Interstial lung disease Chronic diffuse interstitial restrictive lung

- Slides: 43
Interstial lung disease
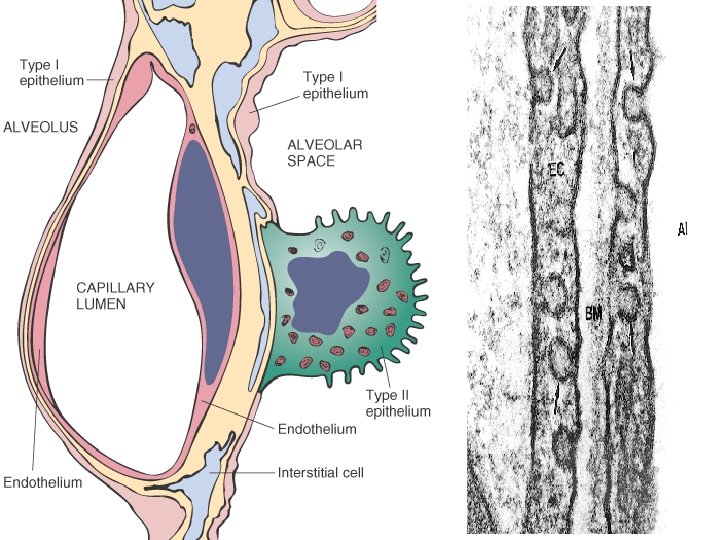
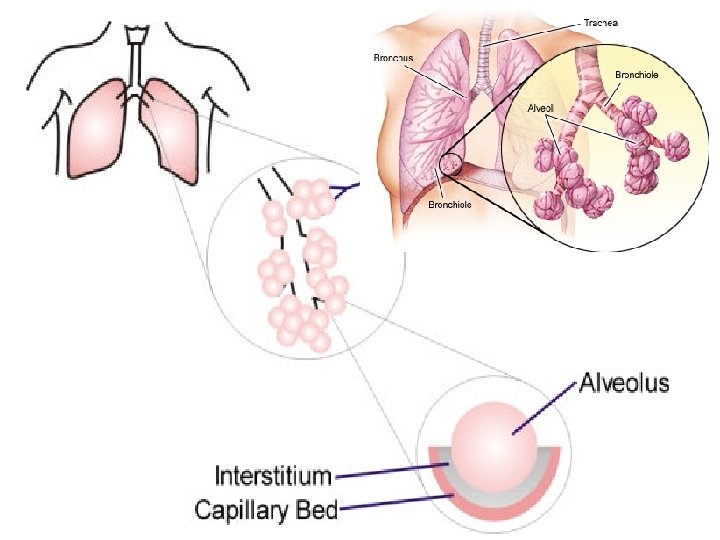
Chronic diffuse interstitial restrictive lung disease • Heterogenous group of diseases characterized by Inflammation & fibrosis of most peripheral interstitial connective tissue in the alveolar walls • • • It concerns alveolar epithelium, pulmonary capillary endothelium, basement membrane, perivascular and perilymphatic tissues.
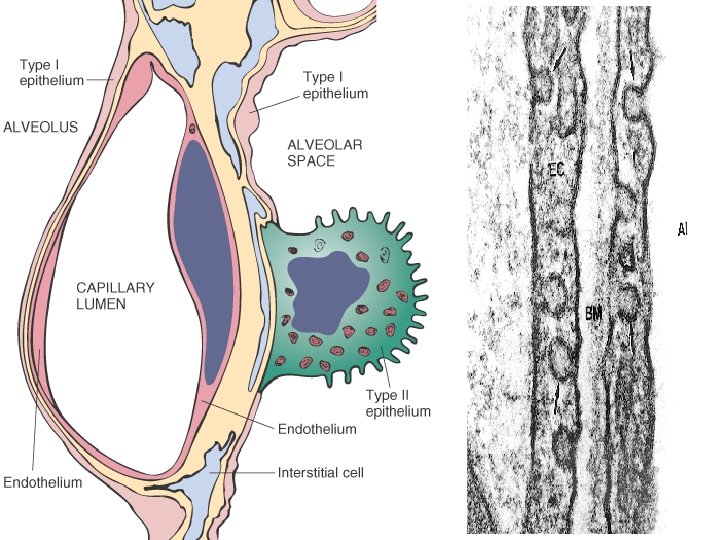
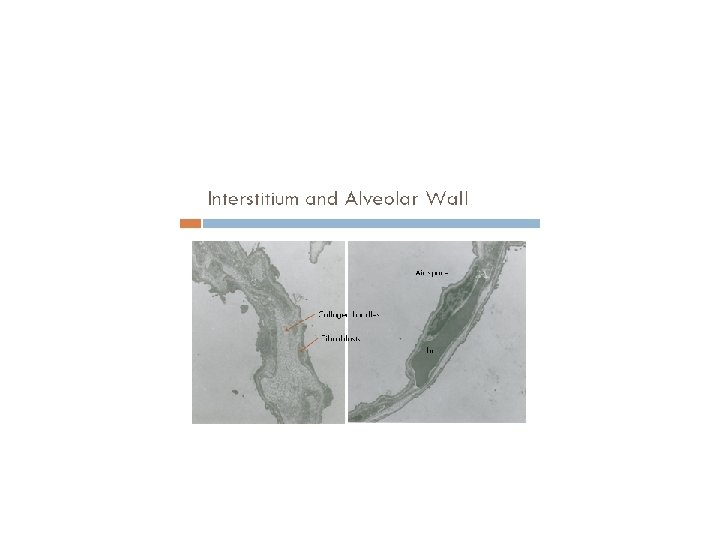
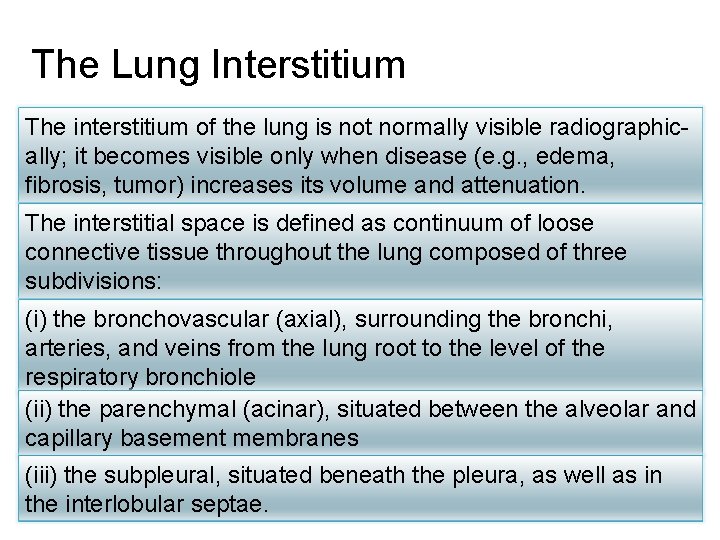
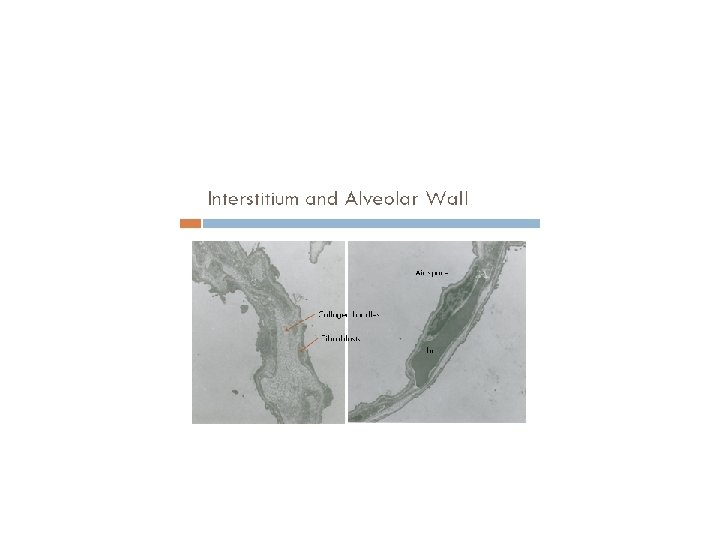
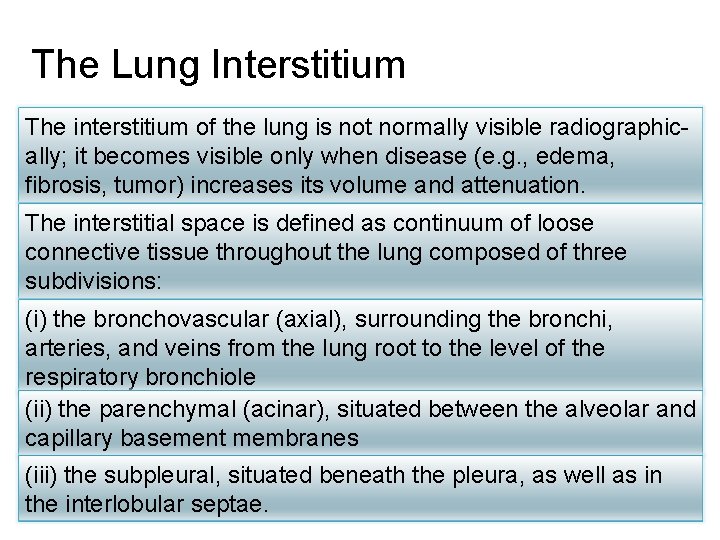
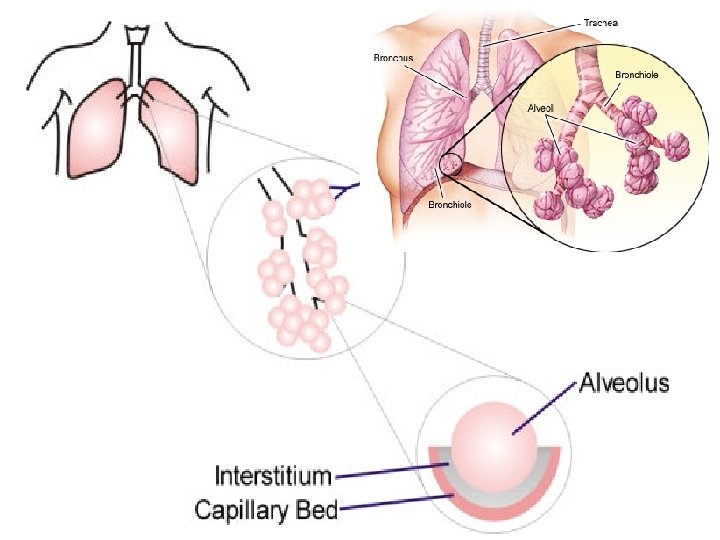
The Lung Interstitium The interstitium of the lung is not normally visible radiographically; it becomes visible only when disease (e. g. , edema, fibrosis, tumor) increases its volume and attenuation. The interstitial space is defined as continuum of loose connective tissue throughout the lung composed of three subdivisions: (i) the bronchovascular (axial), surrounding the bronchi, arteries, and veins from the lung root to the level of the respiratory bronchiole (ii) the parenchymal (acinar), situated between the alveolar and capillary basement membranes (iii) the subpleural, situated beneath the pleura, as well as in the interlobular septae.
