Digestive glands DIGESTIVE SYSTEM Gastrointestinal tract The digestive


- Slides: 31

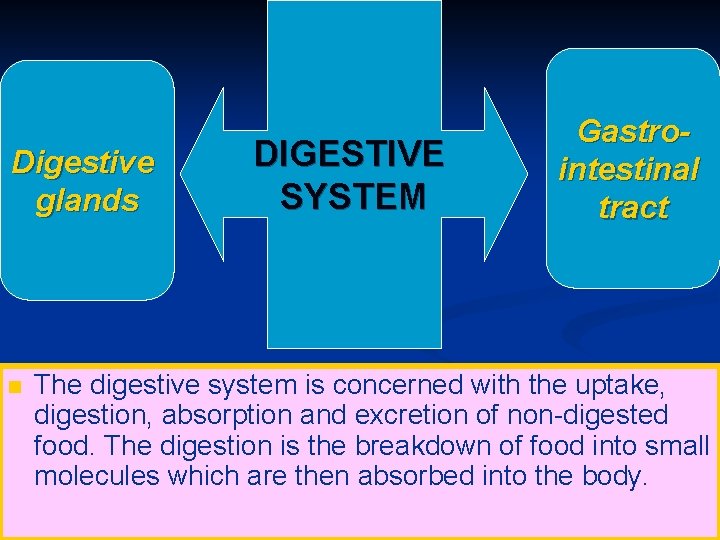
Digestive glands DIGESTIVE SYSTEM Gastrointestinal tract The digestive system is concerned with the uptake, digestion, absorption and excretion of non-digested food. The digestion is the breakdown of food into small molecules which are then absorbed into the body.
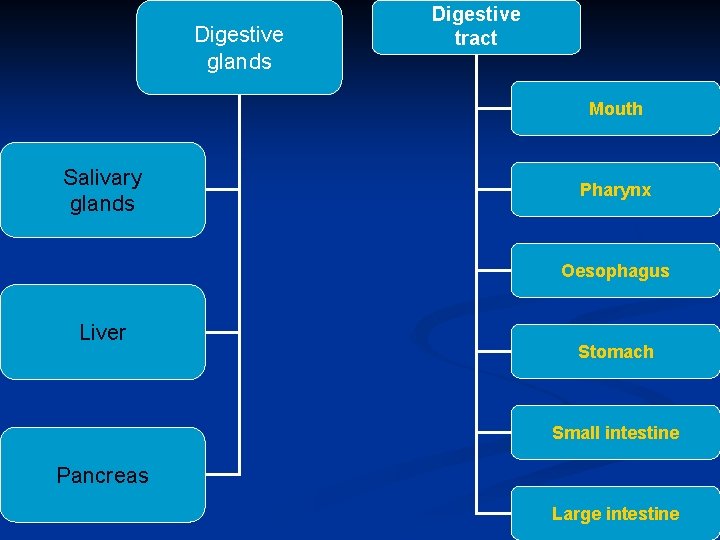
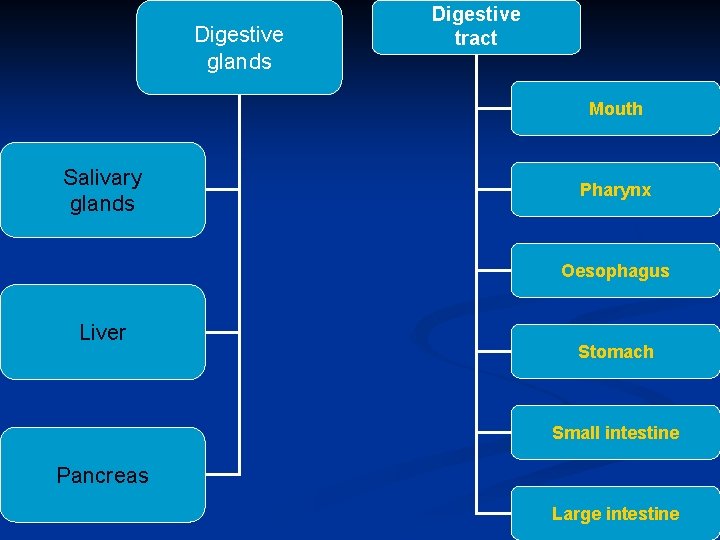
Digestive glands Digestive tract Mouth Salivary glands Pharynx Oesophagus Liver Stomach Small intestine Pancreas Large intestine
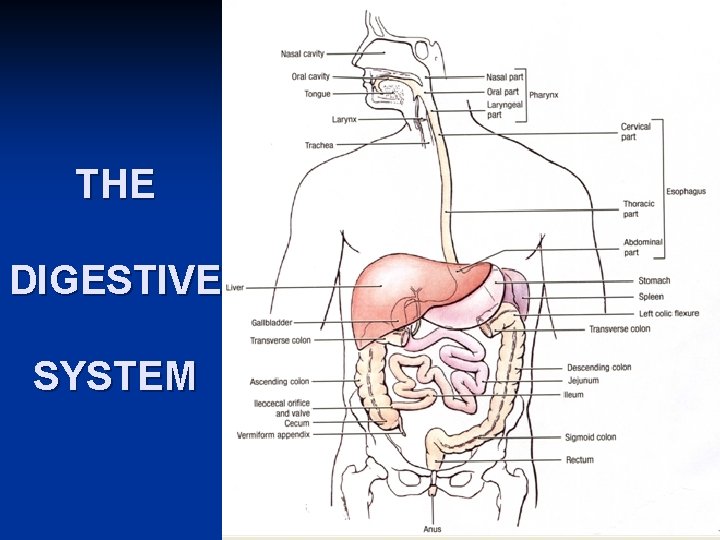
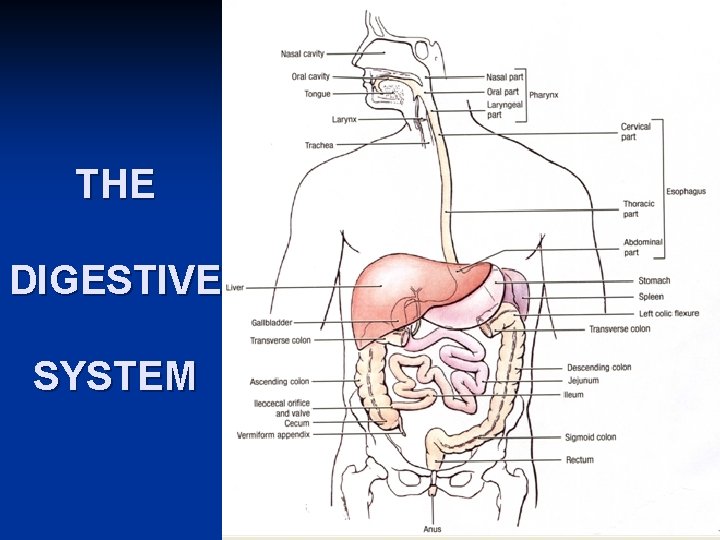
THE DIGESTIVE SYSTEM
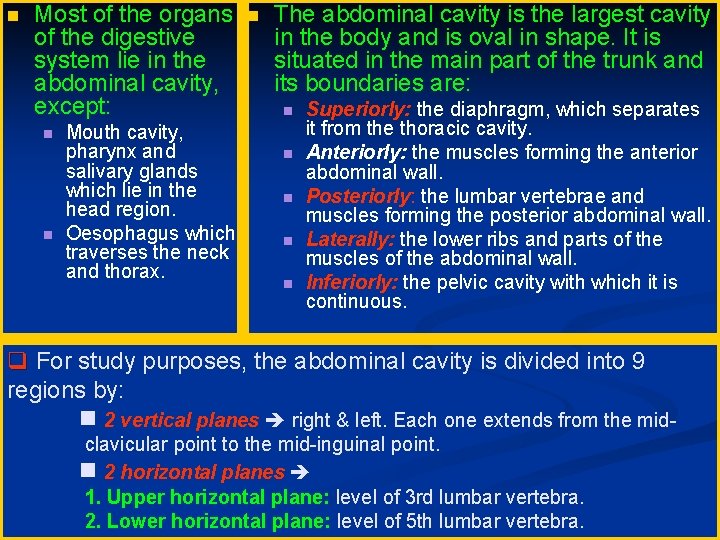
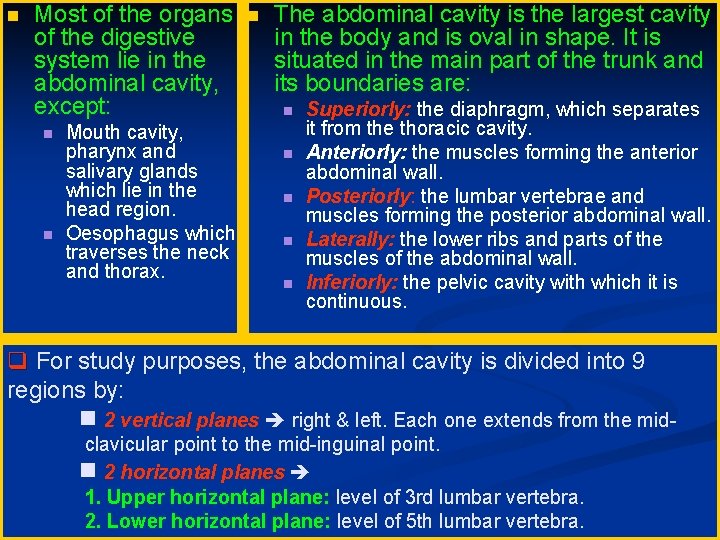
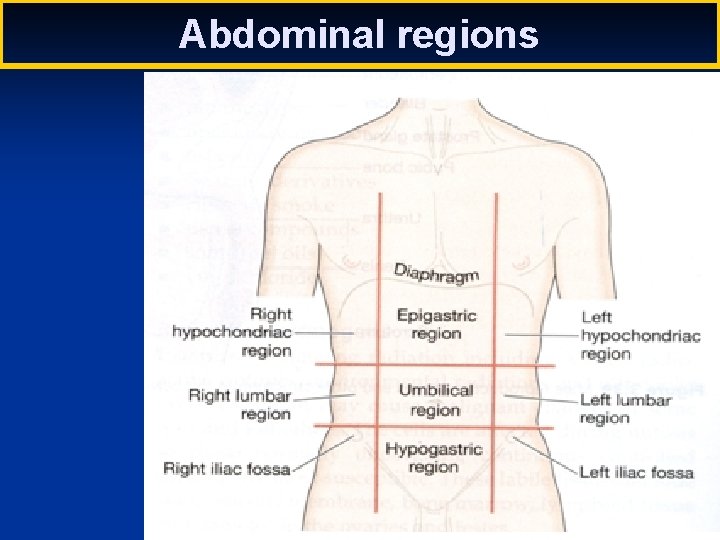
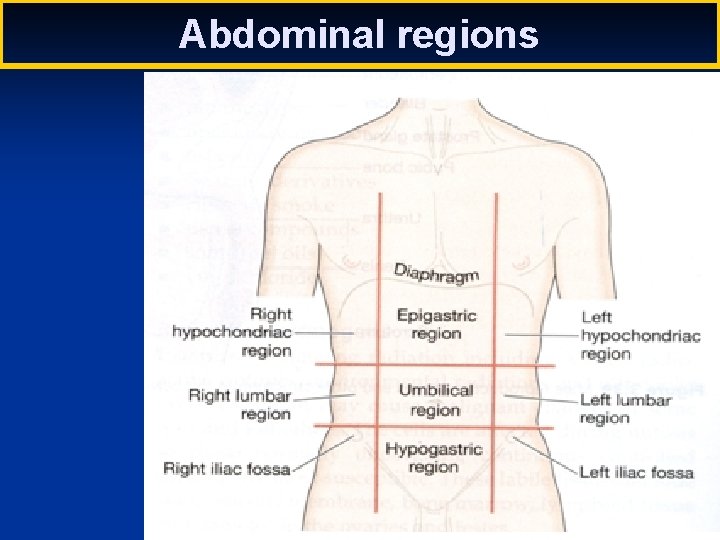
Most of the organs of the digestive system lie in the abdominal cavity, except: Mouth cavity, pharynx and salivary glands which lie in the head region. Oesophagus which traverses the neck and thorax. The abdominal cavity is the largest cavity in the body and is oval in shape. It is situated in the main part of the trunk and its boundaries are: Superiorly: the diaphragm, which separates it from the thoracic cavity. Anteriorly: the muscles forming the anterior abdominal wall. Posteriorly: the lumbar vertebrae and muscles forming the posterior abdominal wall. Laterally: the lower ribs and parts of the muscles of the abdominal wall. Inferiorly: the pelvic cavity with which it is continuous. q For study purposes, the abdominal cavity is divided into 9 regions by: 2 vertical planes right & left. Each one extends from the midclavicular point to the mid-inguinal point. 2 horizontal planes 1. Upper horizontal plane: level of 3 rd lumbar vertebra. 2. Lower horizontal plane: level of 5 th lumbar vertebra.
Abdominal regions
