Oncology PatientCentered Medical Home Oncology Management Services Inc
- Slides: 43
Oncology Patient-Centered Medical Home Oncology Management Services, Inc Building the Business Case for Quality and Value John D. Sprandio, MD, FACP October 3, 2014 Not for redistribution. © 2013 Oncology Management Services, Consultants in Medical Oncology & Hematology
Patient-Centered Medical Home 1967 Standards of Child Health Care American Academy of Pediatrics 2007 Joint Principles of the PCMH American Medical Association American Association of Family Practitioners American Academy of Pediatrics American College of Physicians American Osteopathic Association Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
Joint Principles of PCMH 1. 2. 3. 4. 5. 6. 7. Personal physician coordinates comprehensive care. Physician directed medical team. Whole person orientation for all stages of life (acute, chronic, preventive, and end-of-life care). Coordinated and integrated care across all aspects of the health care system utilizing information technology. Quality and safety with continuous quality improvement and recognition by a non-governmental body. Enhanced access through open scheduling and new communication tools. Appropriate payment recognizing the added value with the model. Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
NCQA Primary Care Recognition Six Standards (validated, tested elements & features) 1. Enhanced Access and Continuity 2. Identify and Manage Populations 3. Plan and Manage Care 4. Provide Self-care Support and Community Resources 5. Track and Coordinate Care 6. Measure and Improve Performance www. ncqa. org Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
Medical Neighborhood American College of Physicians Council of Subspecialty Societies (CSS), Policy Paper 2010 n Addressed relationship between primary care PCMH model and specialty/subspecialty practices n Highlights: n Established definition of Patient Centered Medical Home Neighbor n Approved a framework to categorize interactions between PCMH and PCMH - N n Approved guiding principles of the development of care-coordination agreements between PCMH and PCMH-N Neil Kirschner, Ph. D. American College of Physicians, Senior Associate Regulatory and Insurer Affairs Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
