Cardiovascular Physiology Heart Cardiac Cycle The Cardiac Cycle
- Slides: 26
Cardiovascular Physiology: Heart Cardiac Cycle
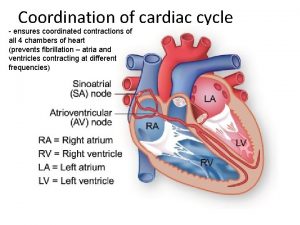
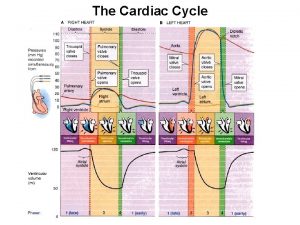
The Cardiac Cycle Cardiac cycle = the period between the start of one heartbeat and the beginning of the next § Consists of systole + diastole § Systole=contraction § Diastole=relaxation
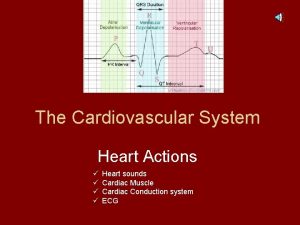
The Cardiac Cycle § Correlate the EKG with systole + diastole of the heart § Electrical events occur before mechanical contraction § EKG animation Copyright © 2009 Pearson Education, Inc. , publishing as Pearson Benjamin Cummings
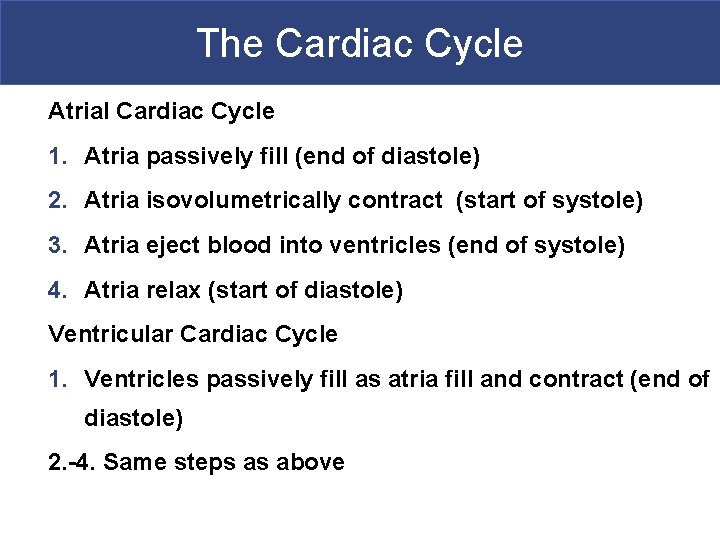
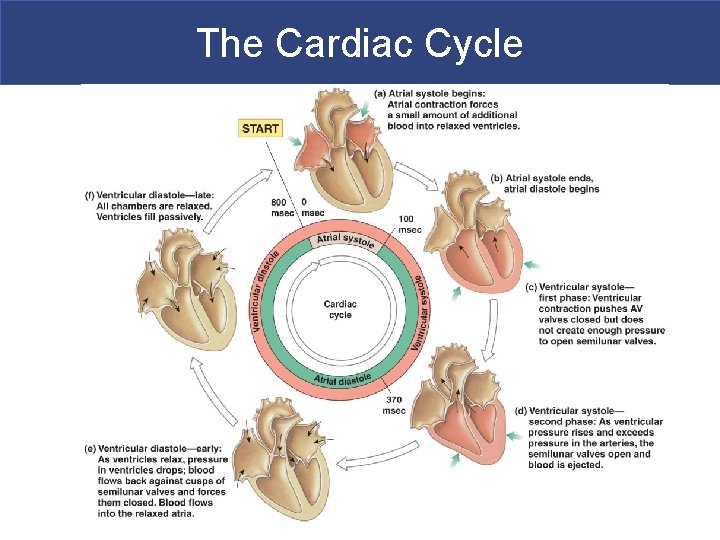
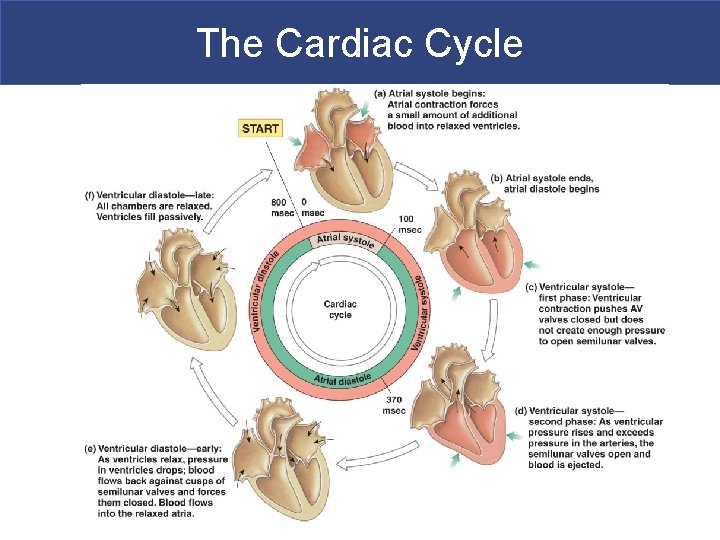
The Cardiac Cycle Atrial Cardiac Cycle 1. Atria passively fill (end of diastole) 2. Atria isovolumetrically contract (start of systole) 3. Atria eject blood into ventricles (end of systole) 4. Atria relax (start of diastole) Ventricular Cardiac Cycle 1. Ventricles passively fill as atria fill and contract (end of diastole) 2. -4. Same steps as above
The Cardiac Cycle
Blood Flow and Pressure § During systole blood pressure increases § During diastole blood pressure decreases § Blood flows from high low pressure § Contractions and valves dictate blood flow through the heart
