The epidemiology and etiology of diarrhea Diarrhea in














- Slides: 68
The epidemiology and etiology of diarrhea
Diarrhea in young children n 3 -4 episodes /child / year n 3200 000 death / year n Causes about 30% of infant death in developing countries n 80% death due to diarrhea occur in first years of life n Diarrhea is an important cause of malnutrition
Three clinical types of diarrhea 1. Acute watery diarrhea 2. Bloody diarrhea 3. Persistent diarrhea dehydration , potassium loss tissue damage, toxemia malnutrition
Host factors that increase susceptibility to diarrhea n Failing to breast - feed until at least 2 years n Malnutrition n Measles n immunosuppression
Behavioral risk factors for diarrhea n Inadequate breast feeding n Using feeding bottles n Eating food hours after cooking it n Drinking contaminated water n Not washing soiled hands n Not disposing of feces
Prevention of diarrhea ( host factors) n Breast feed at least 2 years n Give plenty of good food , start at age 4 -6 month n Immunize against measles
Fluids for home therapy n ORS solution n Water n Food - based fluids soup rice water Yoghurt drink Glucose water
Age of diarrhea 1. 2. n n n Most diarrhea episodes occur during the first 2 years of life Incidence is highest in the age group 6 -11 month Declining levels of maternally acquired antibodies The lack of active immunity in the infant The introduction of food
seasonality n n n In temperate climate ; bacterial diarrhea occur more frequently during the warm season whereas the peak Viral diarrhea particularly rotavirus is during the winter In the tropical areas; rotavirus diarrhea occurs throughout the year and increasing in cool month Whereas bacterial diarrheas peak during warmer , rainy season The incidence persistent diarrhea follows the same seasonal pattern as that acute watery diarrhea
Etiology of diarrhea n n n n Rotavirus Enterotoxigenic Escherichia coli Shigella Campylobacter jejuni cryptosporidium Vibrio cholera salmonella (Non thyphoid ) Entropathogenic Escherchia coli
Pathogenic mechanisms ( viruses) n Replicate within the villous epithelium of small bowel n Patchy epithelial cell destruction and villous shortening n The Loss of normally absorptive villous cells n Replacement immature , secretary , crypt- like cells n Loss of disaccharides , especially lactose
Pathogenic mechanisms (bacteria) n n n Mucosal adhesion to avoid being swept away Entrotoxicogenic E. coli , vibrio. cholera Toxins that cause secretion that reduce the absorption of Na and increase the secretion of chloride Entrotixigenic E. coli , v. cholera Mucosal invasion occurs in the colon and distal ileum and destroying mucosal epithelial cells and cause bloody diarrhea Shigella , C. jejuni , entroinvasive E. coli and salmonella
