Treatment of chronic liver disease Treatment Cause Etiology



- Slides: 40
Treatment of chronic liver disease
Treatment Cause ( Etiology) n Complication n
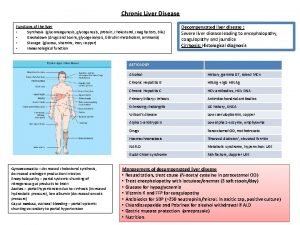
Etiology Infection n Alcohol n Autoimmune n Cholestatic n Infiltrative n Metabolic n Vascular n Drugs n
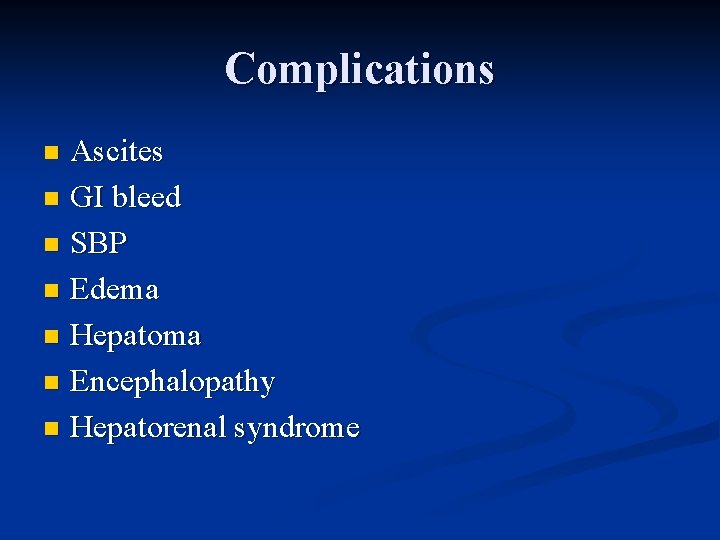
Complications Ascites n GI bleed n SBP n Edema n Hepatoma n Encephalopathy n Hepatorenal syndrome n
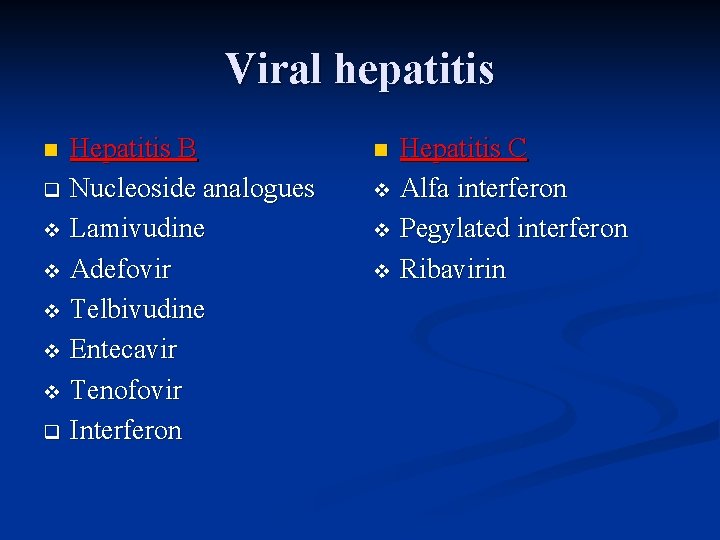
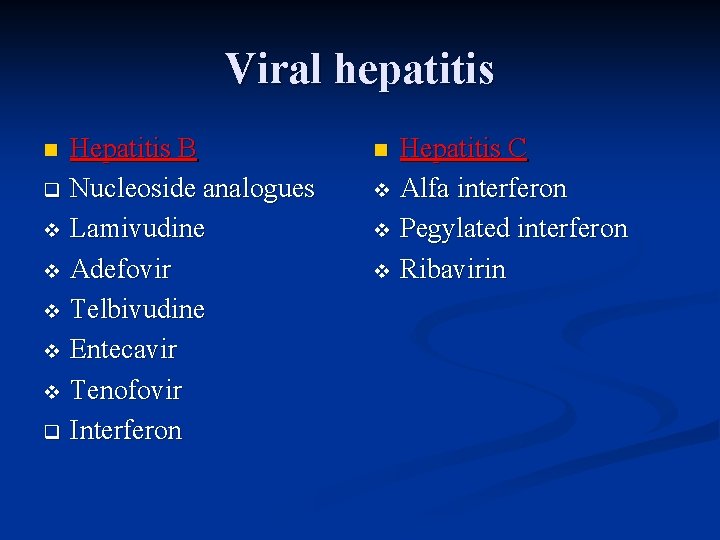
Viral hepatitis Hepatitis B q Nucleoside analogues v Lamivudine v Adefovir v Telbivudine v Entecavir v Tenofovir q Interferon n Hepatitis C v Alfa interferon v Pegylated interferon v Ribavirin n
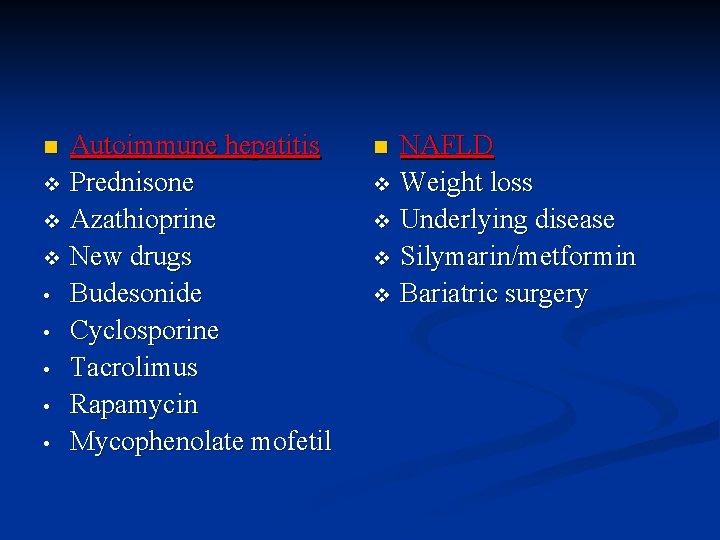
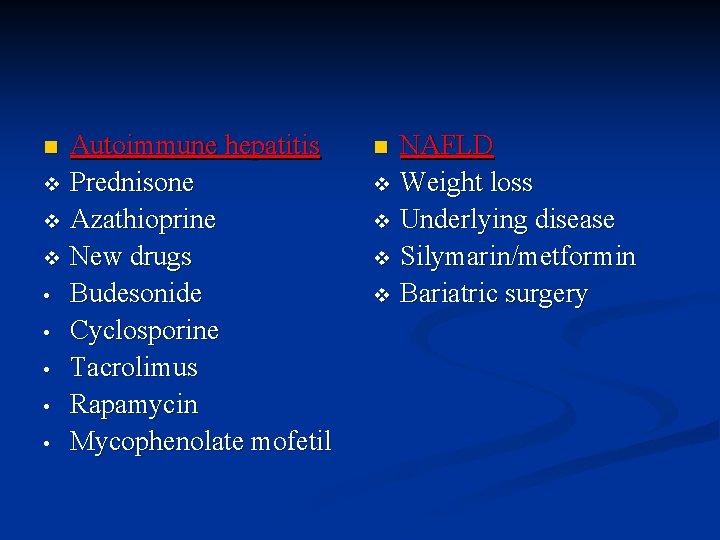
Autoimmune hepatitis v Prednisone v Azathioprine v New drugs • Budesonide • Cyclosporine • Tacrolimus • Rapamycin • Mycophenolate mofetil n NAFLD v Weight loss v Underlying disease v Silymarin/metformin v Bariatric surgery n
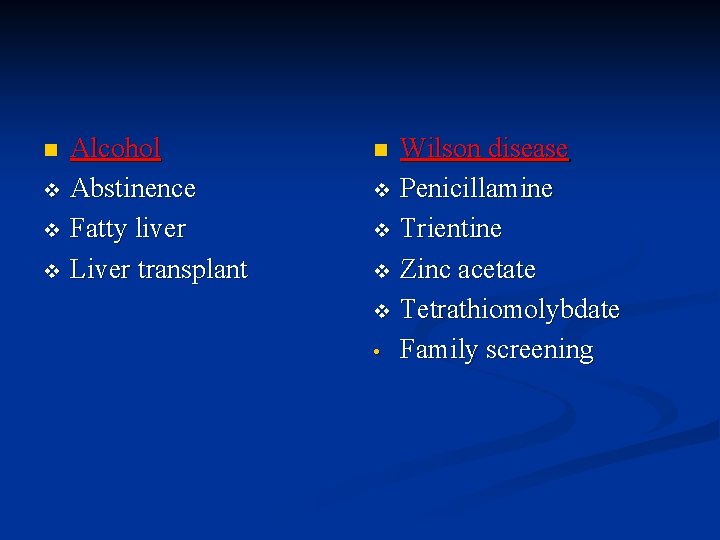
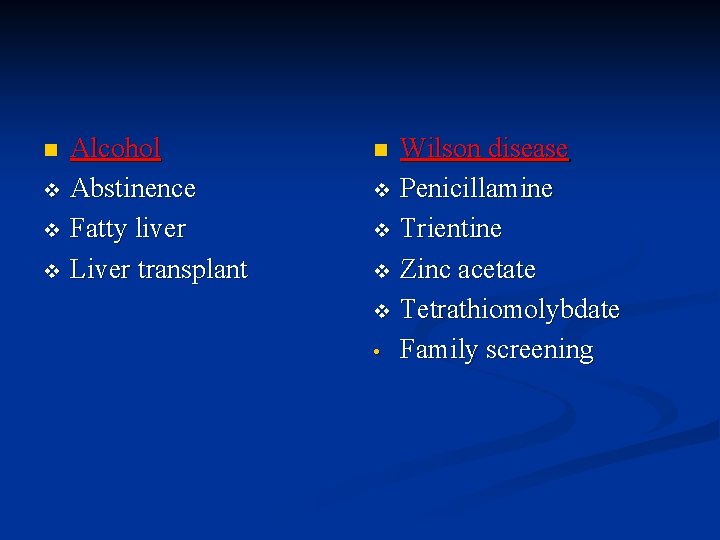
Alcohol v Abstinence v Fatty liver v Liver transplant n Wilson disease v Penicillamine v Trientine v Zinc acetate v Tetrathiomolybdate • Family screening n
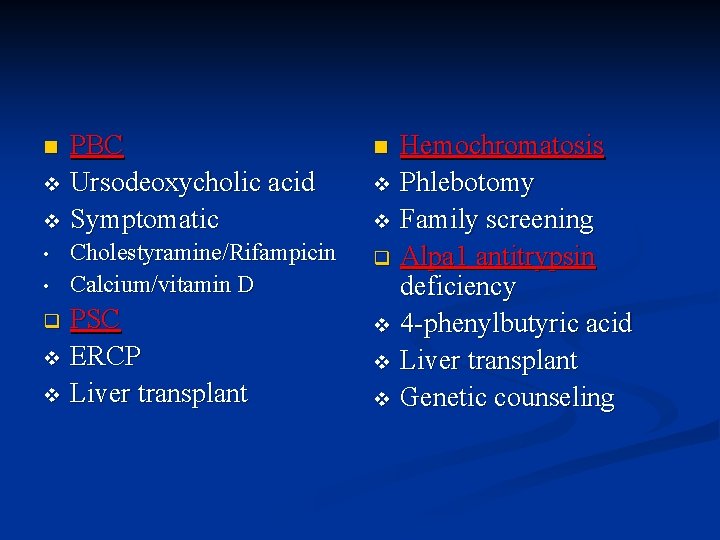
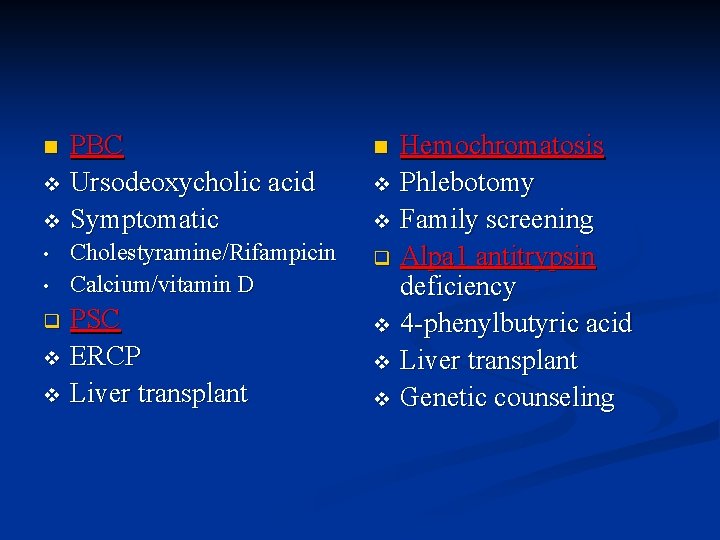
PBC v Ursodeoxycholic acid v Symptomatic n • • Cholestyramine/Rifampicin Calcium/vitamin D PSC v ERCP v Liver transplant q Hemochromatosis v Phlebotomy v Family screening q Alpa 1 antitrypsin deficiency v 4 -phenylbutyric acid v Liver transplant v Genetic counseling n
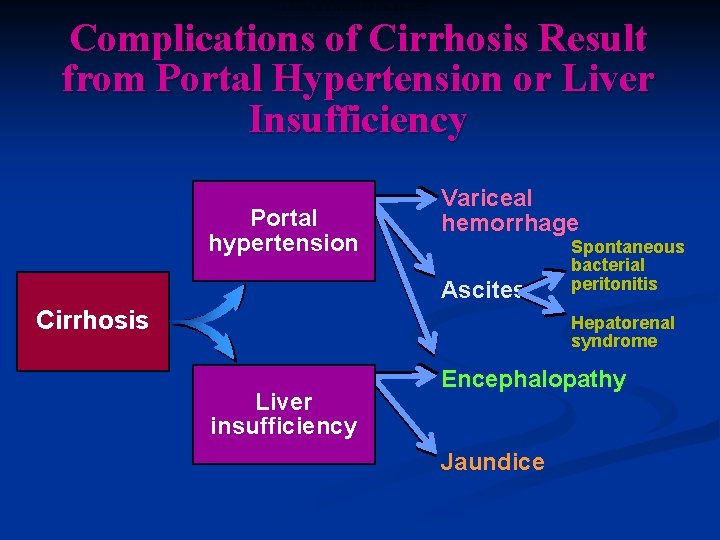
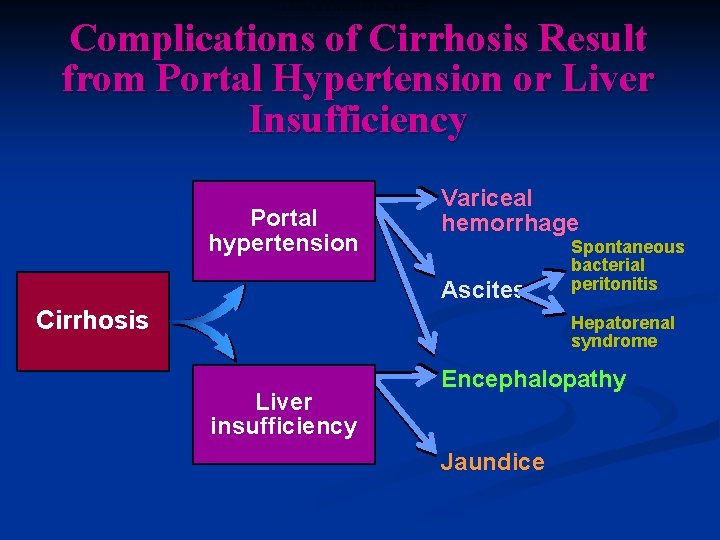
