Region X Cardiac SOPs EKG Rhythms and Interventions











- Slides: 90
Region X Cardiac SOP’s EKG Rhythms and Interventions Condell Medical Center EMS System February 2008 Site Code #10 -7200 E 1208 Prepared by: Sharon Hopkins, RN, BSN, EMT-P
Objectives z. Upon successful completion of this module, the EMS provider should be able to: yreview identification of a variety of EKG rhythms yrelate the dysrhythmia to the presentation of the patient ycomprehend the Region X cardiac SOP’s as they relate to the patient’s presentation yactively participate in case review ysuccessfully complete the quiz with a score of 80% or greater
Introduction to Use of the SOP’s z. Care is initiated for all patients based on your assessment z. A pediatric patient is considered under the age of 16 (15 and less) z. Do not delay care to contact Medical control z. But, prompt communication is encouraged
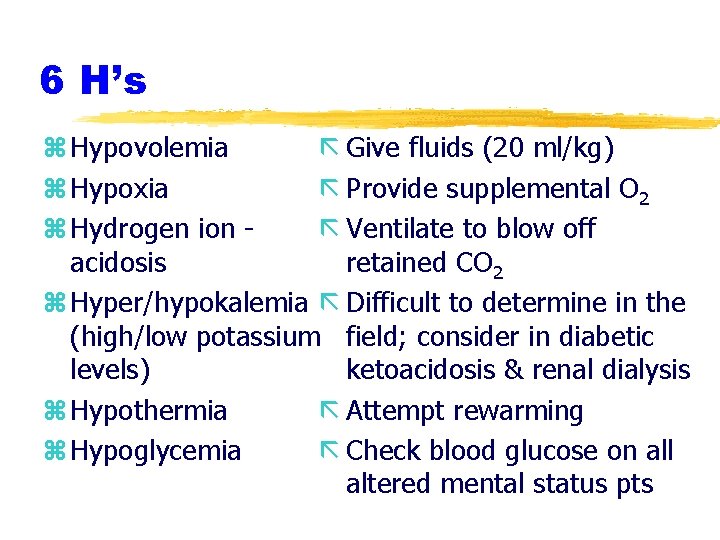
Cardiac SOP’s z. Obtaining a history and performing an assessment can often provide valuable information z. Consider underlying causes for all situations z. In the cardiac SOP’s, think of the 6 H’s and 5 T’s as possible causes of the problem as you progress through assessment & treatment for the patient
6 H’s z Hypovolemia ã Give fluids (20 ml/kg) z Hypoxia ã Provide supplemental O 2 z Hydrogen ion ã Ventilate to blow off acidosis retained CO 2 z Hyper/hypokalemia ã Difficult to determine in the (high/low potassium field; consider in diabetic levels) ketoacidosis & renal dialysis z Hypothermia ã Attempt rewarming z Hypoglycemia ã Check blood glucose on all altered mental status pts

5 T’s z Toxins (overdose) ã Think “out of the box” z Tamponade, cardiac ã Check for JVD, B/P, z Tension pneumothorax absent/decreased breath sounds, difficulty bagging z Thrombosis, coronary ã Obtain 12 lead when (ACS) or Thrombosis, applicable; good history pulmonary taking to lead to suspicions (embolism) (travel, surgery, immobility) z Trauma ã What is history of current status?
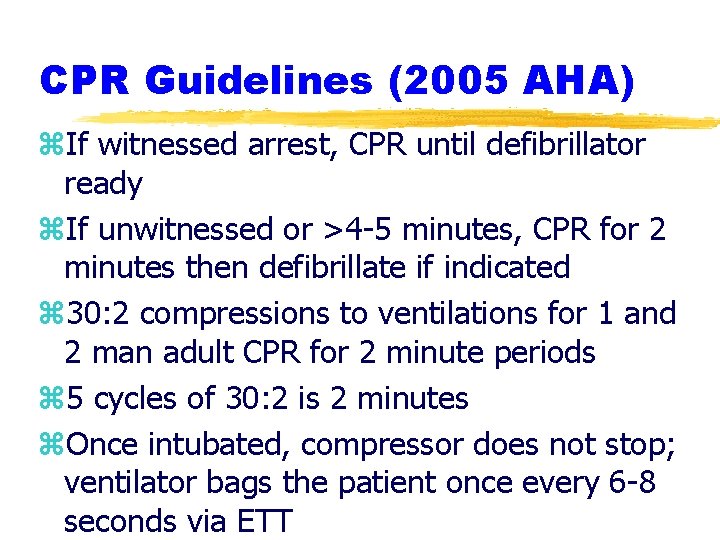
CPR Guidelines (2005 AHA) z. If witnessed arrest, CPR until defibrillator ready z. If unwitnessed or >4 -5 minutes, CPR for 2 minutes then defibrillate if indicated z 30: 2 compressions to ventilations for 1 and 2 man adult CPR for 2 minute periods z 5 cycles of 30: 2 is 2 minutes z. Once intubated, compressor does not stop; ventilator bags the patient once every 6 -8 seconds via ETT
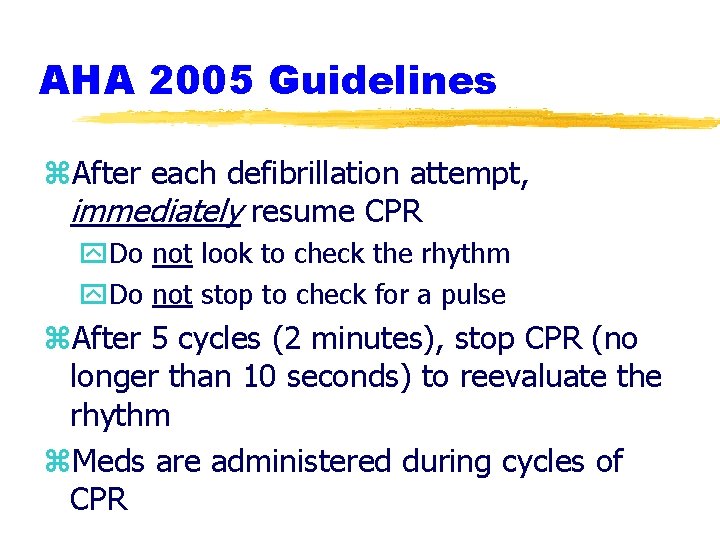
AHA 2005 Guidelines z. After each defibrillation attempt, immediately resume CPR y. Do not look to check the rhythm y. Do not stop to check for a pulse z. After 5 cycles (2 minutes), stop CPR (no longer than 10 seconds) to reevaluate the rhythm z. Meds are administered during cycles of CPR
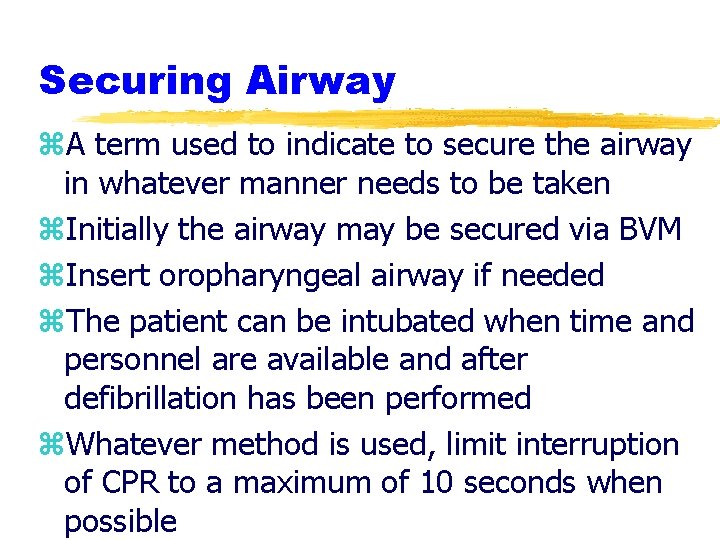
Securing Airway z. A term used to indicate to secure the airway in whatever manner needs to be taken z. Initially the airway may be secured via BVM z. Insert oropharyngeal airway if needed z. The patient can be intubated when time and personnel are available and after defibrillation has been performed z. Whatever method is used, limit interruption of CPR to a maximum of 10 seconds when possible
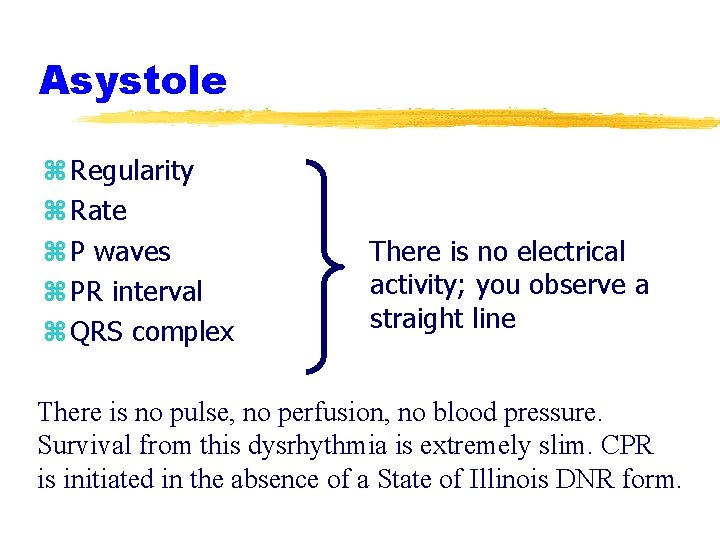
Asystole z Regularity z Rate z P waves z PR interval z QRS complex There is no electrical activity; you observe a straight line There is no pulse, no perfusion, no blood pressure. Survival from this dysrhythmia is extremely slim. CPR is initiated in the absence of a State of Illinois DNR form.
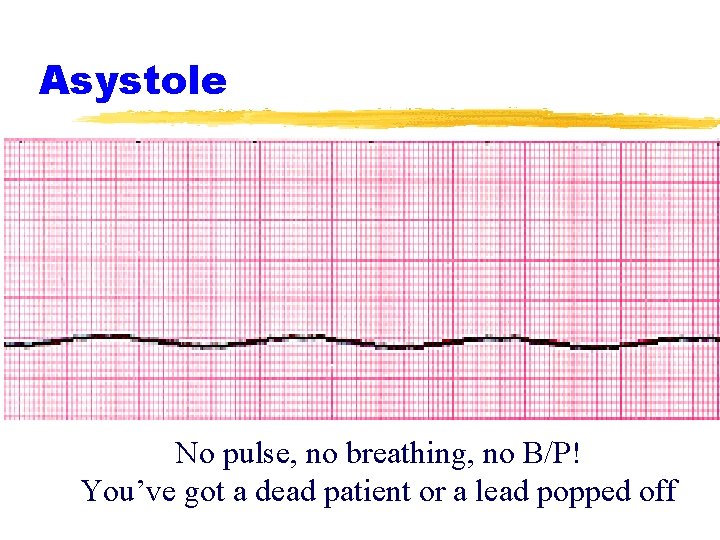
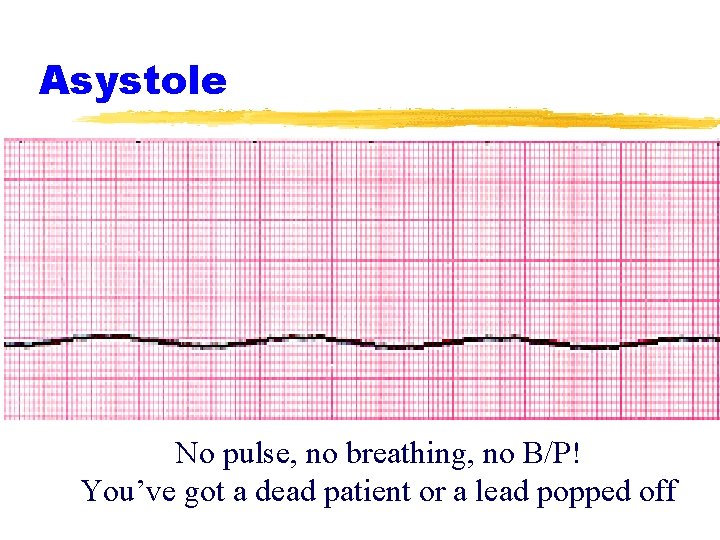
Asystole No pulse, no breathing, no B/P! You’ve got a dead patient or a lead popped off

Asystole and Defibrillation z. The goal in defibrillation is trying to allow the dominant pacemaker (preferably the SA node) to take over pacemaker duties z. When you defibrillate a patient, you place them into asystole z. So, the patient in asystole does not need defibrillation (they’re already there!) z. The patient in PEA has electrical activity and defibrillation would interfere with the one thing that is working for them!
