Treatment principles Schizophrenia 1 The progression of schizophrenia

- Slides: 49
Treatment principles Schizophrenia 1
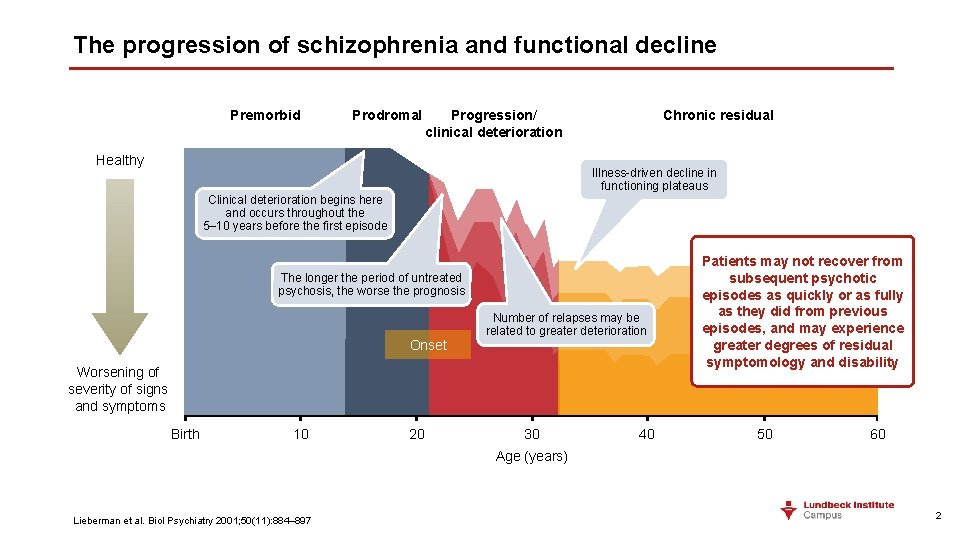
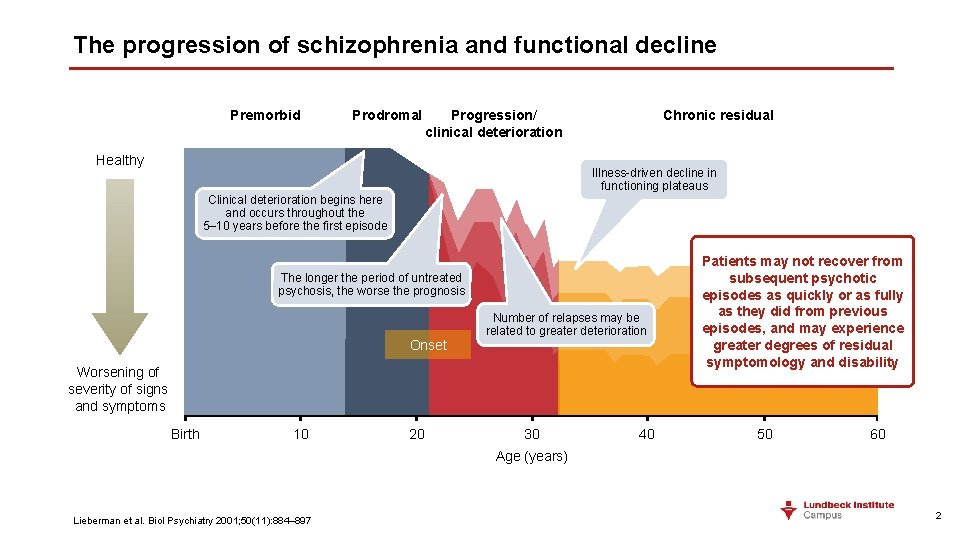
The progression of schizophrenia and functional decline Premorbid Prodromal Progression/ clinical deterioration Healthy Chronic residual Illness-driven decline in functioning plateaus Clinical deterioration begins here and occurs throughout the 5– 10 years before the first episode The longer the period of untreated psychosis, the worse the prognosis Onset Number of relapses may be related to greater deterioration Worsening of severity of signs and symptoms Birth 10 20 30 40 Patients may not recover from subsequent psychotic episodes as quickly or as fully as they did from previous episodes, and may experience greater degrees of residual symptomology and disability 50 60 Age (years) Lieberman et al. Biol Psychiatry 2001; 50(11): 884– 897 2
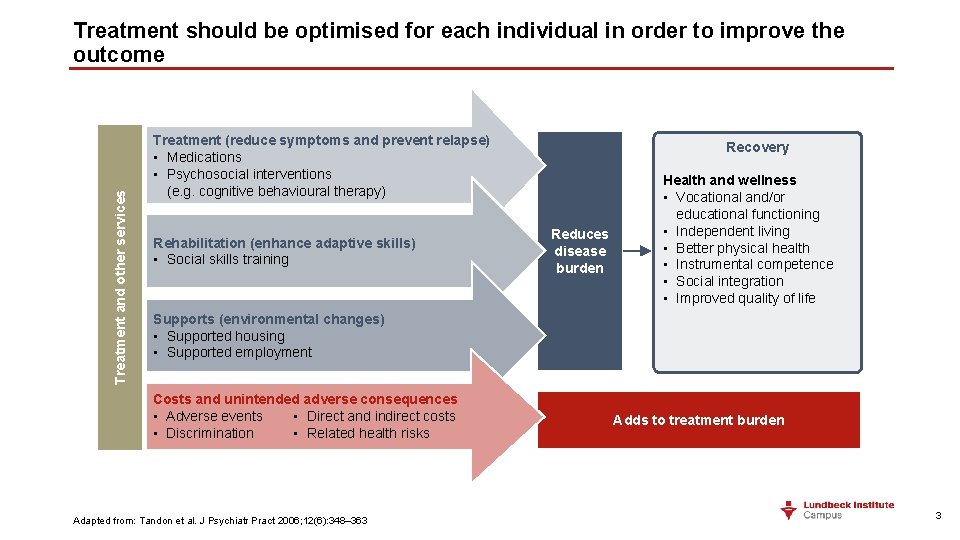
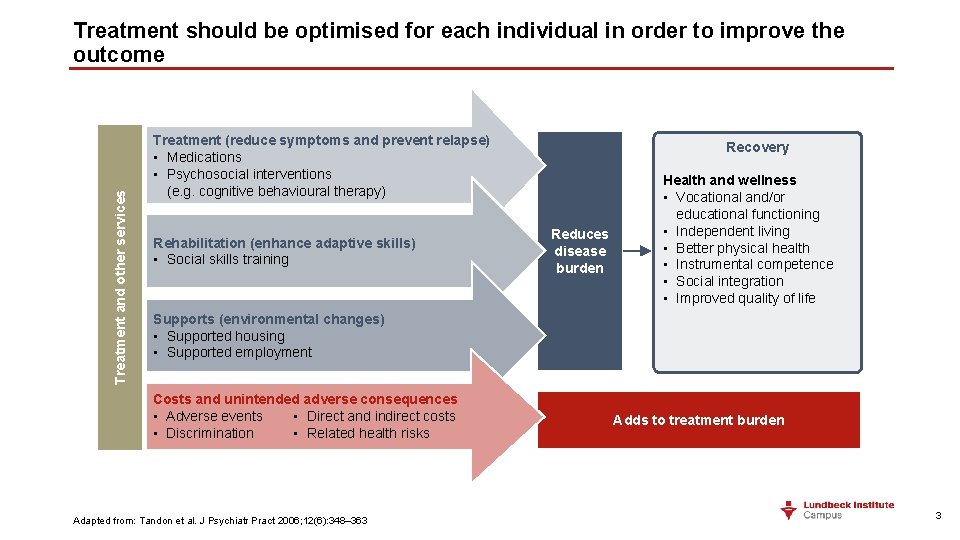
Treatment and other services Treatment should be optimised for each individual in order to improve the outcome Treatment (reduce symptoms and prevent relapse) • Medications • Psychosocial interventions (e. g. cognitive behavioural therapy) Rehabilitation (enhance adaptive skills) • Social skills training Recovery Reduces disease burden Health and wellness • Vocational and/or educational functioning • Independent living • Better physical health • Instrumental competence • Social integration • Improved quality of life Supports (environmental changes) • Supported housing • Supported employment Costs and unintended adverse consequences • Adverse events • Direct and indirect costs • Discrimination • Related health risks Adapted from: Tandon et al. J Psychiatr Pract 2006; 12(6): 348– 363 Adds to treatment burden 3
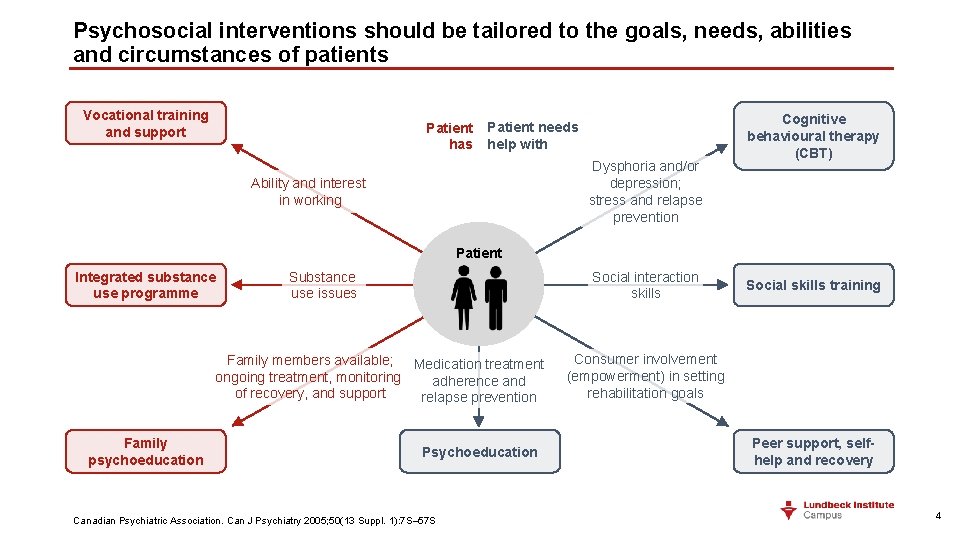
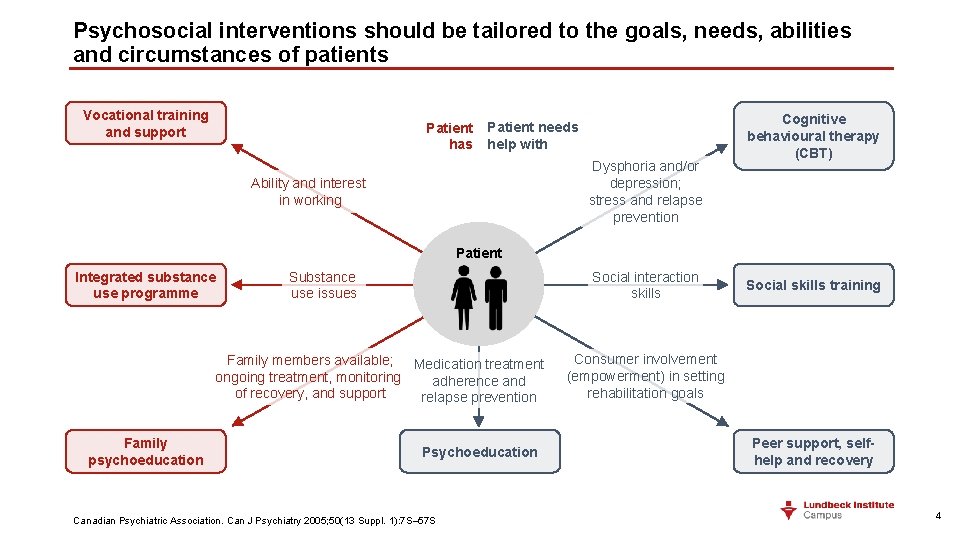
Psychosocial interventions should be tailored to the goals, needs, abilities and circumstances of patients Vocational training and support Patient has Patient needs help with Dysphoria and/or depression; stress and relapse prevention Ability and interest in working Cognitive behavioural therapy (CBT) Patient Integrated substance use programme Social interaction skills Substance use issues Family members available; Medication treatment ongoing treatment, monitoring adherence and of recovery, and support relapse prevention Family psychoeducation Psychoeducation Canadian Psychiatric Association. Can J Psychiatry 2005; 50(13 Suppl. 1): 7 S– 57 S Social skills training Consumer involvement (empowerment) in setting rehabilitation goals Peer support, selfhelp and recovery 4
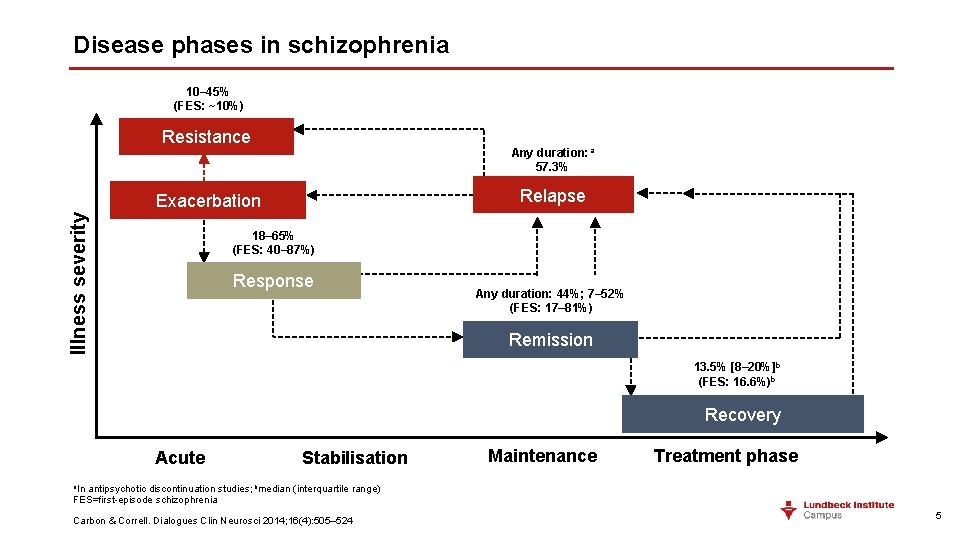
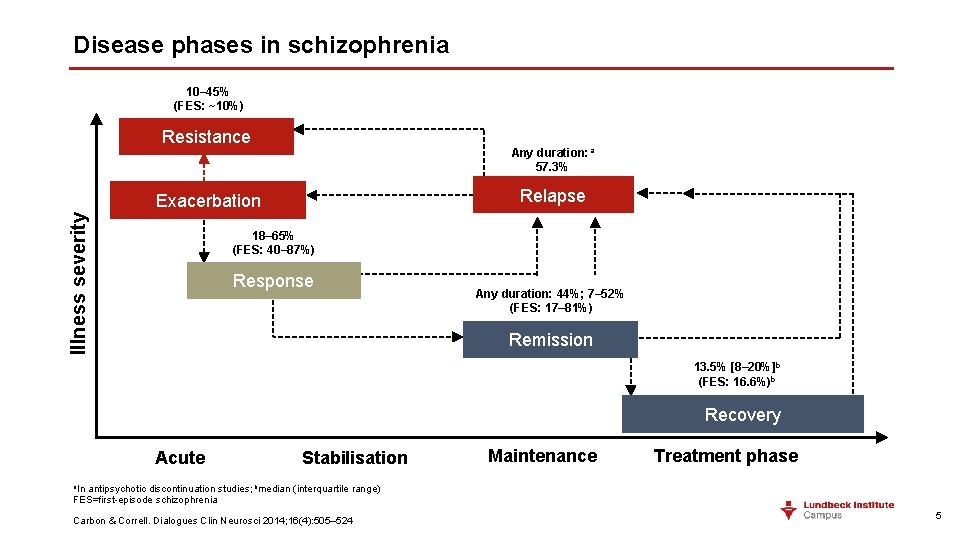
Disease phases in schizophrenia 10– 45% (FES: ~10%) Resistance Any duration: a 57. 3% Relapse Illness severity Exacerbation 18– 65% (FES: 40– 87%) Response Any duration: 44%; 7– 52% (FES: 17– 81%) Remission 13. 5% [8– 20%]b (FES: 16. 6%)b Recovery Acute Stabilisation Maintenance Treatment phase a. In antipsychotic discontinuation studies; bmedian (interquartile range) FES=first-episode schizophrenia Carbon & Correll. Dialogues Clin Neurosci 2014; 16(4): 505– 524 5
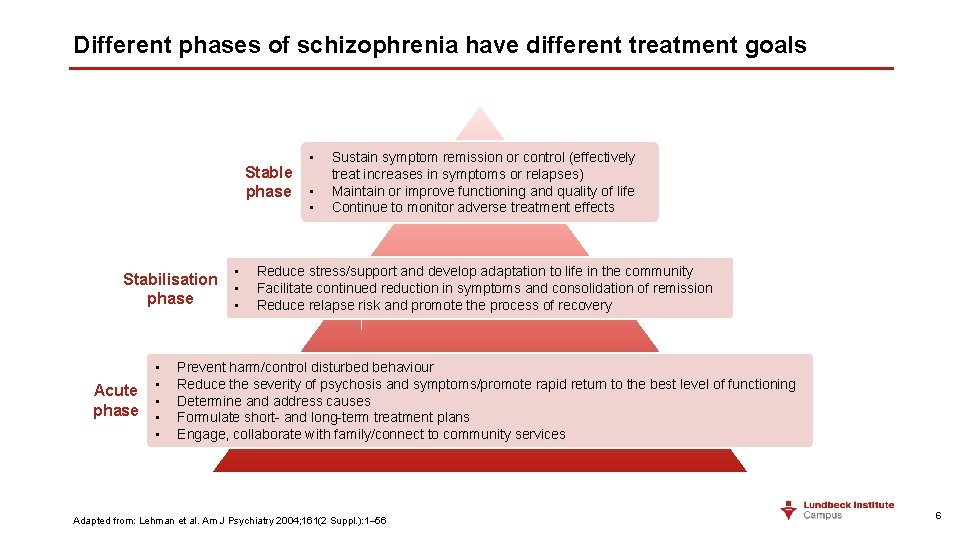
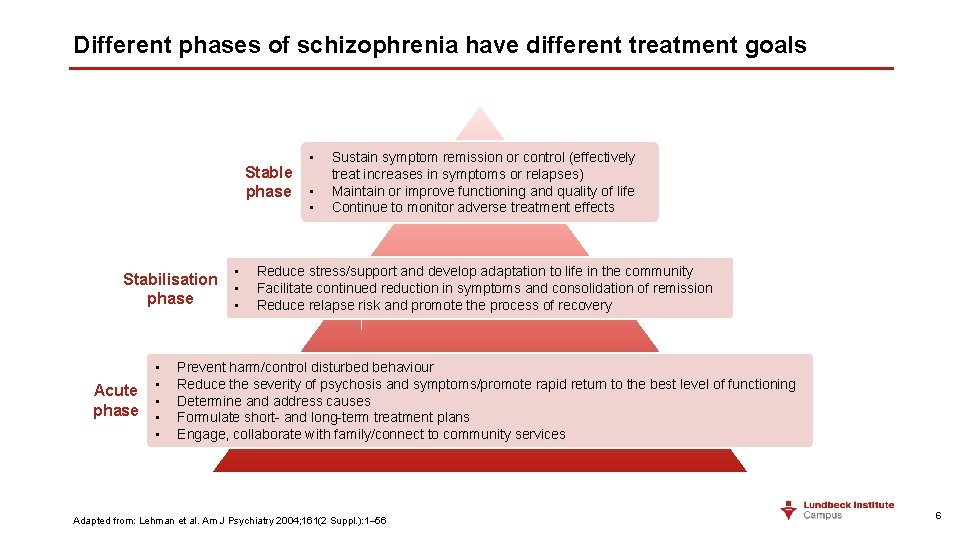
Different phases of schizophrenia have different treatment goals Stable phase • Stabilisation • phase • Acute phase • • Sustain symptom remission or control (effectively treat increases in symptoms or relapses) Maintain or improve functioning and quality of life Continue to monitor adverse treatment effects Reduce stress/support and develop adaptation to life in the community Facilitate continued reduction in symptoms and consolidation of remission Reduce relapse risk and promote the process of recovery Prevent harm/control disturbed behaviour Reduce the severity of psychosis and symptoms/promote rapid return to the best level of functioning Determine and address causes Formulate short- and long-term treatment plans Engage, collaborate with family/connect to community services Adapted from: Lehman et al. Am J Psychiatry 2004; 161(2 Suppl. ): 1– 56 6
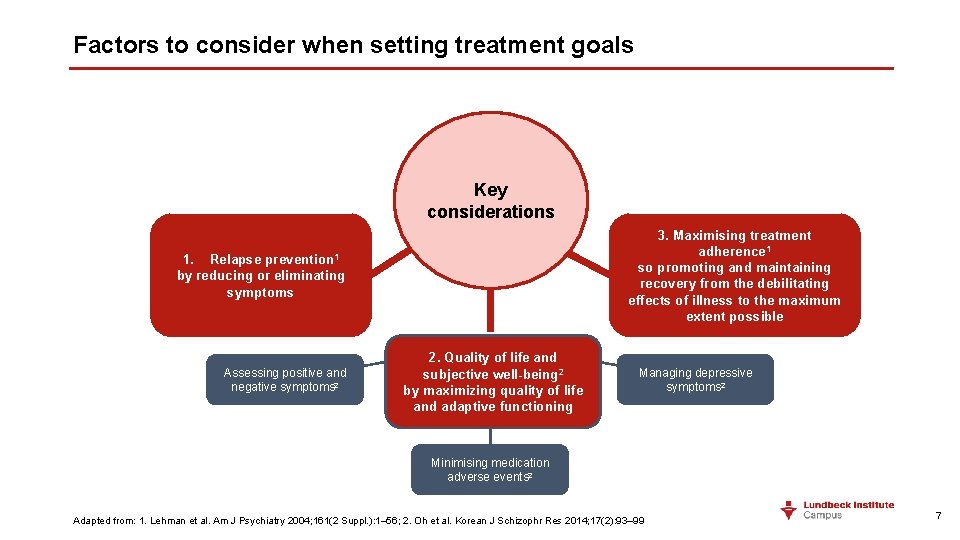
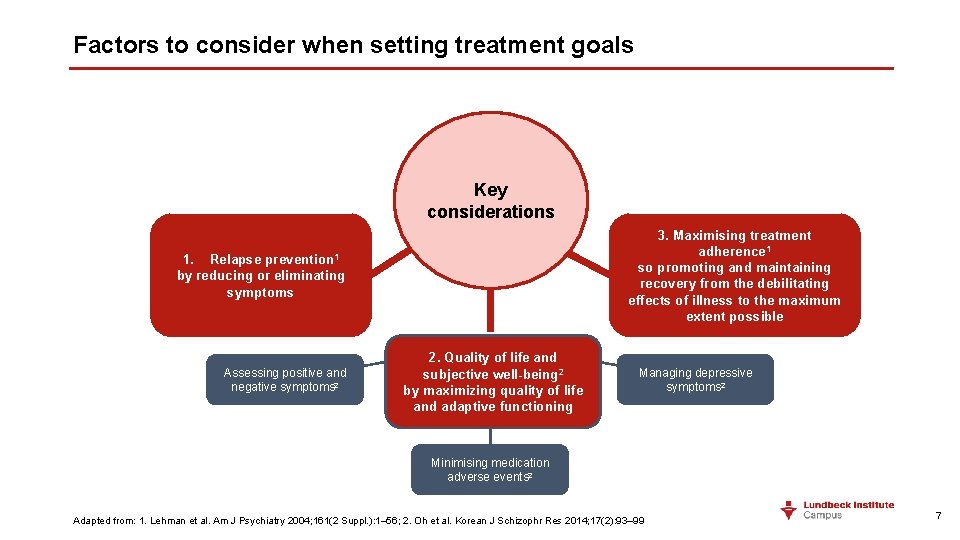
Factors to consider when setting treatment goals Key considerations 3. Maximising treatment adherence 1 so promoting and maintaining recovery from the debilitating effects of illness to the maximum extent possible 1. Relapse prevention 1 by reducing or eliminating symptoms Assessing positive and negative symptoms 2 2. Quality of life and subjective well-being 2 by maximizing quality of life and adaptive functioning Managing depressive symptoms 2 Minimising medication adverse events 2 Adapted from: 1. Lehman et al. Am J Psychiatry 2004; 161(2 Suppl. ): 1– 56; 2. Oh et al. Korean J Schizophr Res 2014; 17(2): 93– 99 7
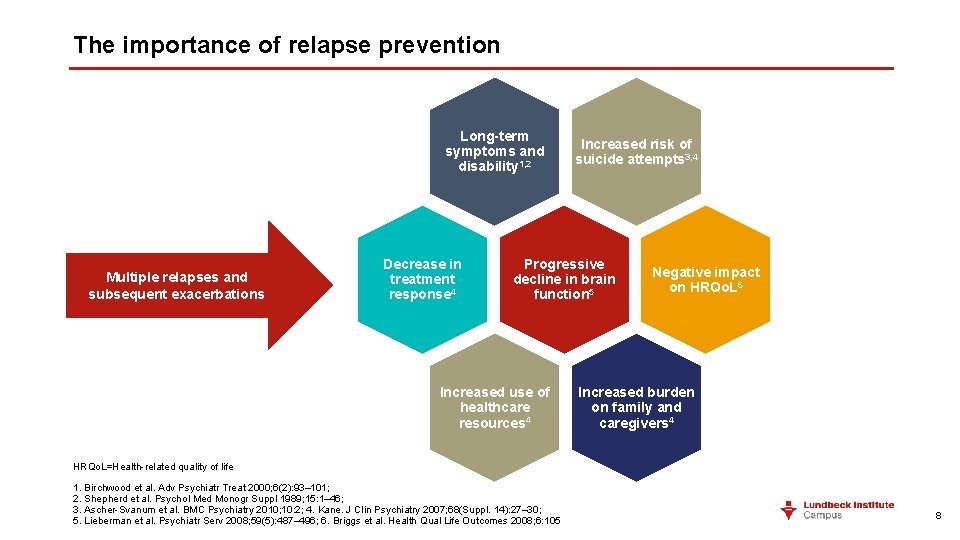
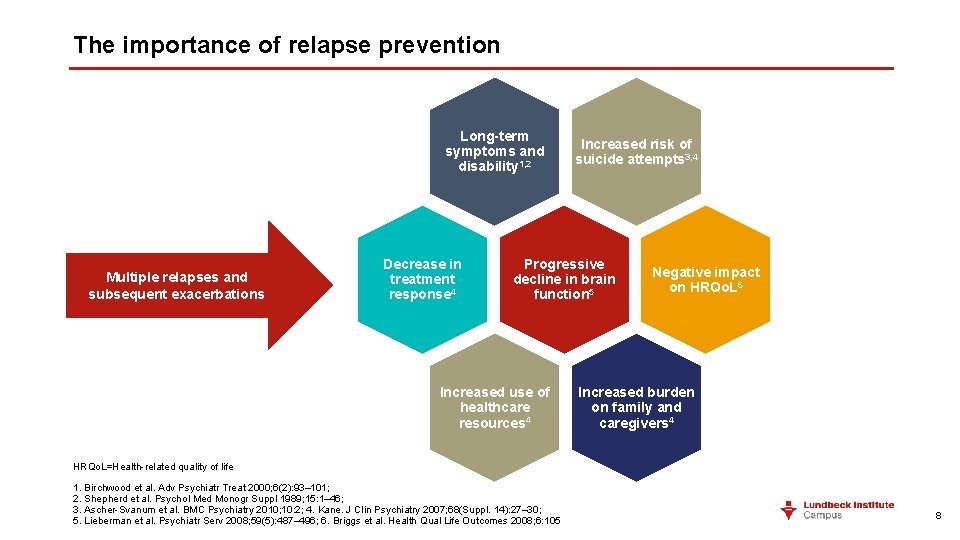
