4 th Course of Diffuse Parenchymal Lung Diseases









- Slides: 51
4 th Course of Diffuse Parenchymal Lung Diseases Clinical Case 11 th February 2015
Presentation Identification Male gender Caucasian 39 years-old Born and resident in Bragança Occupation: car collision repair and painting
First visit at 27/10/2014 Main complaints Chronic (2 years) non-productive cough Dyspnea on exertion
First visit at 27/10/2014 Past medical history Thrombocytopenia of unknown etiology Gastroesophageal reflux disease Allergies: dust mites and grasses Smoker since 16 years (23 pack-year) Environmental exposures: occupational, neighbour with birds Medication: salmeterol/fluticasone inhaler was recently prescribed
First visit at 27/10/2014 Physical examination Good performance status Without respiratory discomfort Neck reveals no significant JVD Heart: S 1 and S 2 present. No murmurs. Lungs: bilateral basal inspiratory crackles Extremities showed no edema
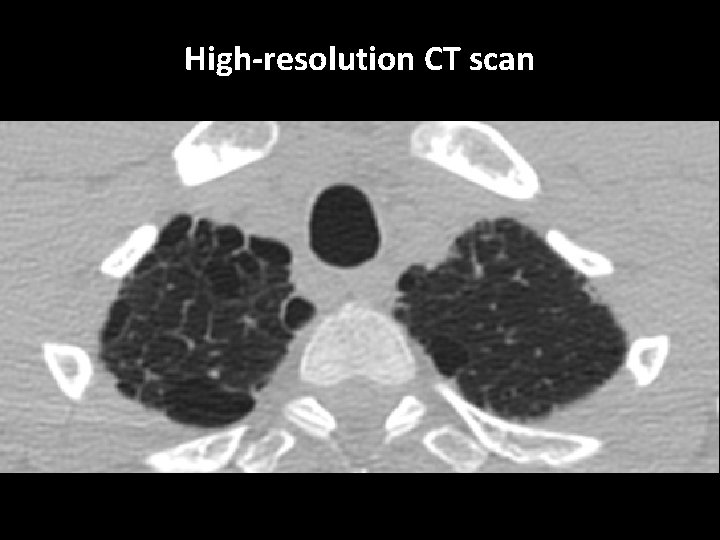
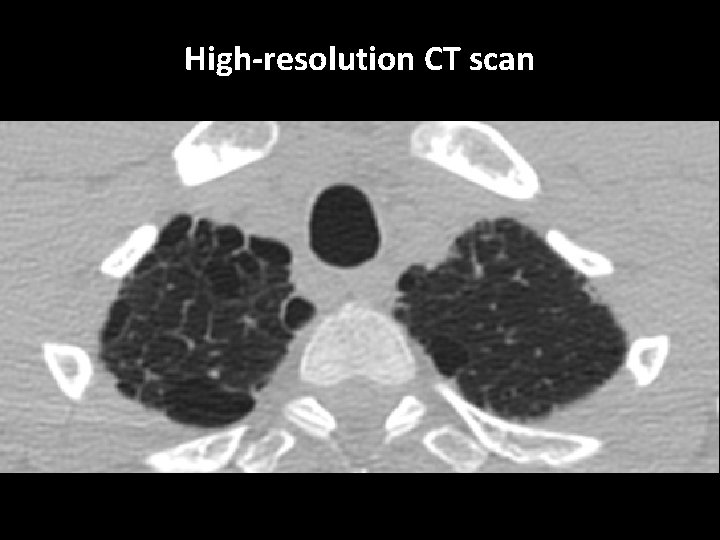
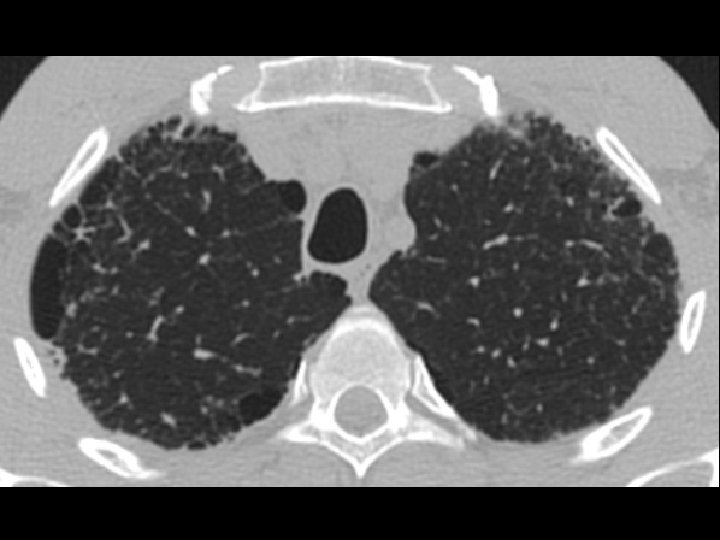
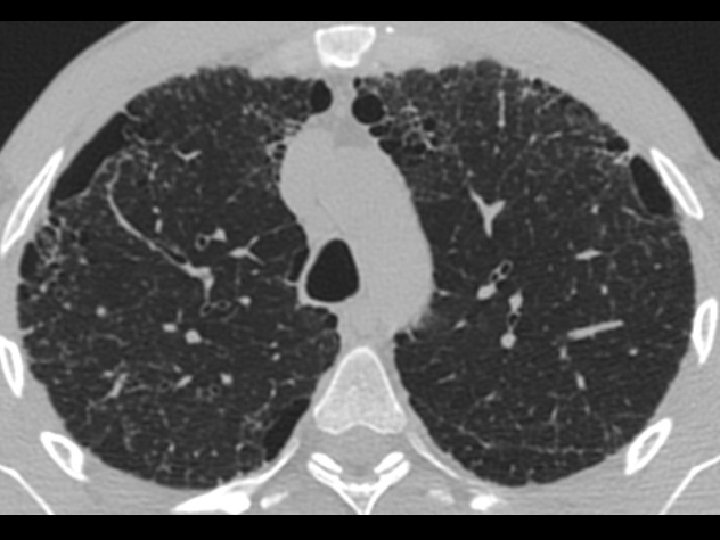
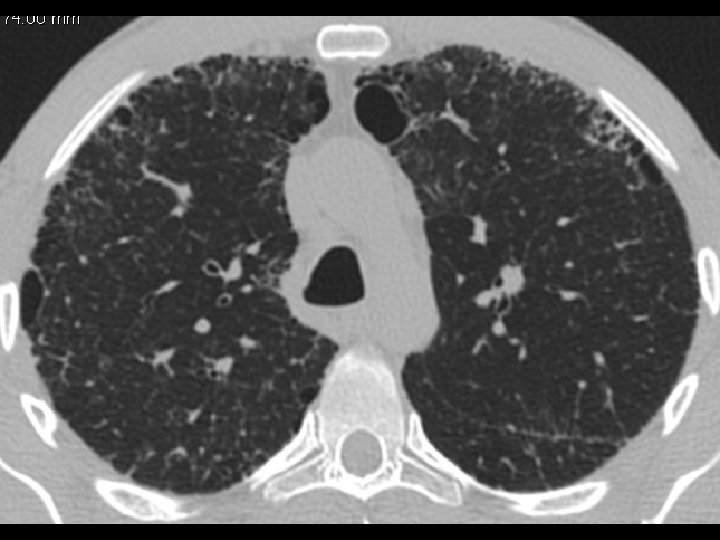
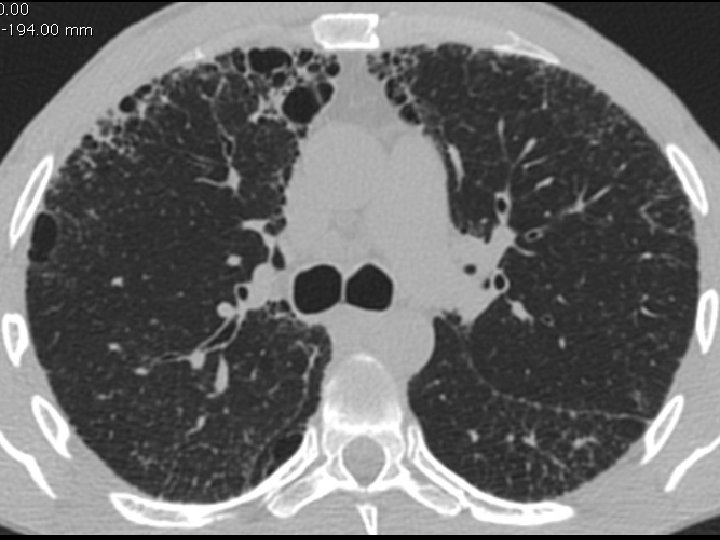
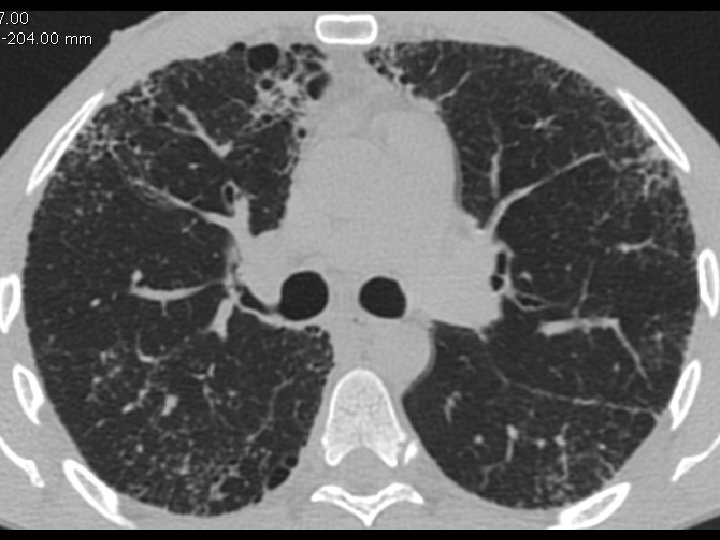
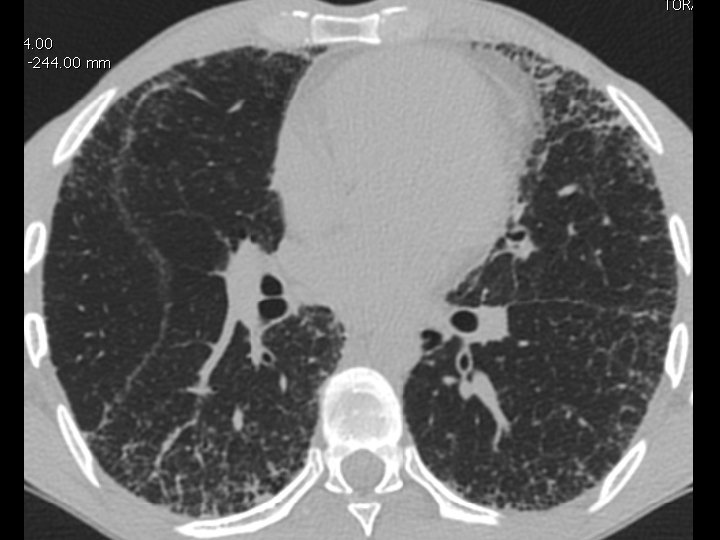
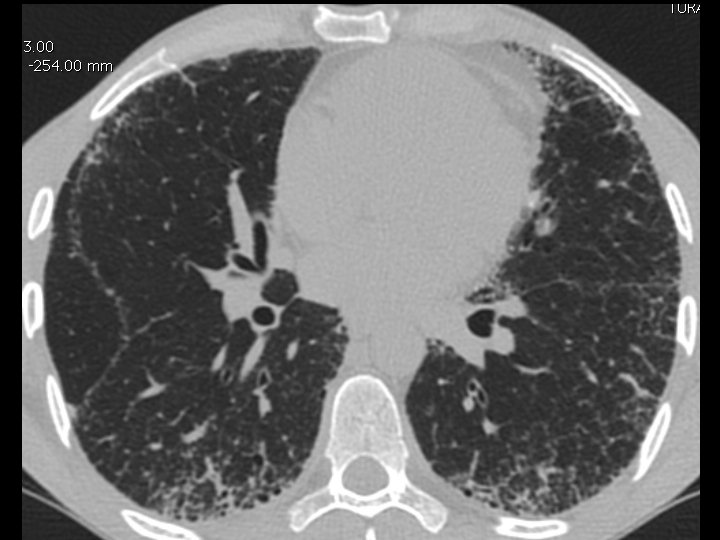
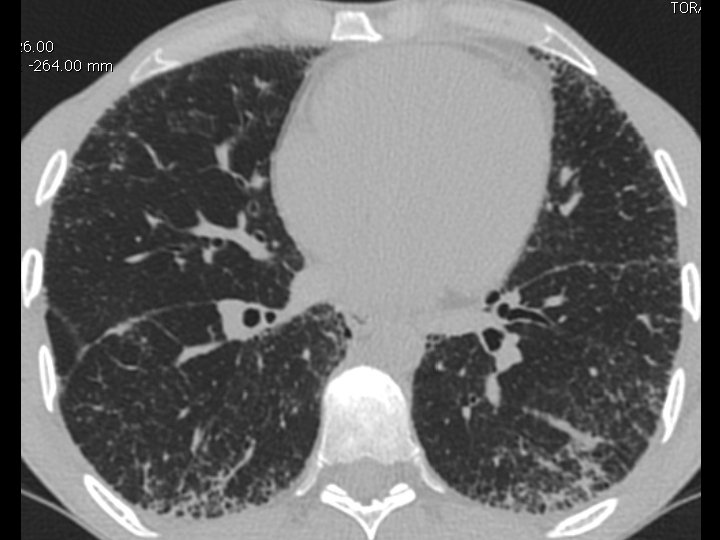
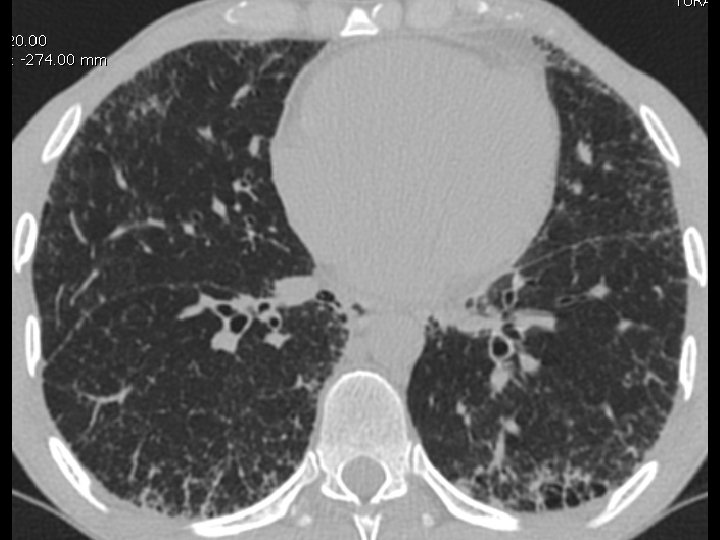
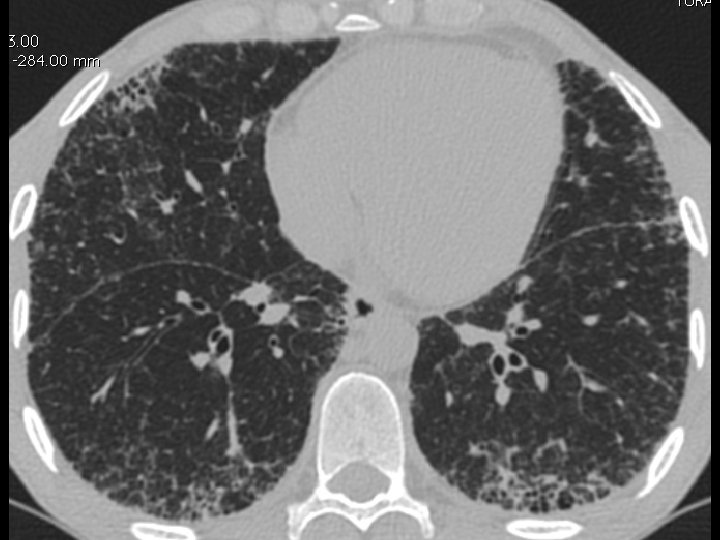
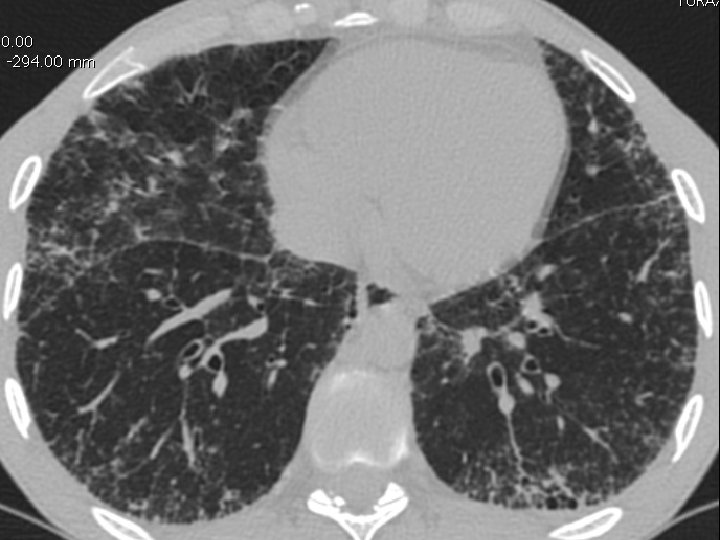
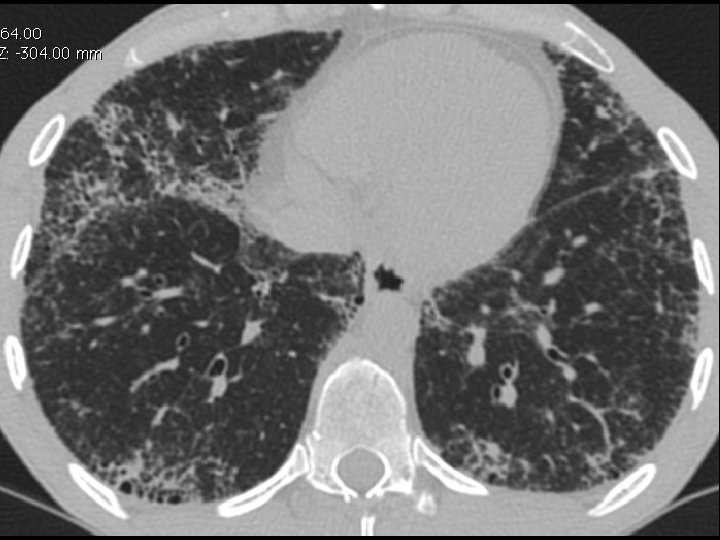
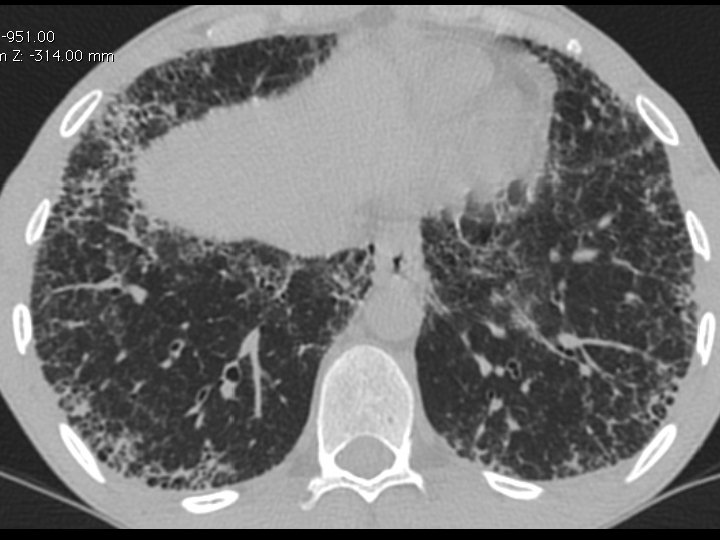
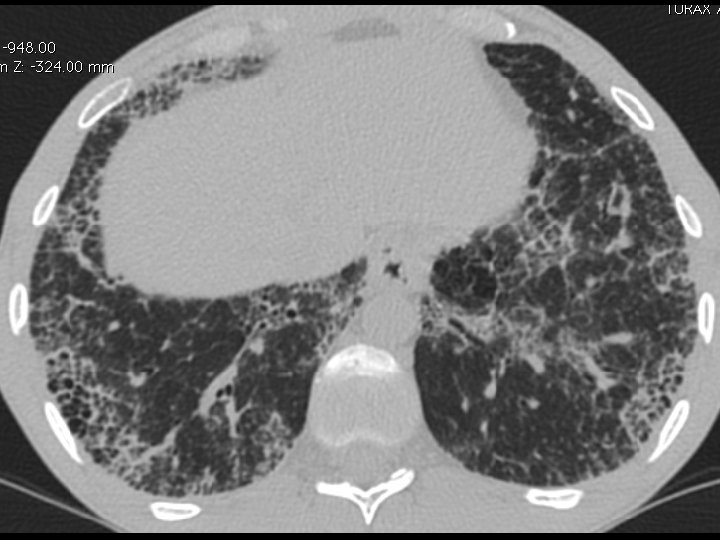
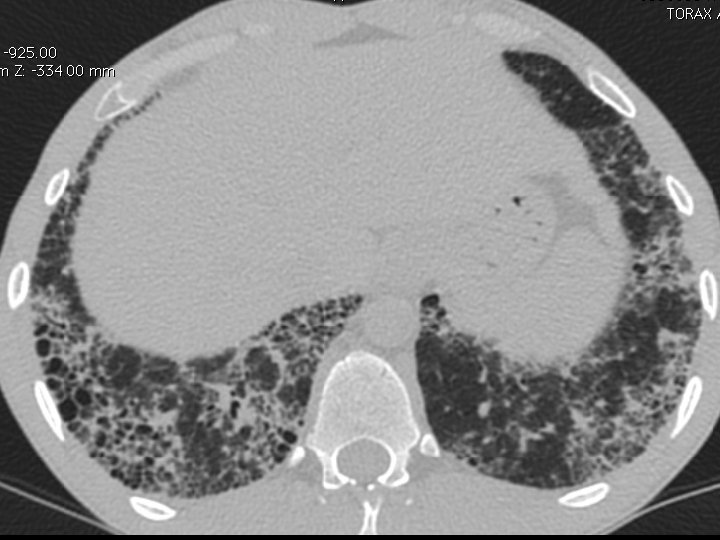
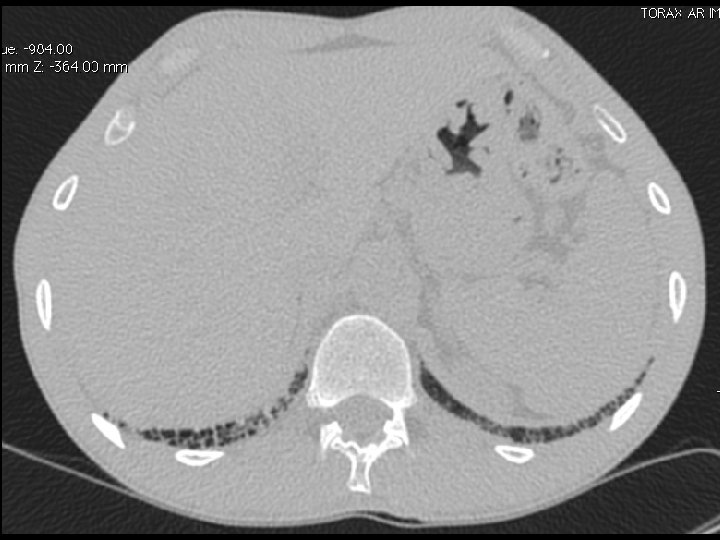
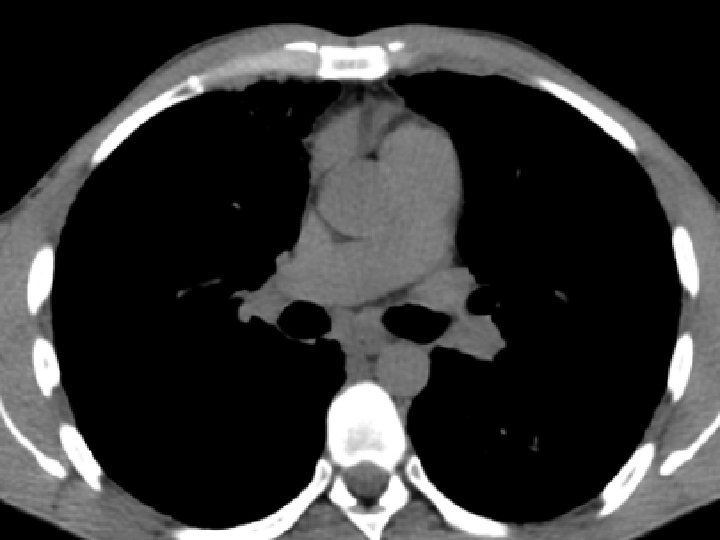
High-resolution CT scan
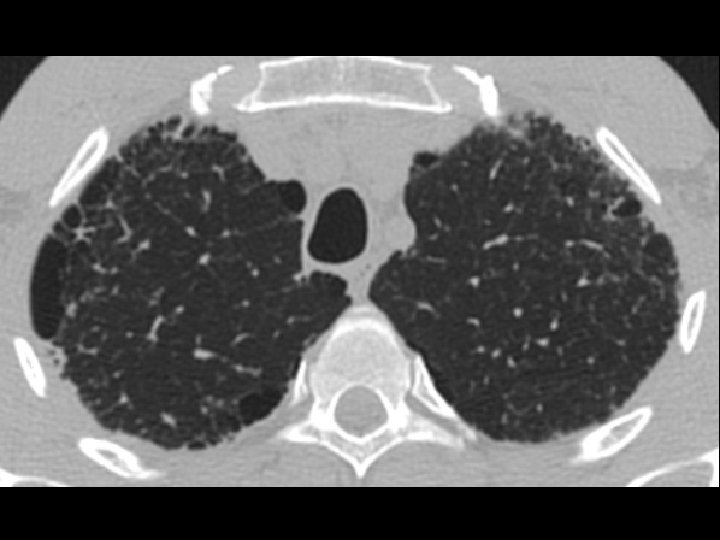


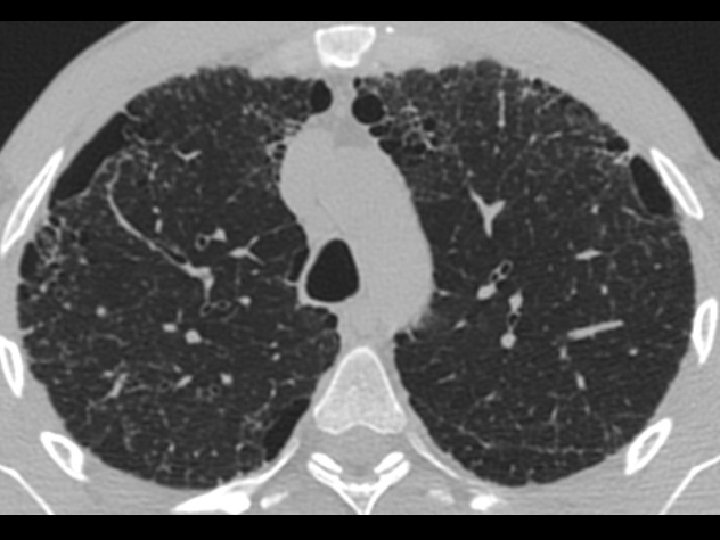
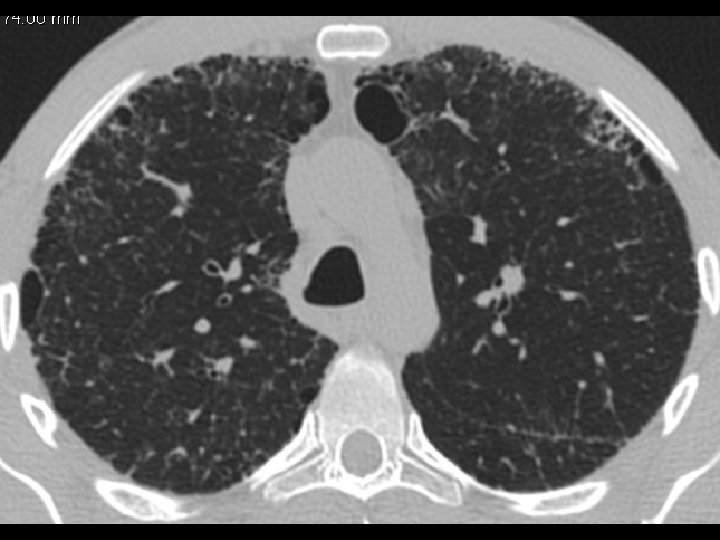

