ENDOCRINE SYSTEM Introduction The endocrine system consists of




- Slides: 78
ENDOCRINE SYSTEM
Introduction • The endocrine system consists of glands and tissues collectively called Endocrine Glands that secrete substances called hormones into the internal environment. • Endocrine glands are ductless; the hormones are secreted directly into the bloodstream for distribution throughout the body.
• A HORMONE is a regulatory molecule that affects the activity of other glands or tissues. Hormones influence the metabolism of cells, the growth and development of body parts and homeostasis. • Most hormones are either steroids or steroid-like substances synthesized from cholesterol, amines, peptides, proteins or glycoproteins synthesized from amino acids. They can stimulate changes in the target cells even in extremely low concentrations.
GENERAL FUNCTIONS OF THE ENDOCRINE SYSTEM Regulating the functions of the human body to maintain homeostasis (equilibrium) is an enormous job. Two organ systems function coordinately to enable body parts to communicate with each other to adjust constantly to changing incoming signals. These are the nervous system and the endocrine system.
• Endocrine glands and their hormones help regulate metabolic processes. They control the rate of certain chemical reactions and in the transportation of substances across membranes and help regulate water and electrolyte balance. • They also play a vital role in reproduction, development and growth
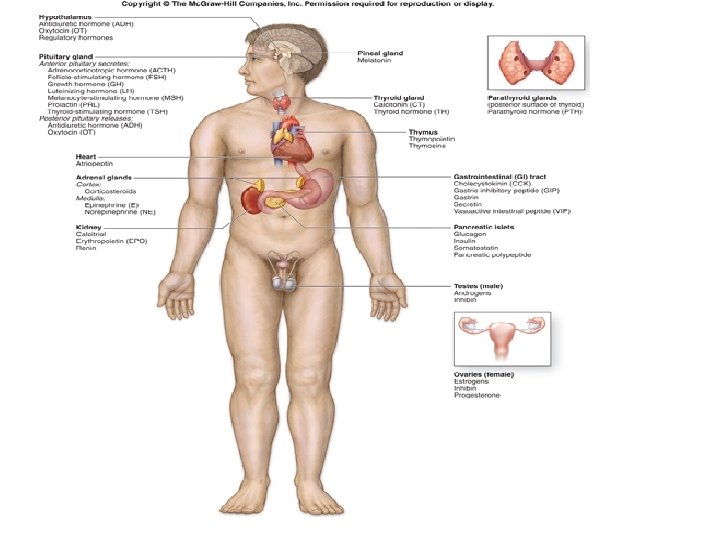
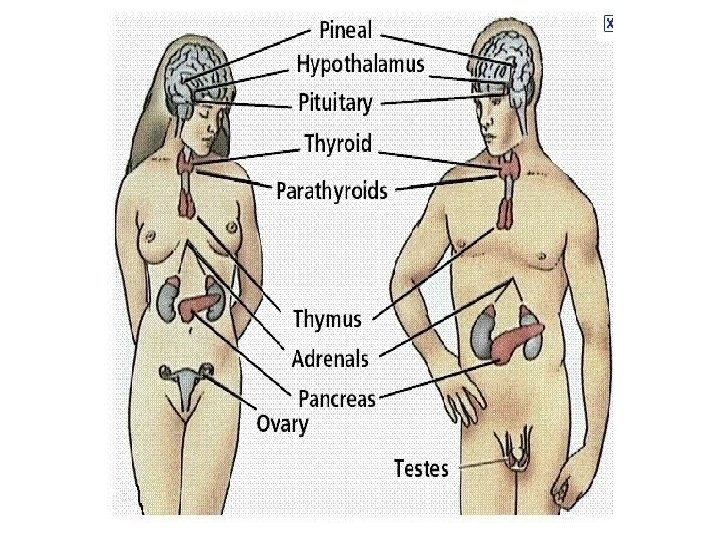
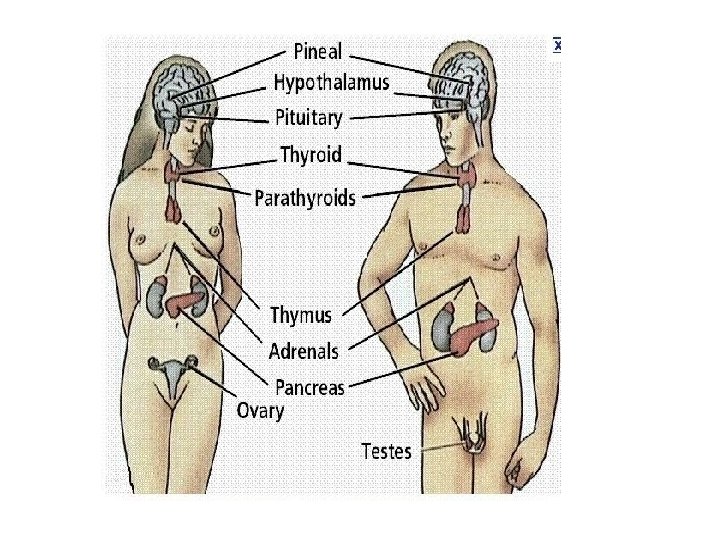
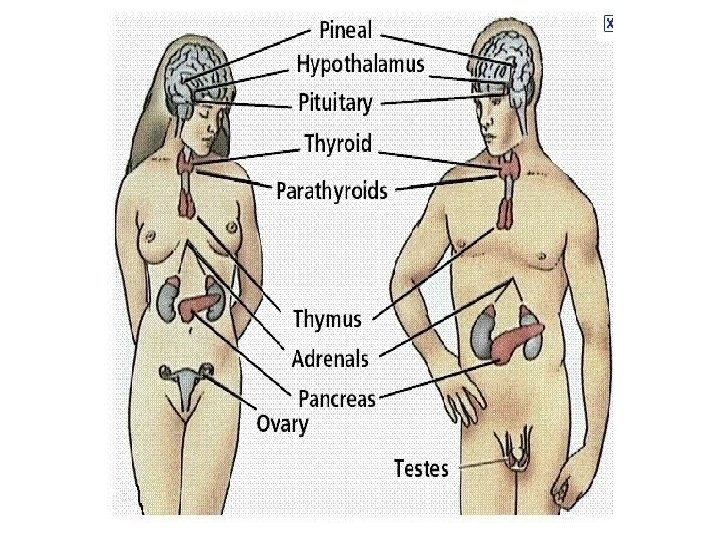
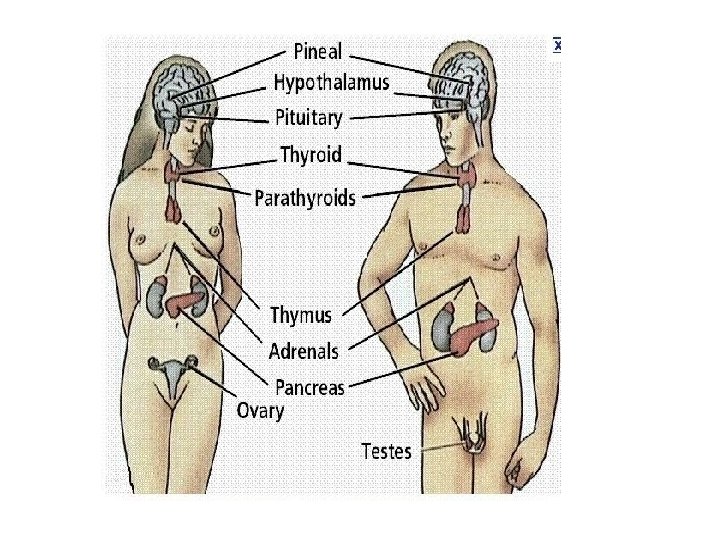
ENDOCRINE GLANDS Specialized small group of cells produce some hormones. However, the major endocrine glands are: 1. Pituitary gland 2. Thyroid gland 3. Parathyroid glands 4. Adrenal glands 5. Pancreas (Islets of langerhans) 6. Pineal gland 7. Thymus gland 8. Reproductive glands (testes and ovaries)
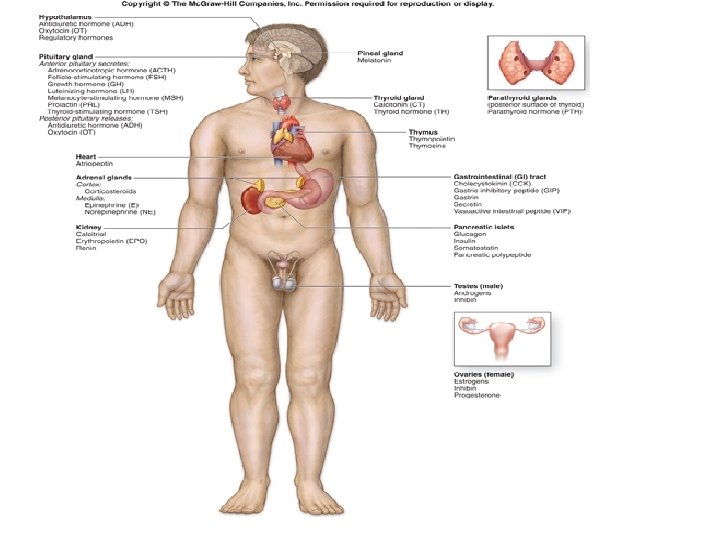
Although the hypothalamus is classified as a part of the brain and not as a direct endocrine gland it has a direct controlling effect on the pituitary and indirect effect on many other organs.
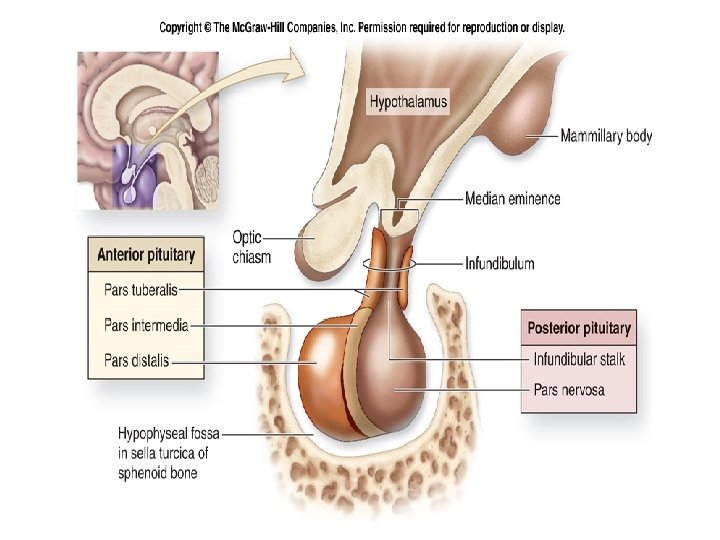
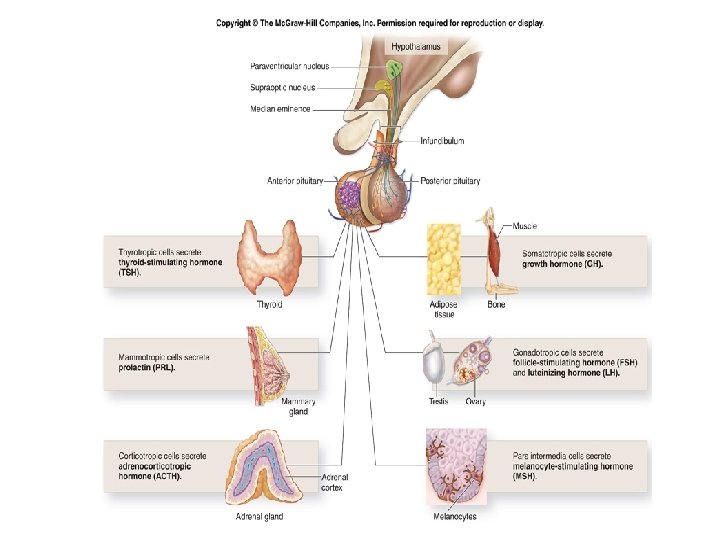
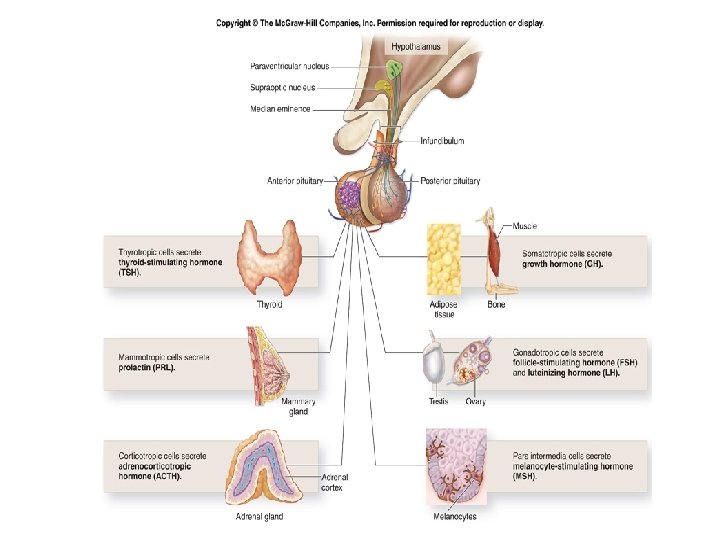
HYPOTHALAMUS AND PITUITARY GLAND • The hypothalamus and the pituitary glands act as a unit, regulating the activity of most of the other endocrine glands. • The pituitary gland (hypophysis) is located on the inferior (base) aspect of the brain where it is attached to the hypothalamus by a stalk- like structure called Infundibulum.

