Asthma Definition Pathophysiology Pathogenesis 1 Asthma is a


- Slides: 41
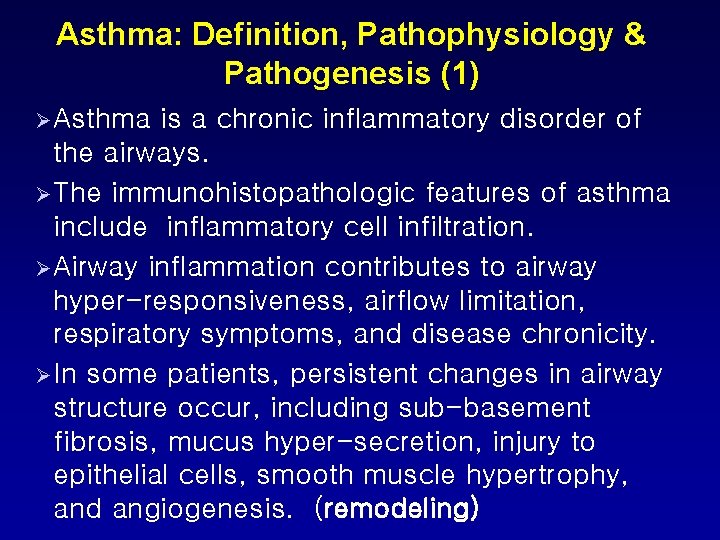
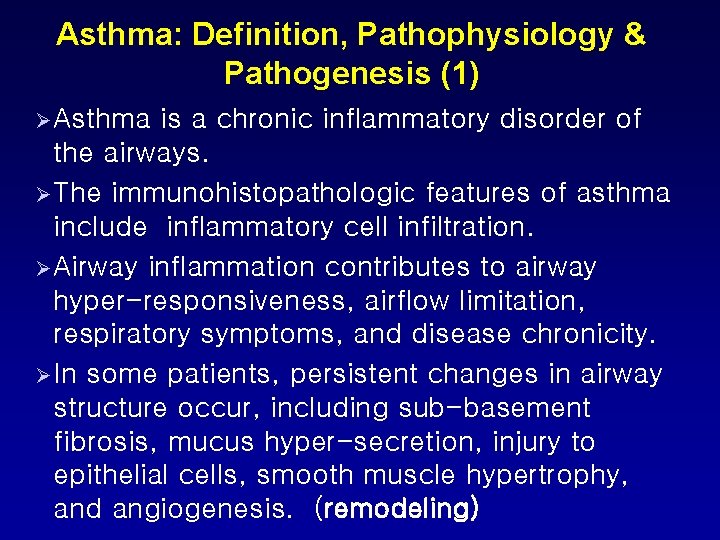
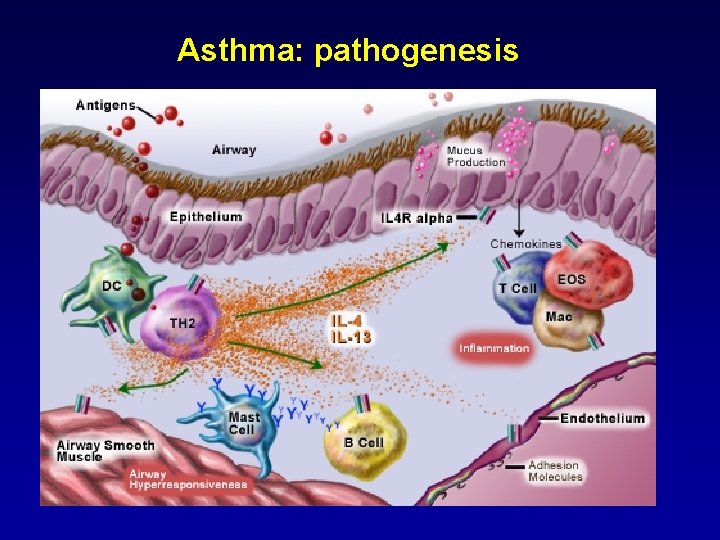
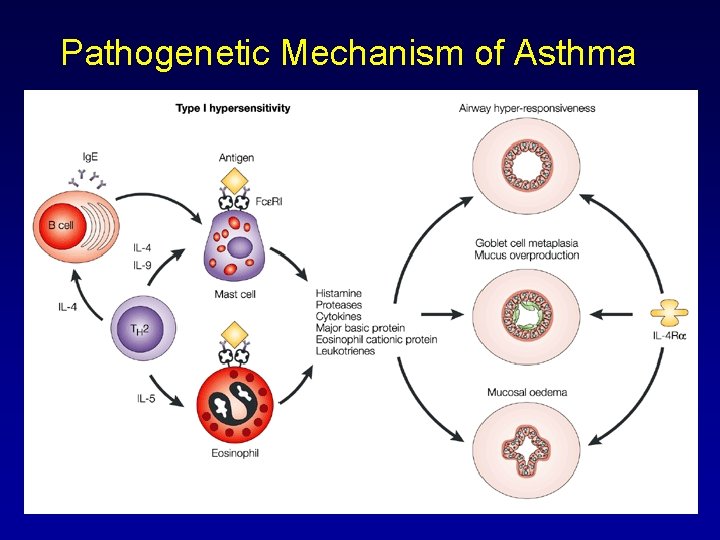
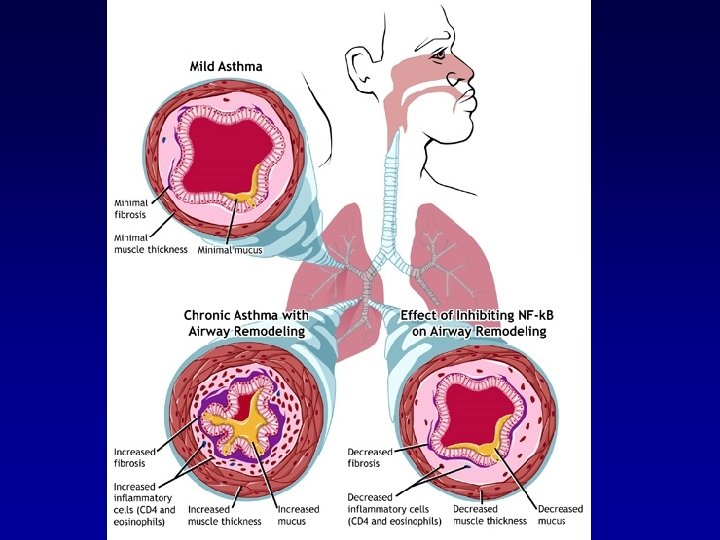
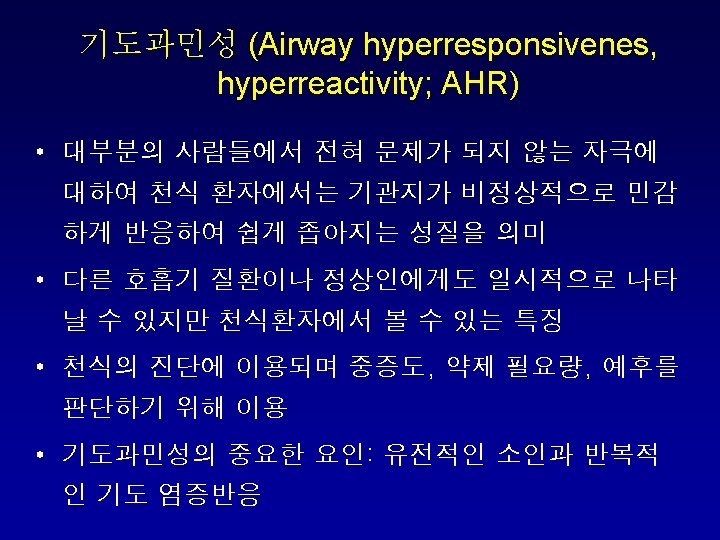
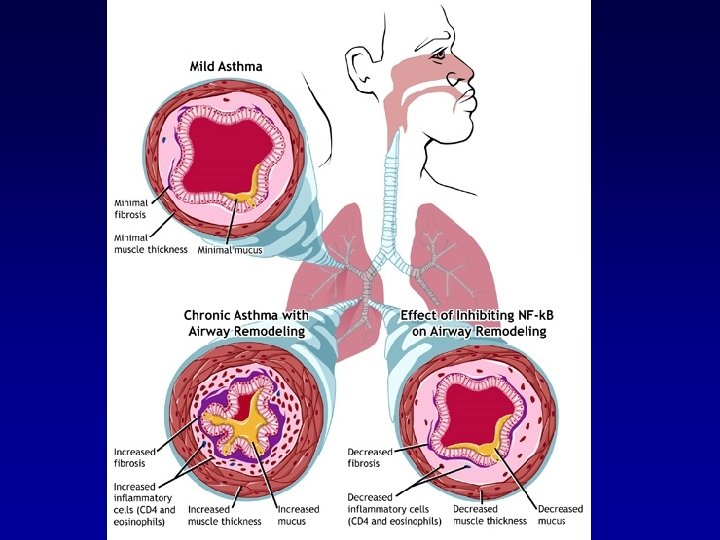
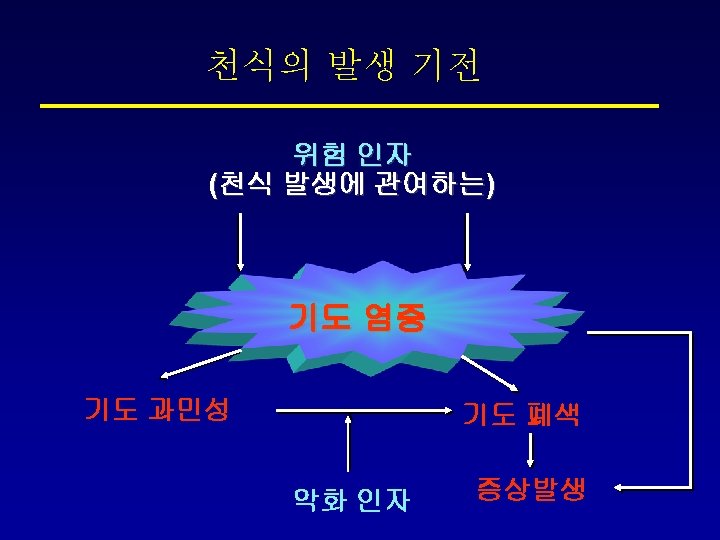
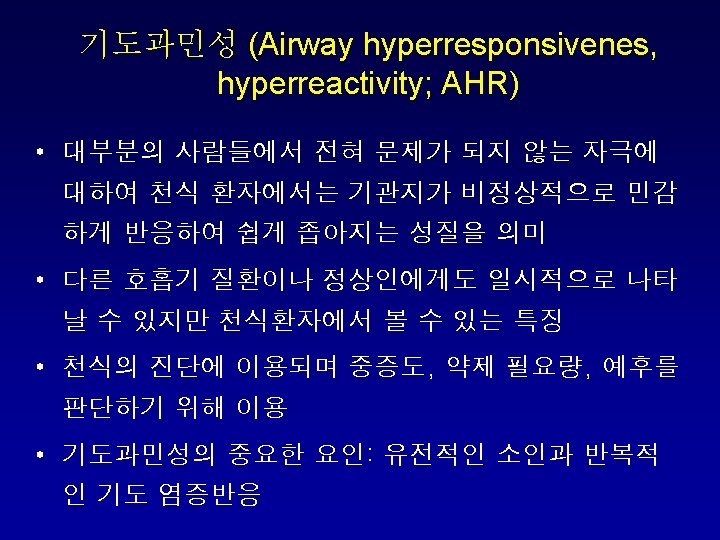
Asthma: Definition, Pathophysiology & Pathogenesis (1) Ø Asthma is a chronic inflammatory disorder of the airways. Ø The immunohistopathologic features of asthma include inflammatory cell infiltration. Ø Airway inflammation contributes to airway hyper-responsiveness, airflow limitation, respiratory symptoms, and disease chronicity. Ø In some patients, persistent changes in airway structure occur, including sub-basement fibrosis, mucus hyper-secretion, injury to epithelial cells, smooth muscle hypertrophy, and angiogenesis. (remodeling)
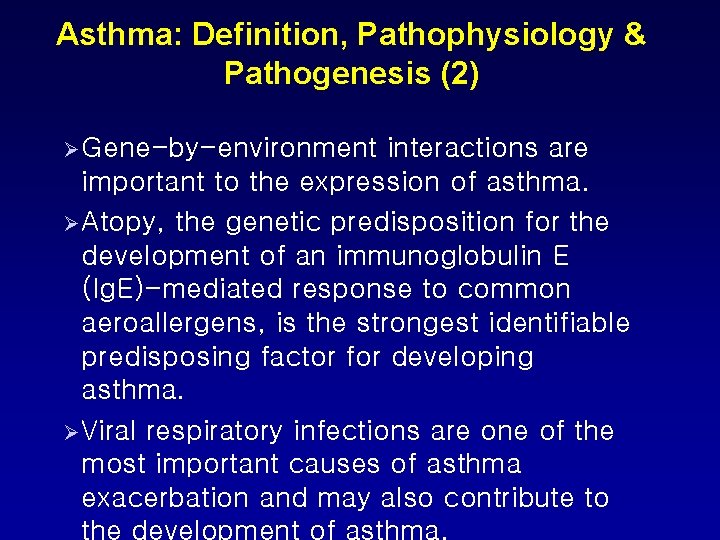
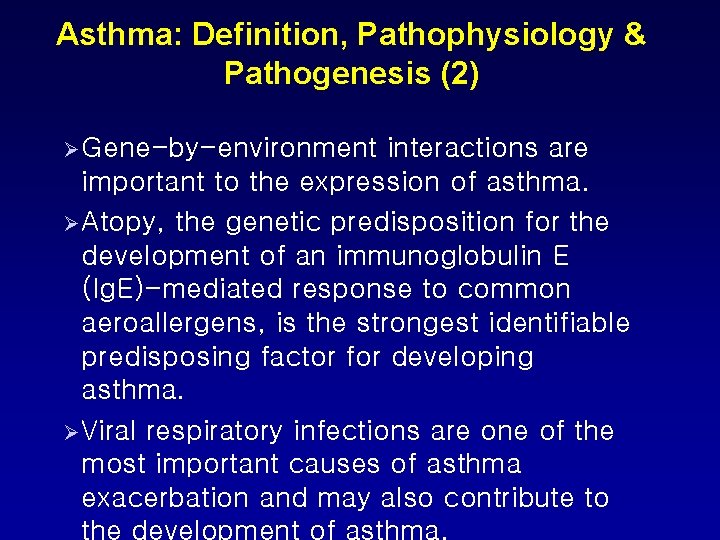
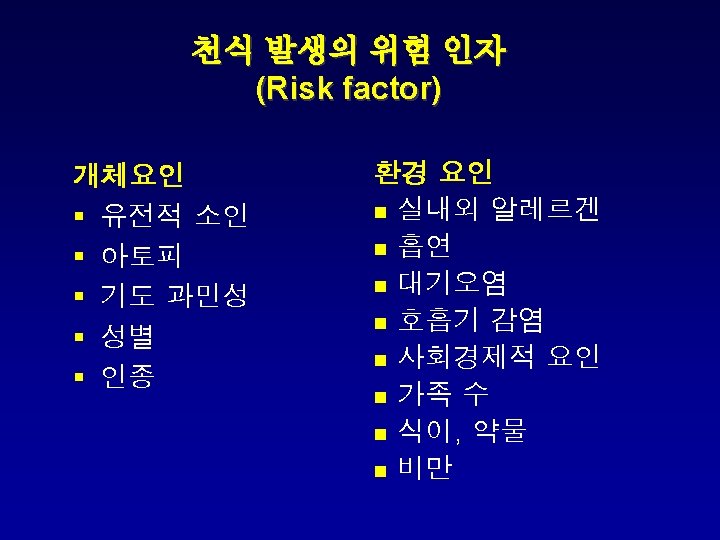