PEA z. A clinical situation in which there is organized electrical activity (other than VT) viewed on the monitor but there is no palpable pulse & no breathing z. In the absence of a palpable pulse, the patient needs high quality CPR z. Focus on the causes (6 H’s and 5 T’s) as you perform CPR and administer medications
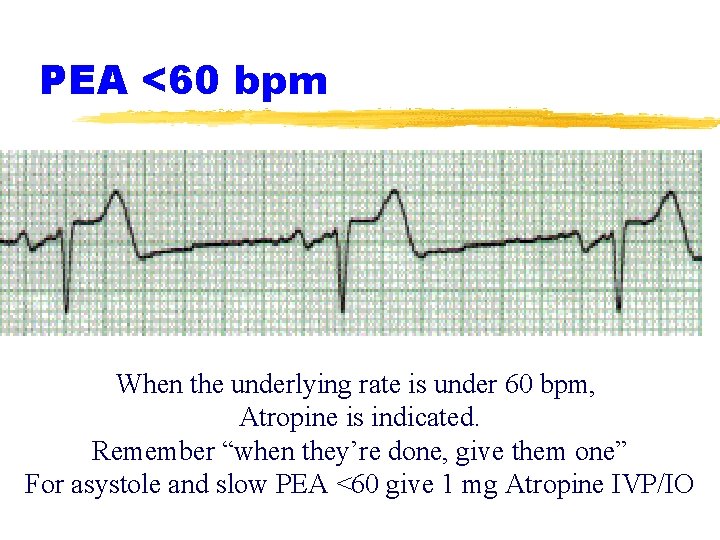
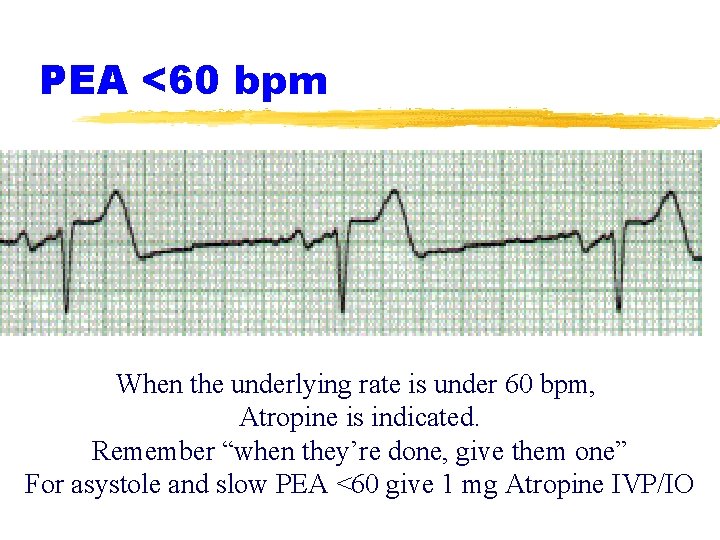
PEA <60 bpm When the underlying rate is under 60 bpm, Atropine is indicated. Remember “when they’re done, give them one” For asystole and slow PEA <60 give 1 mg Atropine IVP/IO
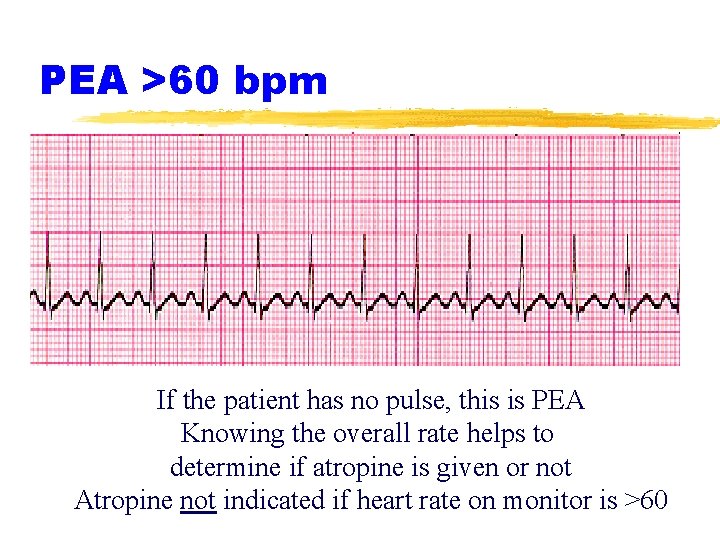
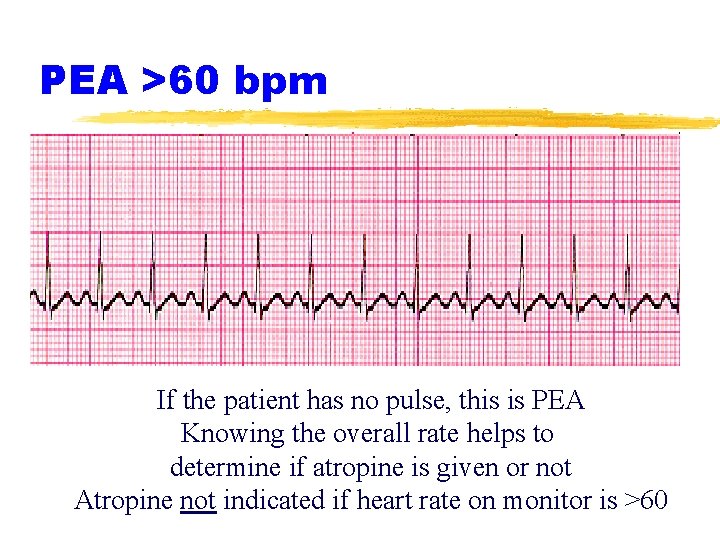
PEA >60 bpm If the patient has no pulse, this is PEA Knowing the overall rate helps to determine if atropine is given or not Atropine not indicated if heart rate on monitor is >60
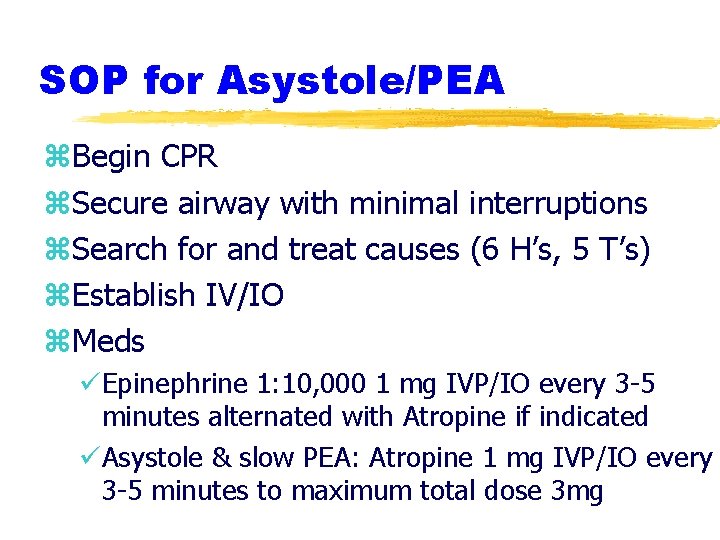
SOP for Asystole/PEA z. Begin CPR z. Secure airway with minimal interruptions z. Search for and treat causes (6 H’s, 5 T’s) z. Establish IV/IO z. Meds üEpinephrine 1: 10, 000 1 mg IVP/IO every 3 -5 minutes alternated with Atropine if indicated üAsystole & slow PEA: Atropine 1 mg IVP/IO every 3 -5 minutes to maximum total dose 3 mg

Medications - Epinephrine z. Stimulates vasoconstriction z. Supports improved blood flow to the heart and brain z. Can place a strain on the heart (this is adrenaline!) by heart rate and strength of contractility (more blood squeezed out) z. Relatively short half-life so needs to be repeated frequently (every 3 -5 minutes) z. There is no maximum
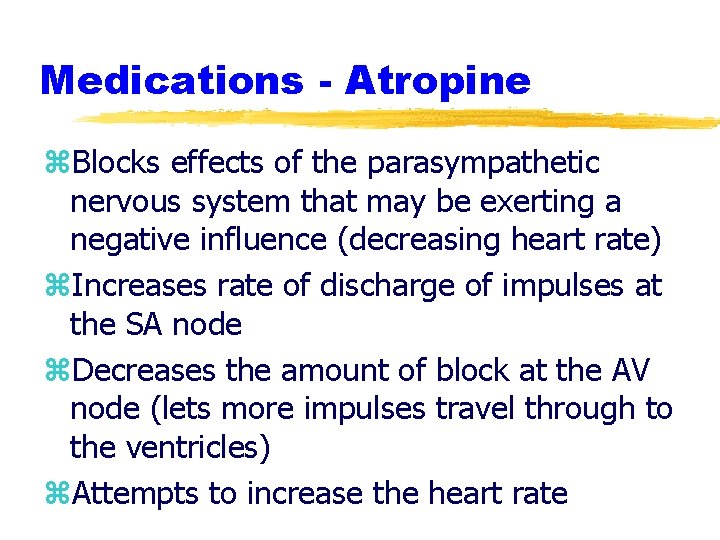
Medications - Atropine z. Blocks effects of the parasympathetic nervous system that may be exerting a negative influence (decreasing heart rate) z. Increases rate of discharge of impulses at the SA node z. Decreases the amount of block at the AV node (lets more impulses travel through to the ventricles) z. Attempts to increase the heart rate
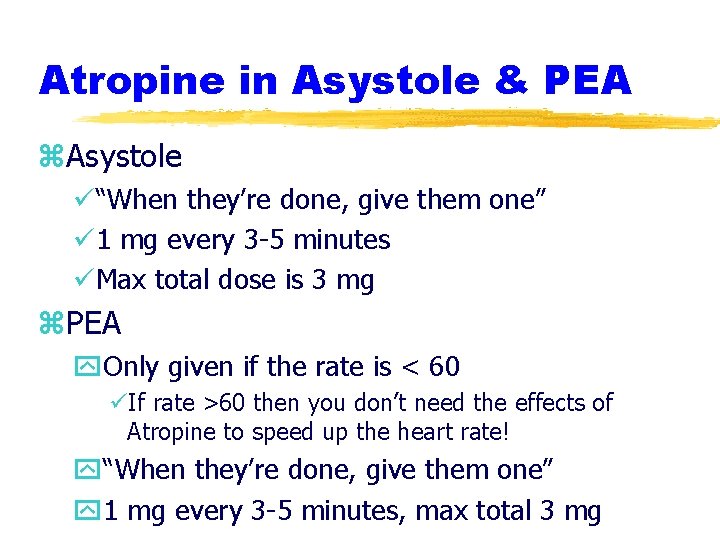
Atropine in Asystole & PEA z. Asystole ü“When they’re done, give them one” ü 1 mg every 3 -5 minutes üMax total dose is 3 mg z. PEA y. Only given if the rate is < 60 üIf rate >60 then you don’t need the effects of Atropine to speed up the heart rate! y“When they’re done, give them one” y 1 mg every 3 -5 minutes, max total 3 mg
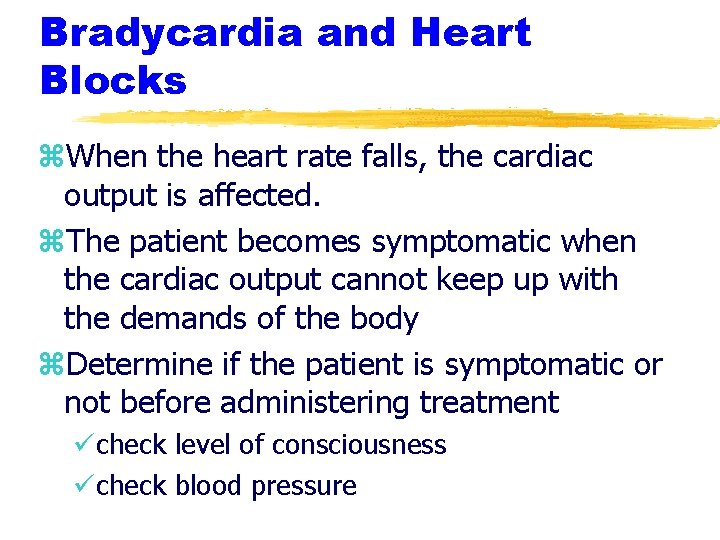
Bradycardia and Heart Blocks z. When the heart rate falls, the cardiac output is affected. z. The patient becomes symptomatic when the cardiac output cannot keep up with the demands of the body z. Determine if the patient is symptomatic or not before administering treatment ücheck level of consciousness ücheck blood pressure
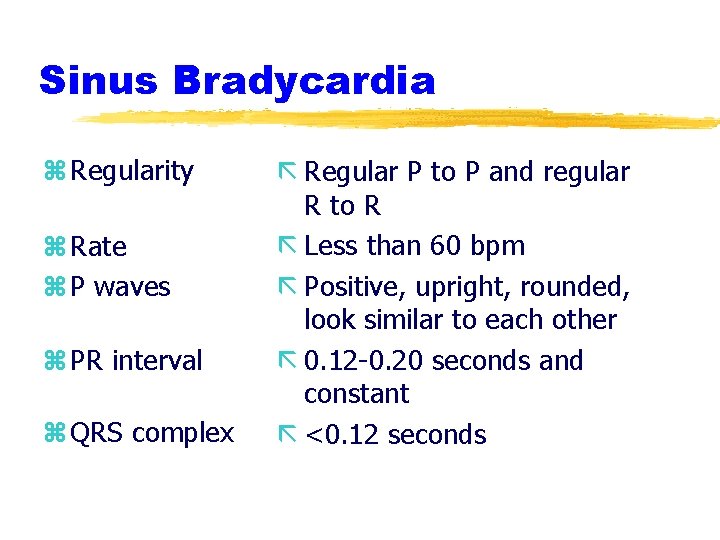
Sinus Bradycardia z Regularity z Rate z P waves z PR interval z QRS complex ã Regular P to P and regular R to R ã Less than 60 bpm ã Positive, upright, rounded, look similar to each other ã 0. 12 -0. 20 seconds and constant ã <0. 12 seconds

Sinus Bradycardia Treatment indicated if the patient is symptomatic EMS needs to provide a thorough assessment to make an accurate clinical decision
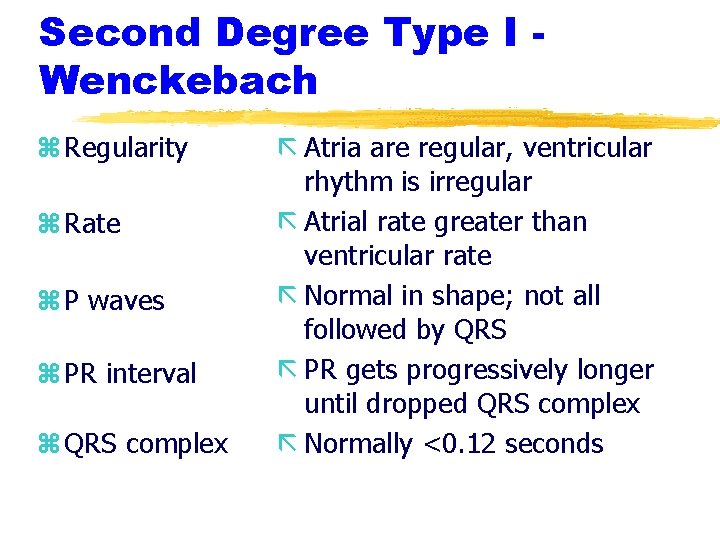
Second Degree Type I Wenckebach z Regularity z Rate z P waves z PR interval z QRS complex ã Atria are regular, ventricular rhythm is irregular ã Atrial rate greater than ventricular rate ã Normal in shape; not all followed by QRS ã PR gets progressively longer until dropped QRS complex ã Normally <0. 12 seconds
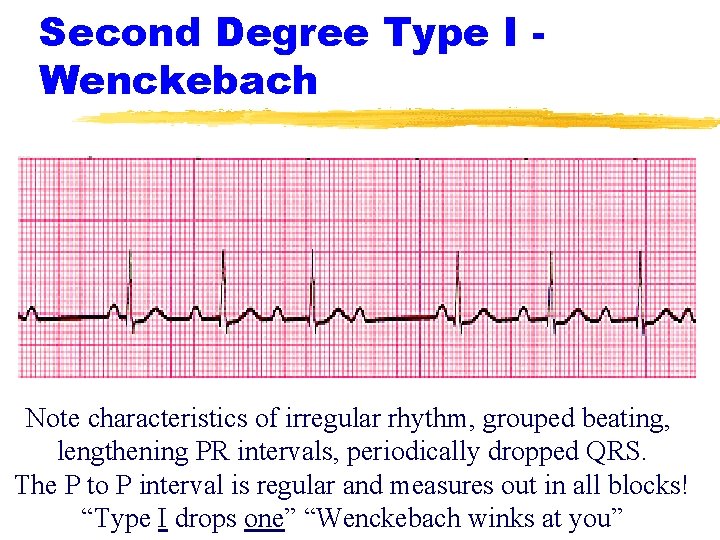
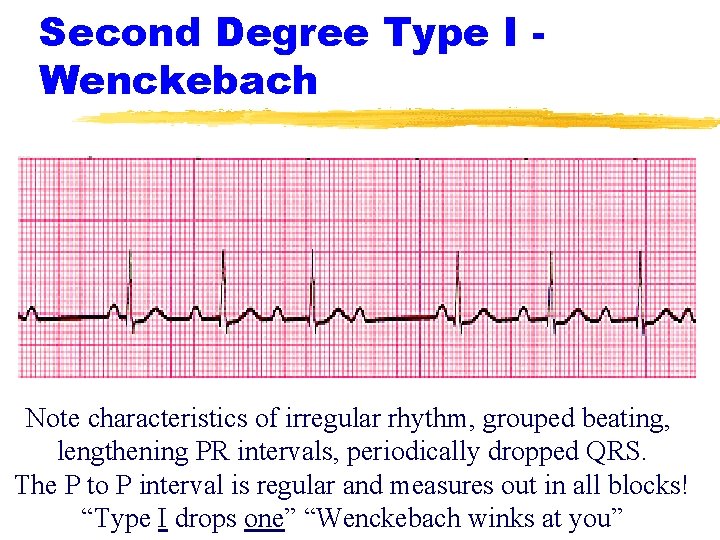
Second Degree Type I Wenckebach Note characteristics of irregular rhythm, grouped beating, lengthening PR intervals, periodically dropped QRS. The P to P interval is regular and measures out in all blocks! “Type I drops one” “Wenckebach winks at you”