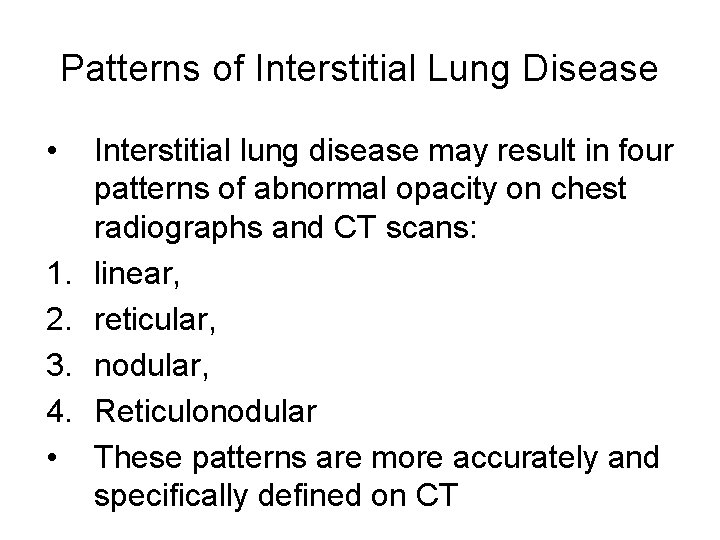
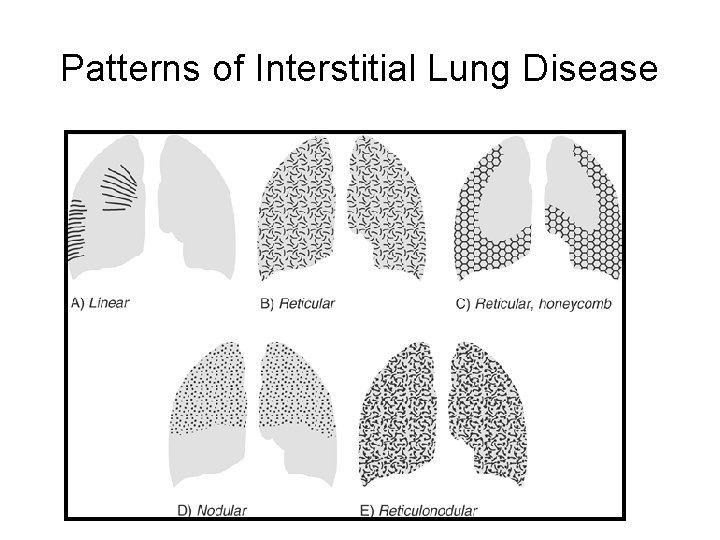
Patterns of Interstitial Lung Disease • 1. 2. 3. 4. • Interstitial lung disease may result in four patterns of abnormal opacity on chest radiographs and CT scans: linear, reticular, nodular, Reticulonodular These patterns are more accurately and specifically defined on CT
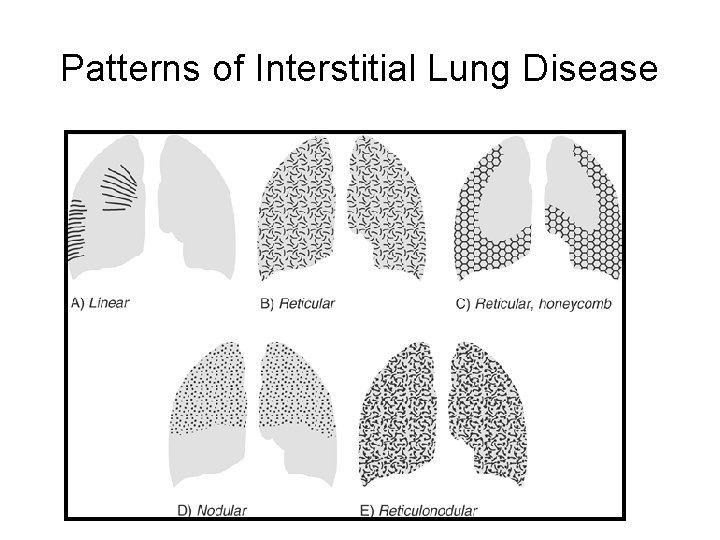
Patterns of Interstitial Lung Disease
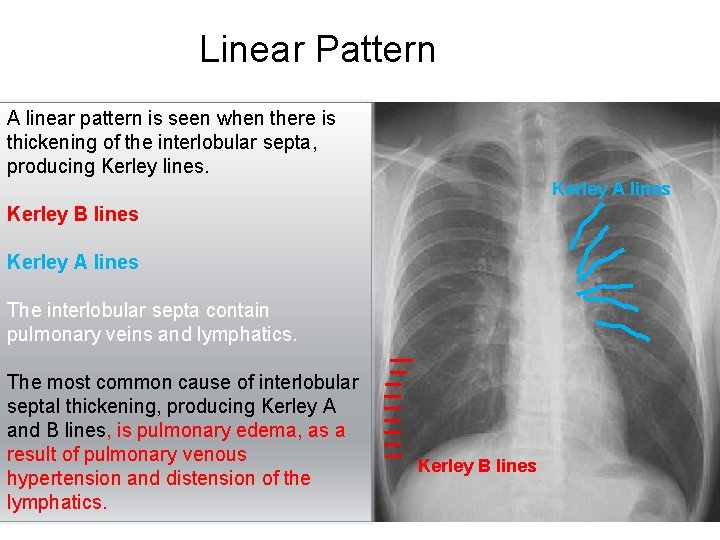
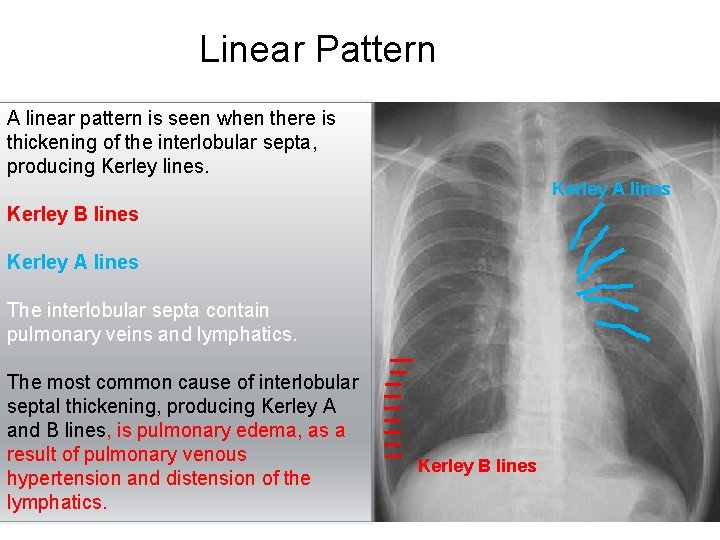
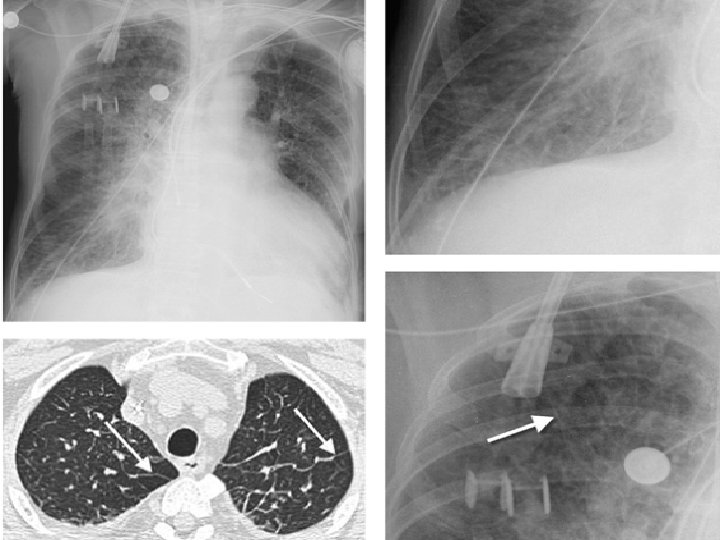
Linear Pattern A linear pattern is seen when there is thickening of the interlobular septa, producing Kerley lines. Kerley A lines Kerley B lines Kerley A lines The interlobular septa contain pulmonary veins and lymphatics. The most common cause of interlobular septal thickening, producing Kerley A and B lines, is pulmonary edema, as a result of pulmonary venous hypertension and distension of the lymphatics. Kerley B lines
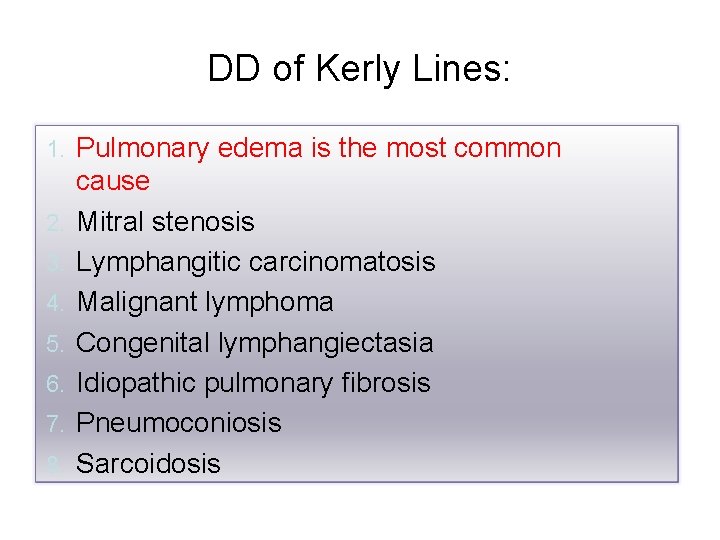
