Aplastic and Hypoplastic Anemias What happens when the
- Slides: 15
Aplastic and Hypoplastic Anemias What happens when the bone marrow shuts down?
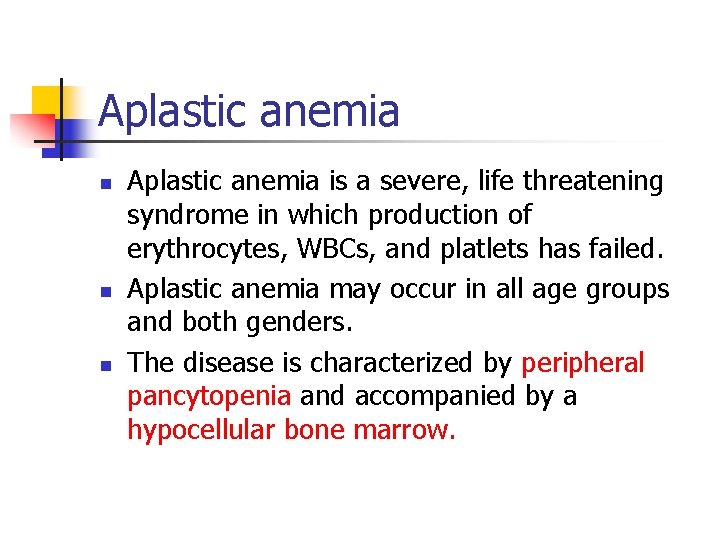
Aplastic anemia n n n Aplastic anemia is a severe, life threatening syndrome in which production of erythrocytes, WBCs, and platlets has failed. Aplastic anemia may occur in all age groups and both genders. The disease is characterized by peripheral pancytopenia and accompanied by a hypocellular bone marrow.
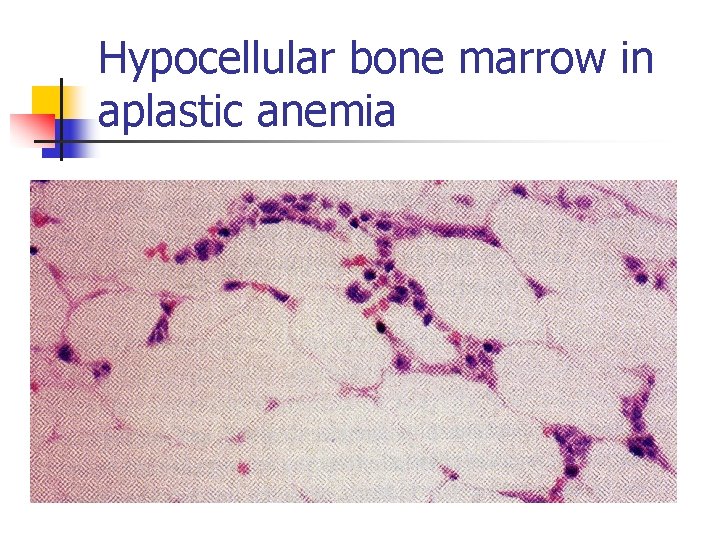
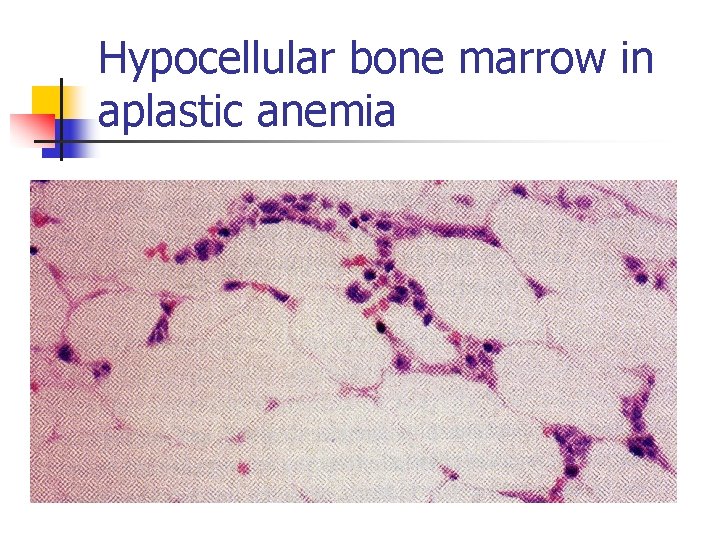
Hypocellular bone marrow in aplastic anemia
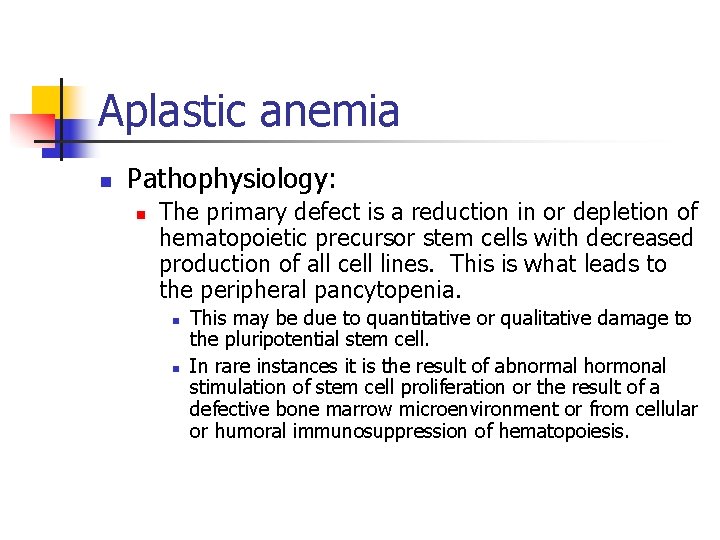
Aplastic anemia n Pathophysiology: n The primary defect is a reduction in or depletion of hematopoietic precursor stem cells with decreased production of all cell lines. This is what leads to the peripheral pancytopenia. n n This may be due to quantitative or qualitative damage to the pluripotential stem cell. In rare instances it is the result of abnormal hormonal stimulation of stem cell proliferation or the result of a defective bone marrow microenvironment or from cellular or humoral immunosuppression of hematopoiesis.
