Telemedicine Transforming the Delivery of Stroke Care TzuChing

- Slides: 65
Telemedicine: Transforming the Delivery of Stroke Care Tzu-Ching (Teddy) Wu, MD Associate Professor of Neurology Director of Teleneurology
Disclosure: Tzu-Ching Wu, M. D. • Dr. Tzu-Ching Wu, has no relevant financial interests to disclose Mc. Govern Medical School
Objectives • Identify the functionality and benefits that telemedicine technology can offer to providers and patients • Review the nuts and bolts of a teleneurology/telestroke network • Discuss the keys to success • Discuss the future of teleneurology Mc. Govern Medical School
What is Telemedicine? • “Telemedicine” term coined by Thomas Bird in 1970’s, “healing at a distance” • Telemedicine: the use of telecommunications technologies to provide medical information and services – – – Telephone Fax Email Mobile devices/apps Store Forward (Asynchronous) Interactive real-time audio/video streams • Used for Telestroke/Teleneurology • Synchronous Mc. Govern Medical School
Why is Teleneurology/Telestroke Needed? • Stroke is the fifth leading cause of death in the United States and second leading cause of death worldwide • Stroke is the leading cause of long-term disability in the United States • Acute ischemic stroke is a treatable disease • IV t-PA is still the only proven medical therapy for acute ischemic stroke –Narrow time window, risk of hemorrhagic conversion –(NNT 1 in 8 for near normal, 1 in 3 will improve) • Intra-Arterial Thrombectomy (IAT) recently shown to improved outcomes in certain acute ischemic stroke patients. NNT = 1 in 4 • Both treatments need to be delivered fast in order to be effective • IV t-PA under-utilized / Access to IAT Mc. Govern Medical School
Why is Teleneurology/Telestroke Needed? • Currently ~800, 000 stroke cases per year and with the aging population, incidence likely to double by 2050 • Shortage of neurologist (11% 19% by 2025), including vascular neurologists –Declining number of neurologist taking hospital call and inpatient consultation –Lack to access to acute stroke expertise • Emergency room physician uncertain about administering IV t-PA without guidance from neurologist; rapidly evolving treatments with IA • Disparities in acute stroke care for rural populations –Ten times less likely to receive IV t-PA when compared to urban hospitals –Texas has one of the largest rural populations Mc. Govern Medical School
How? • Neurologists • Technology • Audio/Video • Broadband access • PACS Mc. Govern Medical School
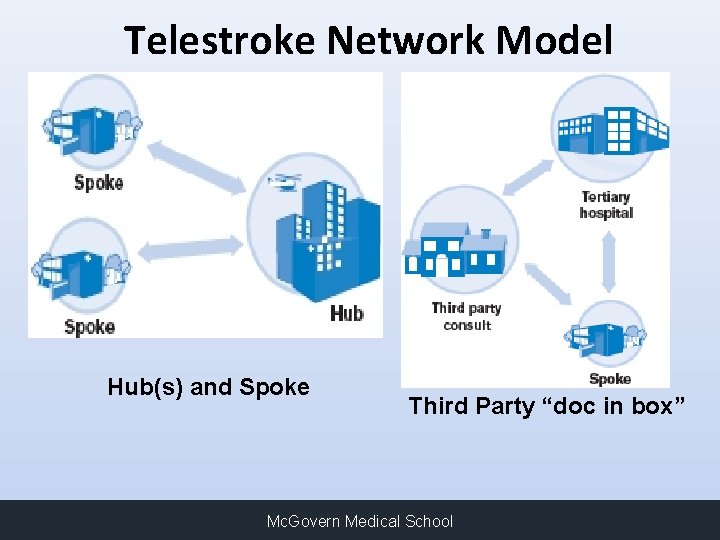
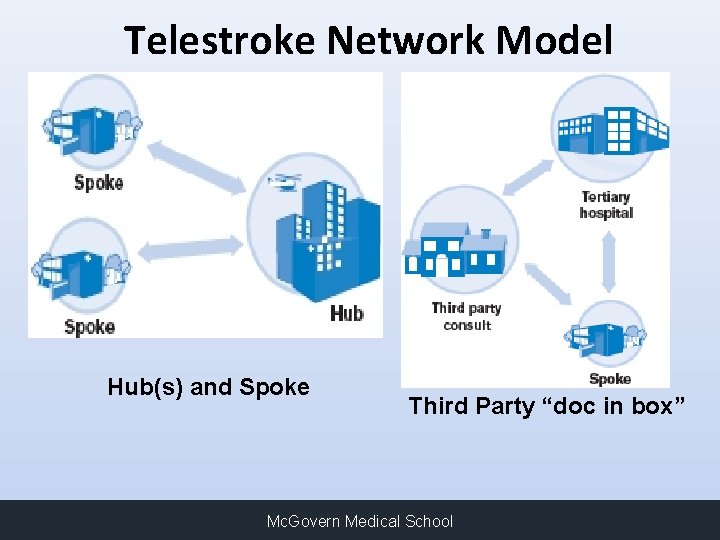
Telestroke Network Model Hub(s) and Spoke Third Party “doc in box” Mc. Govern Medical School
Telestroke Coverage Model • Provide stroke coverage in remote hospitals that lack neurology presence • More difficult to attract neurologist to smaller markets, even more difficult for vascular trained neurologist • Hard to maintain call schedule with only a few neurologist • Provide adjunctive coverage in remote hospitals with local neurology practices/hospitalists • Enhances call schedule • Offers flexibility • Maintain outpatient practice Mc. Govern Medical School