The importance of relapse prevention Long-term symptoms and disability 1, 2 Multiple relapses and subsequent exacerbations Decrease in treatment response 4 Increased risk of suicide attempts 3, 4 Progressive decline in brain function 5 Increased use of healthcare resources 4 Negative impact on HRQo. L 6 Increased burden on family and caregivers 4 HRQo. L=Health-related quality of life 1. Birchwood et al. Adv Psychiatr Treat 2000; 6(2): 93– 101; 2. Shepherd et al. Psychol Med Monogr Suppl 1989; 15: 1– 46; 3. Ascher-Svanum et al. BMC Psychiatry 2010; 10: 2; 4. Kane. J Clin Psychiatry 2007; 68(Suppl. 14): 27– 30; 5. Lieberman et al. Psychiatr Serv 2008; 59(5): 487– 496; 6. Briggs et al. Health Qual Life Outcomes 2008; 6: 105 8
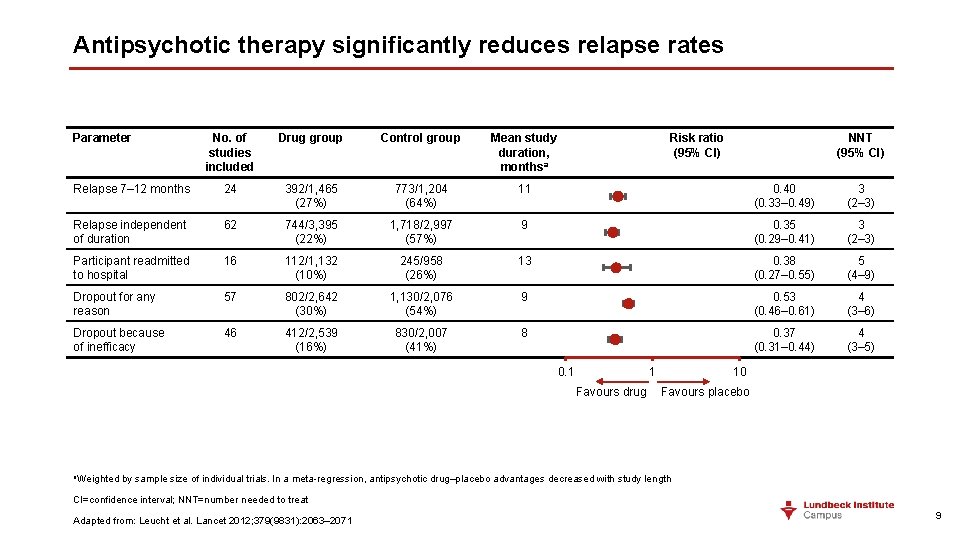
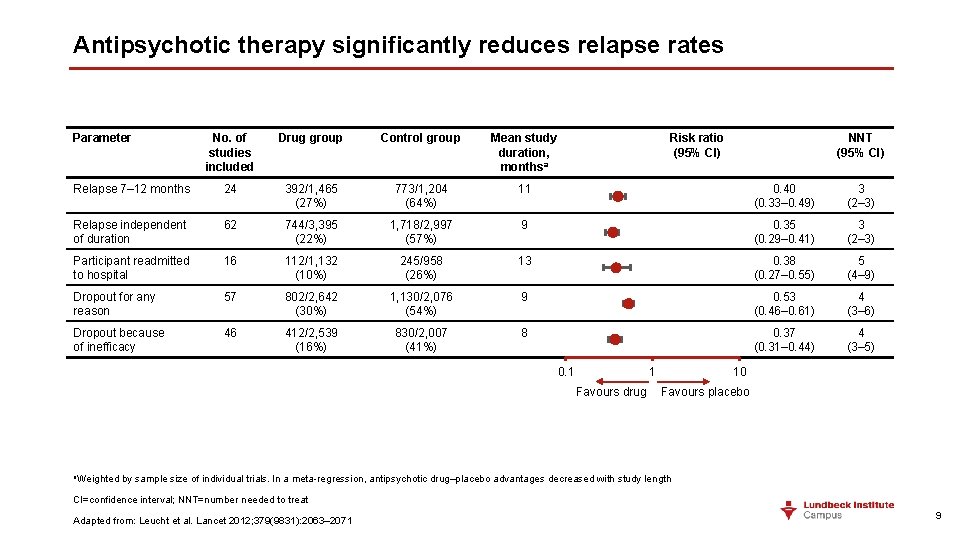
Antipsychotic therapy significantly reduces relapse rates Parameter No. of studies included Drug group Control group Mean study duration, monthsa Risk ratio (95% CI) Relapse 7– 12 months 24 392/1, 465 (27%) 773/1, 204 (64%) 11 0. 40 (0. 33– 0. 49) 3 (2– 3) Relapse independent of duration 62 744/3, 395 (22%) 1, 718/2, 997 (57%) 9 0. 35 (0. 29– 0. 41) 3 (2– 3) Participant readmitted to hospital 16 112/1, 132 (10%) 245/958 (26%) 13 0. 38 (0. 27– 0. 55) 5 (4– 9) Dropout for any reason 57 802/2, 642 (30%) 1, 130/2, 076 (54%) 9 0. 53 (0. 46– 0. 61) 4 (3– 6) Dropout because of inefficacy 46 412/2, 539 (16%) 830/2, 007 (41%) 8 0. 37 (0. 31– 0. 44) 4 (3– 5) 0. 1 1 Favours drug a. Weighted NNT (95% CI) 10 Favours placebo by sample size of individual trials. In a meta-regression, antipsychotic drug–placebo advantages decreased with study length CI=confidence interval; NNT=number needed to treat Adapted from: Leucht et al. Lancet 2012; 379(9831): 2063– 2071 9
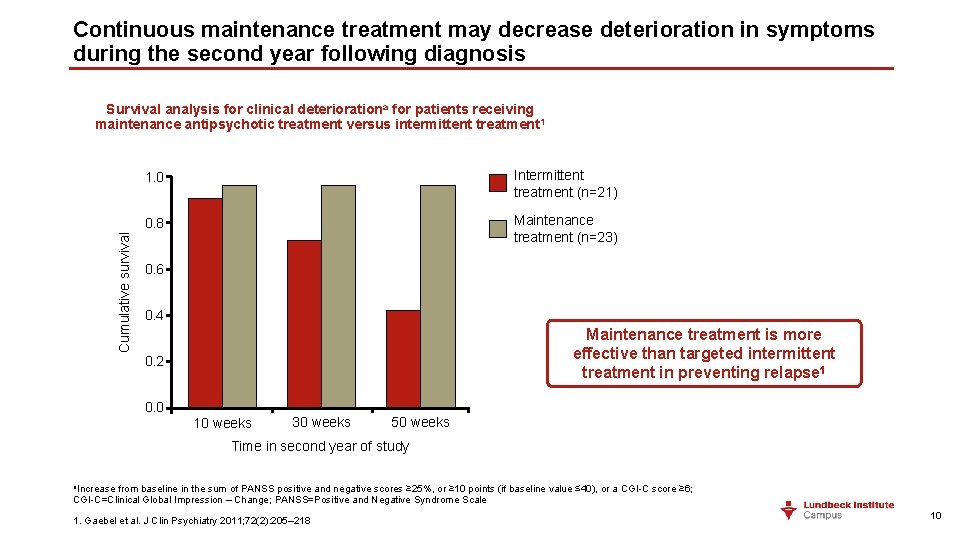
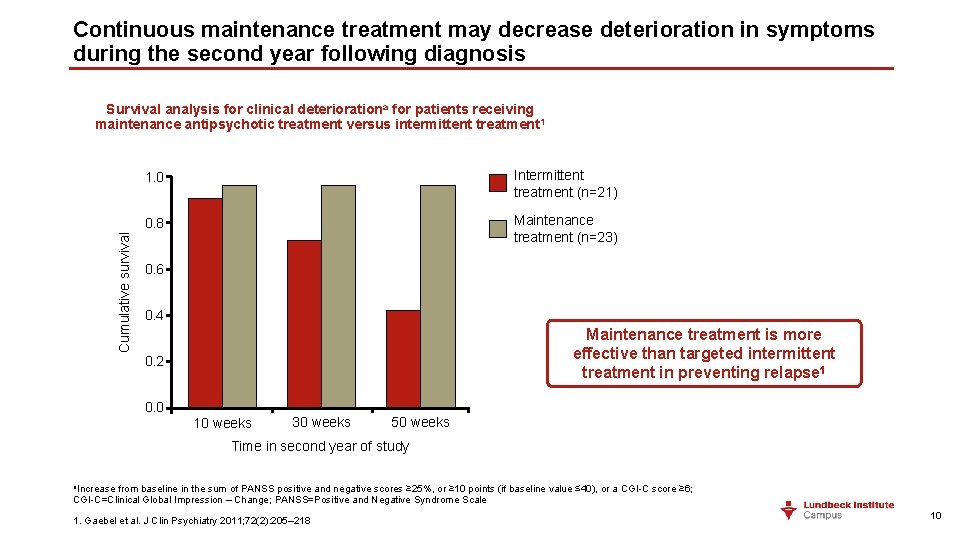
Continuous maintenance treatment may decrease deterioration in symptoms during the second year following diagnosis Cumulative survival Survival analysis for clinical deteriorationa for patients receiving maintenance antipsychotic treatment versus intermittent treatment 1 1. 0 Intermittent treatment (n=21) 0. 8 Maintenance treatment (n=23) 0. 6 0. 4 Maintenance treatment is more effective than targeted intermittent treatment in preventing relapse 1 0. 2 0. 0 10 weeks 30 weeks 50 weeks Time in second year of study a. Increase from baseline in the sum of PANSS positive and negative scores ≥ 25%, or ≥ 10 points (if baseline value ≤ 40), or a CGI-C score ≥ 6; CGI-C=Clinical Global Impression – Change; PANSS=Positive and Negative Syndrome Scale 1. Gaebel et al. J Clin Psychiatry 2011; 72(2): 205– 218 10
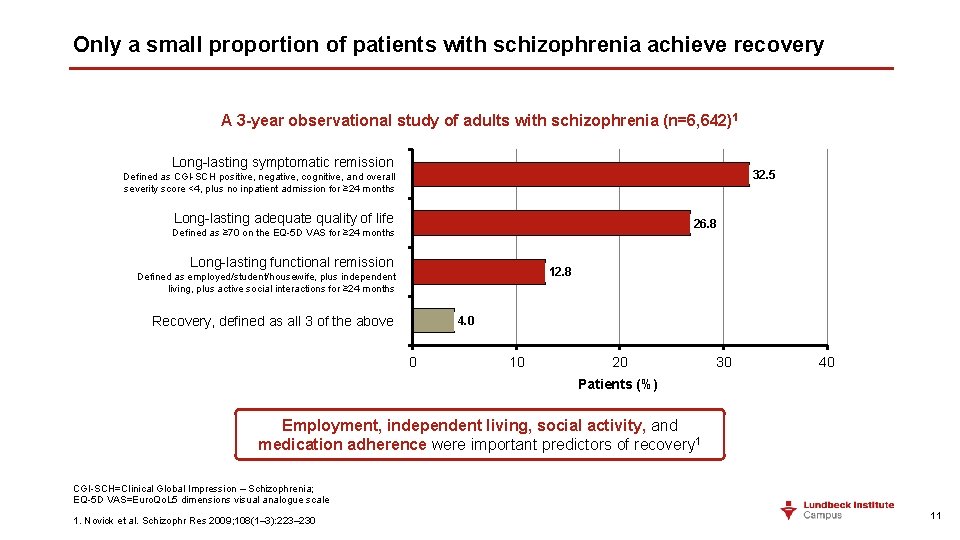
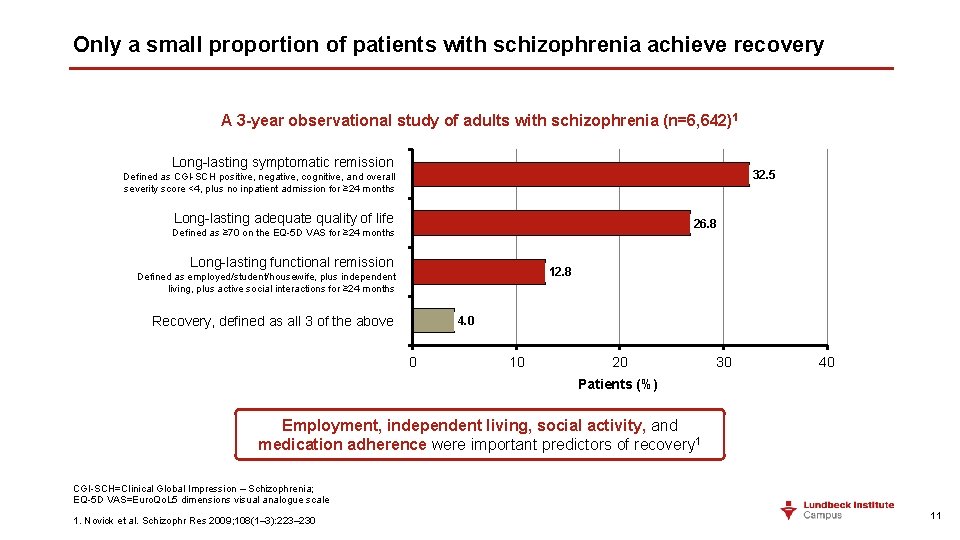
Only a small proportion of patients with schizophrenia achieve recovery A 3 -year observational study of adults with schizophrenia (n=6, 642) 1 Long-lasting symptomatic remission Defined as Long-lasting CGI-SCH positive, symptomatic negative, cognitive, and overall 32. 5 severity score <4, plus no inpatient admission for ≥ 24 months Long-lasting adequate quality of of life 26. 8 Defined as ≥ 70 on the EQ-5 D VAS for ≥ 24 months Long-lasting functional remission Long-lasting functional Defined as employed/student/housewife, plusremission independent living, plus active social interactions for ≥ 24 months 12. 8 Recovery, defined as all 3 of the above 4. 0 0 10 20 30 40 Patients (%) Employment, independent living, social activity, and medication adherence were important predictors of recovery 1 CGI-SCH=Clinical Global Impression – Schizophrenia; EQ-5 D VAS=Euro. Qo. L 5 dimensions visual analogue scale 1. Novick et al. Schizophr Res 2009; 108(1– 3): 223– 230 11
Selecting the most suitable treatment – minimal adverse events and maximum adherence 12
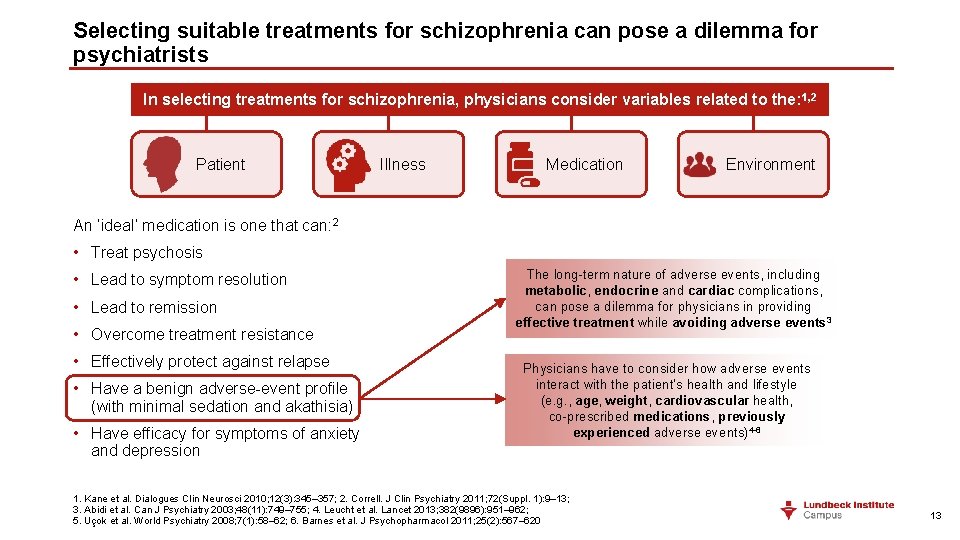
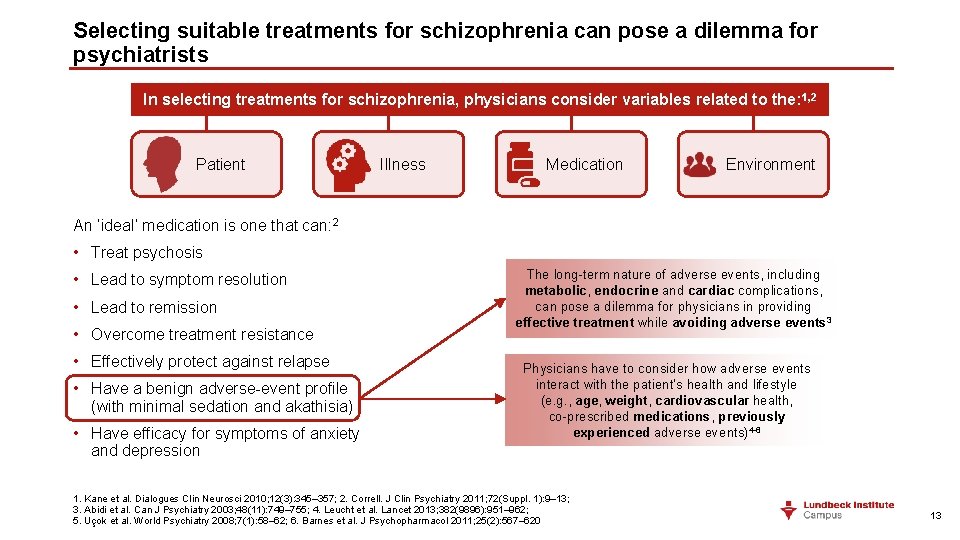
Selecting suitable treatments for schizophrenia can pose a dilemma for psychiatrists In selecting treatments for schizophrenia, physicians consider variables related to the: 1, 2 Patient Illness Medication Environment An ‘ideal’ medication is one that can: 2 • Treat psychosis • Lead to symptom resolution • Lead to remission • Overcome treatment resistance • Effectively protect against relapse • Have a benign adverse-event profile (with minimal sedation and akathisia) • Have efficacy for symptoms of anxiety and depression The long-term nature of adverse events, including metabolic, endocrine and cardiac complications, can pose a dilemma for physicians in providing effective treatment while avoiding adverse events 3 Physicians have to consider how adverse events interact with the patient’s health and lifestyle (e. g. , age, weight, cardiovascular health, co-prescribed medications, previously experienced adverse events)4 -6 1. Kane et al. Dialogues Clin Neurosci 2010; 12(3): 345– 357; 2. Correll. J Clin Psychiatry 2011; 72(Suppl. 1): 9– 13; 3. Abidi et al. Can J Psychiatry 2003; 48(11): 749‒ 755; 4. Leucht et al. Lancet 2013; 382(9896): 951‒ 962; 5. Uçok et al. World Psychiatry 2008; 7(1): 58‒ 62; 6. Barnes et al. J Psychopharmacol 2011; 25(2): 567‒ 620 13
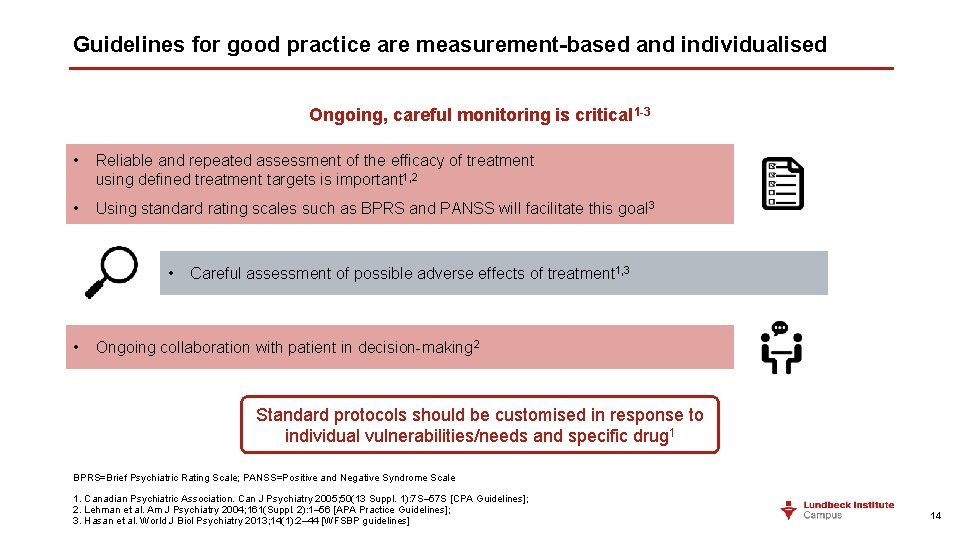
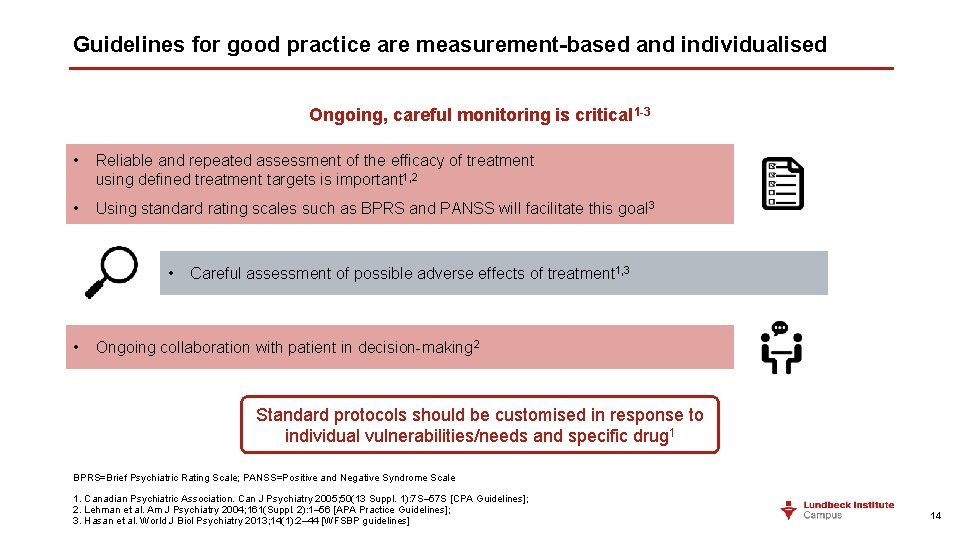