The Cardiac Cycle § Start at ventricular diastole and left side of heart (highest pressure values) § Blood flows from high low pressure § Contractions and valves dictate blood flow § Blood pressure in each chamber rises during systole and falls during diastoles
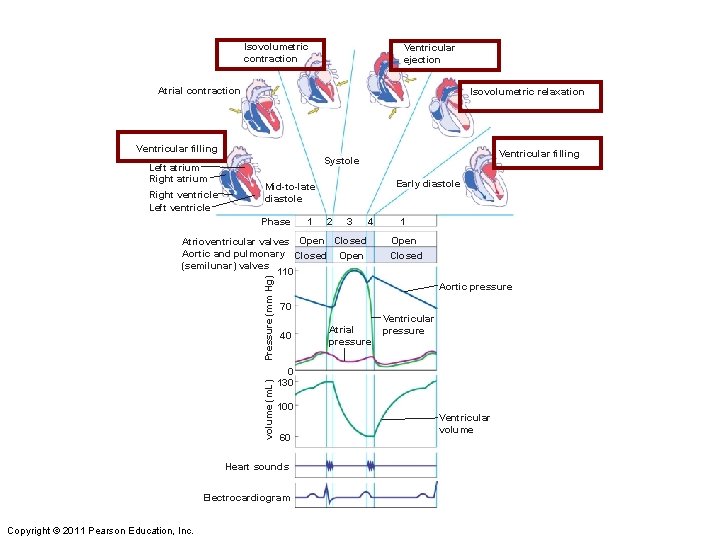
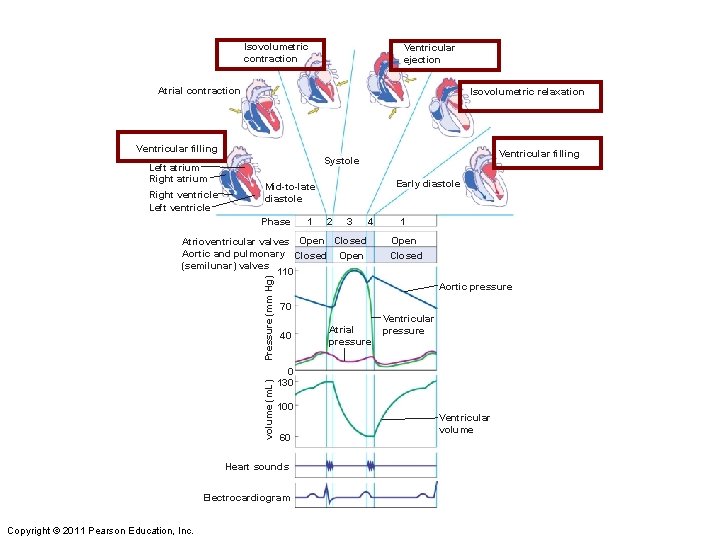
Isovolumetric contraction Ventricular ejection Atrial contraction Isovolumetric relaxation Ventricular filling Left atrium Right ventricle Left ventricle Ventricular filling Systole Early diastole Mid-to-late diastole Phase 1 2 3 4 volume (m. L) Pressure (mm Hg) Atrioventricular valves Open Closed Aortic and pulmonary Closed Open (semilunar) valves 110 Open Closed Aortic pressure 70 40 Atrial pressure Ventricular pressure 0 130 100 60 Heart sounds Electrocardiogram Copyright © 2011 Pearson Education, Inc. 1 Ventricular volume
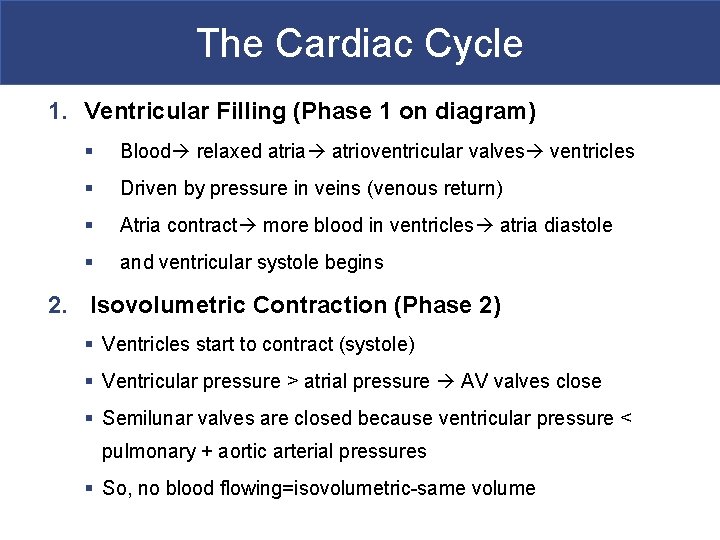
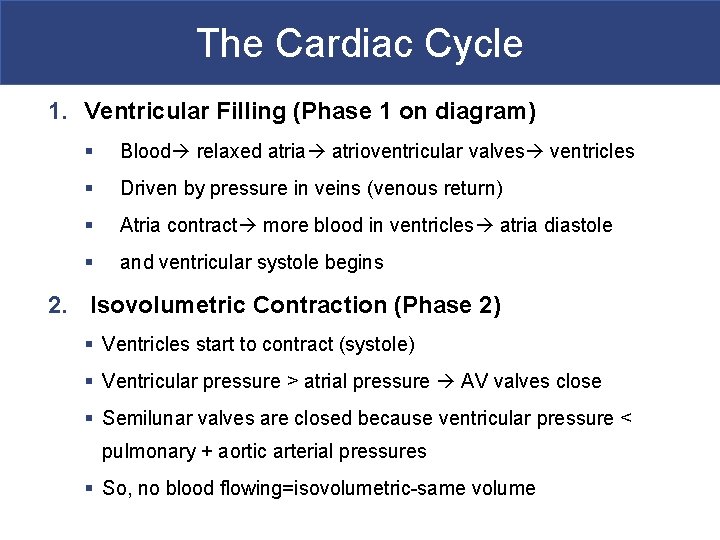
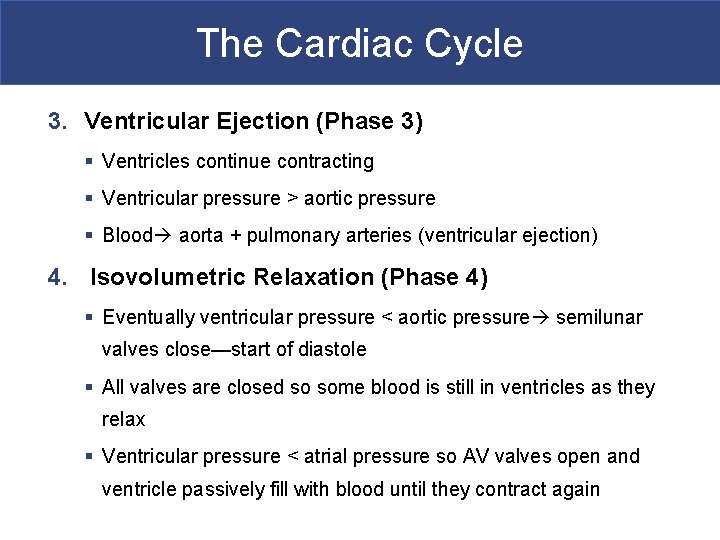
The Cardiac Cycle 1. Ventricular Filling (Phase 1 on diagram) § Blood relaxed atria atrioventricular valves ventricles § Driven by pressure in veins (venous return) § Atria contract more blood in ventricles atria diastole § and ventricular systole begins 2. Isovolumetric Contraction (Phase 2) § Ventricles start to contract (systole) § Ventricular pressure > atrial pressure AV valves close § Semilunar valves are closed because ventricular pressure < pulmonary + aortic arterial pressures § So, no blood flowing=isovolumetric-same volume