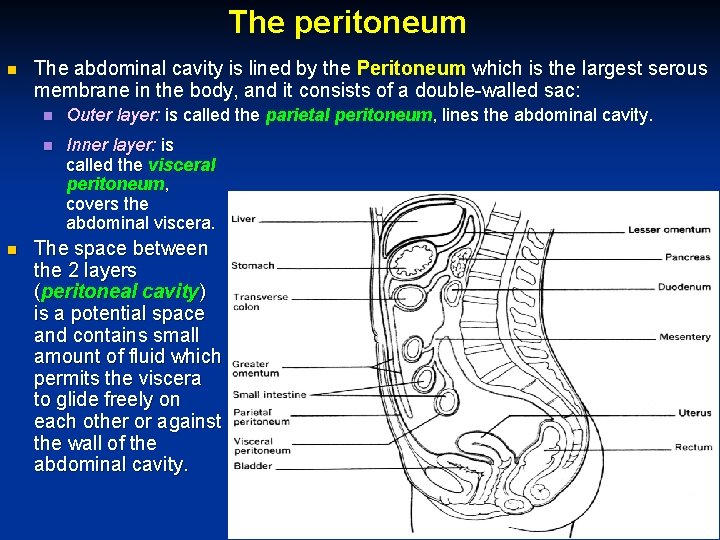
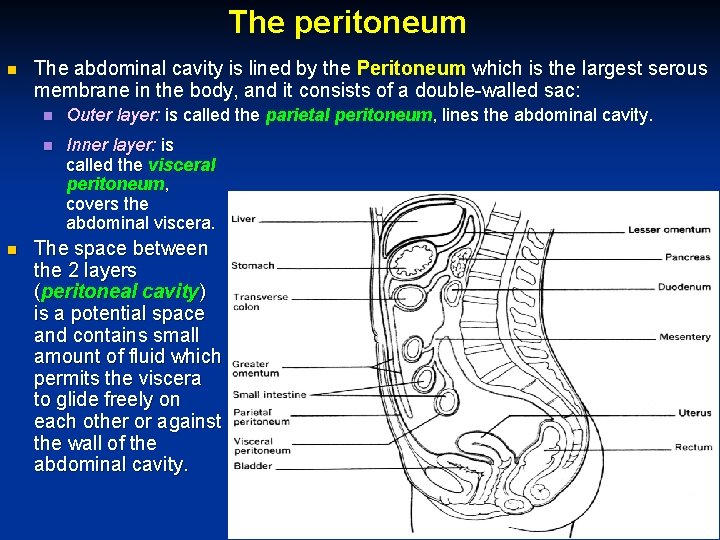
The peritoneum The abdominal cavity is lined by the Peritoneum which is the largest serous membrane in the body, and it consists of a double-walled sac: Outer layer: is called the parietal peritoneum, lines the abdominal cavity. Inner layer: is called the visceral peritoneum, covers the abdominal viscera. The space between the 2 layers (peritoneal cavity) is a potential space and contains small amount of fluid which permits the viscera to glide freely on each other or against the wall of the abdominal cavity.
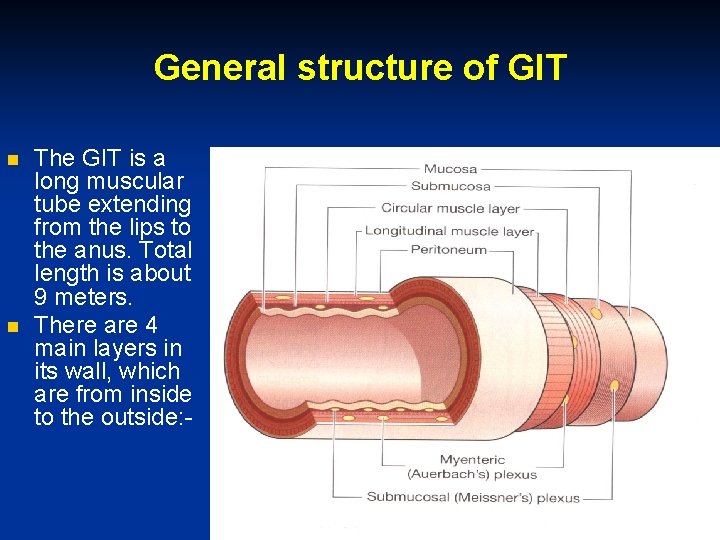
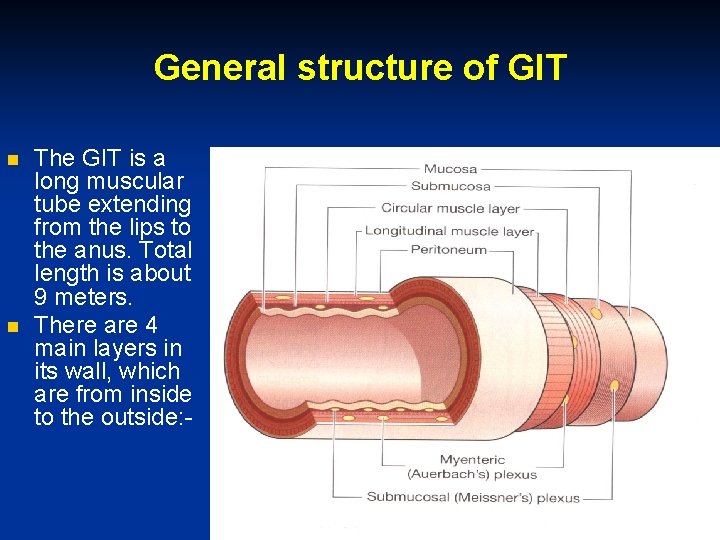
General structure of GIT The GIT is a long muscular tube extending from the lips to the anus. Total length is about 9 meters. There are 4 main layers in its wall, which are from inside to the outside: -
The mucosa or mucous membrane is the innermost layer. Its epithelium varies in structure according to the work being done in the part of the tube that it lines. For example, it is designed for protection (stratified squamous) in the mouth, the pharynx, the oesophagus, and the anal region, but from the stomach to anus, it is primarily designed for processes of secretion and absorption (simple columnar). In addition to two thin layers of smooth muscle tissue (muscularis mucosa), the mucosa contains many glands, blood vessels, and lymphatics. The submucosa connects the mucosa with the main muscular layer. It is composed of loose connective tissue and contains network of blood vessels. The musculosa (muscularis externa) is the third main layer of the wall of the digestive tube. The smooth muscle fibres are placed in two layers; inner circular and outer longitudinal. The external layer of the tube is fibrous above the diaphragm and serous below the diaphragm. The serous membrane below the diaphragm is called “serosa” or visceral peritoneum.
