ASTHMA Definition of asthma 2 Definition The guidelines

























- Slides: 119

ASTHMA

Definition of asthma 2

Definition The guidelines define asthma as: a chronic inflammatory disease of the airways many cells play a role (mast cells, eosinophils, and T lymphocytes)
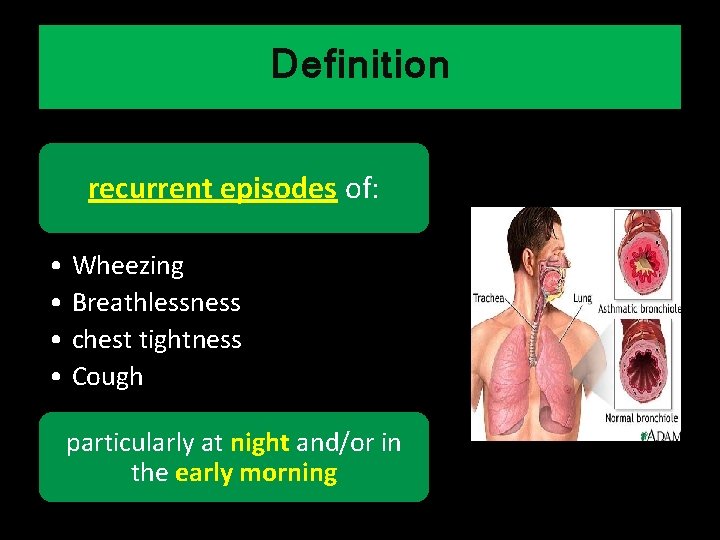
Definition recurrent episodes of: • Wheezing • Breathlessness • chest tightness • Cough particularly at night and/or in the early morning
Definition widespread but variable airflow limitation at least partially reversible either spontaneously or with treatment
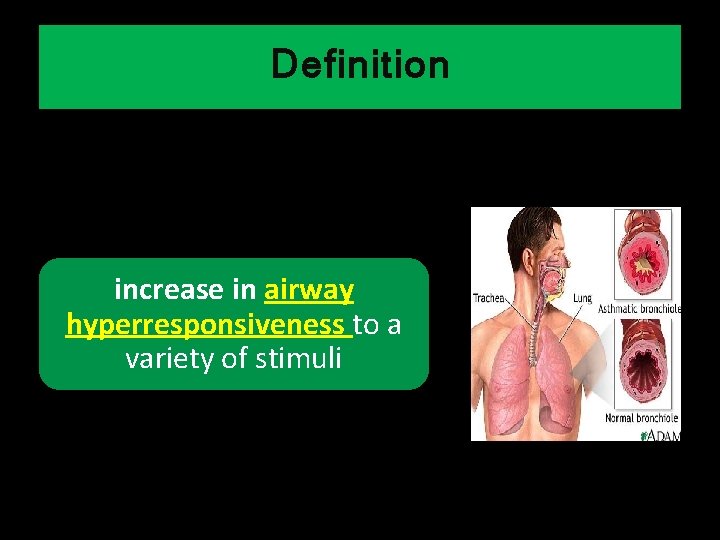
Definition increase in airway hyperresponsiveness to a variety of stimuli

Definition • Chronic Inflammation • Bronchial Hyperresponsivenes s • Reversible Airway Obstruction
Pathophysiologic Mechanism 8
Pathophysiologic Mechanism • Asthma is caused by a complex interaction of: – cells – Mediators and cytokines • that results in inflammation
Pathophysiologic Mechanism Inflammatory cells mediators Effects pathophysiolo gic changes
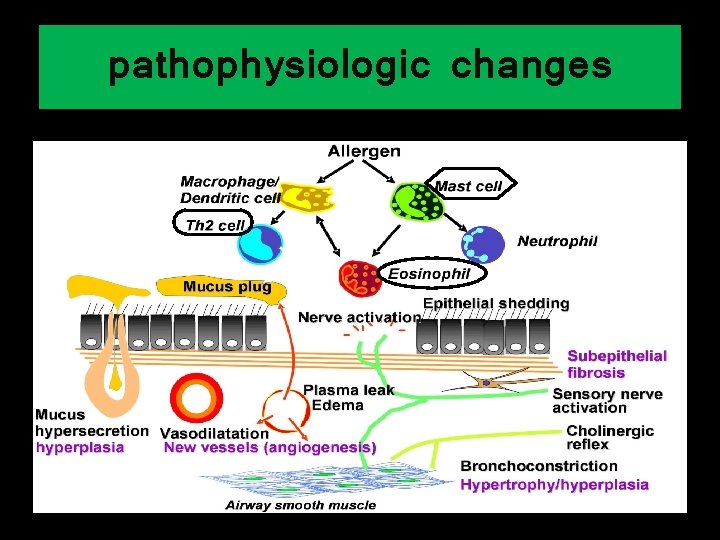
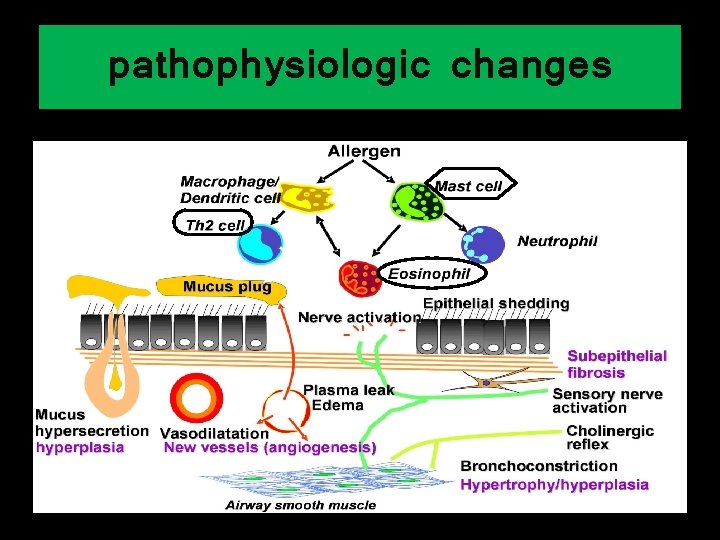
pathophysiologic changes
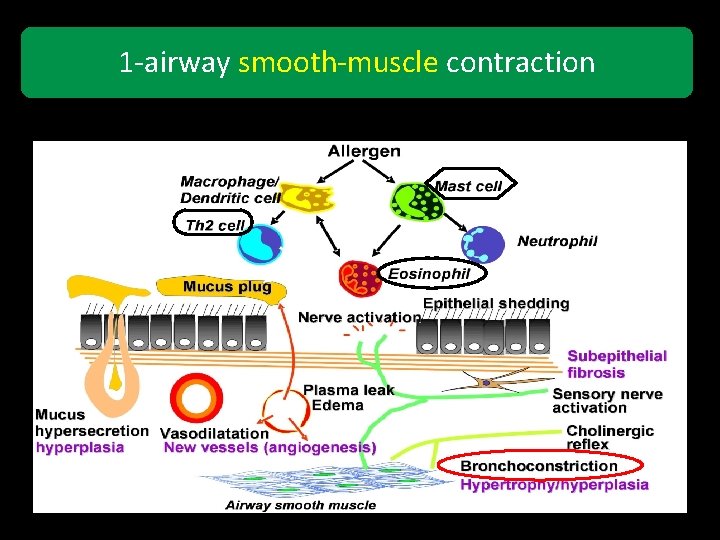
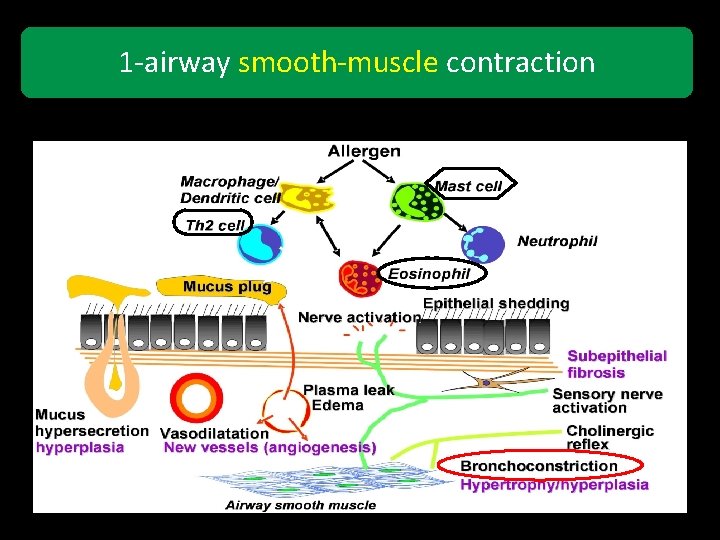
1 -airway smooth-muscle contraction
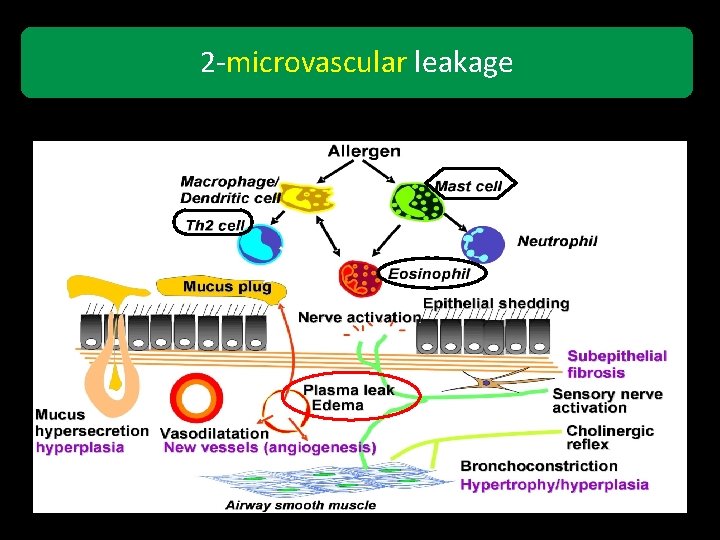
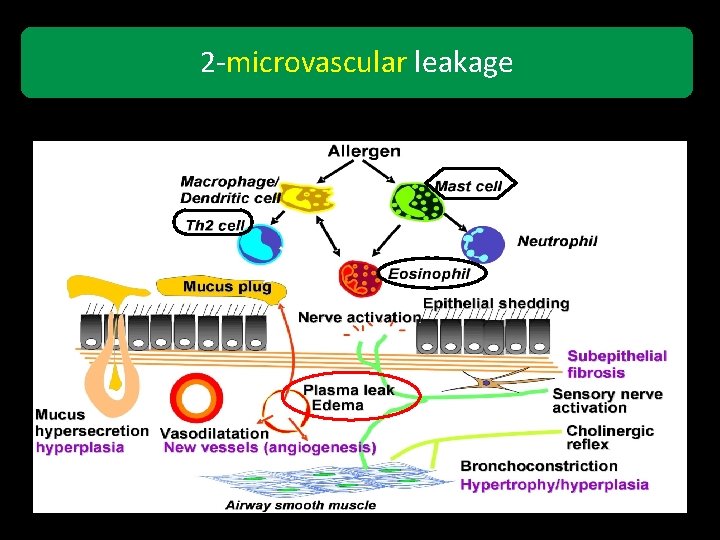
2 -microvascular leakage
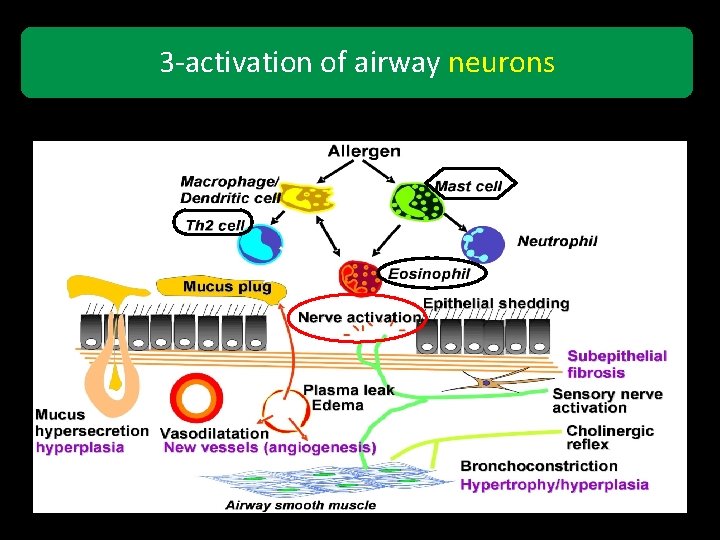
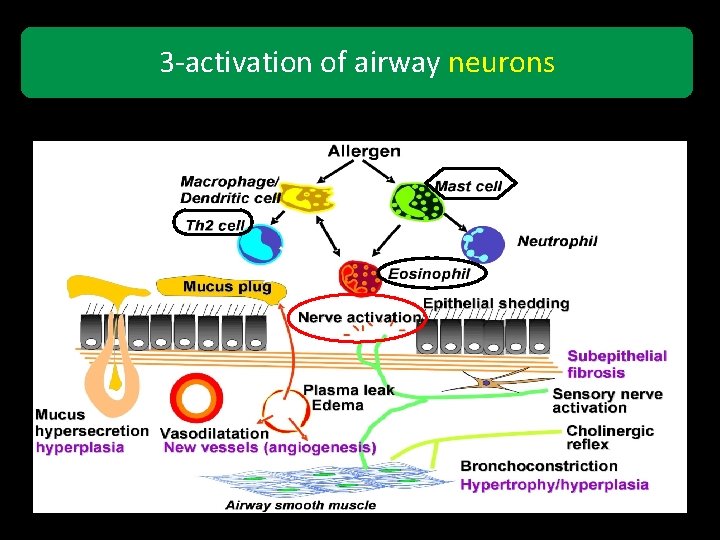
3 -activation of airway neurons
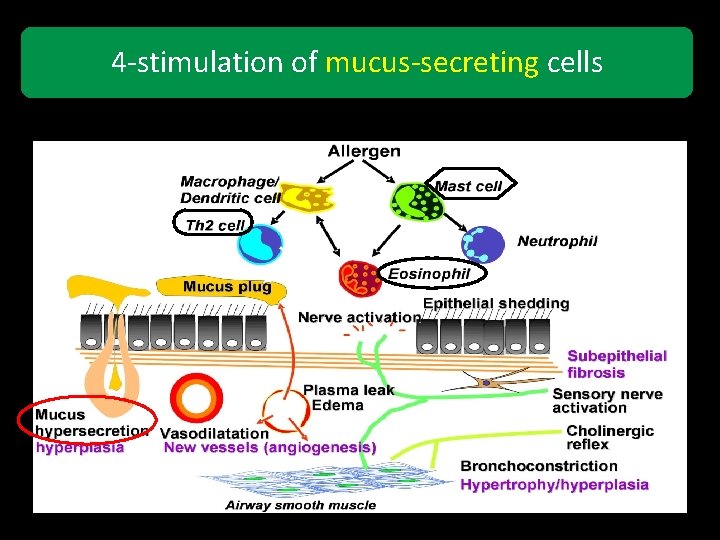
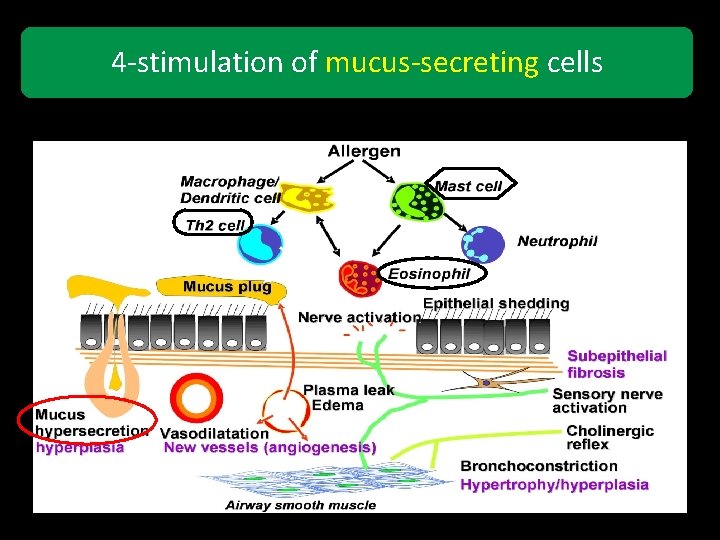
4 -stimulation of mucus-secreting cells
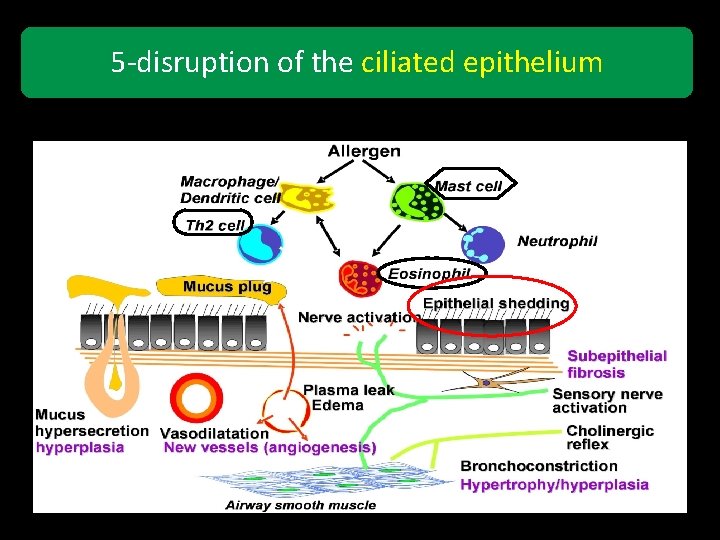
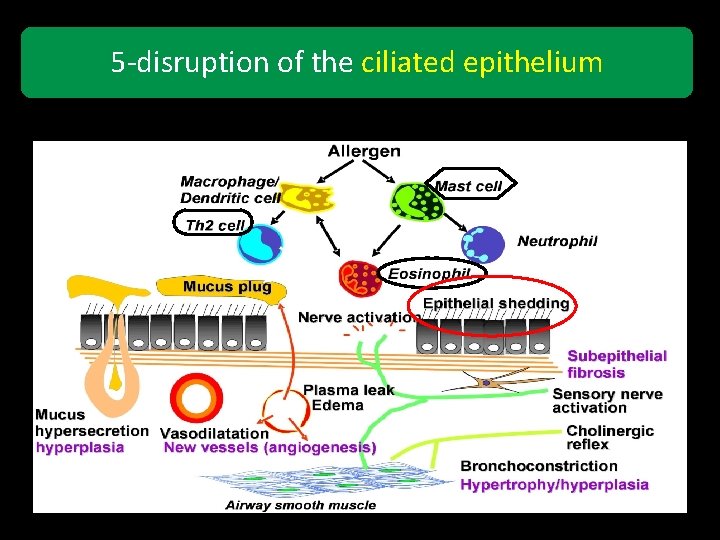
5 -disruption of the ciliated epithelium
airway remodeling • fixed airway narrowing in patients with severe asthma • The airway epithelium becomes an important source of mediators, growth factors, and chemokines