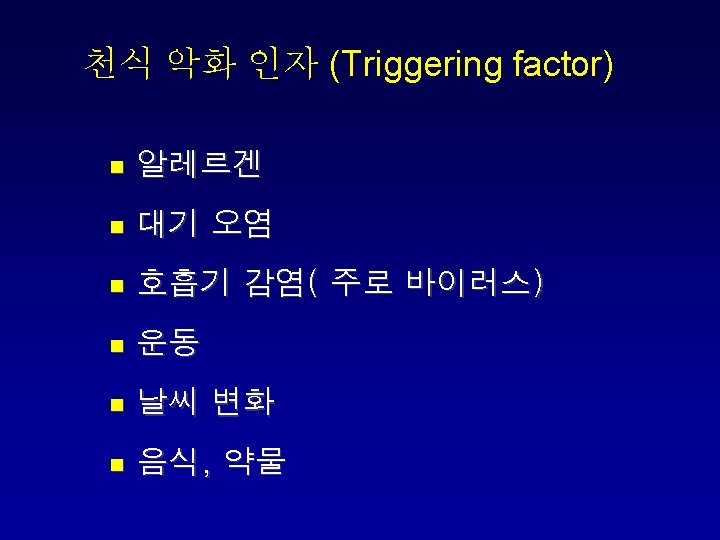
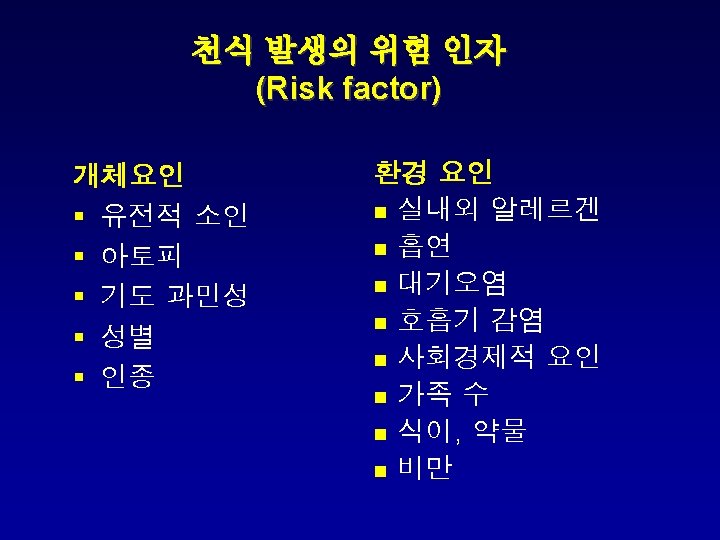
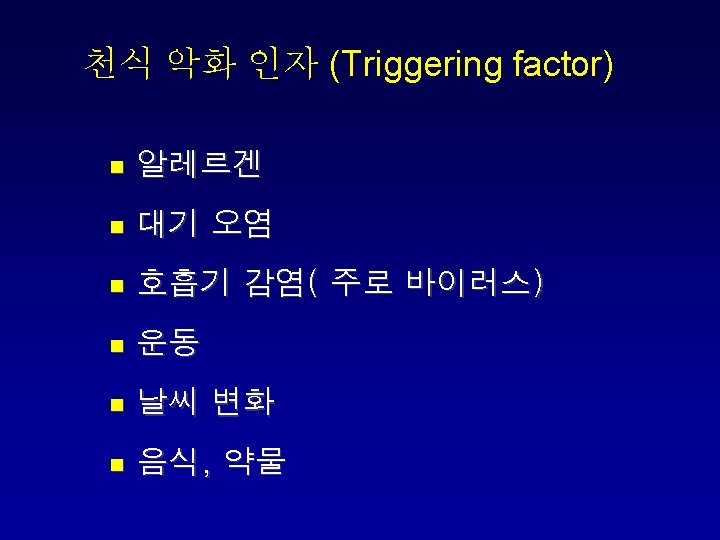
Asthma: Definition, Pathophysiology & Pathogenesis (2) Ø Gene-by-environment interactions are important to the expression of asthma. Ø Atopy, the genetic predisposition for the development of an immunoglobulin E (Ig. E)-mediated response to common aeroallergens, is the strongest identifiable predisposing factor for developing asthma. Ø Viral respiratory infections are one of the most important causes of asthma exacerbation and may also contribute to
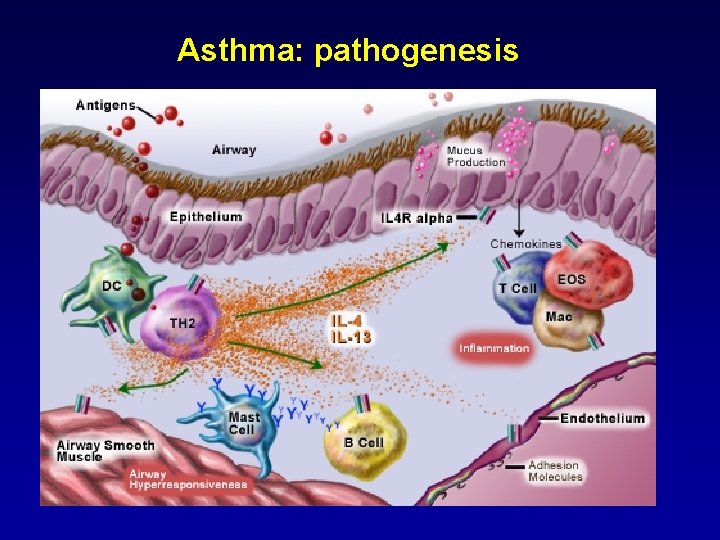
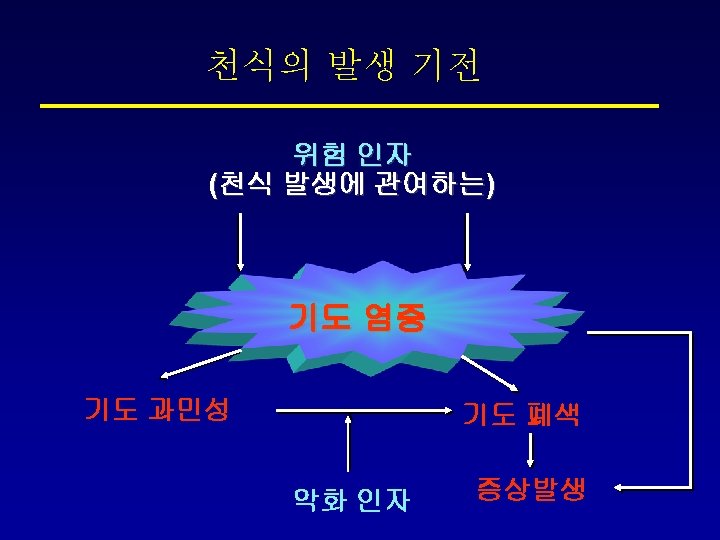
Asthma: pathogenesis
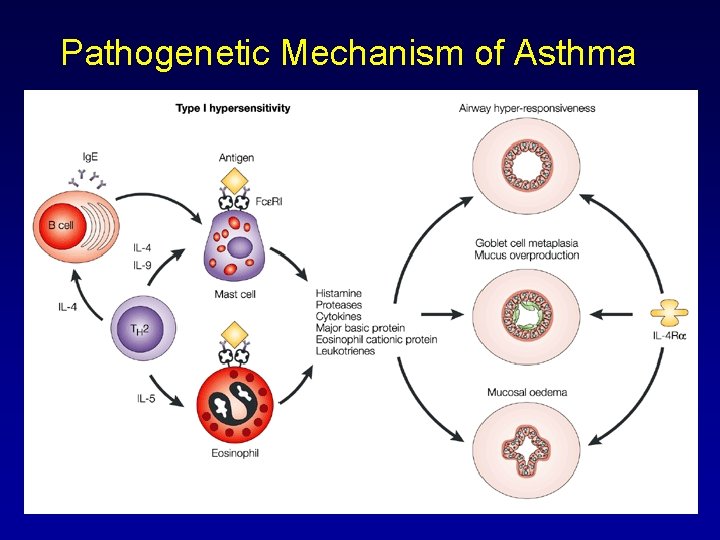
Pathogenetic Mechanism of Asthma
Diagnosis of Asthma
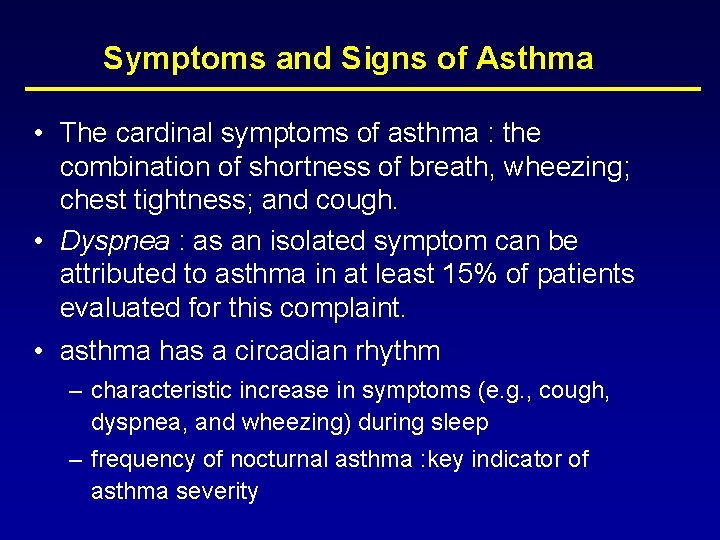
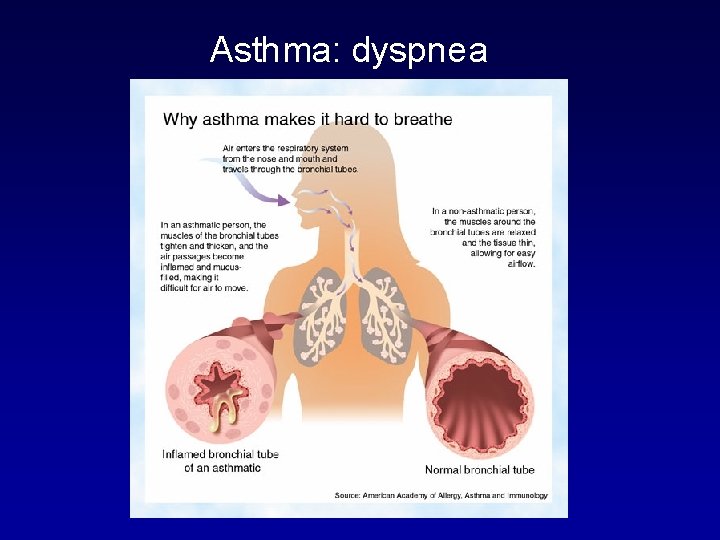
Symptoms and Signs of Asthma • The cardinal symptoms of asthma : the combination of shortness of breath, wheezing; chest tightness; and cough. • Dyspnea : as an isolated symptom can be attributed to asthma in at least 15% of patients evaluated for this complaint. • asthma has a circadian rhythm – characteristic increase in symptoms (e. g. , cough, dyspnea, and wheezing) during sleep – frequency of nocturnal asthma : key indicator of asthma severity