Guidelines for good practice are measurement-based and individualised Ongoing, careful monitoring is critical 1 -3 • Reliable and repeated assessment of the efficacy of treatment using defined treatment targets is important 1, 2 • Using standard rating scales such as BPRS and PANSS will facilitate this goal 3 • • Careful assessment of possible adverse effects of treatment 1, 3 Ongoing collaboration with patient in decision-making 2 Standard protocols should be customised in response to individual vulnerabilities/needs and specific drug 1 BPRS=Brief Psychiatric Rating Scale; PANSS=Positive and Negative Syndrome Scale 1. Canadian Psychiatric Association. Can J Psychiatry 2005; 50(13 Suppl. 1): 7 S– 57 S [CPA Guidelines]; 2. Lehman et al. Am J Psychiatry 2004; 161(Suppl. 2): 1– 56 [APA Practice Guidelines]; 3. Hasan et al. World J Biol Psychiatry 2013; 14(1): 2– 44 [WFSBP guidelines] 14
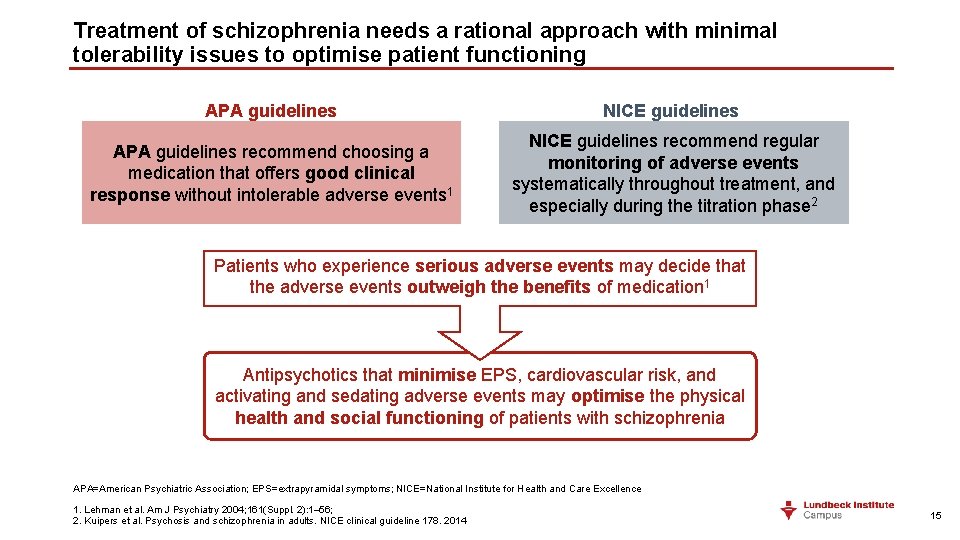
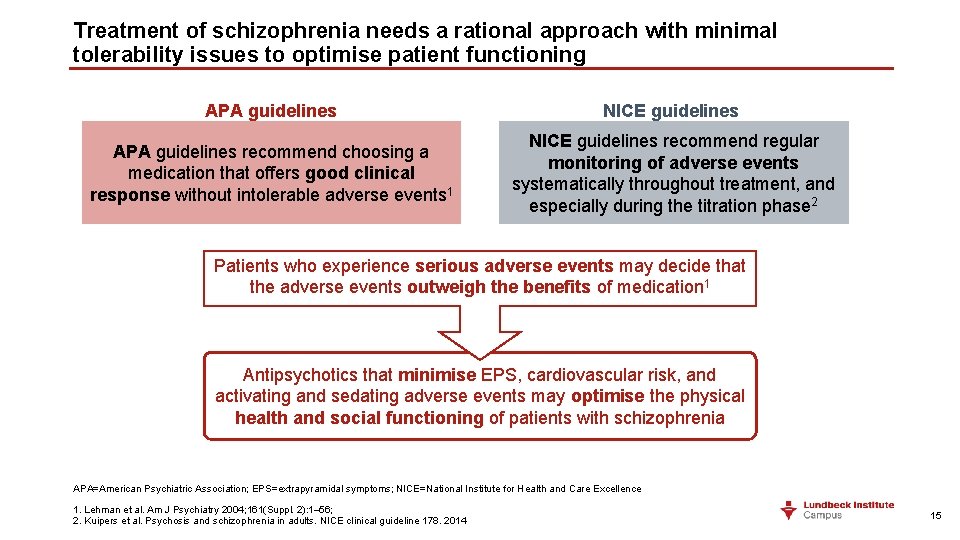
Treatment of schizophrenia needs a rational approach with minimal tolerability issues to optimise patient functioning APA guidelines NICE guidelines APA guidelines recommend choosing a medication that offers good clinical response without intolerable adverse events 1 NICE guidelines recommend regular monitoring of adverse events systematically throughout treatment, and especially during the titration phase 2 Patients who experience serious adverse events may decide that the adverse events outweigh the benefits of medication 1 Antipsychotics that minimise EPS, cardiovascular risk, and activating and sedating adverse events may optimise the physical health and social functioning of patients with schizophrenia APA=American Psychiatric Association; EPS=extrapyramidal symptoms; NICE=National Institute for Health and Care Excellence 1. Lehman et al. Am J Psychiatry 2004; 161(Suppl. 2): 1– 56; 2. Kuipers et al. Psychosis and schizophrenia in adults. NICE clinical guideline 178. 2014 15
” 1. 3. 4. 1 For people with first episode psychosis offer: - Oral antipsychotic medication in conjunction with - Psychological interventions (family intervention and individual CBT) 1. 4. 2. 1 For people with an acute exacerbation or recurrence of psychosis or schizophrenia offer: - Oral antipsychotic medication - Psychological interventions (family intervention and individual CBT) CBT=cognitive behavioural therapy NICE. Psychosis and schizophrenia in adults: prevention and management. NICE clinical guideline 178. 2014 16
” Choice of antipsychotic medication 1. 3. 5. 1 The choice of antipsychotic medication should be made by the service user and healthcare professional together, taking into account the views of the carer if the service user agrees. Provide information and discuss the likely benefits and possible side effects of each drug, including: - Metabolic (including weight gain and diabetes) - Extrapyramidal (including akathisia, dyskinesia, and dystonia) - Cardiovascular (including prolonging the QT interval) - Hormonal (including increasing plasma prolactin) - Other (including unpleasant subjective experiences) NICE. Psychosis and schizophrenia in adults: prevention and management. NICE clinical guideline 178. 2014 17

” Antipsychotics should be chosen individually, respecting the patient’s mental and somatic condition with special attention to side effects The selection of an antipsychotic medication should be guided by the patient’s previous experience of symptom response and side effects, intended route of administration, the patient’s preferences for a particular medication, the presence of comorbid medical conditions, and potential interactions with other prescribed medications. Special attention needs to be given to antipsychotic-related side effects Hasan et al. World J Biol Psychiatry 2012; 13 (5): 318– 378 18
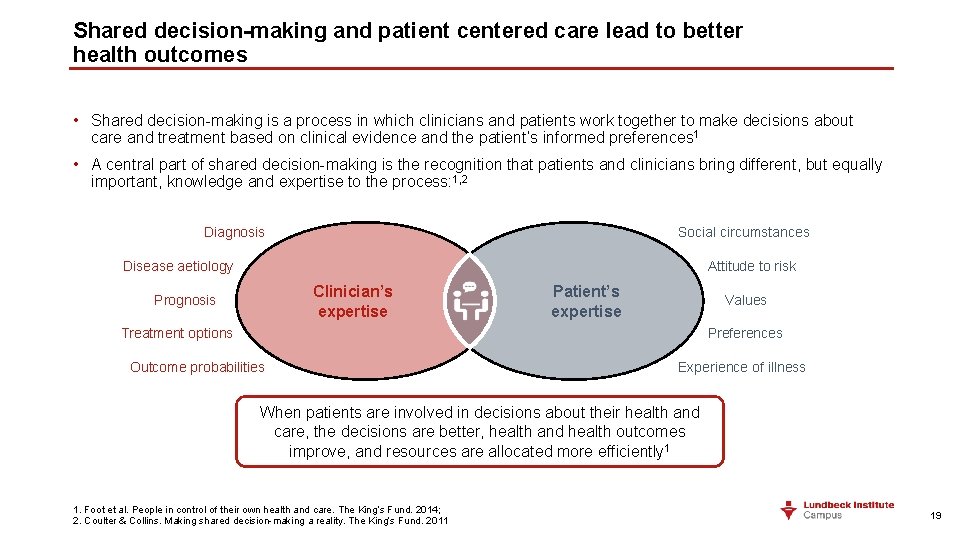
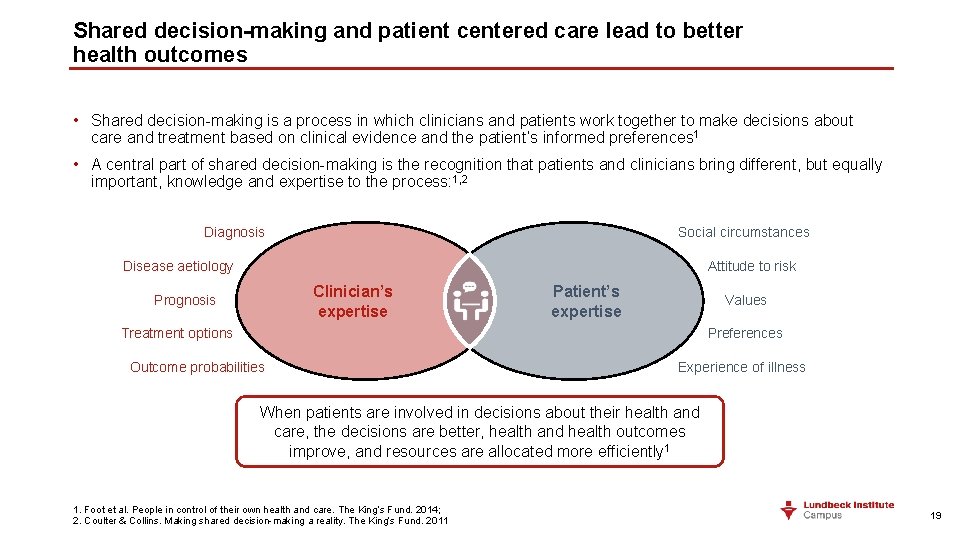
Shared decision-making and patient centered care lead to better health outcomes • Shared decision-making is a process in which clinicians and patients work together to make decisions about care and treatment based on clinical evidence and the patient’s informed preferences 1 • A central part of shared decision-making is the recognition that patients and clinicians bring different, but equally important, knowledge and expertise to the process: 1, 2 Diagnosis Social circumstances Disease aetiology Attitude to risk Clinician’s expertise Prognosis Patient’s expertise Values Treatment options Preferences Outcome probabilities Experience of illness When patients are involved in decisions about their health and care, the decisions are better, health and health outcomes improve, and resources are allocated more efficiently 1 1. Foot et al. People in control of their own health and care. The King’s Fund. 2014; 2. Coulter & Collins. Making shared decision-making a reality. The King’s Fund. 2011 19
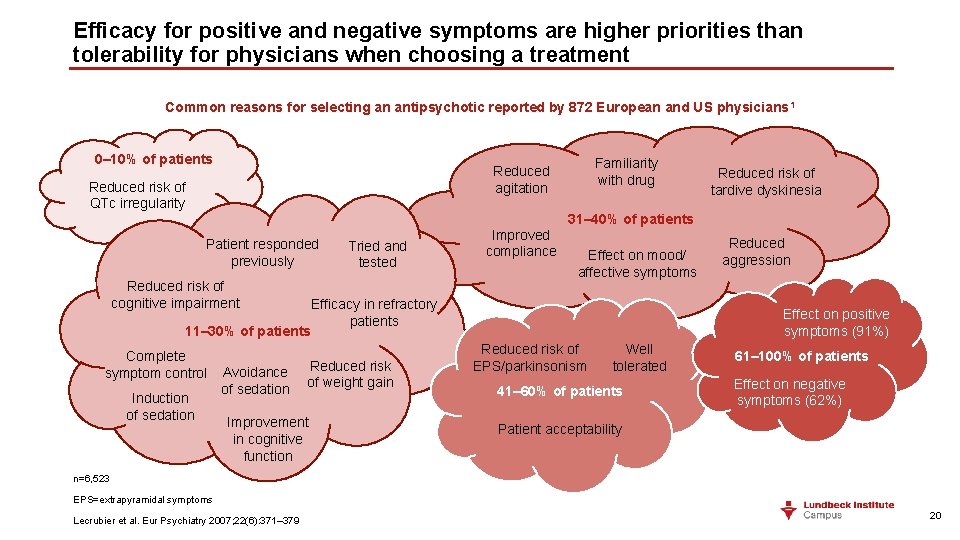
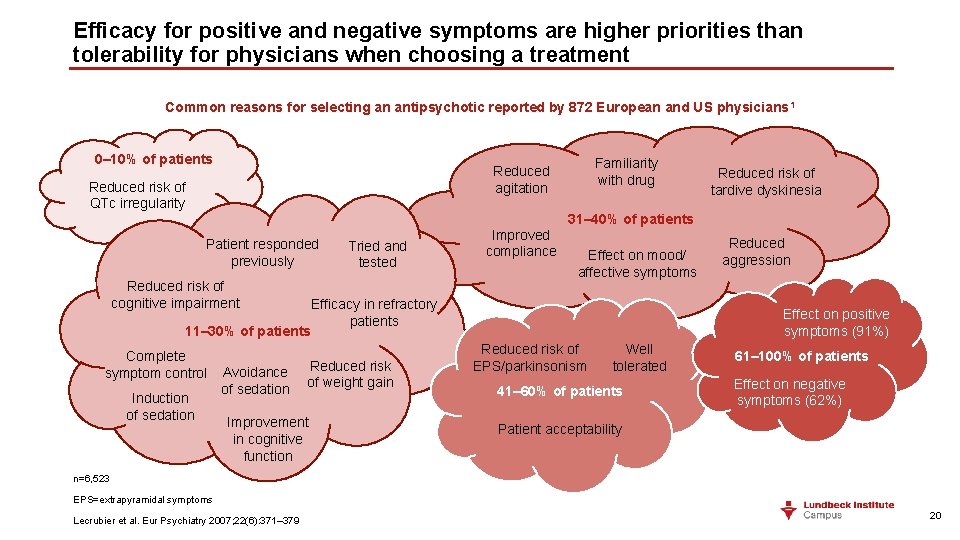