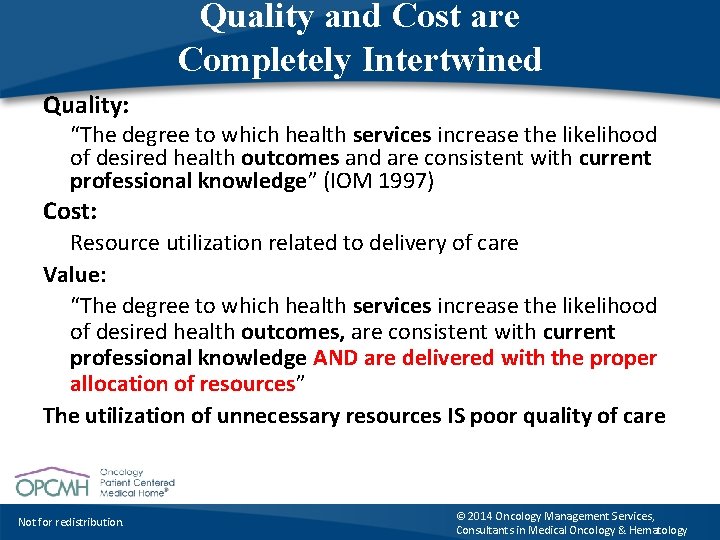
Quality and Cost are Completely Intertwined Quality: “The degree to which health services increase the likelihood of desired health outcomes and are consistent with current professional knowledge” (IOM 1997) Cost: Resource utilization related to delivery of care Value: “The degree to which health services increase the likelihood of desired health outcomes, are consistent with current professional knowledge AND are delivered with the proper allocation of resources” The utilization of unnecessary resources IS poor quality of care Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
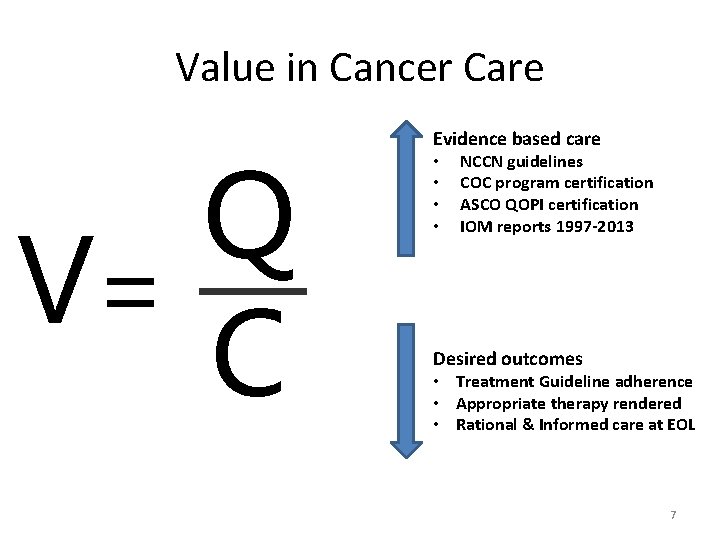
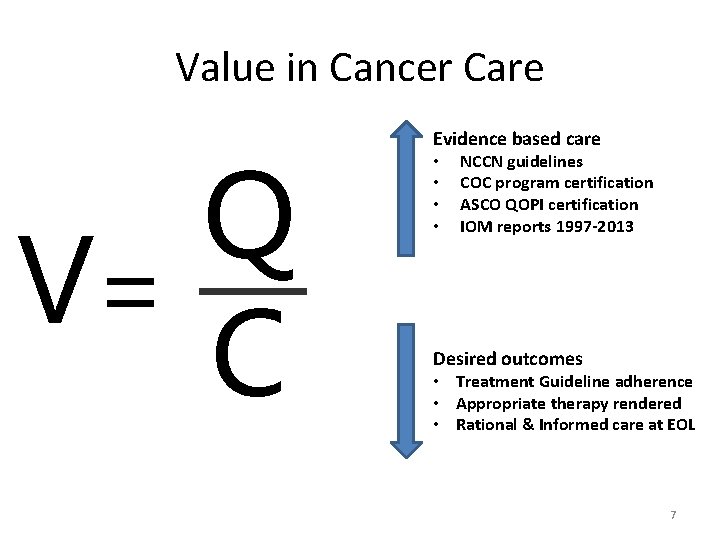
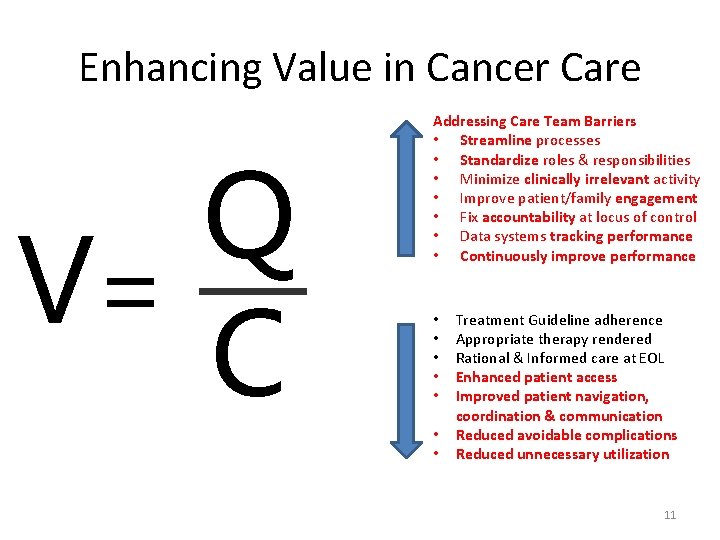
Value in Cancer Care Q V= C Evidence based care • • NCCN guidelines COC program certification ASCO QOPI certification IOM reports 1997 -2013 Desired outcomes • Treatment Guideline adherence • Appropriate therapy rendered • Rational & Informed care at EOL 7
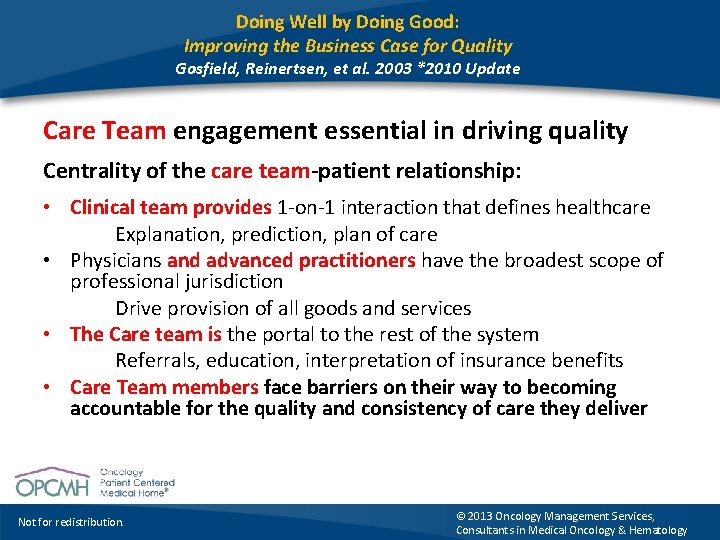
Doing Well by Doing Good: Improving the Business Case for Quality Gosfield, Reinertsen, et al. 2003 *2010 Update Care Team engagement essential in driving quality Centrality of the care team-patient relationship: • Clinical team provides 1 -on-1 interaction that defines healthcare Explanation, prediction, plan of care • Physicians and advanced practitioners have the broadest scope of professional jurisdiction Drive provision of all goods and services • The Care team is the portal to the rest of the system Referrals, education, interpretation of insurance benefits • Care Team members face barriers on their way to becoming accountable for the quality and consistency of care they deliver Not for redistribution. © 2013 Oncology Management Services, Consultants in Medical Oncology & Hematology
