Diffuse lung diseases DR AYSER HAMEED LEC 3

- Slides: 45
Diffuse lung diseases DR. AYSER HAMEED LEC. 3
Diffuse lung diseases. Include two categories: 1. Obstructive lung disorders (airways diseases): Characterized by limitation of airflow usually resulting from an increase of resistance from partial or complete obstruction at any level. 2. Restrictive lung disorders: Characterized by reduced expansion of lung parenchyma accompanied by decreased total lung capacity.
Obstructive pulmonary diseases. 1 - Emphysema. 2 - Chronic bronchitis. 3 - Asthma. 4 - Bronchiectasis. 5 - Cystic fibrosis and Bronchiolitis.
Important note: • Total lung capacity and forced vital capacity (FVC) are either normal or increased. • The hallmark is a decreased expiratory flow rate, usually measured by forced expiratory volume at 1 second (FEV 1). Thus, the ratio of FEV 1 and FVC is characteristically decreased.
ASTHMA: • Asthma is characterized by episodic, reversible bronchospasm resulting from an exaggerated bronchoconstriction response to various stimuli. • The basis of bronchial hyper reactivity is not entirely clear (persistent bronchial inflammation). Clinical Features: • Episodic dyspnea, cough, and wheezing (a soft whistling sound during expiration). • This common disease affects about 5% of adults and 7% to 10% of children.
Classification of asthma: into two major categories: 1. Extrinsic asthma: • Initiated by a type I hypersensitivity reaction. • Induced by exposure to an extrinsic antigen. Three types of extrinsic asthma are recognized: 1. Atopic asthma, 2. Occupational asthma, and 3. Allergic bronchopulmonary aspergillosis.
• Atopic asthma is the most common type of asthma (in the first two decades of life). • There is a positive family history. • Serum Ig. E levels are usually elevated & increase eosinophil count. • CD 4+ T cells is believed to have role in pathogenesis.
2. Intrinsic asthma: • Triggering mechanisms are non immune, could be due to aspirin, pulmonary infections especially viruses, cold, psychological stress, exercise. • No family history of allergic manifestations. • Serum Ig. E levels are normal. • Later in life & can cause status asthmaticus in severe cases.
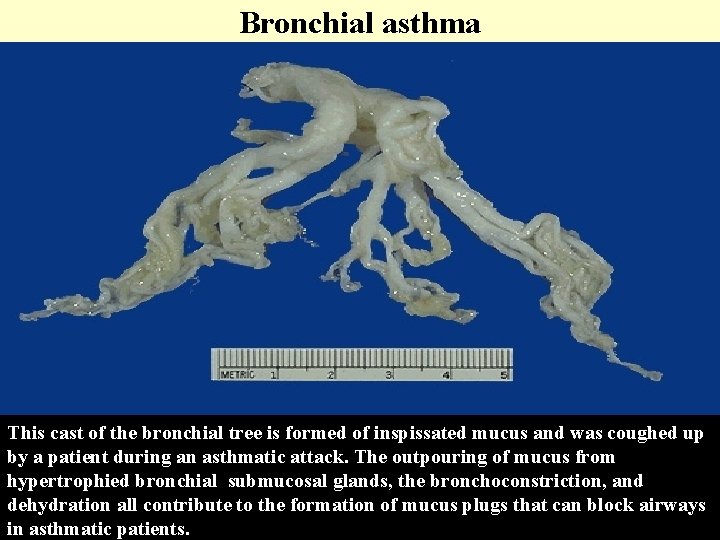
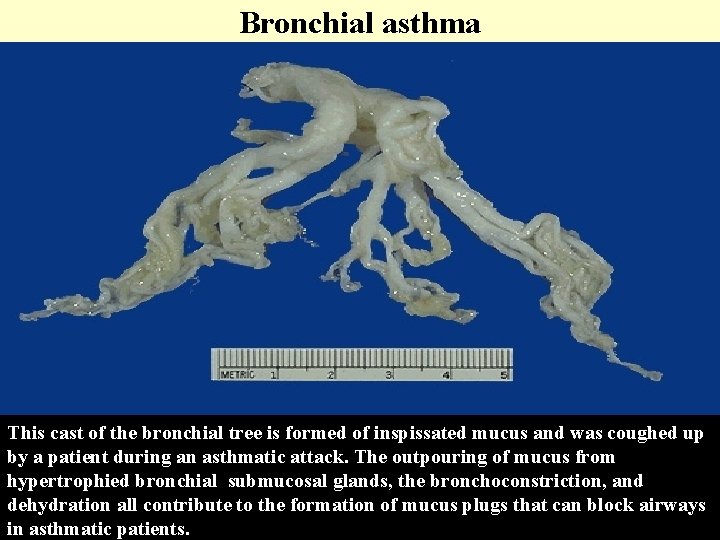
Pathogenesis. • The main underlying pathogenic feature of asthma (all forms of asthma) is airway hyper responsiveness to a variety of stimuli e. g. (histamine)……. . bronchoconstriction. • Hyperresponsiveness is mainly due to bronchial inflammation. Manifested by the presence of inflammatory cells (particularly eosinophil's, lymphocytes, and mast cells), and by damage to the bronchial epithelium.
Details of Pathogenesis of asthma as following: Bronchial inflammation………. . Airways hyper responsiveness (bronchoconstriction) by followings reactions: 1. Sensitization: exposure to allergens ……. . binding of Ig. E to Ig. E receptors on mast cells, less on eosinophils in the airways. 2. Re-exposure to the allergens ……. . degranulation of mast cells………. these cells release preformed mediators that open tight junctions between epithelial cells.
3. Then Antigen can enter the mucosa to activate mucosal mast cells and eosinophils, which, in turn, release additional mediators. 4. These mediators, either directly or via neuronal reflexes, induce bronchospasm, increased vascular permeability, and mucus production or also recruit additional mediator-releasing cells from the blood (within minutes). 5. Late phase: occur after hours, initiated by the accumulated leucocytes from the previous stage.
Intrinsic Asthma. The mechanism of bronchial inflammation and hyper responsiveness is much less clear in patients with intrinsic (non atopic) asthma. Incriminated in such cases are viral infections of the respiratory tract and inhaled air pollutants such as sulfur dioxide, ozone, and nitrogen dioxide. MORPHOLOGY Gross: • Over distended lung (over inflation). • Small areas of atelectasis. • The most striking macroscopic finding is occlusion of bronchi and bronchioles by thick, tenacious mucus plugs.
MIC: characteristic histologic findings in both nonfatal and fatal cases include the followings: 1. Edema, hyperemia, and an inflammatory infiltrate in the bronchial walls, with prominent eosinophils. 2. An increase in size of the submucosal mucous glands. 3. Patchy necrosis and shedding of epithelial cells.
4. Thickened basement membrane. 5. Hypertrophy and hyperplasia of the smooth muscle in the bronchial wall. 6. The mucus plugs contain whorls of shed epithelium (Curschmann spirals). 7. Charcot-Leyden crystals (collections of crystalloids made up of eosinophilic proteins) are also present.