• Roughly the size of a pea and about 1 cm in diameter, the pituitary gland is known as the “master gland”. It weighs about 4 g. The gland lies in the hypophyseal fossa of the sphenoid bone. • The pituitary gland is structurally and functionally divided into ü anterior lobe (adenohypophysis) ü posterior lobe (neurohypophysis). • These two parts have different embryonic origin.
• The adenohypophysis is derived from a pouch of epithelial tissue that migrates upward from the embryonic mouth (pharynx) where as the neurohypophysis is formed as a down growth of nervous tissue of the brain.
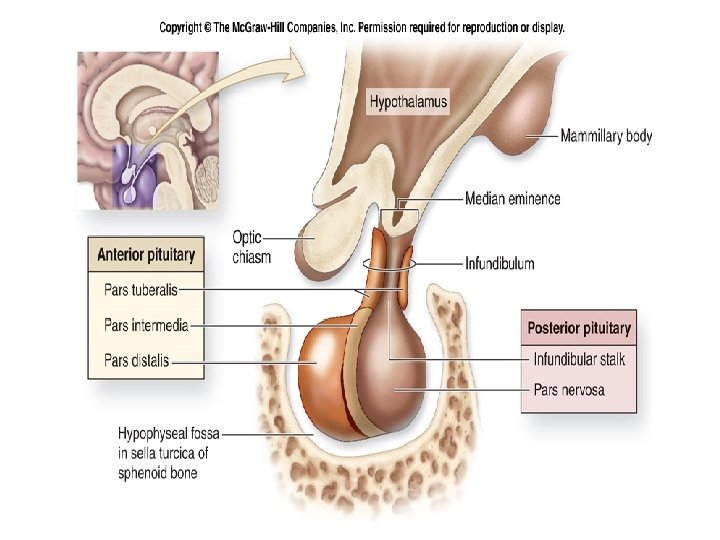
• In the fetus, a narrow region develops between the anterior and posterior lobes of the gland called the intermediate lobe (pars intermediate) which produces melanocyte – stimulating hormone (MSH), which regulates the synthesis of melanin – the pigment in the skin and in portions of the eyes and brain. • The intermediate lobe atrophies during prenatal development and in adults they no longer constitute a separate lobe or structure.
• The posterior pituitary stores and releases hormones that are actually produced by the hypothalamus, whereas the anterior pituitary produces and secretes its own hormones. • The anterior pituitary however, is regulated by hormones secreted by the hypothalamus, as well as feedback from the target gland hormones.
Blood supply • Arterial blood is supplied by branches from the internal carotid artery. The anterior lobe is supplied indirectly by blood that has already passed through a capillary bed in the hypothalamus. • This network of blood vessel, the pituitary portal system, conveys blood from the hypothalamus to the anterior lobe. • As well as conveying oxygen and nutrients, this blood conveys the releasing and inhibiting hormones secreted by the hypothalamus that influence the secretion and release of hormones formed in the anterior lobe.
• The posterior lobe is supplied directly by a branch from the carotid artery. • Venous blood from both lobes, containing hormones leaves the gland in short veins that enter the venous sinuses between the dura mater of the brain.
The anterior lobe (adenohypophysis) • The AP is enclosed in a capsule of dense, collagenous connective tissue and consists largely of epithelial tissue organized in blocks around many thin walled blood vessels. • So far, five types of secretary cells within the epithelium have been identified. Four of these each secrete a different hormone. ü Growth hormone (GH) ü prolactin (PRC) ü thyroid stimulating hormone (TSH) ü adrenocorticotropic hormone (ACTH). ü The 5 th type of cell secretes follicle –stimulating hormone (FSH) and luteinizing hormone (LH). • The hypothalamus controls the AP by producing hypothalamic - releasing hormones and hypothalamic-inhibiting hormones.
• GROWTH HORMONE stimulates cells to increase in size and divide more frequently especially muscles and skeleton. It also enhances the movement of amino acids across the cell membrane and speeds the rate at which cells utilize carbohydrates and fats. • The hormone’s effect on amino acids is important in stimulating growth. Two (2) hormones from the hypothalamus control GH secretion. GH releasing hormone and GH releasing inhibiting hormone (somatostatin). • Somatostatin inhibits secretion of GH, TSH, ACTH, glucagon, insulin, etc. More GH is released during sleep, hypoglycaemia, exercise and anxiety.
• PROLACTIN stimulates and sustains a woman’s milk production following the birth of an infant. Blood level of prolactin is not dependent on a hypothalamic releasing factor but it is lowered by the inhibiting factor dopamine and by an increased blood level of prolactin. • Suckling stimulates prolactin secretion and the resultant high blood level is a factor in reducing the incidence of conception during lactation.
• THYROID STIMULATING HORMONE (TSH) controls thyroid gland secretions (T 3 & T 4). The hypothalamus partially regulates TSH secretion by producing TRH. Circulating TH inhibit release of TRH and TSH. • As the blood concentration of TH increases, secretion of TRH and TSH deceases. It is highest between 9 pm and 6 am. Lowest level is between 7 am and 4 pm (circadian rhythmical release).
ADRENOCORTICOTROPIC HORMONE (ACTH) stimulates the adrenal cortex to secrete the glucocorticoids such as hydrocortisone (cortisol). ACTH secretion is regulated in part by corticotropin-releasing hormone (CRH) from the hypothalamus. CRH production is believed to be influenced by • negative feedback mechanism resulted from increased blood ACTH and cortisol • hypoglyceamia • emotional stress • a low blood level of cortisol • exercise or physical stress
GONADOTROPIN HORMONES- FSH and LH are the gonadotropins meaning they exert their actions on the gonads or reproductive organs. Gonads are the testes in males and the ovaries in females. In females, the FSH stimulates the development and ripening of the ovarian follicle. • During it’s development the ovarian follicle secretes its own hormone, oestrogen. As the level of estrogen increases in the blood FSH secretion is reduced.
• The LH promotes the final maturation of the ovarian follicle and ovulation. It promotes the formation of the corpus luteum which secretes the second ovarian hormone progesterone. • As the level of progesterone increases there is a gradual reduction in the production of the LH.
• In males, the FSH stimulates the epithelial tissue of the seminiferous tubules in the testes to produce spermatozoa. The LH also called interstitial cell stimulating hormone (ICSH) in males stimulates the interstitial cells in the testes to secrete the hormone, testosterone. • The gonadotropic hormones are released in response to LHRH also known as Gn. RH from the hypothalamus.
