CARDIAC MONITORING l Electrocardiography EKG and phonocardiography are

- Slides: 80
CARDIAC MONITORING
l Electrocardiography (EKG) and phonocardiography are the two most important techniques for observing the condition of the heart and its associated arteries. • Since the electrical and the acoustic signals are generated by the same events, it makes sense to discuss both of them at the same time.
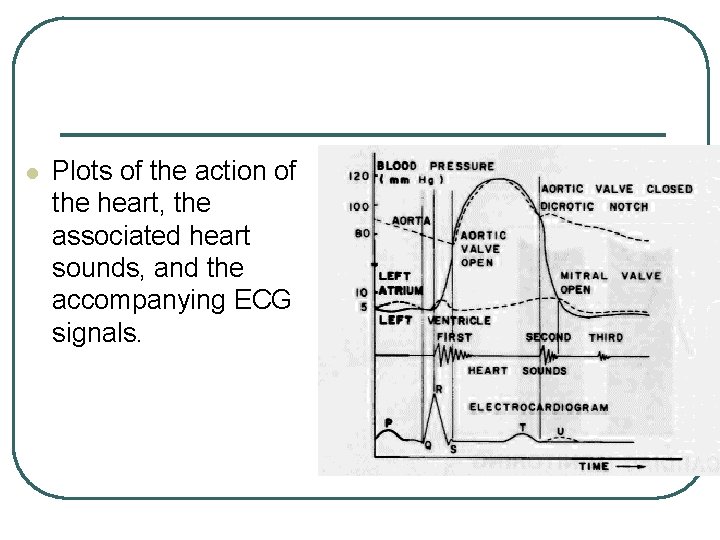
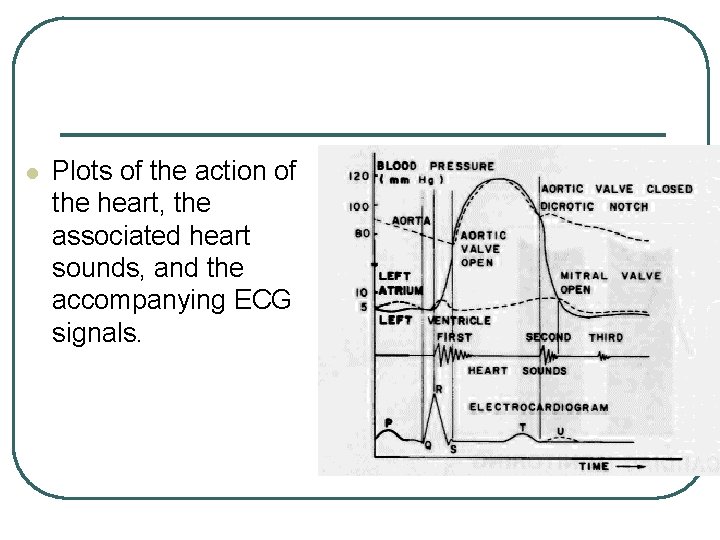
l Plots of the action of the heart, the associated heart sounds, and the accompanying ECG signals.
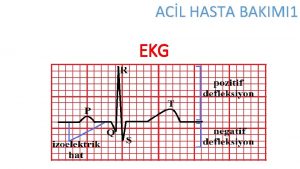
l l The P wave is associated with atrial contraction. The QRS complex signals the atrial repolarization and ventricular contraction sequence. The T wave is generated by the repolarization of the ventricles. The U wave is not completely understood, but it may be associated with some after-potential phenomenon.
l The R-wave frequency is normally taken as a measure of the heart rate. • The P-wave frequency should equal that of the R waves, and the P-to-R interval, which is normally about 0. 12 to 0. 22 second should not vary from beat to beat.
l The appearance of ectopic R waves or missing R waves is usually taken as a serious sign.
l The measurement and recording of acoustic signals associated with the action of the heart is known as phonocardiography. • Listening to the sounds of various phenomena inside the body is one of the oldest medical arts. • Today, the hearing of the nurse or physician may be aided by various electrical and electronic devices, and a graphic record can be obtained of the sounds heard on monitoring the heart.
PHONOCARDIOGRAPHIC TECHNIQUES l The acoustic signals that accompany the action of the heart can be detected with either a stethoscope or a microphone. • The use of a microphone provides some significant advantages in that the signals can be
l An electrocardiogram is a recording of the rhythmic electrical activity of the heart. • The abbreviation for electrocardiogram (EKG) is derived historically from the German spelling "electrokardiogram".
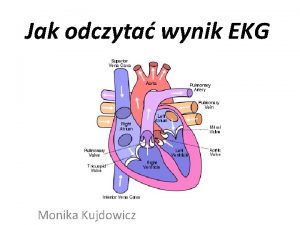
l The electrical activity of the heart is based on the ability of excitable tissue, such as heart muscle (myocardium), to change its membrane permeability to sodium (Na+) and potassium ions (K+). • When these ions move across the cell membrane, a changing electric field (dipole) results which is recorded as electrical activity of the heart.
l Metal electrodes in contact with the skin surface are used to pick up weak EKG signals that are amplified and displayed by an oscilloscope and/or Strip Chart Recorder. • Cardiac muscle goes from relaxed (diastole) to the contractile (systole) state after the onset of "electrical depolarization". • The return from contraction to relaxation occurs after "electrical repolarization".
l The normal heart rhythm is established by a specialized bundle of cells called the "pacemaker" or the sinoatrial (SA) node of the heart. • Electrical impulses are generated spontaneously by the pacemaker, initiating the heart cycle.
l At the onset of the heart cycle, impulses from the SA node induce the right atrium to depolarize. • This depolarization spreads across the atrial muscle causing atrial contraction, increasing atrial pressure and forcing blood into the ventricles.
l The ventricular contraction phase of the heart cycle is brought about by depolarization of the ventricles via the atrioventricular (AV) node, Bundle of His and the Purkinje fibers. • The AV node provides a delay time allowing the atria to pump blood into the ventricles before ventricular contraction.
l This Bundle of His and Purkinje fibers permit the ventricles to be depolarized in a relatively short time. • If the heart relied on impulse conduction through ventricular musculature, total contraction would not occur in a short interval due to long conduction delay of muscle. • Impulse velocity through the conduction system is much faster than through the cardiac muscle itself.

l The heart goes through a periodic sequence of electrical depolarizations and repolarizations that initiate the mechanical events of pumping blood. • Mechanically the heart cycle can be divided into two phases, diastole and systole. • During diastole the atria contract, emptying blood into the ventricles. • During systole the ventricles contract.
THE STANDARD ELECTROCARDIOGRAPHIC LEADS
l A complete EKG consists of 12 tracings, • The standard three leads (I, II, and III), • The precordial or chest lead (V 1 - V 6) and • The augmented unipolar limb leads (a. VR, a. VL and a. VF).
