PATHOPHYSIOLOGY OF THE DIGESTIVE SYSTEM In the GI











![Complications Of Cirrhosis [1] Jaundice Hepatic cells fail to metabolise bilirubin Serum bilirubin levels Complications Of Cirrhosis [1] Jaundice Hepatic cells fail to metabolise bilirubin Serum bilirubin levels](https://slidetodoc.com/presentation_image_h/272abfe0e45b37b30c4a5f86d21f0a67/image-122.jpg)

- Slides: 140
PATHOPHYSIOLOGY OF THE DIGESTIVE SYSTEM
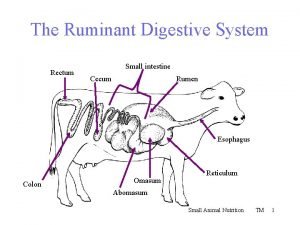
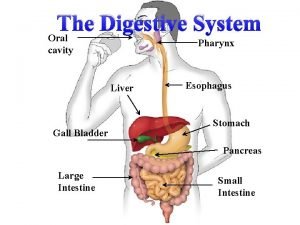
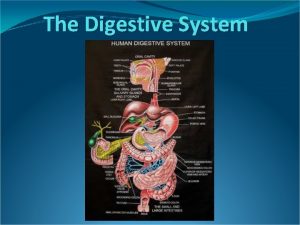
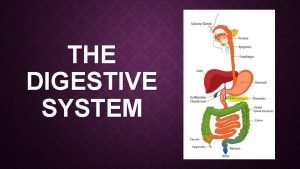
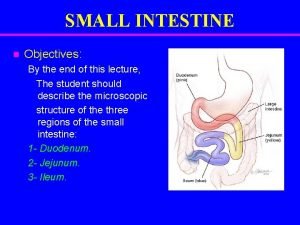
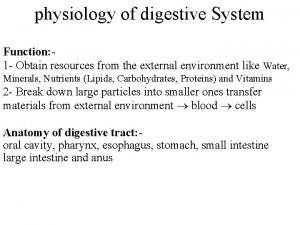
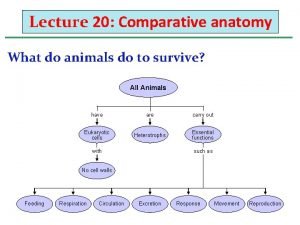
In the GI system, which is the boundary between the external and the internal environments, food is prepared for passage to the internal environment. Nutrients are propelled and mixed by the musculature of the GI tract and broken down into smaller units (digestion) that are absorbed through the intestinal tract mucosa (absorption) into the lymph or portal blood. The absorption process takes place by diffusion, carrier transport, or endocytosis.
GIT regulation Regulation of GIT depended from the autonomic nervous system and local factors of regulation. Autonomic nervous system stimulated (parasympatic) and inhibited (sympatic) secretion and motility in all parts of the GIT. Gastrointestinal hormones regulated some parts of the gastrointestinal system.
Gastrointestinal hormones are peptides secreted by the gastrointestinal mucosa, and controlling all gastrointestinal functions together with other hormones and transmitters. As an example insulin works together with acetylcholine and parasympathomimetics to stimulate secretion and motility, whereas catecholamines, sympatomimetics and parasympatolytics, such as atropine, inhibit gastrointestinal secretion and motility.
Peptide hormone families are groups of regulatory peptides that exhibit sequence homology (i. e. , they possess a common amino acid sequence). The gastrin-family and the secretinglucagon family are the most important. The gastrin family consists of gastrin and cholecystokinin (CCK) in three different forms (CCK-8, CCK-22, and CCK-33).
Ø Gastrin is the strongest stimulator of gastric acid secretion and motility. Ø Gastrin also imposes tropic (growthstimulating) actions on the parietal cells, the mucosa of the small and large intestine and possibly the pancreas. Ø Gastrin stimulates the pepsin secretion from peptic cells, and the glucagon secretion from the α-cells of the pancreatic islets.
Cholecystokinin empties the gall bladder as the name implies, and stimulates pancreatic secretion of an enzyme rich juice. Both gastrin and CCK release glucagon from the α-cells of the pancreatic islets. The most important stimulus for CCK liberation is amino acids and fatty acids, which reach the duodenal mucosa. Bile is ejected into the duodenum, where fat is emulgated to ease its absorption. CCK also acts as an enterogastrone - an intestinal hormone that inhibits gastric activity and emptying. This leaves more time for the bile to emulgate fat.
The secretin-glucagon family Secretin is secreted by S-cells in the mucosa of the upper small intestine, when acid chyme (p. H below 4. 5) arrives to the first part of the duodenum. Fatty acids from fat digestion also contribute to secretin release.
Secretin exhibits sequence homology with pancreatic glucagon, vasoactive intestinal peptide (VIP), growth hormonereleasing hormone (GHRH) and gastric inhibitory polypeptide (GIP). Secretin antagonises gastrin and potentiates CCK. Secretin stimulates the secretion of bicarbonate and water by pancreatic duct cells, and of bicarbonate-rich aqueous bile.
Gastric inhibitory polypeptide (GIP or Glucose-dependent Insulin releasing peptide) works as the two names imply: GIP inhibits the gastric mucosa and releases insulin from the -cells of the pancreatic islets.
Glucagon is actually two different molecules: Intestinal glucagon (glicentin) and pancreatic glucagon. Both are insulin-antagonists. Glucagon stimulate: glycogenolysis, gluconeogenesis (urea genesisglycogenic amino acids), and ketogenesis.
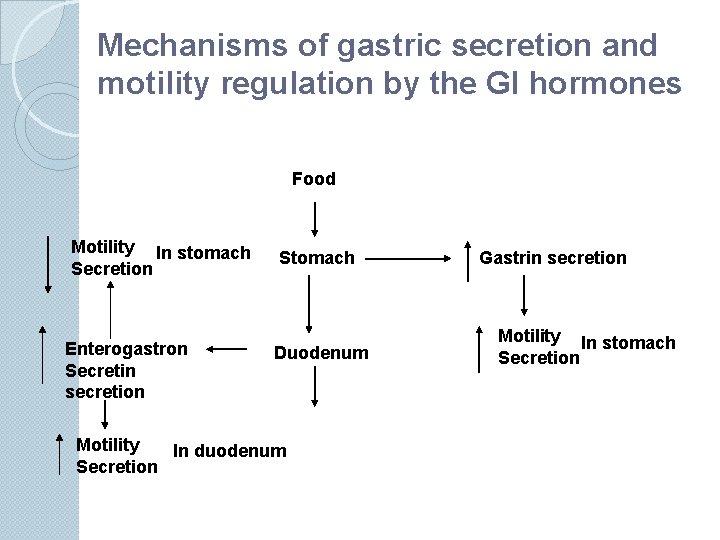
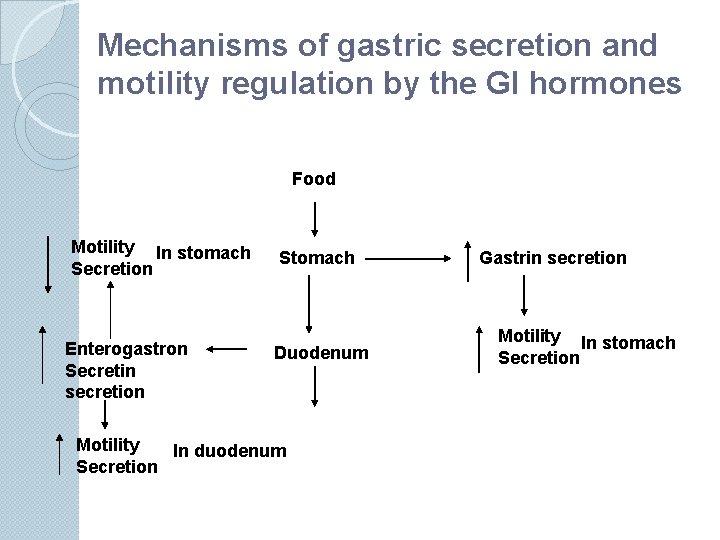
Mechanisms of gastric secretion and motility regulation by the GI hormones Food Motility In stomach Secretion Enterogastron Secretin secretion Stomach Duodenum Motility In duodenum Secretion Gastrin secretion Motility In stomach Secretion
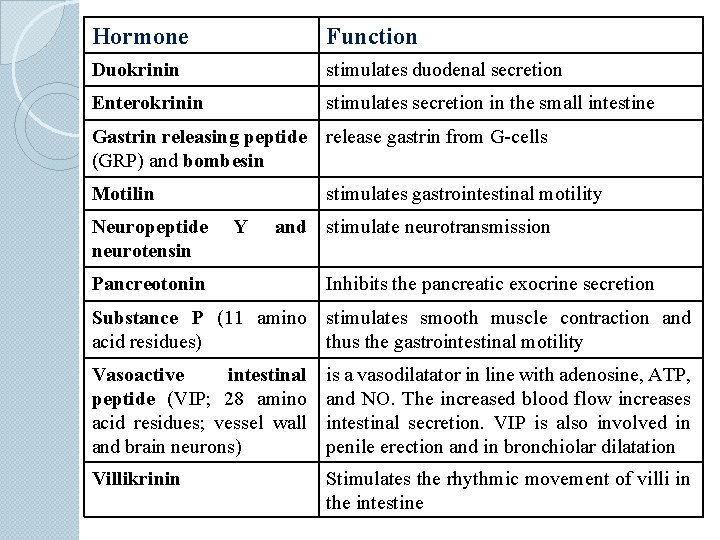
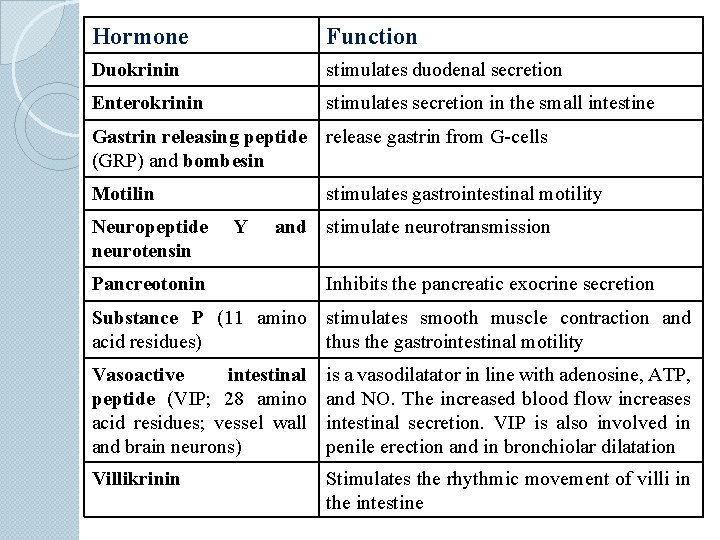
Hormone Function Duokrinin stimulates duodenal secretion Enterokrinin stimulates secretion in the small intestine Gastrin releasing peptide release gastrin from G-cells (GRP) and bombesin Motilin Neuropeptide neurotensin stimulates gastrointestinal motility Y and stimulate neurotransmission Pancreotonin Inhibits the pancreatic exocrine secretion Substance P (11 amino stimulates smooth muscle contraction and acid residues) thus the gastrointestinal motility Vasoactive intestinal peptide (VIP; 28 amino acid residues; vessel wall and brain neurons) is a vasodilatator in line with adenosine, ATP, and NO. The increased blood flow increases intestinal secretion. VIP is also involved in penile erection and in bronchiolar dilatation Villikrinin Stimulates the rhythmic movement of villi in the intestine
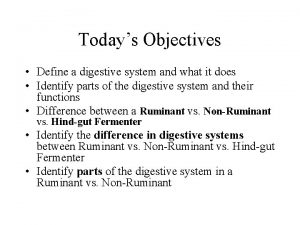
Concept of insufficiency of digestion The main function of digestion is supplying of the organism by main food stuffs, water, salts through olygomers disintegration and monomers absorption. Disorders →insufficiency of digestion→ malnutrition Classification: Ø primary malnutrition (diet) Ø secondary malnutrition - the supply of nutrients is adequate, but malnutrition may result from nutrient malabsorbtion, impaired nutrient use or storage, excess nutrient loss, or increased need for nutrients
Ethiology: inheritance diet problems infections disturbances of neural and humoral regulation
Disorders of appetite
Appetite disorders Anorexia nervosa is self-induced starvation, resulting in marked weight loss. The clinical symptoms of anorexia nervosa is similar to those in typical starvation. In addition, effects on the endocryne system are prominent: amenorrhea, hypothyroidism. A major complication of anorexia nervosa is cardiac arrhythmia and sudden death, resulting from hypokaliemia. Bulimia is a condition when patient binges on food and then induces vomiting. The major complications are: electrolyte imbalances (hypokaliemia), pulmonary aspirations of gastric contents and esophageal and cardiac rupture. Weight and gonadotropin levels are normal.

Vomiting or emesis is initiated by the feeling of nausea, and an array of sympathetic and parasympathetic responses. Sympathetic responses include sweating, pallor, increased respiration and heart rate and dilatation of pupils. Parasympathetic responses include profuse salivation, pronounced motility of the oesophagus, stomach, and duodenum, relaxation of the oesophageal sphincters. Duodenal contents can be forced into the stomach by anti-peristalsis.
Saliva glands disorders Hypersalivation Causes by parasympathetic activation, pregnansy toxicosis etc. Consequences are: stomatitis, hypohydration. Hyposalivation Reasons are: emotions, pain, fever, sympathetic stimulations, dehydration, antidepressants, patients with a rare autoimmune disorder (the Sjögren syndrome) suffer from dry mouth (xerostomia), dry eyes (xerophtalmia), infections of the buccal mucosa and dental caries are prevalent, and rheumatoid arthritis.
Diseases of esophagus
Gastro-oesophageal reflux disease Gastroesophageal reflux with oesophagitis is caused by incomplete closure of the lower oesophageal sphincter (LOS or American LES). Gastric contents with acid reaction then reflux into the oesophagus causing inflammation, erosion and bleeding. This disorder is also called reflux oesophagitis. The wall becomes hyperaemic, and white patches are seen on the epithelium (leucoplakias). The dysphagia most often presents as heartburn.
As dysphagia progress it is likely that an oesophageal stricture is developing. If the squamous epithelium of the lower oesophagus is replaced by columnar epithelium, as a response to long lasting injury, there is an increased risk of transformation of the epithelium into an adenocarcinoma.
Achalasia is a disease characterised by lack of peristalsis in oesophagus and relaxation failure of the lower oesophageal sphincter in response to swallowing. Vomiting and weight loss is major symptoms. The aetiology is unknown.
Stomach disorders
Mucosal protection system Mucous secretion Bicarbonate Epithelial tight junctions High blood flow to submucosa Central role of prostaglandins
Stomach disorders Hypersecretion Reasons may be: hyperacidic gastritis, diet problems, some drugs (insulin, corticosteroids), high tone of n. vagus.