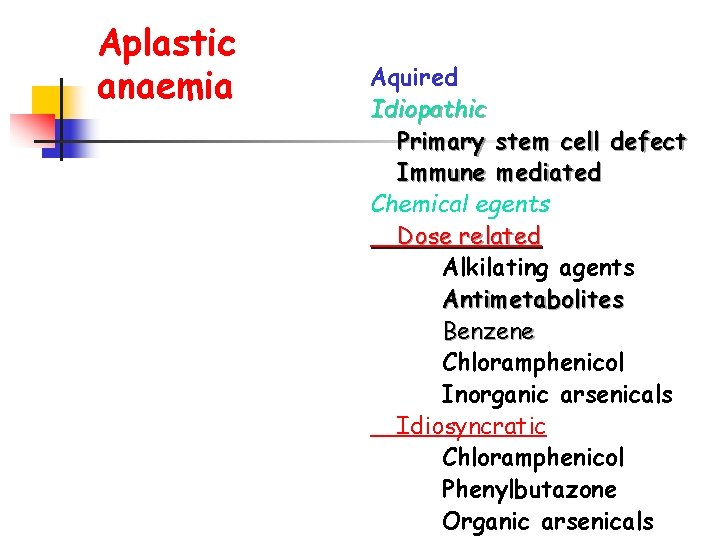
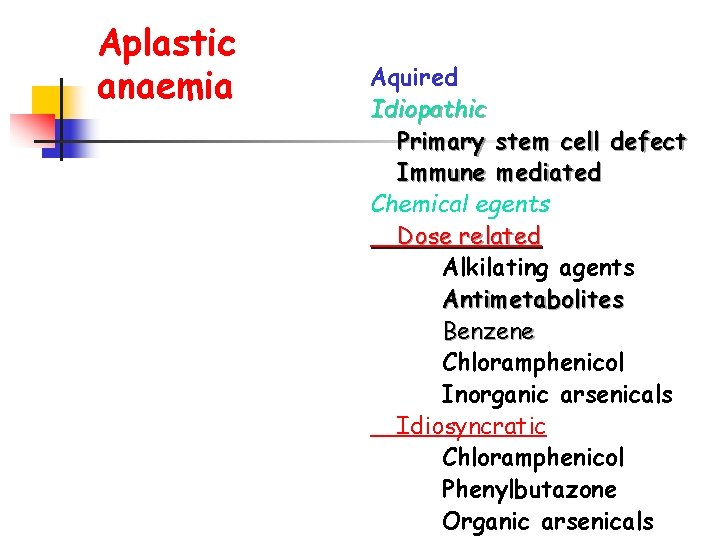
Aplastic anaemia Aquired Idiopathic Primary stem cell defect Immune mediated Chemical egents Dose related Alkilating agents Antimetabolites Benzene Chloramphenicol Inorganic arsenicals Idiosyncratic Chloramphenicol Phenylbutazone Organic arsenicals
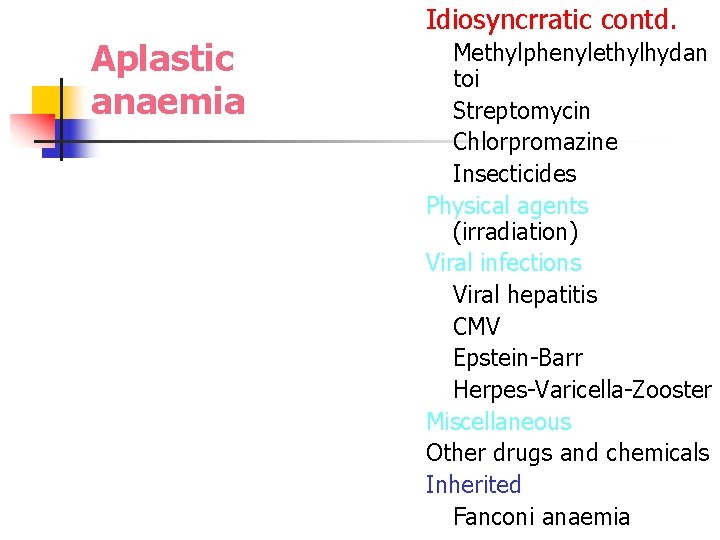
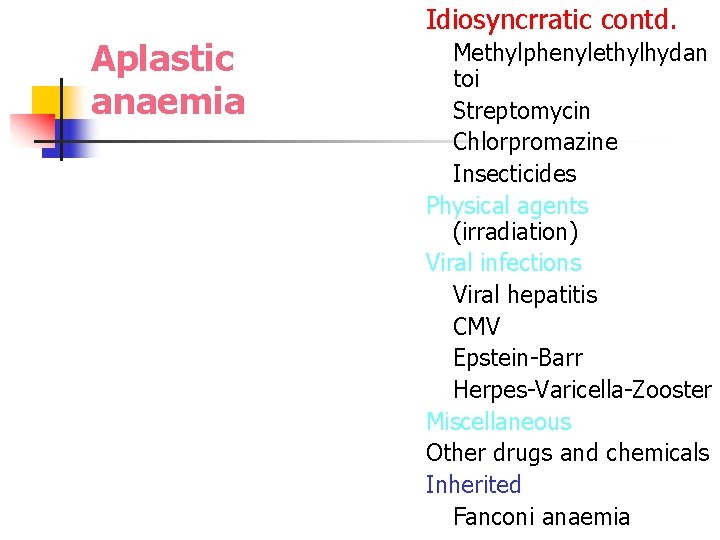
Idiosyncrratic contd. Aplastic anaemia Methylphenylethylhydan toi Streptomycin Chlorpromazine Insecticides Physical agents (irradiation) Viral infections Viral hepatitis CMV Epstein-Barr Herpes-Varicella-Zooster Miscellaneous Other drugs and chemicals Inherited Fanconi anaemia
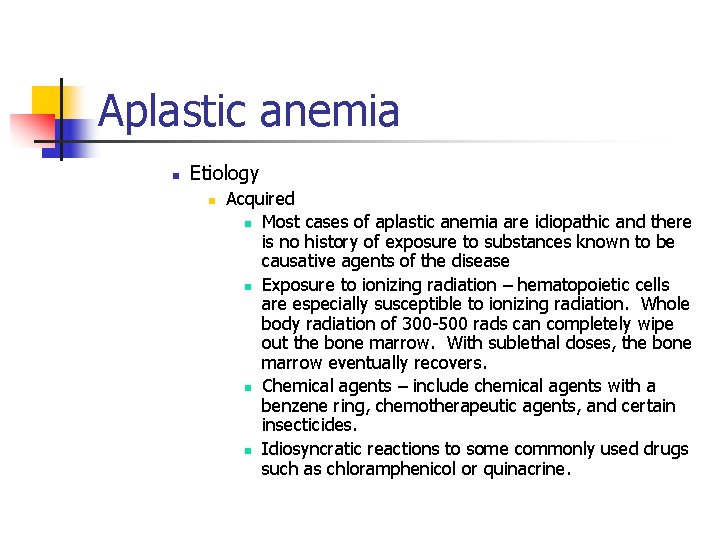
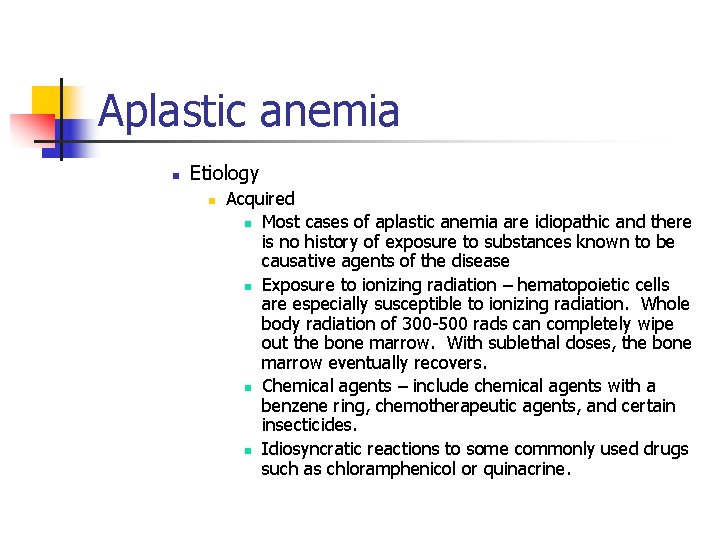
Aplastic anemia n Etiology n Acquired n Most cases of aplastic anemia are idiopathic and there is no history of exposure to substances known to be causative agents of the disease n Exposure to ionizing radiation – hematopoietic cells are especially susceptible to ionizing radiation. Whole body radiation of 300 -500 rads can completely wipe out the bone marrow. With sublethal doses, the bone marrow eventually recovers. n