Thickening of the reticular basement membrane • increased release of fibroproliferative and fibrogenic growth factors • deposition of type III and V collagen and fibronectin beneath the basement membrane

increased bronchial smooth-muscle mass

Mucus gland hyperplasia

increased levels of vascular endothelial growth factor (angiogenesis)
Physiologic Mechanisms • Neurogenic Influences • BHR • Airway Obstruction

Physiologic Mechanisms Neurogenic Influences There is growing evidence that the neural control of the airways is abnormal in patients with asthma
Physiologic Mechanisms Neurogenic Influences autonomic dysfunction is a secondary defect caused by inflammation inflammatory mediators can modulate the release of neurotransmitters from airway nerves
Physiologic Mechanisms Neurogenic Influences The autonomic nervous system regulates many aspects of airway function, such as: • airway tone • airway secretions • blood flow • microvascular permeability • and the release of inflammatory cells
Physiologic Mechanisms BHR an exaggerated bronchoconstrictive response by the airways to a variety of stimuli such as aeroallergens, histamine, methacholine, cold air, and environmental irritants
Physiologic Mechanisms BHR Airway inflammation is thought to be a factor in producing BHR, which is a cardinal feature of asthma
Physiologic Mechanisms BHR It is not clear whether bronchial hyperreactivity is acquired or is present at birth and genetically
Physiologic Mechanisms Airway Obstruction Causes of Airflow Limitation in Asthma • Acute bronchoconstriction • Mucus plugging of airways • Bronchial wall edema • Inflammatory cell infiltration • Airway wall remodeling (fibrosis) • Smooth-muscle hypertrophy • Uncoupling of elastic recoil forces

Atopic Asthma non-atopic Asthma
Atopic Asthma Is more common than non-atopic Asthma

Atopic Asthma • extrinsic asthma • asthma that is triggered by exposure to inhaled aeroallergens Nonatopic Asthma • intrinsic asthma • unidentified antigen “self-antigens”