UT Teleneurology Program Overview • • • Program Goals Improve overall neurological care in the region Solidify relationships with existing referral hospitals, increase access to Memorial Hermann System (4 -Comprehensive Stroke Centers) Avoid unnecessary transfers and encourage hospitals to keep patients who do not need a higher level of care in their own community Educate surrounding hospitals and facilitate the transfer of patients who do need a higher level of care (i. e. Neurosurgery, endovascular or participation in research protocols otherwise not available to patients in the community) Benefits patient, family and community hospitals Mc. Govern Medical School
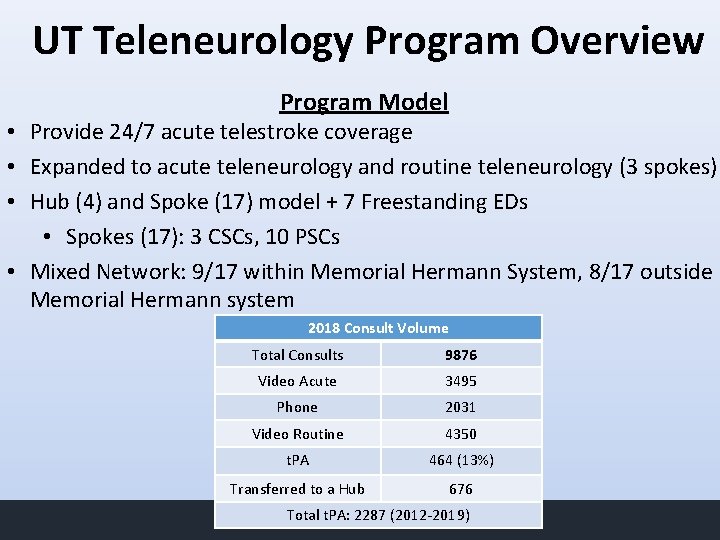
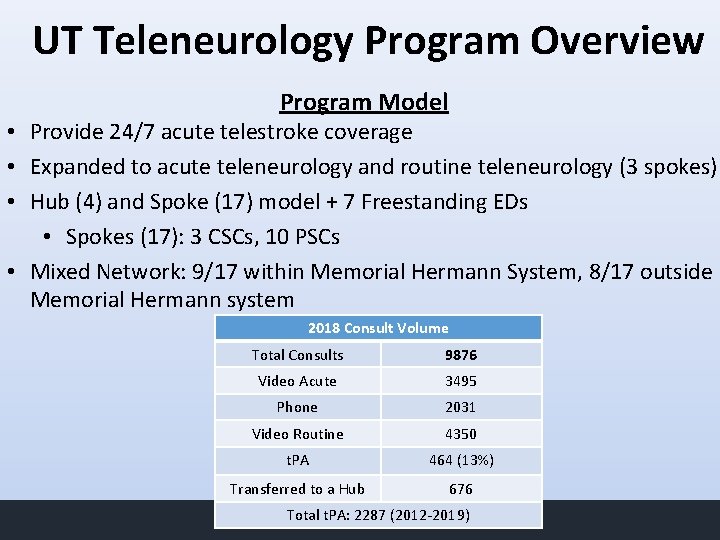
UT Teleneurology Program Overview Program Model • Provide 24/7 acute telestroke coverage • Expanded to acute teleneurology and routine teleneurology (3 spokes) • Hub (4) and Spoke (17) model + 7 Freestanding EDs • Spokes (17): 3 CSCs, 10 PSCs • Mixed Network: 9/17 within Memorial Hermann System, 8/17 outside Memorial Hermann system 2018 Consult Volume Total Consults 9876 Video Acute 3495 Phone 2031 Video Routine 4350 t. PA 464 (13%) Transferred to a Hub 676 Total t. PA: Medical 2287 (2012 -2019) Mc. Govern School
Role of Teleneurology • To provide acute neurological consultative services 24/7 (Emergency room or in-hospital) to supplement current neurological coverage • Flexible coverage: 24/7 vs after hours and weekends only etc. • Examples: Potential IV-t. PA/IAT candidates, cerebral hemorrhage, status epilepticus, etc • Expedite transfers to CSC hubs if needed with preacceptance • To provide routine/non-urgent consultations and follow ups, 7 days a week 8 am to 5 pm where contracted Mc. Govern Medical School
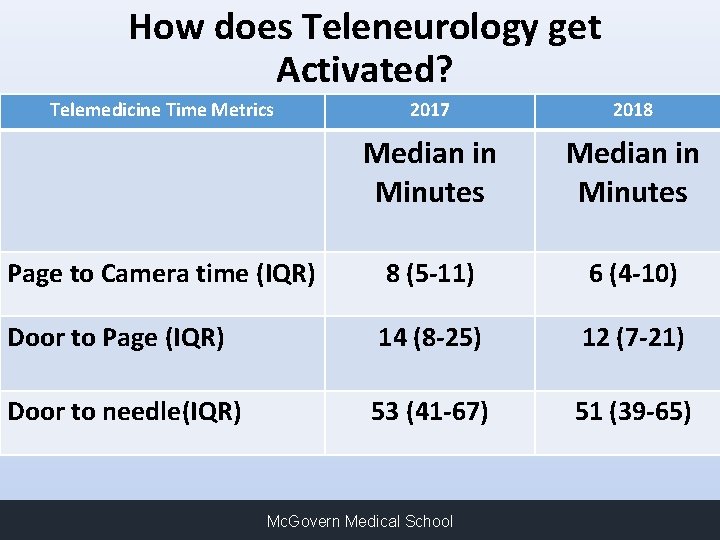
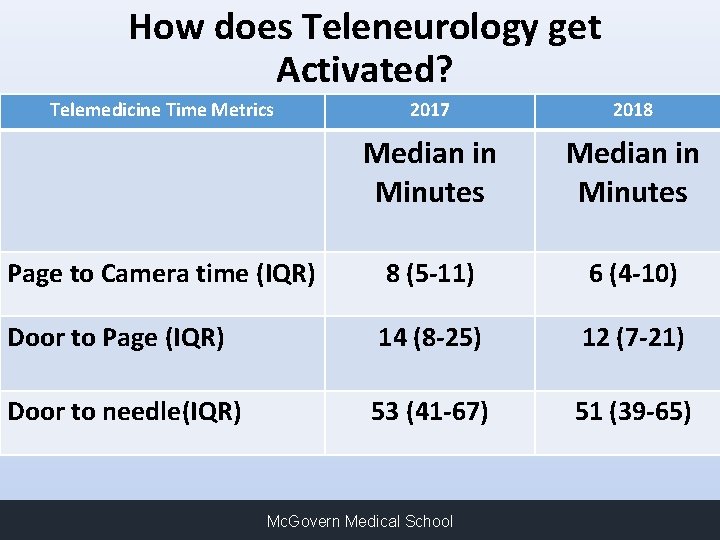
How does Teleneurology get Activated? Time Metrics patient identified 2017 2018 • Telemedicine Acute neurological • Page UT Teleneurology Team thru call Median in center. Median in • Teleneurology protocol activated Minutes • TM physician to be on camera if necessary within 10 of page Page minutes to Camera time (IQR) 8 (5 -11) 6 (4 -10) • Evaluate Patient with bedside nurse Door to Page (IQR) 14 (8 -25) 12 (7 -21) • Give recommendations • Arrange for transfer if needed Door to needle(IQR) 53 (41 -67) 51 (39 -65) Mc. Govern Medical School
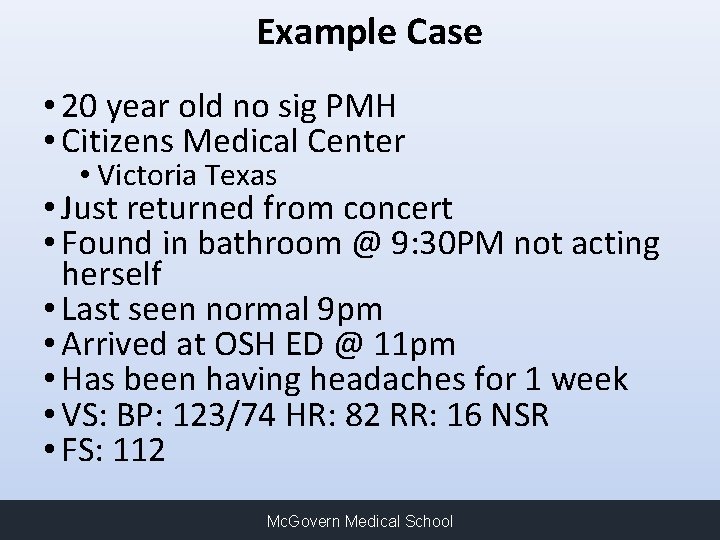
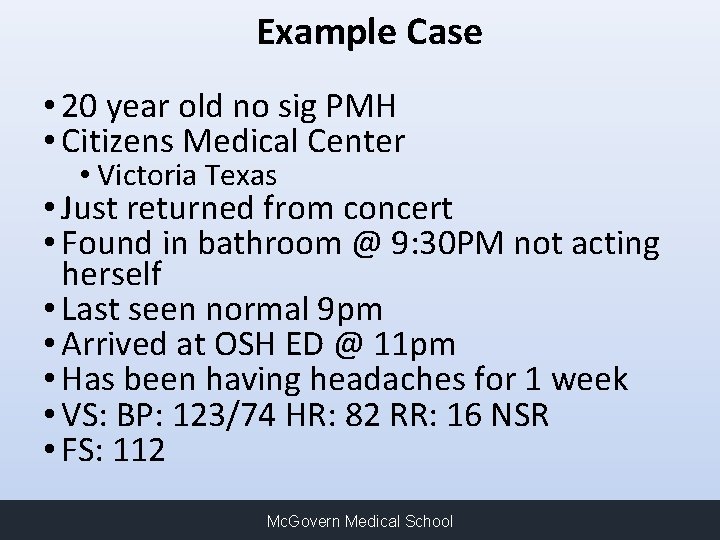
Example Case • 20 year old no sig PMH • Citizens Medical Center • Victoria Texas • Just returned from concert • Found in bathroom @ 9: 30 PM not acting herself • Last seen normal 9 pm • Arrived at OSH ED @ 11 pm • Has been having headaches for 1 week • VS: BP: 123/74 HR: 82 RR: 16 NSR • FS: 112 Mc. Govern Medical School
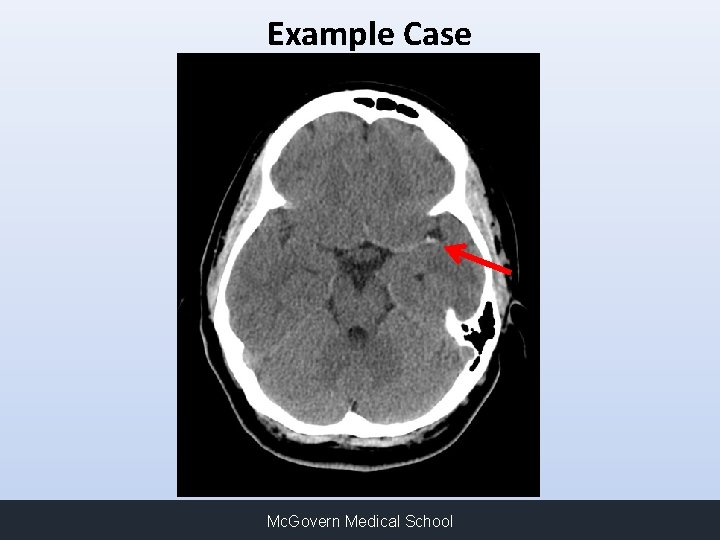
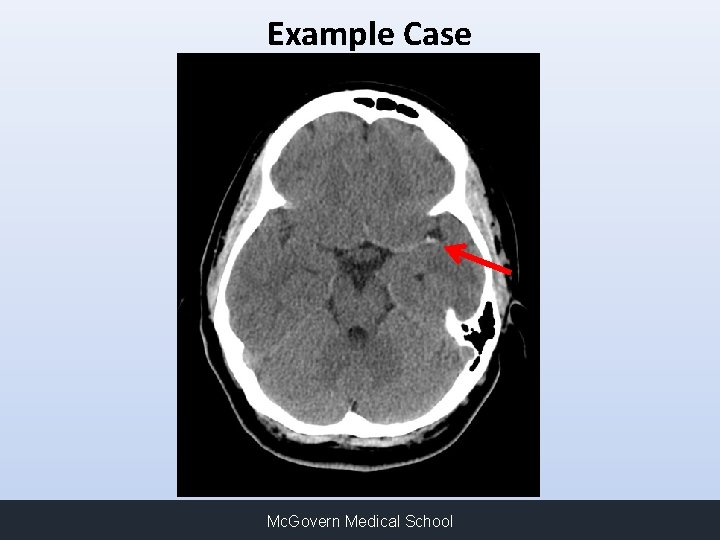
Example Case Mc. Govern Medical School
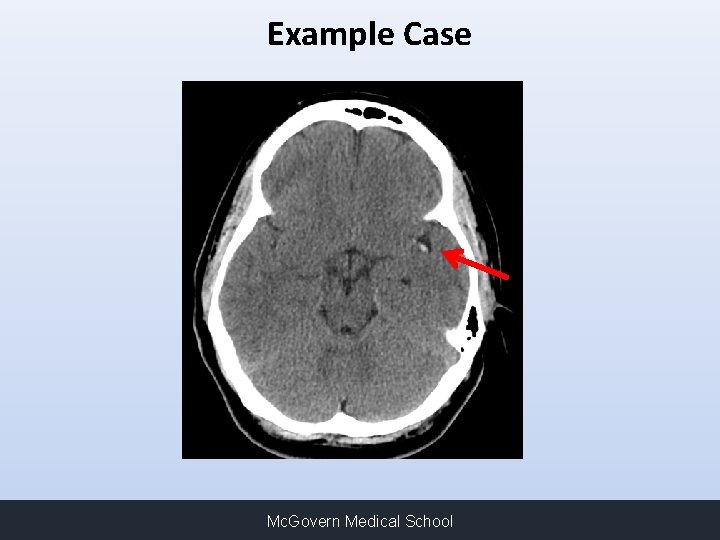
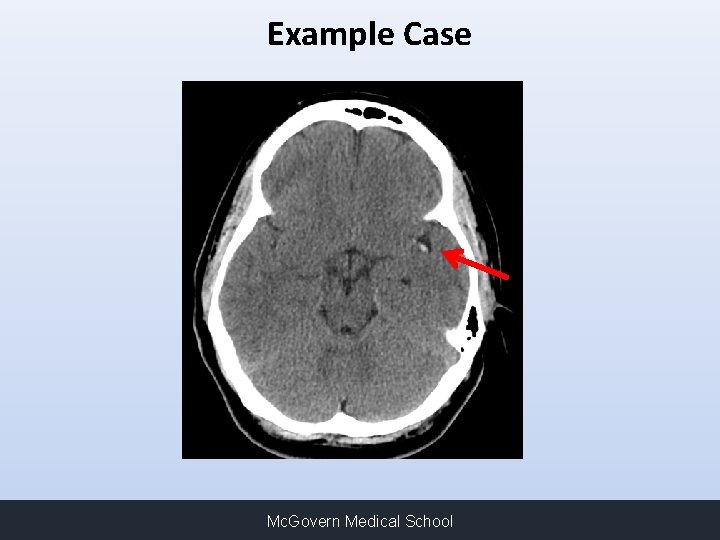
Example Case Mc. Govern Medical School
Example Case • NIHSS = 13 • Expressive aphasia, right FD, Right sided hemiparesis and sensory loss • Arrival to ED @ 11: 00 PM • Paged TM @ 11: 19 PM • On Cam @ 11: 29 PM • TPA Bolus @ 11: 35 PM • Time from page to TPA = 16 minutes Mc. Govern Medical School