COMPLICATIONS OF CIRRHOSIS Complications of Cirrhosis Result from Portal Hypertension or Liver Insufficiency Portal hypertension Variceal hemorrhage Ascites Cirrhosis Spontaneous bacterial peritonitis Hepatorenal syndrome Liver insufficiency Encephalopathy Jaundice
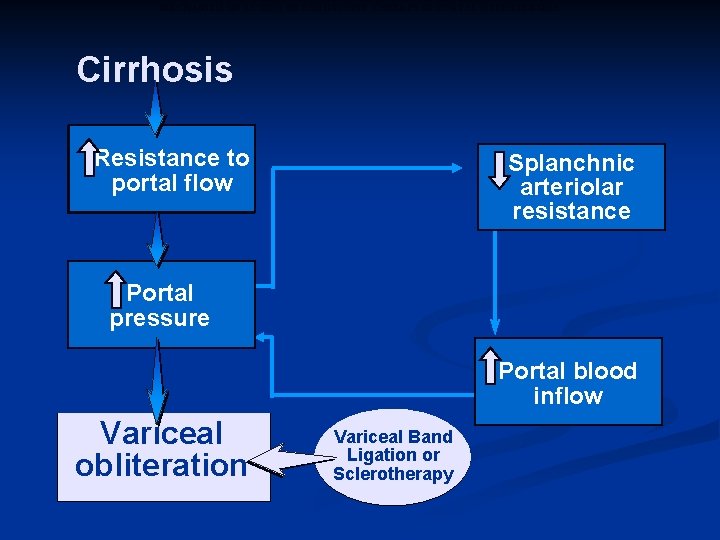
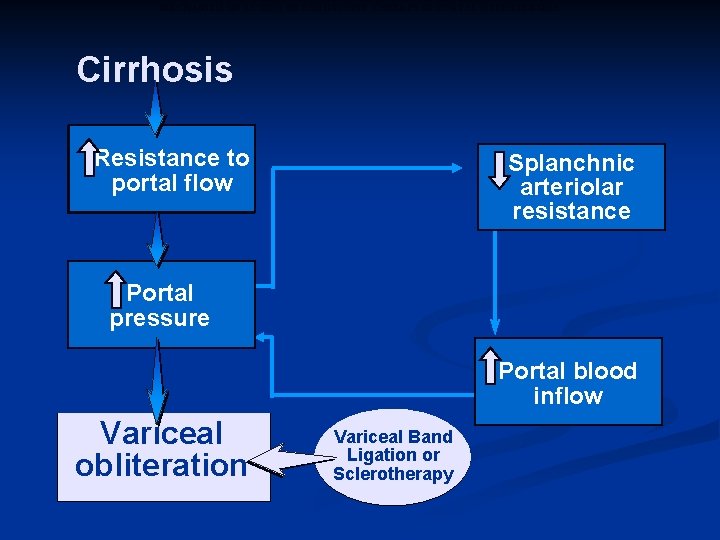
MECHANISM OF ACTION OF ENDOSCOPIC THERAPY IN PORTAL HYPERTENSION Cirrhosis Resistance to portal flow Splanchnic arteriolar resistance Portal pressure Portal blood inflow Varices/ Variceal obliteration Hemorrhage Variceal Band Ligation or Sclerotherapy
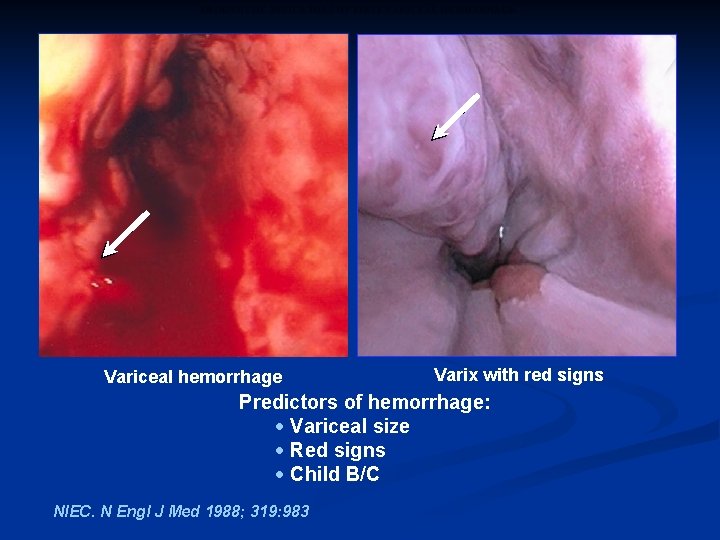
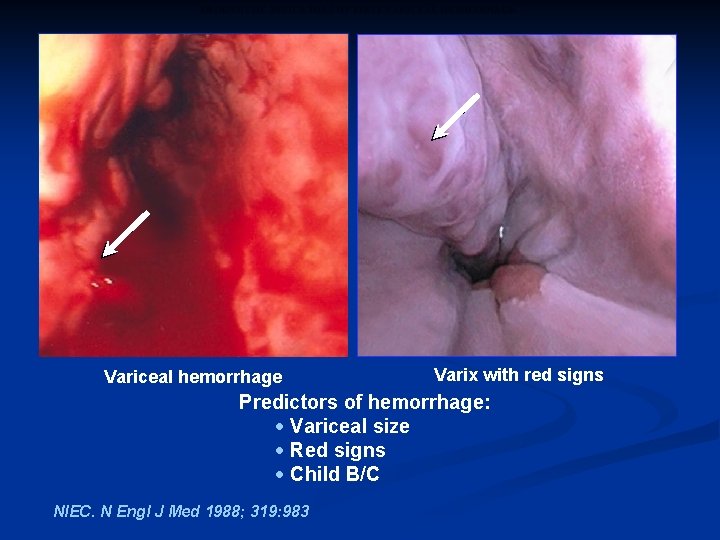
PROGNOSTIC INDICATORS OF FIRST VARICEAL HEMORRHAGE Variceal hemorrhage Varix with red signs Predictors of hemorrhage: · Variceal size · Red signs · Child B/C NIEC. N Engl J Med 1988; 319: 983
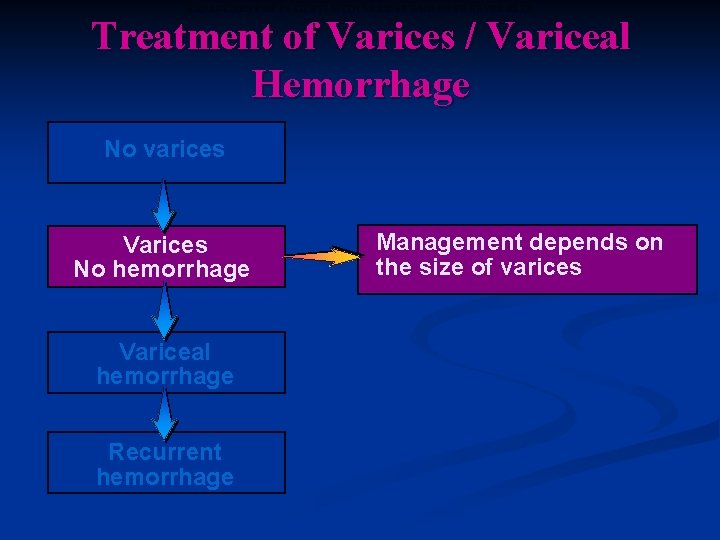
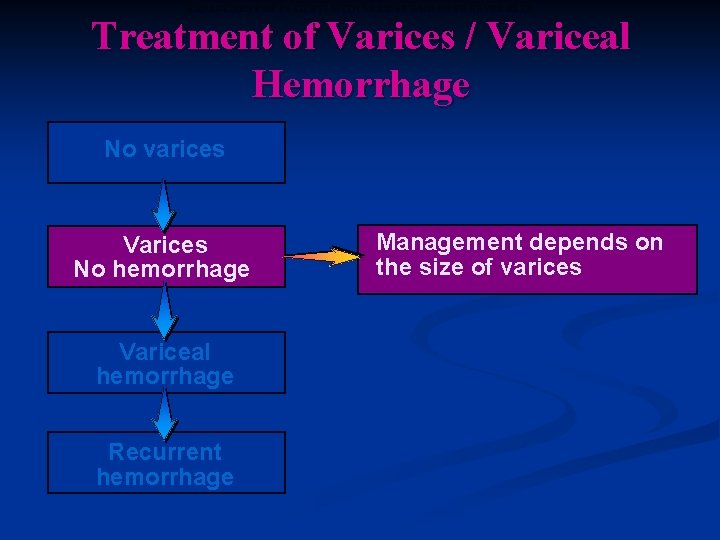
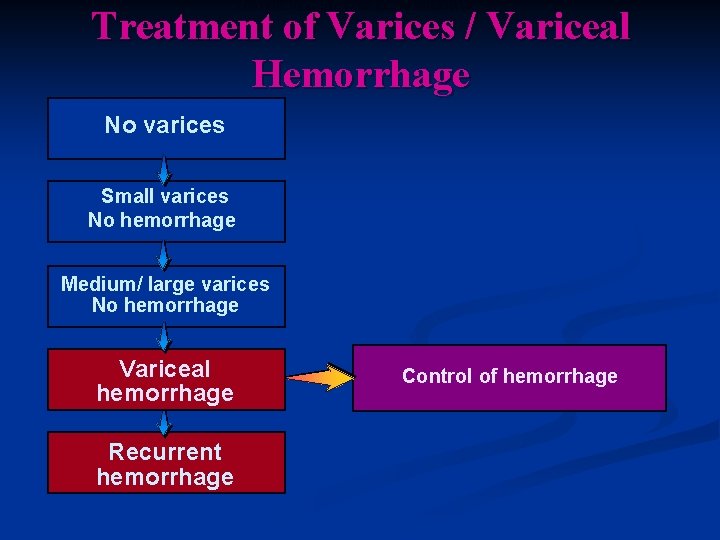
MANAGEMENT OF PATIENTS WITH VARICES WHO HAVE NEVER BLED Treatment of Varices / Variceal Hemorrhage No varices Varices No hemorrhage Variceal hemorrhage Recurrent hemorrhage Management depends on the size of varices

MANAGEMENT OF PATIENTS WITH MEDIUM/LARGE VARICES WITHOUT PRIOR HEMORRHAGE Treatment of Varices / Variceal Hemorrhage No varices Small varices No hemorrhage Medium/ large varices No hemorrhage Variceal hemorrhage Recurrent hemorrhage 1) -blockers (propranolol, nadolol) indefinitely 2) Endoscopic Variceal Ligation in patients intolerant to blockers
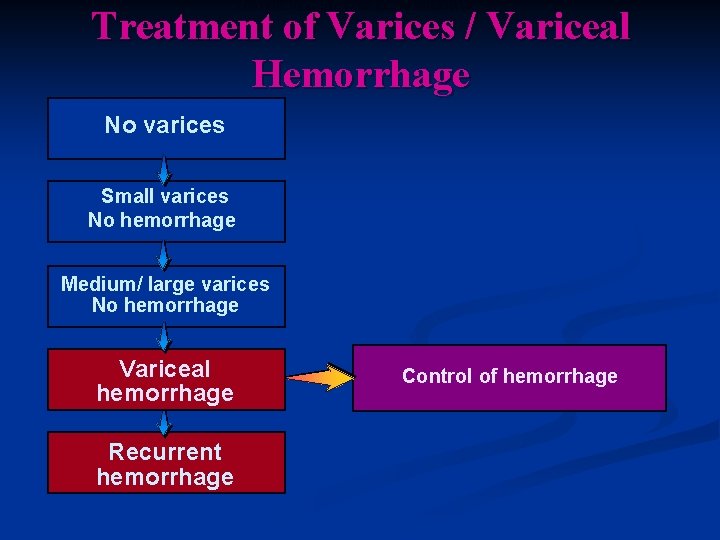
CONTROL OF ACUTE VARICEAL HEMORRHAGE Treatment of Varices / Variceal Hemorrhage No varices Small varices No hemorrhage Medium/ large varices No hemorrhage Variceal hemorrhage Recurrent hemorrhage Control of hemorrhage
