Chapter 27 Nutrional Therapy and Assisted Feeding Copyright
- Slides: 38
Chapter 27 Nutrional Therapy and Assisted Feeding Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Lesson 27. 1 Nutritional Therapy Overview Theory 1) Identify the nurse’s role related to nutritional therapy and special dietary needs. 2) Compare and contrast a full liquid with a clear liquid diet. 3) Explain the different dietary modification levels: puréed, mechanically altered, advanced, and regular. 4) Describe health issues related to nutrition. 5) List disease processes that may benefit from nutritional therapy. Clinical Practice 1) Use therapeutic communication to assist a patient who requires a special diet. 2) Develop a patient education plan for nutritional therapy. Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Goals of Diet Therapy Treat and manage disease Prevent complications and restore health Specific diet for each patient is prescribed on the physician’s order sheet Ø Patients can have nutritional goals met after a thorough diet assessment Ø Some patients may need assistance with feeding Ø Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
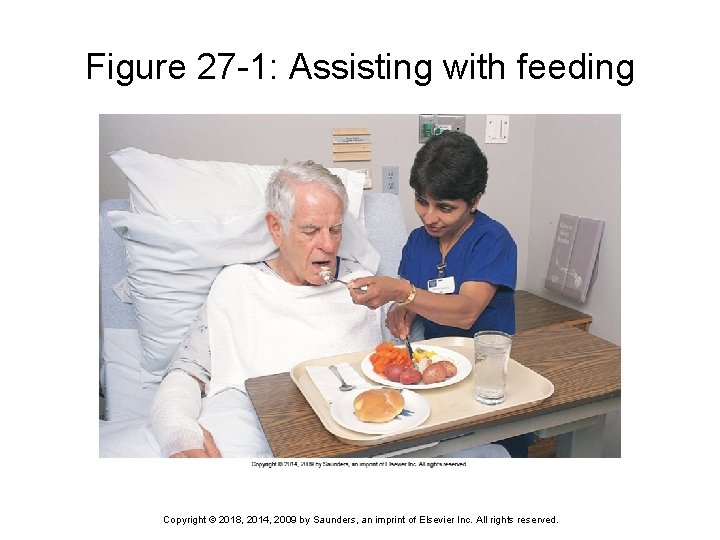
Patients Needing Feeding Assistance Patients with paralysis of the arms Patients with visual impairment Patients with intravenous lines in their hands Severely impaired or weak patients Confused patients Ø Feeding may be delegated to a nursing assistant or family member Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
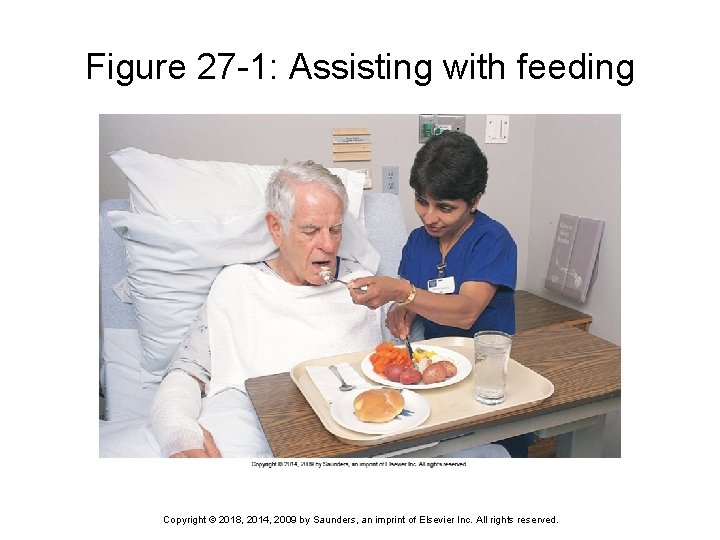