Example Case • Arranged for Transfer to MHH-TMC for possible intra-arterial therapy • Angio showed no proximal occlusion • NIHSS @ 24 hrs = 2 for mild dysarthria and sensory loss • NIHSS @ discharge 1 for sensory changes Mc. Govern Medical School
Follow up • Negative hypercoaguable work up • TTE + right to left shunt, likely PFO • TEE + interatrial septal aneurysm small fenestrated spontaneous shunting • Lower ext dopplers: negative for DVT • MRV Pelvis: no DVT, severe compression of left common iliac vein by right common iliac artery, with increased left sided deep pelvis venous collateralization, may be associated with increase risk of development of DVT • She under went closure of ASD with amplatz device Mc. Govern Medical School
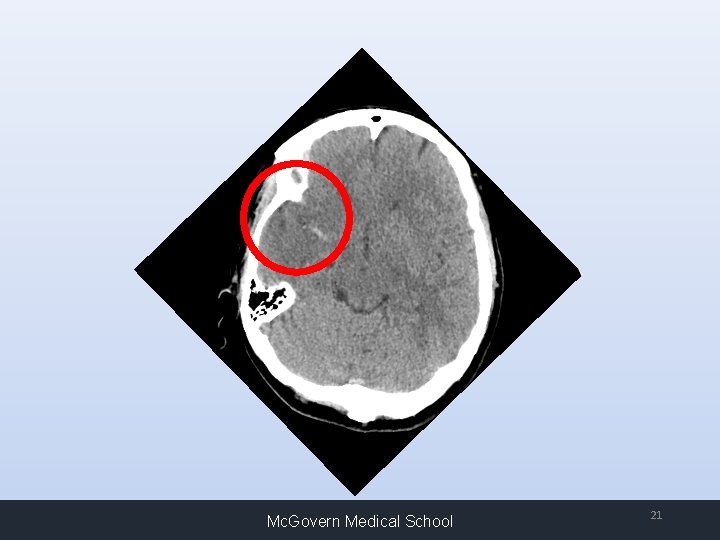
Example Case • 43 year old no sig PMH • On antibiotics for facial infection • Found @ 7: 30 PM on the floor of kitchen by daughter “acting strange”, last seen normal at 7 pm. • Exam: • • • Right gaze deviation Left neglect Left sided plegia and Left facial droop Severe dysarthria NIHSS = 18 Mc. Govern Medical School
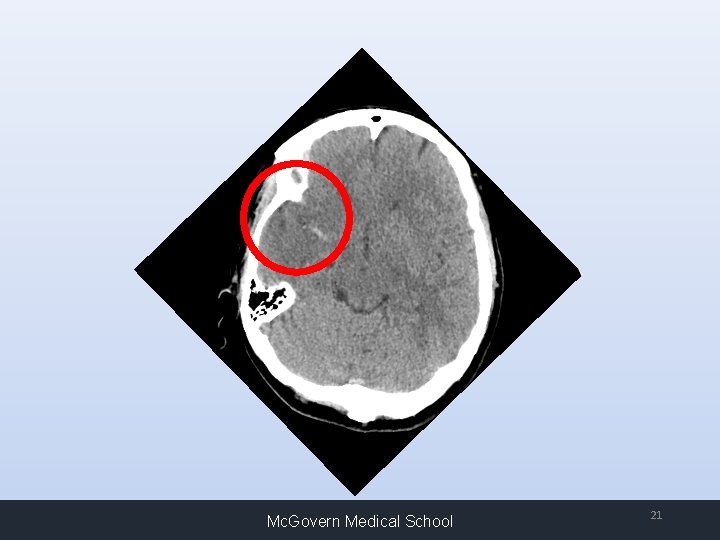
Mc. Govern Medical School 21
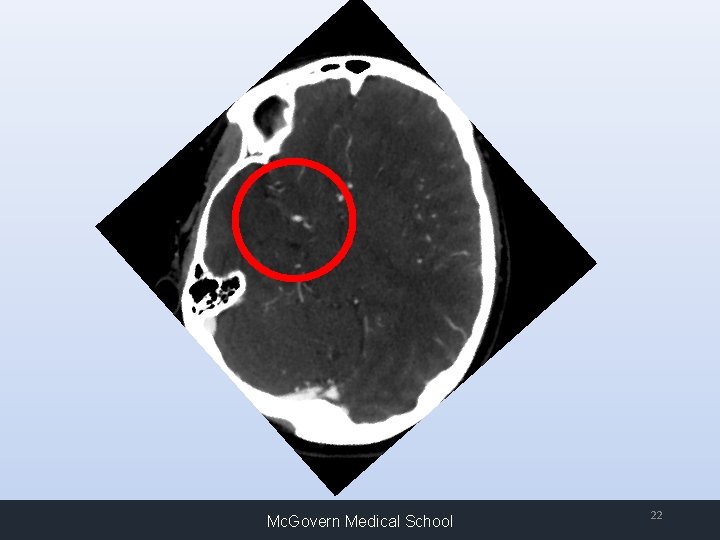
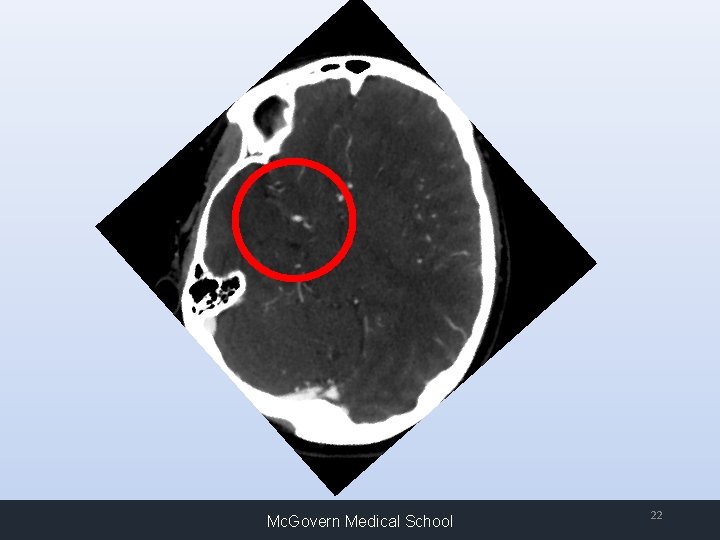
Mc. Govern Medical School 22
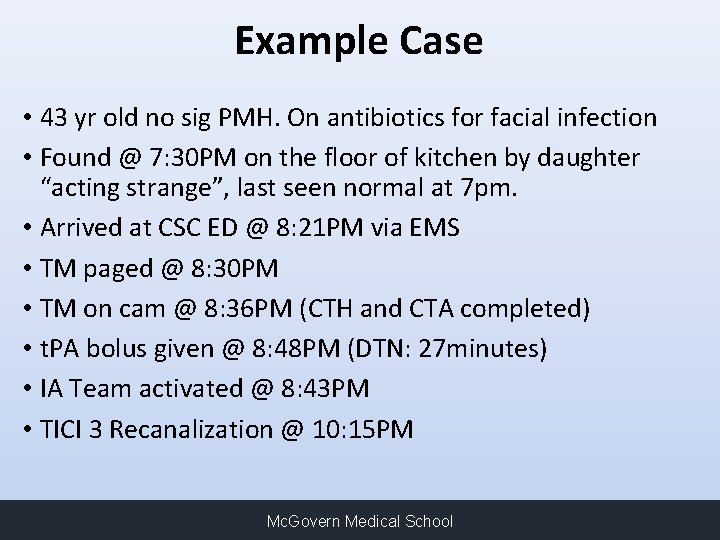
Example Case • 43 yr old no sig PMH. On antibiotics for facial infection • Found @ 7: 30 PM on the floor of kitchen by daughter “acting strange”, last seen normal at 7 pm. • Arrived at CSC ED @ 8: 21 PM via EMS • TM paged @ 8: 30 PM • TM on cam @ 8: 36 PM (CTH and CTA completed) • t. PA bolus given @ 8: 48 PM (DTN: 27 minutes) • IA Team activated @ 8: 43 PM • TICI 3 Recanalization @ 10: 15 PM Mc. Govern Medical School
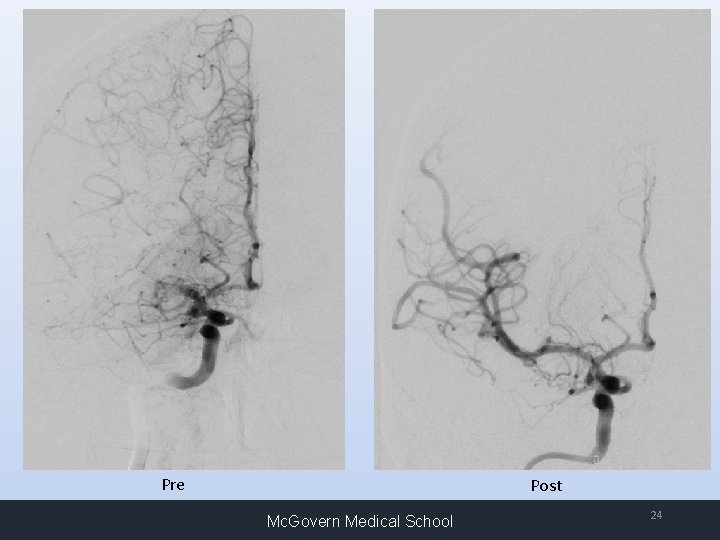
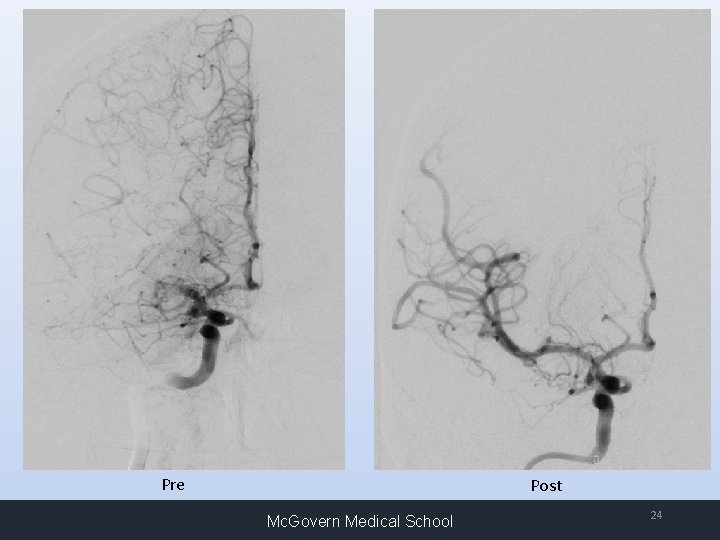
Pre Post Mc. Govern Medical School 24
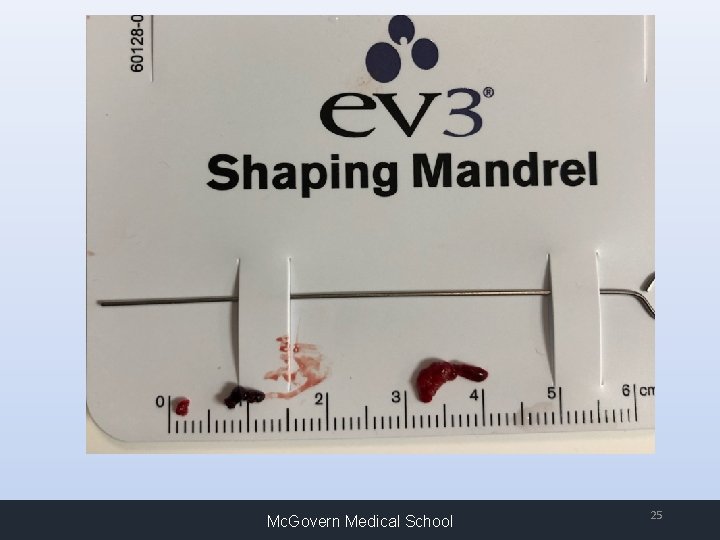
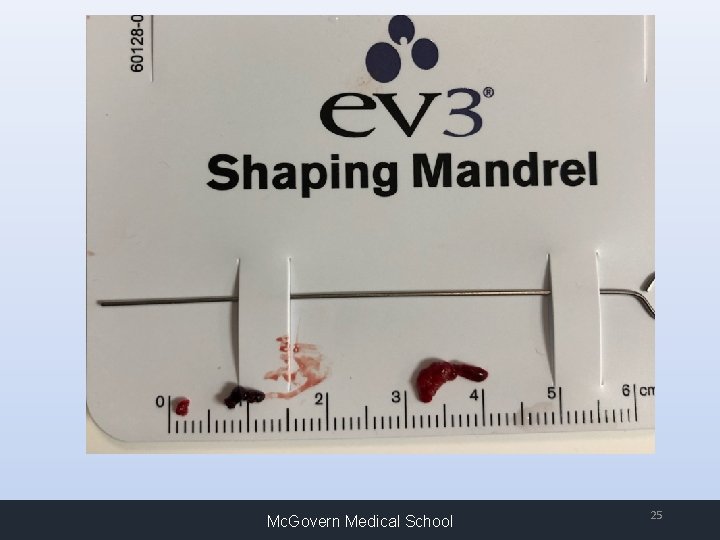
Mc. Govern Medical School 25
Mc. Govern Medical School 26
Example Case: Outcome and Work up • NIHSS = 0 next day • TEE with PFO/ASA • No DVT; Hypercoagulable labs all unremarkable • PFO closed prior to Discharge home • LOS 5 days Mc. Govern Medical School
Benefits of Telestroke • Accurate decision making • Increase use of IV t-PA • Reduce unnecessary transfers • Comparable outcomes • Financial benefits • Research opportunities Mc. Govern Medical School
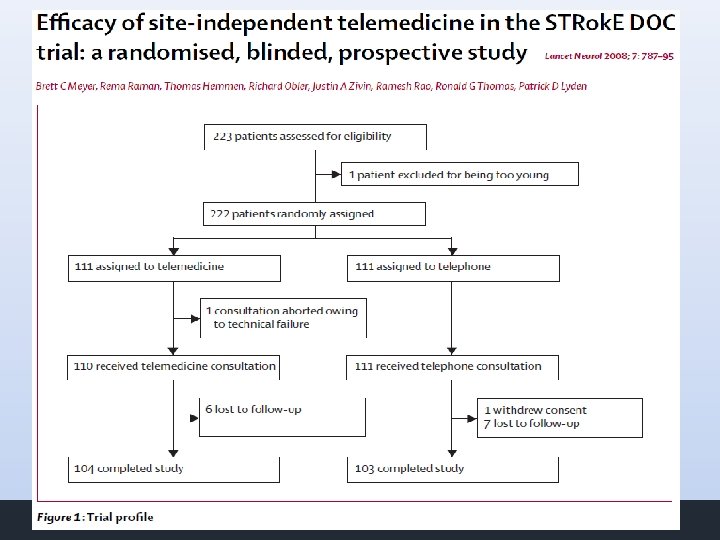
• Assess whether telemedicine consultation is superior to telephonic consultation for acute stroke treatment. • Primary outcome: Decision of thrombolytic treatment • Secondary outcome: s. ICH, m. RS Mc. Govern Medical School
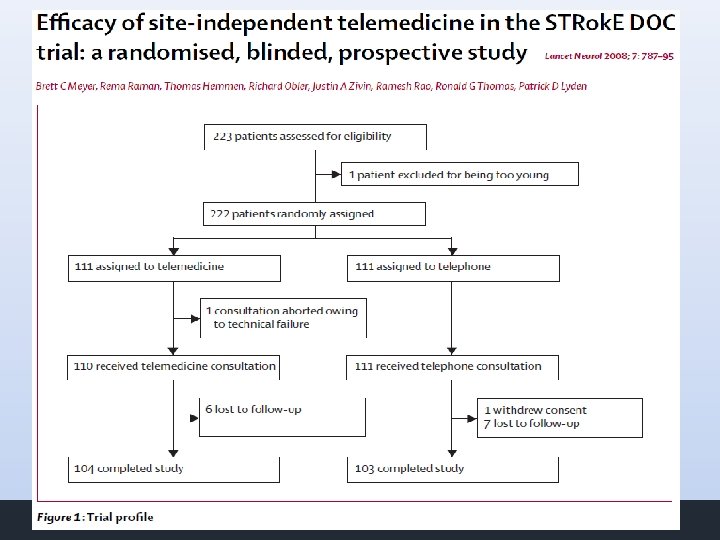
Mc. Govern Medical School
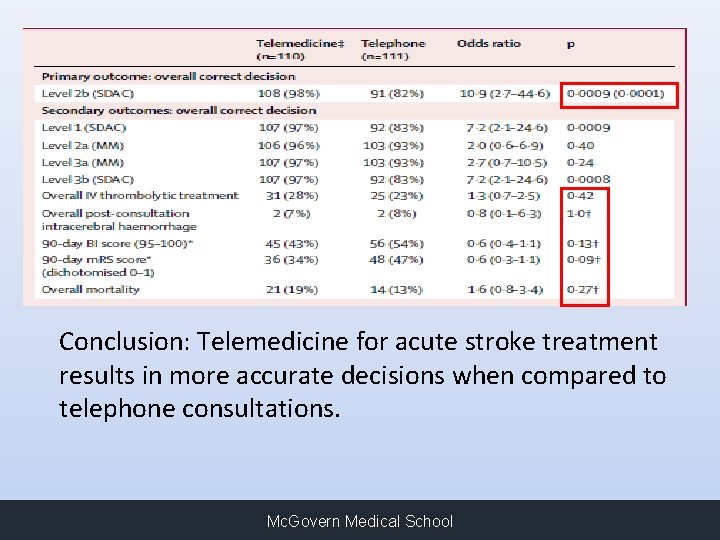
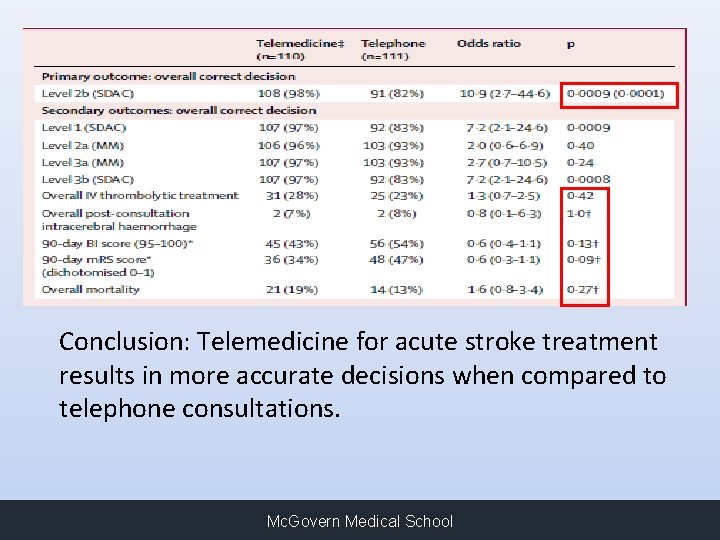
Conclusion: Telemedicine for acute stroke treatment results in more accurate decisions when compared to telephone consultations. Mc. Govern Medical School
Benefits of Telestroke • Accurate decision making • Increase use of IV t-PA • Reduce unnecessary transfers • Comparable outcomes • Financial benefits • Research opportunities Mc. Govern Medical School
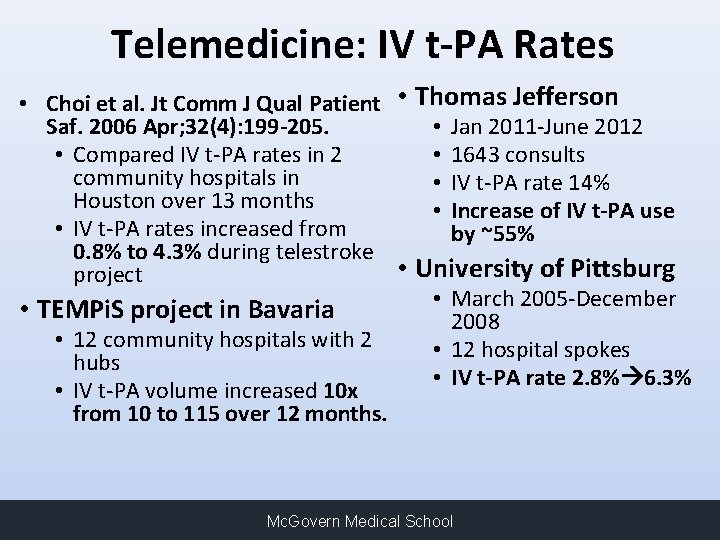
