DIGESTIVE SYSTEM Digestive System of the Frog Digestive


- Slides: 41

DIGESTIVE SYSTEM
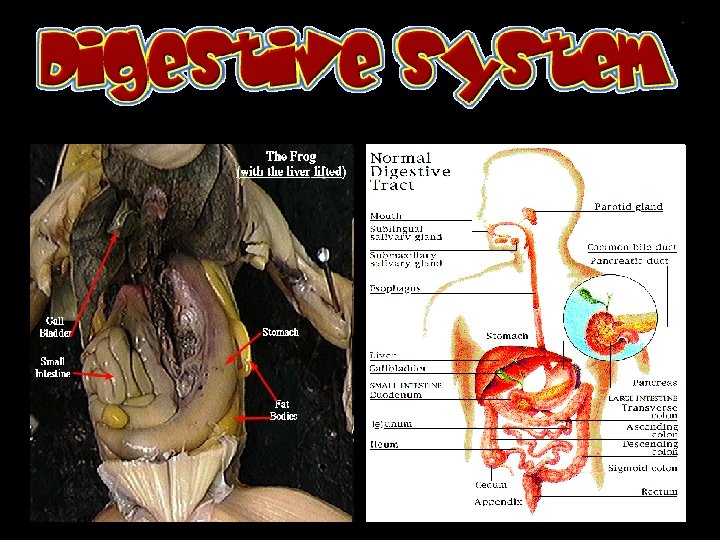
Digestive System of the Frog
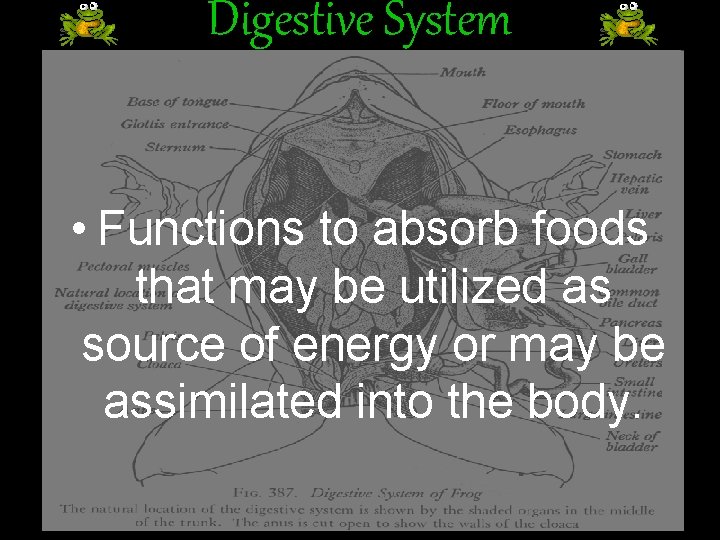
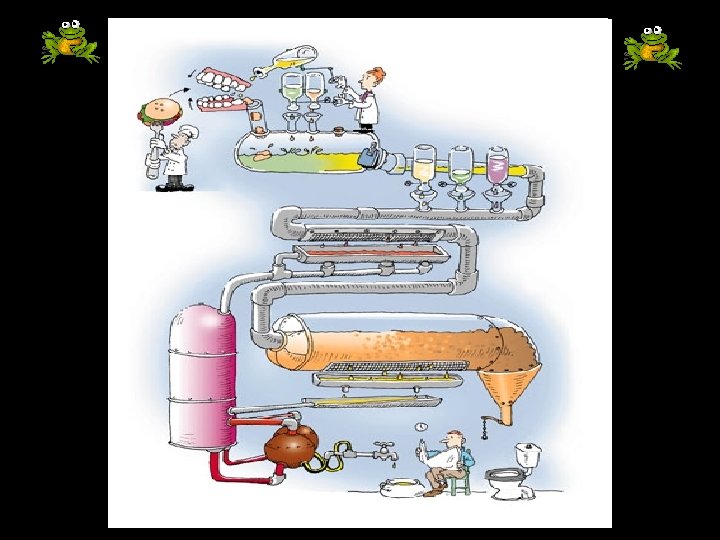
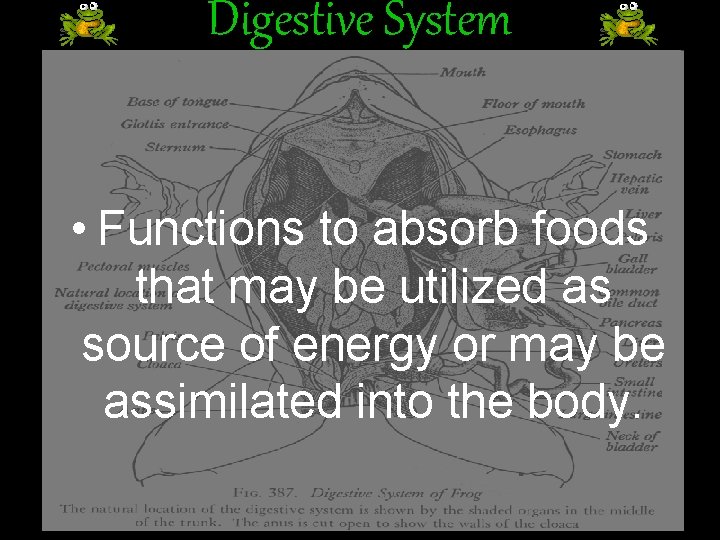
Digestive System • Functions to absorb foods that may be utilized as source of energy or may be assimilated into the body.
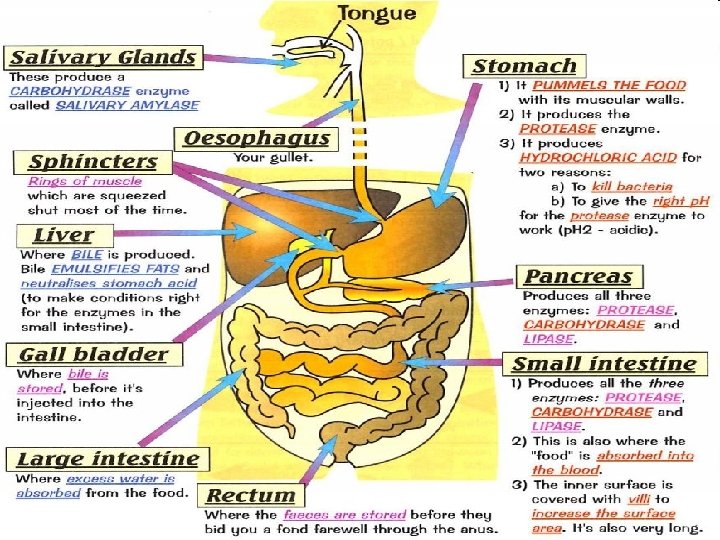
Digestion Is the process by which food is broken down into simpler, usable molecules to be absorbed by the body.