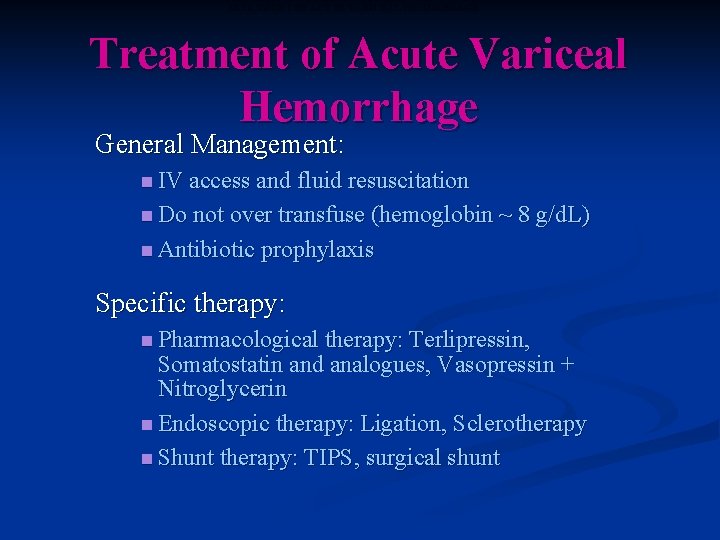
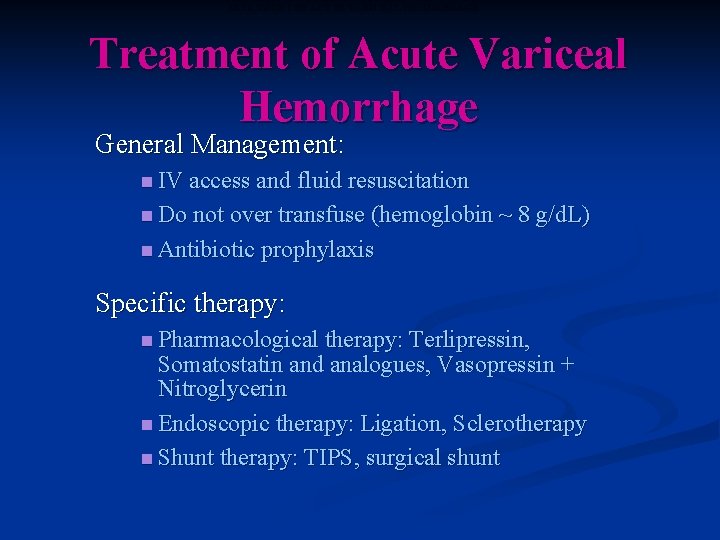
TREATMENT OF ACUTE VARICEAL HEMORRHAGE Treatment of Acute Variceal Hemorrhage General Management: n IV access and fluid resuscitation n Do not over transfuse (hemoglobin ~ 8 g/d. L) n Antibiotic prophylaxis Specific therapy: n Pharmacological therapy: Terlipressin, Somatostatin and analogues, Vasopressin + Nitroglycerin n Endoscopic therapy: Ligation, Sclerotherapy n Shunt therapy: TIPS, surgical shunt
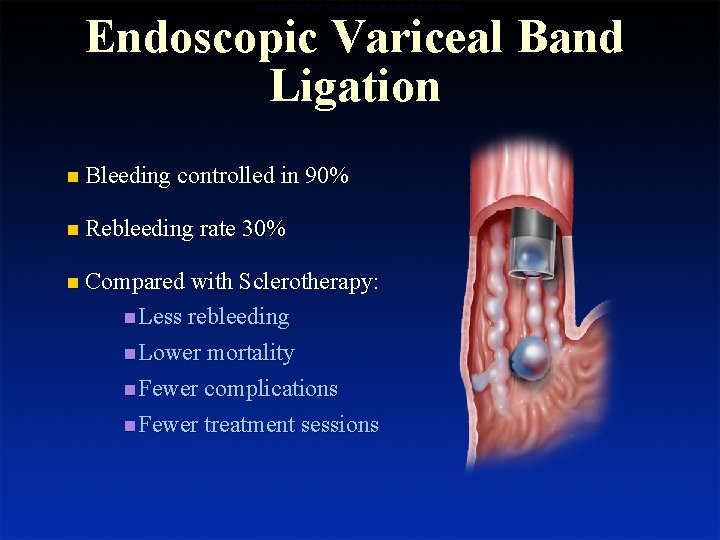
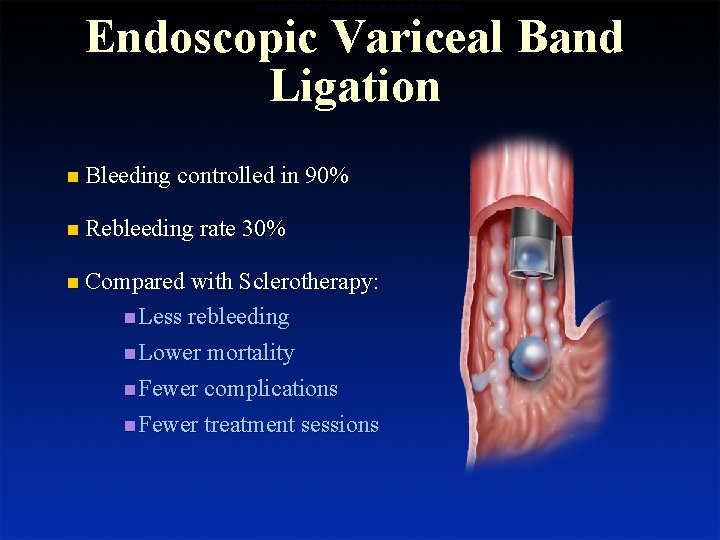
ENDOSCOPIC VARICEAL BAND LIGATION Endoscopic Variceal Band Ligation n Bleeding controlled in 90% n Rebleeding rate 30% n Compared with Sclerotherapy: n Less rebleeding n Lower mortality n Fewer complications n Fewer treatment sessions
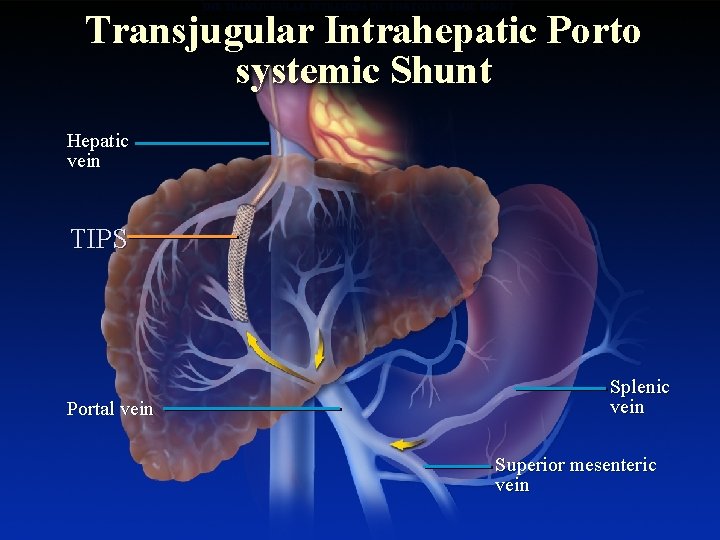
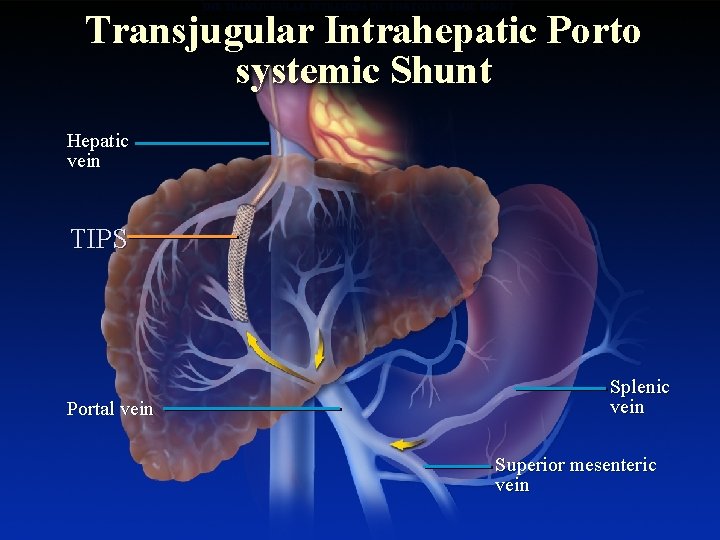
THE TRANSJUGULAR INTRAHEPATIC PORTOSYSTEMIC SHUNT Transjugular Intrahepatic Porto systemic Shunt Hepatic vein TIPS Portal vein Splenic vein Superior mesenteric vein
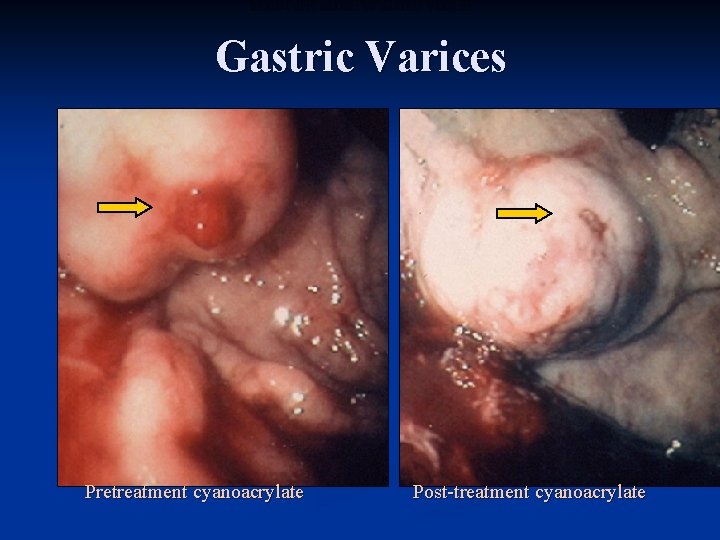
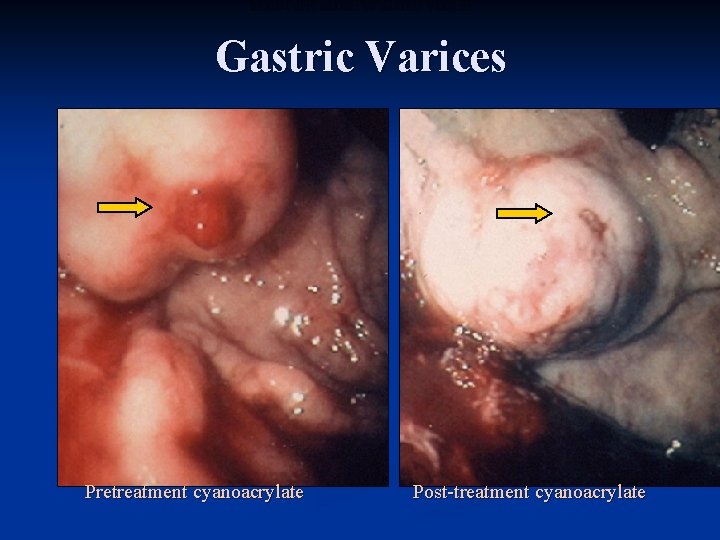
ENDOSCOPIC IMAGES OF GASTRIC VARICES Gastric Varices Pretreatment cyanoacrylate Post-treatment cyanoacrylate

Mild and Severe Portal Hypertensive Gastropathy ENDOSCOPIC IMAGES OF MILD AND SEVERE PORTAL HYPERTENSIVE GASTROPATHY Mild Mosaic pattern Severe Mosaic pattern + red spots Carpinelli et al. Ital J Gastroenterol Hepatol 1997; 29: 533
ASCITES AND HEPATORENAL SYNDROME Ascites and Hepatorenal Syndrome
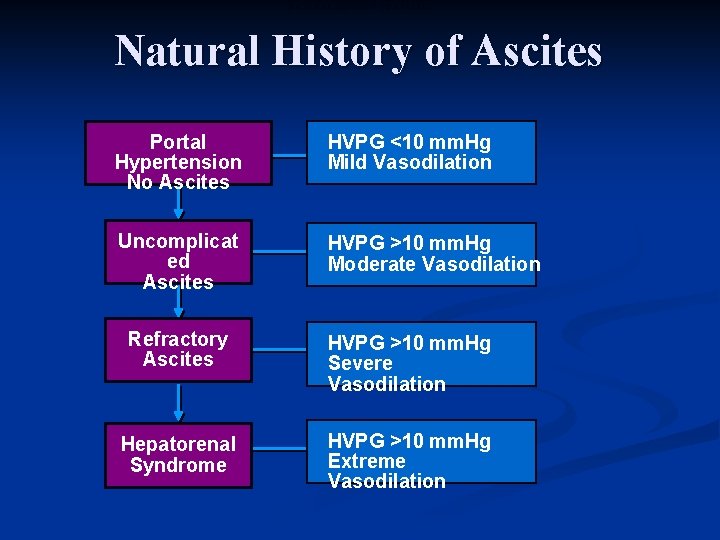
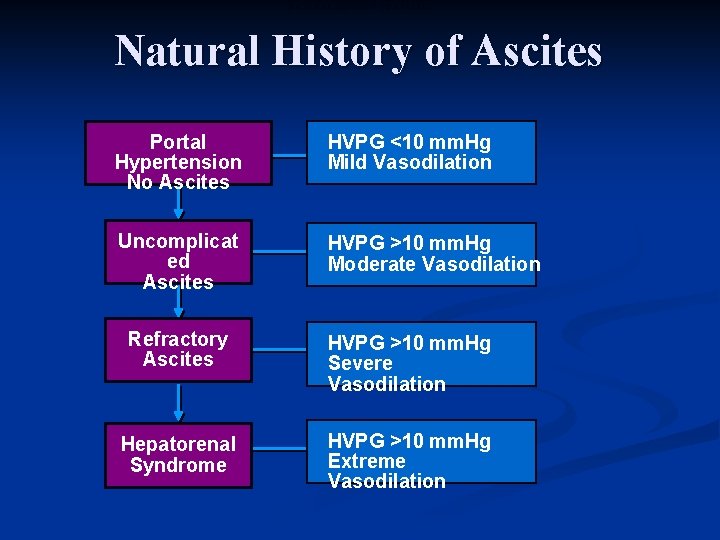
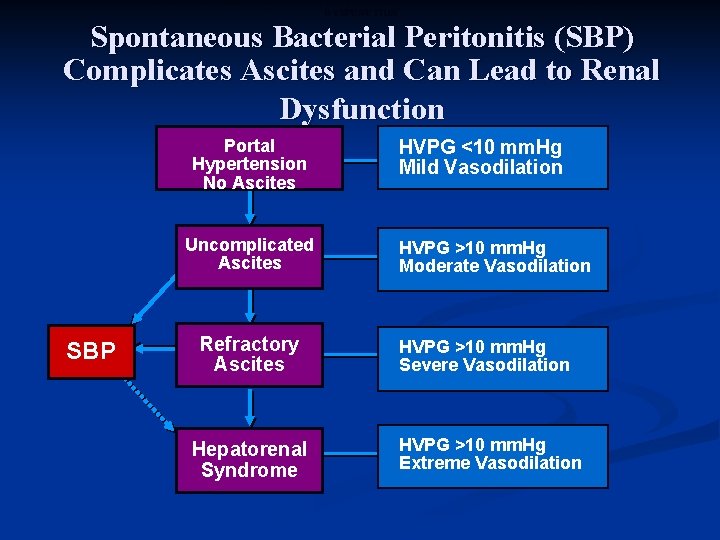