DD of Kerly Lines: 1. 2. 3. 4. 5. 6. 7. 8. Pulmonary edema is the most common cause Mitral stenosis Lymphangitic carcinomatosis Malignant lymphoma Congenital lymphangiectasia Idiopathic pulmonary fibrosis Pneumoconiosis Sarcoidosis
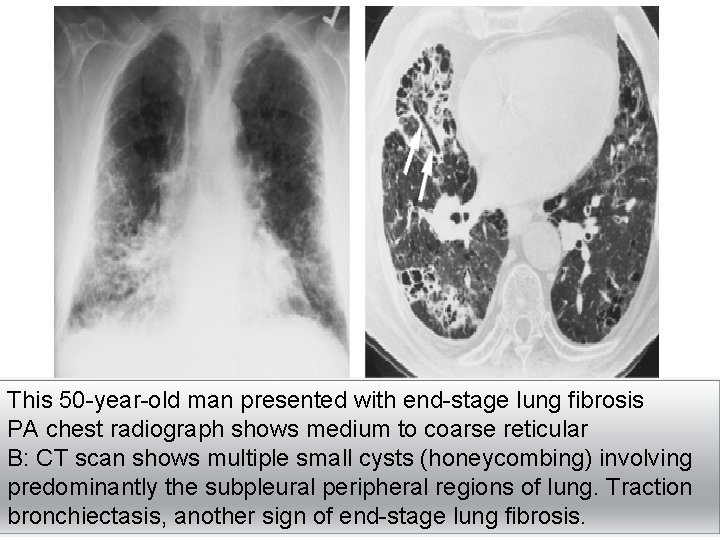
b. Reticular Pattern A reticular pattern results from the summation or superimposition of irregular linear opacities. The term reticular is defined as meshed, or in the form of a network. Reticular opacities can be described as fine, medium, or coarse, as the width of the opacities increases. A classic reticular pattern is seen with pulmonary fibrosis, in which multiple curvilinear opacities form small cystic spaces along the pleural margins and lung bases (honeycomb lung)
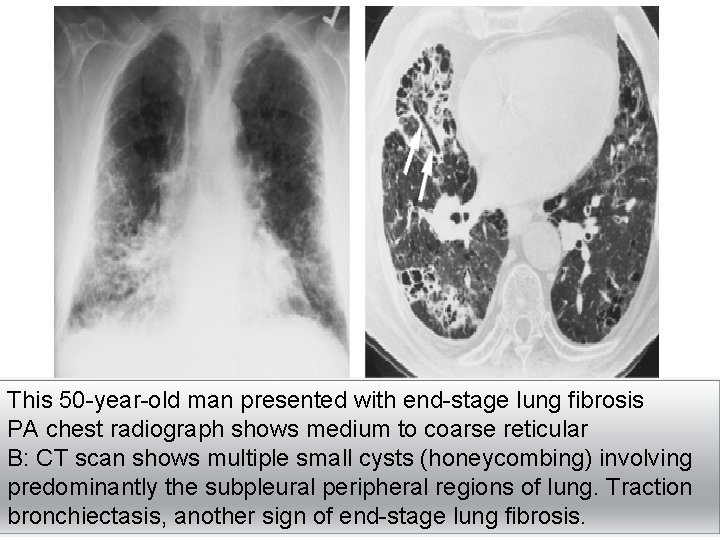
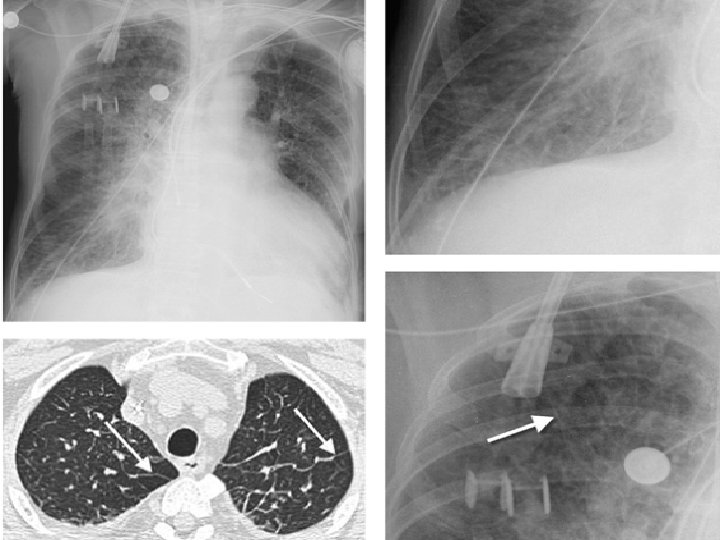
This 50 -year-old man presented with end-stage lung fibrosis PA chest radiograph shows medium to coarse reticular B: CT scan shows multiple small cysts (honeycombing) involving predominantly the subpleural peripheral regions of lung. Traction bronchiectasis, another sign of end-stage lung fibrosis.