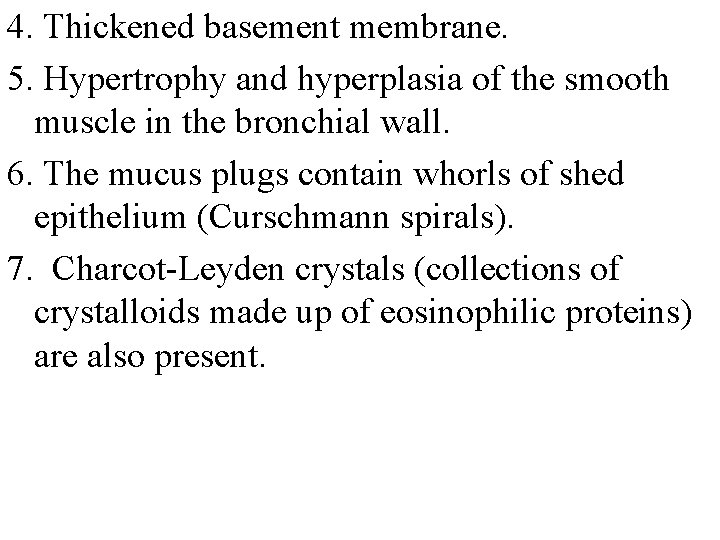
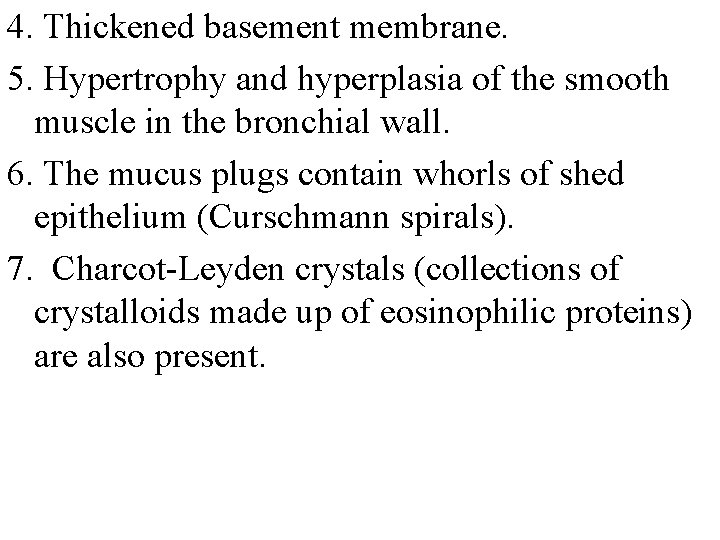
Bronchial asthma This cast of the bronchial tree is formed of inspissated mucus and was coughed up by a patient during an asthmatic attack. The outpouring of mucus from hypertrophied bronchial submucosal glands, the bronchoconstriction, and dehydration all contribute to the formation of mucus plugs that can block airways in asthmatic patients.
Pathogenesis of Asthma
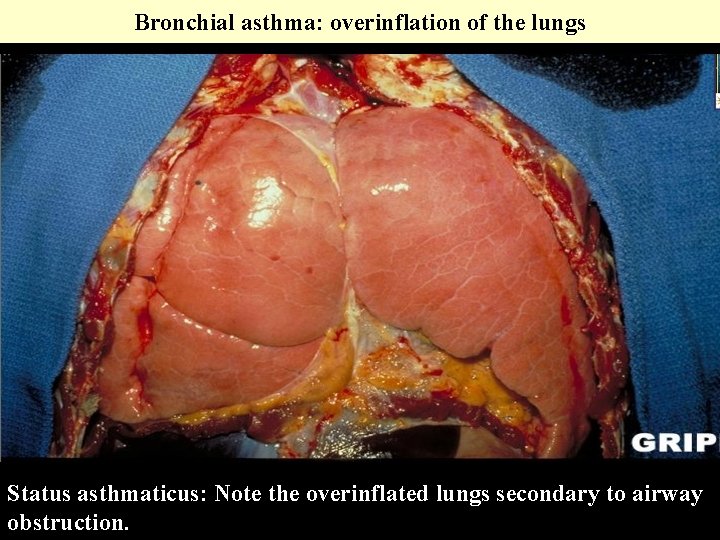
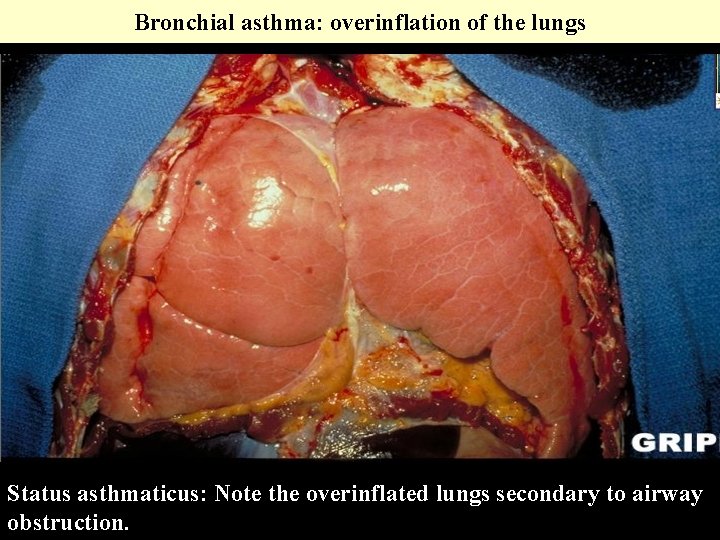
Bronchial asthma: overinflation of the lungs Status asthmaticus: Note the overinflated lungs secondary to airway obstruction.
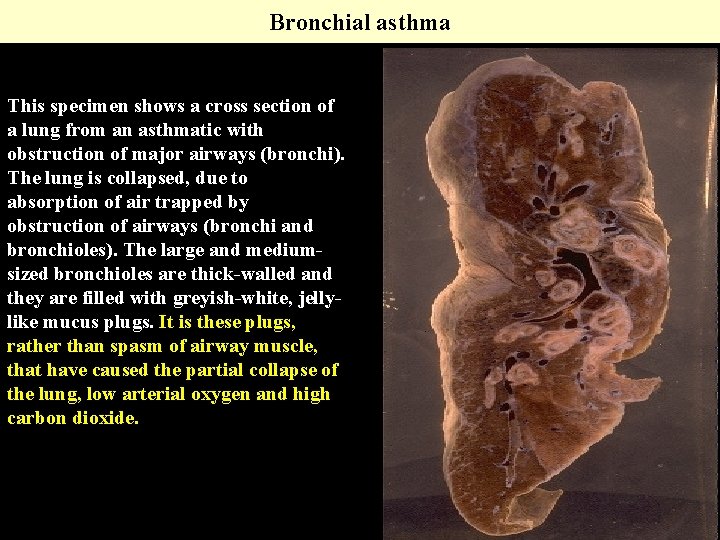
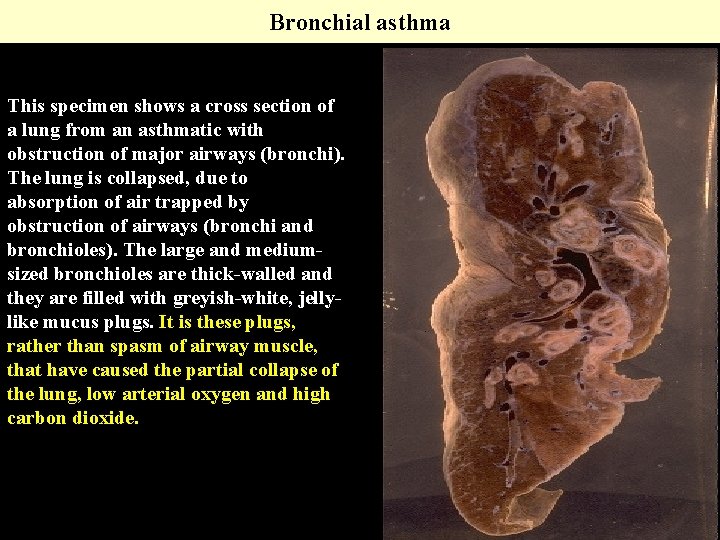
Bronchial asthma This specimen shows a cross section of a lung from an asthmatic with obstruction of major airways (bronchi). The lung is collapsed, due to absorption of air trapped by obstruction of airways (bronchi and bronchioles). The large and mediumsized bronchioles are thick-walled and they are filled with greyish-white, jellylike mucus plugs. It is these plugs, rather than spasm of airway muscle, that have caused the partial collapse of the lung, low arterial oxygen and high carbon dioxide.