NATURAL HISTORY OF ASCITES Natural History of Ascites Portal Hypertension No Ascites HVPG <10 mm. Hg Mild Vasodilation Uncomplicat ed Ascites HVPG >10 mm. Hg Moderate Vasodilation Refractory Ascites HVPG >10 mm. Hg Severe Vasodilation Hepatorenal Syndrome HVPG >10 mm. Hg Extreme Vasodilation
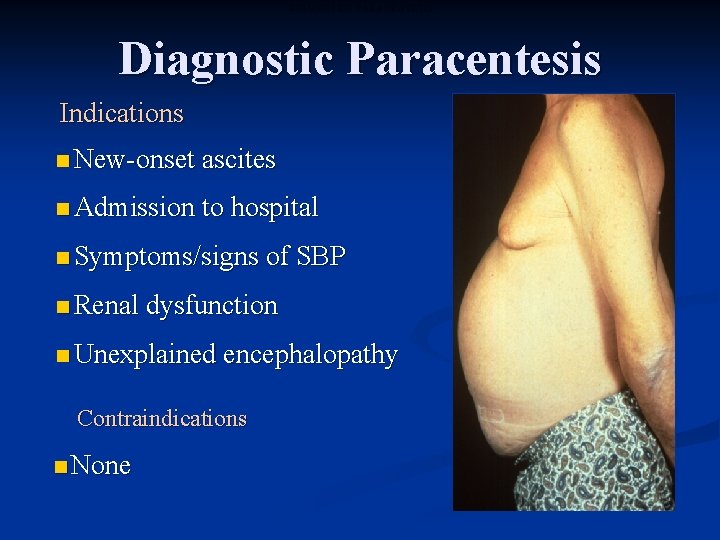
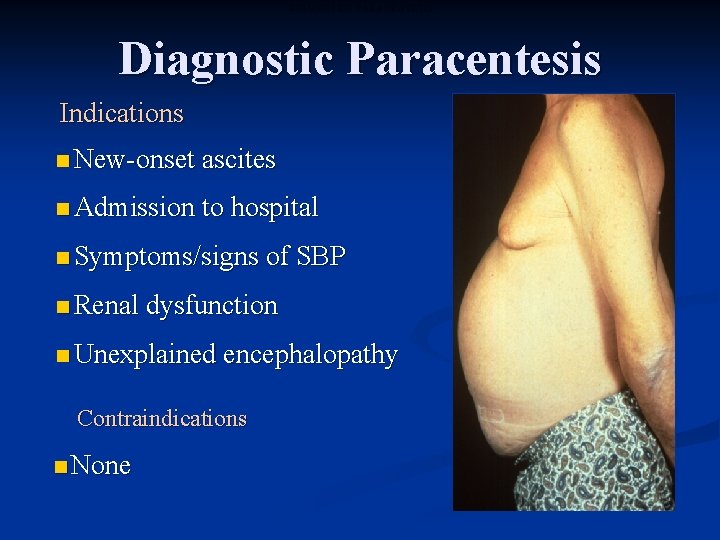
DIAGNOSTIC PARACENTESIS Diagnostic Paracentesis Indications n New-onset ascites n Admission to hospital n Symptoms/signs of SBP n Renal dysfunction n Unexplained encephalopathy Contraindications n None
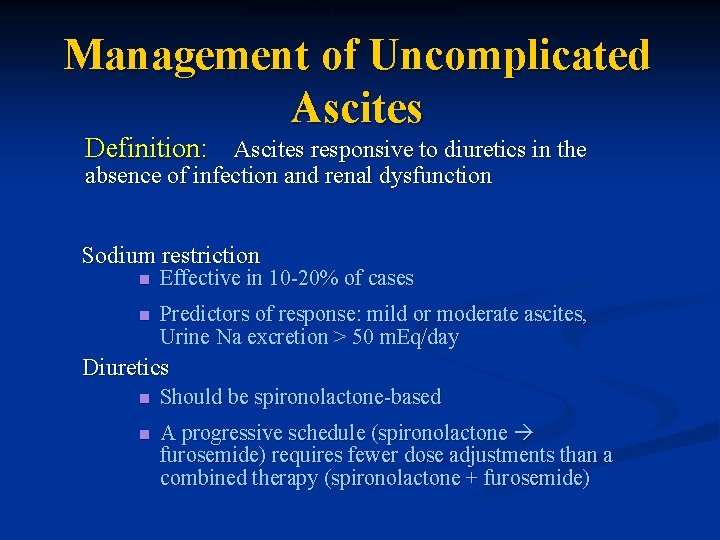
MANAGEMENT OF UNCOMPLICATED ASCITES Management of Uncomplicated Ascites Definition: Ascites responsive to diuretics in the absence of infection and renal dysfunction Sodium restriction n Effective in 10 -20% of cases n Predictors of response: mild or moderate ascites, Urine Na excretion > 50 m. Eq/day Diuretics n Should be spironolactone-based n A progressive schedule (spironolactone furosemide) requires fewer dose adjustments than a combined therapy (spironolactone + furosemide)
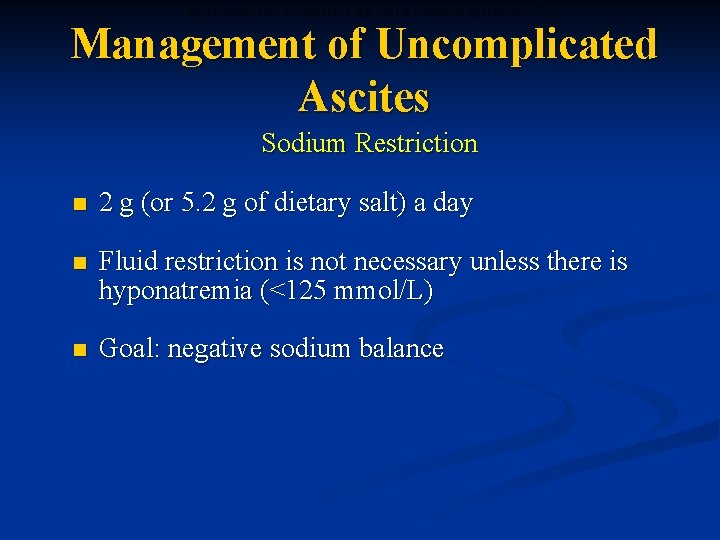
MANAGEMENT OF UNCOMPLICATED ASCITES: SODIUM RESTRICTION Management of Uncomplicated Ascites Sodium Restriction n 2 g (or 5. 2 g of dietary salt) a day n Fluid restriction is not necessary unless there is hyponatremia (<125 mmol/L) n Goal: negative sodium balance
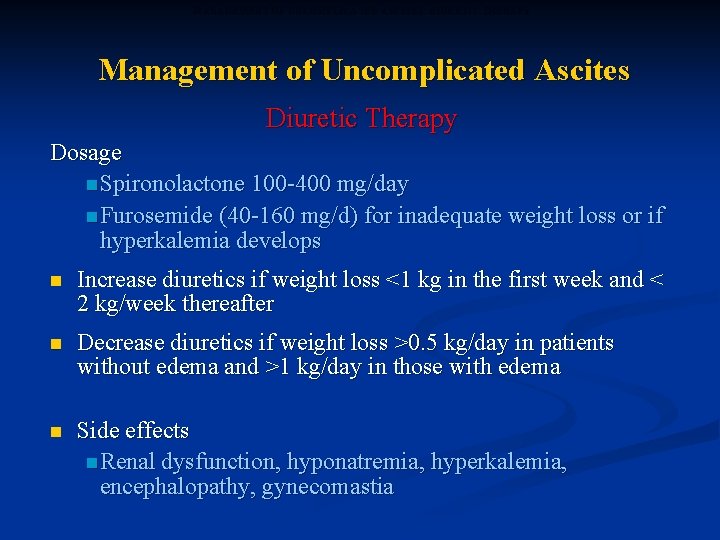
MANAGEMENT OF UNCOMPLICATED ASCITES: DIURETIC THERAPY Management of Uncomplicated Ascites Diuretic Therapy Dosage n Spironolactone 100 -400 mg/day n Furosemide (40 -160 mg/d) for inadequate weight loss or if hyperkalemia develops n Increase diuretics if weight loss <1 kg in the first week and < 2 kg/week thereafter n Decrease diuretics if weight loss >0. 5 kg/day in patients without edema and >1 kg/day in those with edema n Side effects n Renal dysfunction, hyponatremia, hyperkalemia, encephalopathy, gynecomastia
