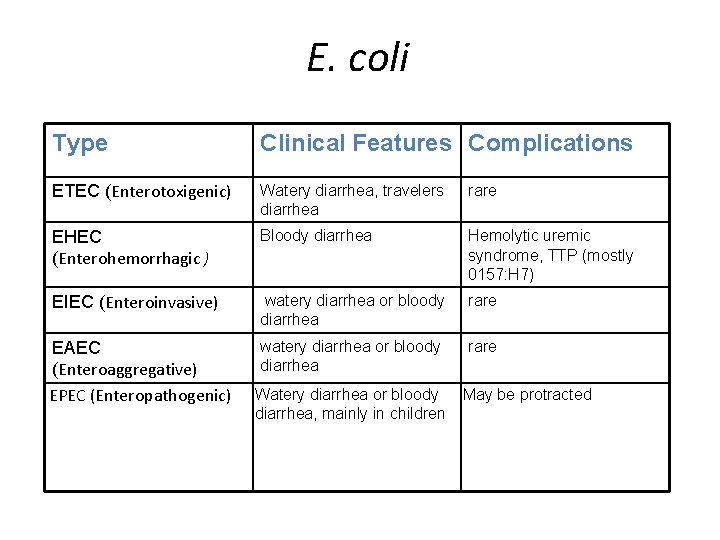
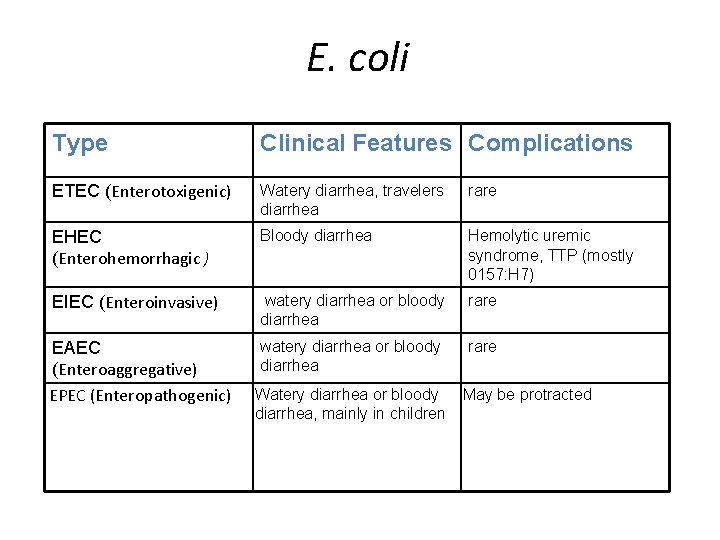
E. coli Type Clinical Features Complications ETEC (Enterotoxigenic) Watery diarrhea, travelers diarrhea rare EHEC (Enterohemorrhagic ) Bloody diarrhea Hemolytic uremic syndrome, TTP (mostly 0157: H 7) EIEC (Enteroinvasive) watery diarrhea or bloody diarrhea rare EAEC (Enteroaggregative) EPEC (Enteropathogenic) Watery diarrhea or bloody diarrhea, mainly in children May be protracted
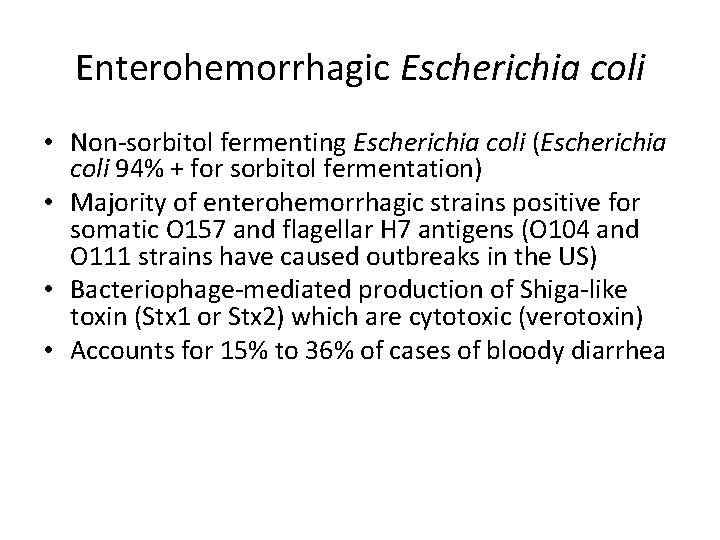
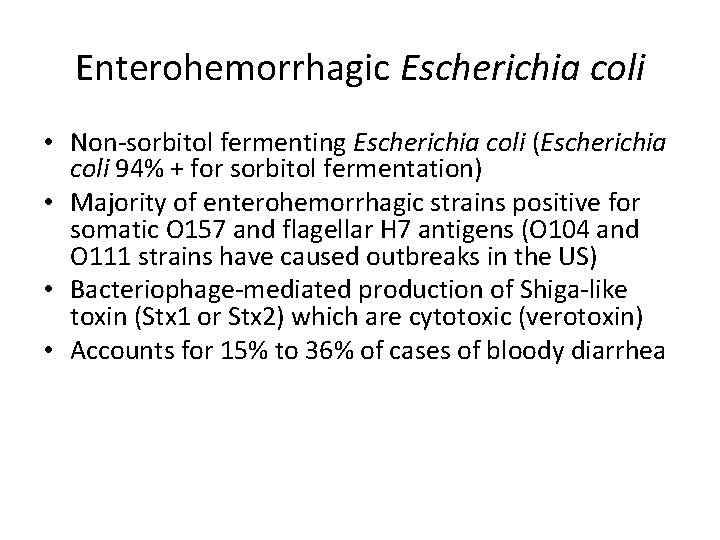
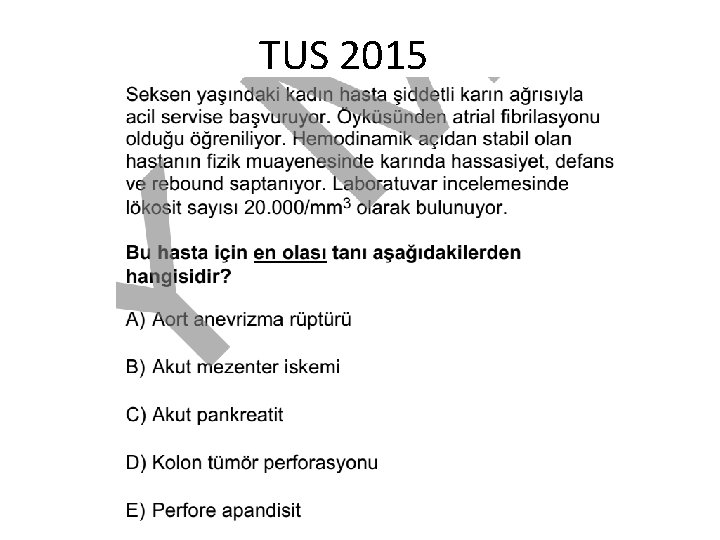
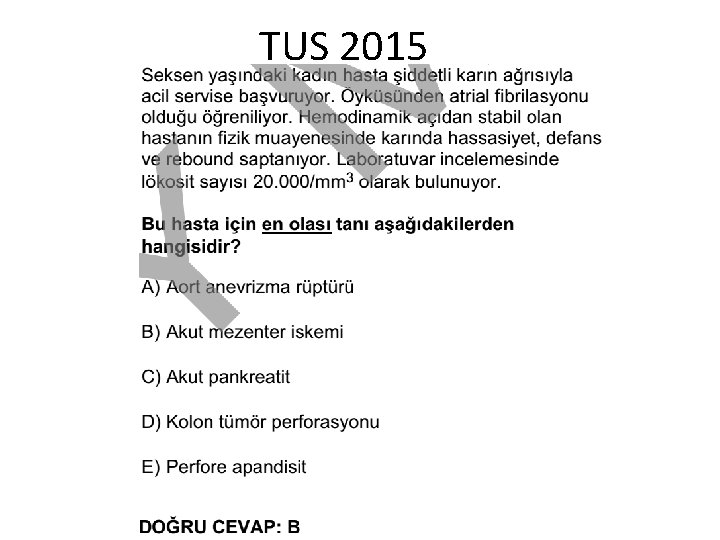
Enterohemorrhagic Escherichia coli • Non-sorbitol fermenting Escherichia coli (Escherichia coli 94% + for sorbitol fermentation) • Majority of enterohemorrhagic strains positive for somatic O 157 and flagellar H 7 antigens (O 104 and O 111 strains have caused outbreaks in the US) • Bacteriophage-mediated production of Shiga-like toxin (Stx 1 or Stx 2) which are cytotoxic (verotoxin) • Accounts for 15% to 36% of cases of bloody diarrhea
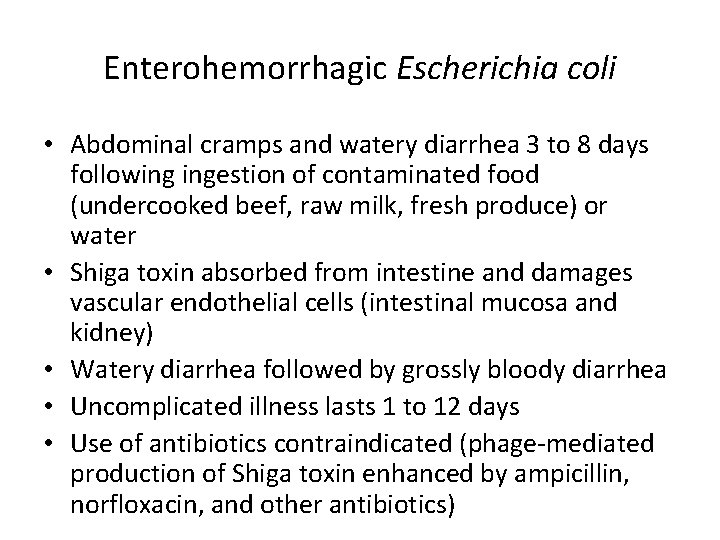
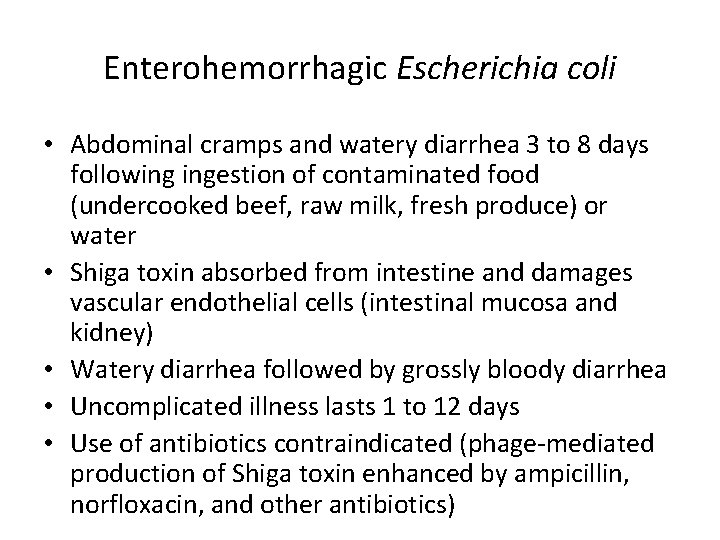
Enterohemorrhagic Escherichia coli • Abdominal cramps and watery diarrhea 3 to 8 days following ingestion of contaminated food (undercooked beef, raw milk, fresh produce) or water • Shiga toxin absorbed from intestine and damages vascular endothelial cells (intestinal mucosa and kidney) • Watery diarrhea followed by grossly bloody diarrhea • Uncomplicated illness lasts 1 to 12 days • Use of antibiotics contraindicated (phage-mediated production of Shiga toxin enhanced by ampicillin, norfloxacin, and other antibiotics)
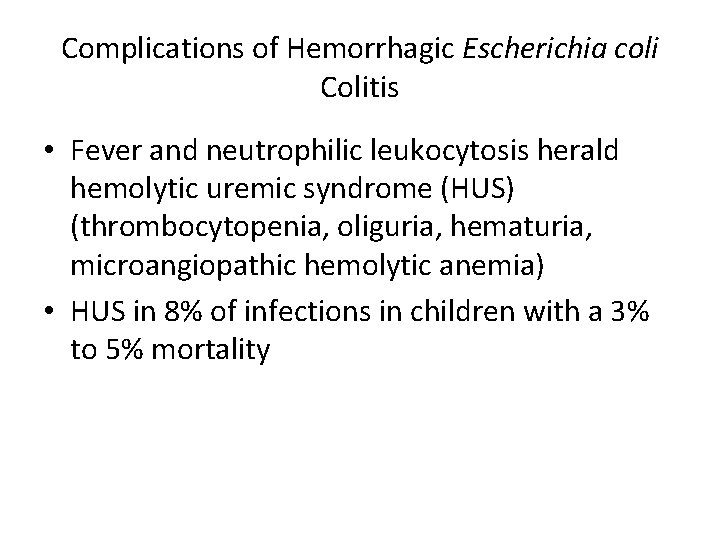
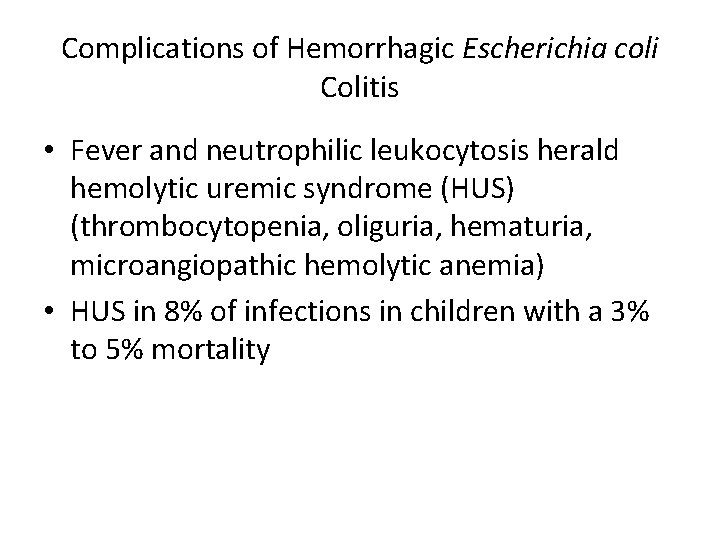
Complications of Hemorrhagic Escherichia coli Colitis • Fever and neutrophilic leukocytosis herald hemolytic uremic syndrome (HUS) (thrombocytopenia, oliguria, hematuria, microangiopathic hemolytic anemia) • HUS in 8% of infections in children with a 3% to 5% mortality
Shiga-toxin (E. coli) • O 157: H 7 • Enterohemorrhagic E. coli (EHEC) • Serious manifestations – hemolytic uremic syndrome, neurologic symptoms • Shiga-toxin gene present on bacteriophage genome • Type III secretion system 58
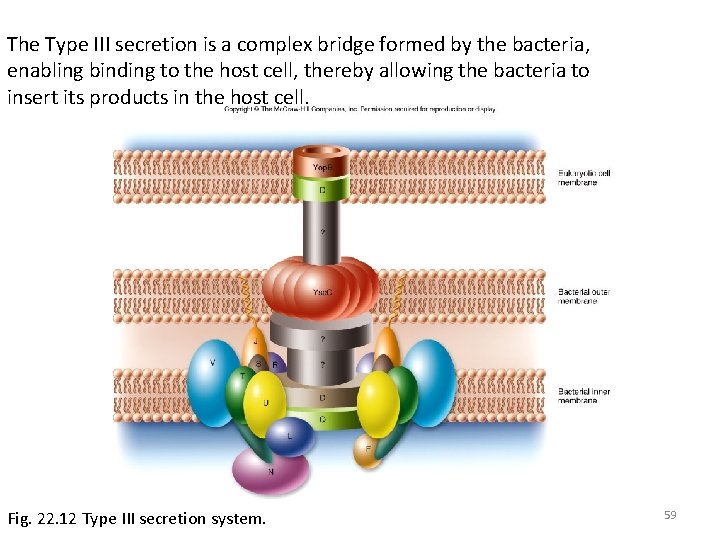
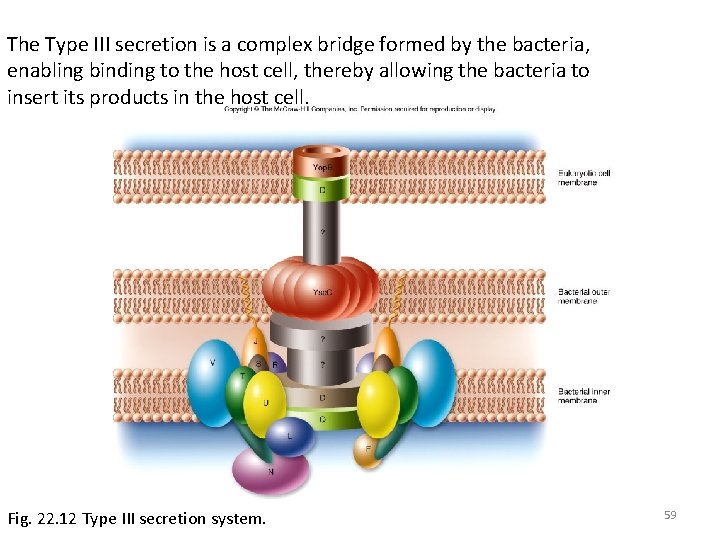
The Type III secretion is a complex bridge formed by the bacteria, enabling binding to the host cell, thereby allowing the bacteria to insert its products in the host cell. Fig. 22. 12 Type III secretion system. 59