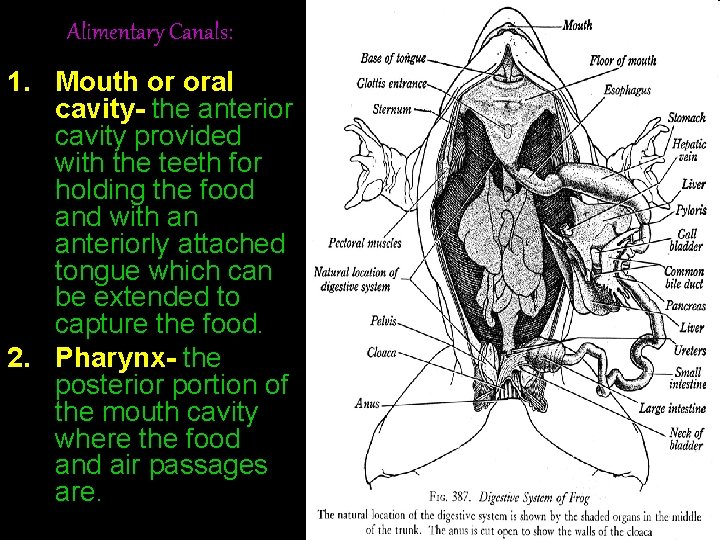
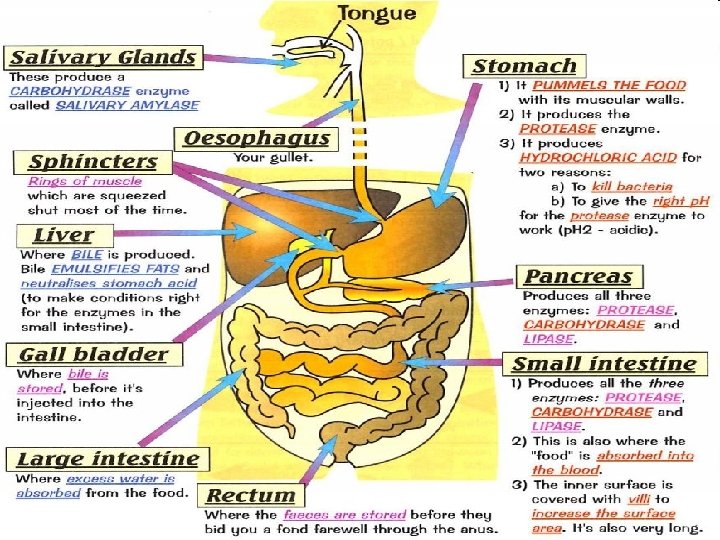
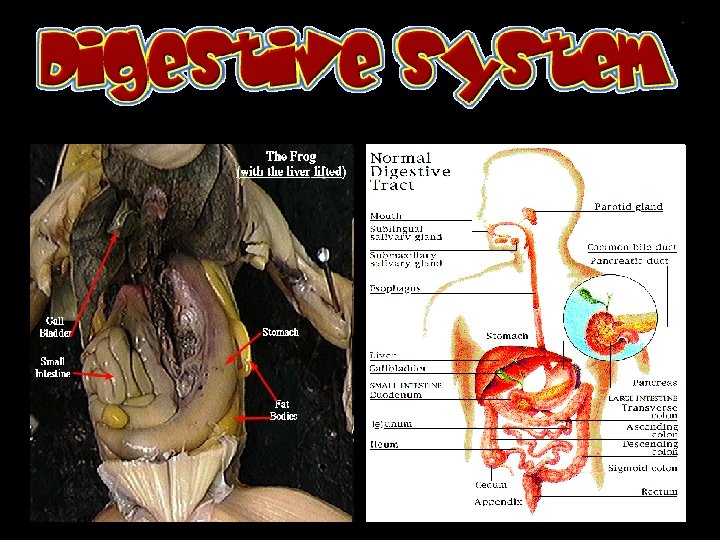
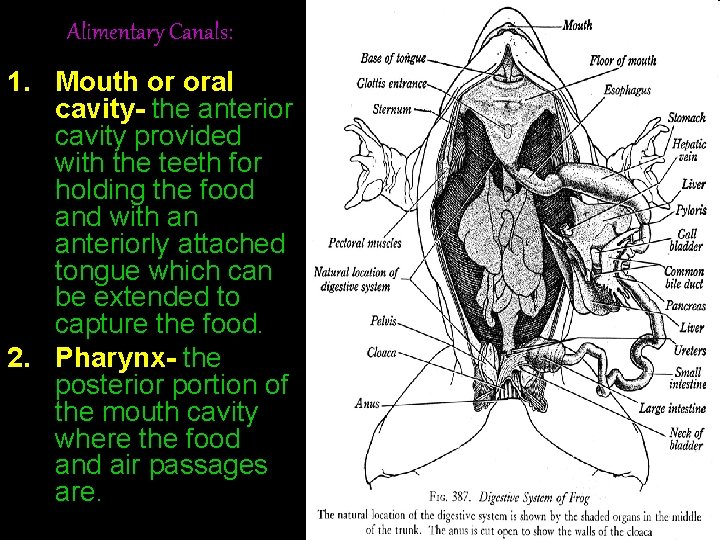
Alimentary Canals: 1. Mouth or oral cavity- the anterior cavity provided with the teeth for holding the food and with an anteriorly attached tongue which can be extended to capture the food. 2. Pharynx- the posterior portion of the mouth cavity where the food and air passages are.
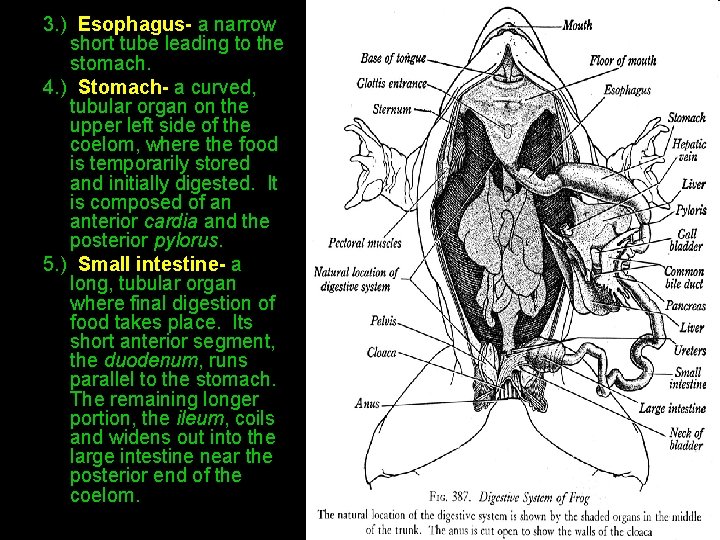
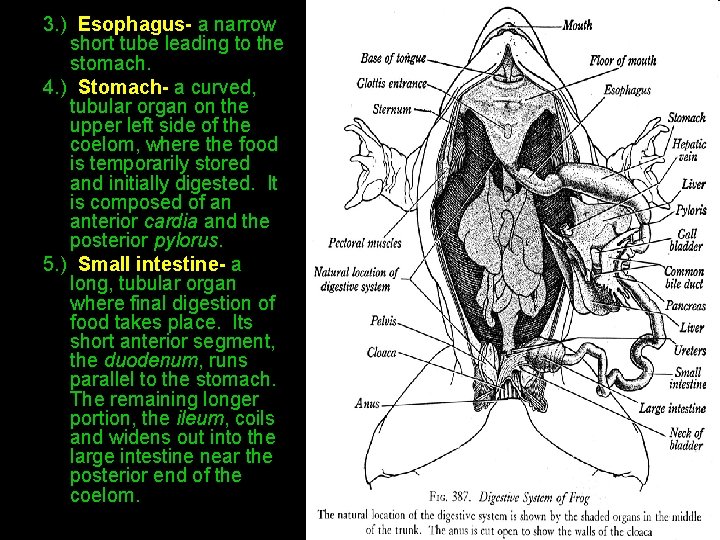
3. ) Esophagus- a narrow short tube leading to the stomach. 4. ) Stomach- a curved, tubular organ on the upper left side of the coelom, where the food is temporarily stored and initially digested. It is composed of an anterior cardia and the posterior pylorus. 5. ) Small intestine- a long, tubular organ where final digestion of food takes place. Its short anterior segment, the duodenum, runs parallel to the stomach. The remaining longer portion, the ileum, coils and widens out into the large intestine near the posterior end of the coelom.
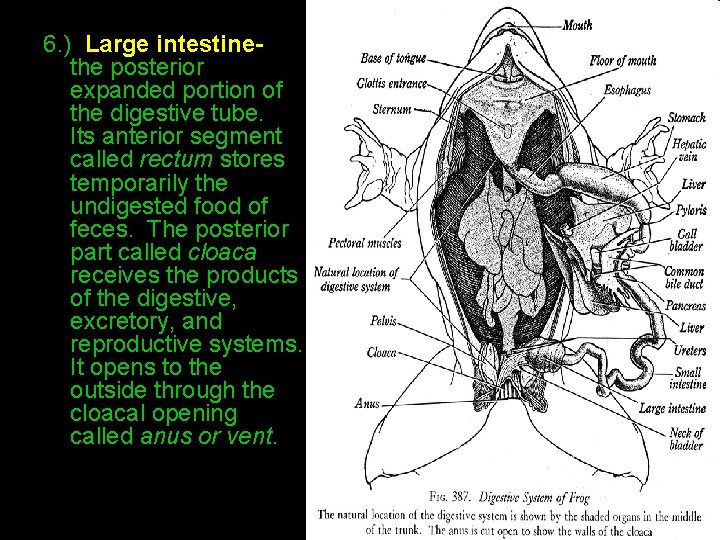
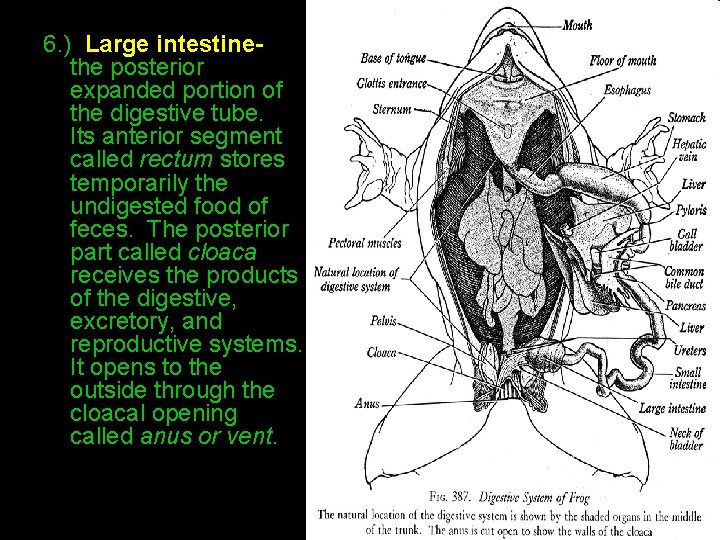
6. ) Large intestine- the posterior expanded portion of the digestive tube. Its anterior segment called rectum stores temporarily the undigested food of feces. The posterior part called cloaca receives the products of the digestive, excretory, and reproductive systems. It opens to the outside through the cloacal opening called anus or vent.
