Nutritional assessment in hospitalized patients M Safarian MD





















































- Slides: 119

Nutritional assessment in hospitalized patients M. Safarian, MD Ph. D.
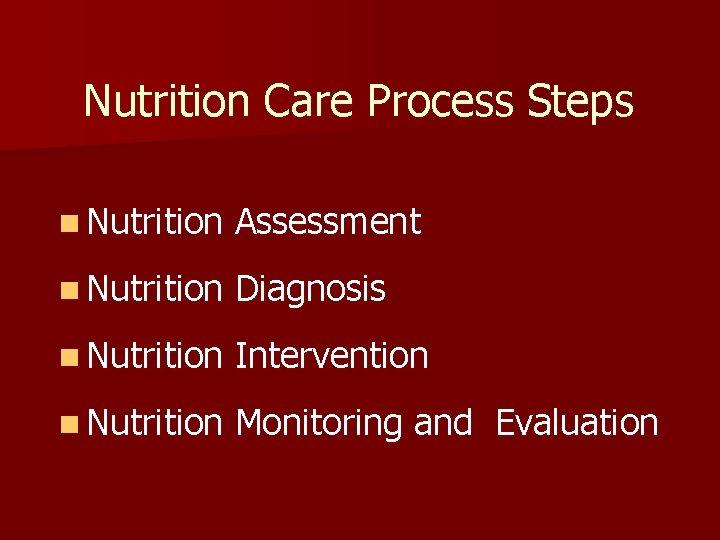
Nutrition Care Process Steps n Nutrition Assessment n Nutrition Diagnosis n Nutrition Intervention n Nutrition Monitoring and Evaluation

Nutritional care process Anthropometrics Nutritional assessment tools
Nutritional Assessment n Anthropometric n Clinical evaluation n Biochemical, n Dietary assessment laboratory assessment evaluation
ESPEN guidelines Questions to be answered: n What n Is is the condition now? the condition stable? n Will the condition get worse? the disease process accelerate nutritional deterioration?
Anthropometric methods in ICU n Weight n Height estimation n Mid-arm n Skin circumference fold thickness n Head circumference

Weight
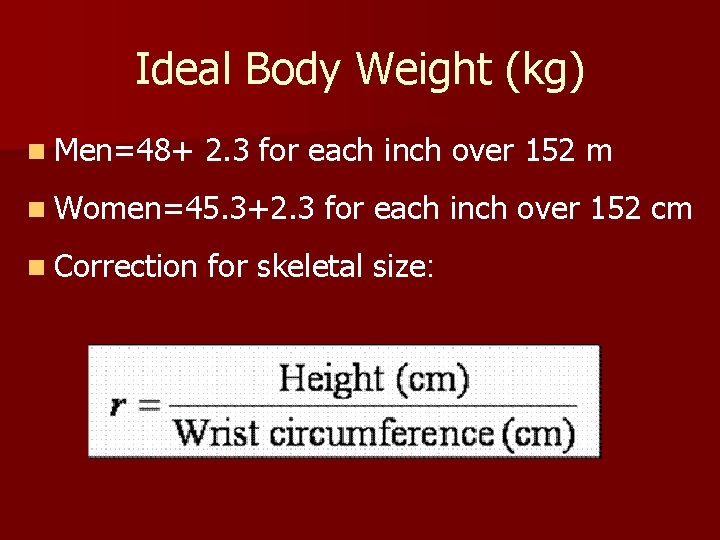
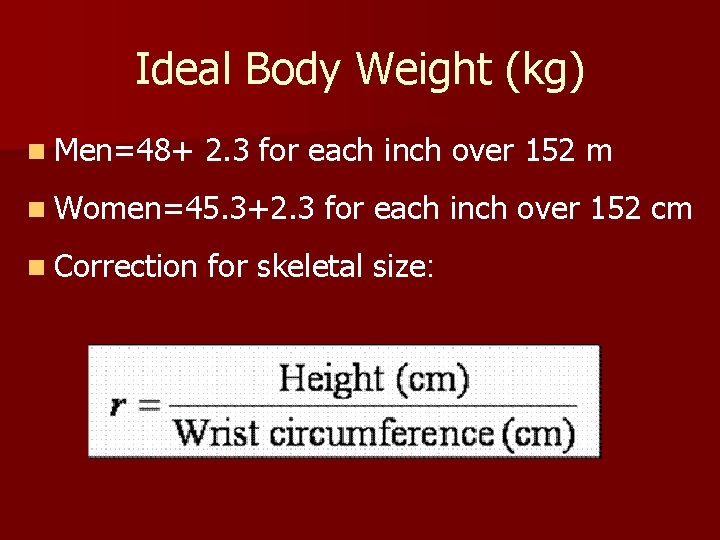
Ideal Body Weight (kg) n Men=48+ 2. 3 for each inch over 152 m n Women=45. 3+2. 3 n Correction for each inch over 152 cm for skeletal size:
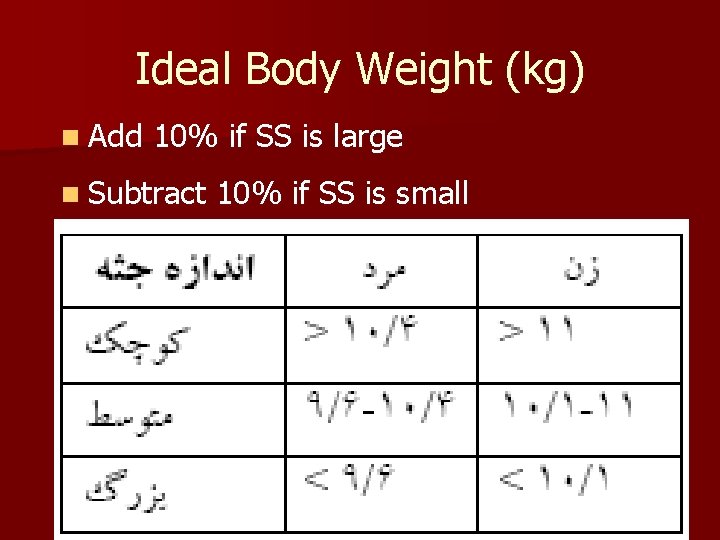
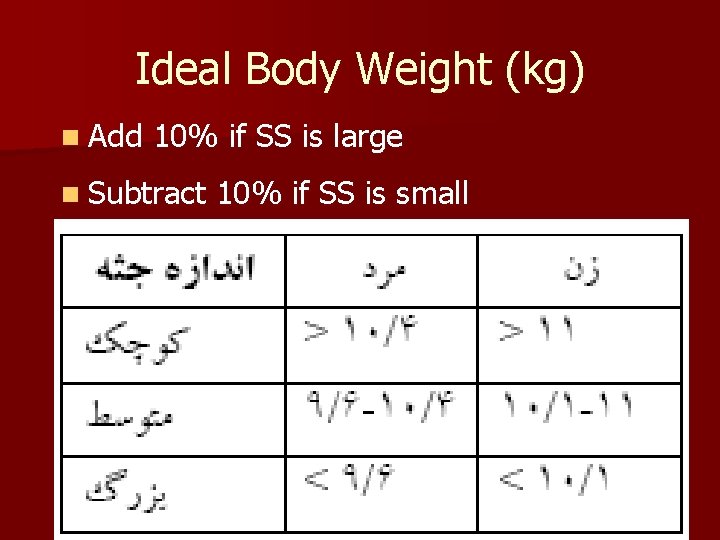
Ideal Body Weight (kg) n Add 10% if SS is large n Subtract 10% if SS is small
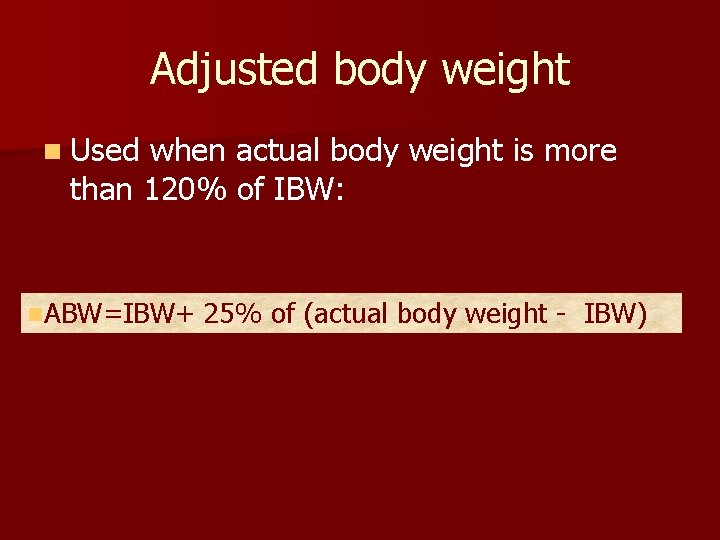
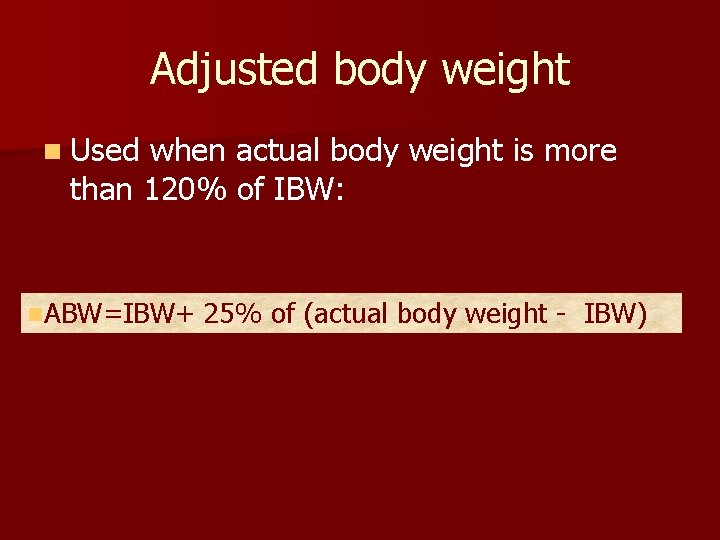
Adjusted body weight n Used when actual body weight is more than 120% of IBW: n. ABW=IBW+ 25% of (actual body weight - IBW)

Height in ICU patients
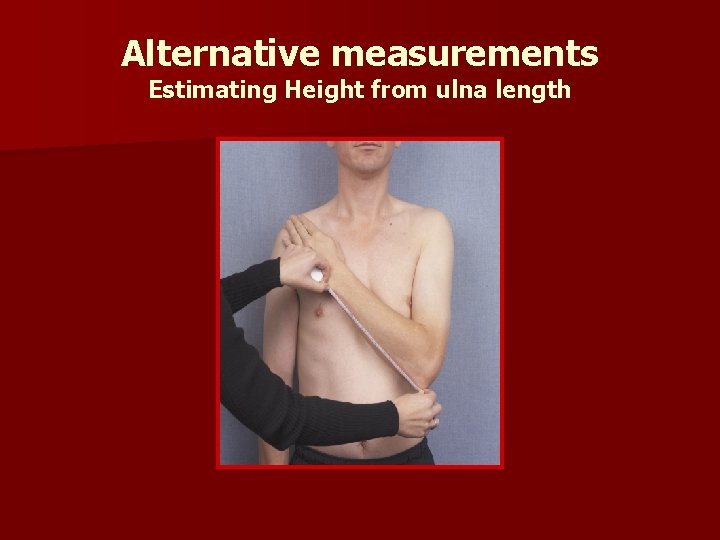
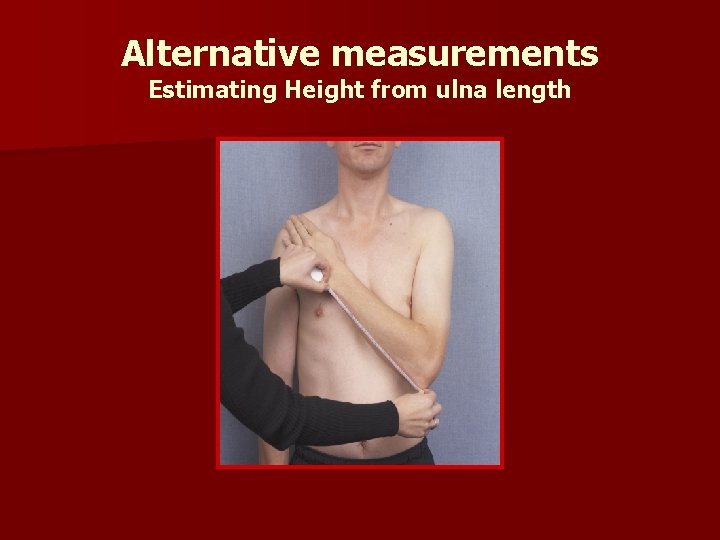
Alternative measurements Estimating Height from ulna length

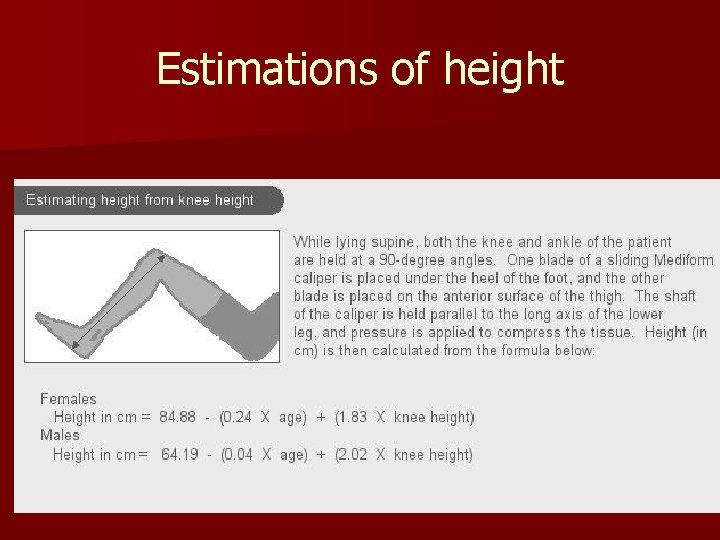
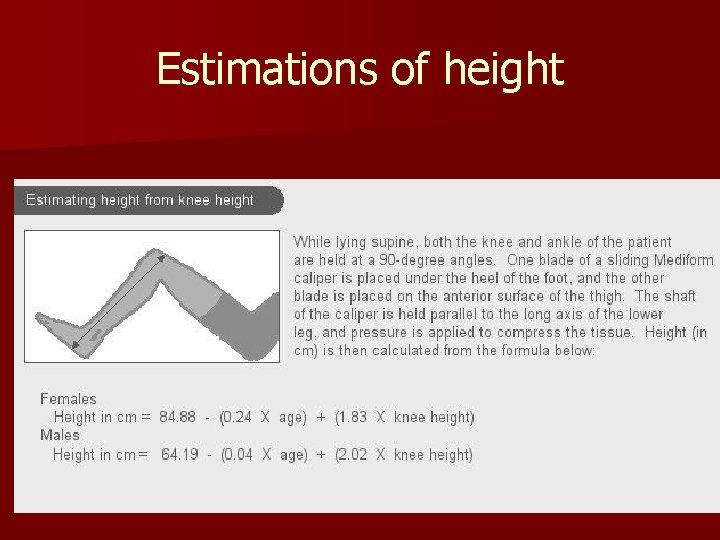
Estimations of height

