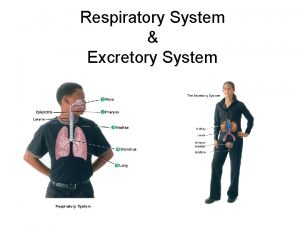
Respiratory System Dr Spandana Charles The Respiratory System
- Slides: 47
Respiratory System Dr. Spandana Charles
The Respiratory System • Major function-respiration – Supply body with O 2 for cellular respiration; dispose of CO 2, a waste product of cellular respiration • Also helps in – Olfaction – Speech © 2013 Pearson Education, Inc.
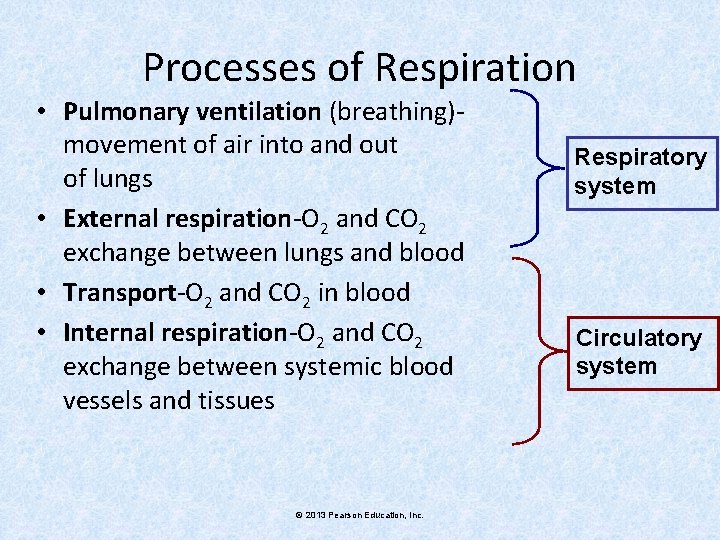
Processes of Respiration • Pulmonary ventilation (breathing)movement of air into and out of lungs • External respiration-O 2 and CO 2 exchange between lungs and blood • Transport-O 2 and CO 2 in blood • Internal respiration-O 2 and CO 2 exchange between systemic blood vessels and tissues © 2013 Pearson Education, Inc. Respiratory system Circulatory system
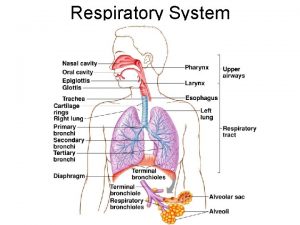
Respiratory System: Functional Anatomy • Major organs – Nose, nasal cavity, and paranasal sinuses – Pharynx – Larynx – Trachea – Bronchi and their branches – Lungs and alveoli © 2013 Pearson Education, Inc.
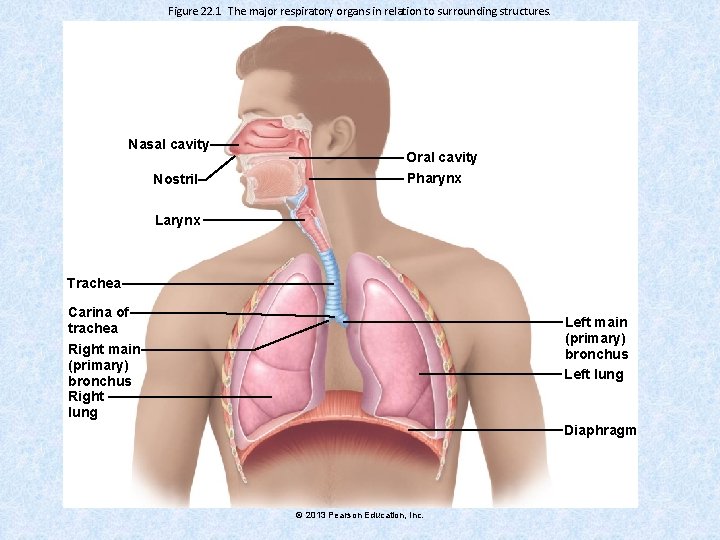
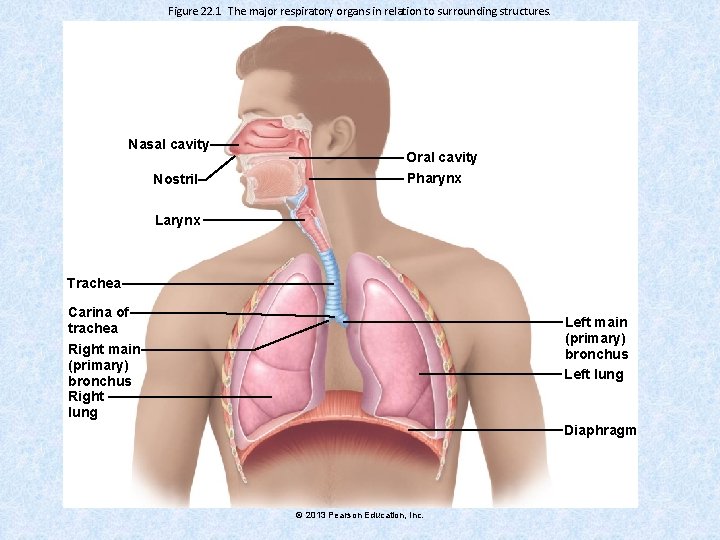
Figure 22. 1 The major respiratory organs in relation to surrounding structures. Nasal cavity Nostril Oral cavity Pharynx Larynx Trachea Carina of trachea Left main (primary) bronchus Left lung Right main (primary) bronchus Right lung Diaphragm © 2013 Pearson Education, Inc.
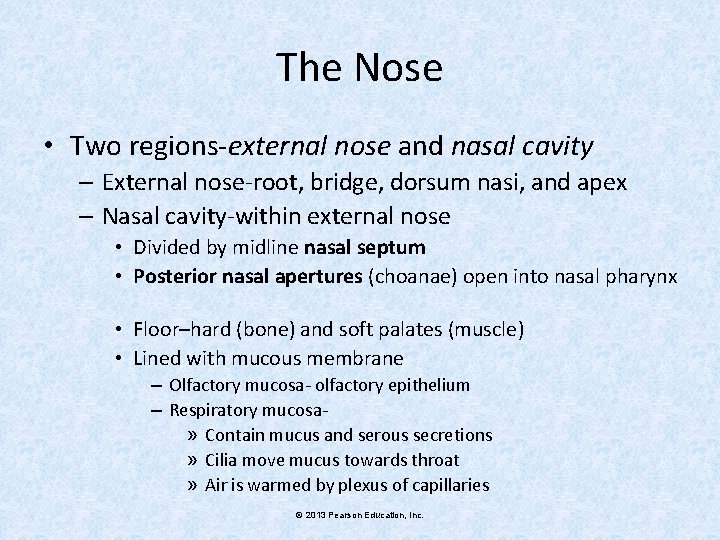
The Nose • Two regions-external nose and nasal cavity – External nose-root, bridge, dorsum nasi, and apex – Nasal cavity-within external nose • Divided by midline nasal septum • Posterior nasal apertures (choanae) open into nasal pharynx • Floor–hard (bone) and soft palates (muscle) • Lined with mucous membrane – Olfactory mucosa- olfactory epithelium – Respiratory mucosa» Contain mucus and serous secretions » Cilia move mucus towards throat » Air is warmed by plexus of capillaries © 2013 Pearson Education, Inc.
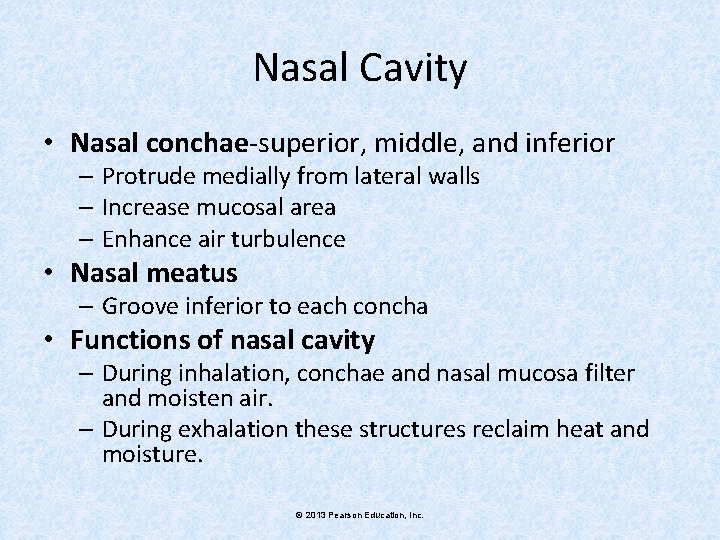
Nasal Cavity • Nasal conchae-superior, middle, and inferior – Protrude medially from lateral walls – Increase mucosal area – Enhance air turbulence • Nasal meatus – Groove inferior to each concha • Functions of nasal cavity – During inhalation, conchae and nasal mucosa filter and moisten air. – During exhalation these structures reclaim heat and moisture. © 2013 Pearson Education, Inc.
