PARENCHYMAL LIVER DISEASE l Parenchymal liver disease may



- Slides: 25
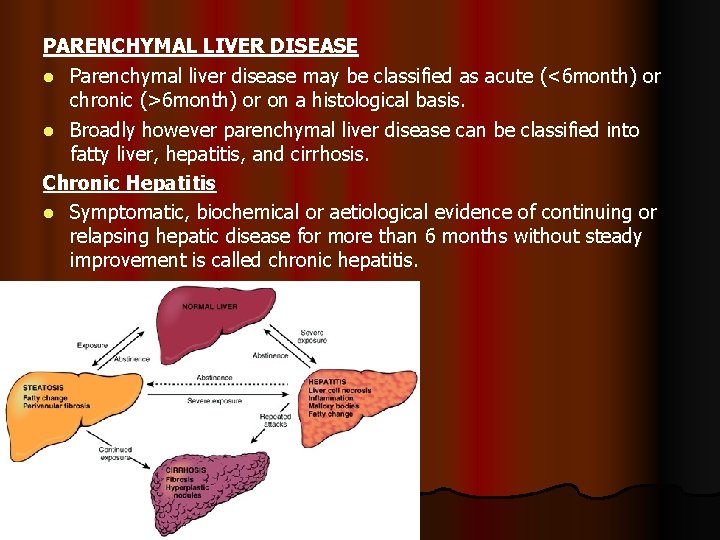
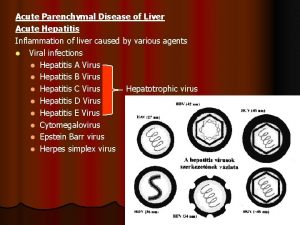
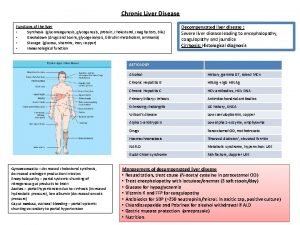
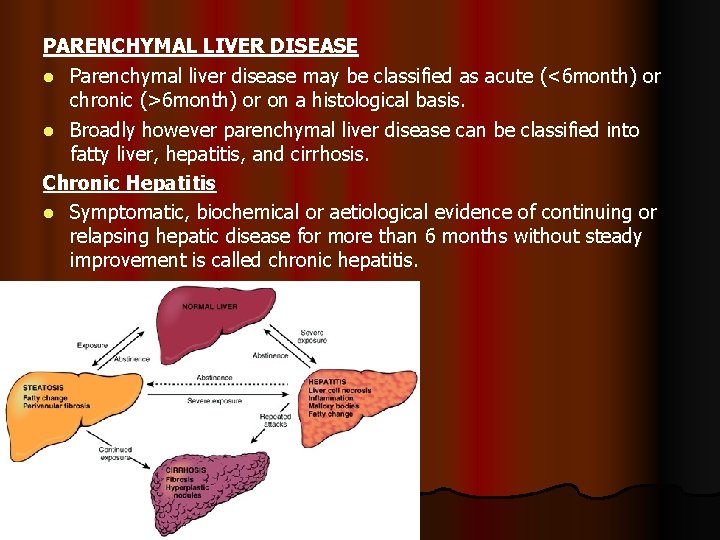
PARENCHYMAL LIVER DISEASE l Parenchymal liver disease may be classified as acute (<6 month) or chronic (>6 month) or on a histological basis. l Broadly however parenchymal liver disease can be classified into fatty liver, hepatitis, and cirrhosis. Chronic Hepatitis l Symptomatic, biochemical or aetiological evidence of continuing or relapsing hepatic disease for more than 6 months without steady improvement is called chronic hepatitis.
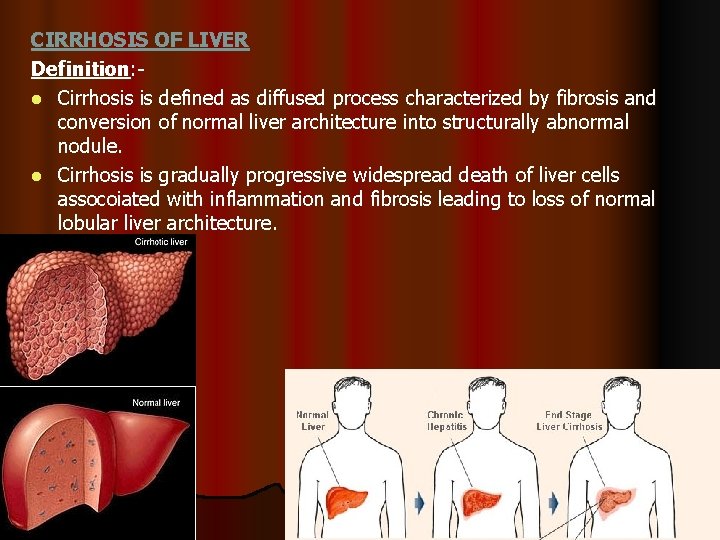
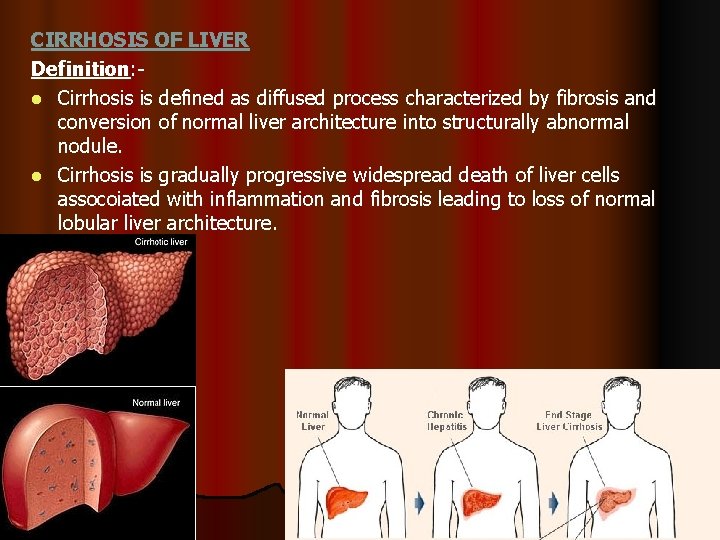
CIRRHOSIS OF LIVER Definition: l Cirrhosis is defined as diffused process characterized by fibrosis and conversion of normal liver architecture into structurally abnormal nodule. l Cirrhosis is gradually progressive widespread death of liver cells assocoiated with inflammation and fibrosis leading to loss of normal lobular liver architecture.