Chemical agents – include chemical agents with a benzene ring, chemotherapeutic agents, and certain insecticides. n Idiosyncratic reactions to some commonly used drugs such as chloramphenicol or quinacrine.
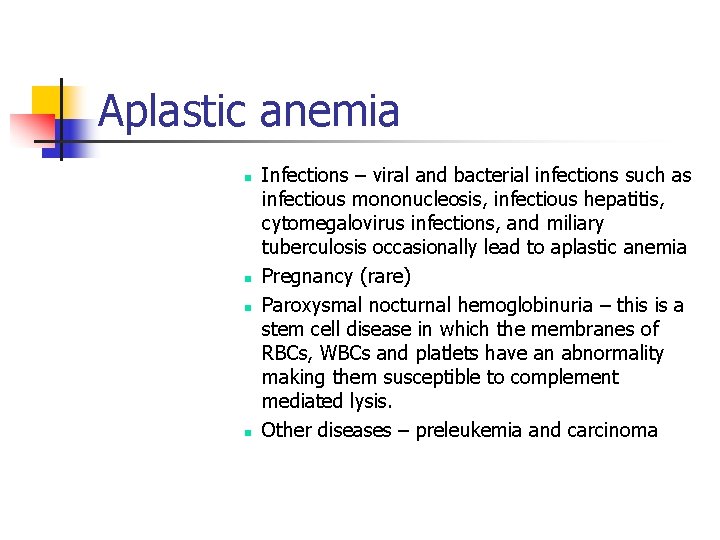
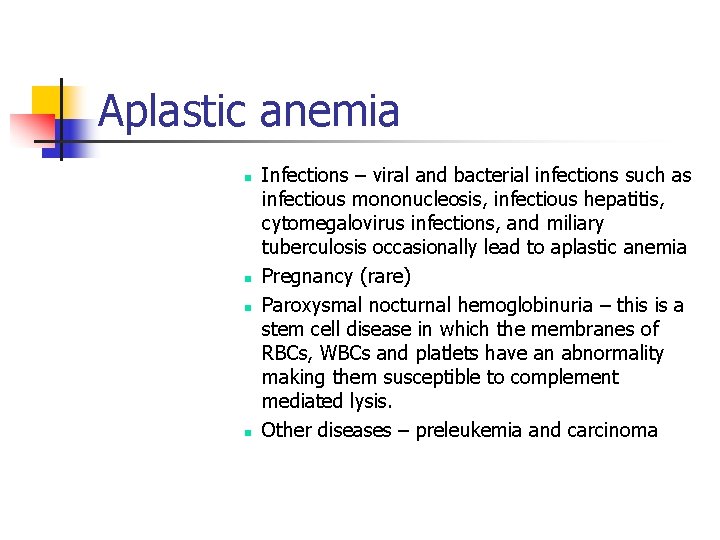
Aplastic anemia n n Infections – viral and bacterial infections such as infectious mononucleosis, infectious hepatitis, cytomegalovirus infections, and miliary tuberculosis occasionally lead to aplastic anemia Pregnancy (rare) Paroxysmal nocturnal hemoglobinuria – this is a stem cell disease in which the membranes of RBCs, WBCs and platlets have an abnormality making them susceptible to complement mediated lysis. Other diseases – preleukemia and carcinoma
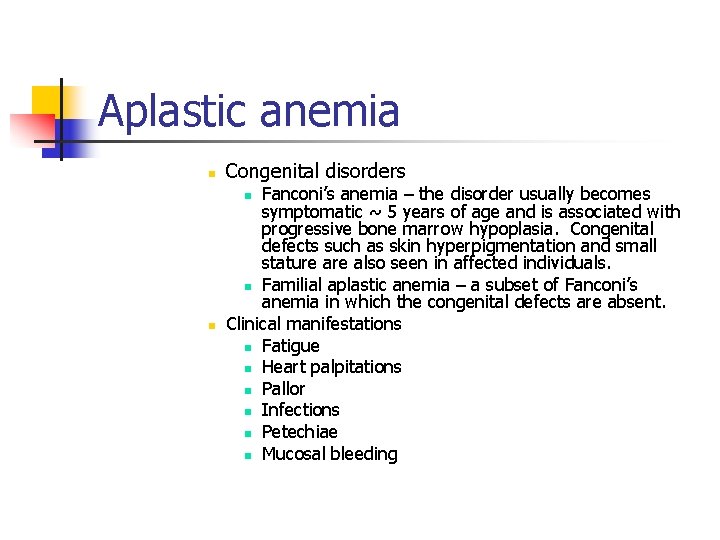
Aplastic anemia n Congenital disorders Fanconi’s anemia – the disorder usually becomes symptomatic ~ 5 years of age and is associated with progressive bone marrow hypoplasia. Congenital defects such as skin hyperpigmentation and small stature also seen in affected individuals. n Familial aplastic anemia – a subset of Fanconi’s anemia in which the congenital defects are absent. Clinical manifestations n Fatigue n Heart palpitations n Pallor n Infections n Petechiae n Mucosal bleeding n n