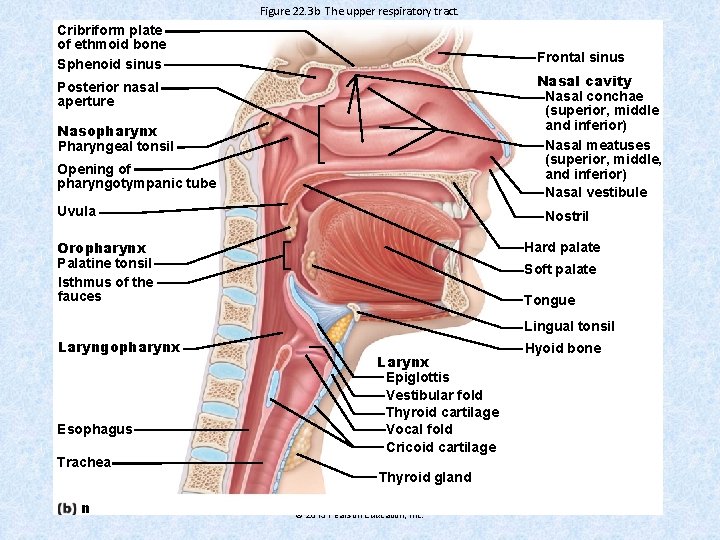
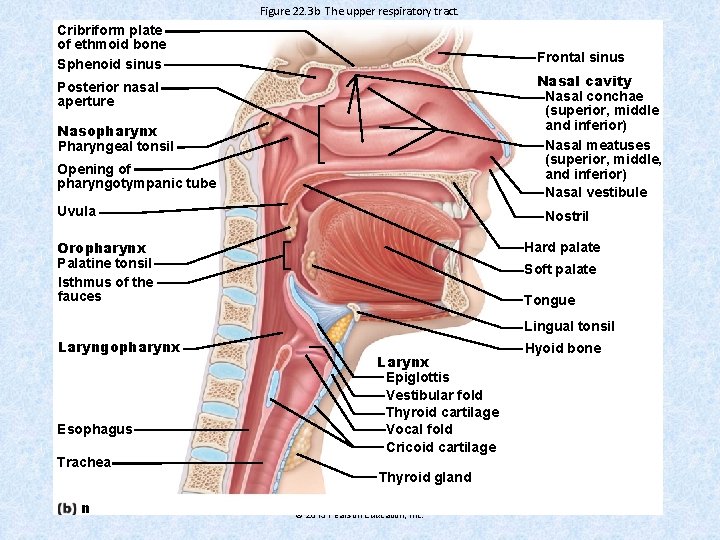
Figure 22. 3 b The upper respiratory tract. Cribriform plate of ethmoid bone Sphenoid sinus Frontal sinus Nasal cavity Nasal conchae (superior, middle and inferior) Nasal meatuses (superior, middle, and inferior) Nasal vestibule Posterior nasal aperture Nasopharynx Pharyngeal tonsil Opening of pharyngotympanic tube Uvula Nostril Oropharynx Palatine tonsil Isthmus of the fauces Hard palate Soft palate Tongue Lingual tonsil Laryngopharynx Esophagus Trachea n Larynx Epiglottis Vestibular fold Thyroid cartilage Vocal fold Cricoid cartilage Thyroid gland © 2013 Pearson Education, Inc. Hyoid bone
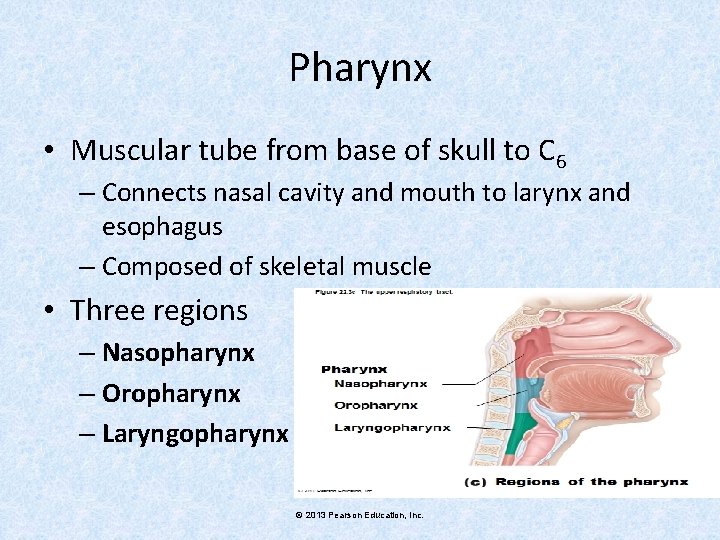
Pharynx • Muscular tube from base of skull to C 6 – Connects nasal cavity and mouth to larynx and esophagus – Composed of skeletal muscle • Three regions – Nasopharynx – Oropharynx – Laryngopharynx © 2013 Pearson Education, Inc.
Nasopharynx • Air passageway posterior to nasal cavity • Lining - pseudostratified columnar epithelium • Soft palate and uvula close nasopharynx during swallowing • Pharyngeal tonsil (adenoids) on posterior wall • Pharyngotympanic (auditory) tubes drain and equalize pressure in middle ear; open into lateral walls © 2013 Pearson Education, Inc.
Oropharynx and Laryngopharynx • • • Oropharynx Passageway for food and air from level of soft palate to epiglottis Isthmus of fauces-opening to oral cavity Palatine tonsils-in lateral walls of fauces Lingual tonsil-on posterior surface of tongue Laryngopharynx Passageway for food and air Posterior to upright epiglottis © 2013 Pearson Education, Inc.
Larynx • Attaches to hyoid bone; opens into laryngopharynx; continuous with trachea • Has 9 cartilages. Thyroid cartilage with laryngeal prominence is Adam s apple • Epiglottis-elastic cartilage; covers laryngeal inlet during swallowing. • Functions – Provides patent airway – Routes air and food into proper channels – Voice production • Houses vocal folds • Glottis-opening between vocal folds • Folds vibrate to produce sound as air rushes up from lungs © 2013 Pearson Education, Inc.
Voice Production • Speech-intermittent release of expired air while opening and closing glottis • Pitch determined by length and tension of vocal cords • Loudness depends upon force of air • Chambers of pharynx, oral, nasal, and sinus cavities amplify and enhance sound quality • Sound is "shaped" into language by muscles of pharynx, tongue, soft palate, and lips © 2013 Pearson Education, Inc.
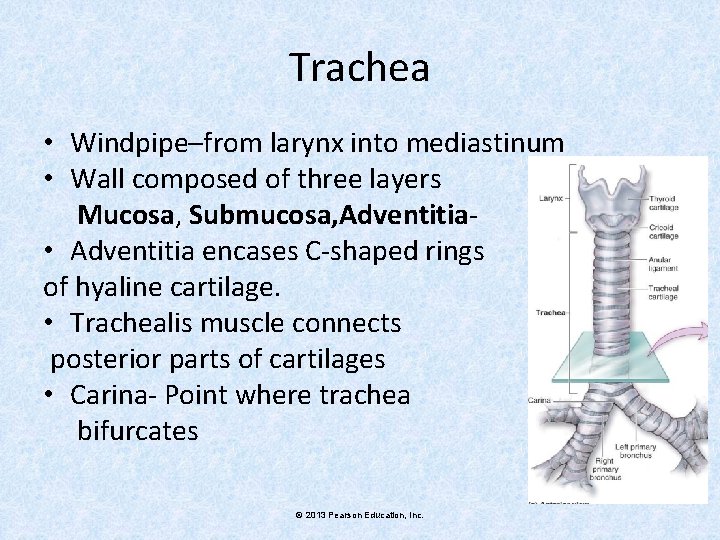
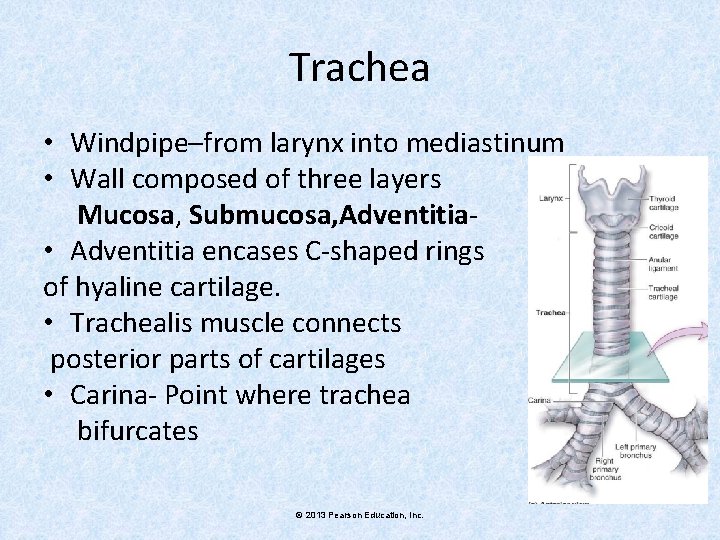
Trachea • Windpipe–from larynx into mediastinum • Wall composed of three layers Mucosa, Submucosa, Adventitia • Adventitia encases C-shaped rings of hyaline cartilage. • Trachealis muscle connects posterior parts of cartilages • Carina- Point where trachea bifurcates © 2013 Pearson Education, Inc.