Figure 27 -1: Assisting with feeding Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Postoperative Patient Should be well-nourished preoperatively to facilitate postoperative healing and recovery Preoperative patients are usually NPO 6 to 8 hours before the procedure Postoperative patients progress from a clear liquid to full liquid diet May progress to a soft diet before attempting a general or regular diet Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
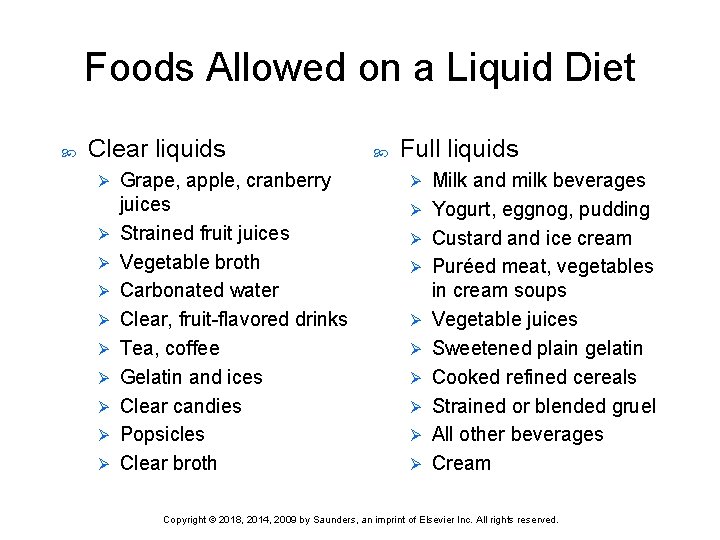
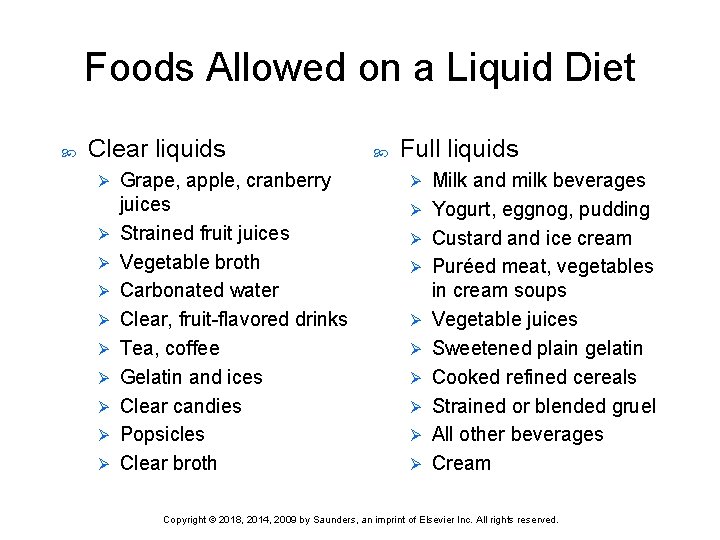
Foods Allowed on a Liquid Diet Clear liquids Ø Ø Ø Ø Ø Grape, apple, cranberry juices Strained fruit juices Vegetable broth Carbonated water Clear, fruit-flavored drinks Tea, coffee Gelatin and ices Clear candies Popsicles Clear broth Full liquids Ø Ø Ø Ø Ø Milk and milk beverages Yogurt, eggnog, pudding Custard and ice cream Puréed meat, vegetables in cream soups Vegetable juices Sweetened plain gelatin Cooked refined cereals Strained or blended gruel All other beverages Cream Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
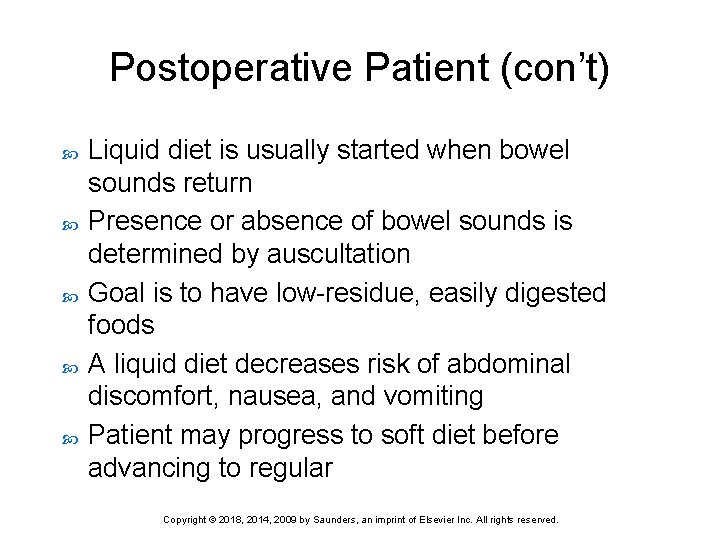
Postoperative Patient (con’t) Liquid diet is usually started when bowel sounds return Presence or absence of bowel sounds is determined by auscultation Goal is to have low-residue, easily digested foods A liquid diet decreases risk of abdominal discomfort, nausea, and vomiting Patient may progress to soft diet before advancing to regular Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Anorexia Nervosa Mental disorder characterized by refusal to maintain a normal weight and fear of becoming obese Patient may refuse to eat despite being extremely underweight Ø If not corrected, may be fatal Ø Treatment is: • Nutritional