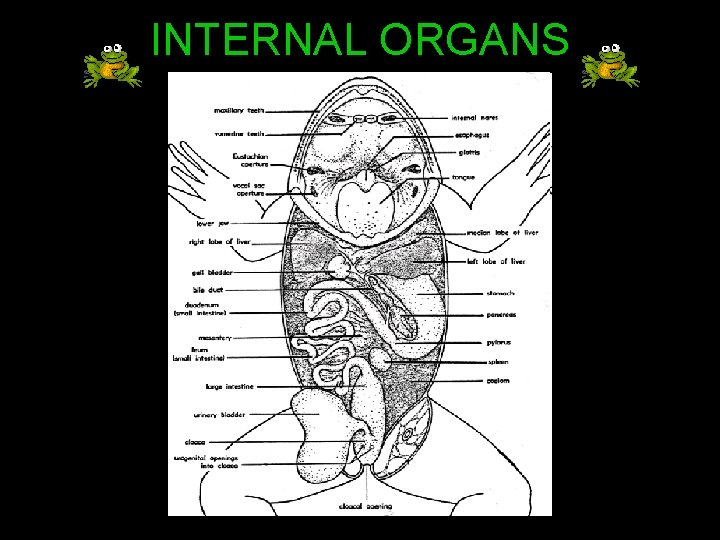
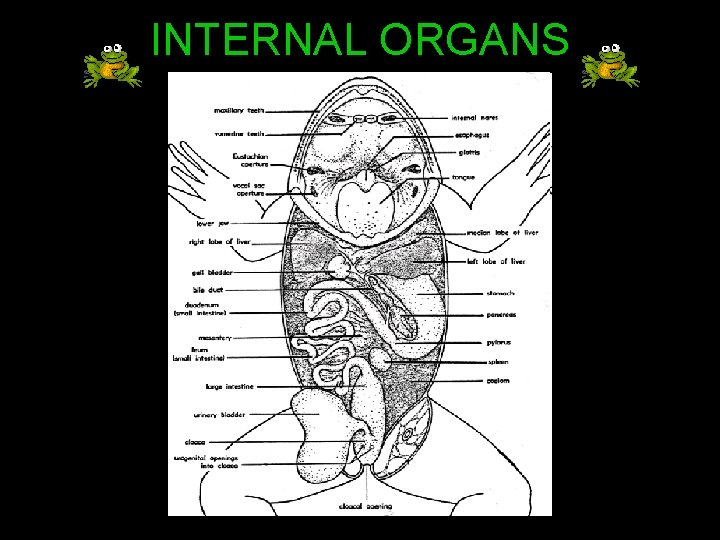
INTERNAL ORGANS
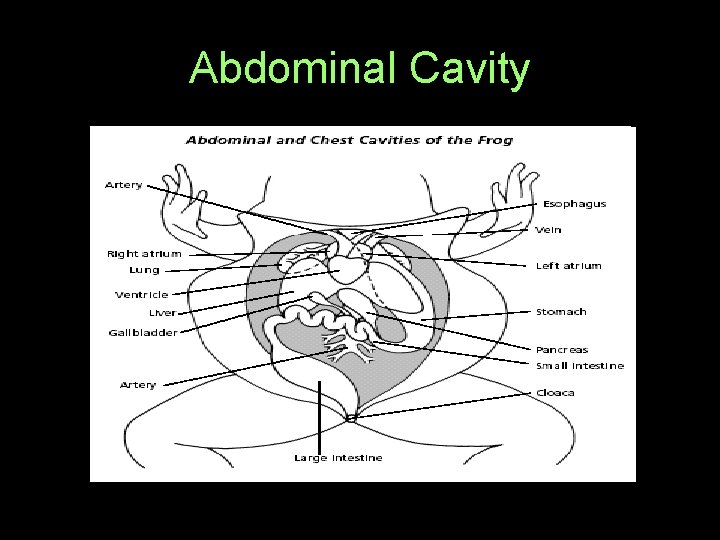
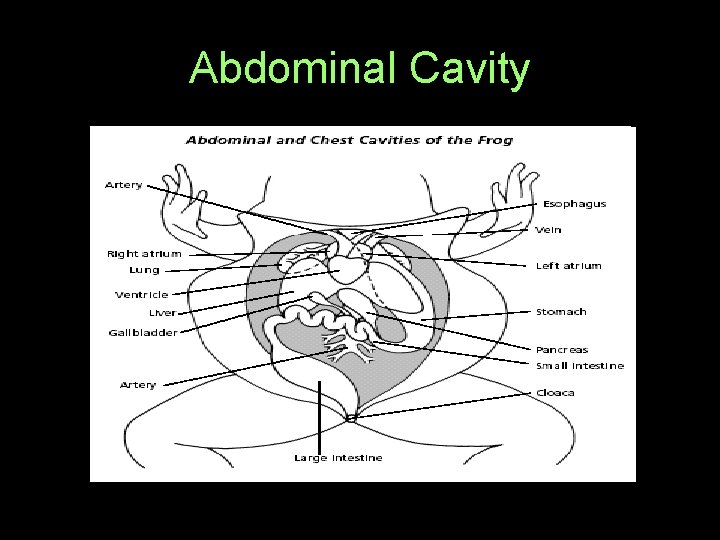
Abdominal Cavity
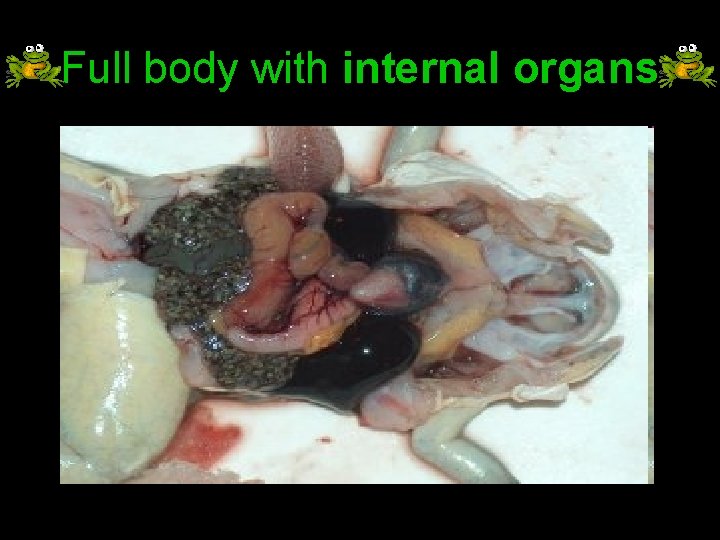
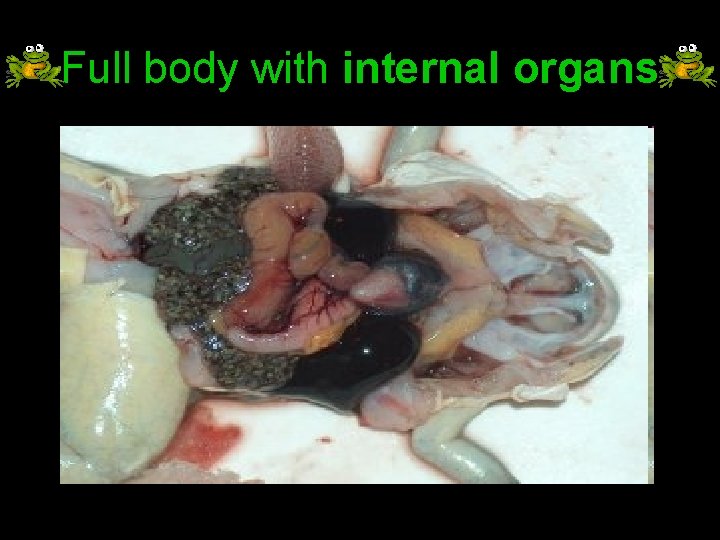
Full body with internal organs
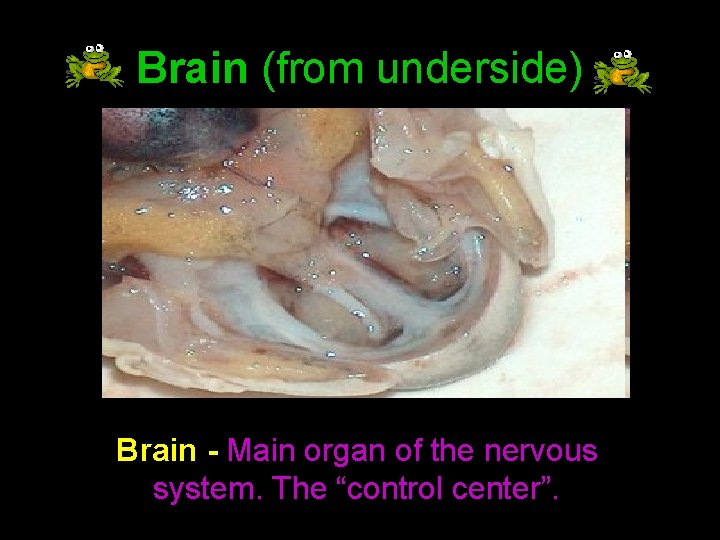
Brain (from underside) Brain - Main organ of the nervous system. The “control center”.