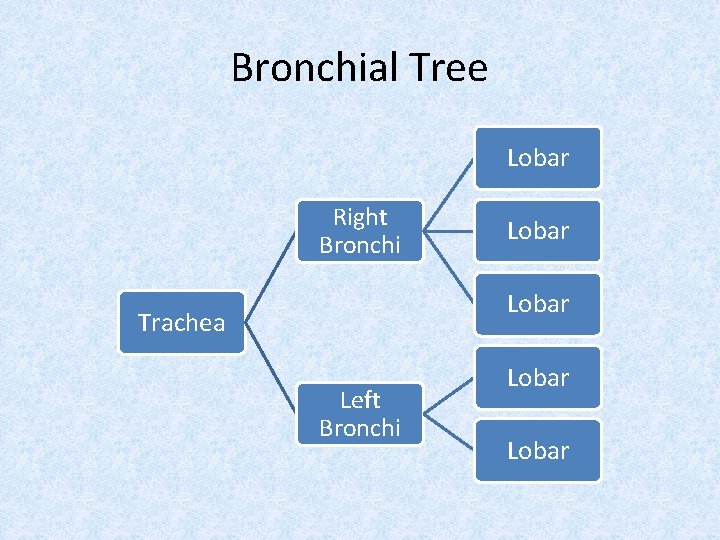
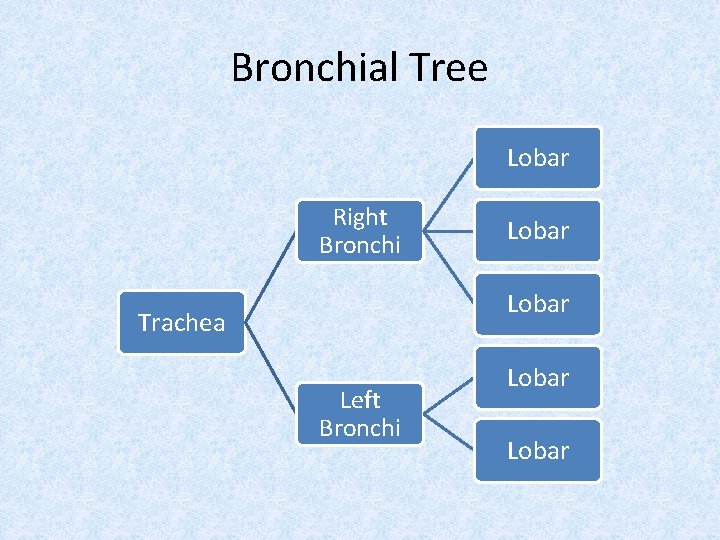
Bronchial Tree Lobar Right Bronchi Lobar Trachea Left Bronchi Lobar
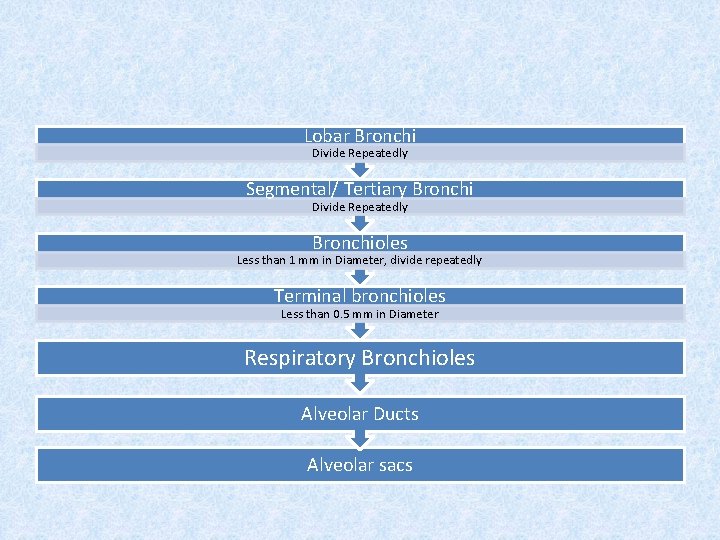
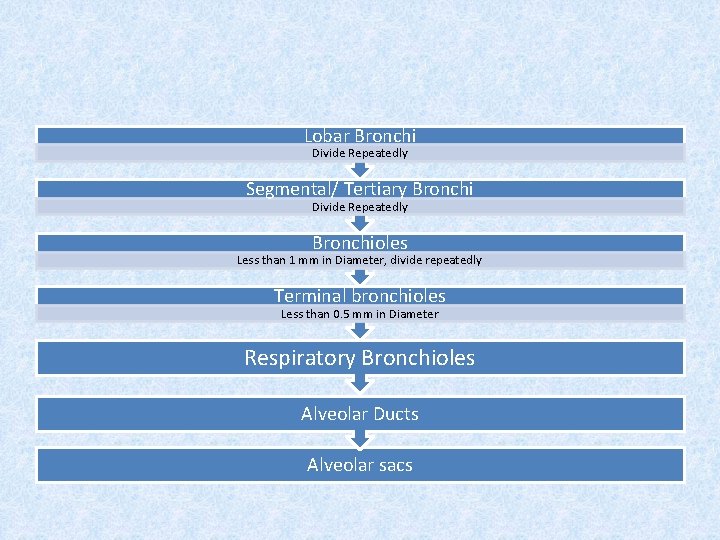
Lobar Bronchi Divide Repeatedly Segmental/ Tertiary Bronchi Divide Repeatedly Bronchioles Less than 1 mm in Diameter, divide repeatedly Terminal bronchioles Less than 0. 5 mm in Diameter Respiratory Bronchioles Alveolar Ducts Alveolar sacs
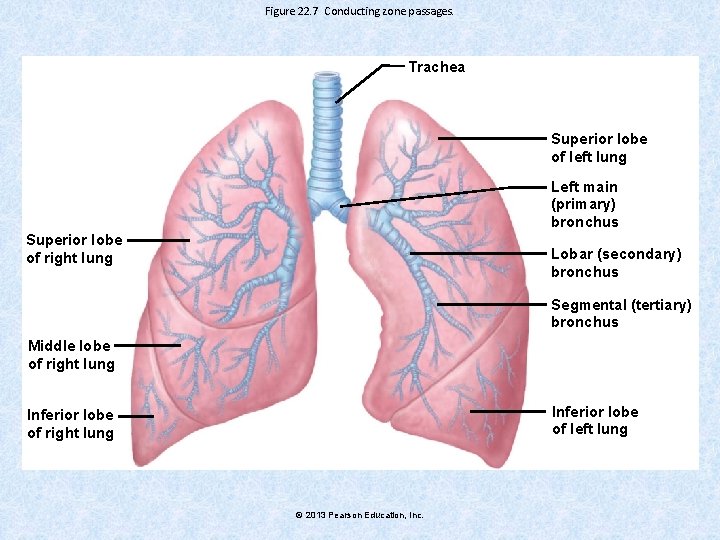
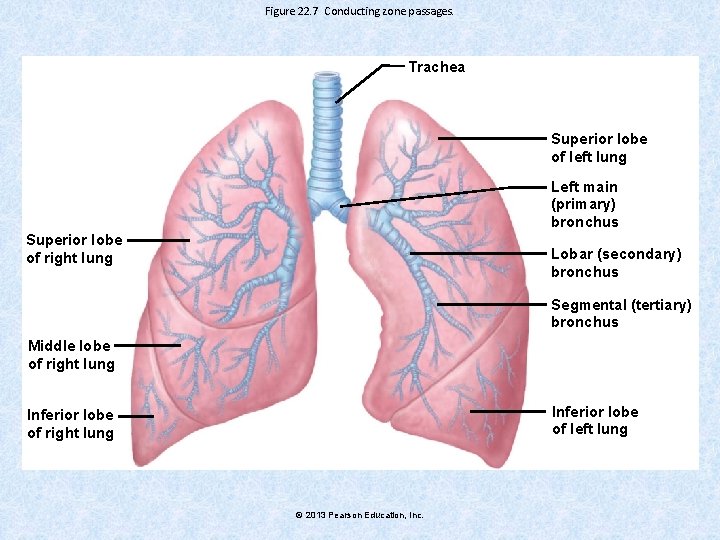
Figure 22. 7 Conducting zone passages. Trachea Superior lobe of left lung Left main (primary) bronchus Superior lobe of right lung Lobar (secondary) bronchus Segmental (tertiary) bronchus Middle lobe of right lung Inferior lobe of left lung Inferior lobe of right lung © 2013 Pearson Education, Inc.