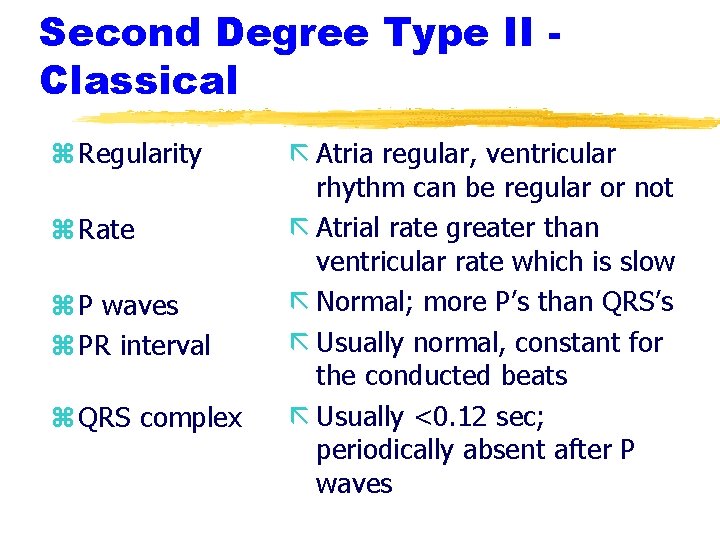
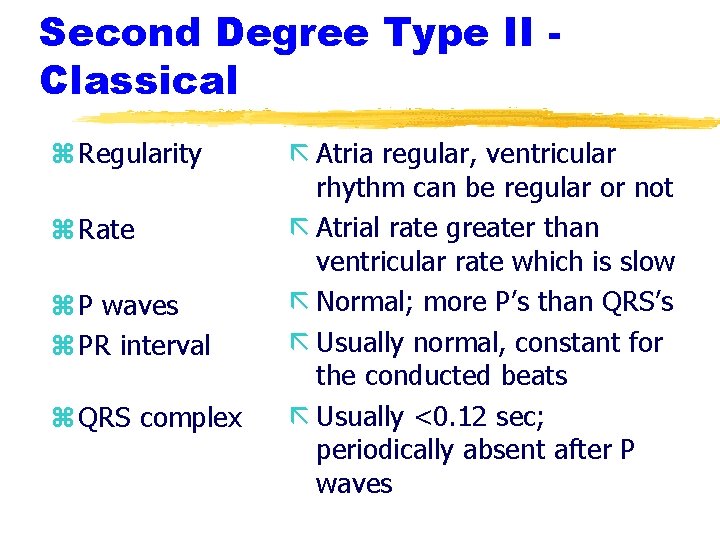
Second Degree Type II Classical z Regularity z Rate z P waves z PR interval z QRS complex ã Atria regular, ventricular rhythm can be regular or not ã Atrial rate greater than ventricular rate which is slow ã Normal; more P’s than QRS’s ã Usually normal, constant for the conducted beats ã Usually <0. 12 sec; periodically absent after P waves

Second degree Type II Classical This rhythm can have a variable block or can have a set pattern (ie: 2: 1; 3: 1, etc). The slower the heart rate, the more symptomatic the patient. Treatment with Atropine versus TCP based on width of QRS. Think “Type II is 2: 1” (but know block can be 3: 1, etc)
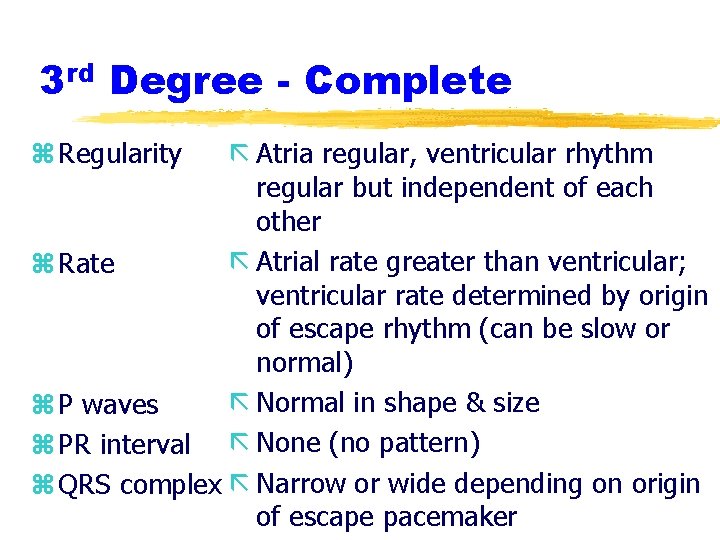
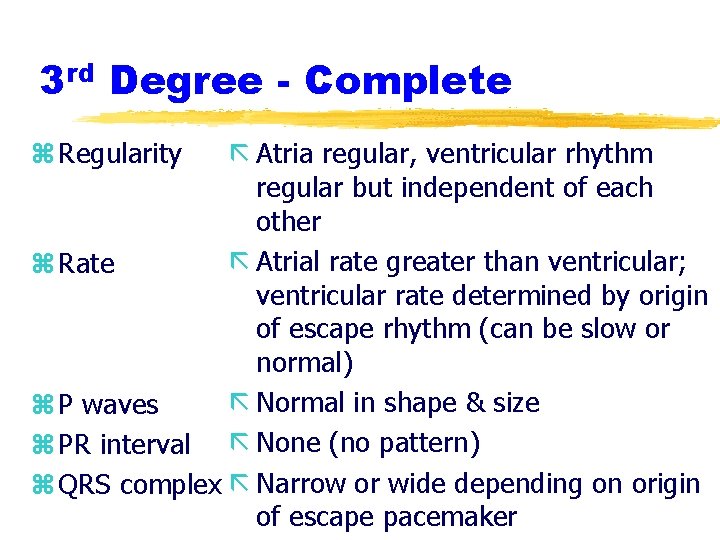
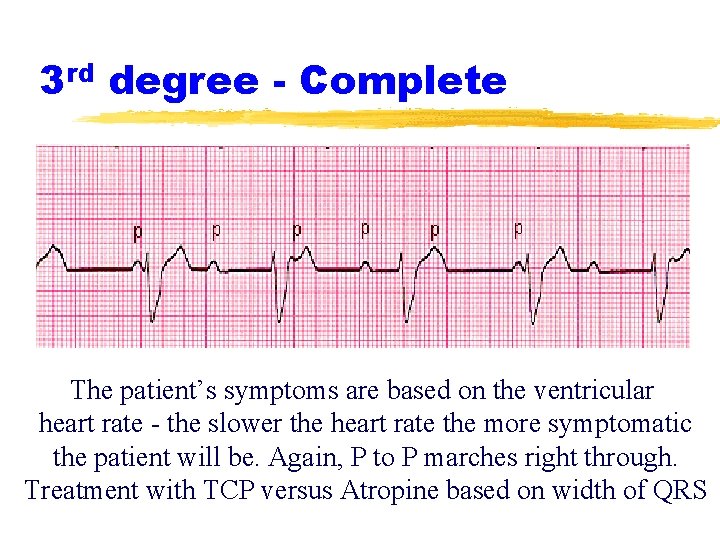
3 rd Degree - Complete z Regularity ã Atria regular, ventricular rhythm regular but independent of each other ã Atrial rate greater than ventricular; z Rate ventricular rate determined by origin of escape rhythm (can be slow or normal) ã Normal in shape & size z P waves z PR interval ã None (no pattern) z QRS complex ã Narrow or wide depending on origin of escape pacemaker
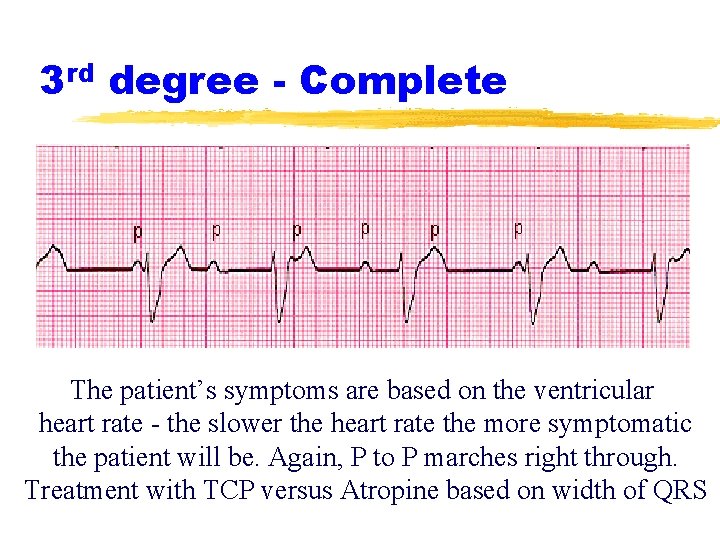
3 rd degree - Complete The patient’s symptoms are based on the ventricular heart rate - the slower the heart rate the more symptomatic the patient will be. Again, P to P marches right through. Treatment with TCP versus Atropine based on width of QRS
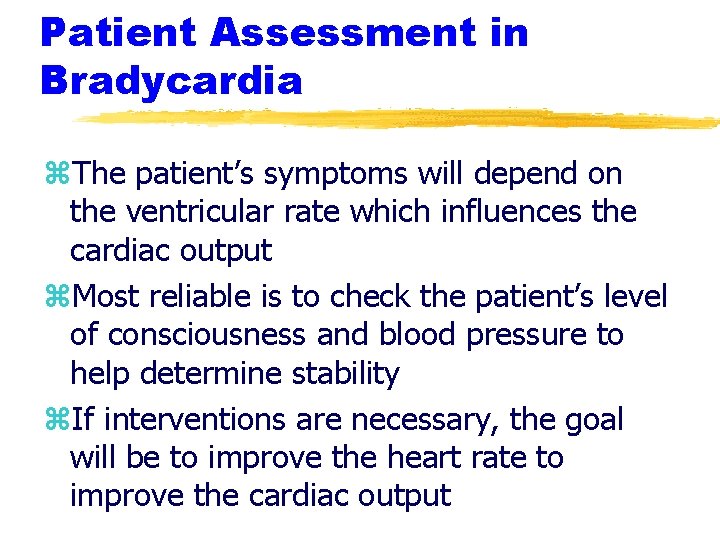
Patient Assessment in Bradycardia z. The patient’s symptoms will depend on the ventricular rate which influences the cardiac output z. Most reliable is to check the patient’s level of consciousness and blood pressure to help determine stability z. If interventions are necessary, the goal will be to improve the heart rate to improve the cardiac output
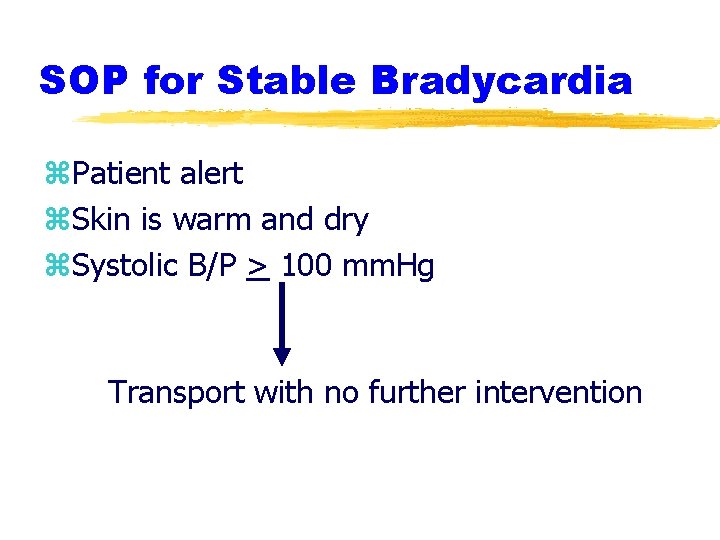
SOP for Stable Bradycardia z. Patient alert z. Skin is warm and dry z. Systolic B/P > 100 mm. Hg Transport with no further intervention
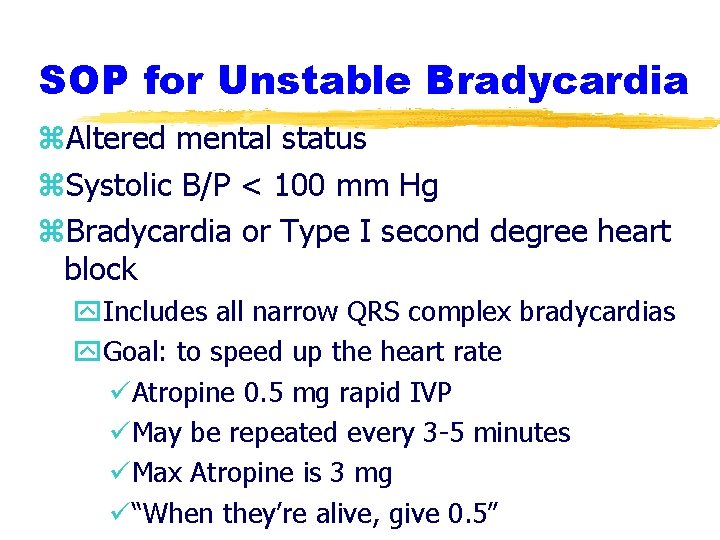
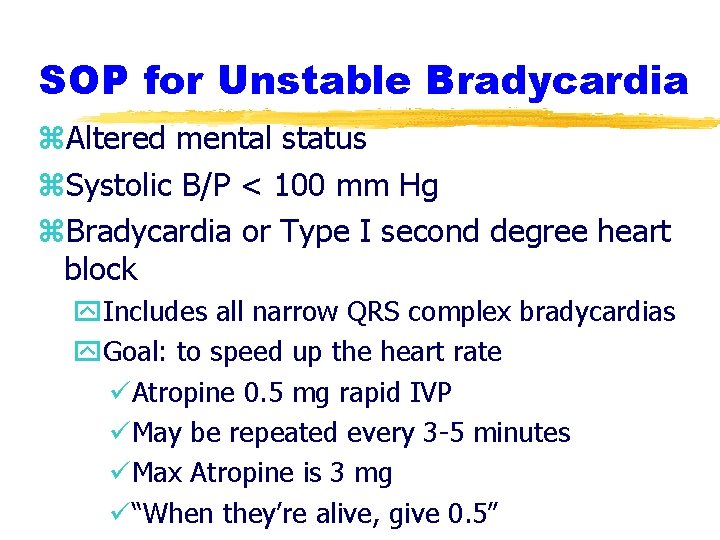
SOP for Unstable Bradycardia z. Altered mental status z. Systolic B/P < 100 mm Hg z. Bradycardia or Type I second degree heart block y. Includes all narrow QRS complex bradycardias y. Goal: to speed up the heart rate üAtropine 0. 5 mg rapid IVP üMay be repeated every 3 -5 minutes üMax Atropine is 3 mg ü“When they’re alive, give 0. 5”
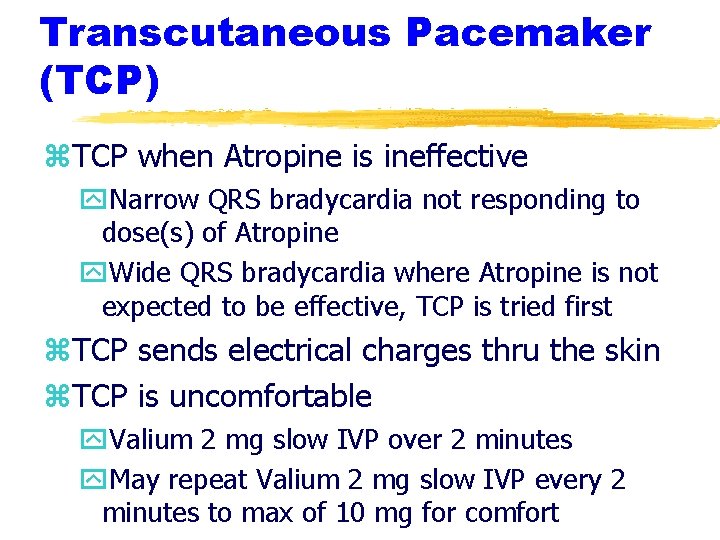
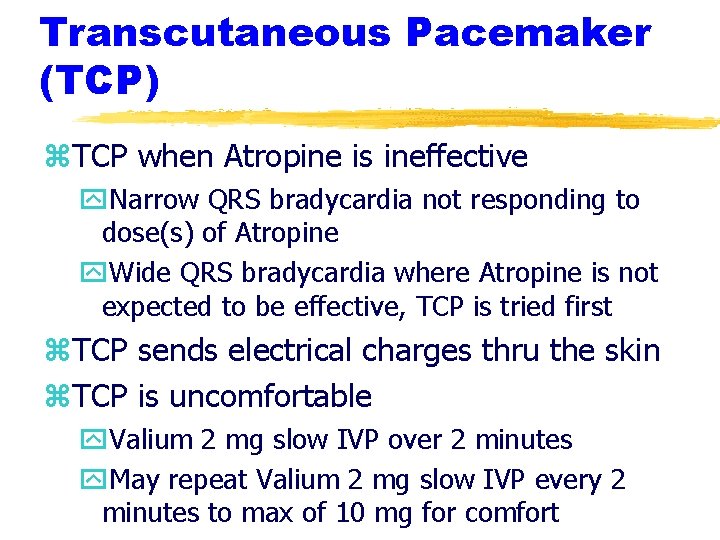
Transcutaneous Pacemaker (TCP) z. TCP when Atropine is ineffective y. Narrow QRS bradycardia not responding to dose(s) of Atropine y. Wide QRS bradycardia where Atropine is not expected to be effective, TCP is tried first z. TCP sends electrical charges thru the skin z. TCP is uncomfortable y. Valium 2 mg slow IVP over 2 minutes y. May repeat Valium 2 mg slow IVP every 2 minutes to max of 10 mg for comfort
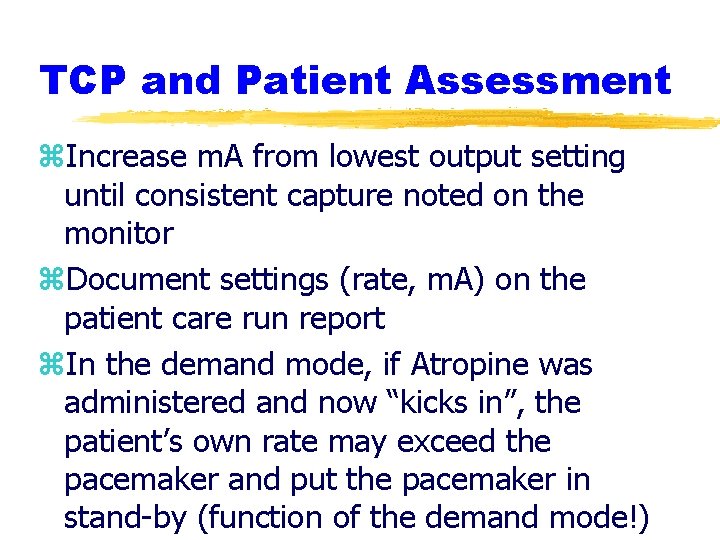
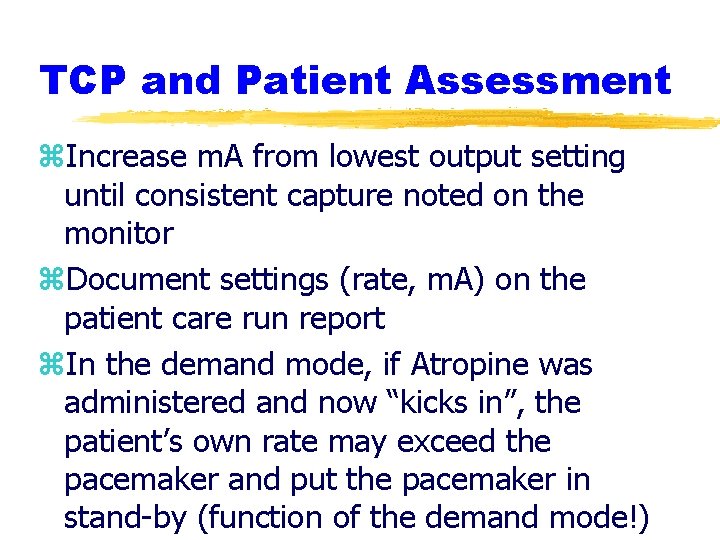
TCP and Patient Assessment z. Increase m. A from lowest output setting until consistent capture noted on the monitor z. Document settings (rate, m. A) on the patient care run report z. In the demand mode, if Atropine was administered and now “kicks in”, the patient’s own rate may exceed the pacemaker and put the pacemaker in stand-by (function of the demand mode!)

TCP with Capture Paced Rhythm Observed is one to one capture. Consider sedation with Valium to make the patient more comfortable.