Pathogenic mechanisms (protozoa) n n Mucosal adhesion and cause shortening of the villi G, lambelia , cryptosporidum Mucosal invasion in the colon or ileum and causing micro absess and ulcer E, histolitica
Campilobacter jejuni n C, jejuni causes disease mostly in infants n C, jejuni also infects animals and spread by contact with their n n feces or consumption of contaminated food , milk , or water n C, jejuni can cause watery diarrhea or dysentery n Fever may be preset and episodes are not sever and last 2 -5 days n Erythromycin shorten the illness
cryptosporidium n This parasite causes diarrhea in infants immunodeficient patients , and a variety of domestic animals n Infection is frequent in developing countries n Most episodes of illness occur in the first year of life n Diarrhea is usually neither severe nor prolonged n Diarrhea is sever in malnutrition , or AIDS , immunodeficient patients
Prevention of diarrhea n Give only breast milk for first 4 -6 month n Do not use feeding bottle n Prepare and store food safely n Use clean water for drinking n Wash hands when soiled n Dispose of faeces safely
Treatment of acute diarrhea the main points n Replace lost water and salt n Continue to feed
Benefit of antibiotics in acute diarrhea n n Helpful for patients with ; Bloody diarrhea Suspected cholera with severe dehydration 5 -15% No practical value for others because ; Ineffective for pathogen Pathogen not known 85 -95%

Treatment acute diarrhea other points n Only give antibiotic for ; Bloody diarrhea Suspected cholera with severe dehydration n Only give anti protozoals ; No response to treatment for shigella Proven amebiasis
Treatment of diarrhea 1. 2. 3. Replacement of fluids and electrolytes Feeding should be continued in all types of diarrhea Antimicrobial and anti parasitic agents should not be used
Treatment of diarrhea 1. Antimicrobial and anti parasitic agents should not be used exception is ; n Dysentery n Suspected cholera with sever dehydration n Persistent diarrhea when trophozoites or cysts of giardia or trophozoites of E, hystolytica are seen in feces or intestinal fluid or pathogenic enteric bacteria are identified by stool culture
Pathophysiology of watery diarrhea
Pathophysiology of watery diarrhea n n Normally absorption and secretion of water and electrolytes occur throughout the intestine Water and electrolytes are simultaneously absorbed by the villi and secreted by the crypts More than 90% of the fluid entering the small intestine is absorbed Only 100 -200 cc of water excreted each day in formed stools

Absorption and secration Villus n Active absorption of Na n Na absorbed with glucose and aminoacids Crypt ; n Active secretion of choloride
Pathophysiology of watery diarrhea n n Watery diarrhea is caused by a disturbance in the mechanism of transport of water and electrolytes in the small intestine Intestinal transport mechanisms are also the basis for the management of diarrhea