Atopic Asthma Nonatopic Asthma • features of atopy including: – positive family history of allergy and asthma – positive immediate hypersensitivity reactions to skin-prick tests after exposure to a variety of aeroallergens – an increased serum Ig. E leve and blood eosinophilia – Evidence of atopy, such as eczema and hay fever • patients who have NONE of the typical features of atopy
Atopic Asthma • The prevalence of atopy increases throughout childhood and adolescence and peaks in the second decade of life Nonatopic Asthma • Usually, such patients are older than atopic asthmatic patients and have a later onset of asthma
Atopic Asthma Nonatopic Asthma In children • (School Aged) • High Rate Of Persistence Into Adulthood (Preschool Children) • Improve or Resolve in a few years •
Atopic Asthma type 1 hypersensitivity reaction Ig. E-mediated inflammatory response
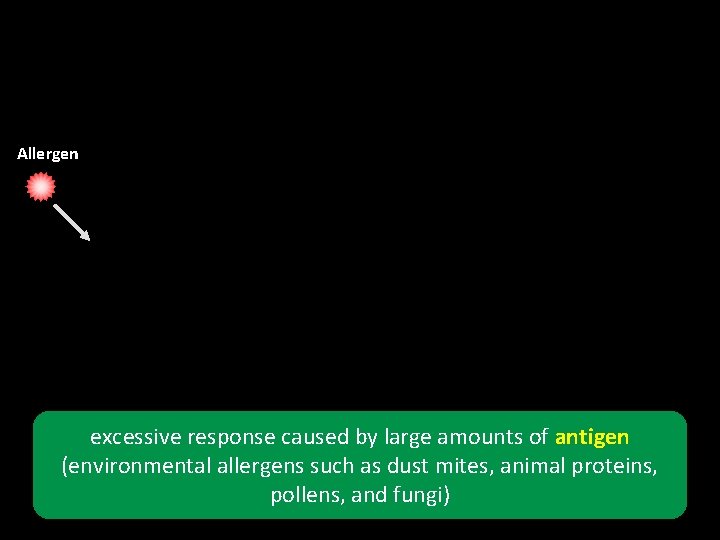
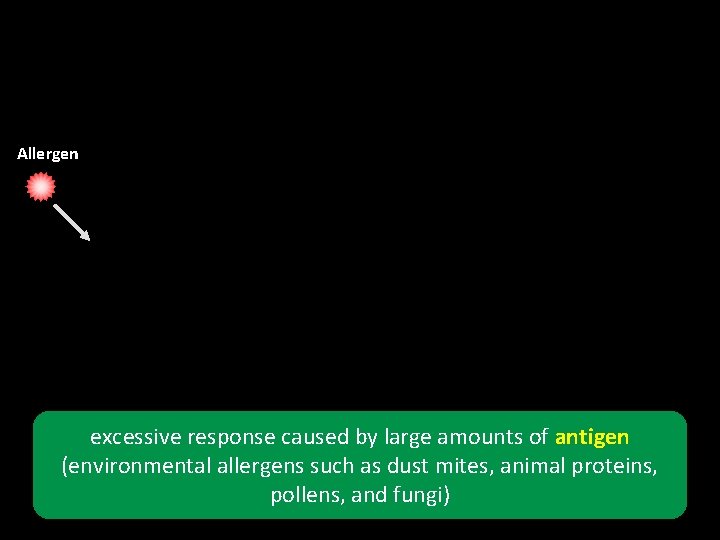
Allergen excessive response caused by large amounts of antigen (environmental allergens such as dust mites, animal proteins, pollens, and fungi)
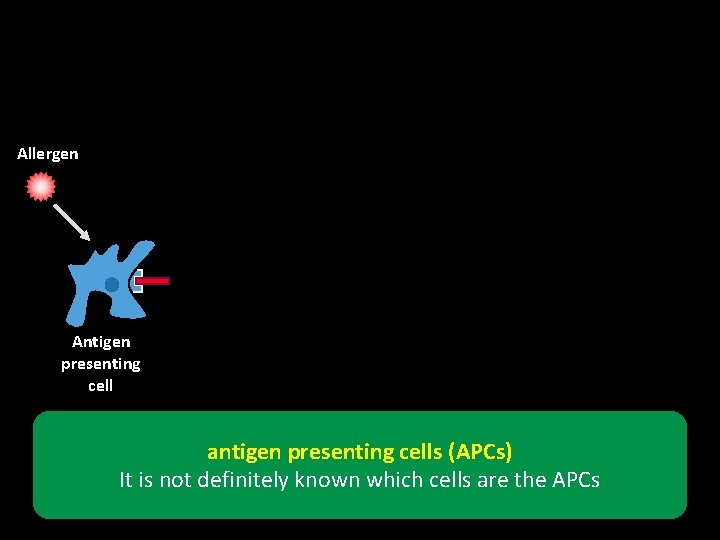
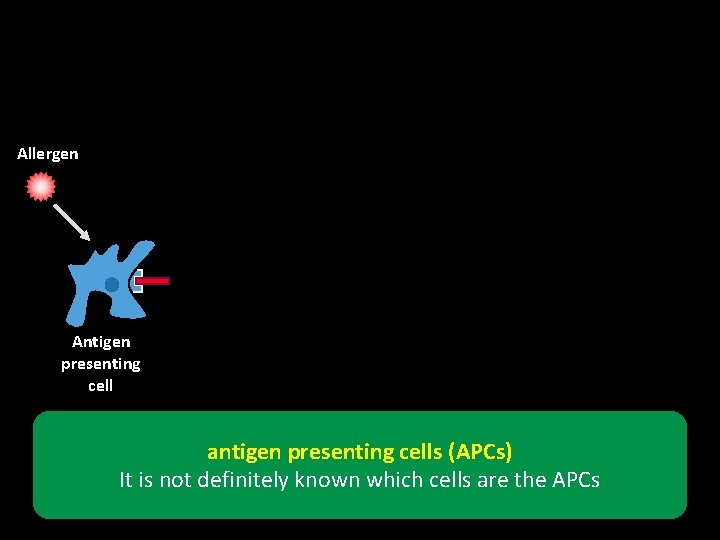
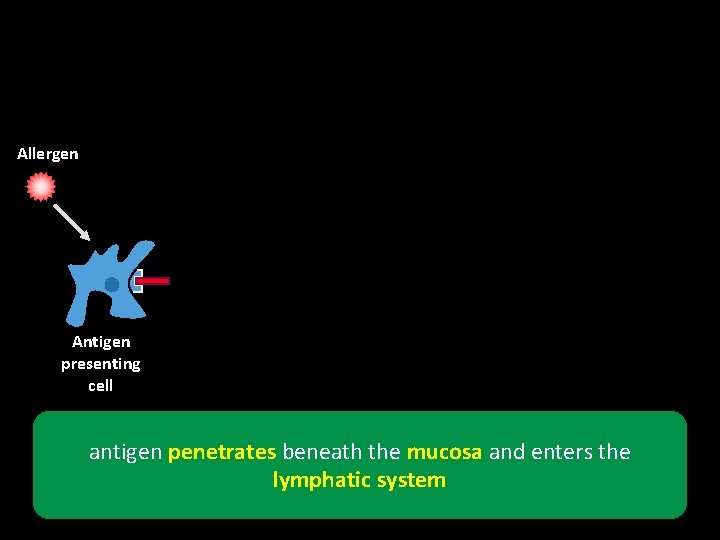
Allergen Antigen presenting cell antigen presenting cells (APCs) It is not definitely known which cells are the APCs
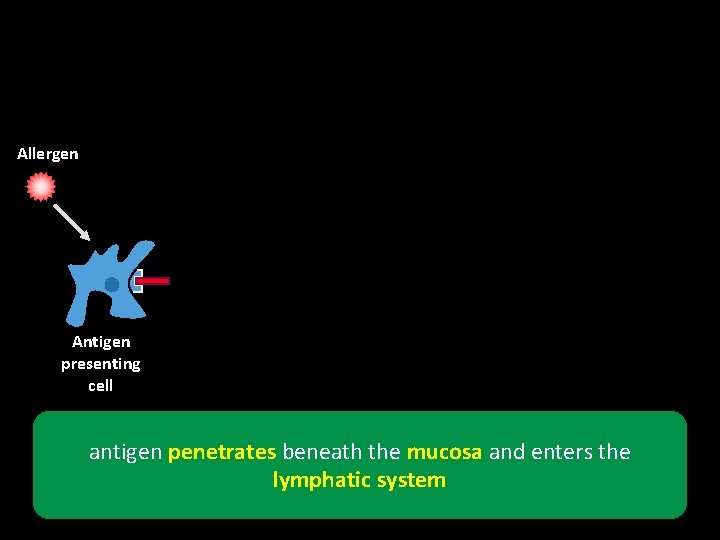
Allergen Antigen presenting cell antigen penetrates beneath the mucosa and enters the lymphatic system
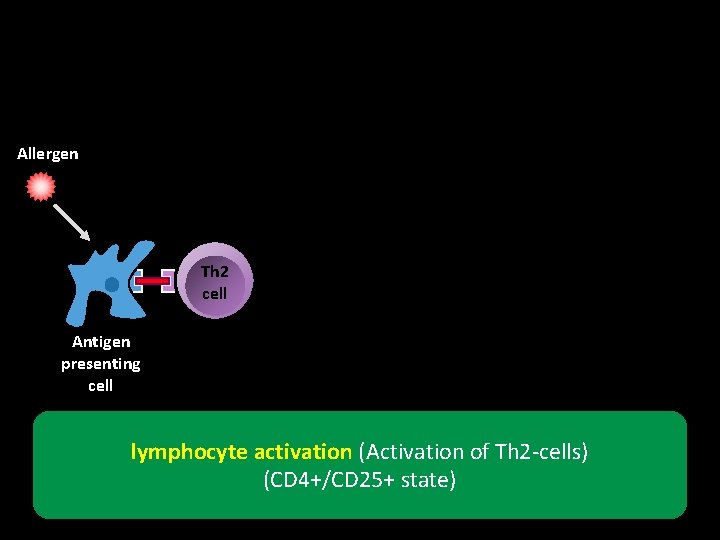
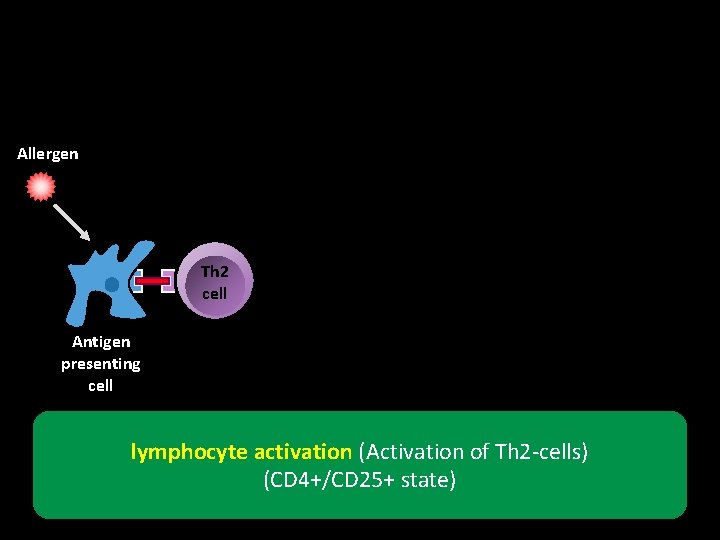
Allergen Th 2 cell Antigen presenting cell lymphocyte activation (Activation of Th 2 -cells) (CD 4+/CD 25+ state)
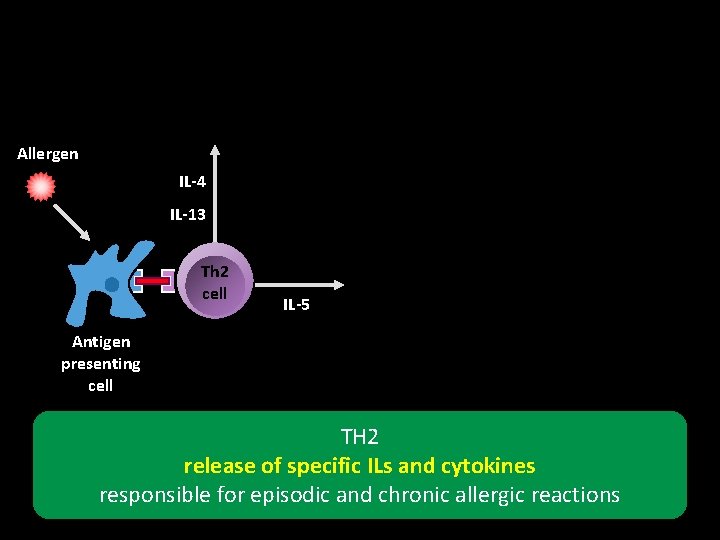
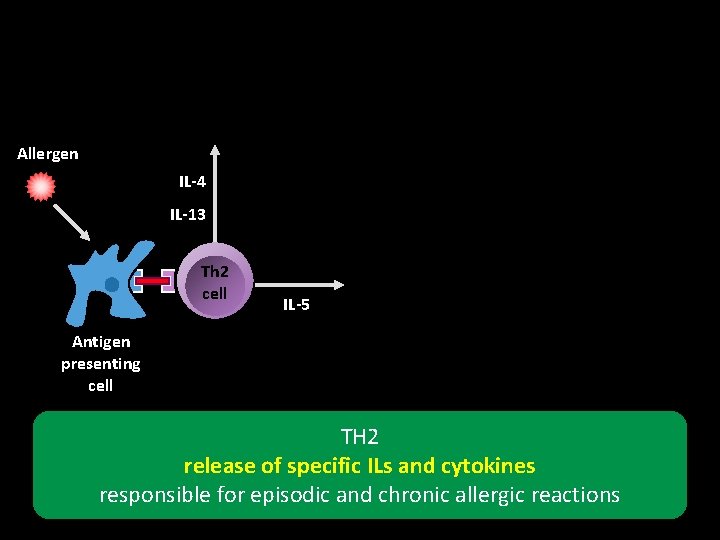
