Optimum Nutritional Management of Hospitalized Pediatric Oncology Patients

- Slides: 42
Optimum Nutritional Management of Hospitalized Pediatric Oncology Patients: A Case Study Qualitative Research Project ANDRIA M. KEATING, RD INTERN CAPSTONE PROJECT PRECEPTOR: ALLIE E. HUBBARD, RD
Acknowledgement I would like to express my gratitude and appreciation to all those whose provided suggestions and encouragement, and helped me to complete my major capstone project. v Allie E. Hubbard, RD Major Capstone Preceptor v Ana Abad-Jorge, Ed. D, MS, RDN, CNSC Major Capstone Project Reviewer v Evelyn Joran-Thiel, MSN, CPNP, CPON v Traci Fisher, RN, BSN
Overview • • • Introduction Nutrition Implications of Pediatric Cancers Project Purpose Methods Results Discussion Limitations Future Research Conclusions
Introduction • In a 2007 study, the National Cancer Institute revealed that an estimated 10, 400 children 15 years of age and below were diagnosed with cancer. 1 • Of those children, about 1, 545 children died from the disease in the United States. 1 • This makes cancer the leading cause of death in children under the age of 14. 1
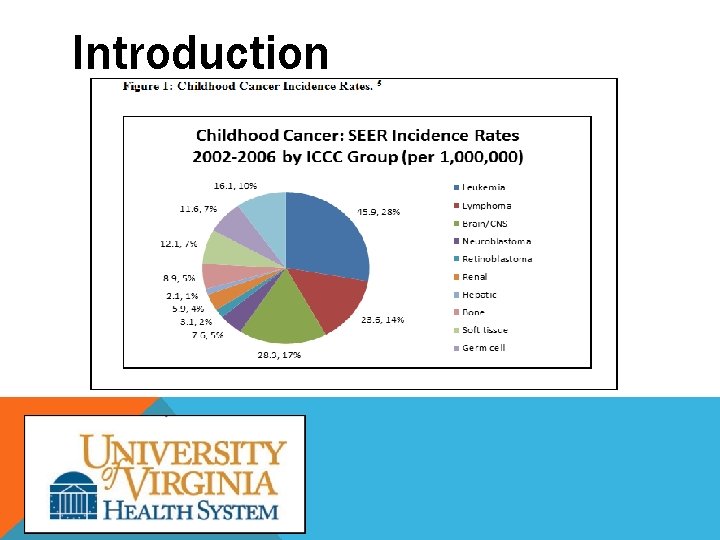
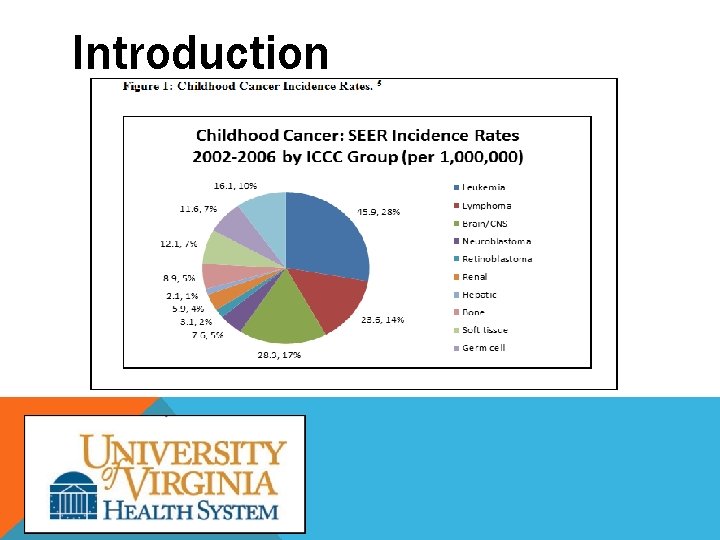
Introduction • The most prevalent cancers affecting children are: • Leukemia, • Central nervous system (CNS) tumors, and • Lymphoma. 4, 5 • Leukemia is the most common pediatric cancer accounting for approximately 28 -30% of total cancer diagnoses. 4, 6 Brain and CNS tumors are the next most prevalent pediatric cancer, followed by lymphoma. 4 -7
Introduction
Nutrition Implications of Pediatric Cancers • Malnutrition at diagnosis exists in 6% to 50% of patients and is dependent upon the histology, stage of disease, and location of the cancer. 17 • The side effects of malnutrition may include tissue wasting, anorexia, weakness, anemia, hypoalbuminemia, and skeletal muscle atrophy. 17 • Protein and calorie malnutrition is associated with a higher incidence of infection, decreased tolerance of chemotherapeutic treatments, and overall diminished quality of life. 17