NEUROHYPOPHYSIS (POSTERIOR PITUITARY) • The PP consists mostly of nerve fibers and neuroglial cells. The gland is composed of secretory cells called pituicytes. The neuroglial cells support the nerve fibers which originate in the hypothalamus. • Specialized neurones in the hypothalamus produce the two hormones associated with the PP, ADH ( vasopressin) and Oxytocin.
These hormones travel down axons through the pituitary stalk to the posterior lobe, and vesicles near the ends of the axons store them. Nerve impulses from the hypothalamus release them into the blood.
ANTIDIURETIC HORMONE (ADH) • A diuretic is a chemical that increases urine production where as antidiuretic decreases urine production. ADH reduces diuretic effect by reducing the volume of water the kidneys excrete. In this way, ADH regulates the water concentration of body fluids. • The hypothalamus regulates ADH secretion. Certain neurons in this part of the brain called osmoreceptors sense changes in the osmotic pressure of body fluids. Dehydration due to lack of water intake increasingly concentrates blood solutes.
• Osmoreceptors, sensing the resulting increase in the osmotic pressure, signals the PP to release ADH which travels in the blood to the kidneys. • As a result, the kidneys produce less urine conserving water. On the other hand, drinking too much water dilutes body fluids, inhibiting ADH release.
• The kidneys excrete more dilute urine until the water concentration of body fluids return to normal. (Diabetes insipidus: injury or tumour damages the ADH regulatory mechanism. Too little or no ADH is released. Much as 25 -30 L of urine is excreted per day). • Pressor effect: vasoconstriction resulting in increased blood pressure
OXYTOCIN (OT) • Oxytocin contracts smooth muscles in the uterine wall and stimulates uterine contractions in the later stages of childbirth. Stretching of uterine and vaginal tissues late in pregnancy triggers OT release during childbirth. • In the breast, OT contracts certain cells (myoepithelial cells) associated with milk producing glands and their ducts. This action forces milk from the milk glands into the milk ducts and ejects the milk from the breast for breastfeeding. • (Commercial preps of OT are used in labour to stimulate uterine contraction and also after labour to arrest haemorrhage.
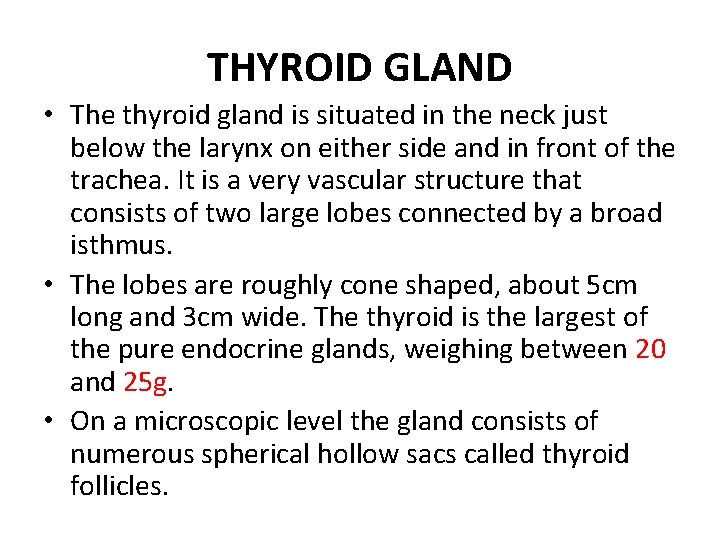
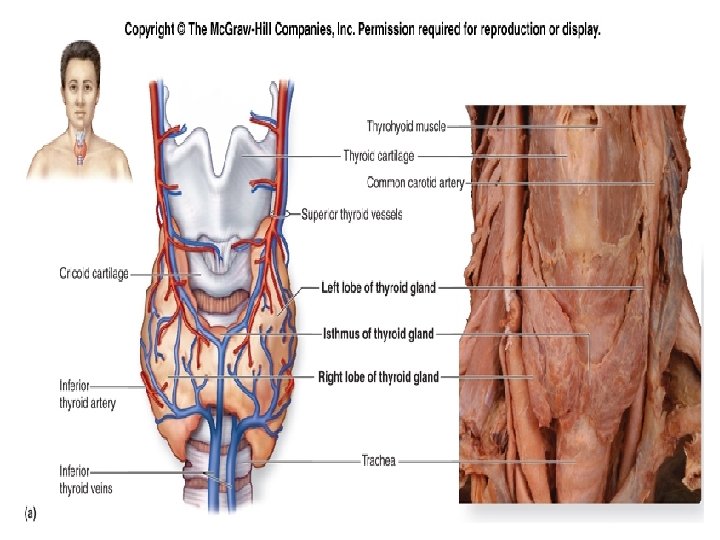
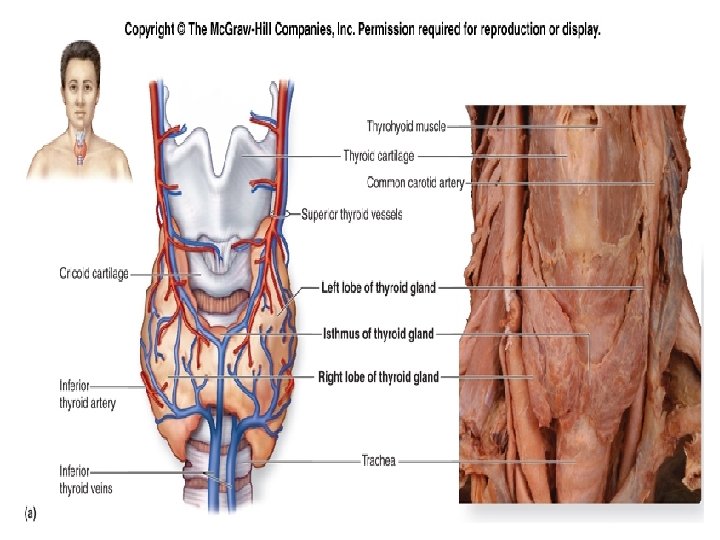
THYROID GLAND • The thyroid gland is situated in the neck just below the larynx on either side and in front of the trachea. It is a very vascular structure that consists of two large lobes connected by a broad isthmus. • The lobes are roughly cone shaped, about 5 cm long and 3 cm wide. The thyroid is the largest of the pure endocrine glands, weighing between 20 and 25 g. • On a microscopic level the gland consists of numerous spherical hollow sacs called thyroid follicles.