c. Nodular pattern A nodular pattern consists of multiple round opacities, generally ranging in diameter from 1 mm to 1 cm Nodular opacities may be described as miliary (1 to 2 mm, the size of millet seeds), small, medium, or large, as the diameter of the opacities increases A nodular pattern, especially with predominant distribution, suggests a specific differential diagnosis
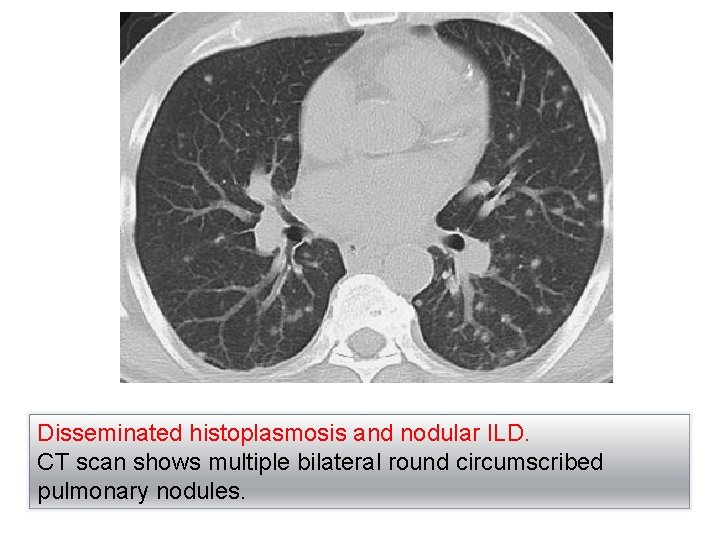
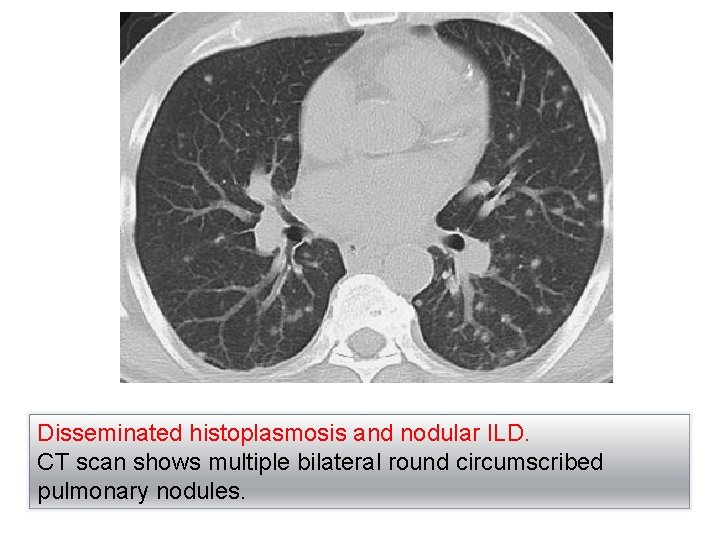
Disseminated histoplasmosis and nodular ILD. CT scan shows multiple bilateral round circumscribed pulmonary nodules.
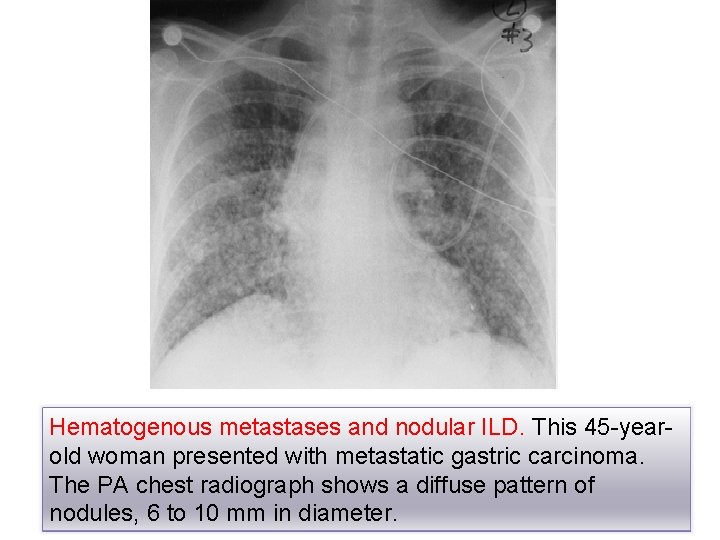
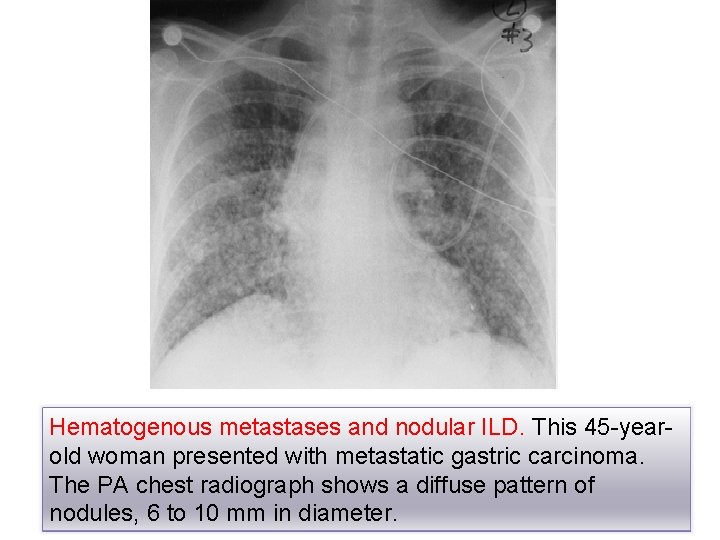
Hematogenous metastases and nodular ILD. This 45 -yearold woman presented with metastatic gastric carcinoma. The PA chest radiograph shows a diffuse pattern of nodules, 6 to 10 mm in diameter.
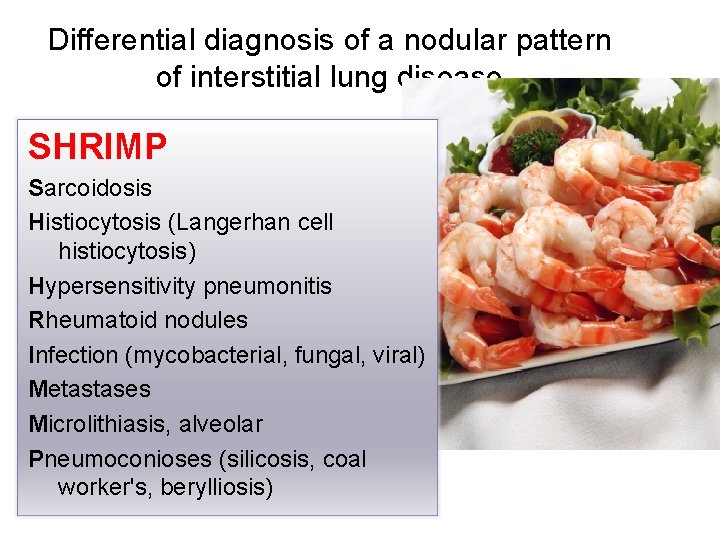
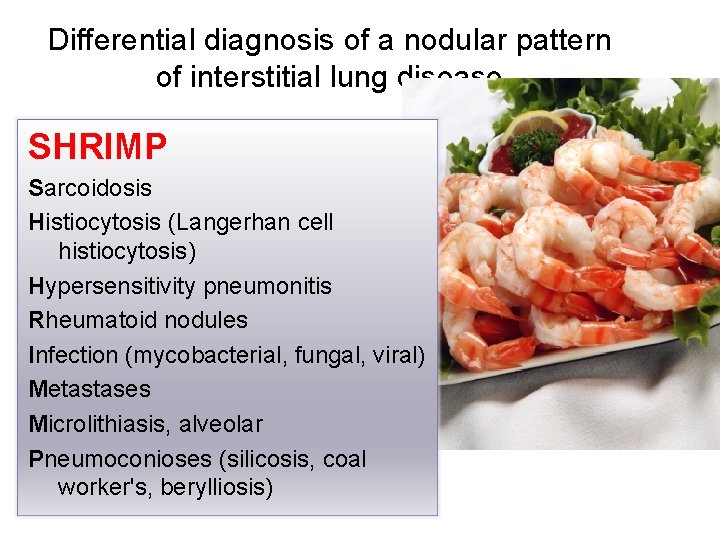
Differential diagnosis of a nodular pattern of interstitial lung disease SHRIMP Sarcoidosis Histiocytosis (Langerhan cell histiocytosis) Hypersensitivity pneumonitis Rheumatoid nodules Infection (mycobacterial, fungal, viral) Metastases Microlithiasis, alveolar Pneumoconioses (silicosis, coal worker's, berylliosis)
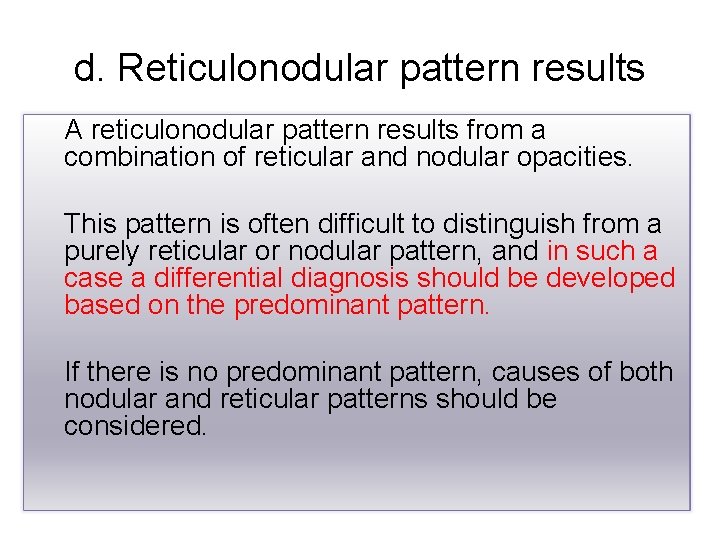
d. Reticulonodular pattern results A reticulonodular pattern results from a combination of reticular and nodular opacities. This pattern is often difficult to distinguish from a purely reticular or nodular pattern, and in such a case a differential diagnosis should be developed based on the predominant pattern. If there is no predominant pattern, causes of both nodular and reticular patterns should be considered.