Nutrition Implications of Pediatric Cancers • Cancer cachexia • A syndrome where the body is unable to absorb, metabolize, and utilize essential nutrients, manifesting in unintentional weight loss. 19 • The pathophysiology of cachexia has not been clearly defined, but may be caused by the outcomes of immunologic and humoral neuroendocrine abnormalities. • The physiological stress caused by cachexia can alter body composition and cause metabolic alterations in carbohydrate, lipid, and protein absorption and metabolism. 17
Nutrition Implications of Pediatric Cancers • Metabolic alterations • Carbohydrates: increased glucose uptake and lactate production by the tumor, hypoinsulinism, insulin resistance • Protein: metabolism is affected by the tumor burden by altering uptake of amino acids. • Lipid metabolism is often less affected than the other macronutrients. However, the depletion of fat stores is higher in pediatric oncology patients due to increased lipolysis. 1
Nutrition Implications of Pediatric Cancers • Treatment options and their nutrition-related side effects • The most common methods of treatment are • Chemotherapy, • Radiation, • Surgery, and • Hematopoietic stem cell transplantation (HCST). 10 • Common side effects associated with cancer treatments may include diarrhea, nausea, vomiting, mucositis, pain, fatigue, early satiety, xerostomia, and loss of taste. 2
Nutrition Implications of Pediatric Cancers • The primary goal for the nutrition management of children and adolescents undergoing cancer treatment is to sustain and promote normal growth and development. 26 • Determining nutritional needs of the pediatric oncology patient should be influenced by: • Providing adequate nutrition for the preservation of lean tissue and to promote normal growth and development, • Identifying and correcting the effects of protein and energy malnutrition and metabolic abnormalities, and • Maximizing quality of life for the patient. 16
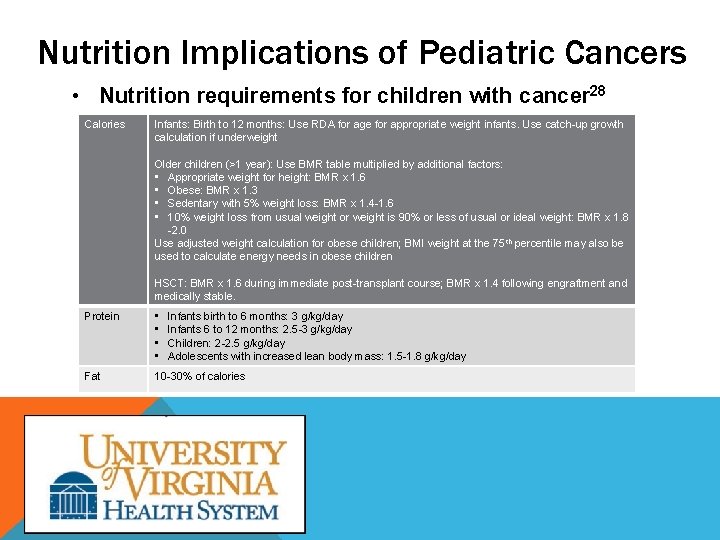
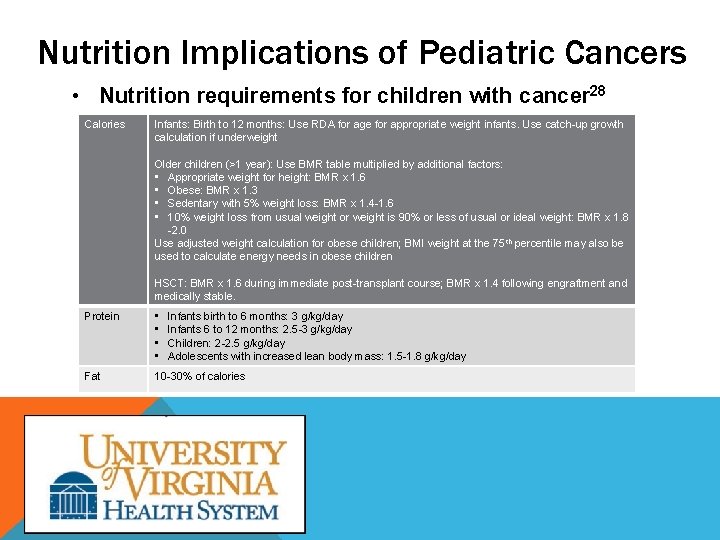