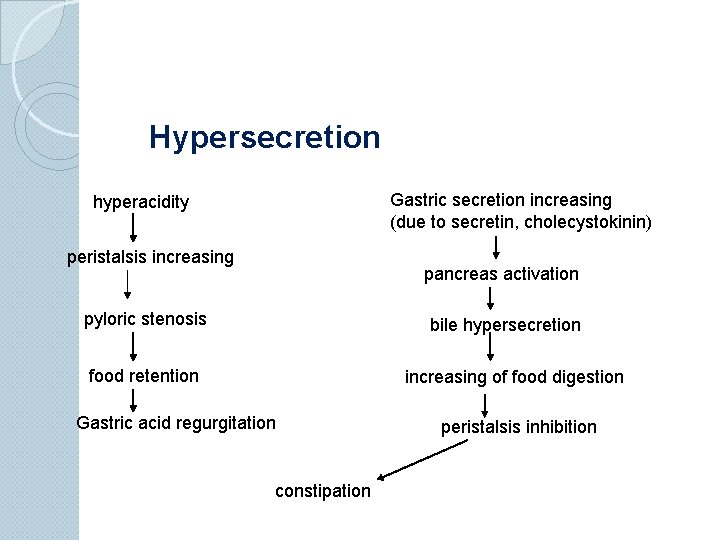
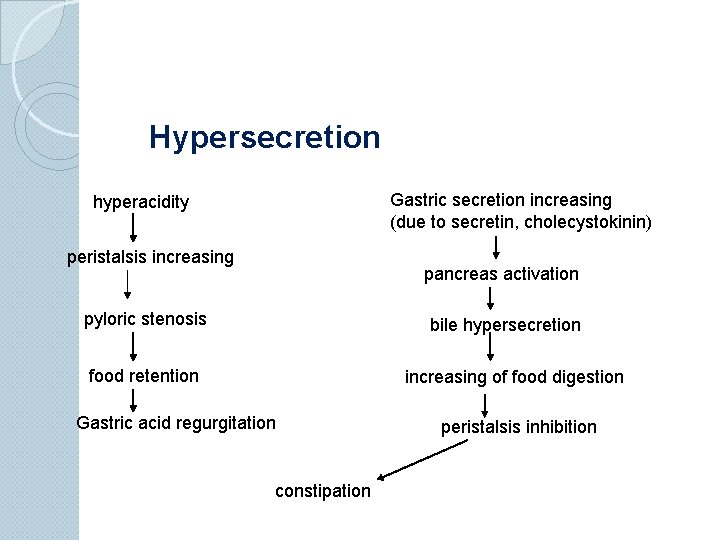
Hypersecretion Gastric secretion increasing (due to secretin, cholecystokinin) hyperacidity peristalsis increasing pancreas activation pyloric stenosis bile hypersecretion food retention increasing of food digestion Gastric acid regurgitation constipation peristalsis inhibition
Hyposecretion Appears due to: chronic atrophic gastritis, stomach cancer, hypohydration.
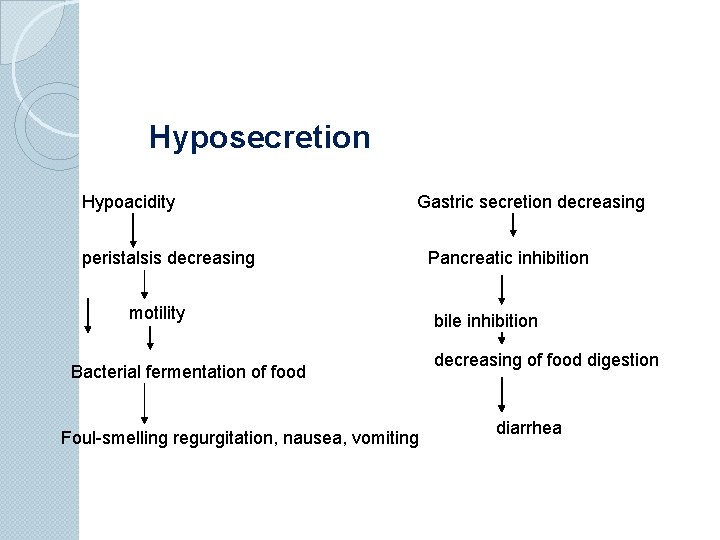
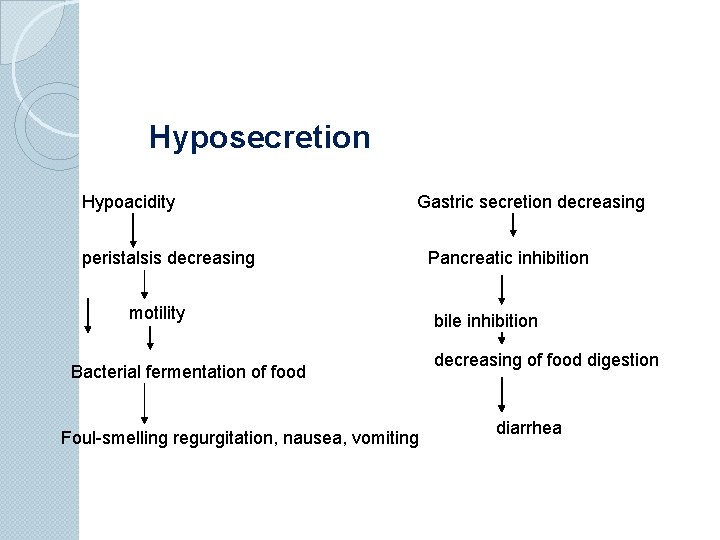
Hyposecretion Hypoacidity Gastric secretion decreasing peristalsis decreasing motility Bacterial fermentation of food Foul-smelling regurgitation, nausea, vomiting Pancreatic inhibition bile inhibition decreasing of food digestion diarrhea
Gastritis occurs as at least two typical manifestations: Acute, erosive gastritis and chronic, non-erosive gastritis.
Acute gastritis Depletion in mucosal protection system Acid/enzyme injury to gastric mucosa Inflammation, erosions, ulceration
Acute gastritis Risk factors Aspirin, NSAIDs Alcohol (acute excess) Heavy smoking Chemotherapy Acute ill patients/ ICU ◦ trauma, sepsis, shock ◦ extensive burns (Curling’s ulcer) Neurological disease (Cushing’s ulcer)
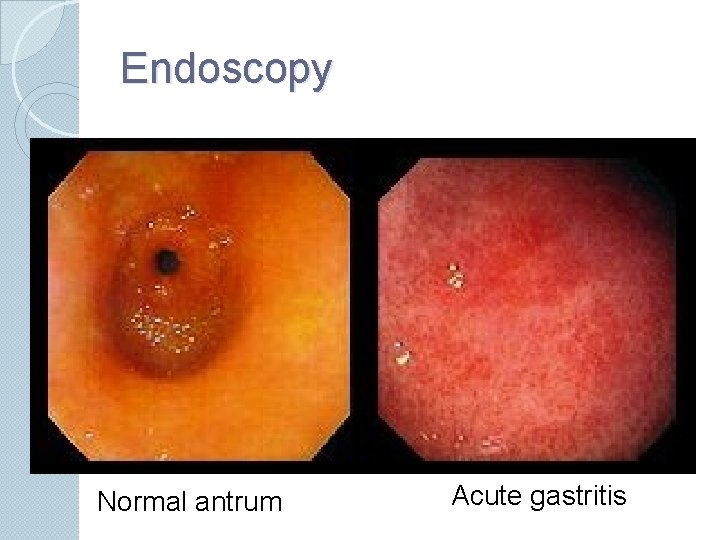
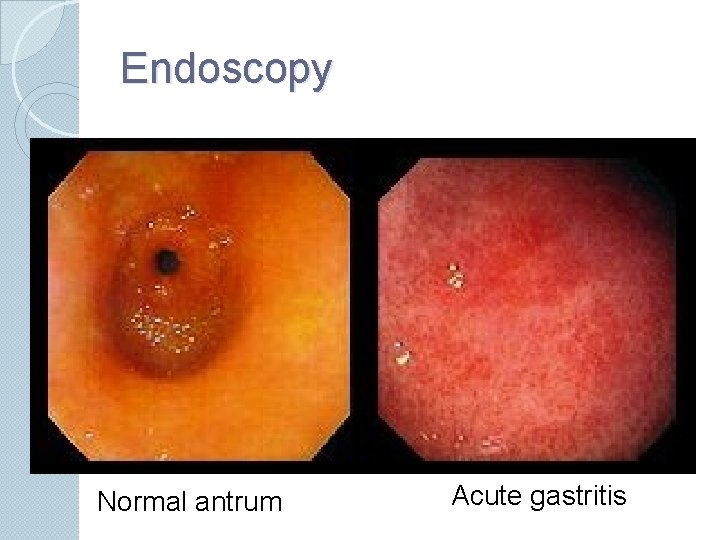
Endoscopy Normal antrum Acute gastritis
Chronic gastritis Type I: Autoimmune gastritis Type II: Helicobacter gastritis Type III: Chemical gastropathy (NSAIDs)
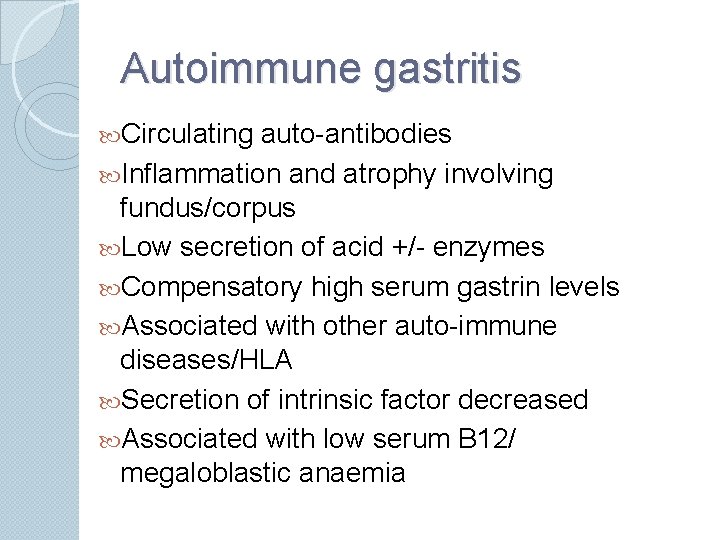
Autoimmune gastritis Circulating auto-antibodies Inflammation and atrophy involving fundus/corpus Low secretion of acid +/- enzymes Compensatory high serum gastrin levels Associated with other auto-immune diseases/HLA Secretion of intrinsic factor decreased Associated with low serum B 12/ megaloblastic anaemia
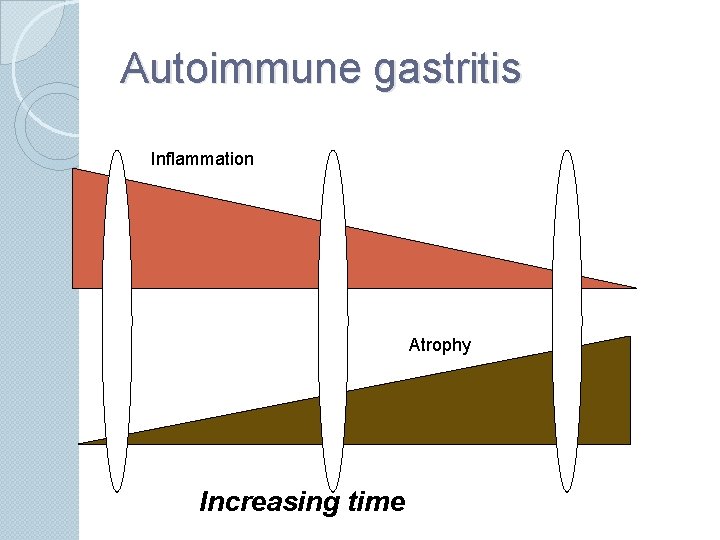
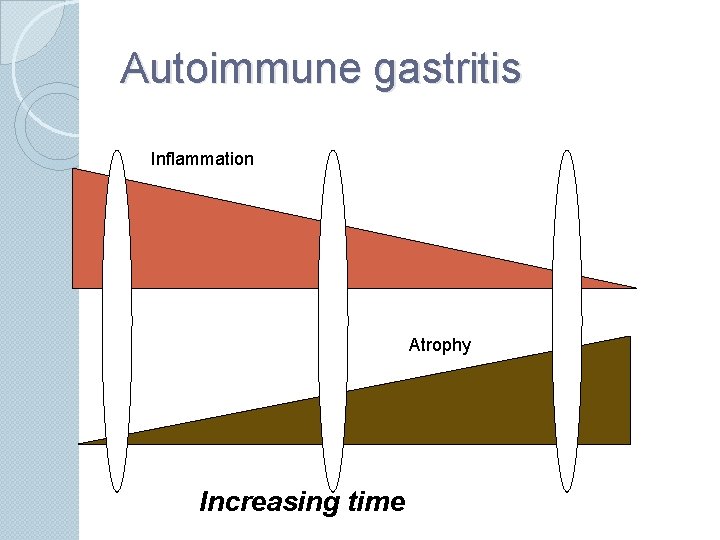
Autoimmune gastritis Inflammation Atrophy Increasing time
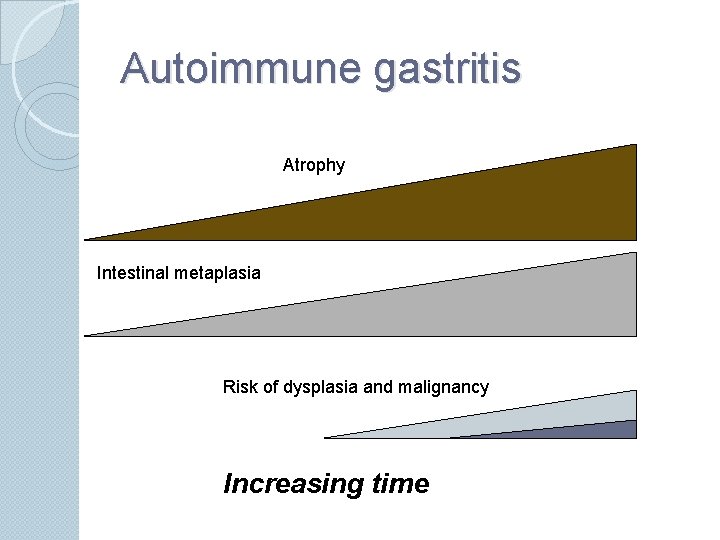
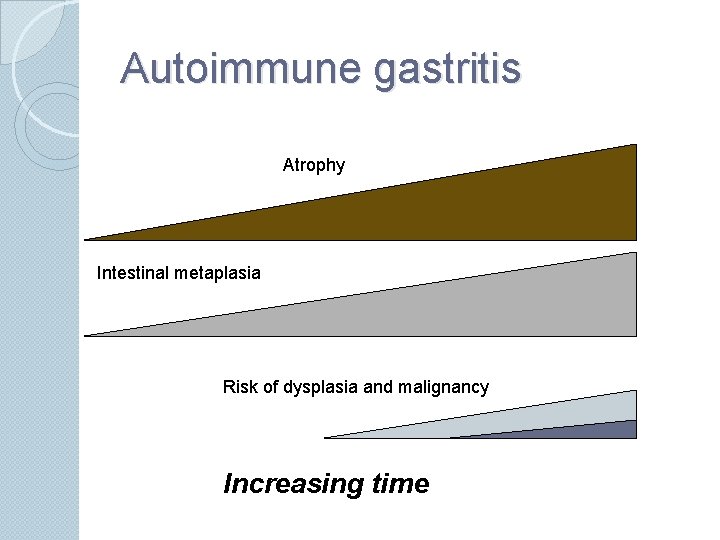
Autoimmune gastritis Atrophy Intestinal metaplasia Risk of dysplasia and malignancy Increasing time
Chronic gastritis ◦ Type II: Not autoimmune in origin Different distribution: antralpredominant Acid secretion increased (some normal) Serum gastrin normal (some increased)

Chronic gastritis Ø Type II: Helicobacter pylori gastritis Øevidence for role of H. pylori in gastritis/ulcer Øepidemiology Ø 90% of patients with duodenal ulcer Ø 70% with gastritis/gastric ulcer (80 -90% if not taking NSAIDs) Øtreatment effect ØHp clearance leads to ulcer healing ØHigh recurrence after ulcer healing without Hp clearance
Helicobacter pylori History In 1982 following the Easter holidays in the Microbiology Dept of the Royal Perth Hospital a culture of a spiral-shaped bacterium from gastric biopsies of patients with gastritis was isolated The discovery was by Dr. Robin Warren and Dr. Barry Marshall
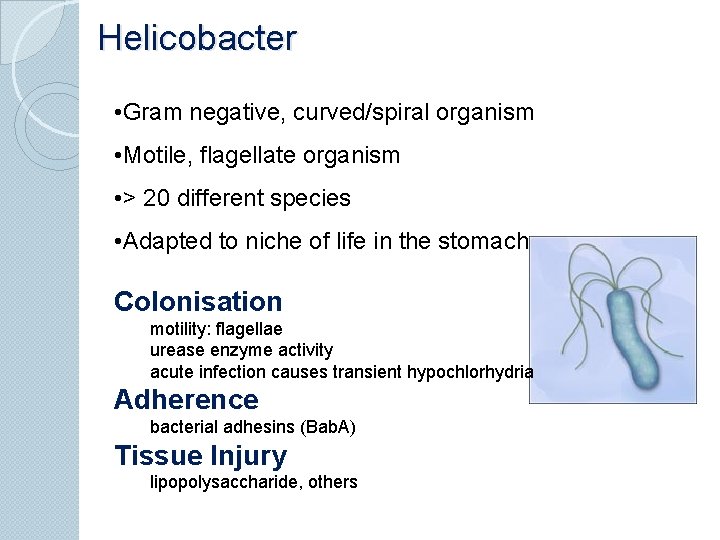
Helicobacter • Gram negative, curved/spiral organism • Motile, flagellate organism • > 20 different species • Adapted to niche of life in the stomach Colonisation motility: flagellae urease enzyme activity acute infection causes transient hypochlorhydria Adherence bacterial adhesins (Bab. A) Tissue Injury lipopolysaccharide, others
Pathogenesis Factors permitting colonisation: Spiral shape and flagellate – for motility within this mucous layer. Urease activity – which generate ammonium ions that buffer gastric activity Micro-aerophilism – for survival within the mucous gel Attachment to epithelial cells Evasion of Immune response

Acute Helicobacter infection - Epithelial cells are the initial sensor of contact with pathogen - Bacterial factors: induce IL-8 secretion by the gastric epithelial cells (also IL-6, IL-7, IL-15) - IL 8: chemotactic, activates neutrophils - IL-6, IL-7, IL-15: activate antigen-specific response -Bacterial lipopolysaccharide: directly chemotactic -Acute neutrophilic response
Establishing chronic active infection However H. pylori remains intra-luminal, so - Neutrophil response fails to clear bacterium - Bacterial persistence sets up T-cell dependent response: lymphocytes, plasma cells - Neutrophil response persists => Chronic active gastritis
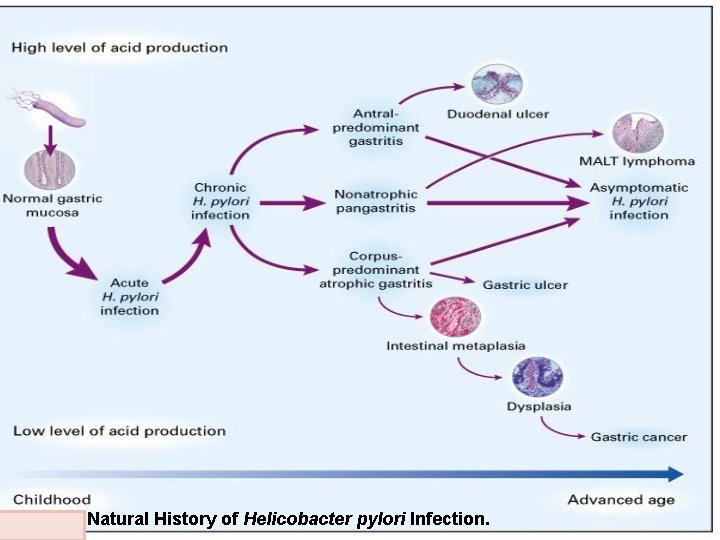
--> (Acute) --> Chronic active gastritis Different possible outcomes --> Antral-predominant gastritis --> duodenal ulcer --> Multi-focal atrophic gastritis --> gastric ulcer --> intestinal metaplasia --> risk of dysplasia --> adenocarcinoma --> Gastric lymphoma (lymphoma of MALT)