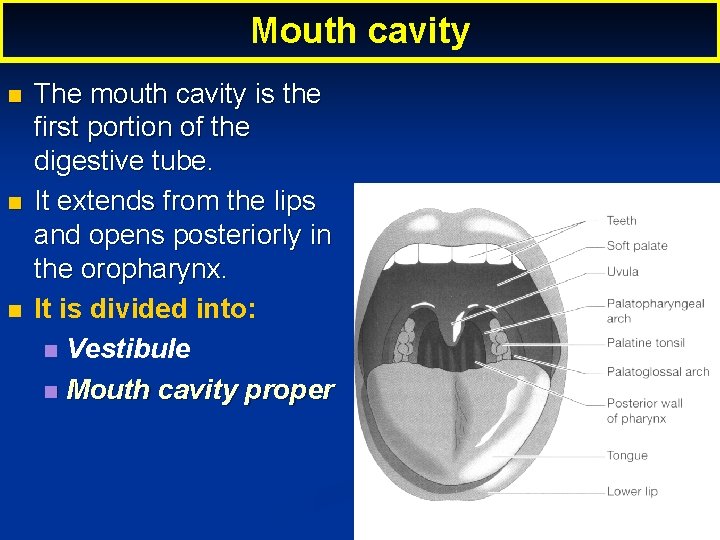
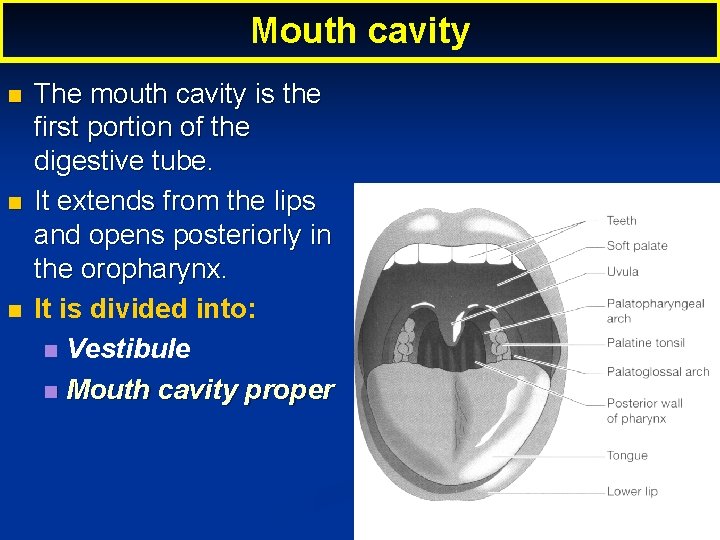
Mouth cavity The mouth cavity is the first portion of the digestive tube. It extends from the lips and opens posteriorly in the oropharynx. It is divided into: Vestibule Mouth cavity proper
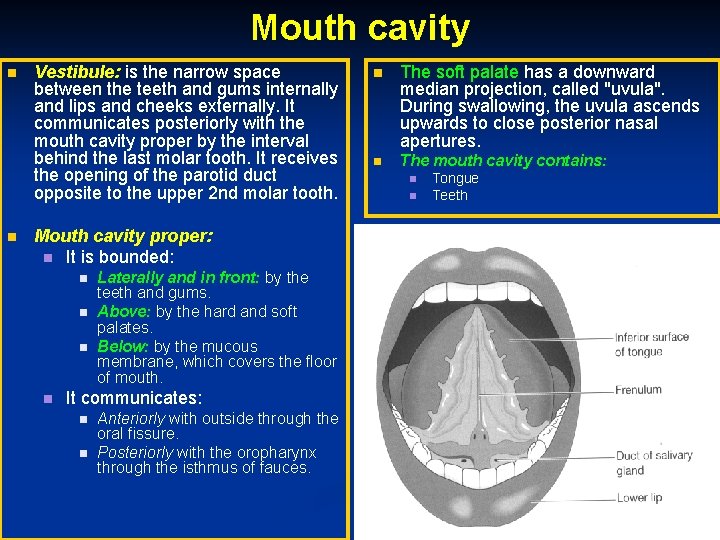
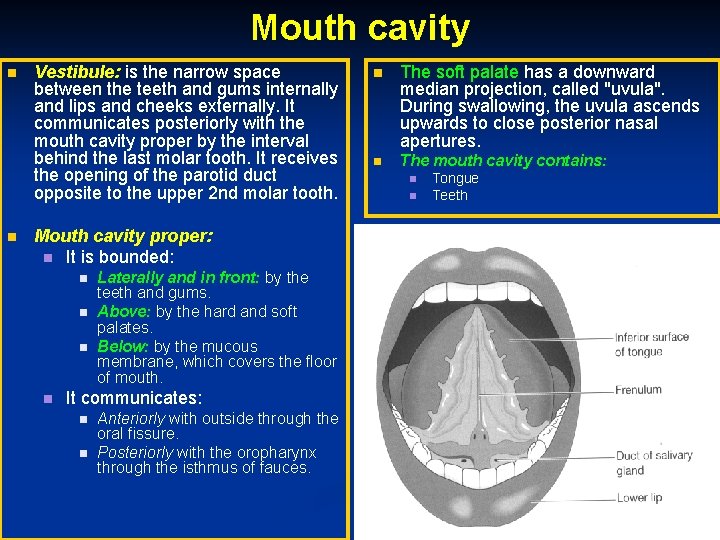
Mouth cavity Vestibule: is the narrow space between the teeth and gums internally and lips and cheeks externally. It communicates posteriorly with the mouth cavity proper by the interval behind the last molar tooth. It receives the opening of the parotid duct opposite to the upper 2 nd molar tooth. Mouth cavity proper: It is bounded: Laterally and in front: by the teeth and gums. Above: by the hard and soft palates. Below: by the mucous membrane, which covers the floor of mouth. It communicates: Anteriorly with outside through the oral fissure. Posteriorly with the oropharynx through the isthmus of fauces. The soft palate has a downward median projection, called "uvula". During swallowing, the uvula ascends upwards to close posterior nasal apertures. The mouth cavity contains: Tongue Teeth
Dorsal surface of tongue. Lingual papillae.
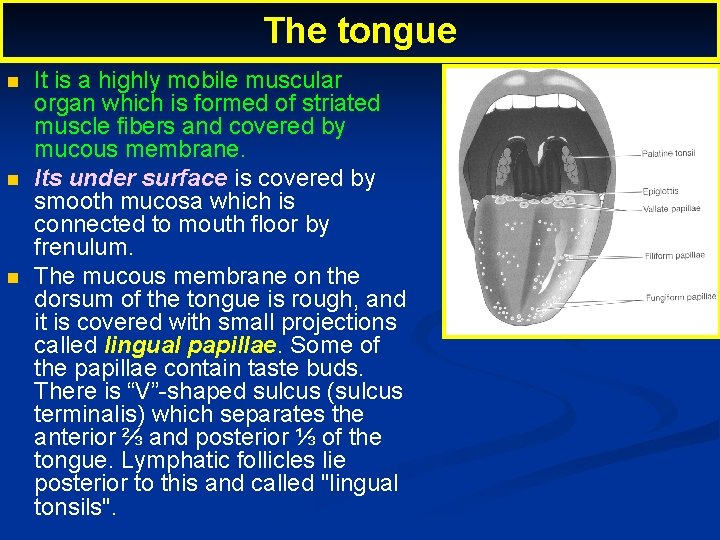
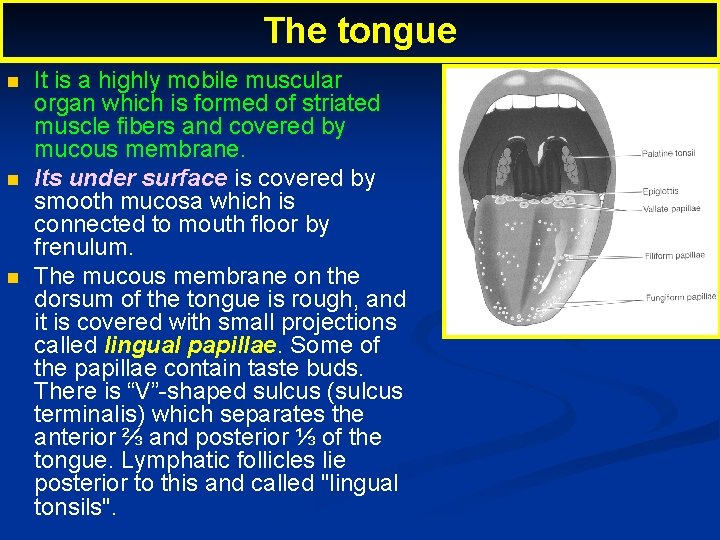
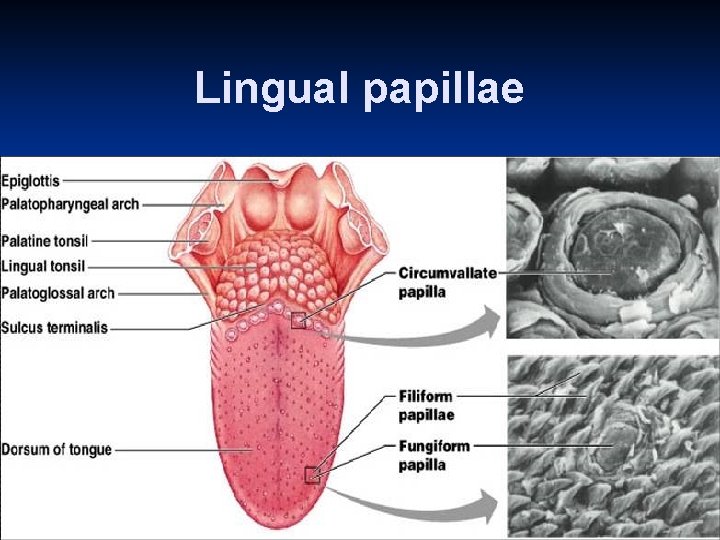
The tongue It is a highly mobile muscular organ which is formed of striated muscle fibers and covered by mucous membrane. Its under surface is covered by smooth mucosa which is connected to mouth floor by frenulum. The mucous membrane on the dorsum of the tongue is rough, and it is covered with small projections called lingual papillae. Some of the papillae contain taste buds. There is “V”-shaped sulcus (sulcus terminalis) which separates the anterior ⅔ and posterior ⅓ of the tongue. Lymphatic follicles lie posterior to this and called "lingual tonsils".