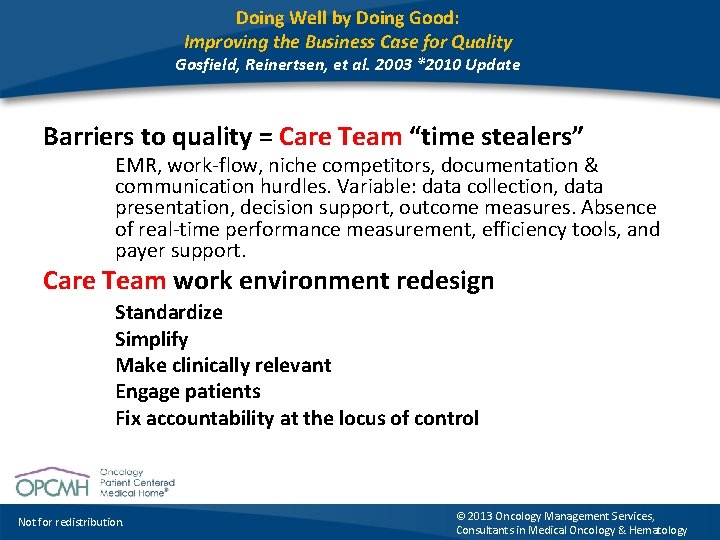
Doing Well by Doing Good: Improving the Business Case for Quality Gosfield, Reinertsen, et al. 2003 *2010 Update Barriers to quality = Care Team “time stealers” EMR, work-flow, niche competitors, documentation & communication hurdles. Variable: data collection, data presentation, decision support, outcome measures. Absence of real-time performance measurement, efficiency tools, and payer support. Care Team work environment redesign Standardize Simplify Make clinically relevant Engage patients Fix accountability at the locus of control Not for redistribution. © 2013 Oncology Management Services, Consultants in Medical Oncology & Hematology
Creating Value • Care Team Work Environment 2003 • Addressing barriers to consistency and accountability • • Standardization of oncology processes Value Proposition Scalability Payer Response Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
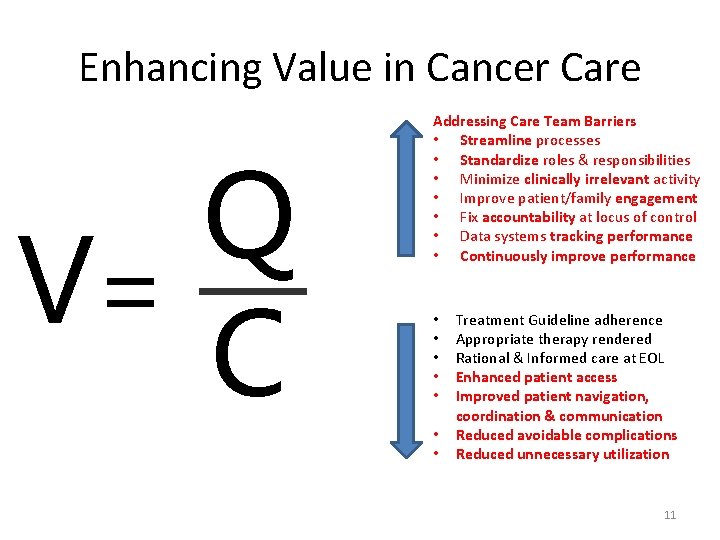
Enhancing Value in Cancer Care Q V= C Addressing Care Team Barriers • Streamline processes • Standardize roles & responsibilities • Minimize clinically irrelevant activity • Improve patient/family engagement • Fix accountability at locus of control • Data systems tracking performance • Continuously improve performance • • Treatment Guideline adherence Appropriate therapy rendered Rational & Informed care at EOL Enhanced patient access Improved patient navigation, coordination & communication Reduced avoidable complications Reduced unnecessary utilization 11
Oncology Patient-Centered Medical Home® • NCQA level III, PCMH recognition April 2010 • Integrated care delivery model for hematology & oncology • PCMH principles: access, engagement, shared decisions, coordination, communication and accountability • Medical oncology serves as the hub of coordination and accountability in meeting cancer care needs • Integrates Primary PCMH, surgical, radiation oncology, inpatient, social, hospice services via information hub • Value Proposition: Better cancer care, health, lower cost • Payer recognition, integration with ACOs, Clinically Integrated Networks Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