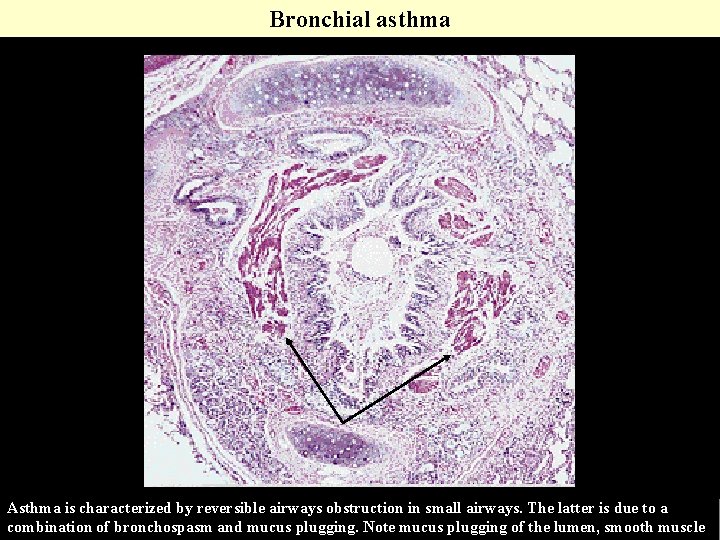
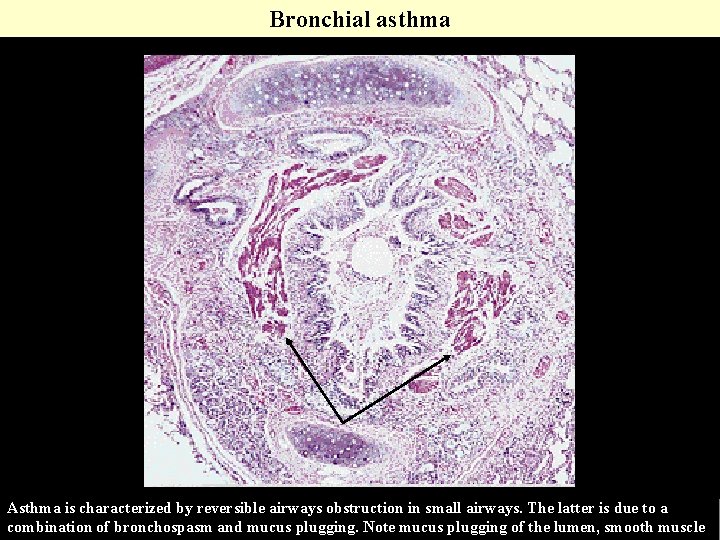
Bronchial asthma Asthma is characterized by reversible airways obstruction in small airways. The latter is due to a combination of bronchospasm and mucus plugging. Note mucus plugging of the lumen, smooth muscle
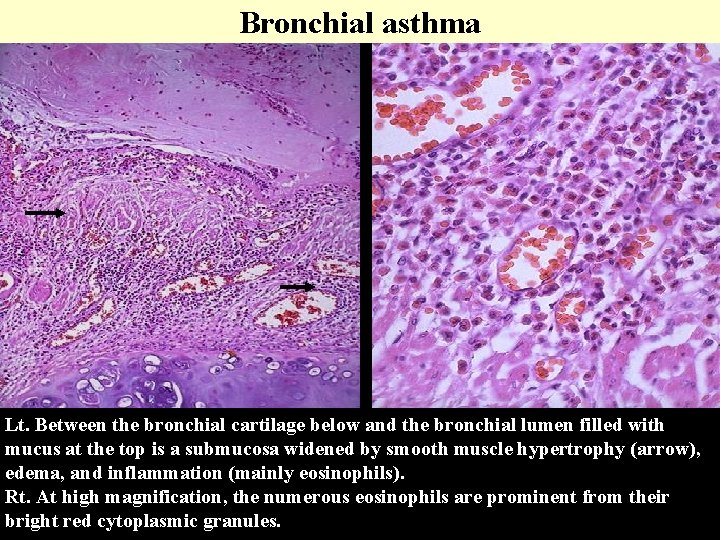
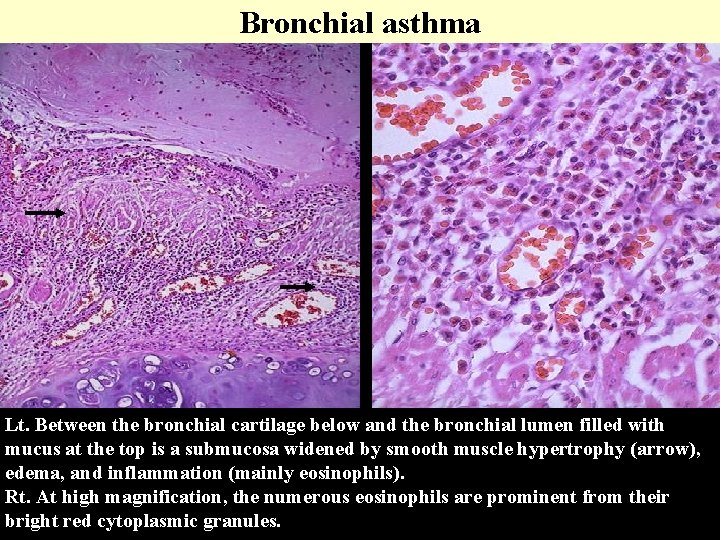
Bronchial asthma Lt. Between the bronchial cartilage below and the bronchial lumen filled with mucus at the top is a submucosa widened by smooth muscle hypertrophy (arrow), edema, and inflammation (mainly eosinophils). Rt. At high magnification, the numerous eosinophils are prominent from their bright red cytoplasmic granules.
Emphysema is characterized by permanent enlargement of the airspaces distal to the terminal bronchioles accompanied by destruction of their walls. Over inflation: enlargement of airspaces is not accompanied by destruction. For example, compensatory over inflation in opposite lung in patient with unilateral pneumonectomy. The relationship between chronic bronchitis and emphysema is complicated. Usually coexist because the major pathogenic mechanism, cigarette smoking, is common to both.
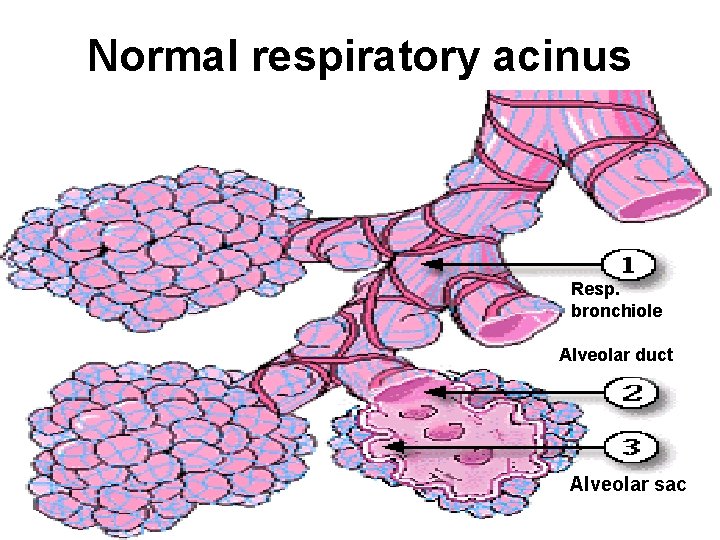
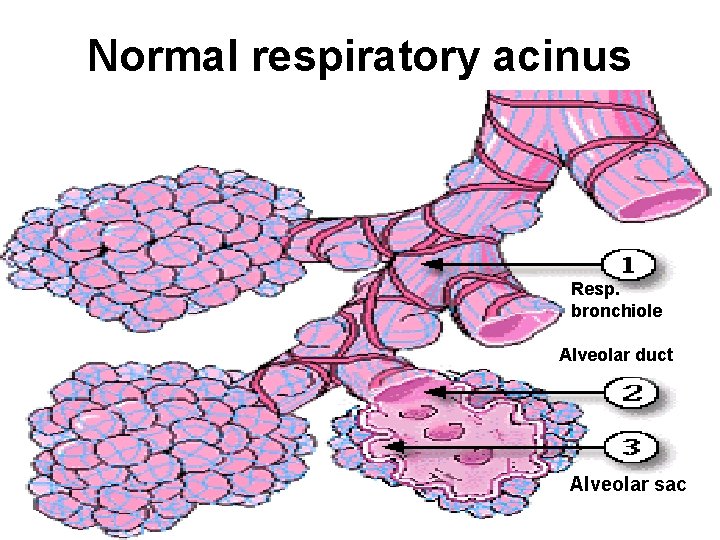
Normal respiratory acinus Resp. bronchiole Alveolar duct Alveolar sac
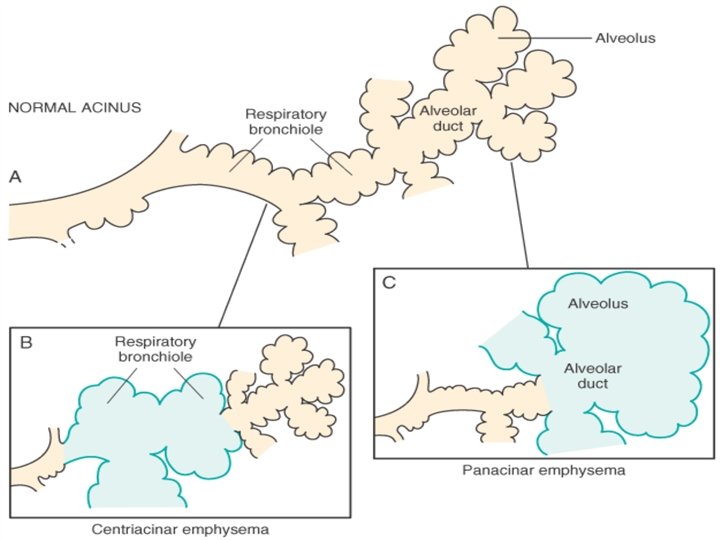
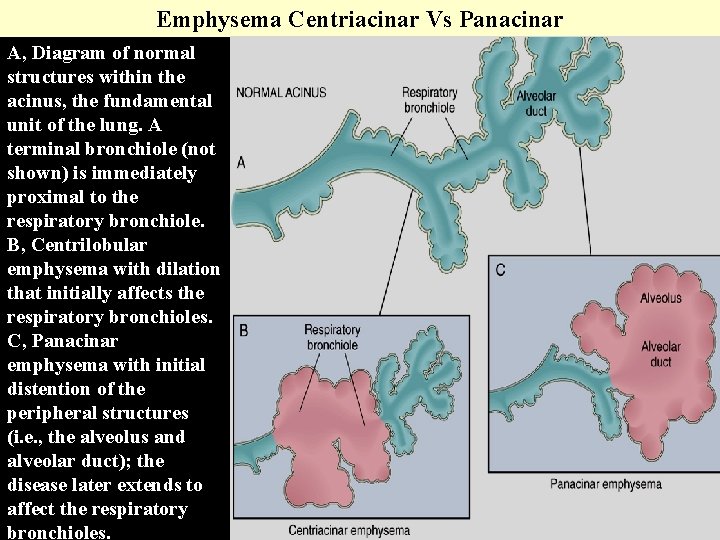
Types of Emphysema: • Classify according to anatomical distribution in the lobule and acinus. • The acinus is the part of the lung distal to the terminal bronchiole and includes the respiratory bronchiole, alveolar ducts, and alveoli; a cluster of three to five acini is referred to as a lobule.