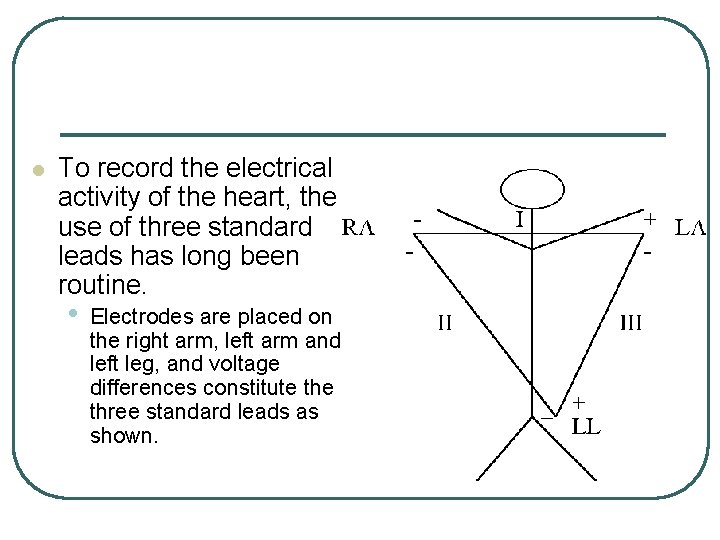
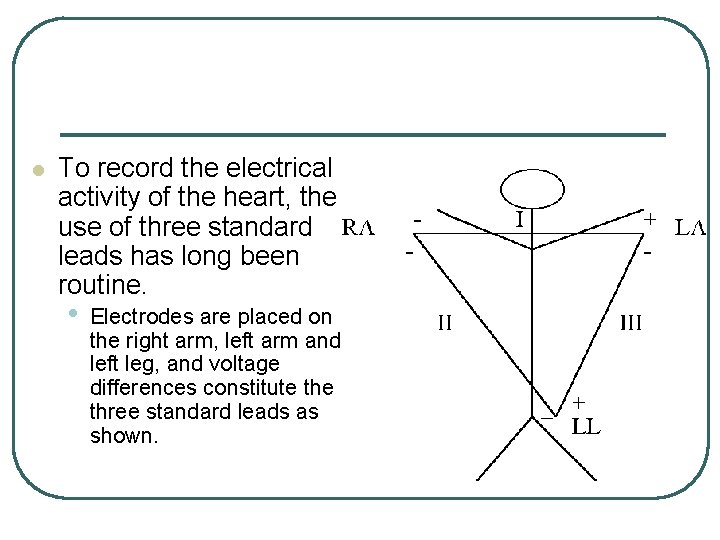
l To record the electrical activity of the heart, the use of three standard leads has long been routine. • Electrodes are placed on the right arm, left arm and left leg, and voltage differences constitute three standard leads as shown.
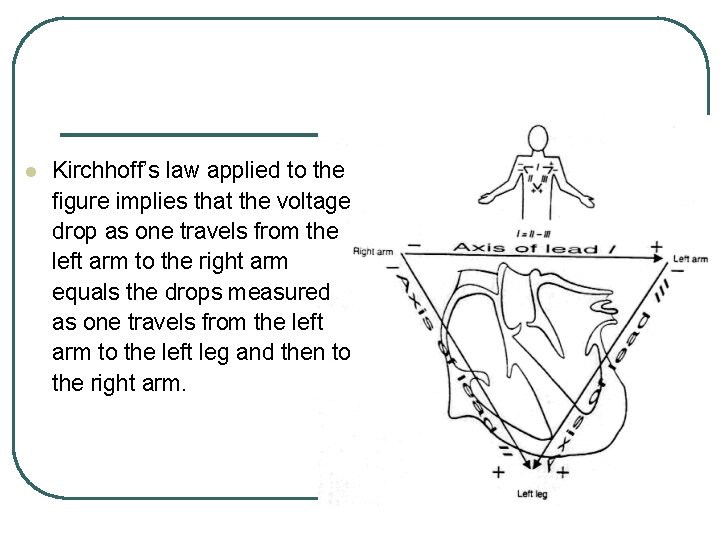
Einthoven Triangle l In summary, the three voltages I, II, and III are measured on the body as: • I—The voltage drop from left arm to right arm. • Il—The voltage drop from left leg to right arm. • Ill—The drop from left leg to left arm. • Anatomically, these points form a triangle on the body, known as the Einthoven triangle.
l The voltages may be represented by vectors, having the tail on the negative pole of the potential and the arrowhead on the positive pole of the potential.
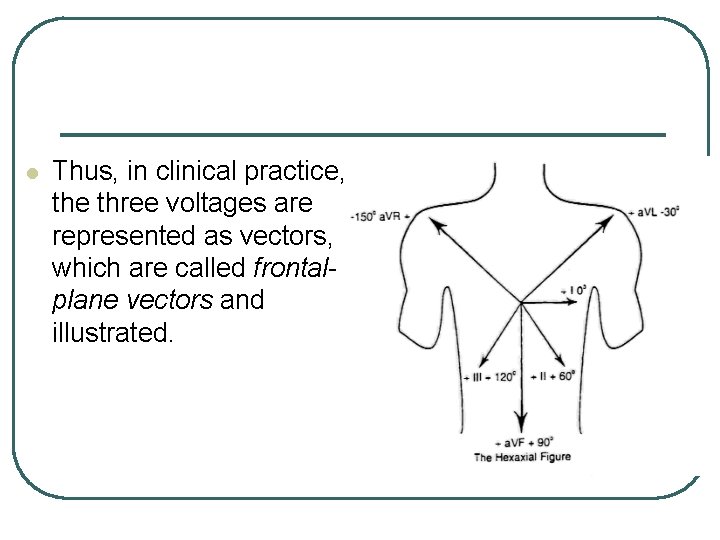
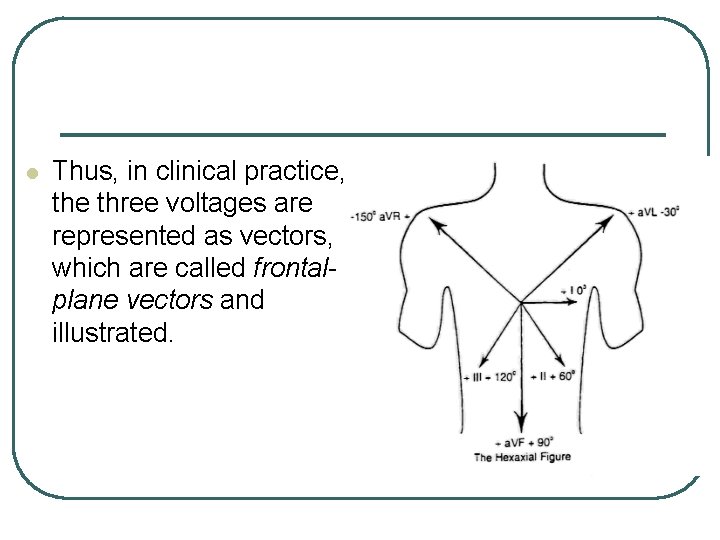
l Thus, in clinical practice, the three voltages are represented as vectors, which are called frontalplane vectors and illustrated.
l The algebraic relationship between these voltages comes from circuit theory applied to the human thorax. • It is the fundamental law of voltage drops that the voltage drop between two points is the same regardless of the path traveled between those two points. • This is known as Kirchhoff’s law of voltages.