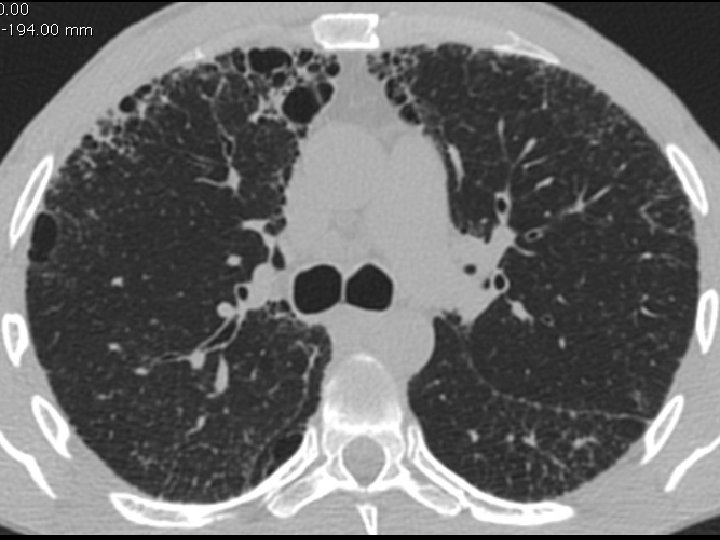
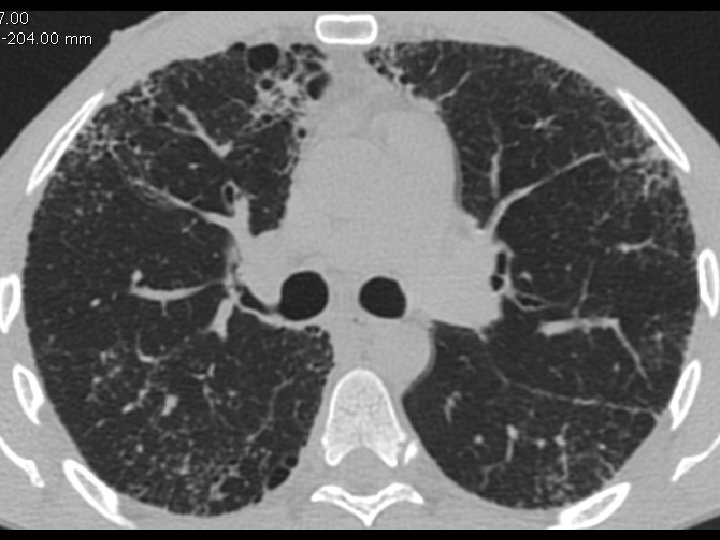



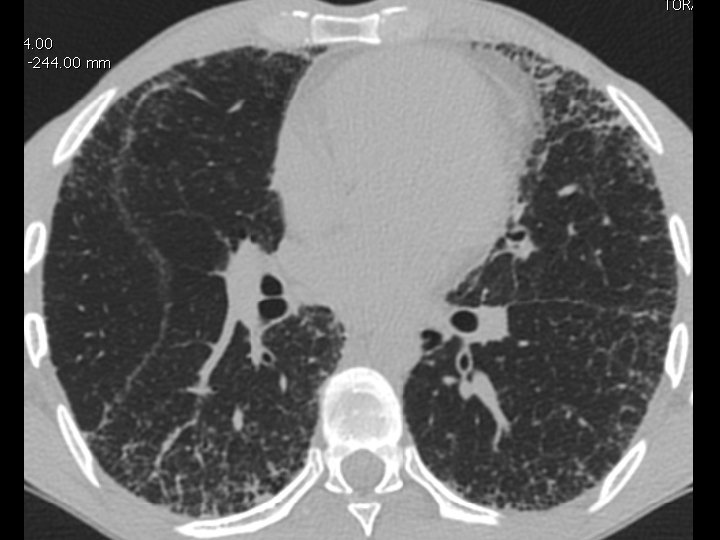
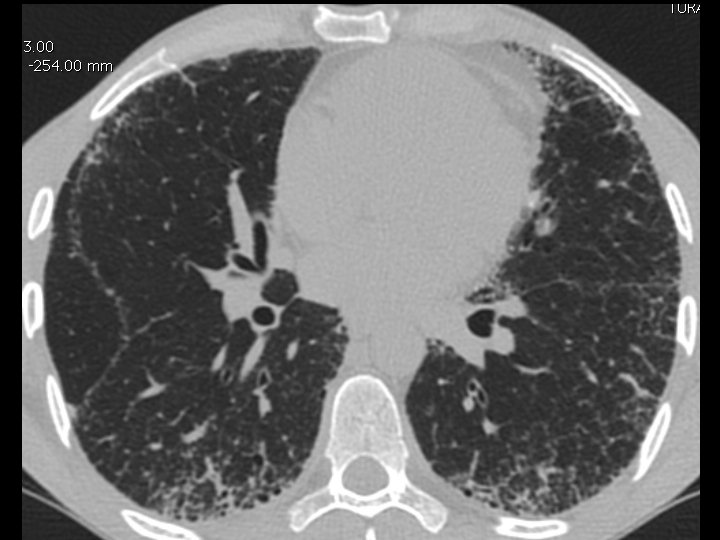
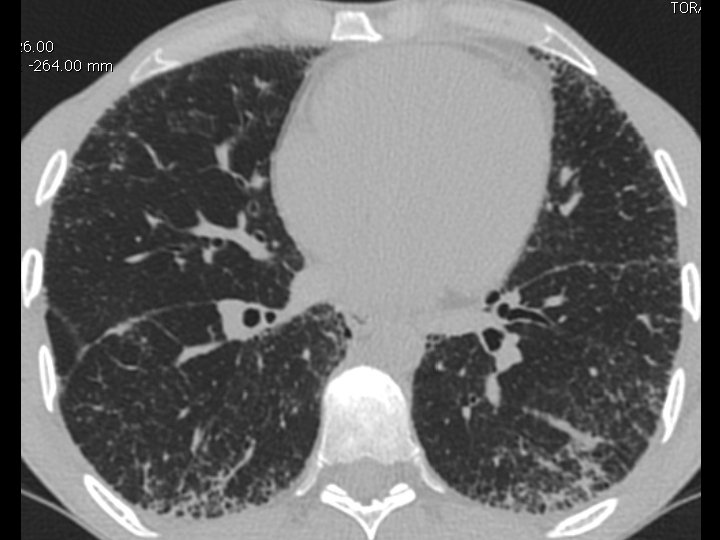
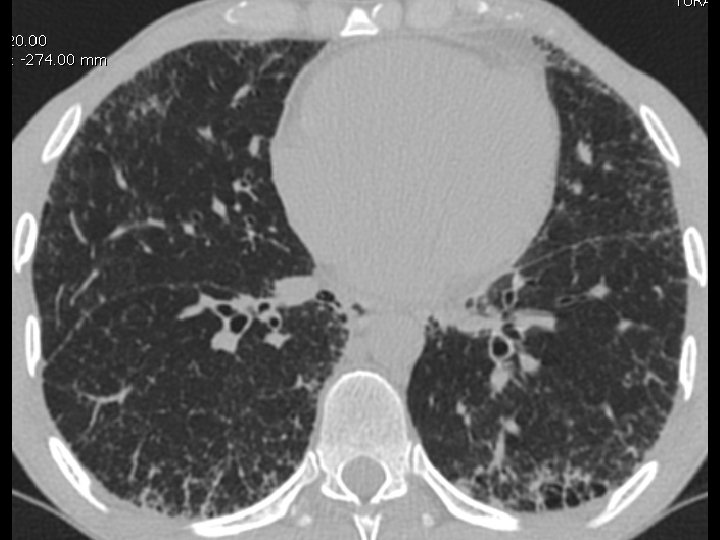
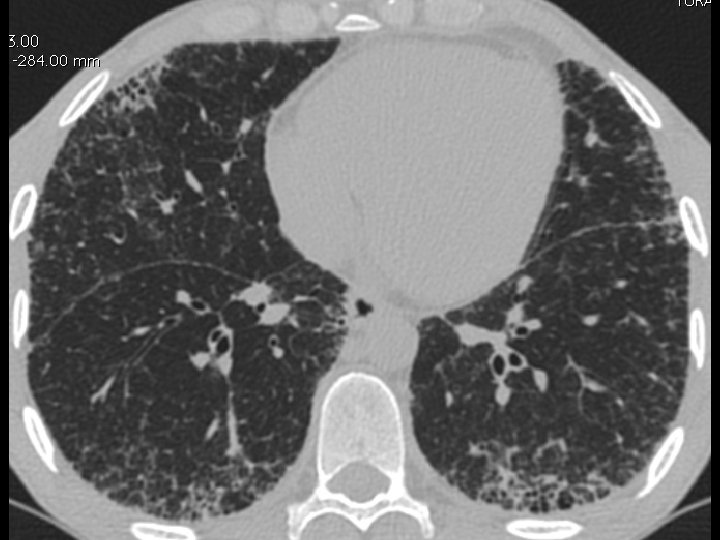
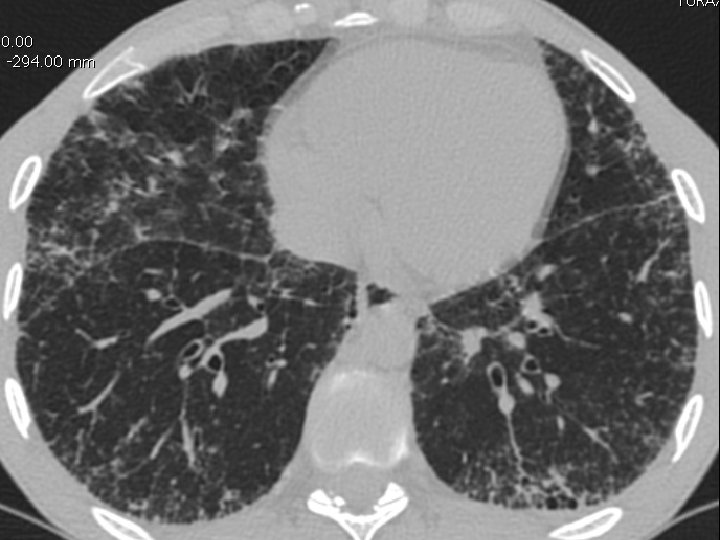
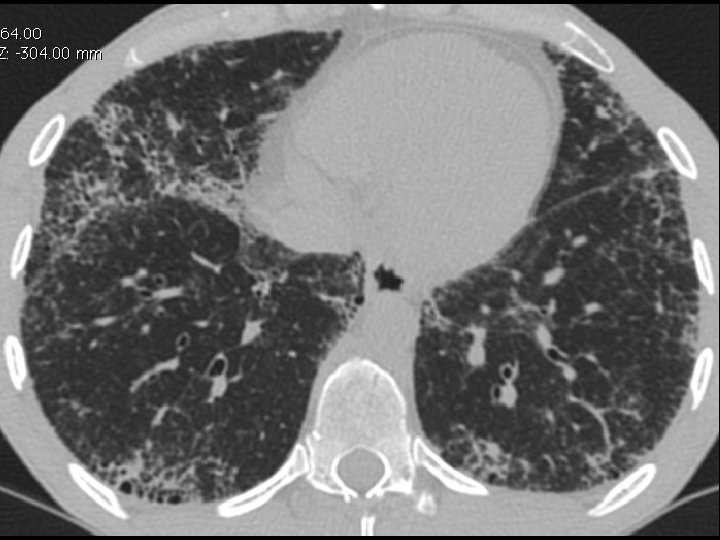
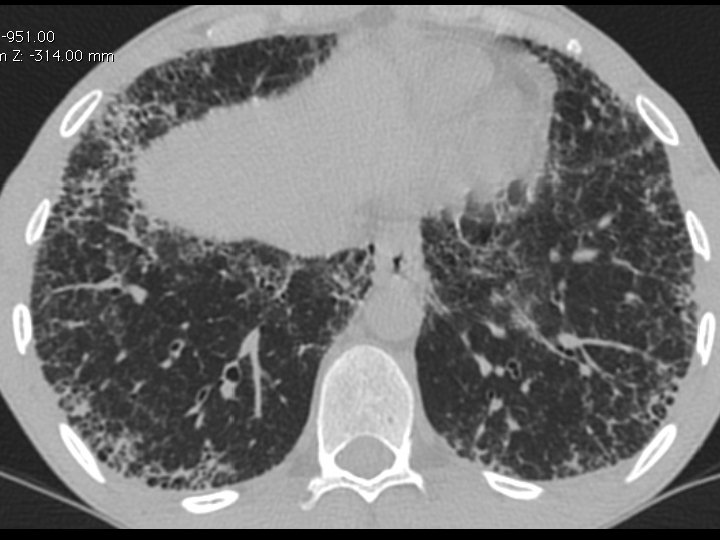
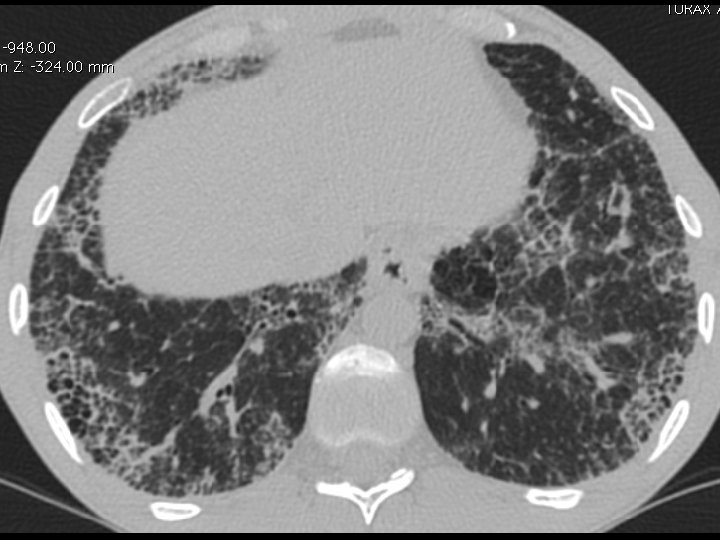
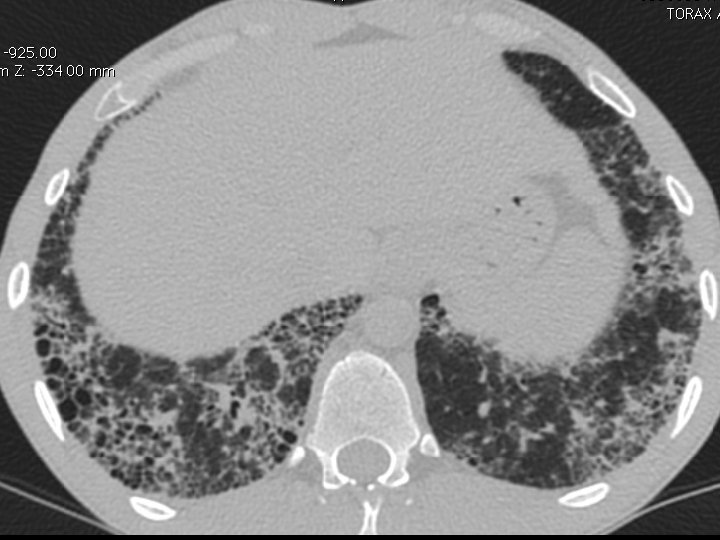


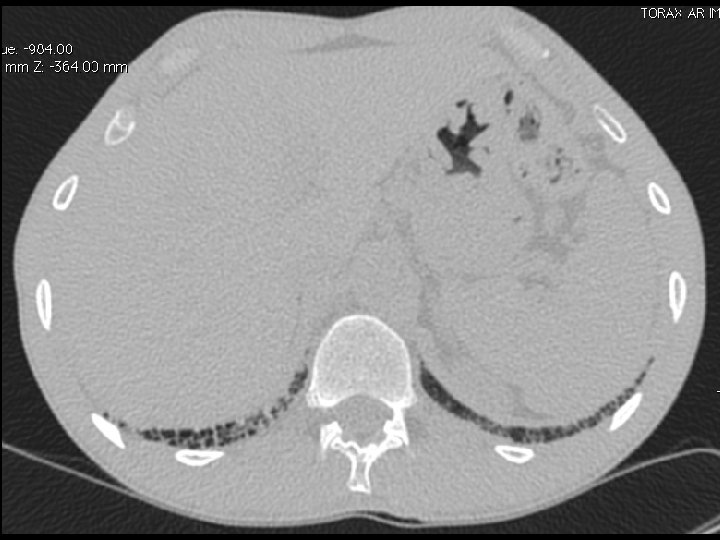
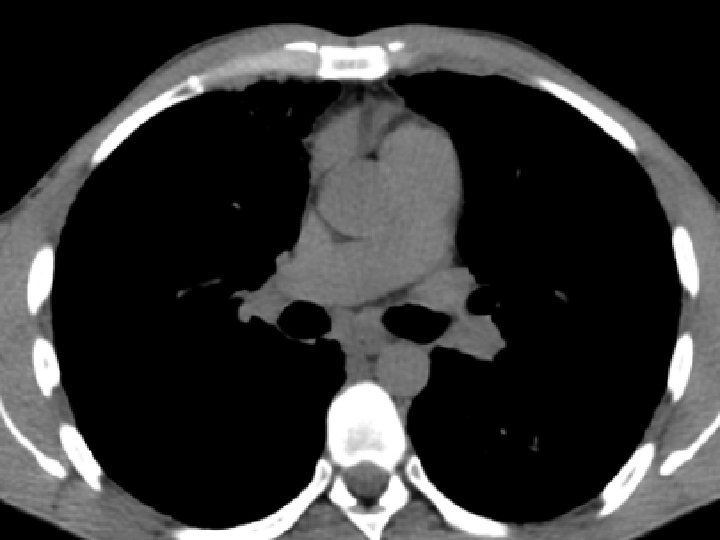
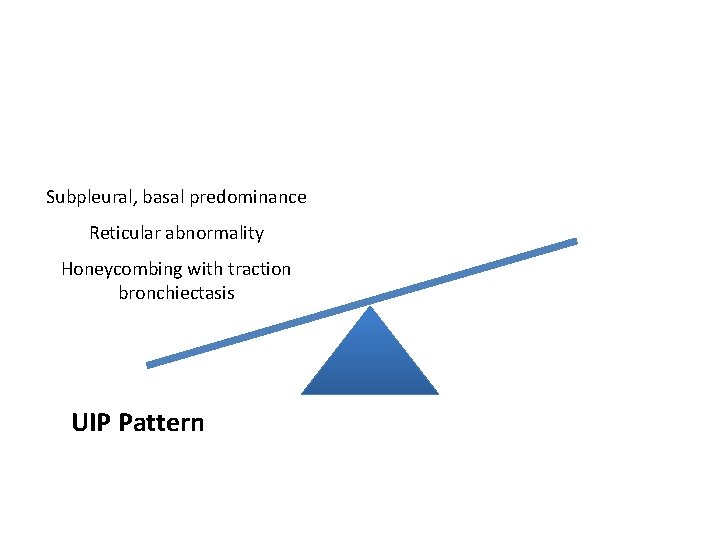
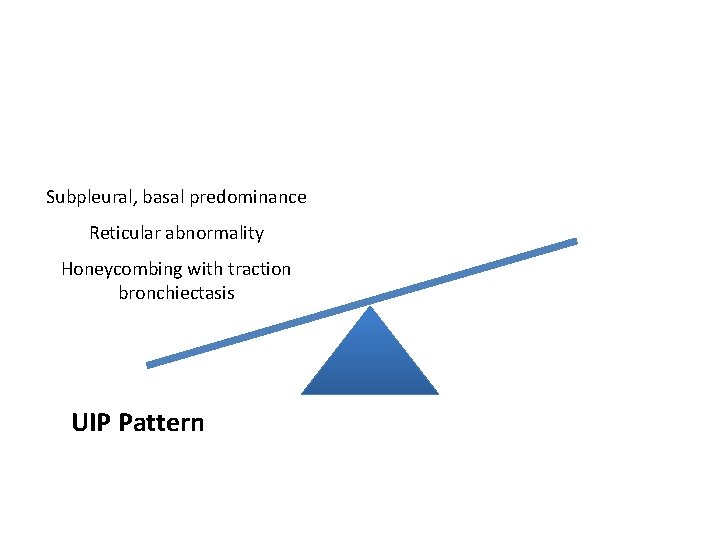
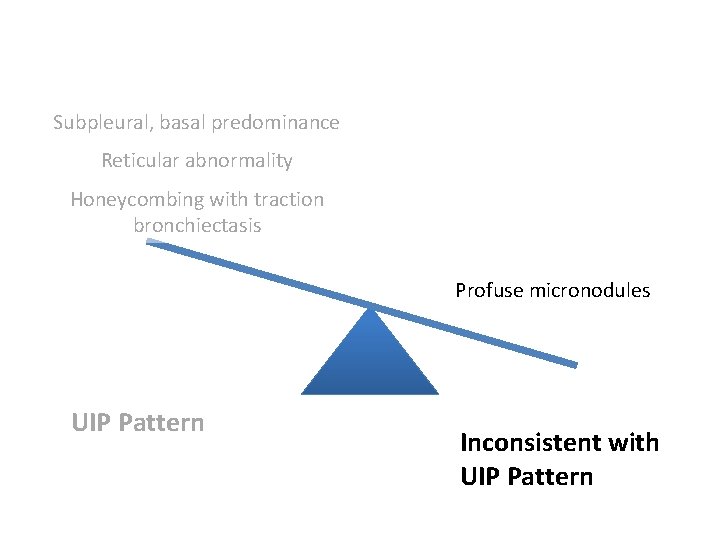
Subpleural, basal predominance Reticular abnormality Honeycombing with traction bronchiectasis UIPUIP Pattern
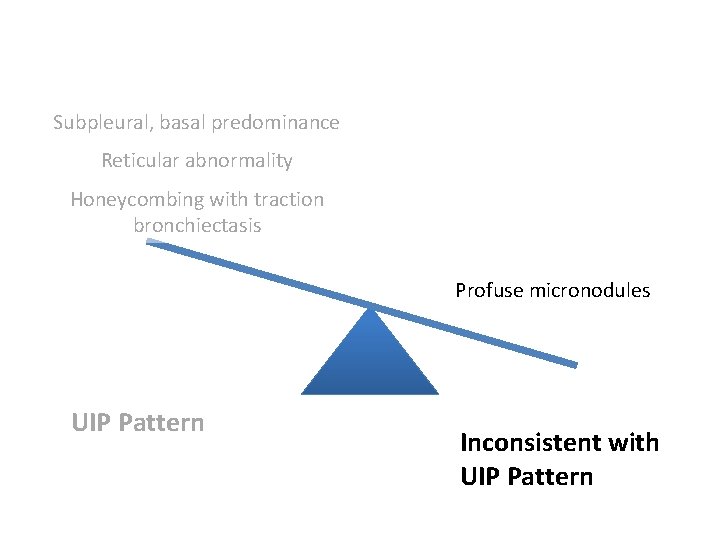
Subpleural, basal predominance Reticular abnormality Honeycombing with traction bronchiectasis Profuse micronodules UIPUIP Pattern Inconsistent with UIP Pattern