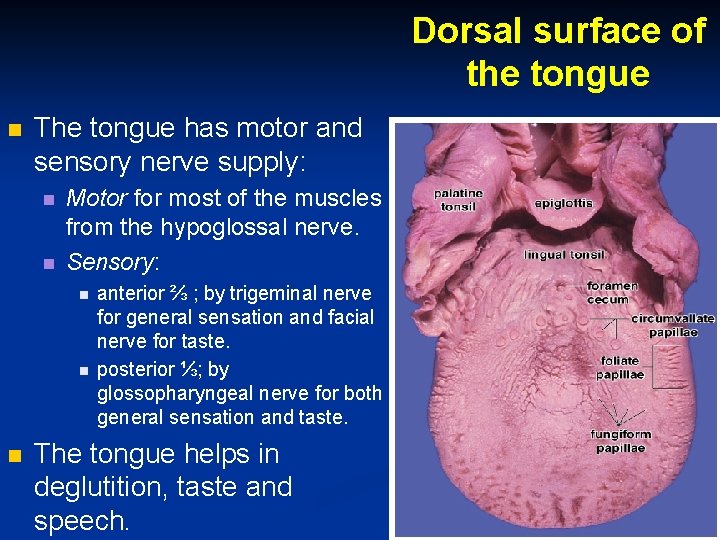
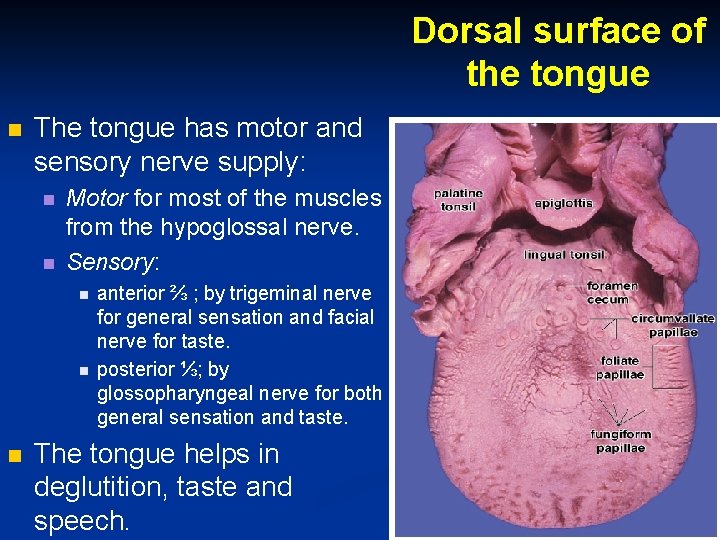
Dorsal surface of the tongue The tongue has motor and sensory nerve supply: Motor for most of the muscles from the hypoglossal nerve. Sensory: anterior ⅔ ; by trigeminal nerve for general sensation and facial nerve for taste. posterior ⅓; by glossopharyngeal nerve for both general sensation and taste. The tongue helps in deglutition, taste and speech.
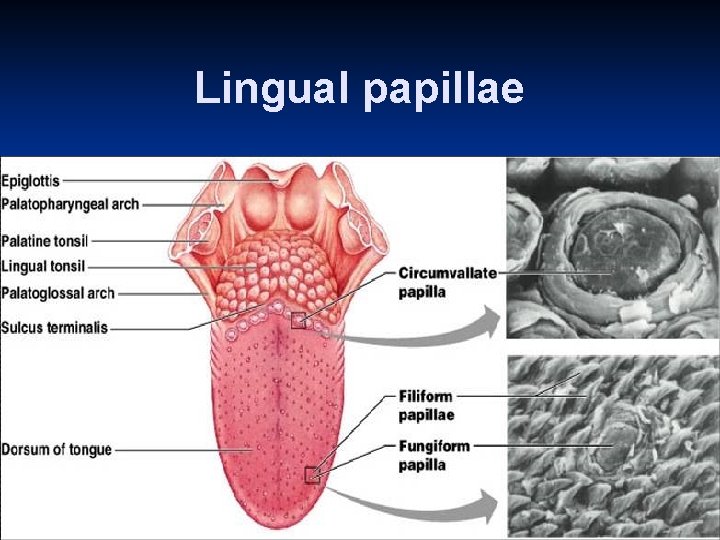
Lingual papillae
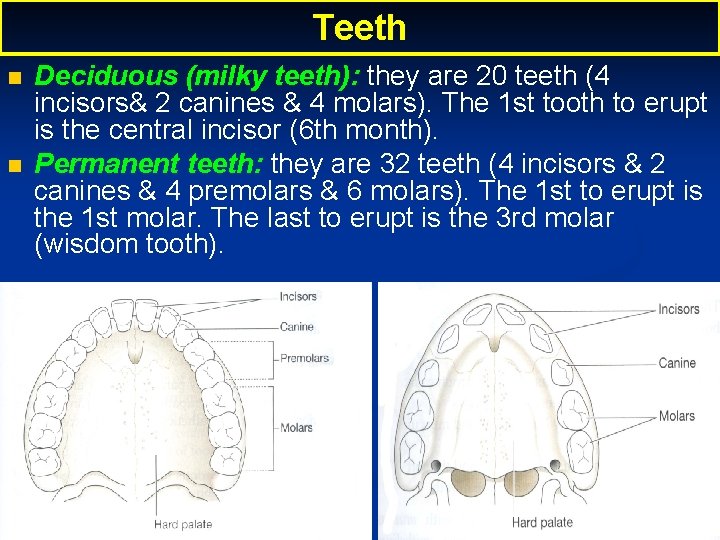
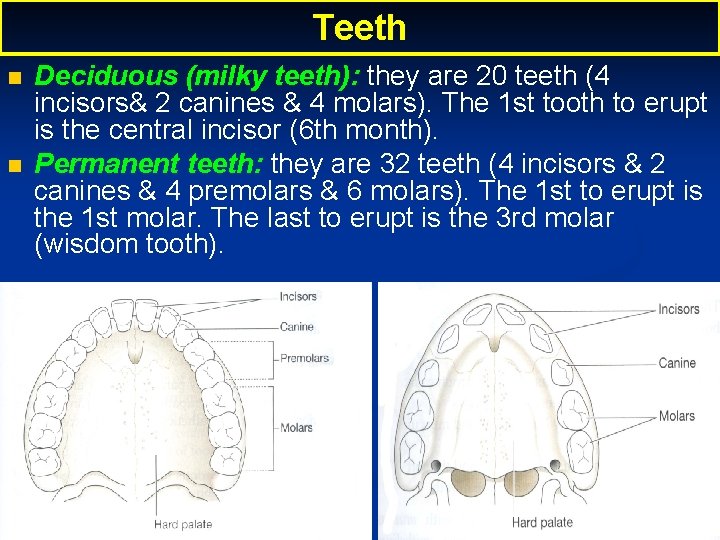
Teeth Deciduous (milky teeth): they are 20 teeth (4 incisors& 2 canines & 4 molars). The 1 st tooth to erupt is the central incisor (6 th month). Permanent teeth: they are 32 teeth (4 incisors & 2 canines & 4 premolars & 6 molars). The 1 st to erupt is the 1 st molar. The last to erupt is the 3 rd molar (wisdom tooth).