Efficacy for positive and negative symptoms are higher priorities than tolerability for physicians when choosing a treatment Common reasons for selecting an antipsychotic reported by 872 European and US physicians 1 0– 10% of patients Familiarity with drug Reduced agitation Reduced risk of QTc irregularity Reduced risk of tardive dyskinesia 31– 40% of patients Patient responded previously Tried and tested Reduced risk of cognitive impairment Improved compliance Effect on mood/ affective symptoms Efficacy in refractory patients 11– 30% of patients Complete symptom control Induction of sedation Avoidance of sedation Reduced risk of weight gain Improvement in cognitive function Reduced aggression Effect on positive symptoms (91%) Reduced risk of EPS/parkinsonism Well tolerated 41– 60% of patients 61– 100% of patients Effect on negative symptoms (62%) Patient acceptability n=6, 523 EPS=extrapyramidal symptoms Lecrubier et al. Eur Psychiatry 2007; 22(6): 371– 379 20
Negative symptoms and the treatment of schizophrenia • Negative symptoms impact greatly on a person’s quality of life, and affect their ability to experience many life-fulfilling activities 1 • Diagnosing schizophrenia can be challenging for the healthcare professional, and complex for the patient to understand 1 • However, negative symptoms are unlikely to result in the person’s hospitalisation, or to the person coming into contact with the criminal justice system 1 • The identification and quantification of negative symptoms, in practice, can be a overwhelming task because: 1, 2 • There is an inherent subjectivity to negative symptoms, and they can be mistaken for other mental illnesses • There is an obvious discomfort for the healthcare professional when identifying the ‘lack’ of something • Negative symptoms have an economic cost to society: 1 • They prevent a large number of people with schizophrenia from working • They result in a substantial economic cost added to the emotional and psychological burden on patients, carers, and healthcare professionals 1. Living with schizophrenia website. https: //www. livingwithschizophreniauk. org/information-sheets/negative-symptoms-understanding/; 2. Mitra et al. Ind Psychiatry J 2016; 25(2): 135– 144 21
Depressive symptoms and the treatment of schizophrenia • Individuals living with schizophrenia are commonly affected by depression: 1 • Some experience episodic major depression • Some experience mild depression symptoms on a chronic basis • In schizophrenia, depression may impact the motivation to perform potentially reinforcing acts, possibly through the induction of anhedonia 1 • Depression has a major adverse impact on everyday functioning 1 Improving the recognition and management of depressive symptoms may reduce the adverse impact of severe mental illness on everyday functioning 1 1. Harvey. Innov Clin Neurosci 2011; 8(10): 14– 18 22
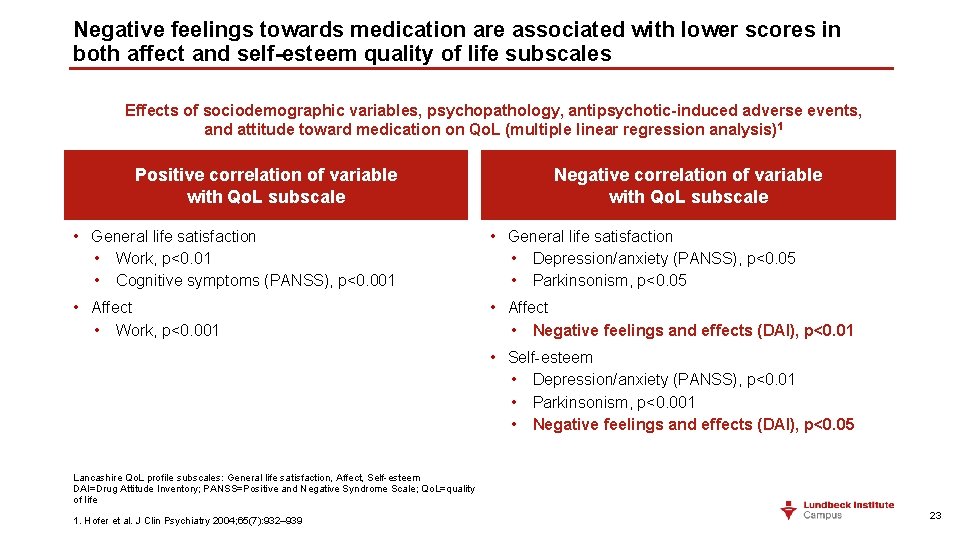
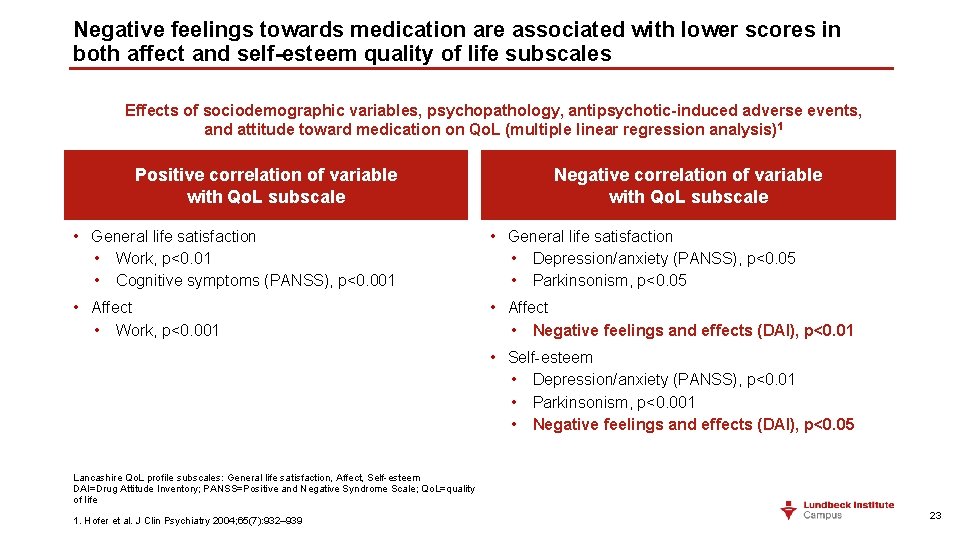
Negative feelings towards medication are associated with lower scores in both affect and self-esteem quality of life subscales Effects of sociodemographic variables, psychopathology, antipsychotic-induced adverse events, and attitude toward medication on Qo. L (multiple linear regression analysis) 1 Positive correlation of variable with Qo. L subscale Negative correlation of variable with Qo. L subscale • General life satisfaction • Work, p<0. 01 • Cognitive symptoms (PANSS), p<0. 001 • General life satisfaction • Depression/anxiety (PANSS), p<0. 05 • Parkinsonism, p<0. 05 • Affect • Work, p<0. 001 • Affect • Negative feelings and effects (DAI), p<0. 01 • Self-esteem • Depression/anxiety (PANSS), p<0. 01 • Parkinsonism, p<0. 001 • Negative feelings and effects (DAI), p<0. 05 Lancashire Qo. L profile subscales: General life satisfaction, Affect, Self-esteem DAI=Drug Attitude Inventory; PANSS=Positive and Negative Syndrome Scale; Qo. L=quality of life 1. Hofer et al. J Clin Psychiatry 2004; 65(7): 932– 939 23
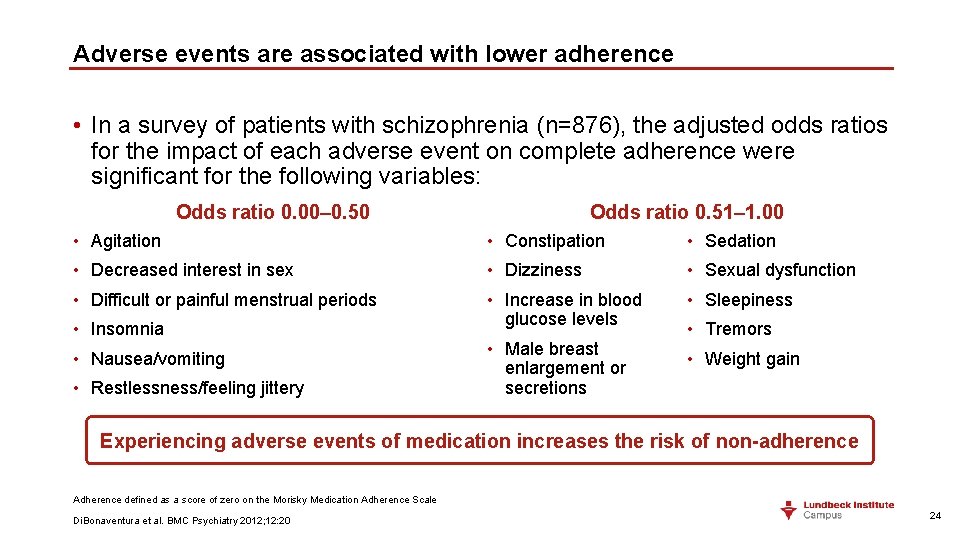
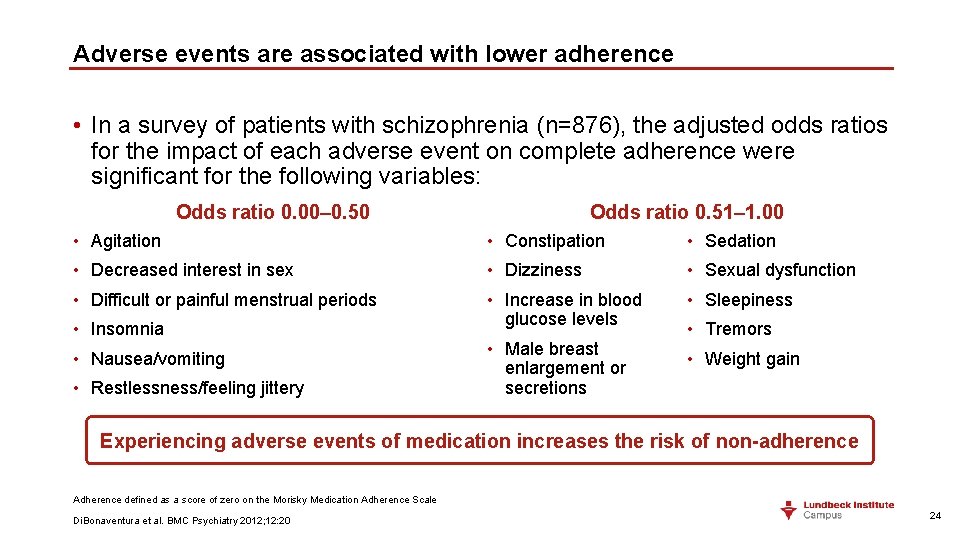
Adverse events are associated with lower adherence • In a survey of patients with schizophrenia (n=876), the adjusted odds ratios for the impact of each adverse event on complete adherence were significant for the following variables: Odds ratio 0. 00– 0. 50 Odds ratio 0. 51– 1. 00 • Agitation • Constipation • Sedation • Decreased interest in sex • Dizziness • Sexual dysfunction • Difficult or painful menstrual periods • Increase in blood glucose levels • Sleepiness • Insomnia • Nausea/vomiting • Restlessness/feeling jittery • Male breast enlargement or secretions • Tremors • Weight gain Experiencing adverse events of medication increases the risk of non-adherence Adherence defined as a score of zero on the Morisky Medication Adherence Scale Di. Bonaventura et al. BMC Psychiatry 2012; 12: 20 24
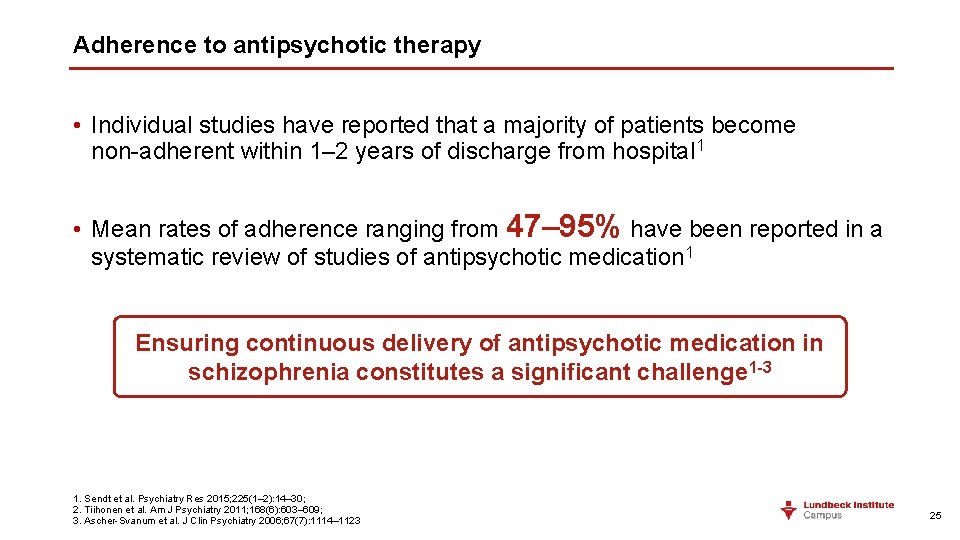
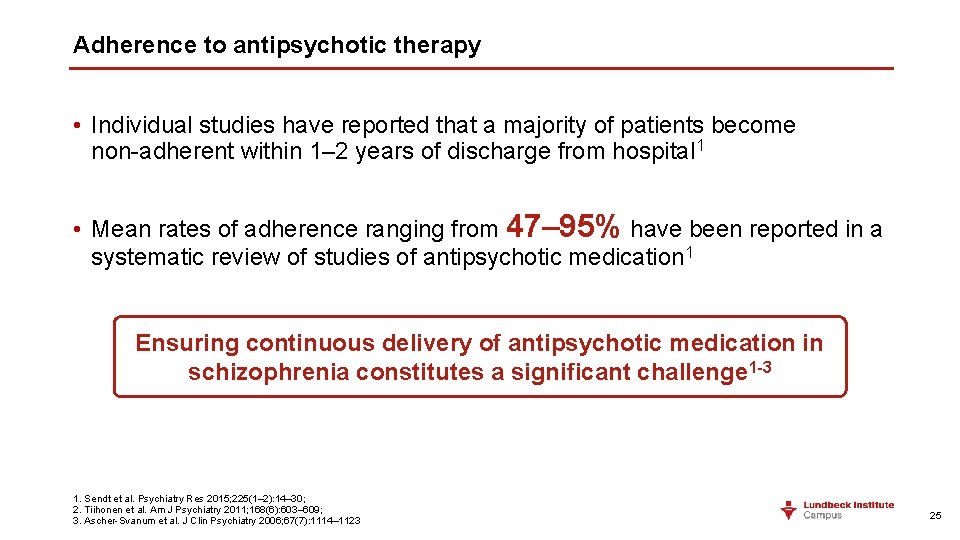
Adherence to antipsychotic therapy • Individual studies have reported that a majority of patients become non-adherent within 1– 2 years of discharge from hospital 1 • Mean rates of adherence ranging from 47– 95% have been reported in a systematic review of studies of antipsychotic medication 1 Ensuring continuous delivery of antipsychotic medication in schizophrenia constitutes a significant challenge 1 -3 1. Sendt et al. Psychiatry Res 2015; 225(1– 2): 14– 30; 2. Tiihonen et al. Am J Psychiatry 2011; 168(6): 603– 609; 3. Ascher-Svanum et al. J Clin Psychiatry 2006; 67(7): 1114– 1123 25