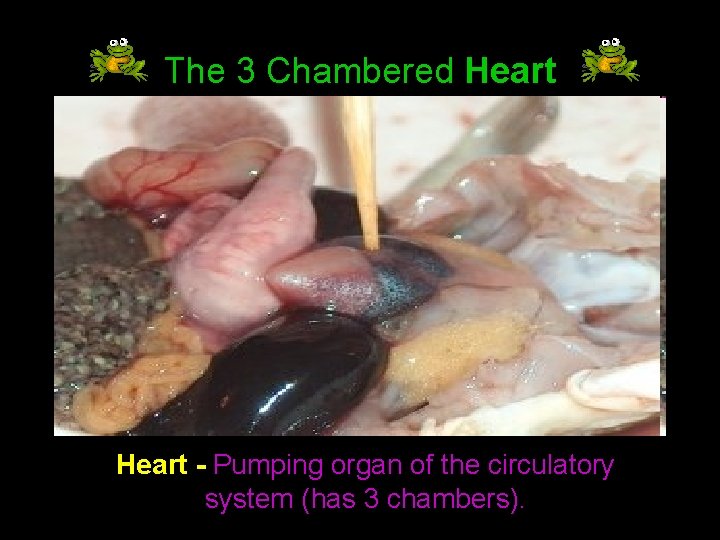
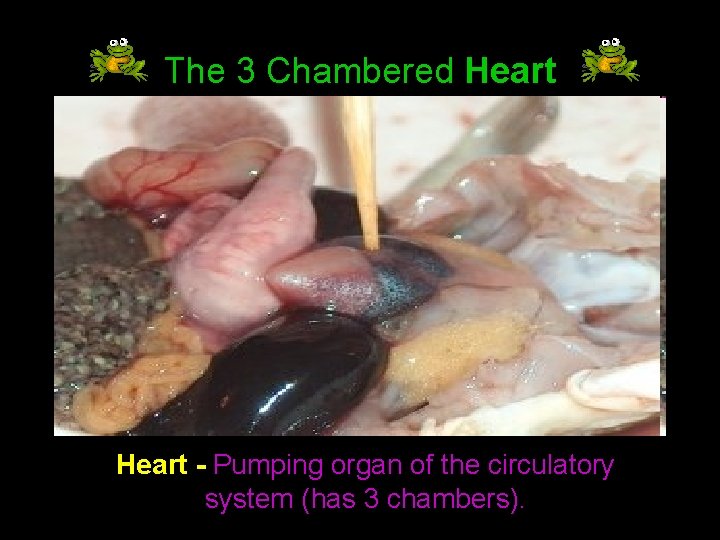
The 3 Chambered Heart - Pumping organ of the circulatory system (has 3 chambers).
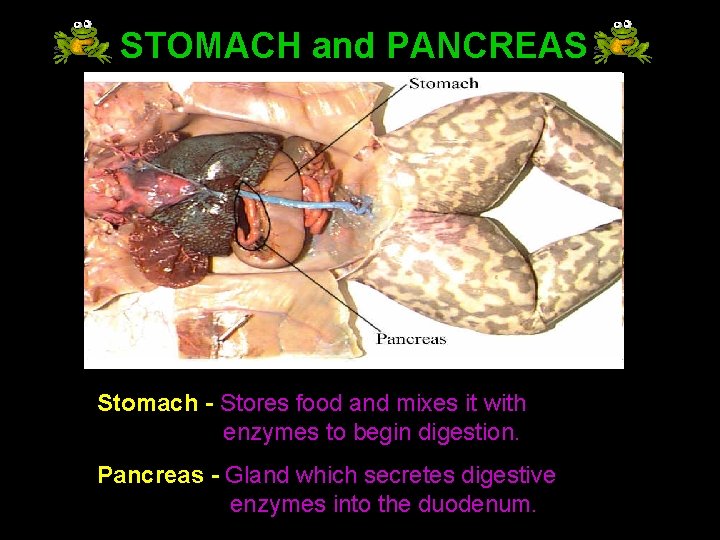
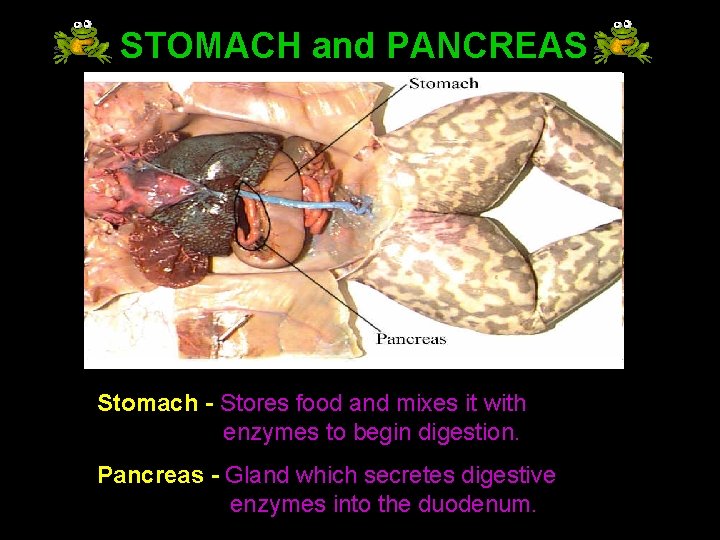
STOMACH and PANCREAS Stomach - Stores food and mixes it with enzymes to begin digestion. Pancreas - Gland which secretes digestive enzymes into the duodenum.
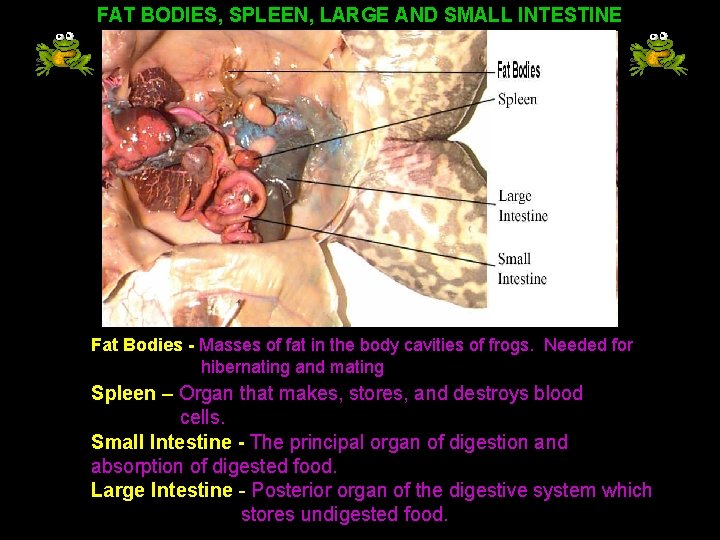
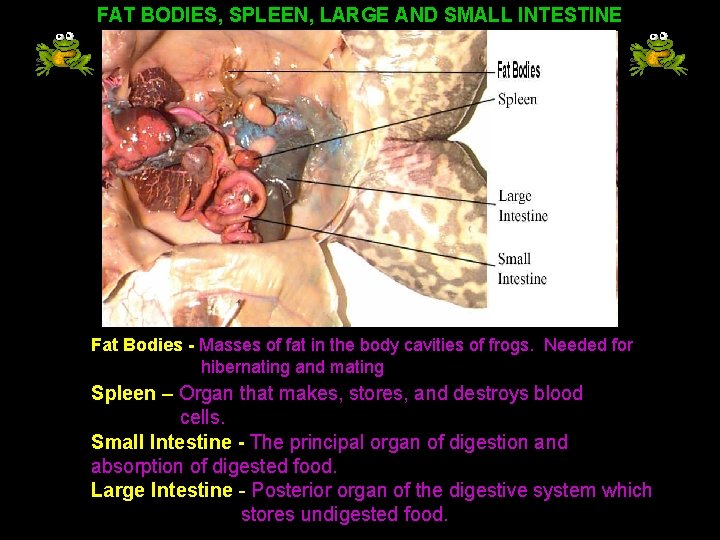
FAT BODIES, SPLEEN, LARGE AND SMALL INTESTINE Fat Bodies - Masses of fat in the body cavities of frogs. Needed for hibernating and mating Spleen – Organ that makes, stores, and destroys blood cells. Small Intestine - The principal organ of digestion and absorption of digested food. Large Intestine - Posterior organ of the digestive system which stores undigested food.