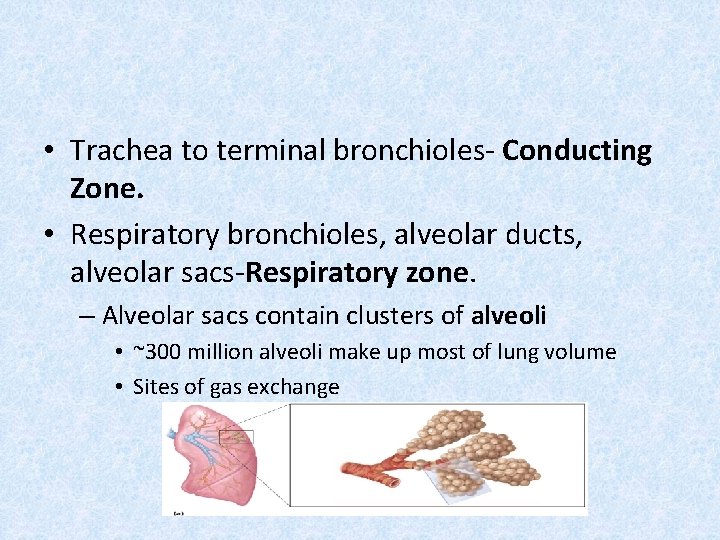
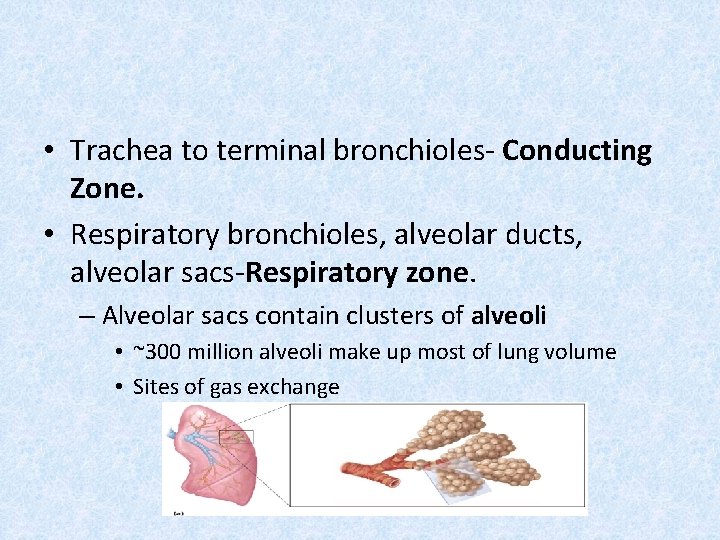
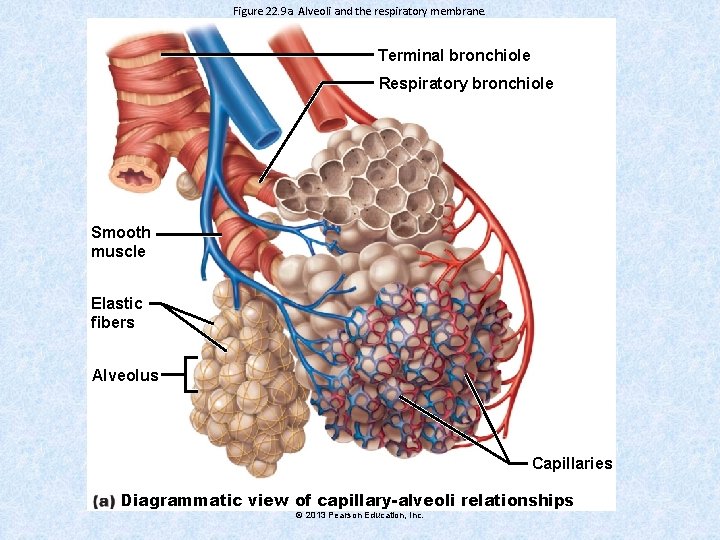
• Trachea to terminal bronchioles- Conducting Zone. • Respiratory bronchioles, alveolar ducts, alveolar sacs-Respiratory zone. – Alveolar sacs contain clusters of alveoli • ~300 million alveoli make up most of lung volume • Sites of gas exchange
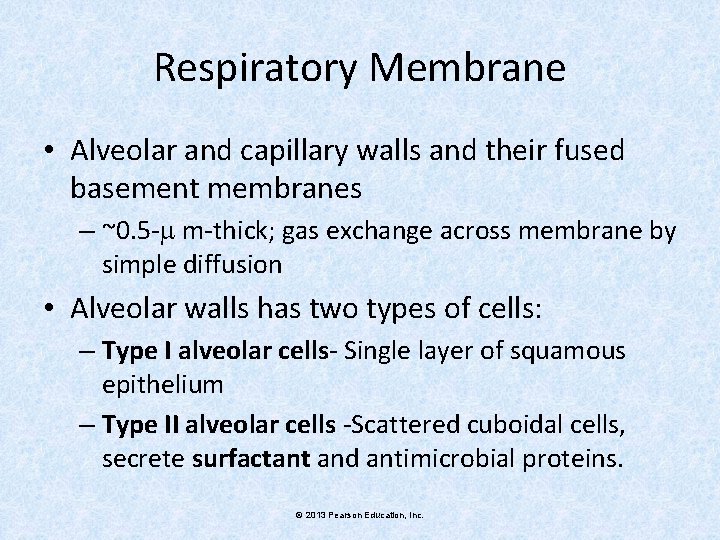
Respiratory Membrane • Alveolar and capillary walls and their fused basement membranes – ~0. 5 - m-thick; gas exchange across membrane by simple diffusion • Alveolar walls has two types of cells: – Type I alveolar cells- Single layer of squamous epithelium – Type II alveolar cells -Scattered cuboidal cells, secrete surfactant and antimicrobial proteins. © 2013 Pearson Education, Inc.
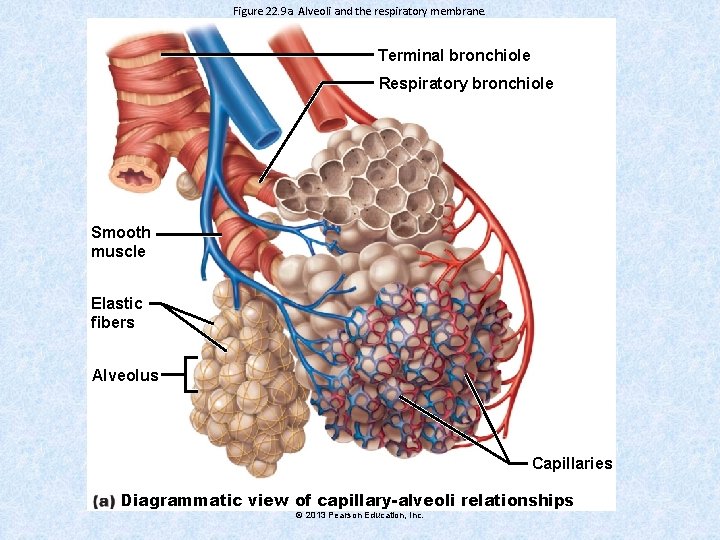
Figure 22. 9 a Alveoli and the respiratory membrane. Terminal bronchiole Respiratory bronchiole Smooth muscle Elastic fibers Alveolus Capillaries Diagrammatic view of capillary-alveoli relationships © 2013 Pearson Education, Inc.