Non-shiga-toxin (E. coli) • • Enterotoxigenic – traveler’s diarrhea Enteroinvasive – no exotoxin Enteropathogenic – similar to EHEC Enteroaggregative – chronic diarrhea 60
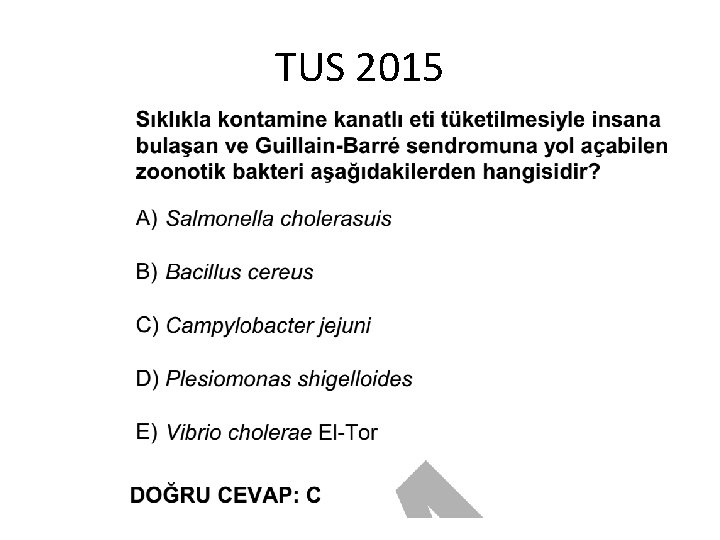
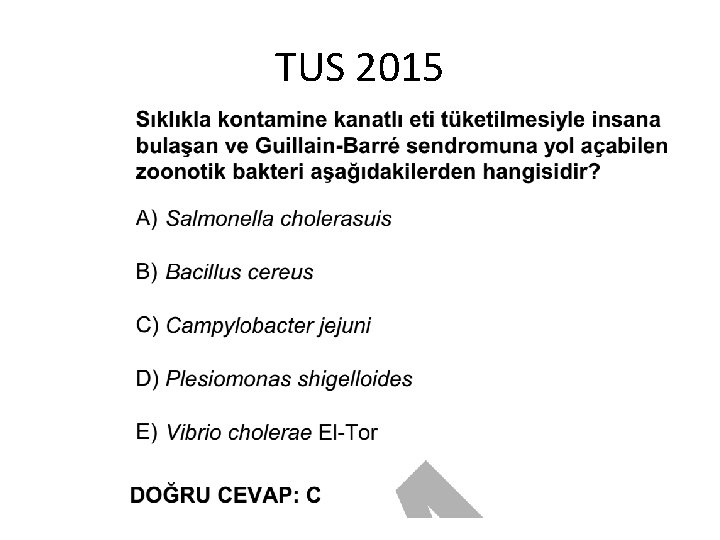
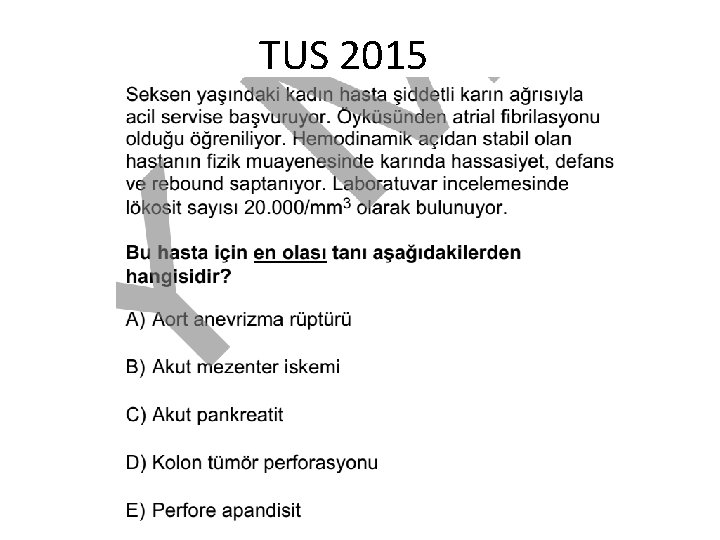
Campylobacter • Most common bacterial cause of diarrhea • Related to Guillain-Barre syndrome (GBS) – paralysis 61
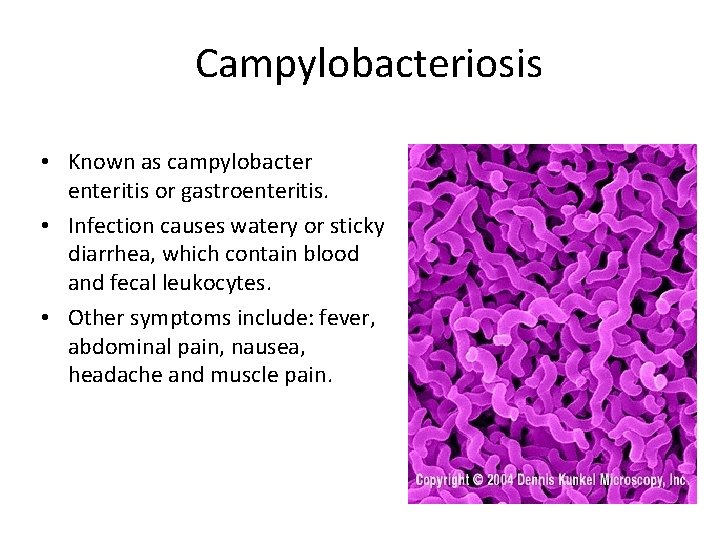
Campylobacter • Mainly C. jejuni • Transmission from infected animals or food products, fresh or salt water • Watery diarrhea or dysentery • May be complicated by Guillain-Barré and IPSID (Immunoproliferative small intestinal disease)

Bacterial infection: Campylobacter Presenting Signs and Symptoms • Clinical Symptoms may evolve • Fever and general malaise, sometimes without GI symptoms • When present, GI symptoms include bloody diarrhea, abdominal pain and weight loss.
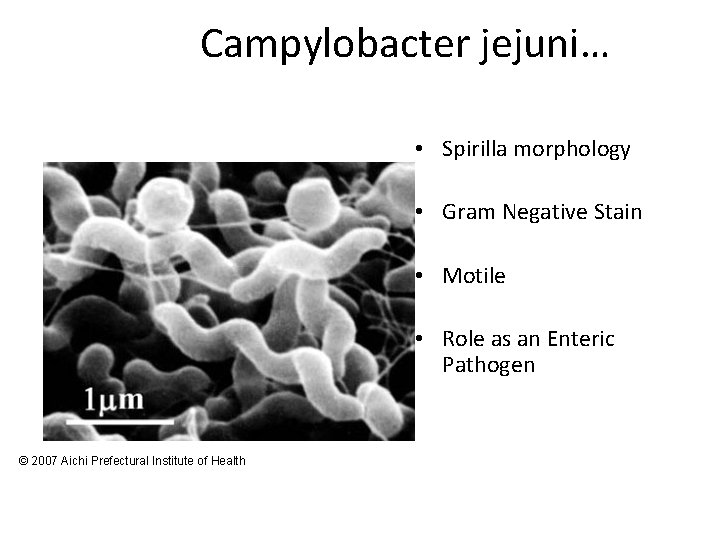
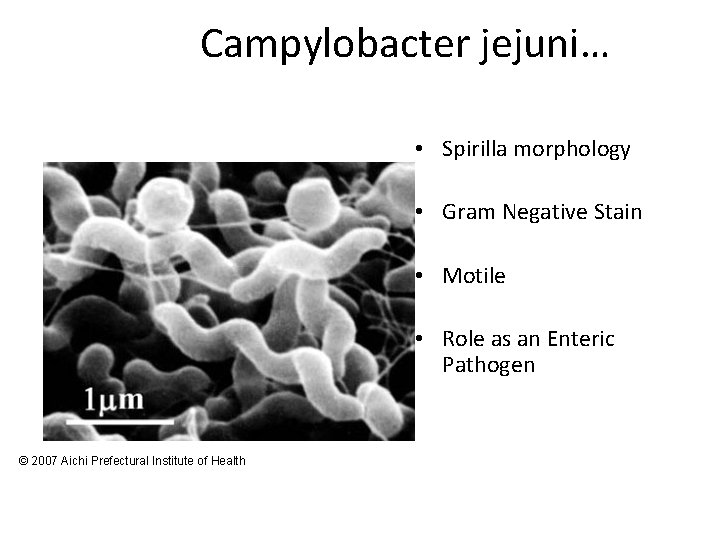
Campylobacter jejuni… • Spirilla morphology • Gram Negative Stain • Motile • Role as an Enteric Pathogen © 2007 Aichi Prefectural Institute of Health
Campylobacter jejuni • Relatively fragile • Microaerophilic organism. • Seems to be well adapted to birds
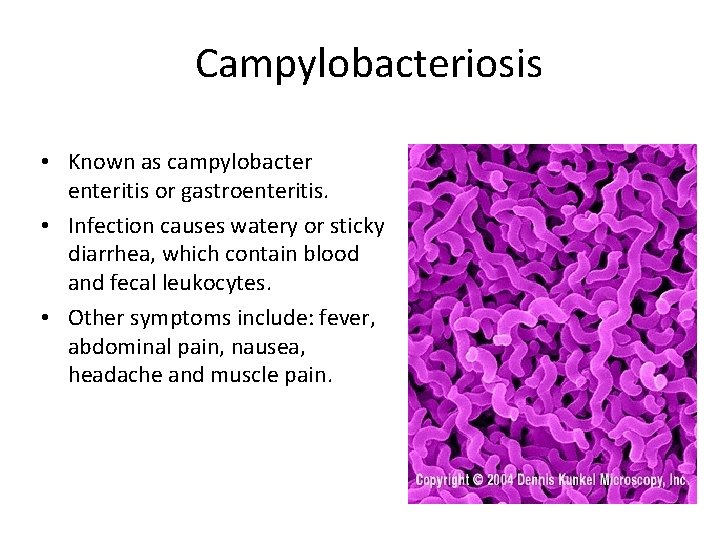
Campylobacteriosis • Known as campylobacter enteritis or gastroenteritis. • Infection causes watery or sticky diarrhea, which contain blood and fecal leukocytes. • Other symptoms include: fever, abdominal pain, nausea, headache and muscle pain.
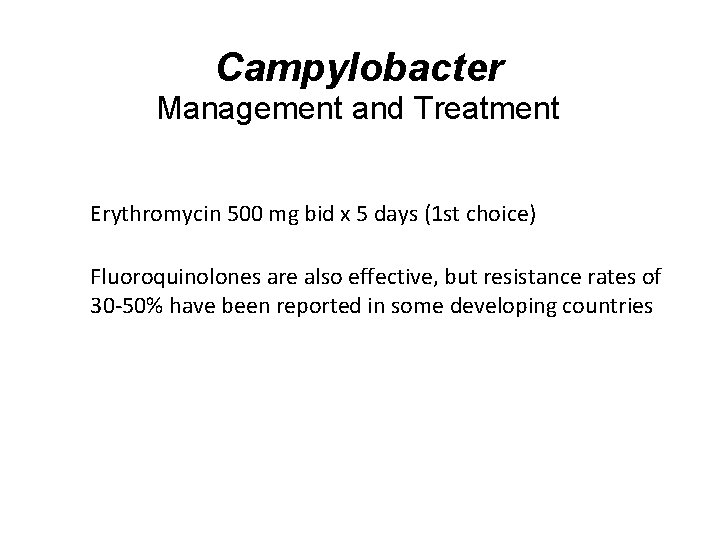
Campylobacter Management and Treatment • Erythromycin 500 mg bid x 5 days (1 st choice) • Fluoroquinolones are also effective, but resistance rates of 30 -50% have been reported in some developing countries
Complications of Campylobacteriosis • Enteritis usually self-limiting (1 day to 1 week or longer) • Guillain-Barré syndrome (structural homology of LPS O-antigen with human nerve gangliosides) • Post-infectious reactive arthritis (associated with HLA-B 27) • Bacteremia (rate of 1. 5/1, 000 intestinal infections)
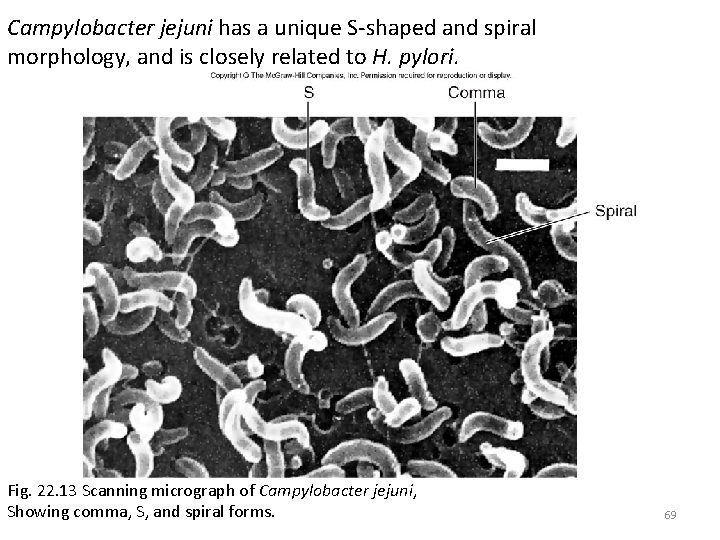
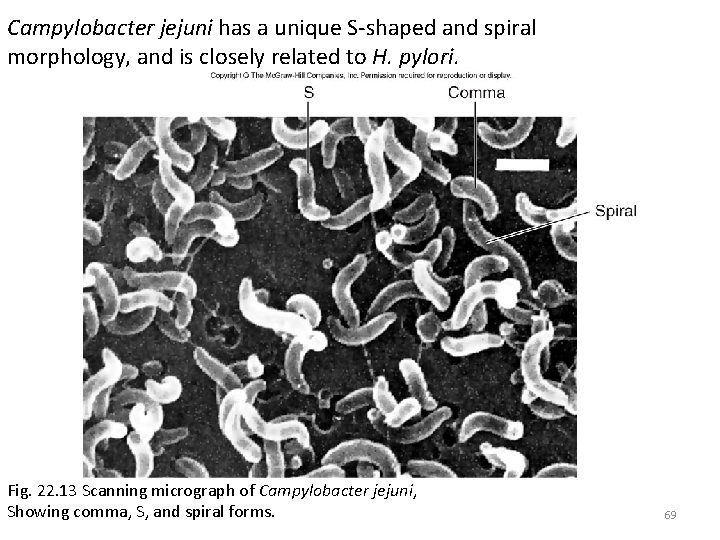
Campylobacter jejuni has a unique S-shaped and spiral morphology, and is closely related to H. pylori. Fig. 22. 13 Scanning micrograph of Campylobacter jejuni, Showing comma, S, and spiral forms. 69
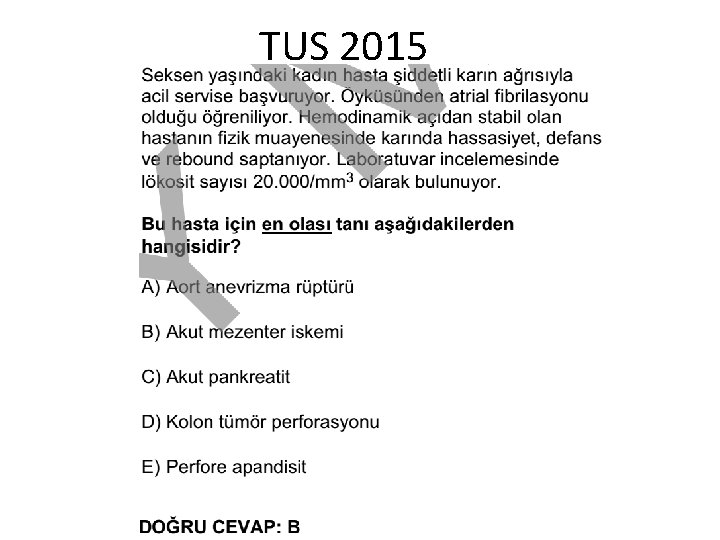
Yersinia • • High degree of abdominal pain Mistaken for appendicitis Infects the small intestine Some can affect the lymphatic system (intracellular) 70
Yersinia enterocolitica • Fermentative, rod-shaped or coccoid gram-negative bacteria, non-motile and metabolically inactive at 37 o. C but motile and metabolically active at 22 -30 o. C • Enteropathogenic strains cytotoxic by penetratating human epithelial cells • Infection results in inflammatory ileitis (generally) and colitis (occasionally involving ascending colon) with mixed neutrophilic and mononuclear cell response • Necrosis of Peyer’s patches, mesenteric lymph node enlargement, and in severe cases thrombosis of mesenteric blood vessels with intestinal necrosis and hemorrhage
Yersinosis • Febrile diarrhea with abdominal pain 16 to 48 hours following ingestion of an infectious inoculum • Duration of illness ranges from 1 day to a prolonged diarrhea of 4 weeks
Complications of Yersinosis • Can simulate acute appendicitis (mesenteric lymphadenitis) • Bacteremic dissemination with hepatic and splenic abscess formation • Reactive arthritis associated with HLA-B 27 histocompatibility antigen (10 -30%) • Exudative pharyngitis (8% of infections accompanied by fever but no diarrhea)
Treatment • Safe food handling • Y. enterocolitica is suscestible to amg, chloram, tetra, TMP/SMZ, pip, cipro, • ß lactamase, resis to pen, ampi, 1. gen. ceph. • Patients with septicemia should receive antb. • Y. pseudotuberculosis usually not require antb, but with septicemia ampi or tetra
Clostridium difficile • Pseudomembranous colitis or antibiotic associated colitis • Capable of superinfecting the large intestine due to drug treatments • Enterotoxins 75