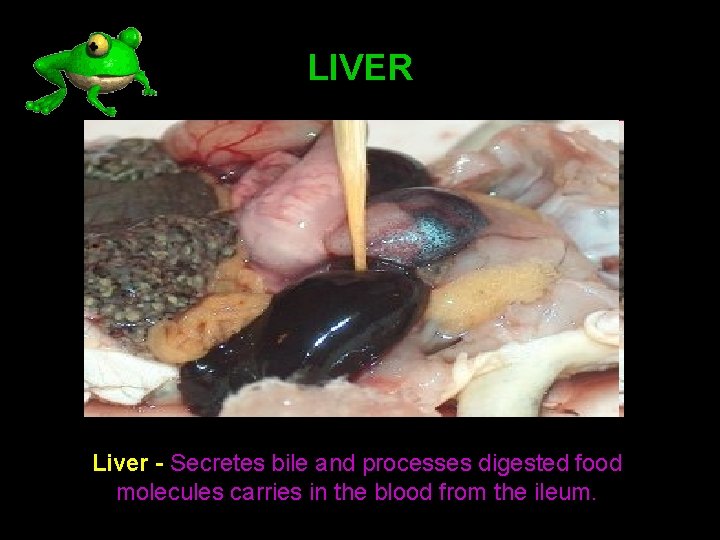
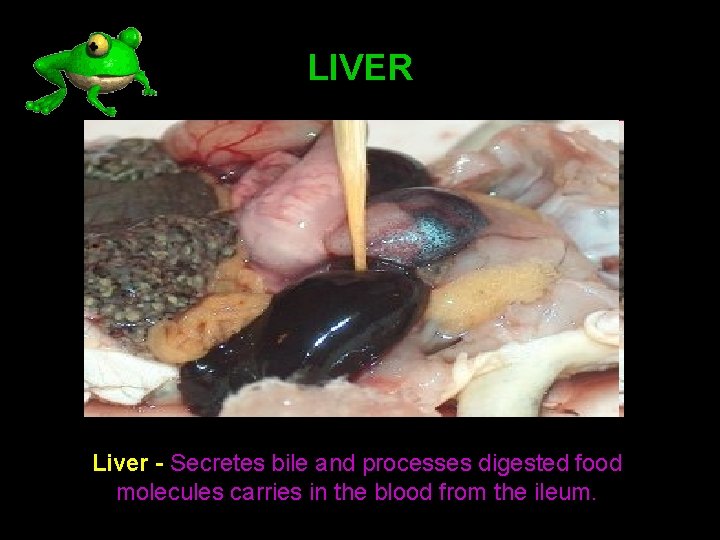
LIVER Liver - Secretes bile and processes digested food molecules carries in the blood from the ileum.
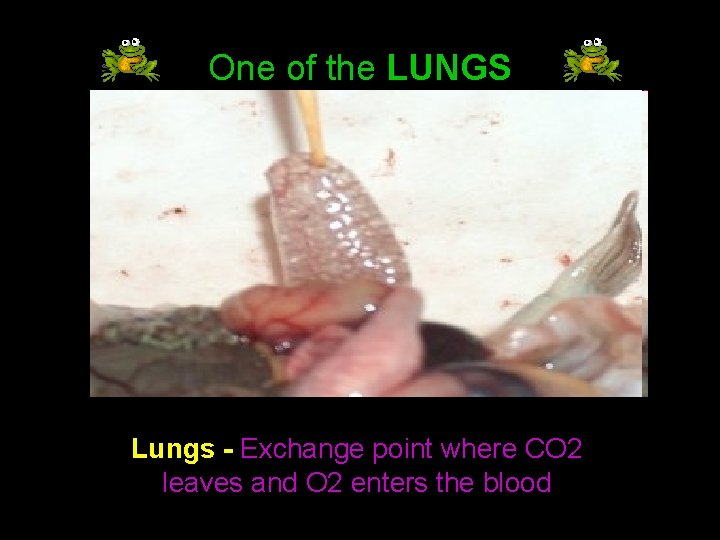
One of the LUNGS Lungs - Exchange point where CO 2 leaves and O 2 enters the blood
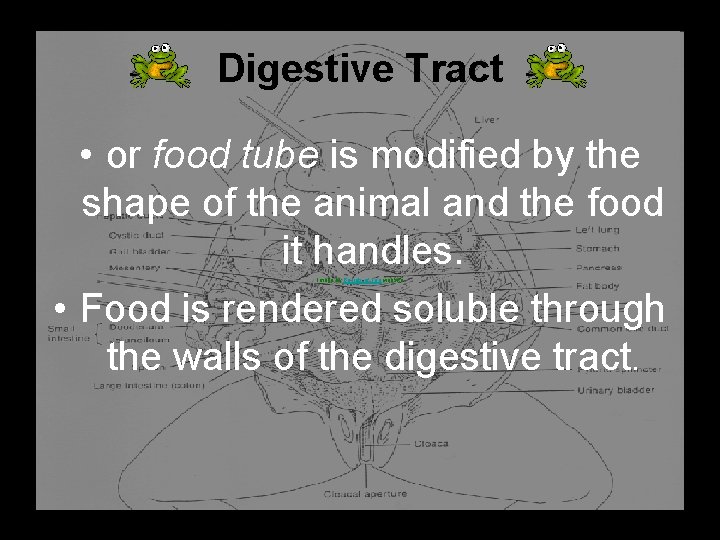
Digestive Tract • or food tube is modified by the shape of the animal and the food it handles. • Food is rendered soluble through the walls of the digestive tract. Image by Barrels of Fun website
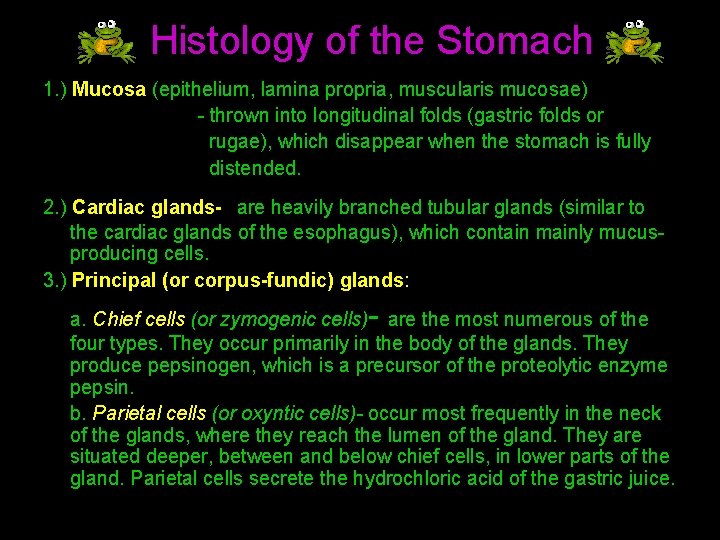
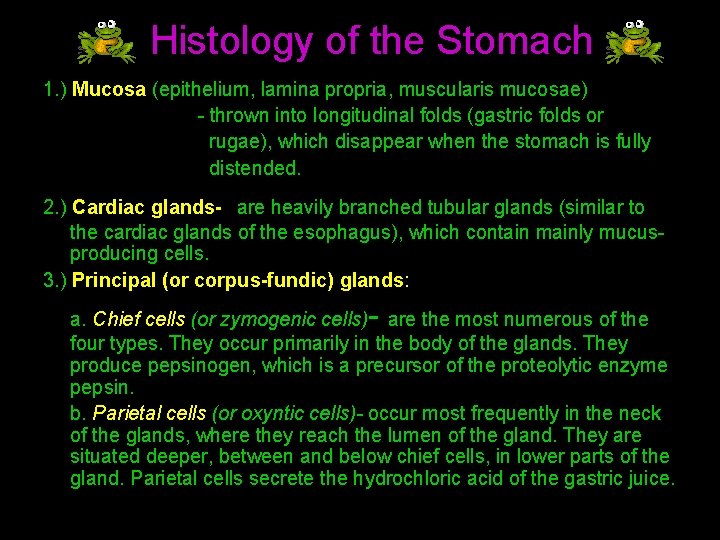
Histology of the Stomach 1. ) Mucosa (epithelium, lamina propria, muscularis mucosae) - thrown into longitudinal folds (gastric folds or rugae), which disappear when the stomach is fully distended. 2. ) Cardiac glands- are heavily branched tubular glands (similar to the cardiac glands of the esophagus), which contain mainly mucusproducing cells. 3. ) Principal (or corpus-fundic) glands: - a. Chief cells (or zymogenic cells) are the most numerous of the four types. They occur primarily in the body of the glands. They produce pepsinogen, which is a precursor of the proteolytic enzyme pepsin. b. Parietal cells (or oxyntic cells)- occur most frequently in the neck of the glands, where they reach the lumen of the gland. They are situated deeper, between and below chief cells, in lower parts of the gland. Parietal cells secrete the hydrochloric acid of the gastric juice.