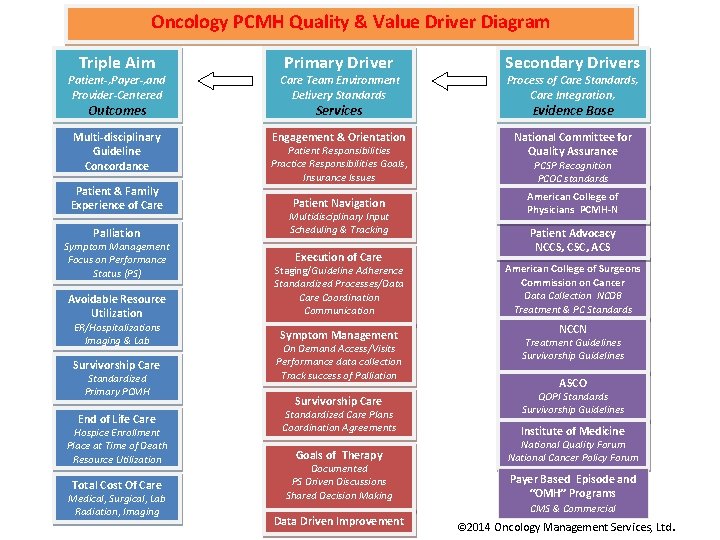
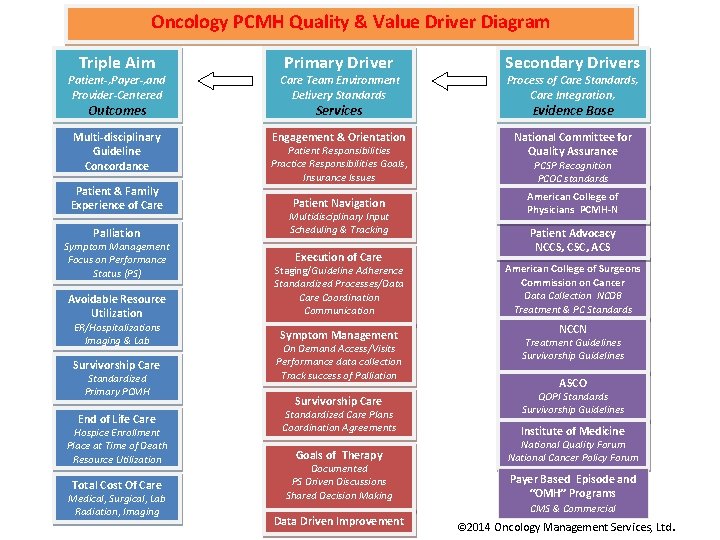
Oncology PCMH Quality & Value Driver Diagram Triple Aim Primary Driver Patient-, Payer-, and Provider-Centered Care Team Environment Delivery Standards Multi-disciplinary Guideline Concordance Engagement & Orientation Outcomes Patient & Family Experience of Care Services Patient Responsibilities Practice Responsibilities Goals, Insurance Issues Patient Navigation Palliation Multidisciplinary Input Scheduling & Tracking Avoidable Resource Utilization Staging/Guideline Adherence Standardized Processes/Data Care Coordination Communication Symptom Management Focus on Performance Status (PS) ER/Hospitalizations Imaging & Lab Survivorship Care Standardized Primary PCMH End of Life Care Hospice Enrollment Place at Time of Death Resource Utilization Total Cost Of Care Medical, Surgical, Lab Radiation, Imaging Execution of Care Symptom Management On Demand Access/Visits Performance data collection Track success of Palliation Survivorship Care Standardized Care Plans Coordination Agreements Goals of Therapy Documented PS Driven Discussions Shared Decision Making Data Driven Improvement Secondary Drivers Process of Care Standards, Care Integration, Evidence Base National Committee for Quality Assurance PCSP Recognition PCOC standards American College of Physicians PCMH-N Patient Advocacy NCCS, CSC, ACS American College of Surgeons Commission on Cancer Data Collection NCDB Treatment & PC Standards NCCN Treatment Guidelines Survivorship Guidelines ASCO QOPI Standards Survivorship Guidelines Institute of Medicine National Quality Forum National Cancer Policy Forum Payer Based Episode and “OMH” Programs CMS & Commercial © 2014 Oncology Management Services, Ltd.
