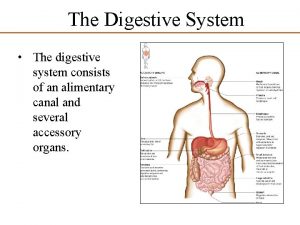
DIGESTIVE SYSTEM The digestive system consists of 1




















- Slides: 80
DIGESTIVE SYSTEM The digestive system consists of: � 1 -Alimentary canal and, � 2 -Associated glands. �

DIGESTIVE SYSTEM -The alimentary canal could be considerd as the � doorway through which all nutrients and energy sources of the body pass before they are utilized it extends from mouth to anus. -The associated glands include salivary glands, liver � and pancreas which empty their secretion into alimentary canal.
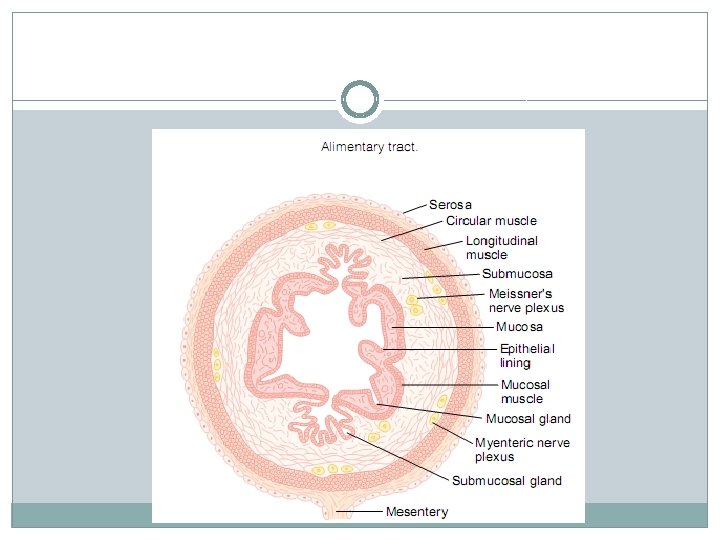
GENERAL ANATOMY OF DIGESTIVE SYSTEM The structure of the wall of the alimentary canal � differs in the various regions, but is usually composed of several layers which are from outside inwards: 1 -A serous or fibrous coat composed of a thin layer � of connective tissue. 2 -The muscular coat, composed of two layers of � smooth muscle fibers, an outer longitudinal layer and an inner circular layer.
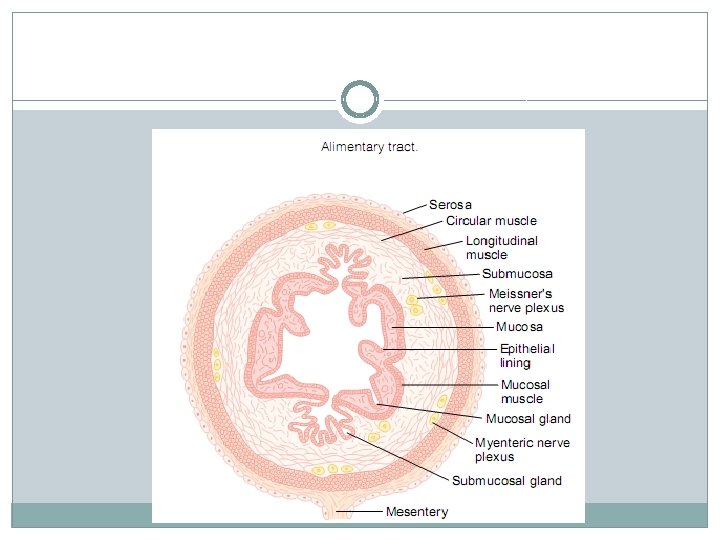
GENERAL ANATOMY OF DIGESTIVE SYSTEM 3 -The submucosa is made up of loose connective � tissue elements containing numerous blood and lymph vessels. 4 -The muscularis mucosa, containing smooth � muscle cells. 5 - The mucosa, or mucous membrane. �
GENERAL ANATOMY OF DIGESTIVE SYSTEM At certain points along the alimentary tract, the � circular muscles are hypertrophied, forming areas of constriction, or sphincters. �
INNERVATION OF THE DIGESTIVE TRACT Except for the striated muscles of the mouth , the � upper part of the esophagus, and the external anal sphincter , the musculature of the digestive tract is composed of smooth muscle fibers. All smooth muscles are involuntary , and nervous control in the GIT takes place by autonomic nerves which are both extrinsic and intrinsic.
INNERVATION OF THE DIGESTIVE TRACT A neural network is located between the longitudinal � and the circular muscle layers(Aurbach's plexus). Another one lies between the circular muscle layer and the submucosa (Meissner's plexus). These plexuses are connected together and receive connections from the extrinsic autonomic nerves. Auerbach's plexus is mainly motor while Meissner's plexus is mainly secretory.

GENERAL ANATOMY OF DIGESTIVE SYSTEM These local reflex arcs play an important role in the � downward transport of food in the GIT. The intrinsic neural structures are modulated by � extrinsic nerves which belong to both divisions of the autonomic nervous system(sympathetic and parasympathetic).