intervention • Counseling Ø Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Bulimia Eating disorder characterized by episodic binge eating followed by behaviors to prevent weight gain; e. g. , purging, fasting, using laxatives Patients aware of their behavior and often feel ashamed Ø Treatment is: • Nutritional counseling • Psychological counseling Ø Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Obesity Excessive accumulation of fat, not just being overweight according to height and weight scales Incidence in United States is increasing Approximately 34. 9% are obese Obesity is the second leading cause of preventable death in the United States Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Obesity (cont’d) Contributing factors Ø Genetics, environment, poor eating habits, lack of knowledge about good nutrition, body physiology, age, and gender Goal of obesity treatment is to improve health and quality of life Ø Must expend more energy than is consumed through intake of calories Bariatric surgery is currently touted as the most effective treatment to provide long lasting weight loss for people with extreme obesity Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Pregnancy Nutritional status before and during pregnancy can influence health status of mother and fetus Weight gain should be 2 to 4 lb for the first trimester and 1 lb/week during the second and third trimesters Ø Recommended—no caloric increase in the first trimester, then 300 calories/day for the second and third trimesters Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Substance-Related and Addictive Disorders Individuals who use alcohol, smoking, and other substances often present with nutritional deficits Interferes with food intake by decreasing appetite and decreasing financial resources for food May lead to impaired absorption of nutrients Ø Thiamine deficiency is seen in alcohol abuse Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Substance Abuse (cont’d) Patients with a history of substance abuse should have dietary counseling Treatment Fluid and electrolyte supplements Ø Vitamin and mineral supplements (particularly thiamine) Ø High-calorie, high-carbohydrate diet Ø Dietary fat restriction if liver function impaired Ø Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Cardiovascular Disease Includes diseases of the blood vessels, hypertension, myocardial infarction, and congestive heart failure Focused on reduction of fat and sodium intake to decrease atherosclerosis Cholesterol, three types: High-density lipoprotein Ø Low-density lipoprotein Ø Very-low-density lipoprotein Ø Sodium: 1 teaspoon salt contains 2300 mg sodium Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Diabetes Mellitus Disturbance of the metabolism of carbohydrates and the use of glucose by the body Two main types Type 1: insulin dependent (juvenile onset) Ø Type 2: non–insulin dependent (adult onset) Ø Higher risk in African Americans and Hispanics Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Diabetes Mellitus (cont’d) Diet therapy to control carbohydrate intake to maintain serum glucose at 75 to 115 mg/d. L Patients should avoid large amounts of carbohydrates in one meal Meals should contain 45% to 60% carbohydrates, 20% to 25% protein, and 20% to 25% fat Calories restricted if patient