Creating Value • • • Care Team Work Environment Standardization of oncology care processes Value Proposition Scalability Payer Response Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
Standardization of Oncology PCMH Processes Consistent approach by the care team • • Not for redistribution. Patient Engagement & Orientation Patient Navigation Shared Decision-Making Execution of Care coordination Symptom Management Survivorship Care Goals of therapy © 2013 Oncology Management Services, Consultants in Medical Oncology & Hematology
Standardization of Oncology PCMH Processes • Patient Engagement & Orientation • • • • Define role of nurse and patient navigators, physicians, etc Modes of enhanced access & coordination defined Financial counseling – details of insurance coverage Patient reporting & practice responsibilities Practice as “Point of First Triage” Symptom and disease management strategies (nurse triage) Patient Portal education Patient Navigation Shared Decision-Making Execution of Care coordination Symptom Management Survivorship Care Goals of therapy Not for redistribution. © 2013 Oncology Management Services, Consultants in Medical Oncology & Hematology
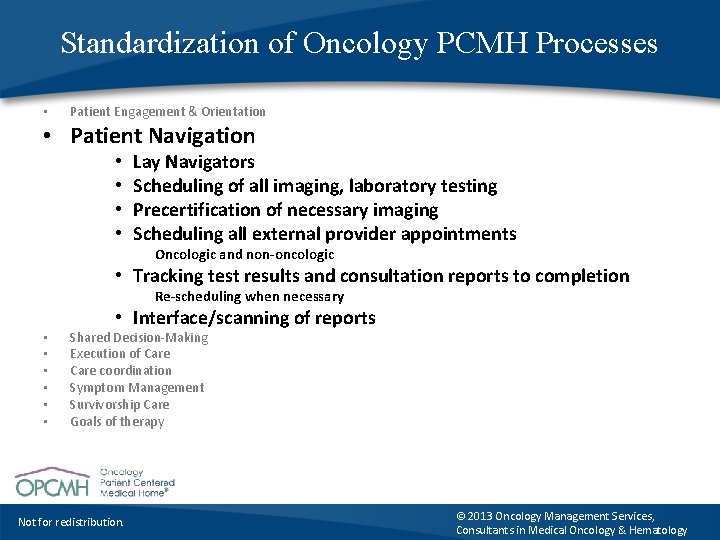