The Cardiac Cycle 3. Ventricular Ejection (Phase 3) § Ventricles continue contracting § Ventricular pressure > aortic pressure § Blood aorta + pulmonary arteries (ventricular ejection) 4. Isovolumetric Relaxation (Phase 4) § Eventually ventricular pressure < aortic pressure semilunar valves close—start of diastole § All valves are closed so some blood is still in ventricles as they relax § Ventricular pressure < atrial pressure so AV valves open and ventricle passively fill with blood until they contract again
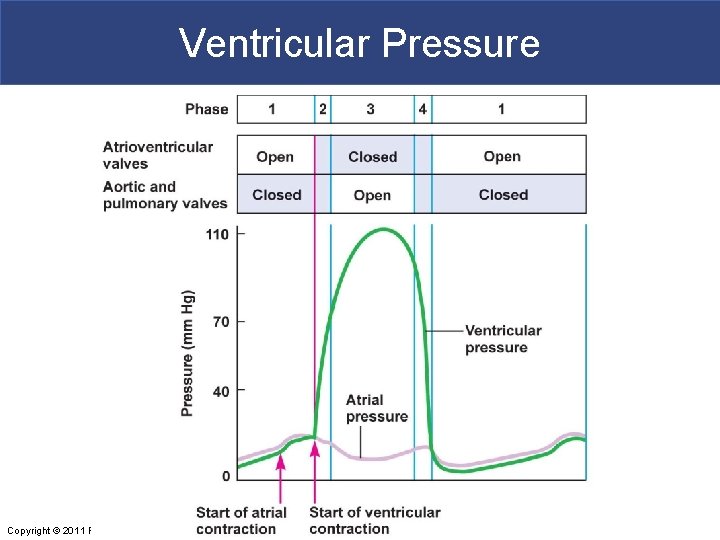
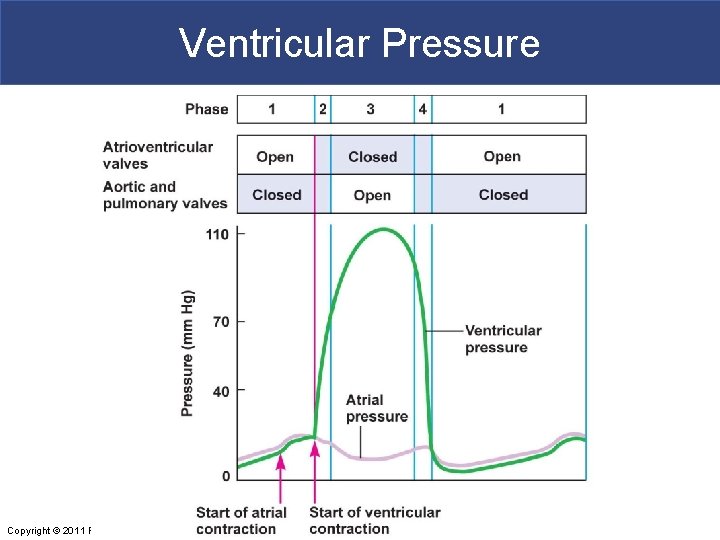
Ventricular Pressure Copyright © 2011 Pearson Education, Inc.
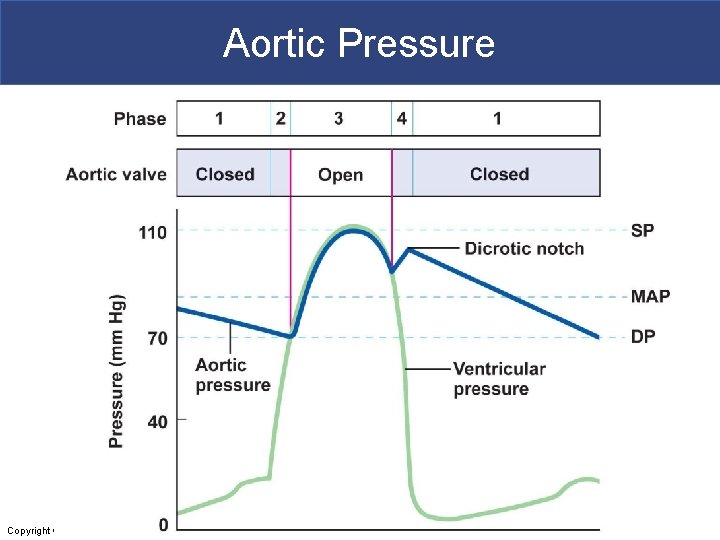
Aortic Pressure Copyright © 2011 Pearson Education, Inc.
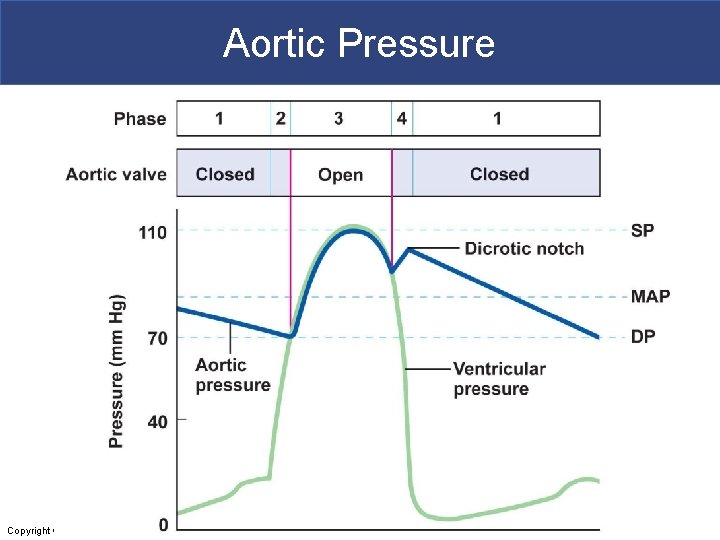
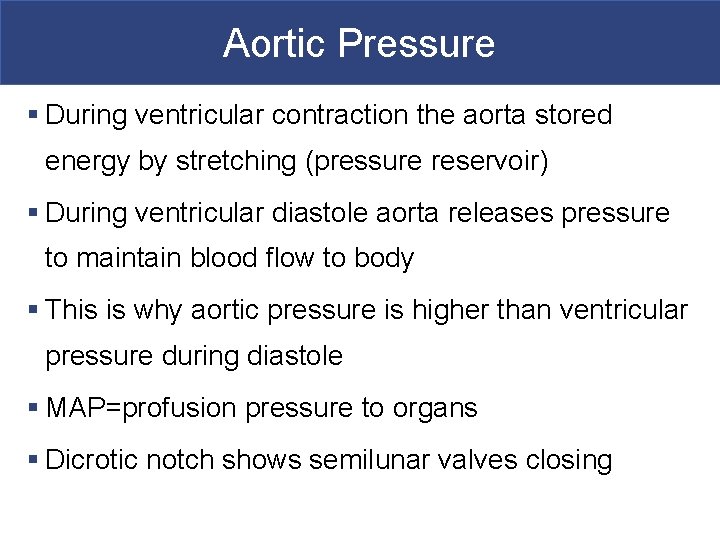
Aortic Pressure § During ventricular contraction the aorta stored energy by stretching (pressure reservoir) § During ventricular diastole aorta releases pressure to maintain blood flow to body § This is why aortic pressure is higher than ventricular pressure during diastole § MAP=profusion pressure to organs § Dicrotic notch shows semilunar valves closing
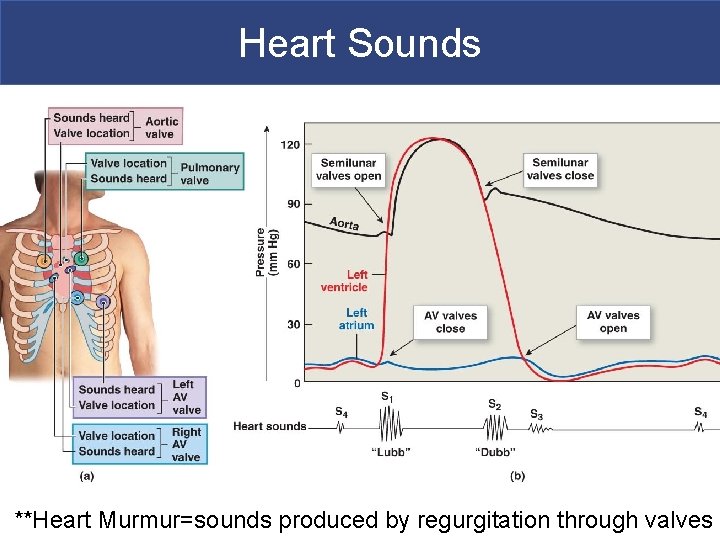
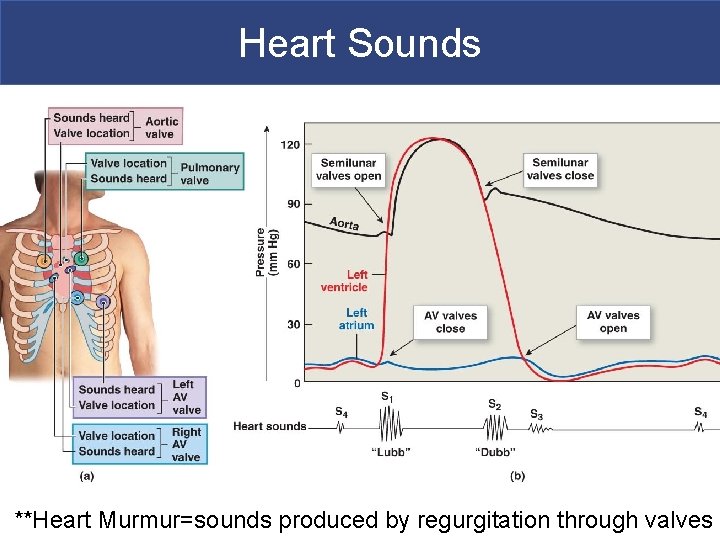
Heart Sounds **Heart Murmur=sounds produced by regurgitation through valves Copyright © 2011 Pearson Education, Inc.