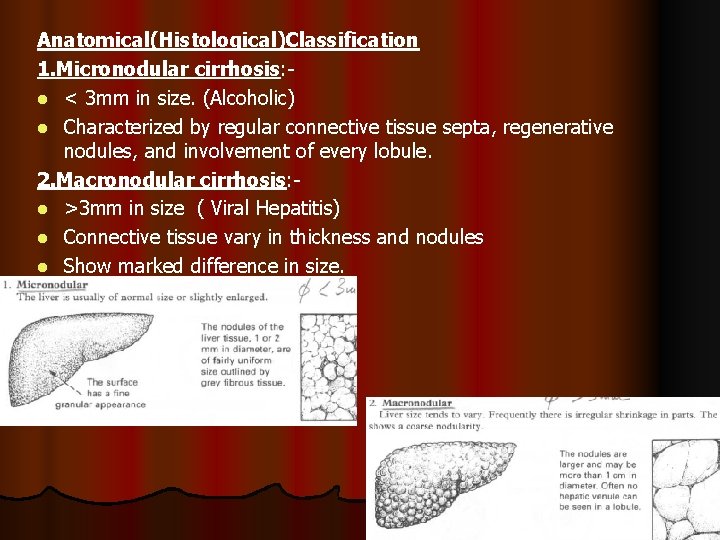
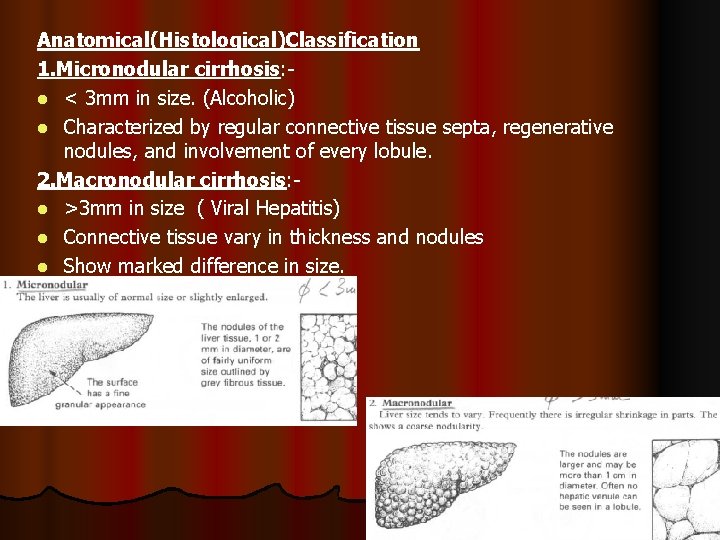
Anatomical(Histological)Classification 1. Micronodular cirrhosis: l < 3 mm in size. (Alcoholic) l Characterized by regular connective tissue septa, regenerative nodules, and involvement of every lobule. 2. Macronodular cirrhosis: l >3 mm in size ( Viral Hepatitis) l Connective tissue vary in thickness and nodules l Show marked difference in size.
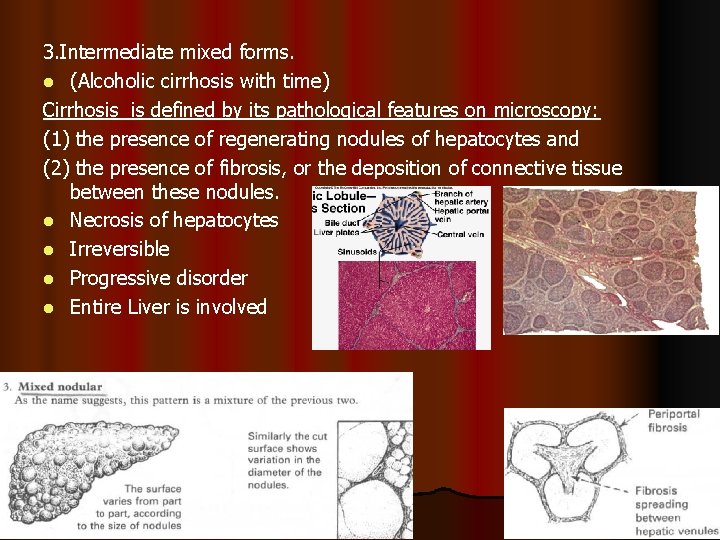
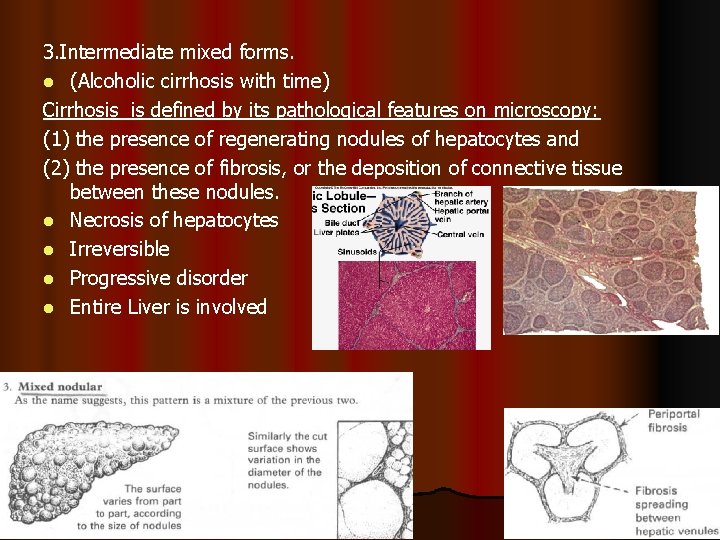
3. Intermediate mixed forms. l (Alcoholic cirrhosis with time) Cirrhosis is defined by its pathological features on microscopy: (1) the presence of regenerating nodules of hepatocytes and (2) the presence of fibrosis, or the deposition of connective tissue between these nodules. l Necrosis of hepatocytes l Irreversible l Progressive disorder l Entire Liver is involved
CAUSES Common l Alcohol l Hepatitis B+/-D l Hepatitis C Others Biliary Obstruction l Primary Biliary cirrhosis l Secondary Biliary cirrhoses (stones, stricture)