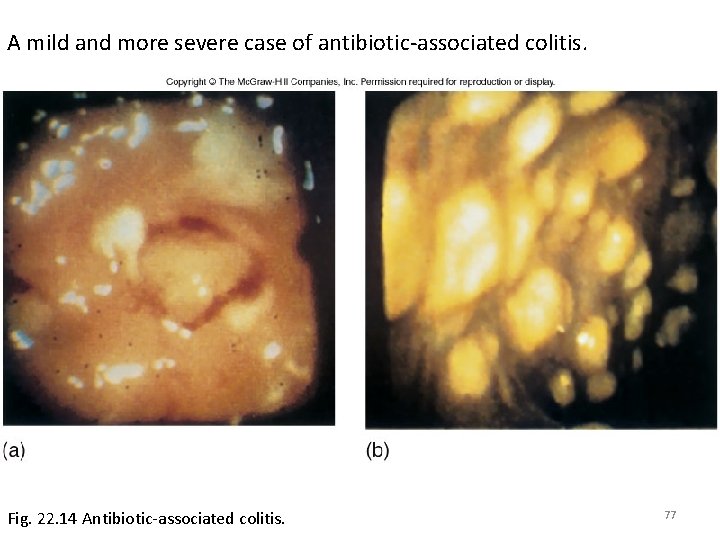
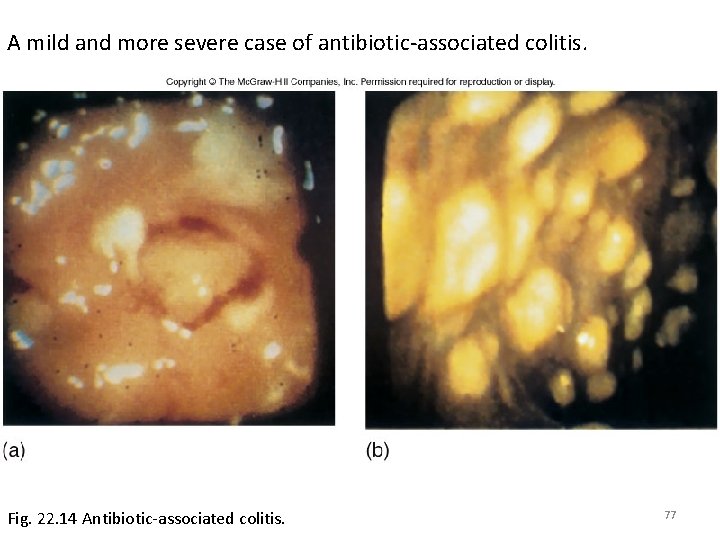
A mild and more severe case of antibiotic-associated colitis. Fig. 22. 14 Antibiotic-associated colitis. 77
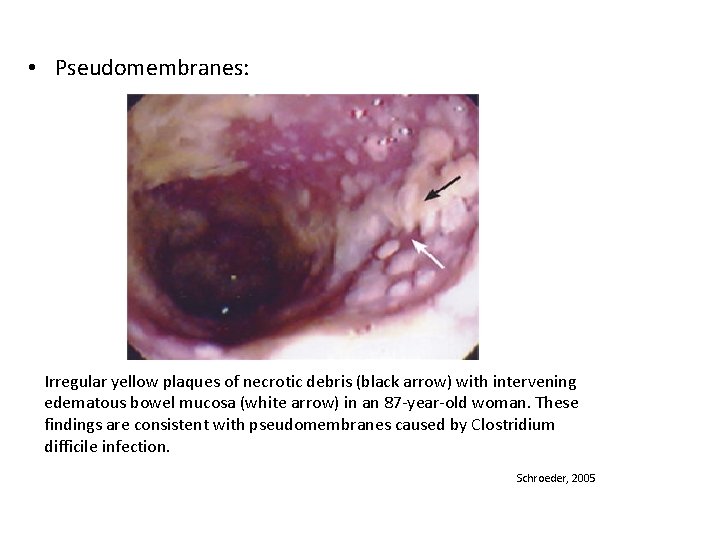
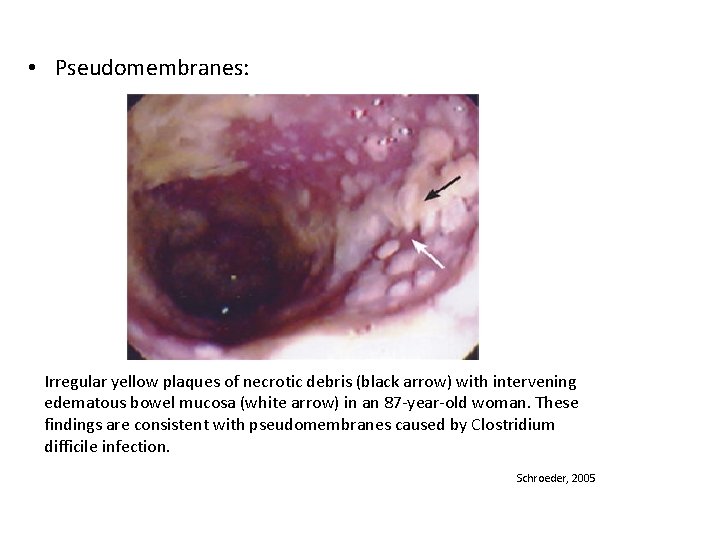
• Pseudomembranes: Irregular yellow plaques of necrotic debris (black arrow) with intervening edematous bowel mucosa (white arrow) in an 87 -year-old woman. These findings are consistent with pseudomembranes caused by Clostridium difficile infection. Schroeder, 2005
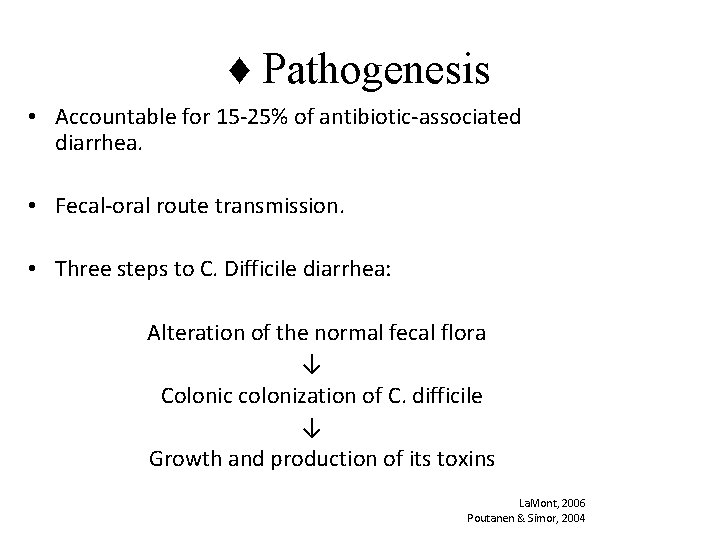
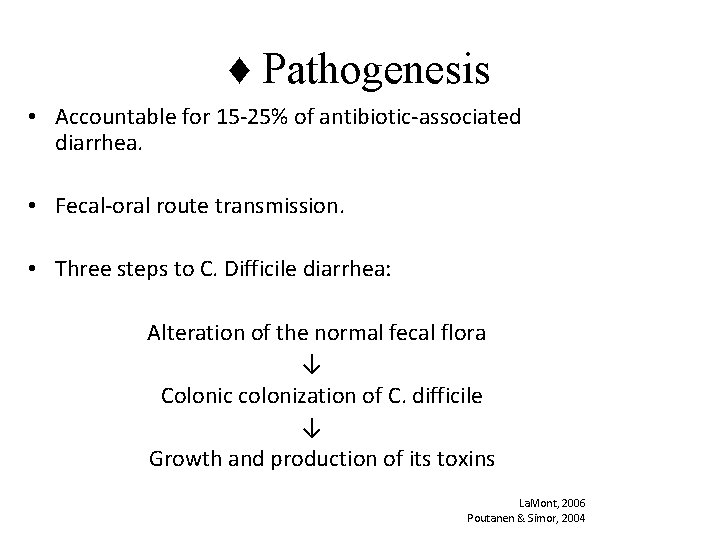
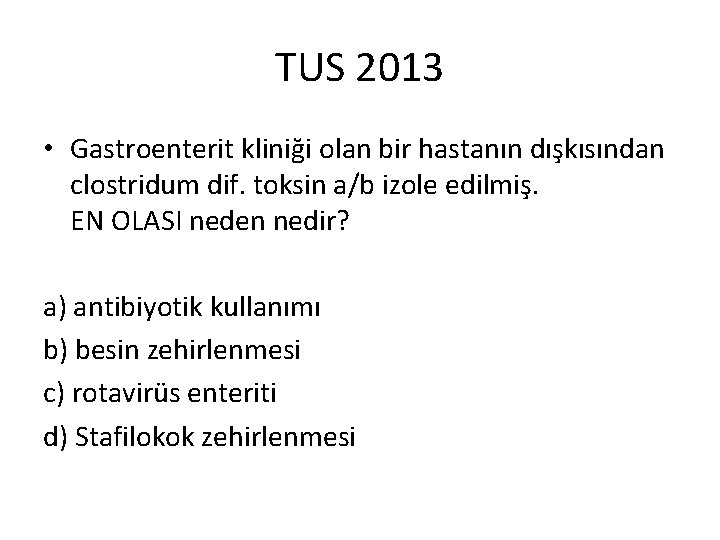
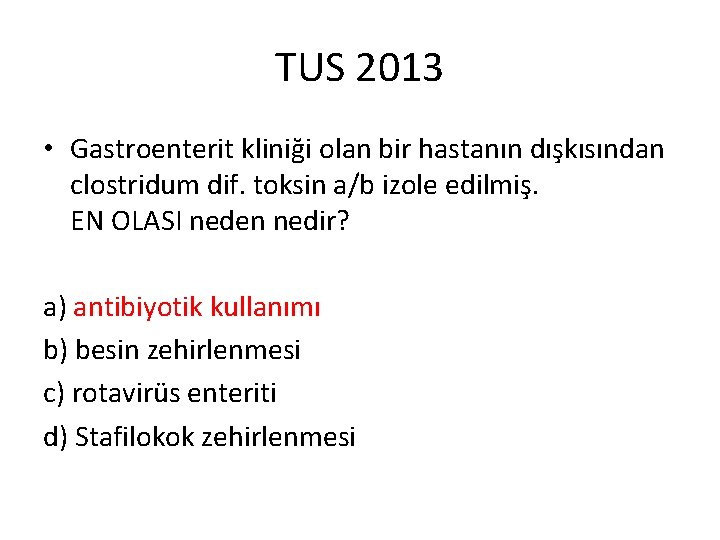
♦ Pathogenesis • Accountable for 15 -25% of antibiotic-associated diarrhea. • Fecal-oral route transmission. • Three steps to C. Difficile diarrhea: Alteration of the normal fecal flora ↓ Colonic colonization of C. difficile ↓ Growth and production of its toxins La. Mont, 2006 Poutanen & Simor, 2004
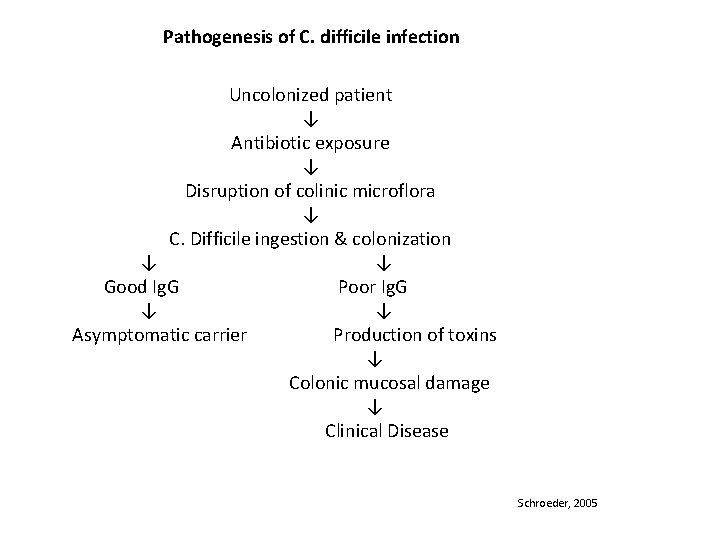
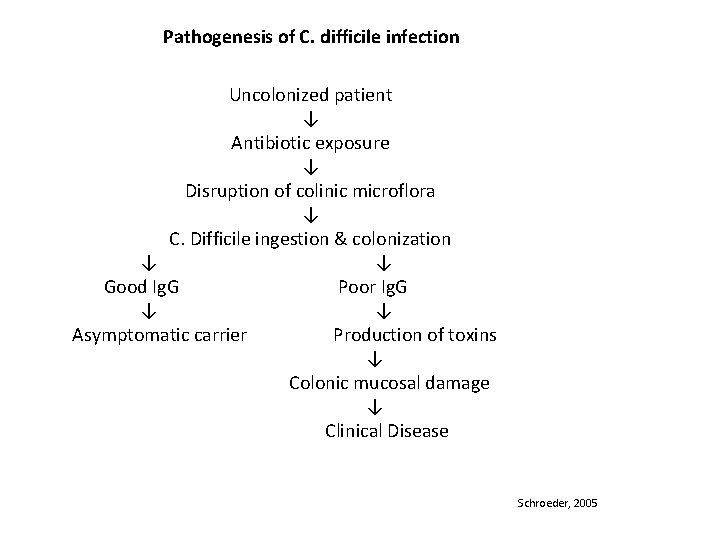
Pathogenesis of C. difficile infection Uncolonized patient ↓ Antibiotic exposure ↓ Disruption of colinic microflora ↓ C. Difficile ingestion & colonization ↓ Good Ig. G Poor Ig. G ↓ Asymptomatic carrier Production of toxins ↓ Colonic mucosal damage ↓ Clinical Disease Schroeder, 2005
♦ Risk Factors • Antibiotics – fluoroquinolones, cephalosporins, clindamycins, penicillins • Medications: – – – Proton pump inhibitor Histamine-2 receptor blockers Non-steroidal anti-inflammatories (except aspirin) Laxatives Narcotics Antiperistaltic drugs • Advanced age ( ≥ 65 yrs. ) • Chemotherapy
• Medical/Surgical procedures – – Gastrointestinal surgery Enemas Enteral tube feedings Endoscopy • Underlying illness and its severity – – Inflammatory bowel disease Diabetes mellitus/Hyperthyroidism Leukemia/Lymphoma Liver/Renal failure • History of C. difficile associated diarrhea • Prolonged hospital stay/Nursing home resident Louie & Meddings, 2004 Mc. Donald, Owings, & Jernigan, 2006 Melillo, 1998 Poutanon & Simor, 2004

• Toxic Megacolon La. Mont, 2006
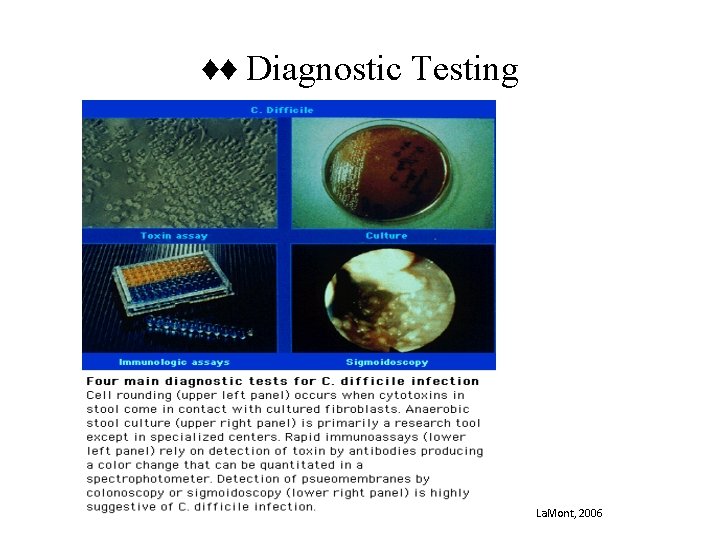
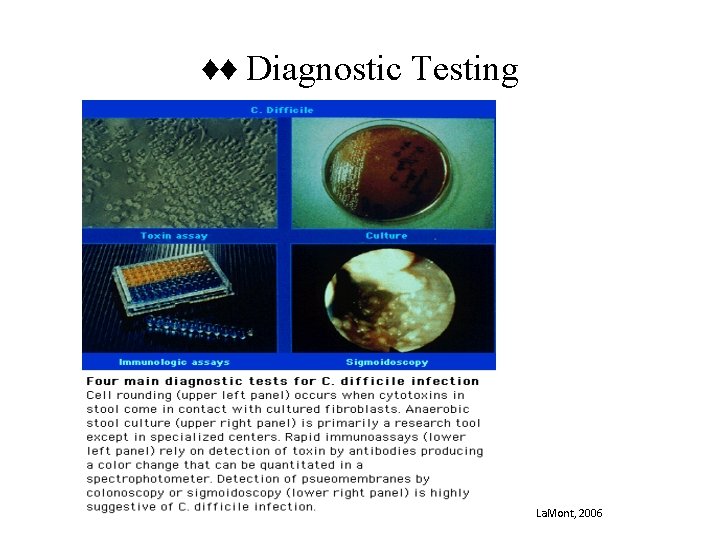
♦♦ Diagnostic Testing La. Mont, 2006
♦ Treatment • Discontinue the offending agent – If unable: • Choose an antibiotic less frequently associated with antibiotic-associated diarrhea (aminoglycosides, sulfonamides, macrolides, vancomycin, tetracyclines) • Prescribe Metronidazole 500 mg PO TID throughout the needed course of antibiotic therapy and for 7 days after. La. Mont, 2006 Schroeder, 2005

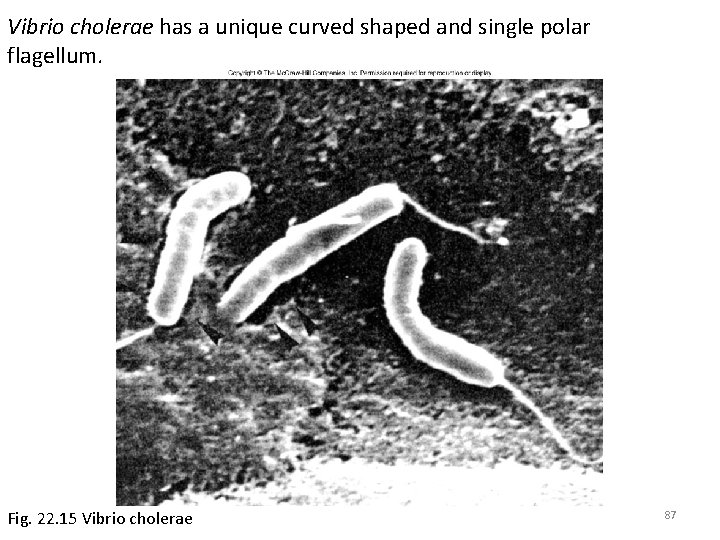
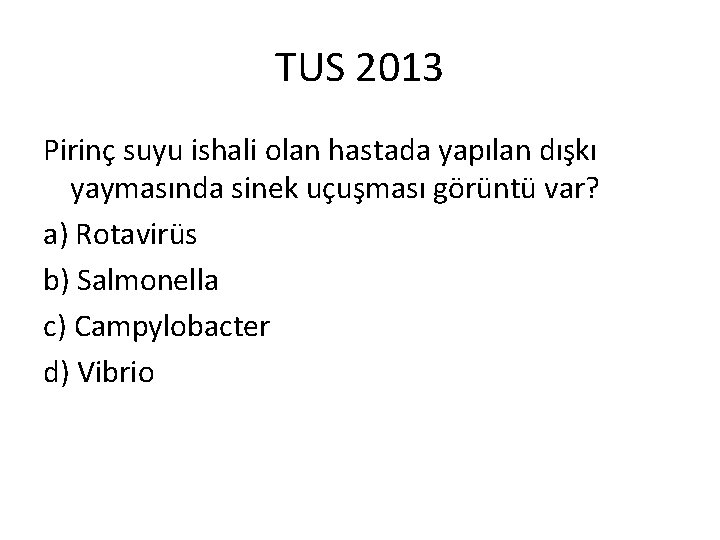
Vibrio cholerae • • • Cholera Unique O and H antigens Cholera toxin (CT) – A-B toxin Bacteria never enter host cells Heavy lost of fluid “rice-water stool” Untreated cases can be fatal 86
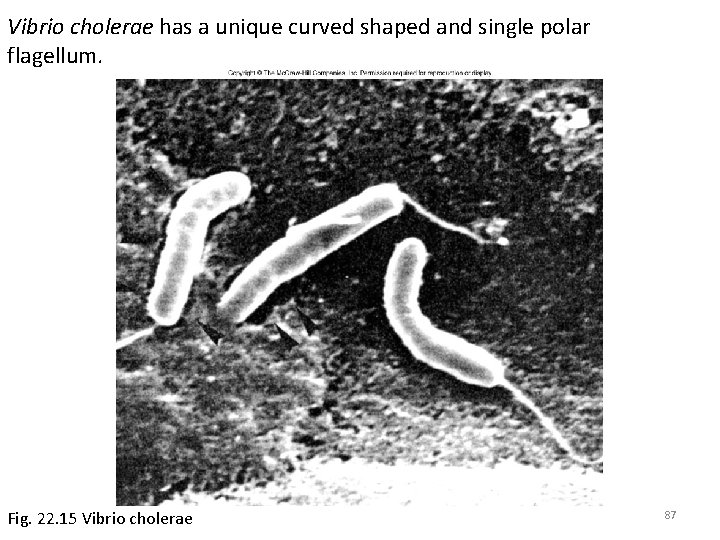
Vibrio cholerae has a unique curved shaped and single polar flagellum. Fig. 22. 15 Vibrio cholerae 87
Common nonbacterial • Cryptosporidium • Rotavirus 89