GENERAL ANATOMY OF DIGESTIVE SYSTEM In general the parasympathetic system is excitatory � to all the musculature forming the walls of the GIT but inhibitory to the sphincters , while the sympathetic nerves have the reverse effects.
GENERAL FUNCTION OF GIT 1 -Digestion: is the breakdown of food material into � small particles , ready for absorption and utilization by the body cells. Digestion mostly occur in the proximal part of the small intestine.
GENERAL FUNCTION OF GIT 2 -Absorption: is the transfer of the contents of the � gut into the mucosa , this occurs as a net result of lumen to blood , and blood to lumen movements. Absorption of sugars , amino acids and bile acids is � mainly Na+ dependent(active transport), in which Na -K ATPase are the source for energy. Lipid absorption occurs by passive diffusion.
THE MAIN PHYSIOLOGICAL FUNCTIONS 3 -Secretion: It is the transport of fluid , electrolytes, � peptides, or proteins from cells or tissues into blood , body fluids, or body cavities (as the lumen of the GIT). Excretion is the same process , but the substances � transported are waste products , e. g. bilirubin. About 7500 ml of secretions added daily to the lumen of � the GIT. About 36 g of protein and 2 g of sodium is present in the � secretion. Secretions are usually isotonic which the plasma, except � the saliva which is hypotonic relative to the plasma.
THE MAIN PHYSIOLOGICAL FUNCTIONS OF GIT ARE 4 -GIT serves also in the body's immune system. � Humoral antibodies and cellular immune system(lymphocytes in the Peyer's patches of the intestine )protecting the body against microorganisms in the lumen of the gut and foreign proteins, which act as antigens. Changes in the cellular activities of GIT are usually � associated with changes in the blood flow.

THE MAIN PHYSIOLOGICAL FUNCTIONS OF GIT ARE The endocrine glands also have a role in controlling � the functions of GIT. The anterior pituitary exerts trophic effects on the gut , adrenal corticosteroids help the transport of water and electrolytes across the intestinal mucosa , and thyroid hormones modify the propagation of intestinal contents via gut.
THE MAIN PHYSIOLOGICAL FUNCTIONS OF GIT ARE � 5 -Endocrine function e. g. release of somatostatin, � intestinal glucagon
SALIVARY SECRETION The principal glands responsible for salivation are � the parotid, submandibular and sublingual salivary glands, and in addition the buccal mucosa contains a large number of small glands which secrete mucus.

SALIVARY SECRETION Each salivary gland opens in the buccal cavity by one � duct except the sublingual gland which has more than one duct. The volume of salivary secretion ranges between 1 -1. 5 L/day.

SALIVARY SECRETION A salivary gland consists of many acini , each one is � made of a layer of polyhydral cells around a central canal and resting on a basement membrane, its secretion is drained by small ducts, the ducts combine with each other forming a large duct which opens in the buccal cavity. A network of blood capillaries , lymphatics and nerve filaments surround each salivary gland


SALIVARY SECRETION TYPES OF SECRETION � 1 -Serous secretion: Containing the enzyme ptyalin(α amylase), which � is an enzyme for starch digestion. The aleoli contain zymogene granules which are precursors of enzymes. 2 -Mucous secretion : This type of secretion(glycoprotein)renders the � salivary secretion viscous for lubricating purposes , i. g. to facilitate easy and rapid swallowing.