Metabolic l Haemochromatosis l Wilson’s disease l a 1 -antitrysin deficiency l Cystic fibrosis Hepatic congestion l Cardiac failure l Budd-chiari syndrome Idiopathic
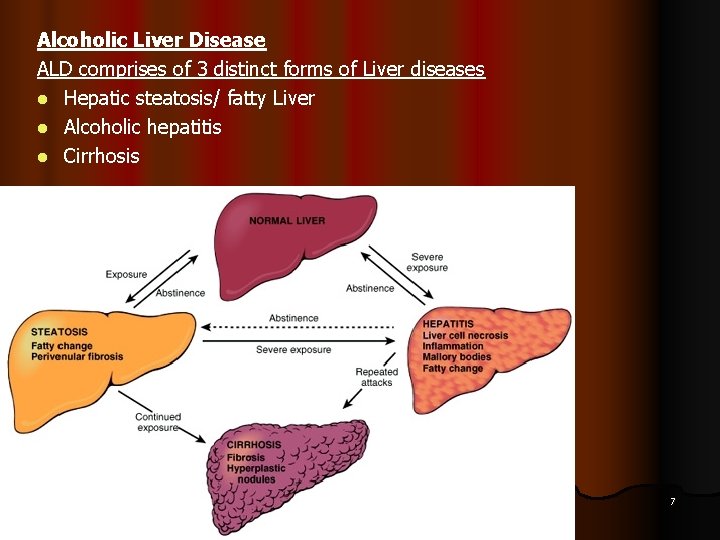
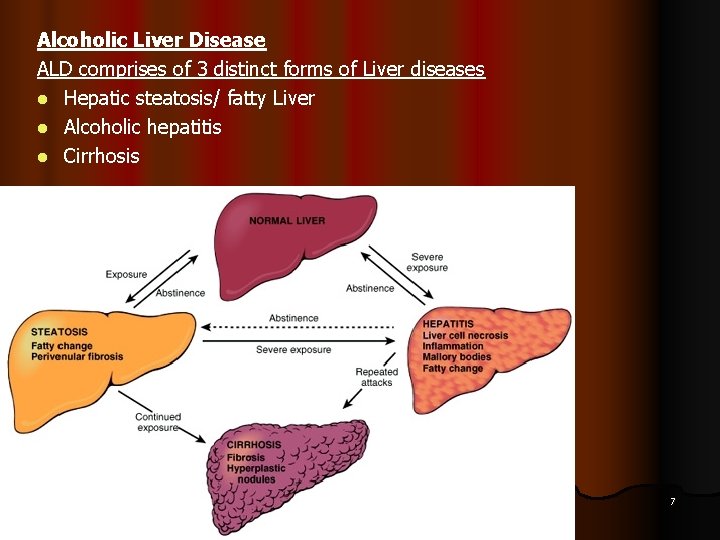
Alcoholic Liver Disease ALD comprises of 3 distinct forms of Liver diseases l Hepatic steatosis/ fatty Liver l Alcoholic hepatitis l Cirrhosis Dr S Chakradhar 7
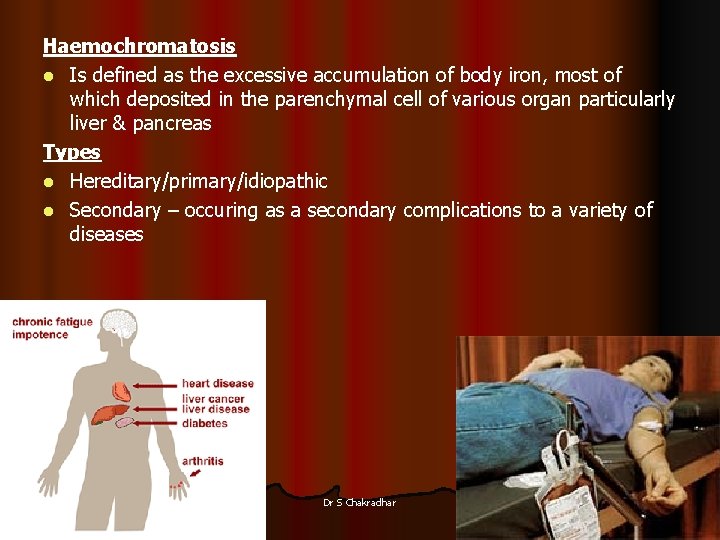
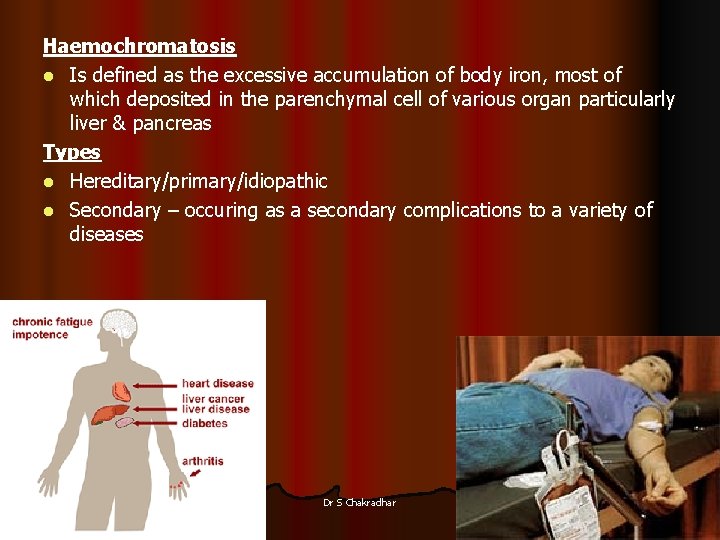
Haemochromatosis l Is defined as the excessive accumulation of body iron, most of which deposited in the parenchymal cell of various organ particularly liver & pancreas Types l Hereditary/primary/idiopathic l Secondary – occuring as a secondary complications to a variety of diseases Dr S Chakradhar 8
Wilson’s Disease l Is an autosomal recessive disorder of copper metabolism & is marked by accumulation of toxic levels of copper in many tissues & organs principally the liver, brain & eye Dr S Chakradhar 9
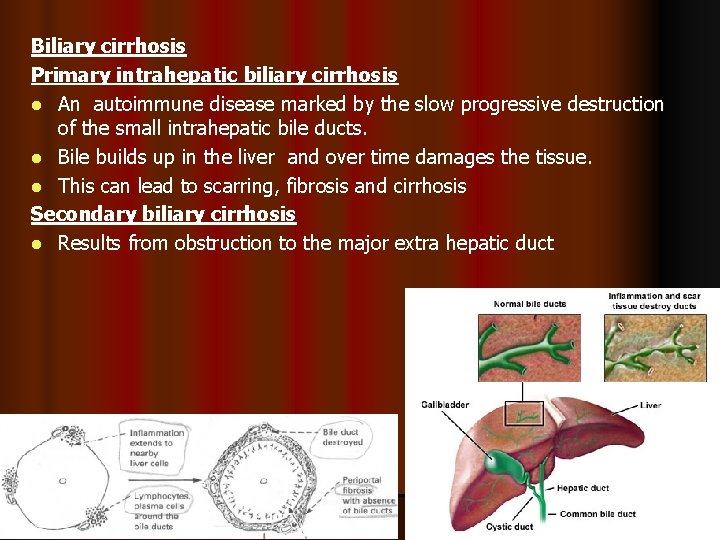
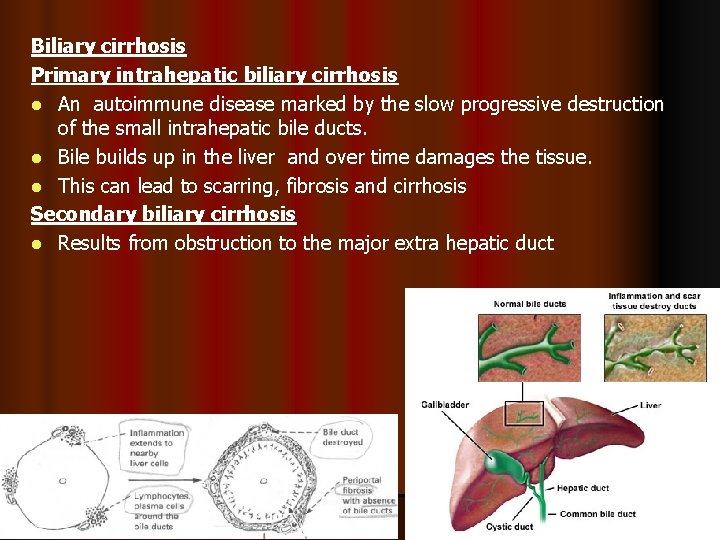