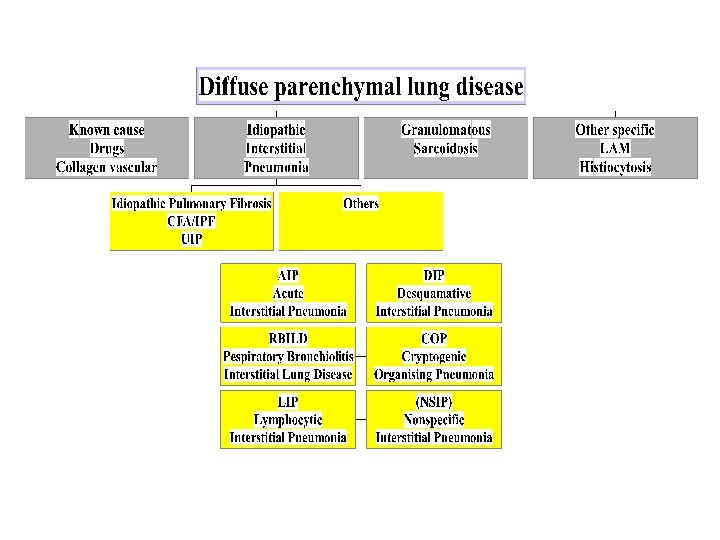
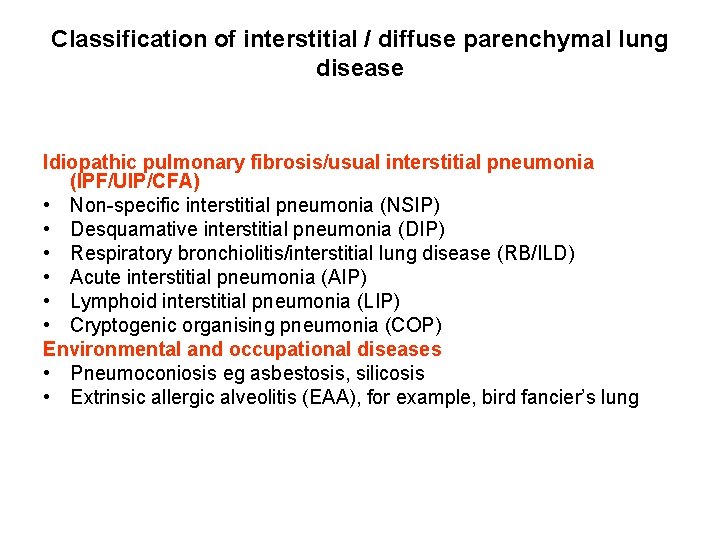
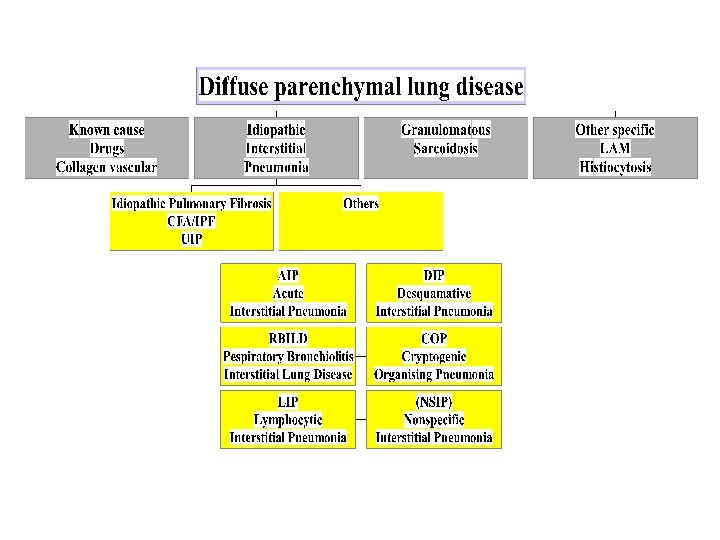
Classification of interstitial / diffuse parenchymal lung disease Idiopathic pulmonary fibrosis/usual interstitial pneumonia (IPF/UIP/CFA) • Non-specific interstitial pneumonia (NSIP) • Desquamative interstitial pneumonia (DIP) • Respiratory bronchiolitis/interstitial lung disease (RB/ILD) • Acute interstitial pneumonia (AIP) • Lymphoid interstitial pneumonia (LIP) • Cryptogenic organising pneumonia (COP) Environmental and occupational diseases • Pneumoconiosis eg asbestosis, silicosis • Extrinsic allergic alveolitis (EAA), for example, bird fancier’s lung
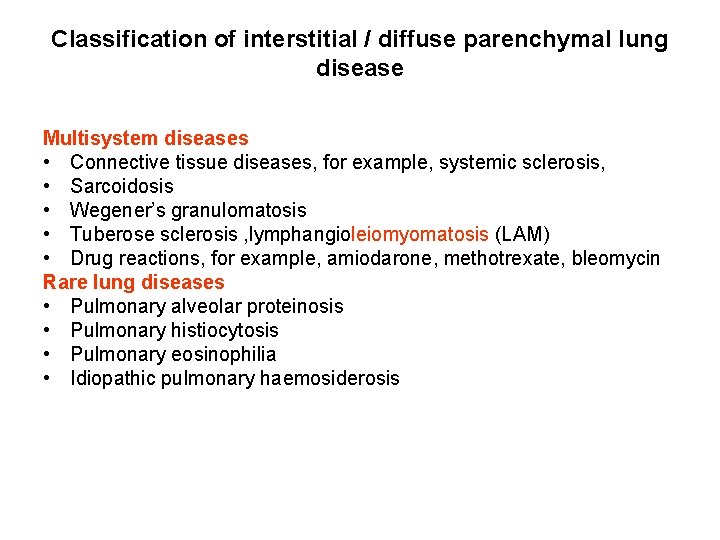
Classification of interstitial / diffuse parenchymal lung disease Multisystem diseases • Connective tissue diseases, for example, systemic sclerosis, • Sarcoidosis • Wegener’s granulomatosis • Tuberose sclerosis , lymphangioleiomyomatosis (LAM) • Drug reactions, for example, amiodarone, methotrexate, bleomycin Rare lung diseases • Pulmonary alveolar proteinosis • Pulmonary histiocytosis • Pulmonary eosinophilia • Idiopathic pulmonary haemosiderosis
Chronic diffuse interstitial lung diseases • RESTRICTIVE (INFILTRATIVE) • Dyspnea, tachypnea, end inspiratory crackles without airway obstruction. • ↓ CO diffusing capacity, ↓lung volume. ↓compliance. • Honey-comb lung • Secondary pulmonary hypertention • Corpulmonale