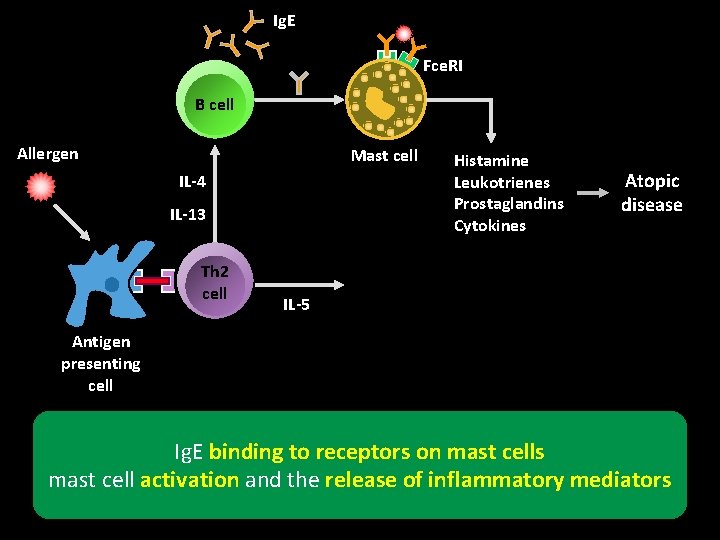
Allergen IL-4 IL-13 Th 2 cell IL-5 Antigen presenting cell TH 2 release of specific ILs and cytokines responsible for episodic and chronic allergic reactions
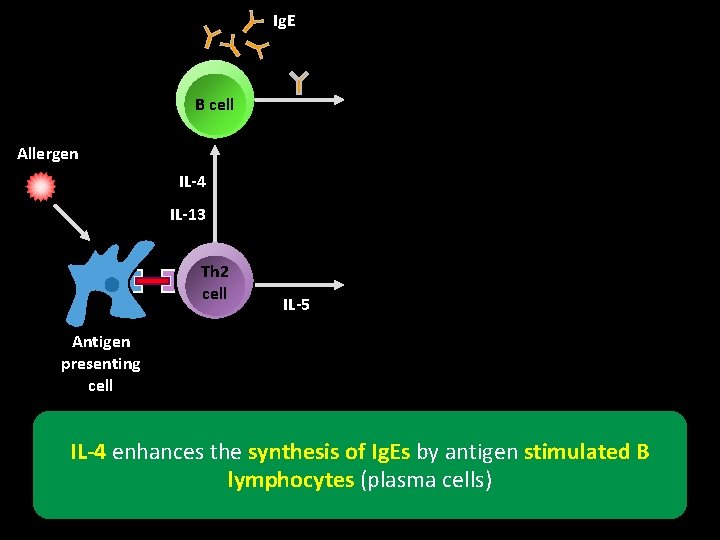
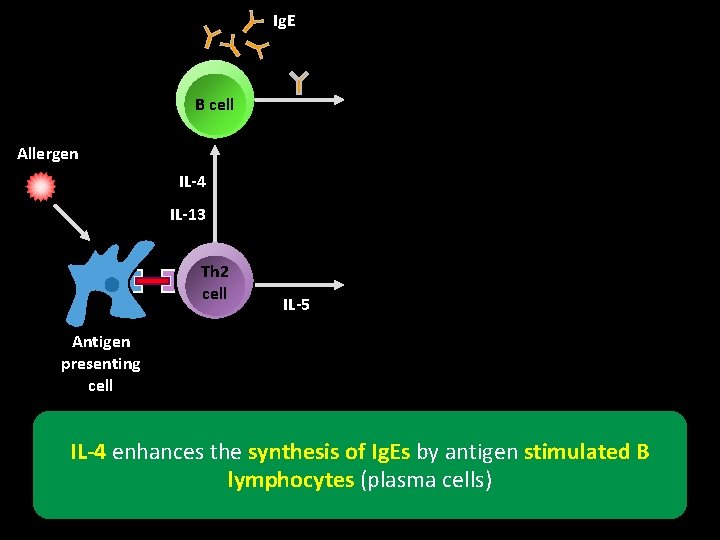
Ig. E B cell Allergen IL-4 IL-13 Th 2 cell IL-5 Antigen presenting cell IL-4 enhances the synthesis of Ig. Es by antigen stimulated B lymphocytes (plasma cells)
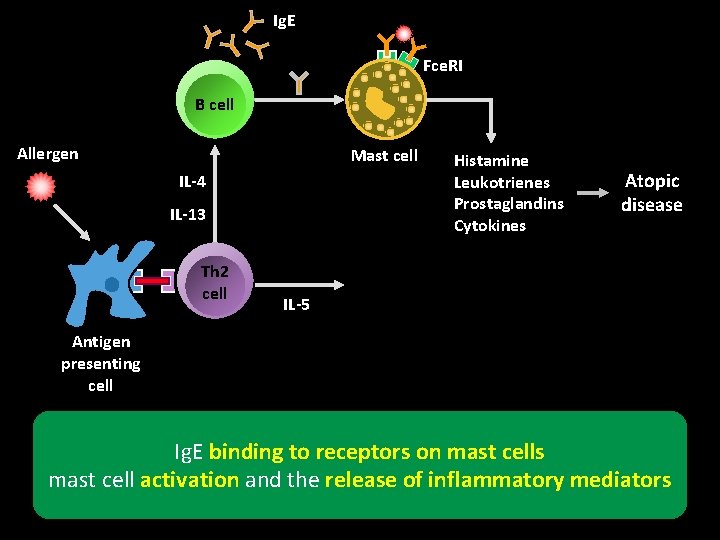
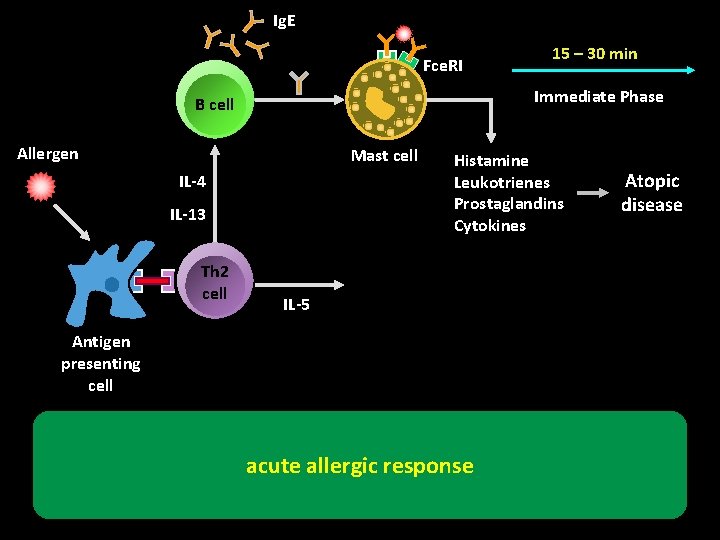
Ig. E Fce. RI B cell Allergen Mast cell IL-4 IL-13 Th 2 cell Histamine Leukotrienes Prostaglandins Cytokines Atopic disease IL-5 Antigen presenting cell Ig. E binding to receptors on mast cells mast cell activation and the release of inflammatory mediators
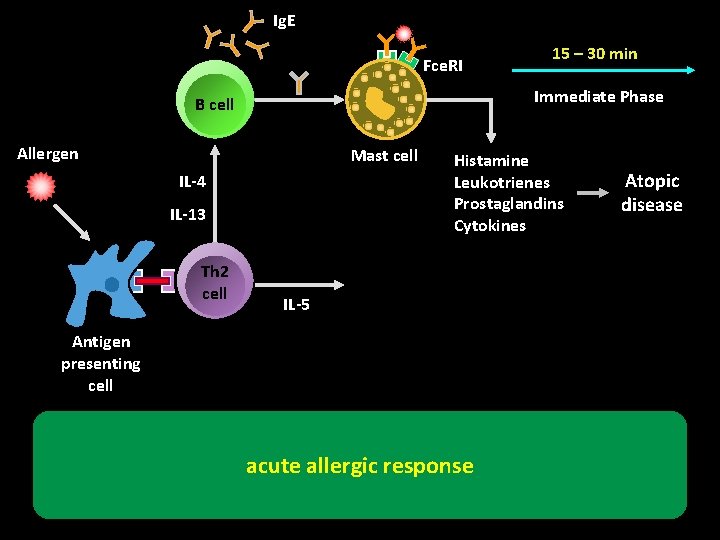
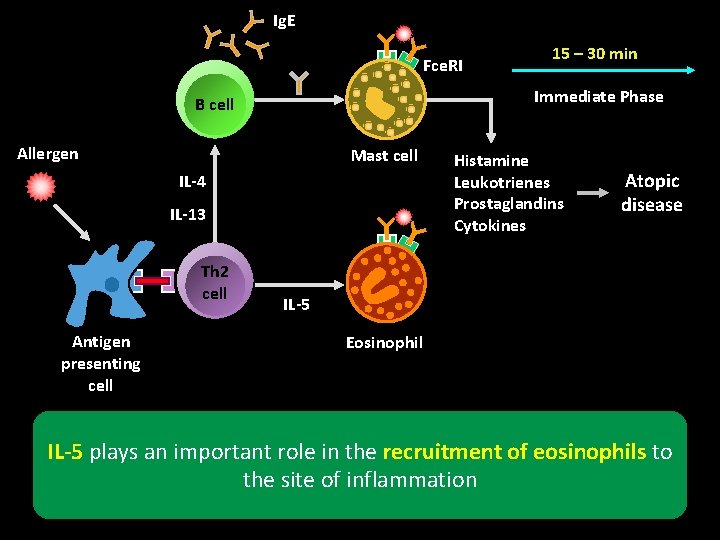
Ig. E Fce. RI Immediate Phase B cell Allergen Mast cell IL-4 IL-13 Th 2 cell 15 – 30 min Histamine Leukotrienes Prostaglandins Cytokines IL-5 Antigen presenting cell acute allergic response Atopic disease
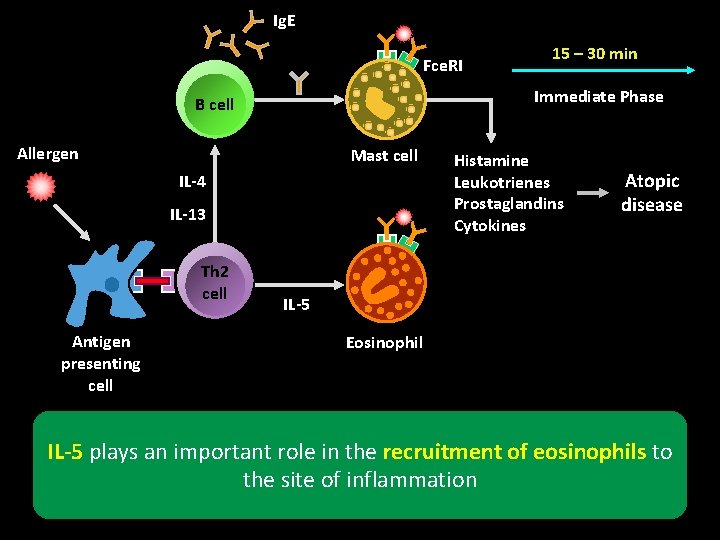
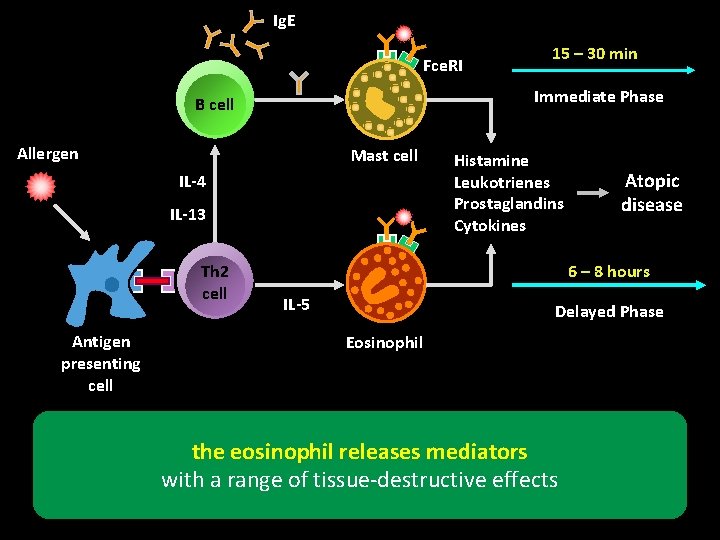
Ig. E Fce. RI Immediate Phase B cell Allergen Mast cell IL-4 IL-13 Th 2 cell Antigen presenting cell 15 – 30 min Histamine Leukotrienes Prostaglandins Cytokines Atopic disease IL-5 Eosinophil IL-5 plays an important role in the recruitment of eosinophils to the site of inflammation
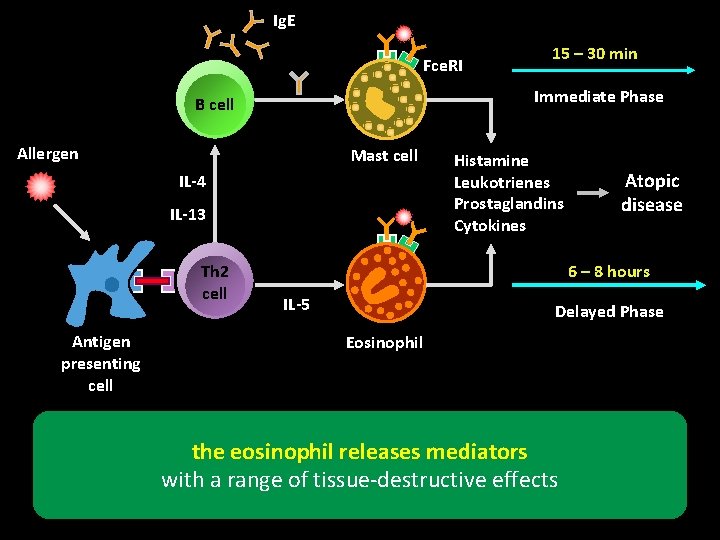
Ig. E Fce. RI Immediate Phase B cell Allergen Mast cell IL-4 IL-13 Th 2 cell Antigen presenting cell 15 – 30 min Histamine Leukotrienes Prostaglandins Cytokines Atopic disease 6 – 8 hours IL-5 Delayed Phase Eosinophil the eosinophil releases mediators with a range of tissue-destructive effects