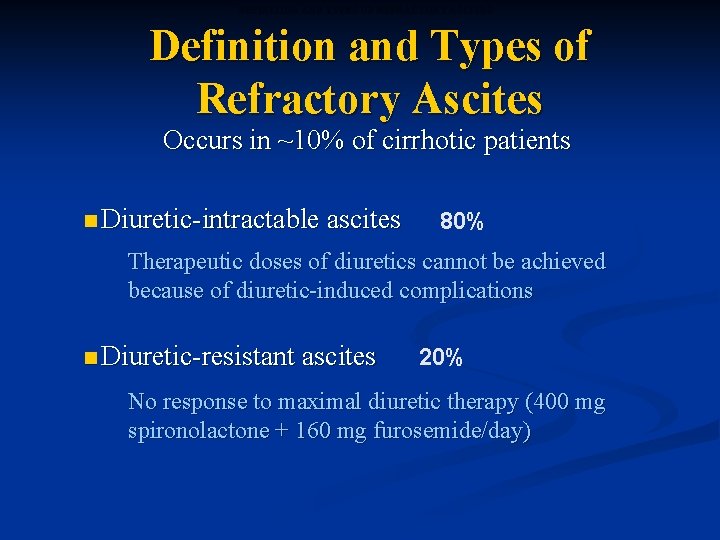
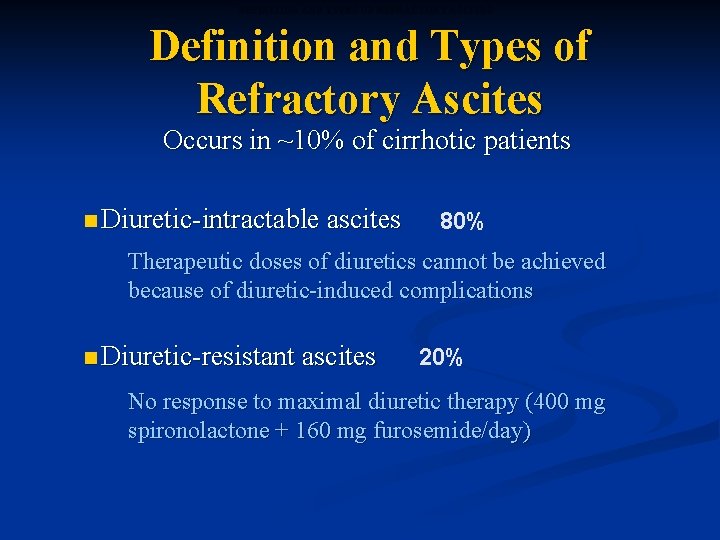
DEFINITION AND TYPES OF REFRACTORY ASCITES Definition and Types of Refractory Ascites Occurs in ~10% of cirrhotic patients n Diuretic-intractable ascites 80% Therapeutic doses of diuretics cannot be achieved because of diuretic-induced complications n Diuretic-resistant ascites 20% No response to maximal diuretic therapy (400 mg spironolactone + 160 mg furosemide/day)
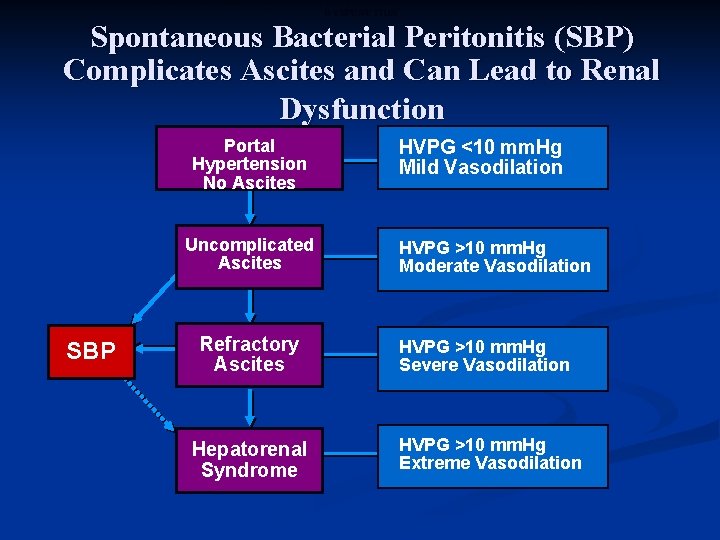
SPONTANEOUS BACTERIAL PERITONITIS (SBP) COMPLICATES ASCITES AND CAN LEAD TO RENAL DYSFUNCTION Spontaneous Bacterial Peritonitis (SBP) Complicates Ascites and Can Lead to Renal Dysfunction Portal Hypertension No Ascites Uncomplicated Ascites SBP Refractory Ascites Hepatorenal Syndrome HVPG <10 mm. Hg Mild Vasodilation HVPG >10 mm. Hg Moderate Vasodilation HVPG >10 mm. Hg Severe Vasodilation HVPG >10 mm. Hg Extreme Vasodilation
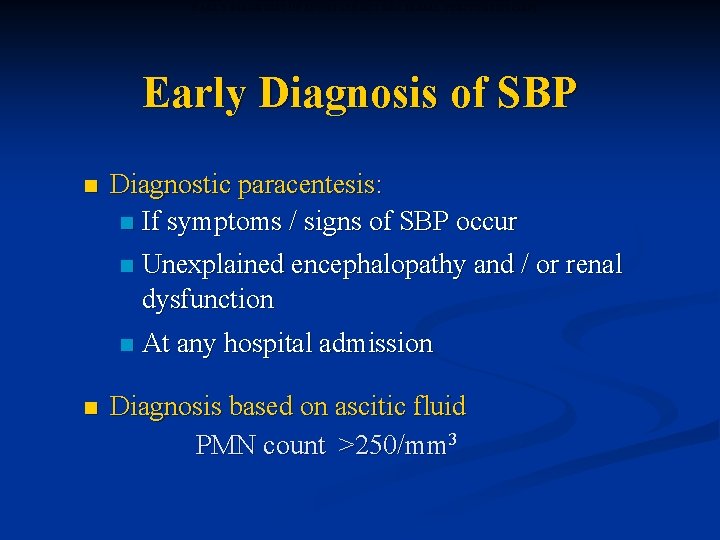
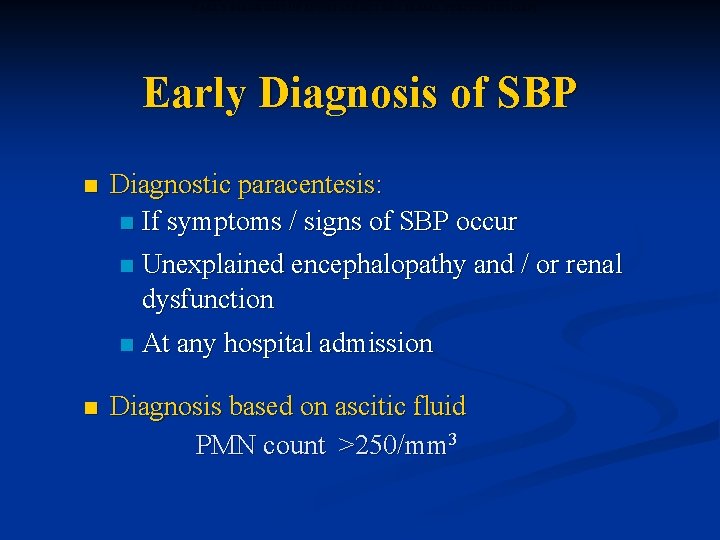
EARLY DIAGNOSIS OF SPONTANEOUS BACTERIAL PERITONITIS (SBP) Early Diagnosis of SBP n Diagnostic paracentesis: n If symptoms / signs of SBP occur n Unexplained encephalopathy and / or renal dysfunction n n At any hospital admission Diagnosis based on ascitic fluid PMN count >250/mm 3
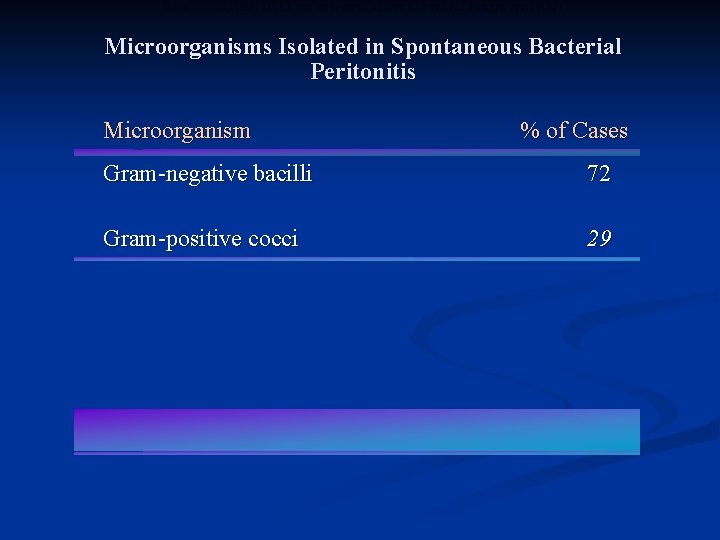
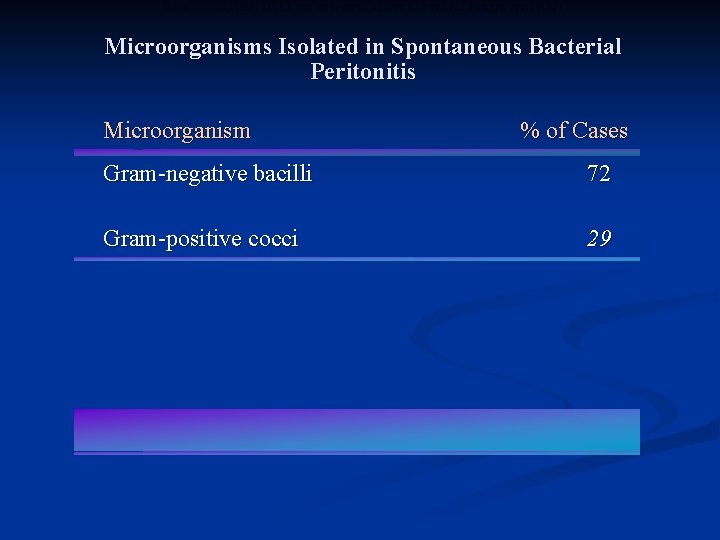
MICROORGANISMS ISOLATED IN SPONTANEOUS BACTERIAL PERITONITIS (SBP) Microorganisms Isolated in Spontaneous Bacterial Peritonitis Microorganism % of Cases Gram-negative bacilli 72 Gram-positive cocci 29
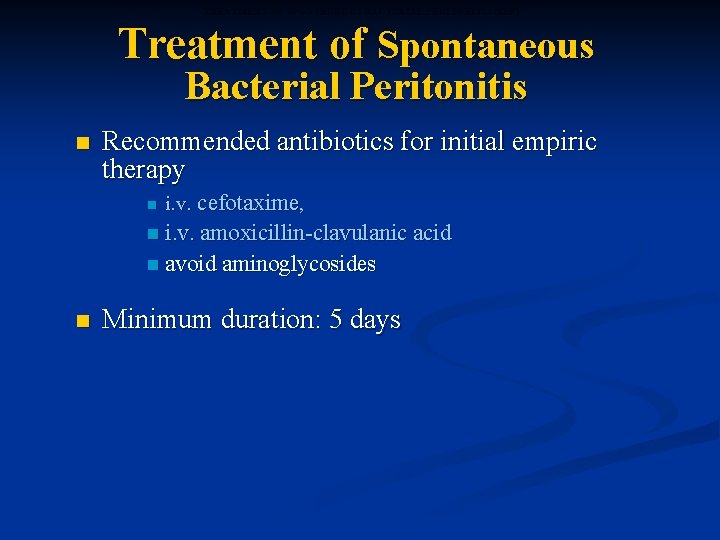
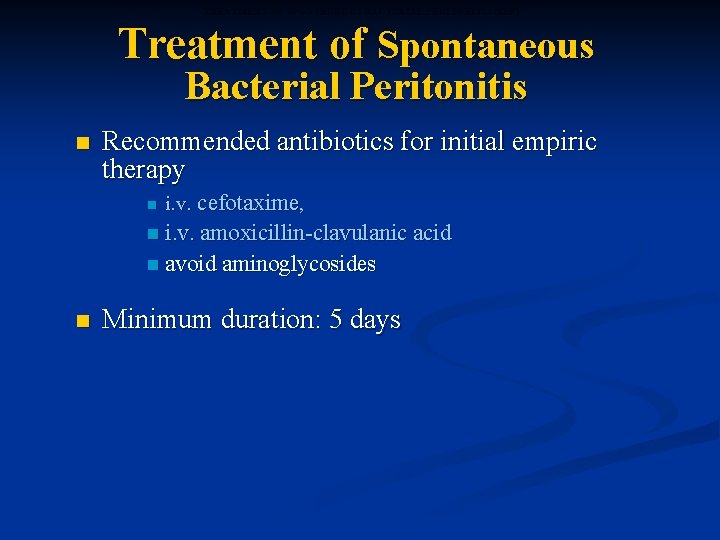