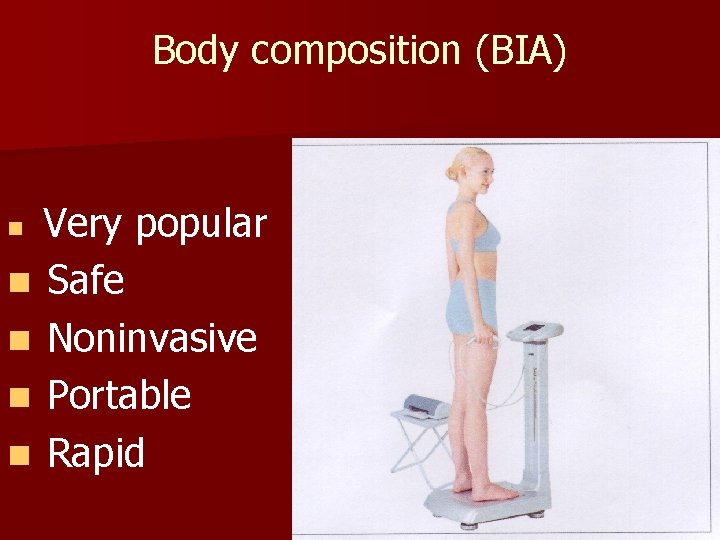
Body composition (BIA) Very popular n Safe n Noninvasive n Portable n Rapid n


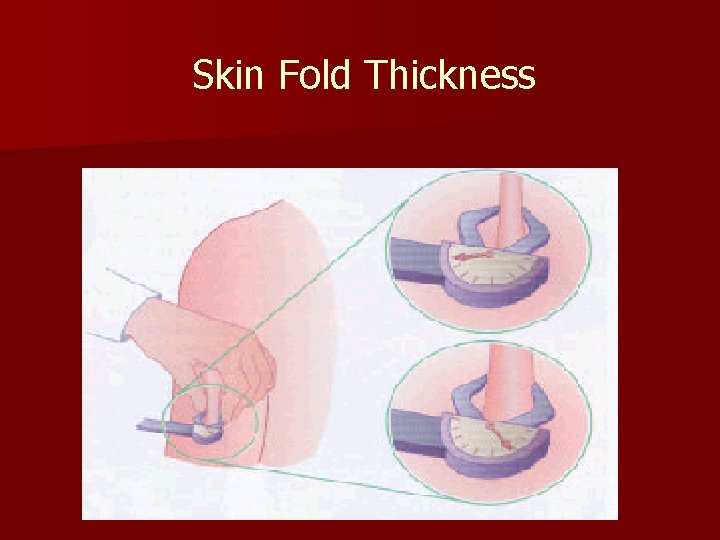
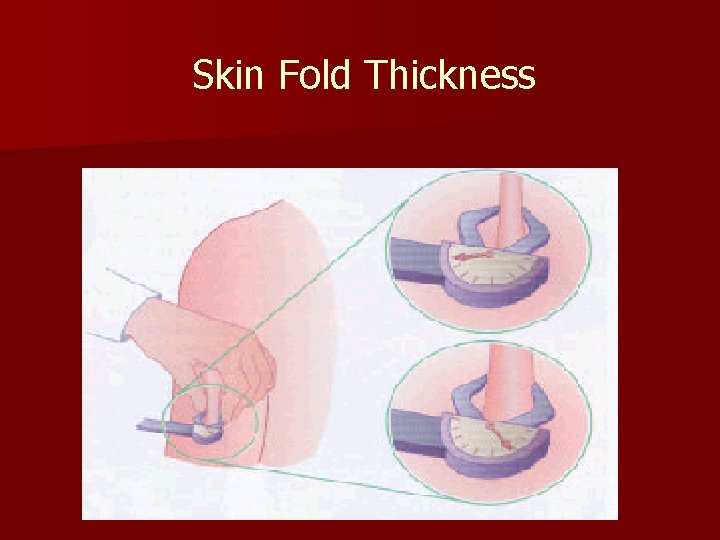
Skin Fold Thickness





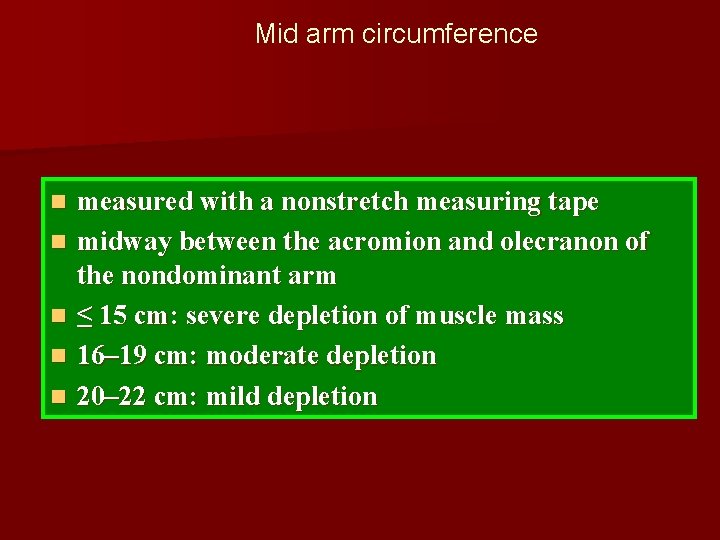
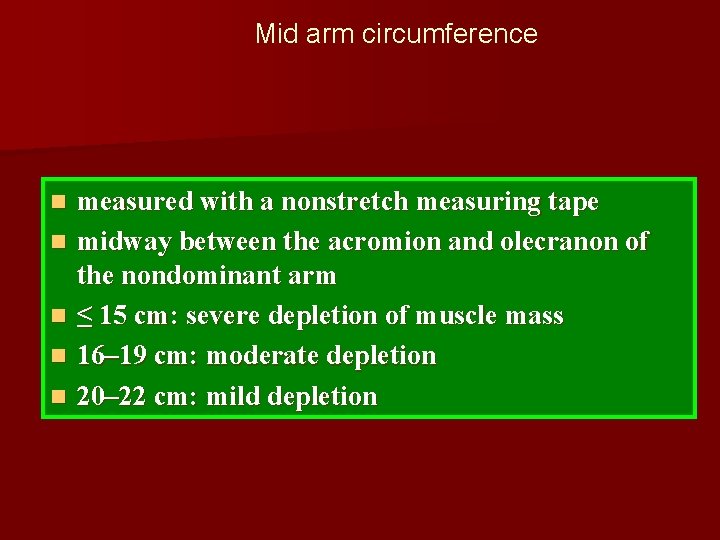
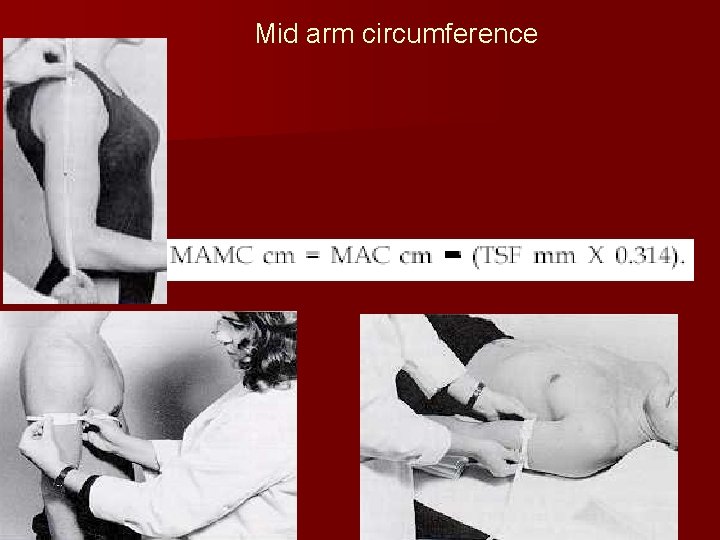
Mid arm circumference n n n measured with a nonstretch measuring tape midway between the acromion and olecranon of the nondominant arm ≤ 15 cm: severe depletion of muscle mass 16– 19 cm: moderate depletion 20– 22 cm: mild depletion
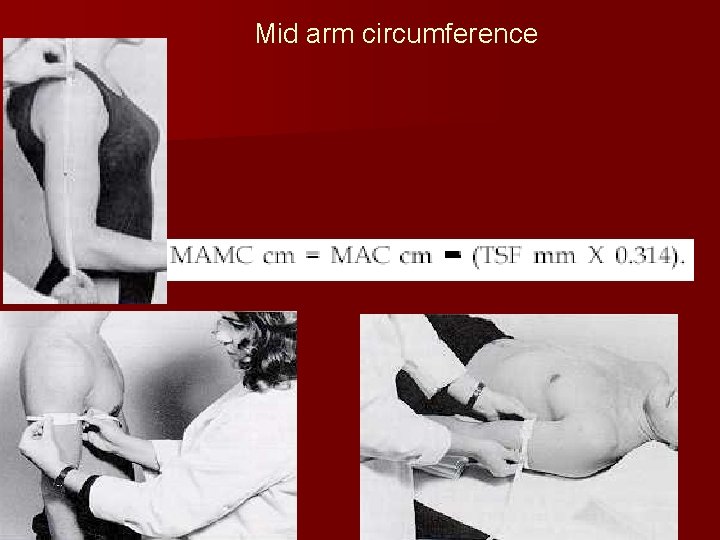
Mid arm circumference
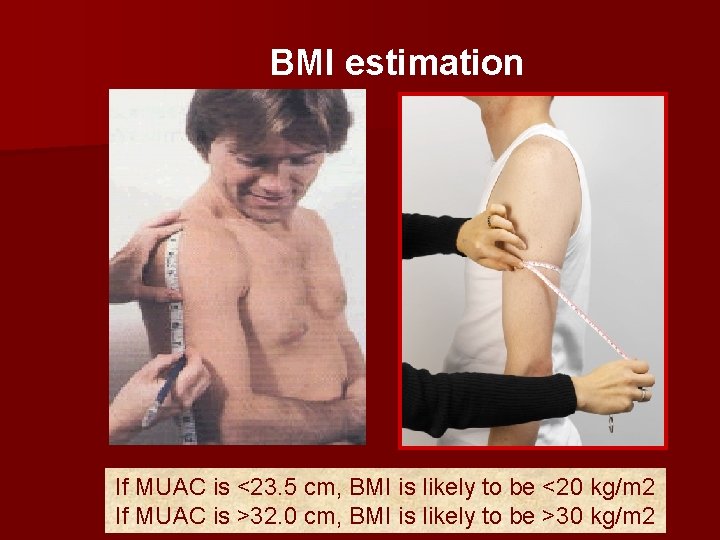
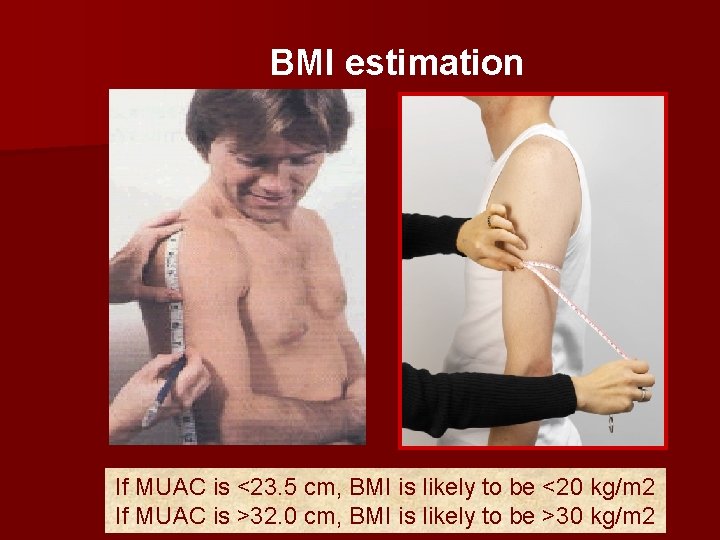
BMI estimation If MUAC is <23. 5 cm, BMI is likely to be <20 kg/m 2 If MUAC is >32. 0 cm, BMI is likely to be >30 kg/m 2
Clinical assessment
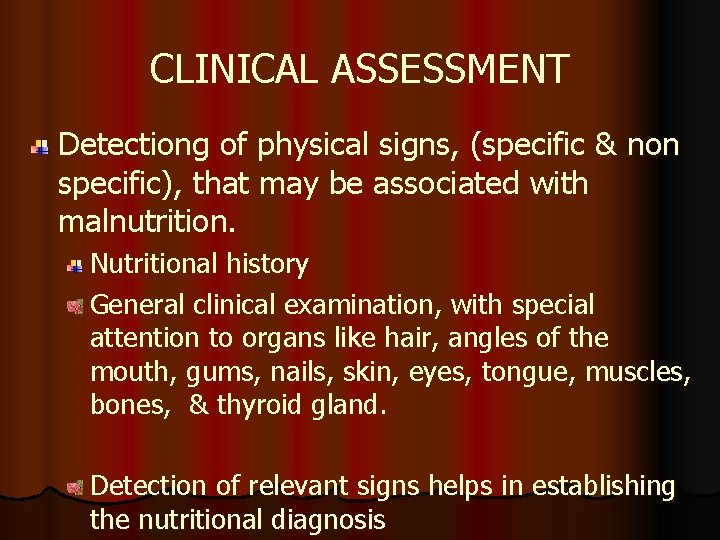
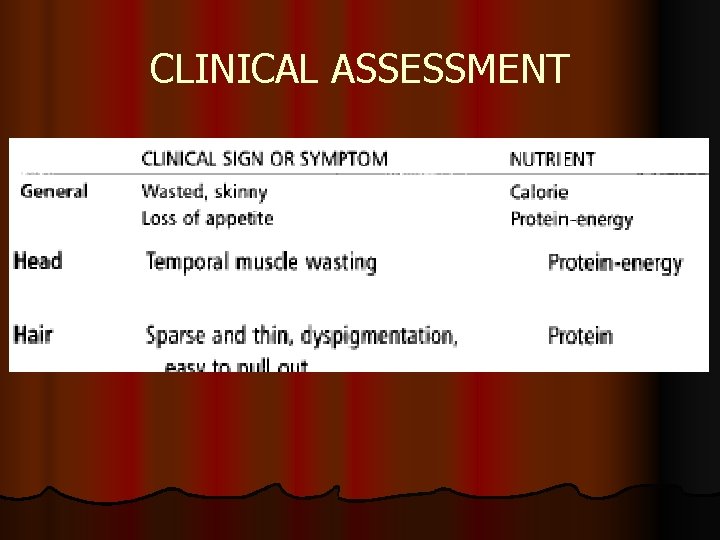
CLINICAL ASSESSMENT Detectiong of physical signs, (specific & non specific), that may be associated with malnutrition. Nutritional history General clinical examination, with special attention to organs like hair, angles of the mouth, gums, nails, skin, eyes, tongue, muscles, bones, & thyroid gland. Detection of relevant signs helps in establishing the nutritional diagnosis
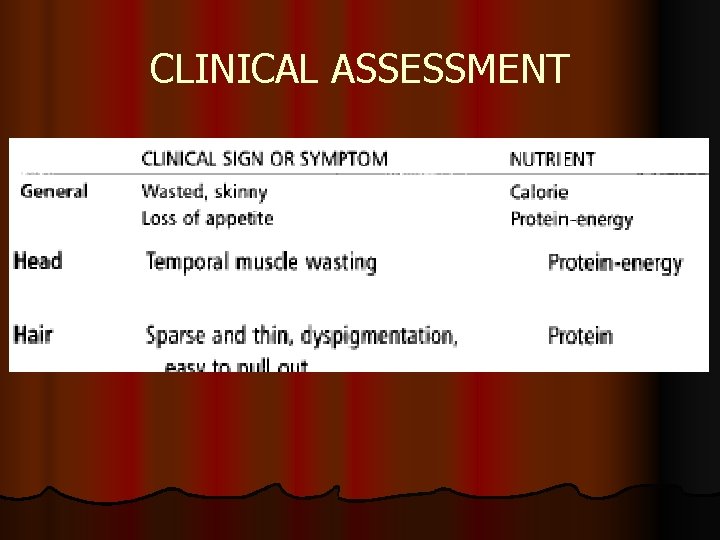
CLINICAL ASSESSMENT