SOP for Wide QRS Bradycardia z. Typically refers to Type II second degree heart block and 3 rd degree (complete) z. Atropine is not effective in wide QRS complex bradycardia (origin most likely below bundle of His if QRS is wide) z. Begin TCP as soon as possible z. If TCP not effective, can give Atropine 0. 5 mg rapid IVP and repeat every 3 -5 minutes to a max of 3 mg
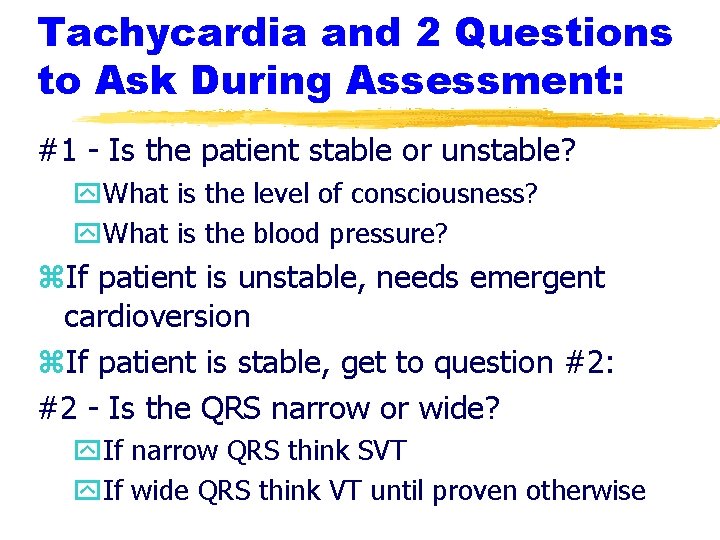
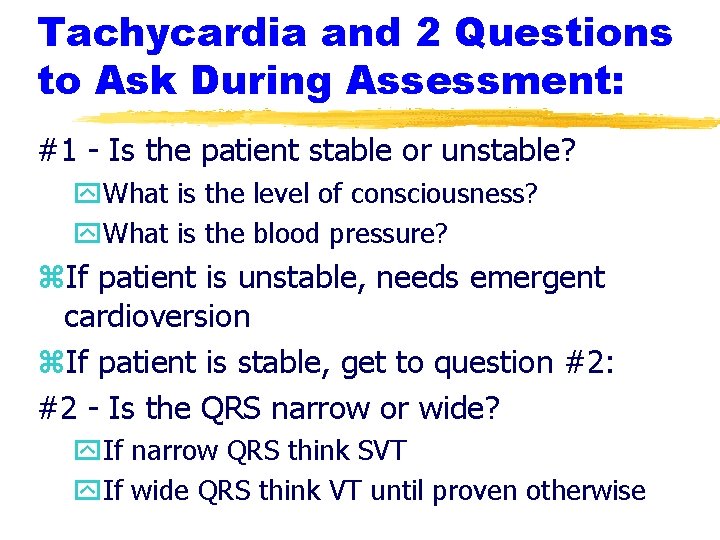
Tachycardia and 2 Questions to Ask During Assessment: #1 - Is the patient stable or unstable? y. What is the level of consciousness? y. What is the blood pressure? z. If patient is unstable, needs emergent cardioversion z. If patient is stable, get to question #2: #2 - Is the QRS narrow or wide? y. If narrow QRS think SVT y. If wide QRS think VT until proven otherwise
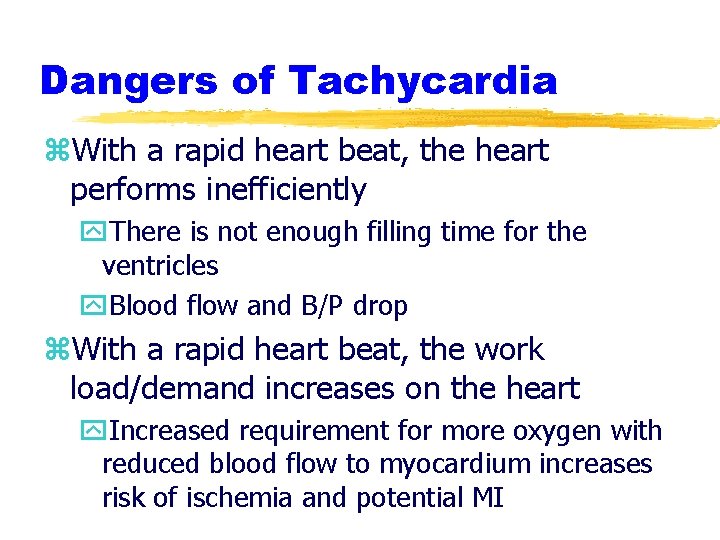
Dangers of Tachycardia z. With a rapid heart beat, the heart performs inefficiently y. There is not enough filling time for the ventricles y. Blood flow and B/P drop z. With a rapid heart beat, the work load/demand increases on the heart y. Increased requirement for more oxygen with reduced blood flow to myocardium increases risk of ischemia and potential MI
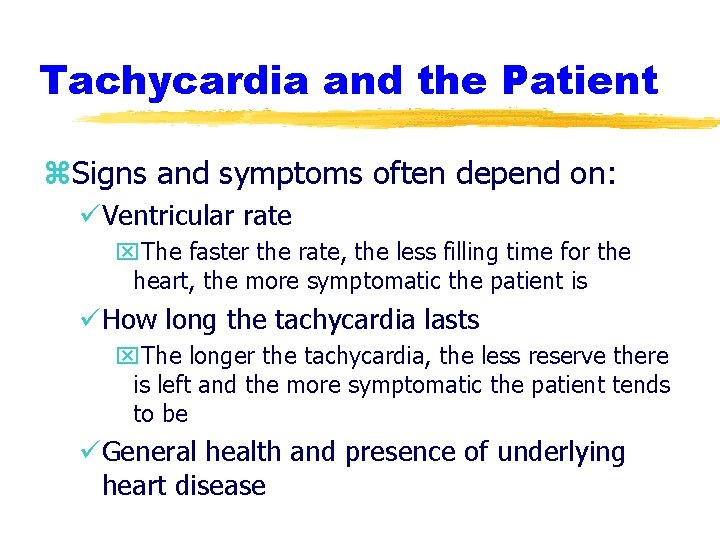
Tachycardia and the Patient z. Signs and symptoms often depend on: üVentricular rate x. The faster the rate, the less filling time for the heart, the more symptomatic the patient is üHow long the tachycardia lasts x. The longer the tachycardia, the less reserve there is left and the more symptomatic the patient tends to be üGeneral health and presence of underlying heart disease
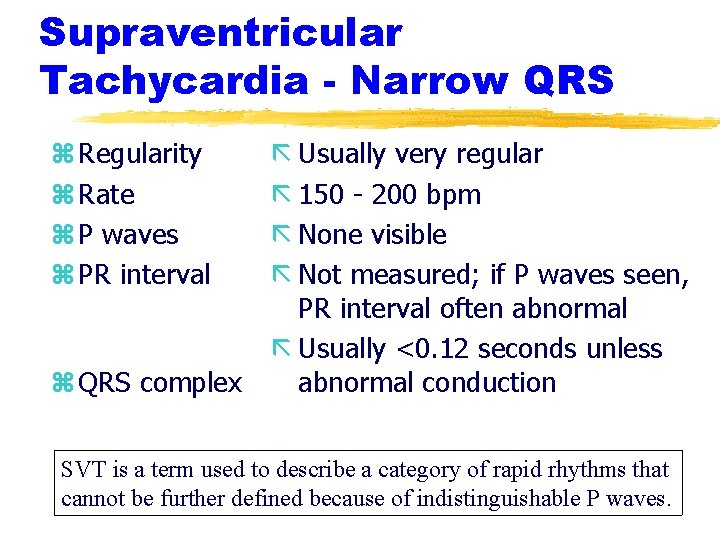
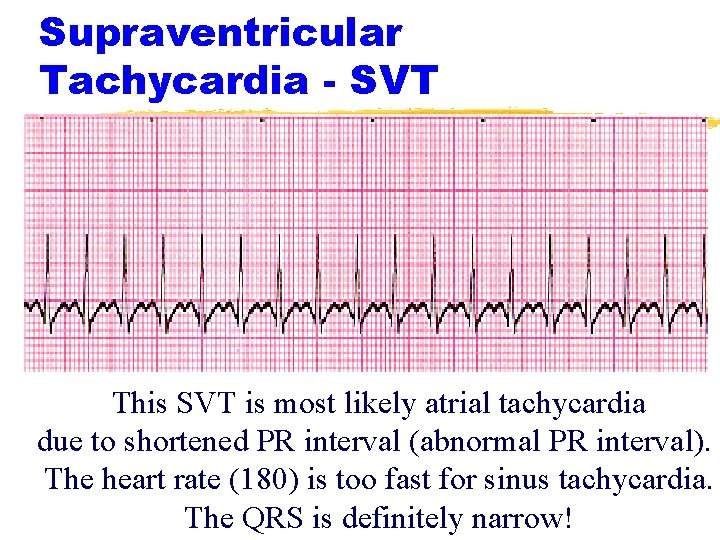
Supraventricular Tachycardia - Narrow QRS z Regularity z Rate z P waves z PR interval z QRS complex ã Usually very regular ã 150 - 200 bpm ã None visible ã Not measured; if P waves seen, PR interval often abnormal ã Usually <0. 12 seconds unless abnormal conduction SVT is a term used to describe a category of rapid rhythms that cannot be further defined because of indistinguishable P waves.
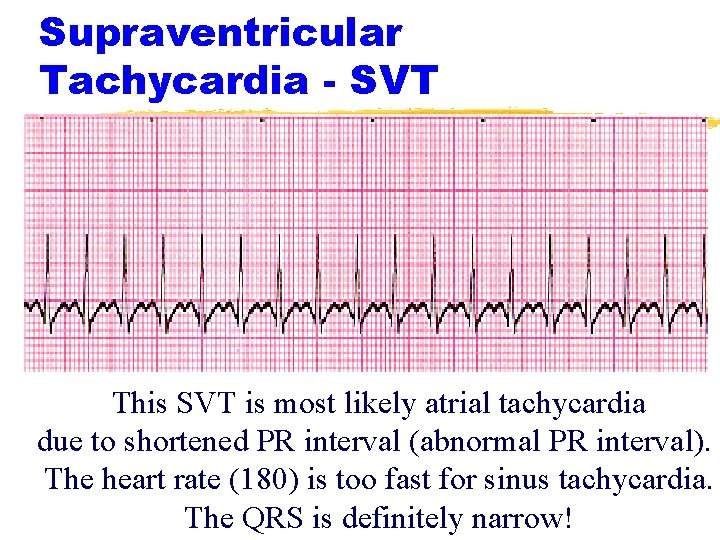
Supraventricular Tachycardia - SVT This SVT is most likely atrial tachycardia due to shortened PR interval (abnormal PR interval). The heart rate (180) is too fast for sinus tachycardia. The QRS is definitely narrow!
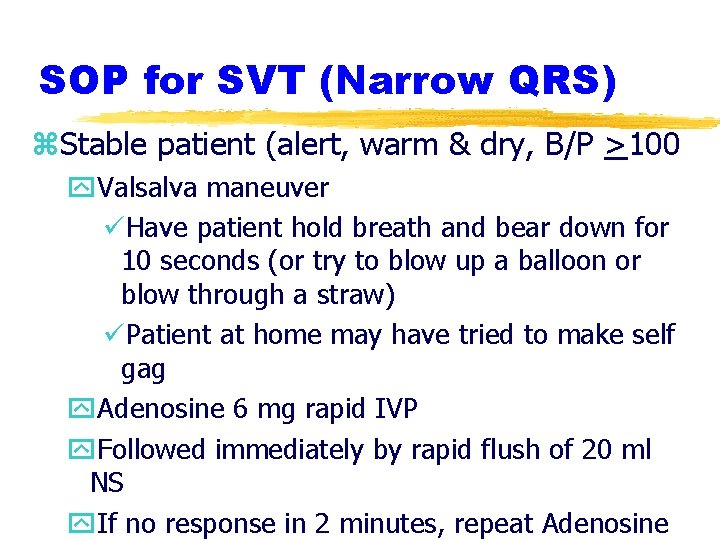
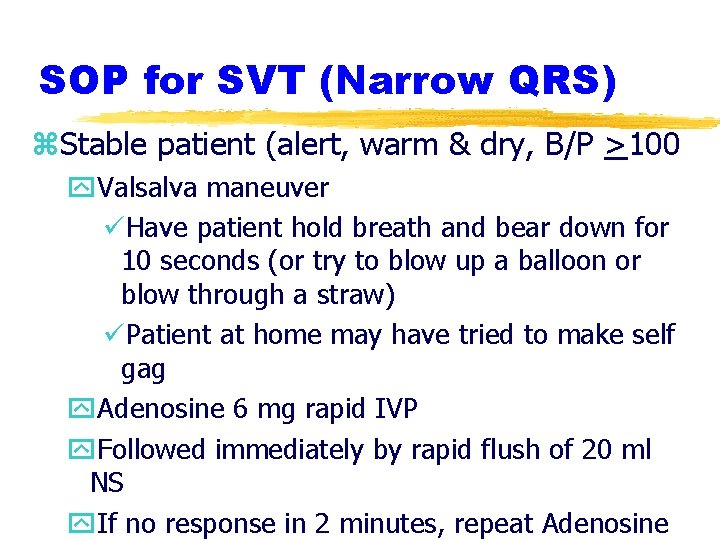
SOP for SVT (Narrow QRS) z. Stable patient (alert, warm & dry, B/P >100 y. Valsalva maneuver üHave patient hold breath and bear down for 10 seconds (or try to blow up a balloon or blow through a straw) üPatient at home may have tried to make self gag y. Adenosine 6 mg rapid IVP y. Followed immediately by rapid flush of 20 ml NS y. If no response in 2 minutes, repeat Adenosine