Intestinal absorption water and electerolytes Absorption water from the small intestine is caused by osmotic gradients that created when Na are actively absorbed
Mechanisms of the watery diarrhea n There are several mechanisms for Na absorption 1. Na is linked to the absorption of chloride ion 2. Absorbed directly as Na ion 3. Exchanged for hydrogen ion 4. Or linked to the absorption of organic substances such as glucose or certain amino acids

Intestinal secretion of water and electrolytes n Secretion of water and electrolytes normally occurs in the crypts n Na is transported from the ECF into the epithelial cell n Na is then pumped back into the ECF by Na k ATPase n n Secretory stimuli cause chloride ions to pass through the luminal membrane of the crypt cells into the bowel lumen Osmotic gradient that causes water and electrolytes to flow passively from the ECF into the bowel

Mechanisms of the watery diarrhea n 1. 2. • n There are two principal mechanisms ; Secretion Osmotic action intestinal infection cause diarrhea by both mechanisms. Secretory diarrhea is more common Both mechanisms may occur in a single individual
Secretory diarrhea n There is abnormal secretion of water and electrolytes into the small bowel n Absorption Na by the villi is impaired n Secretion chloride in the crypt cell cotinuous or increased n fluid secretion and Loss water and Na as watery stools , and dehydration

Causes of secretory diarrhea n n n Toxicogenic bacteria Vibrio cholerae E, choli Campilobacter Shigella Salmonella Enteric viruses n ritaviruse
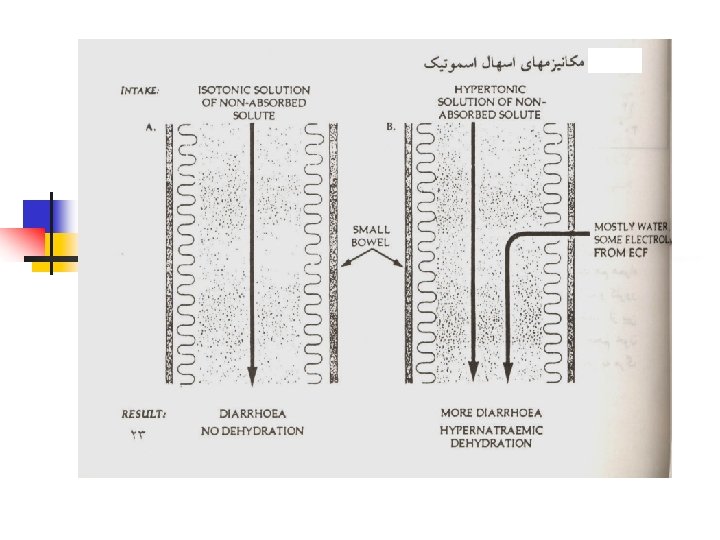
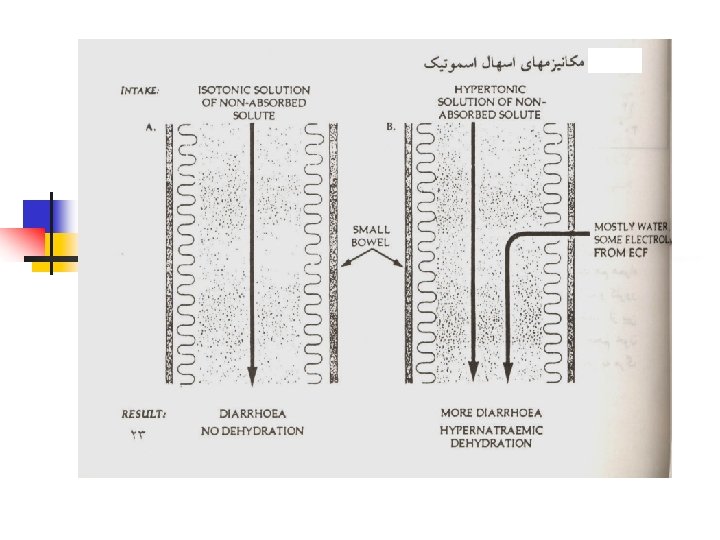
Osmotic diarrhea n n Water and electrolytes move rapidly across the epithelium of small bowel mucosa to maintain osmotic balance Diarrhea can occur when a poorly absorbed osmotically active substance is ingested
Osmotic diarrhea n n If the substance is isotonic solution causing diarrhea but not dehydration (lactose , glucose , magnesium sulfate ) If non absorbed substance is hypertonic solution water move from the ECF into the gut , that causes diarrhea with dehydration and hypernatremia
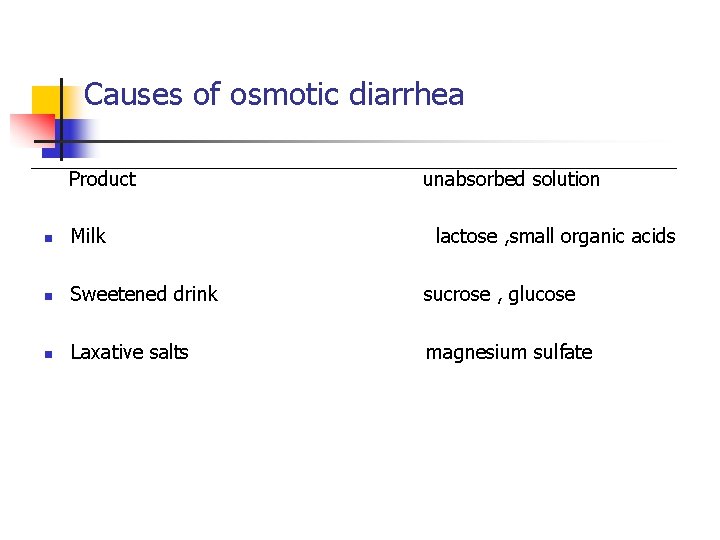
Causes of osmotic diarrhea Product unabsorbed solution n Milk lactose , small organic acids n Sweetened drink sucrose , glucose n Laxative salts magnesium sulfate


Isotonic dehydration This is the most type of dehydration Losses of water and Na are in the same proportion n n There is a balanced deficit of water and Na Serum Na concentration is normal (130 -150 m mol / l ) Serum osmolality is normal (275 -295) Hypovolemia occurs as a result of loss of extra cellular fluid