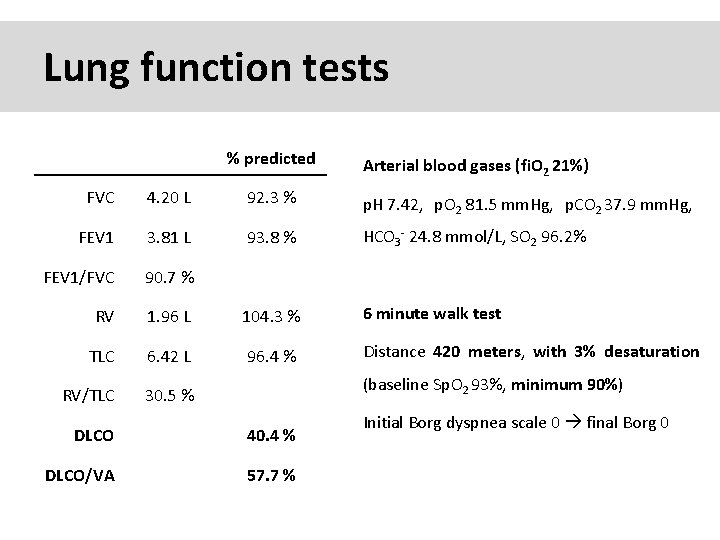
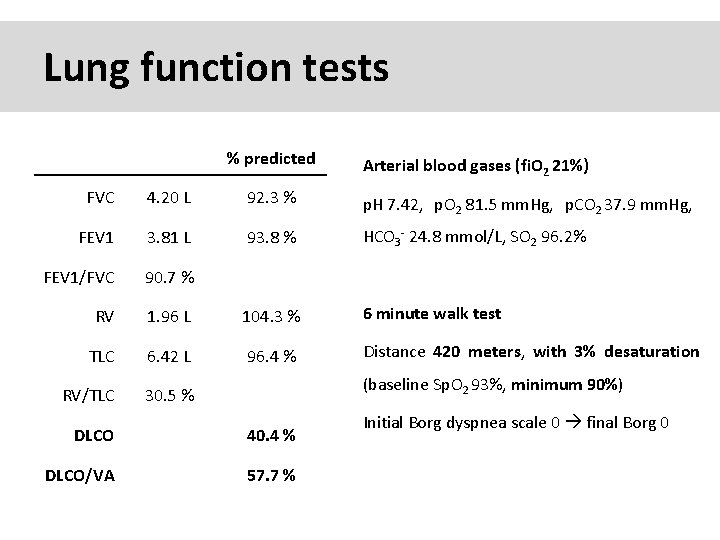
Lung function tests % predicted Arterial blood gases (fi. O 2 21%) FVC 4. 20 L 92. 3 % p. H 7. 42, p. O 2 81. 5 mm. Hg, p. CO 2 37. 9 mm. Hg, FEV 1 3. 81 L 93. 8 % HCO 3 - 24. 8 mmol/L, SO 2 96. 2% FEV 1/FVC 90. 7 % RV 1. 96 L 104. 3 % 6 minute walk test TLC 6. 42 L 96. 4 % Distance 420 meters, with 3% desaturation RV/TLC 30. 5 % (baseline Sp. O 2 93%, minimum 90%) DLCO 40. 4 % DLCO/VA 57. 7 % Initial Borg dyspnea scale 0 final Borg 0
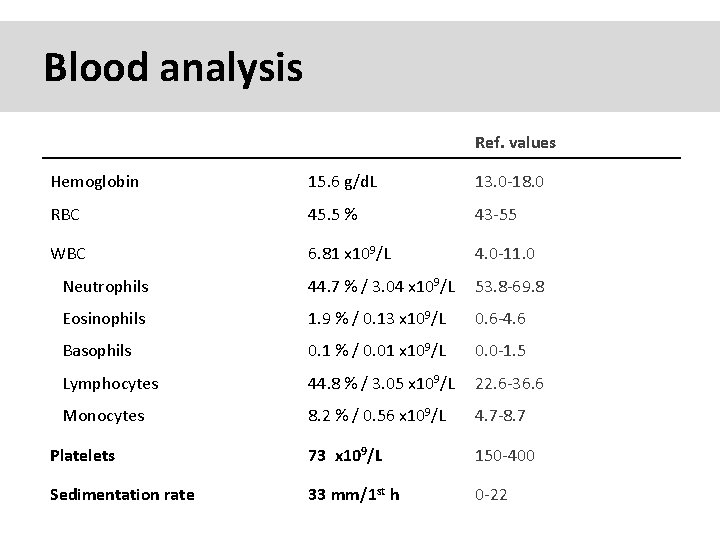
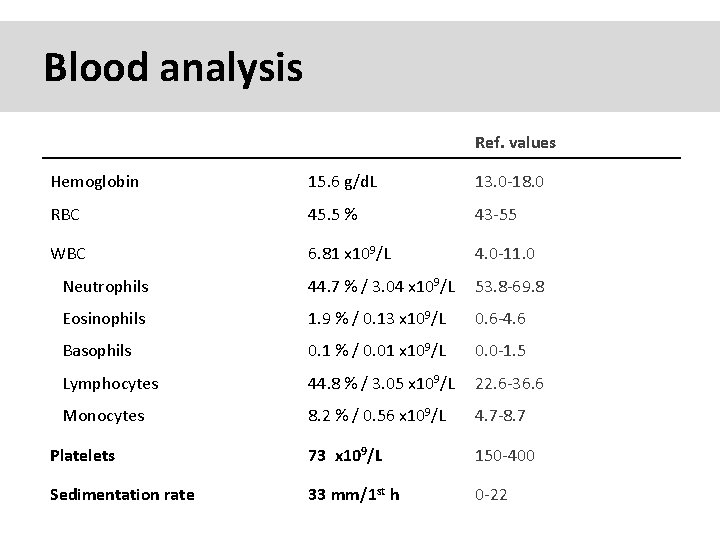
Blood analysis Ref. values Hemoglobin 15. 6 g/d. L 13. 0 -18. 0 RBC 45. 5 % 43 -55 WBC 6. 81 x 109/L 4. 0 -11. 0 Neutrophils 44. 7 % / 3. 04 x 109/L 53. 8 -69. 8 Eosinophils 1. 9 % / 0. 13 x 109/L 0. 6 -4. 6 Basophils 0. 1 % / 0. 01 x 109/L 0. 0 -1. 5 Lymphocytes 44. 