LEAD I l In recording limb lead I, • The negative (-) terminal of the • • electrocardiograph is connected to the right arm (RA), The positive terminal (+) to the left arm (LA), and The ground (G) to the left leg (LL).
l Therefore, when the point on the chest where the right arm connects to the chest is electronegative with respect to the point where the left arm connects, the electrocardiograph records positively (i. e. above the zero voltage line in the electrocardiogram). • When the opposite is true, the electrocardiograph records below the line.
LEAD II l In recording limb lead II, • The negative terminal of the electro • • cardiograph is connected to the right arm (RA), The positive terminal to the left leg (LL), and Ground to the right leg (RL). • Thus, when the right arm is negative with respect to the left leg, the electrocardiograph records positively.
LEAD III l In recording limb lead III, • The negative terminal of the electro • • cardiograph is connected to the left arm The positive terminal to the left leg and Ground to the right leg. • This means that the electrocardiograph records positively when the left arm is negative with respect to the left leg.
l These three leads give electrocardiograms that show the same component waves, but the amplitude (height) and direction of the waves are different
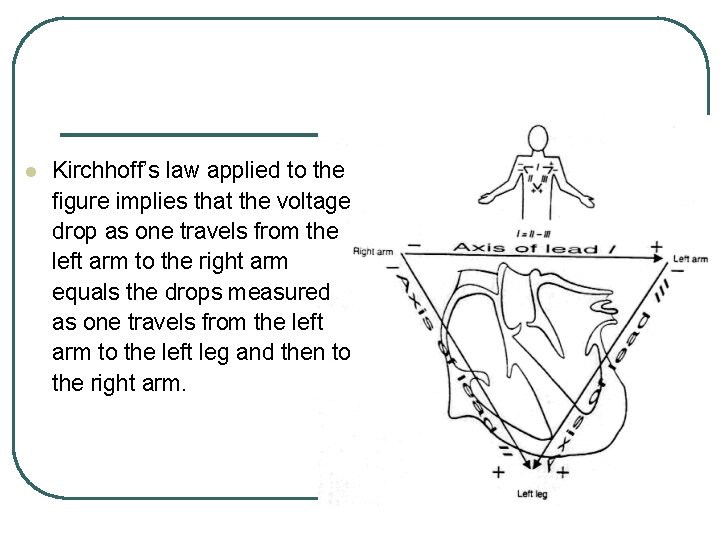
l Kirchhoff’s law applied to the figure implies that the voltage drop as one travels from the left arm to the right arm equals the drops measured as one travels from the left arm to the left leg and then to the right arm.
l In equation form, this implies that • The minus sign appears because III is a negative drop, in accordance with the polarities assigned in the figure. • The three voltages as arranged on the figure have traditionally been called Einthoven’s tnangle, in honor of Willem Einthoven, the physiologist and inventor, who studied ECG voltages in 1903.
l The equation means that only two leads are needed to gather all of the information available to the three leads. • This follows from the fact that, the voltage on any one of the leads can be calculated from the other two. • In other words, one of the leads is redundant.
l This is not wasteful, though, because if one of the leads is poorly connected, the information will still be available for diagnosis. • This is especially important in ECG units that do diagnosis automatically.
CHEST LEADS (PRECORDIAL LEADS)
l Often electrocardiograms are recorded with one electrode placed on the anterior aspect (front) of the chest over the heart.
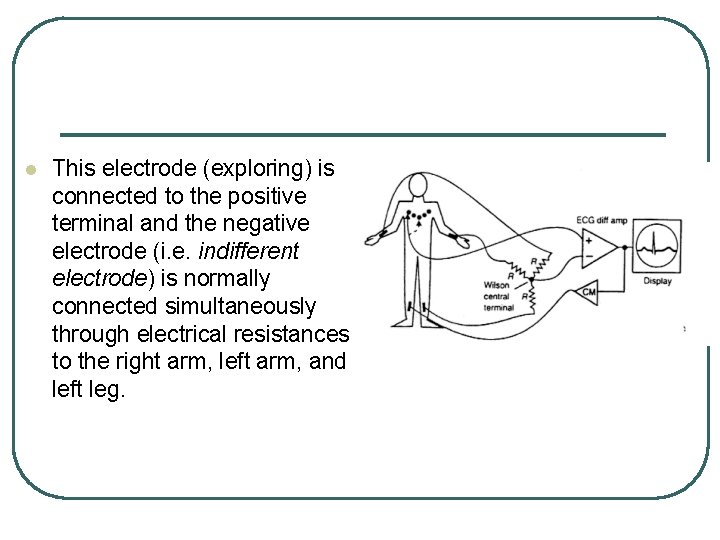
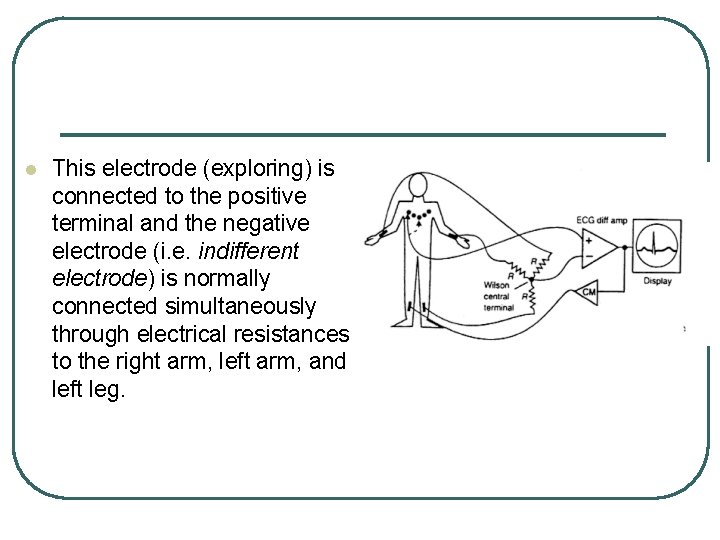
l This electrode (exploring) is connected to the positive terminal and the negative electrode (i. e. indifferent electrode) is normally connected simultaneously through electrical resistances to the right arm, left arm, and left leg.