Cryptosporidium • • • Protozoan infection Zoonotic Oocysts Intracellular AIDS patients are at risk Associated with fresh water outbreaks 90

A SEM of Cryptosporidium shows attachment to the intestinal epithelium, prior to intracellular invasion. Fig. 22. 16 Scanning electron micrograph of Cryptosporidium 91

Acid-fast staining enables oocysts to be identified, as they stain red or purple. Fig. 22. 17 Acid-fast stain in Cryptosporidium 92

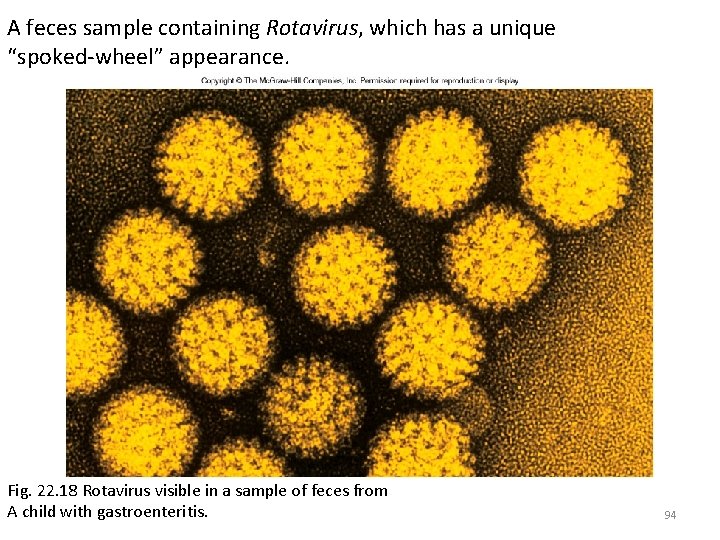
Rotavirus • Responsible for most morbidity and mortality from diarrhea • Babies lacking maternal antibodies are at risk • Unique morphological appearance 93
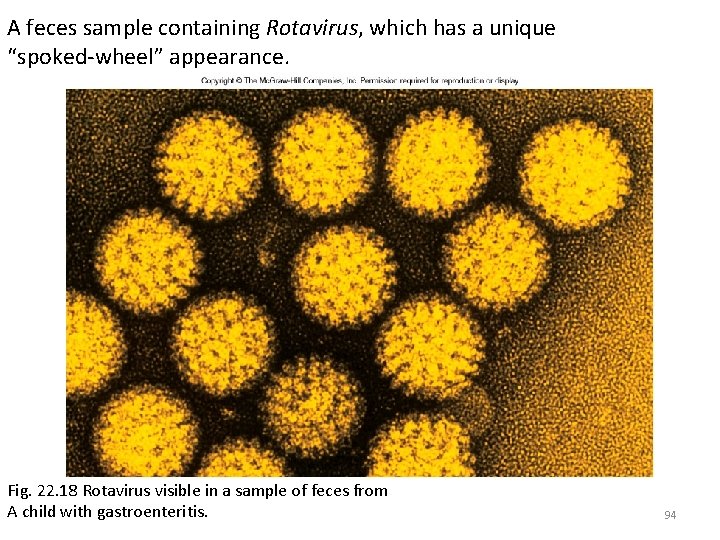
A feces sample containing Rotavirus, which has a unique “spoked-wheel” appearance. Fig. 22. 18 Rotavirus visible in a sample of feces from A child with gastroenteritis. 94

• Acute diarrhea is an episode of diarrhea of <14 days in duration • Persistent diarrhea is of >14 days in duration • Chronic diarrhea lasts >30 days
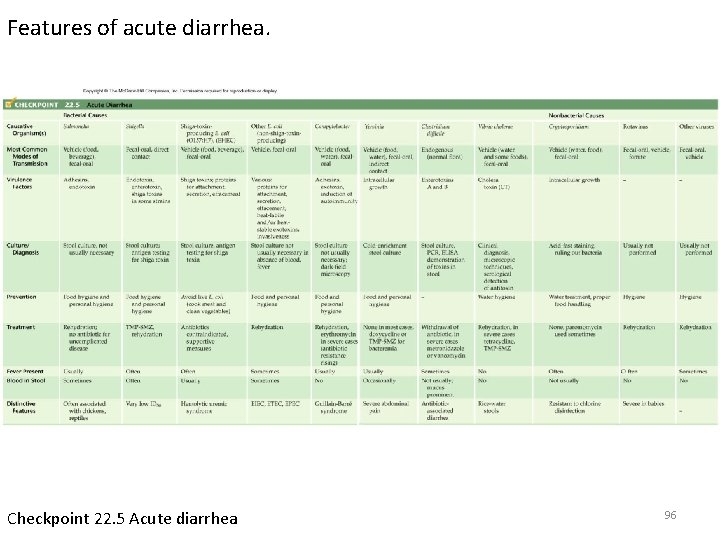
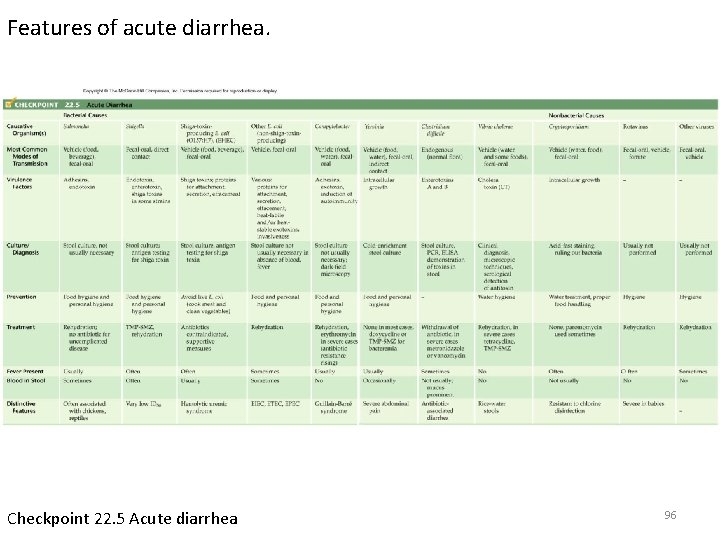
Features of acute diarrhea. Checkpoint 22. 5 Acute diarrhea 96
Acute diarrhea with vomiting • Food poisoning - toxin – Staphylococcus aureus – Bacillus cereus – Clostridium perfringens 97
Classic Syndromes: Acute food poisoning • • • Similar illness in 2 or more persons Epidemiologic evidence of common food source Onset of symptoms typically within 6 hours of ingestion Nausea and vomiting prominent Preformed toxin of S. aureus or B. cereus Longer incubation periods for C. perfringens
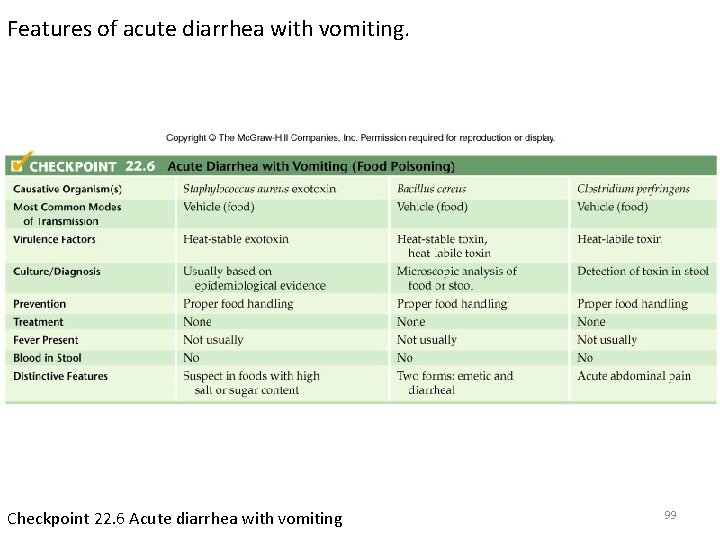
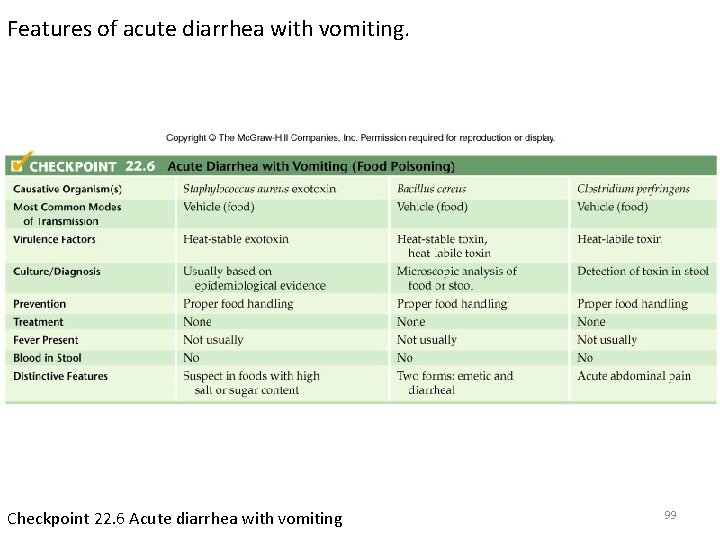
Features of acute diarrhea with vomiting. Checkpoint 22. 6 Acute diarrhea with vomiting 99

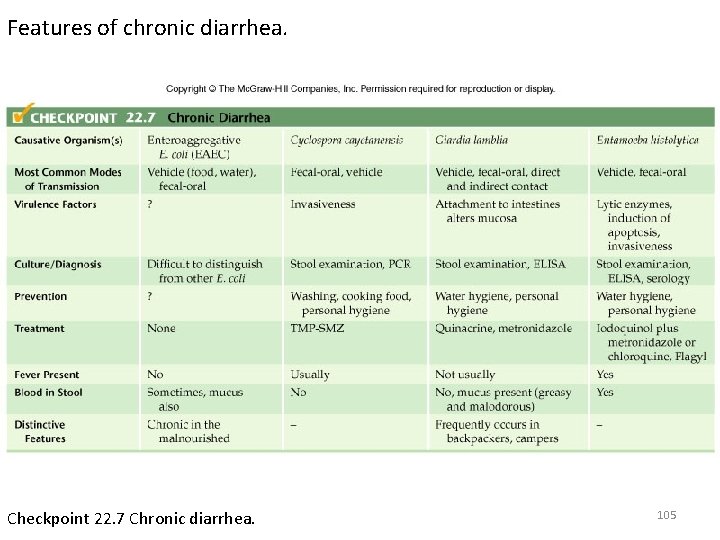
Chronic diarrhea • • Enteroaggregative (EAEC) E. coli Cyclospora cayetanensis Giardia lamblia Entamoeba histolytica 100
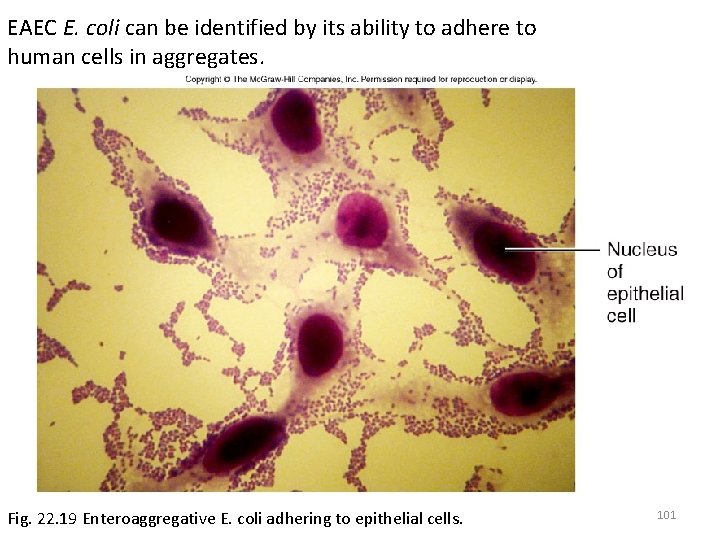
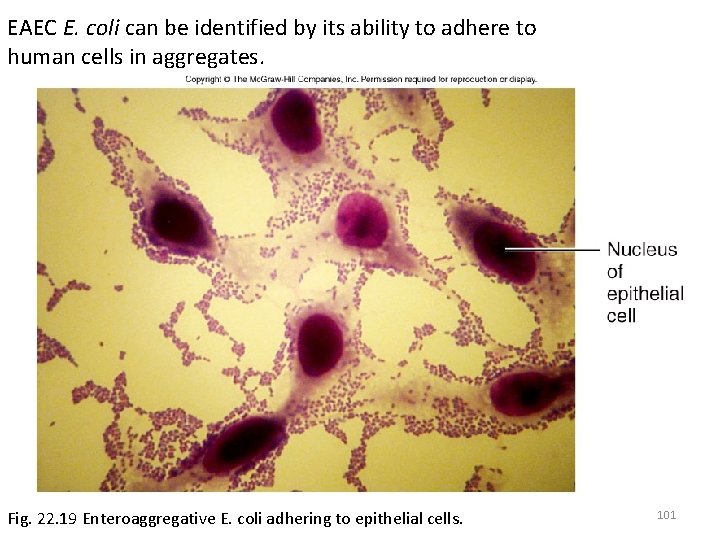
EAEC E. coli can be identified by its ability to adhere to human cells in aggregates. Fig. 22. 19 Enteroaggregative E. coli adhering to epithelial cells. 101