is overweight Carbohydrates should be complex Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Diabetes Mellitus (cont’d) Diabetic patients are at higher risk for: Cardiovascular disease Ø Hypertension Ø Kidney disease Ø Blindness Ø Stroke Ø Dietary counseling is essential Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
HIV/AIDS patients often have: Severe diarrhea Ø Profound weight loss Ø Muscle wasting Ø Therapy is aimed at: Replacement of fluids and electrolytes Ø Weight gain Ø Replacement of lost muscle mass Ø Maintaining the immune system Ø Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Question 1 Diabetes mellitus is a disturbance of carbohydrate metabolism. Which two ethnic backgrounds are at greatest risk of developing diabetes? 1) 2) 3) 4) Whites and African Americans Whites and Hispanics African Americans and Asians Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Question 2 Bill is a recently diagnosed HIV patient. Both Bill and his partner Pat are present for the nurse’s discharge teaching regarding diet. Which of the following is true regarding diet therapy in HIV patients? 1) 2) 3) 4) Patients should be referred to a dietitian within the first year of diagnosis. Emphasis should be placed on carbohydrate intake. Patients should be encouraged to eat three full meals a day. Research suggests that diet therapy can be a factor in delaying full-blown AIDS. Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Question 3 Gabrielle’s patient is admitted with a diagnosis of alcohol abuse. She is assessing her patient for any nutritional deficits. Which deficiency is often present with alcohol abuse? 