TREATMENT OF SPONTANEOUS BACTERIAL PERITONITIS (SBP) Treatment of Spontaneous Bacterial Peritonitis n Recommended antibiotics for initial empiric therapy n i. v. cefotaxime, n i. v. amoxicillin-clavulanic acid n avoid aminoglycosides n Minimum duration: 5 days

INDICATIONS FOR PROPHYLACTIC ANTIBIOTICS TO PREVENT SPONTANEOUS BACTERIAL PERITONITIS (SBP) Indications for Prophylactic Antibiotics to Prevent Spontaneous Bacterial Peritonitis n Patients who have recovered from SBP (long-term) n Norfloxacin 400 mg p. o. daily, indefinitely n Weekly Quinolones
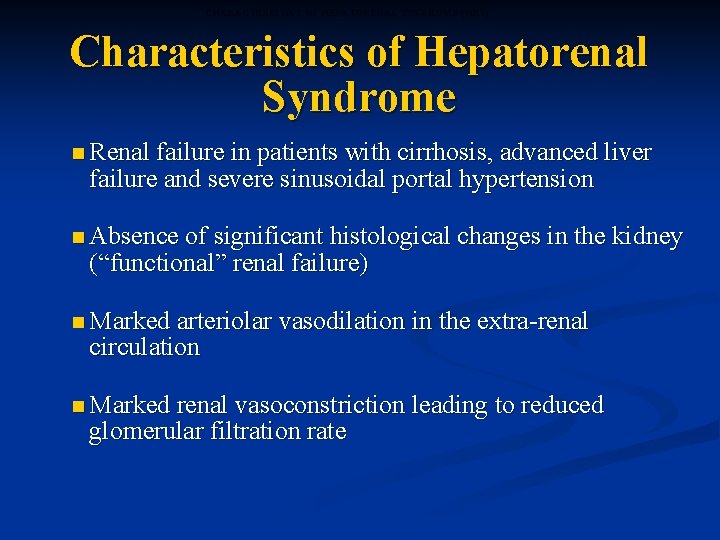
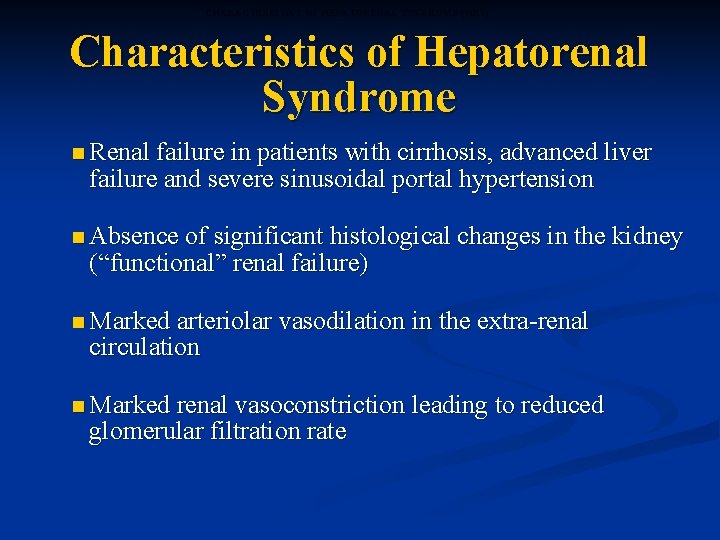
CHARACTERISTICS OF HEPATORENAL SYNDROME (HRS) Characteristics of Hepatorenal Syndrome n Renal failure in patients with cirrhosis, advanced liver failure and severe sinusoidal portal hypertension n Absence of significant histological changes in the kidney (“functional” renal failure) n Marked arteriolar circulation vasodilation in the extra-renal n Marked renal vasoconstriction leading to reduced glomerular filtration rate
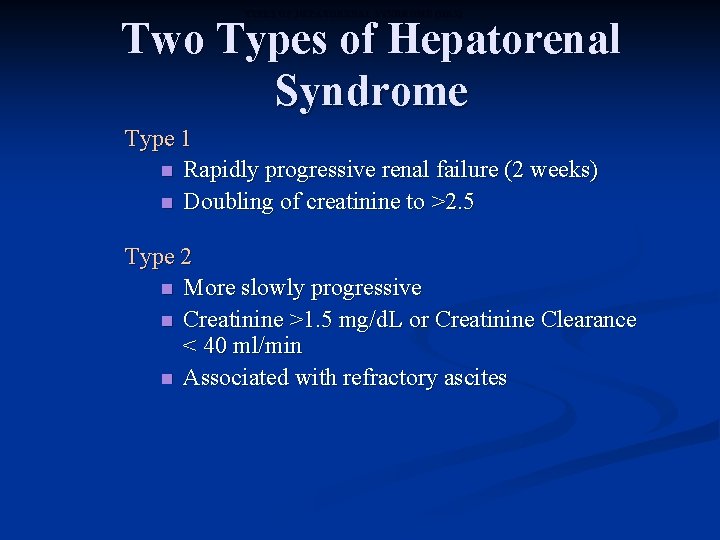
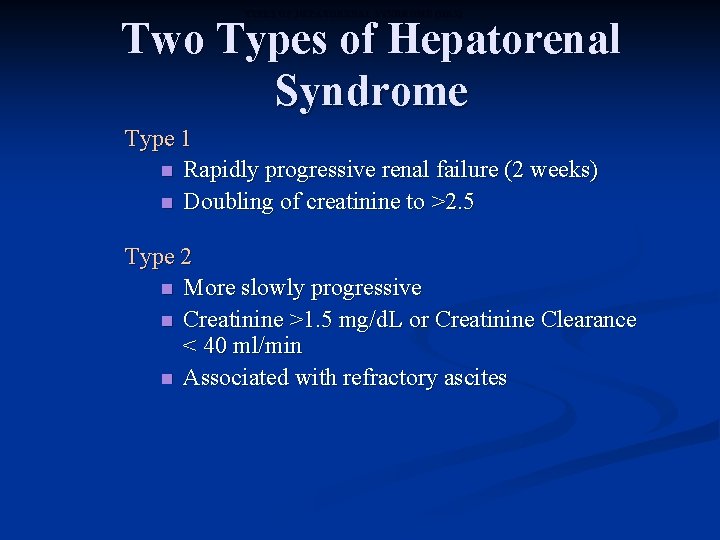
TYPES OF HEPATORENAL SYNDROME (HRS) Two Types of Hepatorenal Syndrome Type 1 n Rapidly progressive renal failure (2 weeks) n Doubling of creatinine to >2. 5 Type 2 n More slowly progressive n Creatinine >1. 5 mg/d. L or Creatinine Clearance < 40 ml/min n Associated with refractory ascites
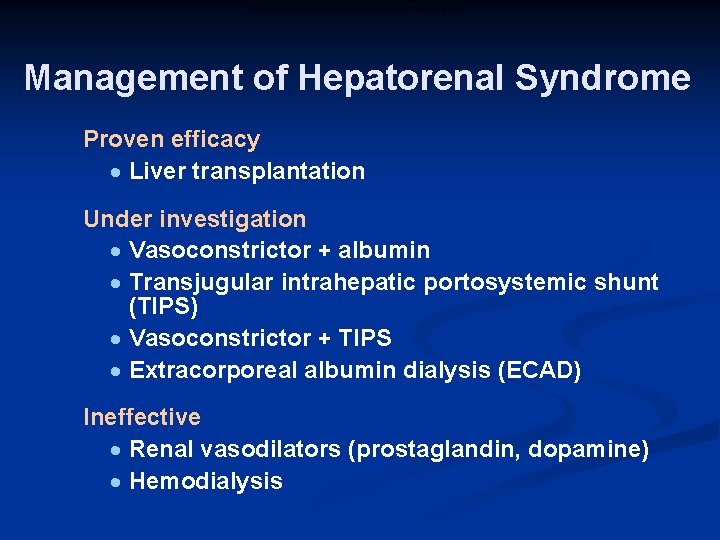
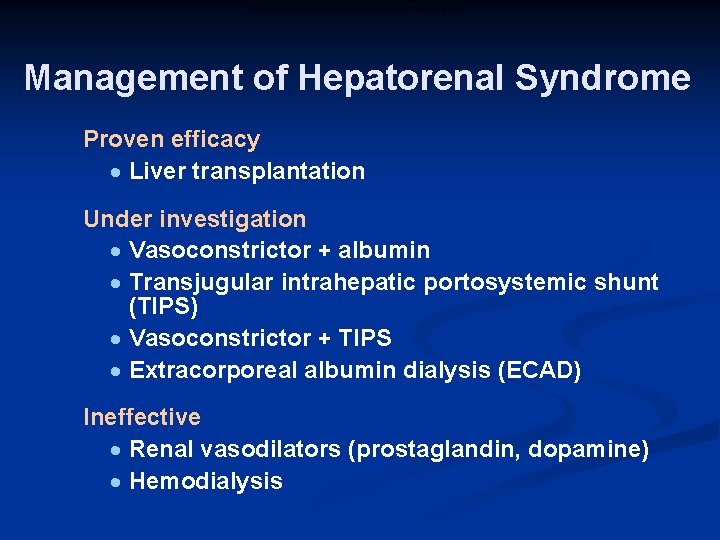
MANAGEMENT OF HEPATORENAL SYNDROME Management of Hepatorenal Syndrome Proven efficacy · Liver transplantation Under investigation · Vasoconstrictor + albumin · Transjugular intrahepatic portosystemic shunt (TIPS) · Vasoconstrictor + TIPS · Extracorporeal albumin dialysis (ECAD) Ineffective · Renal vasodilators (prostaglandin, dopamine) · Hemodialysis