Nutrition Implications of Pediatric Cancers • Nutrition requirements for children with cancer 28 Calories Infants: Birth to 12 months: Use RDA for age for appropriate weight infants. Use catch-up growth calculation if underweight Older children (>1 year): Use BMR table multiplied by additional factors: • Appropriate weight for height: BMR x 1. 6 • Obese: BMR x 1. 3 • Sedentary with 5% weight loss: BMR x 1. 4 -1. 6 • 10% weight loss from usual weight or weight is 90% or less of usual or ideal weight: BMR x 1. 8 -2. 0 Use adjusted weight calculation for obese children; BMI weight at the 75 th percentile may also be used to calculate energy needs in obese children HSCT: BMR x 1. 6 during immediate post-transplant course; BMR x 1. 4 following engraftment and medically stable. Protein • • Fat 10 -30% of calories Infants birth to 6 months: 3 g/kg/day Infants 6 to 12 months: 2. 5 -3 g/kg/day Children: 2 -2. 5 g/kg/day Adolescents with increased lean body mass: 1. 5 -1. 8 g/kg/day
Nutrition Implications of Pediatric Cancers Nutrition support in children with cancer • The goal of nutrition support is to provide adequate nutrients to meet the demands of the growth and development, and also to reverse the possibility of protein-calorie malnutrition. • Nutritional support for patients that are malnourished due to inadequate oral intake has been shown to improve nutritional intake and outcomes. 15
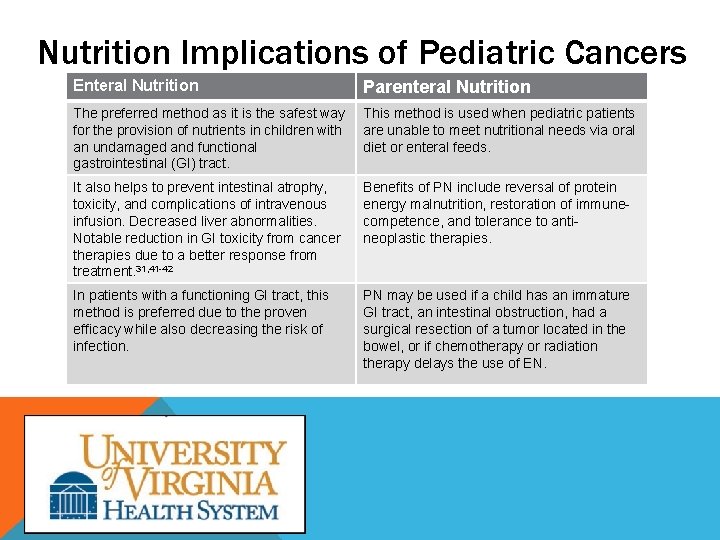
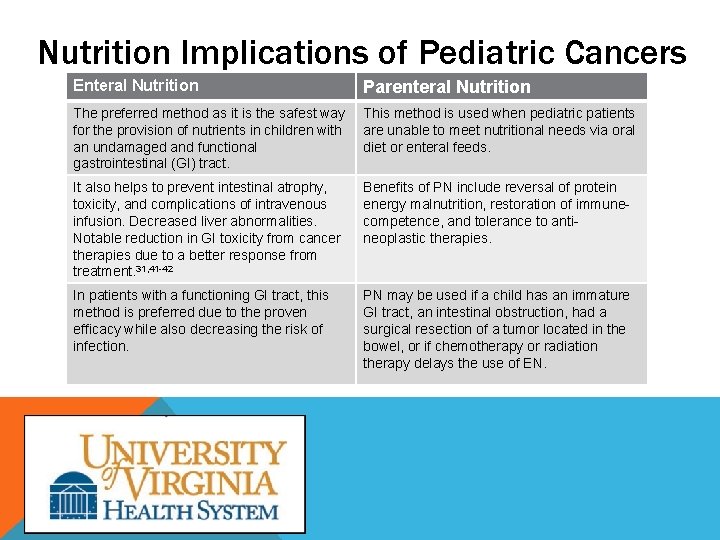
Nutrition Implications of Pediatric Cancers Enteral Nutrition Parenteral Nutrition The preferred method as it is the safest way for the provision of nutrients in children with an undamaged and functional gastrointestinal (GI) tract. This method is used when pediatric patients are unable to meet nutritional needs via oral diet or enteral feeds. It also helps to prevent intestinal atrophy, toxicity, and complications of intravenous infusion. Decreased liver abnormalities. Notable reduction in GI toxicity from cancer therapies due to a better response from treatment. 31, 41 -42 Benefits of PN include reversal of protein energy malnutrition, restoration of immunecompetence, and tolerance to antineoplastic therapies. In patients with a functioning GI tract, this method is preferred due to the proven efficacy while also decreasing the risk of infection. PN may be used if a child has an immature GI tract, an intestinal obstruction, had a surgical resection of a tumor located in the bowel, or if chemotherapy or radiation therapy delays the use of EN.