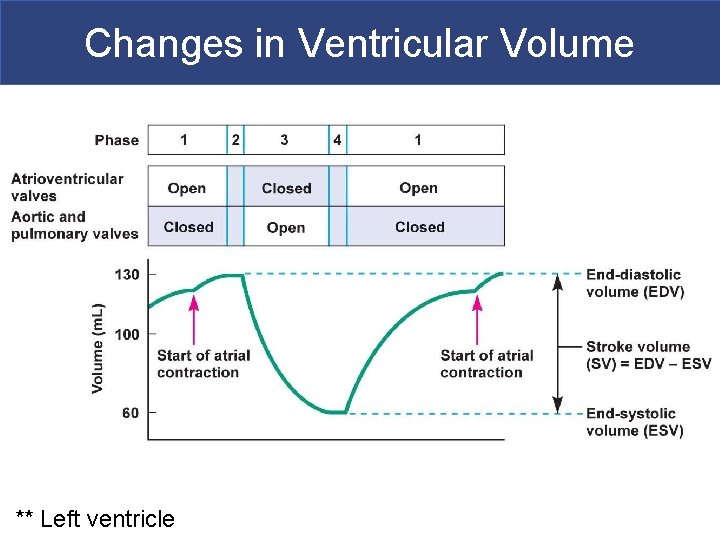
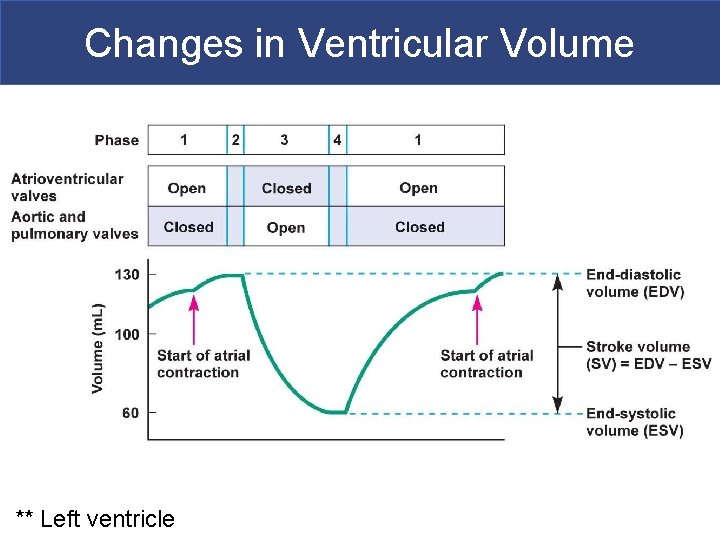
Changes in Ventricular Volume ** Left ventricle Copyright © 2011 Pearson Education, Inc.
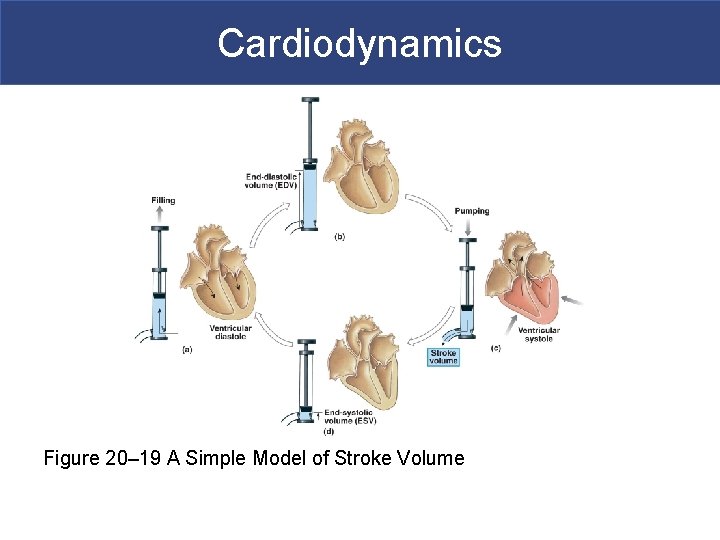
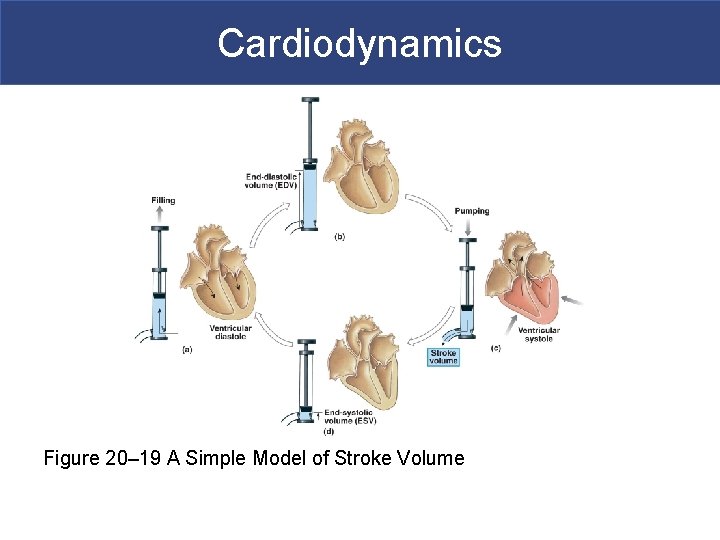
Cardiodynamics Figure 20– 19 A Simple Model of Stroke Volume
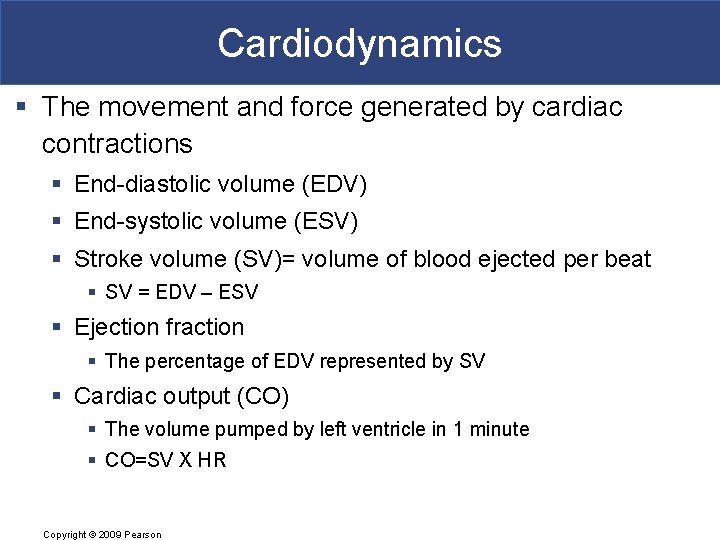
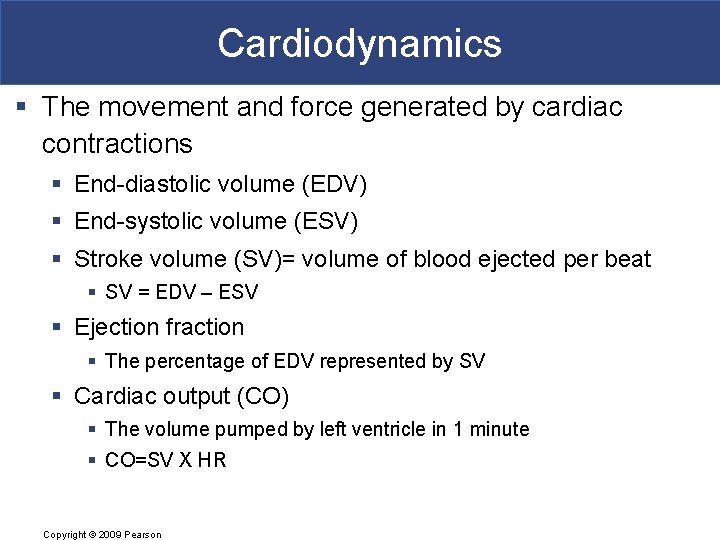
Cardiodynamics § The movement and force generated by cardiac contractions § End-diastolic volume (EDV) § End-systolic volume (ESV) § Stroke volume (SV)= volume of blood ejected per beat § SV = EDV – ESV § Ejection fraction § The percentage of EDV represented by SV § Cardiac output (CO) § The volume pumped by left ventricle in 1 minute § CO=SV X HR Copyright © 2009 Pearson
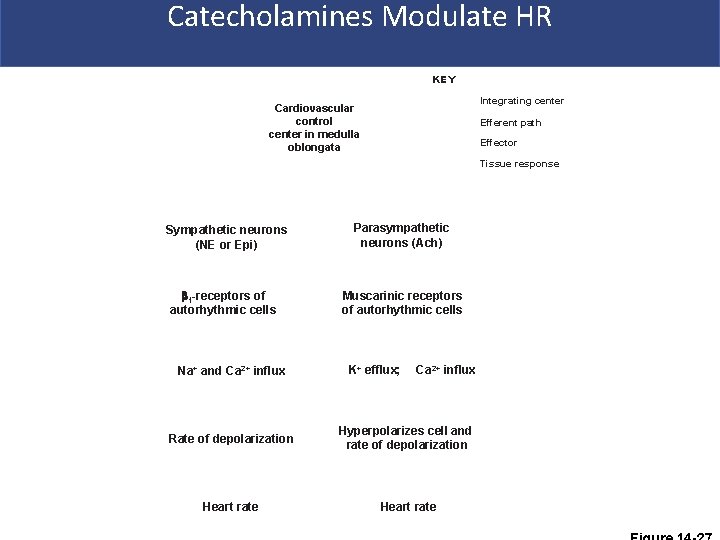
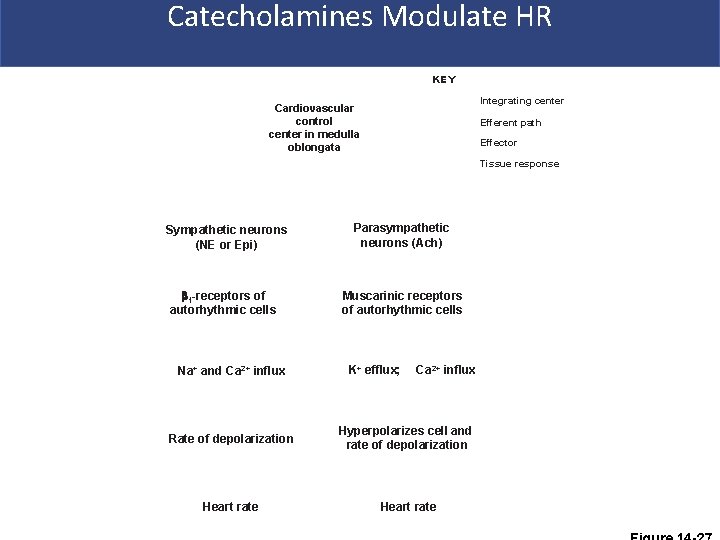