Standardization of Oncology PCMH Processes • Patient Engagement & Orientation • Patient Navigation • • Lay Navigators Scheduling of all imaging, laboratory testing Precertification of necessary imaging Scheduling all external provider appointments Oncologic and non-oncologic • Tracking test results and consultation reports to completion Re-scheduling when necessary • • Interface/scanning of reports Shared Decision-Making Execution of Care coordination Symptom Management Survivorship Care Goals of therapy Not for redistribution. © 2013 Oncology Management Services, Consultants in Medical Oncology & Hematology
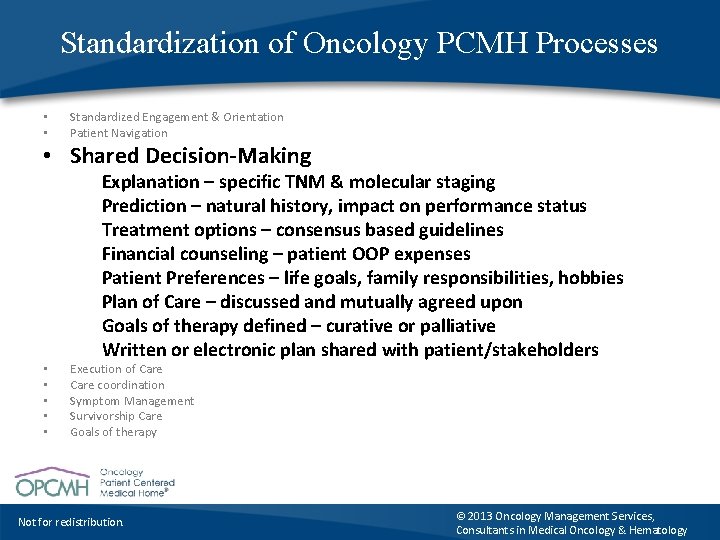
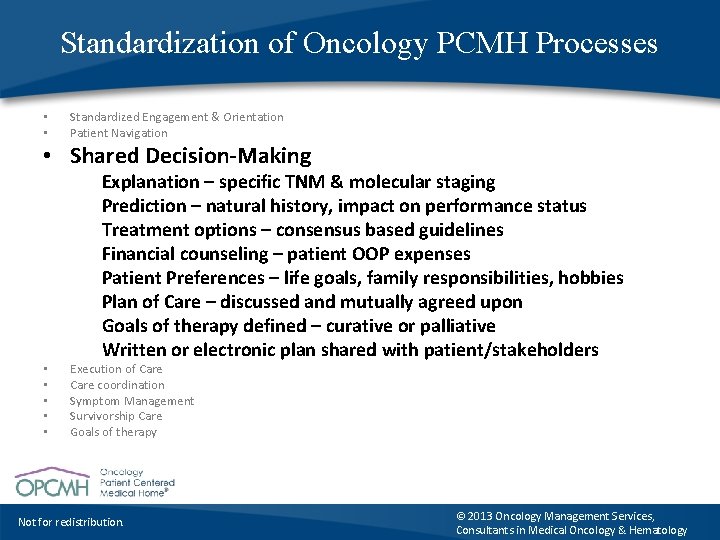
Standardization of Oncology PCMH Processes • • Standardized Engagement & Orientation Patient Navigation • Shared Decision-Making • • • Explanation – specific TNM & molecular staging Prediction – natural history, impact on performance status Treatment options – consensus based guidelines Financial counseling – patient OOP expenses Patient Preferences – life goals, family responsibilities, hobbies Plan of Care – discussed and mutually agreed upon Goals of therapy defined – curative or palliative Written or electronic plan shared with patient/stakeholders Execution of Care coordination Symptom Management Survivorship Care Goals of therapy Not for redistribution. © 2013 Oncology Management Services, Consultants in Medical Oncology & Hematology