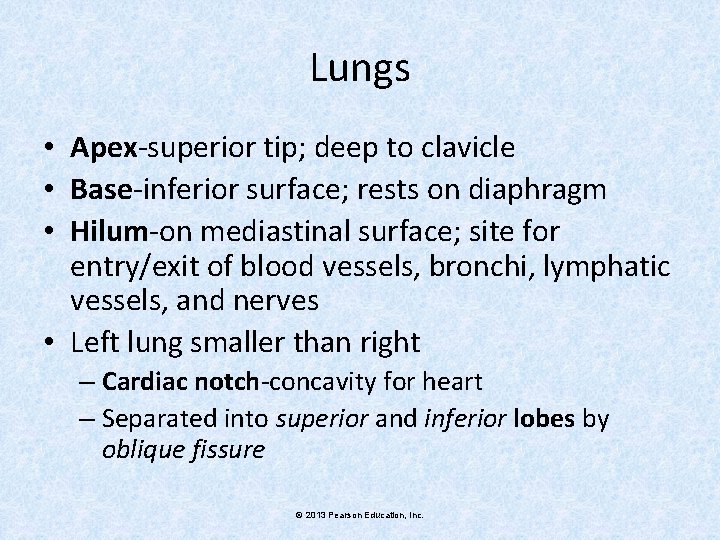
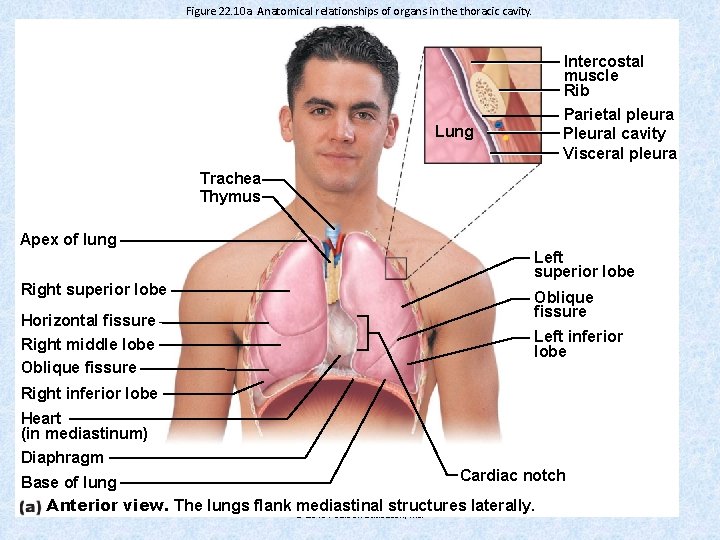
Lungs • Apex-superior tip; deep to clavicle • Base-inferior surface; rests on diaphragm • Hilum-on mediastinal surface; site for entry/exit of blood vessels, bronchi, lymphatic vessels, and nerves • Left lung smaller than right – Cardiac notch-concavity for heart – Separated into superior and inferior lobes by oblique fissure © 2013 Pearson Education, Inc.
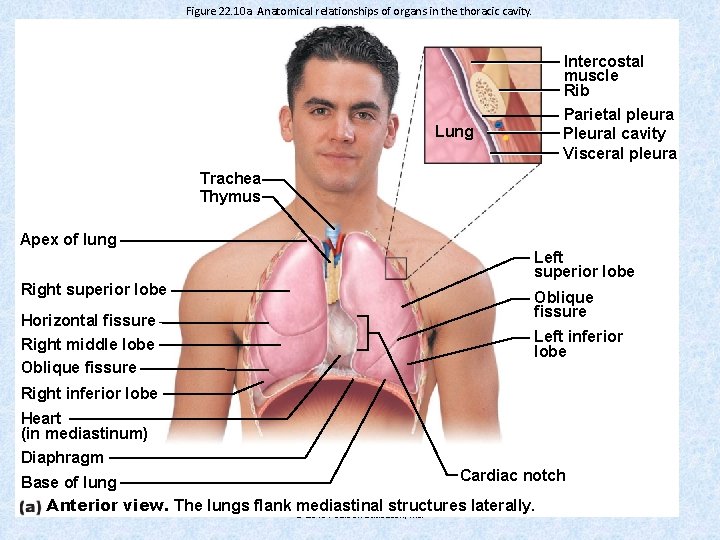
Figure 22. 10 a Anatomical relationships of organs in the thoracic cavity. Intercostal muscle Rib Lung Parietal pleura Pleural cavity Visceral pleura Trachea Thymus Apex of lung Right superior lobe Horizontal fissure Right middle lobe Oblique fissure Left superior lobe Oblique fissure Left inferior lobe Right inferior lobe Heart (in mediastinum) Diaphragm Cardiac notch Base of lung Anterior view. The lungs flank mediastinal structures laterally. © 2013 Pearson Education, Inc.
Blood Supply • Pulmonary circulation (low pressure, high volume) – Pulmonary arteries deliver systemic venous blood to lungs for oxygenation – Pulmonary veins carry oxygenated blood from respiratory zones to heart • Bronchial arteries provide oxygenated blood to lung tissue – Arise from aorta and enter lungs at hilum © 2013 Pearson Education, Inc.
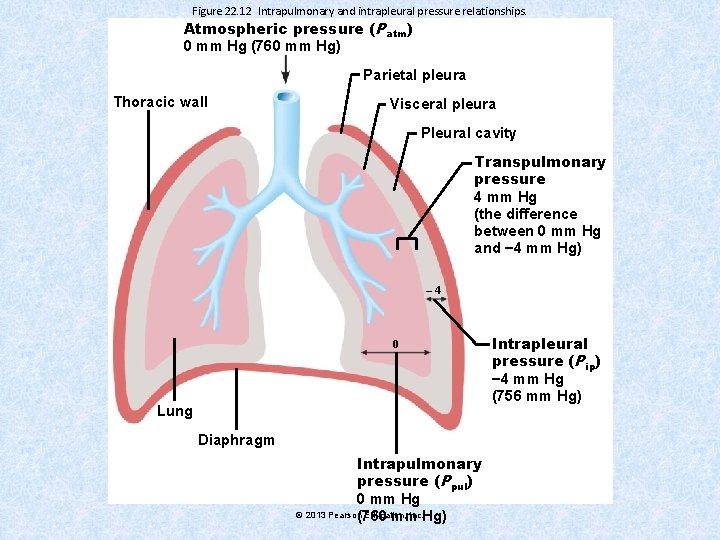
Pleurae • • Thin, double-layered serosa covering the lungs. Parietal pleura Visceral pleura Pleural fluid fills slit like pleural cavity – Provides lubrication and surface tension assists in expansion and recoil © 2013 Pearson Education, Inc.
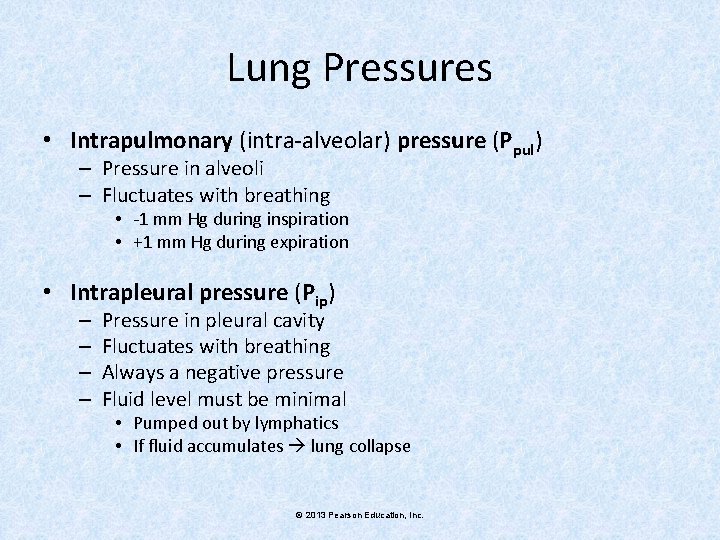
Lung Pressures • Intrapulmonary (intra-alveolar) pressure (Ppul) – Pressure in alveoli – Fluctuates with breathing • -1 mm Hg during inspiration • +1 mm Hg during expiration • Intrapleural pressure (Pip) – – Pressure in pleural cavity Fluctuates with breathing Always a negative pressure Fluid level must be minimal • Pumped out by lymphatics • If fluid accumulates lung collapse © 2013 Pearson Education, Inc.