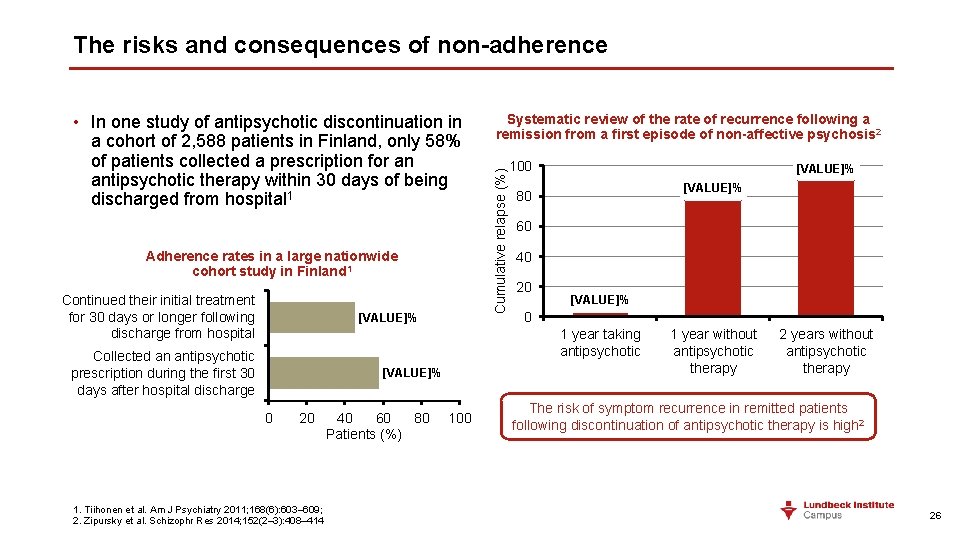
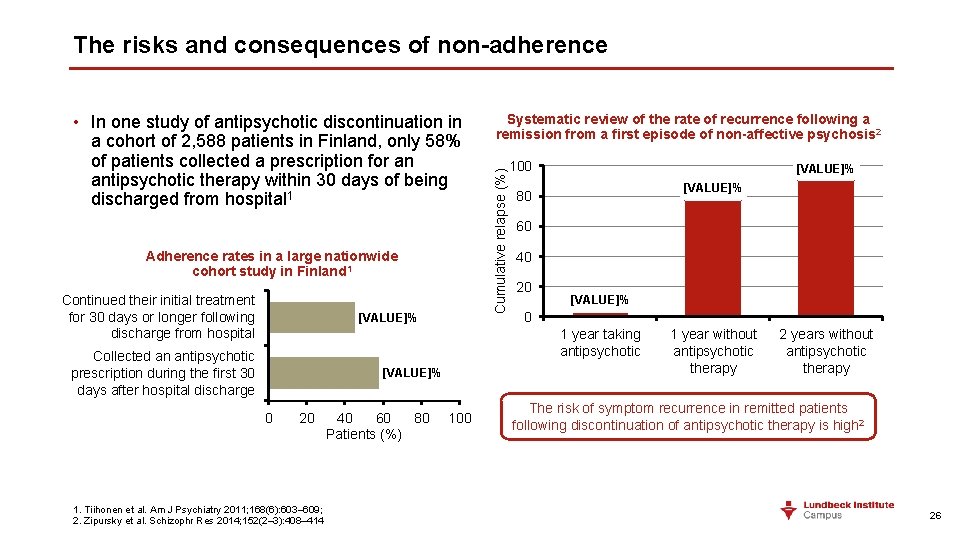
The risks and consequences of non-adherence Adherence rates in a large nationwide cohort study in Finland 1 Continued their initial treatment for 30 days or longer following discharge from hospital [VALUE]% Systematic review of the rate of recurrence following a remission from a first episode of non-affective psychosis 2 Cumulative relapse (%) • In one study of antipsychotic discontinuation in a cohort of 2, 588 patients in Finland, only 58% of patients collected a prescription for an antipsychotic therapy within 30 days of being discharged from hospital 1 100 [VALUE]% 80 60 40 20 [VALUE]% 0 1 year taking antipsychotic Collected an antipsychotic prescription during the first 30 days after hospital discharge [VALUE]% 0 20 1. Tiihonen et al. Am J Psychiatry 2011; 168(6): 603– 609; 2. Zipursky et al. Schizophr Res 2014; 152(2– 3): 408– 414 40 60 80 Patients (%) 100 1 year without antipsychotic therapy 2 years without antipsychotic therapy The risk of symptom recurrence in remitted patients following discontinuation of antipsychotic therapy is high 2 26
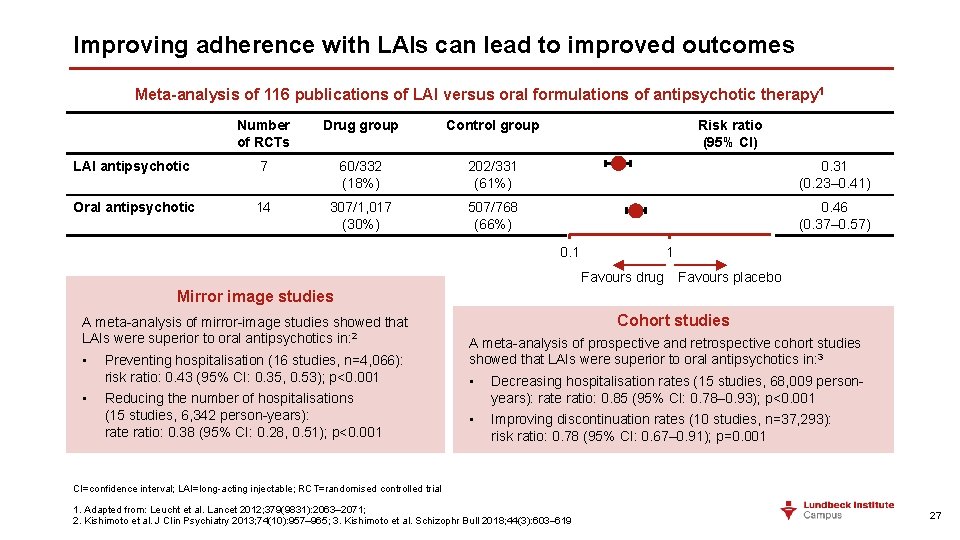
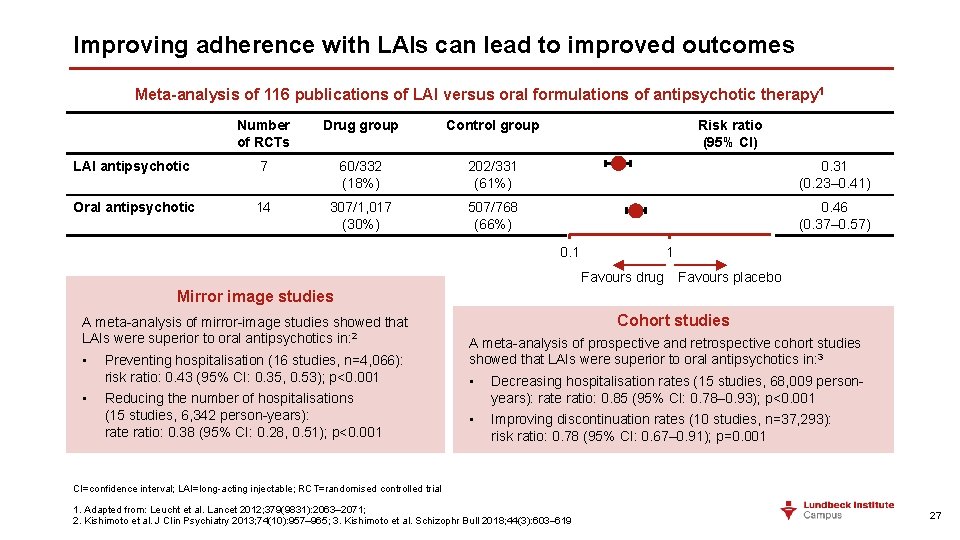
Improving adherence with LAIs can lead to improved outcomes Meta-analysis of 116 publications of LAI versus oral formulations of antipsychotic therapy 1 Number of RCTs Drug group Control group Risk ratio (95% CI) LAI antipsychotic 7 60/332 (18%) 202/331 (61%) 0. 31 (0. 23– 0. 41) Oral antipsychotic 14 307/1, 017 (30%) 507/768 (66%) 0. 46 (0. 37– 0. 57) 0. 1 1 Favours drug Favours placebo Mirror image studies A meta-analysis of mirror-image studies showed that LAIs were superior to oral antipsychotics in: 2 • • Preventing hospitalisation (16 studies, n=4, 066): risk ratio: 0. 43 (95% CI: 0. 35, 0. 53); p<0. 001 Reducing the number of hospitalisations (15 studies, 6, 342 person-years): rate ratio: 0. 38 (95% CI: 0. 28, 0. 51); p<0. 001 Cohort studies A meta-analysis of prospective and retrospective cohort studies showed that LAIs were superior to oral antipsychotics in: 3 • Decreasing hospitalisation rates (15 studies, 68, 009 personyears): rate ratio: 0. 85 (95% CI: 0. 78– 0. 93); p<0. 001 • Improving discontinuation rates (10 studies, n=37, 293): risk ratio: 0. 78 (95% CI: 0. 67– 0. 91); p=0. 001 CI=confidence interval; LAI=long-acting injectable; RCT=randomised controlled trial 1. Adapted from: Leucht et al. Lancet 2012; 379(9831): 2063– 2071; 2. Kishimoto et al. J Clin Psychiatry 2013; 74(10): 957– 965; 3. Kishimoto et al. Schizophr Bull 2018; 44(3): 603– 619 27
Take home points • A key challenge for physicians is to choose an antipsychotic that effectively controls symptoms, while minimising adverse events – however, physicians typically prioritise efficacy for positive and negative symptoms • Adverse events are associated with lower adherence to treatment • Non-adherence to antipsychotic therapy is common, and increases the risk of psychotic relapse • LAI formulations increase adherence rates, and reduce the risk of relapse LAI=Long-acting injectable 28
How do adverse events impact a patient’s functioning? …are these adverse events a necessary compromise for continued symptom control? 29
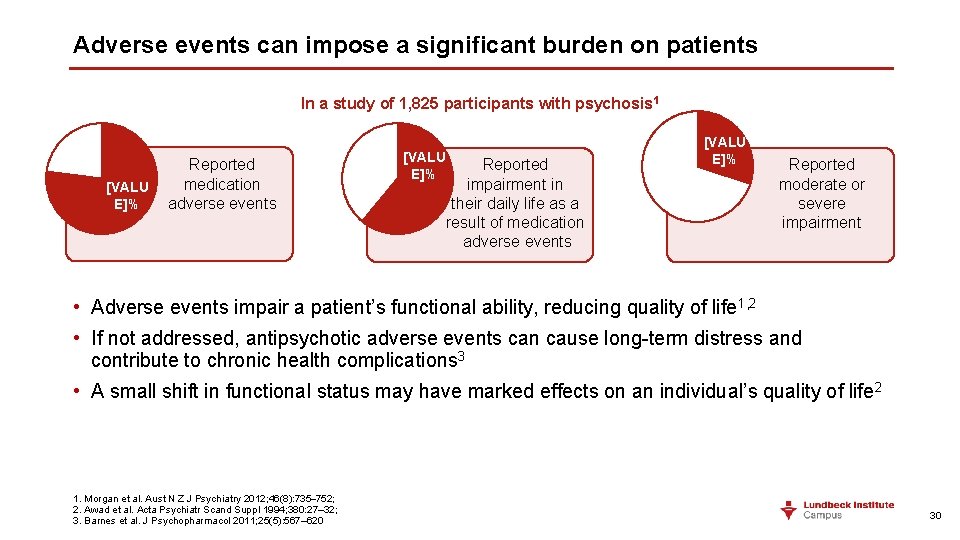
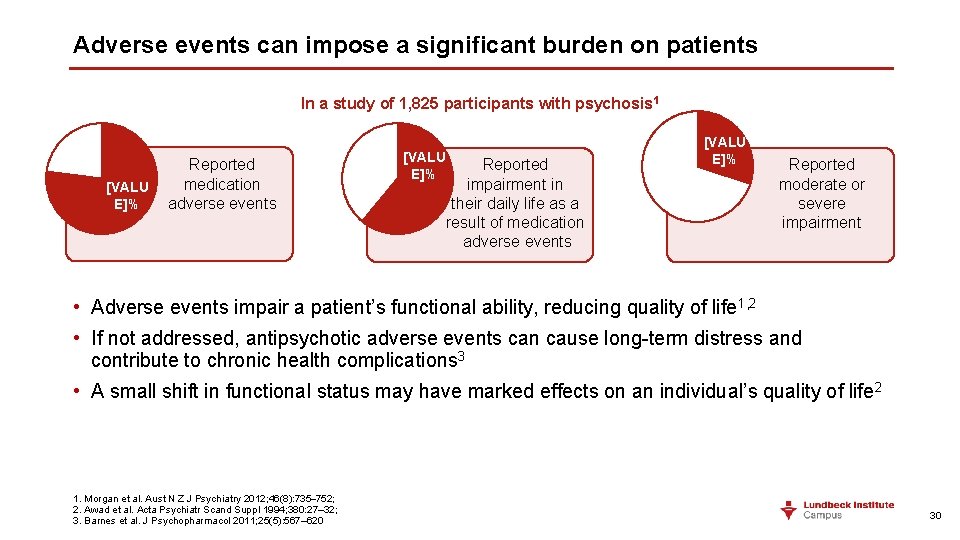
Adverse events can impose a significant burden on patients In a study of 1, 825 participants with psychosis 1 [VALU E]% Reported medication adverse events [VALU E]% Reported impairment in their daily life as a result of medication adverse events [VALU E]% Reported moderate or severe impairment • Adverse events impair a patient’s functional ability, reducing quality of life 1, 2 • If not addressed, antipsychotic adverse events can cause long-term distress and contribute to chronic health complications 3 • A small shift in functional status may have marked effects on an individual’s quality of life 2 1. Morgan et al. Aust N Z J Psychiatry 2012; 46(8): 735– 752; 2. Awad et al. Acta Psychiatr Scand Suppl 1994; 380: 27– 32; 3. Barnes et al. J Psychopharmacol 2011; 25(5): 567– 620 30
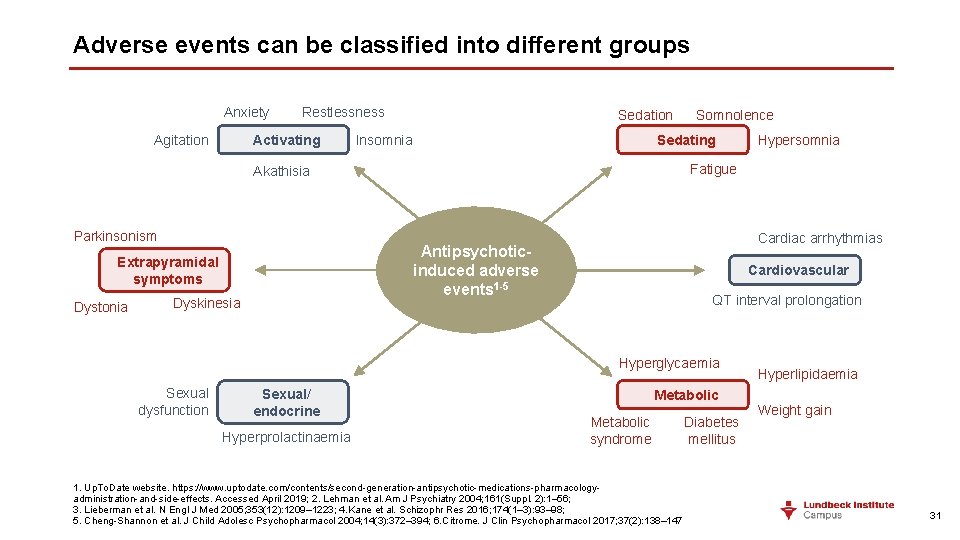
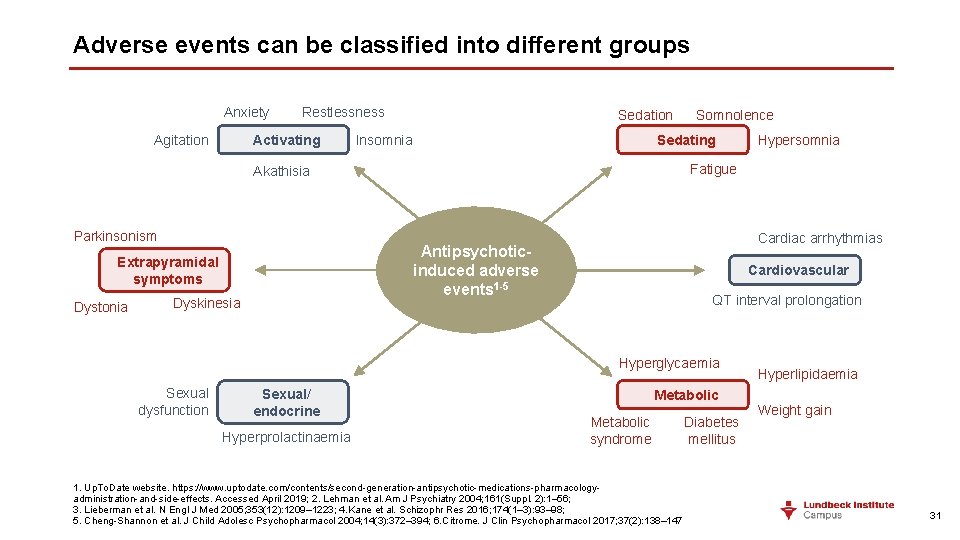
Adverse events can be classified into different groups Anxiety Agitation Restlessness Activating Sedation Insomnia Sedating Dystonia Cardiac arrhythmias Antipsychoticinduced adverse events 1 -5 Extrapyramidal symptoms Dyskinesia Cardiovascular QT interval prolongation Hyperglycaemia Sexual dysfunction Sexual/ endocrine Hyperprolactinaemia Hypersomnia Fatigue Akathisia Parkinsonism Somnolence Metabolic syndrome 1. Up. To. Date website. https: //www. uptodate. com/contents/second-generation-antipsychotic-medications-pharmacologyadministration-and-side-effects. Accessed April 2019; 2. Lehman et al. Am J Psychiatry 2004; 161(Suppl. 2): 1– 56; 3. Lieberman et al. N Engl J Med 2005; 353(12): 1209– 1223; 4. Kane et al. Schizophr Res 2016; 174(1– 3): 93– 98; 5. Cheng-Shannon et al. J Child Adolesc Psychopharmacol 2004; 14(3): 372– 394; 6. Citrome. J Clin Psychopharmacol 2017; 37(2): 138– 147 Diabetes mellitus Hyperlipidaemia Weight gain 31