Biliary cirrhosis Primary intrahepatic biliary cirrhosis l An autoimmune disease marked by the slow progressive destruction of the small intrahepatic bile ducts. l Bile builds up in the liver and over time damages the tissue. l This can lead to scarring, fibrosis and cirrhosis Secondary biliary cirrhosis l Results from obstruction to the major extra hepatic duct Dr S Chakradhar 10
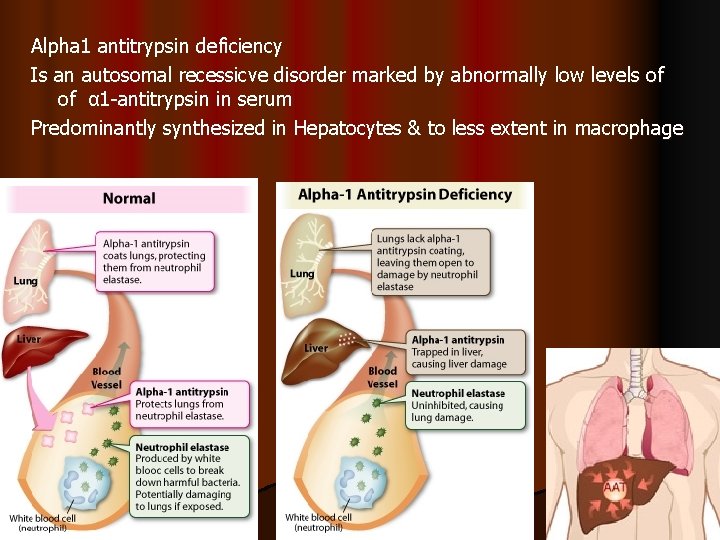
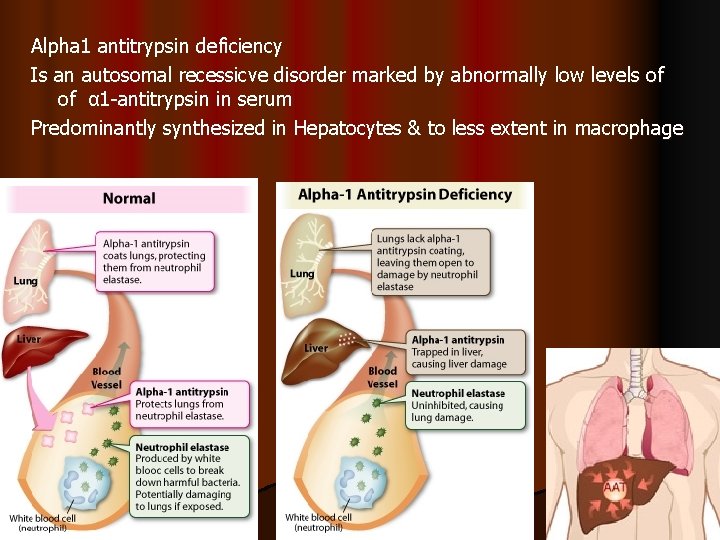
Alpha 1 antitrypsin deficiency Is an autosomal recessicve disorder marked by abnormally low levels of of α 1 -antitrypsin in serum Predominantly synthesized in Hepatocytes & to less extent in macrophage Dr S Chakradhar 11
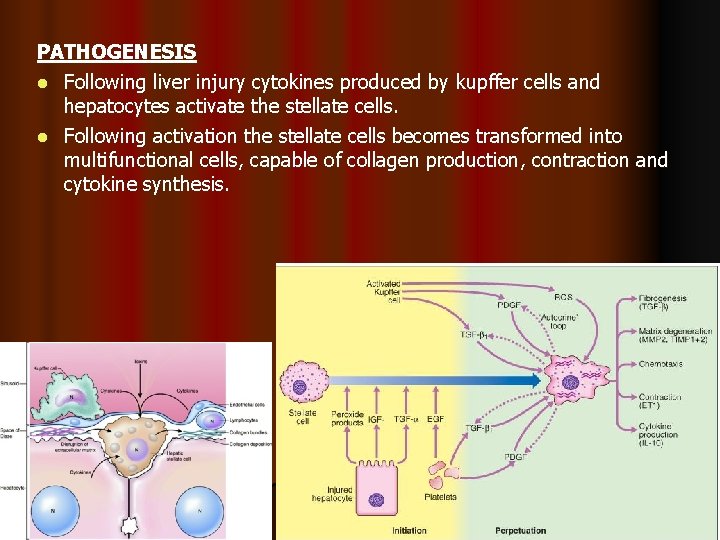
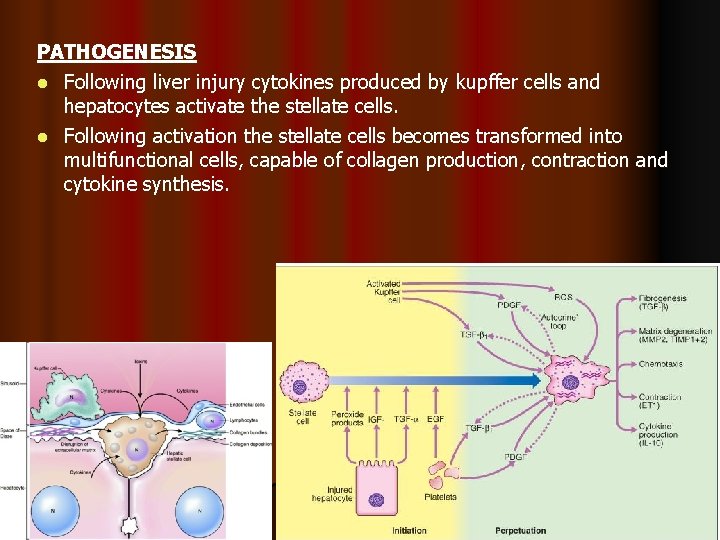
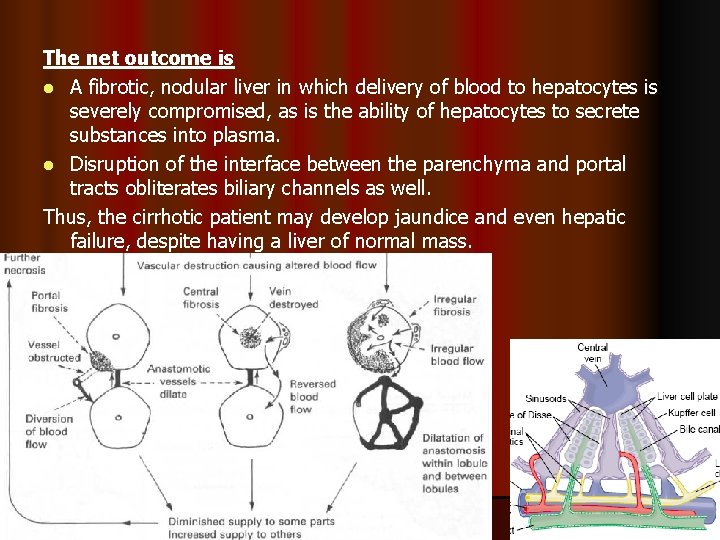
PATHOGENESIS l Following liver injury cytokines produced by kupffer cells and hepatocytes activate the stellate cells. l Following activation the stellate cells becomes transformed into multifunctional cells, capable of collagen production, contraction and cytokine synthesis.