The protozoan Cyclospora can be identified by the acid-fast stain, in which large cysts stain pink to red and have a wrinkled outer wall. Fig. 22. 20 An acid-fast stain of Cyclospora in a human Fecal sample. 102
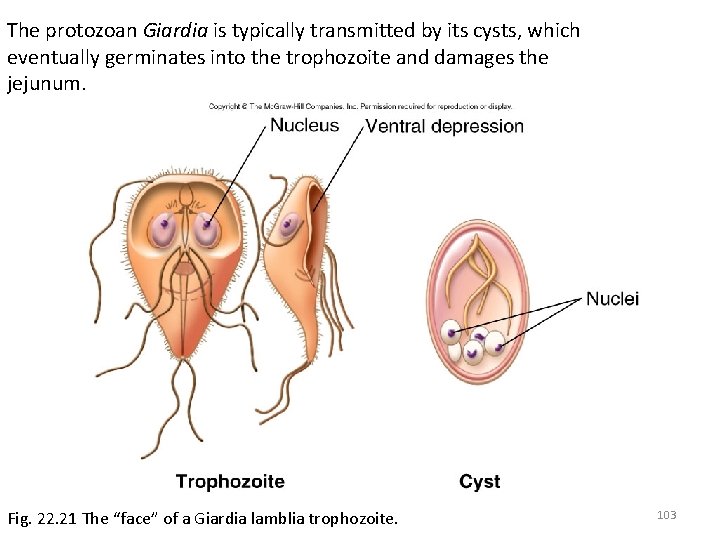
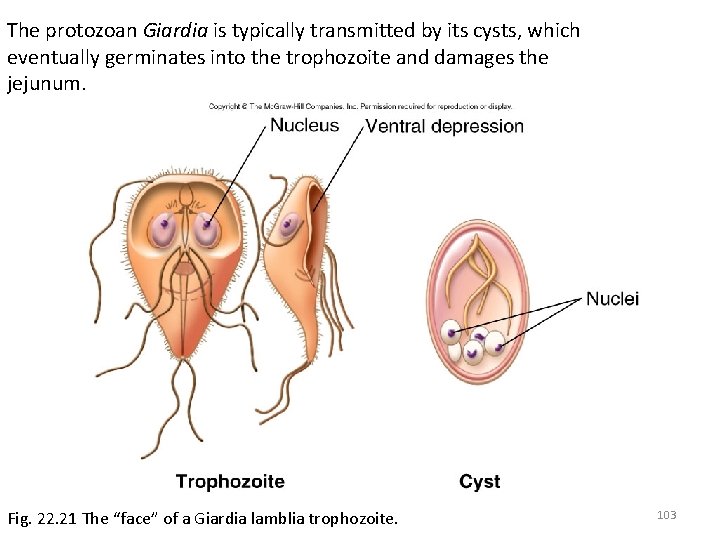
The protozoan Giardia is typically transmitted by its cysts, which eventually germinates into the trophozoite and damages the jejunum. Fig. 22. 21 The “face” of a Giardia lamblia trophozoite. 103
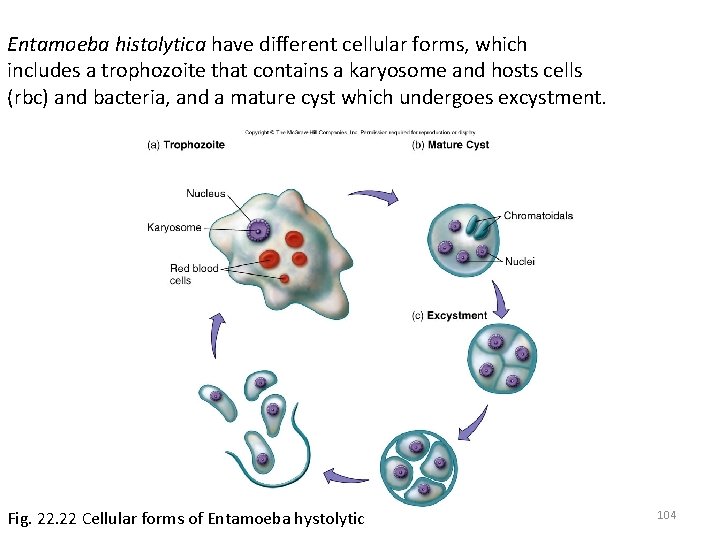
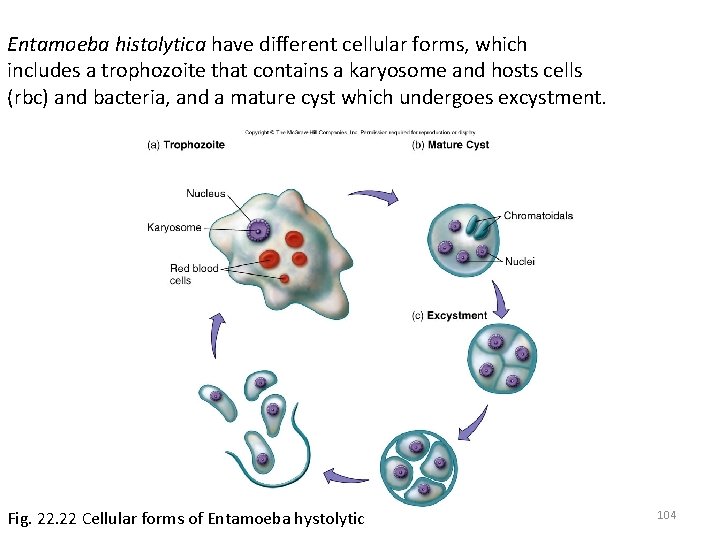
Entamoeba histolytica have different cellular forms, which includes a trophozoite that contains a karyosome and hosts cells (rbc) and bacteria, and a mature cyst which undergoes excystment. Fig. 22 Cellular forms of Entamoeba hystolytic 104
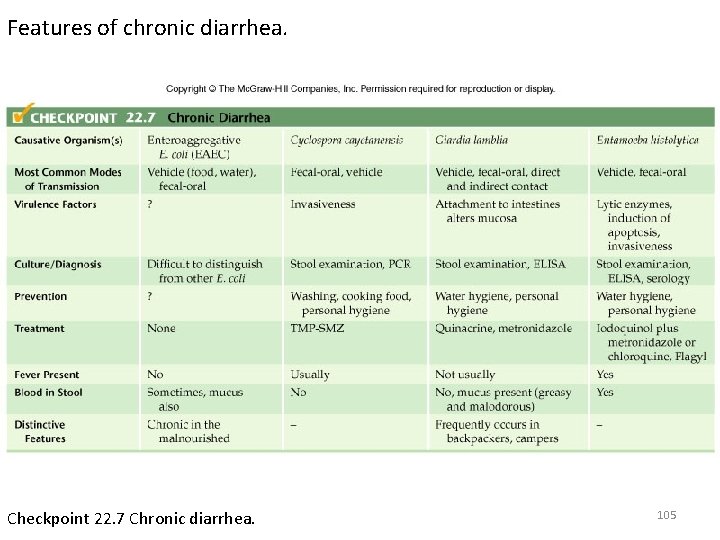
Features of chronic diarrhea. Checkpoint 22. 7 Chronic diarrhea. 105
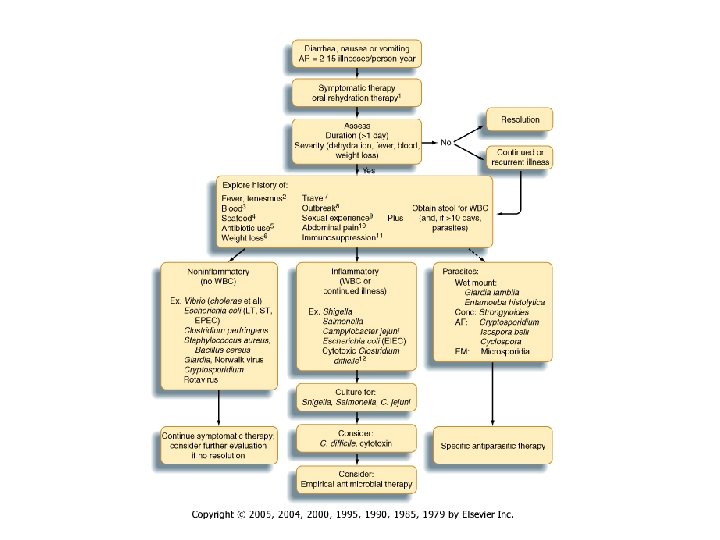
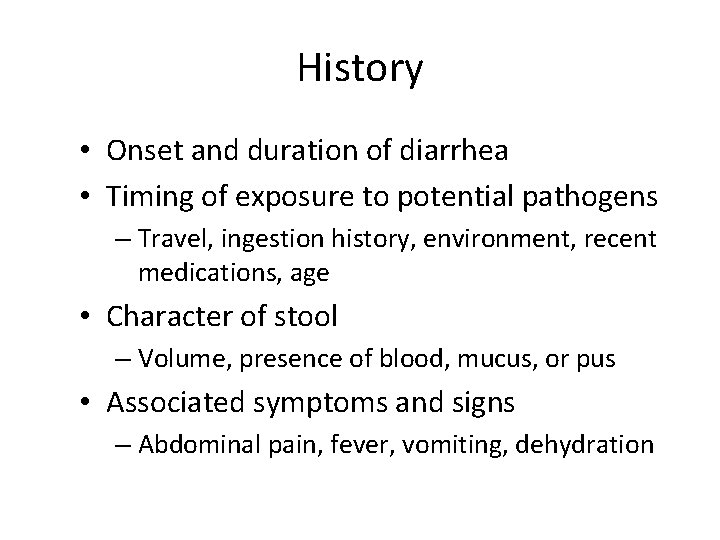
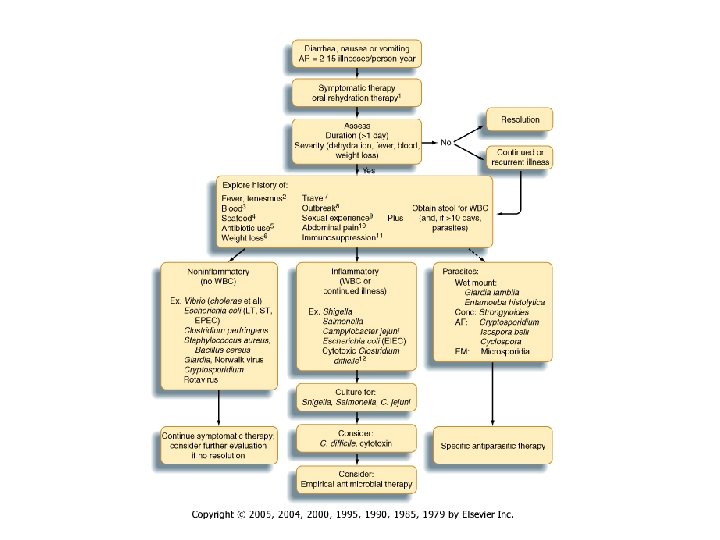
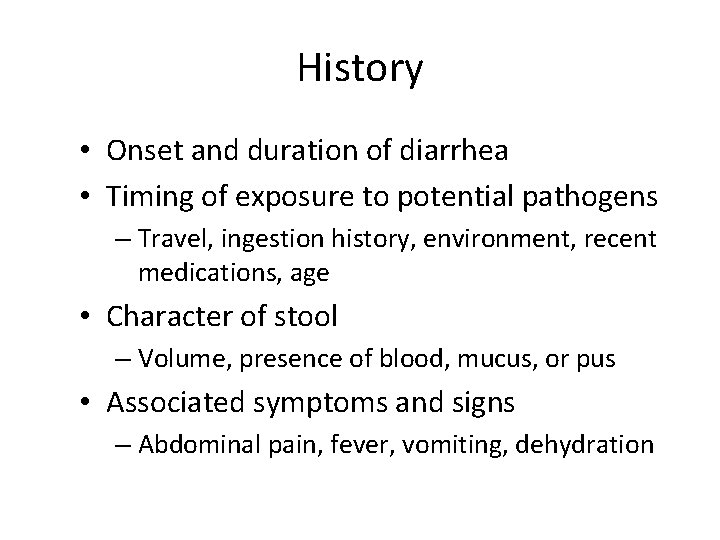
History • Onset and duration of diarrhea • Timing of exposure to potential pathogens – Travel, ingestion history, environment, recent medications, age • Character of stool – Volume, presence of blood, mucus, or pus • Associated symptoms and signs – Abdominal pain, fever, vomiting, dehydration

Physical examination • • Vital signs: Fever, tachycardia Abdominal tenderness or pain Signs of dehydration Blood in stool
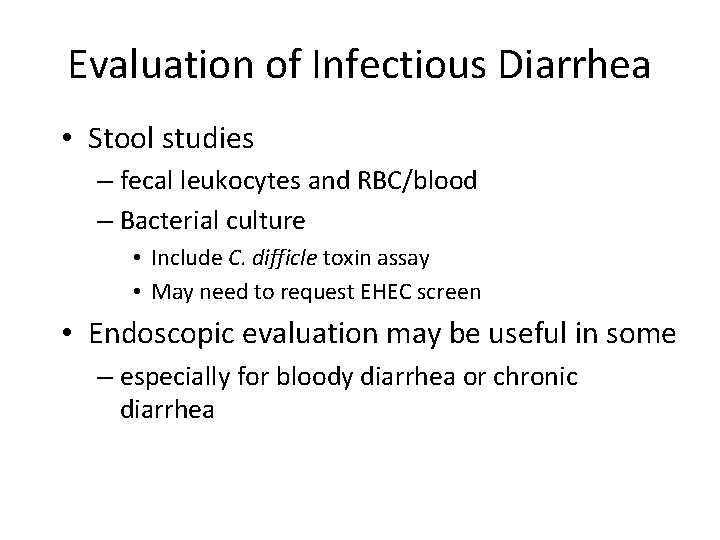
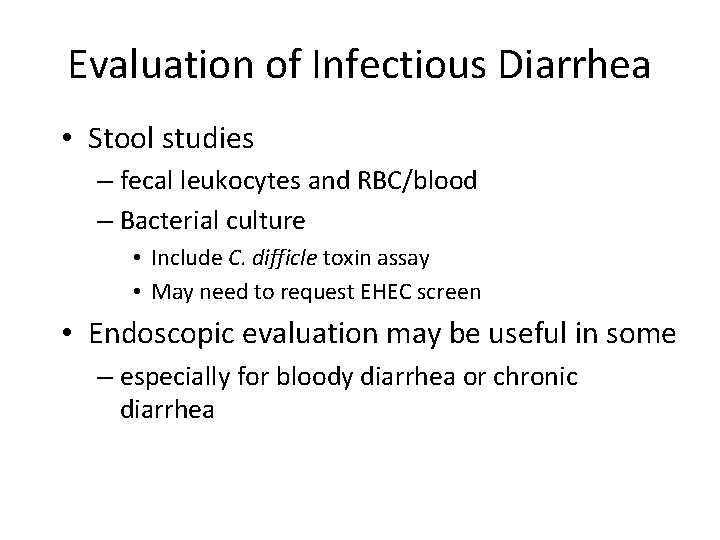
Evaluation of Infectious Diarrhea • Stool studies – fecal leukocytes and RBC/blood – Bacterial culture • Include C. difficle toxin assay • May need to request EHEC screen • Endoscopic evaluation may be useful in some – especially for bloody diarrhea or chronic diarrhea
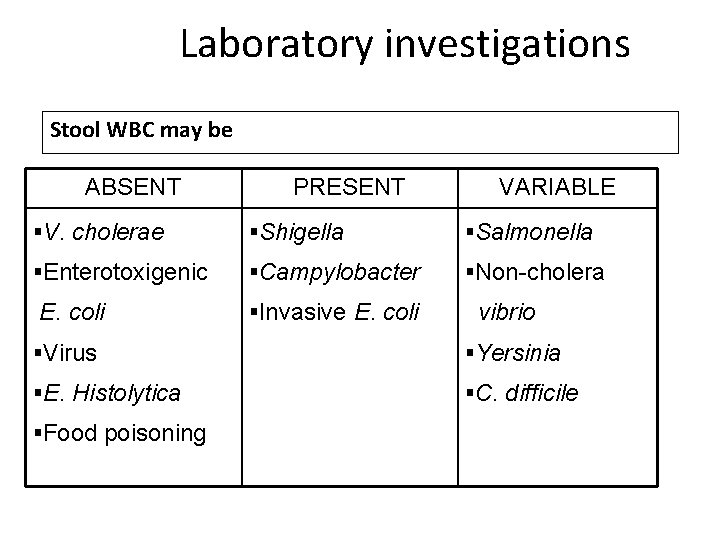
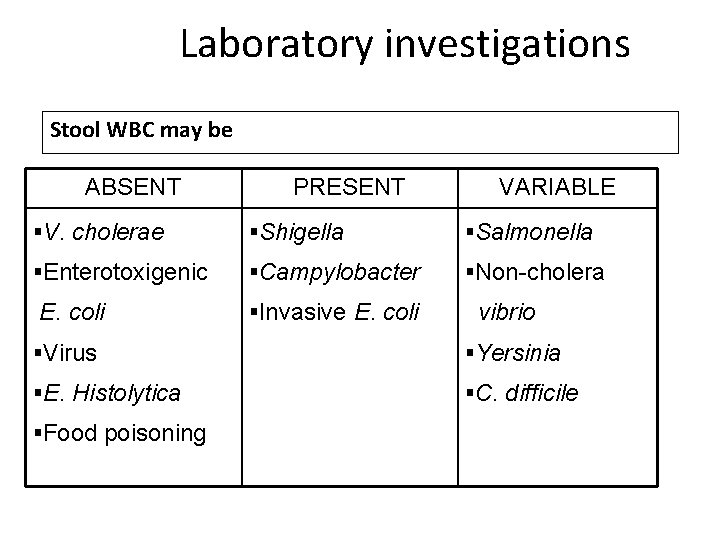
Laboratory investigations Stool WBC may be ABSENT §V. cholerae PRESENT §Shigella §Enterotoxigenic §Campylobacter E. coli §Invasive E. coli VARIABLE §Salmonella §Non-cholera vibrio §Virus §Yersinia §E. Histolytica §C. difficile §Food poisoning
Laboratory investigation § Not routinely indicated • Low yield 1. 5 -2. 4% • Not useful in initial management • More sensitive and specific in stool with WBC
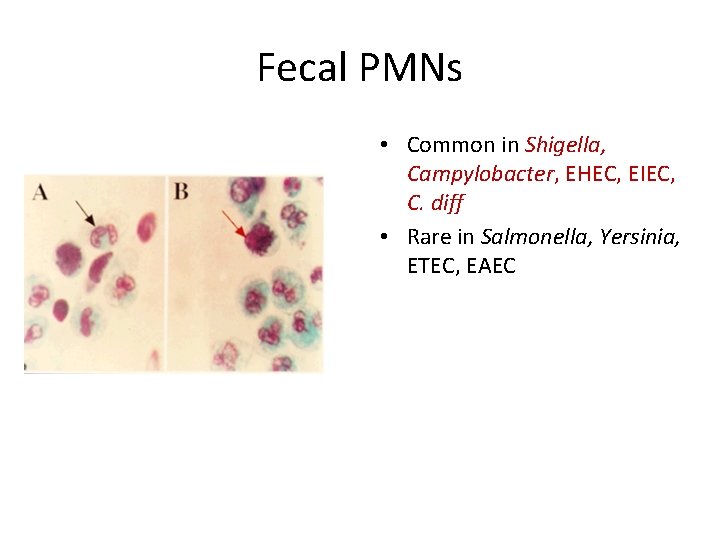
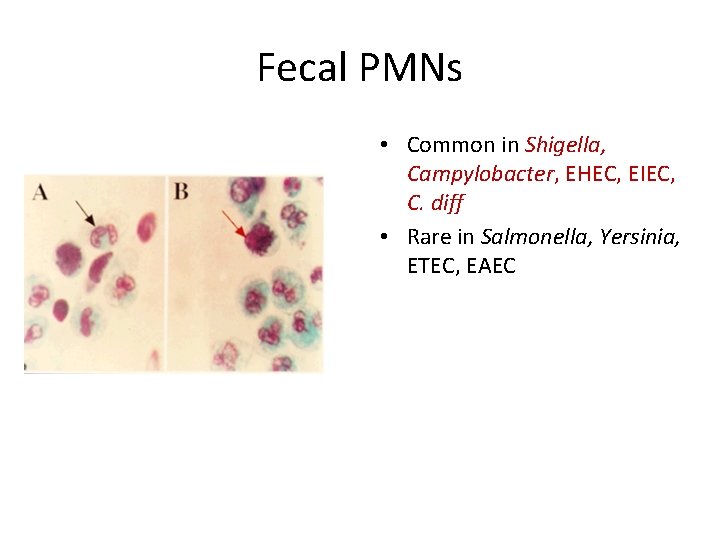
Fecal PMNs • Common in Shigella, Campylobacter, EHEC, EIEC, C. diff • Rare in Salmonella, Yersinia, ETEC, EAEC
MANAGING INFECTIOUS DIARRHEA • Initial rehidration • Perform thorough clinical and epidemiological evaluation • Perform selective fecal studies • Institute selective therapy for – Traveler’s diarrhea – Shigellosis – Campylobacter infection • Avoid administering antimotilty agents • Selectively administer available vaccines
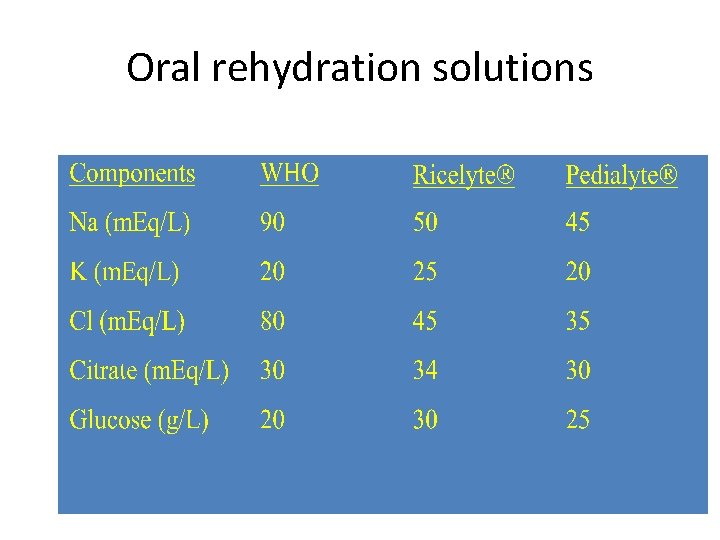
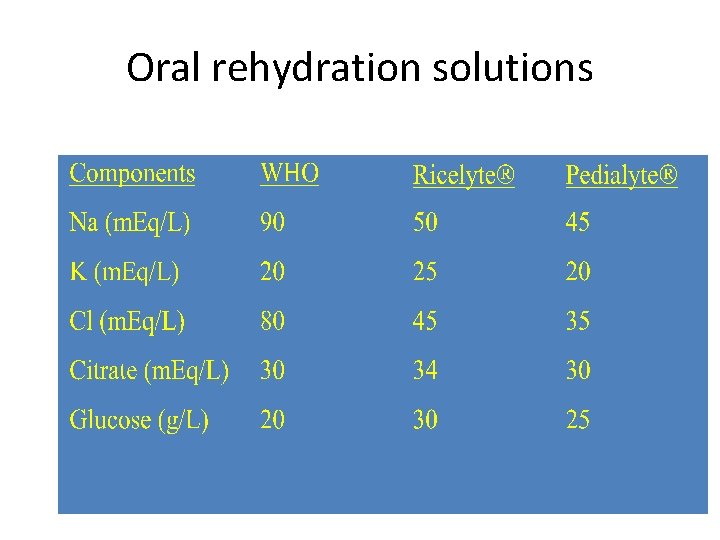
Oral rehydration solutions