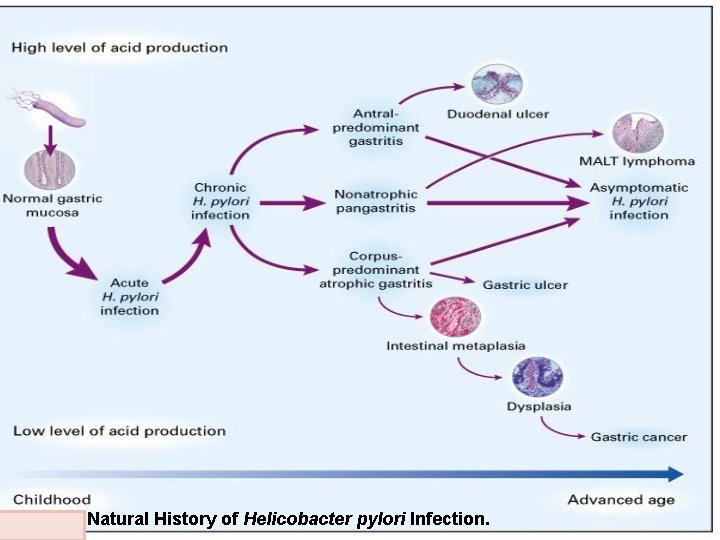
Figure 3. Natural History of Helicobacter pylori Infection.
Peptic ulcer disease
Peptic ulcer disease Condition characterized by �Erosion of GI mucosa resulting from digestive action of HCl and pepsin Epidemiological occurrence can be explained on the prevalence of Helicobacter pylori infection of the stomach and the colonisation of the upper gastrointestinal tract with this bacterium. Helicobacter pylori infection destroys the protective system, and at the same time provokes excess acid secretion.
Peptic Ulcer Disease Ulcer ◦ ◦ development Lower esophagus Stomach Duodenum 10% of men, 4% of women
Types Acute ◦ Superficial erosion ◦ Minimal erosion Chronic ◦ Muscular wall erosion with formation of fibrous tissue ◦ Present continuously for many months or intermittently
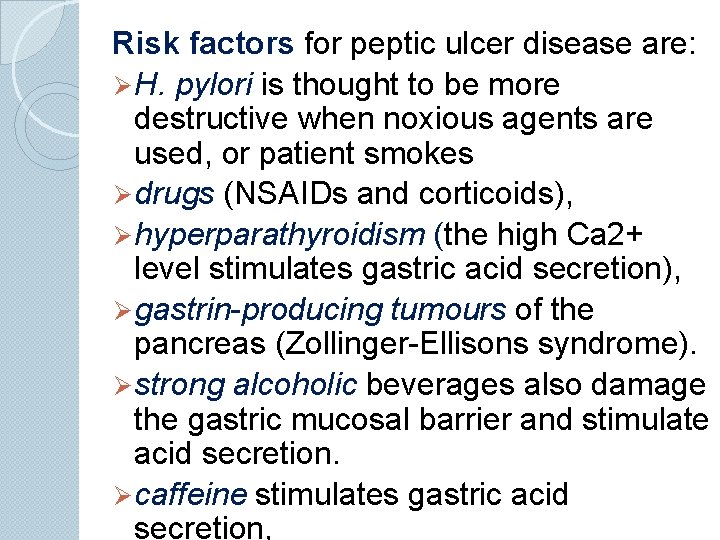
Risk factors for peptic ulcer disease are: Ø H. pylori is thought to be more destructive when noxious agents are used, or patient smokes Ø drugs (NSAIDs and corticoids), Ø hyperparathyroidism (the high Ca 2+ level stimulates gastric acid secretion), Ø gastrin-producing tumours of the pancreas (Zollinger-Ellisons syndrome). Ø strong alcoholic beverages also damage the gastric mucosal barrier and stimulate acid secretion. Ø caffeine stimulates gastric acid secretion,
Peptic Ulcer Disease Etiology and Pathophysiology Some intraluminal acid does seem to be essential for a gastric ulcer to occur Develop only in presence of acid environment Person with a gastric ulcer has normal to less than normal gastric acidity compared with person with a duodenal ulcer Surface mucosa of stomach is renewed about every 3 days Mucosa can continually repair itself except in extreme instances
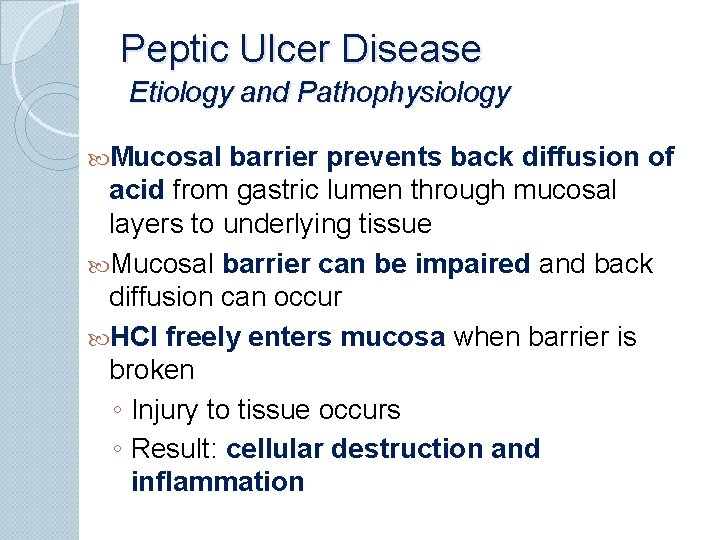
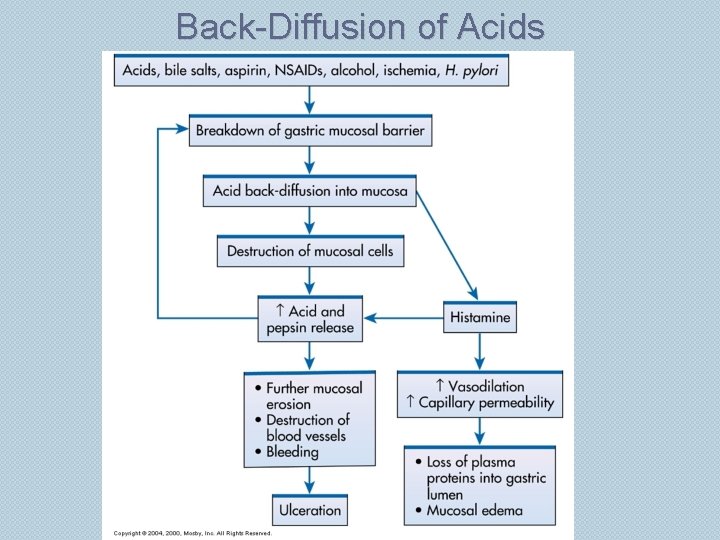
Peptic Ulcer Disease Etiology and Pathophysiology Mucosal barrier prevents back diffusion of acid from gastric lumen through mucosal layers to underlying tissue Mucosal barrier can be impaired and back diffusion can occur HCl freely enters mucosa when barrier is broken ◦ Injury to tissue occurs ◦ Result: cellular destruction and inflammation
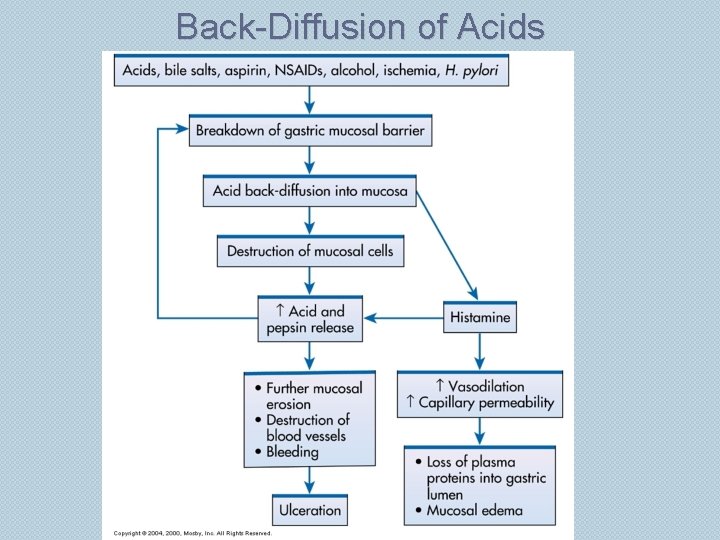
Back-Diffusion of Acids
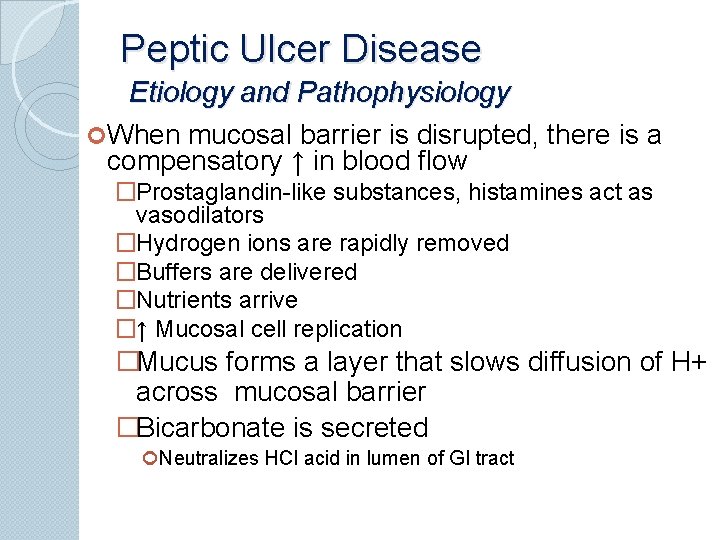
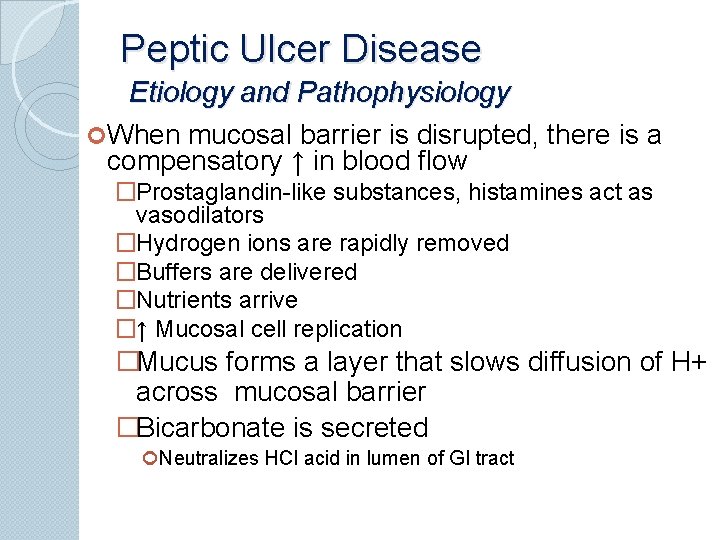
Peptic Ulcer Disease Etiology and Pathophysiology When mucosal barrier is disrupted, there is a compensatory ↑ in blood flow �Prostaglandin-like substances, histamines act as vasodilators �Hydrogen ions are rapidly removed �Buffers are delivered �Nutrients arrive �↑ Mucosal cell replication �Mucus forms a layer that slows diffusion of H+ across mucosal barrier �Bicarbonate is secreted Neutralizes HCl acid in lumen of GI tract
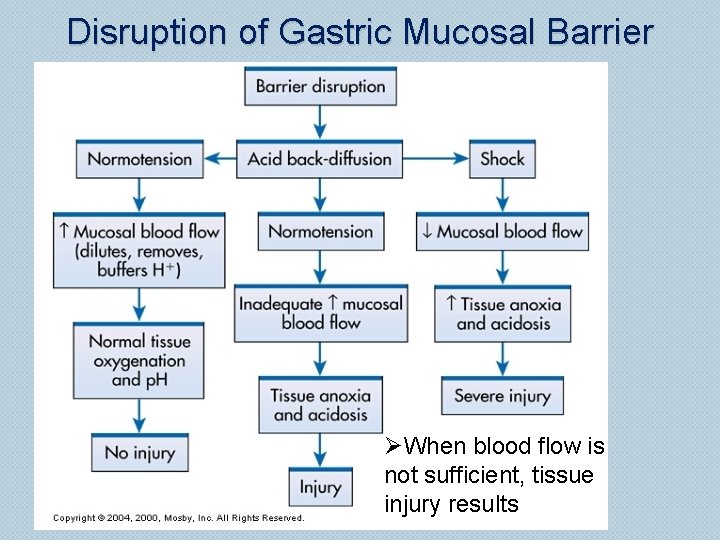
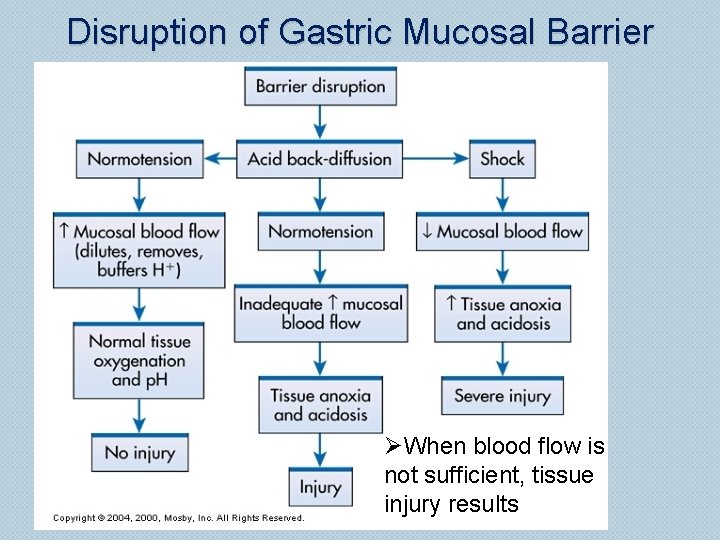
Disruption of Gastric Mucosal Barrier ØWhen blood flow is not sufficient, tissue injury results
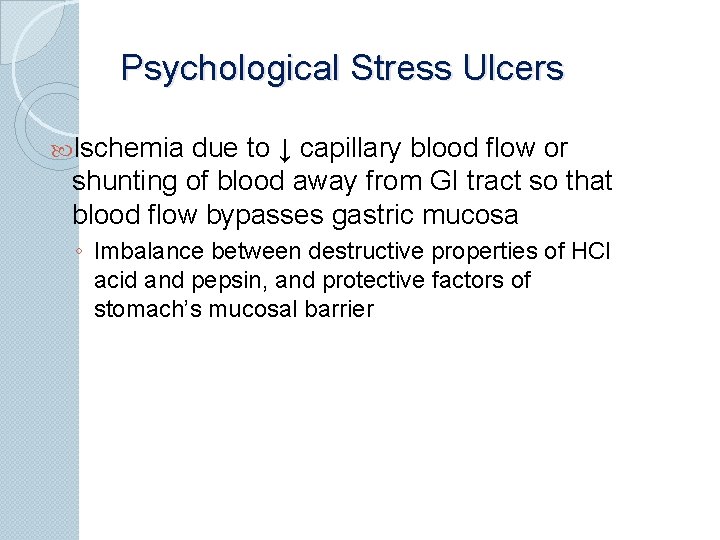
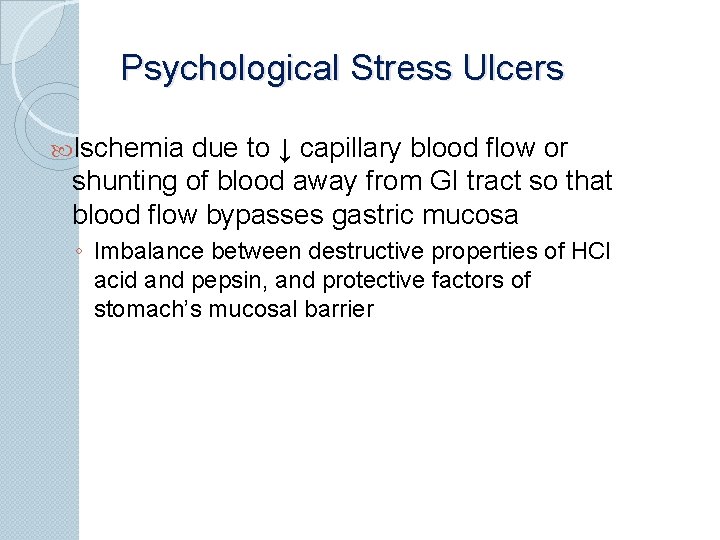
Psychological Stress Ulcers Ischemia due to ↓ capillary blood flow or shunting of blood away from GI tract so that blood flow bypasses gastric mucosa ◦ Imbalance between destructive properties of HCl acid and pepsin, and protective factors of stomach’s mucosal barrier
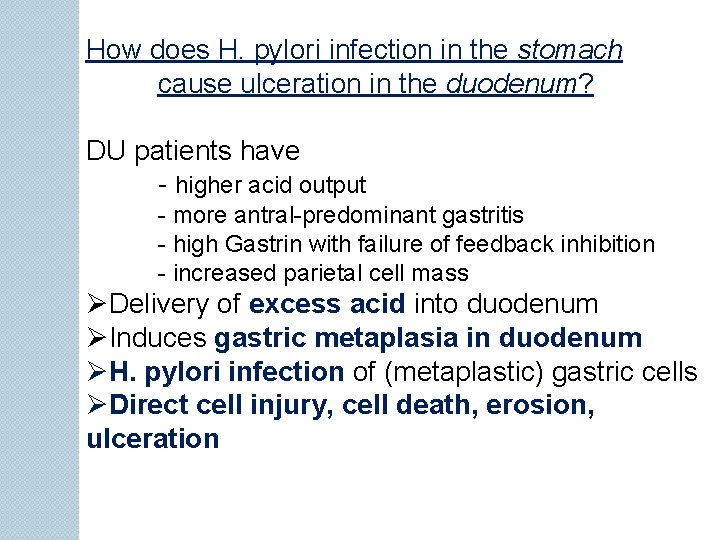
How does H. pylori infection in the stomach cause ulceration in the duodenum? DU patients have - higher acid output - more antral-predominant gastritis - high Gastrin with failure of feedback inhibition - increased parietal cell mass ØDelivery of excess acid into duodenum ØInduces gastric metaplasia in duodenum ØH. pylori infection of (metaplastic) gastric cells ØDirect cell injury, cell death, erosion, ulceration
Peptic ulcer disease Complications Bleeding: chronic low level -> anaemia Massive acute bleeding Perforation Scarring -> obctruction Penetration -> pancreatitis
Bleeding from ulcers can be fatal. Upper gastrointestinal tract bleeding implies a significant loss of blood into the lumen of the foregut. Haematemesis and melaena demonstrate such a bleeding. Haematemesis is defined as vomiting of whole blood or blood clots. Melaena is defined as passage of dark tarry stools (coal-black, shiny, sticky, and foul smelling).