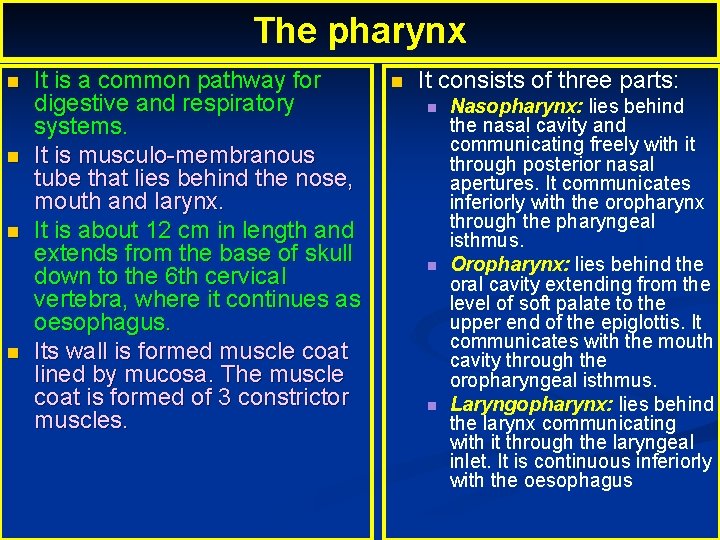
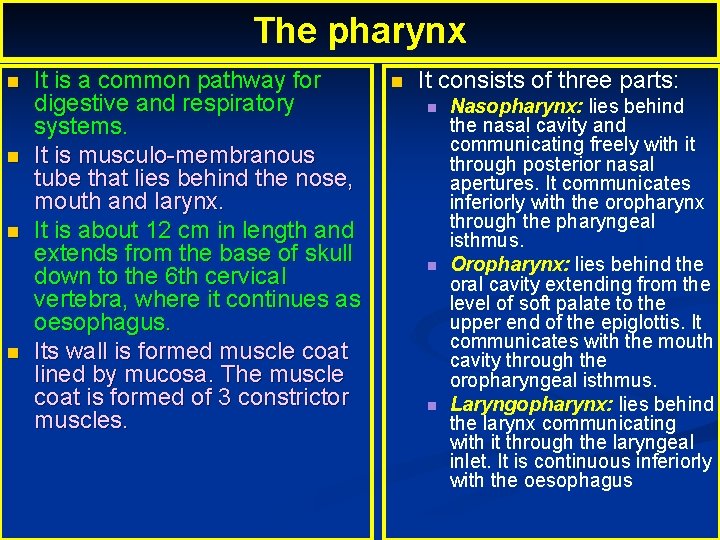
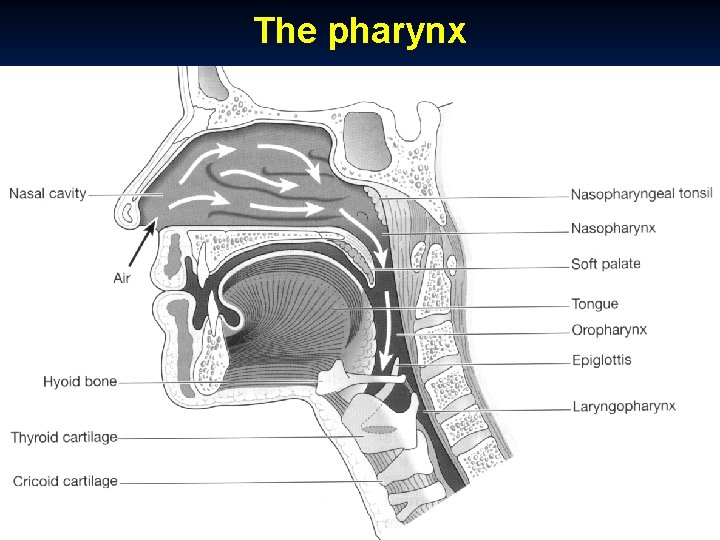
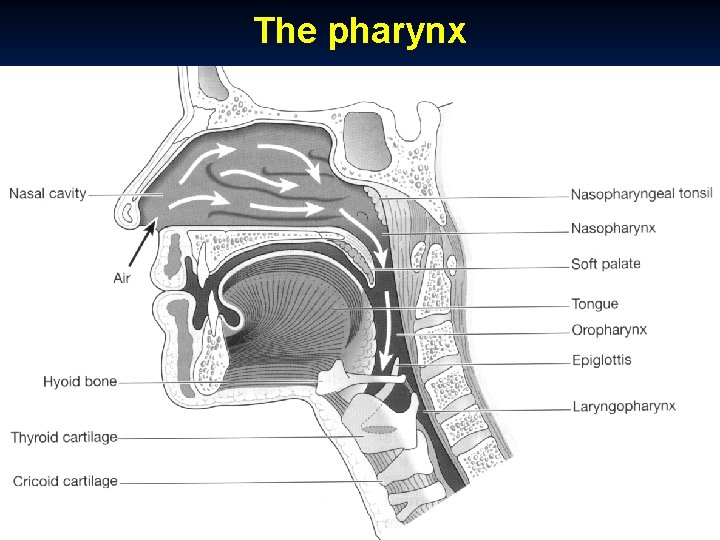
The pharynx It is a common pathway for digestive and respiratory systems. It is musculo-membranous tube that lies behind the nose, mouth and larynx. It is about 12 cm in length and extends from the base of skull down to the 6 th cervical vertebra, where it continues as oesophagus. Its wall is formed muscle coat lined by mucosa. The muscle coat is formed of 3 constrictor muscles. It consists of three parts: Nasopharynx: lies behind the nasal cavity and communicating freely with it through posterior nasal apertures. It communicates inferiorly with the oropharynx through the pharyngeal isthmus. Oropharynx: lies behind the oral cavity extending from the level of soft palate to the upper end of the epiglottis. It communicates with the mouth cavity through the oropharyngeal isthmus. Laryngopharynx: lies behind the larynx communicating with it through the laryngeal inlet. It is continuous inferiorly with the oesophagus
The pharynx
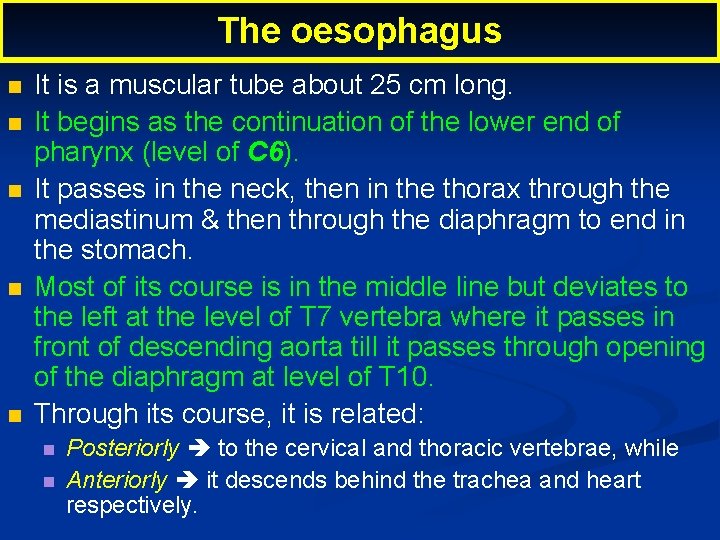
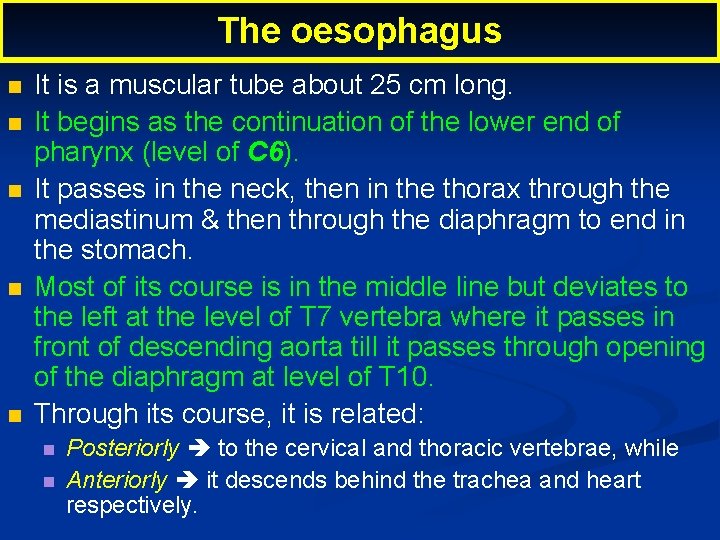
The oesophagus It is a muscular tube about 25 cm long. It begins as the continuation of the lower end of pharynx (level of C 6). It passes in the neck, then in the thorax through the mediastinum & then through the diaphragm to end in the stomach. Most of its course is in the middle line but deviates to the left at the level of T 7 vertebra where it passes in front of descending aorta till it passes through opening of the diaphragm at level of T 10. Through its course, it is related: Posteriorly to the cervical and thoracic vertebrae, while Anteriorly it descends behind the trachea and heart respectively.