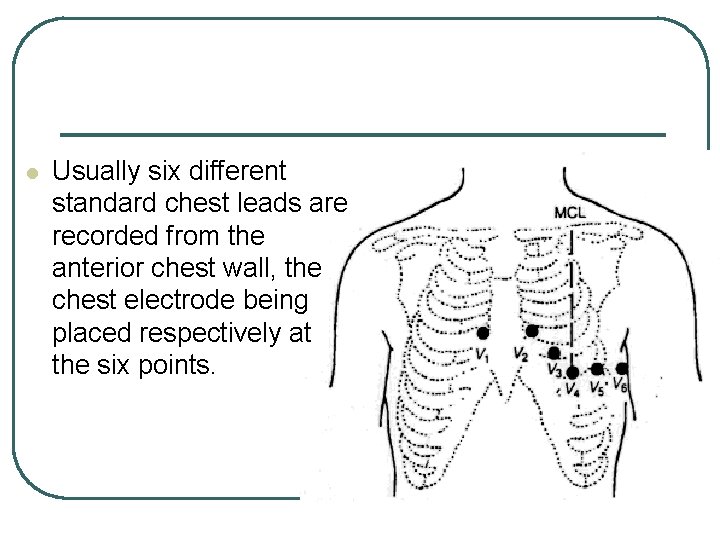
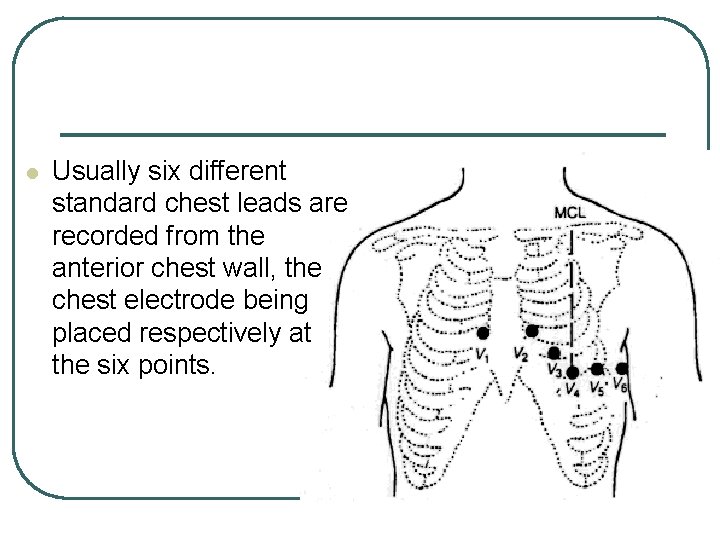
l Usually six different standard chest leads are recorded from the anterior chest wall, the chest electrode being placed respectively at the six points.
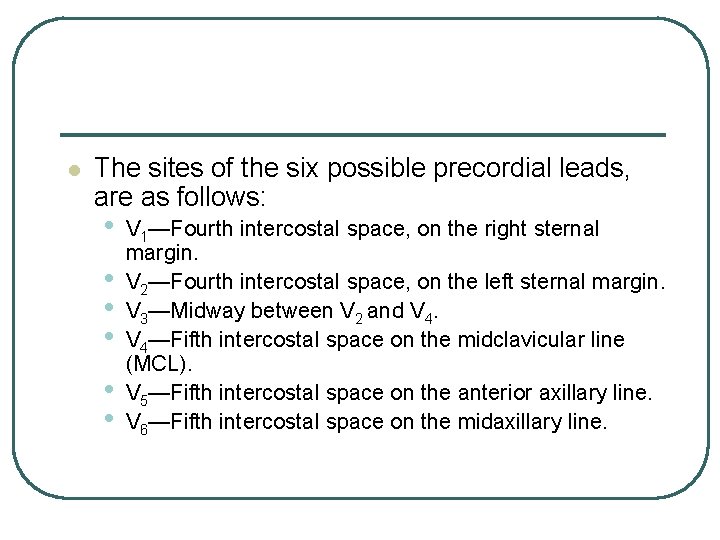
l The sites of the six possible precordial leads, are as follows: • • • V 1—Fourth intercostal space, on the right sternal margin. V 2—Fourth intercostal space, on the left sternal margin. V 3—Midway between V 2 and V 4—Fifth intercostal space on the midclavicular line (MCL). V 5—Fifth intercostal space on the anterior axillary line. V 6—Fifth intercostal space on the midaxillary line.
l The different leads recorded by the method are known as leads V 1, V 2, V 3, V 4, V 5, and V 6. • Because the heart surfaces are close to the chest wall, each chest lead records mainly the electrical potential of the cardiac musculature immediately beneath the electrode. • Therefore, relatively minute abnormalities in the ventricles, particularly in the anterior ventricular wall, frequently cause marked changes in the electrocardiograms recorded from chest leads.
l In leads V 1 and V 2, the QRS recordings of the normal heart are mainly negative because the chest electrode in these leads is nearer the base of the heart than the apex, which is the direction of electronegativity during most of the ventricular depolarization process. • On the other hand, the QRS complexes in leads V 4, V 5, and V 6 are mainly positive because the chest electrode in these leads is near the apex, which is the direction of electropositivity during depolarization.
AUGMENTED UNIPOLAR LIMB LEADS
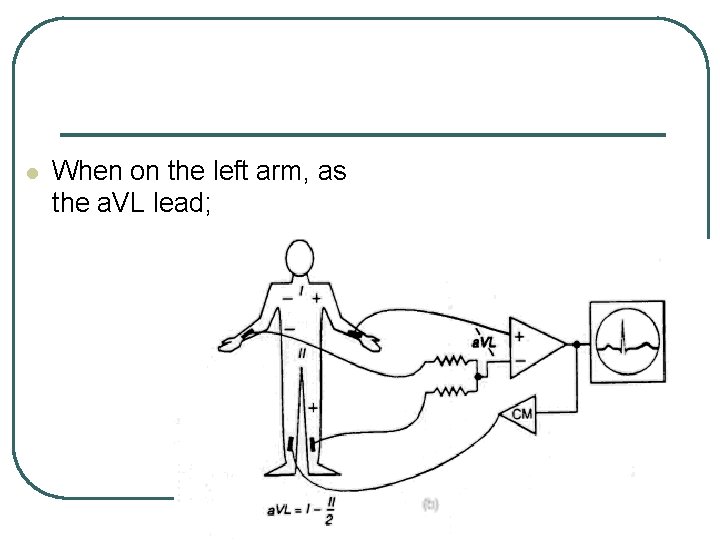
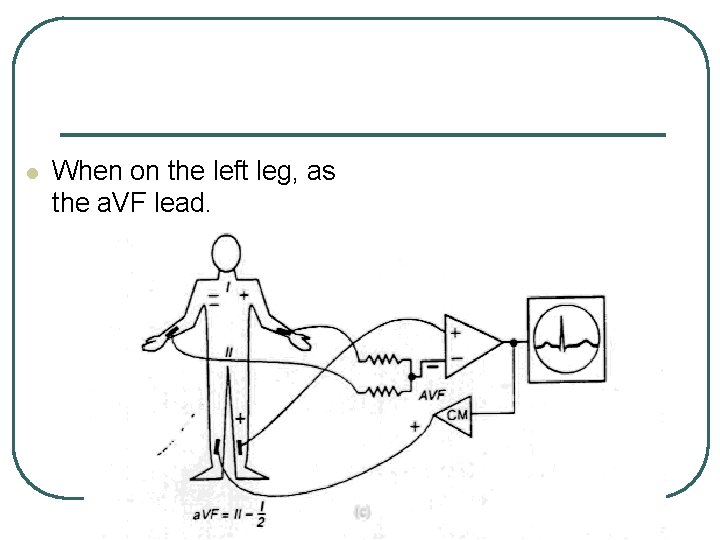
l Another system of leads in wide use is the "augmented unipolar limb lead". • In this type of recording, two of the limbs are connected through electrical resistance to the negative terminal of the electrocardiograph while third limb is connected to the positive terminal.