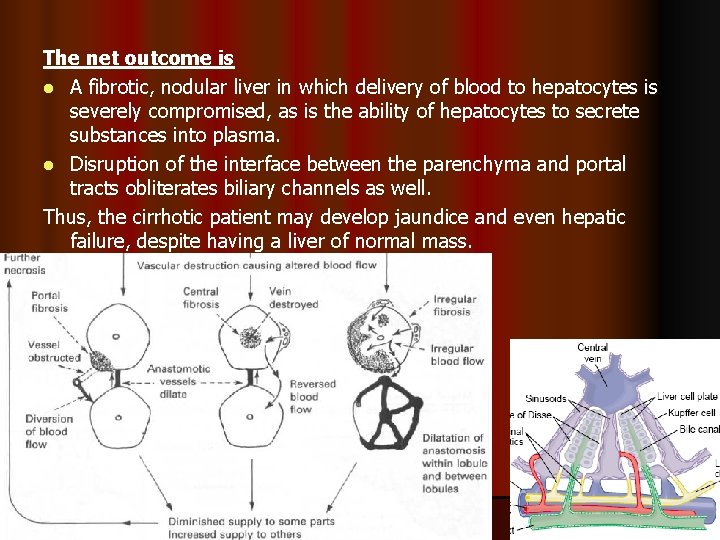
The net outcome is l A fibrotic, nodular liver in which delivery of blood to hepatocytes is severely compromised, as is the ability of hepatocytes to secrete substances into plasma. l Disruption of the interface between the parenchyma and portal tracts obliterates biliary channels as well. Thus, the cirrhotic patient may develop jaundice and even hepatic failure, despite having a liver of normal mass. Dr S Chakradhar 14
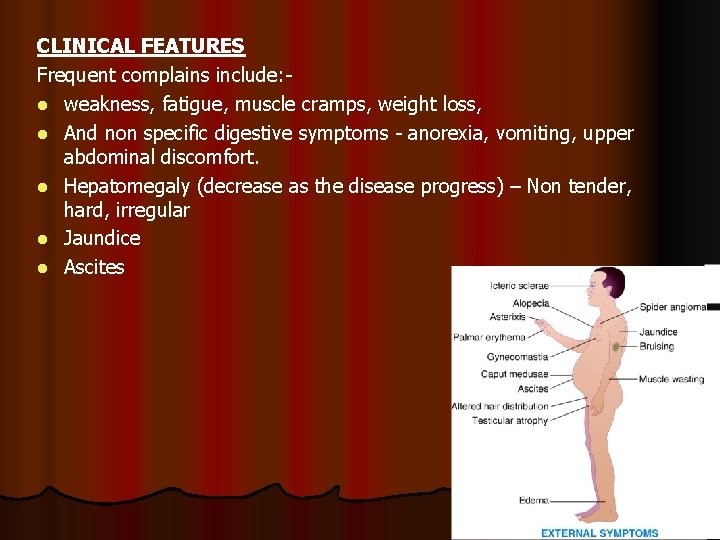
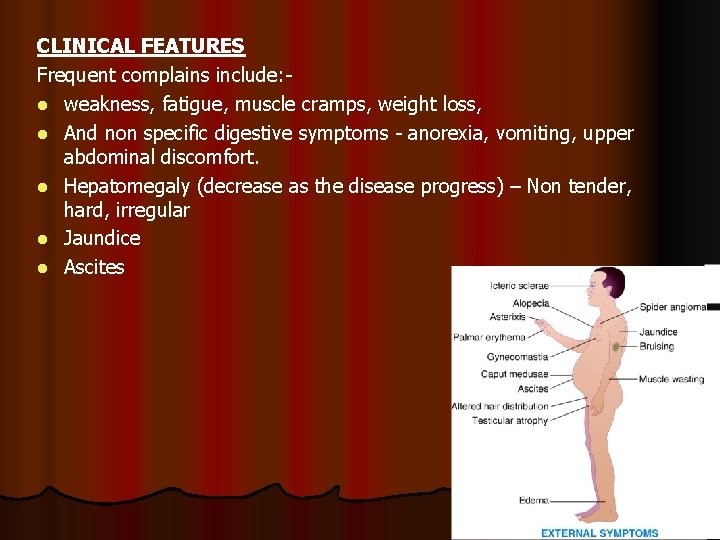
CLINICAL FEATURES Frequent complains include: l weakness, fatigue, muscle cramps, weight loss, l And non specific digestive symptoms - anorexia, vomiting, upper abdominal discomfort. l Hepatomegaly (decrease as the disease progress) – Non tender, hard, irregular l Jaundice l Ascites
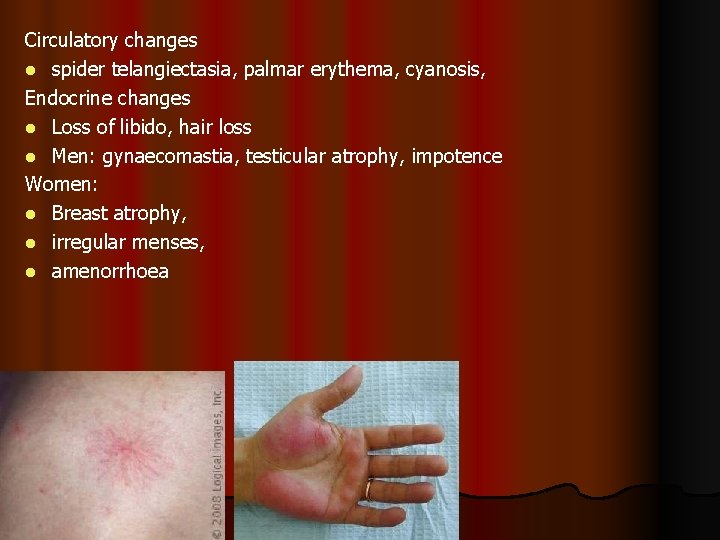
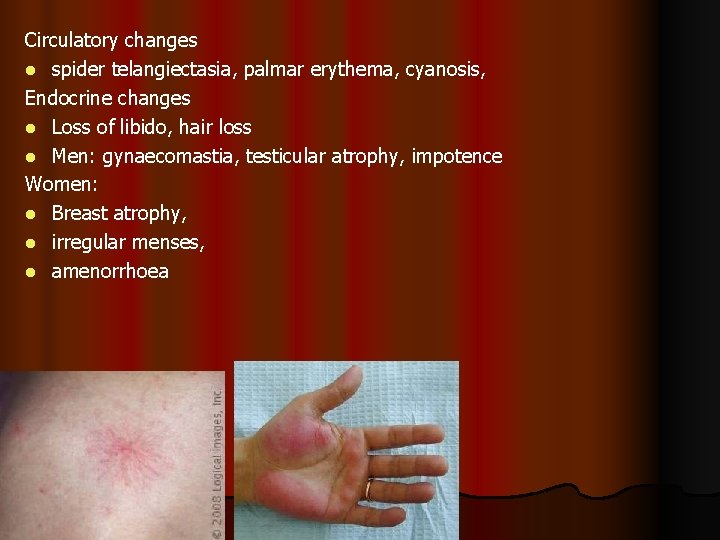
Circulatory changes l spider telangiectasia, palmar erythema, cyanosis, Endocrine changes l Loss of libido, hair loss l Men: gynaecomastia, testicular atrophy, impotence Women: l Breast atrophy, l irregular menses, l amenorrhoea
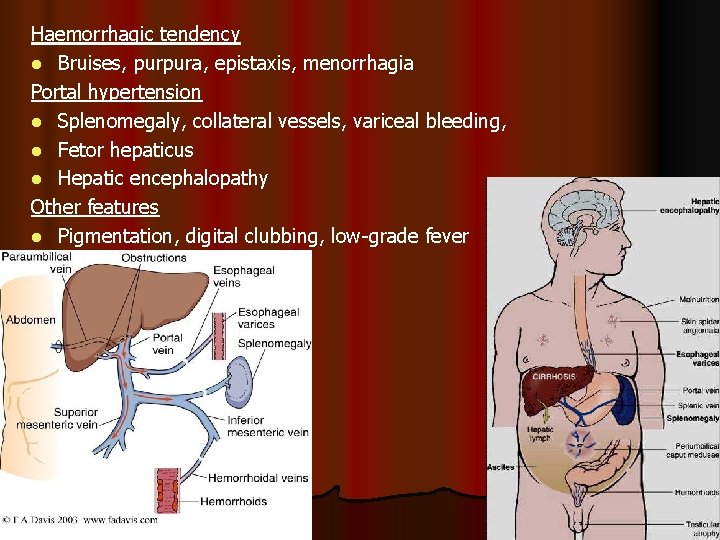