Adenosine for SVT z. Antiarrhythmic z. Decreases heart rate at SA node z. Slows conduction thru AV node z. Does not convert atrial fibrillation, atrial flutter or VT z. Short half life (10 seconds) so start IV in AC area (preferably right), must be given rapidly followed immediately with saline flush
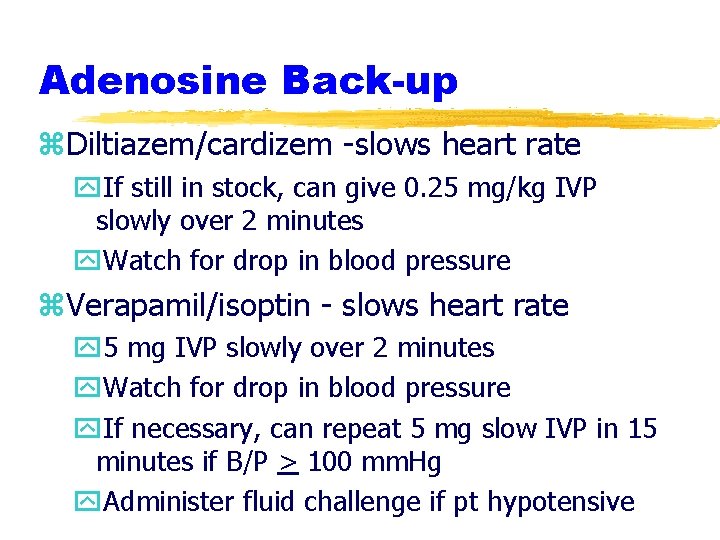
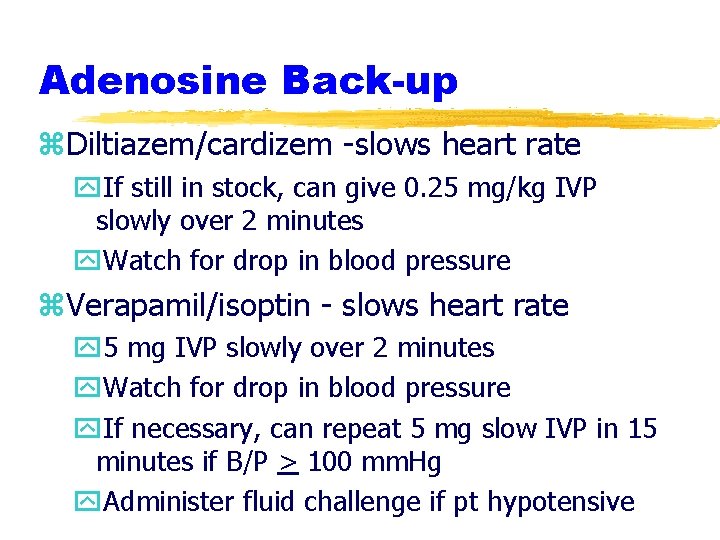
Adenosine Back-up z. Diltiazem/cardizem -slows heart rate y. If still in stock, can give 0. 25 mg/kg IVP slowly over 2 minutes y. Watch for drop in blood pressure z. Verapamil/isoptin - slows heart rate y 5 mg IVP slowly over 2 minutes y. Watch for drop in blood pressure y. If necessary, can repeat 5 mg slow IVP in 15 minutes if B/P > 100 mm. Hg y. Administer fluid challenge if pt hypotensive
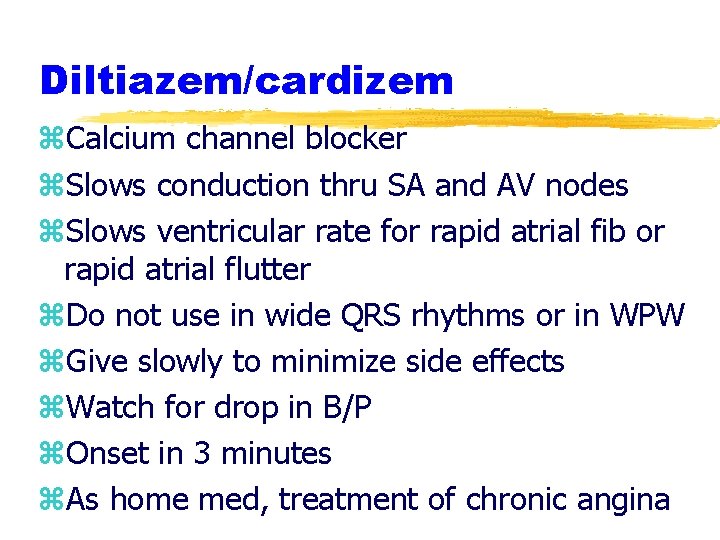
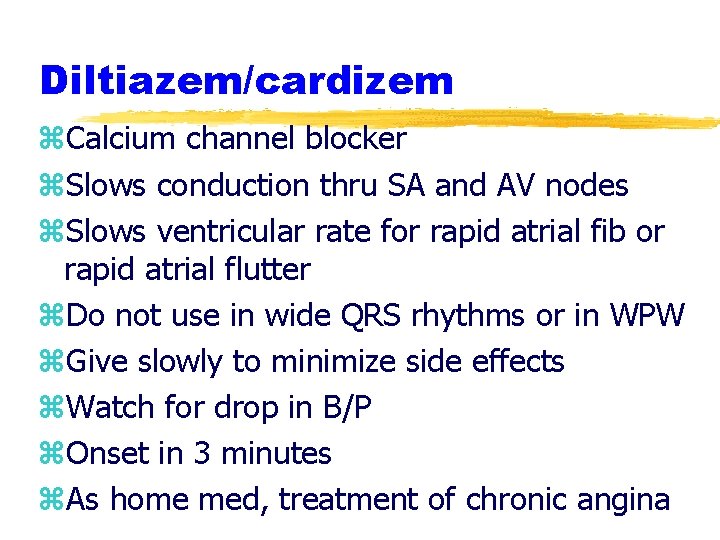
Diltiazem/cardizem z. Calcium channel blocker z. Slows conduction thru SA and AV nodes z. Slows ventricular rate for rapid atrial fib or rapid atrial flutter z. Do not use in wide QRS rhythms or in WPW z. Give slowly to minimize side effects z. Watch for drop in B/P z. Onset in 3 minutes z. As home med, treatment of chronic angina
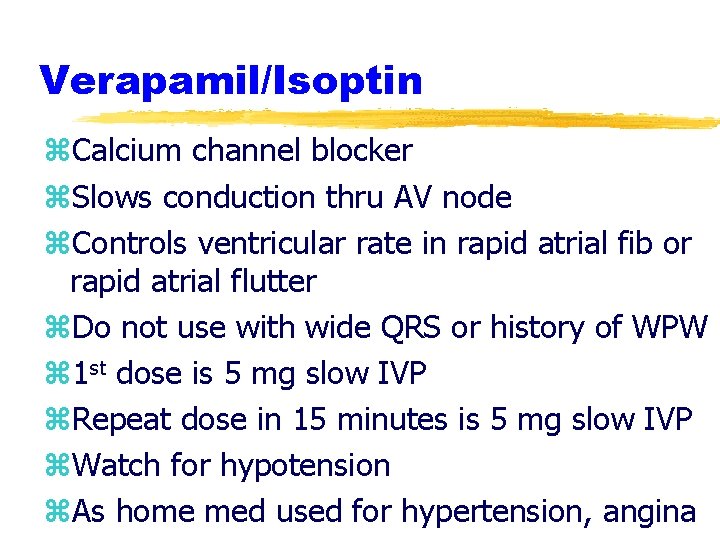
Verapamil/Isoptin z. Calcium channel blocker z. Slows conduction thru AV node z. Controls ventricular rate in rapid atrial fib or rapid atrial flutter z. Do not use with wide QRS or history of WPW z 1 st dose is 5 mg slow IVP z. Repeat dose in 15 minutes is 5 mg slow IVP z. Watch for hypotension z. As home med used for hypertension, angina
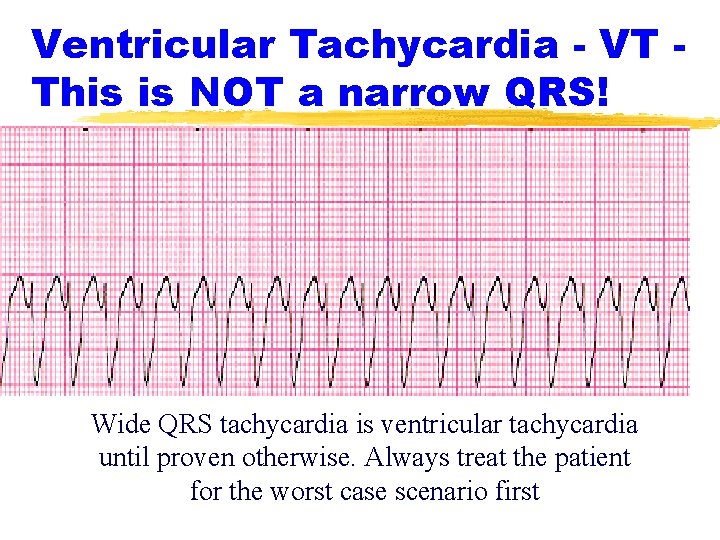
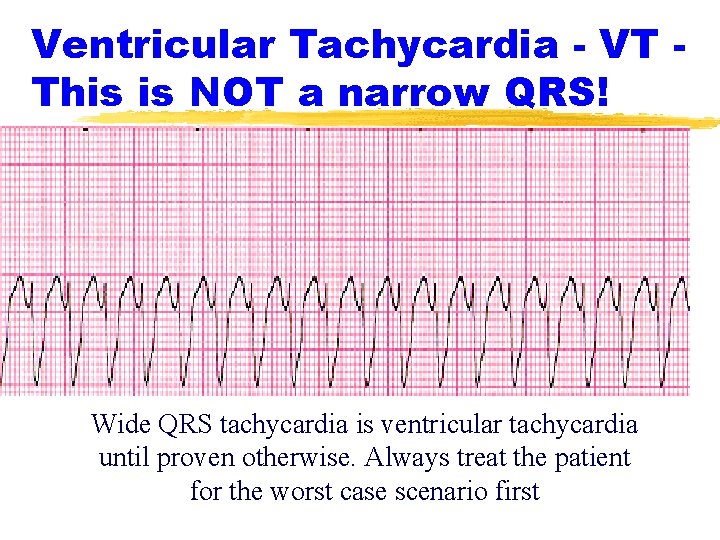
Ventricular Tachycardia - VT This is NOT a narrow QRS! Wide QRS tachycardia is ventricular tachycardia until proven otherwise. Always treat the patient for the worst case scenario first
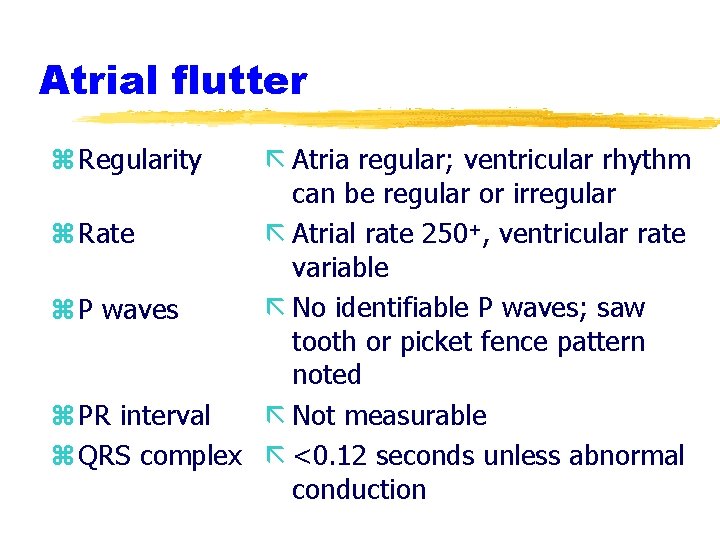
Atrial flutter z Regularity ã Atria regular; ventricular rhythm can be regular or irregular z Rate ã Atrial rate 250+, ventricular rate variable ã No identifiable P waves; saw z P waves tooth or picket fence pattern noted z PR interval ã Not measurable z QRS complex ã <0. 12 seconds unless abnormal conduction
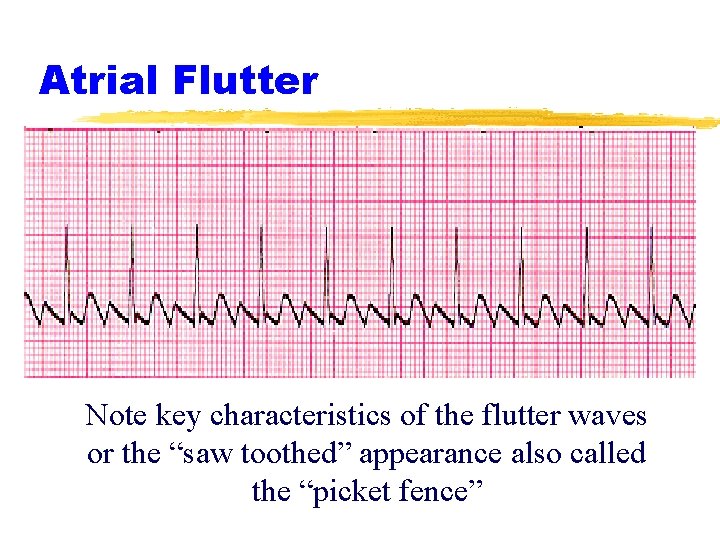
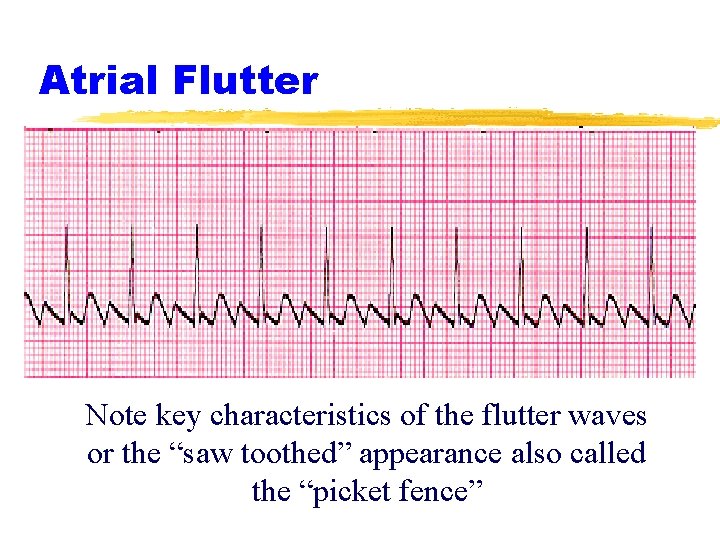
Atrial Flutter Note key characteristics of the flutter waves or the “saw toothed” appearance also called the “picket fence”
Atrial Fibrillation z Regularity z Rate ã Irregularly irregular ã Atrial rate 400 -600; ventricular rate variable ã No identifiable P waves z P waves ã None measured z PR interval z QRS complex ã 0. 12 seconds or less unless abnormal conduction
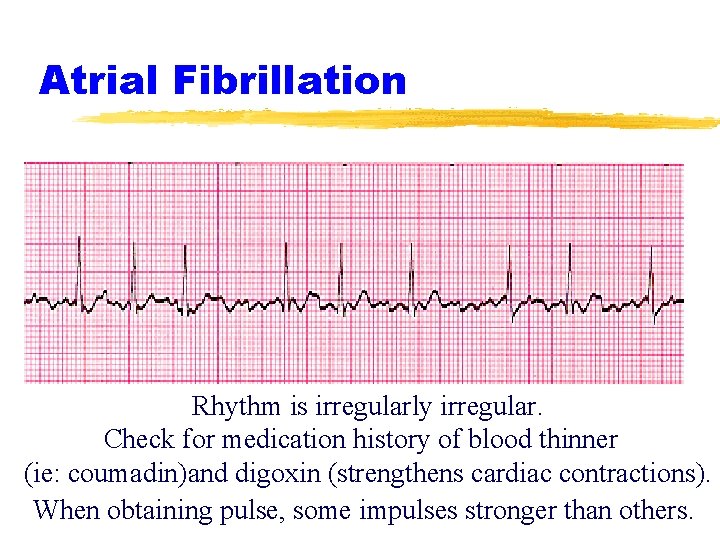
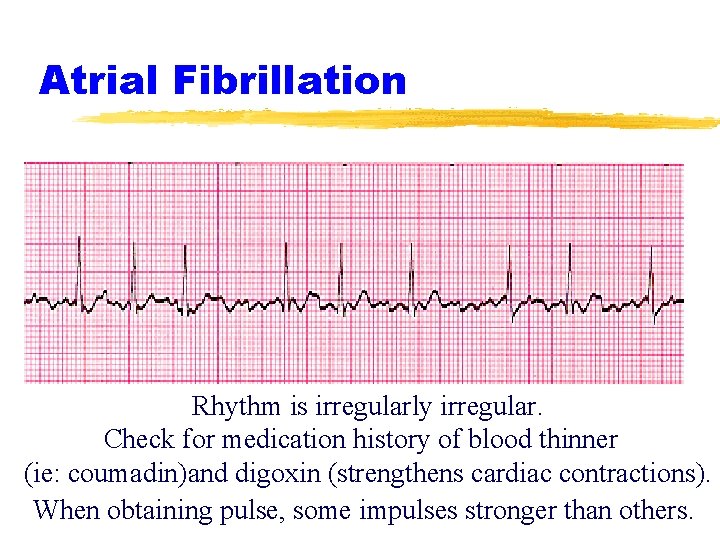
Atrial Fibrillation Rhythm is irregularly irregular. Check for medication history of blood thinner (ie: coumadin)and digoxin (strengthens cardiac contractions). When obtaining pulse, some impulses stronger than others.