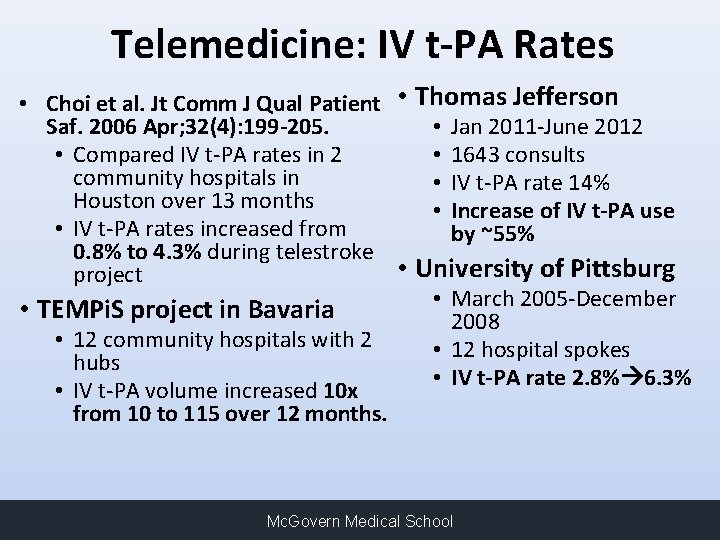
Telemedicine: IV t-PA Rates • Choi et al. Jt Comm J Qual Patient • Thomas Jefferson • Jan 2011 -June 2012 Saf. 2006 Apr; 32(4): 199 -205. • 1643 consults • Compared IV t-PA rates in 2 community hospitals in • IV t-PA rate 14% Houston over 13 months • Increase of IV t-PA use • IV t-PA rates increased from by ~55% 0. 8% to 4. 3% during telestroke • University of Pittsburg project • March 2005 -December • TEMPi. S project in Bavaria 2008 • 12 community hospitals with 2 • 12 hospital spokes hubs • IV t-PA rate 2. 8% 6. 3% • IV t-PA volume increased 10 x from 10 to 115 over 12 months. Mc. Govern Medical School
Benefits of Telestroke • Accurate decision making • Increase use of IV t-PA • Reduce unnecessary transfers • Comparable outcomes • Financial benefits • Research opportunities Mc. Govern Medical School
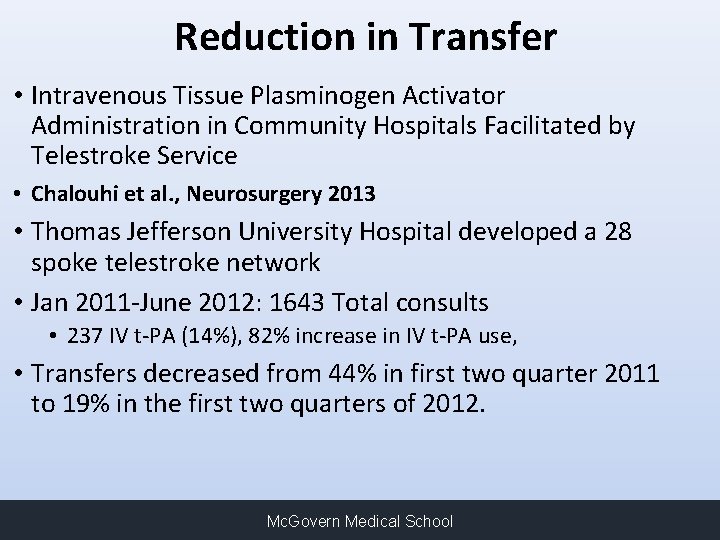
Reduction in Transfer • Intravenous Tissue Plasminogen Activator Administration in Community Hospitals Facilitated by Telestroke Service • Chalouhi et al. , Neurosurgery 2013 • Thomas Jefferson University Hospital developed a 28 spoke telestroke network • Jan 2011 -June 2012: 1643 Total consults • 237 IV t-PA (14%), 82% increase in IV t-PA use, • Transfers decreased from 44% in first two quarter 2011 to 19% in the first two quarters of 2012. Mc. Govern Medical School
Benefits of Telestroke • Accurate decision making • Increase use of IV t-PA • Reduce unnecessary transfers • Comparable outcomes • Financial benefits • Research opportunities Mc. Govern Medical School
• Compared outcomes for Drip and Ship vs Drip and Stay • 9/2015 to 12/2016: Total of 430 t. PA-treated • 232 Drip and Ship (NIHSS = 10) • 192 Drip and Stay (NIHSS = 6) • No difference in LOS, hospital mortality, discharge disposition, 90 day m. RS Mc. Govern Medical School 37
• Stroke outcomes worse when presenting overnight or weekends • We compared outcomes and metrics in our TM network • 9/15 to 12/16: Total 424 patients that received t. PA • 268 after hours and 156 on-hours • Results: no difference in t. PA administration times, complications, and 90 day outcomes • Access to stroke specialist 24/7 via TM can ensure dependable and timely clinical care regardless of time of day or week Mc. Govern Medical School 38
Benefits of Telestroke • Accurate decision making • Increase use of IV t-PA • Reduce unnecessary transfers • Comparable outcomes • Financial benefits • Research opportunities Mc. Govern Medical School
Financial Perspective • Hubs: increase in procedures, complex hospital admissions • Spokes: increase in reimbursement for t. PA patients that stay at spoke; downstream revenue • Healthcare system: reduction in unnecessary transfers • Patients and Families: reduce unnecessary transfers (driving, parking, accommodations) • Tele. Stroke Network: Financial stability Mc. Govern Medical School 40
Reimbursement Model • Fee-for-service models prevail for metropolitan service areas • Hospitals will pay professional fees for telemedicine coverage • Flat fee per month • “Per Click” • The professional fee model allows for “on the ground” physicians to still bill for services • Telemedicine physician does not bill patient* • Neurologists can focus on their out-patient practice • Alleviates burdensome call Mc. Govern Medical School