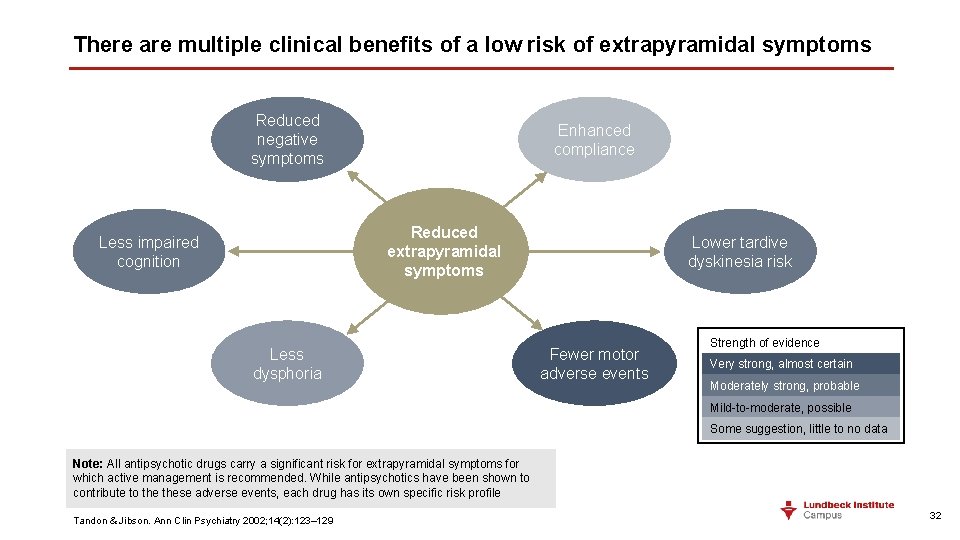
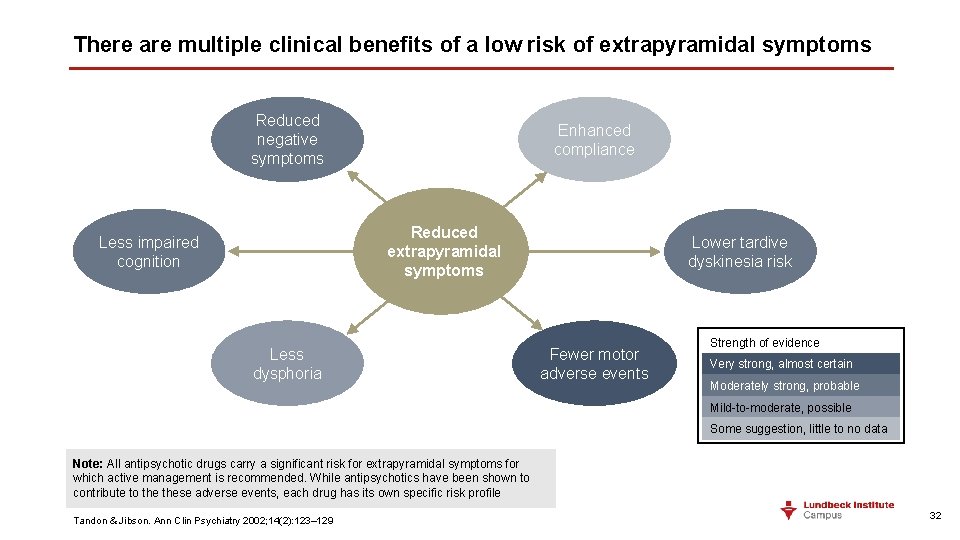
There are multiple clinical benefits of a low risk of extrapyramidal symptoms Reduced negative symptoms Enhanced compliance Reduced extrapyramidal symptoms Less impaired cognition Less dysphoria Lower tardive dyskinesia risk Fewer motor adverse events Strength of evidence Very strong, almost certain Moderately strong, probable Mild-to-moderate, possible Some suggestion, little to no data Note: All antipsychotic drugs carry a significant risk for extrapyramidal symptoms for which active management is recommended. While antipsychotics have been shown to contribute to these adverse events, each drug has its own specific risk profile Tandon & Jibson. Ann Clin Psychiatry 2002; 14(2): 123– 129 32
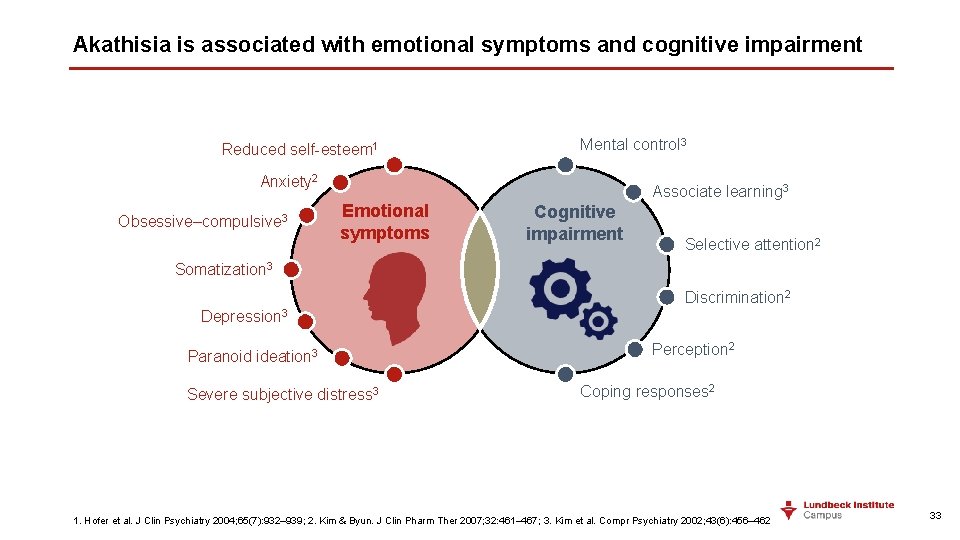
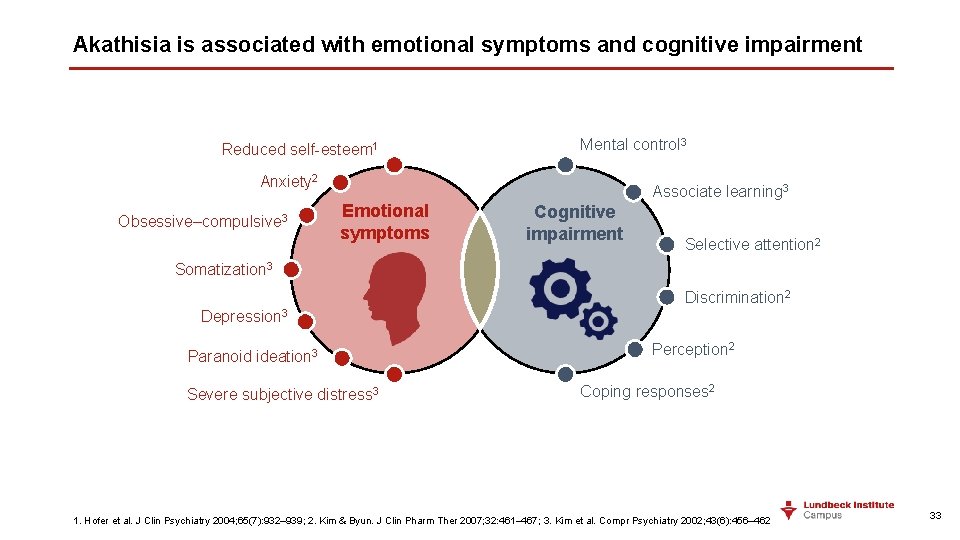
Akathisia is associated with emotional symptoms and cognitive impairment Reduced self-esteem 1 Mental control 3 Anxiety 2 Obsessive–compulsive 3 Associate learning 3 Emotional symptoms Cognitive impairment Selective attention 2 Somatization 3 Discrimination 2 Depression 3 Paranoid ideation 3 Severe subjective distress 3 Perception 2 Coping responses 2 1. Hofer et al. J Clin Psychiatry 2004; 65(7): 932– 939; 2. Kim & Byun. J Clin Pharm Ther 2007; 32: 461– 467; 3. Kim et al. Compr Psychiatry 2002; 43(6): 456– 462 33
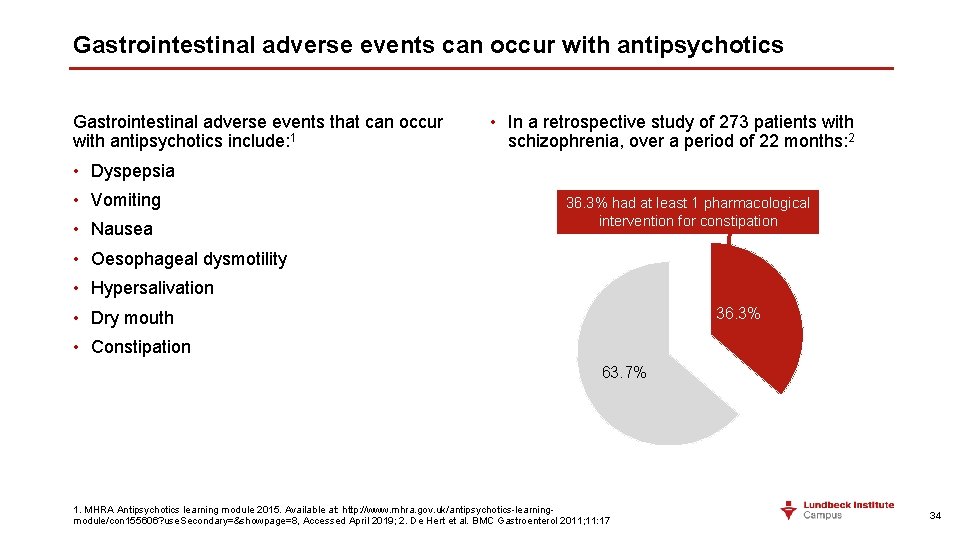
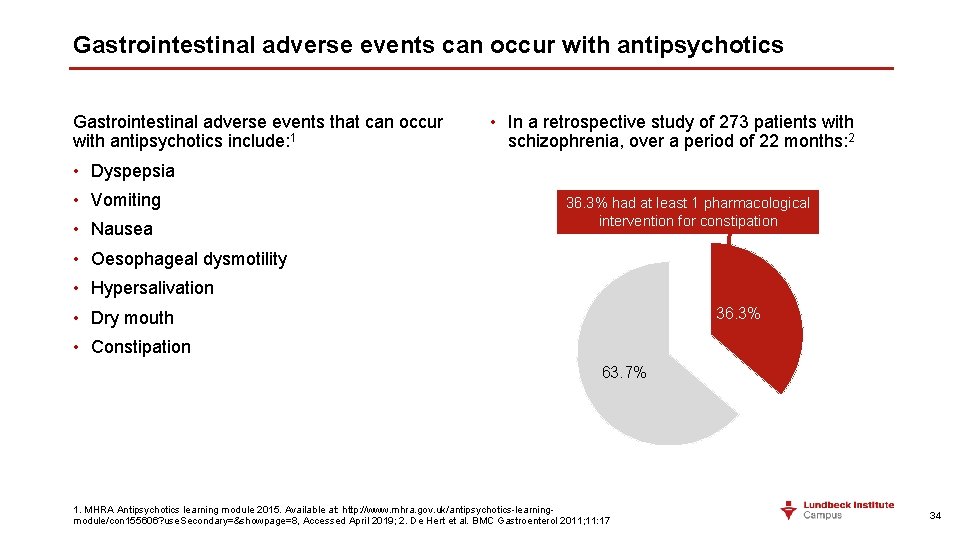
Gastrointestinal adverse events can occur with antipsychotics Gastrointestinal adverse events that can occur with antipsychotics include: 1 • In a retrospective study of 273 patients with schizophrenia, over a period of 22 months: 2 • Dyspepsia • Vomiting • Nausea 36. 3% had at least 1 pharmacological intervention for constipation • Oesophageal dysmotility • Hypersalivation 36. 3% • Dry mouth • Constipation 63. 7% 1. MHRA Antipsychotics learning module 2015. Available at: http: //www. mhra. gov. uk/antipsychotics-learningmodule/con 155606? use. Secondary=&showpage=8, Accessed April 2019; 2. De Hert et al. BMC Gastroenterol 2011; 11: 17 34
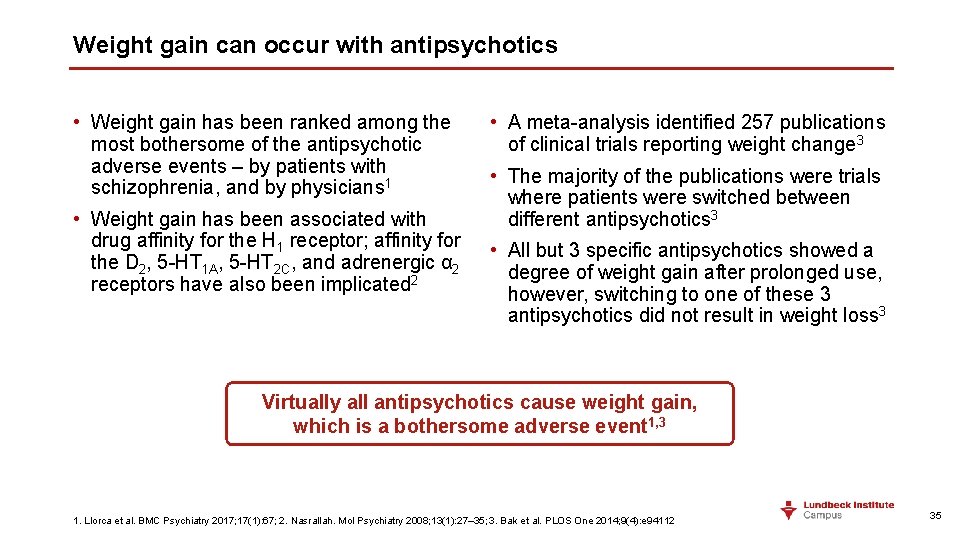
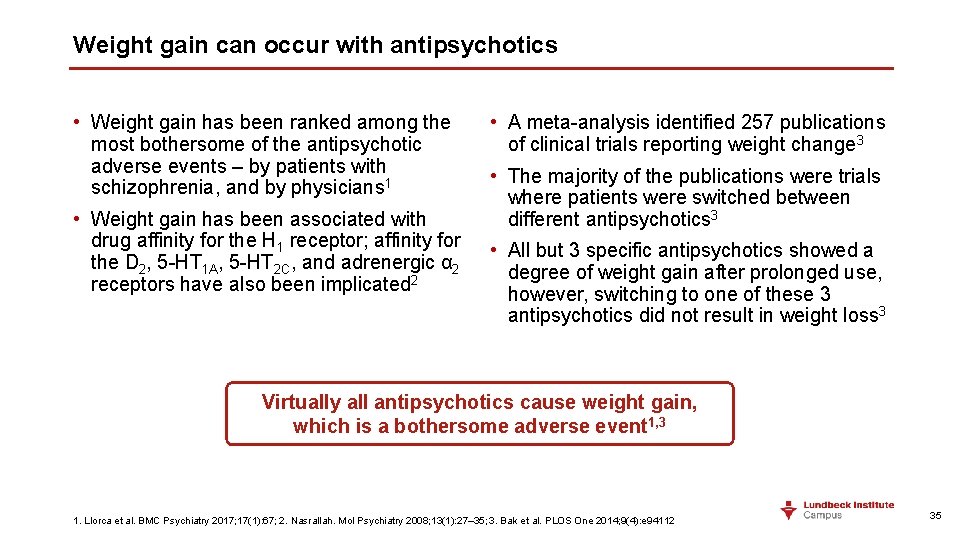
Weight gain can occur with antipsychotics • Weight gain has been ranked among the most bothersome of the antipsychotic adverse events – by patients with schizophrenia, and by physicians 1 • Weight gain has been associated with drug affinity for the H 1 receptor; affinity for the D 2, 5 -HT 1 A, 5 -HT 2 C, and adrenergic α 2 receptors have also been implicated 2 • A meta-analysis identified 257 publications of clinical trials reporting weight change 3 • The majority of the publications were trials where patients were switched between different antipsychotics 3 • All but 3 specific antipsychotics showed a degree of weight gain after prolonged use, however, switching to one of these 3 antipsychotics did not result in weight loss 3 Virtually all antipsychotics cause weight gain, which is a bothersome adverse event 1, 3 1. Llorca et al. BMC Psychiatry 2017; 17(1): 67; 2. Nasrallah. Mol Psychiatry 2008; 13(1): 27– 35; 3. Bak et al. PLOS One 2014; 9(4): e 94112 35
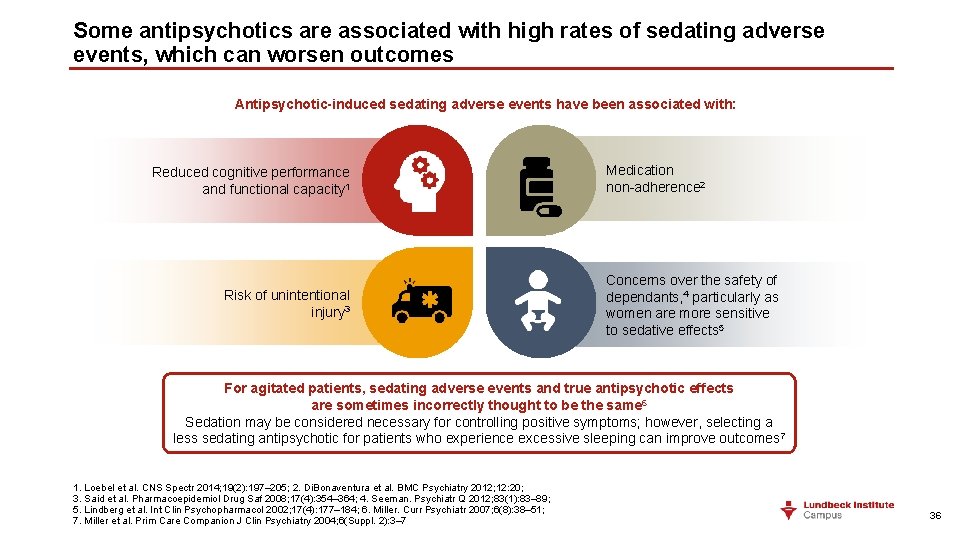
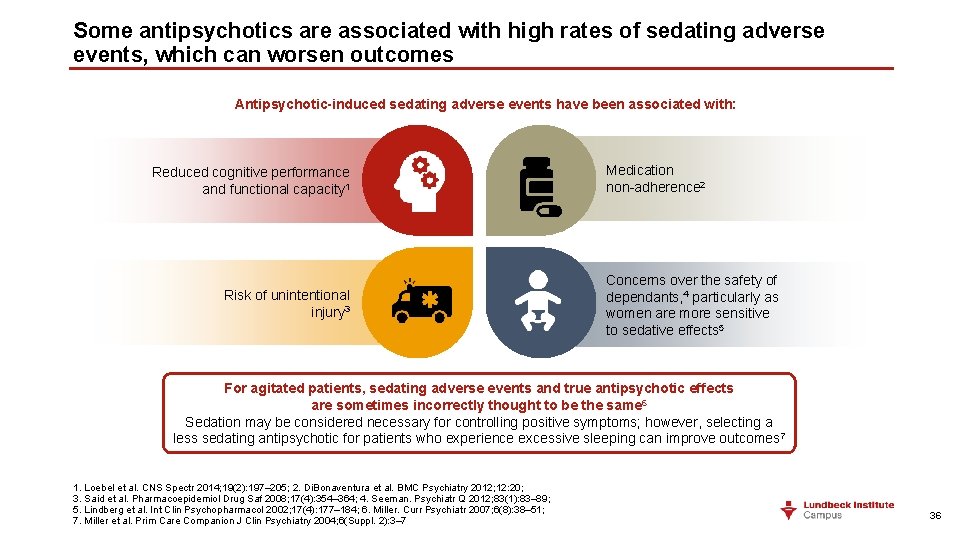
Some antipsychotics are associated with high rates of sedating adverse events, which can worsen outcomes Antipsychotic-induced sedating adverse events have been associated with: Reduced cognitive performance and functional capacity 1 Risk of unintentional injury 3 Medication non-adherence 2 Concerns over the safety of dependants, 4 particularly as women are more sensitive to sedative effects 5 For agitated patients, sedating adverse events and true antipsychotic effects are sometimes incorrectly thought to be the same 6 Sedation may be considered necessary for controlling positive symptoms; however, selecting a less sedating antipsychotic for patients who experience excessive sleeping can improve outcomes 7 1. Loebel et al. CNS Spectr 2014; 19(2): 197– 205; 2. Di. Bonaventura et al. BMC Psychiatry 2012; 12: 20; 3. Said et al. Pharmacoepidemiol Drug Saf 2008; 17(4): 354– 364; 4. Seeman. Psychiatr Q 2012; 83(1): 83– 89; 5. Lindberg et al. Int Clin Psychopharmacol 2002; 17(4): 177– 184; 6. Miller. Curr Psychiatr 2007; 6(8): 38– 51; 7. Miller et al. Prim Care Companion J Clin Psychiatry 2004; 6(Suppl. 2): 3– 7 36
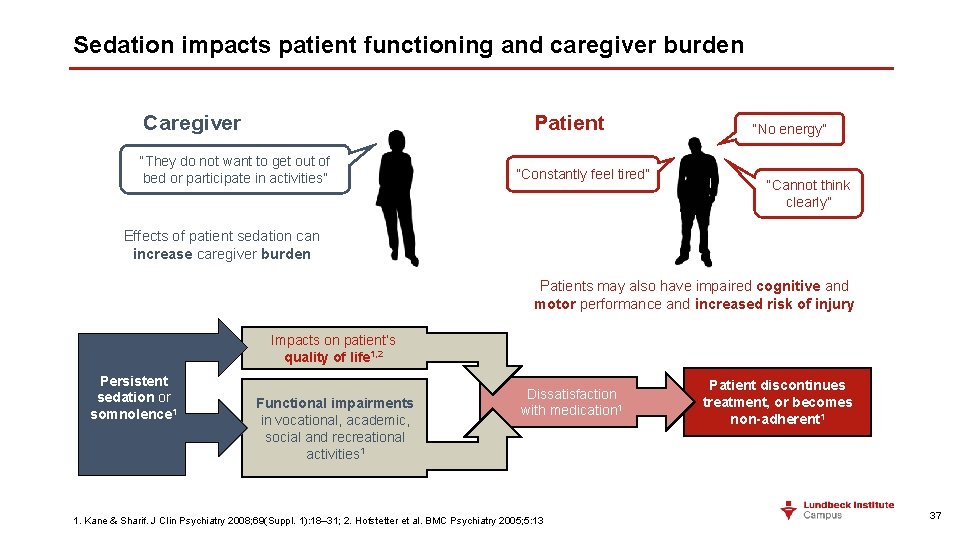
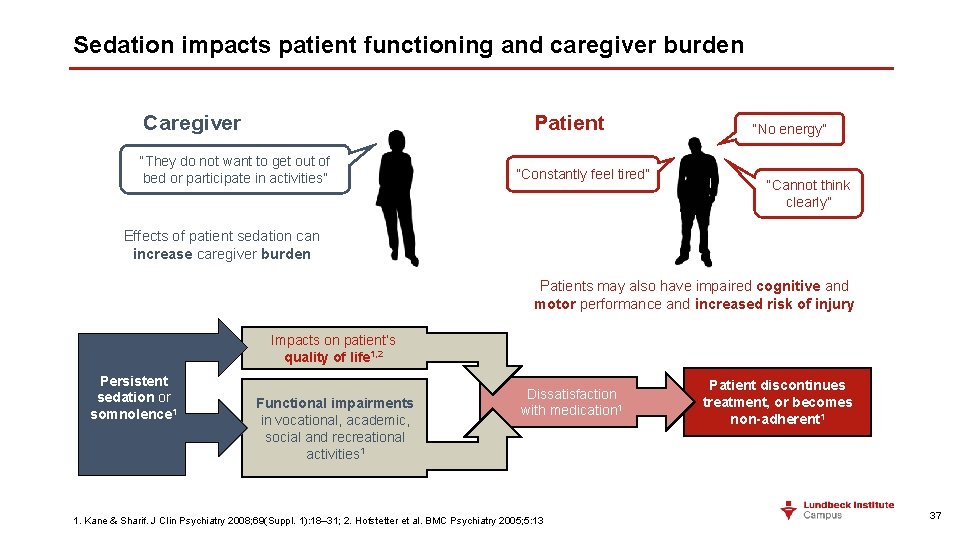
Sedation impacts patient functioning and caregiver burden Patient Caregiver “They do not want to get out of bed or participate in activities” “Constantly feel tired” “No energy” “Cannot think clearly” Effects of patient sedation can increase caregiver burden Patients may also have impaired cognitive and motor performance and increased risk of injury Impacts on patient’s quality of life 1, 2 Persistent sedation or somnolence 1 Functional impairments in vocational, academic, social and recreational activities 1 Dissatisfaction with medication 1 1. Kane & Sharif. J Clin Psychiatry 2008; 69(Suppl. 1): 18– 31; 2. Hofstetter et al. BMC Psychiatry 2005; 5: 13 Patient discontinues treatment, or becomes non-adherent 1 37