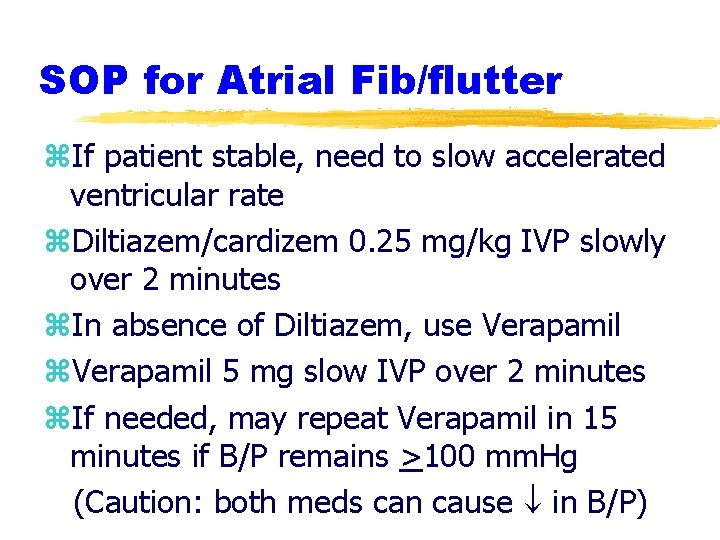
SOP for Atrial Fib/flutter z. If patient stable, need to slow accelerated ventricular rate z. Diltiazem/cardizem 0. 25 mg/kg IVP slowly over 2 minutes z. In absence of Diltiazem, use Verapamil z. Verapamil 5 mg slow IVP over 2 minutes z. If needed, may repeat Verapamil in 15 minutes if B/P remains >100 mm. Hg (Caution: both meds can cause in B/P)
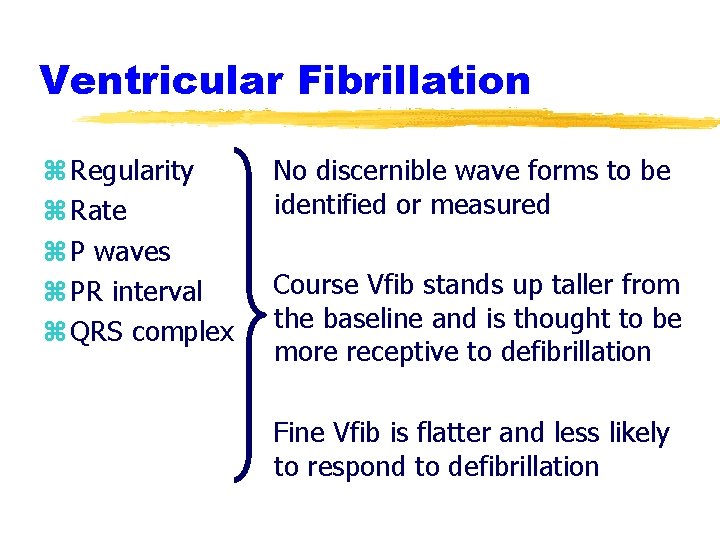
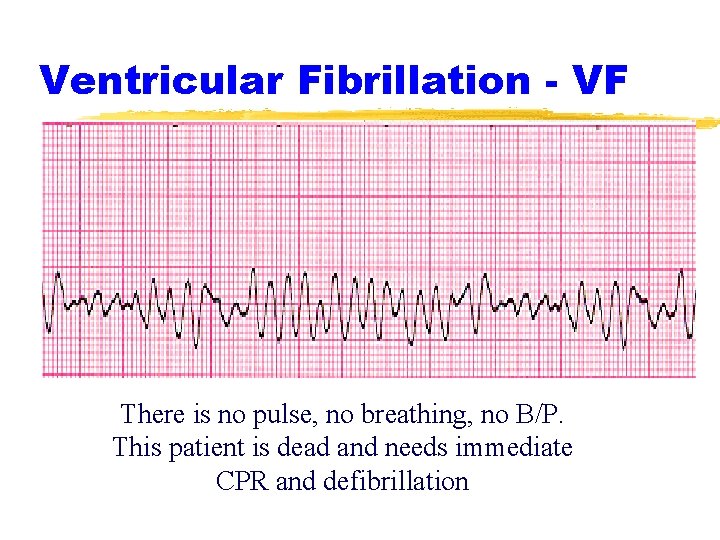
Ventricular Fibrillation z Regularity z Rate z P waves z PR interval z QRS complex No discernible wave forms to be identified or measured Course Vfib stands up taller from the baseline and is thought to be more receptive to defibrillation Fine Vfib is flatter and less likely to respond to defibrillation
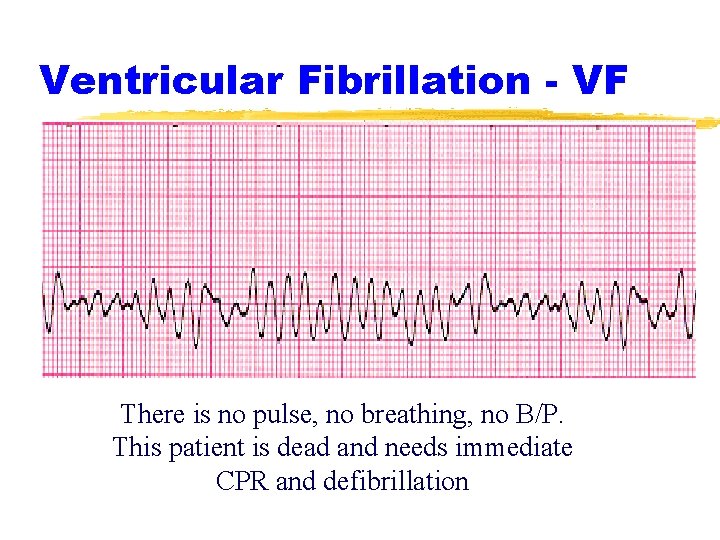
Ventricular Fibrillation - VF There is no pulse, no breathing, no B/P. This patient is dead and needs immediate CPR and defibrillation

Pulseless VT z. This is not PEA! z. PEA does not receive defibrillation z. Pulseless VT is treated just like VF and requires appropriate defibrillation attempts z. If pulseless VT deteriorates to VF, continue with the same SOP
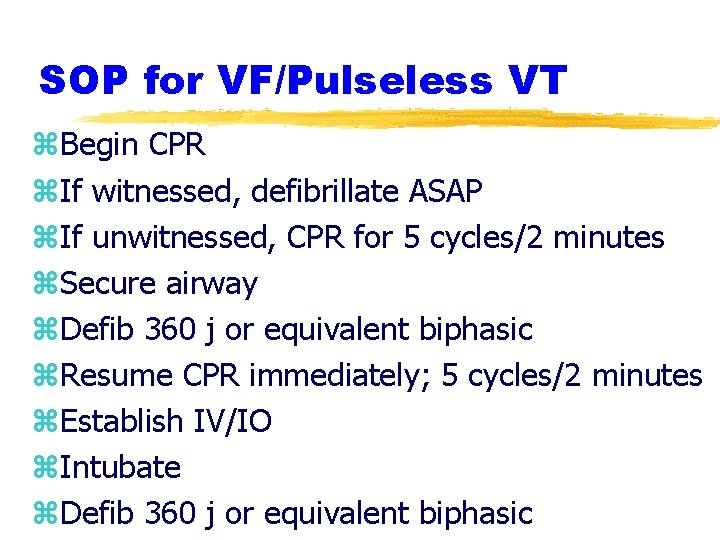
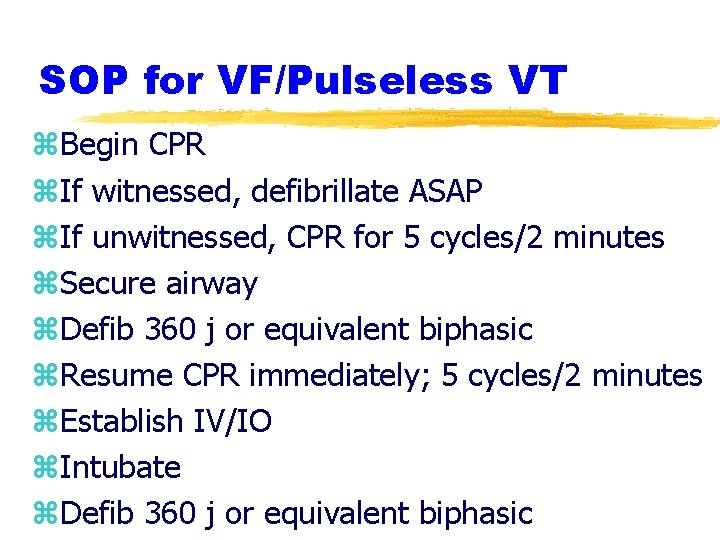
SOP for VF/Pulseless VT z. Begin CPR z. If witnessed, defibrillate ASAP z. If unwitnessed, CPR for 5 cycles/2 minutes z. Secure airway z. Defib 360 j or equivalent biphasic z. Resume CPR immediately; 5 cycles/2 minutes z. Establish IV/IO z. Intubate z. Defib 360 j or equivalent biphasic
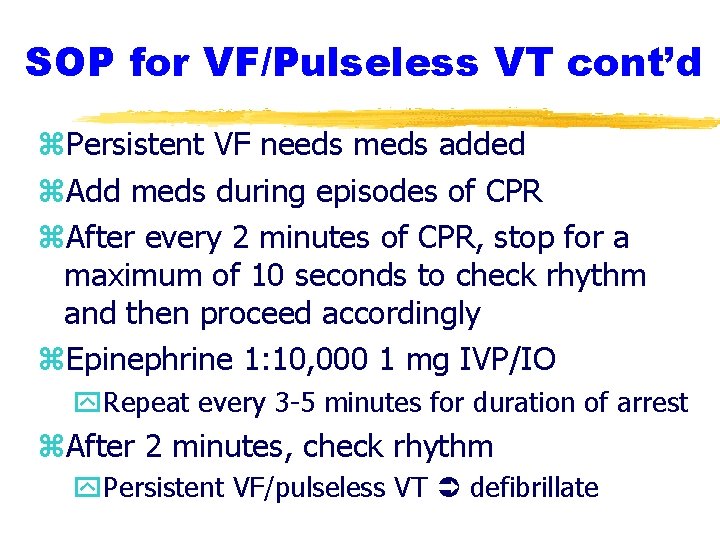
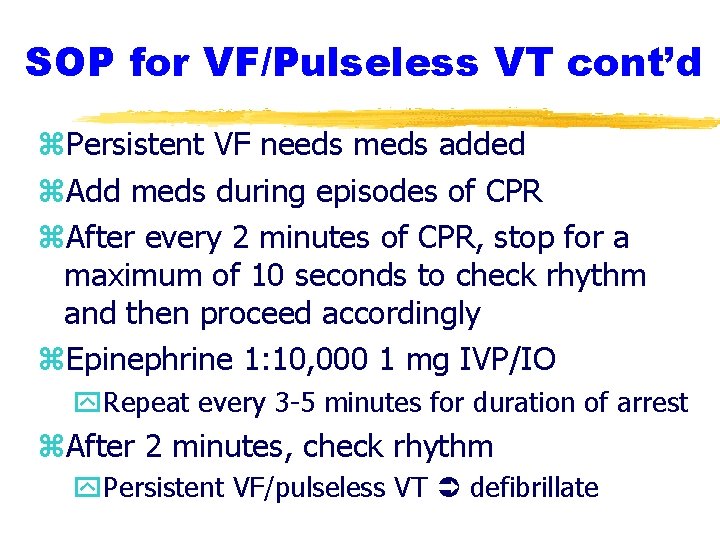
SOP for VF/Pulseless VT cont’d z. Persistent VF needs meds added z. Add meds during episodes of CPR z. After every 2 minutes of CPR, stop for a maximum of 10 seconds to check rhythm and then proceed accordingly z. Epinephrine 1: 10, 000 1 mg IVP/IO y. Repeat every 3 -5 minutes for duration of arrest z. After 2 minutes, check rhythm y. Persistent VF/pulseless VT defibrillate

SOP for VF/Pulseless VT cont’d z. Antidysrhythmics y. Choose one: Amiodarone or Lidocaine y. Do not mix use of these drugs - heart becomes more irritable y. After a repeat dose of antidysrhythmic, need medical control orders for more z. Amiodarone 1 st dose 300 mg IVP/IO z. Can repeat in 5 minutes at 150 mg IVP/IO z. Lidocaine 1. 5 mg/kg IVP/IO z. Can repeat in 5 minutes at 0. 75 mg/kg IVP
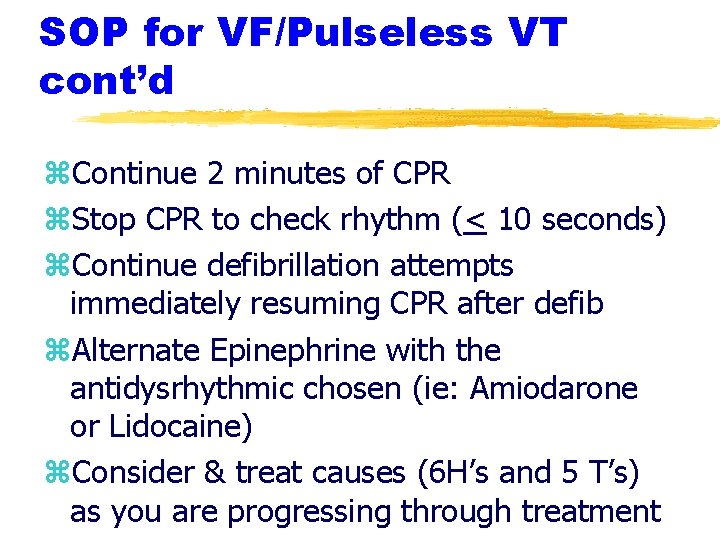
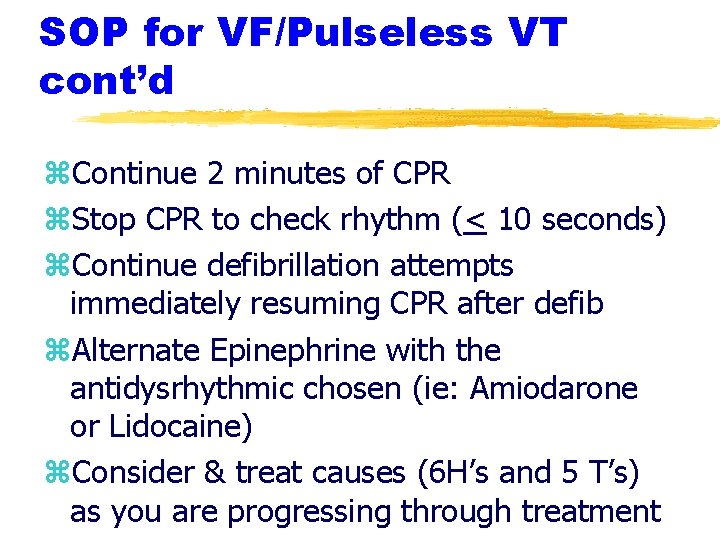
SOP for VF/Pulseless VT cont’d z. Continue 2 minutes of CPR z. Stop CPR to check rhythm (< 10 seconds) z. Continue defibrillation attempts immediately resuming CPR after defib z. Alternate Epinephrine with the antidysrhythmic chosen (ie: Amiodarone or Lidocaine) z. Consider & treat causes (6 H’s and 5 T’s) as you are progressing through treatment
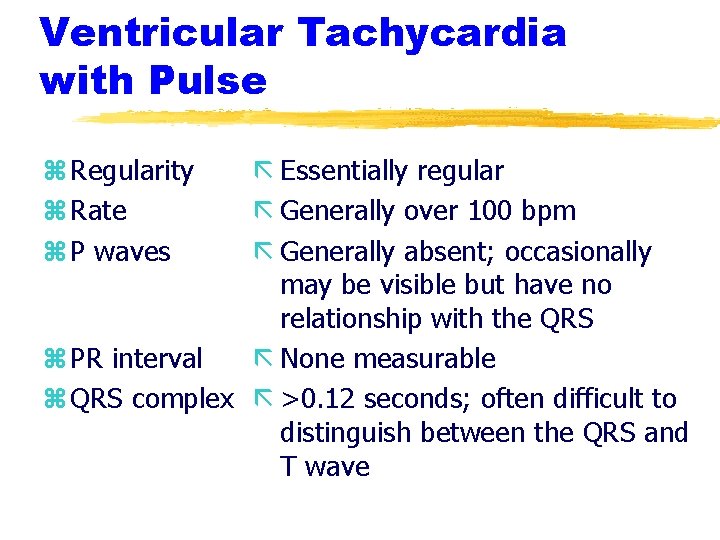
Ventricular Tachycardia with Pulse z Regularity z Rate z P waves ã Essentially regular ã Generally over 100 bpm ã Generally absent; occasionally may be visible but have no relationship with the QRS z PR interval ã None measurable z QRS complex ã >0. 12 seconds; often difficult to distinguish between the QRS and T wave
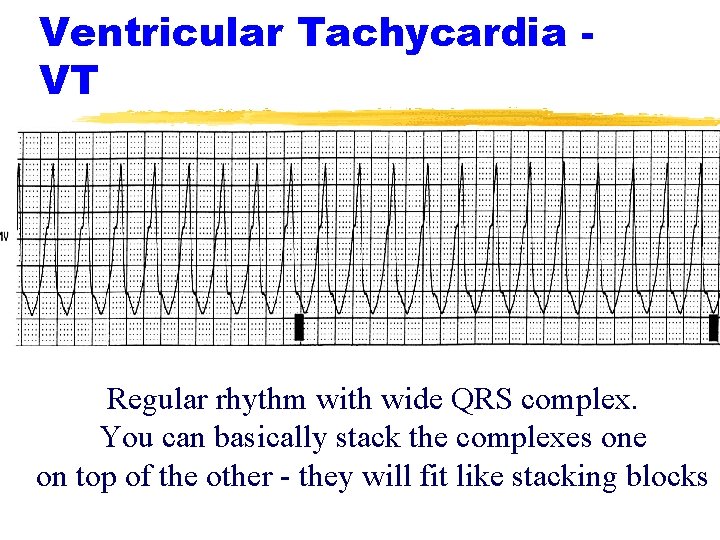
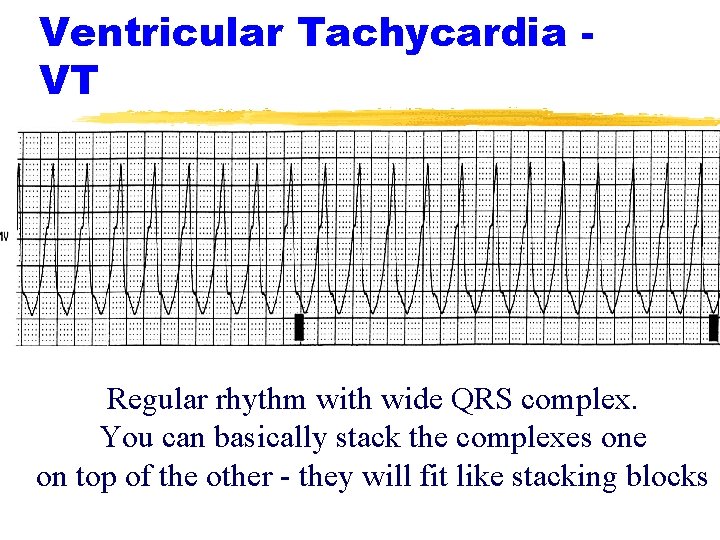
Ventricular Tachycardia VT Regular rhythm with wide QRS complex. You can basically stack the complexes one on top of the other - they will fit like stacking blocks
SOP for VT with Pulse z. This is a tachycardia z. Determine the answer to 2 questions #1 - Is the patient stable? üStable patients treated conservatively (meds) üUnstable patients need immediate cardioversion #2 - If the patient is stable, then you get to this next question - #2 -Is the QRS narrow or wide? üNarrow QRS - consider Adenosine üWide QRS - consider antidysrhythmic
SOP for Stable VT with Pulse Antidysrhythmics: z. Amiodarone 150 mg diluted in 100 ml D 5 W IVPB over 10 minutes OR z. Lidocaine 0. 75 mg/kg IVP z. Contact Medical Control for further orders after the initial bolus
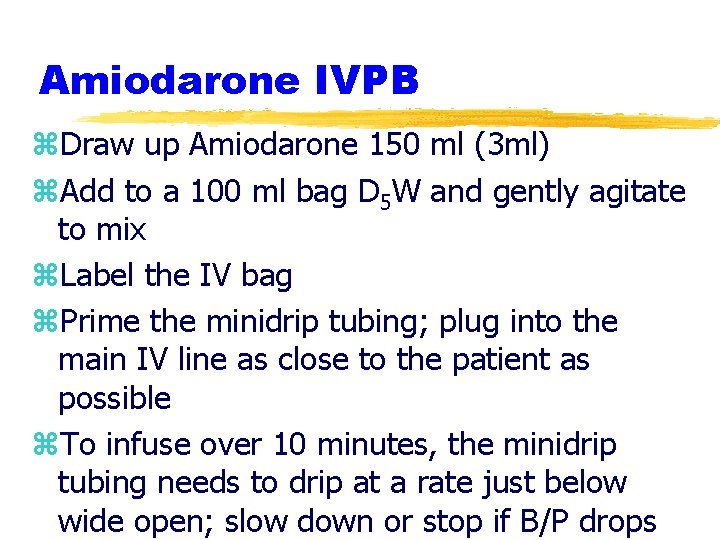
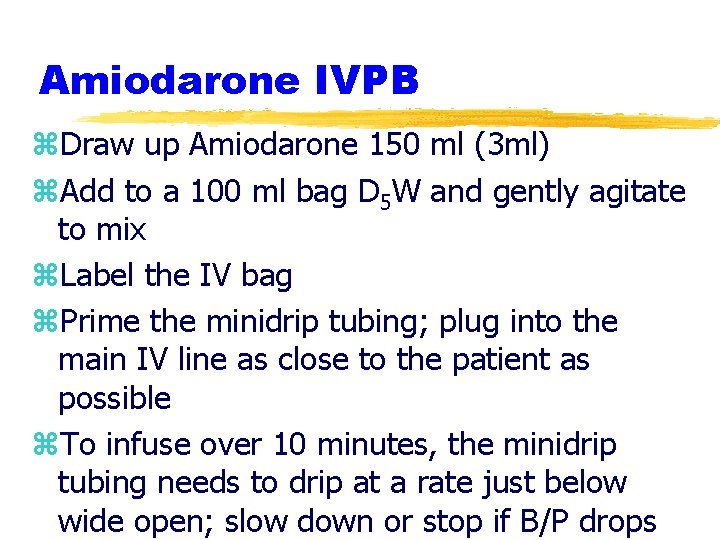
Amiodarone IVPB z. Draw up Amiodarone 150 ml (3 ml) z. Add to a 100 ml bag D 5 W and gently agitate to mix z. Label the IV bag z. Prime the minidrip tubing; plug into the main IV line as close to the patient as possible z. To infuse over 10 minutes, the minidrip tubing needs to drip at a rate just below wide open; slow down or stop if B/P drops
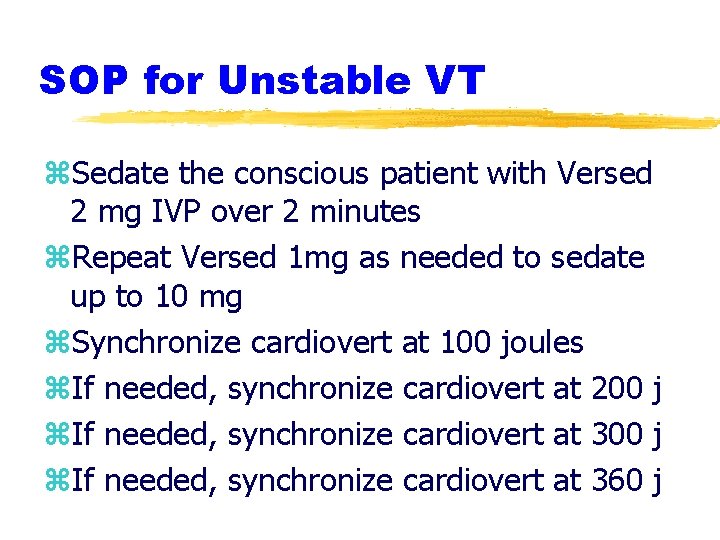