Benefits of Telestroke • Accurate decision making • Increase use of IV t-PA • Reduce unnecessary transfers • Comparable outcomes • Financial benefits • Research opportunities Mc. Govern Medical School
Telemedicine and Clinical Trials • Clinical trials completion advances in stroke treatment • Recruitment is inefficient • Barriers • Access to tertiary centers • Transfer delays • Time sensitive • Patients in rural areas excluded Mc. Govern Medical School
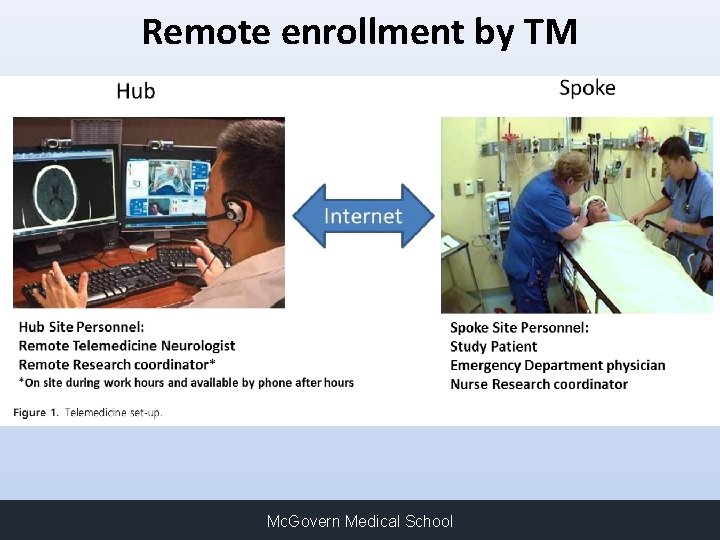
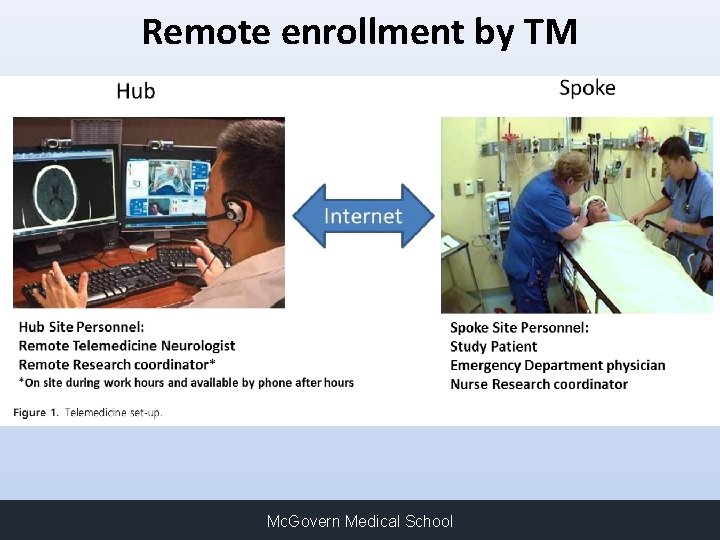
Remote enrollment by TM Mc. Govern Medical School
Results • Between May 2013 and July 2014, 65 patients screened at the two spokes • 10 identified via TM as eligible • 1 case, insufficient time (<5 mins) for consent • Delay in study team notification • 6 of the remaining 9 (56%) agreed to participate Mc. Govern Medical School
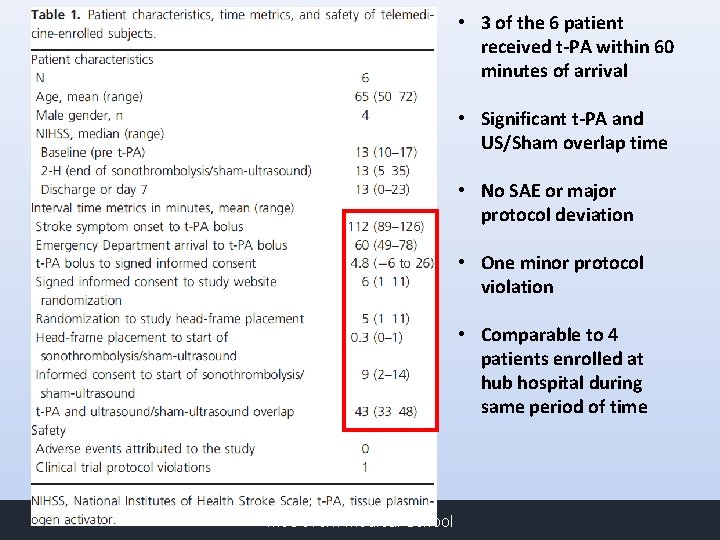
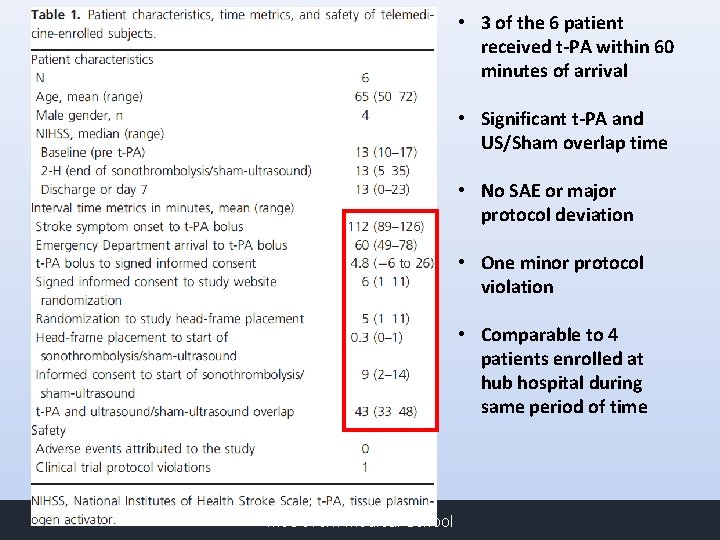
• 3 of the 6 patient received t-PA within 60 minutes of arrival • Significant t-PA and US/Sham overlap time • No SAE or major protocol deviation • One minor protocol violation • Comparable to 4 patients enrolled at hub hospital during same period of time Mc. Govern Medical School
Barriers to Telemedicine • Technology is no longer a barrier to telemedicine – Widely available broadband internet – Reduced cost of equipment • I-Phones, IPADS, Laptops, carts • Facetime/ Skype/ Other video conferencing platforms • Competition – Healthcare market is competitive – For-Profit national providers • Financial Costs – Equipment – Physician coverage – Other resources • Credentialing – Can delay start-up by months • Buy-in by local practitioners – Emergency room physicians and nurses – Hospitalists – Neurologists Mc. Govern Medical School
Keys To Success Mc. Govern Medical School 53
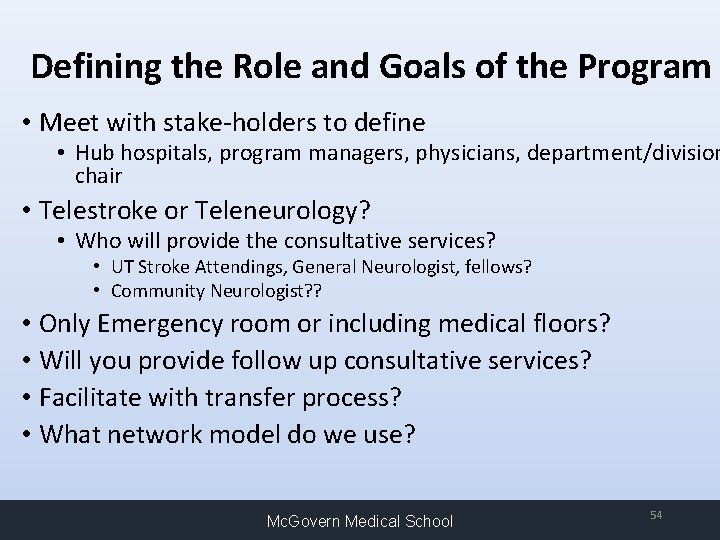
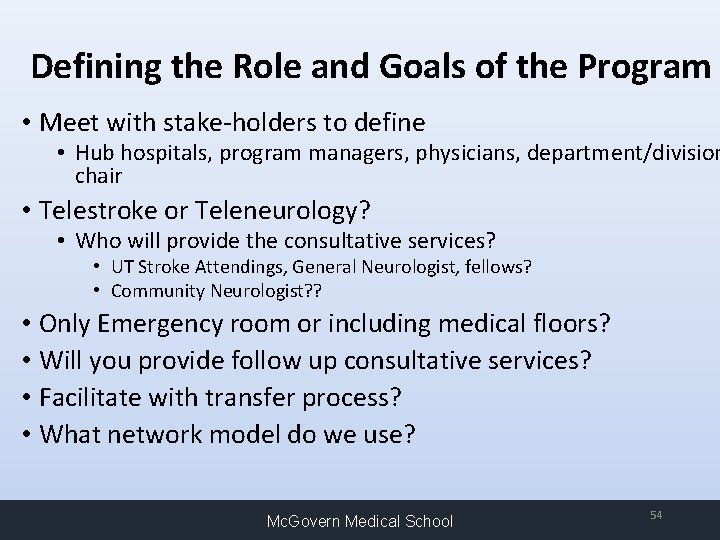
Defining the Role and Goals of the Program • Meet with stake-holders to define • Hub hospitals, program managers, physicians, department/division chair • Telestroke or Teleneurology? • Who will provide the consultative services? • UT Stroke Attendings, General Neurologist, fellows? • Community Neurologist? ? • Only Emergency room or including medical floors? • Will you provide follow up consultative services? • Facilitate with transfer process? • What network model do we use? Mc. Govern Medical School 54
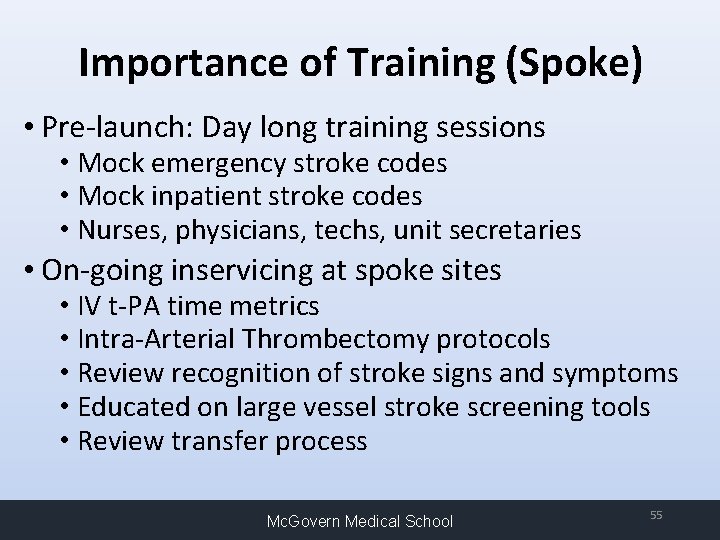
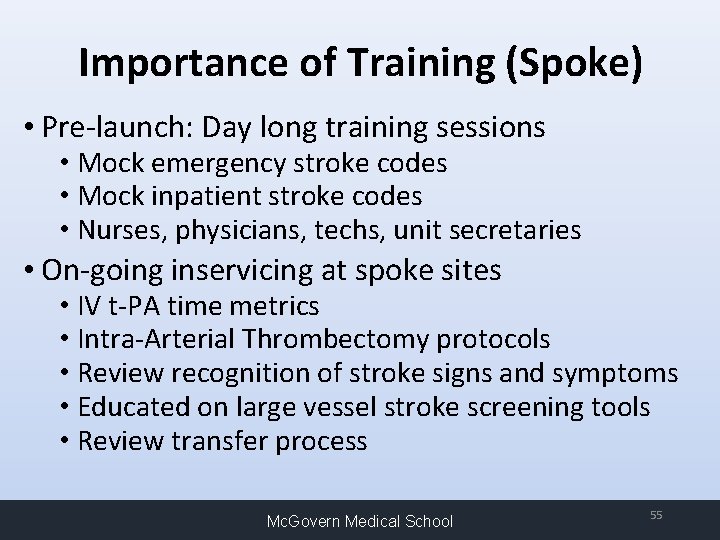
Importance of Training (Spoke) • Pre-launch: Day long training sessions • Mock emergency stroke codes • Mock inpatient stroke codes • Nurses, physicians, techs, unit secretaries • On-going inservicing at spoke sites • IV t-PA time metrics • Intra-Arterial Thrombectomy protocols • Review recognition of stroke signs and symptoms • Educated on large vessel stroke screening tools • Review transfer process Mc. Govern Medical School 55
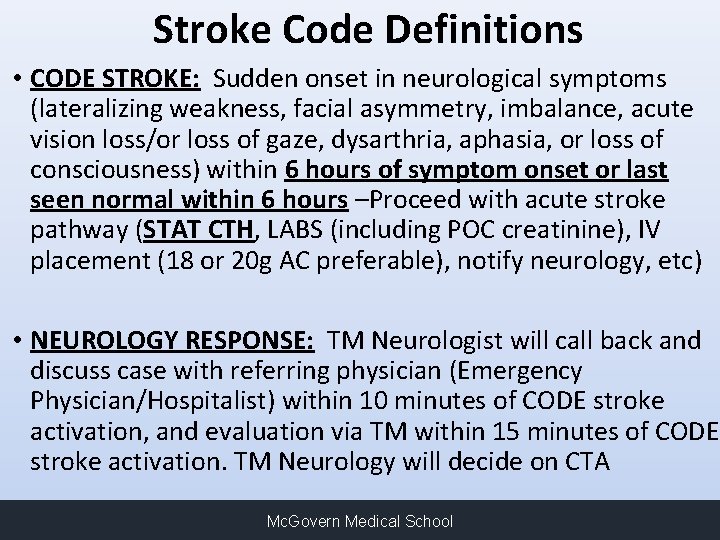
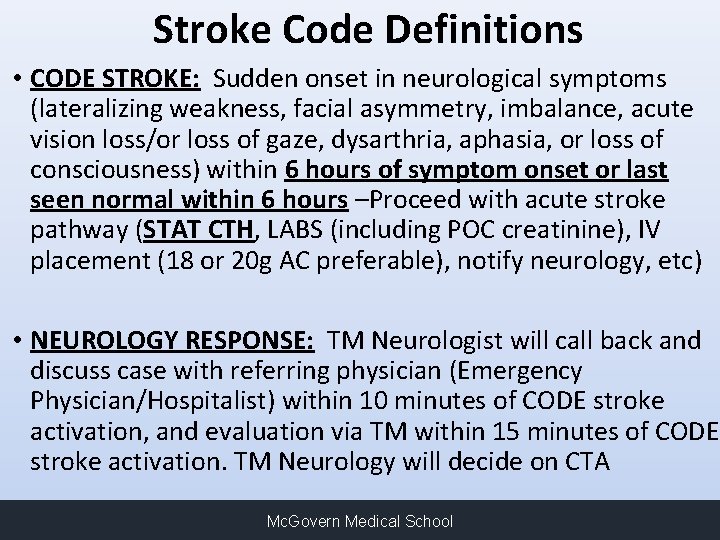