Hypernatremic dehydration n n n There is loss of water excess of Na It is usually results from ; ingestion of hypertonic fluid that not efficiently absorbed Insufficient intake of water or low –solute drink There is a deficit of water and Na deficit of water is greater Serum Na concentration is elevated (>150 mmol/l) Serum osmolality is elevated (>295 m osmol/l ) Thirst is severe and the child is very irritable Sezures may occur (Na >165 mmol /l)
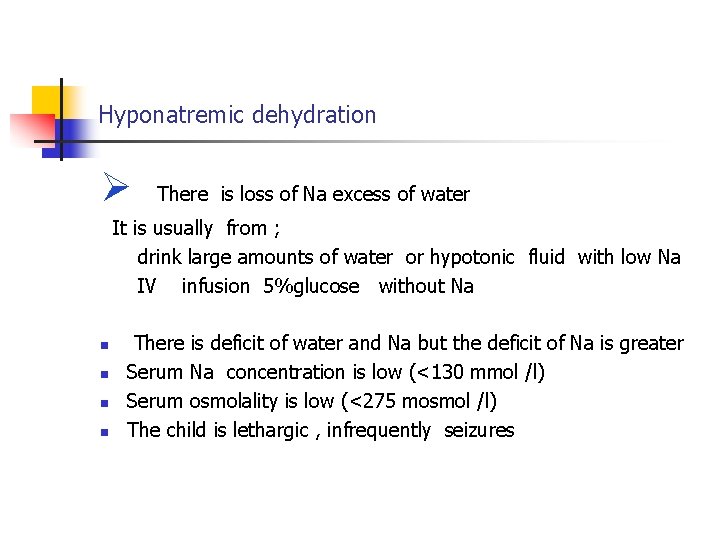
Hyponatremic dehydration There is loss of Na excess of water It is usually from ; drink large amounts of water or hypotonic fluid with low Na IV infusion 5%glucose without Na n n There is deficit of water and Na but the deficit of Na is greater Serum Na concentration is low (<130 mmol /l) Serum osmolality is low (<275 mosmol /l) The child is lethargic , infrequently seizures
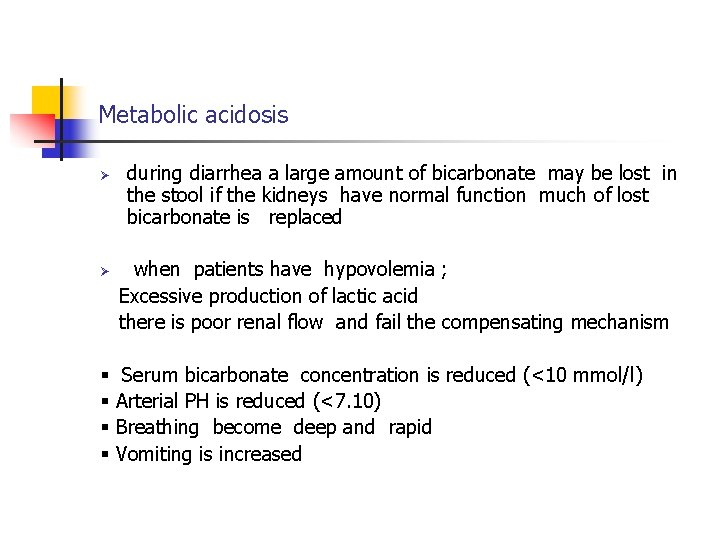
Metabolic acidosis during diarrhea a large amount of bicarbonate may be lost in the stool if the kidneys have normal function much of lost bicarbonate is replaced when patients have hypovolemia ; Excessive production of lactic acid there is poor renal flow and fail the compensating mechanism Serum bicarbonate concentration is reduced (<10 mmol/l) Arterial PH is reduced (<7. 10) Breathing become deep and rapid Vomiting is increased
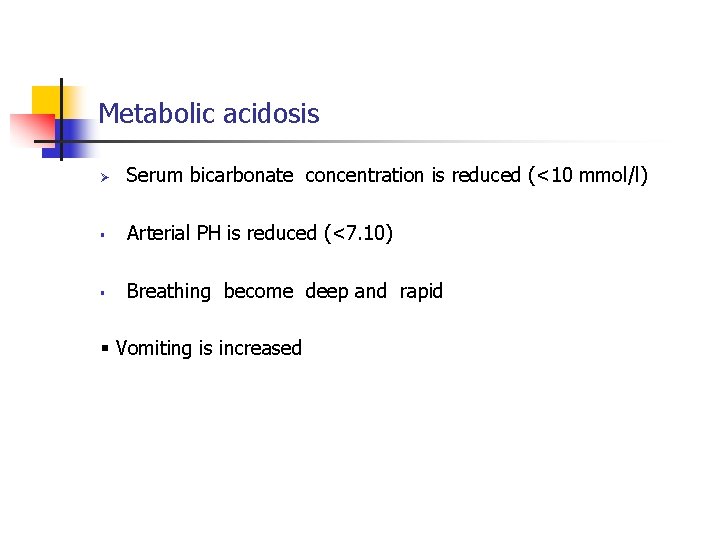
Metabolic acidosis Serum bicarbonate concentration is reduced (<10 mmol/l) Arterial PH is reduced (<7. 10) Breathing become deep and rapid Vomiting is increased
Metabolic effect of watery diarrhea n Loss of water and salt n Excess loss of bicarbonate n Excess loss of K hypovolemia shock acidosis K deplation
hypokalemia Patients with diarrhea often develop K depletion When K and bicarbonate are lost together hypokalemia does not usually develop n n The signs of hypokalemia may include ; General muscular weakness Cardiac arrhythmias Paralytic ileus

Oral rehydration therapy n ORT is based on the principle that intestinal absorption of Na is enhanced by the active absorption of glucose and aminoacids
Oral rehydration therapy n n ORT is based on the principle that intestinal absorption of Na is enhanced by the active absorption of glucose and aminoacids This process is normal during secretory diarrhea If patients with secretory diarrhea drink an isotonic salt solution without glucose or aminoacids Na is not absorbed When a balanced isotonic solution of glucose and salt is given glucose linked Na absorption occurs and this is accompanied the absorption of water by
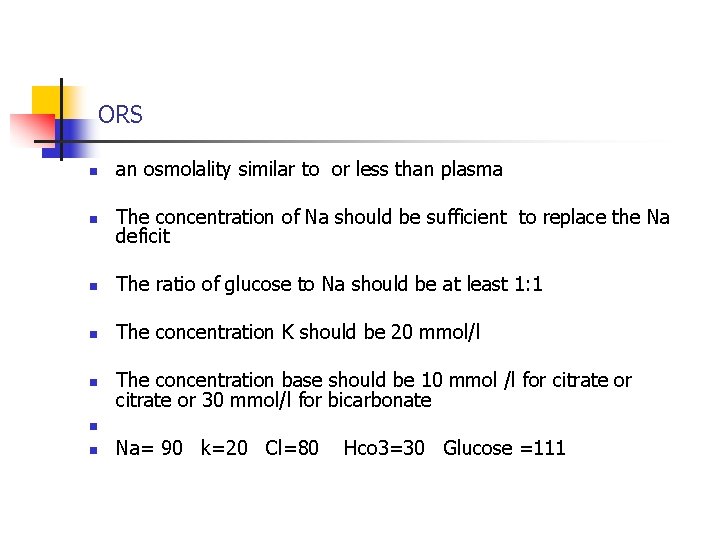
ORS n an osmolality similar to or less than plasma n The concentration of Na should be sufficient to replace the Na deficit n The ratio of glucose to Na should be at least 1: 1 n The concentration K should be 20 mmol/l n The concentration base should be 10 mmol /l for citrate or 30 mmol/l for bicarbonate n n Na= 90 k=20 Cl=80 Hco 3=30 Glucose =111