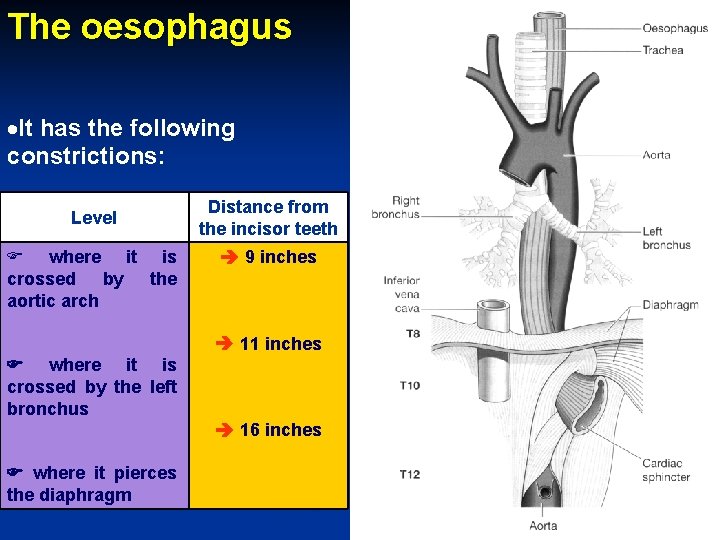
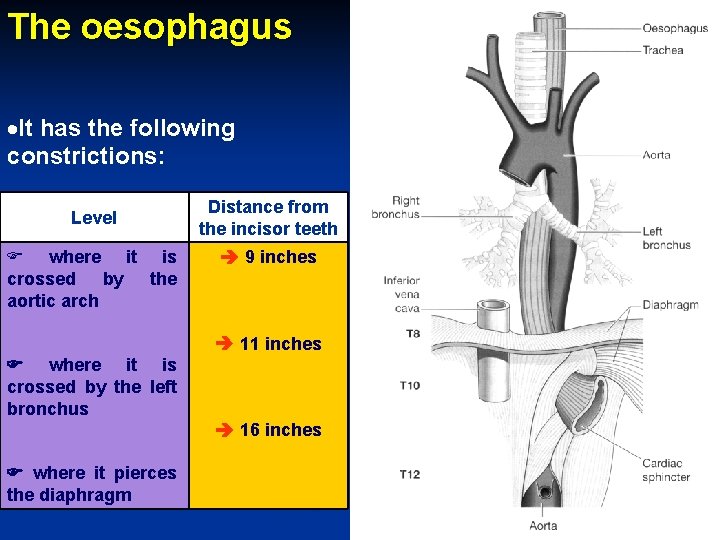
The oesophagus It has the following constrictions: Level where it is crossed by the aortic arch Distance from the incisor teeth 9 inches 11 inches where it is crossed by the left bronchus 16 inches where it pierces the diaphragm
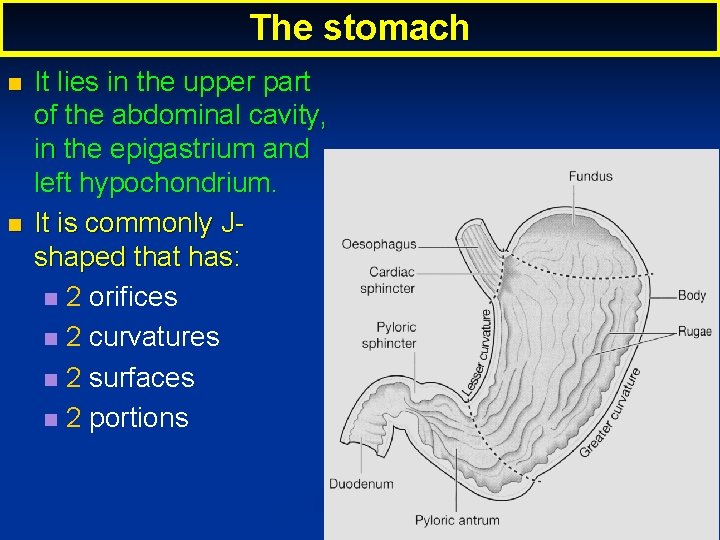
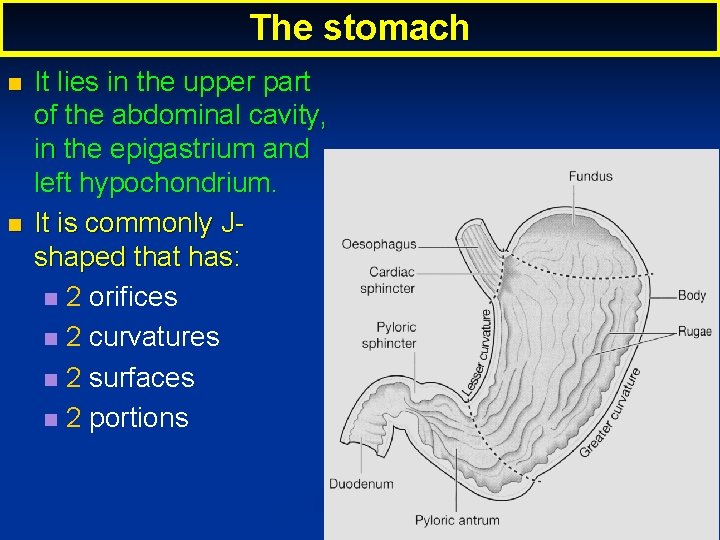
The stomach It lies in the upper part of the abdominal cavity, in the epigastrium and left hypochondrium. It is commonly Jshaped that has: 2 orifices 2 curvatures 2 surfaces 2 portions
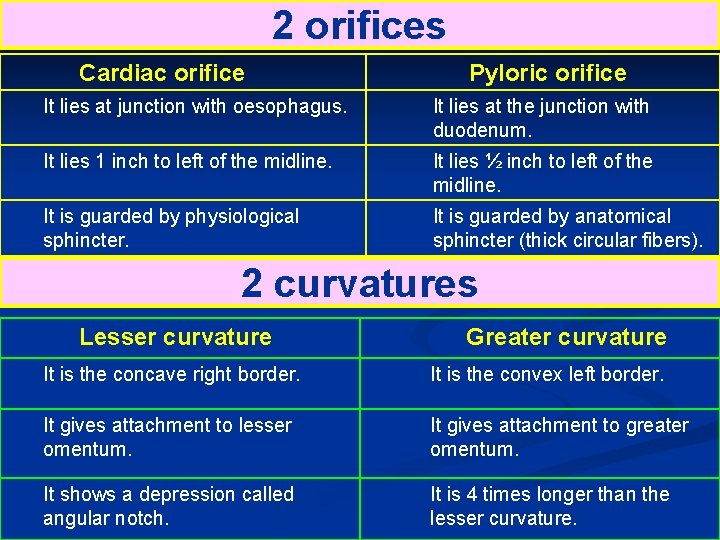
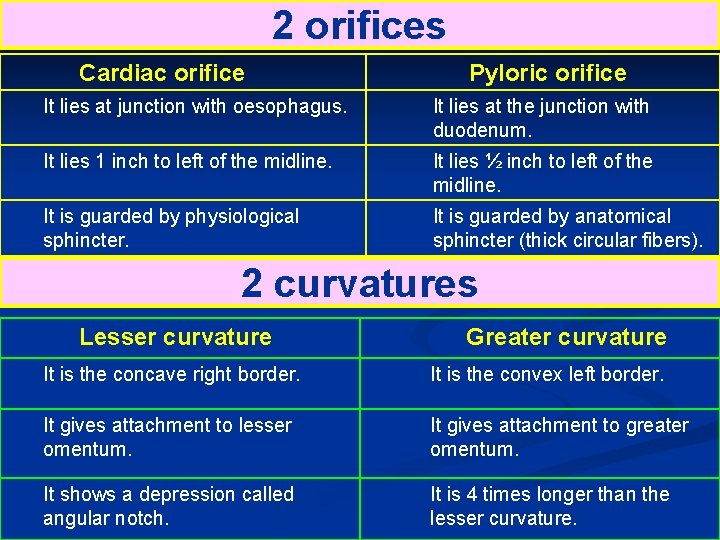
2 orifices Cardiac orifice Pyloric orifice It lies at junction with oesophagus. It lies at the junction with duodenum. It lies 1 inch to left of the midline. It lies ½ inch to left of the midline. It is guarded by physiological sphincter. It is guarded by anatomical sphincter (thick circular fibers). 2 curvatures Lesser curvature Greater curvature It is the concave right border. It is the convex left border. It gives attachment to lesser omentum. It gives attachment to greater omentum. It shows a depression called angular notch. It is 4 times longer than the lesser curvature.