Nonatopic Asthma There is a more intense inflammatory cell infiltrate in the bronchial mucosa macrophages, and CD 3 and CD 4 cells
Risk Factors for Asthma
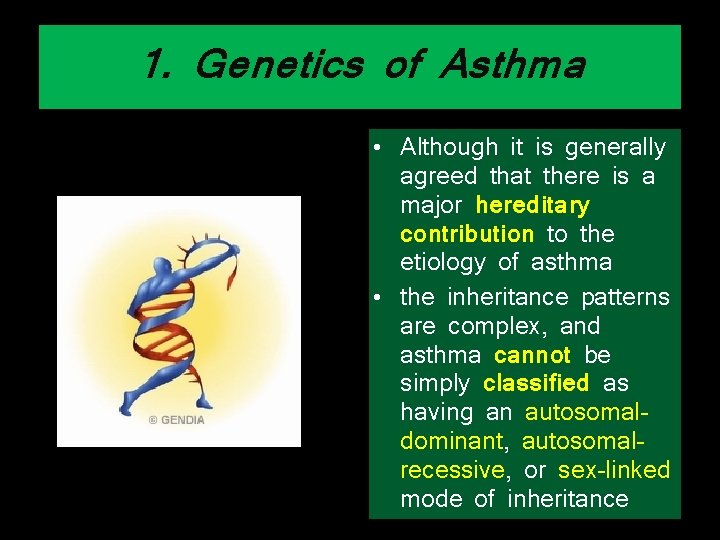
1. Genetics of Asthma • Although it is generally agreed that there is a major hereditary contribution to the etiology of asthma • the inheritance patterns are complex, and asthma cannot be simply classified as having an autosomaldominant, autosomalrecessive, or sex-linked mode of inheritance
1. Genetics of Asthma • However, genetic studies have discovered multiple chromosomal regions that may contain genes that contribute to asthma
1. Genetics of Asthma • Chromosomes 2 q, 3 p, 5 q, 6 p, 12 q, 13 q, 19 q, and 21 q are likely to contain genes for allergy and asthma
1. Genetics of Asthma • One mutation (the substitution of glycine for arginine at position 16) was associated with more severe asthma and especially with more severe nocturnal symptoms
1. Genetics of Asthma • Another mutant at position 27 renders the receptor more resistant to βagonist and has been associated with less intense BHR in patients with asthma