8 % / 3. 05 x 109/L 22. 6 -36. 6 Monocytes 8. 2 % / 0. 56 x 109/L 4. 7 -8. 7 Platelets 73 x 109/L 150 -400 Sedimentation rate 33 mm/1 st h 0 -22
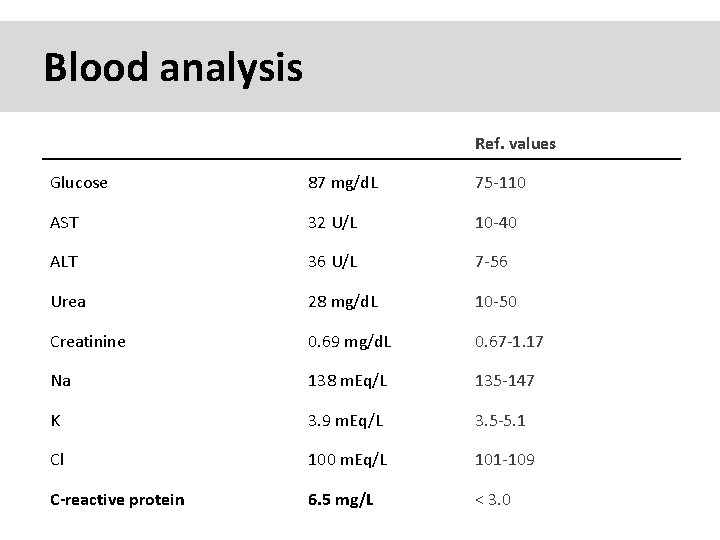
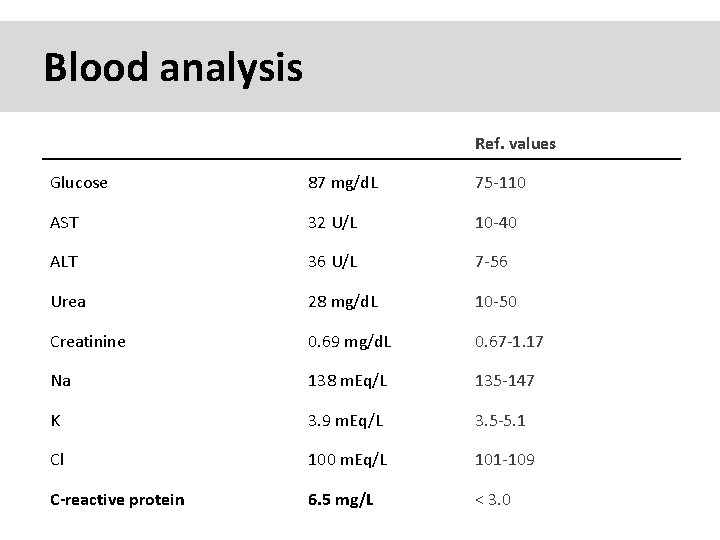
Blood analysis Ref. values Glucose 87 mg/d. L 75 -110 AST 32 U/L 10 -40 ALT 36 U/L 7 -56 Urea 28 mg/d. L 10 -50 Creatinine 0. 69 mg/d. L 0. 67 -1. 17 Na 138 m. Eq/L 135 -147 K 3. 9 m. Eq/L 3. 5 -5. 1 Cl 100 m. Eq/L 101 -109 C-reactive protein 6. 5 mg/L < 3. 0
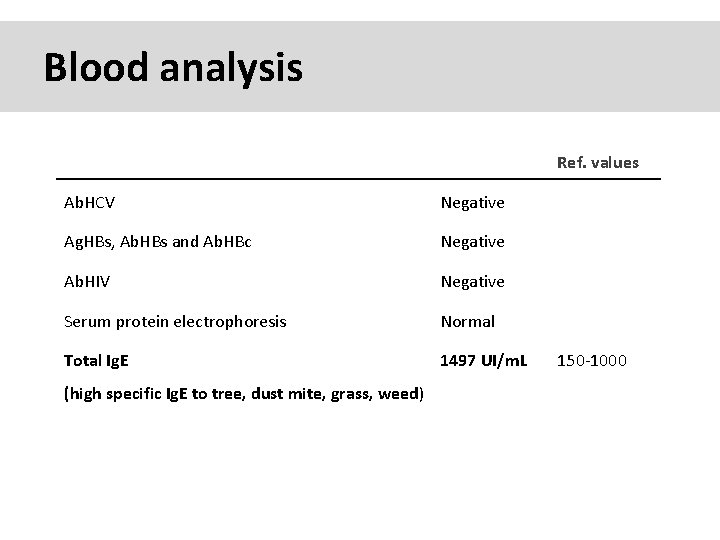
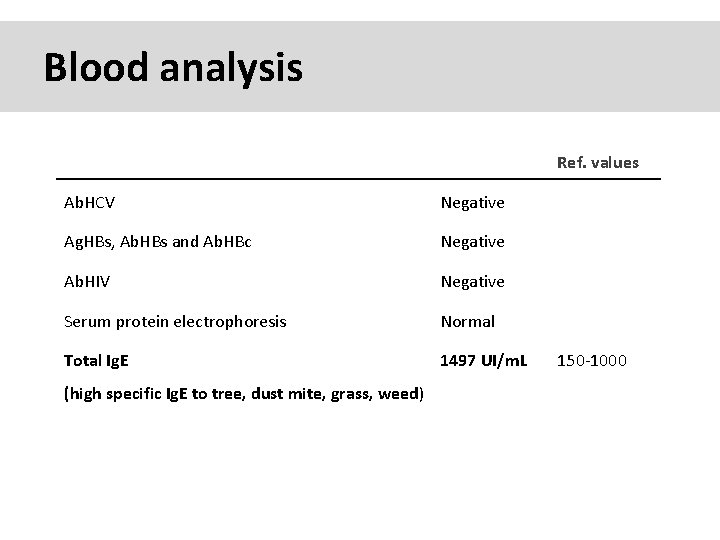
Blood analysis Ref. values Ab. HCV Negative Ag. HBs, Ab. HBs and Ab. HBc Negative Ab. HIV Negative Serum protein electrophoresis Normal Total Ig. E 1497 UI/m. L (high specific Ig. E to tree, dust mite, grass, weed) 150 -1000
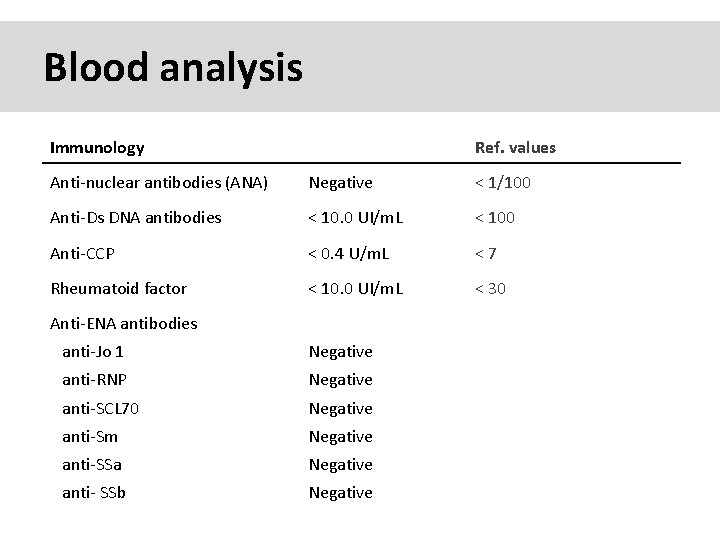
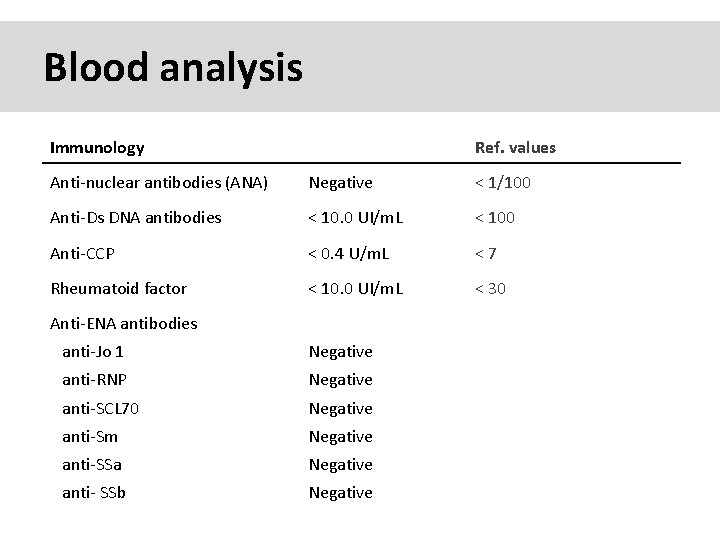