Stroke Code Definitions • CODE STROKE: Sudden onset in neurological symptoms (lateralizing weakness, facial asymmetry, imbalance, acute vision loss/or loss of gaze, dysarthria, aphasia, or loss of consciousness) within 6 hours of symptom onset or last seen normal within 6 hours –Proceed with acute stroke pathway (STAT CTH, LABS (including POC creatinine), IV placement (18 or 20 g AC preferable), notify neurology, etc) • NEUROLOGY RESPONSE: TM Neurologist will call back and discuss case with referring physician (Emergency Physician/Hospitalist) within 10 minutes of CODE stroke activation, and evaluation via TM within 15 minutes of CODE stroke activation. TM Neurology will decide on CTA Mc. Govern Medical School
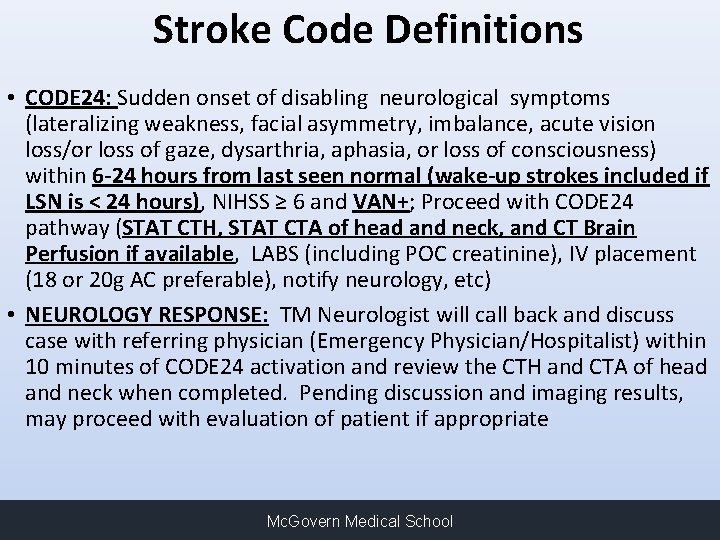
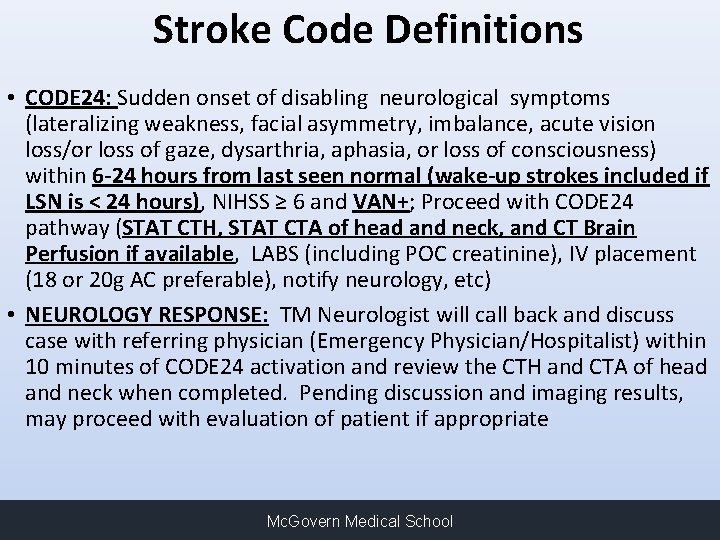
Stroke Code Definitions • CODE 24: Sudden onset of disabling neurological symptoms (lateralizing weakness, facial asymmetry, imbalance, acute vision loss/or loss of gaze, dysarthria, aphasia, or loss of consciousness) within 6 -24 hours from last seen normal (wake-up strokes included if LSN is < 24 hours), NIHSS ≥ 6 and VAN+; Proceed with CODE 24 pathway (STAT CTH, STAT CTA of head and neck, and CT Brain Perfusion if available, LABS (including POC creatinine), IV placement (18 or 20 g AC preferable), notify neurology, etc) • NEUROLOGY RESPONSE: TM Neurologist will call back and discuss case with referring physician (Emergency Physician/Hospitalist) within 10 minutes of CODE 24 activation and review the CTH and CTA of head and neck when completed. Pending discussion and imaging results, may proceed with evaluation of patient if appropriate Mc. Govern Medical School
Urgent Neurology Code Definitions • URGENT NEUROLOGY CONSULT: Other acute neurological issues such as unresolved seizures, unexplained stupor/coma, unstable hemorrhagic or ischemic stroke patients outside of t. PA window or with clear contraindications etc. • NEUROLOGY RESPONSE: TM Neurologist will call back and discuss case with referring physician (Emergency Physician/Hospitalist) within 10 minutes of urgent neurology code activation. TM Evaluation to be provided as needed at neurologist’s discretion • *CODESTROKE, CODE 24 and URGENT NEUROLOGY CONSULT can all be cancelled after discussion between the referring physician (Emergency physician/Hospitalist) and the Neurologist. Mc. Govern Medical School
Importance of Training (Hub) • Physician training • On boarding stroke fellows • On boarding new stroke faculty • Review EMR access, documentation, downtime protocols • Review and update site capabilities, transfer patterns and communication pathways • Call Center training • New hubs/spokes and on call physicians • Implement back up plans • Revise call triaging Mc. Govern Medical School 59
Ways to Improve/Maintain Quality and Efficiency • Build an experience and dedicated team • • 4 full time TM vascular trained neurologist Had TM experience during fellowship Experienced Program manager Smaller core team more nimble for changes • Streamline and simplify protocols and procedures • Technology • Minimize changes to work flow for on the ground personnel • Communicate back to referring physician • • Provide prompt feedback Strategic/calculated growth Re-evaluate goals of network Develop relationship with your technology vendor Mc. Govern Medical School 60