1. Genetics of Asthma • IL 4 RA gene have been associated with severe exacerbations and poor lung function
1. Genetics of Asthma • the ADAM 33 gene is associated with an accelerated decrease in lung function
2. Sex and Race > Before Puberty 6 versus 3. 7 percent = After Puberty • Childhood asthma is more prevalent in boys, but this prevalence is reversed in puberty and adulthood

2. Sex and Race • The overall prevalence, therefore, is greater in female individuals
2. Sex and Race • Black race/ethnicity is associated with a greater risk of asthma death, independent of socioeconomic status and education
2. Sex and Race • The greater incidence of asthma that has been observed with urbanization suggests that environmental factors may be as important as genetic and racial factors
3. Environmental Factors • Allergens and occupational factors are considered to be the most important causes of asthma
Indoor allergens • animal allergens (eg, cats, dogs, and rodents)
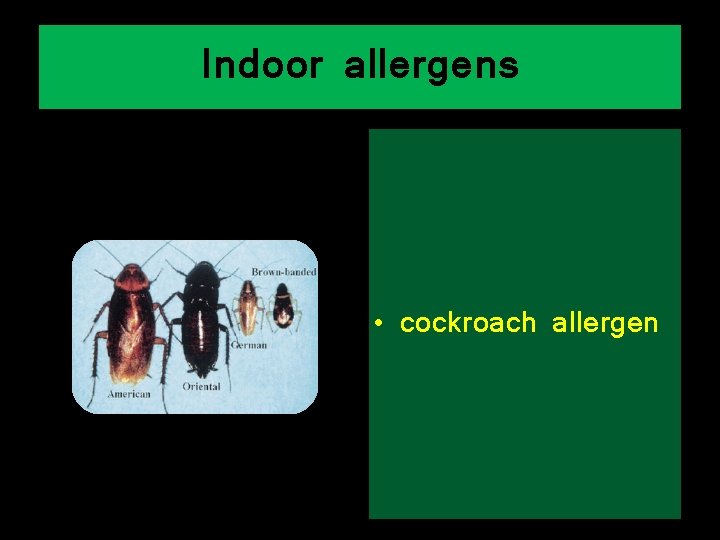
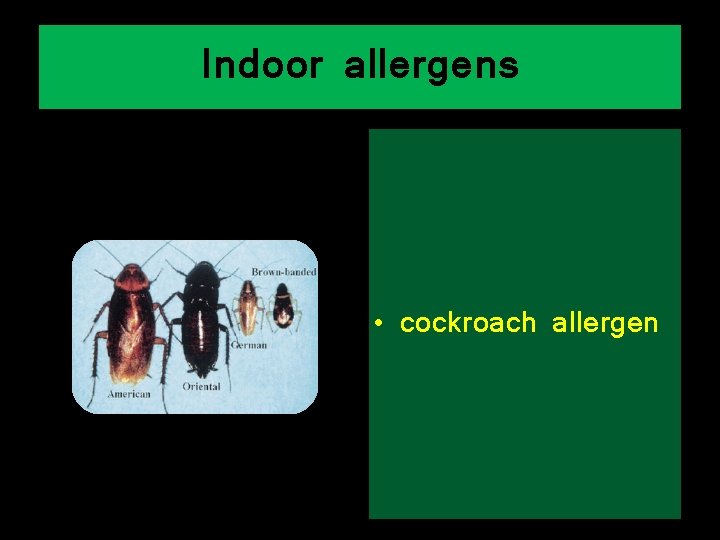
Indoor allergens • cockroach allergen
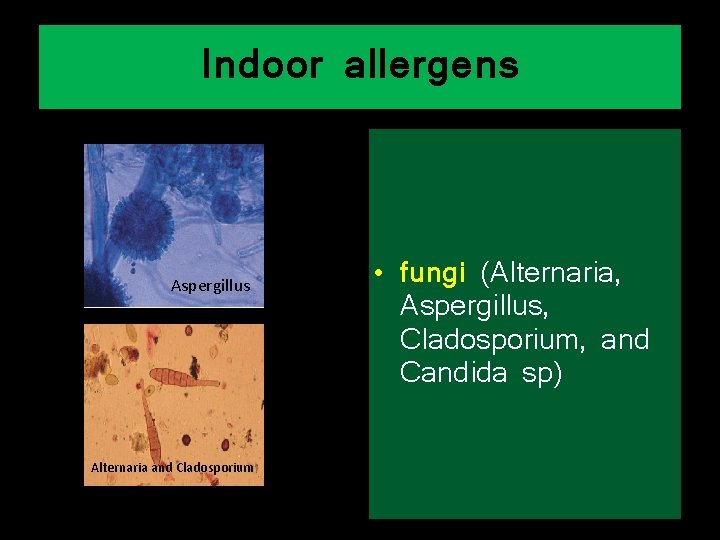
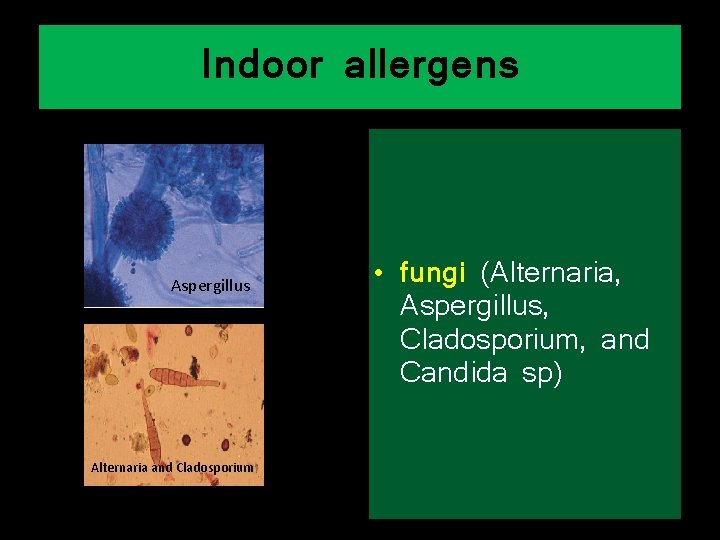
Indoor allergens Aspergillus Alternaria and Cladosporium • fungi (Alternaria, Aspergillus, Cladosporium, and Candida sp)
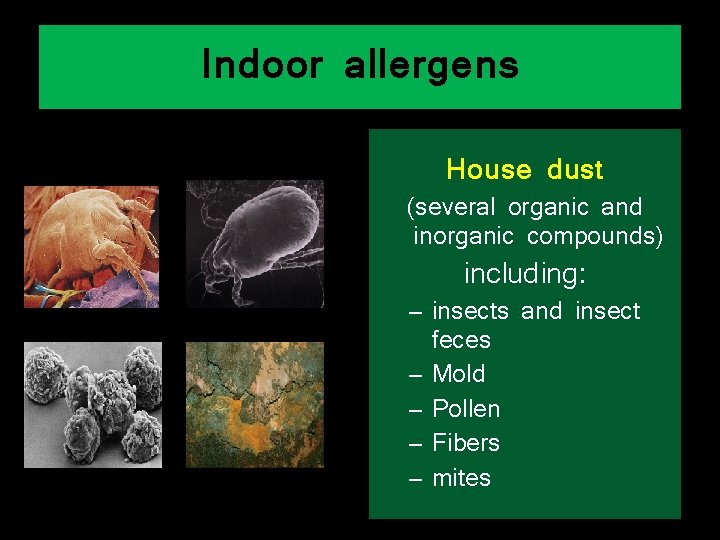
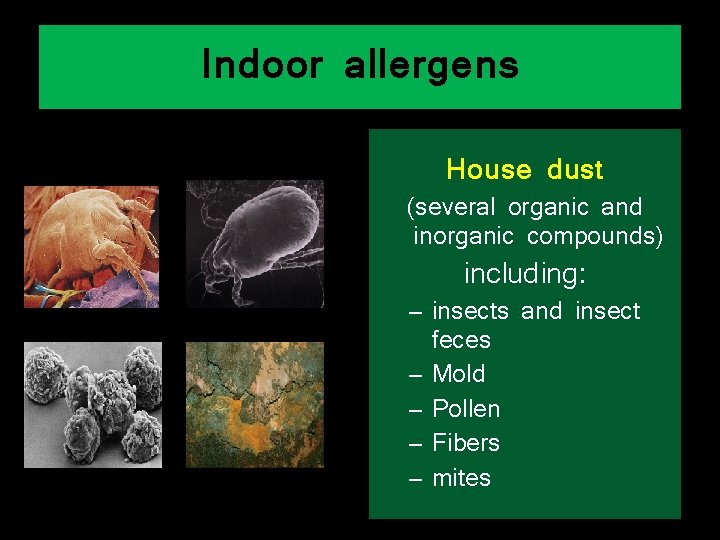
Indoor allergens House dust (several organic and inorganic compounds) including: – insects and insect feces – Mold – Pollen – Fibers – mites
Social Factors 66
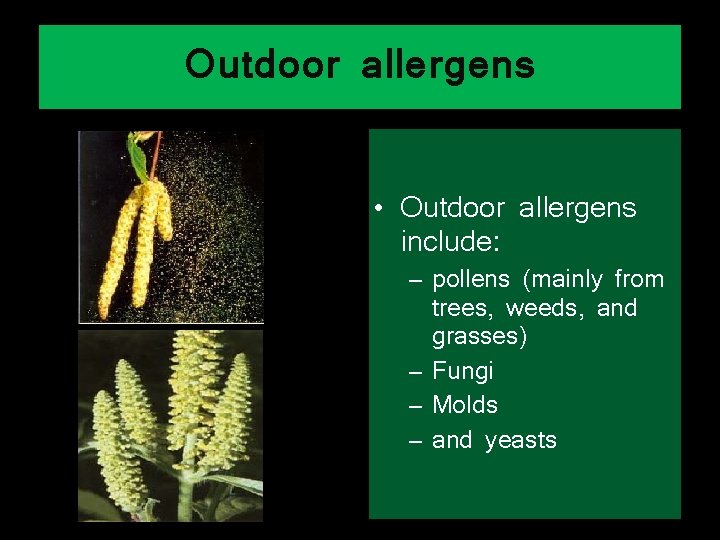
Outdoor allergens • Outdoor allergens include: – pollens (mainly from trees, weeds, and grasses) – Fungi – Molds – and yeasts
4. Air Pollution • Both outdoor and indoor pollutants contribute to worsening asthma symptoms by triggering bronchoconstriction, increasing BHR, and enhancing responses to inhaled aeroallergens
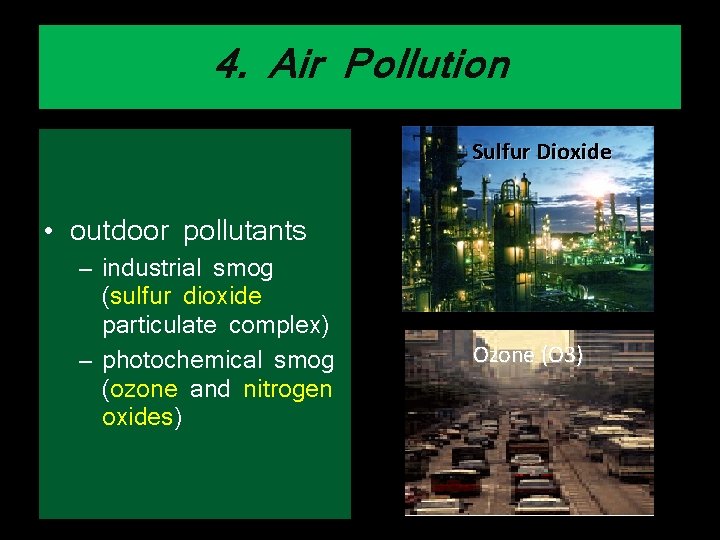
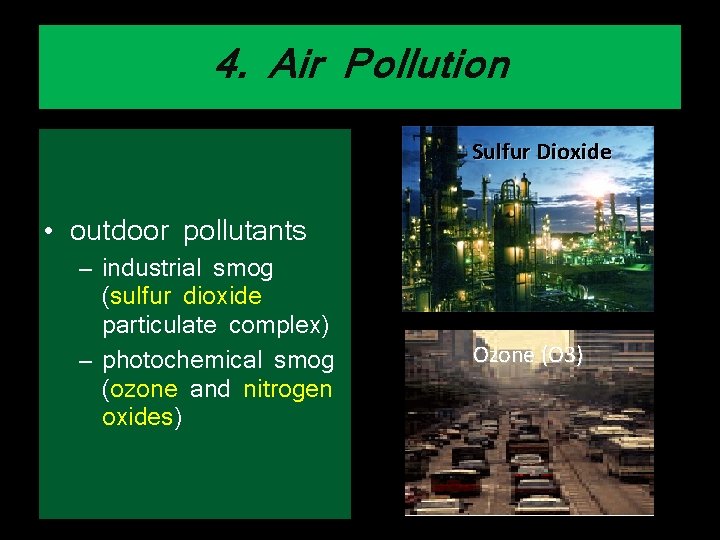
4. Air Pollution Sulfur Dioxide • outdoor pollutants – industrial smog (sulfur dioxide particulate complex) – photochemical smog (ozone and nitrogen oxides) Ozone (O 3)
4. Air Pollution • indoor air pollution – Modern construction techniques have been suspected of causing greater indoor air pollution – there is 50% less turnover of fresh air
4. Air Pollution • Indoor pollutants include: – – – cooking heating fuel exhausts insulating products Paints and varnishes that contain formaldehyde and isocyanates
4. Air Pollution • Smoking and exposure to environmental Tobacco: – Active smoking – Secondhand smoke – Prenatal exposure to maternal smoking
4. Air Pollution • The effect of cleaning solutions and sprays in the home
5. Respiratory Infections • It has been established that viral respiratory infections are common precipitators of asthma
5. Respiratory Infections § Viral and bacterial respiratory infections are triggers that can cause exacerbations in children and adults with asthma
5. Respiratory Infections • There are strong data to suggest that some of the atypical bacteria, such as Chlamydia pneumoniae and Mycoplasma pneumoniae, also may be involved
5. Respiratory Infections • Therapy with the macrolide antibiotic clarithromycin improved lung function and decreased tissue expression of IL-5

5. Respiratory Infections • This finding suggests that antibiotic use in some patients with persistent asthma may help to control the disease
5. Respiratory Infections § The frequent respiratory infection during infancy may protect against the later development of – Asthma – Hay fever – Eczema

6. atopy / Allergic Rhinitis 1. Allergic Rhino Sinusitis 2. Atopic Dermatitis 3. Allergic conjunctivitis

Percentage patients with comorbidity Allergic rhinitis is often accompanied by comorbidities
6. atopy / Allergic Rhinitis • Nasal and sinus diseases are common comorbidities in patients with asthma
6. atopy / Allergic Rhinitis • Allergic rhinitis (AR) and asthma commonly occur together • > 40% of children with AR have asthma • the presence of AR in a child < 7 years of age predicts future asthma
6. atopy / Allergic Rhinitis • smokers with AR have a threefold increased risk for developing asthma
6. atopy / Allergic Rhinitis • patients with AR, despite the paucity of pulmonary symptoms, have abnormal lung function • And when tested with methacholine or histamine, demonstrate BHR
Other Factors