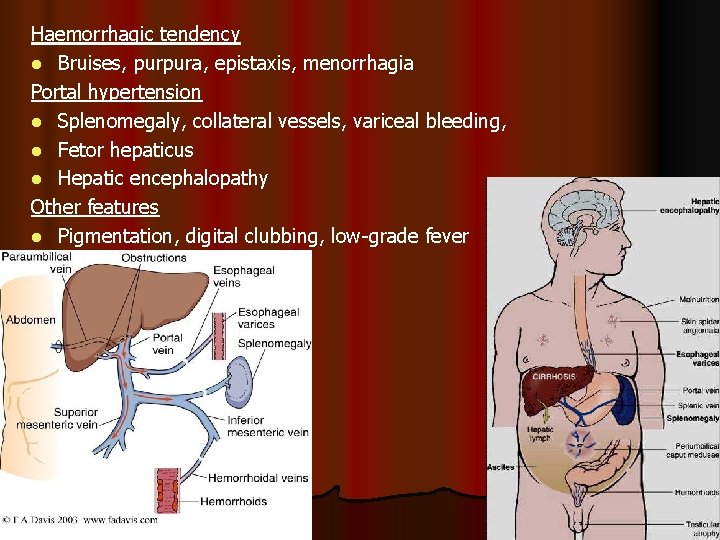
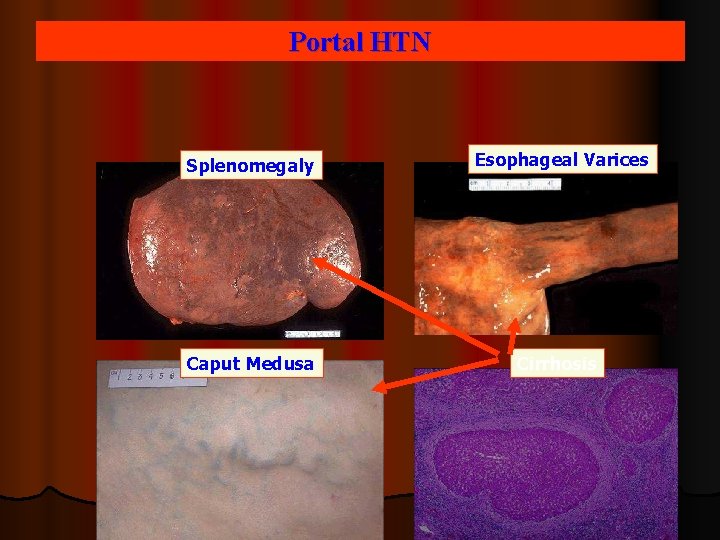
Haemorrhagic tendency l Bruises, purpura, epistaxis, menorrhagia Portal hypertension l Splenomegaly, collateral vessels, variceal bleeding, l Fetor hepaticus l Hepatic encephalopathy Other features l Pigmentation, digital clubbing, low-grade fever
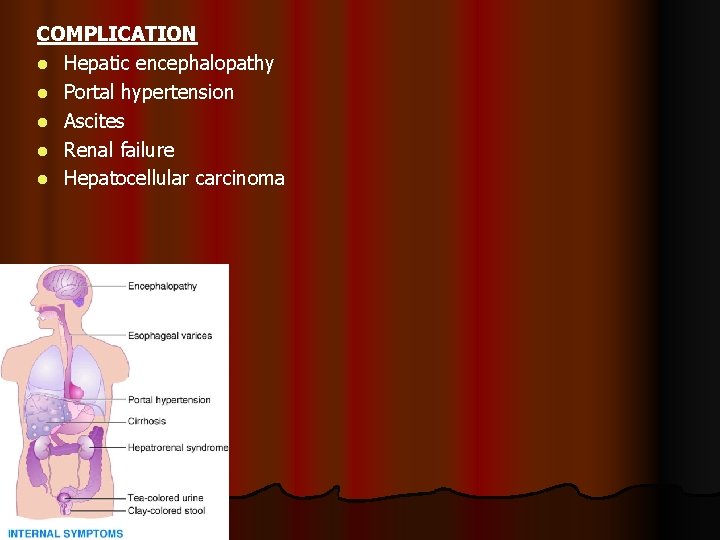
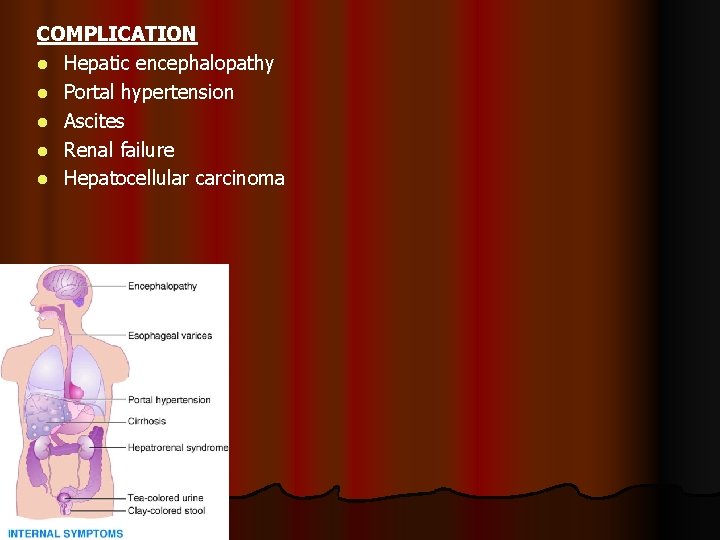
COMPLICATION l Hepatic encephalopathy l Portal hypertension l Ascites l Renal failure l Hepatocellular carcinoma
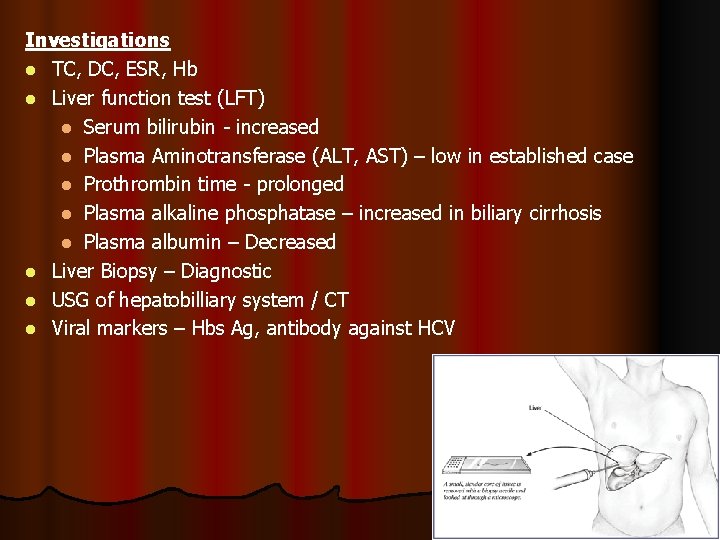
Investigations l TC, DC, ESR, Hb l Liver function test (LFT) l Serum bilirubin - increased l Plasma Aminotransferase (ALT, AST) – low in established case l Prothrombin time - prolonged l Plasma alkaline phosphatase – increased in biliary cirrhosis l Plasma albumin – Decreased l Liver Biopsy – Diagnostic l USG of hepatobilliary system / CT l Viral markers – Hbs Ag, antibody against HCV
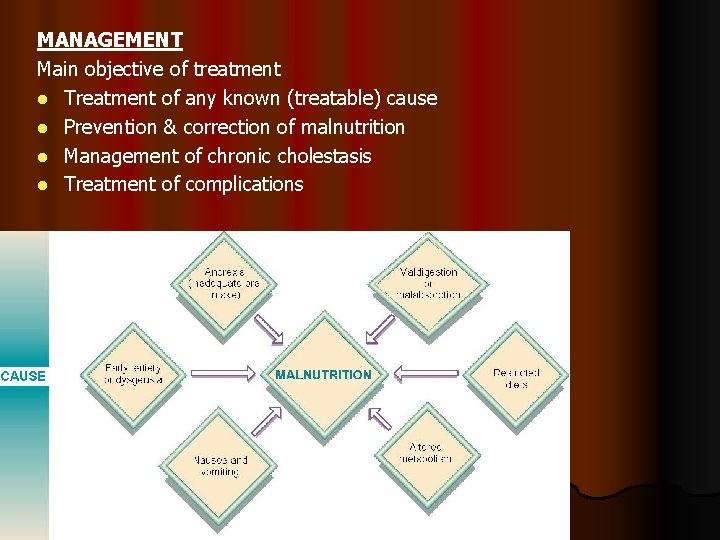
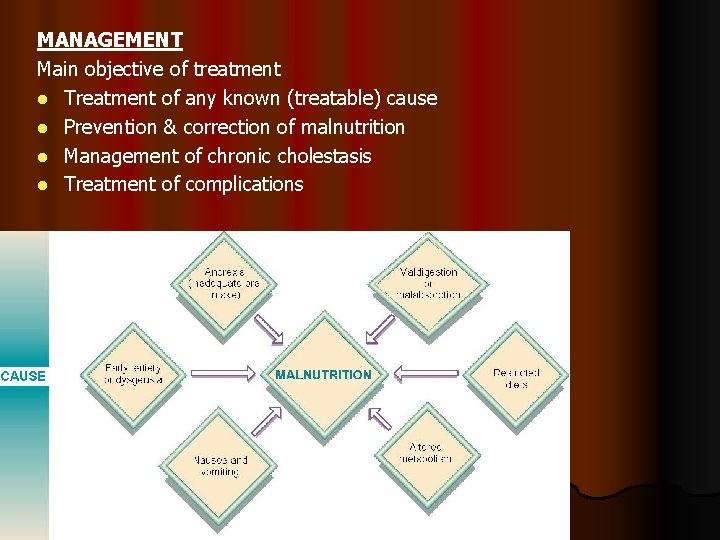
MANAGEMENT Main objective of treatment l Treatment of any known (treatable) cause l Prevention & correction of malnutrition l Management of chronic cholestasis l Treatment of complications