Treatment of Diarrhea • Treatment of specific etiology • Non-specific treatment – hydration – Absorptions (Kaopectate®) – Bismuth – Antiperistaltics/opiate derivatives – Fiber supplementation
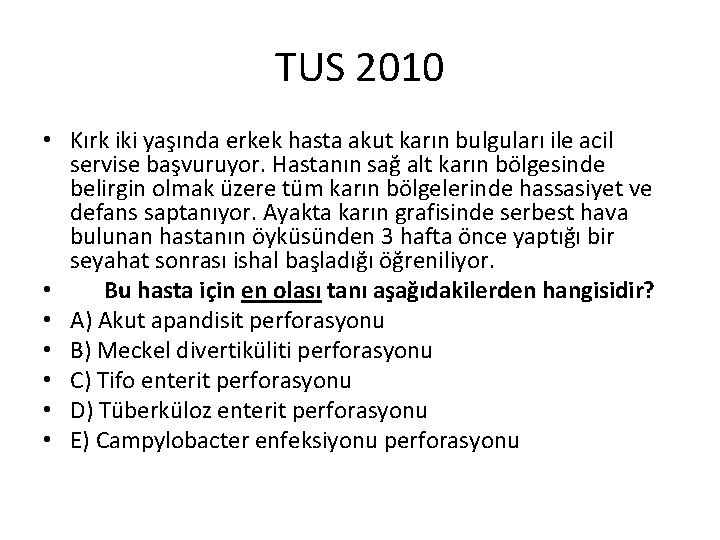
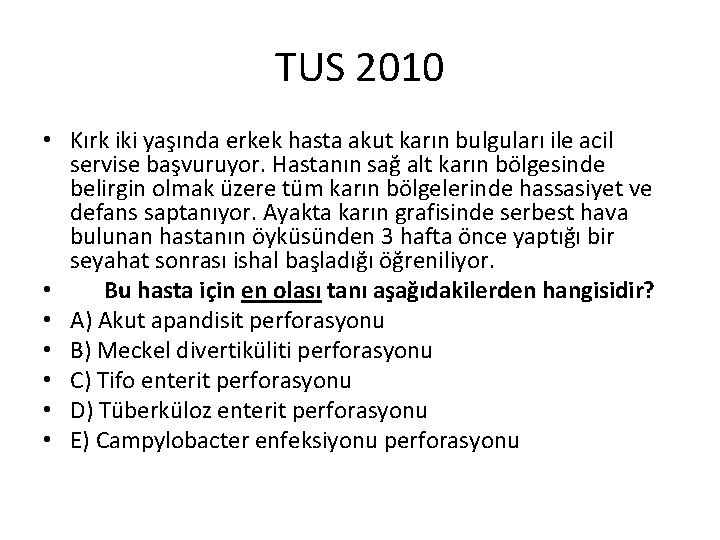
TUS 2010 • Kırk iki yaşında erkek hasta akut karın bulguları ile acil servise başvuruyor. Hastanın sağ alt karın bölgesinde belirgin olmak üzere tüm karın bölgelerinde hassasiyet ve defans saptanıyor. Ayakta karın grafisinde serbest hava bulunan hastanın öyküsünden 3 hafta önce yaptığı bir seyahat sonrası ishal başladığı öğreniliyor. • Bu hasta için en olası tanı aşağıdakilerden hangisidir? • A) Akut apandisit perforasyonu • B) Meckel divertiküliti perforasyonu • C) Tifo enterit perforasyonu • D) Tüberküloz enterit perforasyonu • E) Campylobacter enfeksiyonu perforasyonu
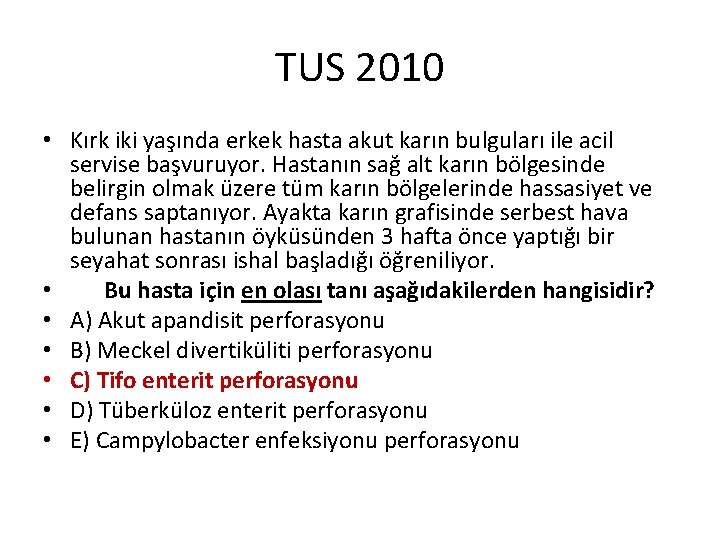
TUS 2010 • Kırk iki yaşında erkek hasta akut karın bulguları ile acil servise başvuruyor. Hastanın sağ alt karın bölgesinde belirgin olmak üzere tüm karın bölgelerinde hassasiyet ve defans saptanıyor. Ayakta karın grafisinde serbest hava bulunan hastanın öyküsünden 3 hafta önce yaptığı bir seyahat sonrası ishal başladığı öğreniliyor. • Bu hasta için en olası tanı aşağıdakilerden hangisidir? • A) Akut apandisit perforasyonu • B) Meckel divertiküliti perforasyonu • C) Tifo enterit perforasyonu • D) Tüberküloz enterit perforasyonu • E) Campylobacter enfeksiyonu perforasyonu
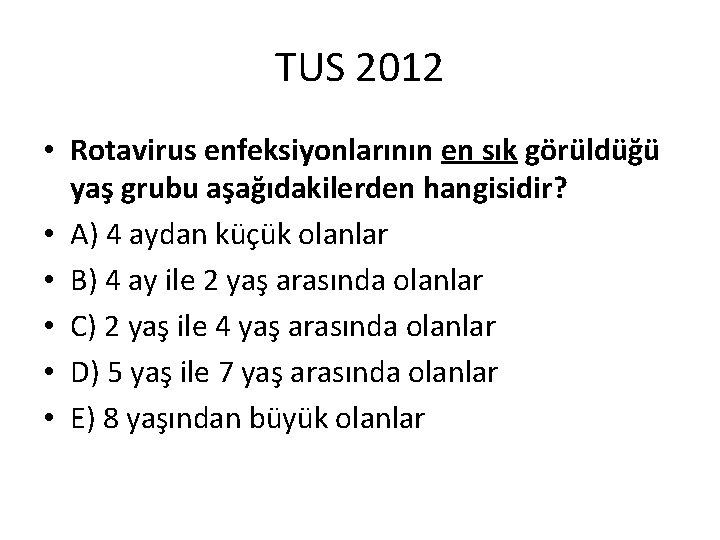
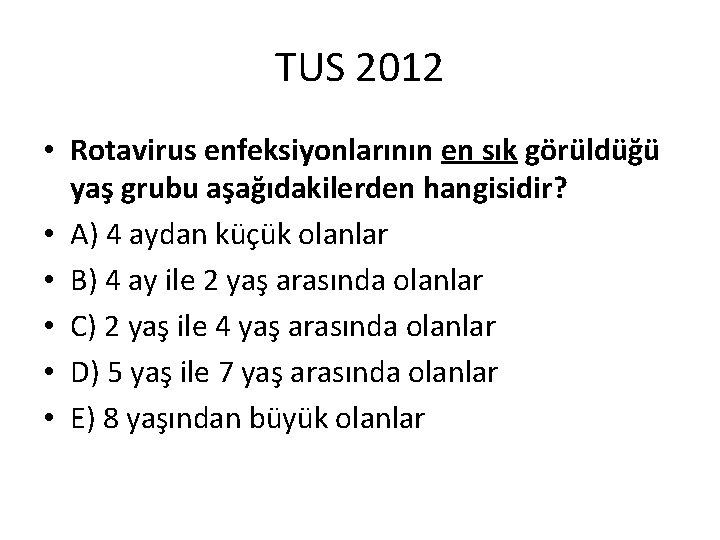
TUS 2012 • Rotavirus enfeksiyonlarının en sık görüldüğü yaş grubu aşağıdakilerden hangisidir? • A) 4 aydan küçük olanlar • B) 4 ay ile 2 yaş arasında olanlar • C) 2 yaş ile 4 yaş arasında olanlar • D) 5 yaş ile 7 yaş arasında olanlar • E) 8 yaşından büyük olanlar
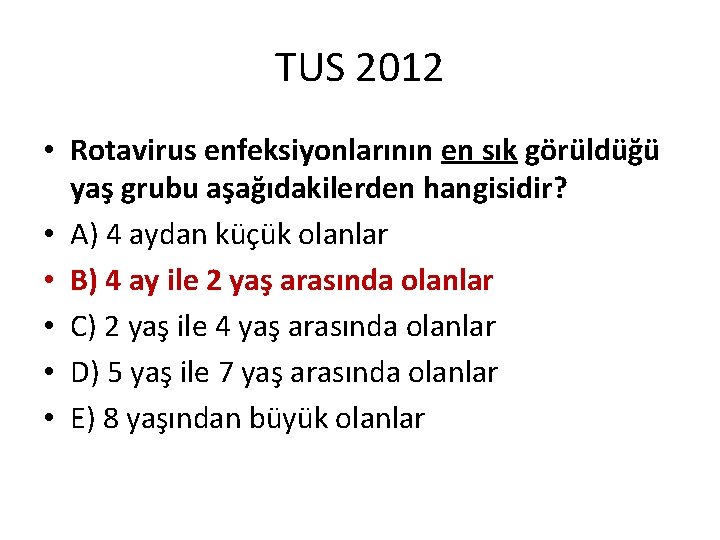
TUS 2012 • Rotavirus enfeksiyonlarının en sık görüldüğü yaş grubu aşağıdakilerden hangisidir? • A) 4 aydan küçük olanlar • B) 4 ay ile 2 yaş arasında olanlar • C) 2 yaş ile 4 yaş arasında olanlar • D) 5 yaş ile 7 yaş arasında olanlar • E) 8 yaşından büyük olanlar
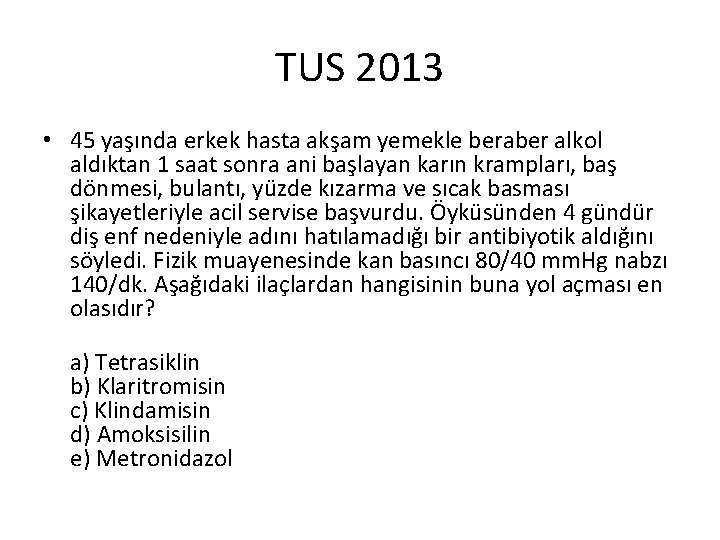
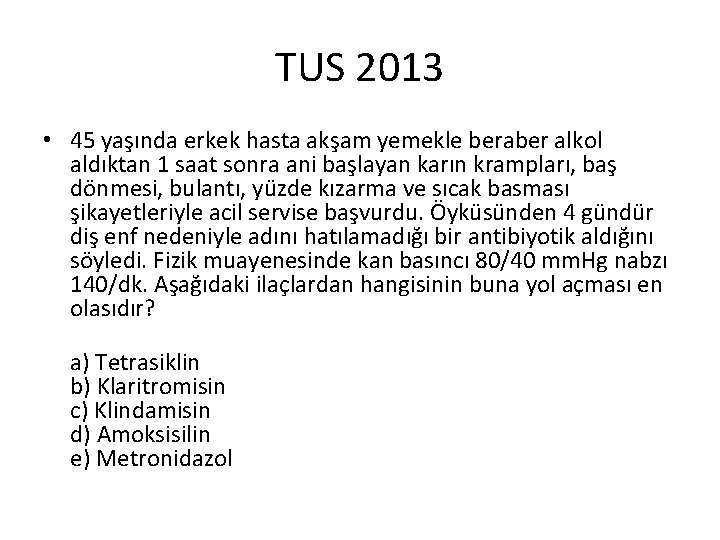
TUS 2013 • 45 yaşında erkek hasta akşam yemekle beraber alkol aldıktan 1 saat sonra ani başlayan karın krampları, baş dönmesi, bulantı, yüzde kızarma ve sıcak basması şikayetleriyle acil servise başvurdu. Öyküsünden 4 gündür diş enf nedeniyle adını hatılamadığı bir antibiyotik aldığını söyledi. Fizik muayenesinde kan basıncı 80/40 mm. Hg nabzı 140/dk. Aşağıdaki ilaçlardan hangisinin buna yol açması en olasıdır? a) Tetrasiklin b) Klaritromisin c) Klindamisin d) Amoksisilin e) Metronidazol

TUS 2013 • 45 yaşında erkek hasta akşam yemekle beraber alkol aldıktan 1 saat sonra ani başlayan karın krampları, baş dönmesi, bulantı, yüzde kızarma ve sıcak basması şikayetleriyle acil servise başvurdu. Öyküsünden 4 gündür diş enf nedeniyle adını hatılamadığı bir antibiyotik aldığını söyledi. Fizik muayenesinde kan basıncı 80/40 mm. Hg nabzı 140/dk. Aşağıdaki ilaçlardan hangisinin buna yol açması en olasıdır? a) Tetrasiklin b) Klaritromisin c) Klindamisin d) Amoksisilin e) Metronidazol

TUS 2013 • 45 yaşında erkek hasta akşam yemekle beraber alkol aldıktan 1 saat sonra ani başlayan karın krampları, baş dönmesi, bulantı, yüzde kızarma ve sıcak basması şikayetleriyle acil servise başvurdu. Öyküsünden 4 gündür diş enf nedeniyle adını hatılamadığı bir antibiyotik aldığını söyledi. Fizik muayenesinde kan basıncı 80/40 mm. Hg nabzı 140/dk. Aşağıdaki ilaçlardan hangisinin buna yol açması en olasıdır? a) Tetrasiklin b) Klaritromisin c) Klindamisin d) Amoksisilin e) Metronidazol