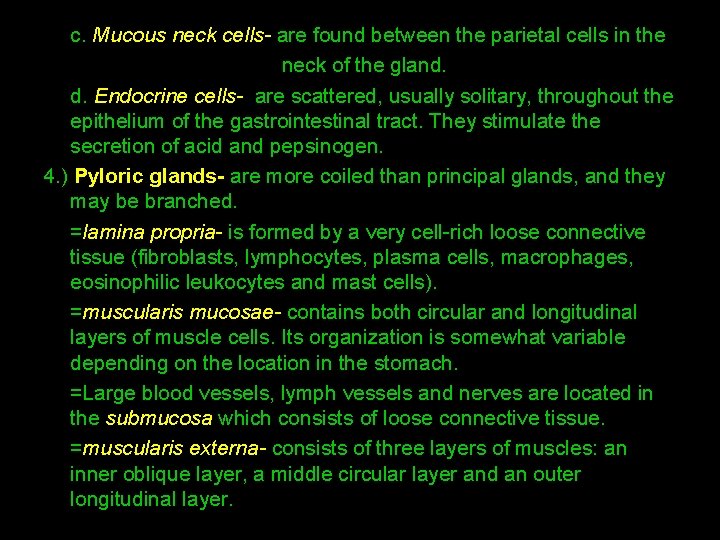
c. Mucous neck cells- are found between the parietal cells in the neck of the gland. d. Endocrine cells- are scattered, usually solitary, throughout the epithelium of the gastrointestinal tract. They stimulate the secretion of acid and pepsinogen. 4. ) Pyloric glands- are more coiled than principal glands, and they may be branched. =lamina propria- is formed by a very cell-rich loose connective tissue (fibroblasts, lymphocytes, plasma cells, macrophages, eosinophilic leukocytes and mast cells). =muscularis mucosae- contains both circular and longitudinal layers of muscle cells. Its organization is somewhat variable depending on the location in the stomach. =Large blood vessels, lymph vessels and nerves are located in the submucosa which consists of loose connective tissue. =muscularis externa- consists of three layers of muscles: an inner oblique layer, a middle circular layer and an outer longitudinal layer.
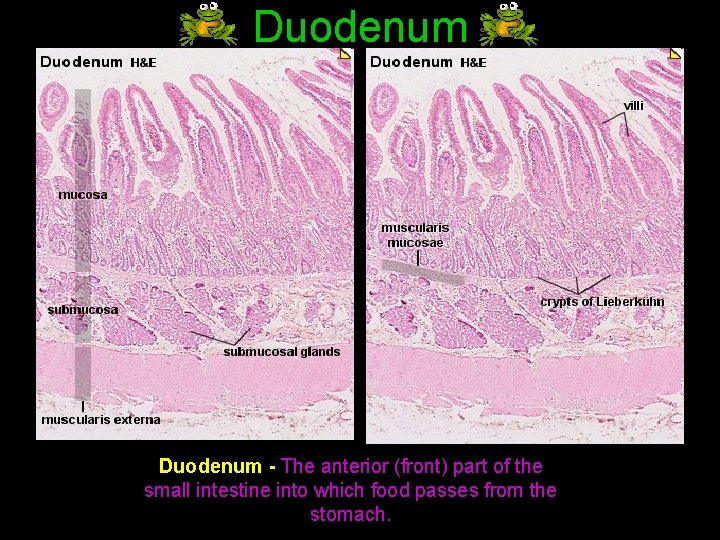
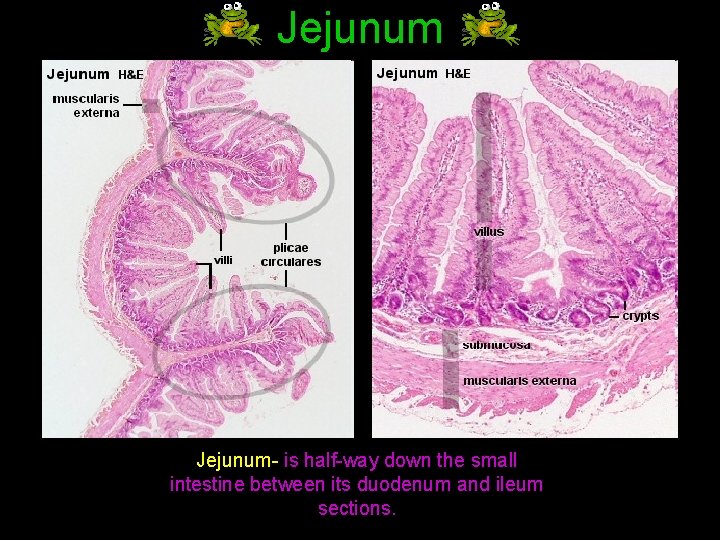
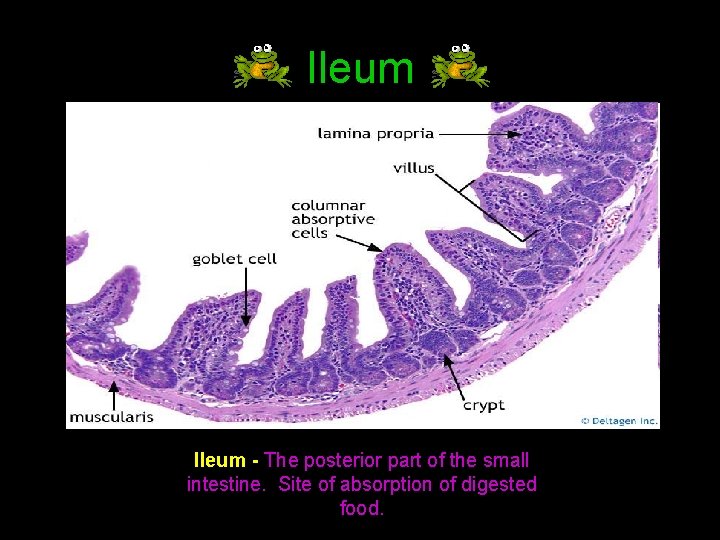
Histology of the Small Intestine • The small intestine is divided into duodenum, jejunum and ileum. The three segments merge imperceptibly and have the same basic histological organization. 1. ) The Mucosa of the small intestine has various structural features which considerably increase the luminal surface area and consequently support the main function of the small intestine - the absorption of the degraded components of the food. =Plicae circulares- are permanent structures, i. e. their presence does not depend on the state of distension of the small intestine. - are absent from the first few centimetres of the duodenum and the distal part of the ileum. - are particularly well developed in the jejunum. • The entire intestinal mucosa forms intestinal villi, which increase the surface area by a factor of ~ ten. The surface of the villi is formed by a simple columnar epithelium. Each absorptive cell or enterocyte of the epithelium forms numerous microvilli. Microvilli increase the surface area by a factor of ~ 20.
=Lamina propria- is similar to the lamina propria of the stomach, unusually cell rich. Lymphocytes often invade the epithelium or form solitary lymphoid nodules in the lamina propria. Lymph nodules may form longitudinal aggregations of 30 -50 nodules in the lamina propria of the ileum. These large aggregations are called Peyer's patches . =Muscularis mucosae- has two layers and extends into the intestinal villi, where the smooth muscle cells form a longitudinal bundle in the centre of the villi. 2. ) The Submucosa contains glands only in the duodenum. Submucosal glands of the duodenum are also called Brunner's glands. Their secretion is mucous and slightly alkaline due to bicarbonate ions
Divisions of SMALL INTESTINE Duodenum Jejunum Ilium
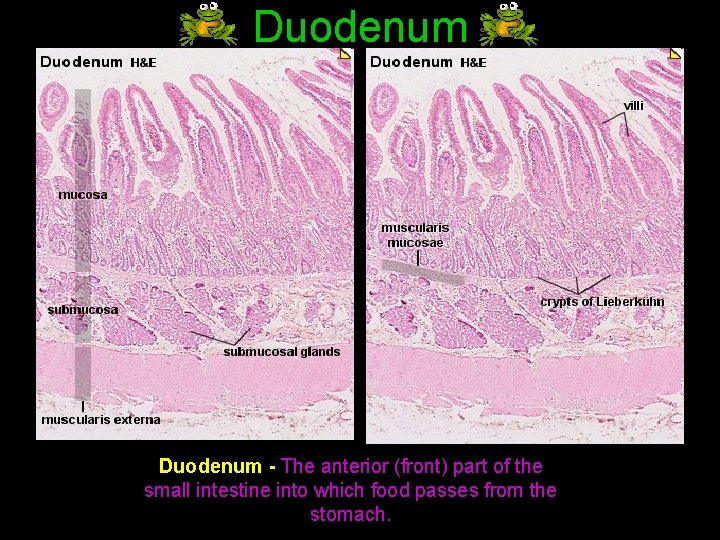
Duodenum - The anterior (front) part of the small intestine into which food passes from the stomach.
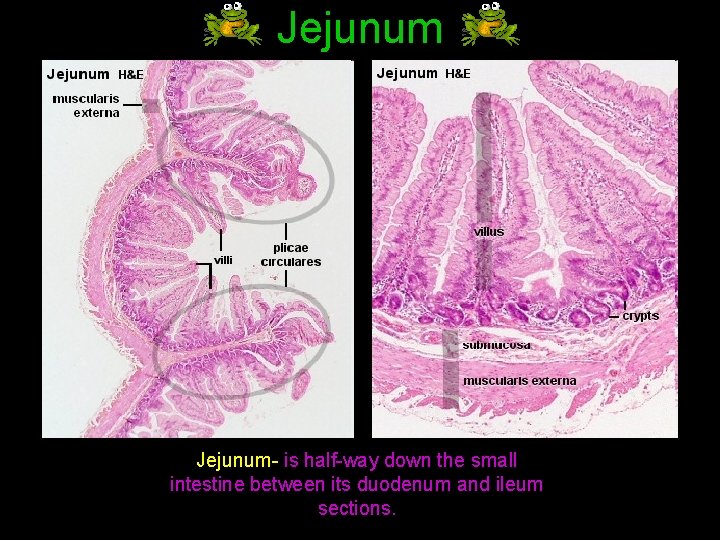
Jejunum- is half-way down the small intestine between its duodenum and ileum sections.