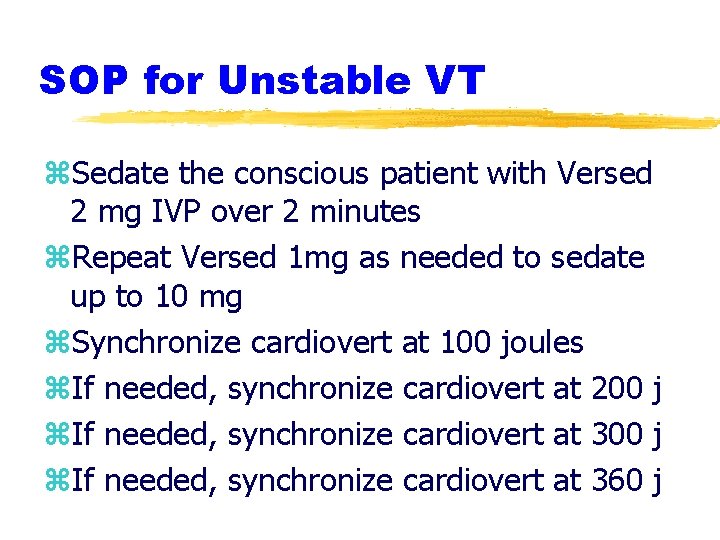
SOP for Unstable VT z. Sedate the conscious patient with Versed 2 mg IVP over 2 minutes z. Repeat Versed 1 mg as needed to sedate up to 10 mg z. Synchronize cardiovert at 100 joules z. If needed, synchronize cardiovert at 200 j z. If needed, synchronize cardiovert at 360 j
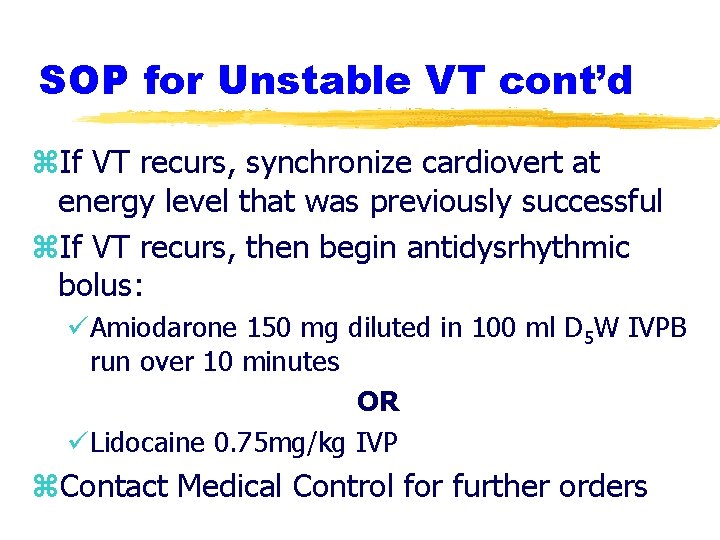
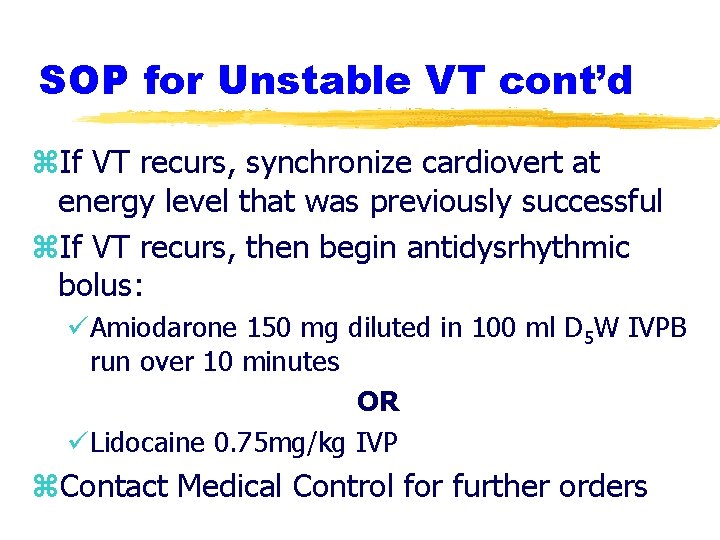
SOP for Unstable VT cont’d z. If VT recurs, synchronize cardiovert at energy level that was previously successful z. If VT recurs, then begin antidysrhythmic bolus: üAmiodarone 150 mg diluted in 100 ml D 5 W IVPB run over 10 minutes OR üLidocaine 0. 75 mg/kg IVP z. Contact Medical Control for further orders
Case Presentations z. Determine an initial impression z. Interpret the rhythm z. Based on your patient assessment and interpretation of data gathered, determine the appropriate intervention z. Discuss the steps in the appropriate SOP and understand why the intervention is necessary
Case #1 z 72 year old female presents with feeling lightheaded, weak and dizzy for one week getting progressively worse especially today z. Assessment: y. Skin pale, slightly moist; responsive to questions; lungs with slight rales in bases y. VS: 89/40; P-36; R-28; Sa. O 2 96% y. Meds: Plavix, lisinopril, Coreg y. No allergies y. Hx: B/P, CVA (no residual effects), angina
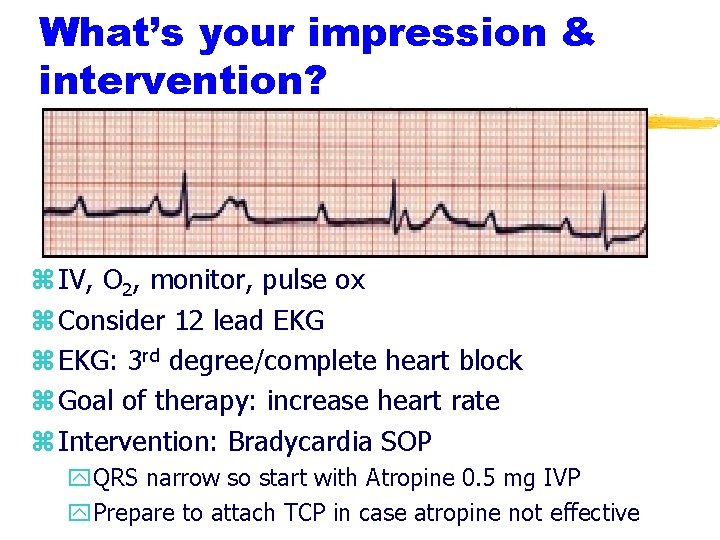
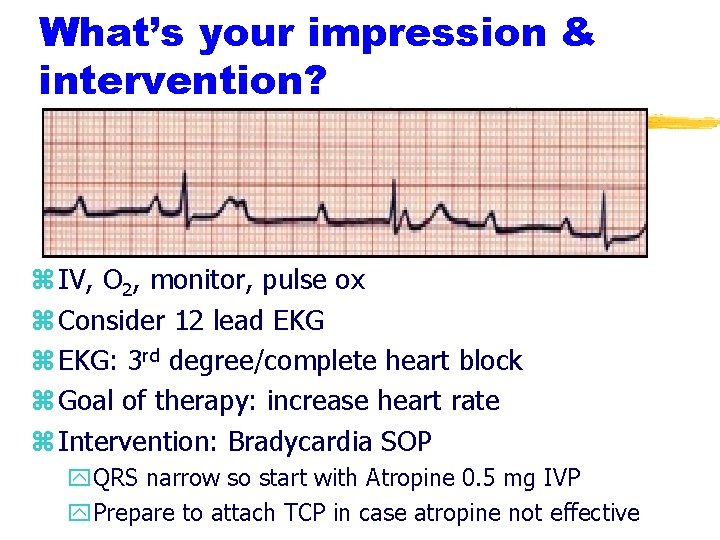
What’s your impression & intervention? z IV, O 2, monitor, pulse ox z Consider 12 lead EKG z EKG: 3 rd degree/complete heart block z Goal of therapy: increase heart rate z Intervention: Bradycardia SOP y. QRS narrow so start with Atropine 0. 5 mg IVP y. Prepare to attach TCP in case atropine not effective
Case #2 z. You were called to the scene for a 66 year old patient with complaints of chest pain, chest pounding, and a feeling like they were going to pass out. z. You had just initiated IV-O 2 -monitor z. You got a 3 second glance at the monitor when the patient grabbed their chest, their head fell back, and they became unresponsive
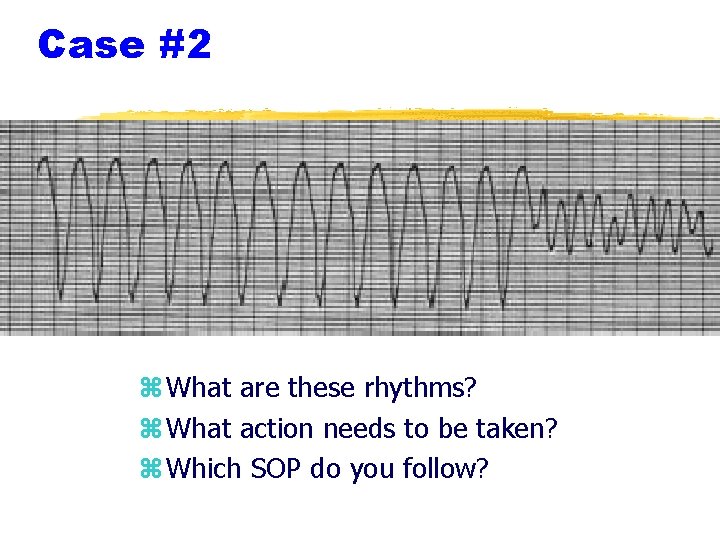
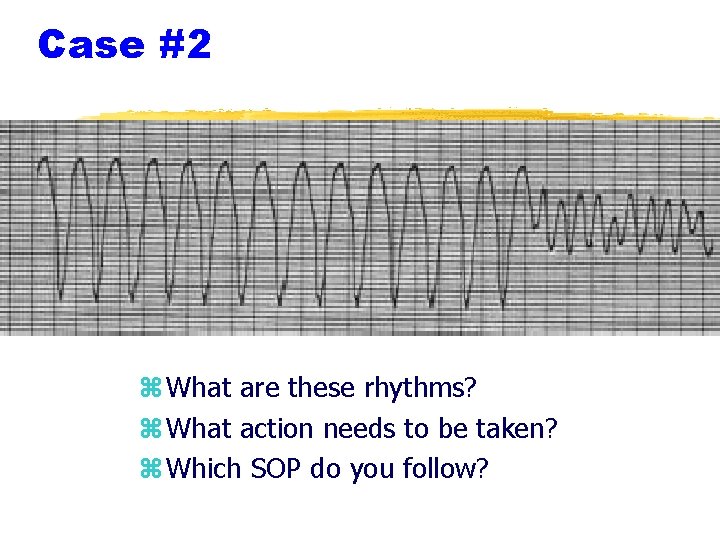
Case #2 z What are these rhythms? z What action needs to be taken? z Which SOP do you follow?
Case #2 z. The patient was initially NSR and changed to VT and then quickly deteriorated to VF z. This was a witnessed arrest - VF SOP z. Begin CPR (30: 2) until the defibrillator is charged and ready z. After each defibrillation, immediately begin CPR for 2 minutes (5 cycles) z. As the IV was already started, begin the Epinephrine after the 1 st shock
Case #3 z. A car drove past your station and “dropped” off a passenger z. Your patient is a 25 year old male with multiple bruising about the chest and abdomen who is apneic and pulseless z. There are no witnesses and no history can be obtained; there is evidence of trauma z. What is the rhythm? z. What is your impression?
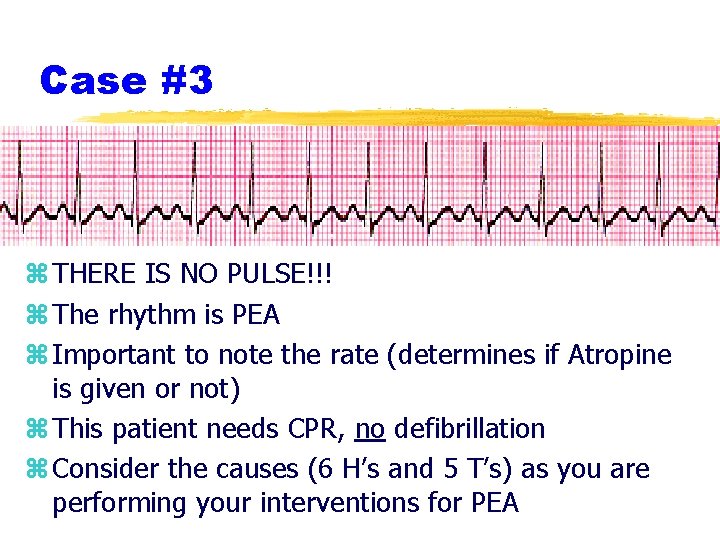
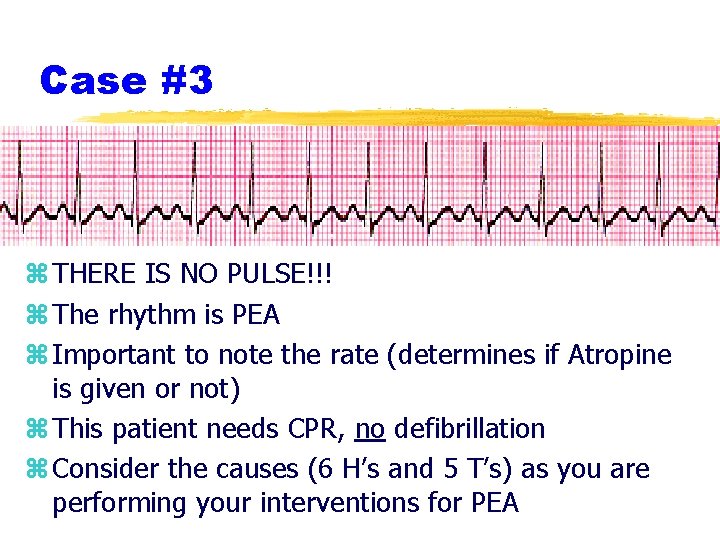
Case #3 z THERE IS NO PULSE!!! z The rhythm is PEA z Important to note the rate (determines if Atropine is given or not) z This patient needs CPR, no defibrillation z Consider the causes (6 H’s and 5 T’s) as you are performing your interventions for PEA
Case #3 z. Medications: y. Epinephrine 1: 10, 000 1 mg IVP/IO every 3 -5 minutes for duration of the arrest y. No Atropine - the heart rate is > 60 bpm z. Shift to thinking most likely causes in this young patient with evidence of trauma y. Hypovolemia - fluid bolus 200 ml at a time y. Hypoxia & acidosis-ventilate with supplemental O 2 y. Tension pneumothorax - check breath sounds y. Tamponade - rapid transport
Case #3 z. To consider: y. Is this a traumatic arrest? üIf you answer yes, then consider bilateral chest decompression with evidence of chest trauma üTransport is to the highest level trauma center within 25 minutes y. After every 5 cycles (2 minutes) of CPR, stop for 10 seconds to evaluate the EKG rhythm üIf patient remains in PEA, continue Epinephrine every 3 -5 minutes; add Atropine only if the rate falls below 60 bpm ürhythm checks are performed when observing a rhythm that might generate a pulse
Case #4 z. Your patient is a 72 year old female who has called you due to feeling short of breath and has a pounding in her chest after shoveling snow. z. What is the rhythm? z. What is your general impression? z. What SOP will be followed and what interventions are necessary?