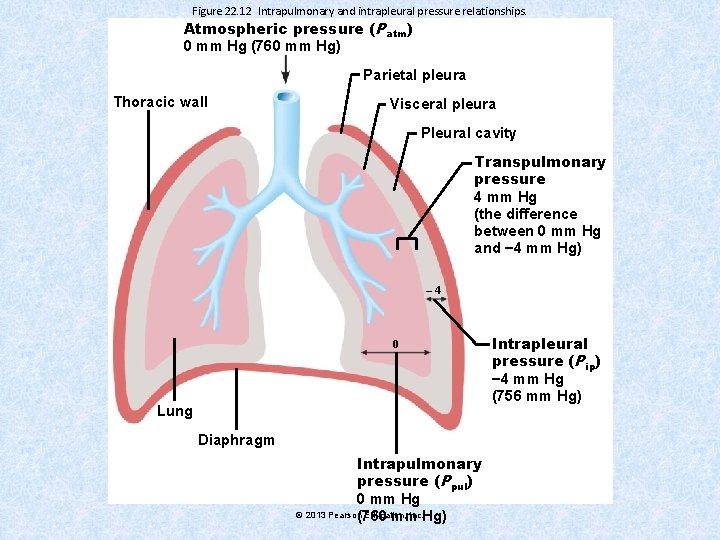
Figure 22. 12 Intrapulmonary and intrapleural pressure relationships. Atmospheric pressure (Patm) 0 mm Hg (760 mm Hg) Parietal pleura Thoracic wall Visceral pleura Pleural cavity Transpulmonary pressure 4 mm Hg (the difference between 0 mm Hg and − 4 mm Hg) – 4 0 Lung Diaphragm Intrapulmonary pressure (Ppul) 0 mm Hg © 2013 Pearson(760 Education, Inc. Hg) mm Intrapleural pressure (Pip) − 4 mm Hg (756 mm Hg)
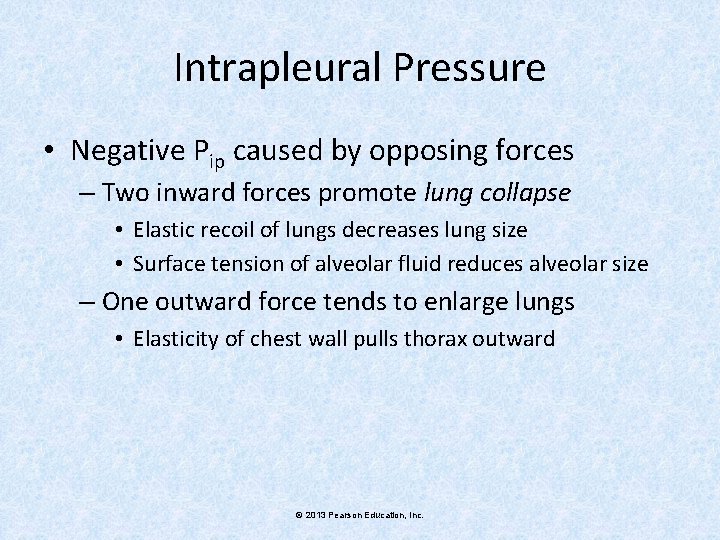
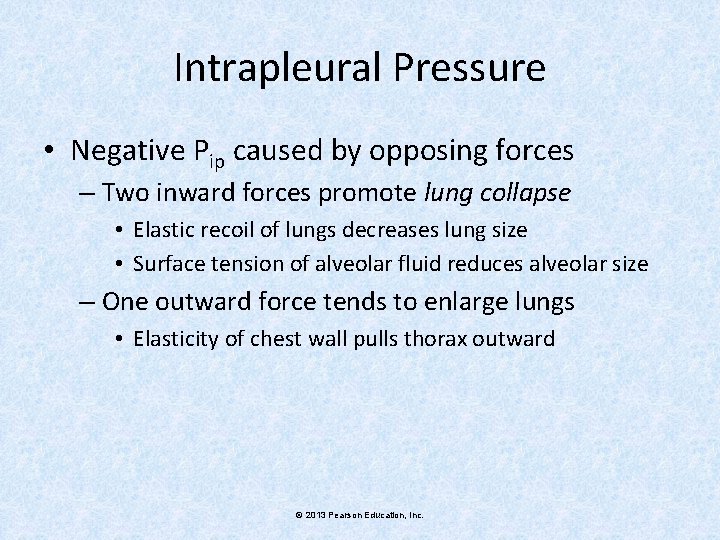
Intrapleural Pressure • Negative Pip caused by opposing forces – Two inward forces promote lung collapse • Elastic recoil of lungs decreases lung size • Surface tension of alveolar fluid reduces alveolar size – One outward force tends to enlarge lungs • Elasticity of chest wall pulls thorax outward © 2013 Pearson Education, Inc.
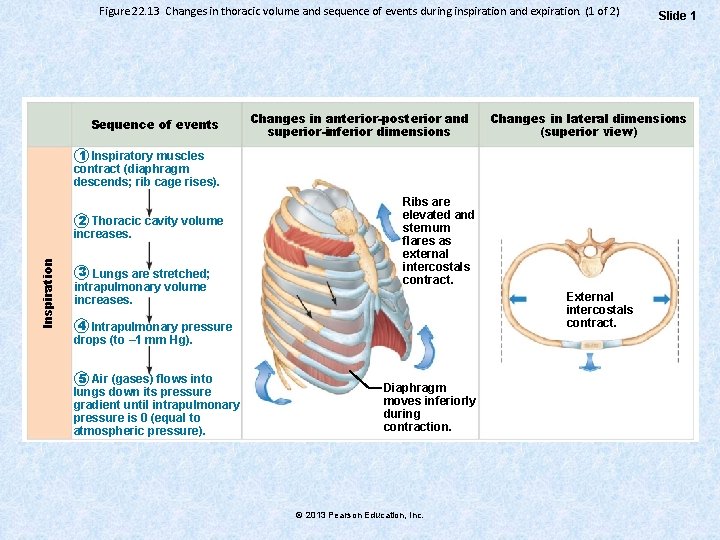
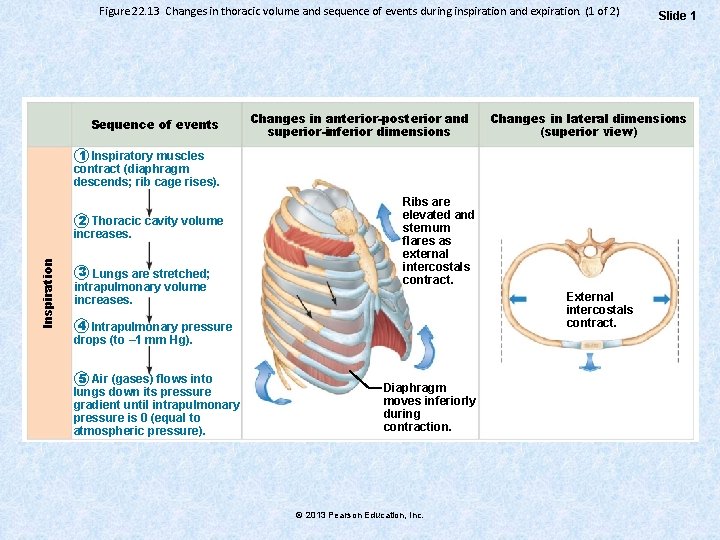
Figure 22. 13 Changes in thoracic volume and sequence of events during inspiration and expiration. (1 of 2) Sequence of events Changes in anterior-posterior and superior-inferior dimensions Changes in lateral dimensions (superior view) 1 Inspiratory muscles contract (diaphragm descends; rib cage rises). Inspiration 2 Thoracic cavity volume increases. 3 Lungs are stretched; intrapulmonary volume increases. Ribs are elevated and sternum flares as external intercostals contract. External intercostals contract. 4 Intrapulmonary pressure drops (to – 1 mm Hg). 5 Air (gases) flows into lungs down its pressure gradient until intrapulmonary pressure is 0 (equal to atmospheric pressure). Diaphragm moves inferiorly during contraction. © 2013 Pearson Education, Inc. Slide 1
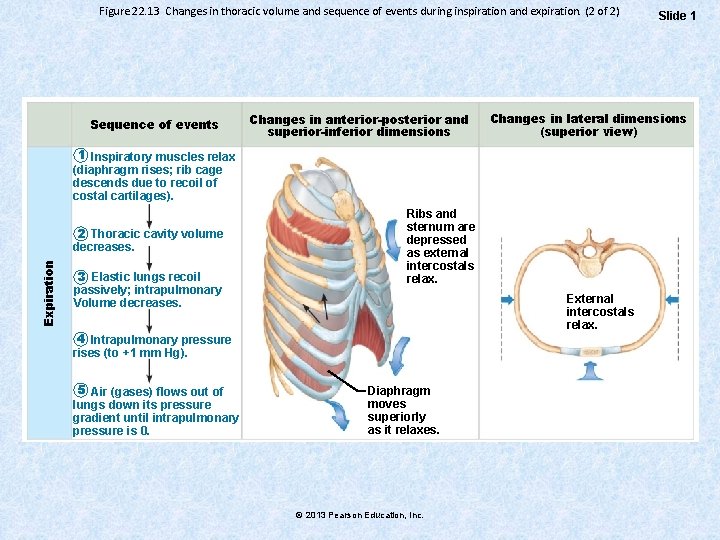
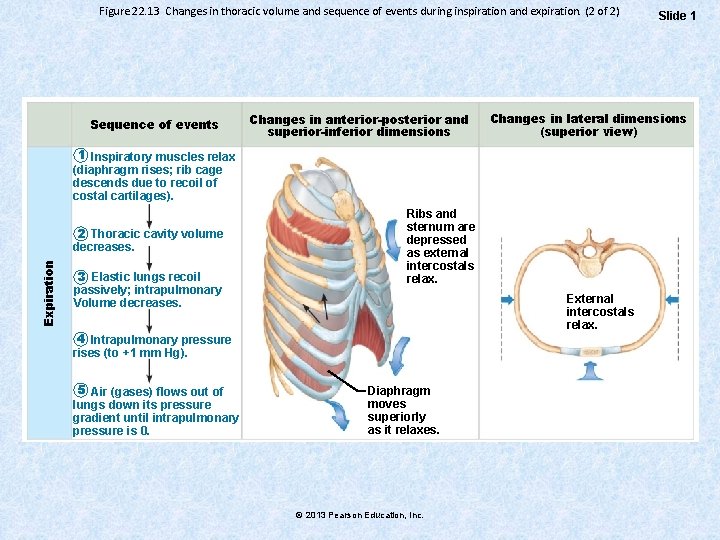
Figure 22. 13 Changes in thoracic volume and sequence of events during inspiration and expiration. (2 of 2) Sequence of events Changes in anterior-posterior and superior-inferior dimensions Changes in lateral dimensions (superior view) 1 Inspiratory muscles relax (diaphragm rises; rib cage descends due to recoil of costal cartilages). Expiration 2 Thoracic cavity volume decreases. 3 Elastic lungs recoil passively; intrapulmonary Volume decreases. Ribs and sternum are depressed as external intercostals relax. External intercostals relax. 4 Intrapulmonary pressure rises (to +1 mm Hg). 5 Air (gases) flows out of lungs down its pressure gradient until intrapulmonary pressure is 0. Diaphragm moves superiorly as it relaxes. © 2013 Pearson Education, Inc. Slide 1
Physical Factors Influencing Pulmonary Ventilation • Three factors hinder air passage and pulmonary ventilation; require energy to overcome – Airway resistance – Alveolar surface tension • Decreased by surfactant secreted by type II alveolar epithelial cells – Lung compliance • Higher compliance, easy distensibility © 2013 Pearson Education, Inc.