Stress
Obesity • underweight and being overweight are both associated with an increased risk of the development of asthma
Obesity • Increased BMI may also be associated with increased asthma severity
Obesity • There is some evidence that weight loss in obese asthmatic patients is associated with improved symptoms and lung function, especially PEFR variability
Family history • Children with one asthmatic parent are 2. 6 times more likely to have asthma
Family history • Children with two asthmatic parents, the odds ratio rises to 5. 2
Family history • Mama > Baba Clin Exp Allergy. 2004 Jun; 34(6): 839 -44
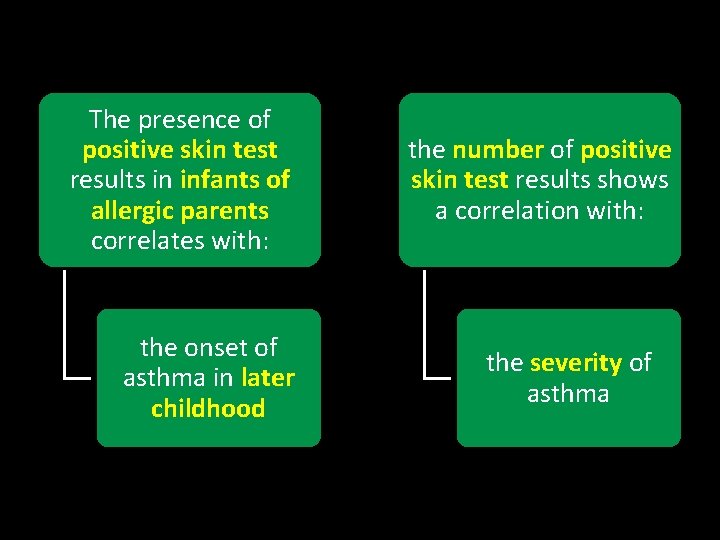
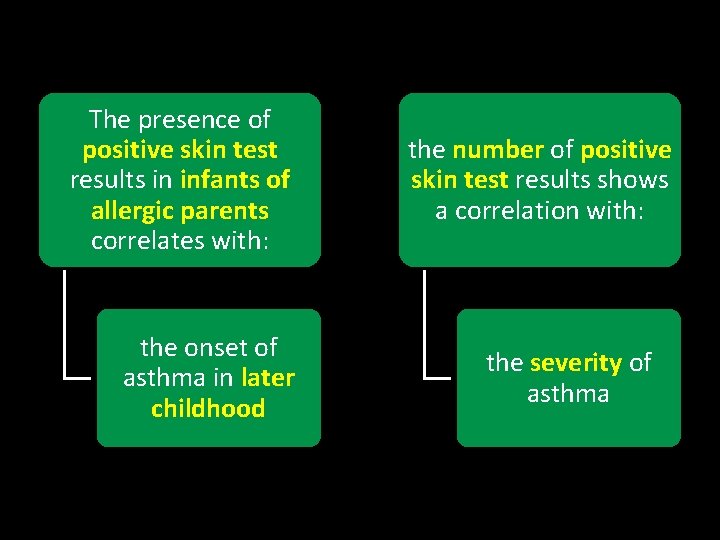
The presence of positive skin test results in infants of allergic parents correlates with: the onset of asthma in later childhood the number of positive skin test results shows a correlation with: the severity of asthma
Studies indicate a reverse relationship between family size and asthma This finding suggest that the exposure of young children to older children at home or to children at day-care centers protects against the development of asthma
Medication Use • Use of paracetamol in the first year of life was associated with a small increase in risk of asthma at age 6 to 7
Medication Use • mothers taking regular acetaminophen during pregnancy
Medication Use • Exposure to antibiotics during infancy has been associated with the development of asthma in later childhood • The “microflora hypothesis”
Pre- and Perinatal Factors v Maternal age • Infant mortality due to respiratory illnesses is inversely related to maternal age • children born to mothers younger than 20 years had the highest risk of developing asthma

Pre- and Perinatal Factors v Maternal diet during pregnancy • maternal diet in pregnancy, in particular intakes of the antioxidant vitamin E and zinc, may modulate the risk for wheezing and asthma in young children Vit etam c a r pa E ol Ant ibio Zin tics c
Pre- and Perinatal Factors v Breastfeeding • • Breastfeeding was associated with a decreased risk of wheeze in the first two years of life by age six this effect was not significant
Pre- and Perinatal Factors v Breastfeeding • in the subset of children with atopy and an asthmatic mother, breastfeeding was associated with an increased risk of asthma
Pre- and Perinatal Factors v Breastfeeding • we encourage this approach for at least 4 to 6 months following delivery, regardless of the child's risk of atopy or the presence of maternal asthma
Pre- and Perinatal Factors v Prematurity • Prematurity was a significant risk factor for both recurrent wheezy bronchitis and asthma
Pre- and Perinatal Factors v Mode of delivery • Delivery by Cesarean section may increase the risk of childhood asthma compared with vaginal delivery

"The Hygiene Hypothesis” • The microbial exposure and infections during early childhood (ie, postnatally) protect against the development of asthma and other allergic disease
Pre- and Perinatal Factors v Head circumference at birth
The Natural History of Asthma
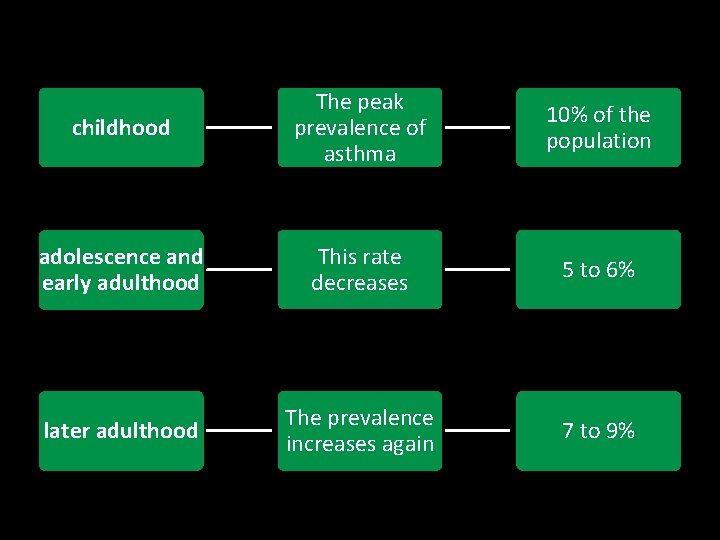
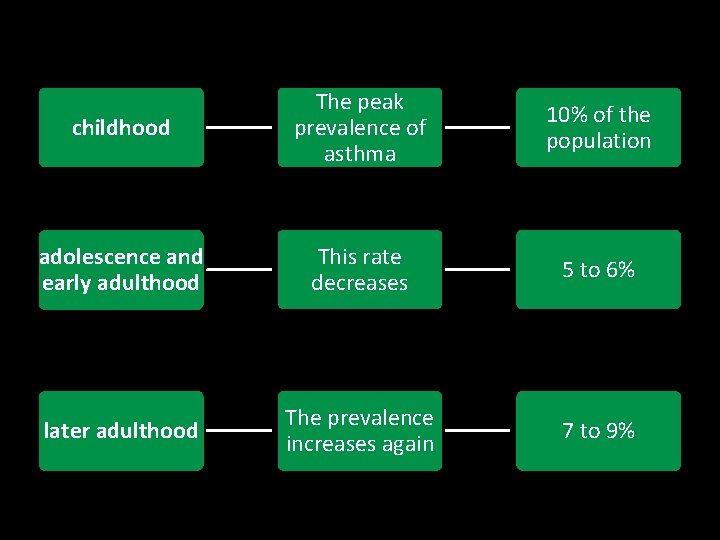
childhood The peak prevalence of asthma 10% of the population adolescence and early adulthood This rate decreases 5 to 6% later adulthood The prevalence increases again 7 to 9%
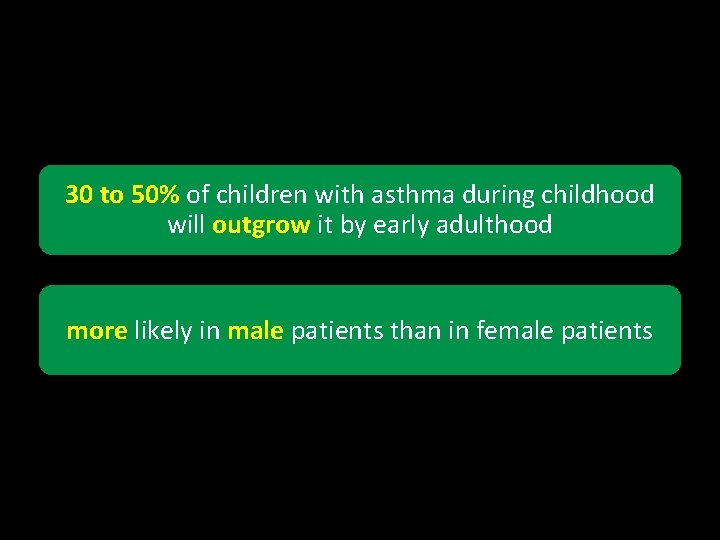
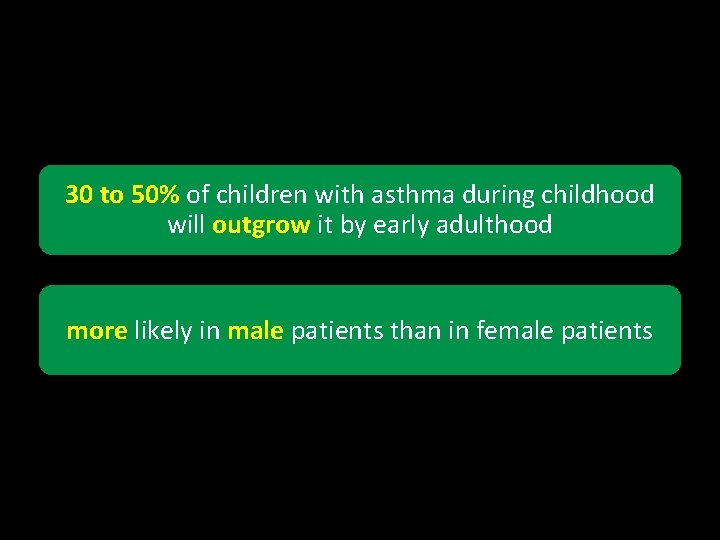
30 to 50% of children with asthma during childhood will outgrow it by early adulthood more likely in male patients than in female patients
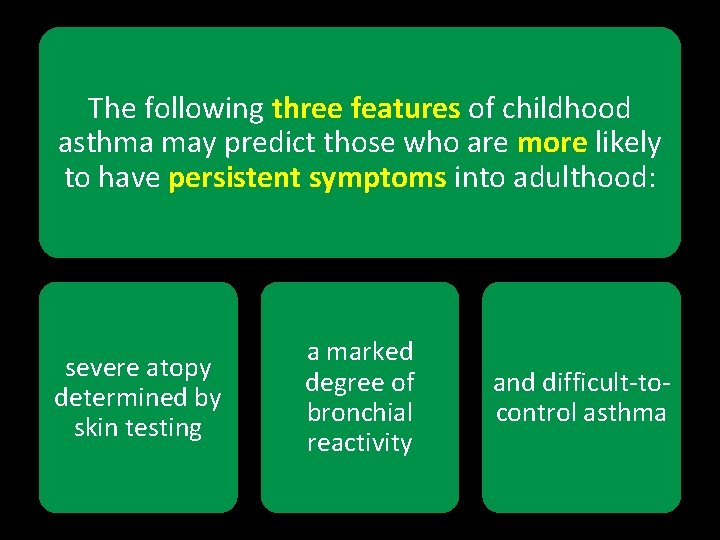
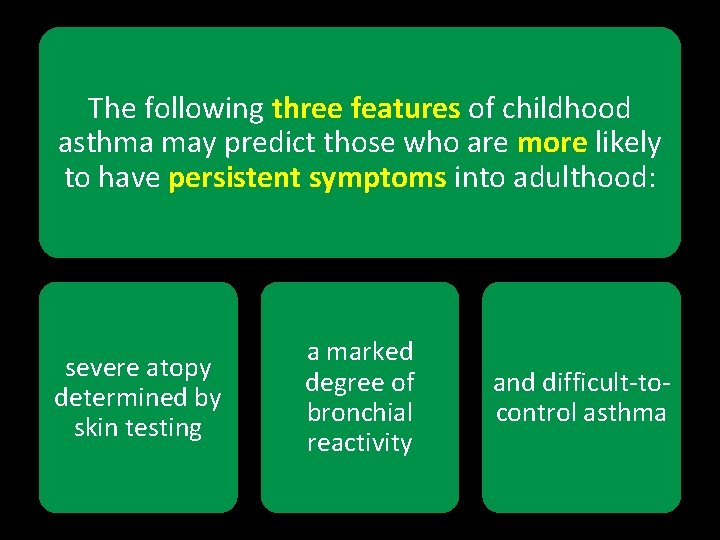
The following three features of childhood asthma may predict those who are more likely to have persistent symptoms into adulthood: severe atopy determined by skin testing a marked degree of bronchial reactivity and difficult-tocontrol asthma