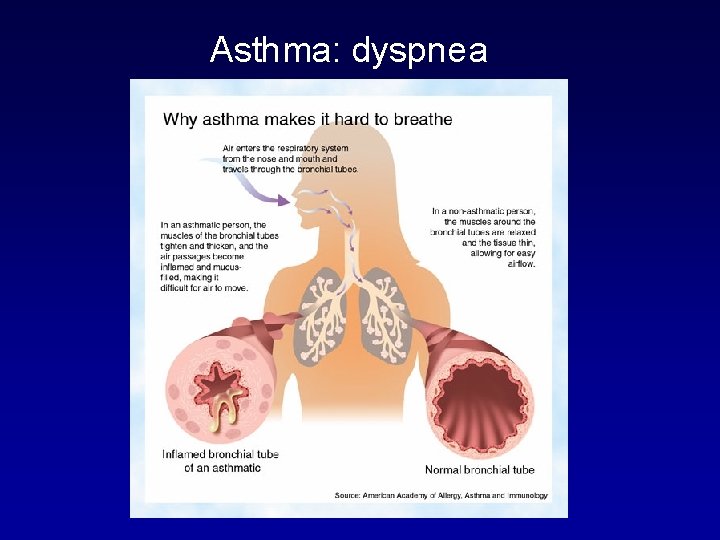
Asthma: dyspnea
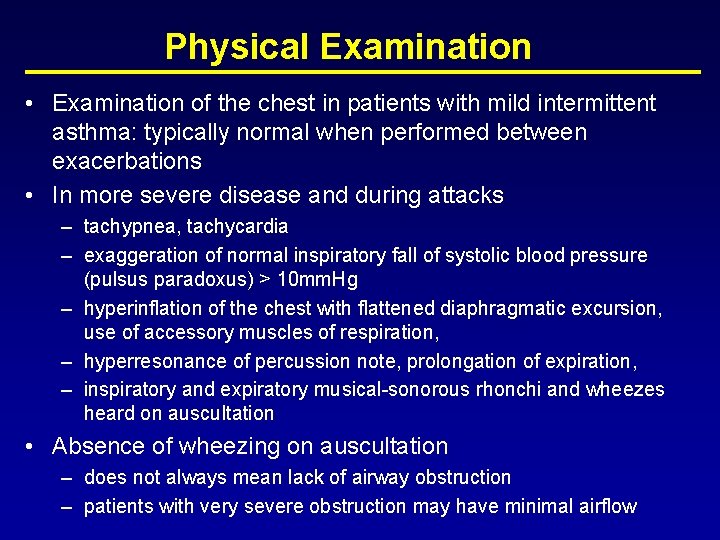
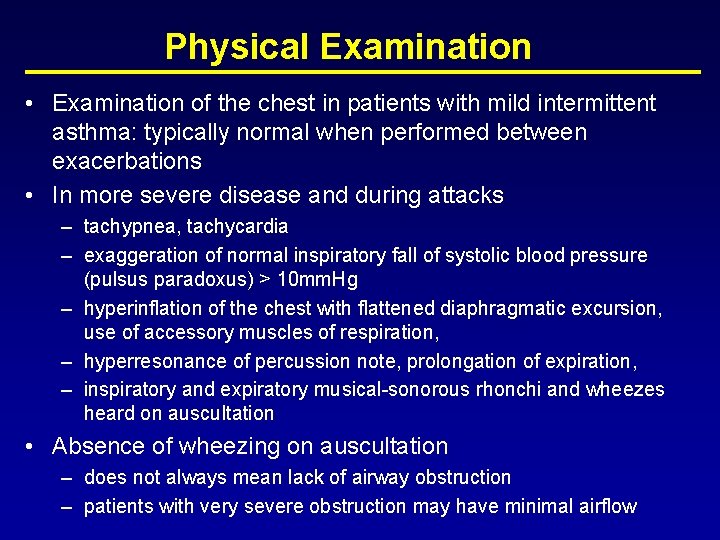
Physical Examination • Examination of the chest in patients with mild intermittent asthma: typically normal when performed between exacerbations • In more severe disease and during attacks – tachypnea, tachycardia – exaggeration of normal inspiratory fall of systolic blood pressure (pulsus paradoxus) > 10 mm. Hg – hyperinflation of the chest with flattened diaphragmatic excursion, use of accessory muscles of respiration, – hyperresonance of percussion note, prolongation of expiration, – inspiratory and expiratory musical-sonorous rhonchi and wheezes heard on auscultation • Absence of wheezing on auscultation – does not always mean lack of airway obstruction – patients with very severe obstruction may have minimal airflow
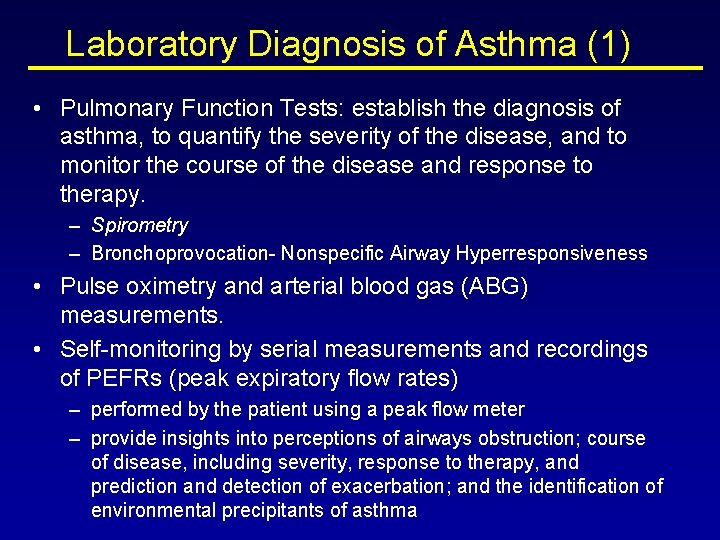
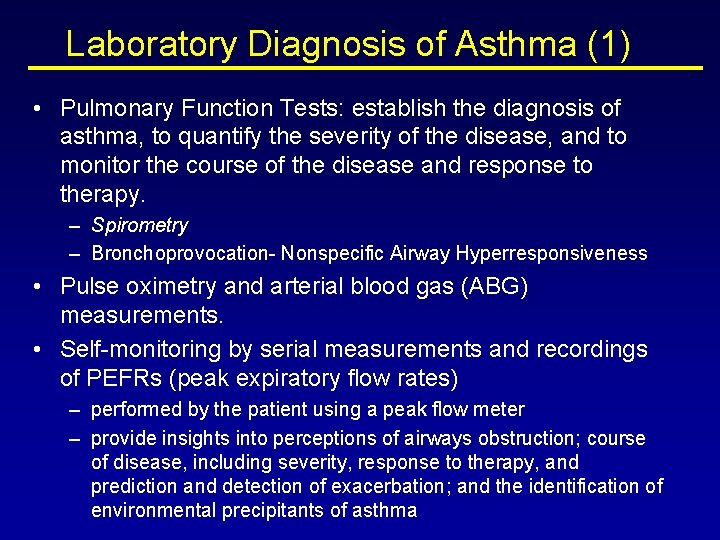