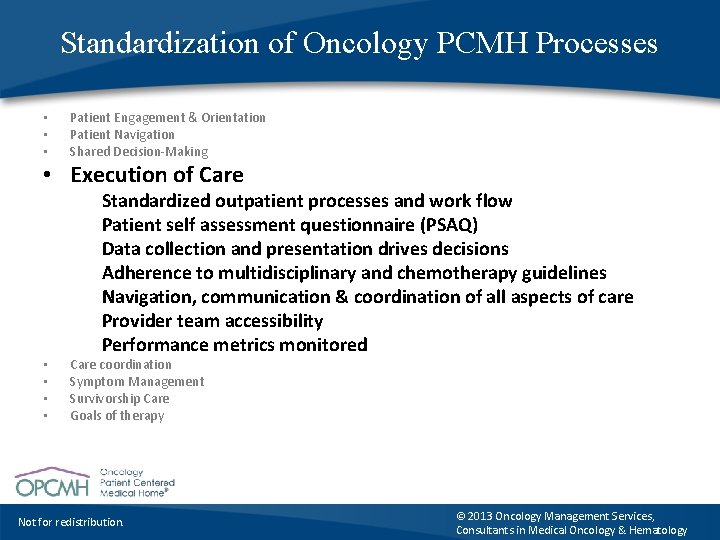
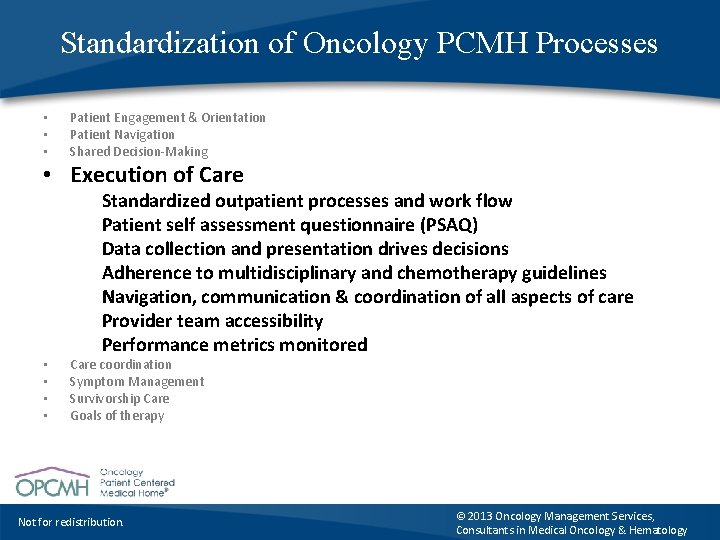
Standardization of Oncology PCMH Processes • • • Patient Engagement & Orientation Patient Navigation Shared Decision-Making • Execution of Care • • Standardized outpatient processes and work flow Patient self assessment questionnaire (PSAQ) Data collection and presentation drives decisions Adherence to multidisciplinary and chemotherapy guidelines Navigation, communication & coordination of all aspects of care Provider team accessibility Performance metrics monitored Care coordination Symptom Management Survivorship Care Goals of therapy Not for redistribution. © 2013 Oncology Management Services, Consultants in Medical Oncology & Hematology
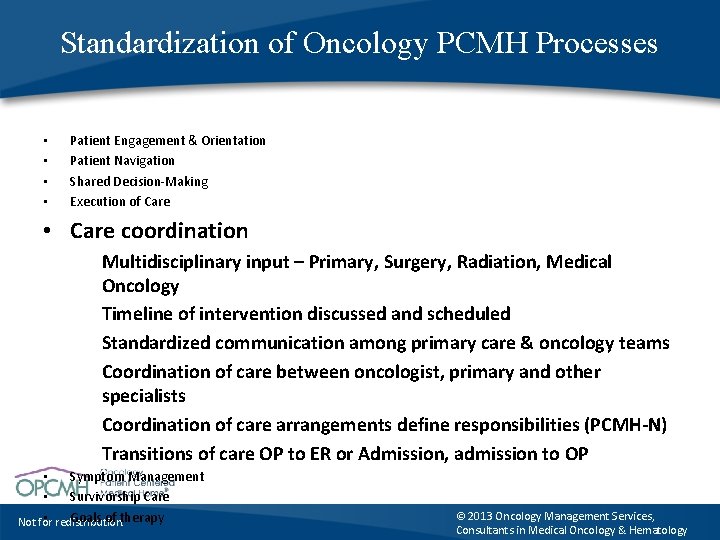
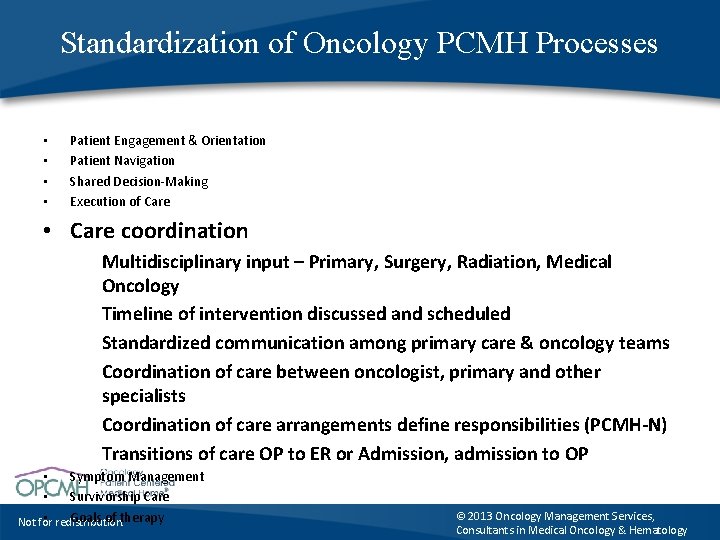
Standardization of Oncology PCMH Processes • • Patient Engagement & Orientation Patient Navigation Shared Decision-Making Execution of Care • Care coordination Multidisciplinary input – Primary, Surgery, Radiation, Medical Oncology Timeline of intervention discussed and scheduled Standardized communication among