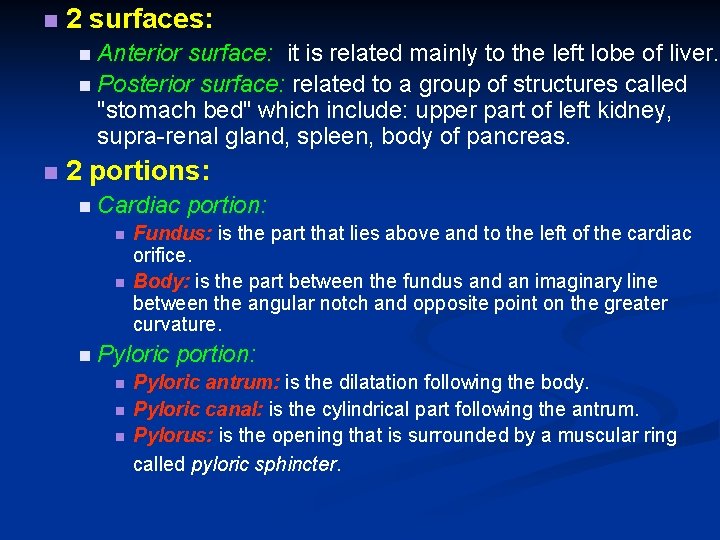
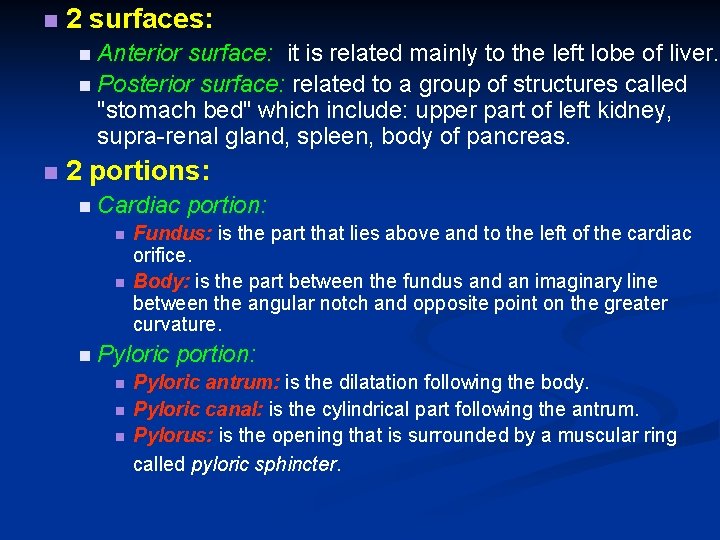
2 surfaces: Anterior surface: it is related mainly to the left lobe of liver. Posterior surface: related to a group of structures called "stomach bed" which include: upper part of left kidney, supra-renal gland, spleen, body of pancreas. 2 portions: Cardiac Fundus: is the part that lies above and to the left of the cardiac orifice. Body: is the part between the fundus and an imaginary line between the angular notch and opposite point on the greater curvature. Pyloric portion: Pyloric antrum: is the dilatation following the body. Pyloric canal: is the cylindrical part following the antrum. Pylorus: is the opening that is surrounded by a muscular ring called pyloric sphincter.

The Small Intestine It is 6 meters long and takes the shape of coiled loops that fill most of the abdominal cavity. It consists of 3 divisions: Duodenum: It is the shortest and widest of the small intestine (about 25 cm in length). It is “C” shaped and is formed of 4 parts. It is firmly attached to the posterior abdominal wall and not mobile. The head of pancreas lies in the “C” shaped concavity. The bile duct and main pancreatic duct unit together and open in the middle of the 2 nd part. NB: cancer head of pancreas leads to obstructive jaundice and intestinal obstruction
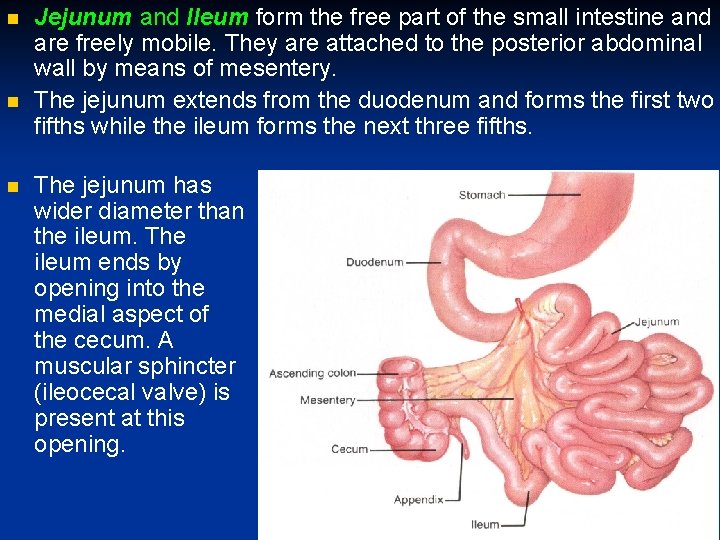
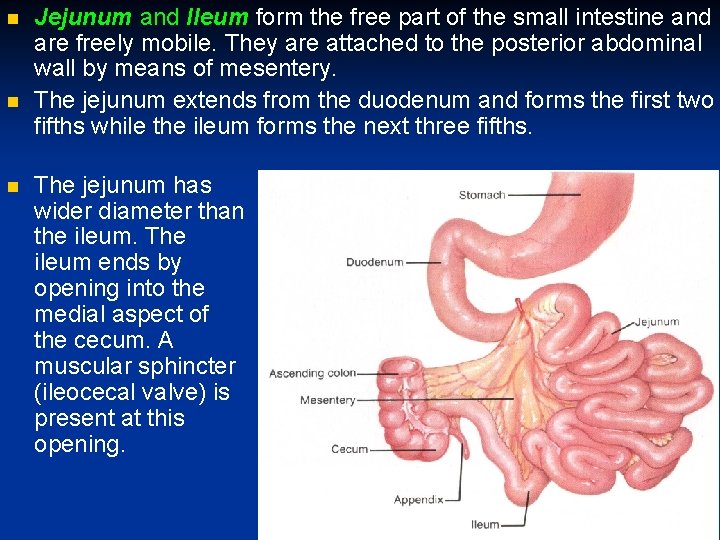
Jejunum and Ileum form the free part of the small intestine and are freely mobile. They are attached to the posterior abdominal wall by means of mesentery. The jejunum extends from the duodenum and forms the first two fifths while the ileum forms the next three fifths. The jejunum has wider diameter than the ileum. The ileum ends by opening into the medial aspect of the cecum. A muscular sphincter (ileocecal valve) is present at this opening.
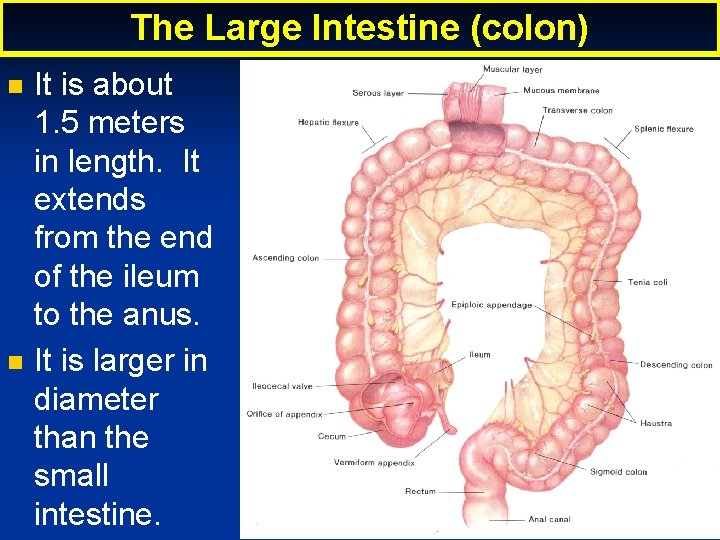
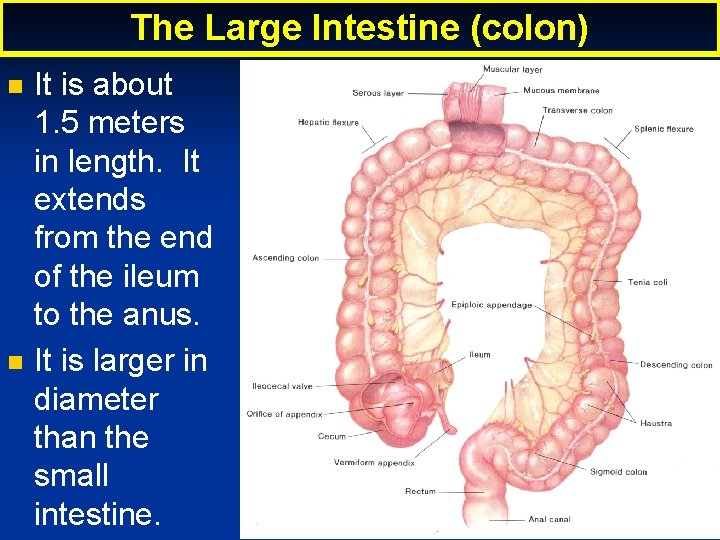
The Large Intestine (colon) It is about 1. 5 meters in length. It extends from the end of the ileum to the anus. It is larger in diameter than the small intestine.
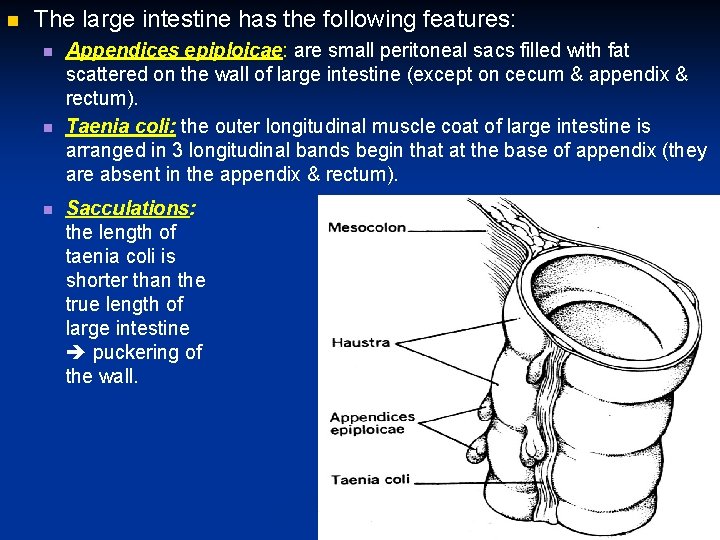
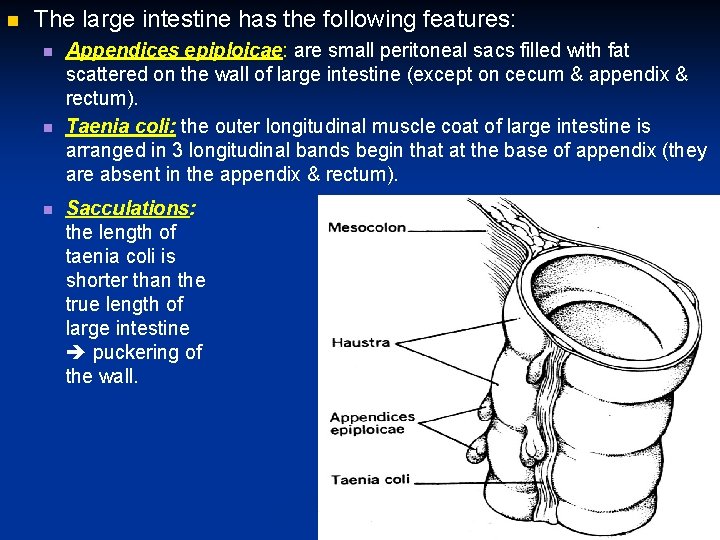
The large intestine has the following features: Appendices epiploicae: are small peritoneal sacs filled with fat scattered on the wall of large intestine (except on cecum & appendix & rectum). Taenia coli: the outer longitudinal muscle coat of large intestine is arranged in 3 longitudinal bands begin that at the base of appendix (they are absent in the appendix & rectum). Sacculations: the length of taenia coli is shorter than the true length of large intestine puckering of the wall.