General: muscle wasting


Flaky paint dermatosis: protein deficiency

Essential fatty acid deficiency syndromes (EFADs(


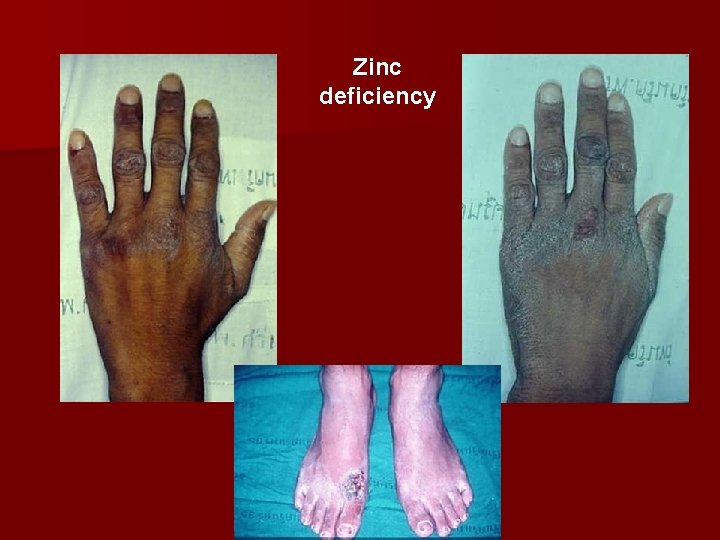
Zinc deficiency
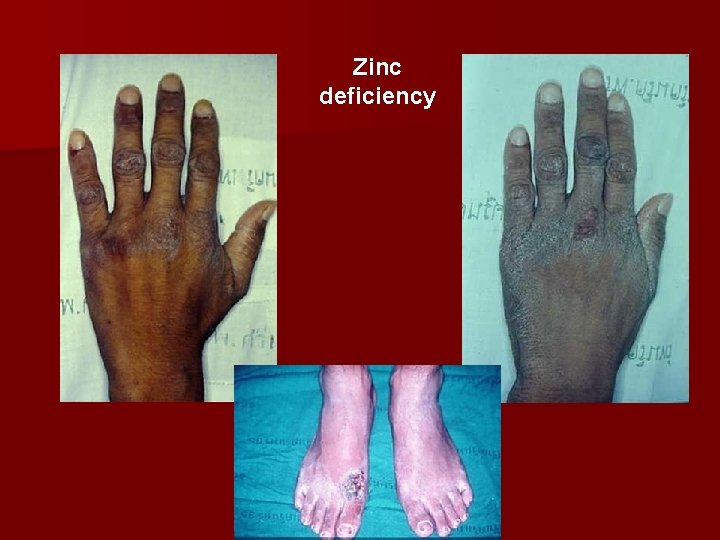
Zinc deficiency



















Wasting Clavicle 59
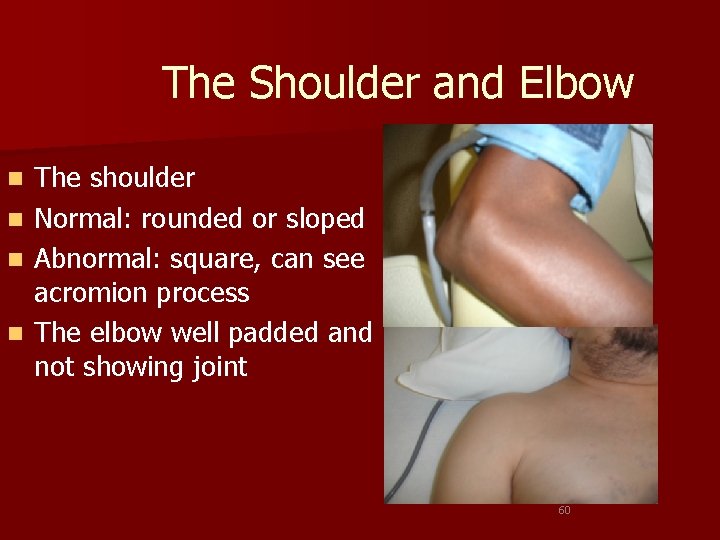
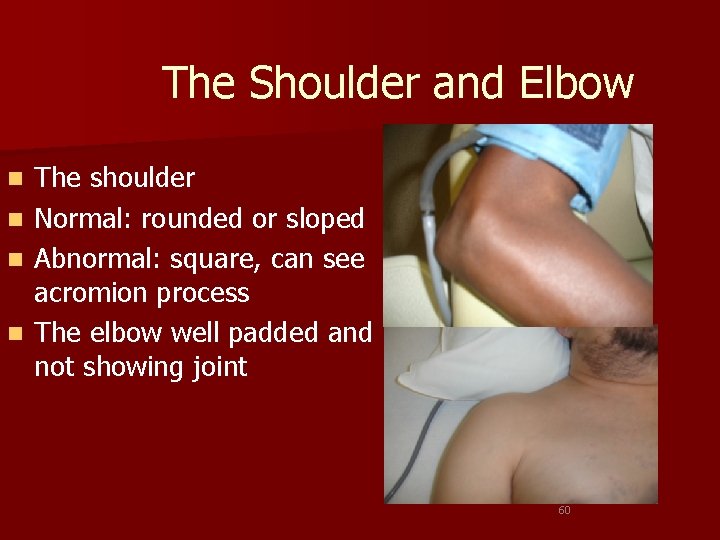
The Shoulder and Elbow n n The shoulder Normal: rounded or sloped Abnormal: square, can see acromion process The elbow well padded and not showing joint 60
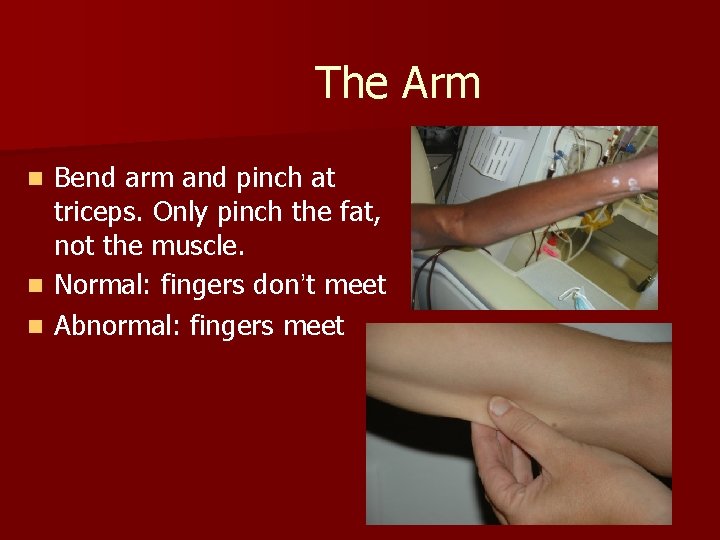
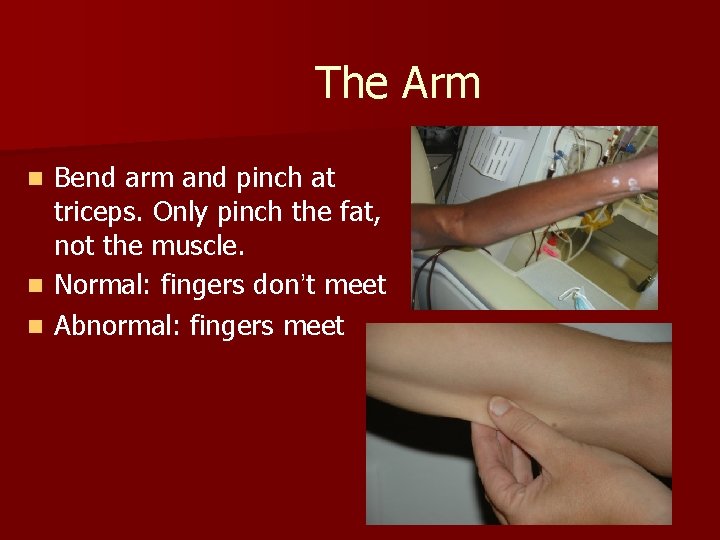
The Arm Bend arm and pinch at triceps. Only pinch the fat, not the muscle. n Normal: fingers don’t meet n Abnormal: fingers meet n 61

The Legs showing muscle wasting 63

Quadriceps and Knees 64
Biochemical, laboratory assessment
The possibilities of biochemical monitoring n On-line monitoring (cardiosurgery – p. H, minerals (K), the electrodes are localized on central cateter, possibility to check parameters on-line. n bed side monitoring (glycaemia, urine /protein, p. H, blood. . /, oximeter O 2 saturation, acidobasis, drugs /dg. strips) n Biochemical analysis
Biochemical parameters n Na, K, Cl, Ca, P, Mg, osmolality - blood, urine n Acidobasis, lactate n urea, creatinin clearence, Nitrogen balance n bilirubine, ALT, AST, LDH, amylase, lipase n cholesterol, triglycerides, glucose – blood, urine
Biochemical parameters n Total protein, albumine, prealbumine n CRP n TSH n Basic analysis are made at the first, must be done within 90 minutes
Other biochemical parameters n Trace elements /Zn, Se. . / n Vitamins n Drugs /methotrexate, antiepileptics, antibiotics. . . / n Aminogram /glutamin. . / n Interleucins, TNF… n Hormones /cortisol, glucagone, adrenaline. . /.
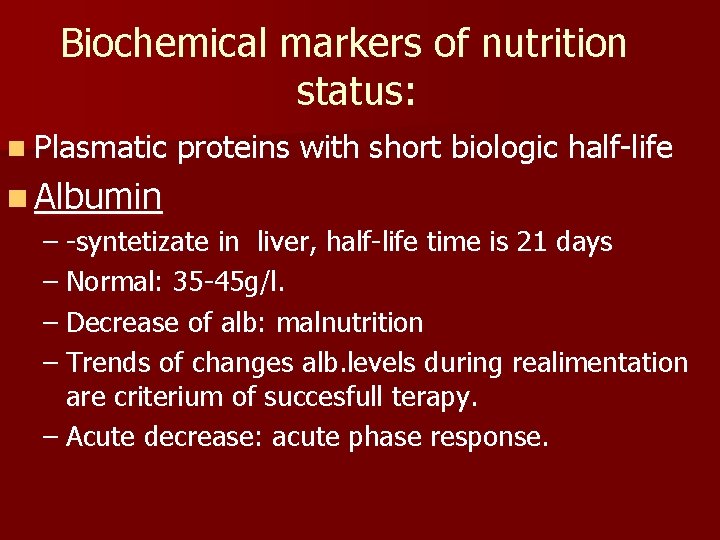
Biochemical markers of nutrition status: n Plasmatic proteins with short biologic half-life n Albumin – -syntetizate in liver, half-life time is 21 days – Normal: 35 -45 g/l. – Decrease of alb: malnutrition – Trends of changes alb. levels during realimentation are criterium of succesfull terapy. – Acute decrease: acute phase response.
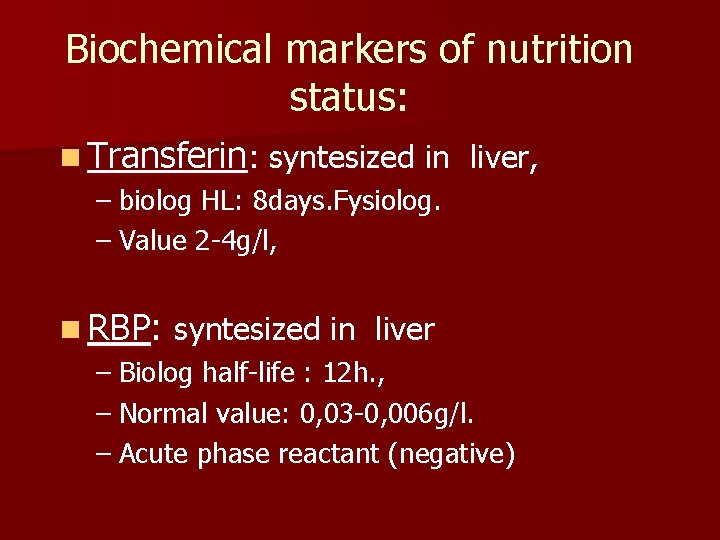
Biochemical markers of nutrition status: n Transferin: syntesized in liver, – biolog HL: 8 days. Fysiolog. – Value 2 -4 g/l, n RBP: syntesized in liver – Biolog half-life : 12 h. , – Normal value: 0, 03 -0, 006 g/l. – Acute phase reactant (negative)
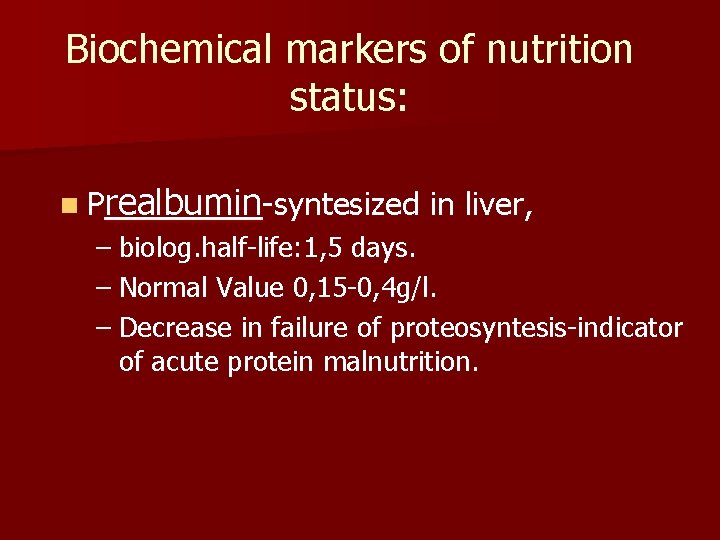
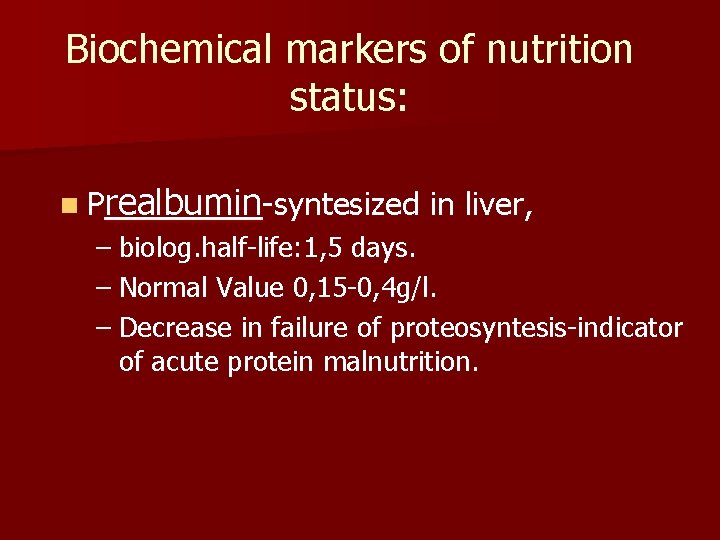
Biochemical markers of nutrition status: n Prealbumin-syntesized in liver, – biolog. half-life: 1, 5 days. – Normal Value 0, 15 -0, 4 g/l. – Decrease in failure of proteosyntesis-indicator of acute protein malnutrition.
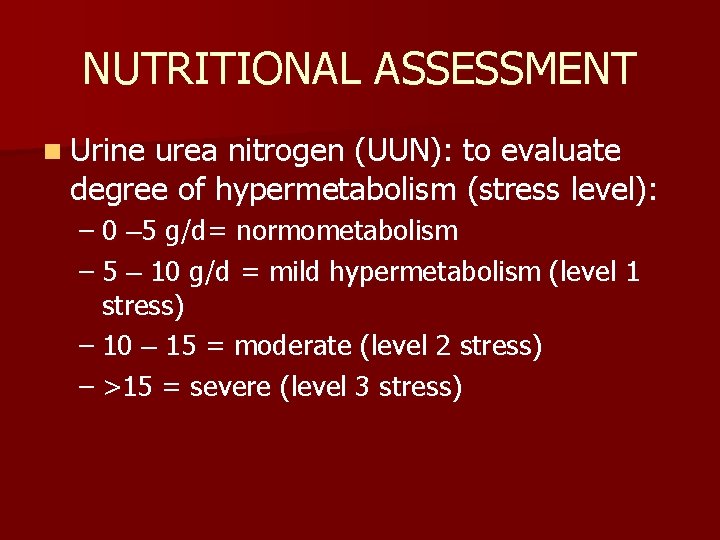
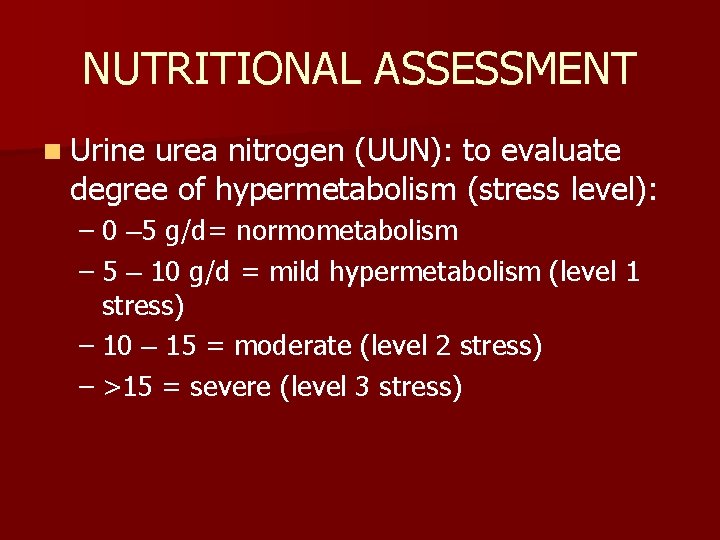
NUTRITIONAL ASSESSMENT n Urine urea nitrogen (UUN): to evaluate degree of hypermetabolism (stress level): – 0 – 5 g/d= normometabolism – 5 – 10 g/d = mild hypermetabolism (level 1 stress) – 10 – 15 = moderate (level 2 stress) – >15 = severe (level 3 stress)