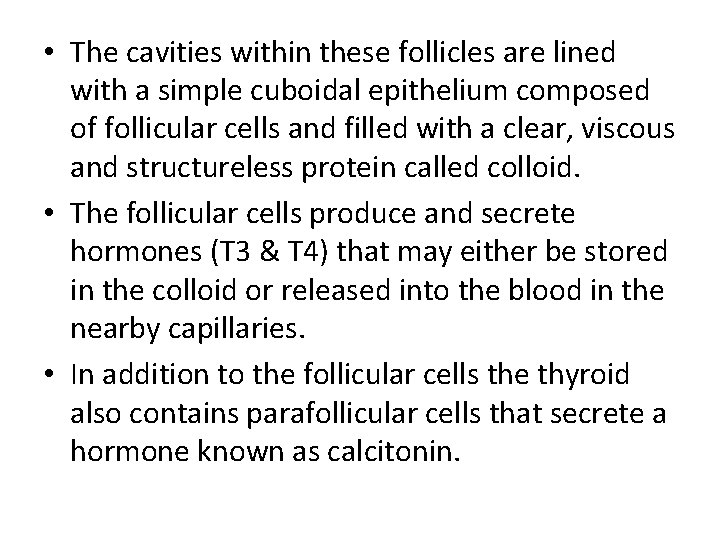
• The cavities within these follicles are lined with a simple cuboidal epithelium composed of follicular cells and filled with a clear, viscous and structureless protein called colloid. • The follicular cells produce and secrete hormones (T 3 & T 4) that may either be stored in the colloid or released into the blood in the nearby capillaries. • In addition to the follicular cells the thyroid also contains parafollicular cells that secrete a hormone known as calcitonin.
BLOOD SUPPLY • Arterial blood supply to the gland is through the superior and inferior thyroid arteries. The superior thyroid artery is a branch of the external carotid artery and the inferior thyroid artery is a branch of the subclavian artery. • The venous return is by the thyroid veins which drain into the internal jugular vein.
THYROID HORMONES • The follicular cells of the thyroid gland synthesizes two hormones- tetraiodothyronine or T 4 and triiodothyronine or T 3. • These two hormones have similar actions, although T 3 is five times more potent. These hormones help regulate the metabolism of carbohydrates, lipids and proteins. They increase the rate at which cells release energy from carbohydrates. • They also increase the rate of protein synthesis and stimulate the breakdown and mobilization of lipids.
• They are the major factors determining how many calories the body must consume at rest in order to maintain life, the basal metabolic rate(BMR). Thyroid hormones are required for normal growth and development and are essential to nervous system maturation. • Follicular cells require iodine salts(IODIDES) to produce thyroxine and triiodothyronine. Foods normally provide iodides and after it has been absorbed from the intestines, blood transports it to the thyroid gland. • An efficient transport system moves the iodides into the follicular cells where they are used to synthesize the hormones.
• After secretion the hormones combine with colloid and are stored in the follicles as thyroglobulin. Their release into the blood is regulated by TSH which is stimulated by TRH from the hypothalamus. • Calcitonin , secreted by the parafollicular cells of the thyroid gland regulates the blood calcium level and phosphates ions. It lowers blood calcium and phosphate ions concentrations by inhibiting the release of calcium and phosphate ions from bones and by increasing excretion of these ions by the kidneys.
PARATHYROID GLANDS • The parathyroid glands are on the posterior surface of the thyroid gland. There are usually 4 parathyroid glands; a superior pair and an inferior pair, although the precise number can vary. • A thin capsule of connective tissue covers each small, yellowish- brown parathyroid gland. • The body of the gland consists of many tightly packed secretory cells closely associated with capillary networks.