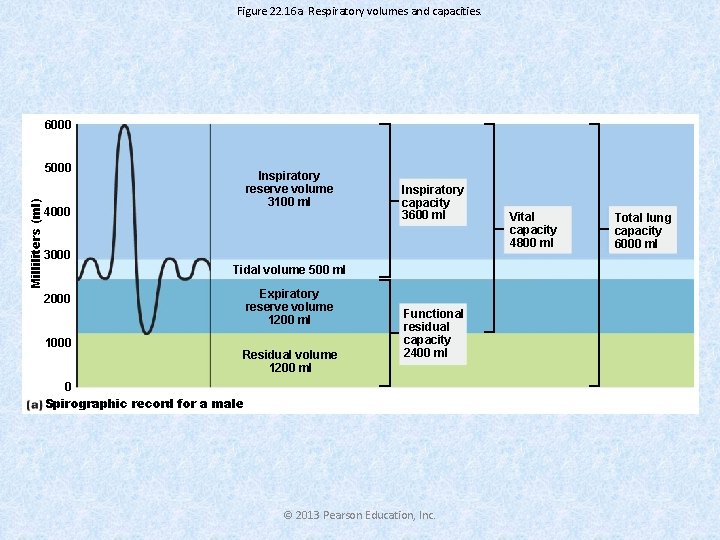
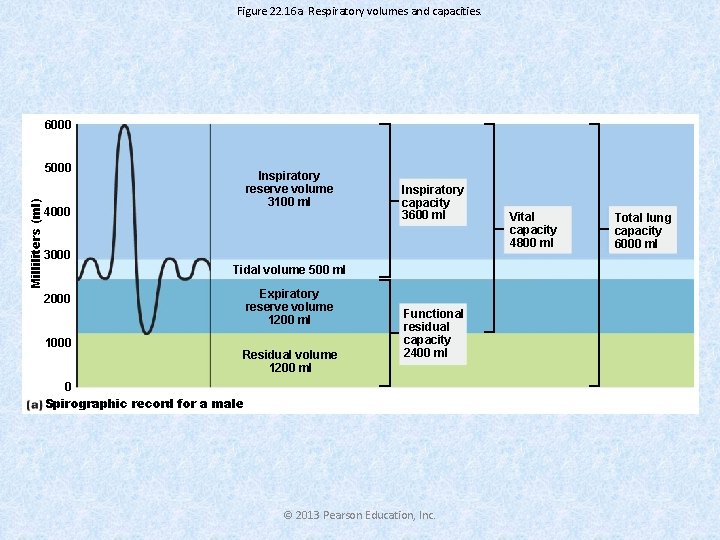
Figure 22. 16 a Respiratory volumes and capacities. 6000 Milliliters (ml) 5000 Inspiratory reserve volume 3100 ml 4000 Inspiratory capacity 3600 ml 3000 Tidal volume 500 ml Expiratory reserve volume 1200 ml 2000 1000 Residual volume 1200 ml Functional residual capacity 2400 ml 0 Spirographic record for a male © 2013 Pearson Education, Inc. Vital capacity 4800 ml Total lung capacity 6000 ml
Dead Space • Anatomical dead space – No contribution to gas exchange – Air remaining in passageways; ~150 ml • Alveolar dead space–non-functional alveoli due to collapse or obstruction • Total dead space-sum of anatomical and alveolar dead space © 2013 Pearson Education, Inc.
Homeostatic Imbalance • Bronchial Asthma • Infant Respiratory Distress Syndrome • Atelectasis
External Respiration • Exchange of O 2 and CO 2 across respiratory membrane • Influenced by – Thickness and surface area of respiratory membrane – Partial pressure gradients and gas solubilities – Ventilation-perfusion coupling © 2013 Pearson Education, Inc.
Partial Pressure Gradients and Gas Solubilities • Steep partial pressure gradient for O 2 in lungs – Venous blood Po 2 = 40 mm Hg – Alveolar Po 2 = 104 mm Hg • Drives oxygen flow to blood • Equilibrium reached across respiratory membrane in ~0. 25 seconds, about 1/3 time a red blood cell in pulmonary capillary – Adequate oxygenation even if blood flow increases 3 X © 2013 Pearson Education, Inc.
Partial Pressure Gradients and Gas Solubilities • Partial pressure gradient for CO 2 in lungs less steep – Venous blood Pco 2 = 45 mm Hg – Alveolar Pco 2 = 40 mm Hg • Though gradient not as steep, CO 2 diffuses in equal amounts with oxygen – CO 2 20 times more soluble in plasma than oxygen © 2013 Pearson Education, Inc.
Ventilation-Perfusion Coupling • Perfusion-blood flow reaching alveoli • Ventilation-amount of gas reaching alveoli • Ventilation and perfusion matched (coupled) for efficient gas exchange © 2013 Pearson Education, Inc.
Transport of Oxygen by Blood • Molecular O 2 carried in blood – 1. 5% dissolved in plasma – 98. 5% loosely bound to each Fe of hemoglobin (Hb) in RBCs (4 O 2 per Hb) – Loading and unloading of O 2 facilitated by change in shape of Hb –Binding of one molecule of O 2 to Hb increases its affinity to bind other molecules of o 2. © 2013 Pearson Education, Inc.
Factors Influencing Hemoglobin Saturation • Increases in temperature, H+, Pco 2, and BPG – Modify structure of hemoglobin; decrease its affinity for O 2 – Occur in systemic capillaries – Enhance O 2 unloading from blood – Shift O 2 -hemoglobin dissociation curve to right • Decreases in these factors shift curve to left – Decreases oxygen unloading from blood © 2013 Pearson Education, Inc.
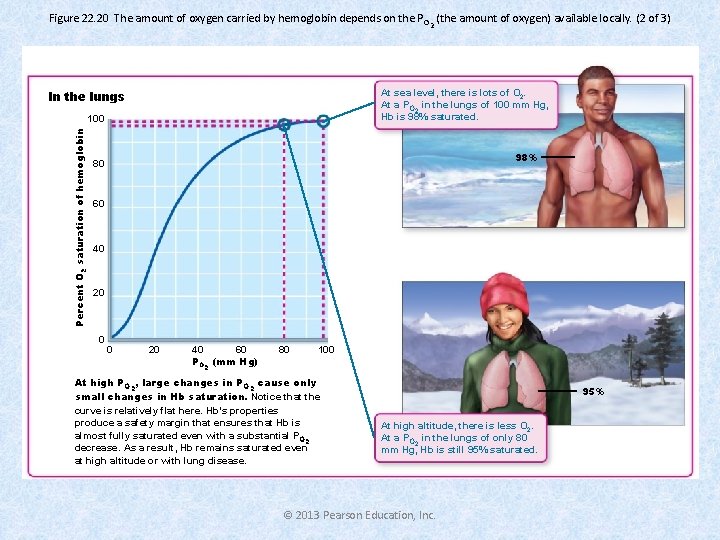
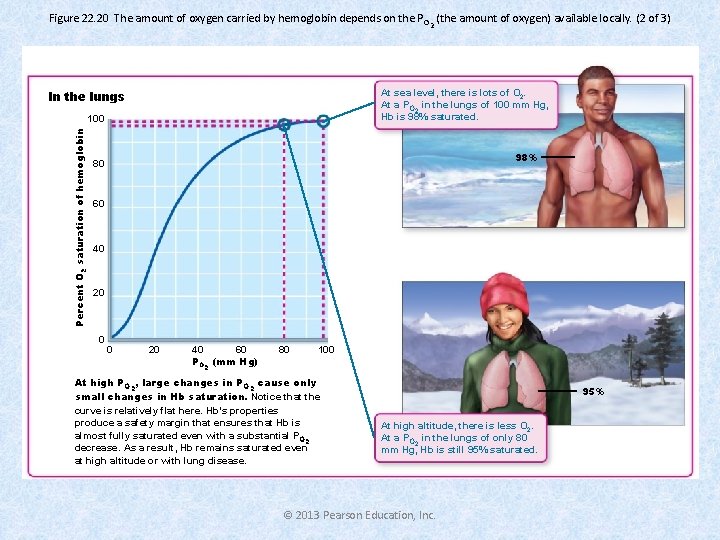
Figure 22. 20 The amount of oxygen carried by hemoglobin depends on the P O 2 (the amount of oxygen) available locally. (2 of 3) At sea level, there is lots of O 2. At a PO 2 in the lungs of 100 mm Hg, Hb is 98% saturated. In the lungs Percent O 2 saturation of hemoglobin 100 98% 80 60 40 20 0 0 20 40 60 PO 2 (mm Hg) 80 100 At high PO 2, large changes in PO 2 cause only small changes in Hb saturation. Notice that the curve is relatively flat here. Hb’s properties produce a safety margin that ensures that Hb is almost fully saturated even with a substantial PO 2 decrease. As a result, Hb remains saturated even at high altitude or with lung disease. 95% At high altitude, there is less O 2. At a PO 2 in the lungs of only 80 mm Hg, Hb is still 95% saturated. © 2013 Pearson Education, Inc.