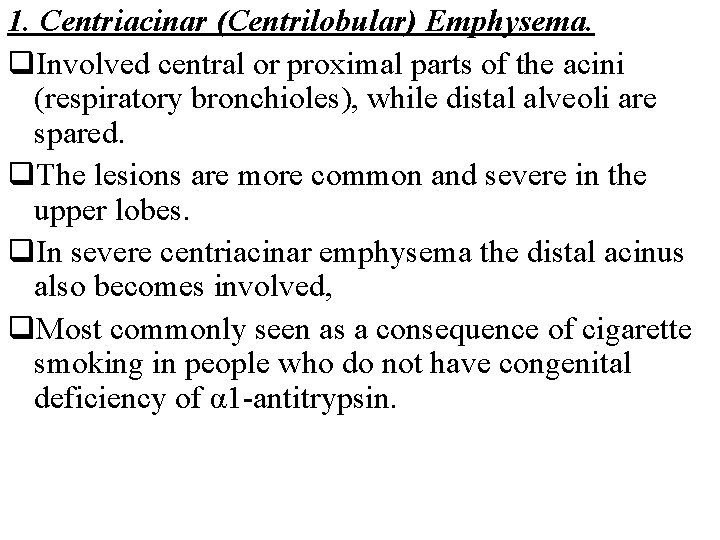
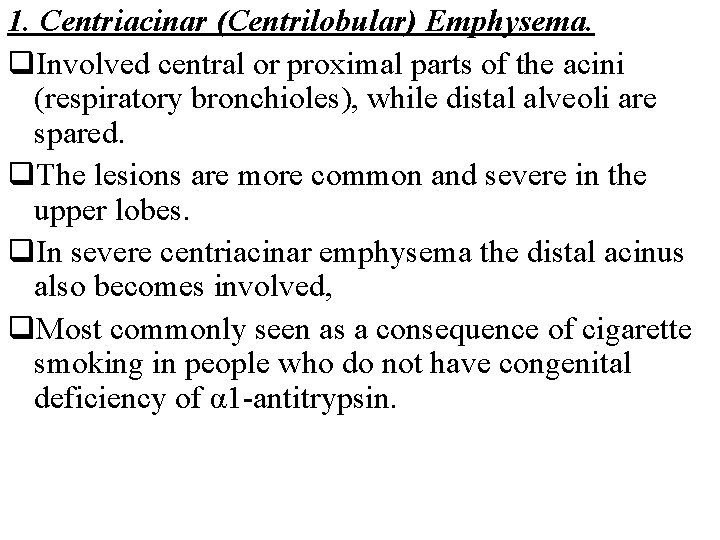
1. Centriacinar (Centrilobular) Emphysema. q. Involved central or proximal parts of the acini (respiratory bronchioles), while distal alveoli are spared. q. The lesions are more common and severe in the upper lobes. q. In severe centriacinar emphysema the distal acinus also becomes involved, q. Most commonly seen as a consequence of cigarette smoking in people who do not have congenital deficiency of α 1 -antitrypsin.
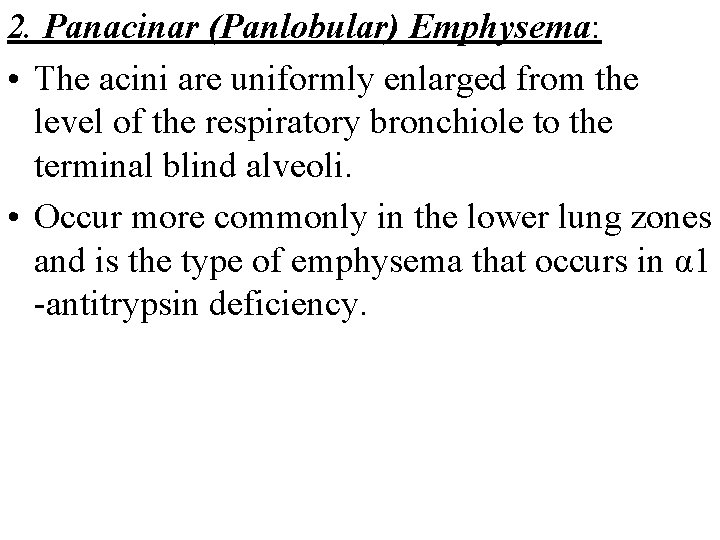
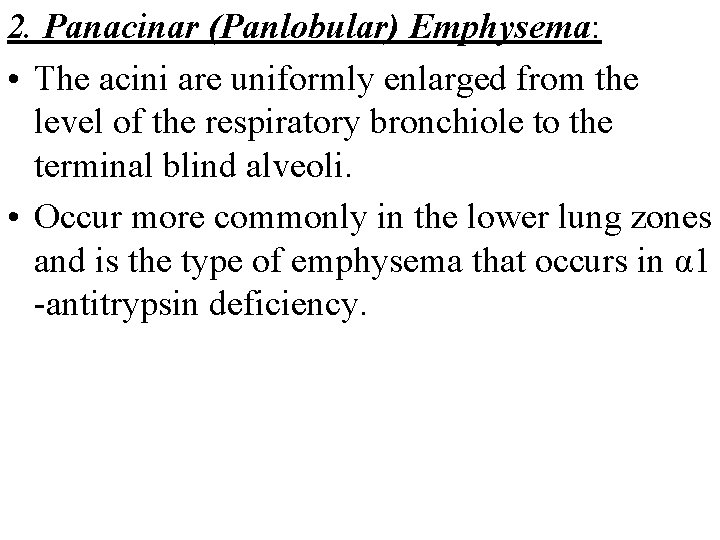
2. Panacinar (Panlobular) Emphysema: • The acini are uniformly enlarged from the level of the respiratory bronchiole to the terminal blind alveoli. • Occur more commonly in the lower lung zones and is the type of emphysema that occurs in α 1 -antitrypsin deficiency.