Hepatic Encephalopathy
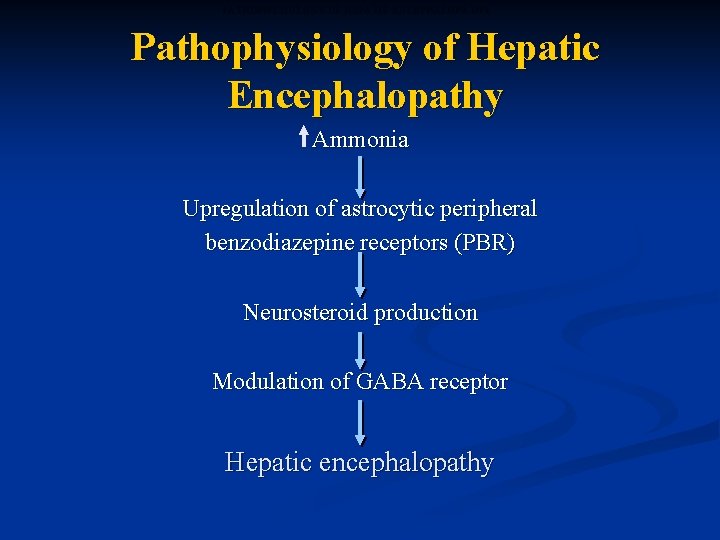
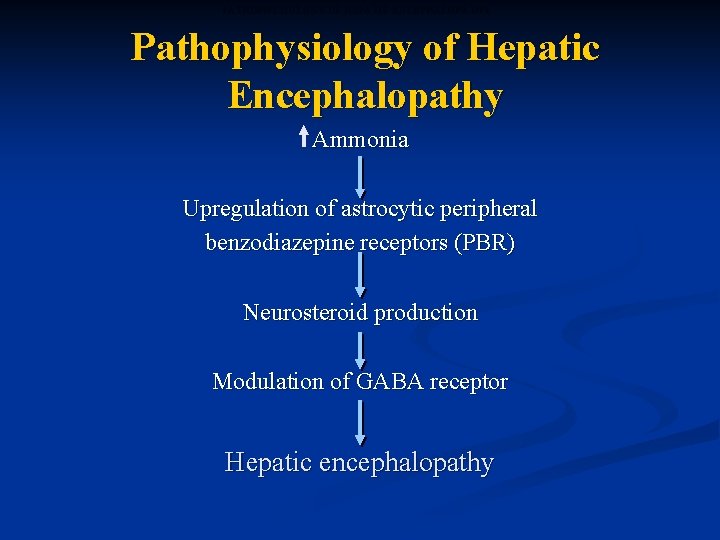
PATHOPHYSIOLOGY OF HEPATIC ENCEPHALOPATHY Pathophysiology of Hepatic Encephalopathy Ammonia Upregulation of astrocytic peripheral benzodiazepine receptors (PBR) Neurosteroid production Modulation of GABA receptor Hepatic encephalopathy
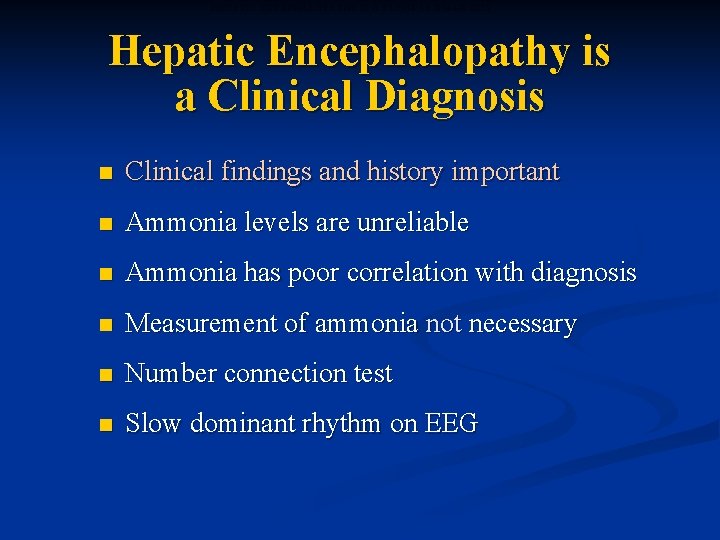
HEPATIC ENCEPHALOPATHY IS A CLINICAL DIAGNOSIS Hepatic Encephalopathy is a Clinical Diagnosis n Clinical findings and history important n Ammonia levels are unreliable n Ammonia has poor correlation with diagnosis n Measurement of ammonia not necessary n Number connection test n Slow dominant rhythm on EEG
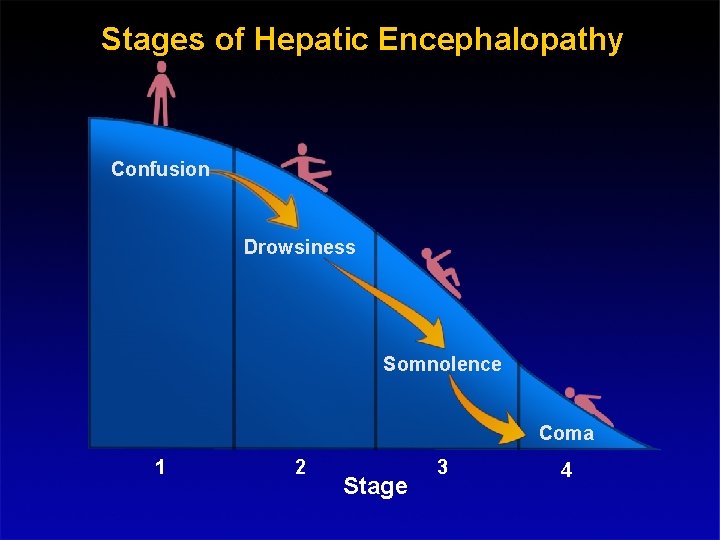
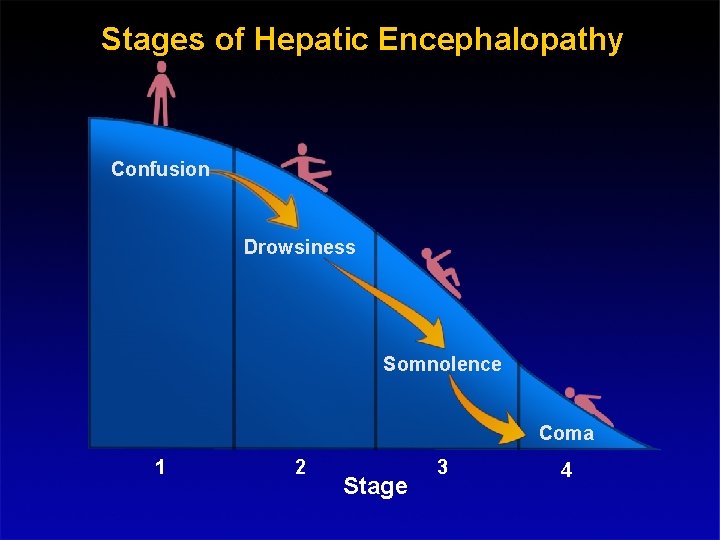
STAGES OF HEPATIC ENCEPHALOPATHY Stages of Hepatic Encephalopathy Confusion Drowsiness Somnolence Coma 1 2 Stage 3 4
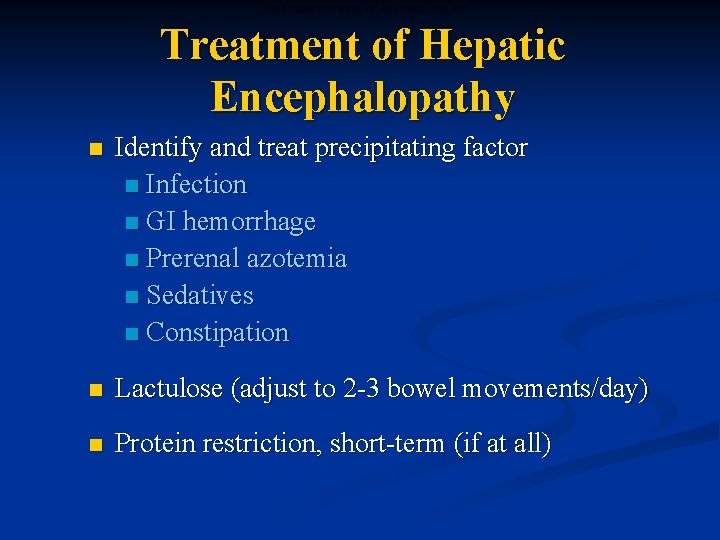
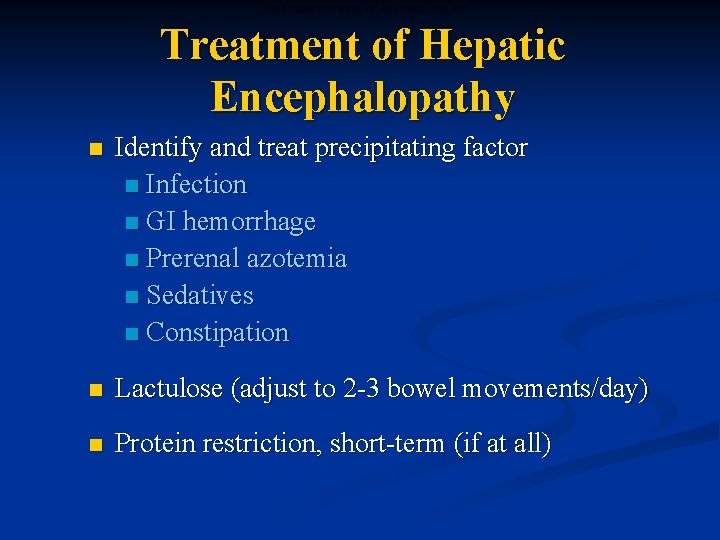
TREATMENT OF HEPATIC ENCEPHALOPATHY Treatment of Hepatic Encephalopathy n Identify and treat precipitating factor n Infection n GI hemorrhage n Prerenal azotemia n Sedatives n Constipation n Lactulose (adjust to 2 -3 bowel movements/day) n Protein restriction, short-term (if at all)
Liver transplant n All patients with end stage liver disease should be assessed for liver transplant when ever is proven to significantly prolong survival and improve quality of life in a coast effective manner over natural history of the liver disease and other medical and non transplant surgical intervention.
 Cld chronic liver disease
Cld chronic liver disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Liver defination