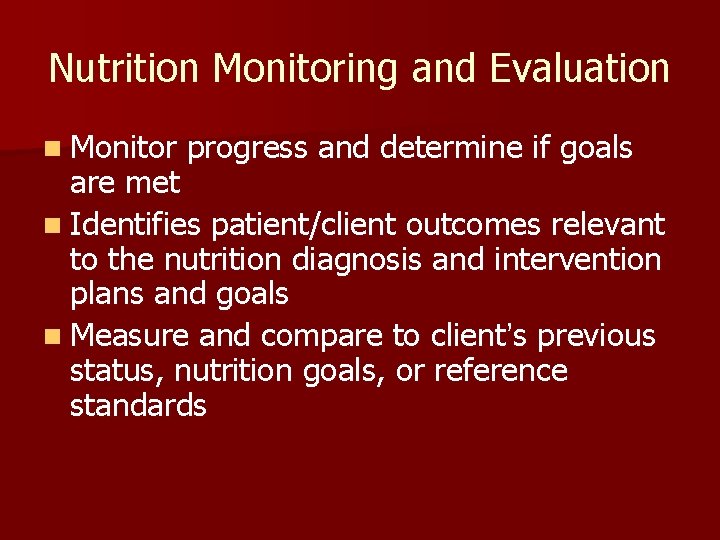
Nutrition Monitoring and Evaluation n Monitor progress and determine if goals are met n Identifies patient/client outcomes relevant to the nutrition diagnosis and intervention plans and goals n Measure and compare to client’s previous status, nutrition goals, or reference standards
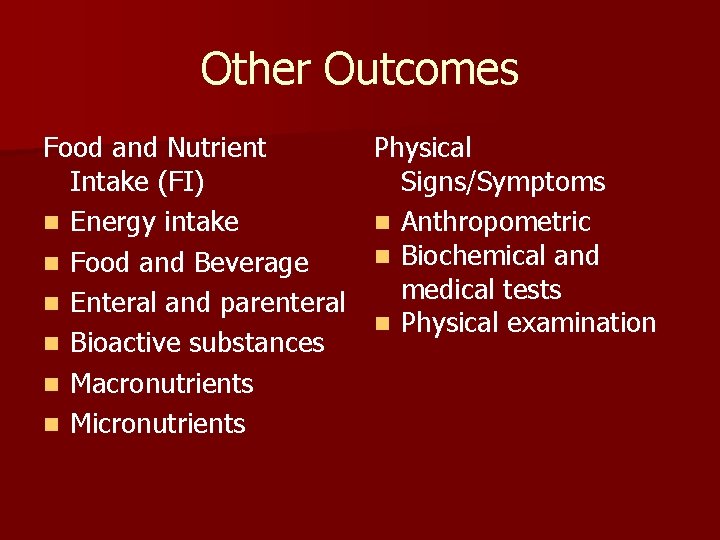
Other Outcomes Food and Nutrient Intake (FI) n Energy intake n Food and Beverage n Enteral and parenteral n Bioactive substances n Macronutrients n Micronutrients Physical Signs/Symptoms n Anthropometric n Biochemical and medical tests n Physical examination