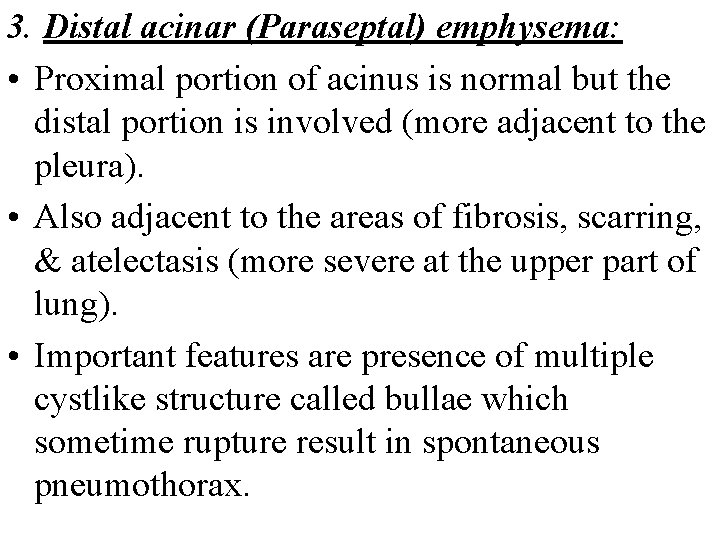
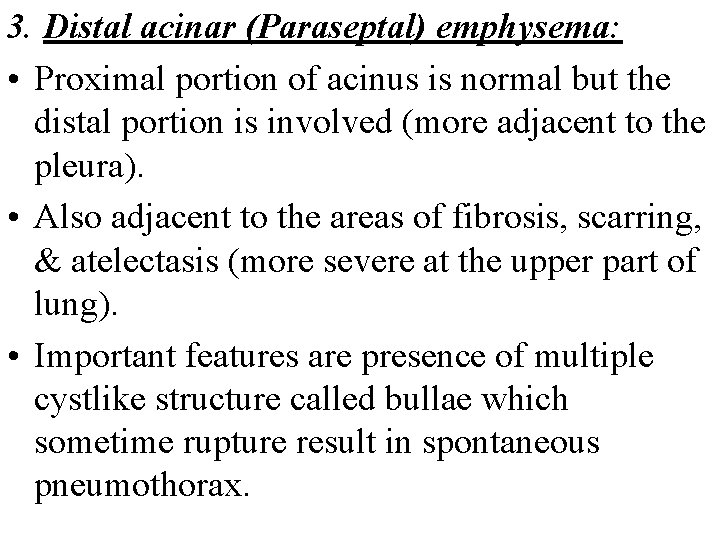
3. Distal acinar (Paraseptal) emphysema: • Proximal portion of acinus is normal but the distal portion is involved (more adjacent to the pleura). • Also adjacent to the areas of fibrosis, scarring, & atelectasis (more severe at the upper part of lung). • Important features are presence of multiple cystlike structure called bullae which sometime rupture result in spontaneous pneumothorax.
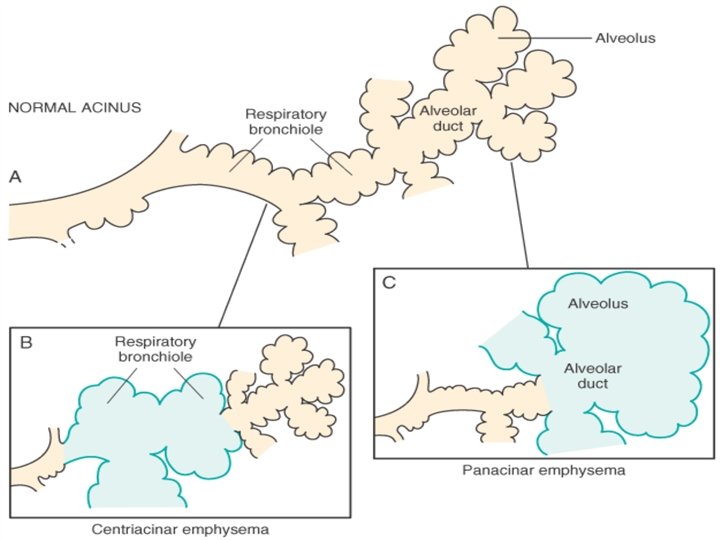
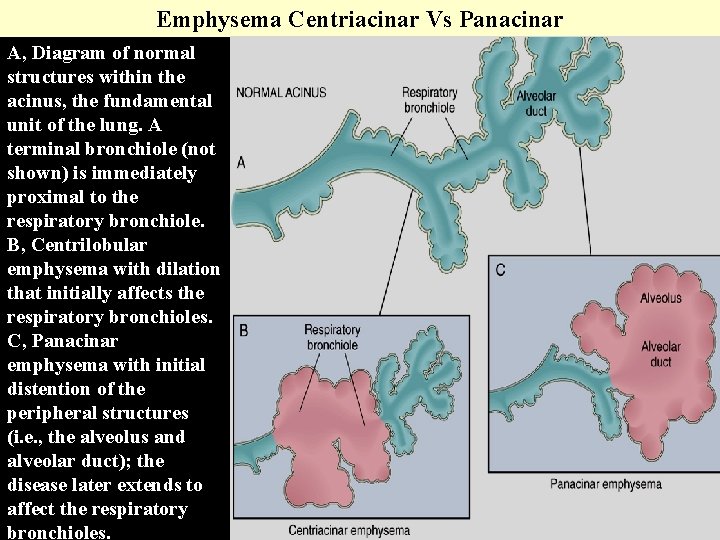
Emphysema Centriacinar Vs Panacinar A, Diagram of normal structures within the acinus, the fundamental unit of the lung. A terminal bronchiole (not shown) is immediately proximal to the respiratory bronchiole. B, Centrilobular emphysema with dilation that initially affects the respiratory bronchioles. C, Panacinar emphysema with initial distention of the peripheral structures (i. e. , the alveolus and alveolar duct); the disease later extends to affect the respiratory bronchioles.
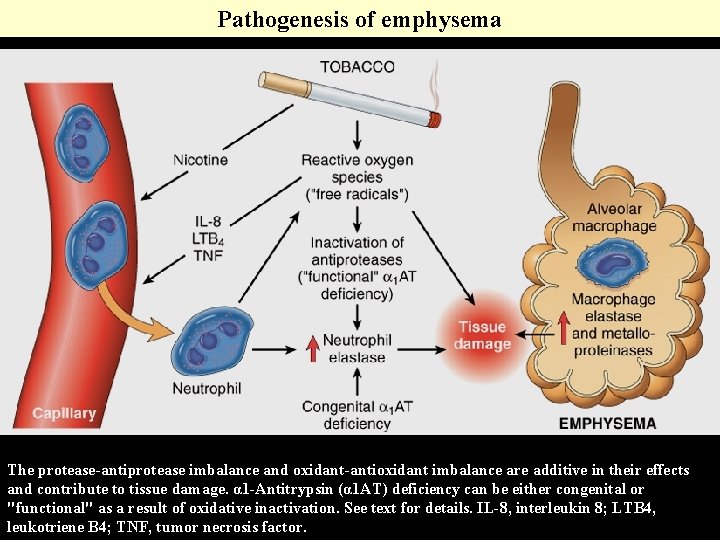
Incidence of emphysema: Is a common disease, about 50% of adults who come to autopsy asymptomatic, mainly centriacinar, male, heavy smoker. Pathogenesis: The current theory favors emphysema arising as a consequence of two coexisting critical imbalances: 1. Protease—antiprotease imbalance. 2. Oxidant------Antioxidant imbalance. Normally protease is secreted by neutrophils. Proteases: are enzymes which digest the tissue. Most important one is elastase.
Anti-proteases : are the counteracting enzymes that stop the action of digestion, important one is antielastase (α-1 anti-trypsin), which is normally present in serum, tissue fluids & macrophages. So the development of emphysema occur : 1. When there is elastase activity as in smoking. 2. When there is anti-elastase activity as in : a. Hereditary α-1 anti- trypsin deficiency. b. Acquired as in smokers due to the effect of nicotine, O 2 free radicals that inhibit the release of anti-elastase.
The effect of smoking in the development of emphysema: • It the no. of neutrophils, macrophages, in the alveoli. • Nicotine is a chemotactic substance for neutrophils. • It stimulates the elastase activity. • The oxidants in the smoke and the free radicals from the accompanying neutrophils inhibit the secretion of anti-elastase.
