SCHIZOPHRENIA BY TIA JENSEN SCHIZOPHRENIA DEMENTIA PRAECOX Schizophrenia

SCHIZOPHRENIA BY TIA JENSEN
SCHIZOPHRENIA - DEMENTIA PRAECOX Schizophrenia is still hard to understand to this day, it's like a puzzle with missing pieces. It's a very complex biochemical brain disorder, which affects a person's ability to determine what's real and what is not. Delusions of all kind fall into place, they may hear voices, or see things others cannot, these are all fixed false beliefs that could be terrifying to the person experiencing them. Schizophrenia is a very serious mental illness.
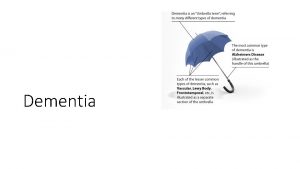
HISTORY OF SCHIZOPHRENIA The word "schizophrenia" is less than 100 years old, however, was discovered in 1887 as a distinct mental illness by German physician Dr. Emile Kraepelin who believed it developed throughout history. There are written documents that identify schizophrenia that can be traced back to the old Pharaonic Egypt, as far back as the second millennium before Christ. Dementia, depression, as well as thought disturbances were mentioned in detail in the Book of Hearts, these are all symptoms of schizophrenia. Early theories proposed that mental disorders were caused by evil possession of the body, and the appropriate treatment was then exorcising these demons, ranging from treatments, such as exposing the patient to certain types of music, sometimes measures were taken to dangerous and sometimes deadly means, such as releasing the evil spirits by drilling holes in the patient's skull. The Swiss psychiatrist, Eugen Bleuler, claimed the term, "schizophrenia" in 1911. The word "schizophrenia" comes from the Greek roots schizo (split) and phrene (mind) to describe the fragmented thinking of people with the disorder. His term was not meant to convey the idea of split or multiple personality, which is a common misunderstanding. Both Bleuler and Kraepelin subdivided schizophrenia into categories, based on prominent symptoms and prognoses. Over the years, those working in this field have continued to attempt to classify types of schizophrenia. Five types were described in the DSM-III: disorganized, catatonic, paranoid, residual, and undifferentiated. The first three categories were originally proposed by Kraepelin. The evidence that schizophrenia biologically-based disease of the brain has accumulated rapidly over the past two decades. Recently this evidence was supported with dynamic brain imaging systems that show very precisely the wave of tissue destruction that takes place in the brain while suffering from schizophrenia.
WHO DOES IT AFFECT & HOW COMMON IS IT • Schizophrenia often begins in late adolescence or early adulthood, it is equally common in men and women. Affecting about 1% of the population, that’s about 40, 000 people in British Columbia. While scientists are still working hard to figure out what causes schizophrenia, Schizophrenia usually first shows up between the ages of 18 and 25 in men and between 25 and 35 in women. Although the age of onset is usually about 10 years later in women than men. Some research has shown that women tend to have more paranoid delusions and hallucinations, whereas men often experience more negative and disorganized symptoms. Schizophrenia seems to run in families. If a close family member (like a parent or sibling) experiences schizophrenia, you may experience an increased risk of schizophrenia. However, it’s important to remember that there is much more to schizophrenia than your genes—genes are one of several risk factors, although not in all cases. Birth trauma and fetal brain damage in the uterus increase the risk for Schizophrenia. Recent research also suggests that heavy marijuana use may trigger the onset of Schizophrenia in youth who are at risk for the illness. Individuals who have an immediate family member with Schizophrenia should avoid using marijuana or other drugs.
WHAT CAUSES IT The causes of schizophrenia, like all mental disorders, are not completely understood or known at this time. There is no known single cause of schizophrenia. Many diseases, such as heart disease, result from an interplay of genetic, behavioral and other factors, and this may be the case for schizophrenia as well. It has been long understood that schizophrenia runs in families. People who have a close relative with schizophrenia are more likely to develop the disorder than are people who have no relatives with the illness. A child whose parent has schizophrenia has about a 10 percent chance of developing schizophrenia themselves. A monozygotic (identical) twin of a person with schizophrenia has the highest risk — a 40 to 65 percent chance of developing the illness. People who have second-degree relatives (aunts, uncles, grandparents, or cousins) with the disease also develop schizophrenia more often than the general population.