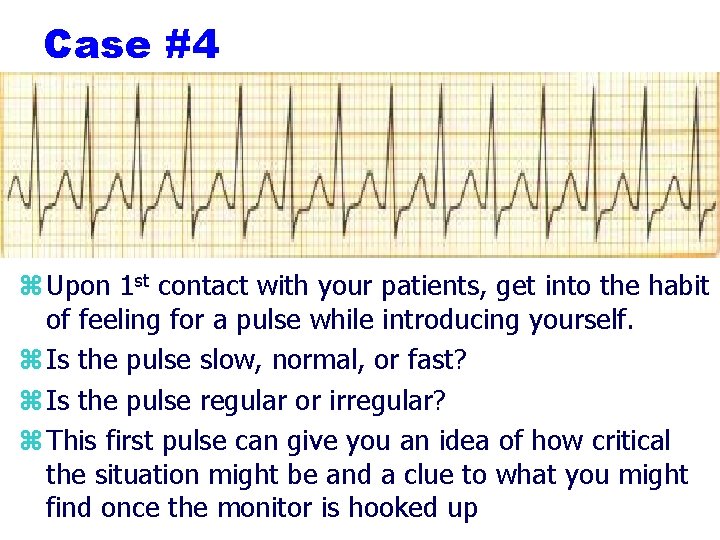
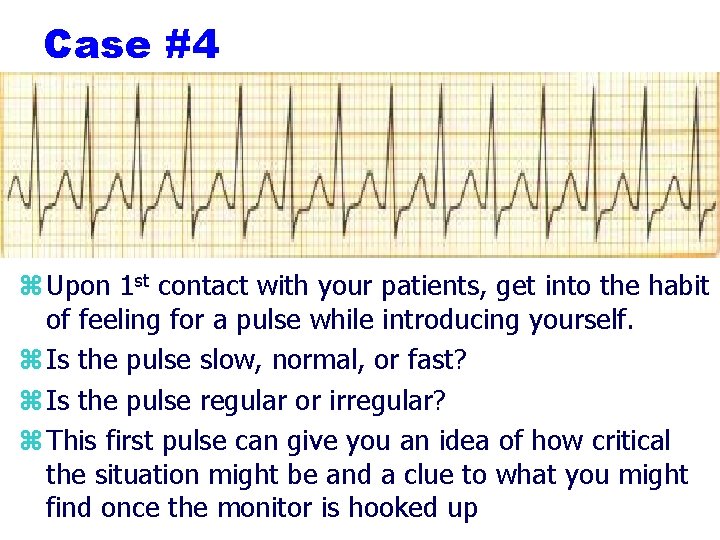
Case #4 z Upon 1 st contact with your patients, get into the habit of feeling for a pulse while introducing yourself. z Is the pulse slow, normal, or fast? z Is the pulse regular or irregular? z This first pulse can give you an idea of how critical the situation might be and a clue to what you might find once the monitor is hooked up
Case #4 z. Rhythm has a narrow complex, no visible P waves, rate over 150 - SVT z 1 st question - is the patient stable? üThis patient is responding to your questions üVS: 102/58; P-140; R-22; Sa. O 2 97% üYes, the patient is stable z 2 nd question - is the QRS narrow or wide? üQRS is narrow so treat as SVT üStart with valsalva maneuvers then meds (Adenosine)
Case #4 - What is unique about giving Adenosine? y. Start the IV in the AC, preferably right y. Give the drug as a quick flush immediately followed by a 20 ml saline flush y. After 2 minutes and reassessment of the patient (B/P, rhythm check), if the 1 st dose (6 mg) was not effective, repeat Adenosine with 12 mg again as a rapid IVP immediately followed with a 20 ml saline flush y. Transient side effects to warn the patient about include chest tightness, shortness of breath, and a flushed hot feeling
Case #5 z. You are called to a patient who is passing out but is still breathing. z. Upon arrival, you have a 65 year-old male who is supine, breathing, looks pale, is diaphoretic, and responds to pain. z. They have a carotid pulse but a very faint radial pulse if at all z. VS: 88/52; P - 190; R - 12; Sa. O 2 94% z. What is the rhythm and your impression?
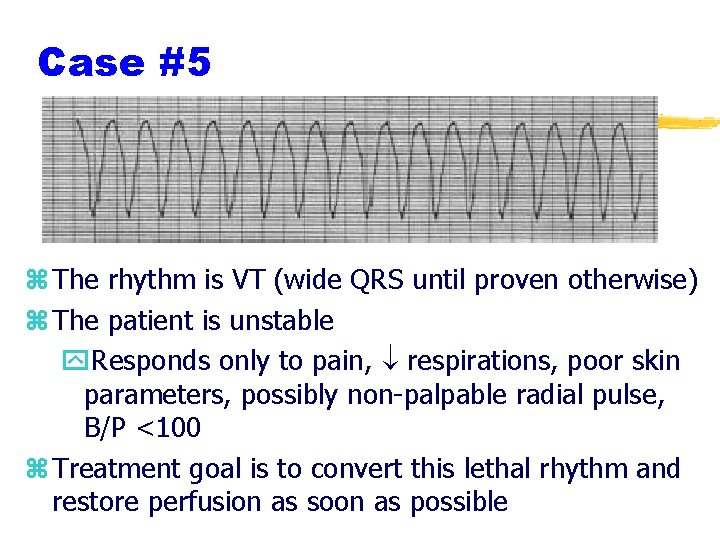
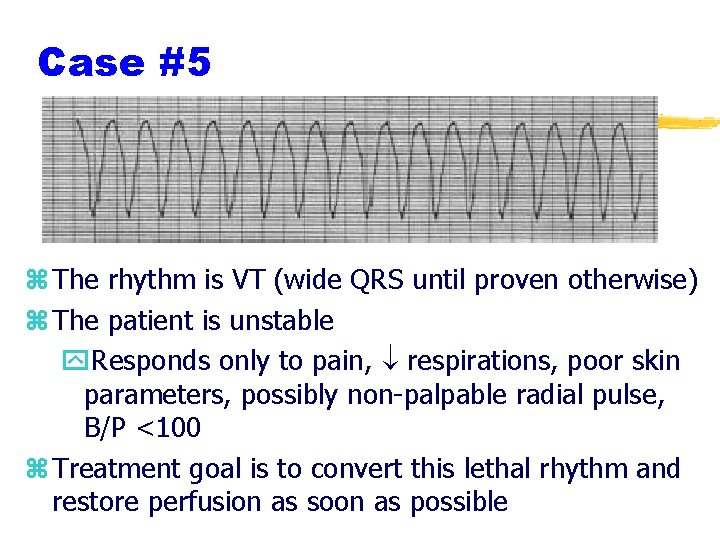
Case #5 z The rhythm is VT (wide QRS until proven otherwise) z The patient is unstable y. Responds only to pain, respirations, poor skin parameters, possibly non-palpable radial pulse, B/P <100 z Treatment goal is to convert this lethal rhythm and restore perfusion as soon as possible
Case #5 z. Immediate synchronized cardioversion needed y. If possible, sedate the patient x. Cardioversion is a painful procedure x. Versed 2 mg IVP over 2 minutes x. Can repeat Versed 1 mg as needed to sedate to a max of 10 mg y. Appropriate pads or conductive material is applied no air bubbles under the pads y. Practice safety - look around and call out “all clear”; have BVM reached out in case of need from sedation with Versed
Case #5 z. Successive cardioversion energy levels ü 100 joules üIf unsuccessful, 200 joules üIf unsuccessful, 360 joules z. If cardioversion is successful and VT recurs, cardiovert at previously successful level z. If VT recurs, then begin bolus of antidysrhythmic of your choice (Amiodarone 300 mg or Lidocaine 0. 75 mg/kg)
Case #6 z. Your 58 year-old fell and has a deformed wrist. z. Upon assessment EMS notes an irregular pulse. z. The patient meds include insulin, a “B/P” med, multiple vitamins z. What points are important to include during your assessment?
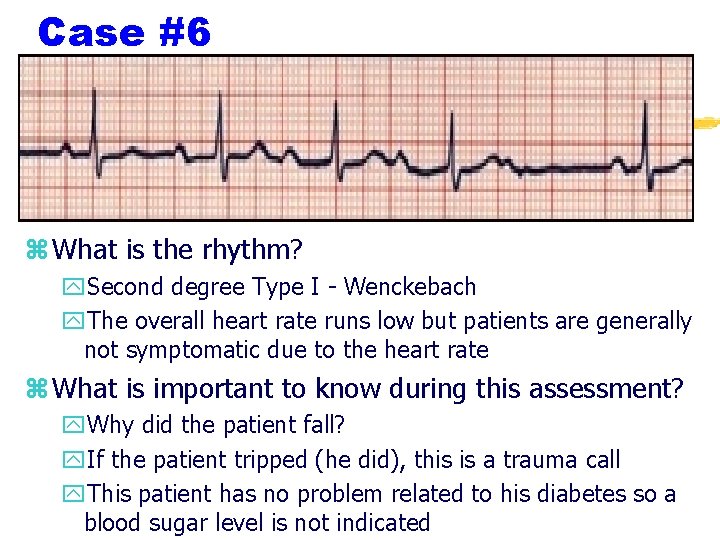
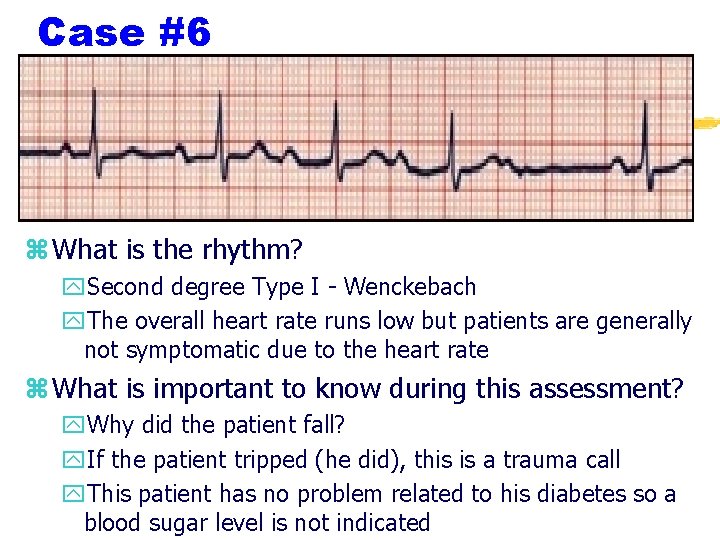
Case #6 z What is the rhythm? y. Second degree Type I - Wenckebach y. The overall heart rate runs low but patients are generally not symptomatic due to the heart rate z What is important to know during this assessment? y. Why did the patient fall? y. If the patient tripped (he did), this is a trauma call y. This patient has no problem related to his diabetes so a blood sugar level is not indicated

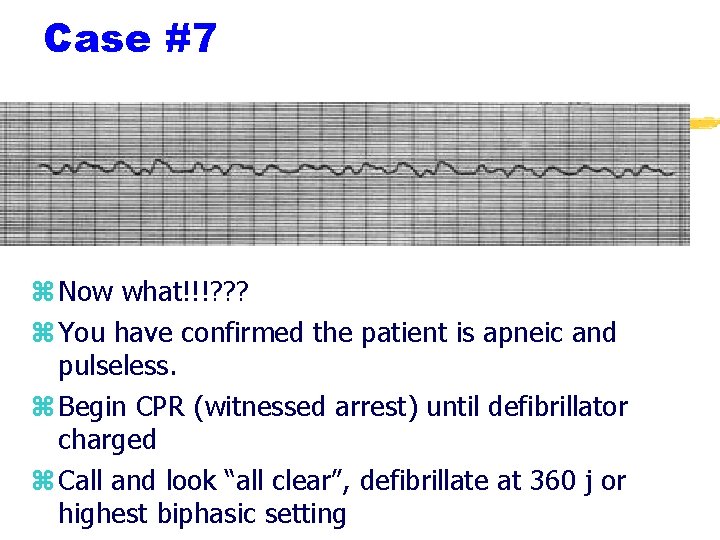
Case #7 z. You were called to the scene of a 48 year-old patient with chest pain for 1 hour. z. VS: 110/72; P - 78; R - 18; Sa. O 2 99% z. Monitor was NSR z. You had the patient begin chewing Aspirin, you had administered a nitroglycerin tablet after establishing an IV; and have just completed sending a 12 lead EKG. z. The patient suddenly becomes unresponsive
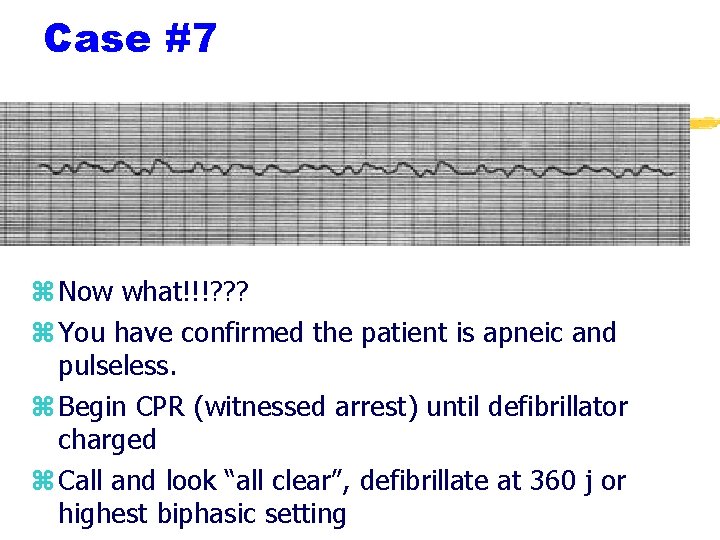
Case #7 z Now what!!!? ? ? z You have confirmed the patient is apneic and pulseless. z Begin CPR (witnessed arrest) until defibrillator charged z Call and look “all clear”, defibrillate at 360 j or highest biphasic setting
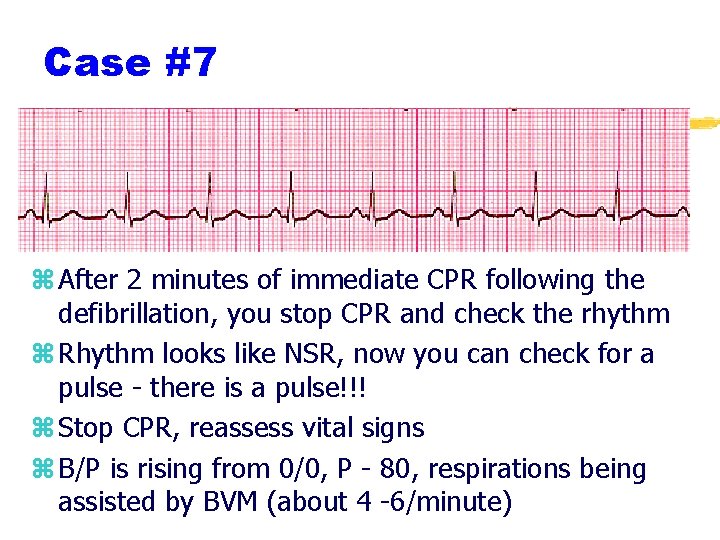
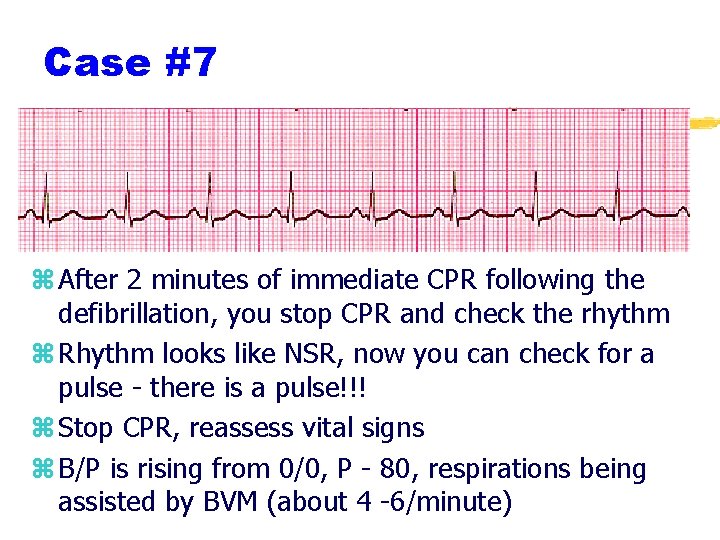
Case #7 z After 2 minutes of immediate CPR following the defibrillation, you stop CPR and check the rhythm z Rhythm looks like NSR, now you can check for a pulse - there is a pulse!!! z Stop CPR, reassess vital signs z B/P is rising from 0/0, P - 80, respirations being assisted by BVM (about 4 -6/minute)
Case #7 z. Any other medications to be given? z. This patient will not receive Epinephrine doesn’t need it now z. As no antidysrhythmic was administered to the patient, EMS must call Medical Control for orders z. If the B/P does not come up, consider a Dopamine drip and fluid bolus z. Continue to support and monitor patient’s ventilation status
References & On-Line Review z. Aehlert, B. ECG’s Made Easy. 3 rd Edition. Mosby. 2006. z. Region X SOP Effective March 1, 2007 z. Walraven, G. Basic Arrhythmias. 6 th Edition. Brady. 2006. Www. co. livingston. mi. us/ems/ekgquiz. htm www. ambulancetechnicianstudy. co. uk/ rhythms. html