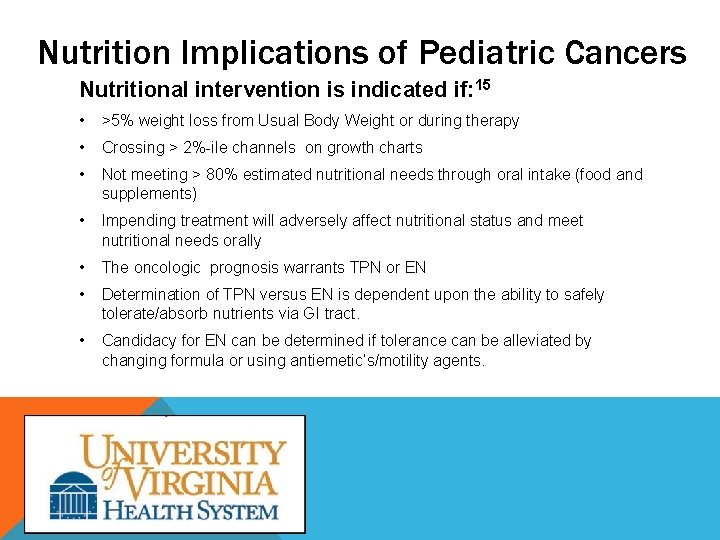
Nutrition Implications of Pediatric Cancers Nutritional intervention is indicated if: 15 • >5% weight loss from Usual Body Weight or during therapy • Crossing > 2%-ile channels on growth charts • Not meeting > 80% estimated nutritional needs through oral intake (food and supplements) • Impending treatment will adversely affect nutritional status and meet nutritional needs orally • The oncologic prognosis warrants TPN or EN • Determination of TPN versus EN is dependent upon the ability to safely tolerate/absorb nutrients via GI tract. • Candidacy for EN can be determined if tolerance can be alleviated by changing formula or using antiemetic’s/motility agents.
Nutrition Implications of Pediatric Cancers • Barriers to adequate nutrition support 18 • Initial low infusion rates • Feeding interruptions due to medical procedures • Holding feeds for specific medication administration • Potential side effects related treatment protocols • Neutropenia or thrombocytopenia increases risk for bleeding when nasoenteric tubes are inserted; however, clinical trials have not supported this theoretical risks. 18
Project Purpose • Determine barriers to optimizing nutrition support at UVAHS • Investigate current practice and the medical team’s preference for use of a particular form of nutrition support. • Provide evidenced-based recommendations for the nutritional management of pediatric oncology patients. • Promote the importance of utilizing EN feedings as a standard nutritional intervention during treatment.
Methods • • • This study used a case series mixed methods approach to investigate nutrition support practice management at UVAHS. Data was retrospectively collected on 3 patients between February 2013 – March 2013. Selection criterion for the hospitalized patients were based on the following: • UVAHS pediatric oncology patient and • Patients receiving long-term nutritional support via EN or PN.
Methods • Patient Overview: • T. W. , a 7 year old male with anaplastic medulloblastoma • N. P. , an 11 month old male with infantile AML diagnosis • N. M. , a 7 year old female with medulloblastoma of the cerebellum