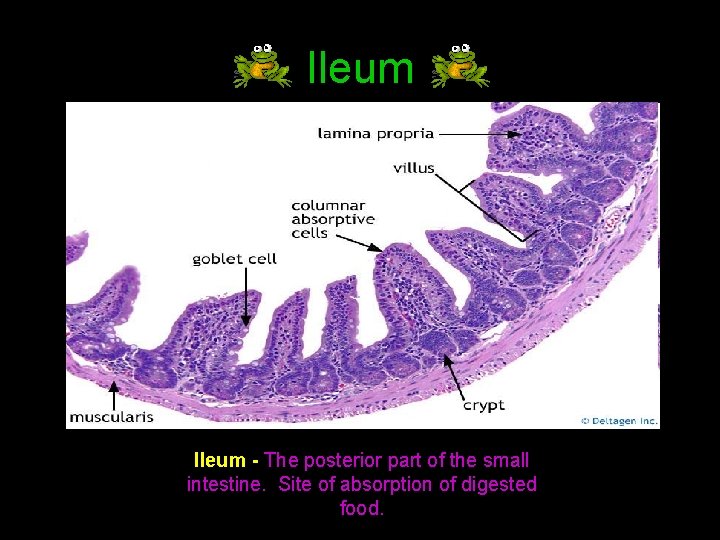
Ileum - The posterior part of the small intestine. Site of absorption of digested food.
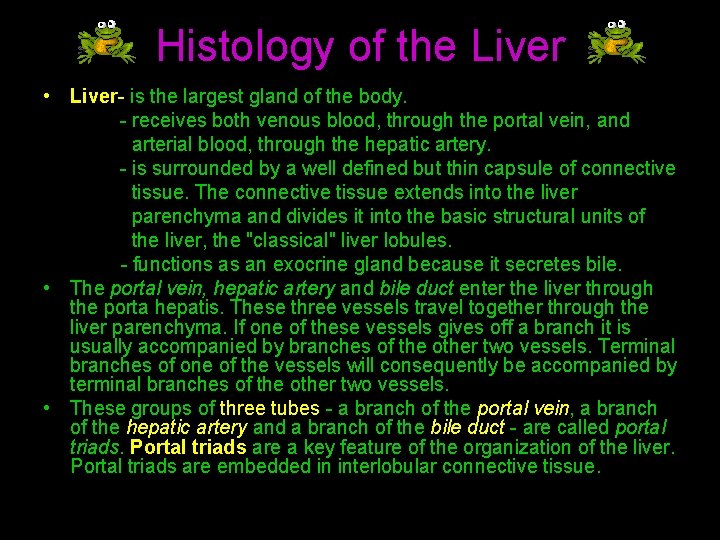
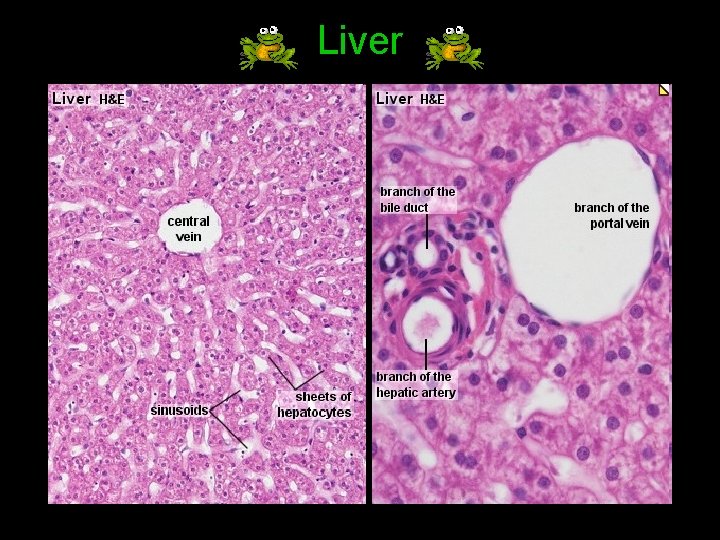
Histology of the Liver • Liver- is the largest gland of the body. - receives both venous blood, through the portal vein, and arterial blood, through the hepatic artery. - is surrounded by a well defined but thin capsule of connective tissue. The connective tissue extends into the liver parenchyma and divides it into the basic structural units of the liver, the "classical" liver lobules. - functions as an exocrine gland because it secretes bile. • The portal vein, hepatic artery and bile duct enter the liver through the porta hepatis. These three vessels travel together through the liver parenchyma. If one of these vessels gives off a branch it is usually accompanied by branches of the other two vessels. Terminal branches of one of the vessels will consequently be accompanied by terminal branches of the other two vessels. • These groups of three tubes - a branch of the portal vein, a branch of the hepatic artery and a branch of the bile duct - are called portal triads. Portal triads are a key feature of the organization of the liver. Portal triads are embedded in interlobular connective tissue.
Liver Lobule • • • Liver lobule- is filled by cords of hepatic parenchymal cells, hepatocytes, which radiate from the central vein and are separated by vascular sinusoids. Portal lobule- emphasize the afferent blood supply and bile drainage by the vessels of the portal triads. The secretory function of the liver is emphasized by the term liver acinus. Hepatocytes are separated from the bloodstream by a thin discontinuous simple squamous epithelium, which lines the sinusoids. Between the hepatocytes and the epithelial cells is a narrow perisinusoidal space. Contents of the blood plasma can freely enter the perisinusoidal space through the openings in the epithelium lining the sinusoids. Fixed macrophages, Kupffer cells, are attached to the epithelium The liver lobule is drained by the central vein, which open into the intercalated or sublobular veins of the liver. These in turn coalesce to form the hepatic veins. They run alone through the tissue, are usually covered by connective tissue and eventually empty into the inferior vena cava. Adjoining liver cells form the walls of the bile canaliculi, which form a three dimensional network within the sheets of hepatocytes. Bile canaliculi connect via very short canals to terminal bile ducts (cholangioles) which empty into the interlobular bile ducts found in the portal triads.
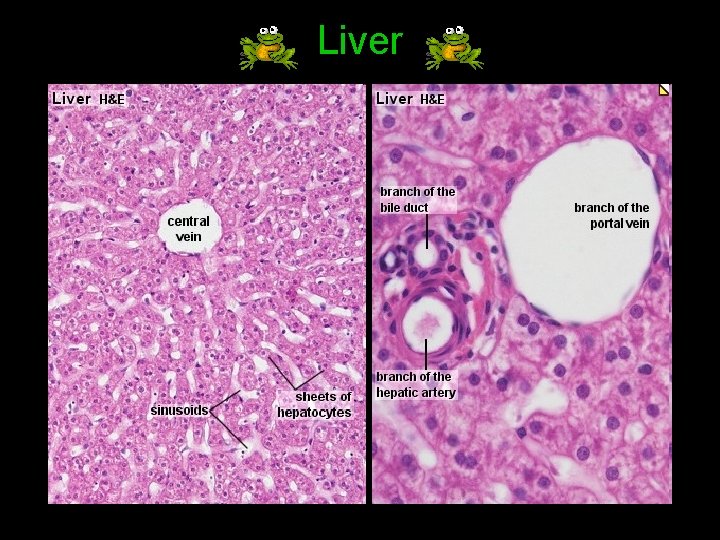
Liver
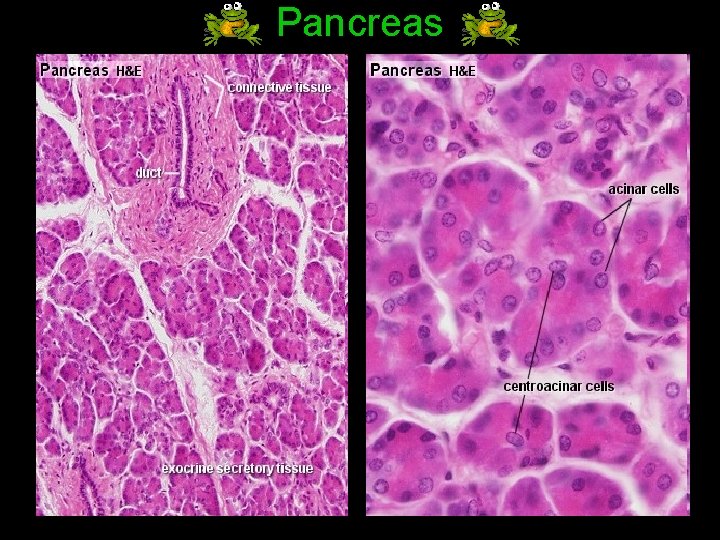
Histology of the Pancreas • Pancreas- is positioned retroperitoneally on the posterior wall of the abdominal cavity at the level of the second and third lumbar vertebrae. - has no distinct capsule, but is covered by a thin layer of loose connective tissue. - is both an exocrine and endocrine gland. The exocrine part produces about 1. 5 l of pancreatic juice every day. The endocrine part, which accounts for ~1% of the pancreas, consists of the cells of the islands of Langerhans. These cells produce insulin, glucagon and a number of other hormones.