Monitoring
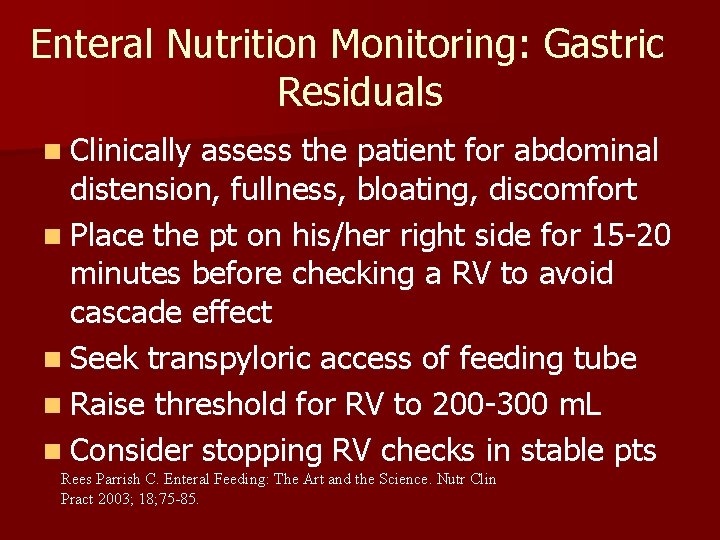
Enteral Nutrition Monitoring: Gastric Residuals n Clinically assess the patient for abdominal distension, fullness, bloating, discomfort n Place the pt on his/her right side for 15 -20 minutes before checking a RV to avoid cascade effect n Seek transpyloric access of feeding tube n Raise threshold for RV to 200 -300 m. L n Consider stopping RV checks in stable pts Rees Parrish C. Enteral Feeding: The Art and the Science. Nutr Clin Pract 2003; 18; 75 -85.
Some Lab tests
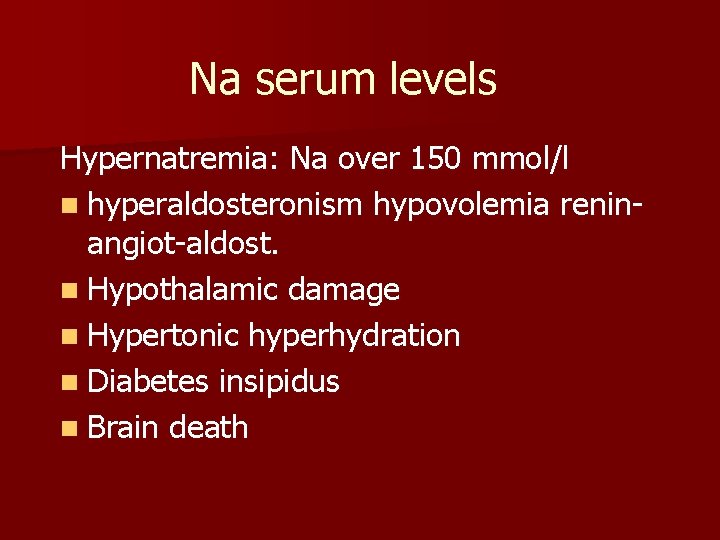
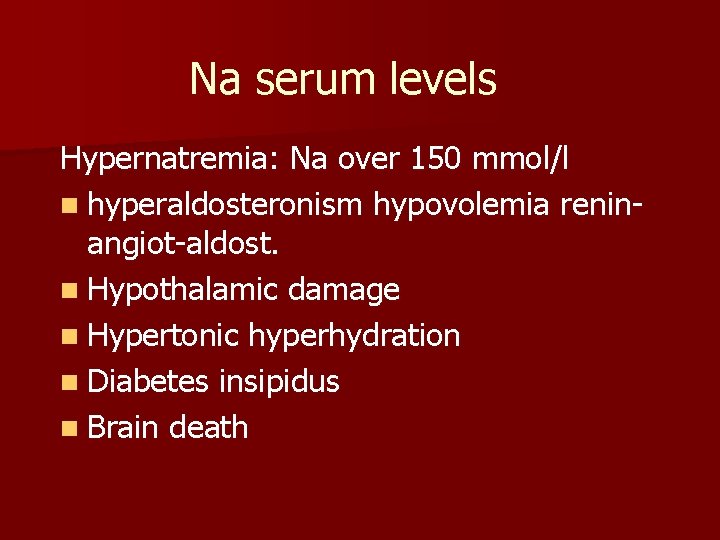
Na serum levels Hypernatremia: Na over 150 mmol/l n hyperaldosteronism hypovolemia reninangiot-aldost. n Hypothalamic damage n Hypertonic hyperhydration n Diabetes insipidus n Brain death
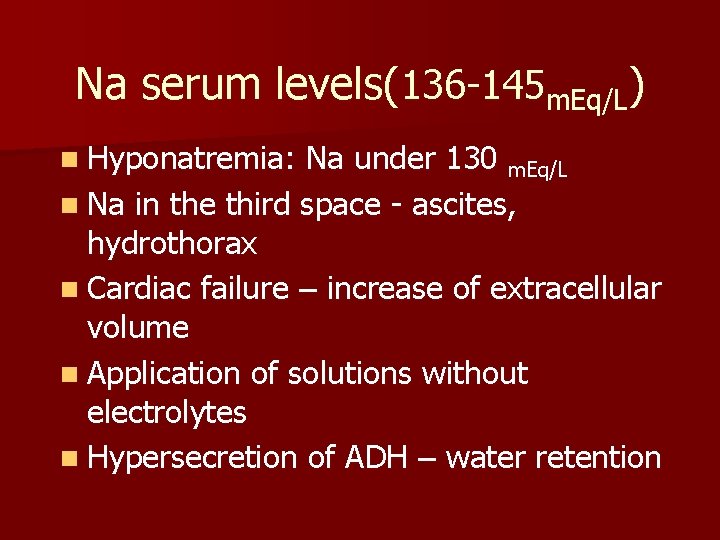
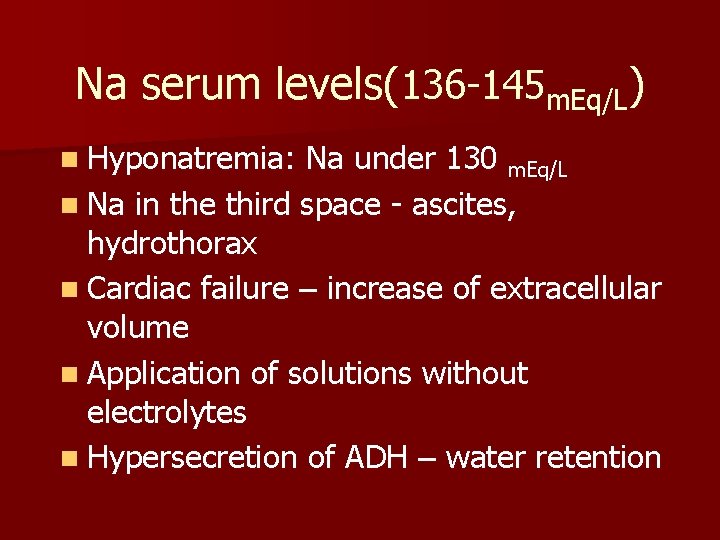
Na serum levels(136 -145 m. Eq/L) n Hyponatremia: Na under 130 m. Eq/L n Na in the third space - ascites, hydrothorax n Cardiac failure – increase of extracellular volume n Application of solutions without electrolytes n Hypersecretion of ADH – water retention
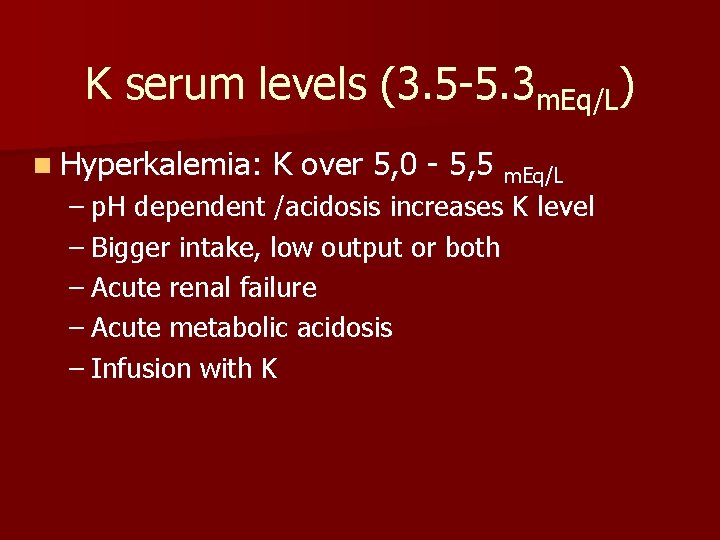
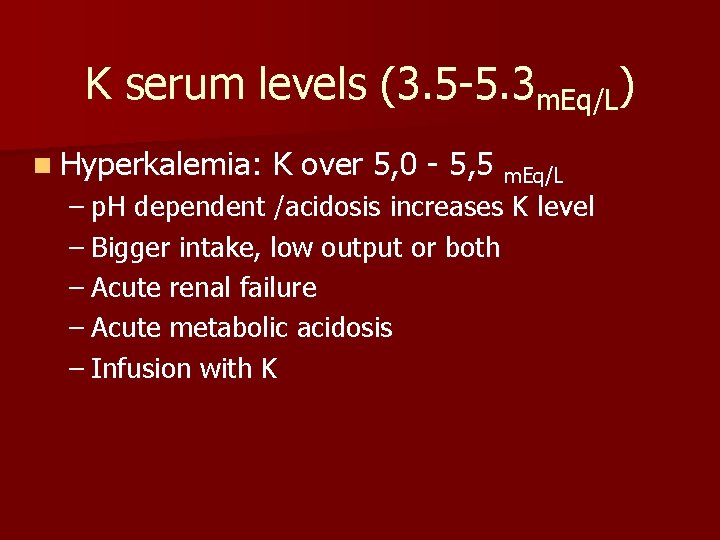
K serum levels (3. 5 -5. 3 m. Eq/L) n Hyperkalemia: K over 5, 0 - 5, 5 m. Eq/L – p. H dependent /acidosis increases K level – Bigger intake, low output or both – Acute renal failure – Acute metabolic acidosis – Infusion with K
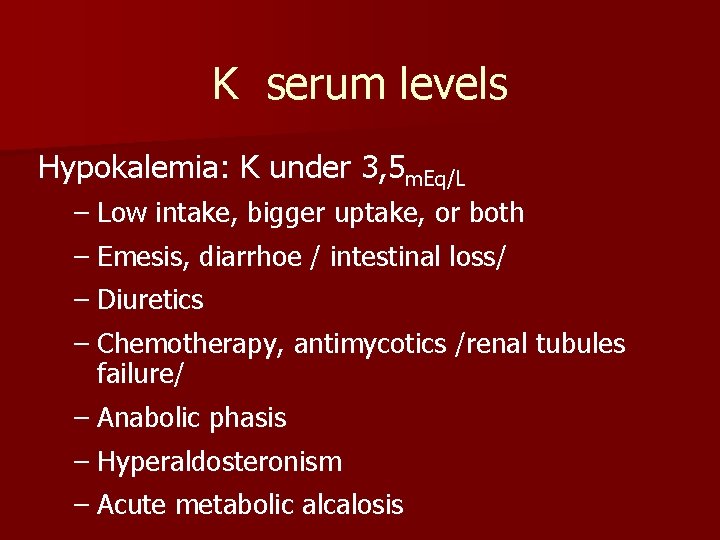
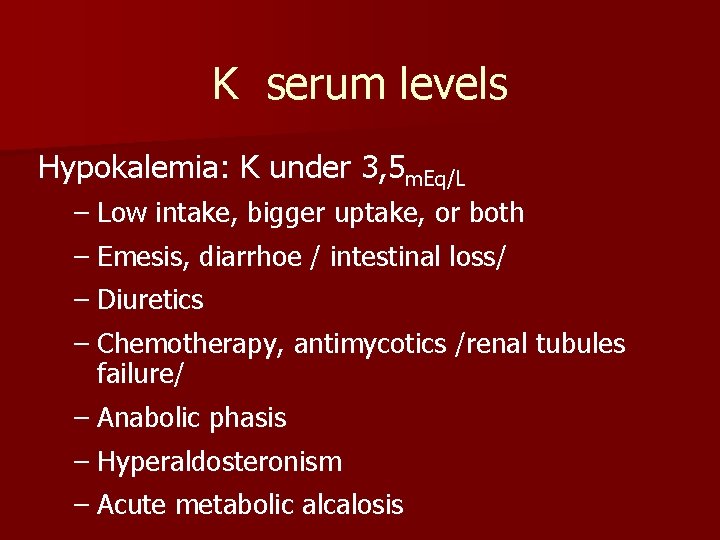
K serum levels Hypokalemia: K under 3, 5 m. Eq/L – Low intake, bigger uptake, or both – Emesis, diarrhoe / intestinal loss/ – Diuretics – Chemotherapy, antimycotics /renal tubules failure/ – Anabolic phasis – Hyperaldosteronism – Acute metabolic alcalosis
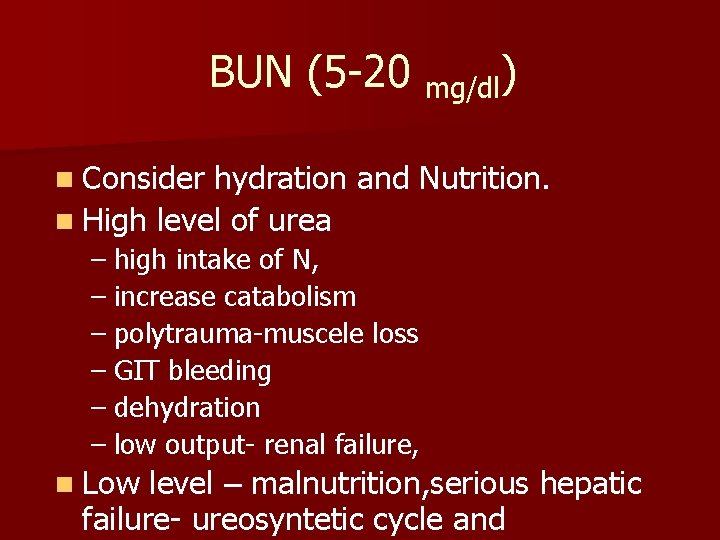
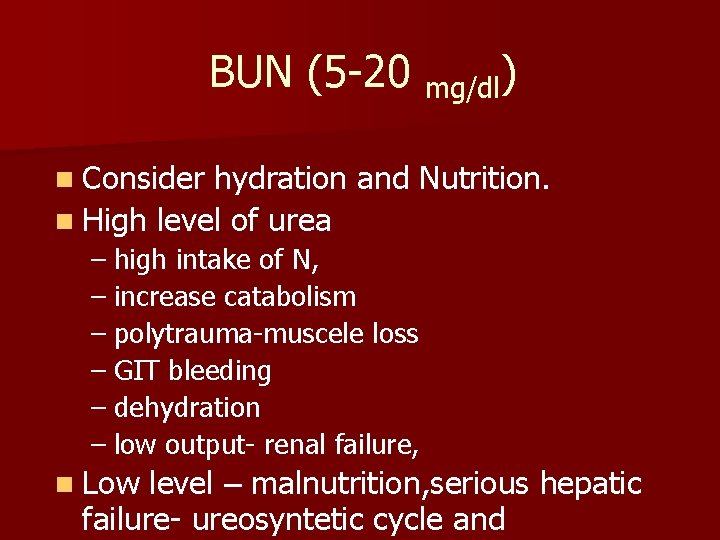
BUN (5 -20 mg/dl) n Consider hydration and Nutrition. n High level of urea – high intake of N, – increase catabolism – polytrauma-muscele loss – GIT bleeding – dehydration – low output- renal failure, n Low level – malnutrition, serious hepatic failure- ureosyntetic cycle and
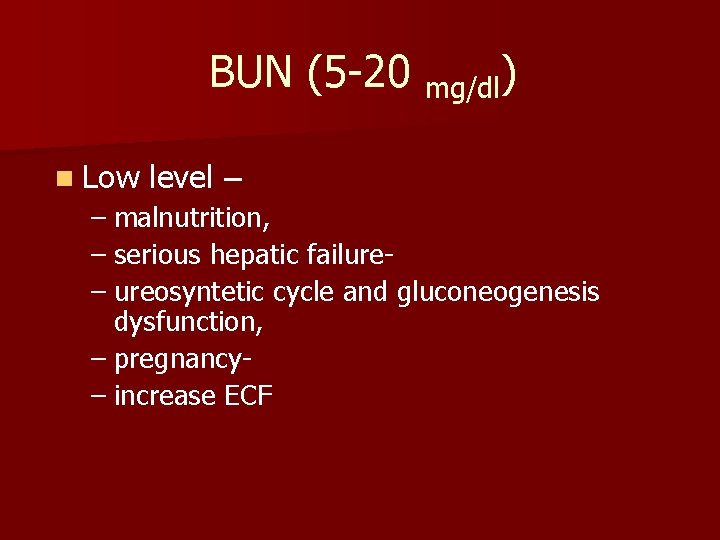
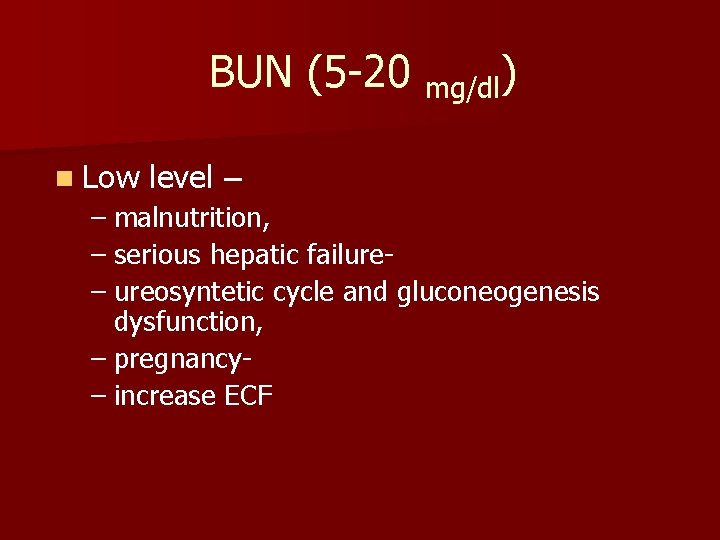
BUN (5 -20 mg/dl) n Low level – – malnutrition, – serious hepatic failure– ureosyntetic cycle and gluconeogenesis dysfunction, – pregnancy– increase ECF