• Parathyroid hormone (Parathormone) is the only hormone secreted by the parathyroid glands. PTH promotes a rise in the blood calcium levels by acting on the bones, intestines and kidneys. • It inhibits the activity of osteoblasts and stimulates osteoclast to resorb bone and release calcium and phosphate ions into the blood. At the same time, PTH causes the kidneys to conserve blood calcium
• Calcitonin and PTH activities maintain stable blood calcium concentration. Calcitonin decreases an above normal blood calcium concentration while PTH increases a below normal blood calcium concentration. • Calcium is essential for muscle contraction, blood clotting and nerve impulse transmission.
• It also stimulates calcium absorption from food in the intestine, further increasing blood calcium concentration. Negative feedback between the parathyroid glands and the blood calcium concentration regulates PTH secretion. • As the blood calcium concentration drops, more PTH is secreted and vice versa.
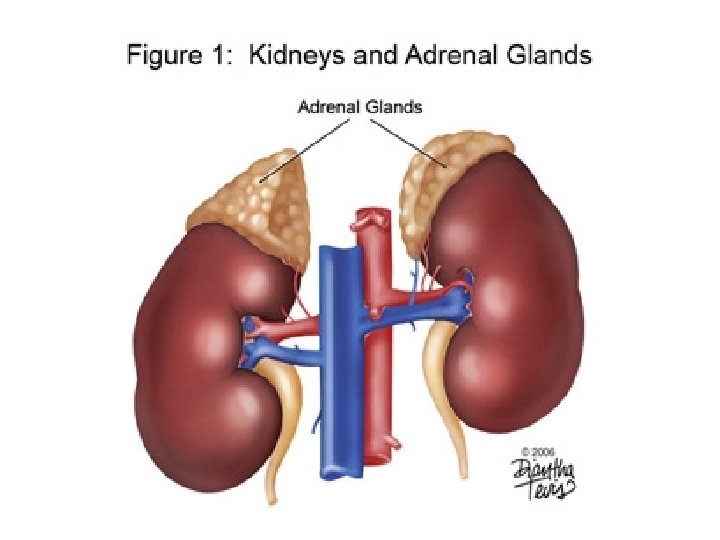
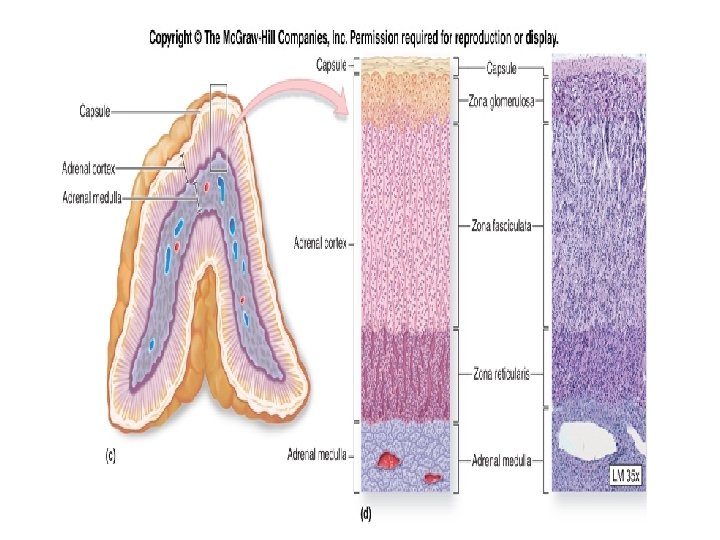
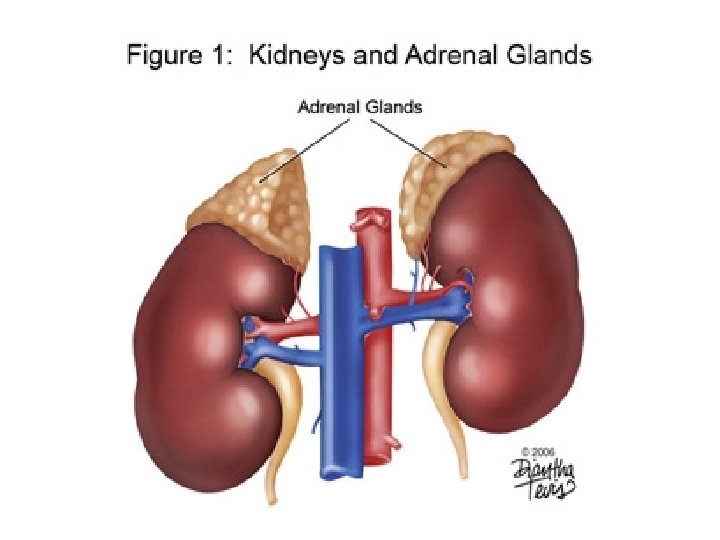
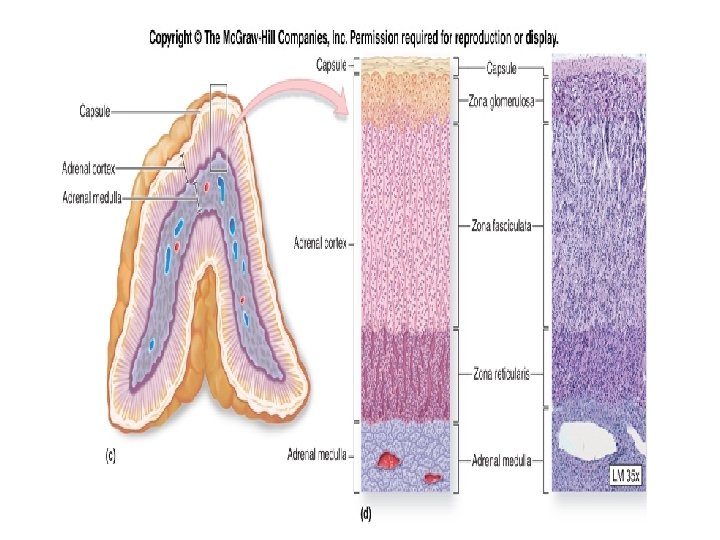
ADRENAL GLANDS • The adrenal glands are paired organs that cap the superior borders of the kidneys. • Each adrenal gland consists of an outer cortex and an inner medulla which differ both anatomically and physiologically.
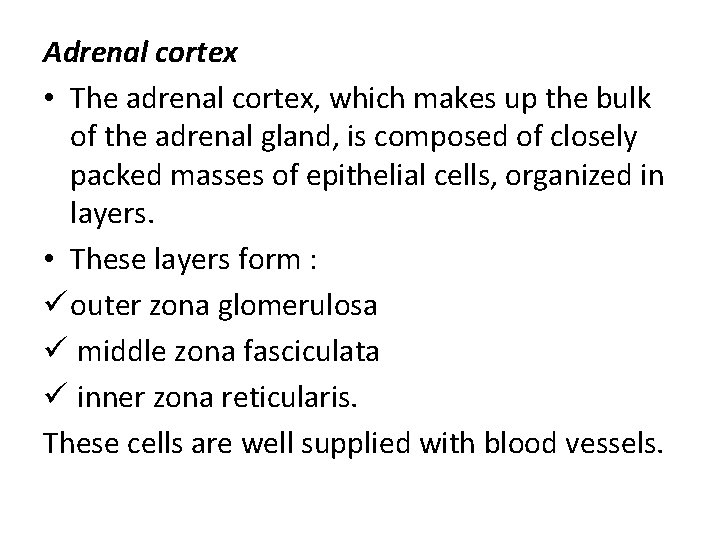
Adrenal cortex • The adrenal cortex, which makes up the bulk of the adrenal gland, is composed of closely packed masses of epithelial cells, organized in layers. • These layers form : ü outer zona glomerulosa ü middle zona fasciculata ü inner zona reticularis. These cells are well supplied with blood vessels.
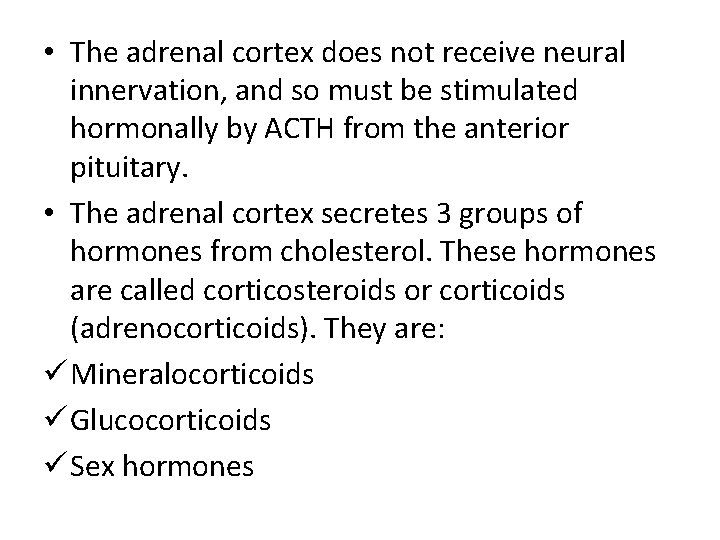
• The adrenal cortex does not receive neural innervation, and so must be stimulated hormonally by ACTH from the anterior pituitary. • The adrenal cortex secretes 3 groups of hormones from cholesterol. These hormones are called corticosteroids or corticoids (adrenocorticoids). They are: ü Mineralocorticoids ü Glucocorticoids ü Sex hormones

MINERALOCORTICOIDS • Aldosterone is the most important of the mineralocorticoids. • It is synthesized by the zona glomeulosa. Aldosterone targets the kidneys where it promotes renal absorption of sodium and renal excretion of potassium. • By conserving sodium ions, aldosterone stimulates water retention indirectly by osmosis, helping to maintain blood volume and blood pressure as well as regulate blood electrolytes.