1) 2) 3) 4) Niacin Thiamine Potassium Sodium Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Lesson 27. 2 Nasogastric Tube Overview Theory 6) Verbalize the rationale for assisted feedings and tube feedings. 7) List the steps for the procedure to insert, irrigate, and remove a nasogastric tube. Clinical Practice 3) Demonstrate insertion, irrigation, and removal of a nasogastric tube. Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Nasogastric and Enteral Tubes Usually a temporary measure to provide nutritional support Check tube placement prior to feeding or administering medications Irrigate to ensure it is patent Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Nasogastric and Enteral Tubes (cont’d) Reasons for use Dysphagia following stroke Ø Inflammatory bowel disease Ø Decompression of the stomach before or after surgery Ø Obtaining gastric specimens for analysis Ø Gastric feeding or lavage Ø Administration of medications Ø Insertion and care (Review Skill 27 -2) Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
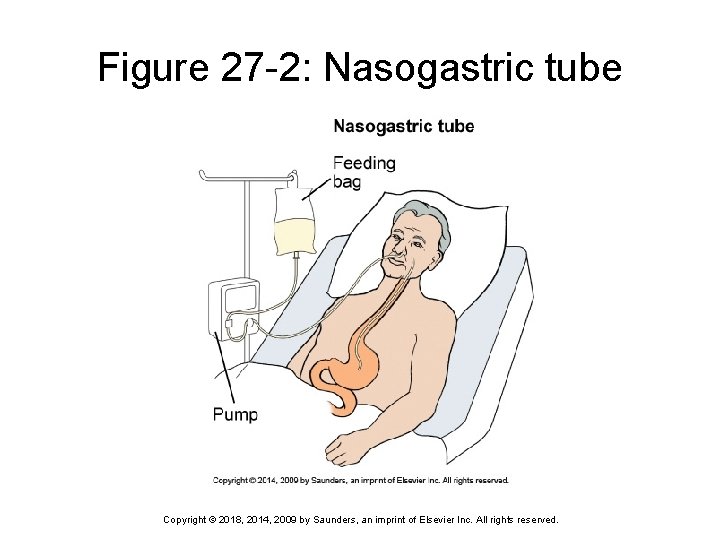
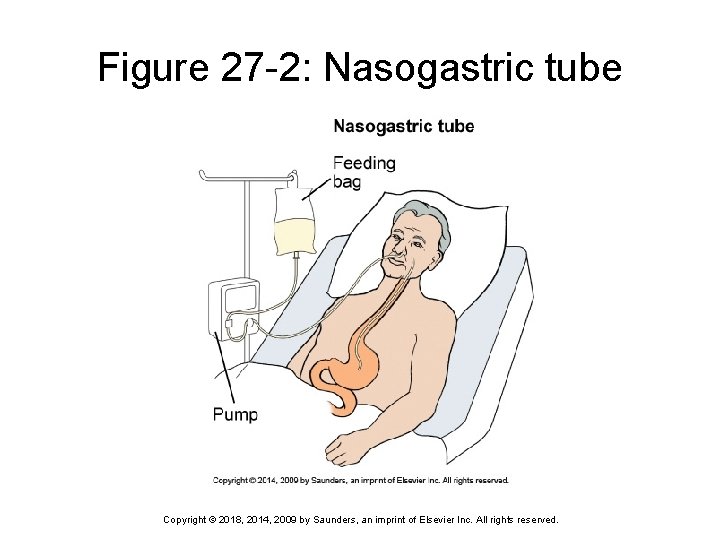
Figure 27 -2: Nasogastric tube Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
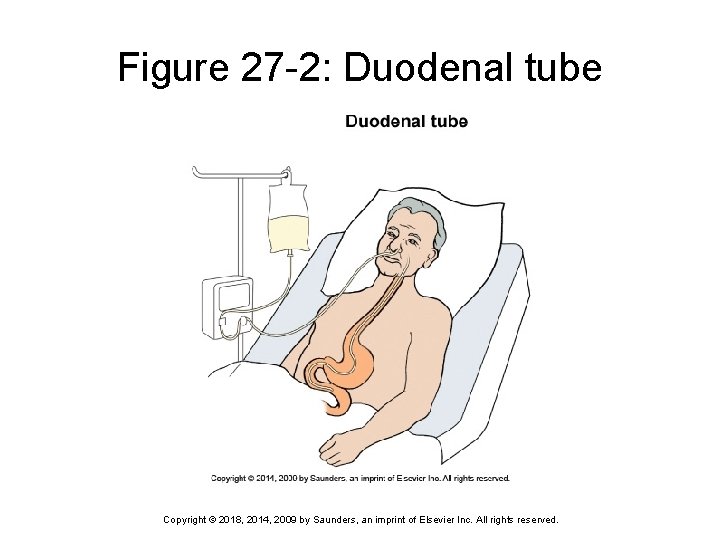
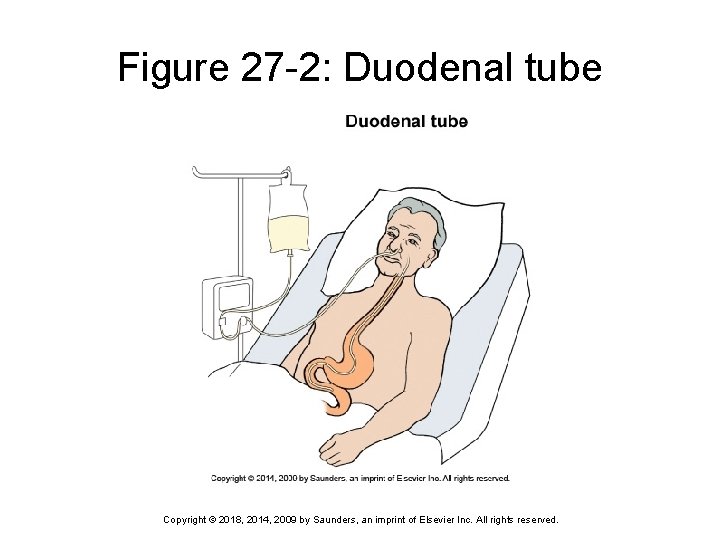
Figure 27 -2: Duodenal tube Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
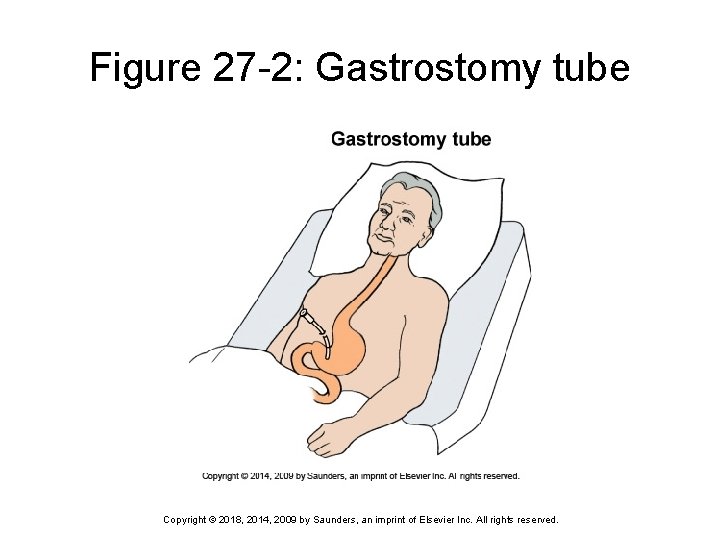
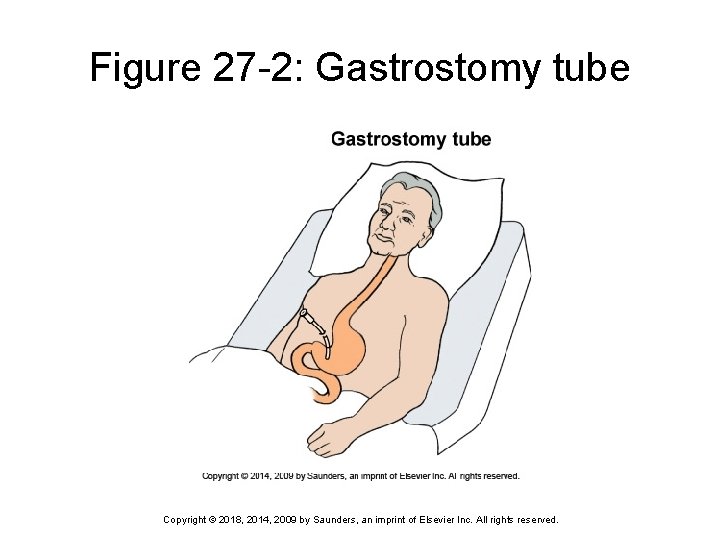
Figure 27 -2: Gastrostomy tube Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
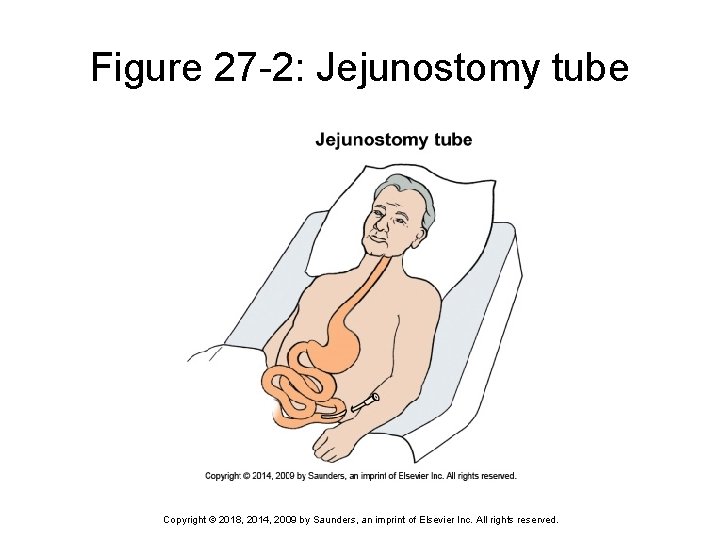
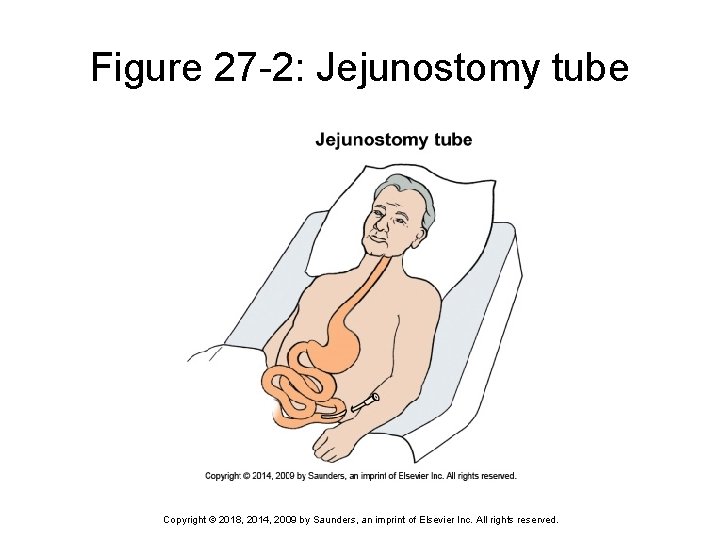