• The exocrine pancreas consists of tubuloacinar glands. A single layer of pyramidal shaped cells forms the secretory acini. The apical cytoplasm (towards the lumen of the acini) is filled with secretory vesicles containing the precursors of digestive enzymes. The first portion of the duct system extends into the centre of the acini, which is lined by small centroacinar cells. These cells form the first part of intercalated ducts. Intercalated ducts are lined by low columnar or cuboidal epithelium. They empty into interlobular ducts, which are lined by a columnar epithelium. Interlobular ducts in turn empty into the main pancreatic duct, which is lined by a tall columnar epithelium. • The main pancreatic duct opens into the summit of the major duodenal papilla, usually in common with the bile duct. A duct draining the lower parts of the head of the pancreas, the accessory pancreatic duct, is very variable. If present, it may open into the minor duodenal papilla ~2 cm above the major papilla in the duodenum. • Pancreatic juice is a clear alkaline fluid which contains the precursors of enzymes of all classes necessary to break down the main components of the diet. • Proteolytic enzymes are secreted as zymogens - inactive precursors of the enzymes. They are activated in the lumen of the digestive canal. The enzyme enteropeptidase is associated with the brush border of enterocytes. It catalyses the conversion of trysinogen into trypsin. Trypsin can activate a number of the other pancreatic zymogens.
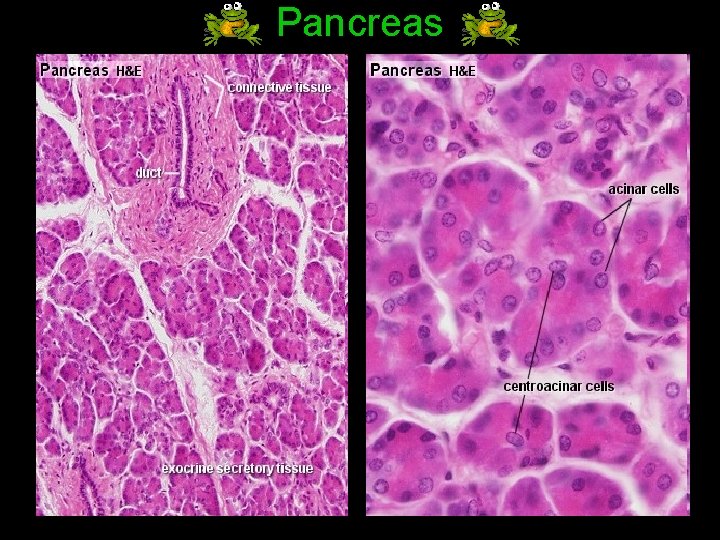
Pancreas
Digestive Enzymes • Enzymes- are protein-based substances essential to every bodily function, including healthy digestion. • Digestive enzymes- are normally present in raw whole foods to aid digestion. Without digestive enzymes, the body may not completely break down ingested foods to absorb their nutrients, and undigested food in the digestive tract can ferment and release harmful toxins.
Enzymes in the Oral cavity • Bromelaine tenderizes meat and acts as an anti-inflamatory agent. • Betaine effects cell fluid balance as osmolytes • Salivary Amylase (also known as ptyalin) (Mouth) produced by salivary glands breaks down starch into sugar.
Enzymes in the Stomach The enzymes that get secreted in the stomach are called gastric enzymes. These are the following: • Pepsin is the main gastric enzyme. As it breaks proteins into smaller peptide fragments. • Gelatinase, degrades type I and type V gelatin and type IV and V collagen, which are proteoglycans in meat. • Gastric amylase degrades starch, but is of minor significance. • Gastric lipase is a tributyrase by its biochemical activity, as it acts almost exclusively on tributyrin, a butter fat enzyme. • Pepsin enzyme is secreted by gastric glands • Renin enzyme change the liquid milk to solid
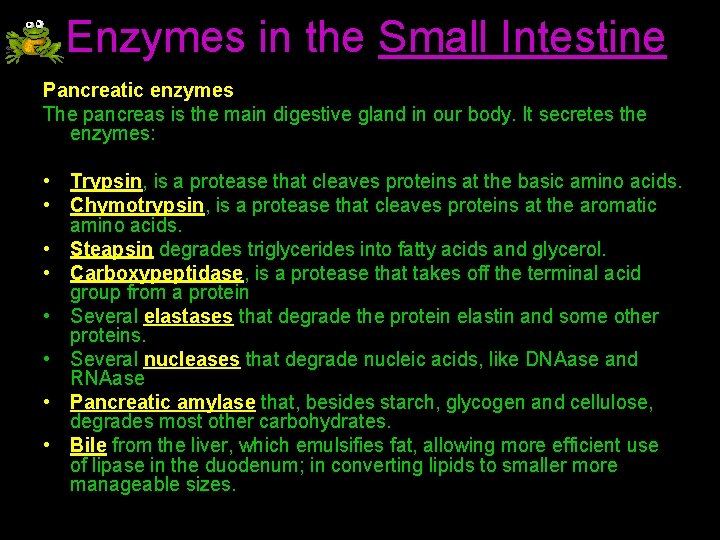
Enzymes in the Small Intestine Pancreatic enzymes The pancreas is the main digestive gland in our body. It secretes the enzymes: • Trypsin, is a protease that cleaves proteins at the basic amino acids. • Chymotrypsin, is a protease that cleaves proteins at the aromatic amino acids. • Steapsin degrades triglycerides into fatty acids and glycerol. • Carboxypeptidase, is a protease that takes off the terminal acid group from a protein • Several elastases that degrade the protein elastin and some other proteins. • Several nucleases that degrade nucleic acids, like DNAase and RNAase • Pancreatic amylase that, besides starch, glycogen and cellulose, degrades most other carbohydrates. • Bile from the liver, which emulsifies fat, allowing more efficient use of lipase in the duodenum; in converting lipids to smaller more manageable sizes.
Proper small intestine enzymes • Several peptidases. • The jejunum and ileum secretes a juice called succus entericus which contains the following: Five types of enzymes degrade disaccharides into monosaccharides: • Sucrase, which breaks down sucrose into glucose and fructose • Maltase, which breaks down maltose into glucose. • Isomaltase, which breaks down maltose and isomaltose • Lactase, which breaks down lactose into glucose and galactose • Intestinal lipase, which breaks down fatty acids
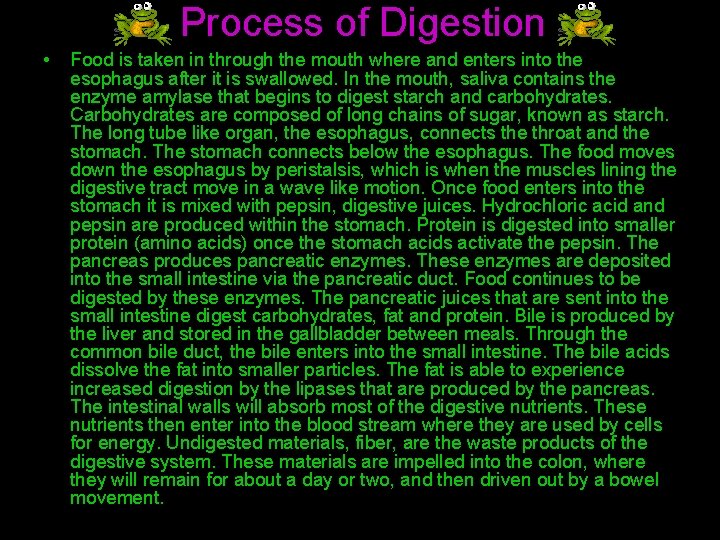
Process of Digestion • Food is taken in through the mouth where and enters into the esophagus after it is swallowed. In the mouth, saliva contains the enzyme amylase that begins to digest starch and carbohydrates. Carbohydrates are composed of long chains of sugar, known as starch. The long tube like organ, the esophagus, connects the throat and the stomach. The stomach connects below the esophagus. The food moves down the esophagus by peristalsis, which is when the muscles lining the digestive tract move in a wave like motion. Once food enters into the stomach it is mixed with pepsin, digestive juices. Hydrochloric acid and pepsin are produced within the stomach. Protein is digested into smaller protein (amino acids) once the stomach acids activate the pepsin. The pancreas produces pancreatic enzymes. These enzymes are deposited into the small intestine via the pancreatic duct. Food continues to be digested by these enzymes. The pancreatic juices that are sent into the small intestine digest carbohydrates, fat and protein. Bile is produced by the liver and stored in the gallbladder between meals. Through the common bile duct, the bile enters into the small intestine. The bile acids dissolve the fat into smaller particles. The fat is able to experience increased digestion by the lipases that are produced by the pancreas. The intestinal walls will absorb most of the digestive nutrients. These nutrients then enter into the blood stream where they are used by cells for energy. Undigested materials, fiber, are the waste products of the digestive system. These materials are impelled into the colon, where they will remain for about a day or two, and then driven out by a bowel movement.