Therapy The Goal of therapy is eradication of the organism as if this is achieved reinfection rate are low and the benefit of treatment is longterm 2 antimicrobials reduces the selection of resistance Testing for Infection only required if treatment is intended If test for H. pylori positive , use eradication therapy
Pathophysiology of the Pancreas
Disorders Of The Pancreas ØPancreatitis ØCarcinoma of the pancreas ØTumours of the islets Acute Pancreatitis Inflammation of the pancreas Mortality rate is higher than 20% Found in conjunction with biliary tract disease in more than 50% of patients
Also in conjunction with alcoholism Other causes include: ØPresence of gall stones in pancreatic duct ØReflux of bile into gland ØInfectious microorganisms Often haemorrhagic Marked by nausea and vomiting WBC count maybe elevated Pancreatic amylase concentration higher in blood
Acute pancreatitis Reasons may be: fatty and fried food, alcohol, infections, and problems with pancreatic secret passage (obturation). Pathogenesis: Inflammation proteolytic enzymes activation increasing of pancreatic juice pressure pain systemic vasodilatation pancreatic shock
Pathophysiology of the liver

Blood Supply – 2 sources Hepatic artery: ◦ 500 ml/min of oxygenated blood Portal vein: ◦ 1000 ml/min of partially oxygenated blood ◦ partly oxygenated blood supplies 50 - 60% O 2 plus rich supply of nutrients, toxins, drugs ◦ from stomach, small and large intestines, pancreas and spleen Both empty into capillaries/sinusoids Liver filters the blood Hepatic vein to inferior vena cava

FUNCTIONS OF THE LIVER The liver is one of the most versatile and active organs in the body. Ø It produces bile; Primary role in anabolism and catabolism: Ø metabolizes hormones and drugs; Ø synthesizes proteins, glucose, and clotting factors; Ø stores vitamins and minerals; Ø changes ammonia produced by deamination of amino acids to urea; Ø and converts fatty acids to ketones.
Ø The liver degrades excess nutrients and converts them into substances essential to the body (Function of detoxication). Ø It builds carbohydrates from proteins, Ø converts sugars to fats that can be stored, Ø interchanges chemical groups on amino acids so that they can be used for a number of purposes. Ø In its capacity for metabolizing drugs and hormones, the liver serves as an excretory organ.
BILE PRODUCTION Ø The secretion of bile is essential for digestion of dietary fats and absorption of fats and fat-soluble vitamins from the intestine. Ø The liver produces approximately 600 to 1200 m. L of yellow-green bile daily. Ø Bile contains water, bile salts, bilirubin, cholesterol, and certain products of organic metabolism. Of these, only bile salts, which are formed from cholesterol, are important in digestion.
BILIRUBIN ELIMINATION Bilirubin is the substance that gives bile its color. It is formed from senescent red blood cells. In the process of degradation the hemoglobin from the red blood cell is broken down to form biliverdin, which is rapidly converted to free bilirubin. Free bilirubin, which is insoluble in plasma, transported in the blood attached to plasma albumin.

Inside the hepatocytes, free bilirubin is converted to conjugated bilirubin, making it soluble in bile. Conjugated bilirubin is secreted as a constituent of bile, and in this form it passes through the bile ducts into the small intestine. In the intestine, approximately one half of the bilirubin is converted into a highly soluble substance called stercobilinogen by the intestinal flora.

Urobilinogen is either absorbed into the portal circulation or excreted in the feces. Most of the urobilinogen that is absorbed is returned to the liver to be reexcreted into the bile. A small amount of urobilinogen, approximately 5%, is absorbed into the general circulation and then excreted by the kidneys.

Usually, only a small amount of bilirubin is found in the blood; the normal level of total serum bilirubin is 0. 1 to 1. 2 mg/d. L. Laboratory measurements of bilirubin usually measure the free and the conjugated bilirubin as well as the total bilirubin. These are reported as the direct (conjugated) bilirubin and the indirect (unconjugated or free) bilirubin.
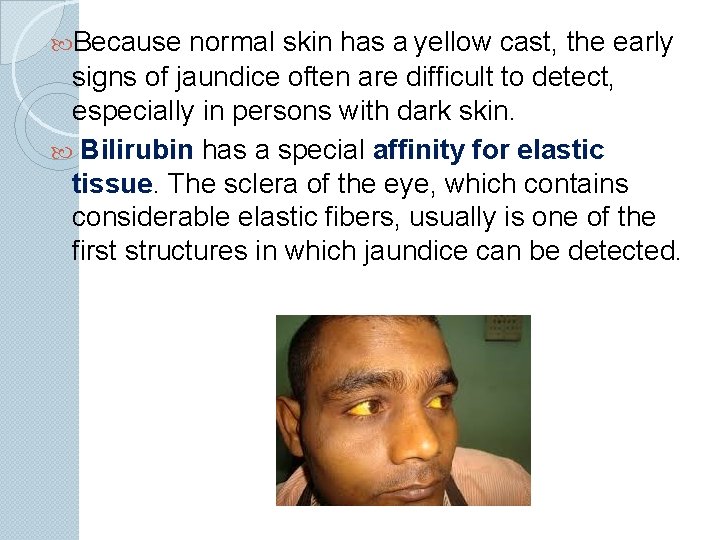
jaundice Jaundice (i. e. , icterus) results from an abnormally high accumulation of bilirubin in the blood, as a result of which there is a yellowish discoloration to the skin and deep tissues. Jaundice becomes evident when the serum bilirubin levels rise above 2. 0 to 2. 5 mg/d. L.