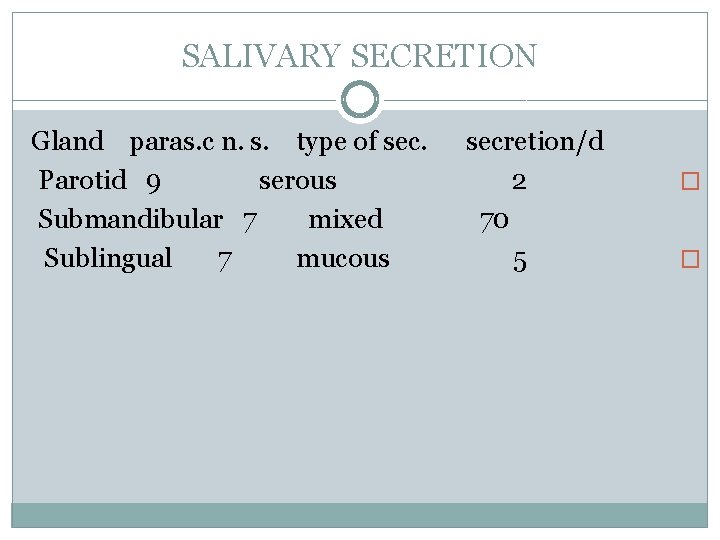
SALIVARY SECRETION In man the parotid secretion is entirely of the serous � type, the submandibular glands secrete both serous and mucus types of secretion and sublingual as well as buccal glands secrete mucus only.
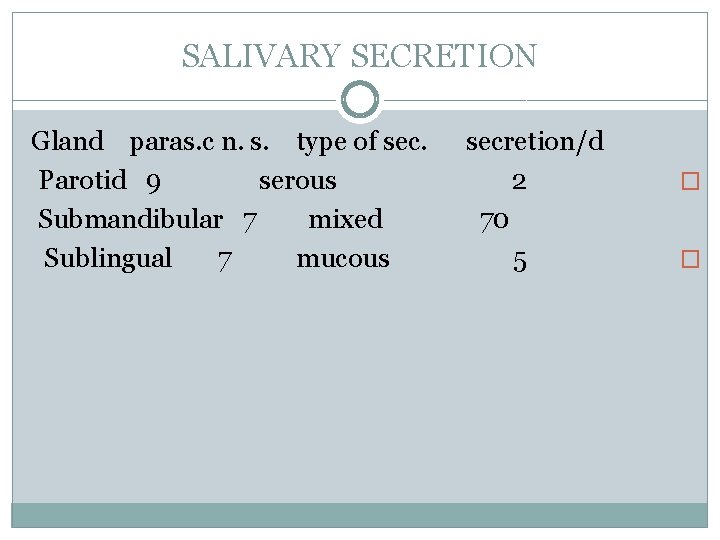
SALIVARY SECRETION Gland paras. c n. s. type of sec. Parotid 9 serous Submandibular 7 mixed Sublingual 7 mucous secretion/d 2 70 5 � �
INNERVATION OF SALIVARY GLANDS Salivary glands are supplied by autonomic nervous �
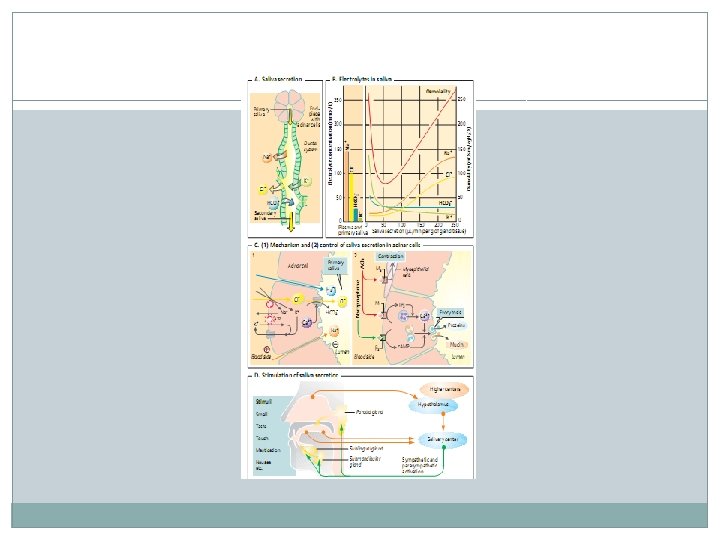
SALIVARY SECRETION EFFECTS OF STIMULATION OF � PARASYMPATHETIC NERVE SUPPLY Stimulation of parasympathetic nerve supply � causes production of the chemical transmitter Ach at the postganglionic nerve endings , which has secretory and vasodilator effects which result in:
SALIVARY SECRETION 1 -Profuse secretion of watery saliva with a relatively � low content of organic material(enzymes , mucin)&has some electrolytes. 2 -Pronounced vasodilation which appears to be due � to local release of the proteolytic enzyme kallikrein from the gland cells to act on plasma α 2 globulins (in the interstitial fluid), leading to the formation of the vasodilator polypeptide , bradykinin.
SALIVARY SECRETION kallkrein � α 2 globulins --------→ bradykinin � Bradykinin is also released in the exocrine portion of � the pancreas and in the sweat glands when they are activated to secrete.
SALIVARY SECRETION Cholinergic blocking agents , as atropine inhibit � salivary secretion. 3 -The blood flow increases up to ten times during � activity. 4 -The O 2 consumption increases about 3 folds the � resting value.
SALIVARY SECRETION EFFECT OF STIMULATION OF THE � SYMPATHETIC NERVE SUPPLY 1 -Release of small amounts of viscid saliva rich in � organic constituents only in the submandibular and sublingual glands. 2 -Marked vasoconstriction and reduction of the � blood flow.
SALIVARY SECRETION COMPOSITION OF SALIVA � The amount of salivary secretion ranges from 1 - � 1. 5 L/day. It is colourless , viscous fluid, slightly acidic, p. H 6. 6 -7. 1. If its CO 2 conent is lost by exposure to atmosphere, the p. H becomes alkaline. It is hypotonic relative to the plasma.
SALIVARY SECRETION SALIVA CONTAINS � a)99. 5% H 2 O � b)0. 2% inorganic constituents � c)0. 3% organic solids. � I-Inorganic constituents � 1 -Na. CL &Kcl : chloric ions act as coenzymes for the � salivary amylase. 2 -H 2 CO 3: Na. HCO 3&Na 2 PO 4: Na 2 HPO 4 �
SALIVARY SECRETION These bicarbonate & phosphate buffer system help to � neutralize acids or alkalis introduced into the mouth cavity. 3 -Calcium salts as calcium bicarbonate and � phosphate. If the Ph of saliva is increased (alkaline) by loss of CO 2 to the atmosphere, precipitation of insoluble calcium salts on teeth occurs and forms with organic matter a crust known as tartar. However, if calcium salts are precipitated in the duct system salivary calculi results. Ca++ also are needed to activate salivary amylase.
SALIVARY SECRETION 4 -Potassium thiocyanate which is formed from � metabolism of proteins. It has bactericidal action. II-Organic constituents: � a-Ptyalin(α –amylase), lysozyme. � b-Serum albumin , globulin , mucin , & traces of urea � , uric acid & lactic acid.
SALIVARY SECRETION Salivary amylase � It acts at an optimum p. H of 6. 9 -7. 1, it hydrolyses � cooked starch only because raw starch granules has a cellulose covering. Cooking favours digestion because it breaks the cellulose wall and in turn facilitates the action of salivary amylase. The action of salivary amylase continues in stomach for � about half an hour until gastric HCl lowers the p. H of the medium. LYZOZYME: has antibacterial action because it destroys � the polysaccharides covering of bacterial capsule.