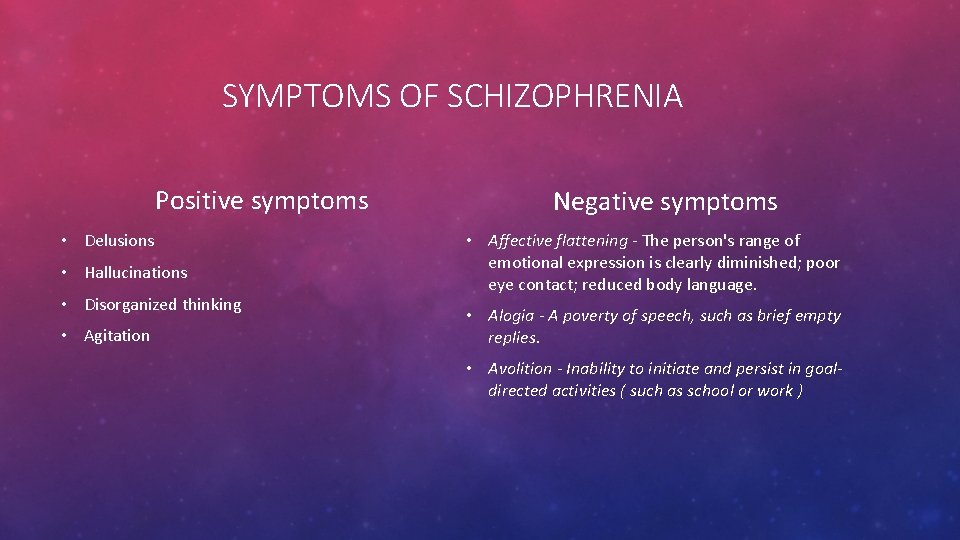
SYMPTOMS OF SCHIZOPHRENIA Positive symptoms • Delusions • Hallucinations • Disorganized thinking • Agitation Negative symptoms • Affective flattening - The person's range of emotional expression is clearly diminished; poor eye contact; reduced body language. • Alogia - A poverty of speech, such as brief empty replies. • Avolition - Inability to initiate and persist in goaldirected activities ( such as school or work )
HOW IS IT DIAGNOSED When doctors suspect someone has schizophrenia, they typically ask for medical and psychiatric histories, conduct a physical exam, and run medical and psychological tests, including: • Tests and screenings. These may include a lab test called a complete blood count (CBC), other blood tests that may help rule out conditions with similar symptoms, and screening for alcohol and drugs. The doctor may also request imaging studies, such as an MRI or CT scan. • Psychological evaluation. A doctor or mental health provider will check mental status by observing appearance and demeanor and asking about thoughts, moods, delusions, hallucinations, substance abuse, and potential for violence or suicide. To be diagnosed with schizophrenia, a person must meet the criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM). A person must have at least two of the following symptoms most of the time during a one-month period, with some level of disturbance being present over six months: • Delusions • Hallucinations • Disorganized speech (indicating disorganized thinking) • Extremely disorganized behavior • Catatonic behavior, which can ranges from a coma-like daze to bizarre, hyperactive behavior • Negative symptoms, which relate to reduced ability or lack of ability to function normally At least one of the symptoms must be delusions, hallucinations or disorganized speech.

CURES, TREATMENTS, AND SUPPORTS Schizophrenia requires lifelong treatment, even when symptoms have subsided. Treatment with medications and psychosocial therapy can help manage the condition. During crisis periods or times of severe symptoms, hospitalization may be necessary to ensure safety, proper nutrition, adequate sleep and basic hygiene. A psychiatrist experienced in treating schizophrenia usually guides treatment. The treatment team also may include a psychologist, social worker, psychiatric nurse and possibly a case manager to coordinate care. Medications are the cornerstone of schizophrenia treatment. However, because medications for schizophrenia can cause serious but rare side effects, people with schizophrenia may be reluctant to take them. Antipsychotic medications are the most commonly prescribed drugs to treat schizophrenia. They're thought to control symptoms by affecting the brain neurotransmitters dopamine and serotonin. A person's willingness to cooperate with treatment may affect medication choice. Someone who is resistant to taking medication consistently may need to be given injections instead of taking a pill. Someone who is agitated may need to be calmed initially with a benzodiazepine such as lorazepam (Ativan), which may be combined with an antipsychotic.