• One of the most common alcohol-antibiotic interactions is with the antimicrobial agent metronidazole (Flagyl). Metronidazole is used for a variety of infections, including gastrointestinal, skin, joint and respiratory tract infections. • Taking metronidazole with alcohol may result in a reaction called a “disulfiram-like reaction”. A “disulfiram-like reaction” may include nausea, flushing of the skin, stomach cramps, vomiting, headaches, rapid heart rate, and difficulty breathing. • A similar reaction may occur with other antibiotics.
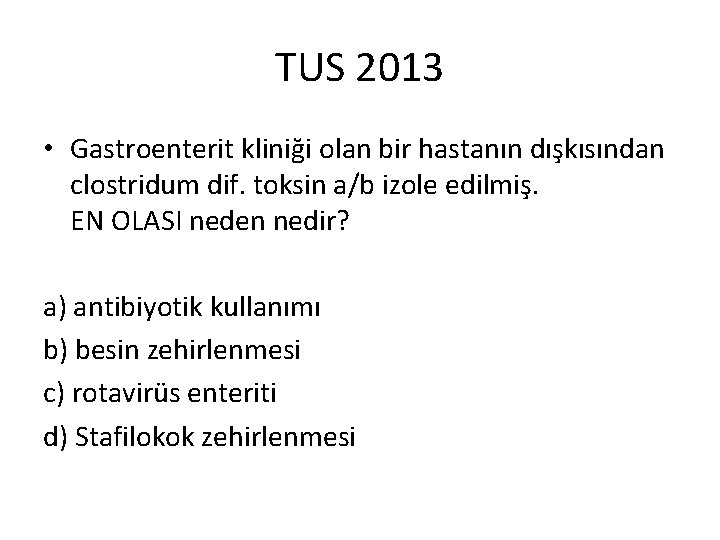
TUS 2013 • Gastroenterit kliniği olan bir hastanın dışkısından clostridum dif. toksin a/b izole edilmiş. EN OLASI neden nedir? a) antibiyotik kullanımı b) besin zehirlenmesi c) rotavirüs enteriti d) Stafilokok zehirlenmesi
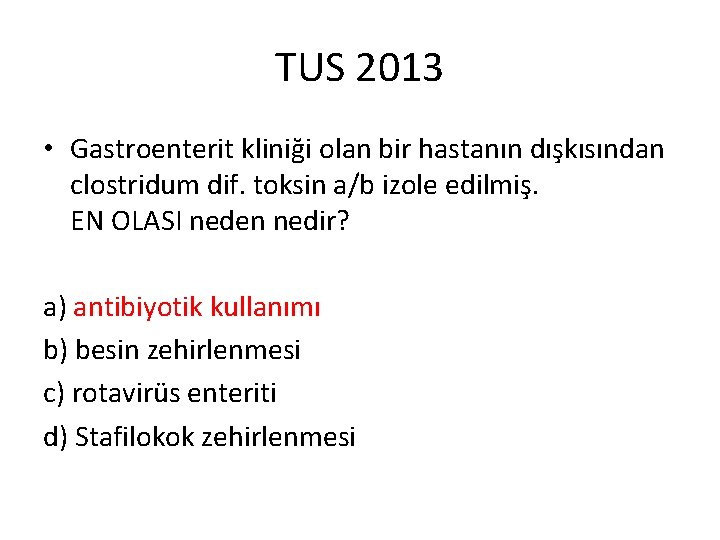
TUS 2013 • Gastroenterit kliniği olan bir hastanın dışkısından clostridum dif. toksin a/b izole edilmiş. EN OLASI neden nedir? a) antibiyotik kullanımı b) besin zehirlenmesi c) rotavirüs enteriti d) Stafilokok zehirlenmesi
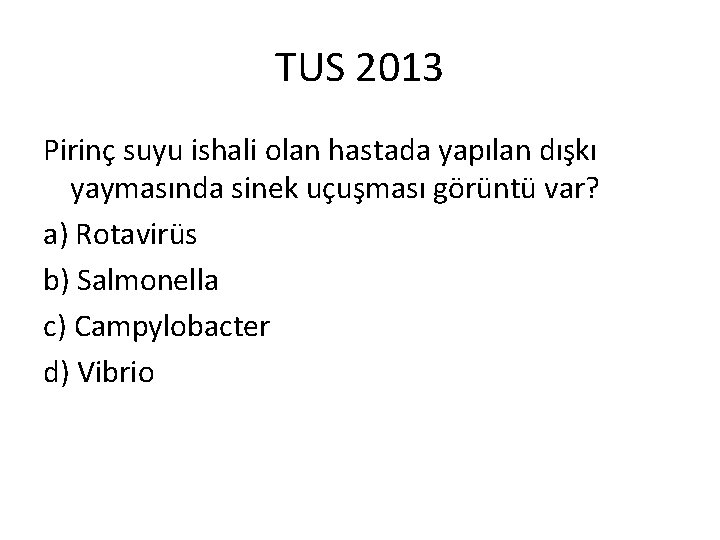
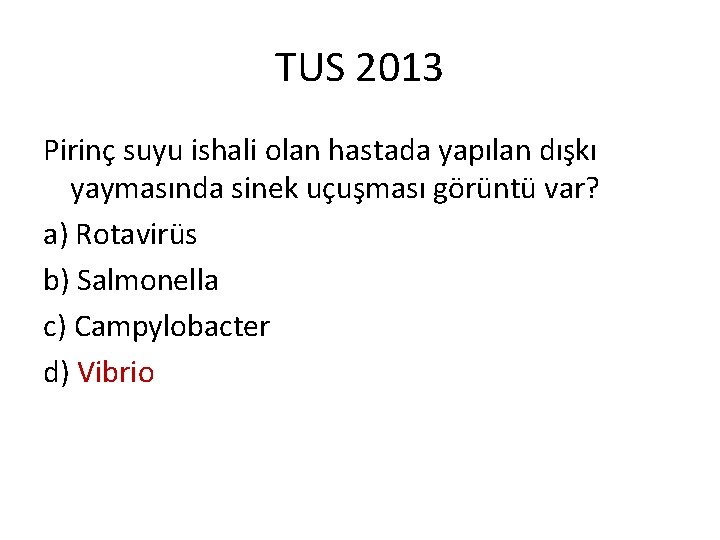
TUS 2013 Pirinç suyu ishali olan hastada yapılan dışkı yaymasında sinek uçuşması görüntü var? a) Rotavirüs b) Salmonella c) Campylobacter d) Vibrio
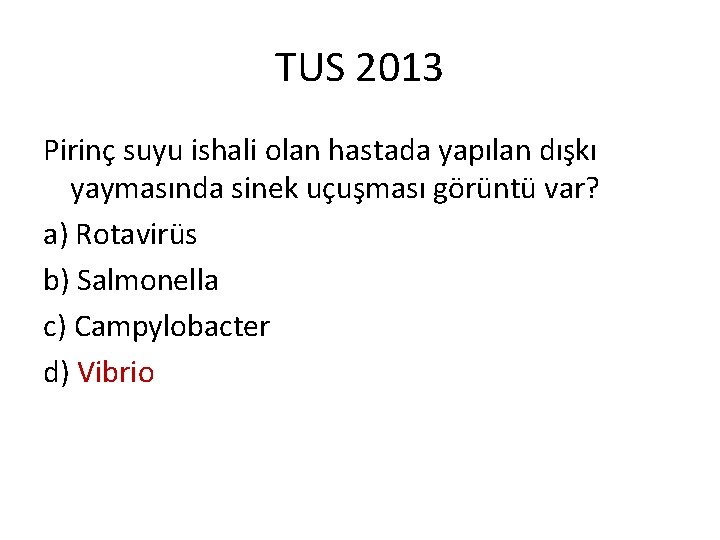
TUS 2013 Pirinç suyu ishali olan hastada yapılan dışkı yaymasında sinek uçuşması görüntü var? a) Rotavirüs b) Salmonella c) Campylobacter d) Vibrio
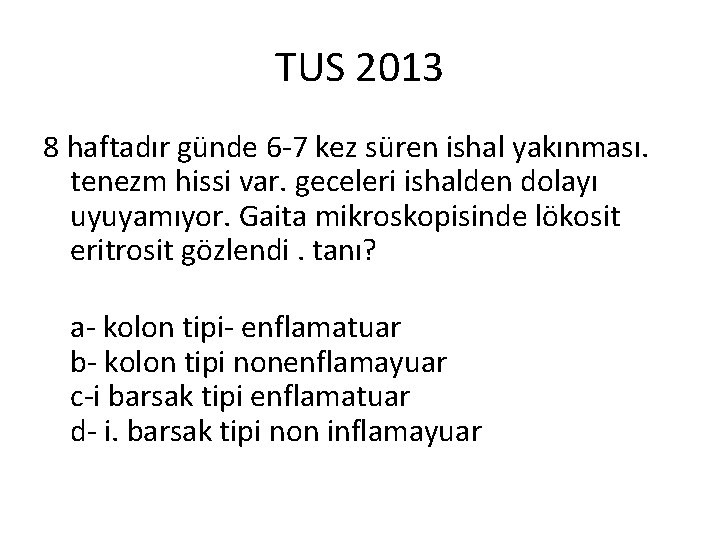
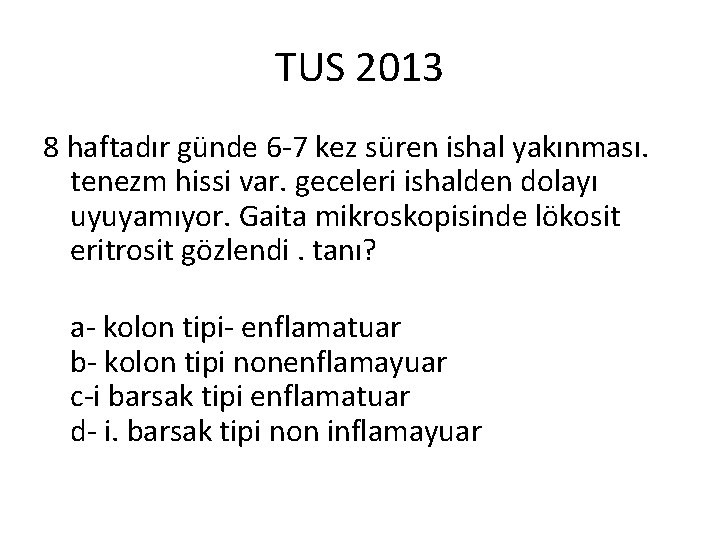
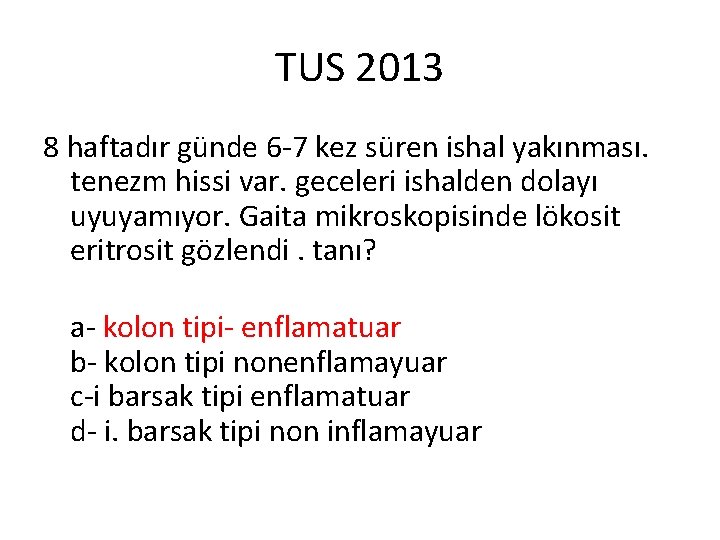
TUS 2013 8 haftadır günde 6 -7 kez süren ishal yakınması. tenezm hissi var. geceleri ishalden dolayı uyuyamıyor. Gaita mikroskopisinde lökosit eritrosit gözlendi. tanı? a- kolon tipi- enflamatuar b- kolon tipi nonenflamayuar c-i barsak tipi enflamatuar d- i. barsak tipi non inflamayuar
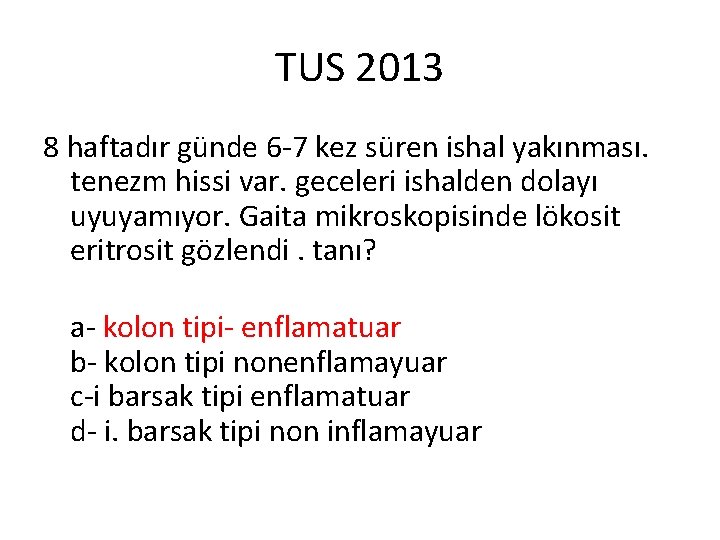
TUS 2013 8 haftadır günde 6 -7 kez süren ishal yakınması. tenezm hissi var. geceleri ishalden dolayı uyuyamıyor. Gaita mikroskopisinde lökosit eritrosit gözlendi. tanı? a- kolon tipi- enflamatuar b- kolon tipi nonenflamayuar c-i barsak tipi enflamatuar d- i. barsak tipi non inflamayuar

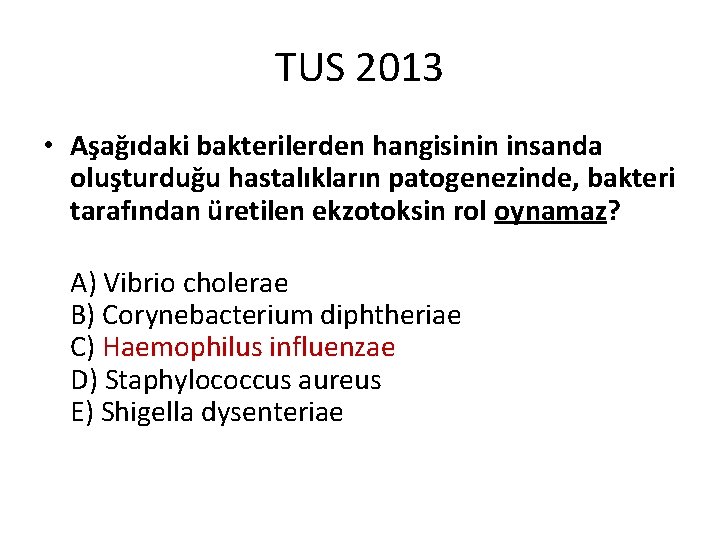
TUS 2013 • Aşağıdaki bakterilerden hangisinin insanda oluşturduğu hastalıkların patogenezinde, bakteri tarafından üretilen ekzotoksin rol oynamaz? A) Vibrio cholerae B) Corynebacterium diphtheriae C) Haemophilus influenzae D) Staphylococcus aureus E) Shigella dysenteriae
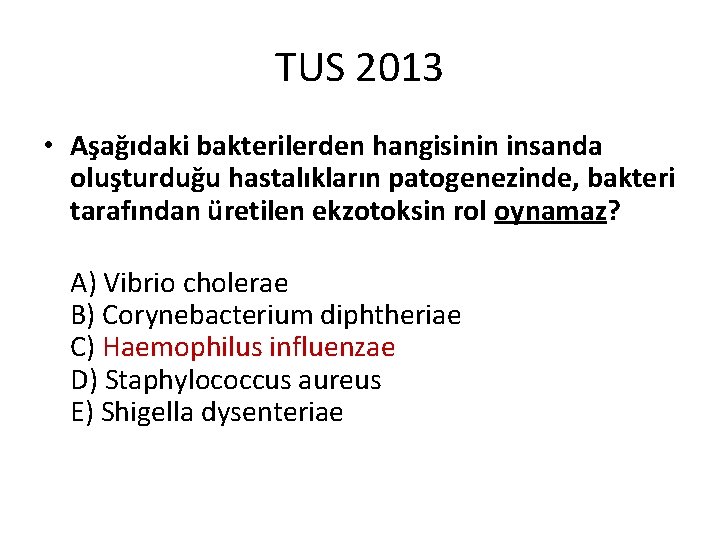
TUS 2013 • Aşağıdaki bakterilerden hangisinin insanda oluşturduğu hastalıkların patogenezinde, bakteri tarafından üretilen ekzotoksin rol oynamaz? A) Vibrio cholerae B) Corynebacterium diphtheriae C) Haemophilus influenzae D) Staphylococcus aureus E) Shigella dysenteriae
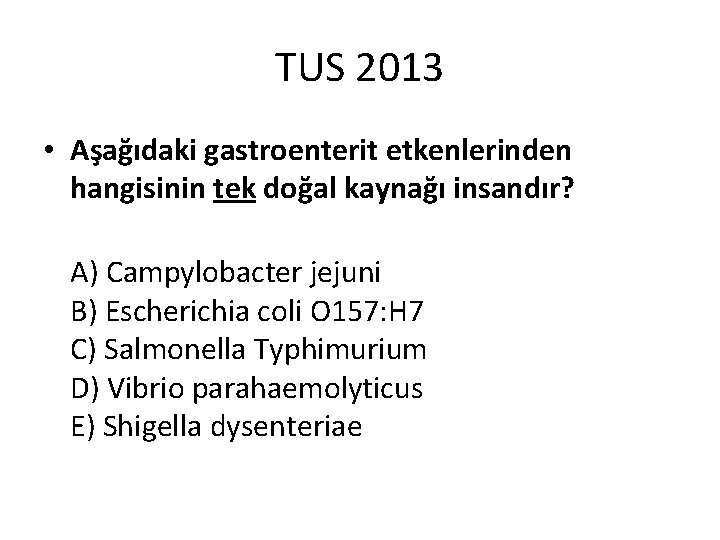
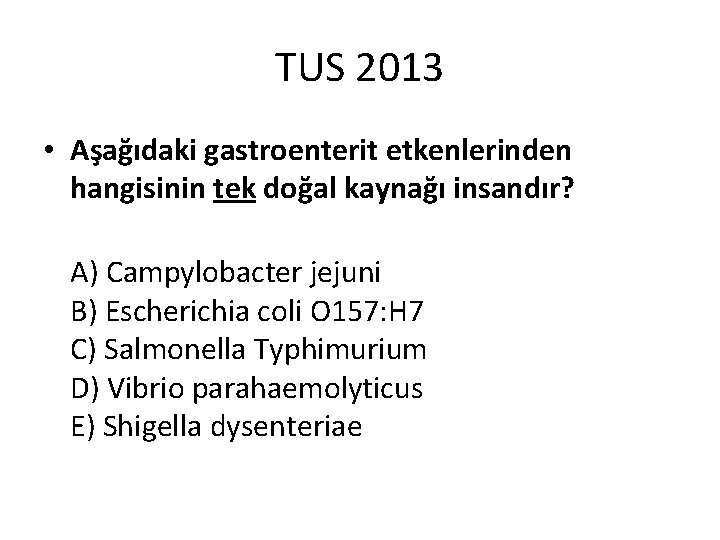
TUS 2013 • Aşağıdaki gastroenterit etkenlerinden hangisinin tek doğal kaynağı insandır? A) Campylobacter jejuni B) Escherichia coli O 157: H 7 C) Salmonella Typhimurium D) Vibrio parahaemolyticus E) Shigella dysenteriae
TUS 2013 • Aşağıdaki gastroenterit etkenlerinden hangisinin tek doğal kaynağı insandır? A) Campylobacter jejuni B) Escherichia coli O 157: H 7 C) Salmonella Typhimurium D) Vibrio parahaemolyticus E) Shigella dysenteriae