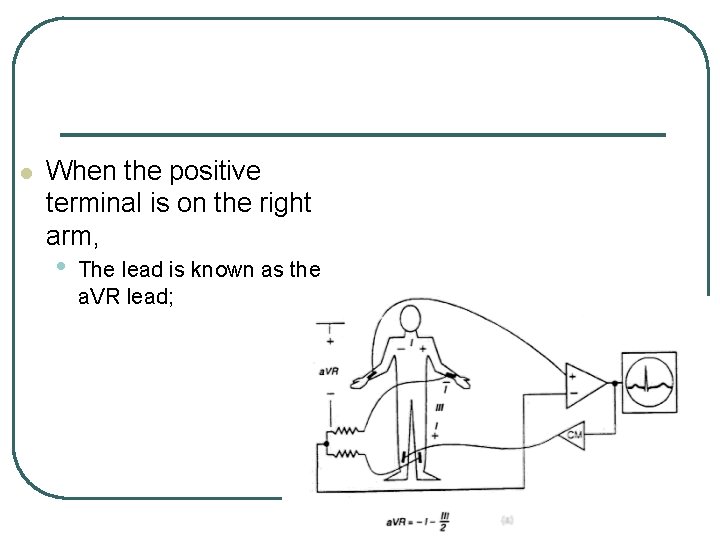
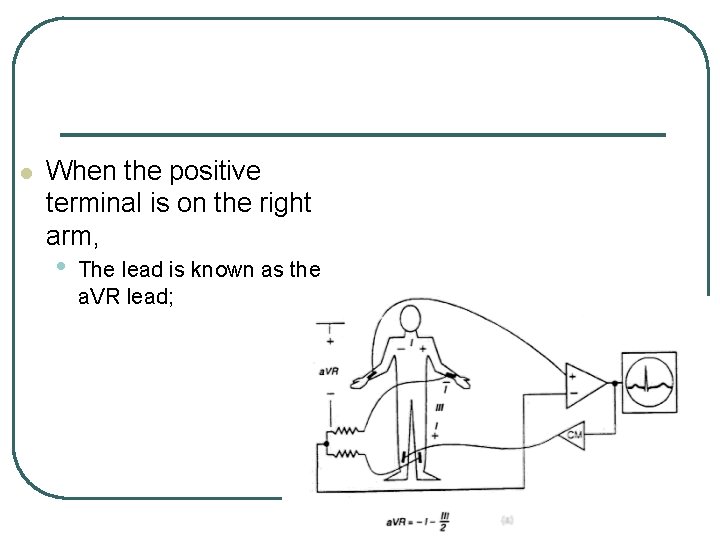
l When the positive terminal is on the right arm, • The lead is known as the a. VR lead;
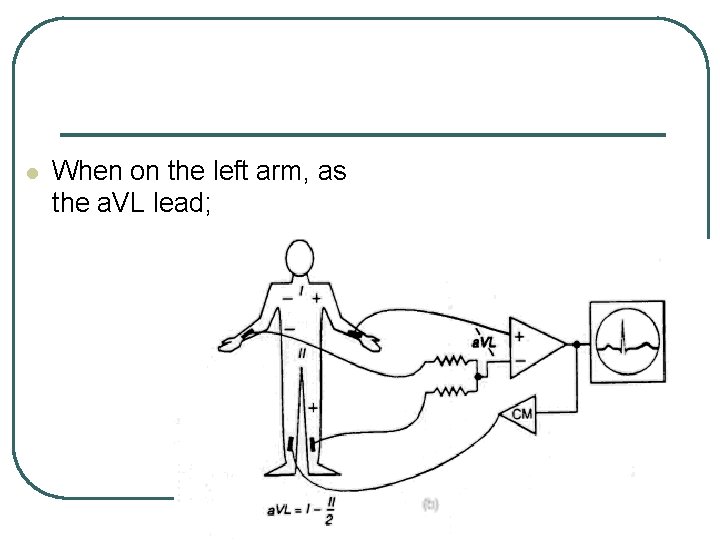
l When on the left arm, as the a. VL lead;
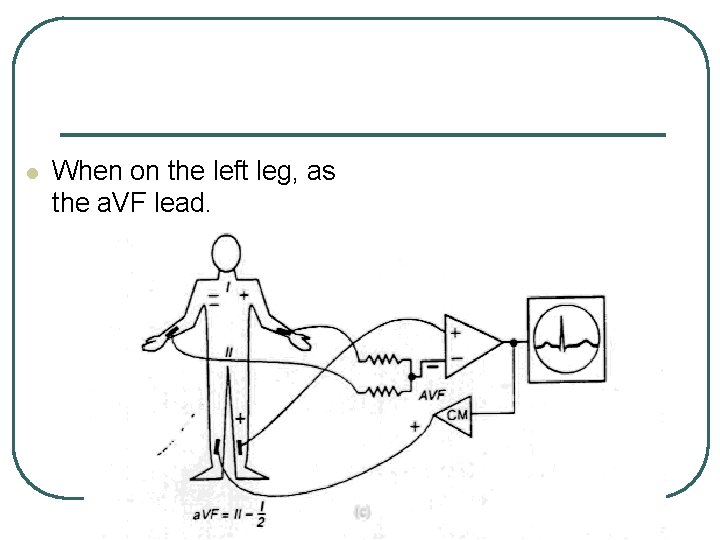
l When on the left leg, as the a. VF lead.
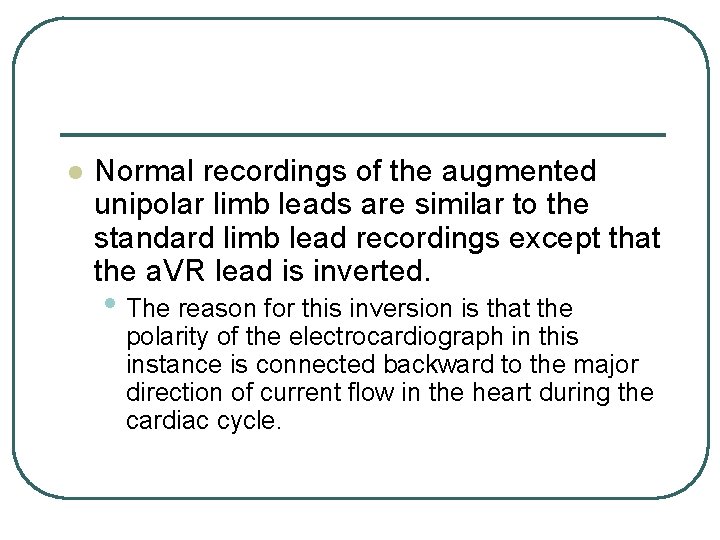
l Normal recordings of the augmented unipolar limb leads are similar to the standard limb lead recordings except that the a. VR lead is inverted. • The reason for this inversion is that the polarity of the electrocardiograph in this instance is connected backward to the major direction of current flow in the heart during the cardiac cycle.