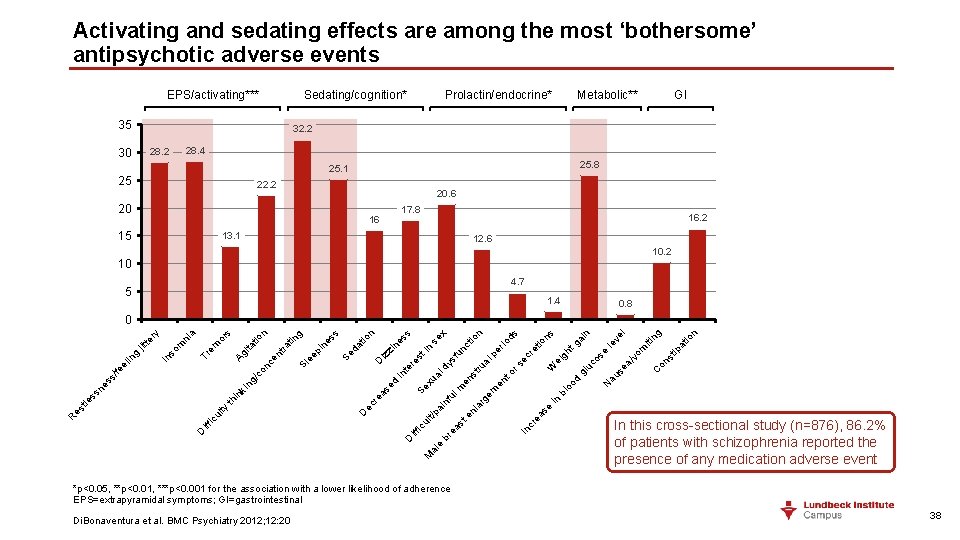
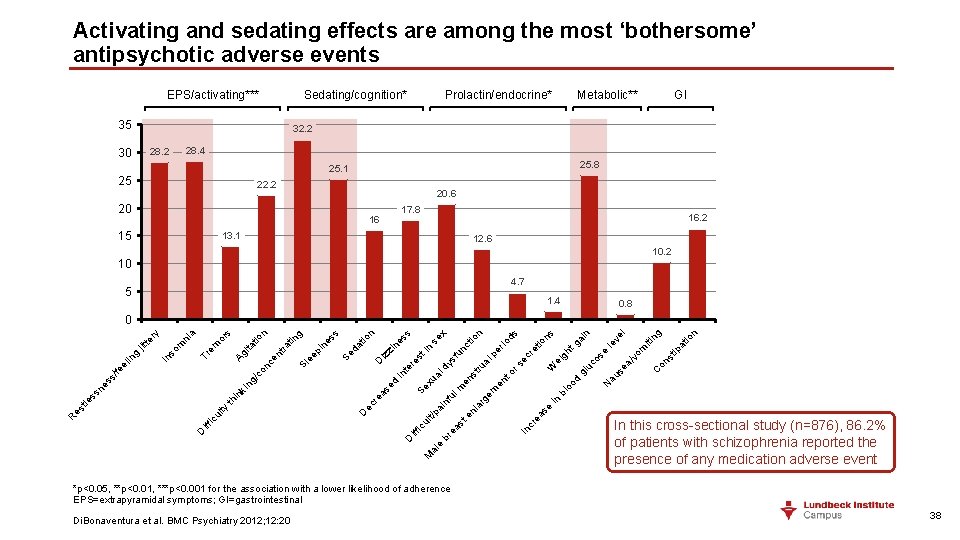
Activating and sedating effects are among the most ‘bothersome’ antipsychotic adverse events EPS/activating*** Sedating/cognition* 35 Prolactin/endocrine* Metabolic** GI 32. 2 28. 4 28. 2 30 25. 8 25. 1 25 22. 2 20. 6 20 17. 8 16 15 16. 2 13. 1 12. 6 10. 2 10 4. 7 5 1. 4 0. 8 n io ng C on st ip m vo a/ at iti ve le se au oo bl N d gl uc os e tg gh W ei l n ai ns tio re ec en em in rg In cr ea se la en st ea br e al M rs to st en m ul nf ai t/p ul ic iff D rio pe al ru dy al xu Se re ec D ds n ct un sf st re te in ed as io se in ne D iz zi at ki in th ty D iff ic ul x ss n io s Se d in ep Sl e nt ra tin es g n on /c ng ss ss ne tle es R ce Ag ita em Tr m so In tio or a ni ry te jit g in /fe el s 0 In this cross-sectional study (n=876), 86. 2% of patients with schizophrenia reported the presence of any medication adverse event *p<0. 05, **p<0. 01, ***p<0. 001 for the association with a lower likelihood of adherence EPS=extrapyramidal symptoms; GI=gastrointestinal Di. Bonaventura et al. BMC Psychiatry 2012; 12: 20 38
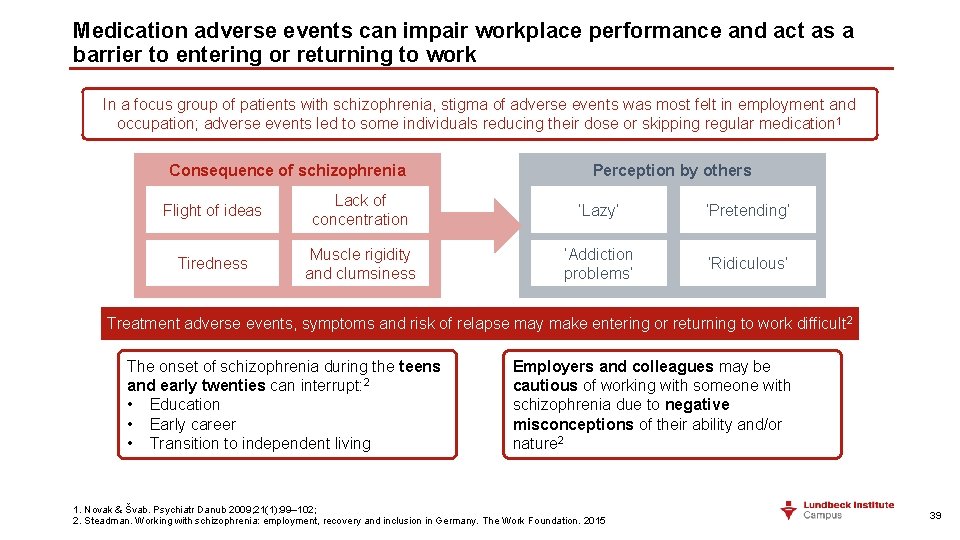
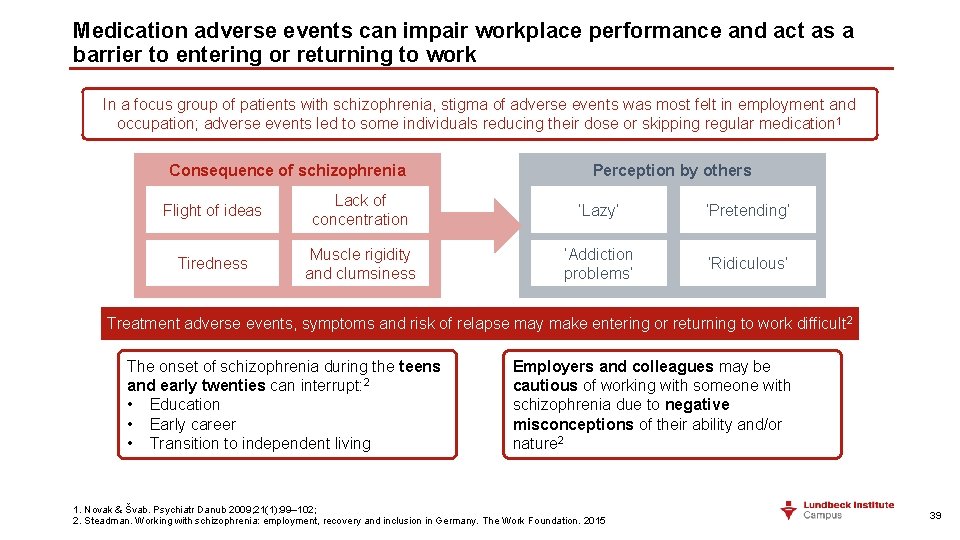
Medication adverse events can impair workplace performance and act as a barrier to entering or returning to work In a focus group of patients with schizophrenia, stigma of adverse events was most felt in employment and occupation; adverse events led to some individuals reducing their dose or skipping regular medication 1 Consequence of schizophrenia Perception by others Flight of ideas Lack of concentration ‘Lazy’ ‘Pretending’ Tiredness Muscle rigidity and clumsiness ‘Addiction problems’ ‘Ridiculous’ Treatment adverse events, symptoms and risk of relapse may make entering or returning to work difficult 2 The onset of schizophrenia during the teens and early twenties can interrupt: 2 • Education • Early career • Transition to independent living Employers and colleagues may be cautious of working with someone with schizophrenia due to negative misconceptions of their ability and/or nature 2 1. Novak & Švab. Psychiatr Danub 2009; 21(1): 99– 102; 2. Steadman. Working with schizophrenia: employment, recovery and inclusion in Germany. The Work Foundation. 2015 39
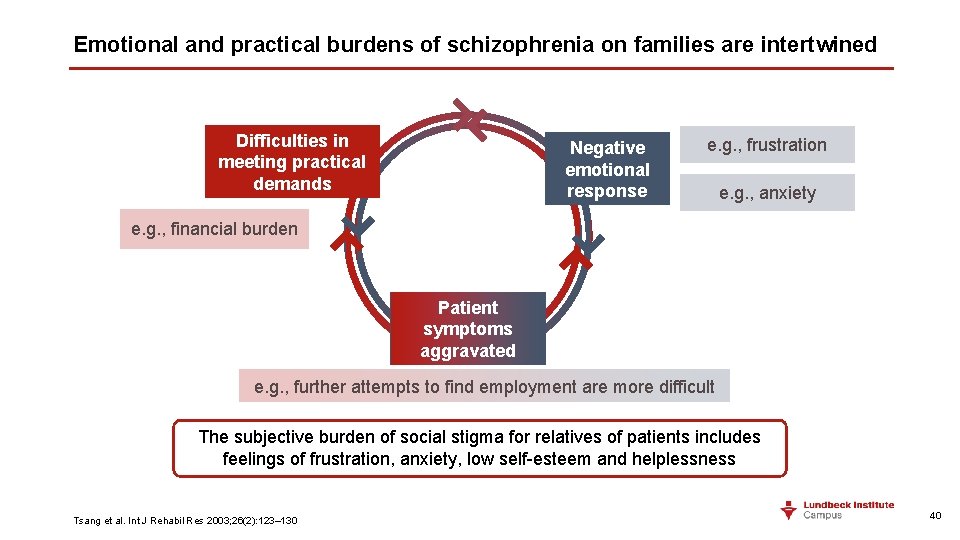
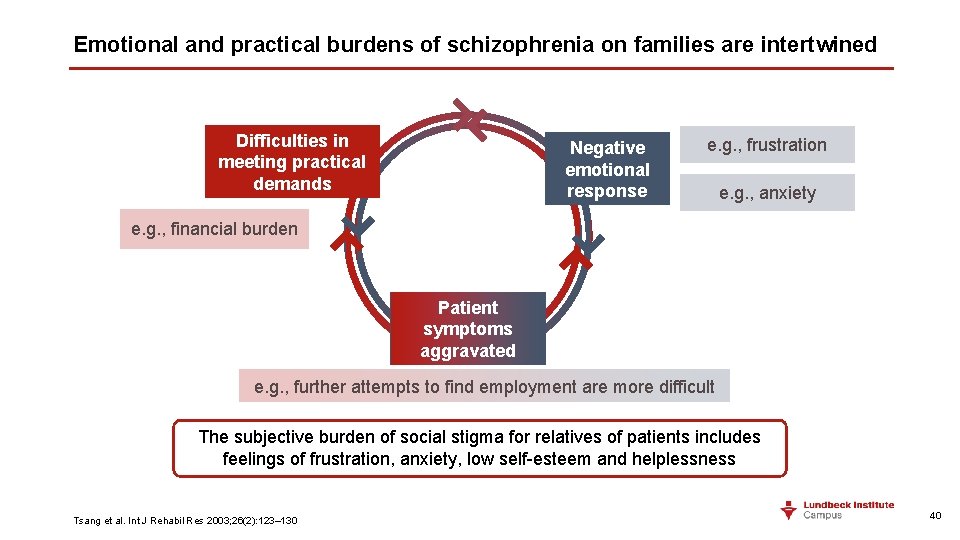
Emotional and practical burdens of schizophrenia on families are intertwined Difficulties in meeting practical demands Negative emotional response e. g. , frustration e. g. , anxiety e. g. , financial burden Patient symptoms aggravated e. g. , further attempts to find employment are more difficult The subjective burden of social stigma for relatives of patients includes feelings of frustration, anxiety, low self-esteem and helplessness Tsang et al. Int J Rehabil Res 2003; 26(2): 123– 130 40
Take home points • Treatment adverse events – including activating, sedating, cardiovascular, metabolic, sexual, and endocrine effects, and extrapyramidal symptoms – are burdensome for patients, reducing functioning and quality of life • Some antipsychotics are associated with sedation, which worsens outcomes and increases caregiver burden • The adverse-event burden of antipsychotics reduces patient functioning, and can act as a barrier to entering or returning to work EPS=extrapyramidal symptoms 41
The importance of early intervention for patients with schizophrenia 42
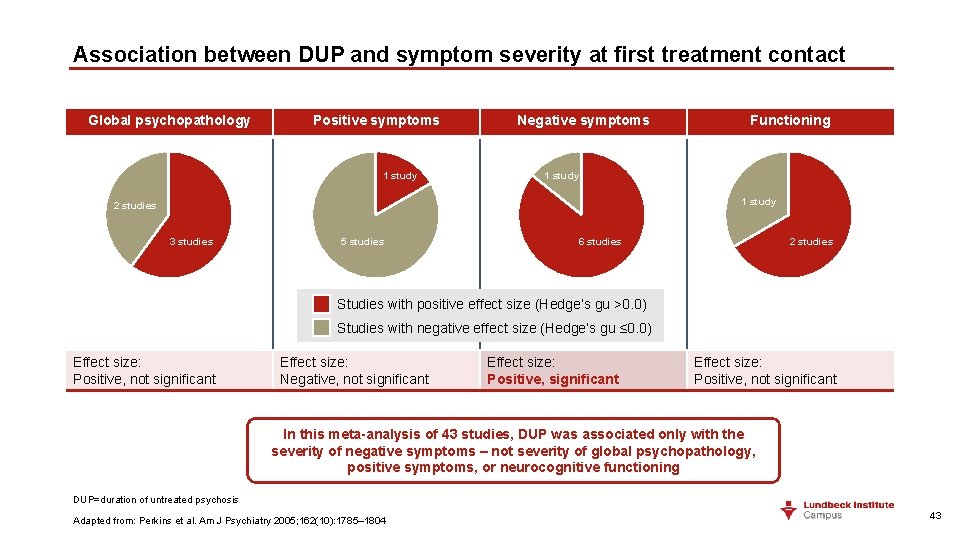
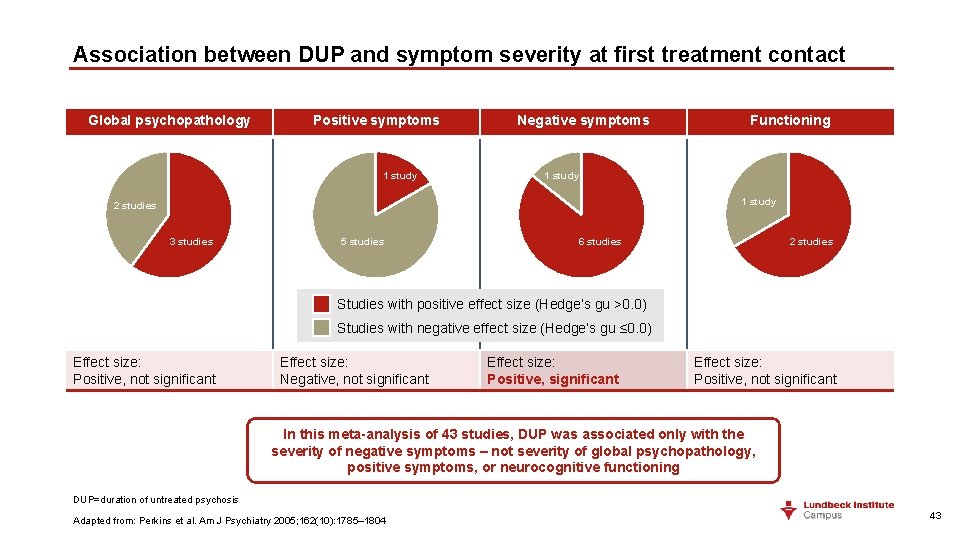
Association between DUP and symptom severity at first treatment contact Global psychopathology Positive symptoms 1 study Negative symptoms Functioning 1 study 2 studies 3 studies 5 studies 2 studies 6 studies Studies with positive effect size (Hedge’s gu >0. 0) Studies with negative effect size (Hedge’s gu ≤ 0. 0) Effect size: Positive, not significant Effect size: Negative, not significant Effect size: Positive, not significant In this meta-analysis of 43 studies, DUP was associated only with the severity of negative symptoms – not severity of global psychopathology, positive symptoms, or neurocognitive functioning DUP=duration of untreated psychosis Adapted from: Perkins et al. Am J Psychiatry 2005; 162(10): 1785– 1804 43
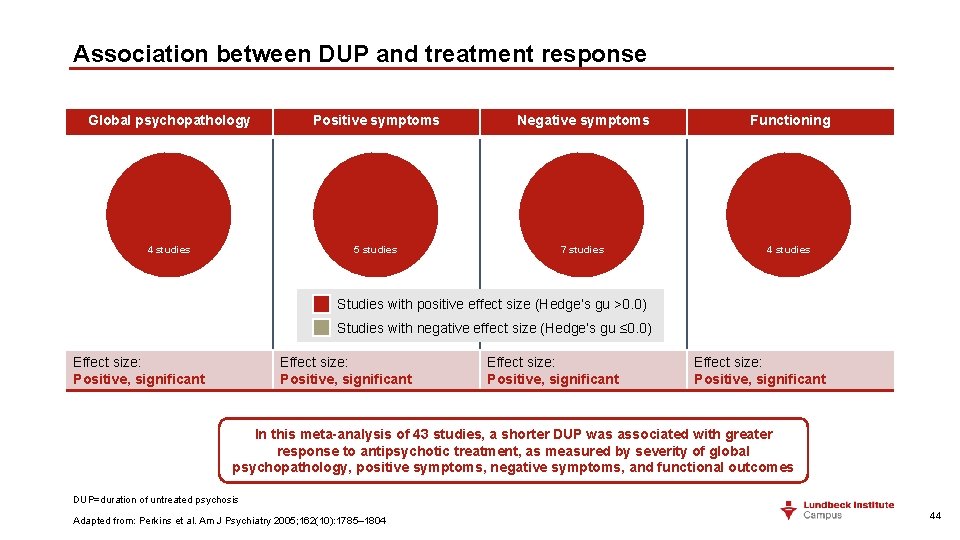
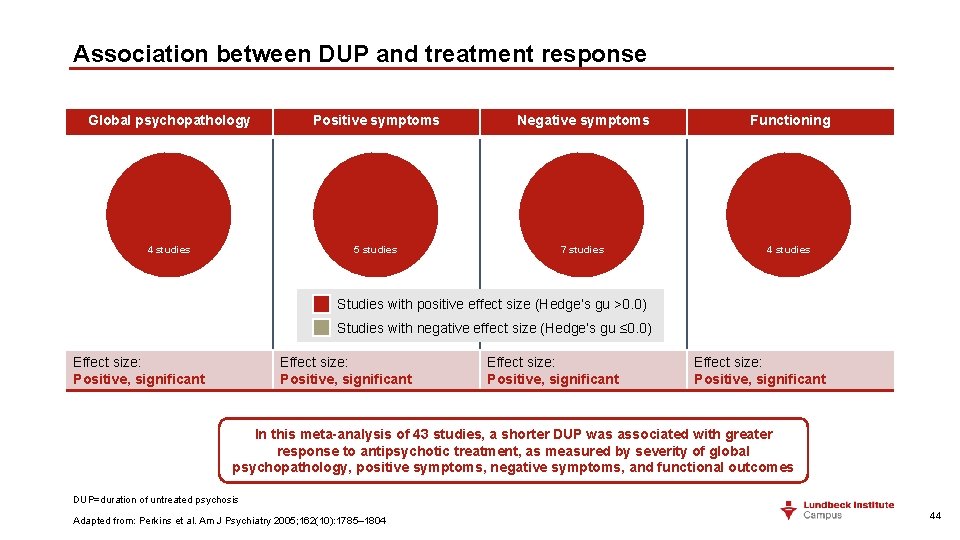
Association between DUP and treatment response Global psychopathology Positive symptoms Negative symptoms Functioning 4 studies 5 studies 7 studies 4 studies Studies with positive effect size (Hedge’s gu >0. 0) Studies with negative effect size (Hedge’s gu ≤ 0. 0) Effect size: Positive, significant In this meta-analysis of 43 studies, a shorter DUP was associated with greater response to antipsychotic treatment, as measured by severity of global psychopathology, positive symptoms, negative symptoms, and functional outcomes DUP=duration of untreated psychosis Adapted from: Perkins et al. Am J Psychiatry 2005; 162(10): 1785– 1804 44