Aplastic anemia n n Lab findings n Severe pancytopenia with relative lymphocytosis (lymphocytes live a long time) n Normochromic, normocytic RBCs (may be slightly macrocytic) n Mild to moderate anisocytosis and poikilocytosis n Decreased reticulocyte count n Hypocellular bone marrow with > 70% yellow marrow Treatment – in untreated cases the prognosis is poor n Remove causative agent, if known n Multiple transfusions n Bone marrow transplant
Related disorders n Disorders in which there is peripheral pancytopenia, but the bone marrow is normocellular, hypercellular, or infiltrated with abnormal cellular elements n Myelopthesic anemia – replacement of bone marrow by fibrotic, granulomatous, or neoplastic cells
Related disorders n n Myelodysplastic syndromes – are primary, neoplastic stem cell disorders that tend to terminate in acute leukemia. The bone marrow is usually normocellular, or hypercellular with evidence of qualitative abnormalities in one or more cell lines resulting on ineffective erythropoiesis and/or granulopoiesis and/or megakaryopoiesis. The peripheral smear shows dysplastic (abnormality in development) cells including nucleated RBCs, oval macrocytes, pseudo-Pelger-Huet PMNs (hyposegmented neutrophils) with hyperchromatin clumping, hypogranulated neutrophils, and giant bizarre platlets. Hypersplenism – why can this lead to pancytopenia?
Pure Red Cell Aplasia n Pure red cell aplasia s characterized by a selective decrease in erythroid precursor cells in the bone marrow. WBCs and platlets are unaffected. n Acquired n n n Transitory with viral or bacterial infections Patients with hemolytic anemias may suddenly halt erythropoiesis Patients with thymoma – T-cell mediated responses against bone marrow erythroblasts or erythropoietin are sometimes produced.
Pure Red Cell Aplasia n Congenital n Diamond-Blackfan syndrome – occurs in young children and is progressive. It is probably due to an intrinsic or regulatory defect in the committed erythroid stem cell.
Other hypoproliferative anemias n n Renal disease – due to decreased erythropoietin Endocrine deficiencies – may lead to decreased erythropoietin production. For example: hypothyroidism leads to decreased demand for oxygen from tissues; decreased androgens in males; decreased pituitary function