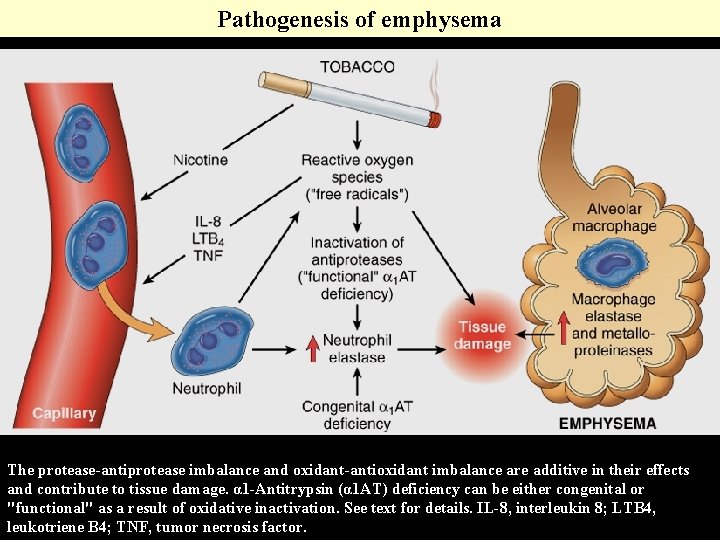
Pathogenesis of emphysema The protease-antiprotease imbalance and oxidant-antioxidant imbalance are additive in their effects and contribute to tissue damage. α 1 -Antitrypsin (α 1 AT) deficiency can be either congenital or "functional" as a result of oxidative inactivation. See text for details. IL-8, interleukin 8; LTB 4, leukotriene B 4; TNF, tumor necrosis factor.
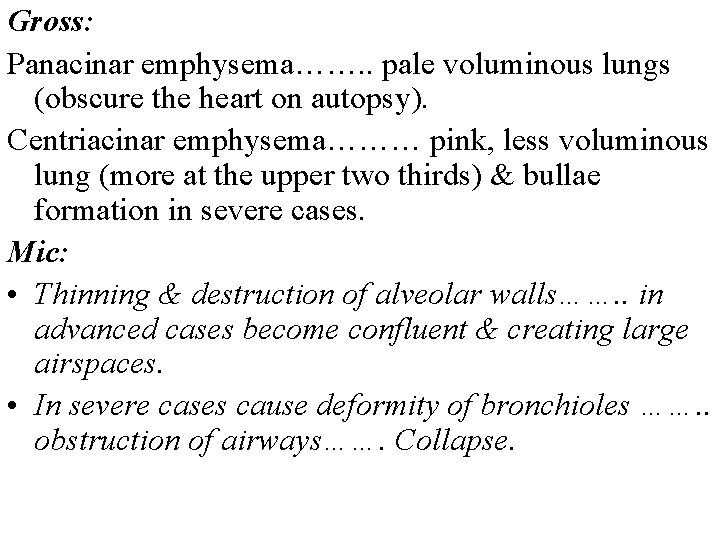
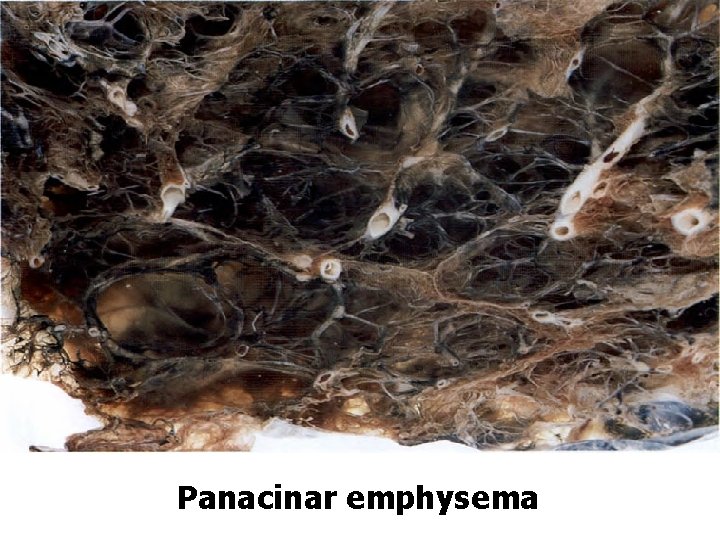
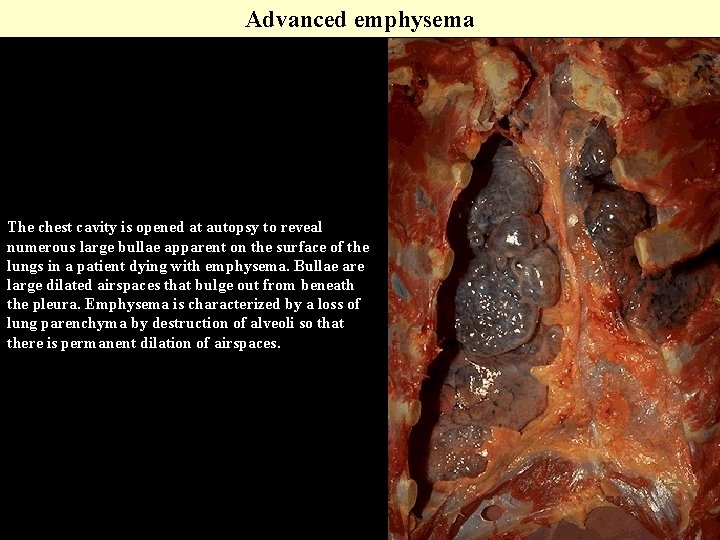
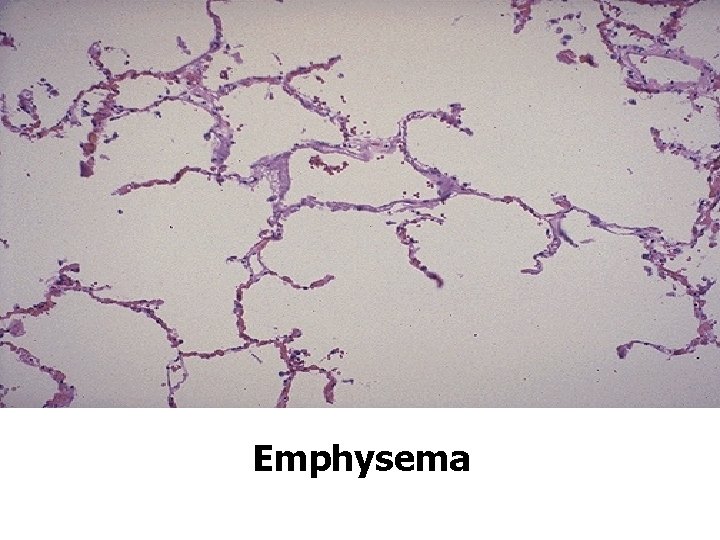
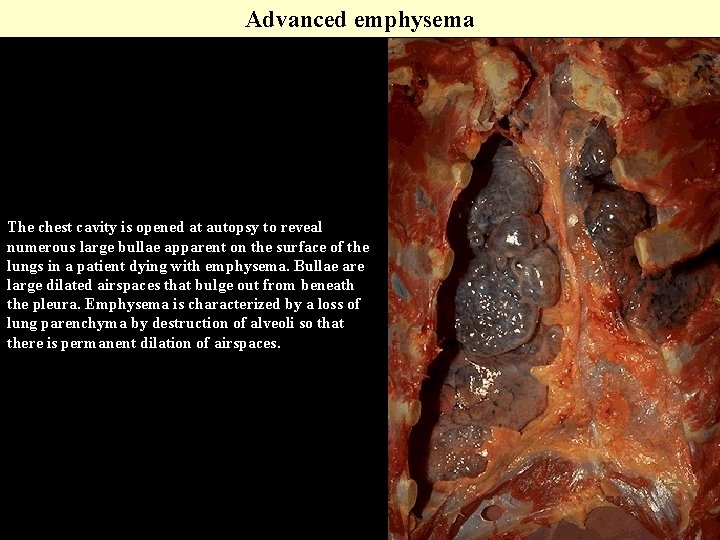
Gross: Panacinar emphysema……. . pale voluminous lungs (obscure the heart on autopsy). Centriacinar emphysema……… pink, less voluminous lung (more at the upper two thirds) & bullae formation in severe cases. Mic: • Thinning & destruction of alveolar walls……. . in advanced cases become confluent & creating large airspaces. • In severe cases cause deformity of bronchioles ……. . obstruction of airways……. Collapse.