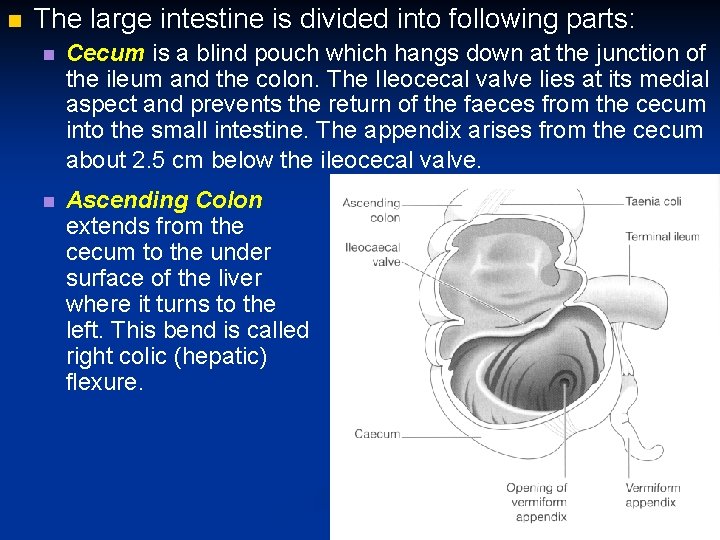
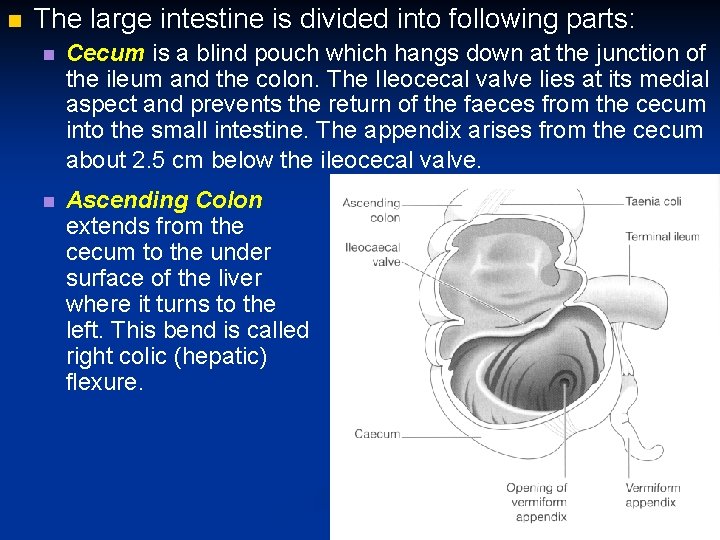
The large intestine is divided into following parts: Cecum is a blind pouch which hangs down at the junction of the ileum and the colon. The Ileocecal valve lies at its medial aspect and prevents the return of the faeces from the cecum into the small intestine. The appendix arises from the cecum about 2. 5 cm below the ileocecal valve. Ascending Colon extends from the cecum to the under surface of the liver where it turns to the left. This bend is called right colic (hepatic) flexure.
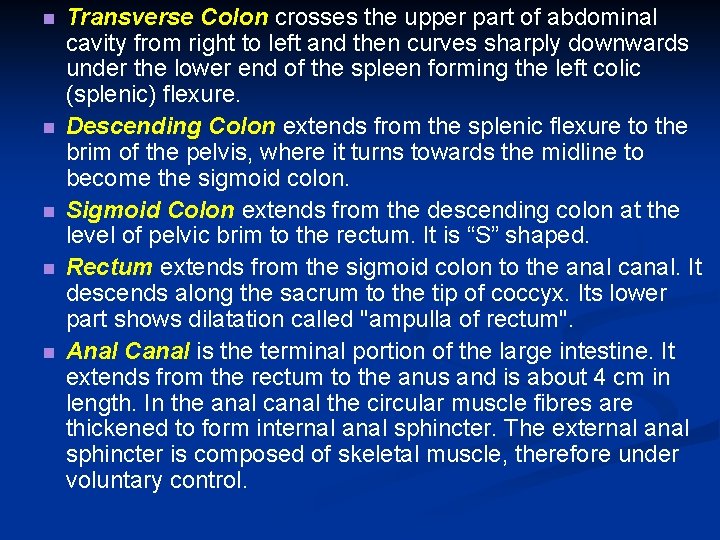
Transverse Colon crosses the upper part of abdominal cavity from right to left and then curves sharply downwards under the lower end of the spleen forming the left colic (splenic) flexure. Descending Colon extends from the splenic flexure to the brim of the pelvis, where it turns towards the midline to become the sigmoid colon. Sigmoid Colon extends from the descending colon at the level of pelvic brim to the rectum. It is “S” shaped. Rectum extends from the sigmoid colon to the anal canal. It descends along the sacrum to the tip of coccyx. Its lower part shows dilatation called "ampulla of rectum". Anal Canal is the terminal portion of the large intestine. It extends from the rectum to the anus and is about 4 cm in length. In the anal canal the circular muscle fibres are thickened to form internal anal sphincter. The external anal sphincter is composed of skeletal muscle, therefore under voluntary control.
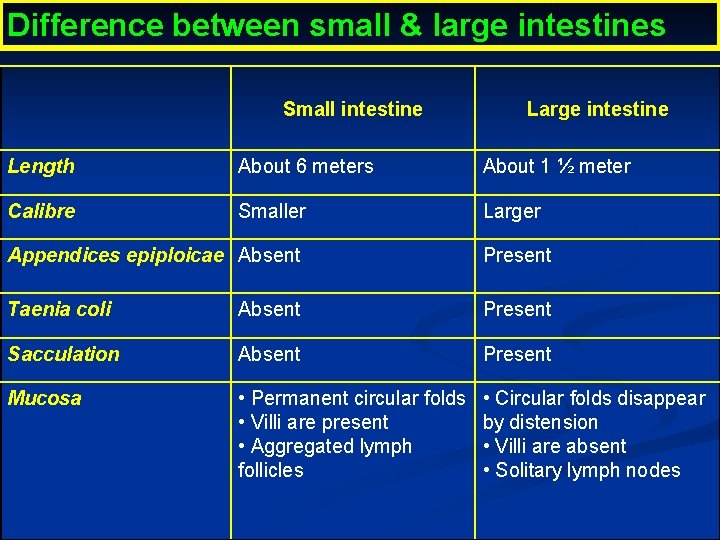
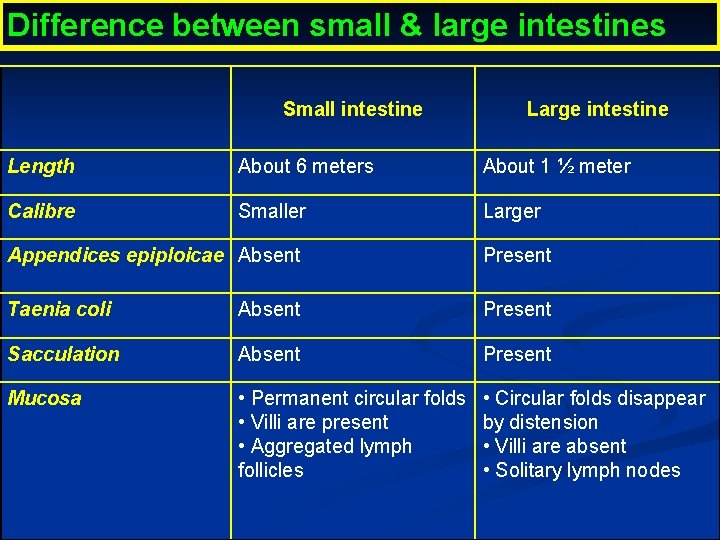
Difference between small & large intestines Small intestine Large intestine Length About 6 meters About 1 ½ meter Calibre Smaller Larger Appendices epiploicae Absent Present Taenia coli Absent Present Sacculation Absent Present Mucosa • Permanent circular folds • Villi are present • Aggregated lymph follicles • Circular folds disappear by distension • Villi are absent • Solitary lymph nodes