Liver defination Portal hypertension
Portal hypertension Periradicular diseases
Periradicular diseases Etiology of cerebrovascular disease
Etiology of cerebrovascular disease Costal margin
Costal margin Hobnail fibrotic liver
Hobnail fibrotic liver Nutmeg liver slideshare
Nutmeg liver slideshare Chronic rheumatic heart disease
Chronic rheumatic heart disease Jewish chronic disease hospital study
Jewish chronic disease hospital study Chronic disease
Chronic disease Ersd
Ersd Chronic disease
Chronic disease Kate lorig stanford
Kate lorig stanford Nih scale
Nih scale Pneumonia
Pneumonia Chronic granulomatous disease
Chronic granulomatous disease Wagner model of chronic disease management
Wagner model of chronic disease management Gennifer shafer liver disease
Gennifer shafer liver disease Gastroenterology board review
Gastroenterology board review Alcoholic liver disease
Alcoholic liver disease Elisabetta bugianesi
Elisabetta bugianesi Infiltrative liver disease
Infiltrative liver disease Symptoms of portal hypertension
Symptoms of portal hypertension Cml stages
Cml stages Types of bronchial asthma
Types of bronchial asthma Mantoux test reading
Mantoux test reading Examples of pes
Examples of pes Etiology of eclampsia
Etiology of eclampsia Pathophysiology definition
Pathophysiology definition Criminology etiology
Criminology etiology Etiology
Etiology Etiology synonym
Etiology synonym Subcecal appendix
Subcecal appendix Etiological models of addiction
Etiological models of addiction Synonyms for etiology
Synonyms for etiology Etiology of malaria
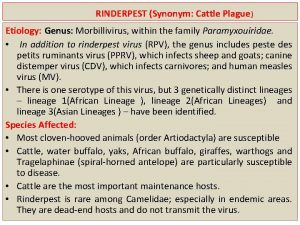
Etiology of malaria Difference between nursing bottle caries and rampant caries
Difference between nursing bottle caries and rampant caries