Chronic diffuse interstitial lung diseases • • Restrictive (infiltrative) Reduced compliance, reduced gas exchange) Are also diffuse Heterogeneous main categories of CILD 1. 2. 3. 4. 5. FIBROSING GRANULOMATOUS EOSINOPHILIC SMOKING RELATED PAP (Pulmonary Alveolar Proteinosis)
1. FIBROSING • Usual interstitial pneumonia-Idiopathic pulmonary fibrosis (UIP-IPF-CFA). • Nonspecific interstitial pneumonia / fibrosis • Cryptogenic organizing pneumonia • Connective tissue (Collagen vascular) diseases • Pneumoconioses • Drug reactions • Radiation changes
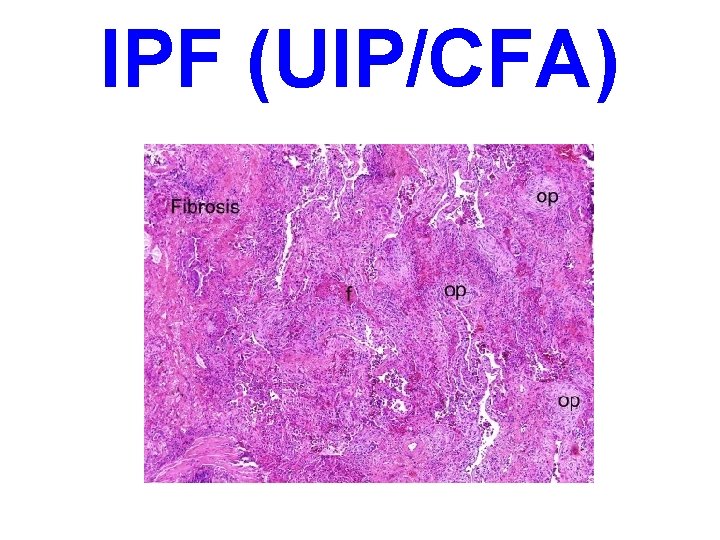
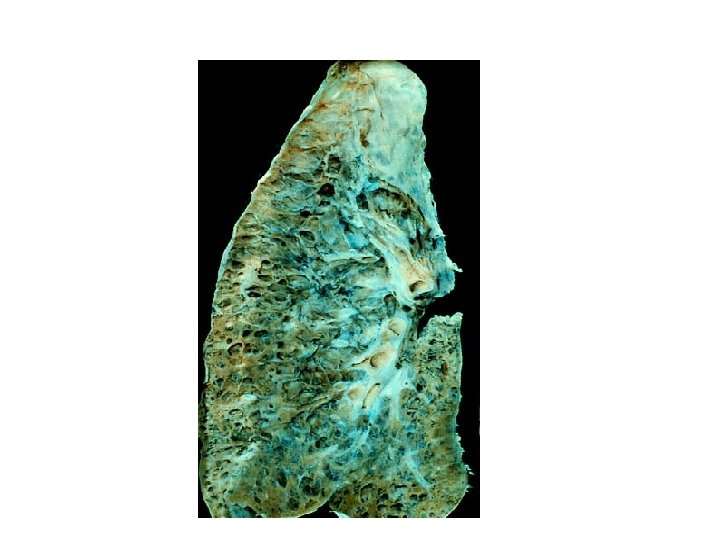
IPF (UIP/CFA) • Cobblestone pleural surface by retraction scar along interlobular septa. • Lower lobe subpleural & interlobular septal fibrosis. • Fibroblastic foci - honeycomb fibrosis
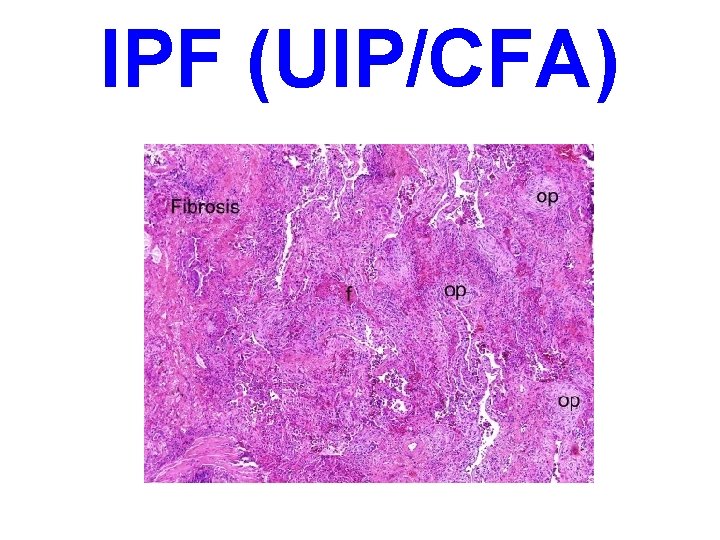
IPF (UIP/CFA)
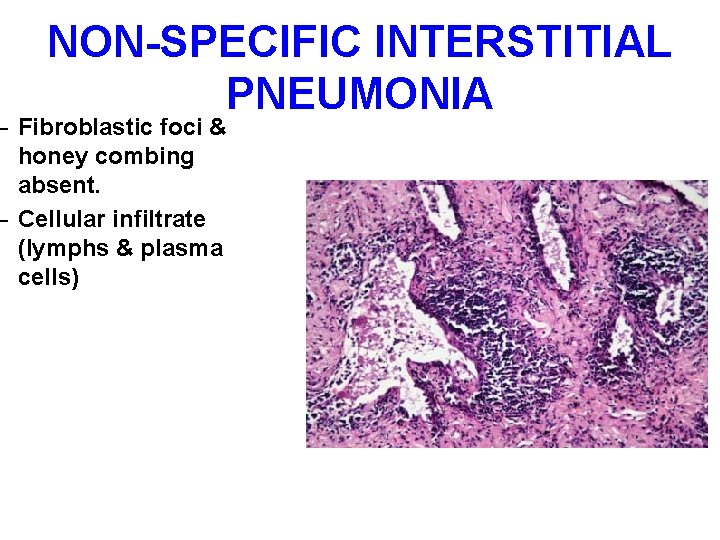
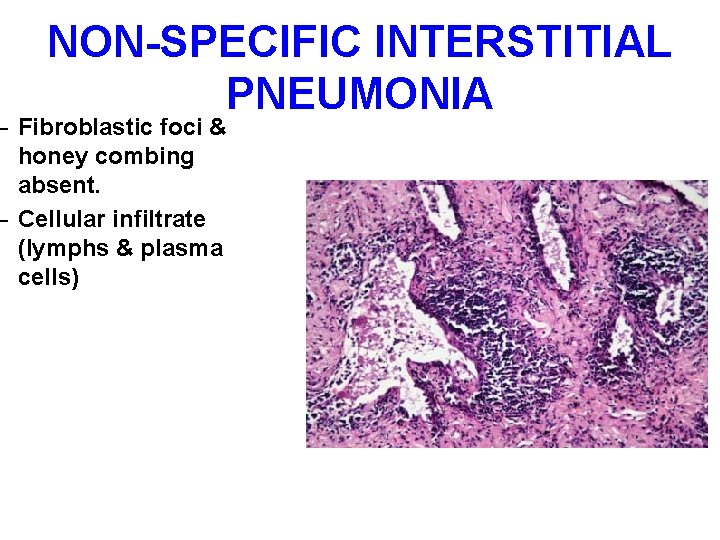
NON-SPECIFIC INTERSTITIAL PNEUMONIA – Fibroblastic foci & honey combing absent. – Cellular infiltrate (lymphs & plasma cells)
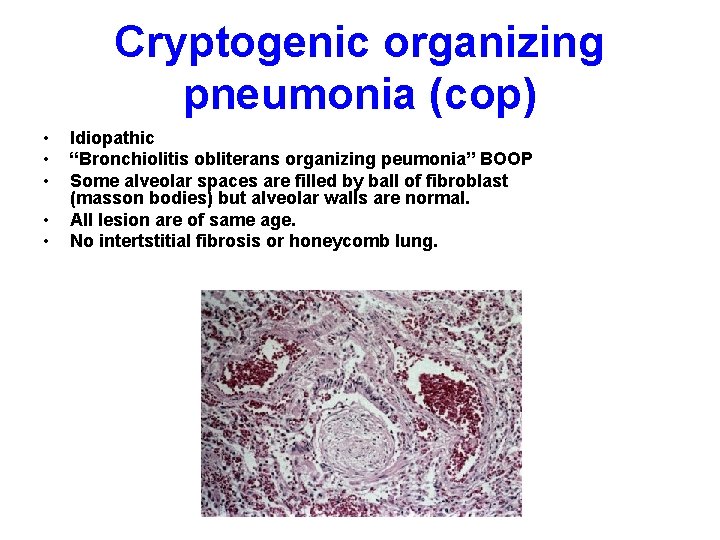
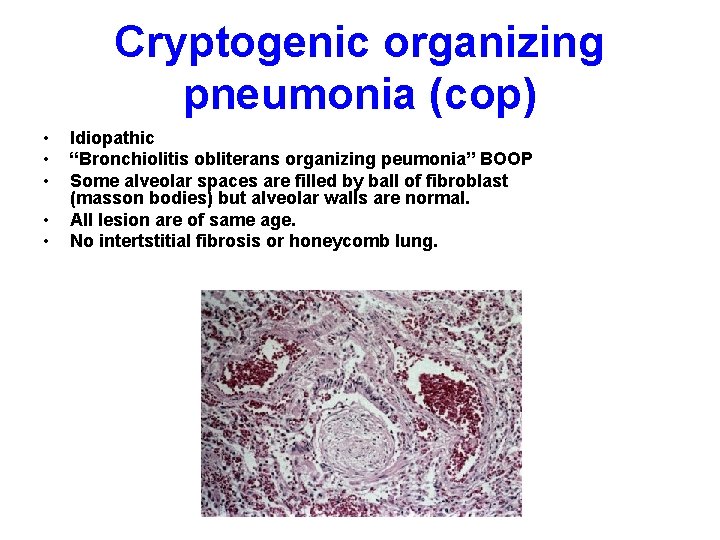
Cryptogenic organizing pneumonia (cop) • • • Idiopathic “Bronchiolitis obliterans organizing peumonia” BOOP Some alveolar spaces are filled by ball of fibroblast (masson bodies) but alveolar walls are normal. All lesion are of same age. No intertstitial fibrosis or honeycomb lung.