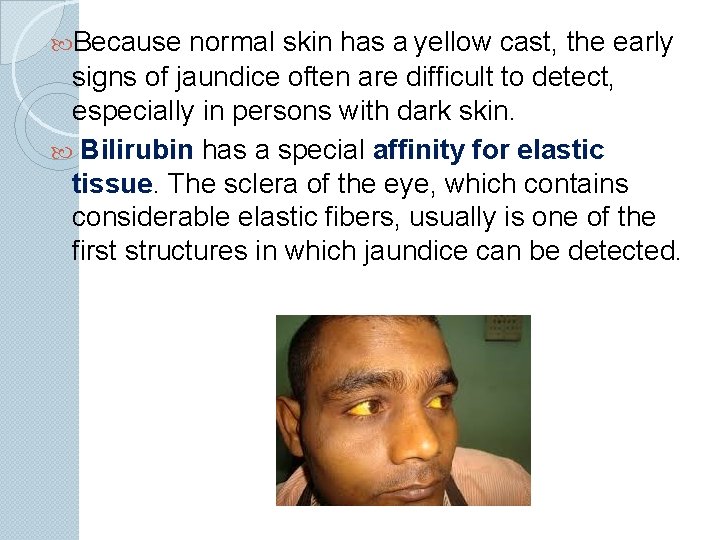
Because normal skin has a yellow cast, the early signs of jaundice often are difficult to detect, especially in persons with dark skin. Bilirubin has a special affinity for elastic tissue. The sclera of the eye, which contains considerable elastic fibers, usually is one of the first structures in which jaundice can be detected.
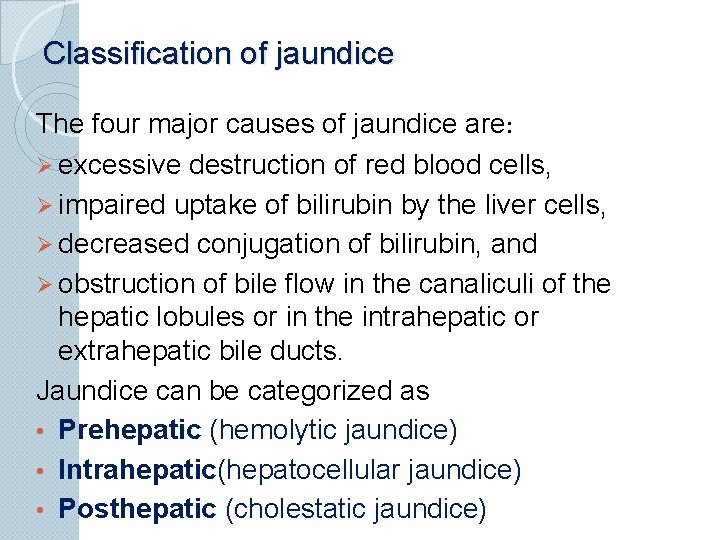
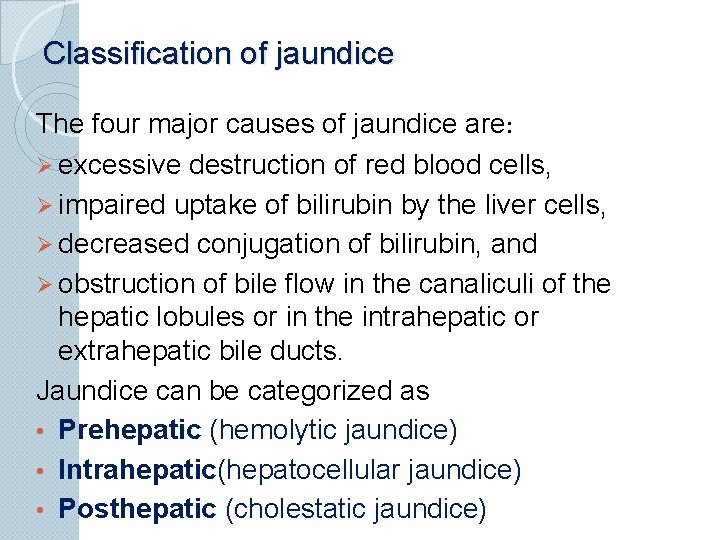
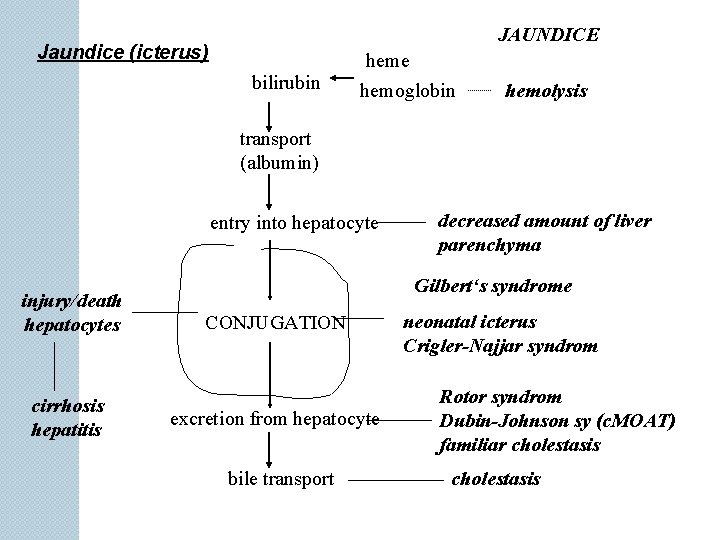
Classification of jaundice The four major causes of jaundice are: Ø excessive destruction of red blood cells, Ø impaired uptake of bilirubin by the liver cells, Ø decreased conjugation of bilirubin, and Ø obstruction of bile flow in the canaliculi of the hepatic lobules or in the intrahepatic or extrahepatic bile ducts. Jaundice can be categorized as • Prehepatic (hemolytic jaundice) • Intrahepatic(hepatocellular jaundice) • Posthepatic (cholestatic jaundice)
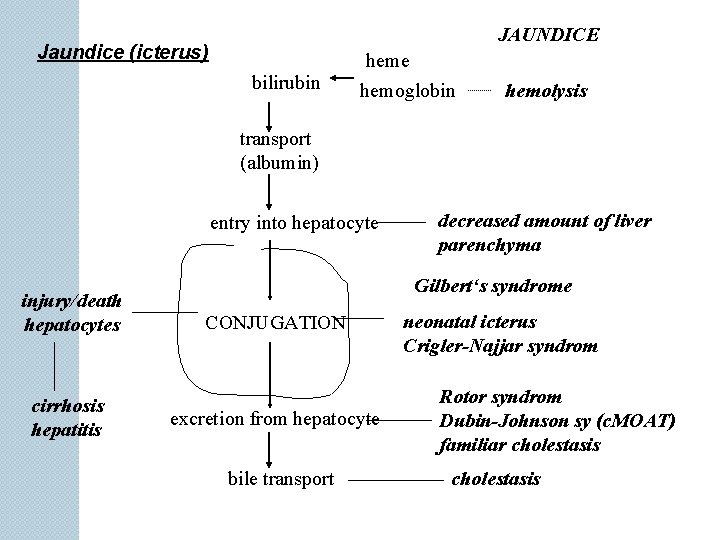
JAUNDICE Jaundice (icterus) bilirubin heme hemoglobin hemolysis transport (albumin) entry into hepatocyte injury/death hepatocytes cirrhosis hepatitis decreased amount of liver parenchyma Gilbert‘s syndrome CONJUGATION excretion from hepatocyte bile transport neonatal icterus Crigler-Najjar syndrom Rotor syndrom Dubin-Johnson sy (c. MOAT) familiar cholestasis
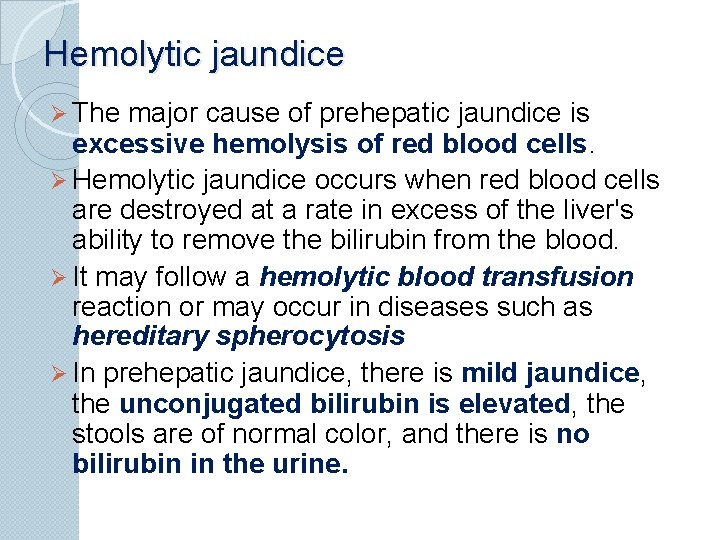
Hemolytic jaundice Ø The major cause of prehepatic jaundice is excessive hemolysis of red blood cells. Ø Hemolytic jaundice occurs when red blood cells are destroyed at a rate in excess of the liver's ability to remove the bilirubin from the blood. Ø It may follow a hemolytic blood transfusion reaction or may occur in diseases such as hereditary spherocytosis Ø In prehepatic jaundice, there is mild jaundice, the unconjugated bilirubin is elevated, the stools are of normal color, and there is no bilirubin in the urine.
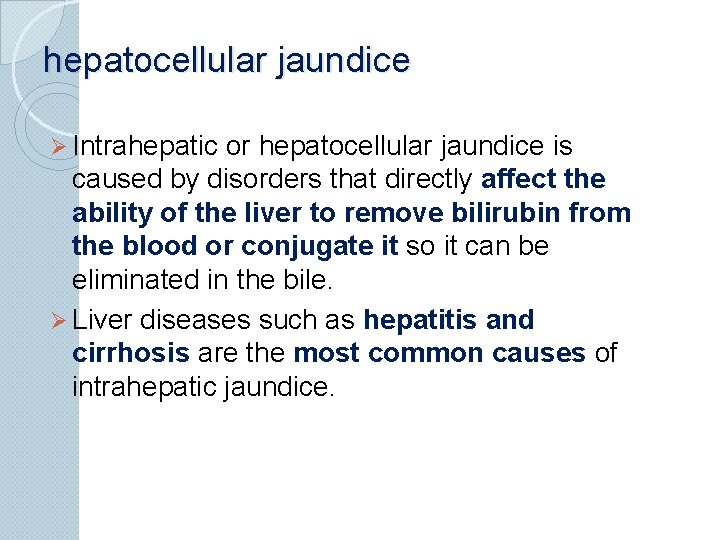
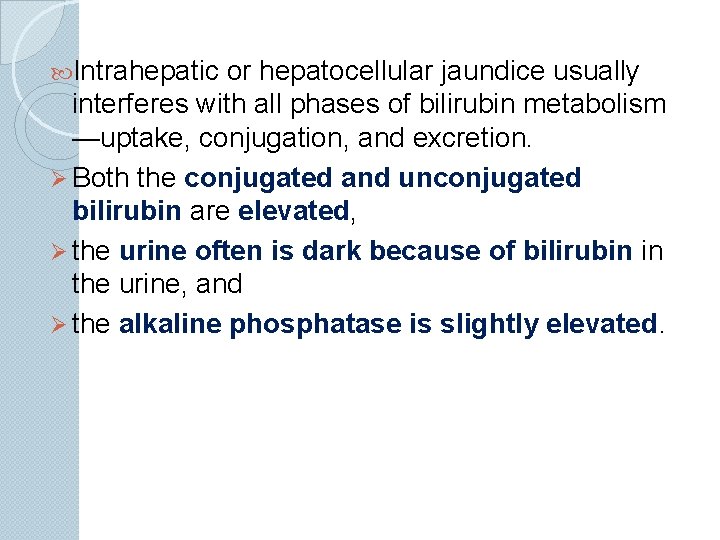
hepatocellular jaundice Ø Intrahepatic or hepatocellular jaundice is caused by disorders that directly affect the ability of the liver to remove bilirubin from the blood or conjugate it so it can be eliminated in the bile. Ø Liver diseases such as hepatitis and cirrhosis are the most common causes of intrahepatic jaundice.
Intrahepatic or hepatocellular jaundice usually interferes with all phases of bilirubin metabolism —uptake, conjugation, and excretion. Ø Both the conjugated and unconjugated bilirubin are elevated, Ø the urine often is dark because of bilirubin in the urine, and Ø the alkaline phosphatase is slightly elevated.
cholestatic jaundice Posthepatic or obstructive jaundice, also called cholestatic jaundice, occurs when bile flow is obstructed between the liver and the intestine, with the obstruction located at any point between the junction of the right or left hepatic duct and the point where the bile duct opens into the intestine. Among the causes are: Ø strictures of the bile duct, Ø gallstones, and Ø tumors of the bile duct or the pancreas.
Ø Conjugated bilirubin levels usually are elevated; Ø the stools are clay colored because of the lack of bilirubin in the bile; Ø the urine is dark; Ø the levels of serum alkaline phosphatase are markedly elevated; Ø the aminotransferase levels are slightly increased.
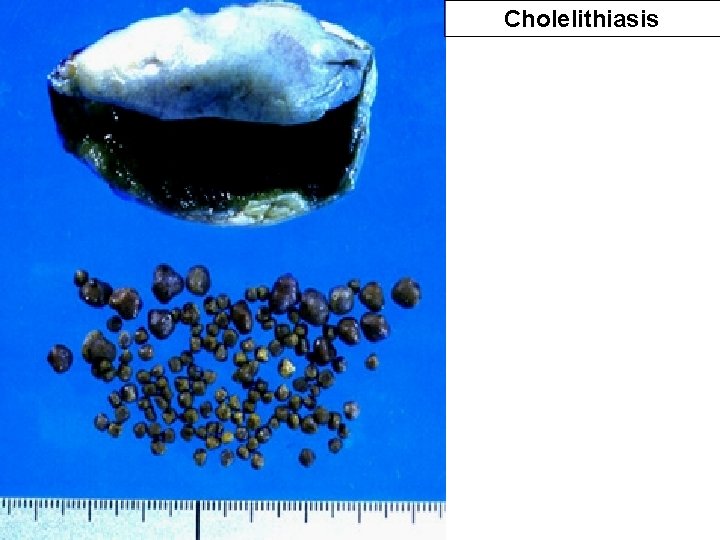
Cholelithiasis or gallstone disease
Cholelithiasis or gallstone disease is defined as a condition with gallstones within the lumen of the gallbladder, wether symptoms occur or not. More than 70% are cholesterol stones; the remainder is a so-called brown pigment gallstone composed of Ca 2+ salts of bilirubin, carbonate, cholesterol and phosphate The incidence of cholesterol stones among females is three times higher than among males.