• The secretion of mineralocorticoids is not controlled by the AP. When the blood sodium level and therefore the blood pressure are low, the kidneys secrete renin. • Renin is an enzyme that converts the plasma protein angiotensinogen produced by the liver to angiotensin 1, which is changed to angiotensin 2 by a converting enzyme found in lung capillaries. Angiotensin 2 stimulates the adrenal cortex to release aldosterone.
• The effect of this system known as the reninangiotensin-aldosterone system is to raise blood pressure in 2 ways. • Angiotensin 2 constricts the arterioles and aldosterone causes the kidneys to reabsorp sodium. • Raised sodium level in the blood leads to water retention in the blood increasing the blood volume.
GLUCOCORTICOIDS • Cortisol (hydrocortisone) and corticosterone are the main glucocorticoids. It is produced in the middle layer of the cortex, zona fasciculata. Cortisol raises blood glucose level by: 1. Promoting the metabolism of fatty acids rather than carbohydrates and this spares glucose. 2. Promoting the breakdown of muscle proteins to amino acids, which are taken up by the liver from the bloodstream.
• The liver then breaks down these excess amino acids to glucose which enters the blood. • Cortisol also counteracts the inflammatory response that leads to pain and swelling. Very high levels of glucocorticoids in the blood can suppress the body’s defense system. • By suppressing inflammation and immunity, they can also make a person highly susceptible to infection and injury. They also delay wound healing. • Secretion of cortisol is stimulated by ACTH and stress.
SEX HORMONE (ANDROGENS) • Cells in the inner zona reticularis produce sex hormones. These hormones are male types including dehydroepiandrosterone (DHEA) which are weak androgens. • Some of these weak androgens are converted to female hormones (oestrogen) in the skin, adipose tissue and liver. • Adrenal sex hormones may supplement sex steroids from the gonads and stimulate early development of reproductive organs.
ADRENAL MUDULLA • The medulla is completely surrounded by the cortex. It consists of irregularly shaped cells organized in groups around blood vessels. • These cells are intimately connected with sympathetic division of the autonomic nervous system. • The adrenal medulla secretes catecholamines which complement the sympathetic nervous system in the “fight or flight” reaction.
• The cells of the medulla secrete two closely related hormones epinephrine (adrenaline) and nor epinephrine (noradrnaline) in a ratio of 4: 1 respectively. • These hormones have similar molecular structures and physiological functions. Infact, epinephrine which makes up 80% of the adrenal medullary secretion is synthesized from norepinephrine.
• The main function of norepinerphrine is maintenance of blood pressure by causing general vasoconstriction except of the coronary arteries.
Adrenaline is associated with potentiating the conditions needed for fight or flight after the initial sympathetic stimulation, example: 1. Constricting skin blood vessels 2. Dilating blood vessels of muscles, heart, brain 3. Converting glycogen to glucose 4. Increasing metabolic rate 5. Dilating the pupils 6. Dilating the bronchioles, allowing an increase in air intake 7. Increase heart rate and force of contraction
• The effects of these hormones are similar to those caused by stimulation of the sympathetic nervous system except that the hormonal effect lasts about 10 times longer.

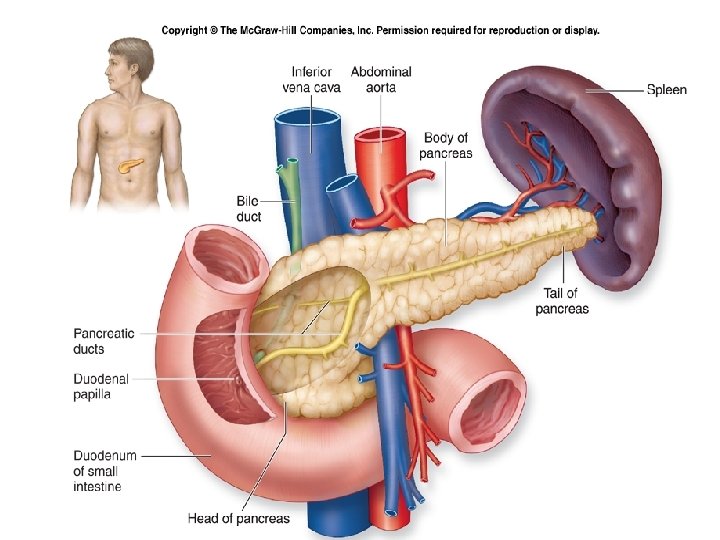
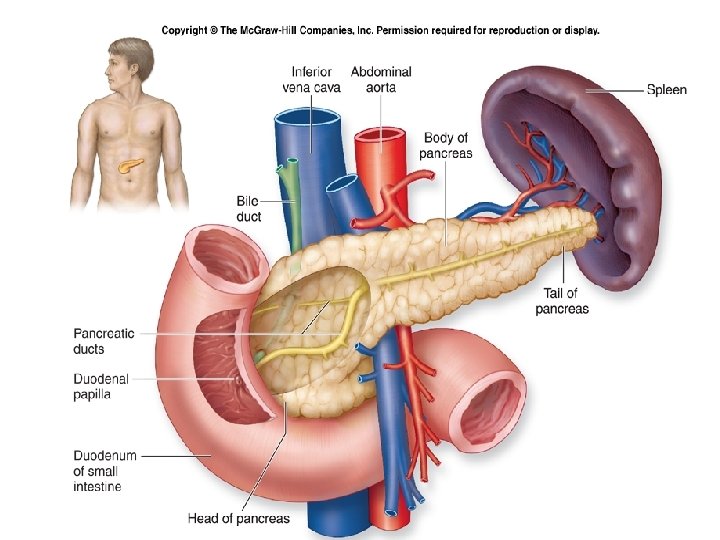
PANCREAS • The pancreas is a long organ that lies transversely in the abdomen between the kidneys and near the duodenum of the small intestine. • It lies posterior to the stomach. • It is composed of two types of tissue.
• Exocrine tissue produces and secretes digestive juices and endocrine tissue called the pancreatic islets (islets of langerhans) produces and secretes the hormones insulin and glucagon directly into the blood. • The pancreatic islet has two distinct cells – 1. alpha cells which secrete glucagon 2. beta cells which secrete insulin
INSULIN • The main function of insulin is to participate to maintain homeostasis of blood glucose. When absorbed nutrients especially glucose are in excess of immediate needs insulin promotes storage. • It reduces high blood nutrient levels by:
1. Acting on cell membranes and stimulating uptake and utilization of glucose by muscle and connective tissue cells. 2. Increasing conversion of glucose to glycogen, especially in the liver and skeletal muscles 3. Accelerating uptake of amino acids by cells and the synthesis of protein 4. Promoting synthesis of fatty acids and storage of fat in adipose tissue 5. Preventing the breakdown of protein and fat
• The negative feedback sensitive to blood glucose concentration regulates insulin secretion. • When blood glucose concentration is high as after a meal, beta cells release insulin to promote glycogen formation. • When glucose concentration falls as occurs between meals of during the night, insulin secretion decreases.