Figure 27 -2: Jejunostomy tube Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Percutaneous Endoscopic Gastrostomy or Jejunostomy Tubes Generally used when a patient requires longterm nutritional support Tube placement should be checked every shift and before feeding or administering medication Before feeding or administering medications, amount of residual fluid in the stomach should be assessed Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Question 4 Sienna’s patient is having difficulty swallowing. Her doctor has ordered a gastrostomy tube. Sienna explains to her patient that a gastrostomy tube is a tube placed: 1) 2) 3) 4) through the nose into the stomach. directly into the intestines. directly into the veins. Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Lesson 27. 3 Tube Feeding Theory 8) Discuss the procedure for tube feeding. 9) Identify medical rationale and nursing care for a patient receiving peripheral parenteral nutrition (PPN) and total parenteral nutrition (TPN). 10) Understand the possible complications associated with modified diets, tube feedings, PPN, and TPN. Clinical Practice 4) Demonstrate feeding a patient through a nasogastric tube or percutaneous endoscopic gastrostomy (PEG) tube. 5) Know your facility’s policies, procedures, and protocols for nutrition-related problems and complications with tube feedings. Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Feeding Tubes and Pumps Continuous feeding effective for patients who cannot tolerate large amounts of fluids at one time Intermittent feeding beneficial for patients who are able to feed themselves or when beginning to reintroduce oral feeding Amount of tube feeding is prescribed by the physician; ranges from 8 to 12 oz per feeding Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