Homeostatic Imbalance • Hypoxia Inadequate O 2 delivery to tissues cyanosis Anemic hypoxia–too few RBCs; abnormal or too little Hb Ischemic/Stagnant hypoxia–impaired/blocked circulation Histotoxic hypoxia–cells unable to use O 2, as in metabolic poisons – Hypoxic hypoxia–abnormal ventilation; pulmonary disease – Carbon monoxide poisoning–especially from fire; 200 X greater affinity for Hb than oxygen – – © 2013 Pearson Education, Inc.
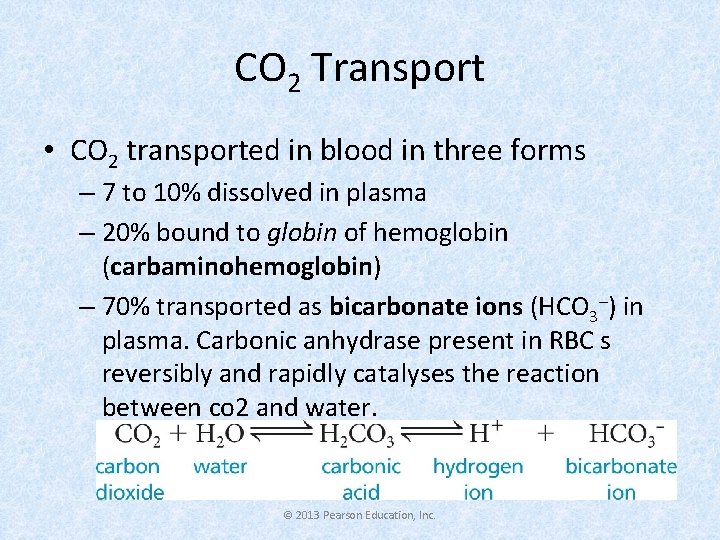
CO 2 Transport • CO 2 transported in blood in three forms – 7 to 10% dissolved in plasma – 20% bound to globin of hemoglobin (carbaminohemoglobin) – 70% transported as bicarbonate ions (HCO 3–) in plasma. Carbonic anhydrase present in RBC s reversibly and rapidly catalyses the reaction between co 2 and water. © 2013 Pearson Education, Inc.
Influence of CO 2 on Blood p. H • Changes in respiratory rate and depth affect blood p. H – Slow, shallow breathing increased CO 2 in blood drop in p. H – Rapid, deep breathing decreased CO 2 in blood rise in p. H • Changes in ventilation can adjust p. H when disturbed by metabolic factors © 2013 Pearson Education, Inc.
Control of Respiration • Involves higher brain centers, chemoreceptors, and other reflexes • Neural controls Ø Neurons in reticular formation of medulla and pons Ø Clustered neurons in medulla important Ø Ventral respiratory group- • Its inspiratory neurons excite inspiratory muscles via phrenic (diaphragm) and intercostal nerves (external intercostals) • Expiratory neurons inhibit inspiratory neurons Ø Dorsal respiratory group • Integrates input from peripheral stretch and chemoreceptors; sends information VRG © 2013 Pearson Education, Inc.
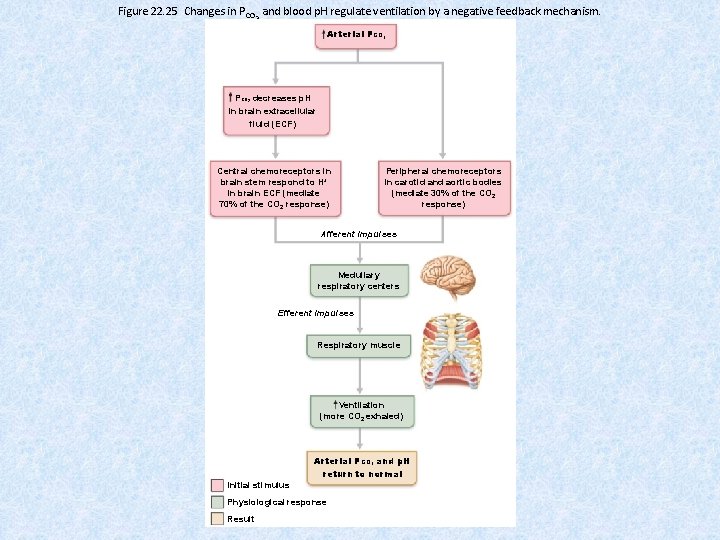
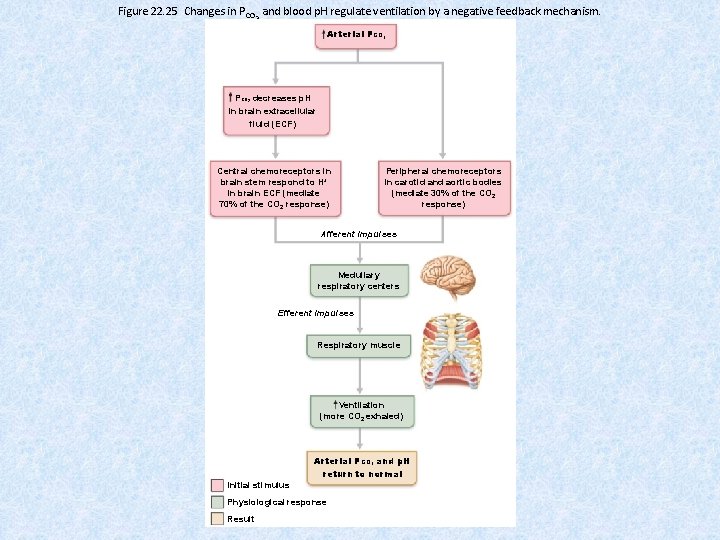
Figure 22. 25 Changes in PCO 2 and blood p. H regulate ventilation by a negative feedback mechanism. Arterial PCO 2 decreases p. H in brain extracellular fluid (ECF) Central chemoreceptors in brain stem respond to H+ in brain ECF (mediate 70% of the CO 2 response) Peripheral chemoreceptors in carotid and aortic bodies (mediate 30% of the CO 2 response) Afferent impulses Medullary respiratory centers Efferent impulses Respiratory muscle Ventilation (more CO 2 exhaled) Arterial PCO 2 and p. H return to normal Initial stimulus Physiological response Result © 2013 Pearson Education, Inc.
Respiratory Adjustments • Exercise: Increase in ventilation due to: – Psychological stimuli—anticipation of exercise – Simultaneous activation of skeletal muscles and respiratory centers – Excitatory impulses to respiratory centers from proprioceptors in moving muscles, tendons, joints • High Altitude-Hypoxia - Increase in Ventilation - Increased production of Erythropoietin.
Thank you
 Dr spandana hegde
Dr spandana hegde Spandana foundation guntur
Spandana foundation guntur Spandana foundation
Spandana foundation Respiratory zone vs conducting zone
Respiratory zone vs conducting zone Charles luther manson
Charles luther manson Respiratory system circulatory system digestive system
Respiratory system circulatory system digestive system How respiratory system work with circulatory system
How respiratory system work with circulatory system Circulatory system and respiratory system work together
Circulatory system and respiratory system work together Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Tư thế worm breton là gì
Tư thế worm breton là gì Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Môn thể thao bắt đầu bằng từ chạy
Môn thể thao bắt đầu bằng từ chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công của trọng lực
Công của trọng lực Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Phép trừ bù
Phép trừ bù Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế
Cái miệng nó xinh thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thế nào là giọng cùng tên? *
Thế nào là giọng cùng tên? * Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Tia chieu sa te
Tia chieu sa te Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot Số nguyên là gì
Số nguyên là gì Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Sơ đồ cơ thể người
Sơ đồ cơ thể người