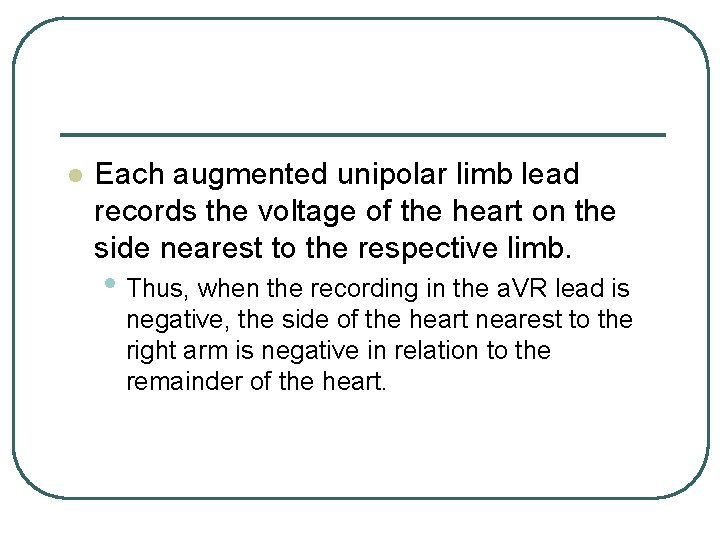
l Each augmented unipolar limb lead records the voltage of the heart on the side nearest to the respective limb. • Thus, when the recording in the a. VR lead is negative, the side of the heart nearest to the right arm is negative in relation to the remainder of the heart.
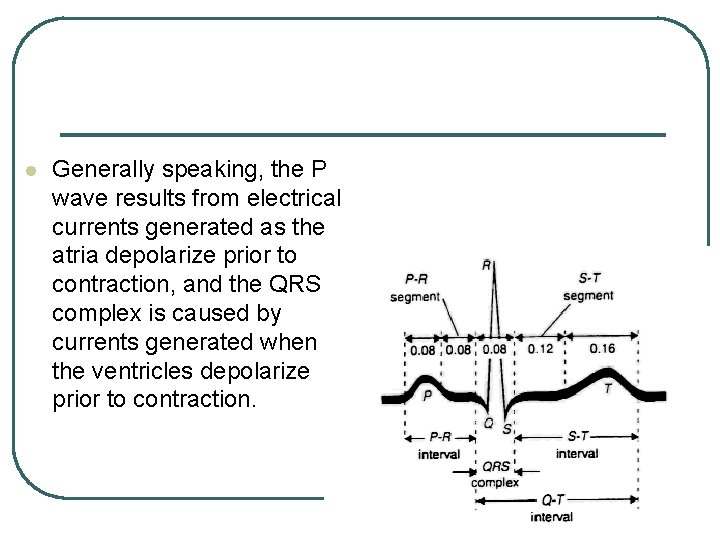
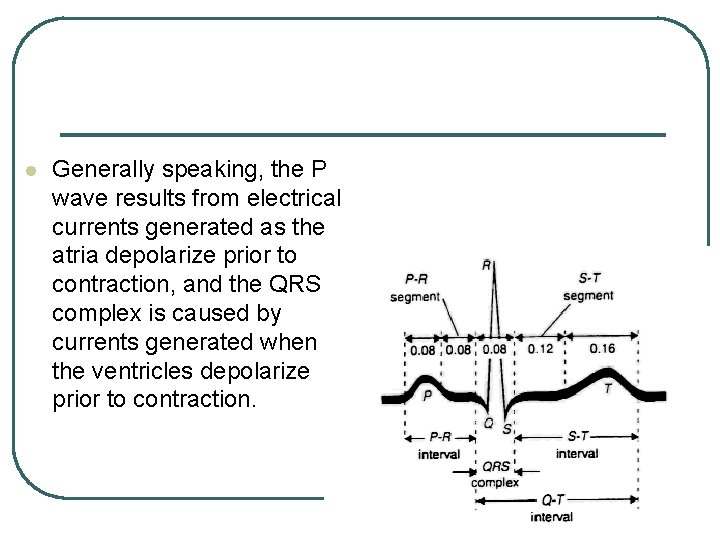
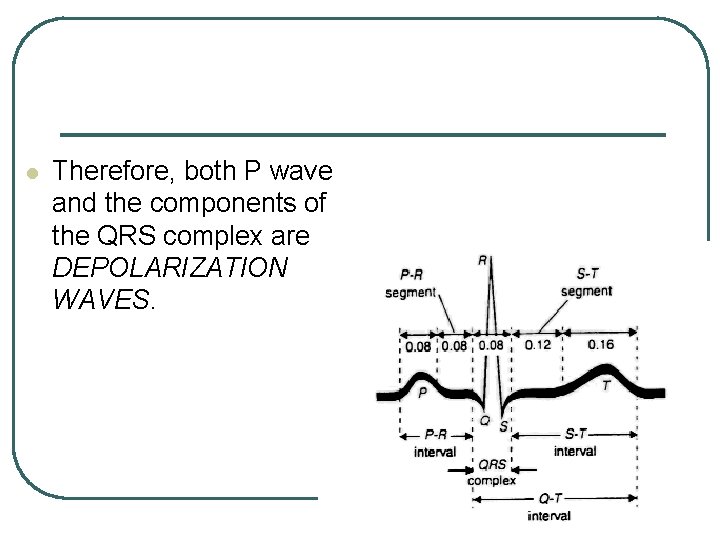
l Generally speaking, the P wave results from electrical currents generated as the atria depolarize prior to contraction, and the QRS complex is caused by currents generated when the ventricles depolarize prior to contraction.
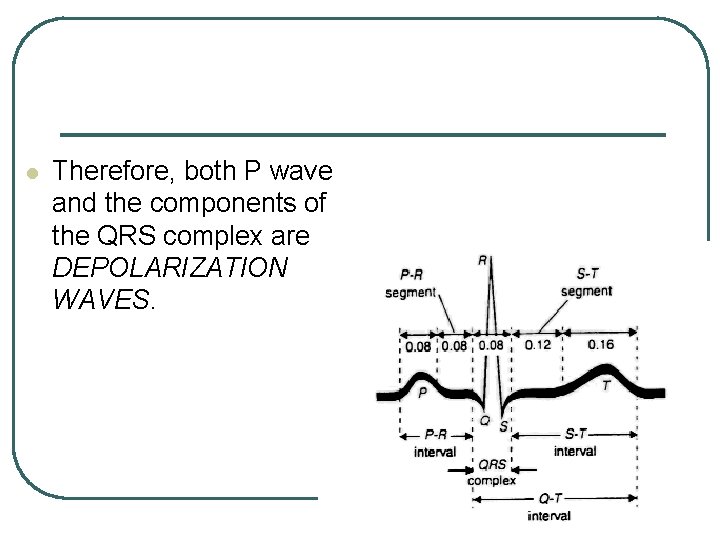
l Therefore, both P wave and the components of the QRS complex are DEPOLARIZATION WAVES.