SALIVARY SECRETION FUNCTIONS OF SALIVA: � 1 -Moistening of food to facilitate its swallowing. � 2 -Cleaning of the mouth by: � a)mechanical wash of the food residues and shed � epithelial cells which prevents putrefaction b)antibacterial action by lysozyme. � C)the bactericidal effect of thiocyanate ions. � d)saliva contains protein antibodies that can destroy � the bacteria in the oral cavity.
SALIVARY SECRETION 3 -Facilitatin of speech by moistening of the oral � cavity which includes soft palate , tonge and lips. 4 -Salivary secretion has a role in digestion of starch � (up to 70% in mouth and stomach)by salivary amylase but it is composed by pancreatic amylase. 5 -It dissolves some food materials to facilitate its � stimulating effect on taste buds. 6 -It has a role in water balance because dryness of � the buccal and pharyngeal mucosa initiate the sensation of thirst.
SALIVARY SECRETION 7 -Saliva has a buffering action via its contents of � bicarbonates, phosphates, and mucin, to protect the buccal cavity from excessive acids or alkalis. Excessive alkalis lead to precipitation of calcium salts around the teeth which forms with organic matter hard concretion called tarter , bacteria flourish underneath the tarter leading to chronic inflammation of the gums , while excessive acids dissolves enamel and dentine of teeth after prolonged exposure. 8 -Protection against any irritating substances and � neutralization of the excessive cold or hot food.
SALIVARY SECRETION 9 -Excretion of iodides and mercury which may � produce inflammation of buccal mucosa (stomatitis)also in lead poisoning a blue line formed at margins of teeth and gums. Urea is excreted in saliva in renal diseases and some little glucose may be also excreted in diabetes mellitus. This excretory process is not very effective because these materials are swallowed again.
SALIVARY SECRETION CONTROL OF SALIVARY SEC SALIVARY � SECRETION Naturally salivary secretion is evoked by reflex action � i. e. nervous mechanism. Hormonal regulation would be very slow to meet with such a function which needs a rapid response as swallowing. There are two types of reflexes:

SALIVARY SECRETION a)The inborn or unconditioned � b)Acquired or conditioned. � a)Unconditioned reflexes: (Inborn do not depend on � training) If food , acids, alkalis are introduced into the buccal cavity, they stimulate the buccal mucosa either mechanically or chemically leading to profuse salivation. Also any irritation of buccal cavity by moving the tongue inside the mouth or during speech cause salivary secretion.
SALIVARY SECRETION RECEPTORS : Four types of receptors for taste � sensation exist in the tongue namely salt acid , sweet , and bitter receptors. AFFERENT: Impulses for taste sensation from the � anterior two thirds of the tongue are conducted by the chorda tympani branch of the facial nerve. From the posterior third of the tongue and pharynx impulses for taste sensations are carried by the glossopharyngeal nerve while the vagus nerve is responsible for bitter sensation from epiglottis and larynx.
SALIVARY SECRETION Impulses from mechanical stimuli and common � sensations (touch, pain, warm and cold) are conducted by lingual nerve, palatine branch of the trigeminal nerve and pharyngeal branch of the vagus nerve. CENTERE: These afferent nerves reach salivary � centers in medulla oblongata. EFFERENT: The efferent nerves are long the � autonomic nerves supplying the salivary glands.
SALIVARY SECRETION Reflex salivation may occur after irritation of gastric � or esophageal mucosa. The volume and constituents of saliva differ according to the nature of the stimulus.
SALIVARY SECRETION b)Conditioned reflexes: � Stimulation of any sensory nerve endings in the � body in absence of food from the buccal cavity as (optic , auditory , and olfactory nerves) can be converted by training into conditioned stimuli for salivation , as a proof, Pavlov experiment. He used to ring a bell befor giving the food to a dog , the process was repeated several times for training. Ringing the bell without any food intake some other time, develop the ability to bring about salivary secretion.
SALIVARY SECRETION In this case the dog considers the sound as an index � of food. Hearing of the bell is associated in the cerebral cortex with food intake. The center for the conditioned reflexes lie in the cerebral cortex , from it impulses travels to the salivary centers in the medulla oblongata , then the efferent pathway is along the autonomic nerves supplying the salivary glands.
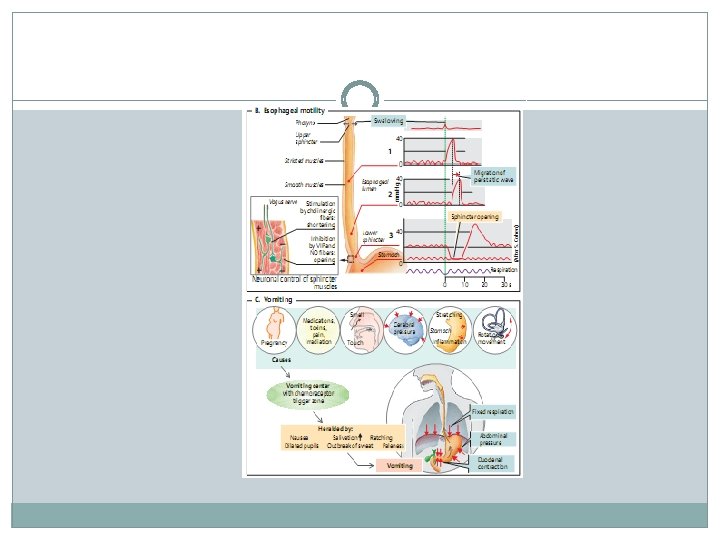
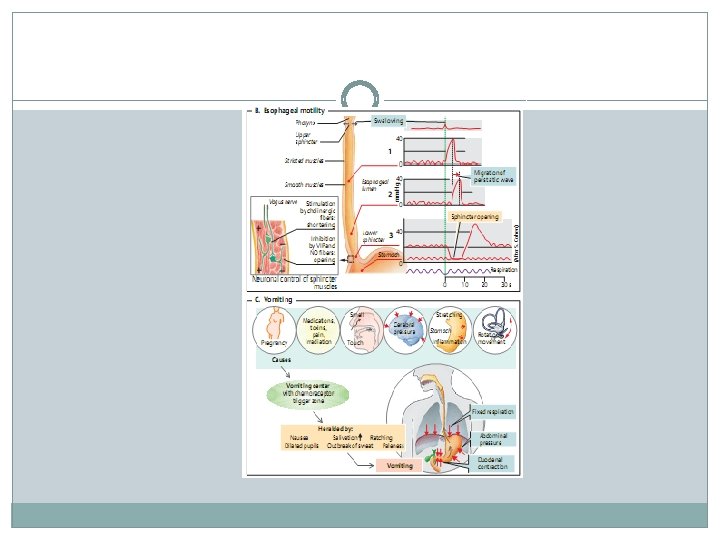
DEGLUTITION (SWALLOWING) Deglutition is the transfer of food from the mouth to � stomach, various groups of muscles striated and plain take part in this highly coordinated action. The start of Deglutition is voluntary, but it is completed by reflex actions. The deglutition center is present in the medulla oblongata. The speed of swallowing depends on the consistency of food. Fluids reach the stomach very rapidly (in about 6 second).
DEGLUTITION (SWALLOWING) They transverse esophagus faster than the � esophageal peristaltic waves , this is due to gravity in erect posture, but they remain above cardiac sphincter until a peristaltic wave opens this sphincter whereby the fluid enters the stomach. Semisolids take a longer time than fluids and solid materials are slower than semisolids.
DEGLUTITION (SWALLOWING) Phases of deglutition: (is divided into 3 � phases, without an interval in between) The first phases: � This phase is voluntary during which passage of � the bolus of food through the anterior pillars of the fauces take place. The bolus of food is placed on the dorsum of the tongue, then the tongue is suddenly elevated by contraction of mylohyoid muscles, and its root is pulled backwards forcing the bolus into the pharynx and press strongly against the hard palate.