Catecholamines Modulate HR KEY Integrating center Cardiovascular control center in medulla oblongata Efferent path Effector Tissue response Sympathetic neurons (NE or Epi) Parasympathetic neurons (Ach) 1 -receptors of autorhythmic cells Muscarinic receptors of autorhythmic cells Na+ and Ca 2+ influx K+ efflux; Ca 2+ influx Rate of depolarization Hyperpolarizes cell and rate of depolarization Heart rate
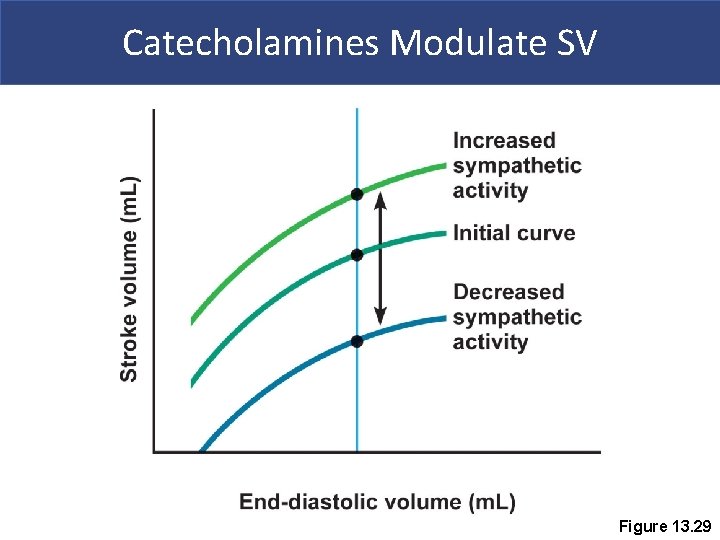
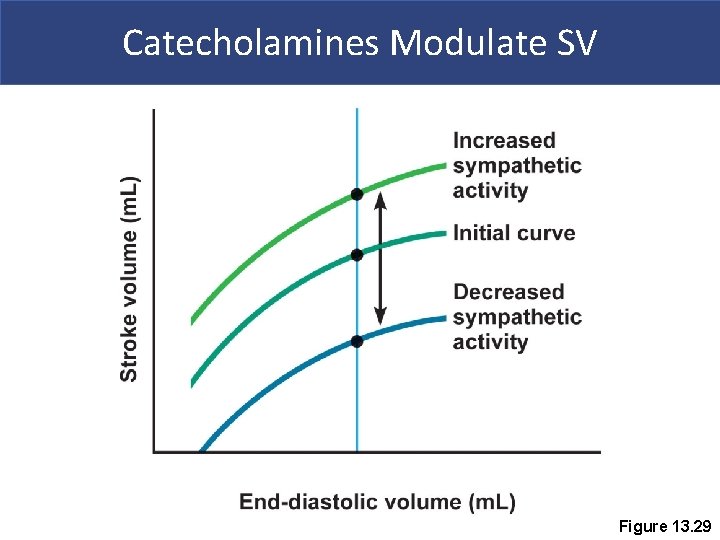
Catecholamines Modulate SV Figure 13. 29
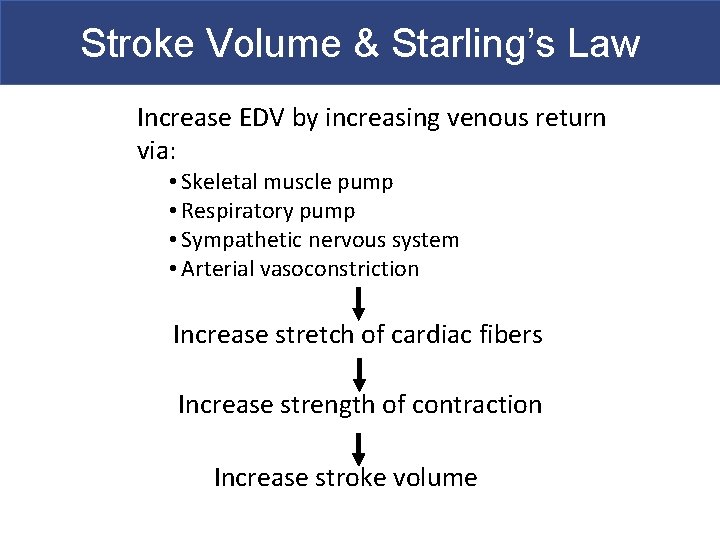
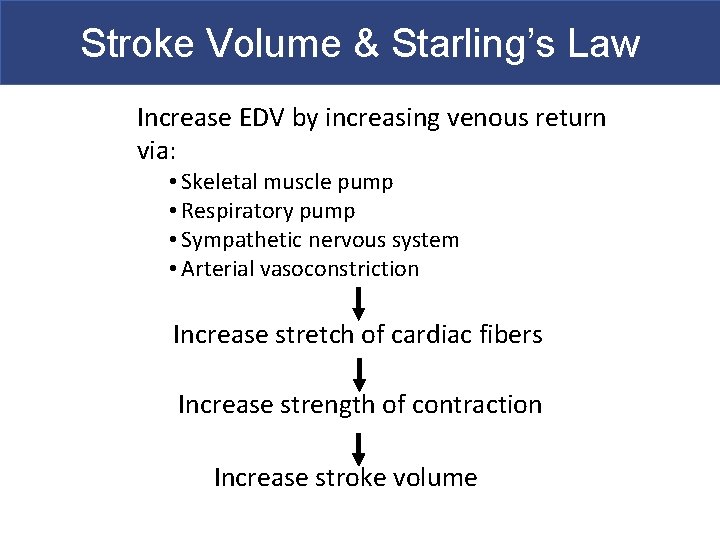
Stroke Volume & Starling’s Law Increase EDV by increasing venous return via: • Skeletal muscle pump • Respiratory pump • Sympathetic nervous system • Arterial vasoconstriction Increase stretch of cardiac fibers Increase strength of contraction Increase stroke volume
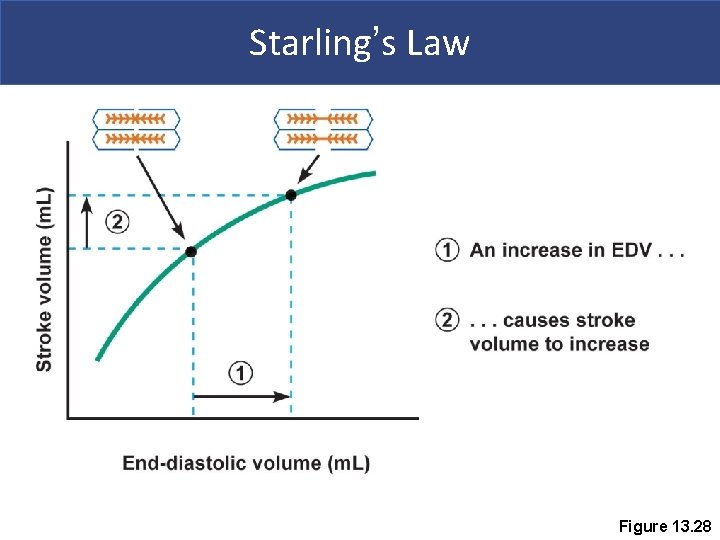
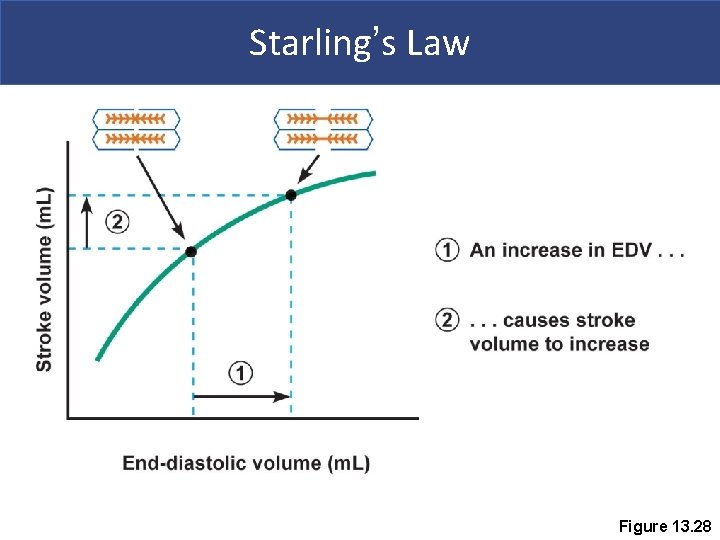
Starling’s Law Figure 13. 28
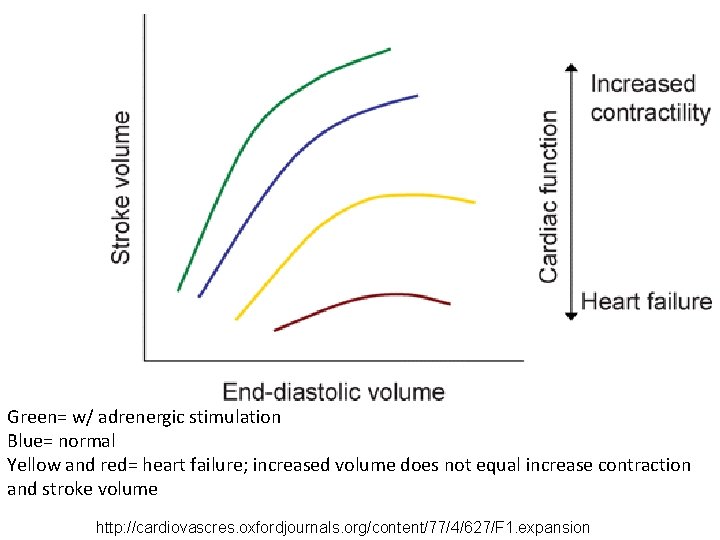
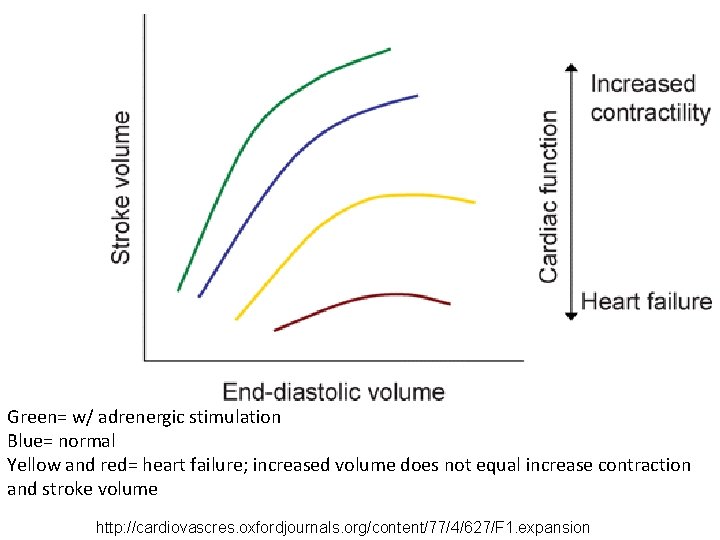