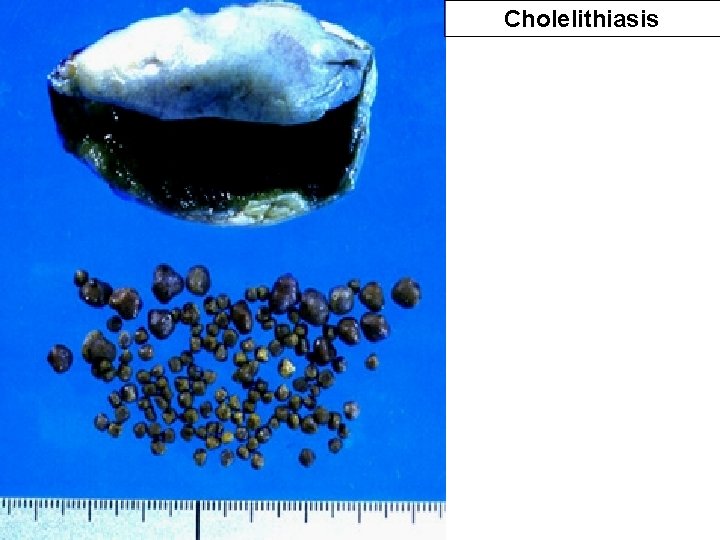
Cholelithiasis

Calcified Gall Stones Can Be Detected On XRays

Image Of A Gall Stone Within The Intrahepatic Bile Duct
Hepatitis
hepatitis Causes of Hepatitis ◦ Most common cause (viral types include A, B, C, D, E, and G) Other possible causes ◦ Drugs (alcohol) drug-induced liver injury is now the leading cause of acute liver failure ◦ Chemicals ◦ Autoimmune liver disease ◦ Bacteria (rarely) ◦ Epstein-Barr, Herpes, Coxsackie virus, Rubella virus
Hepatitis A Mainly by ingestion of food or liquid infected with the virus ◦ ◦ poor hygiene improper handling of food crowded housing poor sanitation conditions Occurs more frequently in underdeveloped countries Contaminated waters ◦ drinking water, contaminated seafood Food-borne Hepatitis A outbreaks usually due to infected food handler
Hepatitis B � Hepatitis B virus (HBV) Transmission of HBV occurs when infected blood or other body fluids enter the body of a person who is not immune to the virus �Perinatally by mothers infected 90% of infants infected, have chronic HBV The younger you are the more likely chronic disease will occur �Percutaneously �Mucosal exposure infectious blood, blood products other body fluids
Hepatitis C ◦ No vaccination available ◦ Transmitted primarily percutaneously Risk Factors �IV drug use �Blood transfusions High-risk sexual behavior Hemodialysis Occupational exposure Sharing personal care items Perinatal transmission Body piercings & tattooing Up to 10% cannot identify the source
Hepatitis D virus (HDV) ◦ Also called delta virus ◦ Defective single-stranded RNA virus ◦ Cannot survive on its own ◦ Requires the helper function of HBV to replicate
Hepatitis E ◦ RNA virus ◦ Transmitted fecal–oral route ◦ Most common contaminated drinking water occurs primarily in developing countries
Hepatitis G ◦ RNA virus ◦ Poorly characterized parenterally & sexually transmitted virus ◦ Can be transmitted by blood transfusion ◦ Coexists with other hepatitis viruses and HIV ◦ Does not appear to cause liver damage by itself
Pathophysiology of Hepatitis �Acute infection- widespread inflammation of liver tissue Liver damage mediated by �Cytotoxic cytokines �Natural killer cells Liver cell damaged results in hepatic cell necrosis With time & no complications �Liver cells will regenerate �Eventually resume their normal appearance & function
There are two mechanisms of liver injury in viral hepatitis: direct cellular injury and induction of immune responses against the viral antigens.
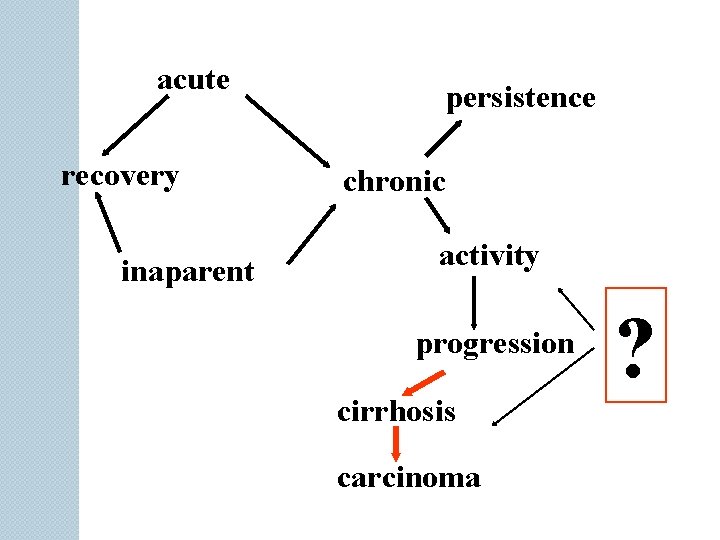
The clinical course of viral hepatitis involves a number of syndromes, including asymptomatic infection with only serologic evidence of disease; acute hepatitis; the carrier state without clinically apparent disease or with chronic hepatitis; chronic hepatitis with or without progression to cirrhosis; or fulminating disease (>1% to 3%) with rapid onset of liver failure.
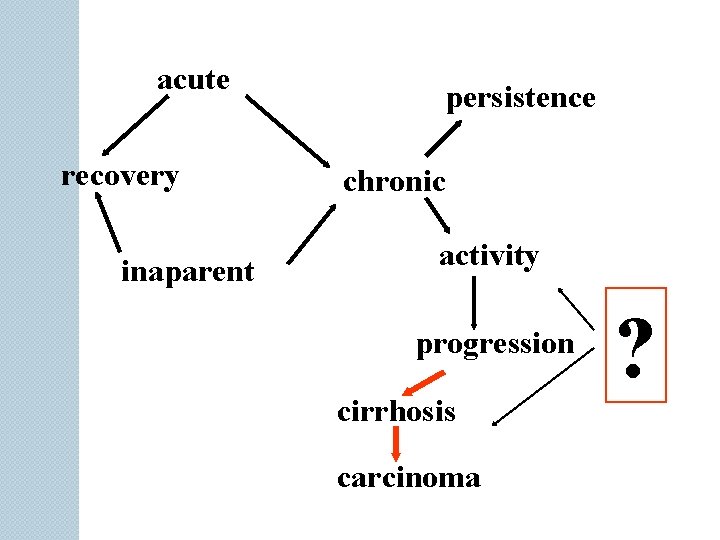
acute recovery inaparent persistence chronic activity progression cirrhosis carcinoma ?
The manifestations of acute hepatitis can be divided into three phases: Øthe prodromal or preicterus period, Øthe convalescent period.
Hepatitis – Clinical Manifestations Preicteric or Prodromal phase Precedes jaundice Lasts 1 – 21 days Maximal infectivity for hepatitis A Symptoms: ü anorexia, ü right upper quadrant pain, ü constipation or diarrhea, ü malaise, ü fever,
Hepatitis – Clinical Manifestations Icteric phase Ø Lasts 2 – 4 weeks Ø characterized by jaundice results when bilirubin diffuses into tissues sometimes accompanied by puritis Ø Symptoms: dark urine, light stools, fatigue, weight loss Posticteric phase Ø Begins as jaundice clears and lasts months Ø Major complaints include Ø Malaise and easy fatigability Ø Relapses may occur
Hepatitis Complications Chronic persistent hepatitis Usually benign with fatigue and hepatomegaly Abnormal LFT’s for several years Chronic active hepatitis Persistent signs and symptoms of hepatitis Fulminant Hepatic Failure Severe liver impairment Liver necrosis with potential liver failure Cirrhosis Hepatocellular Carcinoma
Cirrhosis
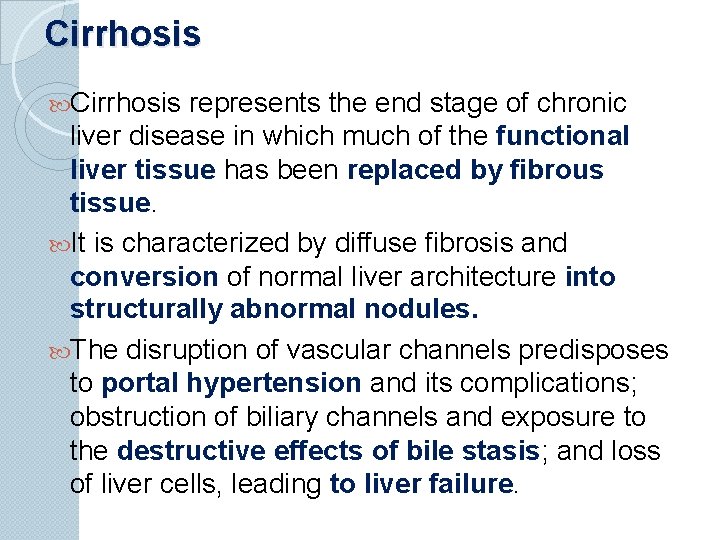
Cirrhosis represents the end stage of chronic liver disease in which much of the functional liver tissue has been replaced by fibrous tissue. It is characterized by diffuse fibrosis and conversion of normal liver architecture into structurally abnormal nodules. The disruption of vascular channels predisposes to portal hypertension and its complications; obstruction of biliary channels and exposure to the destructive effects of bile stasis; and loss of liver cells, leading to liver failure.
Cirrhosis Causes Ø Any chemical or organism that causes liver destruction and irregular regeneration Ø carbon tetrachloride, arsenic, phosphorus Ø Alcohol Etiology Ø Affects more men than women Ø Generally affects ages 40 - 60
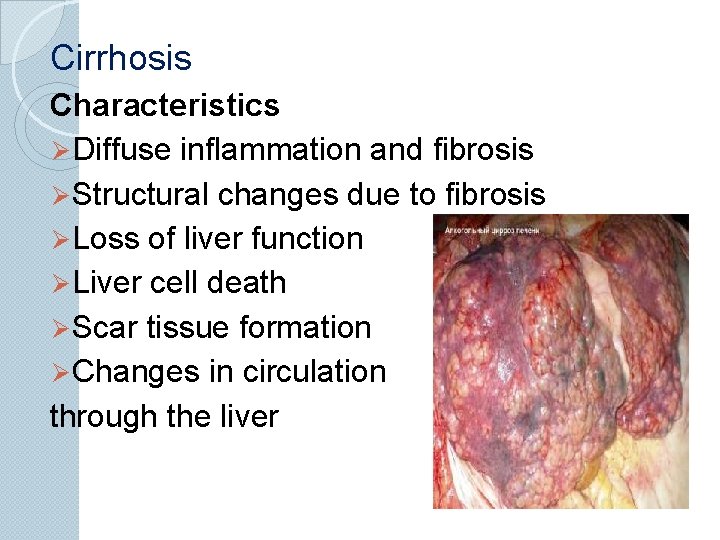
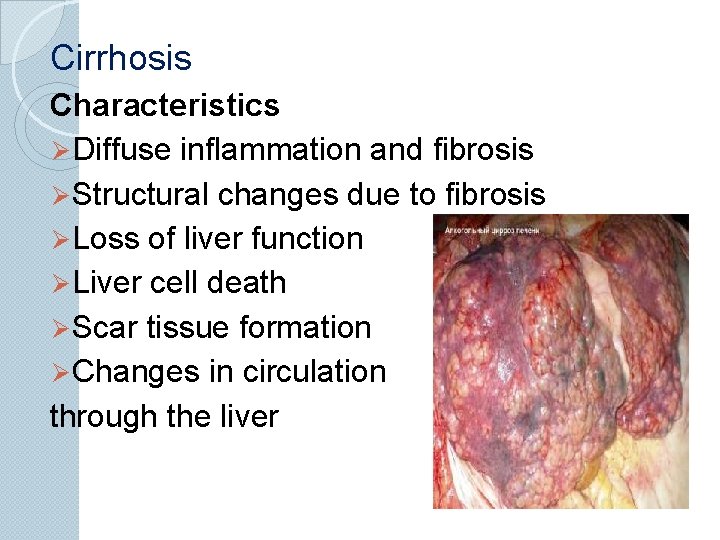
Cirrhosis Characteristics Ø Diffuse inflammation and fibrosis Ø Structural changes due to fibrosis Ø Loss of liver function Ø Liver cell death Ø Scar tissue formation Ø Changes in circulation through the liver
Cirrhosis - Types Laennec’s Ø Alcoholic or nutritional Ø Most common type Ø 50 - 80% are found in chronic alcoholics Ø Insidious with slow progression Ø Faulty nutrition Postnecrotic Ø Post viral (B) hepatitis Ø Intoxication of industrial chemicals Ø Broad bands of scar tissue Biliary Ø Stasis of bile in ducts, immune processes, infection Ø Perilobar scarring Cardiac Ø Severe Rt. sided, long term CHF Ø Constrictive pericarditis Ø Cor pulmonale
Pathophysiology of The Cirrhotic Liver Cirrhosis is final stage of many types of liver injury Appearance of cirrhotic liver varies Early - liver is large and fatty Later - scar tissue forms, liver becomes small and rough Blood flow through liver is compromised Dams up in spleen and G. I. tract Organs become congested and can’t function properly