When ORT is not effective n Severe repeated vomiting n Severe diarrhea >15 cc /kg /h n Glucose malabsorption
ORT inappropriate for n n paralytic ileus abdominal distension initial treatment of Severe dehydration because fluid must be replaced very rapidly Patients who are unable to drink
Assessing the patient with diarrhea n n n Ask, look and feel for dehydration General condition? Well , alert? Restless , irritable? floppy, lethargic, or unconscious?
Assessing the patient with diarrhea n n Eyes: normal? Sunken? Very sunken and dry? Tear: have tear? Mouth and tongue: wet? dry? very dry? Thirst: drinks normal? drinks eagerly? drinks poorly? n Skin pinch: immediately? Slowly(>2 se) ? very slowly? n Additional sign: anterior fontanel? pulse? Breathing?
Determine the degree of dehydration and select tereatment n n Two or more signs in one column including at least one key sign means that the patient falls in that category. C-severe dehydration deficit equal more than 10% B- some dehydration ( mild or moderate ) deficit equal 5 -10% A-no dehydration
Assessing the child for other problems n n n Dysentry? Persistent diarrhea? Malnutrition? Feeding history? Pre-illness , feeding during diarrhea and mother, s beliefs Physical finding? Sings of marasmus or kwashiorkor?
Treatment plan a to treat dirrhea at home n Explain 3 rules for treating diarrhea at home: Give the child more fluid for prevent dehydration 2. Give the child plenty of food to prevent malnutrition 3. Take the child to the health worker if the child not get better in 3 days or develops any of the following: Fever , eating or drinking poorly , bloody stool , marked thirst , repeated vomiting , many watery stools 1.
Treatment plan a to treat dirrhea at home n n Give ORS at home if: they have been on treatment plan B or C They can not return to the health worker if the diarrhea worse It is national policy give ORS to all children
If the child will be given ORS at home n n n Age less than 24 months 50 -100 ml after each loose stool and 500 ml /day at home 2 -10 year 100 -200 ml after each loose stool and 1000 ml / day 10 years or more as much as wanted and 2000 ml/ day Give a teaspoon every 1 -2 minutes for under 2 year If a child vomits wait 10 minutes and then every 2 -3 minutes
Treatment plan B to treat dehydration n n n Estimate the amount of ORS solution to be given during the 4 hours To show the mother how to give ORS To continue breast- feeding To monitor treatment and reassess the child To identify patients who can not be treated satisfactory After rehydration following plan. A
Treatment plan B n n n Amount of ORS is 75 ml /kg in the 4 hours If the child wants more ORS give more The mother continue breast- feeding For infant < 6 month who are not breast – fed give 100 -200 ml water after 4 hours reassess the child then select plan A, B , C
Thanks… But it’s not the end !!