Green= w/ adrenergic stimulation Blue= normal Yellow and red= heart failure; increased volume does not equal increase contraction and stroke volume http: //cardiovascres. oxfordjournals. org/content/77/4/627/F 1. expansion
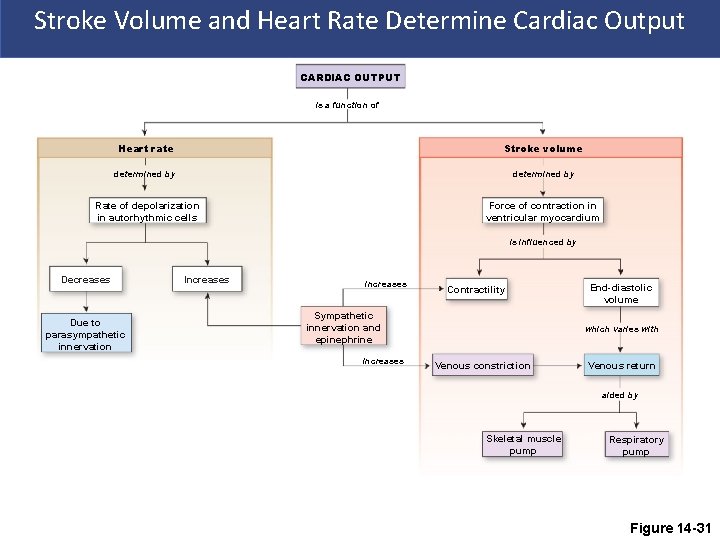
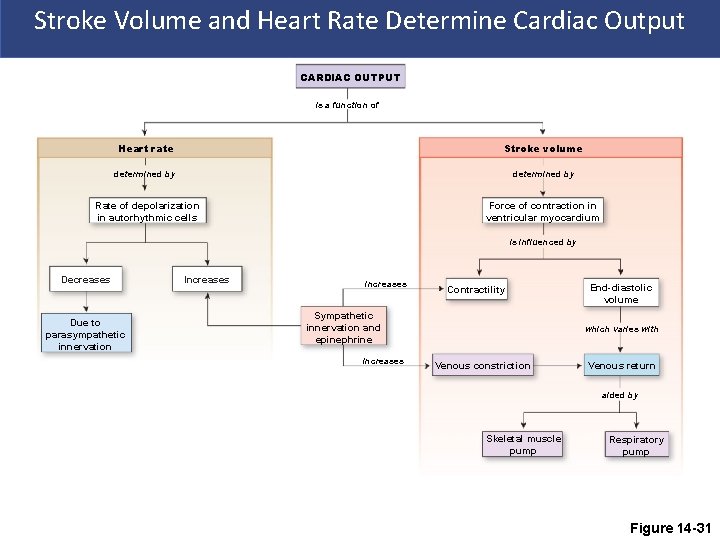
Stroke Volume and Heart Rate Determine Cardiac Output CARDIAC OUTPUT is a function of Heart rate Stroke volume determined by Rate of depolarization in autorhythmic cells Force of contraction in ventricular myocardium is influenced by Decreases Due to parasympathetic innervation Increases increases Contractility Sympathetic innervation and epinephrine increases End-diastolic volume which varies with Venous constriction Venous return aided by Skeletal muscle pump Respiratory pump Figure 14 -31
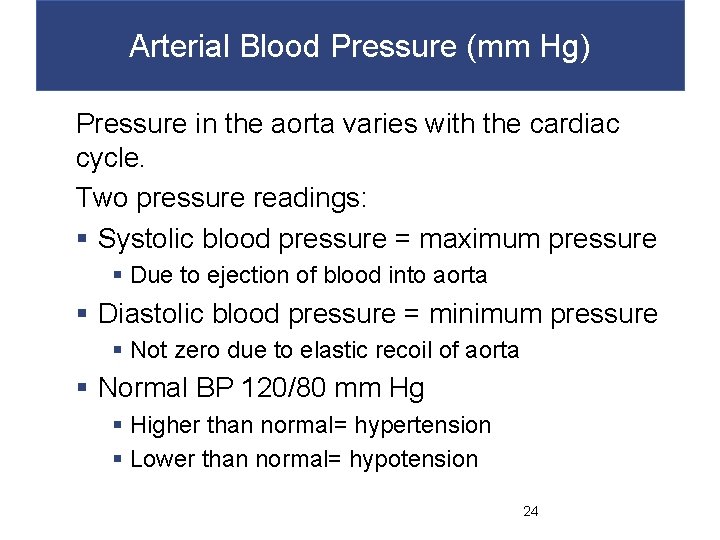
Arterial Blood Pressure (mm Hg) Pressure in the aorta varies with the cardiac cycle. Two pressure readings: § Systolic blood pressure = maximum pressure § Due to ejection of blood into aorta § Diastolic blood pressure = minimum pressure § Not zero due to elastic recoil of aorta § Normal BP 120/80 mm Hg § Higher than normal= hypertension § Lower than normal= hypotension 24
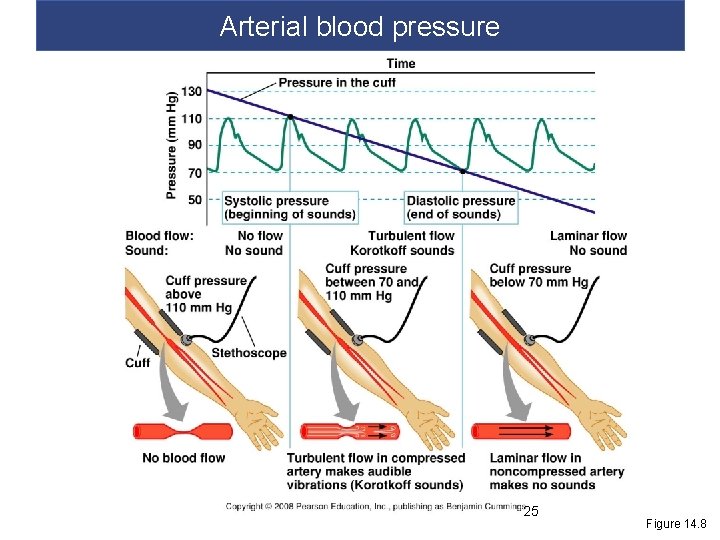
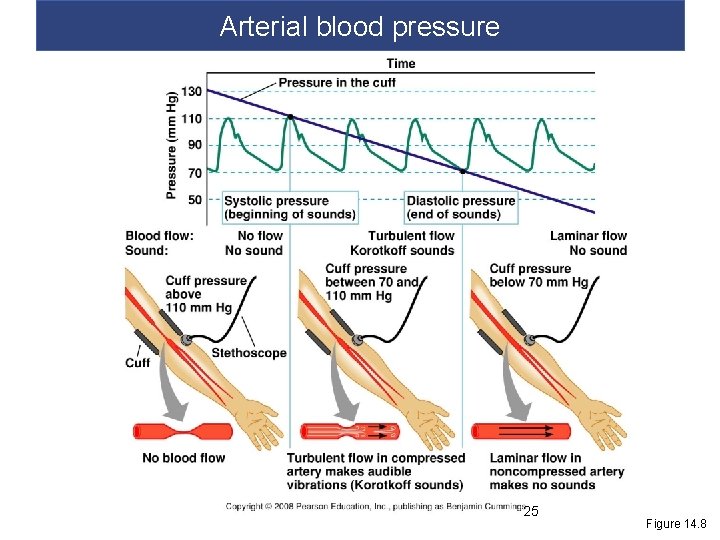
Arterial blood pressure 25 Figure 14. 8
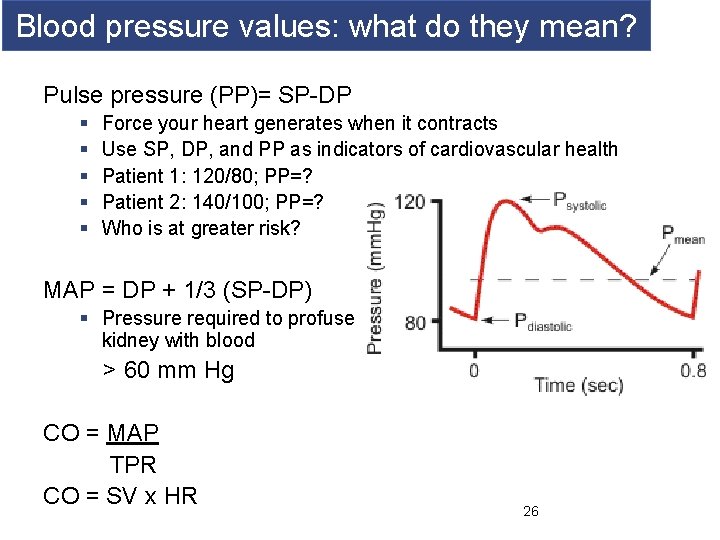
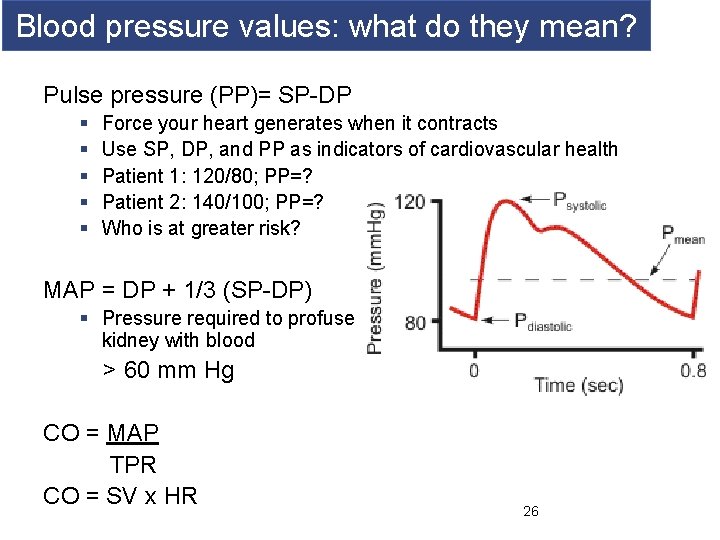
Blood pressure values: what do they mean? Pulse pressure (PP)= SP-DP § § § Force your heart generates when it contracts Use SP, DP, and PP as indicators of cardiovascular health Patient 1: 120/80; PP=? Patient 2: 140/100; PP=? Who is at greater risk? MAP = DP + 1/3 (SP-DP) § Pressure required to profuse brain, coronary arteries, and kidney with blood > 60 mm Hg CO = MAP TPR CO = SV x HR 26
 Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Refractory period heart
Refractory period heart Heart as a pump physiology
Heart as a pump physiology Events of cardiac cycle class 11
Events of cardiac cycle class 11 Cardiac output and heart rate
Cardiac output and heart rate Cardiac cycle
Cardiac cycle Ecg phases
Ecg phases Cardiac cycle animation
Cardiac cycle animation Cardiac cycle graph
Cardiac cycle graph Wigger diagram
Wigger diagram Why mba ppt
Why mba ppt Cardiac cycle
Cardiac cycle Cardiac cycle
Cardiac cycle Atrial systole
Atrial systole Cardiac cycle
Cardiac cycle Heart dullness
Heart dullness Sheep heart vs human heart
Sheep heart vs human heart Heart 2 heart
Heart 2 heart Capillary bed labeled
Capillary bed labeled Riesgo cardiovascular por perimetro abdominal
Riesgo cardiovascular por perimetro abdominal Maniobra de azoulay
Maniobra de azoulay What makes up the cardiovascular system
What makes up the cardiovascular system Rutas integrales de atencion en salud
Rutas integrales de atencion en salud Pithed rat meaning
Pithed rat meaning Fresenius national cardiovascular partners
Fresenius national cardiovascular partners Totally tubular dude
Totally tubular dude Cardiovascular drift
Cardiovascular drift