Blood analysis Immunology Ref. values Anti-nuclear antibodies (ANA) Negative < 1/100 Anti-Ds DNA antibodies < 10. 0 UI/m. L < 100 Anti-CCP < 0. 4 U/m. L <7 Rheumatoid factor < 10. 0 UI/m. L < 30 Anti-ENA antibodies anti-Jo 1 Negative anti-RNP Negative anti-SCL 70 Negative anti-Sm Negative anti-SSa Negative anti- SSb Negative
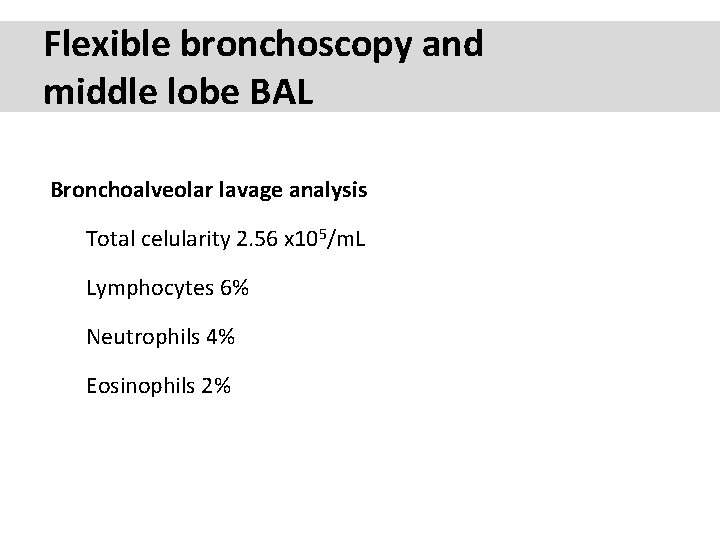
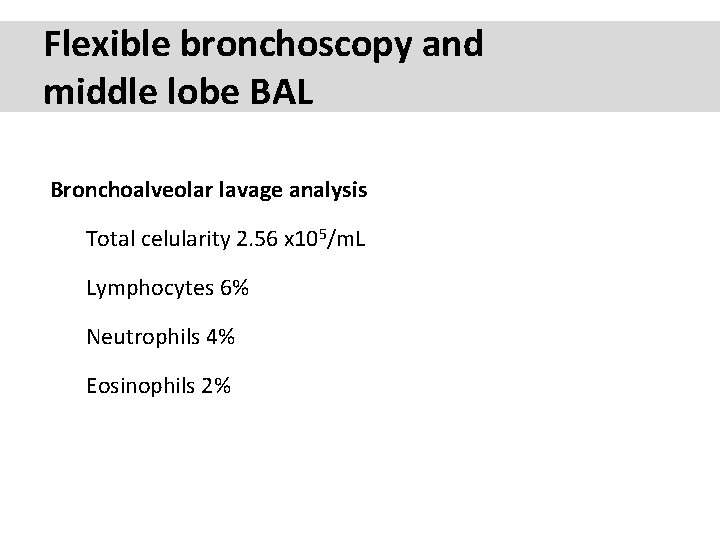
Flexible bronchoscopy and middle lobe BAL Bronchoalveolar lavage analysis Total celularity 2. 56 x 105/m. L Lymphocytes 6% Neutrophils 4% Eosinophils 2%
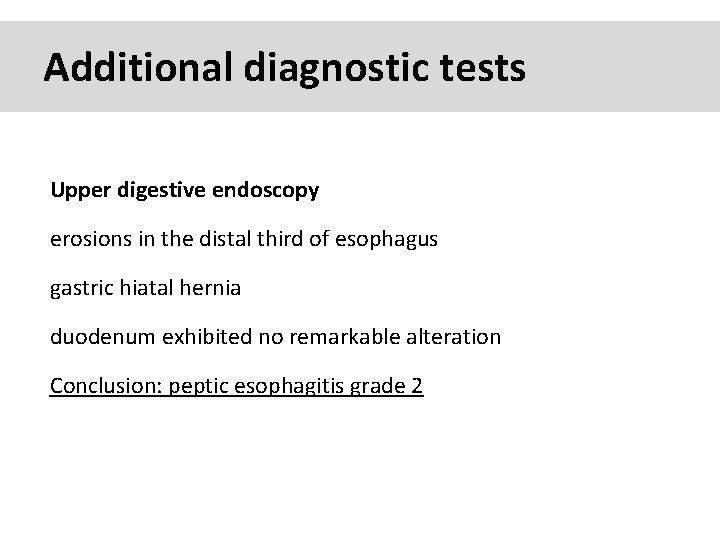
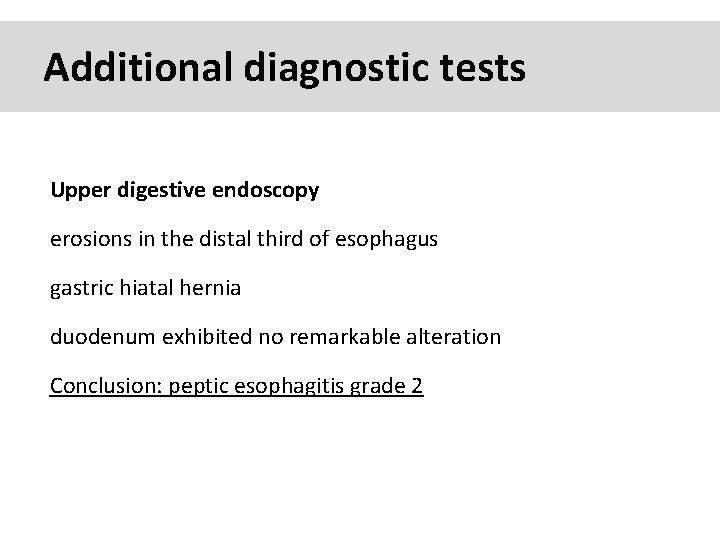
Additional diagnostic tests Upper digestive endoscopy erosions in the distal third of esophagus gastric hiatal hernia duodenum exhibited no remarkable alteration Conclusion: peptic esophagitis grade 2
39 yo caucasian male, works in car collision repair and painting Multiple allergies, Gastroesophageal reflux disease and Thrombocytopenia of unknown etiology Smoker. No drugs CT: Reticular abnormality and honeycombing of subpleural basal predominance + micronodules Lung function tests: decreased diffusion capacity of the lung Blood tests: small increase of ESR and CRP; Autoimmune screening blood tests were normal BAL: normal celularity, with a mild increase in the neutrophil and eosinophil count
39 yo caucasian male, works in car collision repair and painting Multiple allergies, Gastroesophageal reflux disease and Thrombocytopenia of unknown etiology Smoker. No drugs CT: Reticular abnormality and honeycombing of subpleural basal predominance + micronodules Lung function tests: decreased diffusion capacity of the lung Blood tests: small increase of ESR and CRP; Autoimmune Screening Blood Tests were normal BAL: normal celularity, with a mild increase in the neutrophil and eosinophil count Definitive diagnosis can be established? Additional diagnostic tests required? Which tests?