CENTRIACINAR EMPHYSEMA
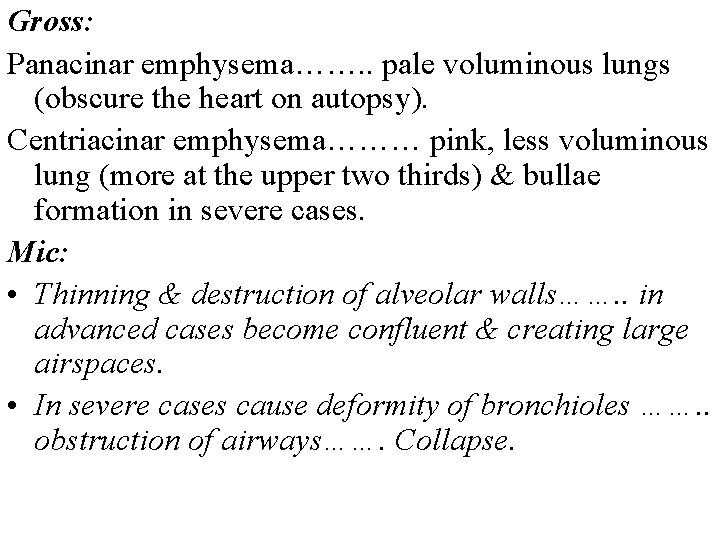
Panacinar emphysema
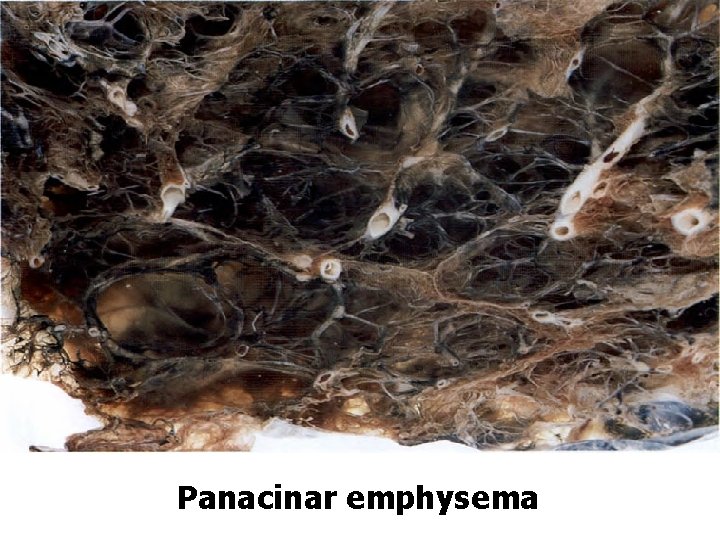
Advanced emphysema The chest cavity is opened at autopsy to reveal numerous large bullae apparent on the surface of the lungs in a patient dying with emphysema. Bullae are large dilated airspaces that bulge out from beneath the pleura. Emphysema is characterized by a loss of lung parenchyma by destruction of alveoli so that there is permanent dilation of airspaces.
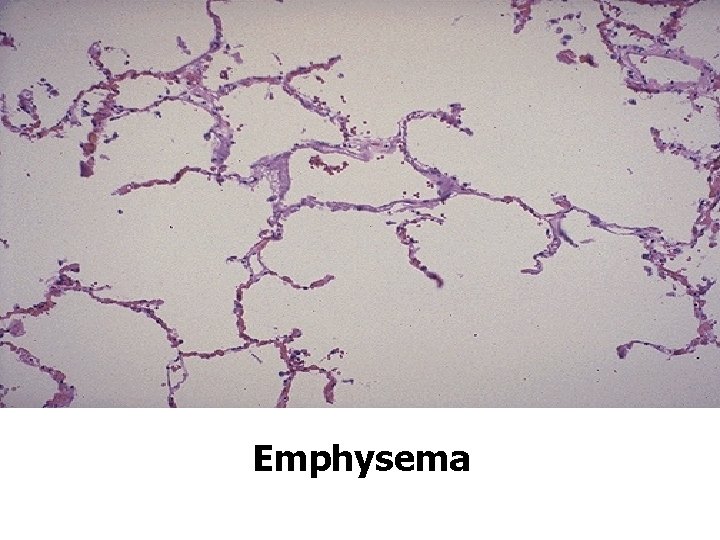
Emphysema
Chronic Bronchitis: • Persistent productive cough for at least 3 consecutive months in at least 2 consecutive years. • 20% - 25% of men at 40 – 65 years have chronic bronchitis (more in smoker). Types of chronic bronchitis: 1. Simple Chronic bronchitis: (mucoid sputum). 2. Chronic mucopurulent bronchitis: (pus containing sputum due to secondary infection). 3. Asthmatic chronic bronchitis: some of patient may develop intermittent episode of asthma. 4. Chronic obstructive bronchitis: develop chronic pulmonary outflow obstruction.
Pathogenesis: Two distinctive etiological factors of chronic bronchitis: 1. Chronic irritation by smoking, air pollutants (sulfur dioxide), nitrogen dioxide which result in followings: I. Hypersecretion of mucus due to hypertrophy of mucus glands & goblet cells……. Excess mucin production. II. Resulting in infiltration of inflammatory cells (CD 8+ T CELLS), MQ & neutrophils………. Continuous inflammation……. Tissue destruction. 2. Microbial infection is often present but play secondary role in maintaining inflammation & irritation.