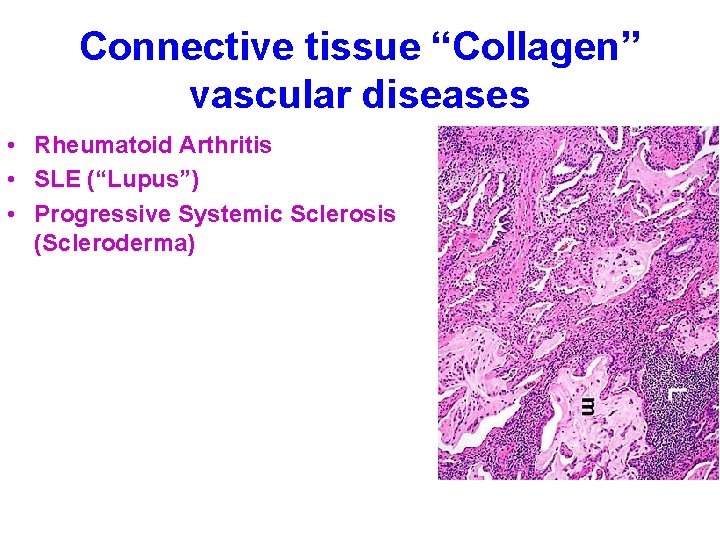
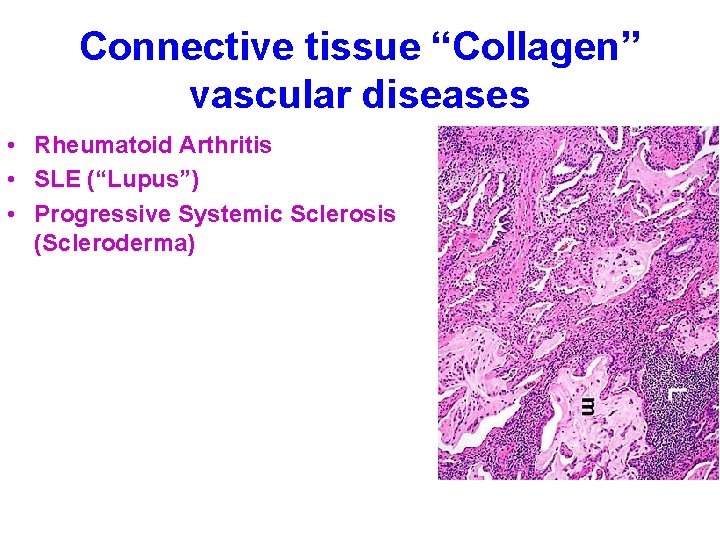
Connective tissue “Collagen” vascular diseases • Rheumatoid Arthritis • SLE (“Lupus”) • Progressive Systemic Sclerosis (Scleroderma)
Pneumoconioses • Non-neoplastic lung reaction to inhalation of mineral dust or chemicals or organic materials • “Occupational”-“Coal miners lung” • 1 -5µm diameter particles can reach airsacs & settle in their linning. – Coal (anthracosis) – Silica – Asbestos – Be, Fe. O, Ba. So 4, Tin oxide – HAY, FLAX, Benzene, Insecticides, etc.
Pneumoconioses • • • Coal workers peumoconiosis CWP Asymtomatic anthracosis Simple CWP Complicated CWP or PMF Silicosis Hard collagenous scars in upper lobes of lung • Eggshell calcification of lymphnodes
Pneumoconioses • • Asbestos-related disease Localized fibrous plaque Pleural effusions Interstitial fibrosis Carcinoma lung Mesothelioma Laryngeal or colonic carcinomas

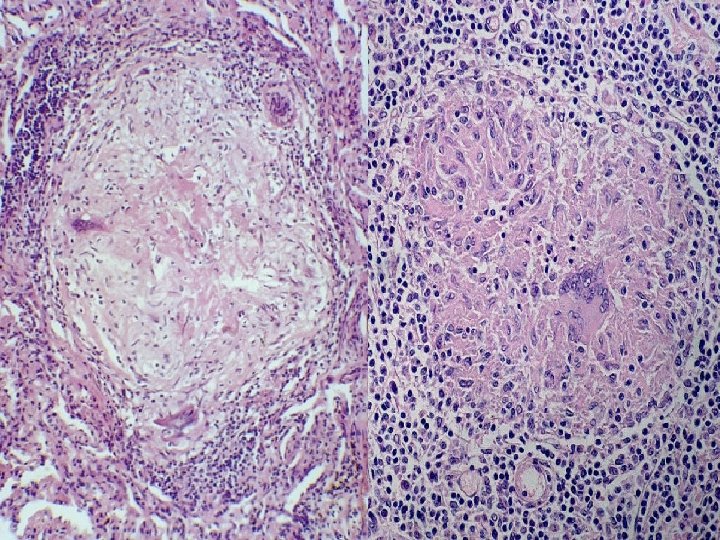
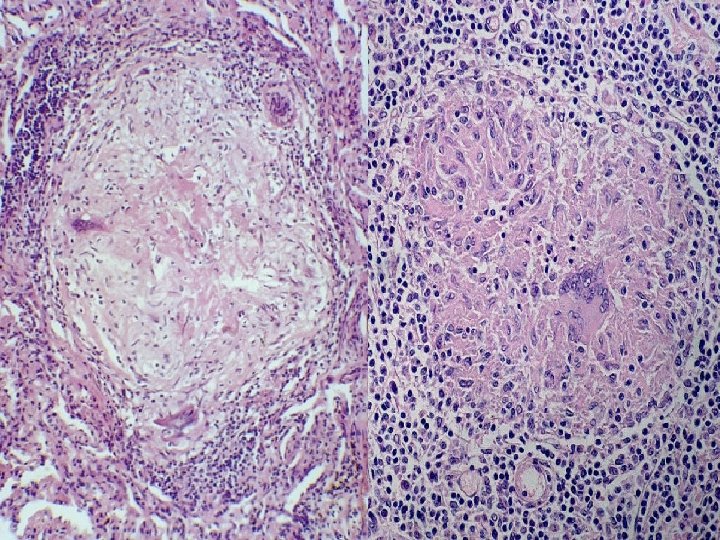
2. Granulomatous • Sarcoidosis, • Hypersensitivity peumonitis
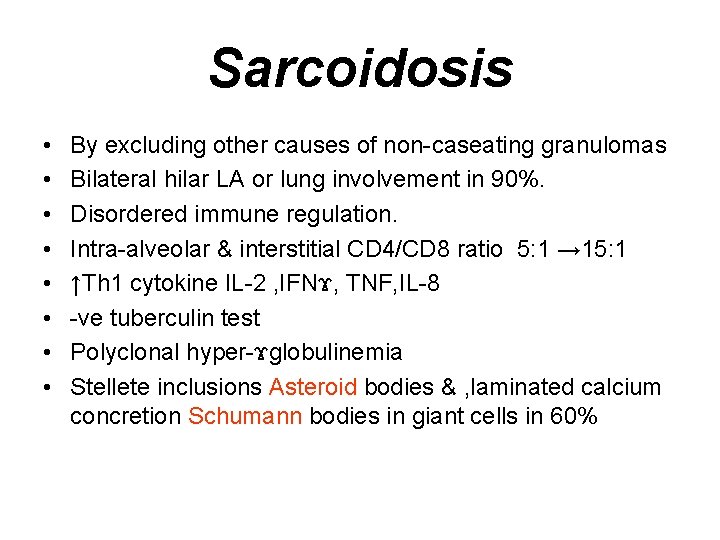
Sarcoidosis • • By excluding other causes of non-caseating granulomas Bilateral hilar LA or lung involvement in 90%. Disordered immune regulation. Intra-alveolar & interstitial CD 4/CD 8 ratio 5: 1 → 15: 1 ↑Th 1 cytokine IL-2 , IFNϫ, TNF, IL-8 -ve tuberculin test Polyclonal hyper-ϫglobulinemia Stellete inclusions Asteroid bodies & , laminated calcium concretion Schumann bodies in giant cells in 60%