Methods: Quantitative Data • Retrospective data was collected on the three selected patients using the EPIC electronic medical records to include: • • Specific cancer diagnoses Reason for admissions Previous surgical and medical history Anthropometrics (weight (kg), length (cm), head circumference (cm), % weight loss) • Oncologic treatments received & other relevant medications • Degree of malnutrition assessed by the Waterlow Criteria • Nutritional intake data included: • PN data (if applicable): PN order, goal caloric provision (kcal/kg) from PN, and actual intake • EN data: formula, caloric density, goal feeding schedule, route, goal caloric provision (kcal/kg), and actual intake • Patient’s nutritional goals and percentage of the goals achieved • Noted barriers to starting or advancing nutritional support
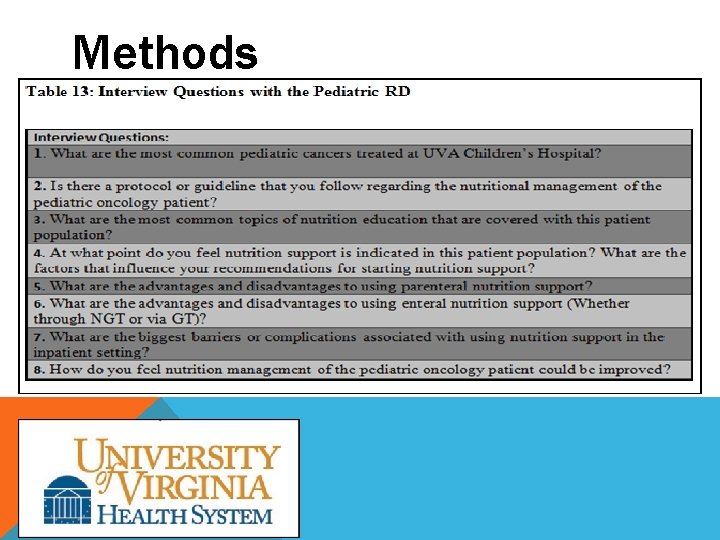
Methods: Qualitative Data • In order to obtain information on the nutritional support practices at UVAHS, interviews were conducted with various members of the pediatric oncology team: • Pediatric oncology nurse practitioner (NP), • Pediatric oncology bedside nurse (RN), and • The pediatric oncology RD employed at UVAHS. • These professionals provided their perspectives on the ideal approach and challenges in the management of pediatric oncology patients
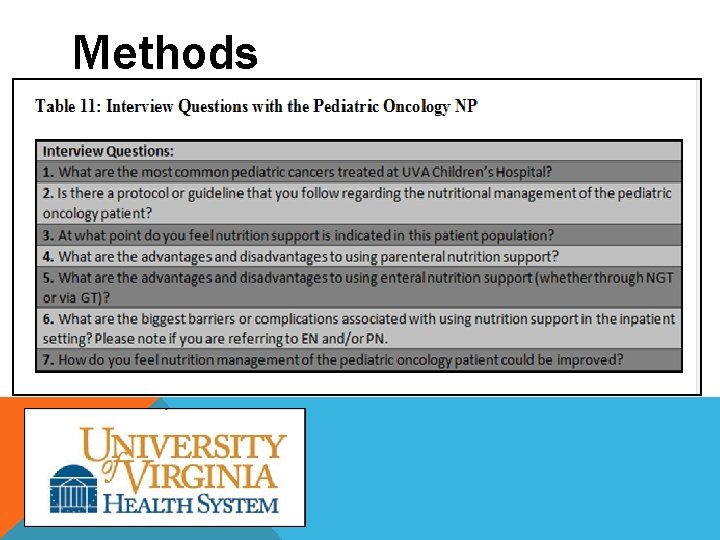
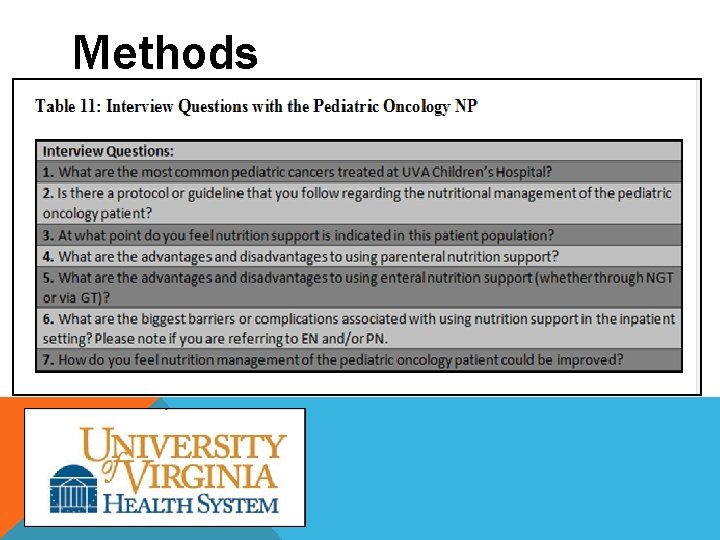
Methods
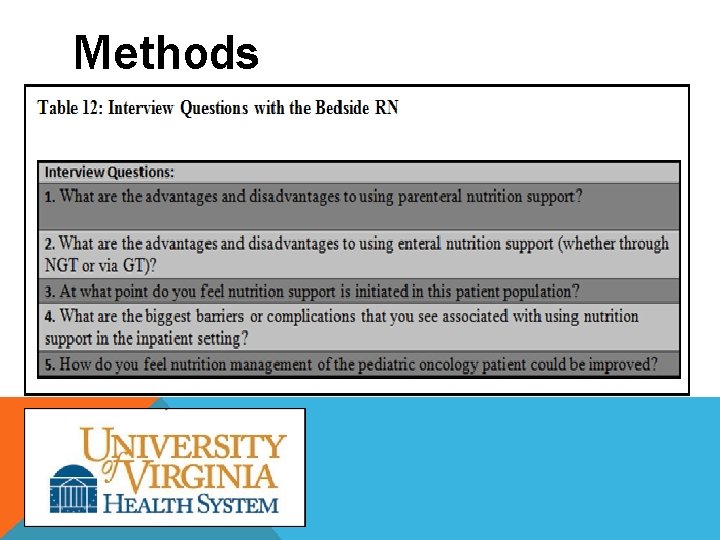
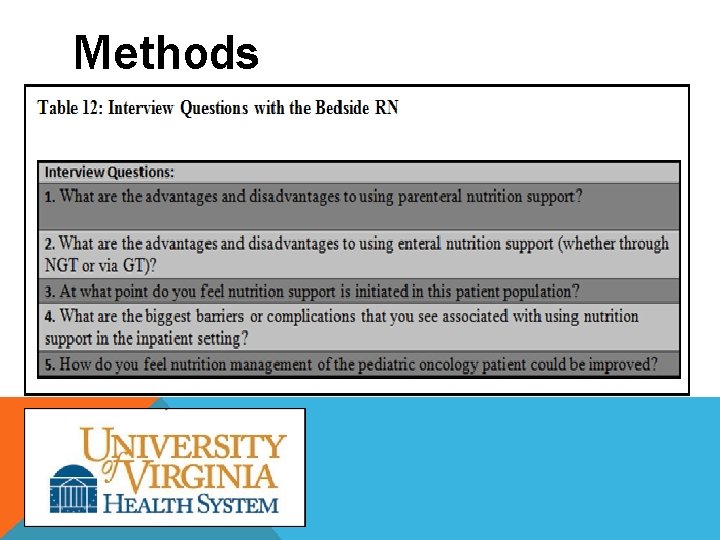
Methods
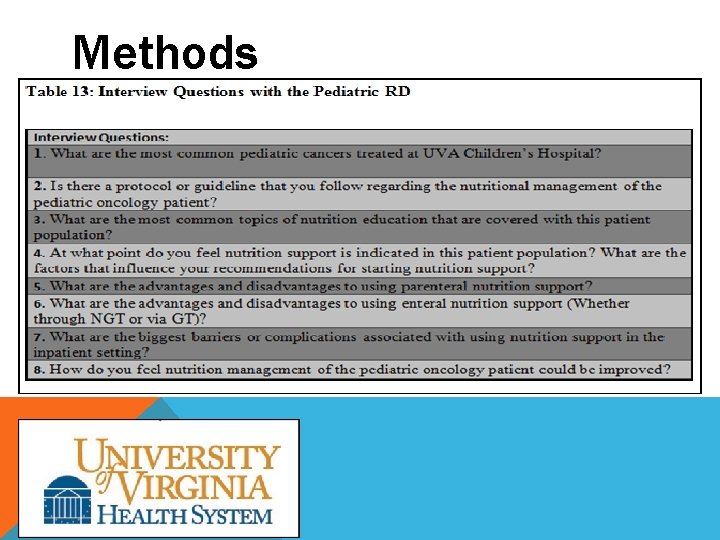
Methods
Methods • All of the collected data was recorded and organized into a Microsoft Excel spreadsheet. • Basic descriptive statistics were used for data analysis. • The data obtained in this study was used to provide a general overview of the outcomes and current nutritional practices at UVAHS, as well as to investigate the use of EN versus PN at UVAHS.
Results T. W. Highlights • December 21 st, 2011: Weight of 19. 5 kg (3. 45% weight-for-age); 76% of IBW, BMI-for-age 2. 90 th%-ile • February 2012: Placement of G-tube. Weight of 18. 7 kg; initiated on nocturnal G-tube feeds • March 2012: Weight of 20. 6 kg, Up ~2 kg in a month since the placement of the G-tube. • July 2012: Weight of 21. 55 kg (8% weight-for-age); 90% of IBW and improved BMI-for-age 13 th%-ile • Main challenges with nutrition support: EN held for episodes of emesis, TPN held due to central line infection, Bone Marrow procedure, cellulitis, peritoneal infection, EN caloric density
Results N. P. Highlights: • • • Admitted to PICU August 14 th, 2012: 9. 2 kg (21 st %-ile), weight for length: 29 th%-ile (Percentile); On TPN feeds initially started on trophic NG feeds August 26 th, 2012 October 2012: Weighed 9. 86 kg (47%ile weight for age) upon transfer to the floor, gaining an average of 10 grams per day since admission due to EN support. October 23 rd, 2012: Placed on bowel rest with TPN initiated but resumed EN feeds on November 16 th, 2012 November 2012: Weighed 10. 17 kg (50% weight for age) due to continued progress with EN support Main challenges with nutrition support: radiation schedule (M-F), anesthesia, pneumatosis, increased risk for mucositis and concern for typhilits