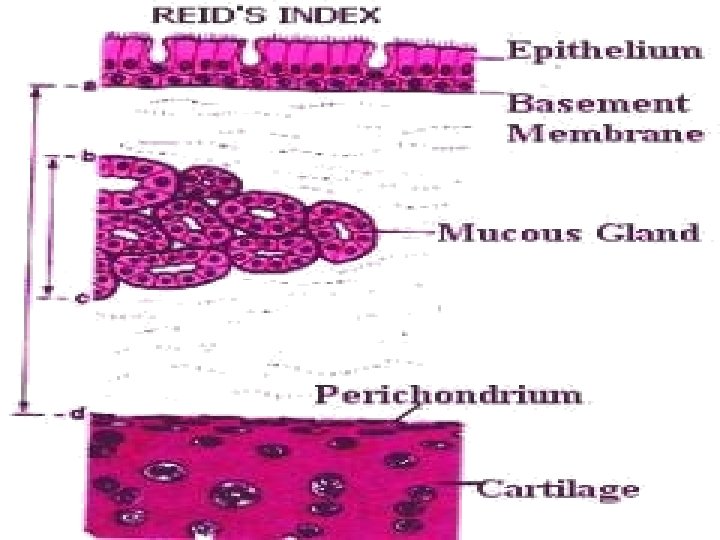
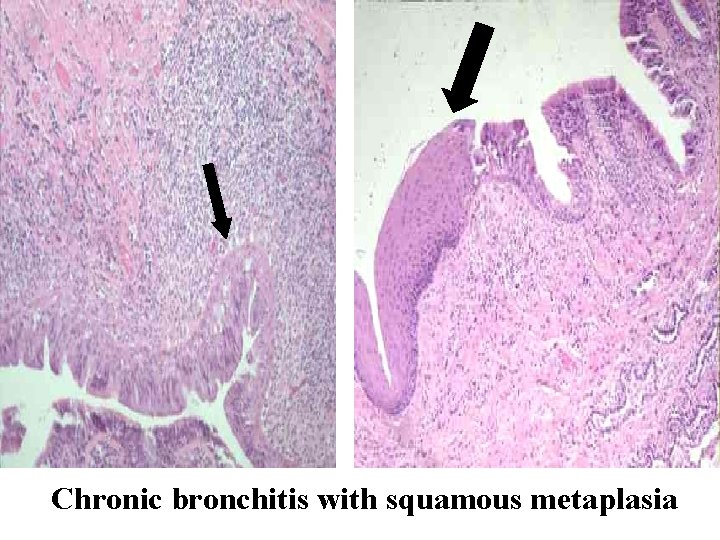
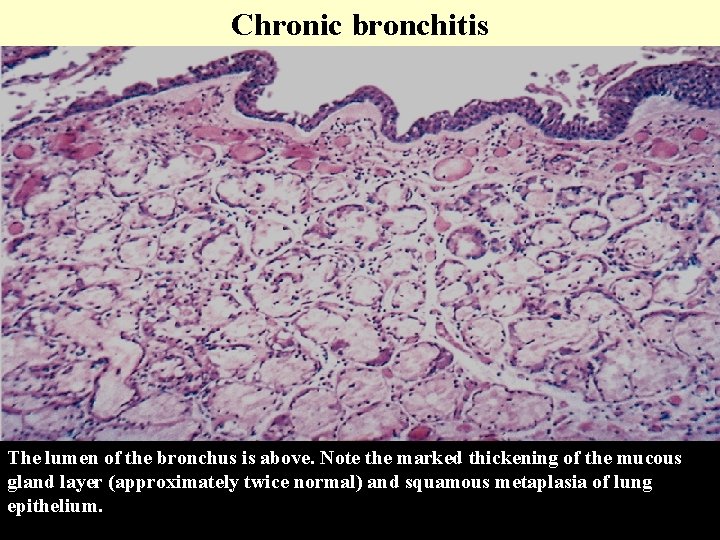
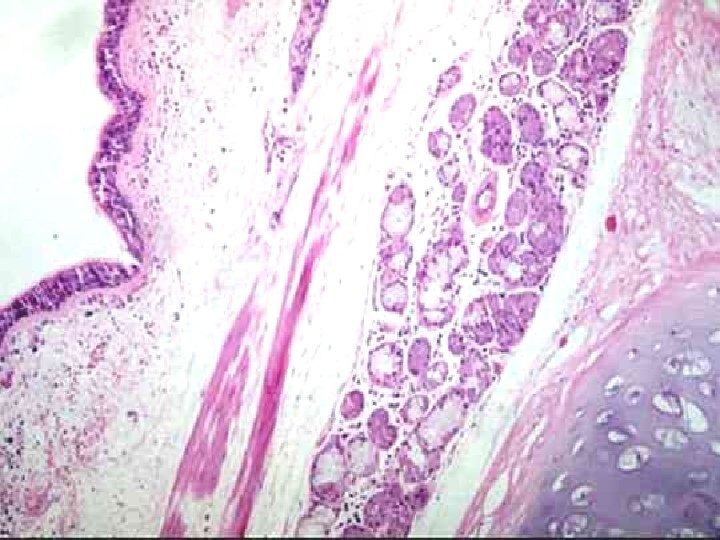
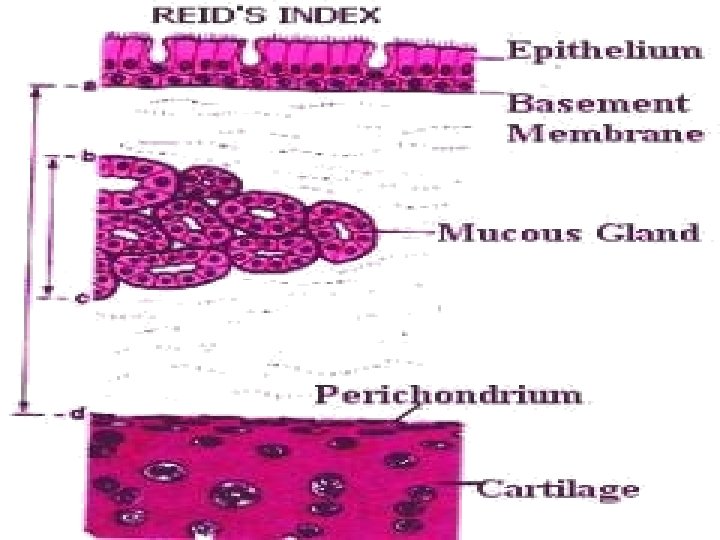
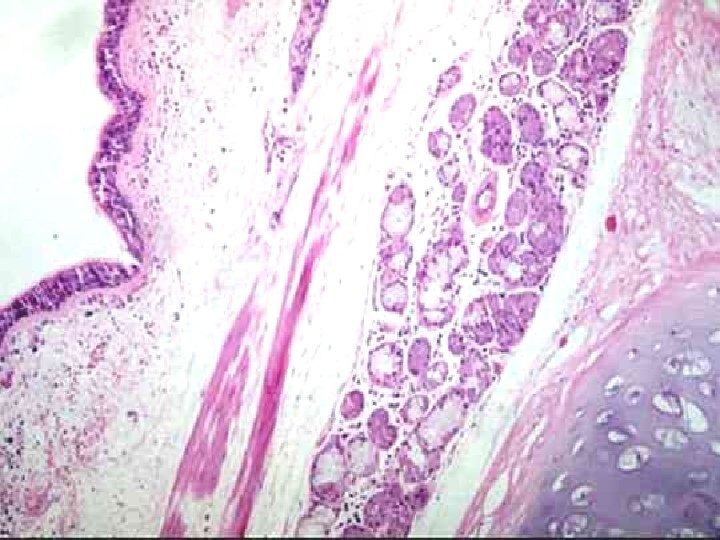
Gross: Airways are hyperemic, swollen & filled with mucopurulent secretion. Microscopically: • Enlarged mucous secreting glands in the trachea & bronchus, this is best estimated by the increase in the Reid Index. • Marked narrowing of the bronchioles due to goblet cell metaplasia, mucous plug, inflammation & fibrosis. • The bronchial epithelium may show squamous metaplasia and dysplasia. Reid index: It is the ratio of the thickness of the mucous gland layer / thickness of the wall between the epithelium and the cartilage. Normally it is 0. 4 , it increases in chronic bronchitis.
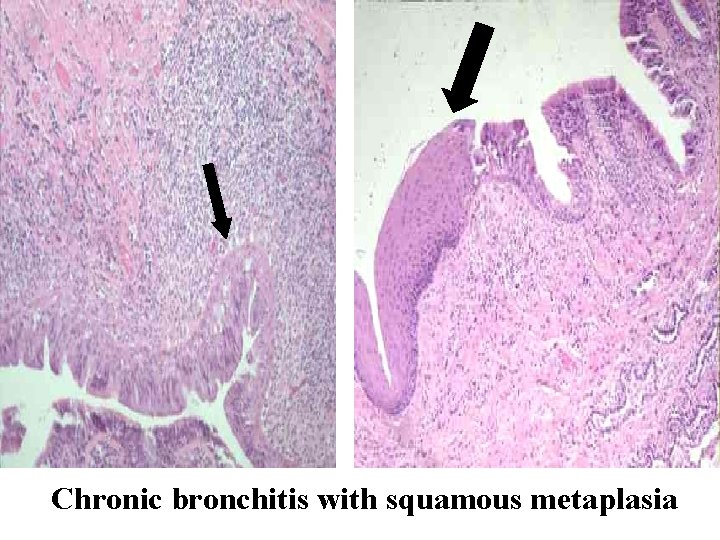
Chronic bronchitis with squamous metaplasia
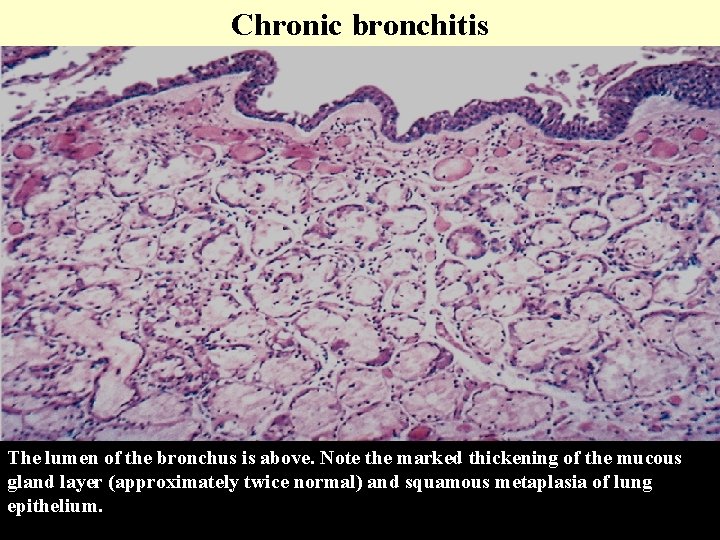
Chronic bronchitis The lumen of the bronchus is above. Note the marked thickening of the mucous gland layer (approximately twice normal) and squamous metaplasia of lung epithelium.
Complications: 1. Pulmonary hypertension & cardiac failure. 2. Recurrent pulmonary infections & respiratory failure. 3. May result in metaplasia……Dysplasia…. . carcinoma squence.