Laboratory Diagnosis of Asthma (1) • Pulmonary Function Tests: establish the diagnosis of asthma, to quantify the severity of the disease, and to monitor the course of the disease and response to therapy. – Spirometry – Bronchoprovocation- Nonspecific Airway Hyperresponsiveness • Pulse oximetry and arterial blood gas (ABG) measurements. • Self-monitoring by serial measurements and recordings of PEFRs (peak expiratory flow rates) – performed by the patient using a peak flow meter – provide insights into perceptions of airways obstruction; course of disease, including severity, response to therapy, and prediction and detection of exacerbation; and the identification of environmental precipitants of asthma
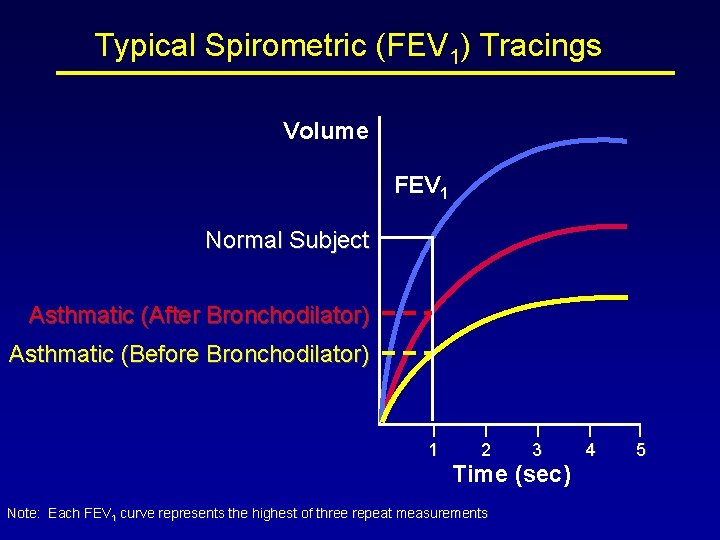
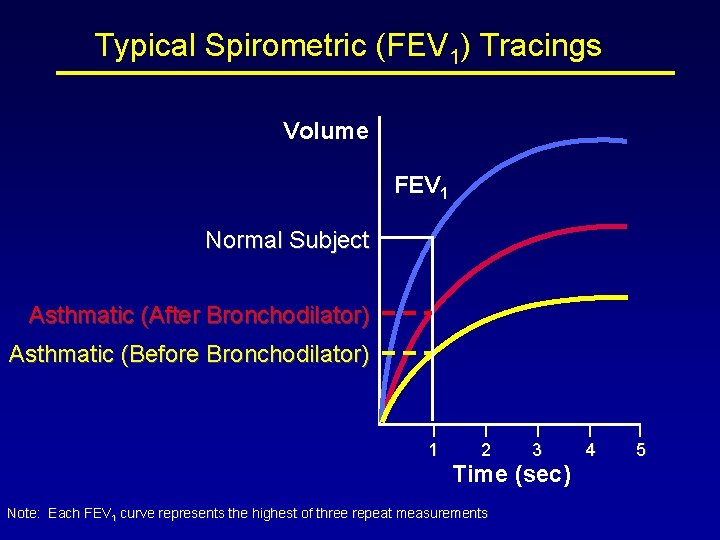
Typical Spirometric (FEV 1) Tracings Volume FEV 1 Normal Subject Asthmatic (After Bronchodilator) Asthmatic (Before Bronchodilator) 1 2 3 Time (sec) Note: Each FEV 1 curve represents the highest of three repeat measurements 4 5
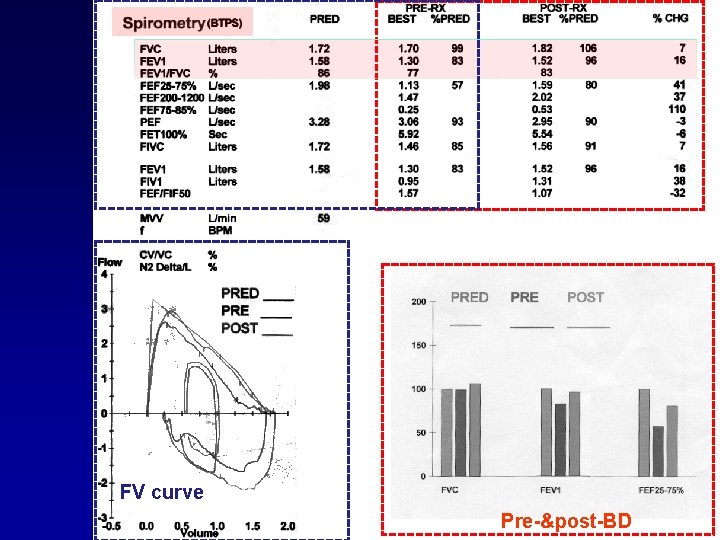
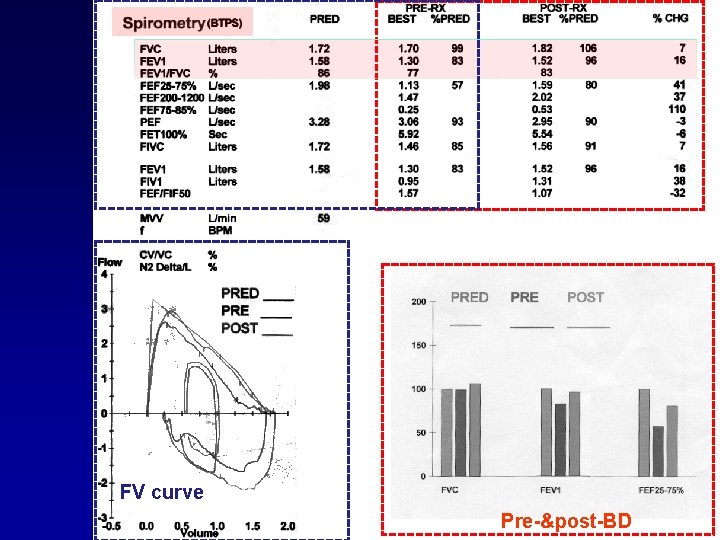
FV curve Pre-&post-BD