Results N. M. Highlights: • • • October 3, 2012: Weight of 24. 2 kg, down from UBW of 29 kg in 3. 5 months (17% weight loss since diagnosis). Decision made to place Gtube in anticipation of upcoming chemotherapy regimen. October 24, 2012: Weight of 26 kg, Up 1. 8 kg due to improved appetite while on steroid therapy. G-tube placed, continuous nocturnal feeding regimen initiated. December 6, 2012: Weight of 30. 9 kg and a weight-for-age percentile of 90 th. Weight improved significantly since g-tube placement. Had regained beyond UBW. March 4, 2013: Weight of 25. 2 kg (18% weight loss) due to feeding intolerance with g-tube feedings, severe abdominal pain, and emesis. The RD recommended interventions to advance back to goal feeds but recommendations were not implemented per the primary team. Main challenges with nutrition support: Significant frequency of N/V, intolerance to continuous feeds overnight (previous regimen bolus), infection at the g-tube site
Results What are the advantages and disadvantages to using parenteral nutrition support? • Advantages: Eliminates burden of oral intake, relieves tension between child and parent, electrolytes are easier to maintain with TPN, extra bolster of nutrition. • Disadvantages: Higher risk for infection, damaging to the liver. What are the advantages and disadvantages to using enteral nutrition support? Advantages: • NP: provide oral medication through tube, alleviate tension with child and parent, not as expensive as TPN, easier to administer. • RN: The ability to meet nutritional needs if the patient refuses to take all calories by mouth • RD: more physiologic, improved benefits in terms of maintaining the gut mucosa. less expensive than TPN and has lower risks for infection Disadvantages: • NP: “Children hate the NG tubes”, tube dislodgement during emesis, source of infection, gtube requires surgical placement. • RN: family and patient adapting to meeting all calorie needs via NGT/GT versus via mouth • RD: tube placement which may require surgery, uncomfortable nasoenteric tubes, possible self -image issues, patients with active mucositis without prior enteral access, team hesitant to place a tube that might irritate the mucositis or cause bleeding in a child with thrombocytopenia.