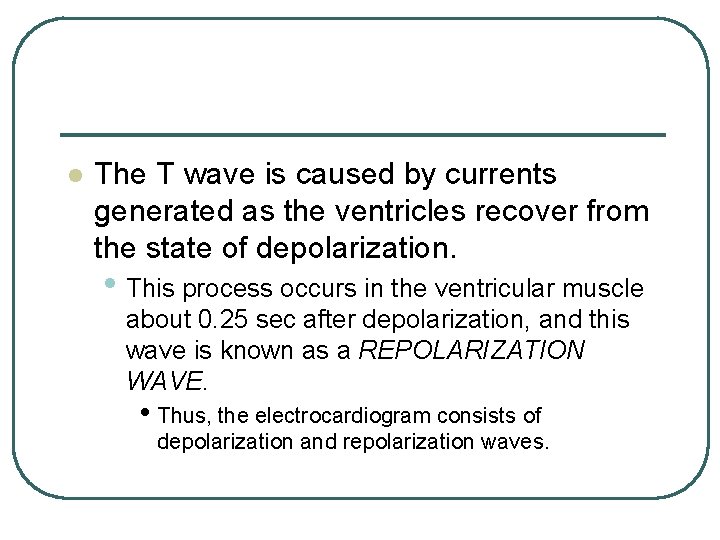
l The T wave is caused by currents generated as the ventricles recover from the state of depolarization. • This process occurs in the ventricular muscle about 0. 25 sec after depolarization, and this wave is known as a REPOLARIZATION WAVE. • Thus, the electrocardiogram consists of depolarization and repolarization waves.
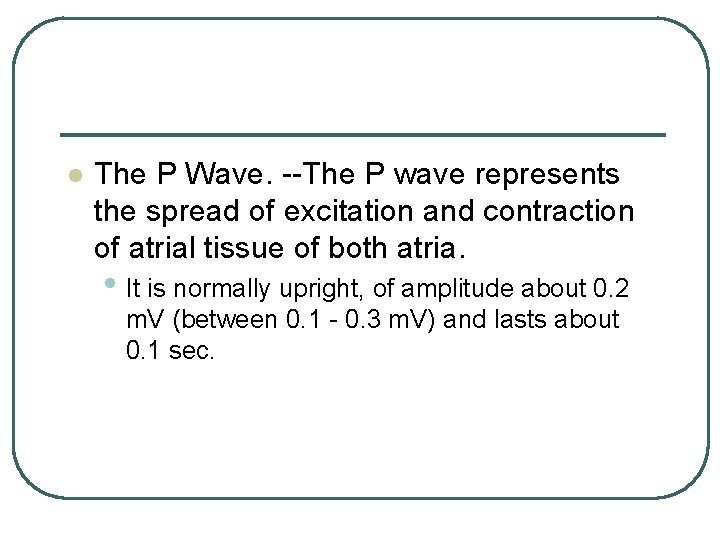
l The P Wave. --The P wave represents the spread of excitation and contraction of atrial tissue of both atria. • It is normally upright, of amplitude about 0. 2 m. V (between 0. 1 - 0. 3 m. V) and lasts about 0. 1 sec.
l Atrial repolarization takes place in the period when ventricular depolarization is occurring; • That is, the "Ta" would fall within the QRS complex of the ventricles and so is obscured in the record.
l The QRS Complex. --This complex signals the depolarization of conduction system (Q) and of the ventricular muscle. • "Q" is an initial downward deflection; • "R", a large upward deflection; • "S", a downward deflection that follows, sometimes, to below the base line, when the small upward deflection that follows is called R 1. • The duration of the QRS complex is approximately 0. 08 sec.
l The S-T Segment. --The S-T segment represents the depolarized state, when all of the ventricular muscle is depolarized. • Its level is normally very close to the baseline. The duration of the S-T segment is approximately 0. 24 sec.
l The T Wave. --The T wave represents the final difference in rate of repolarization of the different parts of the ventricular muscle. • Its amplitude and form is the most variable of all the waves in the electrocardiogram, and it is the most sensitive index of disturbances in normal conduction.
l This is illustrated by the range given for normal amplitude in lead I: from 0. 05 to +0. 55 m. V. • A minus sign would mean that the T wave in lead I was inverted, that is, downward. • The duration of the T wave is approximately 0. 12 sec.
l The time intervals between the different waves give valuable physiological information. • The two important intervals that are routinely used are the P-R and Q-T intervals or segments.
l The P-Q Interval (sometimes called P-R interval because the Q wave is frequently absent) is measured from the beginning of the P wave to the beginning of the R wave (or QRS complex).
l It represents the time taken from the start of the excitation at the pacemaker (sinoatrial node) to the beginning of ventricular depolarization (i. e. depolarization of the atrium, conduction through the atrioventricular node and through the conduction system to reach the ventricular muscle).
l This is normally 0. 16 - 0. 20 sec. • An increase in the P-R interval indicates a slowing of the conduction system, usually in the atrioventricular node.
l The Q-T Interval represents the total time for the ventricular muscle to depolarize and repolarize, from the beginning of the Q wave to the end of the T wave. • This interval is longer for men and children than for women, and it is usually reduced as the heart rate increases (but not proportionally to the decrease in total period of the heartbeat).
l Speeding (Tachycardia) of the heart is thus accomplished more by shortening the electrical rest period of the heart muscle than by shortening the period of electrical activity. • The normal duration of the Q-T interval is 0. 30 sec.
WHAT THE ELECTROCARDIOGRAM CANNOT TELL US
l The electrical activity of the heart is due to the depolarization and repolarization of the physiological membranes of the neuromuscular and muscular tissues of the heart. • Depolarization normally is accompanied by contraction of the muscle beneath these membranes.
l The magnitude of the voltages recorded by local or distant electrodes depends on the amount of the resting and action potentials. • In contrast, the strength of the contraction depends on the amount and state of the muscle contractile substance. • Thus, it is a mistake to expect that the amplitude of the electrocardiogram can tell us, except in extreme cases, anything about the strength of contraction or the force of the heartbeat (e. g. level of arterial pressure pulse produced).
l Where changes in the ionic environment (e. g. abnormal K+) or in the metabolic state of the tissue have altered the resting and action potentials of the muscle, there will, of course, be some correlation of the amplitude of the electrocardiogram with the strength of the beat.
l The amplitude of the waves is also affected by the electrical resistance of the pathways to the distant electrodes; in addition, as has been already pointed out, the recorded voltages represent only the difference between the influences of simultaneous and opposite electrical dipoles in a complicated pattern. • The resultant depends as much on the synchrony or asynchrony of the component dipoles as on the magnitude of the original potentials.