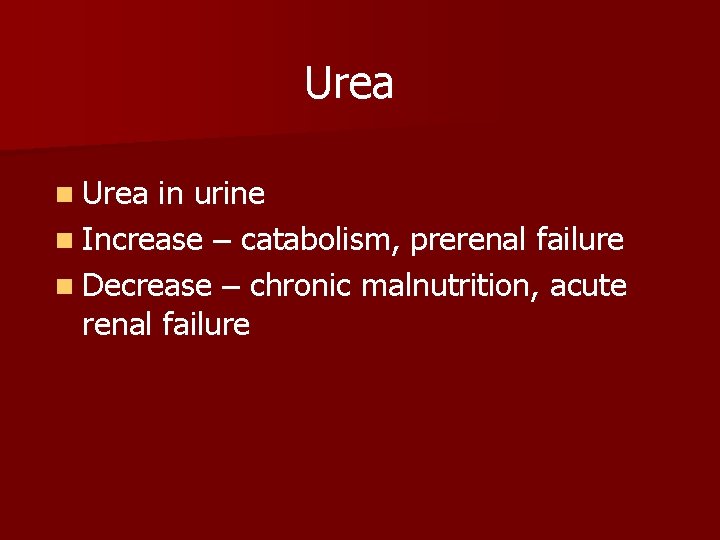
Urea n Urea in urine n Increase – catabolism, prerenal failure n Decrease – chronic malnutrition, acute renal failure
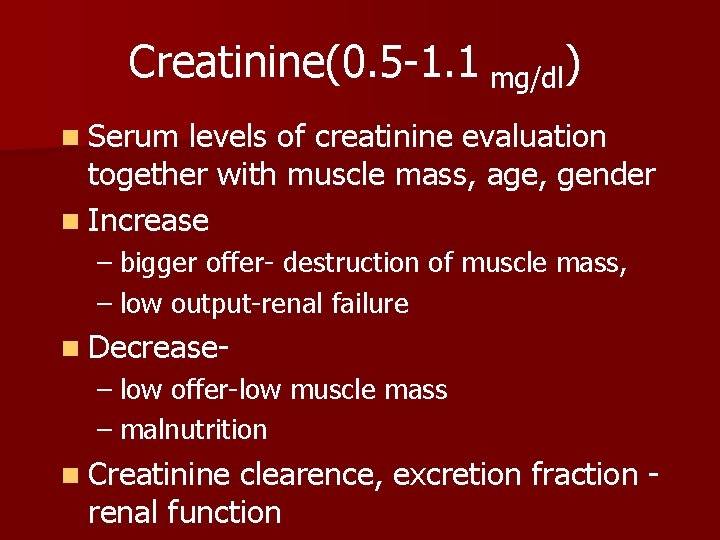
Creatinine(0. 5 -1. 1 mg/dl) n Serum levels of creatinine evaluation together with muscle mass, age, gender n Increase – bigger offer- destruction of muscle mass, – low output-renal failure n Decrease- – low offer-low muscle mass – malnutrition n Creatinine clearence, excretion fraction renal function
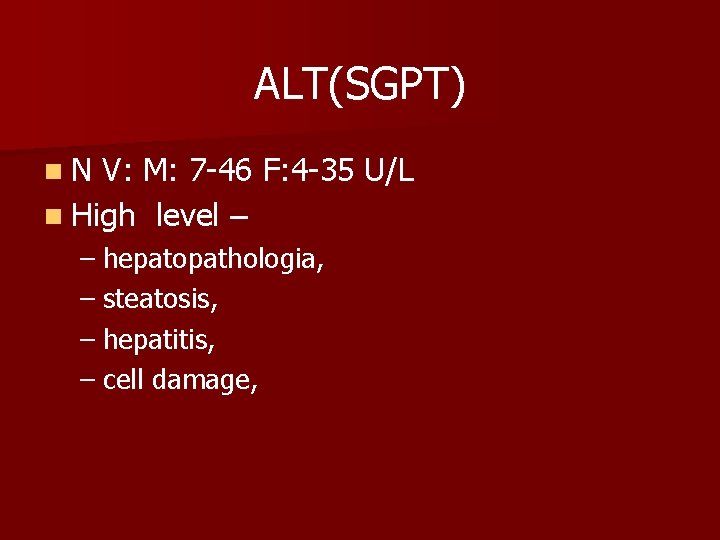
ALT(SGPT) n. N V: M: 7 -46 F: 4 -35 U/L n High level – – hepatopathologia, – steatosis, – hepatitis, – cell damage,
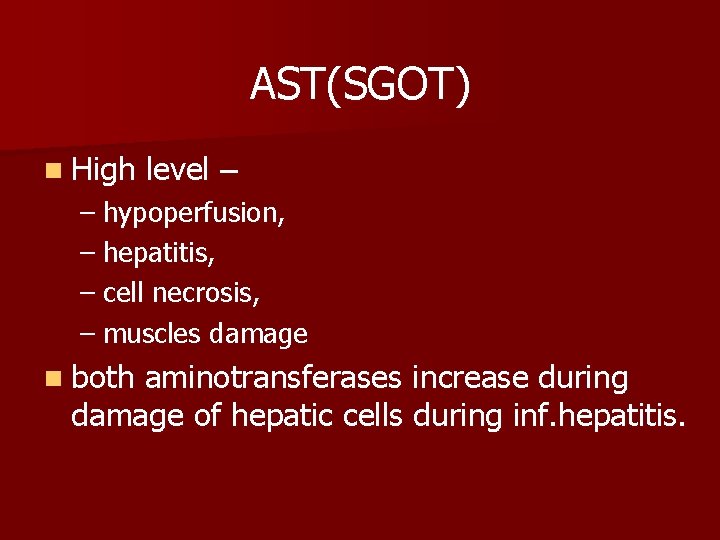
AST(SGOT) n High level – – hypoperfusion, – hepatitis, – cell necrosis, – muscles damage n both aminotransferases increase during damage of hepatic cells during inf. hepatitis.
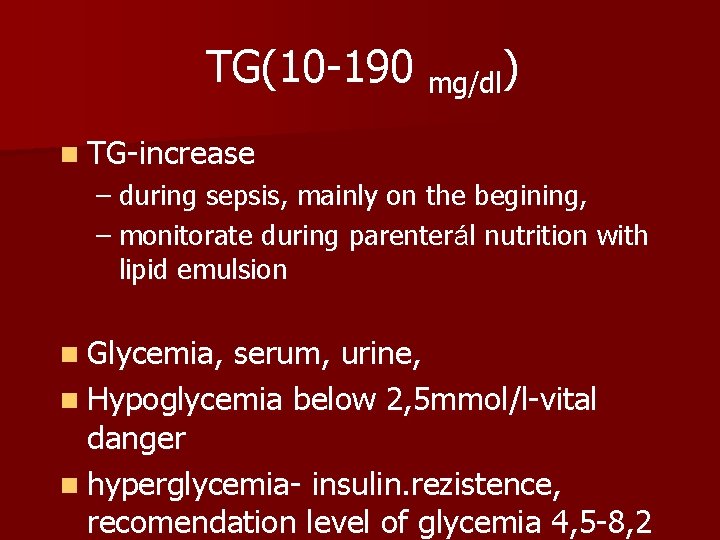
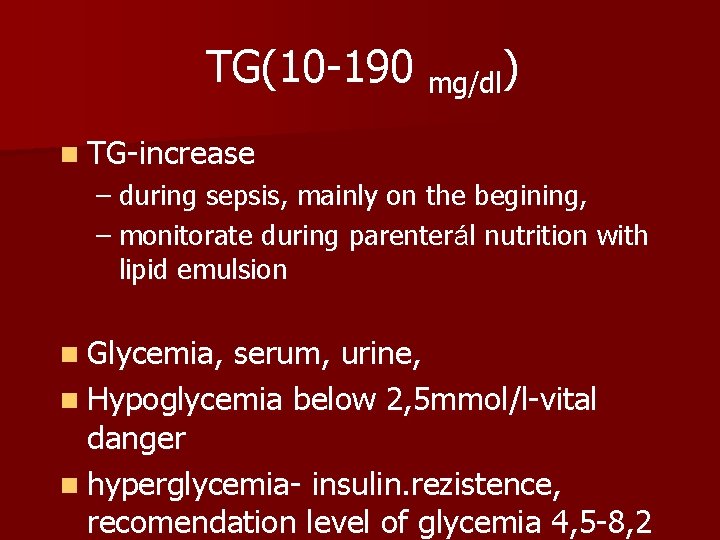
TG(10 -190 mg/dl) n TG-increase – during sepsis, mainly on the begining, – monitorate during parenterál nutrition with lipid emulsion n Glycemia, serum, urine, n Hypoglycemia below 2, 5 mmol/l-vital danger n hyperglycemia- insulin. rezistence, recomendation level of glycemia 4, 5 -8, 2
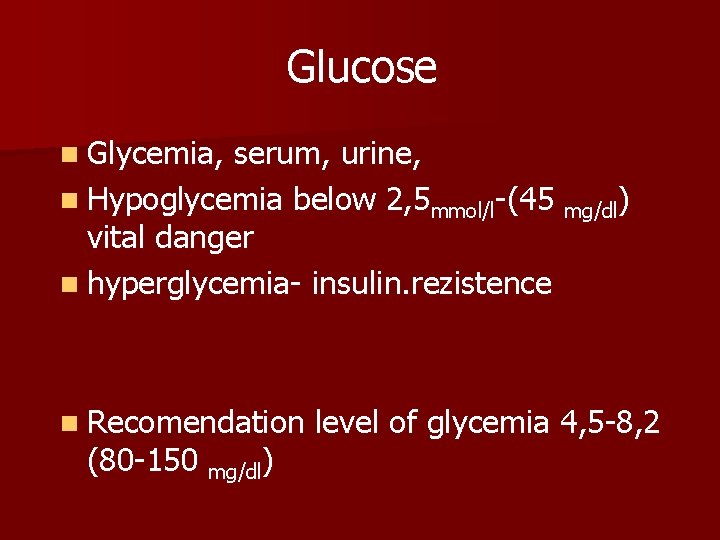
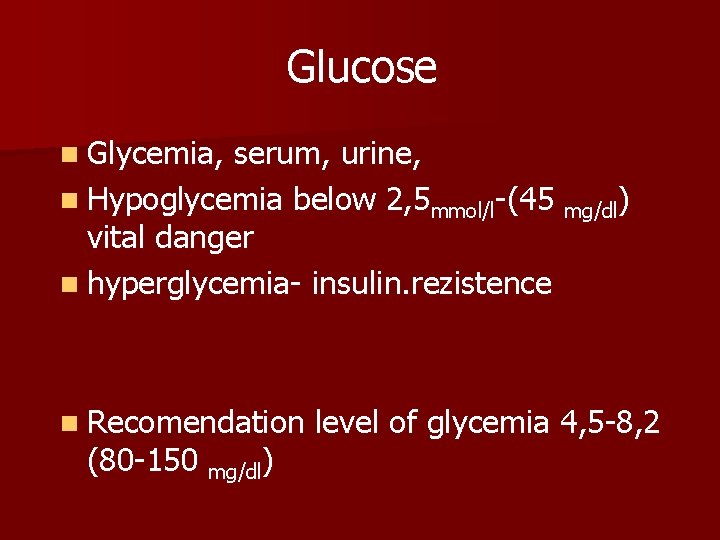
Glucose n Glycemia, serum, urine, n Hypoglycemia below 2, 5 mmol/l-(45 mg/dl) vital danger n hyperglycemia- insulin. rezistence n Recomendation (80 -150 mg/dl) level of glycemia 4, 5 -8, 2
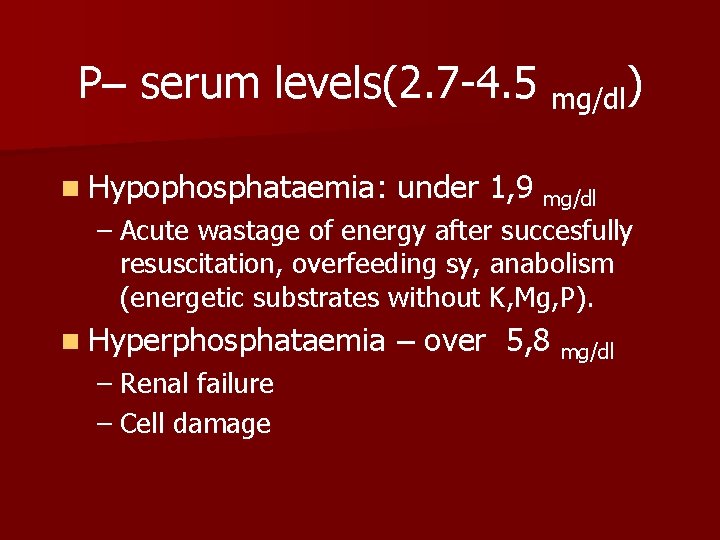
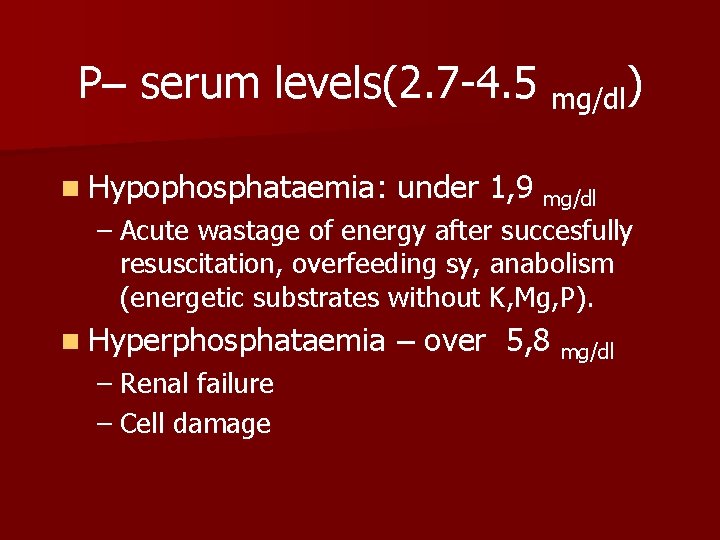
P– serum levels(2. 7 -4. 5 mg/dl) n Hypophosphataemia: under 1, 9 mg/dl – Acute wastage of energy after succesfully resuscitation, overfeeding sy, anabolism (energetic substrates without K, Mg, P). n Hyperphosphataemia – Renal failure – Cell damage – over 5, 8 mg/dl
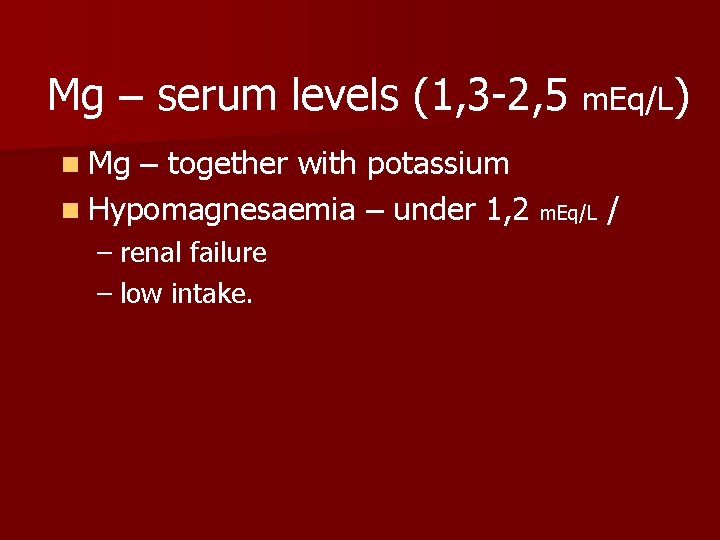
Mg – serum levels (1, 3 -2, 5 m. Eq/L) n Mg – together with potassium n Hypomagnesaemia – under 1, 2 m. Eq/L / – renal failure – low intake.
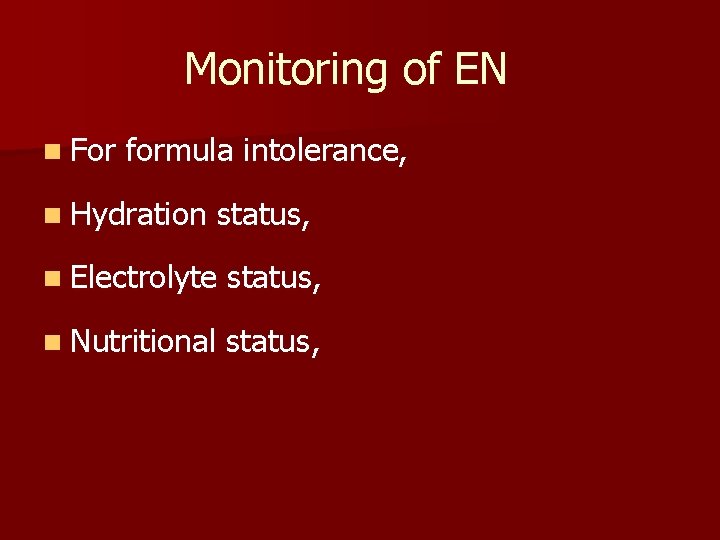
Monitoring of EN n For formula intolerance, n Hydration status, n Electrolyte status, n Nutritional status,
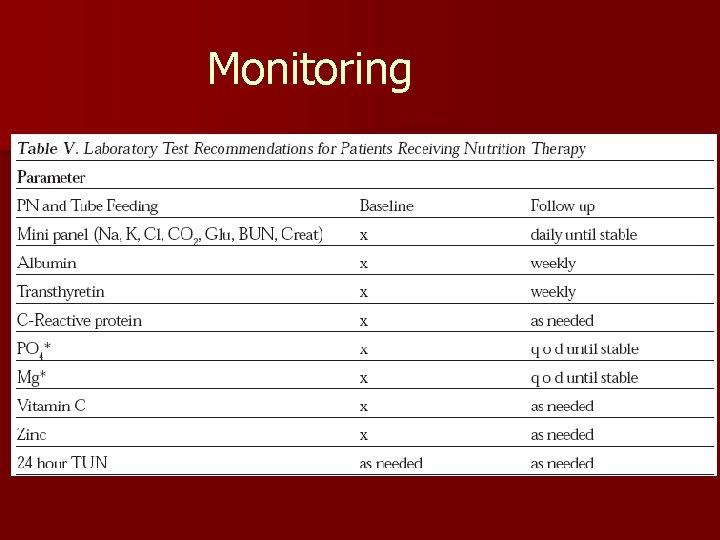
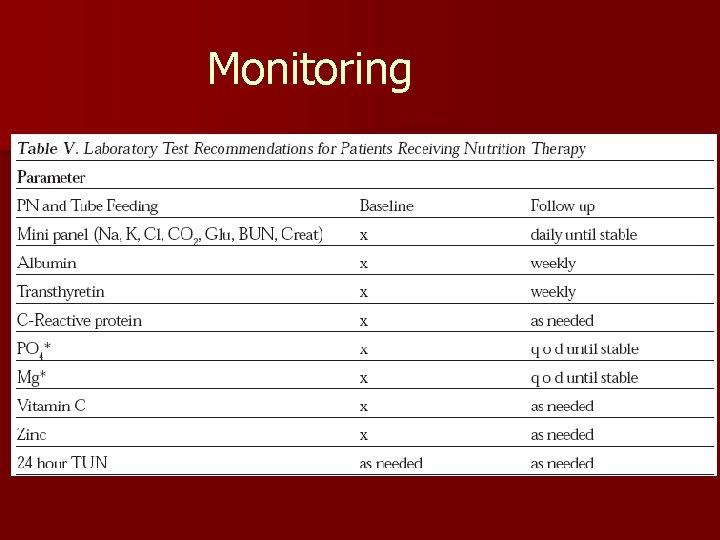
Monitoring