No treatment can reverse cirrhosis or even ensure that no further progression occurs. Rx is symptomatic and supportive. l Withdrawal or treatment of aetiological factors e. g. Alcohol consumption, drugs, Haemochromatosis. l No strenuous activity to reduce metabolism l Nutrition l High energy protein (in absence of encephalopathy) & CHO rich diet l Fat restriction (if Cholestasis) l Alcohol must be forbidden l Vitamin B-complex. l Treatment of complications l Ascites – low salt diet , Diuretics l Liver Transplant l 6 monthly USG and AFP to detect the development of hepatocellular carcinoma

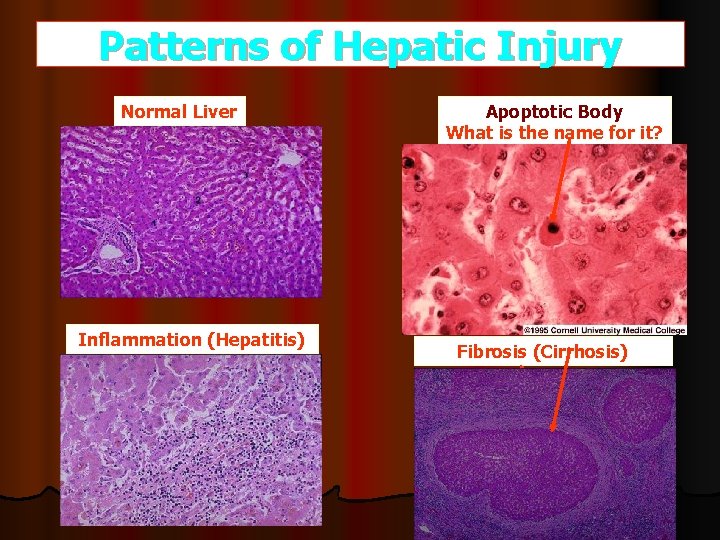
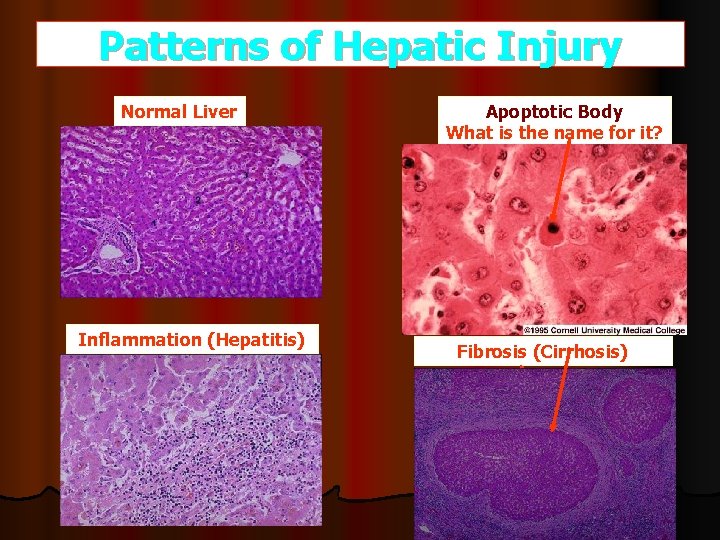
Patterns of Hepatic Injury Normal Liver Inflammation (Hepatitis) Apoptotic Body What is the name for it? Fibrosis (Cirrhosis)
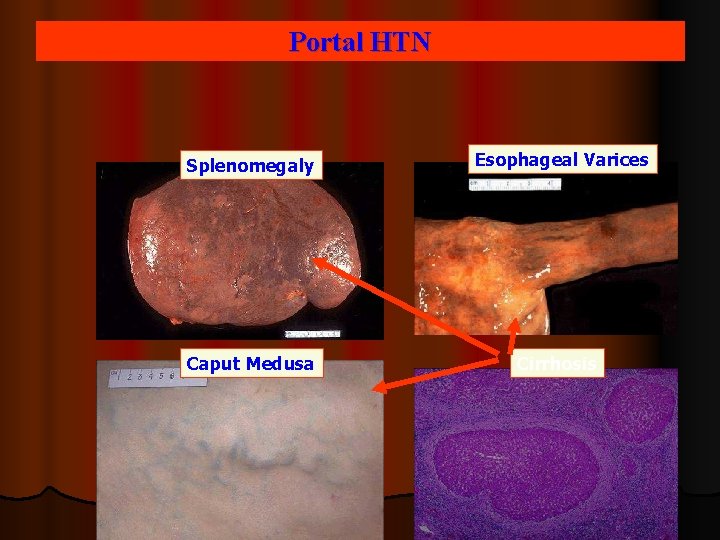
Portal HTN Splenomegaly Esophageal Varices Caput Medusa Cirrhosis

 Portal hypertension symptoms and signs
Portal hypertension symptoms and signs Gastroenterology board review
Gastroenterology board review Infiltrative liver disease
Infiltrative liver disease Features of cld
Features of cld Stage 3 liver cirrhosis