DEGLUTITION (SWALLOWING) The second phase: � It is involuntary reflex and starts by the passage � of food through the pharynx , it is very rapid phase which takes about 1 -2 seconds. During this phase, contraction of the constrictor muscles of the pharynx occurs accompanied by receptive relaxation of the upper esophageal sphincter. This phase passes by the following sequence of events: 1 -The posterior pillars of the fauces approximate to � shut off the mouth cavity from the pharynx and prevent the back passage of food to it.
DEGLUTITION (SWALLOWING) 2 -Protective reflexes take place to prevent the � passage of food into the respiratory openings: a)Elevation of the soft palate in contact with the � posterior pharyngeal wall to shut off the posterior nares and prevent the passage of food into the nasal cavity.

DEGLUTITION b)Elevation of the larynx and closure of its opening � (glottis) by the epiglottis and posterior part of the tongue and approximation of the vocal cords to into the air ways. guard against the passage of food c)Inhibition of respiration by a reflex mechanism i. e �. reflex apnea

DEGLUTITION (SWALLOWING) The third phase: � During it, passage of food along the esophagus to the � stomach occurs, it is voluntary , the movements in the upper third of the esophagus are rapid while in the lower third are slow, because the muscles of the upper third are striated and supplied by the vagus while in its lower third are plain and depend on local plexus of Auerbach. The middle third contains both types of muscles.
DEGLUTITION (SWALLOWING) Nervous pathways in deglutition � The reflexes of the involuntary phases are mediated � by: 1 -Afferent: start from receptors that discharge impulses � from the upper pharynx along the 5, 9, 10 th cranial nerves. 2 -Center: is the deglutition center in the medulla � oblongata. 3 -Efferents along: � a)5 th cranial nerve to mylohyoid muscles. � b)9 th, 10 th, 11 th (accessory)cranial nerves to the pharyngeal � and esophageal myscles. c)12 th (hypoglossal) cranial nerve to the tongue muscles. �
DEGLUTITION (SWALLOWING) Esophageal secretion: � The esophageal secretion are mucoid in nature to � facilitate swallowing. The presence of mucus in the upper part of the esophagus prevents the excoriation of the mucosa by the food , and its presence in the lower part(esophago-gastric junction) protects the esophageal wall from digestion by gastric reflux into the esophagus. Cardiac sphincter: � It is present at the opening of the esophagus into the � stomach , it is a functional and not a true anatomical sphincter
GASTRIC SECRETION The stomach is the most dilated part of the � alimentary canal. The stomach wall has a good tone , which is inhibited reflexly by food intake to accommodate it. Both afferent and efferent fibers for such inhibitory reflex are via the vagus nerve. The functions of the stomach are: � 1 -Digestive functions. � 2 -Storage of large quantities of food until they can be � accommodated in the lower portion of the GIT.