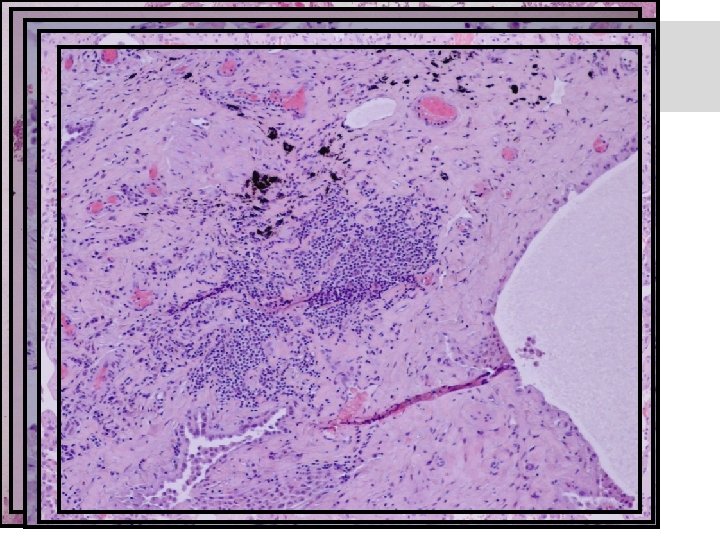
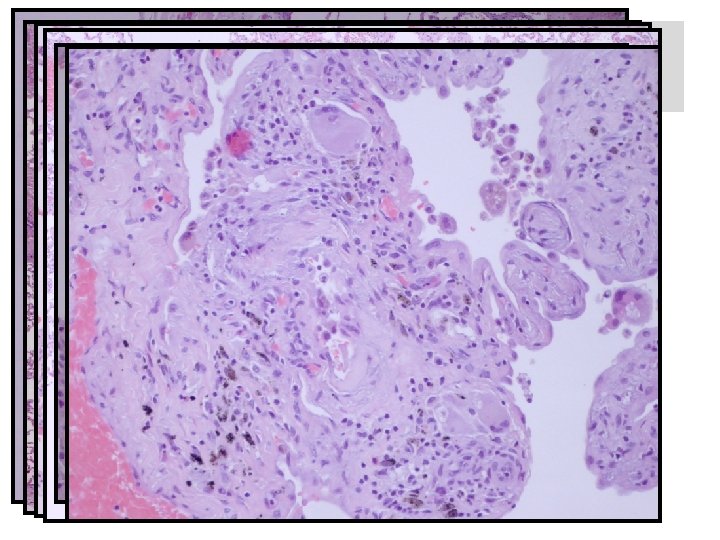
Transbronchial cryobiopsy - Peribronchiolar fibrosis, associated to the presence of inflammatory cells infiltration, mostly lymphoplasmacytic and some aggregates of neutrophils - Focal subepitelial loose fibrosis (fibroblastic foci? ) Inconclusive
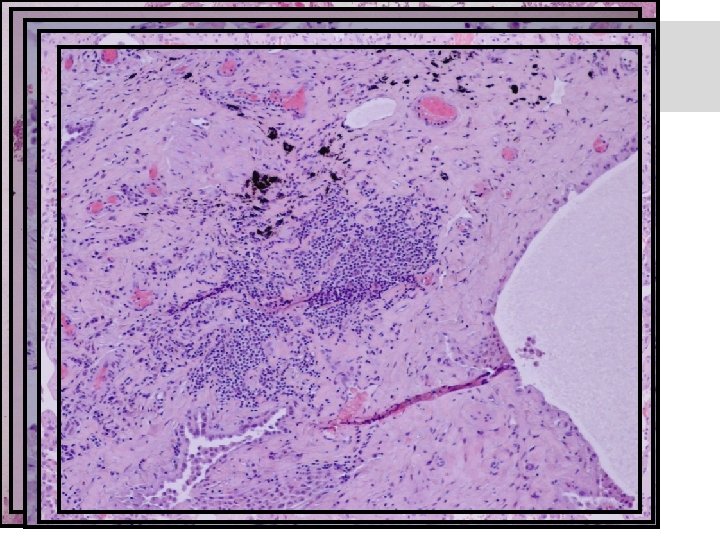
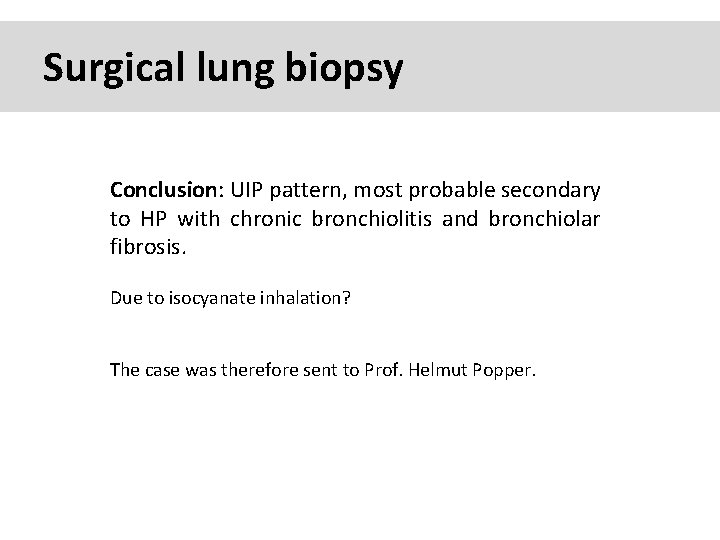
Surgical lung biopsy
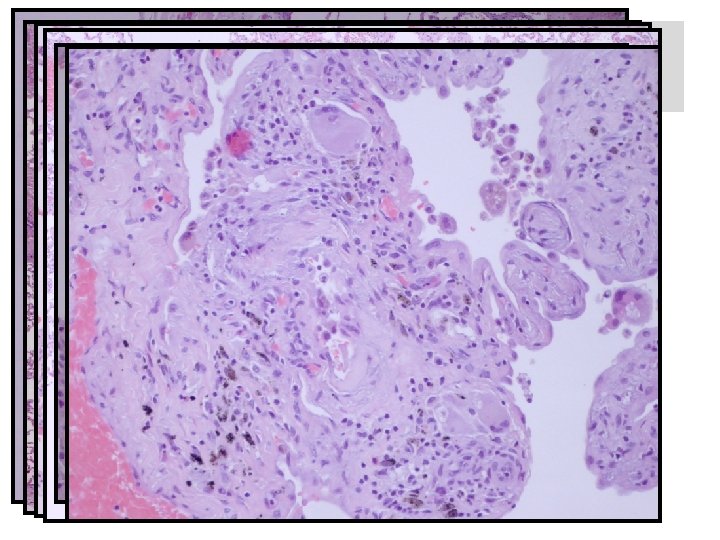
Surgical lung biopsy
Surgical lung biopsy Conclusion: UIP pattern, most probable secondary to HP with chronic bronchiolitis and bronchiolar fibrosis. Due to isocyanate inhalation? The case was therefore sent to Prof. Helmut Popper.
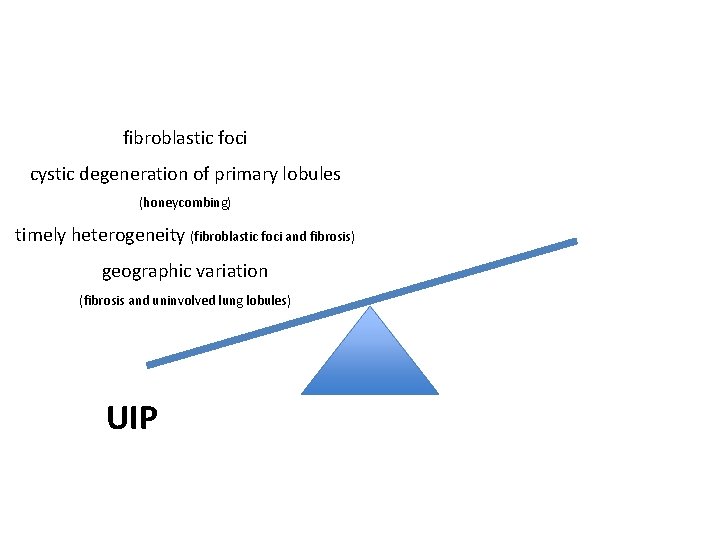
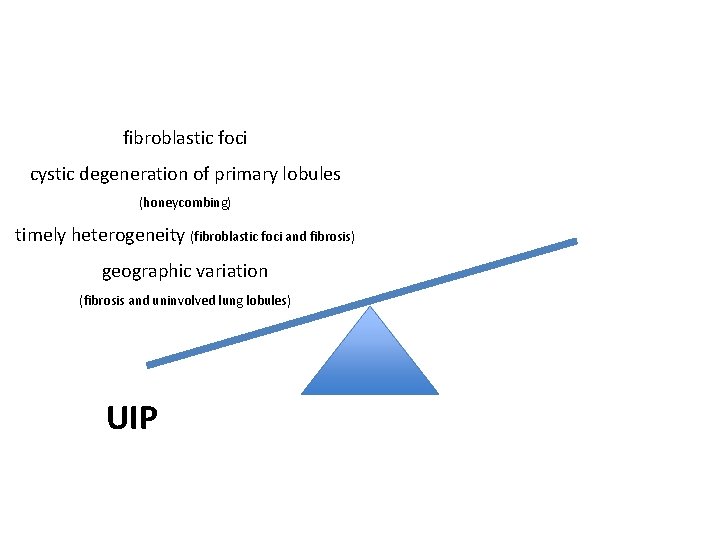
fibroblastic foci cystic degeneration of primary lobules (honeycombing) timely heterogeneity (fibroblastic foci and fibrosis) geographic variation (fibrosis and uninvolved lung lobules) UIP
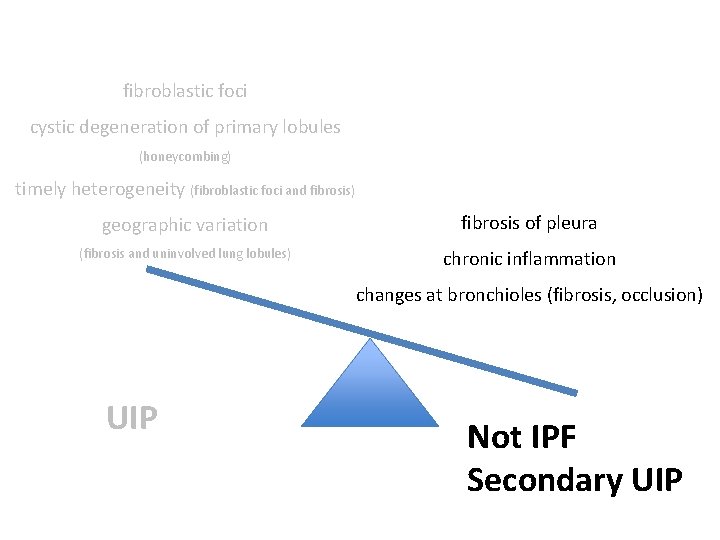
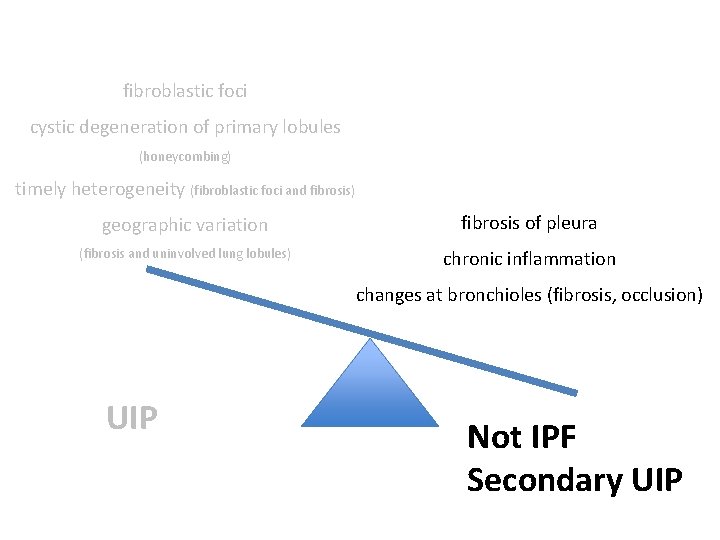
fibroblastic foci cystic degeneration of primary lobules (honeycombing) timely heterogeneity (fibroblastic foci and fibrosis) geographic variation fibrosis of pleura (fibrosis and uninvolved lung lobules) chronic inflammation changes at bronchioles (fibrosis, occlusion) UIP Not IPF Secondary UIP
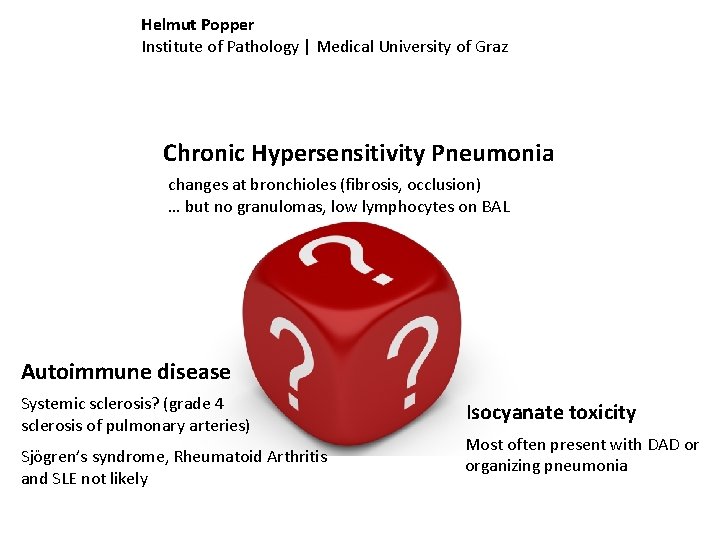
Helmut Popper Institute of Pathology | Medical University of Graz Chronic Hypersensitivity Pneumonia changes at bronchioles (fibrosis, occlusion) … but no granulomas, low lymphocytes on BAL Autoimmune disease Systemic sclerosis? (grade 4 sclerosis of pulmonary arteries) Sjögren’s syndrome, Rheumatoid Arthritis and SLE not likely Isocyanate toxicity Most often present with DAD or organizing pneumonia
What’s the most probable diagnosis? Which treatment is indicated? Should he be advised to change job?