Stage 3 liver cirrhosis Stigmata of chronic liver disease
Stigmata of chronic liver disease Peripheral stigmata of cld
Peripheral stigmata of cld Gennifer shafer liver disease
Gennifer shafer liver disease Complications of cirrhosis
Complications of cirrhosis Nonalcoholic fatty liver disease
Nonalcoholic fatty liver disease Alcoholic liver disease
Alcoholic liver disease Elisabetta bugianesi
Elisabetta bugianesi Bharathi viswanathan
Bharathi viswanathan Hci design patterns
Hci design patterns Ligamentum venosum
Ligamentum venosum Malignant neoplasm of liver
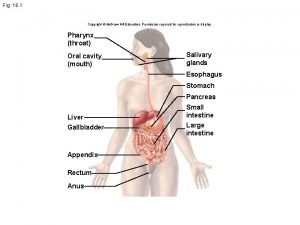
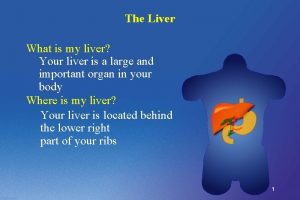
Malignant neoplasm of liver Where are the liver and pancreas located
Where are the liver and pancreas located Health education on hepatitis ppt
Health education on hepatitis ppt Bare area liver
Bare area liver Echogensity
Echogensity Porosis of the liver
Porosis of the liver Liver zones
Liver zones Image permission
Image permission Synthetic function of liver
Synthetic function of liver Heterogeneous hypoechoic lesion in liver
Heterogeneous hypoechoic lesion in liver Carcinoid tumor metastatic liver prognosis
Carcinoid tumor metastatic liver prognosis