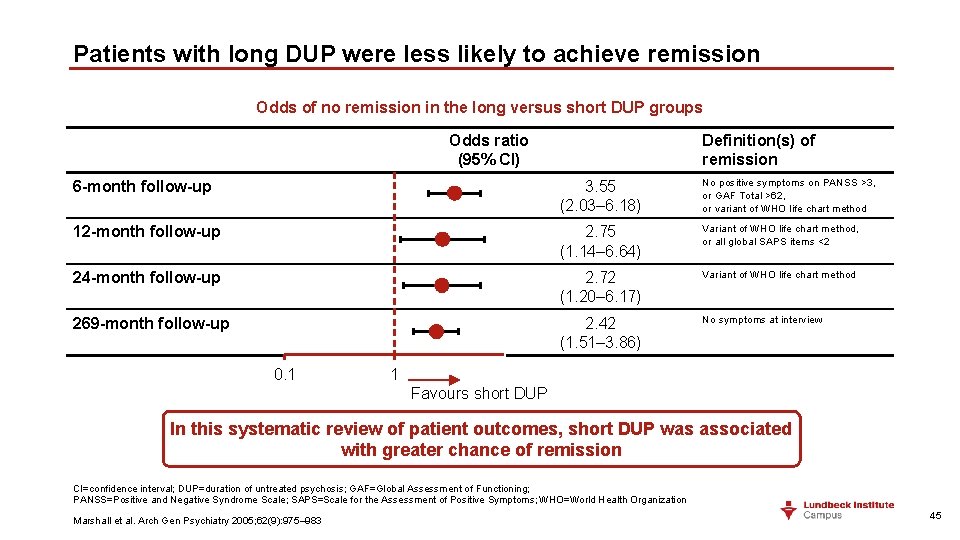
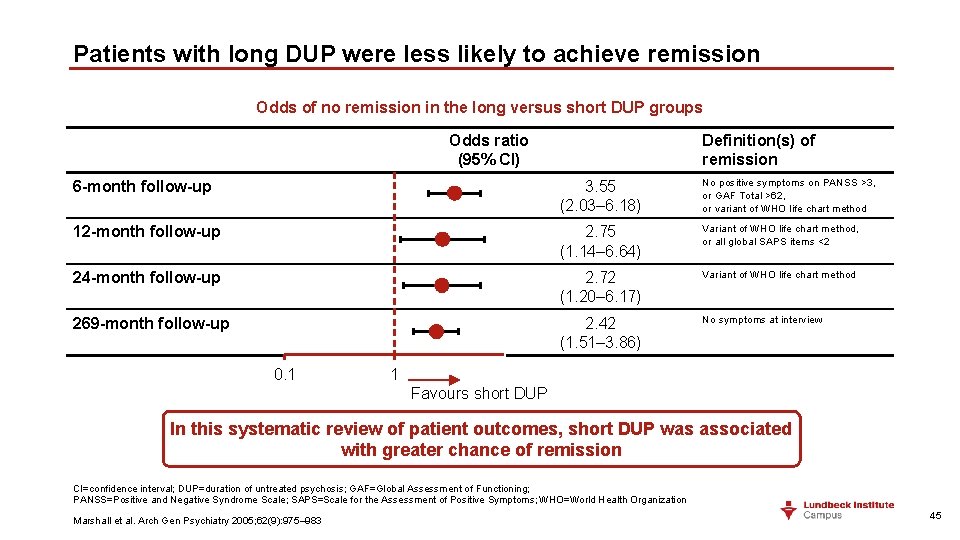
Patients with long DUP were less likely to achieve remission Odds of no remission in the long versus short DUP groups Odds ratio (95% CI) Definition(s) of remission 6 -month follow-up 3. 55 (2. 03– 6. 18) No positive symptoms on PANSS >3, or GAF Total >62, or variant of WHO life chart method 12 -month follow-up 2. 75 (1. 14– 6. 64) Variant of WHO life chart method, or all global SAPS items <2 24 -month follow-up 2. 72 (1. 20– 6. 17) Variant of WHO life chart method 269 -month follow-up 2. 42 (1. 51– 3. 86) No symptoms at interview 0. 1 1 Favours short DUP In this systematic review of patient outcomes, short DUP was associated with greater chance of remission CI=confidence interval; DUP=duration of untreated psychosis; GAF=Global Assessment of Functioning; PANSS=Positive and Negative Syndrome Scale; SAPS=Scale for the Assessment of Positive Symptoms; WHO=World Health Organization Marshall et al. Arch Gen Psychiatry 2005; 62(9): 975– 983 45
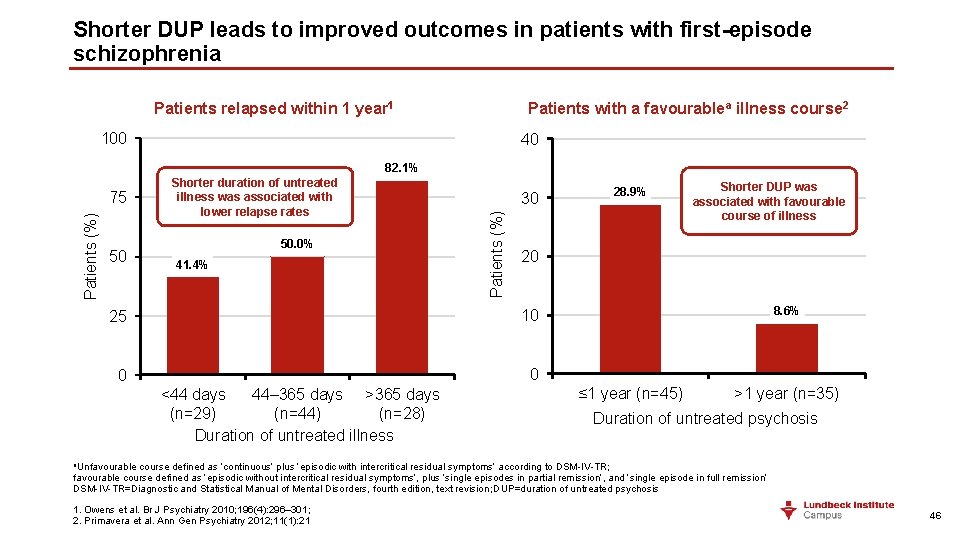
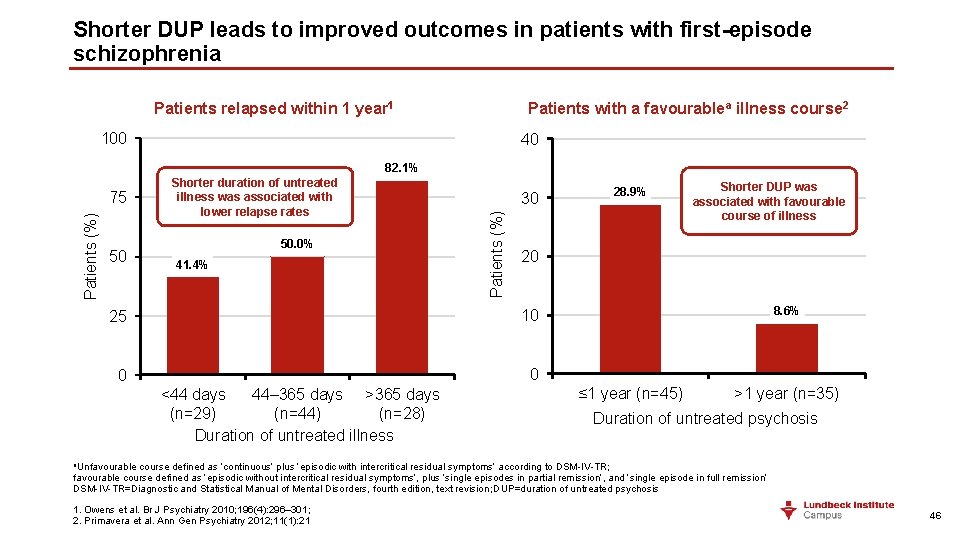
Shorter DUP leads to improved outcomes in patients with first-episode schizophrenia Patients relapsed within 1 year 1 Patients with a favourablea illness course 2 100 40 82. 1% 50 50. 0% 41. 4% 30 Patients (%) 75 Shorter duration of untreated illness was associated with lower relapse rates Shorter DUP was associated with favourable course of illness 20 25 10 0 0 <44 days 44– 365 days >365 days (n=29) (n=44) (n=28) Duration of untreated illness 28. 9% 8. 6% ≤ 1 year (n=45) >1 year (n=35) Duration of untreated psychosis a. Unfavourable course defined as ‘continuous’ plus ‘episodic with intercritical residual symptoms’ according to DSM-IV-TR; favourable course defined as ‘episodic without intercritical residual symptoms’, plus ‘single episodes in partial remission’, and ‘single episode in full remission’ DSM-IV-TR=Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision; DUP=duration of untreated psychosis 1. Owens et al. Br J Psychiatry 2010; 196(4): 296– 301; 2. Primavera et al. Ann Gen Psychiatry 2012; 11(1): 21 46
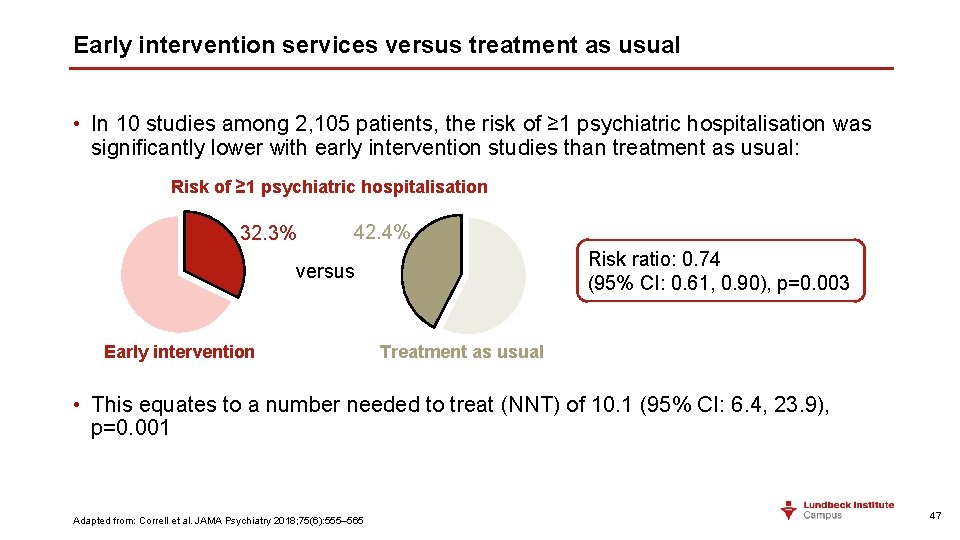
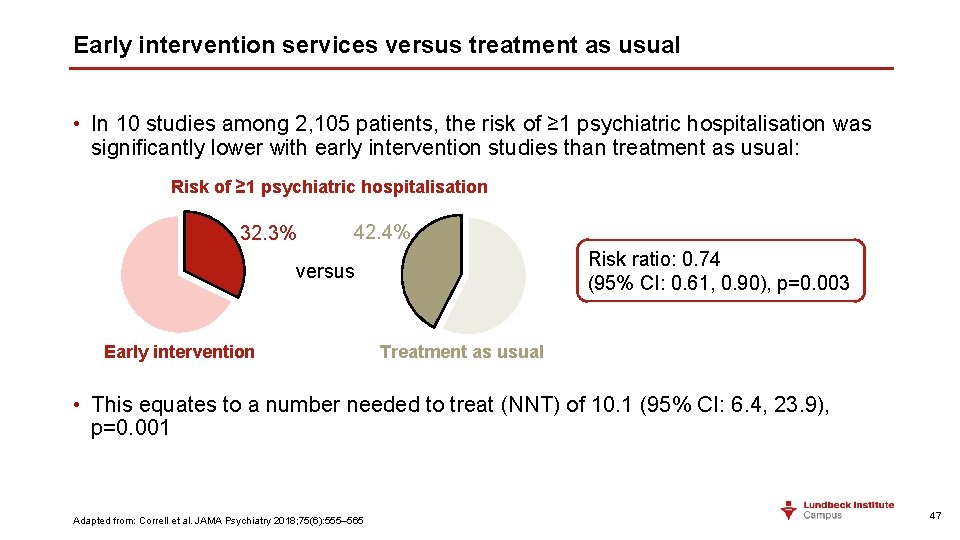
Early intervention services versus treatment as usual • In 10 studies among 2, 105 patients, the risk of ≥ 1 psychiatric hospitalisation was significantly lower with early intervention studies than treatment as usual: Risk of ≥ 1 psychiatric hospitalisation 32. 3% 42. 4% Risk ratio: 0. 74 (95% CI: 0. 61, 0. 90), p=0. 003 versus Early intervention Treatment as usual • This equates to a number needed to treat (NNT) of 10. 1 (95% CI: 6. 4, 23. 9), p=0. 001 Adapted from: Correll et al. JAMA Psychiatry 2018; 75(6): 555– 565 47
Summary 48
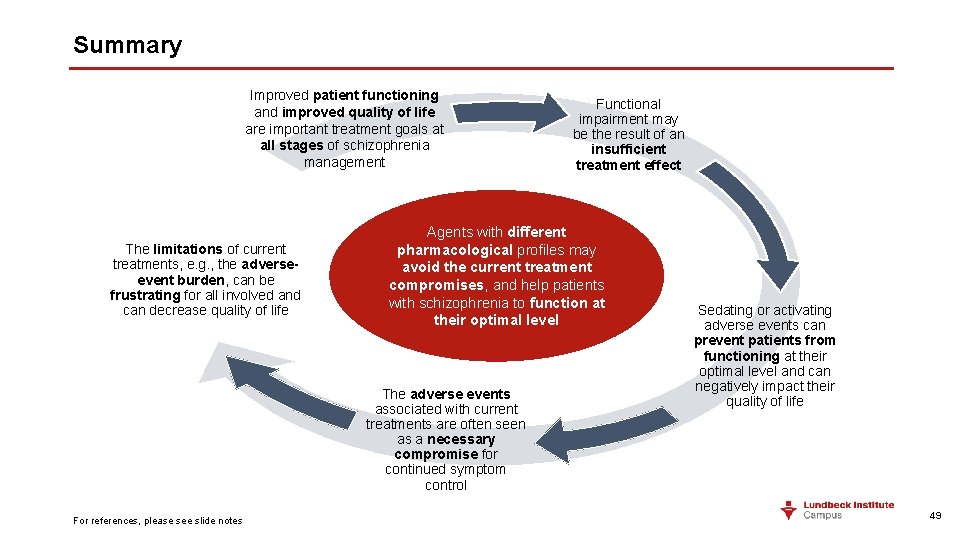
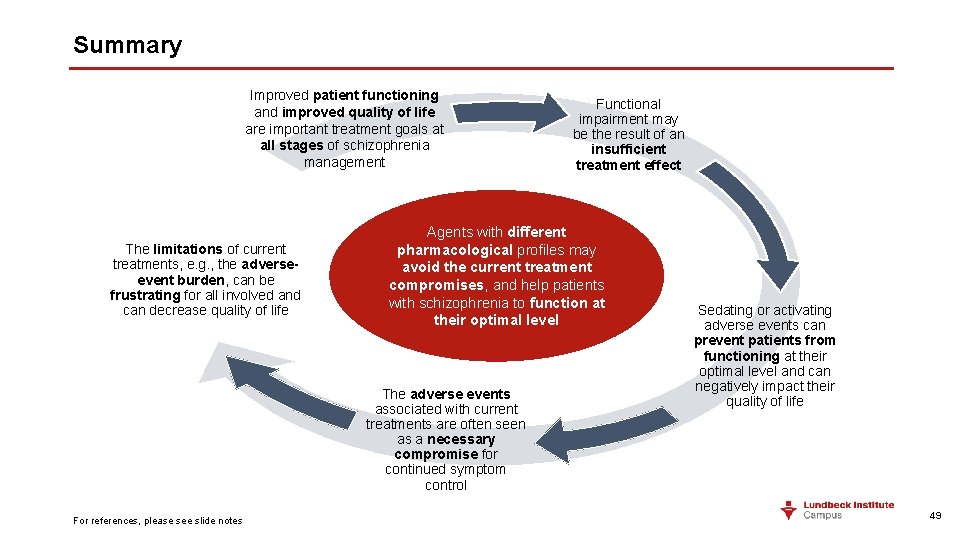
Summary Improved patient functioning and improved quality of life are important treatment goals at all stages of schizophrenia management The limitations of current treatments, e. g. , the adverseevent burden, can be frustrating for all involved and can decrease quality of life Agents with different pharmacological profiles may avoid the current treatment compromises, and help patients with schizophrenia to function at their optimal level The adverse events associated with current treatments are often seen as a necessary compromise for continued symptom control For references, please see slide notes Functional impairment may be the result of an insufficient treatment effect Sedating or activating adverse events can prevent patients from functioning at their optimal level and can negatively impact their quality of life 49
 First-line treatment for schizophrenia
First-line treatment for schizophrenia First-line treatment for schizophrenia
First-line treatment for schizophrenia Variation principle of training
Variation principle of training Principles effective addiction treatment
Principles effective addiction treatment Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Tư thế worms-breton
Tư thế worms-breton Hát lên người ơi alleluia
Hát lên người ơi alleluia Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Phép trừ bù
Phép trừ bù Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ V cc cc
V cc cc Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phối cảnh
Phối cảnh Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Các số nguyên tố
Các số nguyên tố Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Hổ sinh sản vào mùa nào
Hổ sinh sản vào mùa nào Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Hệ hô hấp
Hệ hô hấp Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi National literacy and numeracy learning progressions
National literacy and numeracy learning progressions Victorian curriculum reporting levels
Victorian curriculum reporting levels Atibulon
Atibulon Progression points victorian curriculum english
Progression points victorian curriculum english