 Criminology etiology
Criminology etiology Models of etiology of addiction
Models of etiology of addiction Asthma grades
Asthma grades Pathology of asthma
Pathology of asthma Definition of acute appendicitis
Definition of acute appendicitis Difference between nursing bottle caries and rampant caries
Difference between nursing bottle caries and rampant caries What is a pes statement
What is a pes statement Etiology
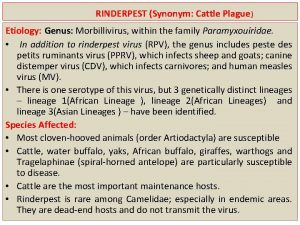
Etiology Etiology synonym
Etiology synonym Etiology
Etiology Periradicular disease
Periradicular disease Color of amniotic fluid
Color of amniotic fluid Tccdtccd
Tccdtccd Etiology synonym
Etiology synonym Site:slidetodoc.com
Site:slidetodoc.com Mantoux test positive 15mm
Mantoux test positive 15mm Difference between descriptive and analytical epidemiology
Difference between descriptive and analytical epidemiology Nutrition epidemiology definition
Nutrition epidemiology definition Difference between descriptive and analytical epidemiology
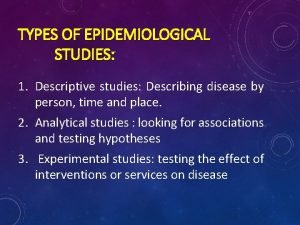
Difference between descriptive and analytical epidemiology Descriptive epidemiology
Descriptive epidemiology Certification board of infection control and epidemiology
Certification board of infection control and epidemiology Descriptive epidemiology
Descriptive epidemiology Perbedaan relative risk dan odds ratio
Perbedaan relative risk dan odds ratio Logistic regression epidemiology
Logistic regression epidemiology Formula for attack rate
Formula for attack rate Descriptive vs analytical epidemiology
Descriptive vs analytical epidemiology Attack rate epidemiology formula
Attack rate epidemiology formula Bibliography of epidemiology
Bibliography of epidemiology Temporal relationship epidemiology example
Temporal relationship epidemiology example Formula for attack rate
Formula for attack rate Ramboman
Ramboman Wheel model of disease causation example
Wheel model of disease causation example Defination of incidence
Defination of incidence Defination of epidemiology
Defination of epidemiology Concept of epidemiology
Concept of epidemiology What is descriptive study in epidemiology
What is descriptive study in epidemiology Spurious association
Spurious association Field epidemiology ppt
Field epidemiology ppt Aims of epidemiology
Aims of epidemiology Gordon nichols
Gordon nichols Epidemiology kept simple
Epidemiology kept simple Diabetic ketoacidosis epidemiology
Diabetic ketoacidosis epidemiology Distribution in epidemiology
Distribution in epidemiology Effect modification vs confounding
Effect modification vs confounding Distribution in epidemiology
Distribution in epidemiology Ramboman analysis
Ramboman analysis Meaning of epidermiology
Meaning of epidermiology Period prevalence formula
Period prevalence formula How dr. wafaa elsadr epidemiology professor
How dr. wafaa elsadr epidemiology professor Nutritional epidemiology
Nutritional epidemiology Malaria parasites under microscope
Malaria parasites under microscope Secondary attack rate formula
Secondary attack rate formula How dr. wafaa elsadr epidemiology professor
How dr. wafaa elsadr epidemiology professor Epidemiology definition
Epidemiology definition Seven uses of epidemiology
Seven uses of epidemiology Epidemiological triad
Epidemiological triad Celiac beri beri
Celiac beri beri Orlies
Orlies Nicholas seeliger, md flpen panama city beach
Nicholas seeliger, md flpen panama city beach Diarrhea plan a
Diarrhea plan a Reflexology tips
Reflexology tips Causes of secretory diarrhea
Causes of secretory diarrhea Bile acid diarrhea
Bile acid diarrhea Types of diarrhoea
Types of diarrhoea Plan b of dehydration management
Plan b of dehydration management History taking of diarrhea
History taking of diarrhea Diarrhea in children
Diarrhea in children Osmotic diarrhea meaning
Osmotic diarrhea meaning Causes of secretory diarrhea
Causes of secretory diarrhea