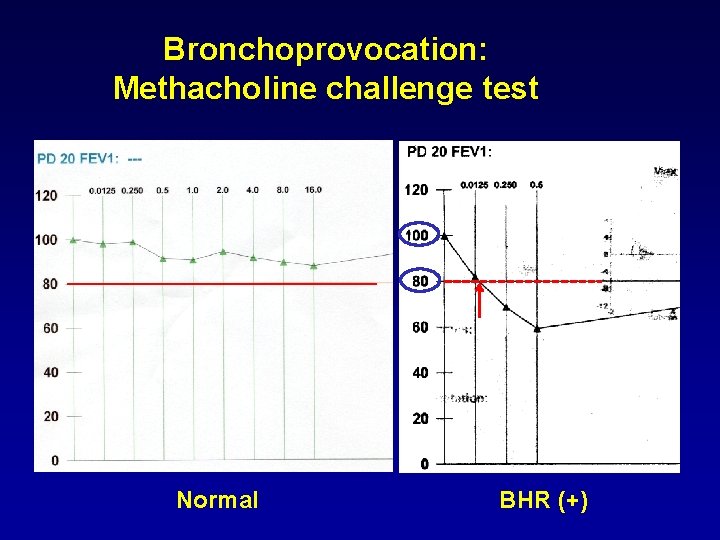
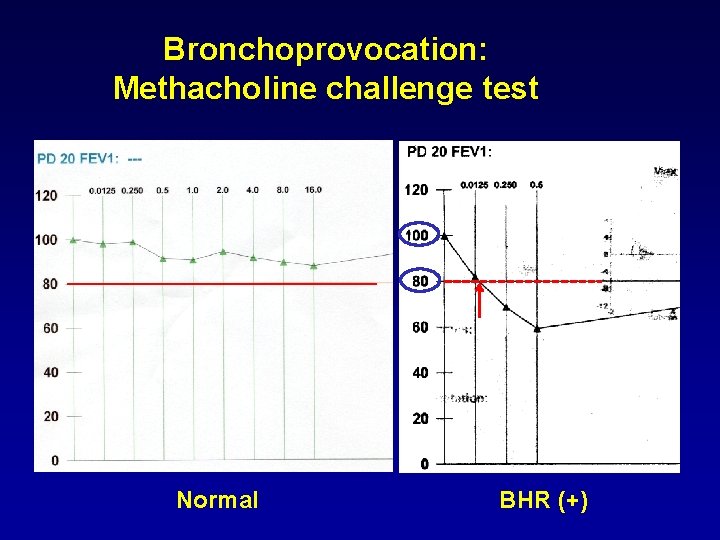
Bronchoprovocation: Methacholine challenge test Normal BHR (+)
Mini-Wright Peak Flow Meter
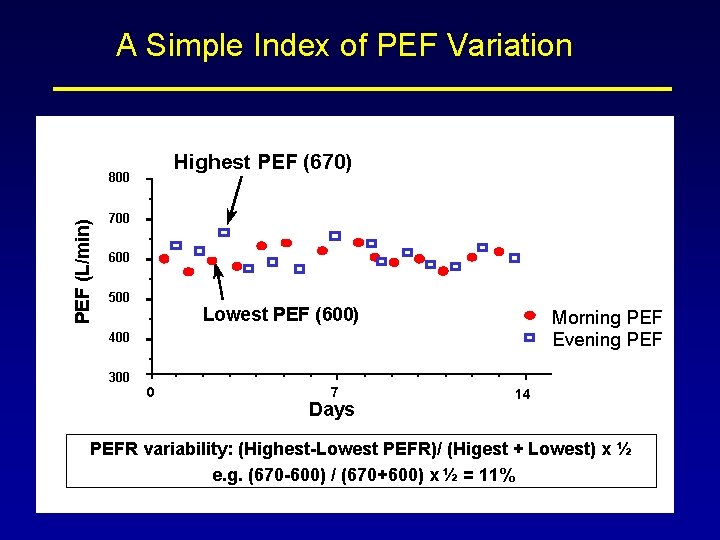
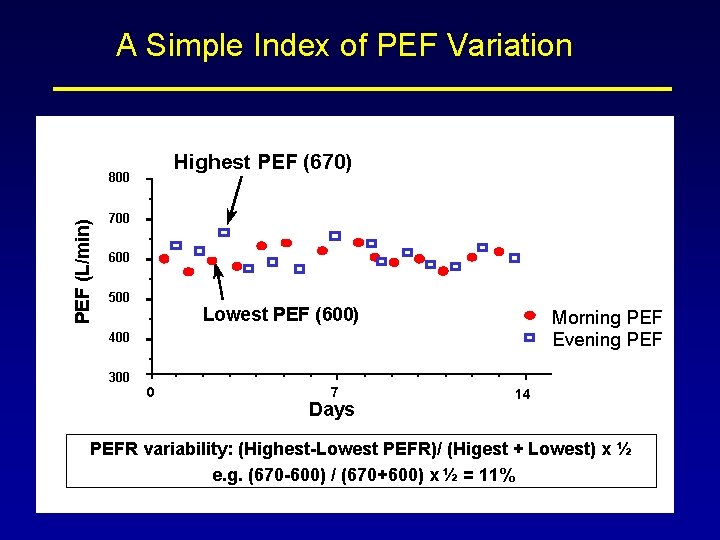
A Simple Index of PEF Variation Highest PEF (670) PEF (L/min) 800 700 600 500 Lowest PEF (600) Morning PEF Evening PEF 400 300 0 7 Days 14 PEFR variability: (Highest-Lowest PEFR)/ (Higest + Lowest) x ½ e. g. (670 -600) / (670+600) x ½ = 11%
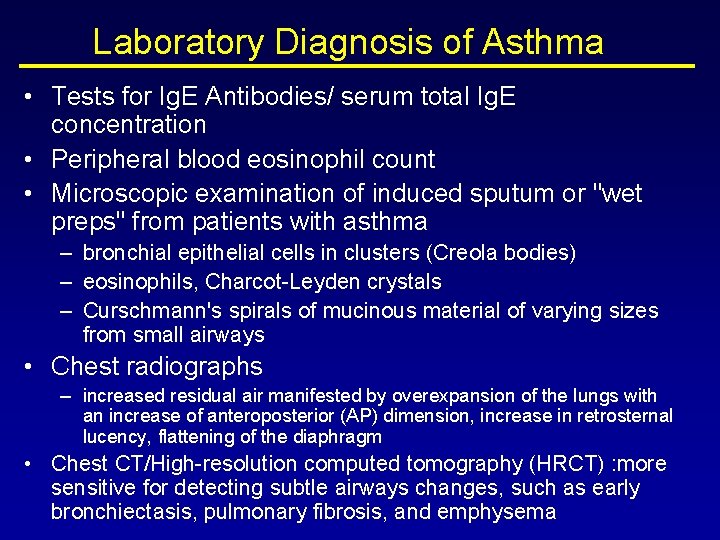
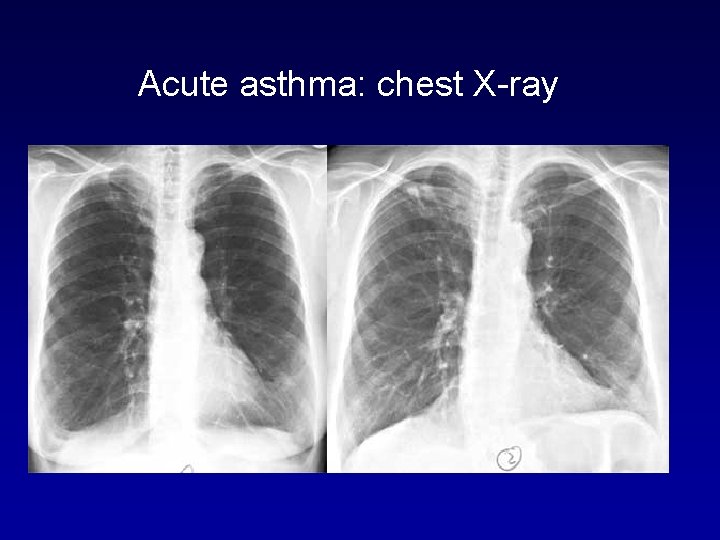
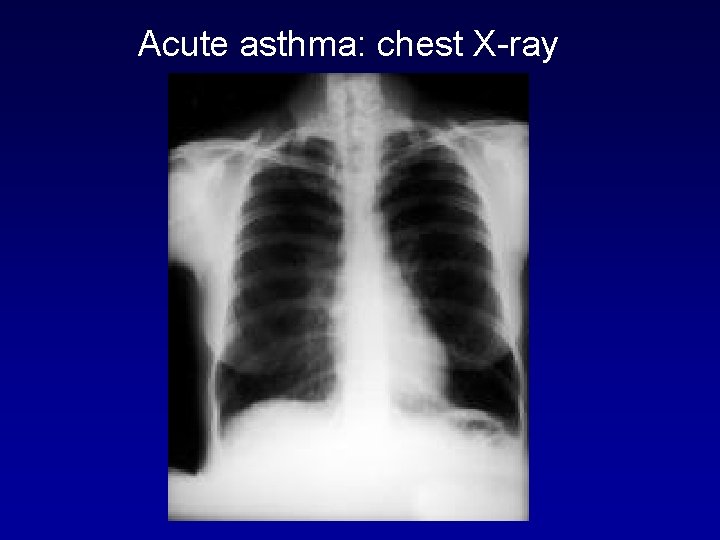
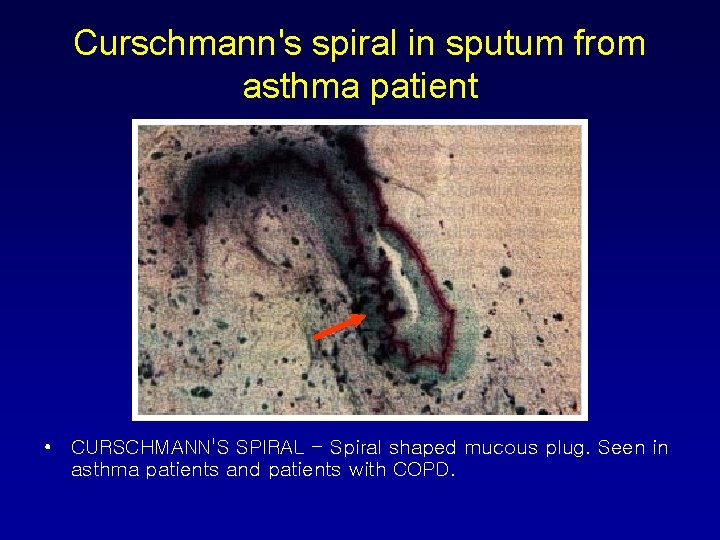
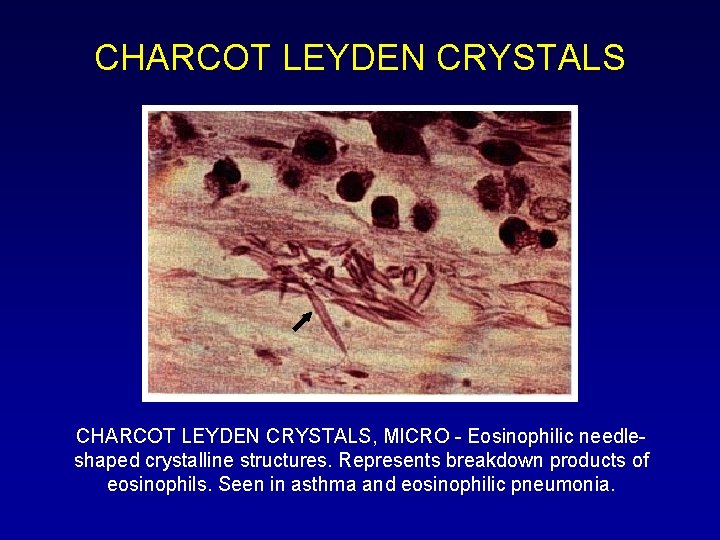
Laboratory Diagnosis of Asthma • Tests for Ig. E Antibodies/ serum total Ig. E concentration • Peripheral blood eosinophil count • Microscopic examination of induced sputum or "wet preps" from patients with asthma – bronchial epithelial cells in clusters (Creola bodies) – eosinophils, Charcot-Leyden crystals – Curschmann's spirals of mucinous material of varying sizes from small airways • Chest radiographs – increased residual air