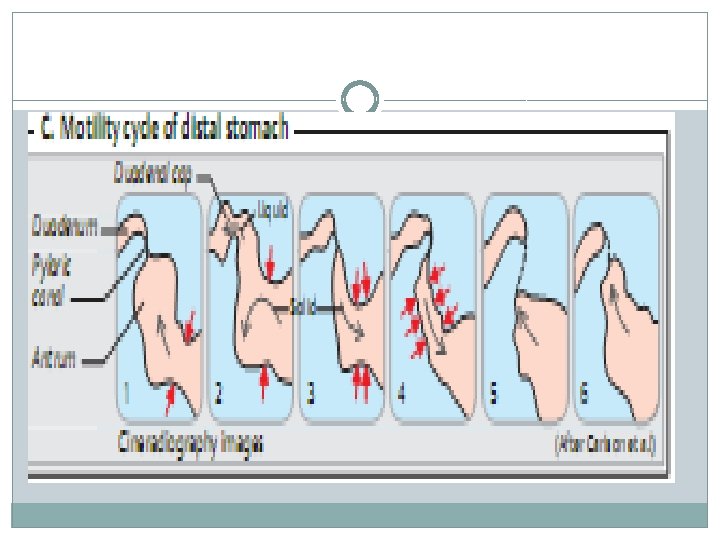
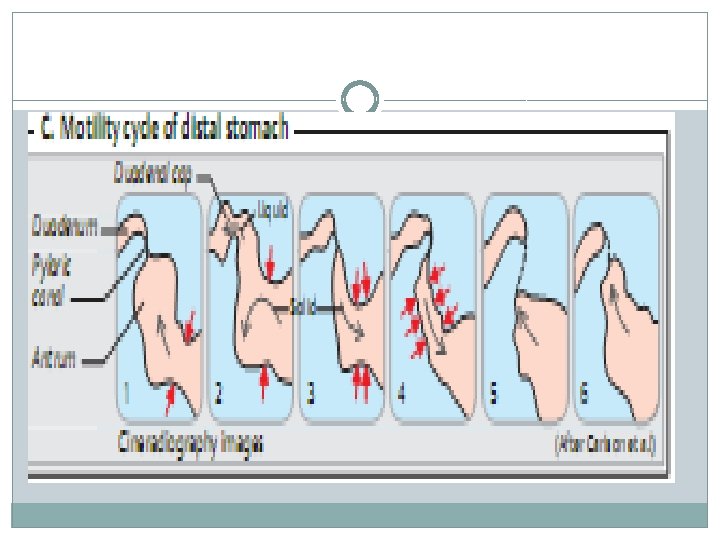
GASTRIC SECRETION 3 -Mixing of food with gastric secretions. � 4 -The acidic gastric juice facilitates the absorption of � various substances from the upper intestine such as calcium and iron. 5 - Regulation of the rate of evacuation of chime into � the duodenum via the pyloric pump , to prevent rapid passage of food into the small intestine to give more time for digestion and absorption. 6 -Release intrinsic factor for vit. B 12 absorption. � 7 -Secretion of mucin. �

GASTRIC SECRETION Anatomical &histological considerations � The stomach can be divided into 2 major parts, � the body and the antrum. The fundus located at the upper end of the body of the stomach is actually a functional part of the body. Mucous secreting cells line the entire surface of � the stomach, the gastric mucosa contains many deep glands in the pyloric and cardiac regions, the glands secrete mucus for protection of the mucosa.
GASTRIC SECRETION In the fundus and body of the stomach the gastric � glands are composed of four different types of cells: 1 -The mucous neck cells, which secrete mucin. � 2 -The chief cells, which secrete the digestive enzyme � pepsin. 3 -The parietal cell, which secrete hydrochloric acid. � 4 -Argentaffine cells, which are rich in serotonin. � Many of the glands open on a common chamber � (gastric pit) that opens in turn on the surface of the mucosa.
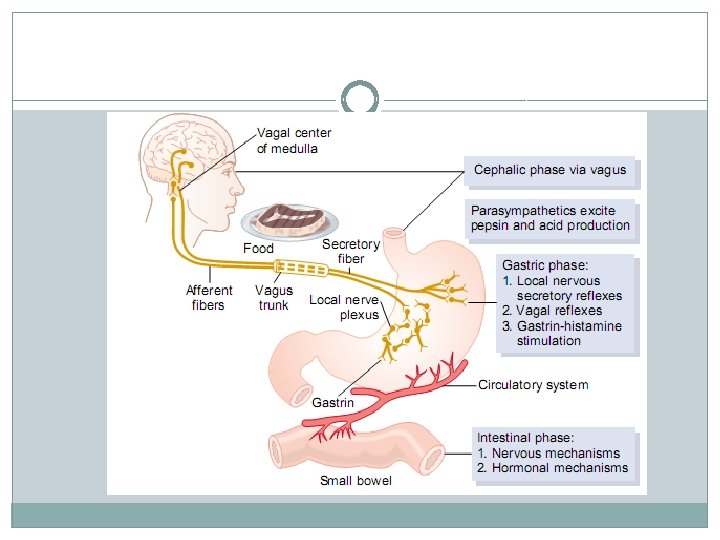
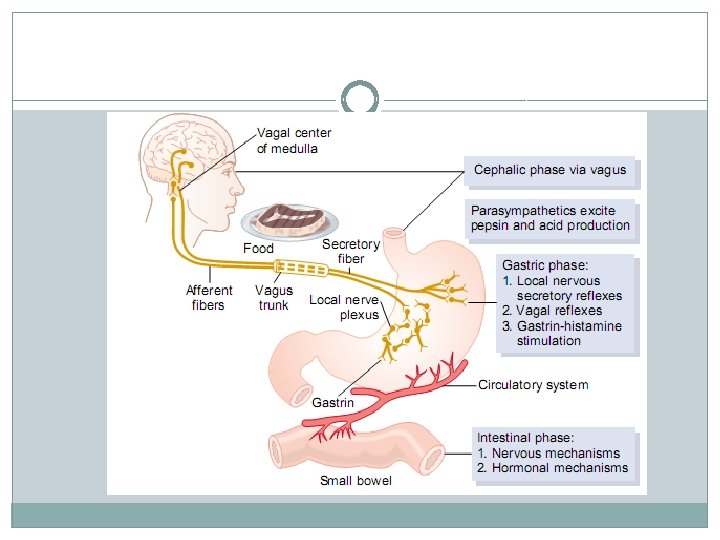
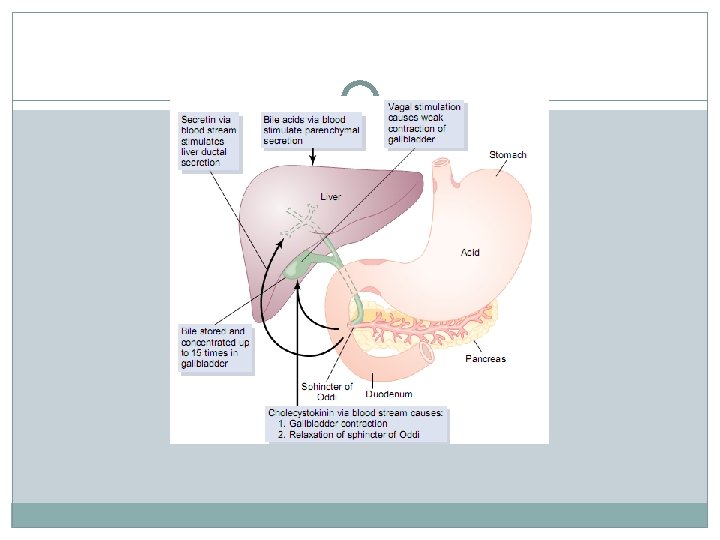
1 -Parasympathetic supply The vagi supply preganglionic fibers which relay at the � ganglia of the local nerve plexuses (Auerbach's and Meissner's) in the gastric wall. The vagi seve the following functions: a-Secretory to the gastric glands. � b-Motor to the muscles of the wall, but inhibitory to both � cardiac and pyloric sphincters. It increases the rate of emptying of the stomach. c-Some vasodilator fibers probably are present in the vagi. � d-Some reflexes are also initiated from the stomach via � the vagi as gastric-ileal or the gastrocolic reflexes.
2 -Sympathetic supply: It is a branch of the greater splanchnic , this preganglionic � fibers relay in the celiac ganglia. The post ganglionic fibers pass to the stomach along its arterial blood supply and have the following effects: a-Inhibitory to the muscles of the wall and motor cardiac � and pyloric sphincters, it delays the rate of evacuation of the stomach. b-Reduction of the blood flow due to vasoconstriction, � and also some vasodilator fibers may present. c-Sympathetic stimulation may produce alkaline mucous � secretion from the pyloric glands.
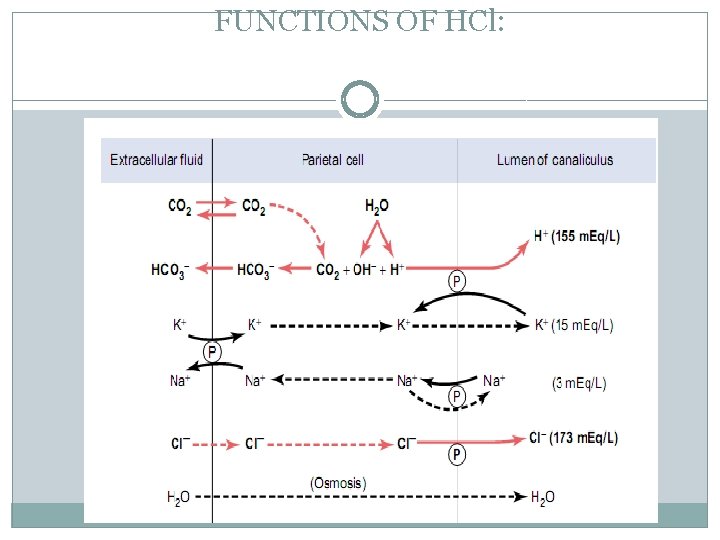
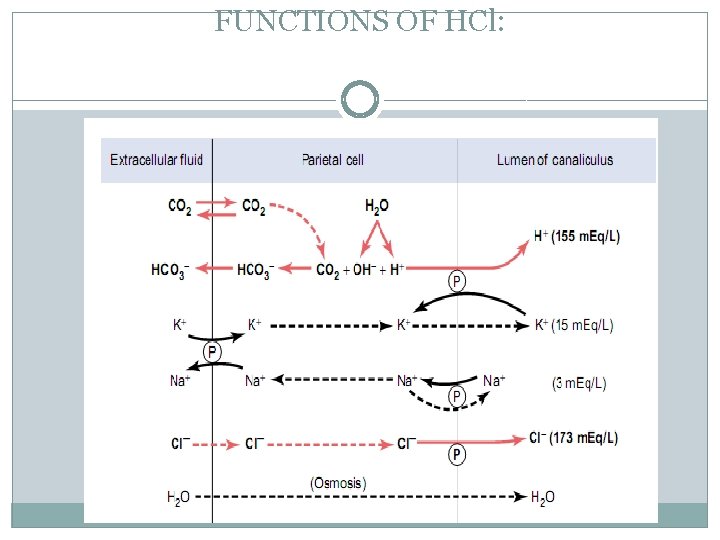
Compositions of gastric secretion: 1 -Hydrochloric acid(HCl) � It is secreted by the parietal cells of the gastric � glands, these cells contain small channels, which communicate with the lumens of the gastric glands. HCl is formed at intracellular membrane by ionic exchange, and is passed directly into the canaliculi, the most probable mechanism of its secretion is as follows:
HCl 1 -The parietal cells exert an electrochemical work to � dissociated molecule of water into H+ and OH-. Active transport of H+ across the membrane of the parietal cells to the gastric lumen occurs, the energy for this active transport is derived from aerobic glycolysis, since acid secretion ceases under anaerobic conditions. Two molecules of H+ are secreted for each molecule of O 2 consumed.