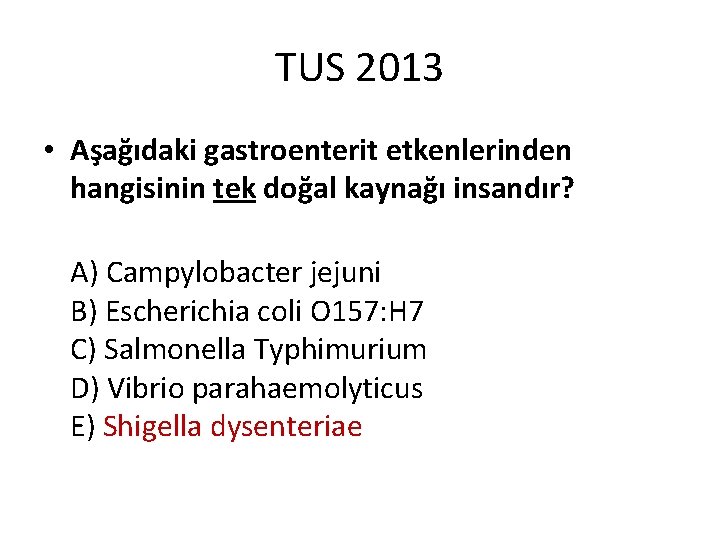
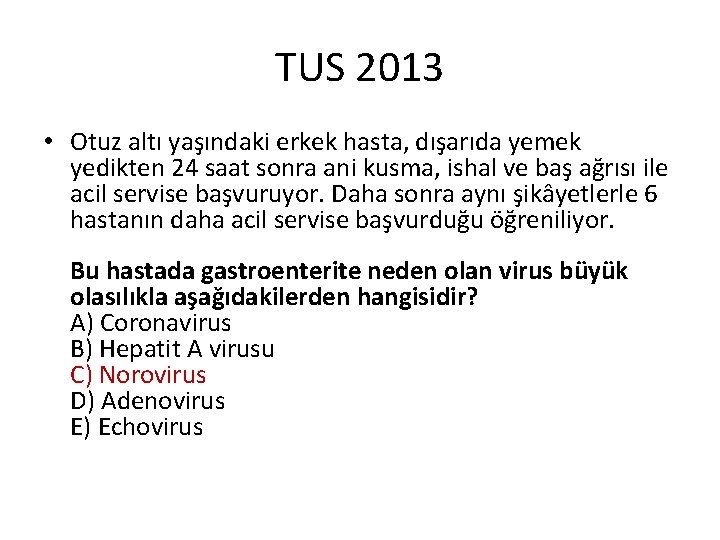
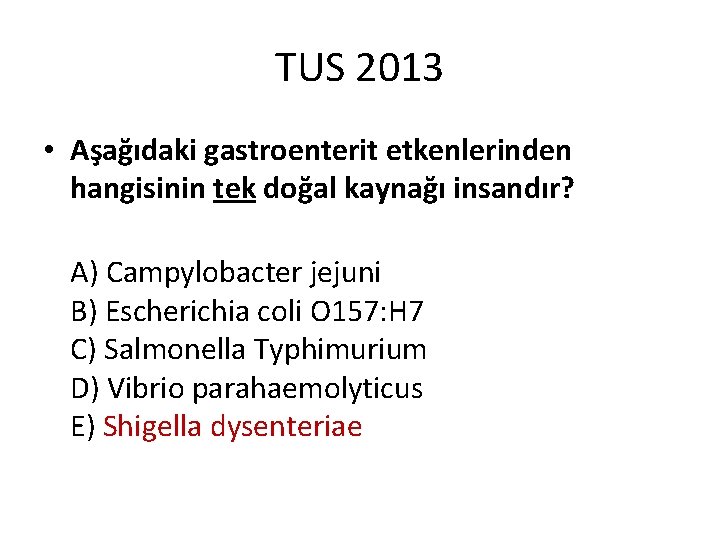
TUS 2013 • Otuz altı yaşındaki erkek hasta, dışarıda yemek yedikten 24 saat sonra ani kusma, ishal ve baş ağrısı ile acil servise başvuruyor. Daha sonra aynı şikâyetlerle 6 hastanın daha acil servise başvurduğu öğreniliyor. Bu hastada gastroenterite neden olan virus büyük olasılıkla aşağıdakilerden hangisidir? A) Coronavirus B) Hepatit A virusu C) Norovirus D) Adenovirus E) Echovirus
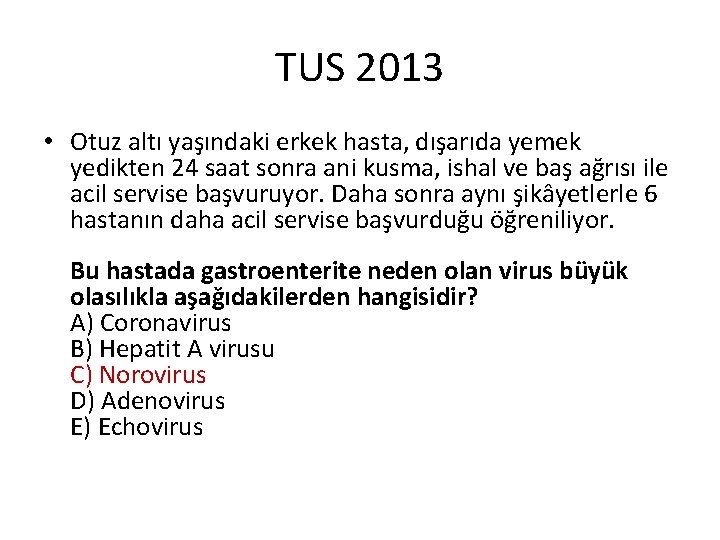
TUS 2013 • Otuz altı yaşındaki erkek hasta, dışarıda yemek yedikten 24 saat sonra ani kusma, ishal ve baş ağrısı ile acil servise başvuruyor. Daha sonra aynı şikâyetlerle 6 hastanın daha acil servise başvurduğu öğreniliyor. Bu hastada gastroenterite neden olan virus büyük olasılıkla aşağıdakilerden hangisidir? A) Coronavirus B) Hepatit A virusu C) Norovirus D) Adenovirus E) Echovirus
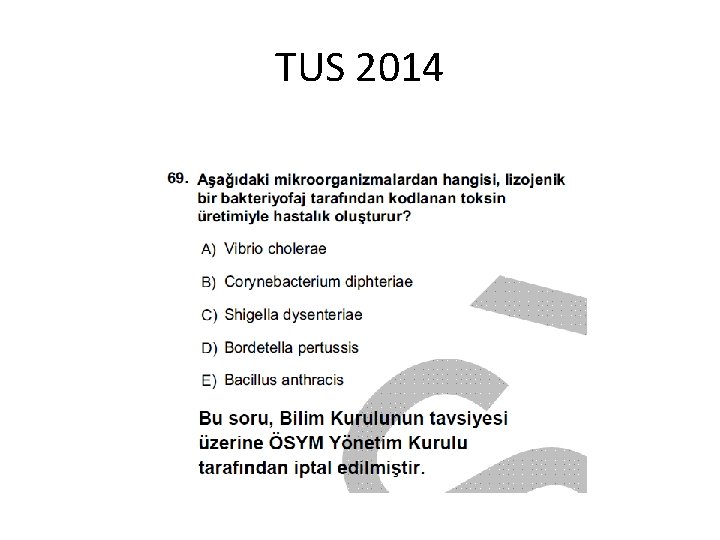
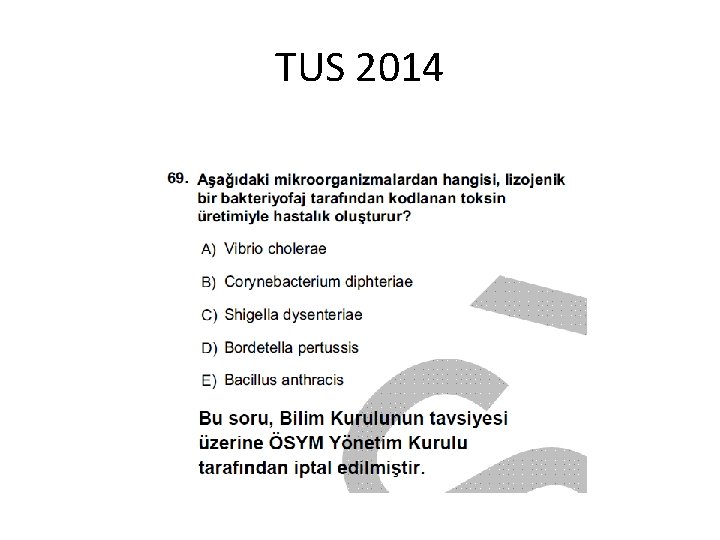
TUS 2014
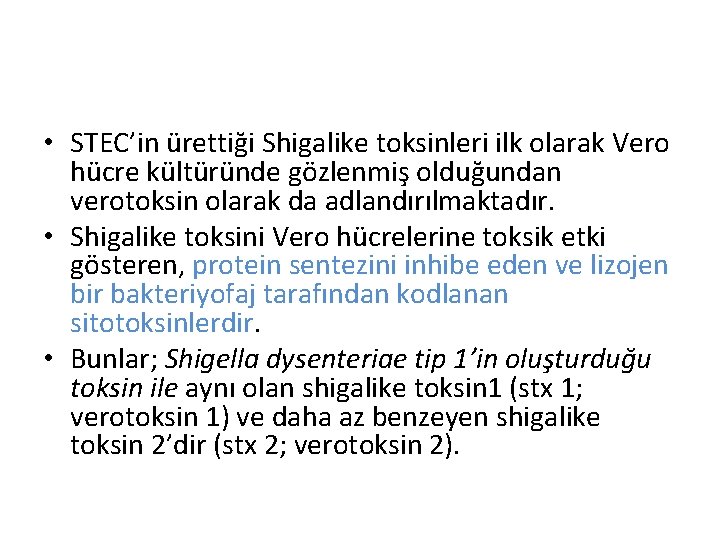
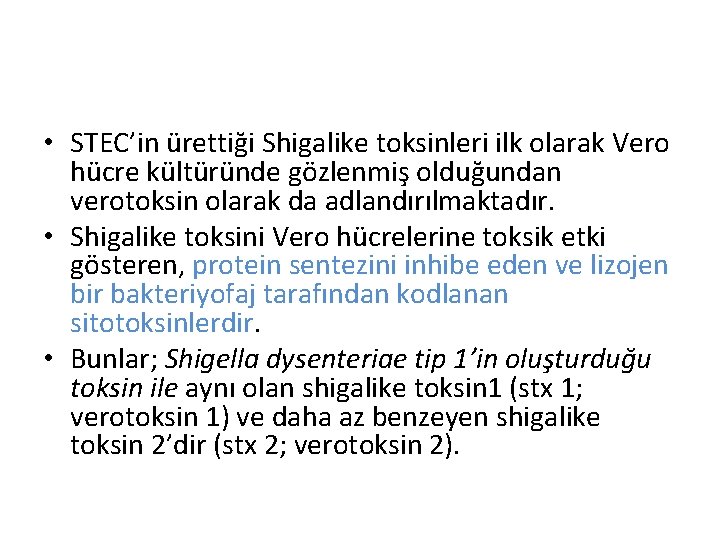
• STEC’in ürettiği Shigalike toksinleri ilk olarak Vero hücre kültüründe gözlenmiş olduğundan verotoksin olarak da adlandırılmaktadır. • Shigalike toksini Vero hücrelerine toksik etki gösteren, protein sentezini inhibe eden ve lizojen bir bakteriyofaj tarafından kodlanan sitotoksinlerdir. • Bunlar; Shigella dysenteriae tip 1’in oluşturduğu toksin ile aynı olan shigalike toksin 1 (stx 1; verotoksin 1) ve daha az benzeyen shigalike toksin 2’dir (stx 2; verotoksin 2).

TUS 2014

TUS 2014

TUS 2015
TUS 2015
TUS 2015
TUS 2015
 Ekzotoksin
Ekzotoksin Medivia
Medivia Coadsysexam yeditepe
Coadsysexam yeditepe Coadsys exam
Coadsys exam Meral yılmaz öğretmen
Meral yılmaz öğretmen Pınar seden meral
Pınar seden meral Meral nur ergin
Meral nur ergin Meral dogan
Meral dogan Protokol sıra düzeni
Protokol sıra düzeni Colposcopy biopsy
Colposcopy biopsy Gastroenteritis suffix
Gastroenteritis suffix Gastroenteritis at a university in texas
Gastroenteritis at a university in texas Akutni enterokolitis
Akutni enterokolitis Gastroenteritis bacterial
Gastroenteritis bacterial Aerosolisolation
Aerosolisolation Viral gastroenteritis
Viral gastroenteritis Akutni gastroenteritis
Akutni gastroenteritis The element at the end of a medical term is a
The element at the end of a medical term is a Gastroenteritis
Gastroenteritis Rotatest
Rotatest Acute gastroenteritis
Acute gastroenteritis Unit 2 food food food
Unit 2 food food food Sequence of food chain
Sequence of food chain Food chain
Food chain What do the arrows on the food web represent
What do the arrows on the food web represent Food chain and food web
Food chain and food web Food web
Food web Food chain for kids
Food chain for kids Food chains, food webs and ecological pyramids
Food chains, food webs and ecological pyramids Food webs and energy pyramids
Food webs and energy pyramids Food webs and energy pyramids worksheet answers
Food webs and energy pyramids worksheet answers Bill nye food webs
Bill nye food webs Role play on healthy food and junk food
Role play on healthy food and junk food Introduction of role play
Introduction of role play Temperate rainforest food web
Temperate rainforest food web Junk food names
Junk food names A paragraph about fast food
A paragraph about fast food Food scientists measure food energy in
Food scientists measure food energy in Importance of food
Importance of food Which food is a tcs food
Which food is a tcs food Very little food
Very little food Food handlers can contaminate food when they answer
Food handlers can contaminate food when they answer Food product design eric schlosser
Food product design eric schlosser Ladybug food chain
Ladybug food chain Fast food can be defined as any food that contributes
Fast food can be defined as any food that contributes Easy food web
Easy food web Explore food.foodafactoflife
Explore food.foodafactoflife Junk food vs healthy food project
Junk food vs healthy food project How many food chains are there in the food web
How many food chains are there in the food web Milk junk
Milk junk Pyramid food
Pyramid food What is food safety
What is food safety Changes caused by agriculture and overgrazing
Changes caused by agriculture and overgrazing Food a fact of life
Food a fact of life When should hand antiseptics be used
When should hand antiseptics be used A food handler stored a sanitizer spray bottle
A food handler stored a sanitizer spray bottle Food product knowledge training
Food product knowledge training List three examples of in-transit foodservice operations
List three examples of in-transit foodservice operations Abbreviations for tablespoon and teaspoon
Abbreviations for tablespoon and teaspoon Health audit directorate
Health audit directorate Food and dining in pompeii and herculaneum
Food and dining in pompeii and herculaneum Illuminate aqa food preparation and nutrition
Illuminate aqa food preparation and nutrition Catering provision
Catering provision Unit 5 food and entertaining
Unit 5 food and entertaining Tudor food for the rich
Tudor food for the rich Tudor food and drink
Tudor food and drink What tudors ate
What tudors ate Food and fiber industry
Food and fiber industry Tudor food and drink
Tudor food and drink Foodinsight.org
Foodinsight.org Pros and cons of organic farming
Pros and cons of organic farming Ch 36 apush
Ch 36 apush Food and beverage industry in sri lanka
Food and beverage industry in sri lanka Animal quarantine department
Animal quarantine department Paramecia use _________ to move and capture food.
Paramecia use _________ to move and capture food. Service sequence
Service sequence Application for the post of a waitress
Application for the post of a waitress Sequence of service in restaurant
Sequence of service in restaurant Accompaniments garnishes and decorations for desserts
Accompaniments garnishes and decorations for desserts My favourite drink
My favourite drink Medieval times drink menu
Medieval times drink menu Basic food and beverage knowledge
Basic food and beverage knowledge Datingoo
Datingoo Food and nutrition unit 4
Food and nutrition unit 4 Attributes of food and beverage service personnel
Attributes of food and beverage service personnel 38-2 the process of digestion
38-2 the process of digestion School food and beverage policy
School food and beverage policy Attributes of food and beverage service personnel
Attributes of food and beverage service personnel Attributes of food and beverage service personnel
Attributes of food and beverage service personnel Food chain is
Food chain is Food vocabulary presentation
Food vocabulary presentation Primary and secondary processing
Primary and secondary processing Food product development examples
Food product development examples Primary and secondary food processing
Primary and secondary food processing Food and nutrition unit 4
Food and nutrition unit 4 Konya food and agriculture university
Konya food and agriculture university Food web with a decomposer
Food web with a decomposer Food web words
Food web words Food web and chain
Food web and chain Food and beverage marketing management
Food and beverage marketing management Food and beverage management system
Food and beverage management system 38-1 food and nutrition
38-1 food and nutrition Need food and energy
Need food and energy Food and beverage service sequence
Food and beverage service sequence Kasavana and smith matrix
Kasavana and smith matrix Food and beverage management book pdf
Food and beverage management book pdf Food and beverage management notes
Food and beverage management notes Food and beverage cost control 5th edition pdf
Food and beverage cost control 5th edition pdf Food and beverage cycle
Food and beverage cycle New wave brasserie (gastrodome)
New wave brasserie (gastrodome) Food and beverage organizational chart
Food and beverage organizational chart Food web with decomposers producers consumers
Food web with decomposers producers consumers Ethics of food production and consumption
Ethics of food production and consumption How does energy flow in a food web
How does energy flow in a food web Wat is convenience food
Wat is convenience food It is the process of removing food and other types of soil
It is the process of removing food and other types of soil Food and beverage service areas
Food and beverage service areas Food and fun class 4 evs ppt
Food and fun class 4 evs ppt Food safety regulations and standards
Food safety regulations and standards Types of food and beverage service operation
Types of food and beverage service operation Chapter 10 lesson 4 nutrition labels and food safety
Chapter 10 lesson 4 nutrition labels and food safety Chapter 10 lesson 4 nutrition labels and food safety
Chapter 10 lesson 4 nutrition labels and food safety Hotel beverage operation
Hotel beverage operation Commercial and noncommercial food service operations
Commercial and noncommercial food service operations Root beer food pairing
Root beer food pairing Favorite food answers
Favorite food answers How does energy flow in an ecosystem
How does energy flow in an ecosystem Food and research action center
Food and research action center Disadvantages of russian service
Disadvantages of russian service Lbv foods examples
Lbv foods examples Usda food and nutrition service
Usda food and nutrition service Unit 3 food and drink
Unit 3 food and drink Understanding standards advanced higher geography
Understanding standards advanced higher geography Natural and artificial food additives
Natural and artificial food additives Food and nutrition unit 5
Food and nutrition unit 5 National center for food protection and defense
National center for food protection and defense Funtions of food
Funtions of food Intrinsic parameters of food
Intrinsic parameters of food Cooking makes food soft tasty and
Cooking makes food soft tasty and Higher health and food technology
Higher health and food technology Food loss and waste
Food loss and waste Gm foods advantages and disadvantages
Gm foods advantages and disadvantages Energy pyrmaid
Energy pyrmaid Food safety and inspection service definition
Food safety and inspection service definition