GLUCAGON • The effects of glucagon increase blood glucose levels by stimulating: 1. Conversion of glycogen to glucose (in the liver and skeletal muscles) 2. Gluconeogenesis 3. Lipolysis (hydrophysis of stored fat and the consequent release of free fatty acids into the blood. • Glucagon is thus a hormone that helps to maintian homeostasis during times of fasting when the body’s energy reserves must be utilized.
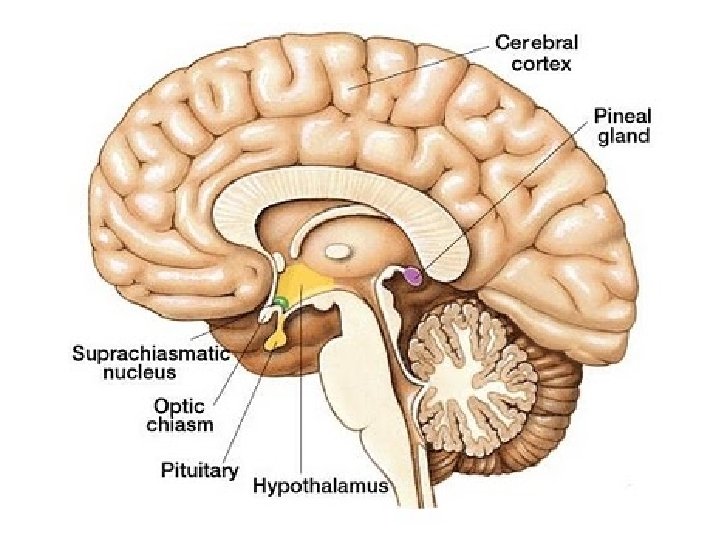
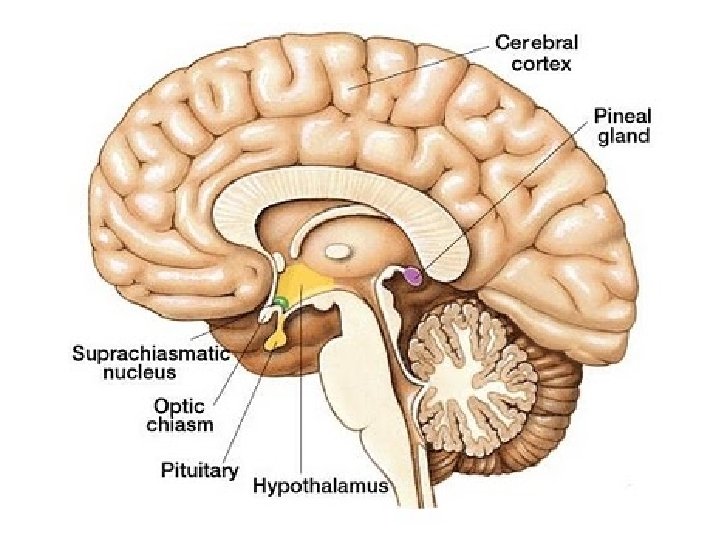
PINEAL BODY • The pineal body is a small structure situated deep between the cerebral hemispheres where it attaches to the upper portion of the thalamus near the roof of the 3 rd ventricle. • It is connected to the brain by a short stalk containing nerves, many of which terminate in the hypothalamus.
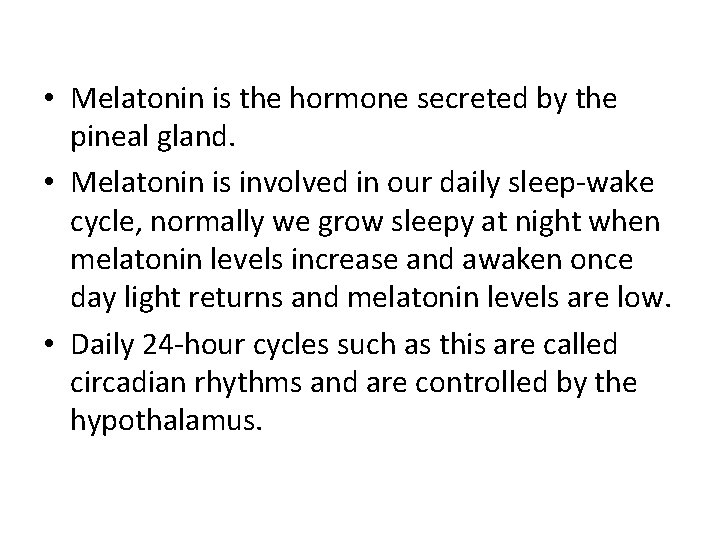
• Melatonin is the hormone secreted by the pineal gland. • Melatonin is involved in our daily sleep-wake cycle, normally we grow sleepy at night when melatonin levels increase and awaken once day light returns and melatonin levels are low. • Daily 24 -hour cycles such as this are called circadian rhythms and are controlled by the hypothalamus.
• It is also thought to inhibit growth and development of the sex organs before puberty possibly by preventing synthesis or release of gonadotrophins. • The gland atrophies after puberty.
THYMUS GLAND • The thymus gland which lies in the mediaternum posterior to the stenum and between the lungs is relatively large in younger children but shrinks with age. • This gland secretes a group of hormones called thymosins that affects the production and differentiation of certain white blood cells. • Lymphocytes that originate in the bone marrow and then pass through the thymus are transformed into T -lymphocytes. • The thymus gland plays an important role in cellmediated immunity.
GONADS • The ovaries and testes are the gonads. The testes are located in the scrotum and the ovaries are located in the pelvic cavity. • The testes produce androgens (eg testosterone) which are the male sex hormones, and the ovaries produce estrogen and progesterone, the female sex hormones. • The hypothalamus and the pituitary gland control the hormonal secretions of these organs.
• Greatly increased testosterone secretion at the time of puberty stimulates the growth of the penis and the testes. • Testosterone also brings about and maintains the male secondary sex characteristics that develop during puberty including the growth of beard, axillary hair and pubic hair. • It prompts the larynx and the vocal cords to enlarge causing the voice to deepen. It is partially responsible for the muscular strength of males.
• The female sex hormones, estrogen and progestrone have many effects on the body. In particular estrogen secreted at the time of puberty stimulates the growth of the uterus and the vagina. • Estrogen is necessary for egg maturation and is largely responsible for secondary sex characteristics in females, including female body hair and fat distribution. • Both estrogen and progesterone are required for breast development and for regulation of the uterine cycle which includes monthly menstruation
The End, THANK YOU