HCl 2 -The parietal cells take CO 2 from the blood and � reacts with H 2 O to form H 2 CO 3. This reaction is catalyzed by carbonic anhydrase enzyme. Dissociation of H 2 CO 3 into H+ &HCO 3 occurs , H+ combines with OH- produced in the first step forming H 2 O. CO 2 +H 2 O ↔ H 2 CO 3 ↔ H+ + HCO 3 - � Secretion of HCl is directly proportional to the CO 2 � tension of blood, in overventillation HCl formation is depressed. Diamox, a carbonic anhydrase inhibitor depresses gastric secretion of HCl.
HCl 3 -The HCO 3 - ions pass from the parietal cells to the � blood in exchange with Cl- , that enter the cell and later will be secreted into the canaliculus. Cl- ions are secreted by the parietal cells at the luminal side of the gastric mucosa by active process against a relatively high concentration gradient and coupled with H+ ion produced in the first reaction. The blood coming from the stomach is alkaline , and has a high HCO 3 - content, when gastric acid secretion is elevated after a meal, the p. H of the systemic blood rises and alkaline urine is excreted. This is the probable explanation of the high p. H of the urine excreted after a meal, the so called postprandial alkaline tide
FUNCTIONS OF HCl:


 The digestive system consists of
The digestive system consists of Digestive respiratory and circulatory system
Digestive respiratory and circulatory system Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Lp html
Lp html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Chụp tư thế worms-breton
Chụp tư thế worms-breton Hát lên người ơi alleluia
Hát lên người ơi alleluia Các môn thể thao bắt đầu bằng tiếng bóng
Các môn thể thao bắt đầu bằng tiếng bóng Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ V. c c
V. c c Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Fecboak
Fecboak Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Số.nguyên tố
Số.nguyên tố Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Hổ đẻ mỗi lứa mấy con
Hổ đẻ mỗi lứa mấy con Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi 2 pipe system drainage
2 pipe system drainage Autonomic nervous system consists of
Autonomic nervous system consists of What is marketing mis
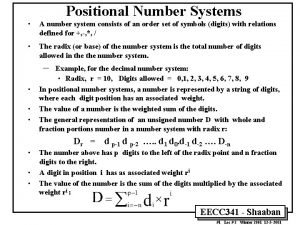
What is marketing mis Define number system
Define number system Reservoir system
Reservoir system The lymphatic system consists of
The lymphatic system consists of A transportation system consists of
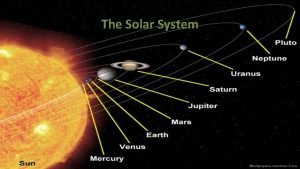
A transportation system consists of The solar system consists of the
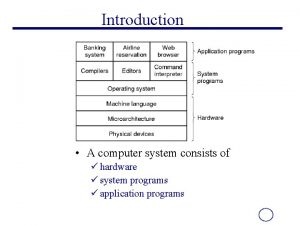
The solar system consists of the A computer system consists of
A computer system consists of The endocrine system consists of
The endocrine system consists of Four major data processing functions of a computer
Four major data processing functions of a computer Mass produced copyrighted retail software
Mass produced copyrighted retail software Roman goddess of love and beauty
Roman goddess of love and beauty The lymphatic system consists of
The lymphatic system consists of Peripheral nervous system consists of
Peripheral nervous system consists of Peripheral nervous system consists of
Peripheral nervous system consists of Saturn is a
Saturn is a Define number system
Define number system Misمعنی
Misمعنی Introduction to mis
Introduction to mis Chapter 25 the urinary system
Chapter 25 the urinary system Nervous system and digestive system
Nervous system and digestive system What is work energy theorem
What is work energy theorem Sliding into a slit sandwhich
Sliding into a slit sandwhich Network consists of
Network consists of Great britain consists of three parts
Great britain consists of three parts Euphenics
Euphenics Smear layer in operative dentistry
Smear layer in operative dentistry A slingshot consists of a light leather cup
A slingshot consists of a light leather cup Statistic vs parameter example
Statistic vs parameter example Sub processes of project management
Sub processes of project management In the game of roulette a wheel consists of 38
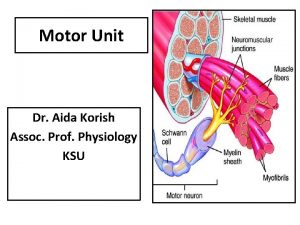
In the game of roulette a wheel consists of 38 Motor unit consists of
Motor unit consists of Main actors and forces in a modern marketing system
Main actors and forces in a modern marketing system Long term manpower planning
Long term manpower planning Cpu consists of
Cpu consists of Defination of lever
Defination of lever