The late manifestations of cirrhosis are related to portal hypertension and liver cell failure. Splenomegaly, ascites, and portosystemic shunts (i. e. , esophageal varices, anorectal varices, and caput medusae) result from portal hypertension. Other complications include Ø bleeding due to decreased clotting factors, Ø thrombocytopenia due to splenomegaly, Ø gynecomastia in men because of testicular atrophy
Diagnostics Liver function studies ◦ ALT (Alanine aminotransferase) elevates: enzyme in liver cells released into bloodstream with injury or disease ◦ AST (Aspartate aminotransferase) elevates: enzyme in liver & heart cells released into bloodstream ◦ GGT – gamma glutamyltransferase present in all cell membranes, injury or disease elevates in cell lysis increases when bile ducts are blocked & hepatitis elevated until function returns. ◦ Alkaline phosphatase present in liver & bone cells elevated in hepatitis ◦ AFP
![Complications Of Cirrhosis 1 Jaundice Hepatic cells fail to metabolise bilirubin Serum bilirubin levels Complications Of Cirrhosis [1] Jaundice Hepatic cells fail to metabolise bilirubin Serum bilirubin levels](https://slidetodoc.com/presentation_image_h/272abfe0e45b37b30c4a5f86d21f0a67/image-122.jpg)
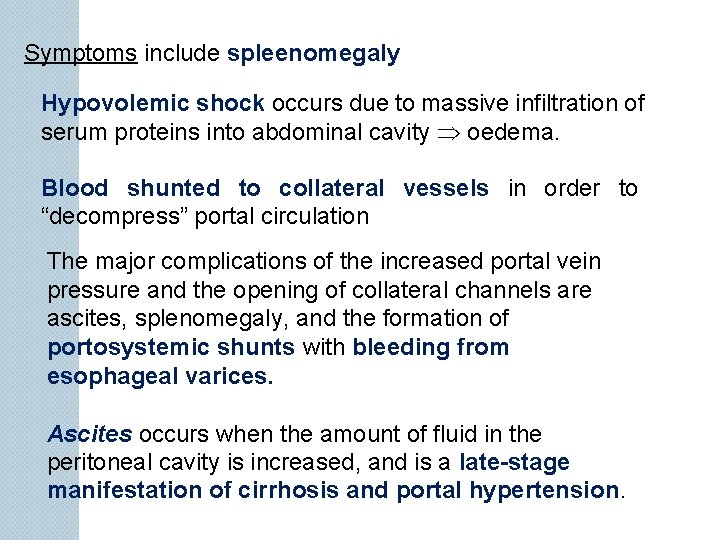
Complications Of Cirrhosis [1] Jaundice Hepatic cells fail to metabolise bilirubin Serum bilirubin levels increase Bilirubin is bound to albumin localized oedema [2] Portal Hypertension a) Prehepatic b) Intrahepatic c) Posthepatic
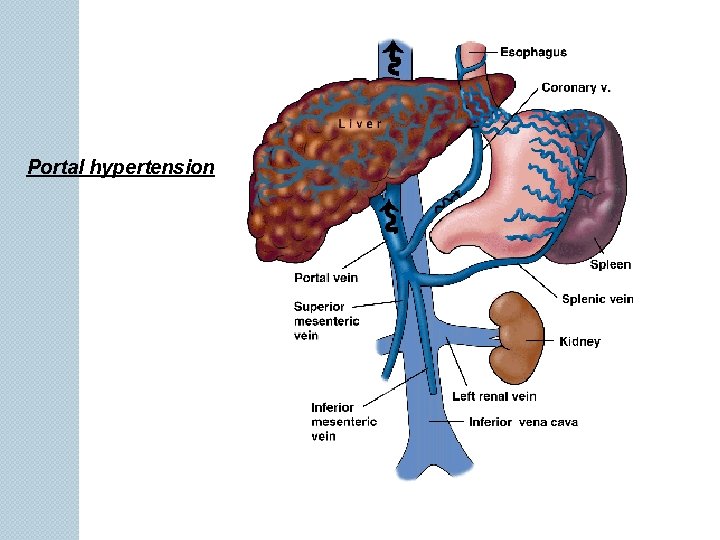
Portal Hypertension Ø is characterized by increased resistance to flow in the portal venous system and sustained portal vein pressure above 12 mm Hg (normal, 5 to 10 mm Hg) Ø Portal hypertension can be caused by a variety of conditions that increase resistance to hepatic blood flow, including pre-hepatic, posthepatic, and intrahepatic obstructions
a) Prehepatic Due to portal vein thrombosis b) Intrahepatic Congenital hepatic fibrosis Non-cirrhotic portal hypertension Hyperplastic liver c) Posthepatic Occlusion of hepatic vein (Dudd-Chiari Syndrome) Renal tumours
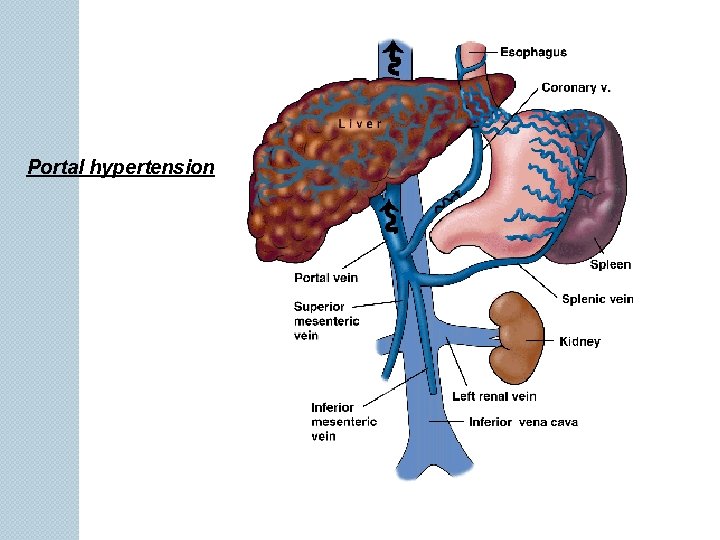
Portal hypertension
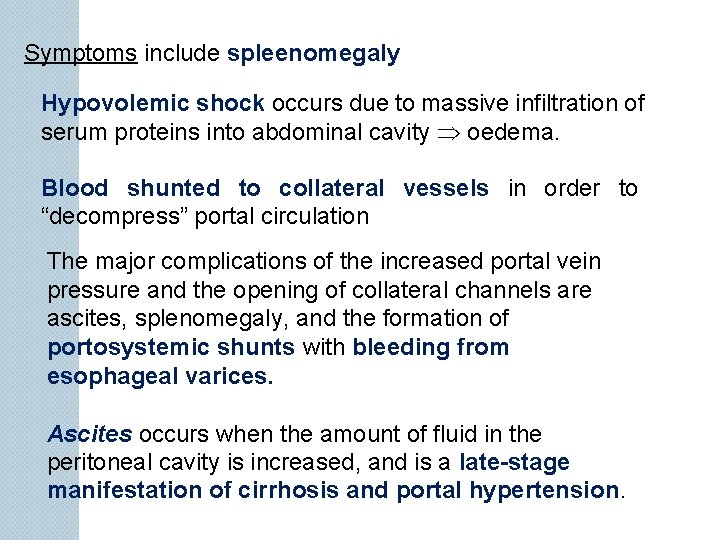
Symptoms include spleenomegaly Hypovolemic shock occurs due to massive infiltration of serum proteins into abdominal cavity oedema. Blood shunted to collateral vessels in order to “decompress” portal circulation The major complications of the increased portal vein pressure and the opening of collateral channels are ascites, splenomegaly, and the formation of portosystemic shunts with bleeding from esophageal varices. Ascites occurs when the amount of fluid in the peritoneal cavity is increased, and is a late-stage manifestation of cirrhosis and portal hypertension.
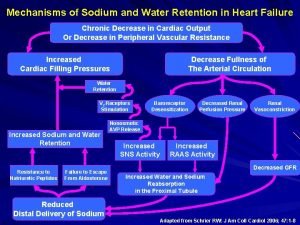
Ascites Fluid accumulation in the peritoneal cavity Due to: Portal hypertension causing increased plasma and lymphatic hydrostatic pressure Hypoalbuminemia causing decreased oncotic pressure Hyperaldosteronism causing increased Na and water retention
Liver Failure
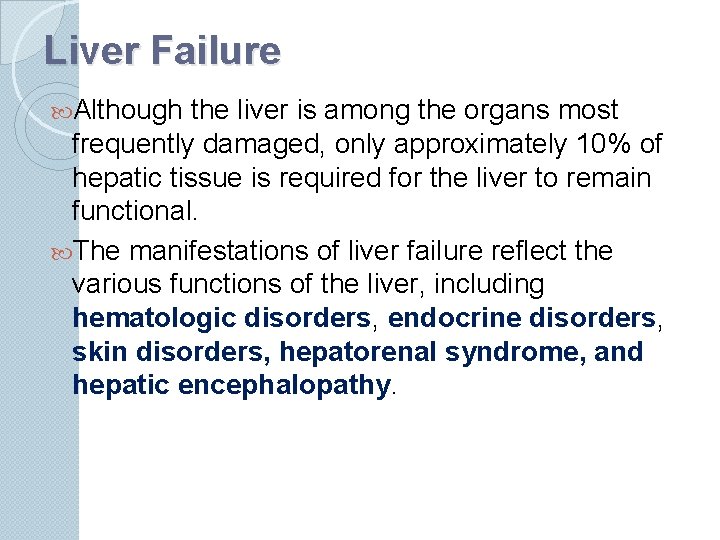
Liver Failure Although the liver is among the organs most frequently damaged, only approximately 10% of hepatic tissue is required for the liver to remain functional. The manifestations of liver failure reflect the various functions of the liver, including hematologic disorders, endocrine disorders, skin disorders, hepatorenal syndrome, and hepatic encephalopathy.

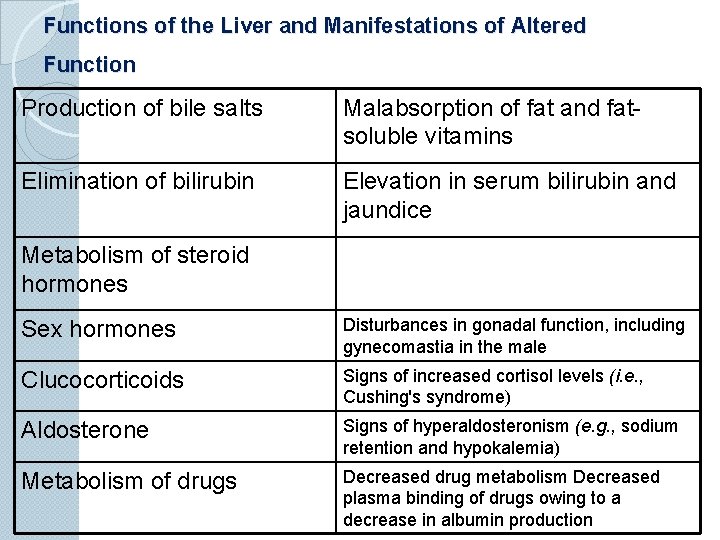
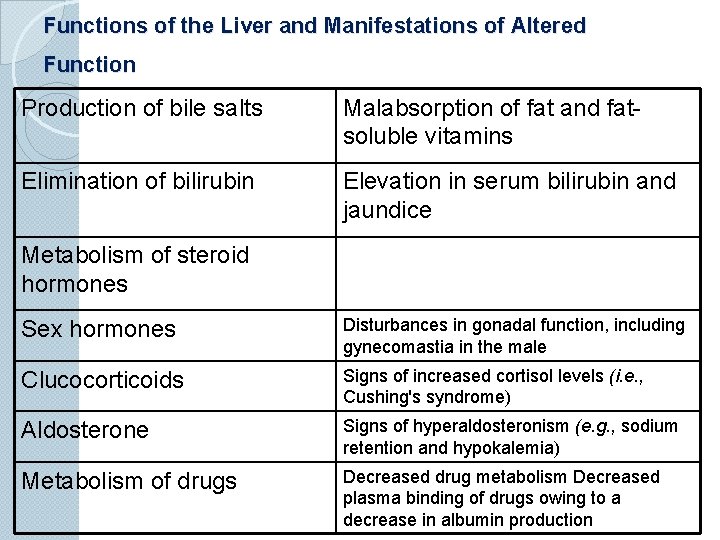
Functions of the Liver and Manifestations of Altered Function Production of bile salts Malabsorption of fat and fatsoluble vitamins Elimination of bilirubin Elevation in serum bilirubin and jaundice Metabolism of steroid hormones Sex hormones Disturbances in gonadal function, including gynecomastia in the male Clucocorticoids Signs of increased cortisol levels (i. e. , Cushing's syndrome) Aldosterone Signs of hyperaldosteronism (e. g. , sodium retention and hypokalemia) Metabolism of drugs Decreased drug metabolism Decreased plasma binding of drugs owing to a decrease in albumin production
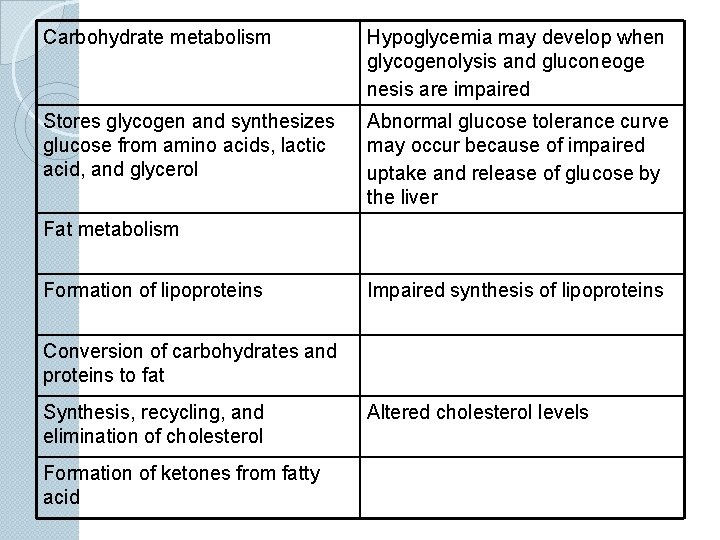
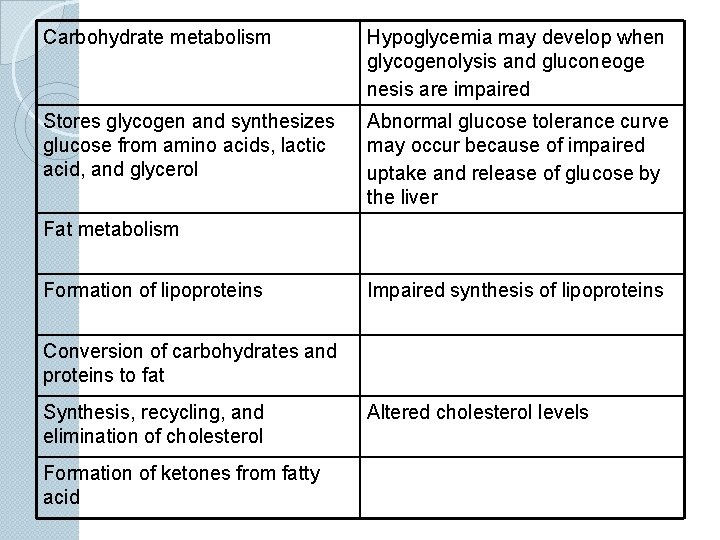
Carbohydrate metabolism Hypoglycemia may develop when glycogenolysis and gluconeoge nesis are impaired Stores glycogen and synthesizes glucose from amino acids, lactic acid, and glycerol Abnormal glucose tolerance curve may occur because of impaired uptake and release of glucose by the liver Fat metabolism Formation of lipoproteins Impaired synthesis of lipoproteins Conversion of carbohydrates and proteins to fat Synthesis, recycling, and elimination of cholesterol Formation of ketones from fatty acid Altered cholesterol levels
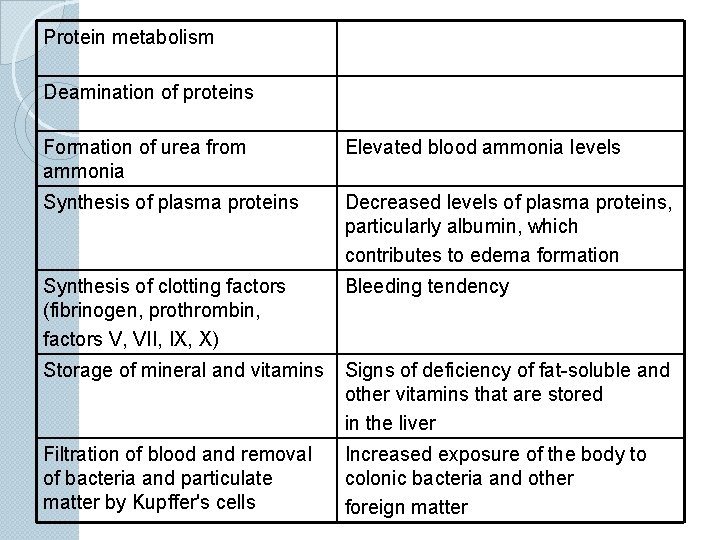
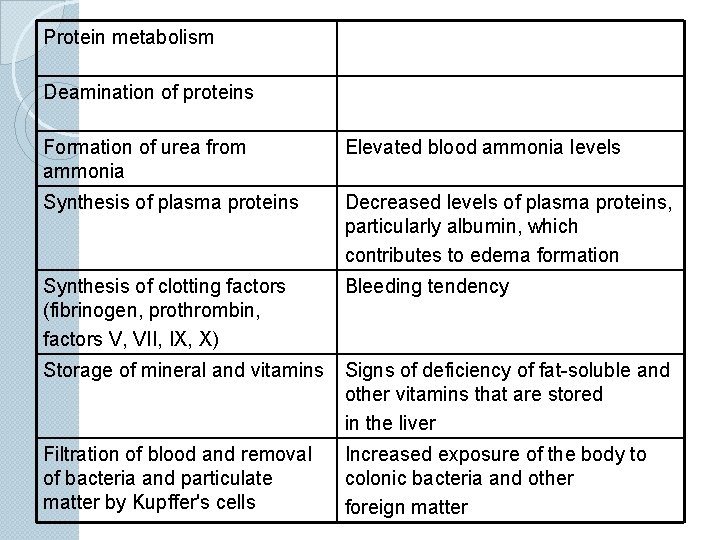
Protein metabolism Deamination of proteins Formation of urea from ammonia Elevated blood ammonia levels Synthesis of plasma proteins Decreased levels of plasma proteins, particularly albumin, which contributes to edema formation Synthesis of clotting factors (fibrinogen, prothrombin, factors V, VII, IX, X) Bleeding tendency Storage of mineral and vitamins Signs of deficiency of fat-soluble and other vitamins that are stored in the liver Filtration of blood and removal of bacteria and particulate matter by Kupffer's cells Increased exposure of the body to colonic bacteria and other foreign matter
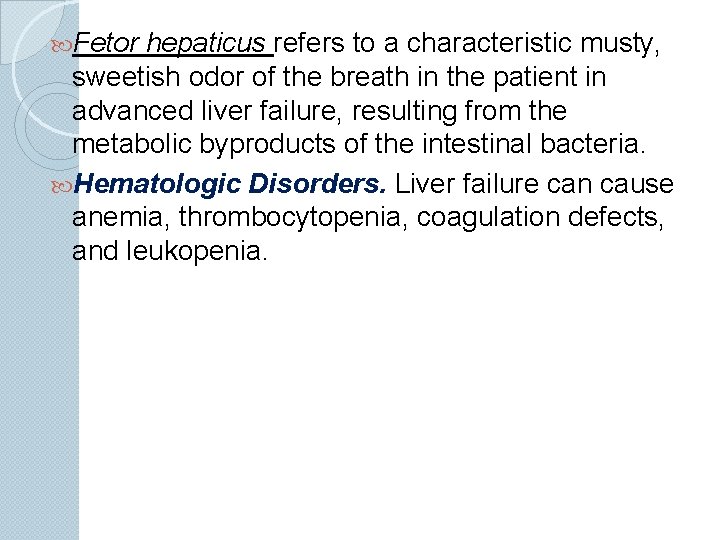
Fetor hepaticus refers to a characteristic musty, sweetish odor of the breath in the patient in advanced liver failure, resulting from the metabolic byproducts of the intestinal bacteria. Hematologic Disorders. Liver failure can cause anemia, thrombocytopenia, coagulation defects, and leukopenia.