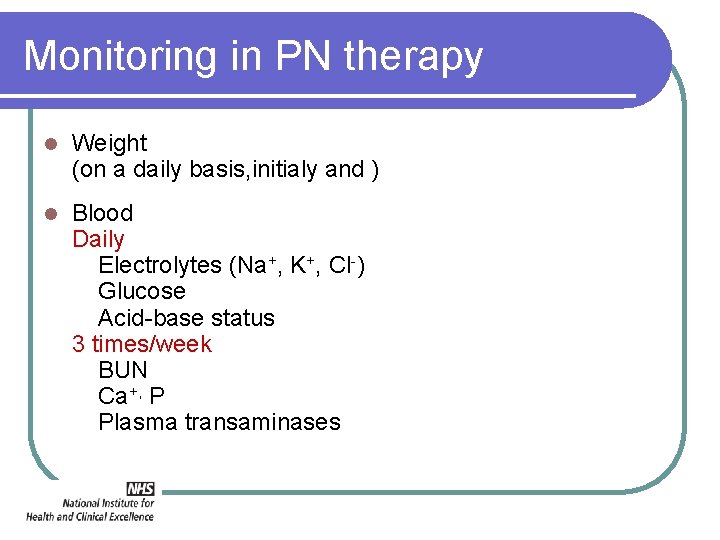
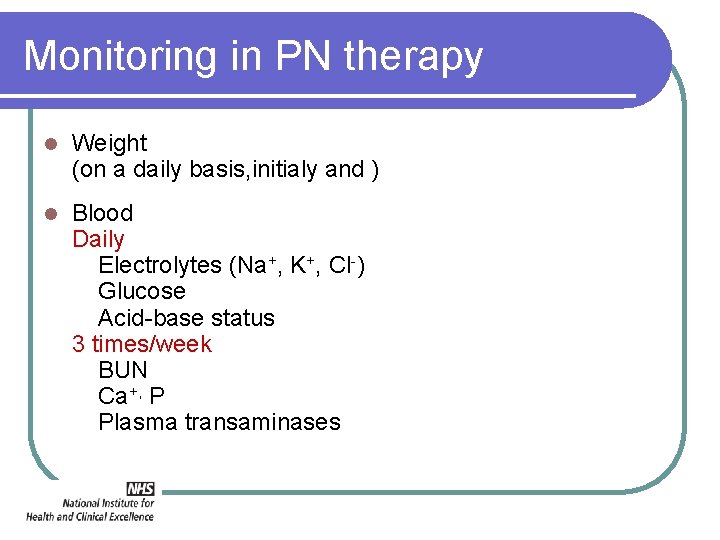
Monitoring in PN therapy l Weight (on a daily basis, initialy and ) l Blood Daily Electrolytes (Na+, K+, Cl-) Glucose Acid-base status 3 times/week BUN Ca+, P Plasma transaminases
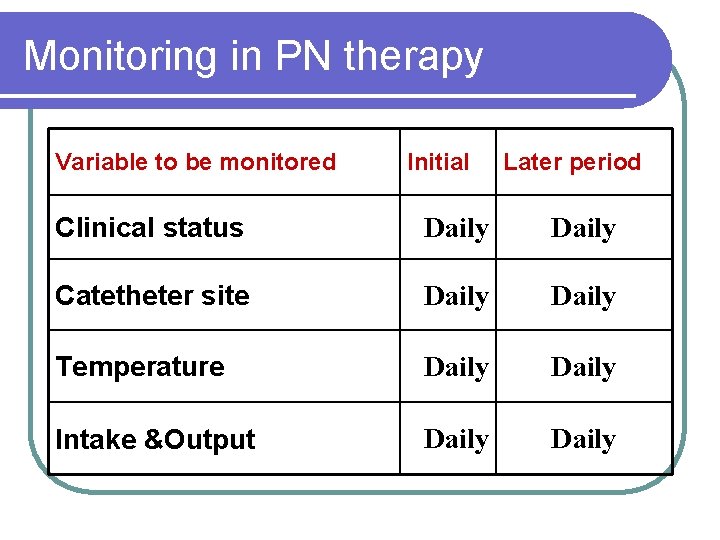
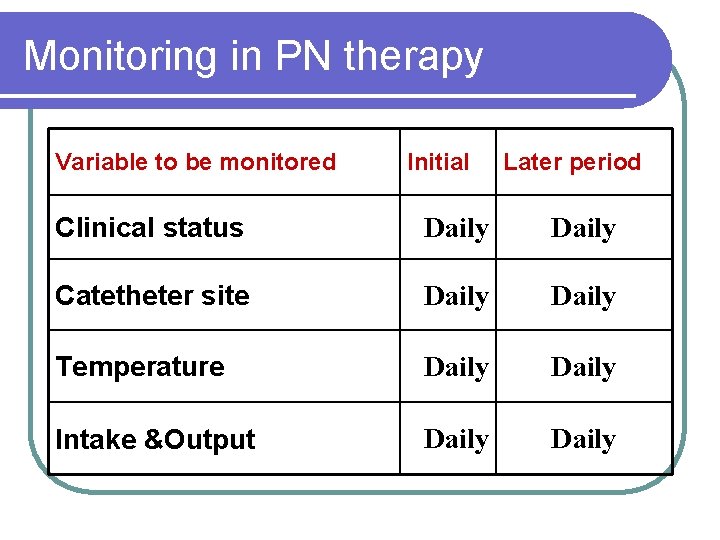
Monitoring in PN therapy Variable to be monitored Initial Later period Clinical status Daily Catetheter site Daily Temperature Daily Intake &Output Daily
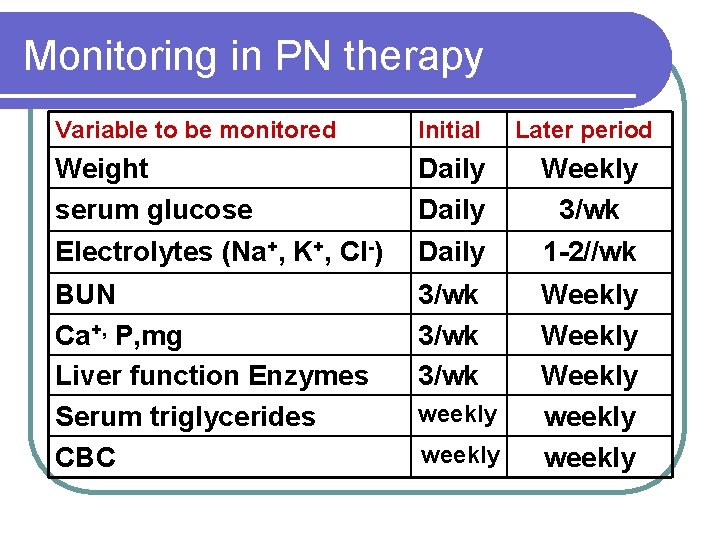
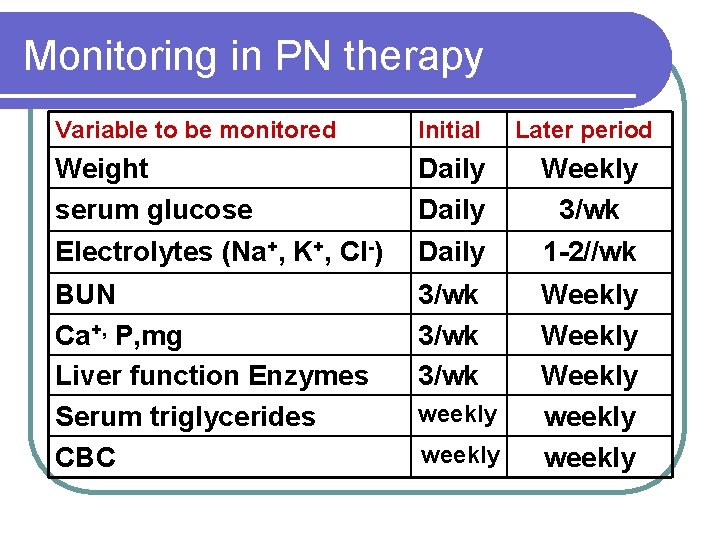
Monitoring in PN therapy Variable to be monitored Initial Later period Weight serum glucose Daily Weekly 3/wk Electrolytes (Na+, K+, Cl-) Daily 1 -2//wk BUN Ca+, P, mg Liver function Enzymes Serum triglycerides CBC 3/wk Weekly weekly
Problems 1. Catheter sepsis 2. Placement problems 3. Metabolic complications
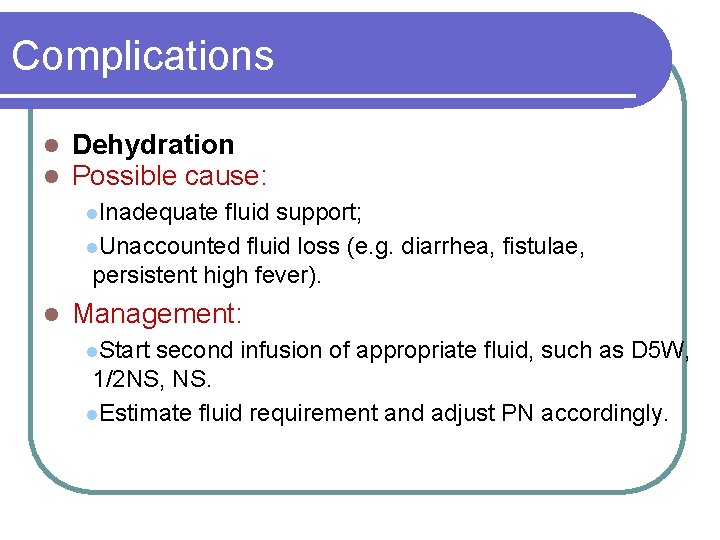
Complications l l Dehydration Possible cause: l. Inadequate fluid support; l. Unaccounted fluid loss (e. g. diarrhea, fistulae, persistent high fever). l Management: l. Start second infusion of appropriate fluid, such as D 5 W, 1/2 NS, NS. l. Estimate fluid requirement and adjust PN accordingly.
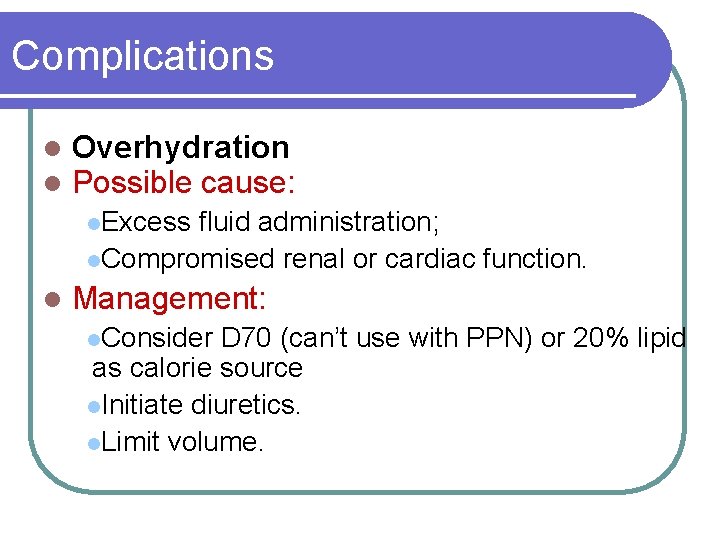
Complications l l Overhydration Possible cause: l. Excess fluid administration; l. Compromised renal or cardiac function. l Management: l. Consider D 70 (can’t use with PPN) or 20% lipid as calorie source l. Initiate diuretics. l. Limit volume.
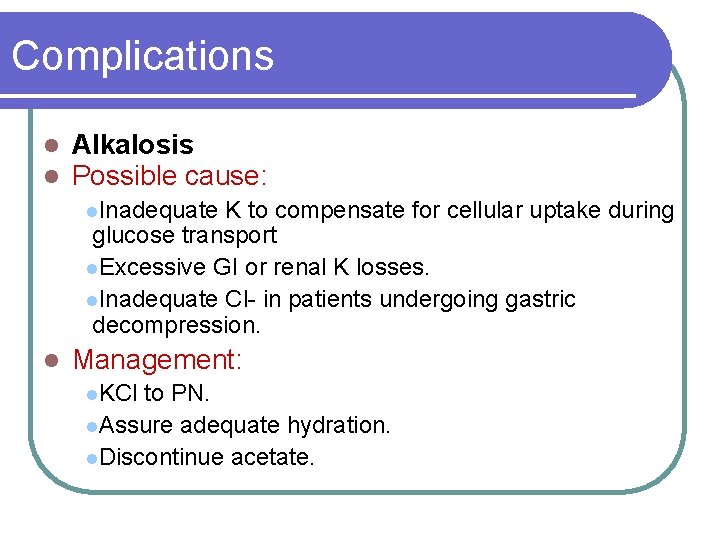
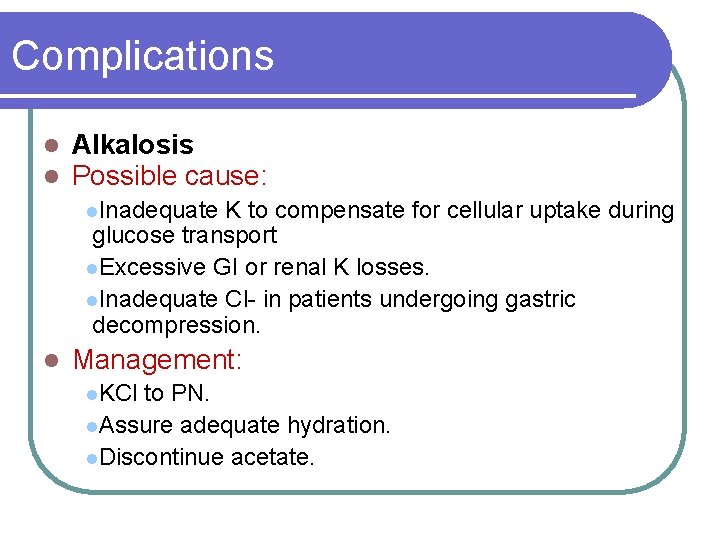
Complications l l Alkalosis Possible cause: l. Inadequate K to compensate for cellular uptake during glucose transport l. Excessive GI or renal K losses. l. Inadequate Cl- in patients undergoing gastric decompression. l Management: l. KCl to PN. l. Assure adequate hydration. l. Discontinue acetate.
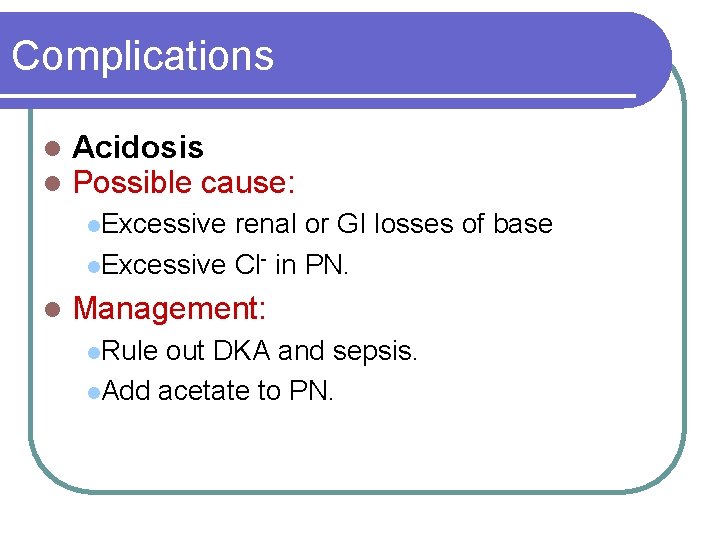
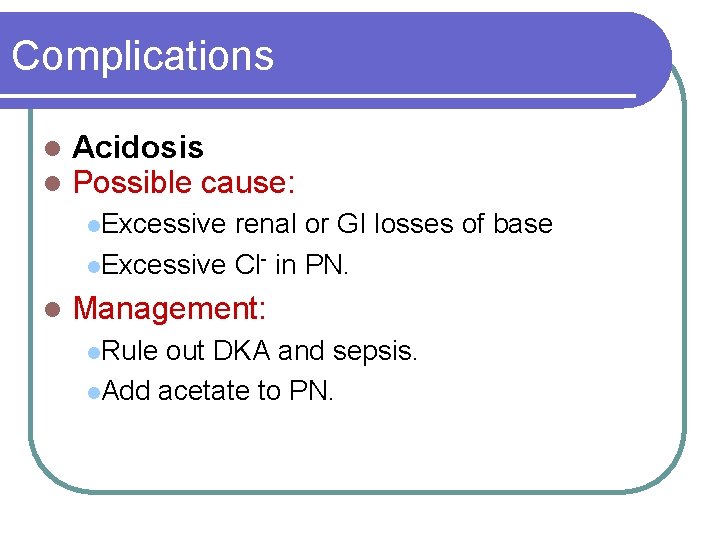
Complications l l Acidosis Possible cause: l. Excessive renal or GI losses of base l. Excessive Cl- in PN. l Management: l. Rule out DKA and sepsis. l. Add acetate to PN.
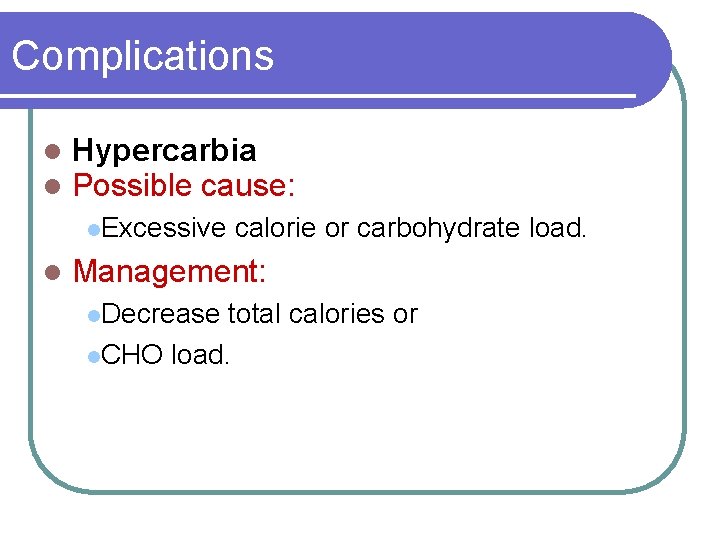
Complications l l Hypercarbia Possible cause: l. Excessive l calorie or carbohydrate load. Management: l. Decrease total calories or l. CHO load.
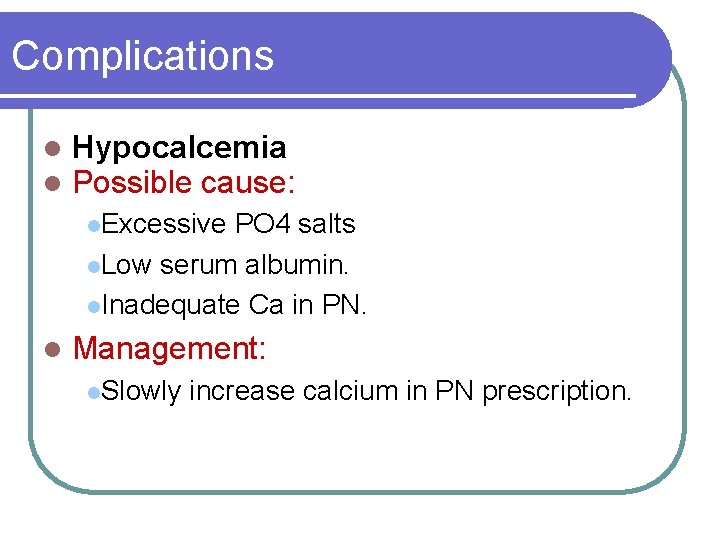
Complications l l Hypocalcemia Possible cause: l. Excessive PO 4 salts l. Low serum albumin. l. Inadequate Ca in PN. l Management: l. Slowly increase calcium in PN prescription.
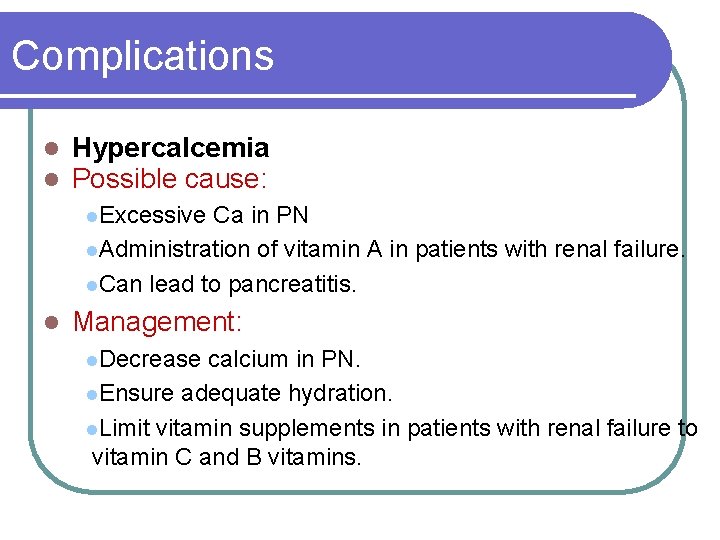
Complications l l Hypercalcemia Possible cause: l. Excessive Ca in PN l. Administration of vitamin A in patients with renal failure. l. Can lead to pancreatitis. l Management: l. Decrease calcium in PN. l. Ensure adequate hydration. l. Limit vitamin supplements in patients with renal failure to vitamin C and B vitamins.
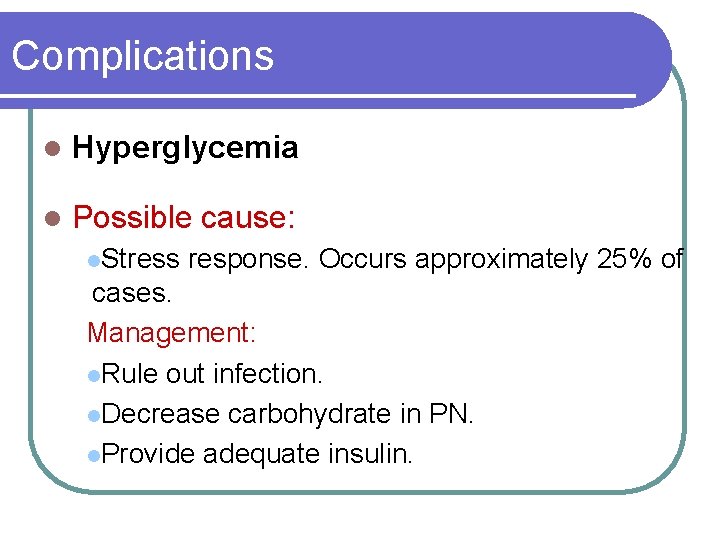
Complications l Hyperglycemia l Possible cause: l. Stress response. Occurs approximately 25% of cases. Management: l. Rule out infection. l. Decrease carbohydrate in PN. l. Provide adequate insulin.
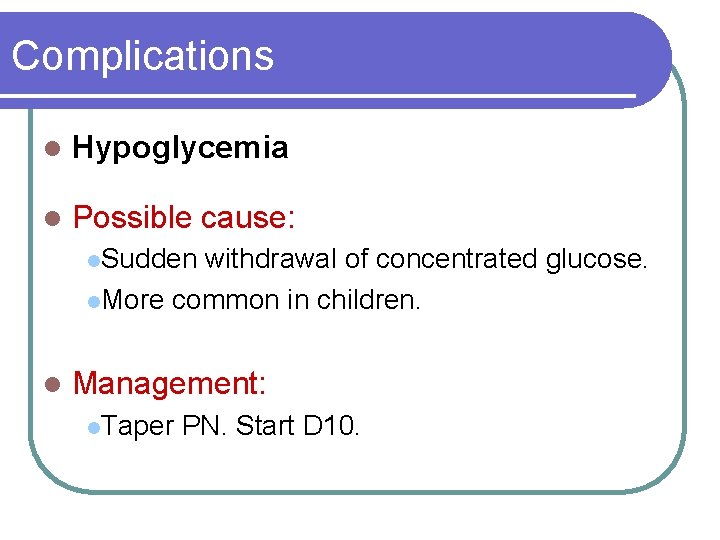
Complications l Hypoglycemia l Possible cause: l. Sudden withdrawal of concentrated glucose. l. More common in children. l Management: l. Taper PN. Start D 10.
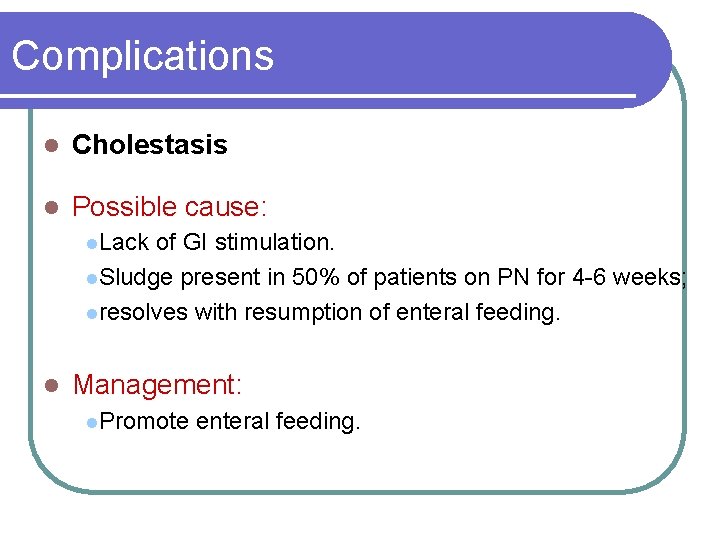
Complications l Cholestasis l Possible cause: l. Lack of GI stimulation. l. Sludge present in 50% of patients on PN for 4 -6 weeks; lresolves with resumption of enteral feeding. l Management: l. Promote enteral feeding.
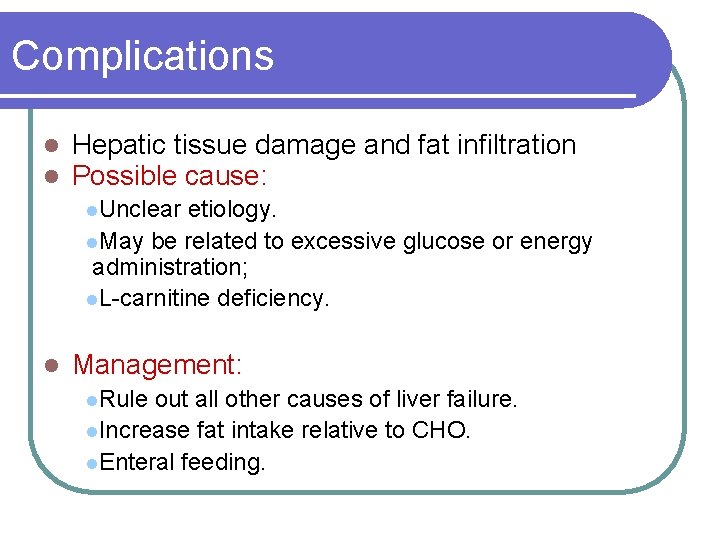
Complications l l Hepatic tissue damage and fat infiltration Possible cause: l. Unclear etiology. l. May be related to excessive glucose or energy administration; l. L-carnitine deficiency. l Management: l. Rule out all other causes of liver failure. l. Increase fat intake relative to CHO. l. Enteral feeding.