manifested by overexpansion of the lungs with an increase of anteroposterior (AP) dimension, increase in retrosternal lucency, flattening of the diaphragm • Chest CT/High-resolution computed tomography (HRCT) : more sensitive for detecting subtle airways changes, such as early bronchiectasis, pulmonary fibrosis, and emphysema
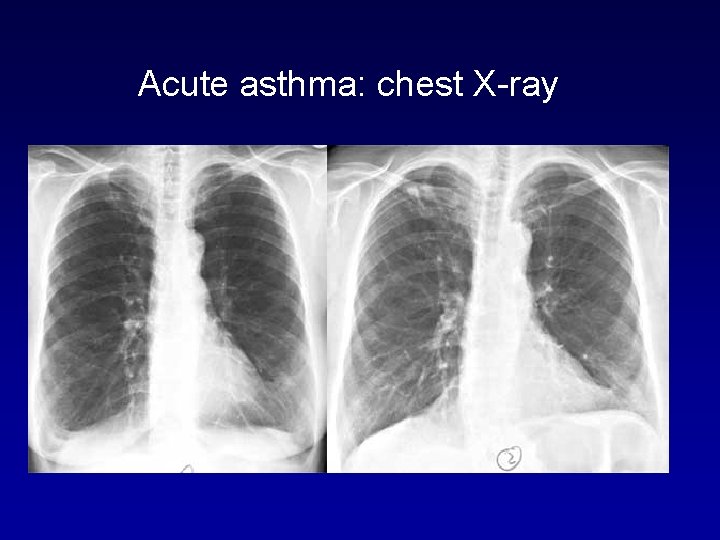
Acute asthma: chest X-ray
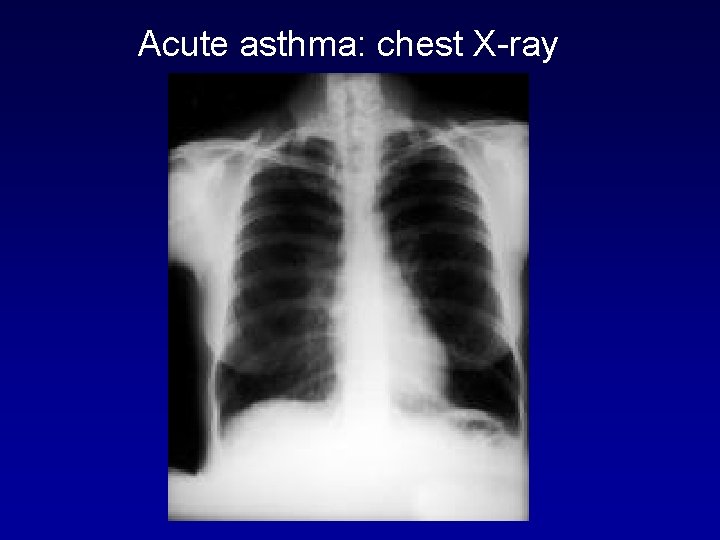
Acute asthma: chest X-ray
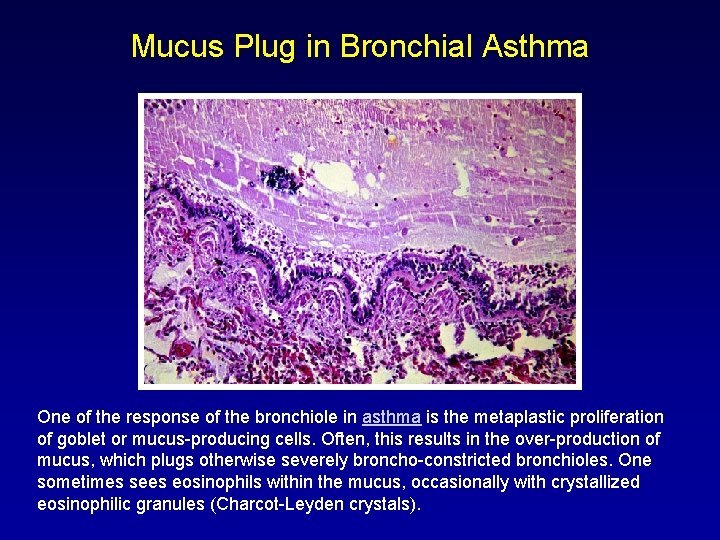
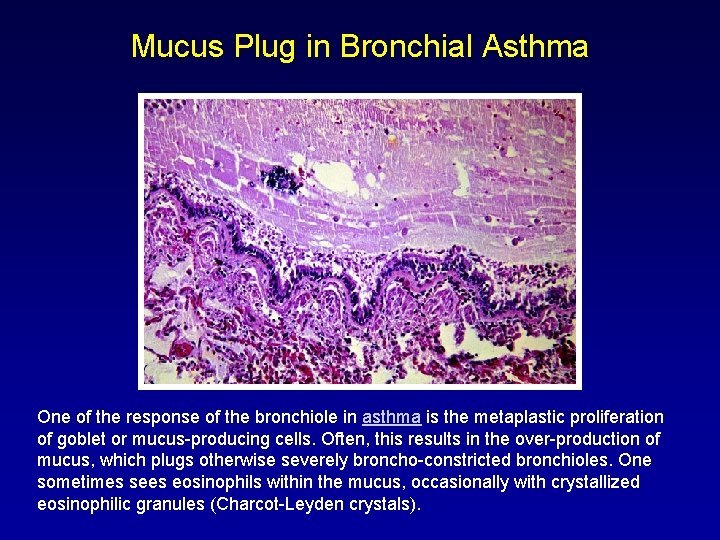
Mucus Plug in Bronchial Asthma One of the response of the bronchiole in asthma is the metaplastic proliferation of goblet or mucus-producing cells. Often, this results in the over-production of mucus, which plugs otherwise severely broncho-constricted bronchioles. One sometimes sees eosinophils within the mucus, occasionally with crystallized eosinophilic granules (Charcot-Leyden crystals).
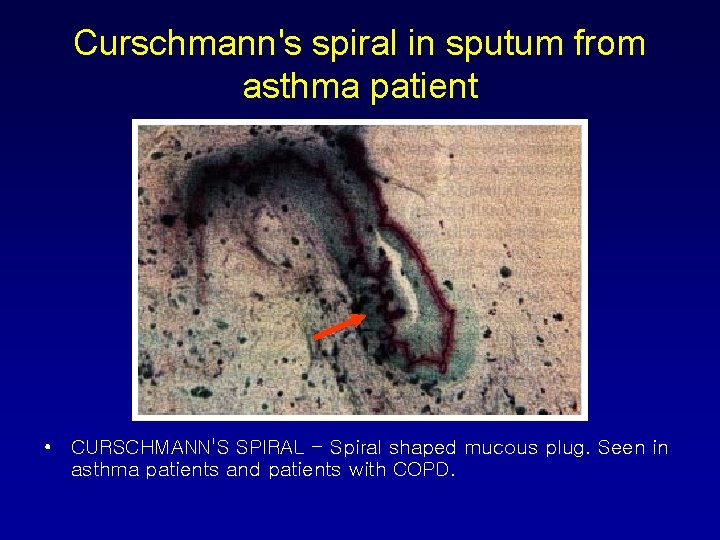
Curschmann's spiral in sputum from asthma patient • CURSCHMANN'S SPIRAL - Spiral shaped mucous plug. Seen in asthma patients and patients with COPD.