Results At what point do you feel that nutrition support is indicated in this patient population? • NP: weight loss of 5 -10% usual body weight • RD: lost >5 of their UBW, upcoming treatments , anticipated side effects when making recommendations, Anticipate PO intake in the interim, overall % weight loss, nutrition status prior to diagnosis • RN: Depends which attending is on service and how the parents feel about the lack of PO intake How do you feel nutrition management of the pediatric oncology patient could be improved? • Improved patient education handouts for clinic • Earlier initiation of nutritional support • RD to follow-up with patients in the outpatient clinic
Discussion • The quantitative data collected within this study showed that each of the three patients did not receive adequate nutritional support with EN during their admissions. • Data also showed that when nutrition support was initiated it was not advanced to the goal rate or was often delayed due to procedures during at least one admission date recorded for each patient.
Discussion • Each of the health care professionals identified the lack of protocols regarding the initiation of nutrition support as a barrier to initiating and optimizing nutritional support delivery. • The data from our study suggests nutrition management is not consistently being carried out per those guidelines despite timely and repeated RD recommendations. • The outpatient clinic was identified as an area where nutrition management is lacking, and that the presence of the RD in clinic would be beneficial.
Limitations • Small sample size (n=3) • Retrospective data collection from previous admissions • Intermittent data collection due to prolonged admissions or serial admissions • Limited target group for qualitative data collection
Future Research • Prospective study with daily serial data collection upon admission to more closely monitor recommendations and time/barriers to implementation. • Expand survey population for medical health professionals • Include families of patients in further qualitative data collection for a more robust and comprehensive perspective • Survey other facilities to compare protocols for nutrition intervention
Conclusions • In a few circumstances, the appropriate route of nutrition support, whether EN versus TPN, were utilized in an effective manner. • However, this was the exception rather than the norm. • The establishment of nutrition support protocols would uniformly provide pediatric oncology healthcare professions with guidelines for the timely initiation of appropriate nutritional support in our pediatric oncology patients and help to support normal growth and development during treatment.
Conclusions • Furthermore, the availability of an RD in the outpatient clinic is very important to having an effective medical staff in which to provide recommendations for nutritional support and information on symptom management in the pediatric oncology patient following the continuum of care.
Questions?
References
References, cont.
References, cont.