VARIETIES OF HEART BLOCK
l Since the primary information from the electrocardiogram concerns the conduction pathways, it is most useful in the diagnosis of cases of interruption of normal pathways. • Bundle-branch block means that the impulses have come from the atrial pacemaker (sinoatrial node), reached and passed the atrioventricular node, but travel down only one of the two main branches of the conduction system (left or right bundle-branch block).
l Excitation of the "blocked" ventricle still occurs, but by spread from the normal ventricle. • The QRS complex of the electrocardiogram is greatly prolonged from the normal 0. 06 - 0. 10 sec to more than 0. 12 sec (First Degree). • This is because conduction takes longer route to the block ventricle and because the velocity is less in the muscle than in the conduction system.
l In total sinoatrial block (Third Degree), the ventricles may continue to beat in a new rhythm, called a "nodal, or ideoventricular, rhythm, " according to whether the initiation of the impulse is taken up by the sinoatrial node itself or an ectopic focus in the ventricular muscle becomes the pacemaker. • Such varieties of block are diagnosed from the electrocardiogram by noting a dissociation of the P waves (atrial activity) from the QRST waves (ventricular activity). • The P wave may be absent (atrial standstill) or present from an abnormal origin in the atrium.
l In cases where the atrioventricular node is partly blocked, the atrial rhythm may be conducted to the ventricles only every second beat, or in-groups of two or three beats (bigeminal and trigeminal rhythms, meaning "two twins" and "three twins", respectively – Second Degree).
FLUTTER AND FIBRILLATION ARRHYTHMIAS
l The normal rhythms dominated by the atrial pacemaker are known as "sinus rhythms". • Nodal and ventricular rhythms are examples of escape from the dominance of the normal pacemaker. • In a different category of arrhythmias are atrial flutter and fibrillation and ventricular fibrillation.
l In atrial flutter, a regular succession of P waves is seen in the electrocardiogram at a rate many times the normal sinus rhythm. • Only every second, third, fourth, or fifth of these waves may be followed by the ventricular complex (QRST complex).
l One explanation for flutter is that the wave of depolarization is following some unusual path in the atrial tissue and is returning to re-excite repetitively the pacemaker tissue, which is capable of responding to stimuli at intervals much shorter than those of its own normal spontaneous rhythm.
l If the wave of depolarization spreads normally from the node in all directions, it could obviously not so return (because of the refractory period); but if conduction were blocked in certain areas, one could conceive of such a "circus" route.
l In fibrillation, which often develops from flutter, the whole atrium beats in an uncoordinated manner with multiple apparent foci of the impulses (it quivers like jelly). • The atrioventricular node is thus bombarded with hundreds of impulses every minute, and only now and then does an impulse find the atrioventricular node out of its refractory state (i. e. susceptible to stimulation).
l The ventricular rhythm that results is very irregular. • The whole base line of the electrocardiogram shows tiny irregular waves, less regular and more frequent than those of flutter. • The atria no longer achieve a significant pumping of blood; but it turns out that this does not, per se, reduce the output of the heart greatly, although the accompanying irregularity of the ventricular contractions does significantly reduce the output.
l Ventricular fibrillation is a similar quivering of the ventricles (the ventricle feels to hand like a sack of worms). • In this case the cardiac output ceases, and this is an emergency with fatal outcome unless cardiac massage and a means of defibrillation is at once employed.
l Defibrillation is accomplished by administering a severe electrical shock to the heart, which arrests all excitation and conduction. • On recovery from the refractoriness produced by the shock, a normal rhythm may be taken up. • It is not surprising that electrocardiographic records of human ventricular fibrillation are not readily available for illustration.
 Insidan region jh
Insidan region jh Phonocardiography definition
Phonocardiography definition Saumya mohan
Saumya mohan Jones and bartlett 2012 ekg strips
Jones and bartlett 2012 ekg strips Jones and bartlett ekg strips
Jones and bartlett ekg strips Ekg plain and simple answer key
Ekg plain and simple answer key Pediatric triangle assessment
Pediatric triangle assessment Comparison of skeletal cardiac and smooth muscle
Comparison of skeletal cardiac and smooth muscle Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Pearson
Pearson Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed Slide
Slide Comparison of skeletal cardiac and smooth muscle
Comparison of skeletal cardiac and smooth muscle Refractory period cardiac
Refractory period cardiac Mitochondrian
Mitochondrian Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Cardiac stimulants and depressants
Cardiac stimulants and depressants Factors affecting cardiac output
Factors affecting cardiac output Cardiac output and stroke volume
Cardiac output and stroke volume Heart sounds and murmurs
Heart sounds and murmurs Hemodynamic disorders
Hemodynamic disorders The conduction system
The conduction system Ecg lead orientation
Ecg lead orientation Ekg kytkennät
Ekg kytkennät Pea rhythm
Pea rhythm Normal ecg
Normal ecg Sniffing position adalah
Sniffing position adalah Amiodaron endikasyonları
Amiodaron endikasyonları Gambaran ekg pea
Gambaran ekg pea Respiratorna aritmija
Respiratorna aritmija A fib ecg
A fib ecg Ekg ni o'qish
Ekg ni o'qish Asistoli ekg
Asistoli ekg Ekg aks nedir
Ekg aks nedir Asistoli nedir
Asistoli nedir Sinistogram
Sinistogram Wandering atrial pacemaker ecg
Wandering atrial pacemaker ecg Youtube
Youtube Ventrikel ekstra sistol ekg
Ventrikel ekstra sistol ekg Ekg prop yerleri
Ekg prop yerleri Ves unifocal
Ves unifocal R on t phenomenon
R on t phenomenon Ekg elektroder placering
Ekg elektroder placering Patološki q zubac
Patološki q zubac Walls of heart in ecg
Walls of heart in ecg Vf ecg
Vf ecg Av blok prvog stepena
Av blok prvog stepena Ekg dorsalis elvezetések
Ekg dorsalis elvezetések Which ekg leads are bipolar
Which ekg leads are bipolar Asistoli ekg
Asistoli ekg J punkt ekg
J punkt ekg Idioventrikuler adalah
Idioventrikuler adalah 1 kotak kecil ekg berapa mm
1 kotak kecil ekg berapa mm Diagnosa keperawatan takikardi
Diagnosa keperawatan takikardi Elektromekanik disosiasyon
Elektromekanik disosiasyon Limb leads
Limb leads Jussi-pekka haikio
Jussi-pekka haikio Tahta pabuç manzarası
Tahta pabuç manzarası Ekg 25mm/s 1 kratka
Ekg 25mm/s 1 kratka Trifasiküler blok
Trifasiküler blok Gambaran ekg sinus aritmia
Gambaran ekg sinus aritmia Axul electric al inimii
Axul electric al inimii Sağ ventrikül hipertrofisi ekg bulguları
Sağ ventrikül hipertrofisi ekg bulguları Ekg paperin nopeus
Ekg paperin nopeus Blok pravého raménka
Blok pravého raménka Bradycardia
Bradycardia Elektrokardiográfia
Elektrokardiográfia Brugada sindroms
Brugada sindroms Nsvt definition
Nsvt definition Ra rl la ll
Ra rl la ll Ekg script
Ekg script Driven right leg
Driven right leg Zátěžové ekg
Zátěžové ekg Sydänifarkti
Sydänifarkti Vernier ekg
Vernier ekg Ekg stundenplan
Ekg stundenplan Keith rischer
Keith rischer Ekg
Ekg Horizontal
Horizontal Dorsalis ekg
Dorsalis ekg