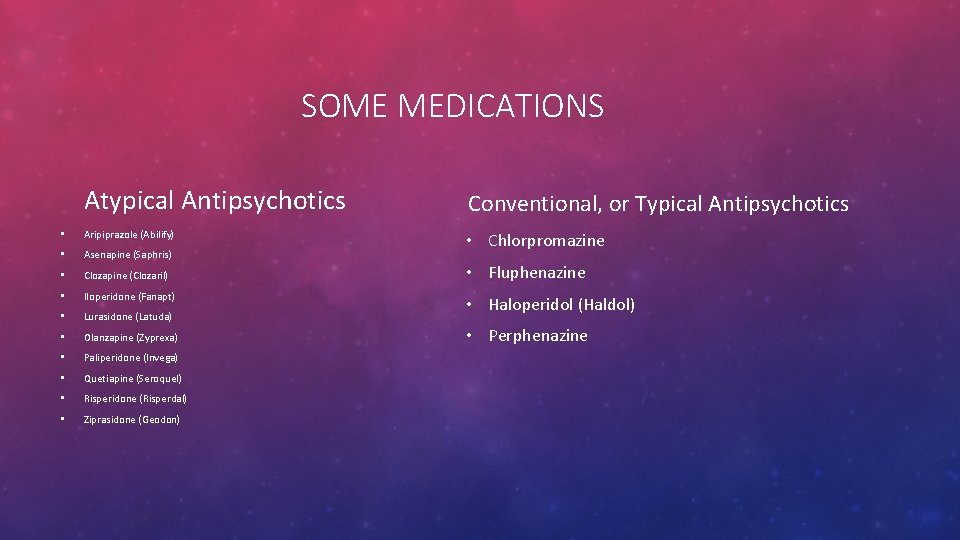
SOME MEDICATIONS Atypical Antipsychotics • Aripiprazole (Abilify) • Asenapine (Saphris) • Clozapine (Clozaril) • Iloperidone (Fanapt) • Lurasidone (Latuda) • Olanzapine (Zyprexa) • Paliperidone (Invega) • Quetiapine (Seroquel) • Risperidone (Risperdal) • Ziprasidone (Geodon) Conventional, or Typical Antipsychotics • Chlorpromazine • Fluphenazine • Haloperidol (Haldol) • Perphenazine
SUPPORT • Individual therapy. Learning to cope with stress and identify early warning signs of relapse can help people with schizophrenia manage their illness. • Social skills training. This focuses on improving communication and social interactions. • Family therapy. This provides support and education to families dealing with schizophrenia. • Vocational rehabilitation and supported employment. This focuses on helping people with schizophrenia prepare for, find and keep jobs. • Most individuals with schizophrenia require some form of daily living support. Many communities have programs to help people with schizophrenia with jobs, housing, self-help groups and crisis situations. A case manager or someone on the treatment team can help find resources. With appropriate treatment, most people with schizophrenia can manage their condition.
LONG-TERM PROGNOSIS A psychiatric follow-up study which included 502 schizophrenics was carried out using well-defined criteria to evaluate the patients. After an average course of 22 years, 22. 1 % of the patients showed complete psychopathological remission, 43. 2 % had non-characteristic types of remission and 34. 7 % suffered from characteristic schizophrenic deficiency syndromes. At the time of the last follow-up investigation, 86. 7 % of the patients were living at home, while 13. 3 % were permanently hospitalized. All together, 55. 9 % were found to be socially recovered. Higher education, depressive traits, perception of delusions, catatonic agitation, and non-characteristic thought disorders at the onset of the illness tended to carry with them a favorable prognosis. On the other hand, low intelligence, abnormal primary personality, premorbid disturbances in social behavior, broken homes, pneumoence-phalographically measurable atrophic or dysplastic changes in the brain ventricles as well as somatic and auditory hallucinations and predominance of hebephrenic symptoms at the onset of the illness tended to lead to an unfavorable Prognosis. The principle of the basic reversibility of typical schizophrenic symptoms and the extensive irreversibility of the non-characteristic defect is important for the psychopathological and social long-term prognosis.
HOW DOES IT IMPACT YOUTH OR OTHERS Adolescents with schizophrenia may see a change in the way they think or decisions they make. Relating to others, including friends and family, may also become challenging. Adolescents with schizophrenia may find it hard to manage their feelings and may act or speak in ways that seem unacceptable or confusing. This is because they may have a distorted or unclear view of their surroundings. Symptoms are the same at any age, but may vary on the person. Schizophrenia is much less common in adolescents than in adults. People with schizophrenia may begin having symptoms in their 20 s, but sometimes symptoms may occur during the later teenage years. Schizophrenia affects both genders equally, but it’s more common for men to experience symptoms in their late teens.
WHAT IS THE ECONOMIC COST OF SCHIZOPHRENIA The burden that schizophrenia imposes on healthcare systems varies among industrialized countries. Over the past decade studies have demonstrated that the direct costs of schizophrenia represented 1. 7% of Canada’s national health expenditures Among those suffering from severe symptoms, inpatient and residential care consume much of these costs, in some cases upwards of 75%. With an upwards of 10% of Canada’s prison population affected by “some form of schizophrenia, ” it is not surprising that the illness placed a $61 -million burden on our criminal justice system in 2004. People with schizophrenia occupy one out of every 12 hospital beds in our country, more than any other illness. In their 2005 analysis, Ron Goeree et al. found that the health and non-healthcare costs of schizophrenia in Canada amounted to over $2 billion. Since many individuals with schizophrenia require inpatient care, hospital-related and residential care expenses make up.

BIBLIOGRAPHY • http: //schizophrenia. com/history. htm • https: //www. cmha. ca/mental-health/understanding-mental-illness/schizophrenia/ • http: //teenmentalhealth. org/toolbox/ • http: //www. schizophrenia. ca • http: //cannabisandpsychosis. ca • http: //psychcentral. com/lib/what-causes-schizophrenia/ • https: //www. cmha. bc. ca/get-informed/mental-health-information/schizophrenia • http: //www. mayoclinic. org/diseases-conditions/schizophrenia/basics/tests-diagnosis/con-20021077 • http: //onlinelibrary. wiley. com/doi/10. 1111/j. 1600 -0447. 1975. tb 00022. x/abstract • http: //www. invega. com/
- Slides: 14