In adulthood there is a steady incidence of new-onset asthma through patients of all ages, even in elderly patients
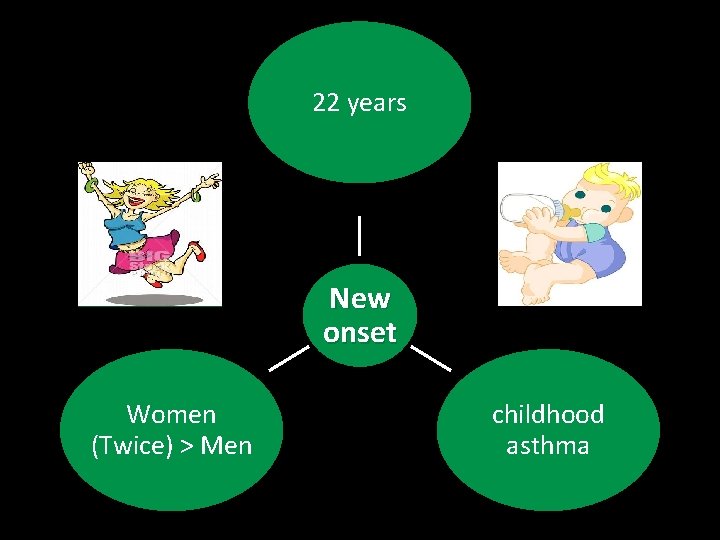
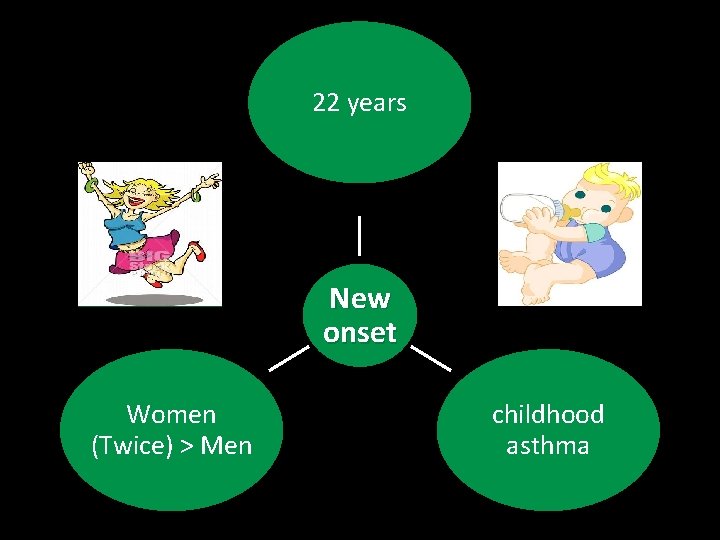
22 years New onset Women (Twice) > Men childhood asthma
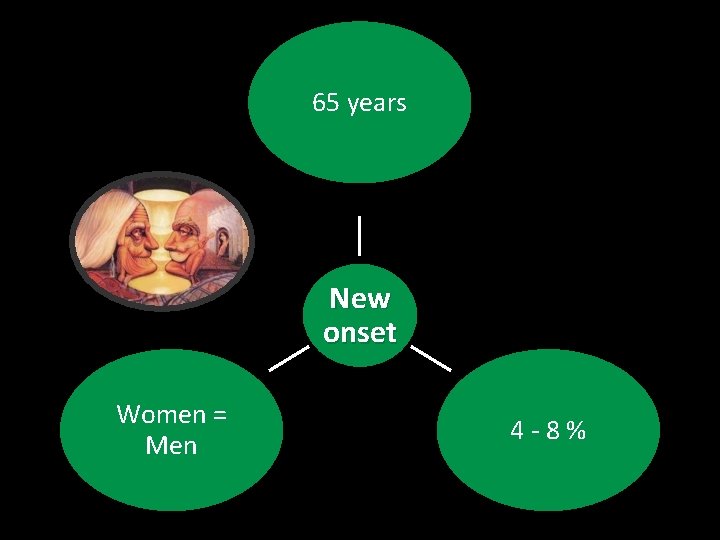
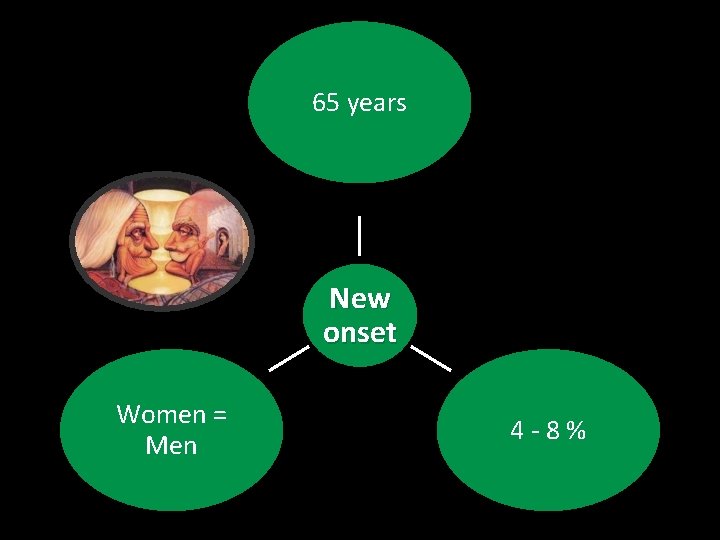
65 years New onset Women = Men 4 -8%
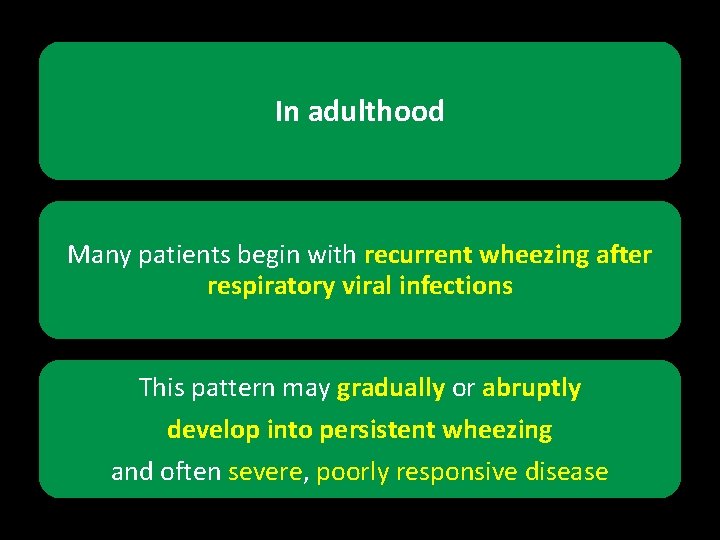
In adulthood Many patients begin with recurrent wheezing after respiratory viral infections This pattern may gradually or abruptly develop into persistent wheezing and often severe, poorly responsive disease
In adulthood remission is much less common in older age groups although it still may be as high as 20 to 30% • severe symptoms • reduced ventilatory function • and a concomitant diagnosis of COPD
In adulthood Asthma may also result from exposure to occupational hazards Remission usually occurs when the patient is removed from the offending environment, but unfortunately, this is not always the case


1. Triggers
 Cardiac asthma vs bronchial asthma
Cardiac asthma vs bronchial asthma Gina guidelines asthma
Gina guidelines asthma Asthma classification
Asthma classification Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Thang điểm glasgow
Thang điểm glasgow Bài hát chúa yêu trần thế alleluia
Bài hát chúa yêu trần thế alleluia Các môn thể thao bắt đầu bằng tiếng bóng
Các môn thể thao bắt đầu bằng tiếng bóng Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Giọng cùng tên là
Giọng cùng tên là Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phối cảnh
Phối cảnh Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot So nguyen to
So nguyen to Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Hệ hô hấp
Hệ hô hấp Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Aerochamber definition
Aerochamber definition Spirometry
Spirometry Types of bronchial asthma
Types of bronchial asthma Asthma treatment
Asthma treatment Asthma diagnosis criteria
Asthma diagnosis criteria Asthma grading
Asthma grading Seasonal allergy icd10
Seasonal allergy icd10 Hltaid 003
Hltaid 003 Gina asthma
Gina asthma Gina 2015
Gina 2015 Asthma vs copd spirometry
Asthma vs copd spirometry Cough varient asthma
Cough varient asthma Mild moderate severe asthma exacerbation
Mild moderate severe asthma exacerbation Cause of asthma
Cause of asthma Asthma grades
Asthma grades Asthma types
Asthma types Asthma index
Asthma index Hengameh raissy
Hengameh raissy Asthma step up therapy
Asthma step up therapy X ray of asthma patient
X ray of asthma patient 3392chest
3392chest Asthma stages
Asthma stages Asthma complications
Asthma complications What is life
What is life Asthma attack
Asthma attack Occupational asthma
Occupational asthma Co2 narcosis
Co2 narcosis Asthma pathophysiology
Asthma pathophysiology Occupational asthma
Occupational asthma Specific objectives of asthma
Specific objectives of asthma Non atopic asthma
Non atopic asthma Oshit asthma
Oshit asthma Subjective and objective data for asthma
Subjective and objective data for asthma Pediatric asthma care near santa rosa
Pediatric asthma care near santa rosa Ionotrops
Ionotrops Asthma
Asthma Hippocrates asthma
Hippocrates asthma Asthma in the bronx
Asthma in the bronx Mepolizumab
Mepolizumab Asthma symptoma
Asthma symptoma Unmet needs in severe asthma
Unmet needs in severe asthma Laba asthma
Laba asthma Asthma stufenplan
Asthma stufenplan Nwts asthma
Nwts asthma Score pulmonar pediatrica
Score pulmonar pediatrica International severe asthma registry
International severe asthma registry Asthma types
Asthma types Gina 2019
Gina 2019 Global initiative for asthma
Global initiative for asthma Www.ginasthma.org
Www.ginasthma.org Amas faa drugs
Amas faa drugs Asthma
Asthma Brainpop respiratory system
Brainpop respiratory system Abcde assessment asthma
Abcde assessment asthma Asthma games
Asthma games Asthma internist kenai peninsula
Asthma internist kenai peninsula Driver diagram asthma
Driver diagram asthma American academy of allergy asthma and immunology 2018
American academy of allergy asthma and immunology 2018 Allergy asthma immunol res impact factor
Allergy asthma immunol res impact factor Definition of essential documents as per ich gcp guidelines
Definition of essential documents as per ich gcp guidelines Large size at starbucks
Large size at starbucks Post fall management
Post fall management Critical thinking guidelines
Critical thinking guidelines User documentation guidelines
User documentation guidelines Time management guidelines
Time management guidelines Tii project appraisal guidelines
Tii project appraisal guidelines Pathophysiology of hypothyroidism
Pathophysiology of hypothyroidism Lsu thesis and dissertation library
Lsu thesis and dissertation library Fruit pyramid
Fruit pyramid Pmtct guidelines 2019
Pmtct guidelines 2019 Bni branding
Bni branding Technical guidelines for disposal to land
Technical guidelines for disposal to land The talent show by susan wojciechowski
The talent show by susan wojciechowski Swachhta action plan for school
Swachhta action plan for school Sterile gloves
Sterile gloves