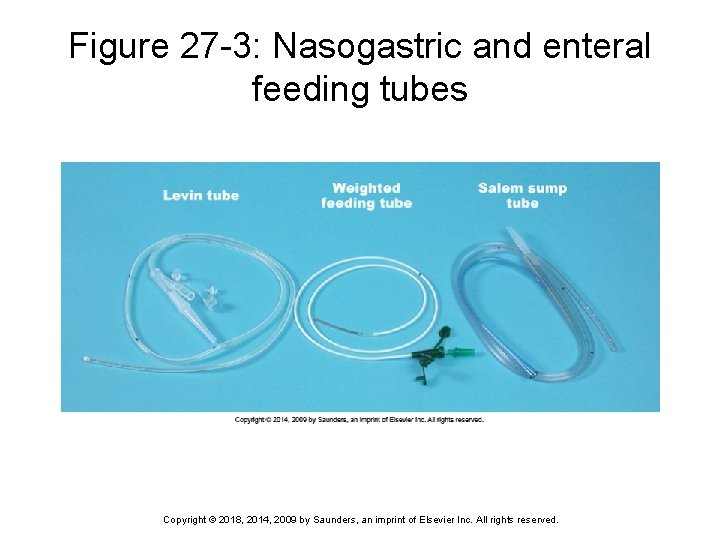
Feeding Tubes and Pumps (con’t) Plastic nasogastric tubes: can be used for lavage, tube feeding, and administering medications Small-bore silicone feeding tubes: usually used only for tube feeding Percutaneous endoscopic gastrostomy (PEG) tube and jejunostomy tube: used for tube feeding and administering medication Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
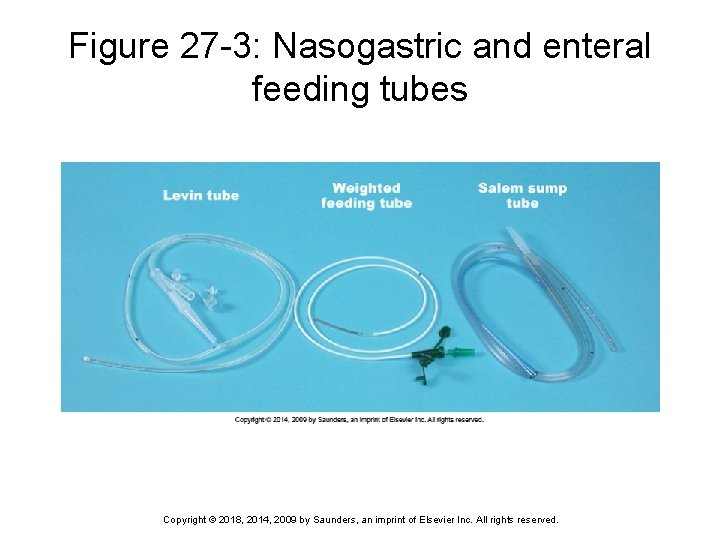
Figure 27 -3: Nasogastric and enteral feeding tubes Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
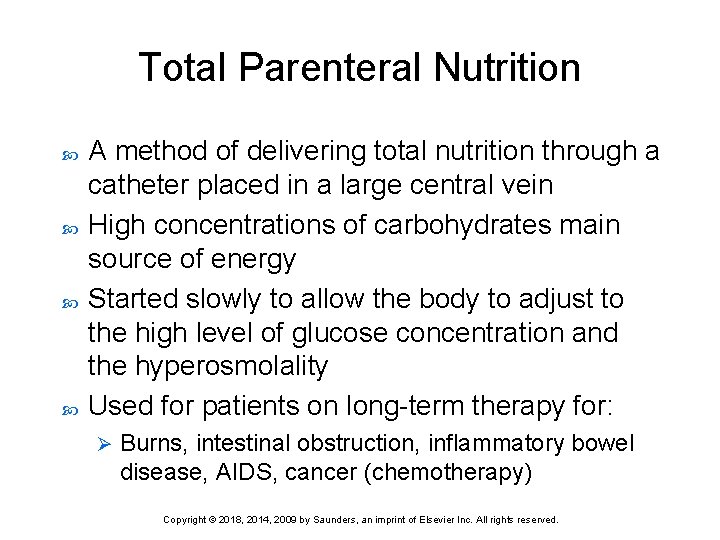
Total Parenteral Nutrition A method of delivering total nutrition through a catheter placed in a large central vein High concentrations of carbohydrates main source of energy Started slowly to allow the body to adjust to the high level of glucose concentration and the hyperosmolality Used for patients on long-term therapy for: Ø Burns, intestinal obstruction, inflammatory bowel disease, AIDS, cancer (chemotherapy) Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Question 5 As a nurse, when taking care of a patient with a nasogastric tube, you should remember all of the following except: 1) 2) 3) 4) that tube placement should be checked at least every shift and before every feeding. to elevate the head of the bed 15 degrees before feedings and leave it up for 30 to 60 minutes after the feeding. that the amount of the tube feeding is prescribed by the physician. to record intake and output. Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.