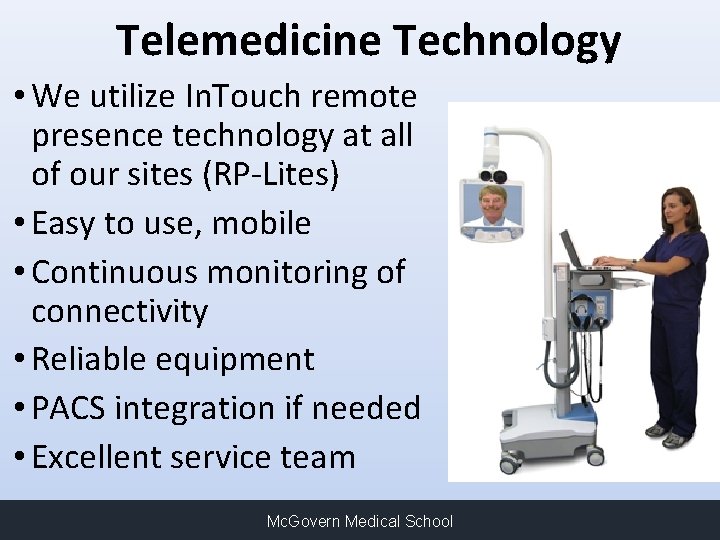
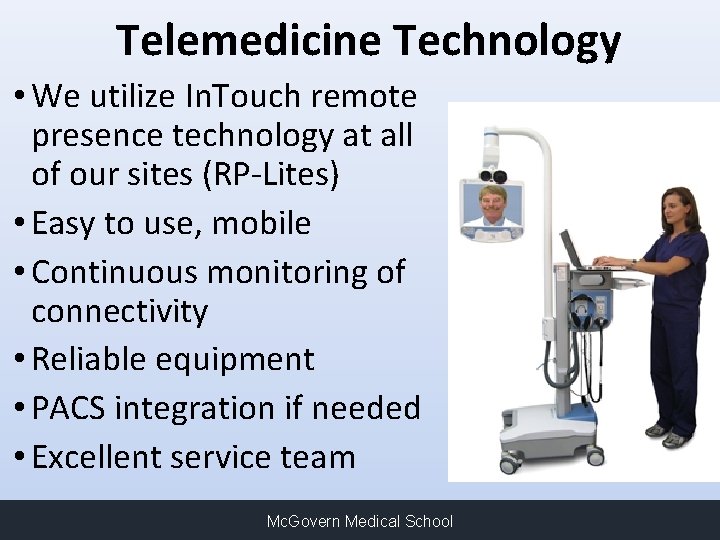
Telemedicine Technology • We utilize In. Touch remote presence technology at all of our sites (RP-Lites) • Easy to use, mobile • Continuous monitoring of connectivity • Reliable equipment • PACS integration if needed • Excellent service team Mc. Govern Medical School
Data Tracking and Quality Assurance • Provide annual consult data to all spoke sites • Review quality metrics (Door to t-PA times, transfer times, etc) annually with sites • LESTER Registry • Statewide Telemedicine stroke registry • Long-term outcomes • Provide feedback to TM providers Mc. Govern Medical School
Sharing Success • Provide feedback to the spokes • Cases when metrics are met or exceeded • Share good patient outcomes • Highlight positive interactions • EMS, Nurses, ED physicians, unit secretaries • Provide support for local stroke coordinators/staff • Participate in site surveys for stroke center certification • Spokes learning from each other Mc. Govern Medical School 63
Reimbursement • Reimbursement for telemedicine is improving: As of January 2019 Telestroke is reimbursed by Medicare • Reimbursement by Medicare/Medicaid and third-party payers are now equal to traditional care • Eligible providers: Physicians, NP/PA, nurse-midwives, CNS, clinical psychologists and social workers, registered dietitians and nutrition professionals • Encourage your company or institution to dedicate someone to educating themselves and becoming the expert on telehealth reimbursement – the landscape is changing constantly Mc. Govern Medical School 64
Future Directions for Teleneurology • Inpatient Teleneurology (now available) • Increase in demand for this service • Many spokes will transfer ALL stroke patients to our hub after telestroke consultation • Strains the hub • Accepting patients from multiple spokes/hospitals • May prohibit acceptance of patients requiring Comprehensive Stroke Center capabilities • Inconveniences patient/family • Less family support during hospitalization • Provide neurology consultative services; 7 days a week, 8 am-5 pm • Post t. PA follow up and stroke management • General Neurology consultations and follow up Mc. Govern Medical School
Future Directions for Teleneurology • Outpatient Teleneurology Follow Up visits (Spring 2020) • Epilepsy and post stroke follow ups • Lower costs (less overhead), decrease clinic noshow rates, increase compliance • Follow patients in their community • Includes other neurology subspecialities , including pediatric neurology Mc. Govern Medical School
DEMONSTRATION Mc. Govern Medical School
Conclusion • TM has transformed acute stroke care • Expanding access to stroke expertise • Safe and effective • Increase IV t-PA rates/IAT access/enhance transfer process • Improves diagnostic accuracy compared to phone • TM can be used to expand high quality care in the inpatient and outpatient setting • Ample research opportunities • Important to educate about telemedicine • Medical school and residency curriculum • Future is bright for Teleneurology Mc. Govern Medical School
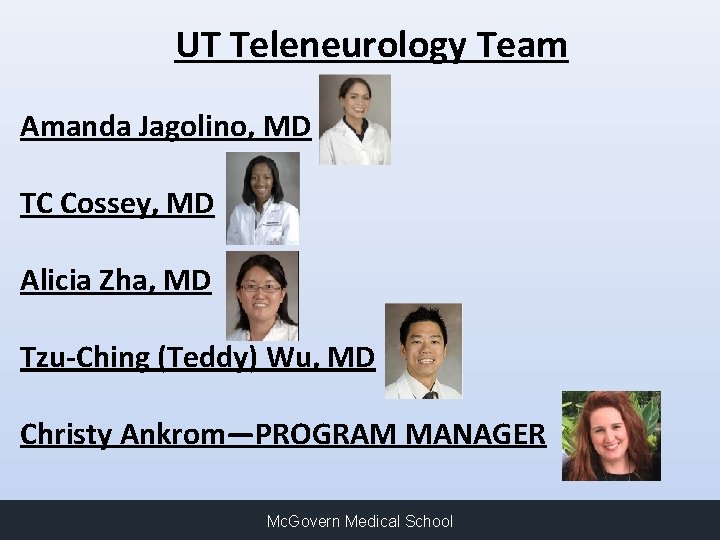
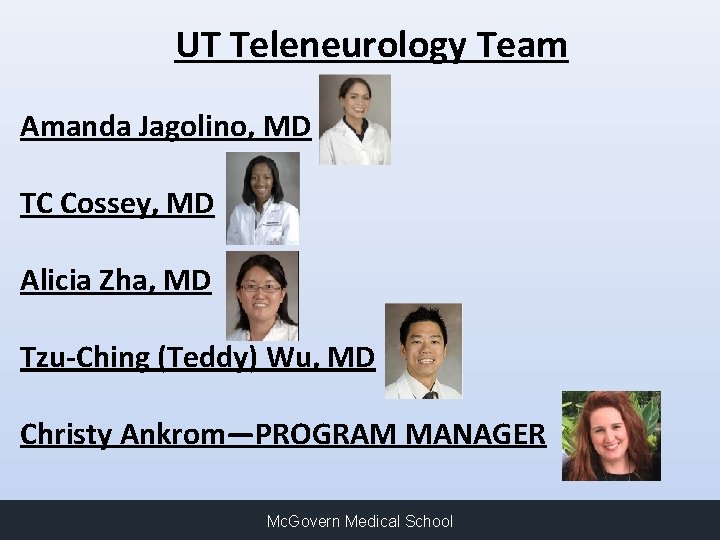