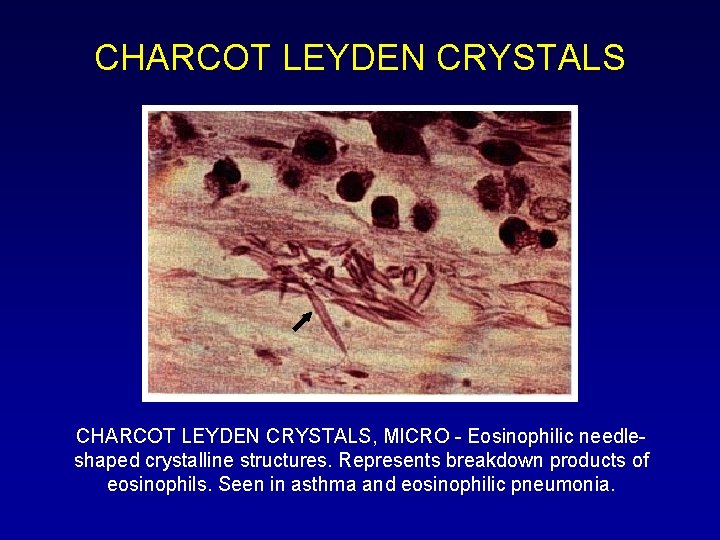
CHARCOT LEYDEN CRYSTALS, MICRO - Eosinophilic needleshaped crystalline structures. Represents breakdown products of eosinophils. Seen in asthma and eosinophilic pneumonia.
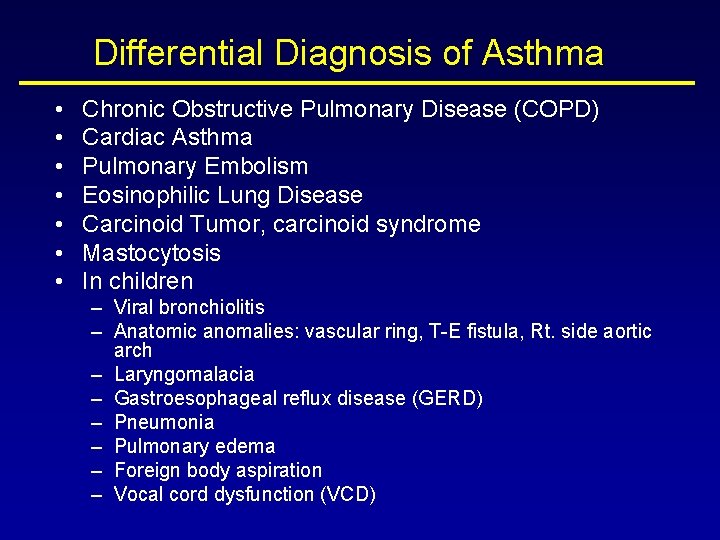
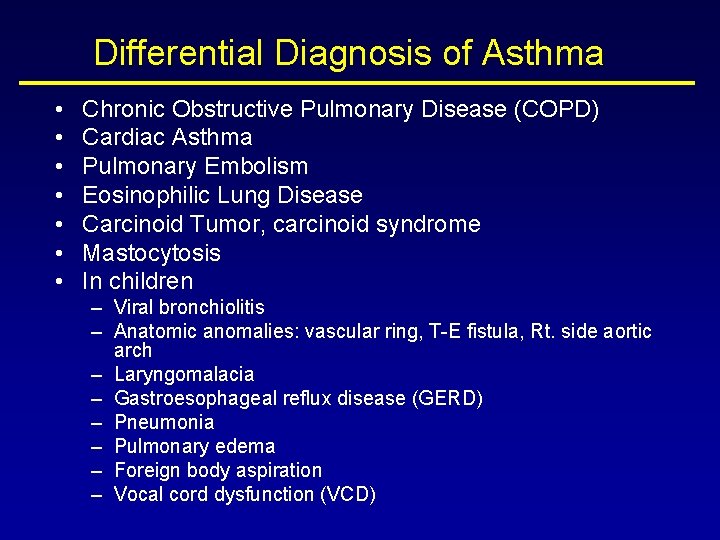
Differential Diagnosis of Asthma • • Chronic Obstructive Pulmonary Disease (COPD) Cardiac Asthma Pulmonary Embolism Eosinophilic Lung Disease Carcinoid Tumor, carcinoid syndrome Mastocytosis In children – Viral bronchiolitis – Anatomic anomalies: vascular ring, T-E fistula, Rt. side aortic arch – Laryngomalacia – Gastroesophageal reflux disease (GERD) – Pneumonia – Pulmonary edema – Foreign body aspiration – Vocal cord dysfunction (VCD)

Treatment of Asthma
2007 - Guidelines For The Diagnosis & Management Of Asthma Expert Review Panel (EPR-3)
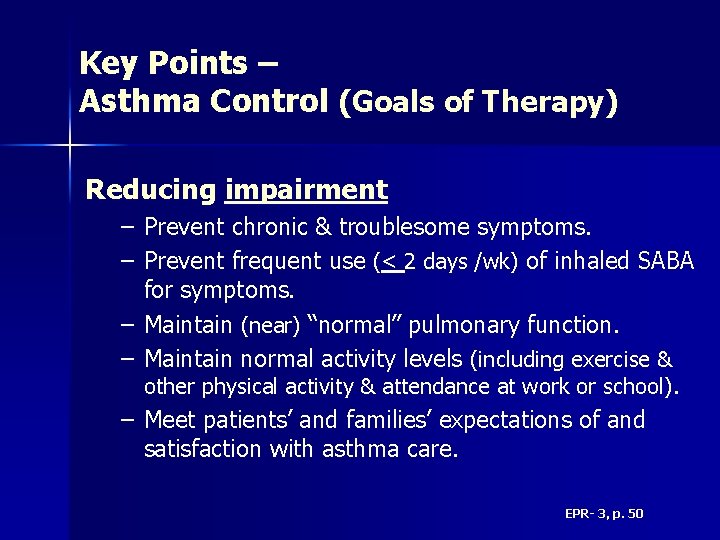
Key Points – Asthma Control (Goals of Therapy) Reducing impairment – Prevent chronic & troublesome symptoms. – Prevent frequent use (< 2 days /wk) of inhaled SABA for symptoms. – Maintain (near) “normal” pulmonary function. – Maintain normal activity levels (including exercise & other physical activity & attendance at work or school). – Meet patients’ and families’ expectations of and satisfaction with asthma care. EPR- 3, p. 50
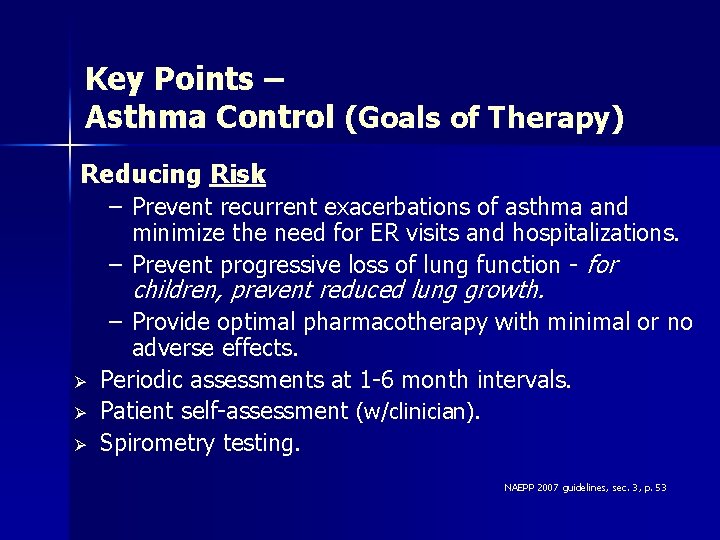
Key Points – Asthma Control (Goals of Therapy) Reducing Risk – Prevent recurrent exacerbations of asthma and minimize the need for ER visits and hospitalizations. – Prevent progressive loss of lung function - for children, prevent reduced lung growth. Ø Ø Ø – Provide optimal pharmacotherapy with minimal or no adverse effects. Periodic assessments at 1 -6 month intervals. Patient self-assessment (w/clinician). Spirometry testing. NAEPP 2007 guidelines, sec. 3, p. 53
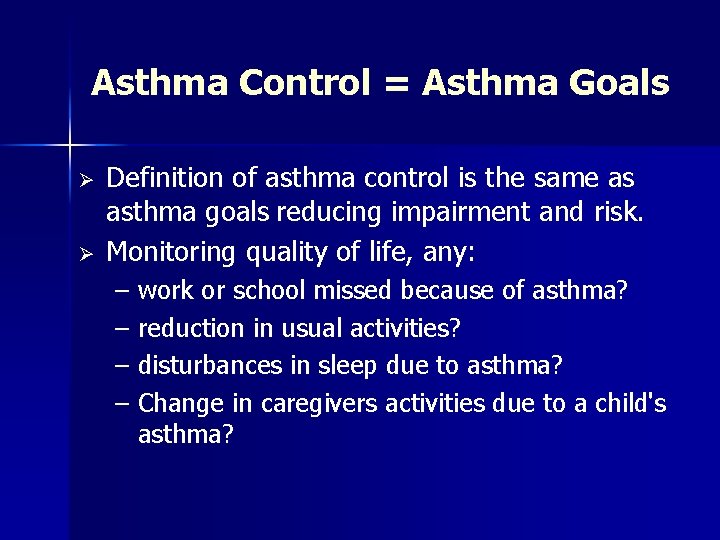
Asthma Control = Asthma Goals Ø Ø Definition of asthma control is the same as asthma goals reducing impairment and risk. Monitoring quality of life, any: – work or school missed because of asthma? – reduction in usual activities? – disturbances in sleep due to asthma? – Change in caregivers activities due to a child's asthma?