References, cont. 31. den Broeder E, Lippens R, Hof M, et al. Nasogastric Tube Feeding in Children with Cancer: The Effect of Two Different Formulas on Weight, Body Composition, and serum Protein Concentrations. Journal of Parenteral and Enteral Nutrition. 2000; 24 (6): 351 -360. 32. Markey T. , Nutritional Considerations in Pediatric Oncology. Journal of Oncology Nursing. 2000; 16 (2): 146 -151. 33. Bakish J, Bouffet E, Hargrave D, Laperriere N, Rutka J, Tariq N, . Evaluation of Dietetic Intervention in Children with Medulloblastoma or Supratentorial Primitive Neuroectodermal Tumors. Journal of American Cancer Society. 2003; 98 (5): 1014 -1020. 34. Aquino VM, Smryl CB, Hagg R, Mchard KM, Prestridge I, Sandler ES. Enteral Nutritional. Support by Gastrostomy Tube in Children with Cancer. Journal of Pediatrics. 1995; 1: 58 -62. 35. Azarnoush, Z, Bruno B, Beghin L, et al. Enteral Nutrition: a first option for nutritional support of children following allo-SCT. Bone Marrow Transplantation. 2012; 47: 1191 -1995 36. Garofolo A. , Enteral Nutrition During Bone Marrow Transplantation in Patients with Pediatric Cancer: A Prospective Cohort Study. Sao Paulo Medical Journal. 2012; 130 (3): 159 -166. 37. Christensen M, Gattuso J, Mc. Cormick J. Parenteral Nutrition Associated with Increased Infection Rate in Children with Cancer. Journal of Cancer. 1993; 72 (9): 2732 -2738. Cario MS, Spoone S, Sowden L, Bennetts GA, Towne B, Hodder F. Long-term use of indwelling multipurpose silastic catheters in pediatric patients treated with aggressive chemotherapy. Journal of Clinical Oncology. 1986; 4: 784 -788. 39. Sacks, G, Enhancing the Response to Parenteral Nutrition in Critical Care. Nutrition in Clinical Practice. 2003; 19: 226 -234. 40. Broeder E, Lippens R, Hof M, Tolboom J, Sengers R, Berg A, Houdt N, Hofman Z. Nasogastric Tube Feeding in Children with Cancer: The Effect of Two Different Formulas on Weight, Body Composition, and serum Protein Concentrations. Journal of Parenteral and Enteral Nutrition. 2000; 24 (6): 351 -360.
References, cont. 41. Fuchs GJ: Enteral Support of the Hospitalized Child. In: Textbook of Pediatric Nutrition, 2 nd edition, Suskind RM, Lewinter-Suskind L (eds. ). Raven Press, Ltd, New York, 1993: 230 -246. 42. Maroun J, Anthony L, Blais N, Burkes R, Dowden S: Prevention and Management of Chemotherapy-induced diarrhea in patients with colorectal cancer: a consensus statement by the Canadian Working Group on Chemotherapy-Induced Diarrhea. Current Oncology. 2007; 14 (1): 13 -20 43. American Cancer Society. Cancer Facts & Figures 2013. Atlanta: American Cancer Society. 2013; 1 -64 44. Devita, Hellman, and Rosenburg’s Cancer 2009: Nutrition Support 45. Locher J, Bonner J, Carroll W, Caudell J, Keith J, Kilgore M: Prophylactic Percutaneous Endoscopic Gastromy Tube Placement in Treatment of Head and Neck Cancer. Journal of Parenteral and Enteral Nutrition. 2011; 35 (3): 365 -374
 Nursing care of hospitalized child
Nursing care of hospitalized child Nursing care of hospitalized child
Nursing care of hospitalized child Pico questions
Pico questions Unc benign hematology
Unc benign hematology Pediatric board review course
Pediatric board review course Impact of nf1pn
Impact of nf1pn Feasible interesting novel ethical relevant
Feasible interesting novel ethical relevant Nutritional management of diabetes mellitus
Nutritional management of diabetes mellitus Achog
Achog Mylosuppresion
Mylosuppresion Management of patients with neurologic trauma
Management of patients with neurologic trauma Management of patients with neurologic trauma
Management of patients with neurologic trauma Periodontal management of medically compromised patients
Periodontal management of medically compromised patients Betragsoptimum symmetrisches optimum
Betragsoptimum symmetrisches optimum Perfectly discriminating monopolist
Perfectly discriminating monopolist Demand shifter
Demand shifter Optimal arousal theory
Optimal arousal theory Social optimum economics
Social optimum economics Optimum sports nutrition
Optimum sports nutrition Optimal inventory level
Optimal inventory level Bpimanager
Bpimanager Optimum weight gcse pe definition
Optimum weight gcse pe definition Optimum notch filter in digital image processing
Optimum notch filter in digital image processing Claim in literature
Claim in literature Interior optimum for utility maximization
Interior optimum for utility maximization Optimum pricing strategy
Optimum pricing strategy Ewz punkt optimum
Ewz punkt optimum Optimum ekonomiczne
Optimum ekonomiczne Optimum temperature for enzymes
Optimum temperature for enzymes Optimum hand hygiene steps
Optimum hand hygiene steps Rainfall
Rainfall Optimum temperature for enzymes
Optimum temperature for enzymes Optimum word scramble
Optimum word scramble Optimum volume
Optimum volume Optimal portfolio diversification
Optimal portfolio diversification Fms deep squat corrective exercises
Fms deep squat corrective exercises Crown root ratio
Crown root ratio Solusi optimum adalah
Solusi optimum adalah Optimum temperature for photosynthesis
Optimum temperature for photosynthesis Optimum temperature for photosynthesis
Optimum temperature for photosynthesis Nákladové optimum firmy
Nákladové optimum firmy Optimum global thresholding using otsu's method
Optimum global thresholding using otsu's method Baumol model assumptions
Baumol model assumptions