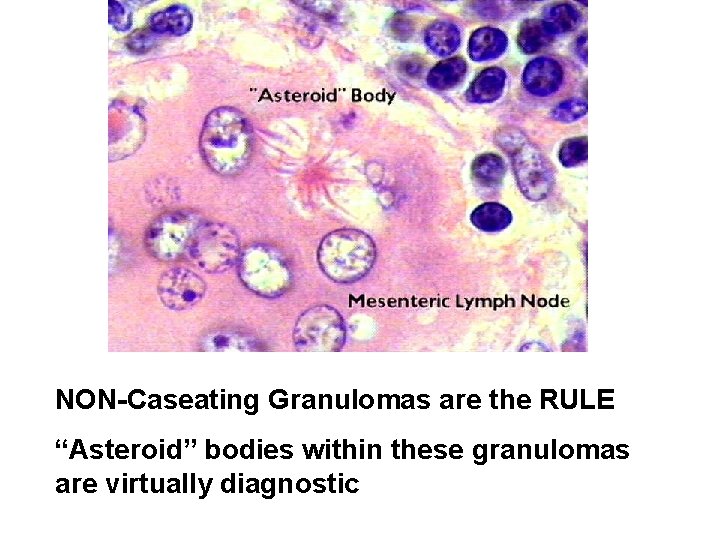
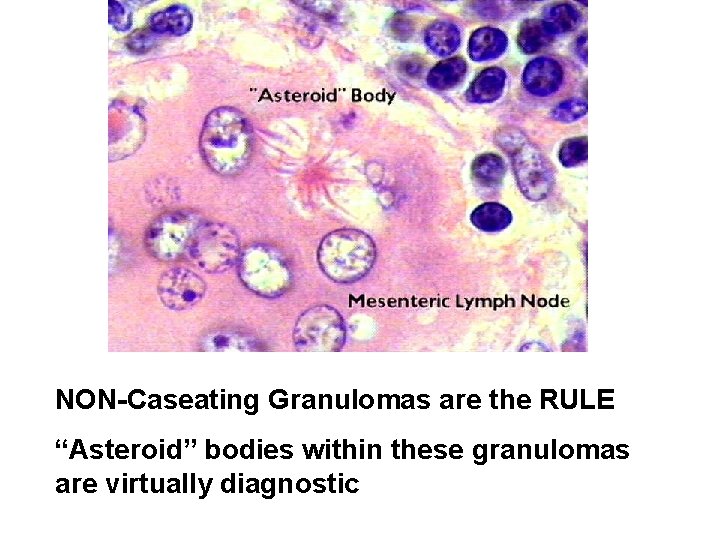
NON-Caseating Granulomas are the RULE “Asteroid” bodies within these granulomas are virtually diagnostic
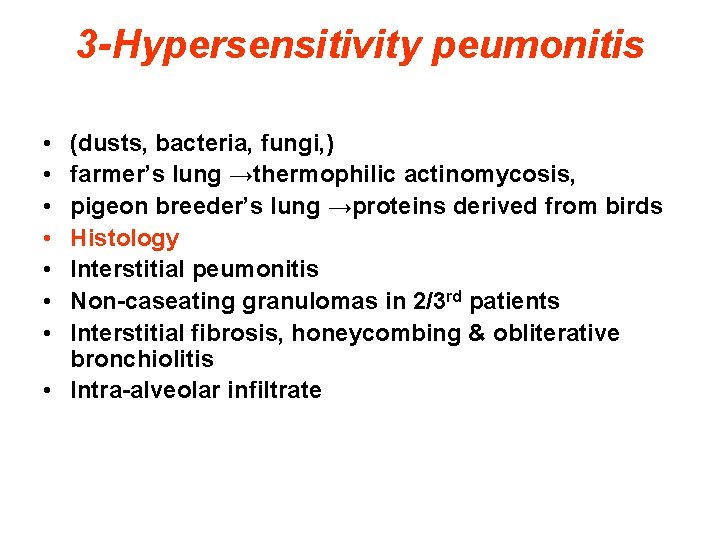
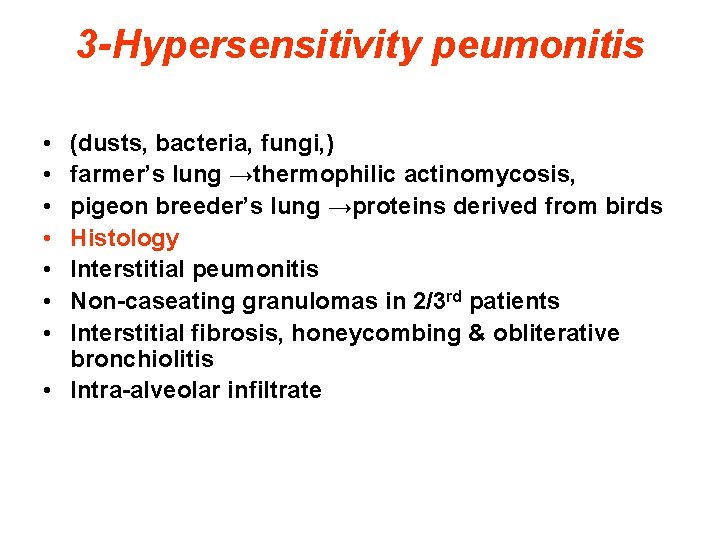
3 -Hypersensitivity peumonitis • • (dusts, bacteria, fungi, ) farmer’s lung →thermophilic actinomycosis, pigeon breeder’s lung →proteins derived from birds Histology Interstitial peumonitis Non-caseating granulomas in 2/3 rd patients Interstitial fibrosis, honeycombing & obliterative bronchiolitis • Intra-alveolar infiltrate
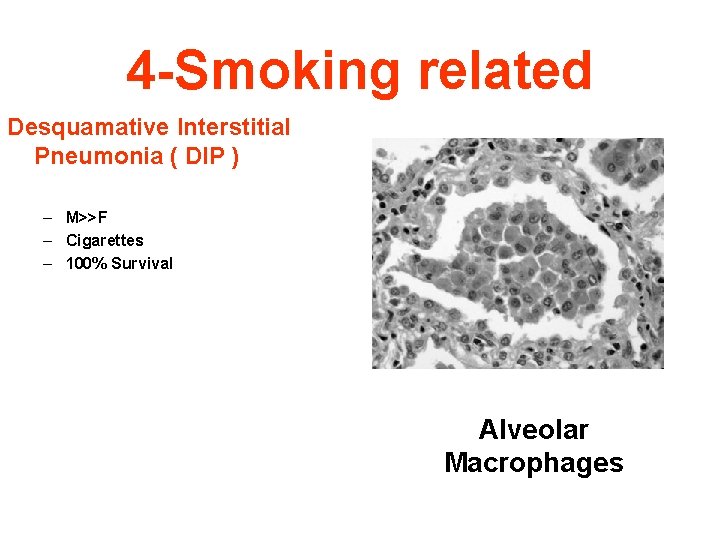
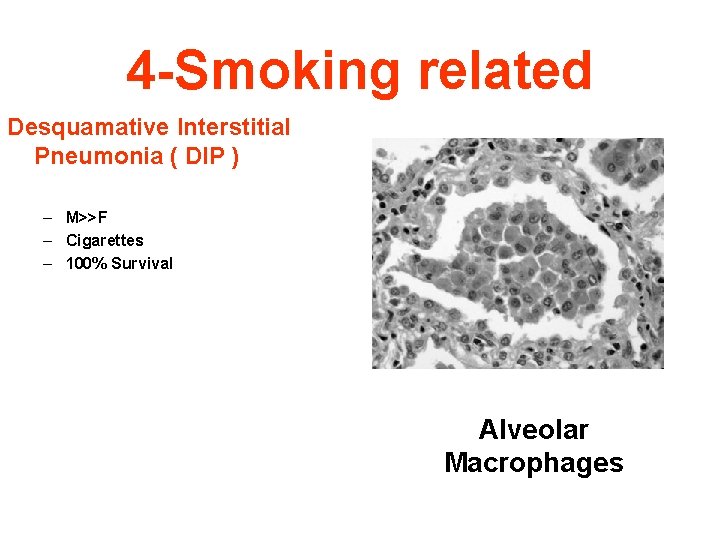
4 -Smoking related Desquamative Interstitial Pneumonia ( DIP ) – M>>F – Cigarettes – 100% Survival Alveolar Macrophages
4 -Smoking related • Respiratory Bronchiolitis-Associated Interstitial Lung Disease • Pigmented intraluminal macrophages within Resp. bronchioles. Macrophages are similar to those in DIP.
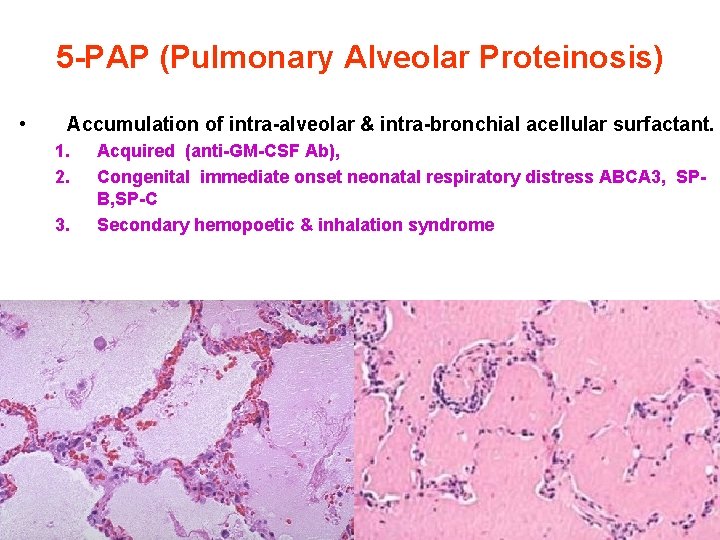
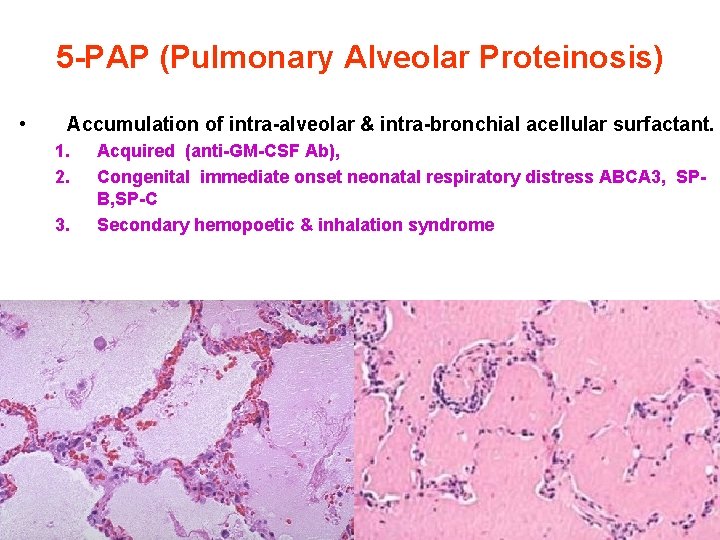
5 -PAP (Pulmonary Alveolar Proteinosis) • Accumulation of intra-alveolar & intra-bronchial acellular surfactant. 1. 2. 3. Acquired (anti-GM-CSF Ab), Congenital immediate onset neonatal respiratory distress ABCA 3, SPB, SP-C Secondary hemopoetic & inhalation syndrome
END