Assessing Asthma Control In Youths 12 Years of Age & Adults

NOT Currently Taking Controllers
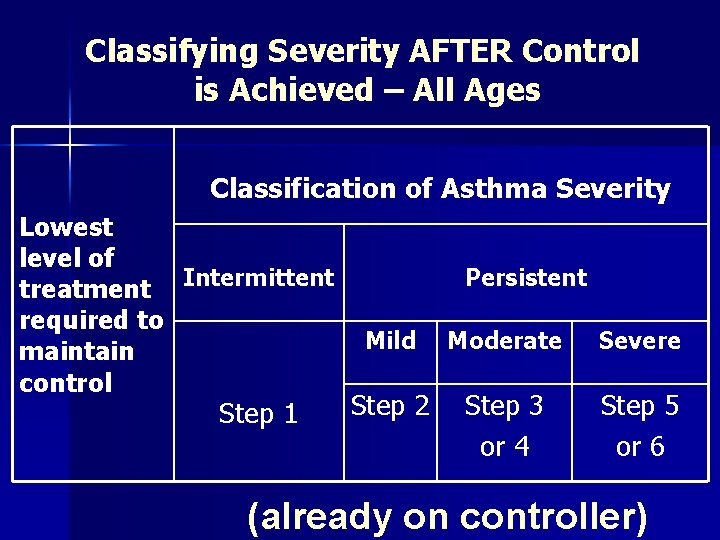
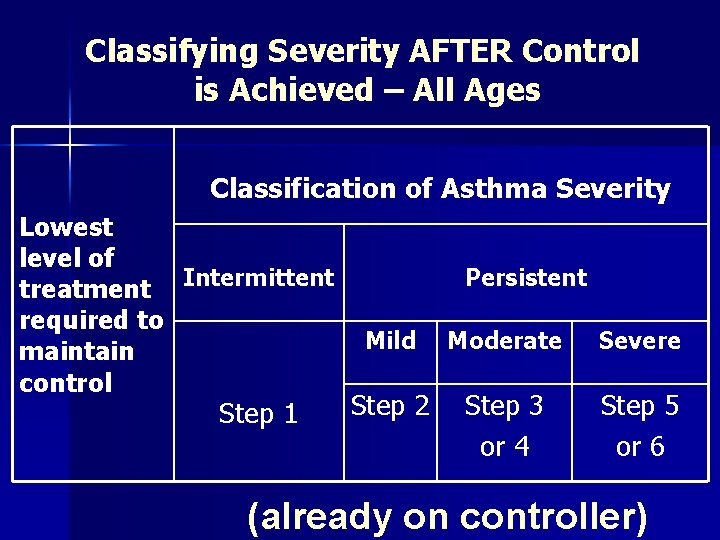
Classifying Severity AFTER Control is Achieved – All Ages Classification of Asthma Severity Lowest level of treatment Intermittent required to maintain control Step 1 Persistent Mild Moderate Severe Step 2 Step 3 or 4 Step 5 or 6 (already on controller)
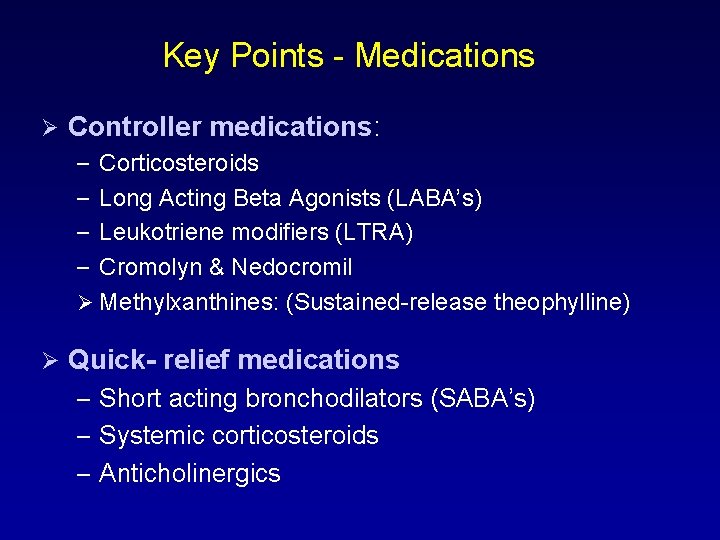
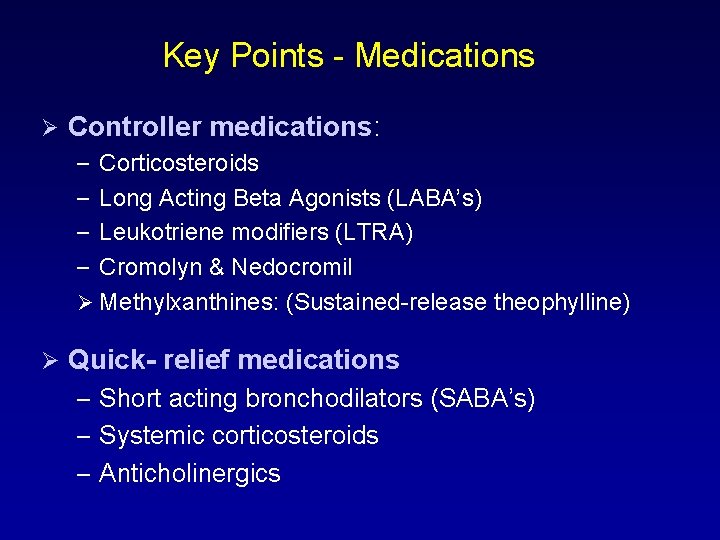
Key Points - Medications Ø Controller medications: – Corticosteroids – Long Acting Beta Agonists (LABA’s) – Leukotriene modifiers (LTRA) – Cromolyn & Nedocromil Ø Methylxanthines: (Sustained-release theophylline) Ø Quick- relief medications – Short acting bronchodilators (SABA’s) – Systemic corticosteroids – Anticholinergics
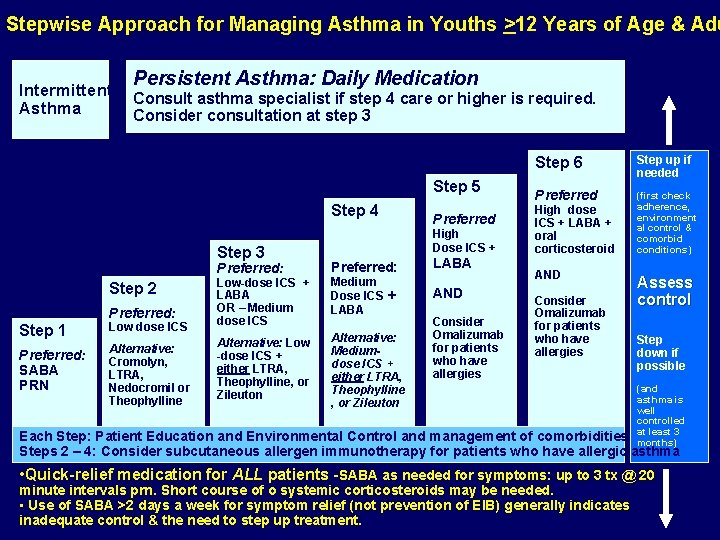
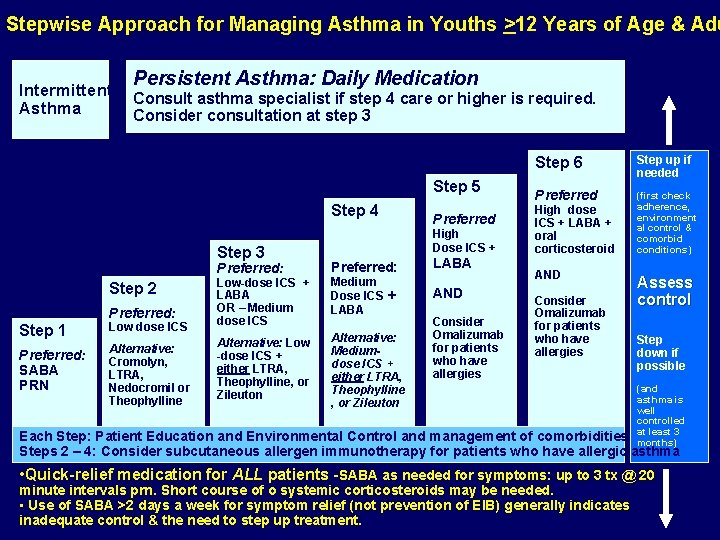
Stepwise Approach for Managing Asthma in Youths >12 Years of Age & Adu Intermittent Asthma Persistent Asthma: Daily Medication Consult asthma specialist if step 4 care or higher is required. Consider consultation at step 3 Step 5 Step 4 Step 3 Preferred: Step 1 Low dose ICS Low-dose ICS + LABA OR – Medium dose ICS Preferred: SABA PRN Alternative: Cromolyn, LTRA, Nedocromil or Theophylline Alternative: Low -dose ICS + either LTRA, Theophylline, or Zileuton Step 2 Preferred: Preferred High Dose ICS + Preferred: Medium Dose ICS + LABA Alternative: Mediumdose ICS + either LTRA, Theophylline , or Zileuton LABA AND Consider Omalizumab for patients who have allergies Step 6 Step up if needed Preferred (first check adherence, environment al control & comorbid conditions) High dose ICS + LABA + oral corticosteroid AND Consider Omalizumab for patients who have allergies Assess control Step down if possible (and asthma is well controlled at least 3 months) Each Step: Patient Education and Environmental Control and management of comorbidities Steps 2 – 4: Consider subcutaneous allergen immunotherapy for patients who have allergic asthma • Quick-relief medication for ALL patients -SABA as needed for symptoms: up to 3 tx @ 20 minute intervals prn. Short course of o systemic corticosteroids may be needed. • Use of SABA >2 days a week for symptom relief (not prevention of EIB) generally indicates inadequate control & the need to step up treatment.