UT Teleneurology Team Amanda Jagolino, MD TC Cossey, MD Alicia Zha, MD Tzu-Ching (Teddy) Wu, MD Christy Ankrom—PROGRAM MANAGER Mc. Govern Medical School

Contact Information Christy Ankrom Teleneurology Program Manager Christy. Ankrom@uth. tmc. edu 713 -500 -7124 Tzu-Ching (Teddy) Wu Director of Teleneurology Tzu-ching. wu@uth. tmc. edu 713 -500 -7082 Mc. Govern Medical School
 Anterior stroke vs posterior stroke
Anterior stroke vs posterior stroke Telemedicine wikipedia
Telemedicine wikipedia Telehealth and telemedicine
Telehealth and telemedicine Bric telemedicine market
Bric telemedicine market Unclosed quotation mark after the character string '
Unclosed quotation mark after the character string ' Telemedicine basics
Telemedicine basics Vsee telemedicine kit
Vsee telemedicine kit Telemedicine wikipedia
Telemedicine wikipedia Medisoft telemedicine pvt ltd
Medisoft telemedicine pvt ltd Telemedicine software
Telemedicine software Hr tiered service delivery model
Hr tiered service delivery model Levels of care primary secondary tertiary quaternary
Levels of care primary secondary tertiary quaternary Stroke fast assessment
Stroke fast assessment Businesses that accenture delivery suite(ads) support
Businesses that accenture delivery suite(ads) support Customer wants open delivery means in xpressbees
Customer wants open delivery means in xpressbees Introduction to healthcare delivery systems
Introduction to healthcare delivery systems Care delivery value chain
Care delivery value chain Team nursing
Team nursing Nursing delivery models
Nursing delivery models Integrated delivery network definition
Integrated delivery network definition The objective for health service delivery is to
The objective for health service delivery is to Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Chúa yêu trần thế
Chúa yêu trần thế Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Phép trừ bù
Phép trừ bù Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Lời thề hippocrates
Lời thề hippocrates đại từ thay thế
đại từ thay thế Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Cong thức tính động năng
Cong thức tính động năng Các môn thể thao bắt đầu bằng tiếng nhảy
Các môn thể thao bắt đầu bằng tiếng nhảy Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ Phản ứng thế ankan
Phản ứng thế ankan Gấu đi như thế nào
Gấu đi như thế nào Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan điện thế nghỉ
điện thế nghỉ Một số thể thơ truyền thống
Một số thể thơ truyền thống Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Lp html
Lp html Số nguyên tố là số gì
Số nguyên tố là số gì Tia chieu sa te
Tia chieu sa te đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton Sơ đồ cơ thể người
Sơ đồ cơ thể người ưu thế lai là gì
ưu thế lai là gì Tư thế ngồi viết
Tư thế ngồi viết Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Bổ thể
Bổ thể Tư thế ngồi viết
Tư thế ngồi viết Thẻ vin
Thẻ vin Thứ tự các dấu thăng giáng ở hóa biểu
Thứ tự các dấu thăng giáng ở hóa biểu Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Standard 9 care certificate answers
Standard 9 care certificate answers Palliative care versus hospice care
Palliative care versus hospice care Hip fracture care clinical care standard
Hip fracture care clinical care standard