 Nursing care of hospitalized child
Nursing care of hospitalized child Nursing care of hospitalized child
Nursing care of hospitalized child Skin fold thickness
Skin fold thickness Subjective global assessment scoring sheet
Subjective global assessment scoring sheet Heather rawls
Heather rawls Abcd of nutritional assessment
Abcd of nutritional assessment Mini nutritional assessment short form
Mini nutritional assessment short form Nutritional status assessment
Nutritional status assessment Abcd of nutritional assessment
Abcd of nutritional assessment Ada 411
Ada 411 Chapter 11 nutrition and diets
Chapter 11 nutrition and diets Indirect method of nutritional assessment
Indirect method of nutritional assessment Calcul valoare energetica
Calcul valoare energetica Nutritional requirements of plants
Nutritional requirements of plants Chapter 2 nutritional needs
Chapter 2 nutritional needs Nutritional management of diabetes mellitus
Nutritional management of diabetes mellitus Conclusion of nutritional problems in india
Conclusion of nutritional problems in india Chapter 28 nutritional support and iv therapy
Chapter 28 nutritional support and iv therapy Nutritional diseases
Nutritional diseases Nutritional requirements for ruminant animals
Nutritional requirements for ruminant animals Nutritional recovery syndrome
Nutritional recovery syndrome Culinary nutrition definition
Culinary nutrition definition Public health nutrition definition
Public health nutrition definition Nonvascular plants phylum name
Nonvascular plants phylum name Concept of nutritional standard
Concept of nutritional standard Nutritional intervention
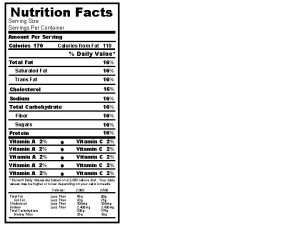
Nutritional intervention 8 servings per container
8 servings per container Nutritional needs throughout the life cycle
Nutritional needs throughout the life cycle Cut in mixing method
Cut in mixing method What is nutritional quackery
What is nutritional quackery Hyperglyceremia
Hyperglyceremia Keratomelacia
Keratomelacia Define nutritional epidemiology
Define nutritional epidemiology Nutritional requirements for beef cattle
Nutritional requirements for beef cattle Epi
Epi As nutritional energy passes through the food chain energy
As nutritional energy passes through the food chain energy Chapter 28 nutritional support and iv therapy
Chapter 28 nutritional support and iv therapy Fat malabsorption
Fat malabsorption Chapter 24 nutritional care and support
Chapter 24 nutritional care and support Foodafactoflife nutritional analysis
Foodafactoflife nutritional analysis Purpose of malnutrition
Purpose of malnutrition How can we crack nature’s secret nutritional code
How can we crack nature’s secret nutritional code Chapter 27 nutritional therapy and assisted feeding
Chapter 27 nutritional therapy and assisted feeding Objectives of nutrition
Objectives of nutrition Nutritional requirements of microorganisms
Nutritional requirements of microorganisms Food exchange chart
Food exchange chart Chapter 28 nutritional support and iv therapy
Chapter 28 nutritional support and iv therapy Specialized nutrition support
Specialized nutrition support Nutritional diseases
Nutritional diseases Major nutritional deficiency diseases in emergencies
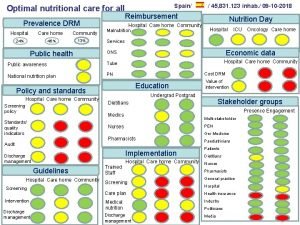
Major nutritional deficiency diseases in emergencies Optimal nutritional care for all
Optimal nutritional care for all Semi fowler position
Semi fowler position Prevention of vte in nonorthopedic surgical patients
Prevention of vte in nonorthopedic surgical patients How does nurse ratched manipulate the patients
How does nurse ratched manipulate the patients Cingulate herniation
Cingulate herniation Patients rights charter
Patients rights charter Diet chart for icu patients
Diet chart for icu patients Rocking chair therapy for dementia patients
Rocking chair therapy for dementia patients Leader rounding
Leader rounding Lippincott williams
Lippincott williams Daily intentional nurse leader rounding on patients
Daily intentional nurse leader rounding on patients Chapter 55 care of patients with stomach disorders
Chapter 55 care of patients with stomach disorders What are the positions used in nursing
What are the positions used in nursing Sengstaken blakemore tube nursing care
Sengstaken blakemore tube nursing care Nursing care of male patients with genitourinary disorders
Nursing care of male patients with genitourinary disorders Emergency move vs rapid extrication
Emergency move vs rapid extrication Introduction of admission in hospital
Introduction of admission in hospital Patient safety goals
Patient safety goals Medicare improvements for patients and providers act
Medicare improvements for patients and providers act Some patients shout in pain while ______ an injection.
Some patients shout in pain while ______ an injection. Broadmoor patients
Broadmoor patients Ethical issues in treating lgbt patients
Ethical issues in treating lgbt patients Management of patients with neurologic trauma
Management of patients with neurologic trauma Perimylolysis
Perimylolysis Power grip emt
Power grip emt Safe staffing ratios: benefiting nurses and patients
Safe staffing ratios: benefiting nurses and patients Dealing with challenging patients
Dealing with challenging patients Pico questions
Pico questions Cva
Cva Module 70 introduction to therapy
Module 70 introduction to therapy Nursing care plan of patients with cataract
Nursing care plan of patients with cataract Food safety for immunocompromised patients
Food safety for immunocompromised patients Rostering patients
Rostering patients Patients rights and responsibilities
Patients rights and responsibilities Neil's lateral throat form classification
Neil's lateral throat form classification Chapter 36 patients with special challenges
Chapter 36 patients with special challenges Factors of care patients can expect
Factors of care patients can expect Chapter 8 lifting and moving patients
Chapter 8 lifting and moving patients How to wash a bedridden patients hair
How to wash a bedridden patients hair Safe patient handling algorithms
Safe patient handling algorithms Wendylett sheets 1 carer
Wendylett sheets 1 carer Lifting and moving patients
Lifting and moving patients Nursing care plan on obsessive compulsive disorder
Nursing care plan on obsessive compulsive disorder Tena shampoo cap
Tena shampoo cap Chapter 58 care of patients with liver problems
Chapter 58 care of patients with liver problems Life expectancy of sickle cell patients
Life expectancy of sickle cell patients Guideline clinical nutrition in patients with stroke
Guideline clinical nutrition in patients with stroke Characteristics of portfolio assessment
Characteristics of portfolio assessment Static assessment vs dynamic assessment
Static assessment vs dynamic assessment Portfolio assessment matches assessment to teaching
Portfolio assessment matches assessment to teaching Level of mdm
Level of mdm Chapter 7 ionic and metallic bonding assessment answer key
Chapter 7 ionic and metallic bonding assessment answer key Life cycle assessment
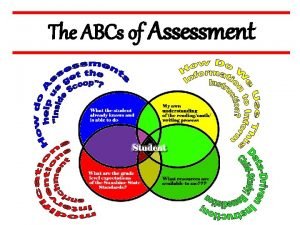
Life cycle assessment Abcs assessment
Abcs assessment Difference between formative and summative assessment
Difference between formative and summative assessment Nsw department of education
Nsw department of education Student assessment examples
Student assessment examples Egd practical assessment task 2020
Egd practical assessment task 2020 Designing assessment tasks
Designing assessment tasks Pediatric physical therapy assessment tools
Pediatric physical therapy assessment tools Round robin charts formative assessment
Round robin charts formative assessment Abecedarian reading assessment
Abecedarian reading assessment Michigan educational assessment program
Michigan educational assessment program Kent internet risk assessment tool
Kent internet risk assessment tool Ebtesam ahmed
Ebtesam ahmed Ttess smart goals examples
Ttess smart goals examples Washington comprehensive assessment program
Washington comprehensive assessment program Community needs assessment steps
Community needs assessment steps Dessa devereux
Dessa devereux Comprehensive pain assessment
Comprehensive pain assessment