Endocrine Disorders The liver metabolizes the sex hormones. Endocrine disorders, particularly disturbanca in gonadal function, are common accompaniments of cirrhosis and liver failure. Women may have menstrual irregularities (usually amenorrhea), loss of libido, and sterility. In men, testosterone levels usually fall, the testicular atrophy, and loss of libido, impotence, and gynecomastia occur. Secondary hyperaldosteronism
Skin Disorders Liver failure brings on numerous skin disorders. These lesions, called variously vascular spiden telangiectases, spider angiomas, and spider nevi, are seen most often in the upper half of the body. They consist of a central pulsating arteriole from which smaller vessels radiate.
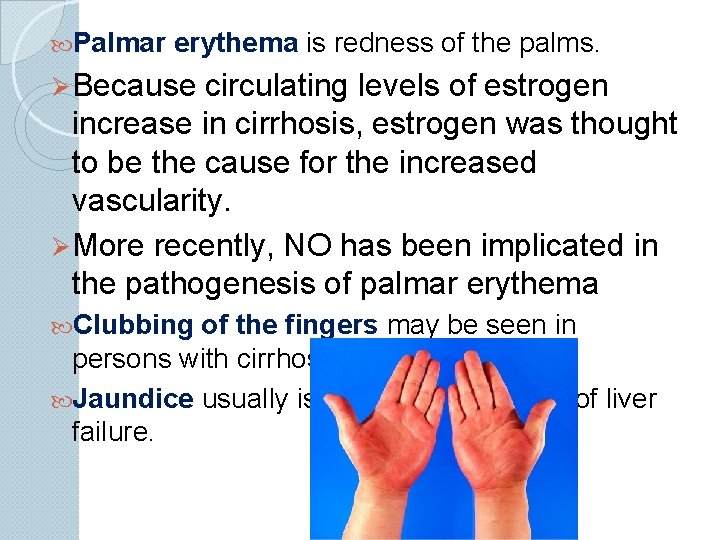
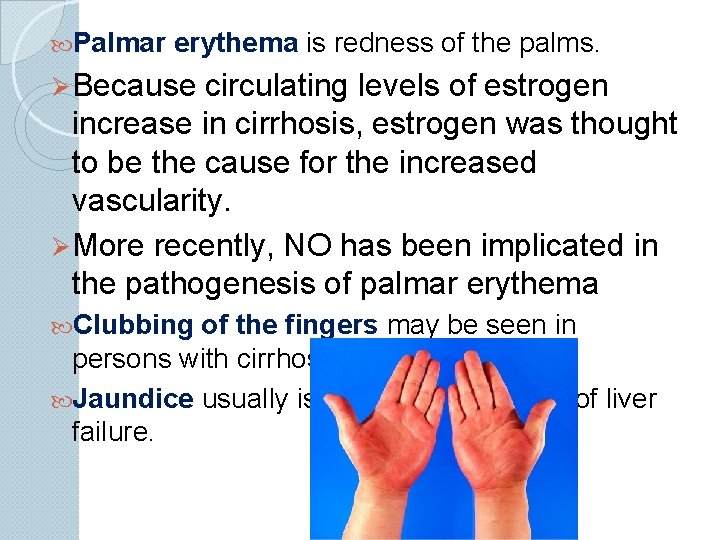
Palmar erythema is redness of the palms. Ø Because circulating levels of estrogen increase in cirrhosis, estrogen was thought to be the cause for the increased vascularity. Ø More recently, NO has been implicated in the pathogenesis of palmar erythema Clubbing of the fingers may be seen in persons with cirrhosis. Jaundice usually is a late manifestation of liver failure.
Hepatorenal Syndrome Ø The hepatorenal syndrome refers to a functional state of renal failure sometimes seen during the terminal stages of liver failure with ascites. l Ø t is characterized by progressive azotemia, increased serum creatinine levels, and oliguria. Ø Ultimately, when renal failure is superimposed on liver failure, azotemia and elevated levels of blood ammonia occur; this condition is thought to contribute to hepatic encephalopathy and coma.
Hepatic Encephalopathy Ø Hepatic encephalopathy refers to the totality of central nervous system manifestations of liver failure. Ø It is characterized by neural disturbances ranging from a lack of mental alertness to confusion, coma, and convulsions. Ø A very early sign of hepatic encephalopathy is a flapping tremor called asterixis.
Hepatic Encephalopathy/coma Signs and symptoms Ø Mental changes Ø Handwriting difficulty Ø Asterixis – liver flap Ø Hyperactive reflexes Ø Fetor hepaticus Ø Coma
 Circularory system
Circularory system Nervous system and digestive system
Nervous system and digestive system Perinephric abscess symptoms
Perinephric abscess symptoms Dumping syndrome pathophysiology
Dumping syndrome pathophysiology Pathophysiology of epistaxis
Pathophysiology of epistaxis Electrocauterization
Electrocauterization Hepatic encephalopathy pathophysiology
Hepatic encephalopathy pathophysiology Thyroglossal cyst pathophysiology
Thyroglossal cyst pathophysiology Hyperthyroidism hypokalemia
Hyperthyroidism hypokalemia Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Paroxysmal nocturnal dyspnea pathophysiology
Paroxysmal nocturnal dyspnea pathophysiology Pathophysiology of jaundice
Pathophysiology of jaundice Cholecystitis pathogenesis
Cholecystitis pathogenesis Nursing interventions for thyroid storm
Nursing interventions for thyroid storm Pathophysiology of sodium and water retention
Pathophysiology of sodium and water retention Taxis maneuver hernia
Taxis maneuver hernia Toxic multinodular goiter
Toxic multinodular goiter Methimasole
Methimasole Pathophysiology of hirschsprung disease
Pathophysiology of hirschsprung disease Hellp syndrome meaning
Hellp syndrome meaning Excessive acid production
Excessive acid production Pathophysiology of hiatal hernia
Pathophysiology of hiatal hernia Pathophysiology of hypovolemic shock
Pathophysiology of hypovolemic shock Pathophysiology of measles
Pathophysiology of measles Disseminated intravascular coagulation pathophysiology
Disseminated intravascular coagulation pathophysiology Jihan nezir
Jihan nezir Cholecystitis pathophysiology
Cholecystitis pathophysiology X ray of asthma patient
X ray of asthma patient Pathology of asthma
Pathology of asthma 3392chest
3392chest What is the pathophysiology of appendicitis?
What is the pathophysiology of appendicitis? Pathophysiology of appendicitis
Pathophysiology of appendicitis Aplastic anemia lab findings
Aplastic anemia lab findings Cyphalic
Cyphalic 4th stage renal failure
4th stage renal failure Pathophysiology of appendicitis
Pathophysiology of appendicitis Case mysteries in pathophysiology (doc or html) file
Case mysteries in pathophysiology (doc or html) file Preductal vs postductal
Preductal vs postductal Cerebral salt wasting
Cerebral salt wasting Asthma pathophysiology
Asthma pathophysiology Asthma pathophysiology
Asthma pathophysiology Open angle glaucoma symptoms
Open angle glaucoma symptoms Interruption of the aortic arch
Interruption of the aortic arch Joffroy sign pathophysiology
Joffroy sign pathophysiology Cyanotic vs acyanotic
Cyanotic vs acyanotic Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Site:slidetodoc.com
Site:slidetodoc.com Pathophysiology type 1 diabetes
Pathophysiology type 1 diabetes Valsalva maneuver
Valsalva maneuver Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Hyperkalemia pathophysiology
Hyperkalemia pathophysiology Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Pathophysiology ankylosing spondylitis
Pathophysiology ankylosing spondylitis Burn injury pathophysiology of burns
Burn injury pathophysiology of burns Mitral facies vs malar flush
Mitral facies vs malar flush Tanda ruptur bulbi
Tanda ruptur bulbi Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Examples of pathophysiology
Examples of pathophysiology Nursing management of chronic pancreatitis
Nursing management of chronic pancreatitis Hhns
Hhns Lund and browder chart formula
Lund and browder chart formula Pathophysiology of asthm
Pathophysiology of asthm Pathophysiology of hemophilia ppt
Pathophysiology of hemophilia ppt Chickenpox pathophysiology
Chickenpox pathophysiology Pathophysiology of otosclerosis in flowchart
Pathophysiology of otosclerosis in flowchart Primary complex in children
Primary complex in children Treatment for hyperthyroidism in pregnancy
Treatment for hyperthyroidism in pregnancy Diarrhea plan a
Diarrhea plan a Ckd stage คือ
Ckd stage คือ Præprandielt
Præprandielt Neurogenic shock
Neurogenic shock Rds pathophysiology
Rds pathophysiology Emphysema
Emphysema Renal vein thrombosis pathophysiology
Renal vein thrombosis pathophysiology Dyslipidemia pathophysiology
Dyslipidemia pathophysiology Reactive arthritis pathophysiology
Reactive arthritis pathophysiology Stages of pneumonia
Stages of pneumonia What is pathophysiology
What is pathophysiology Pain pathophysiology
Pain pathophysiology Nature of pain
Nature of pain Pathophysiology of acute pancreatitis
Pathophysiology of acute pancreatitis Glisson üçgeni
Glisson üçgeni 6 liters of oxygen is what percentage
6 liters of oxygen is what percentage Otosclerosis pathophysiology ppt
Otosclerosis pathophysiology ppt Pathophysiology of tuberculosis flow chart
Pathophysiology of tuberculosis flow chart Nursing management of gastrointestinal disorders
Nursing management of gastrointestinal disorders Learning outcomes nursing
Learning outcomes nursing Pathophysiology of anemia
Pathophysiology of anemia Pathophysiology of migraine slideshare
Pathophysiology of migraine slideshare Pathophysiology of migraine
Pathophysiology of migraine Intestinal obstruction nursing management
Intestinal obstruction nursing management Pathophysiology of syphilis
Pathophysiology of syphilis Pathophysiology of aortic aneurysm ppt
Pathophysiology of aortic aneurysm ppt Atopic dermatitis pathophysiology
Atopic dermatitis pathophysiology Hypothyrodism
Hypothyrodism Morphology of peptic ulcer
Morphology of peptic ulcer Pathophysiology of cholelithiasis ppt
Pathophysiology of cholelithiasis ppt Pathophysiology of cirrhosis of liver
Pathophysiology of cirrhosis of liver Pathophysiology of pulmonary hypertension
Pathophysiology of pulmonary hypertension Uterine bleeding
Uterine bleeding Panacinar and centriacinar emphysema
Panacinar and centriacinar emphysema Homocystinuria
Homocystinuria Heparinq
Heparinq Schizophrenia
Schizophrenia Zuzana 6357
Zuzana 6357 Goat digestive system
Goat digestive system Monogastric
Monogastric What energy transformations take place during digestion
What energy transformations take place during digestion Animal digestive system parts and functions
Animal digestive system parts and functions Ruminant digestion
Ruminant digestion Define ruminant digestive system
Define ruminant digestive system øhuman digestive system
øhuman digestive system Digestive system roller coaster project
Digestive system roller coaster project Digestive system facts
Digestive system facts Animali monogastrici
Animali monogastrici Adventitia vs serosa
Adventitia vs serosa Function of liver and pancreas in digestion
Function of liver and pancreas in digestion Introduction of digestive system
Introduction of digestive system Plicae digestive system
Plicae digestive system Digestive system function
Digestive system function Output of digestive system
Output of digestive system Intestine
Intestine Egestion vs excretion
Egestion vs excretion Make me genius digestive system
Make me genius digestive system Figure 14-1 anatomy and physiology
Figure 14-1 anatomy and physiology Chapter 14 the digestive system and body metabolism
Chapter 14 the digestive system and body metabolism Human digestive system facts
Human digestive system facts M cells
M cells What is this
What is this Circulation in reptiles
Circulation in reptiles Dissected frog diagram
Dissected frog diagram Anthozoa diagram
Anthozoa diagram Earthworm reproduction
Earthworm reproduction Digestive system order
Digestive system order First phylum with complete digestive system
First phylum with complete digestive system Correct order of digestive system
Correct order of digestive system Modified monogastric
Modified monogastric Parapodia in polychaetes
Parapodia in polychaetes Respiratory organs of invertebrates
Respiratory organs of invertebrates