primary care & oncology teams Coordination of care between oncologist, primary and other specialists Coordination of care arrangements define responsibilities (PCMH-N) Transitions of care OP to ER or Admission, admission to OP • Symptom Management • Survivorship Care • redistribution. Goals of therapy Not for © 2013 Oncology Management Services, Consultants in Medical Oncology & Hematology
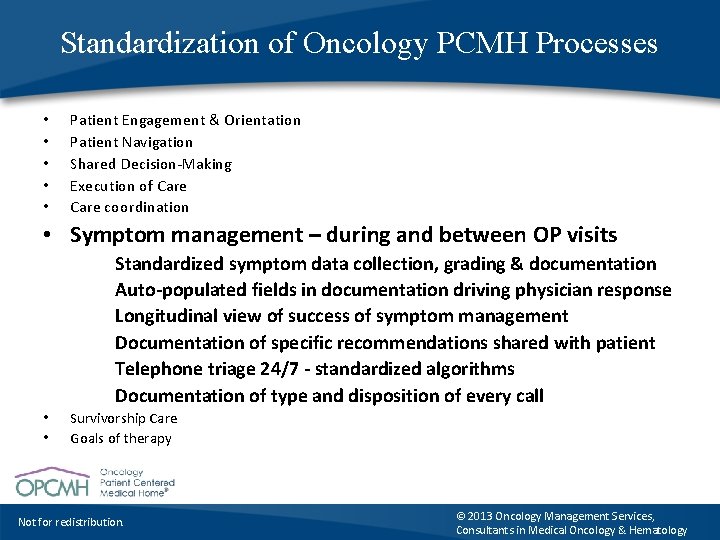
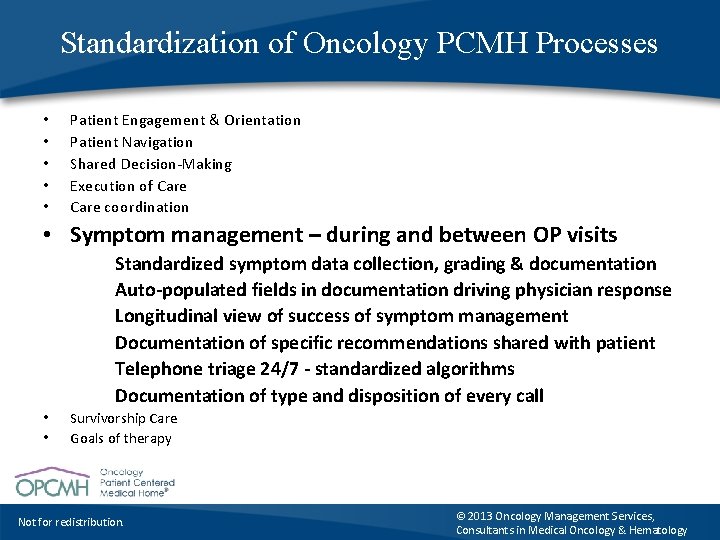
Standardization of Oncology PCMH Processes • • • Patient Engagement & Orientation Patient Navigation Shared Decision-Making Execution of Care coordination • Symptom management – during and between OP visits Standardized symptom data collection, grading & documentation Auto-populated fields in documentation driving physician response Longitudinal view of success of symptom management Documentation of specific recommendations shared with patient Telephone triage 24/7 - standardized algorithms Documentation of type and disposition of every call • • Survivorship Care Goals of therapy Not for redistribution. © 2013 Oncology Management Services, Consultants in Medical Oncology & Hematology
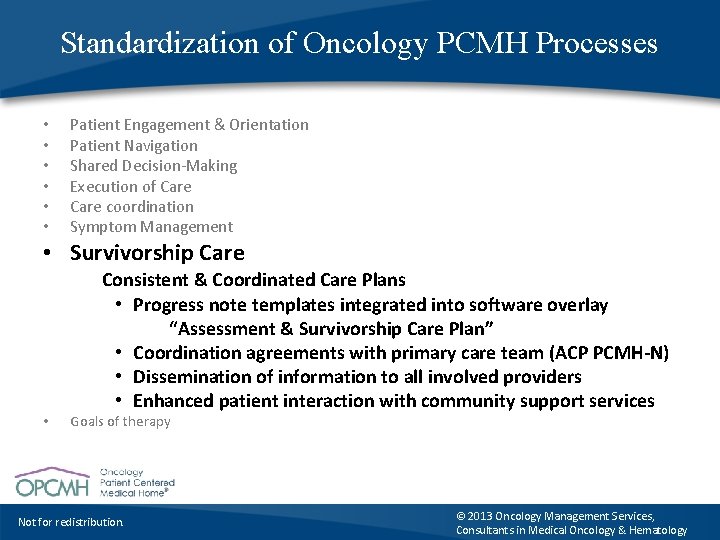
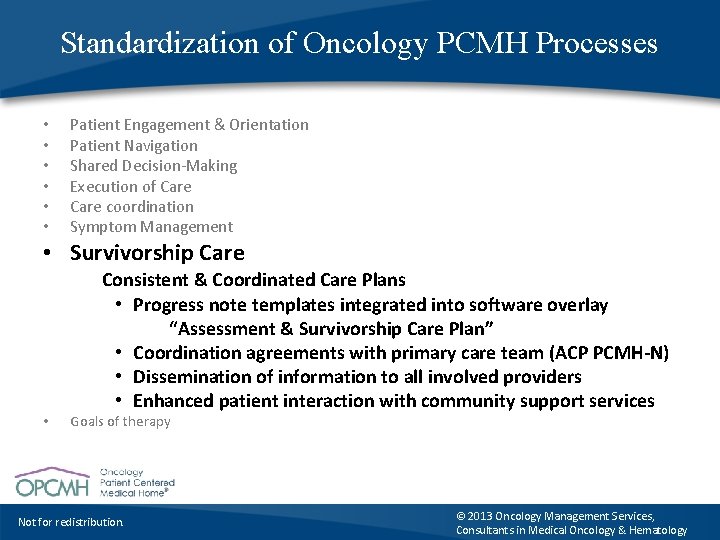
Standardization of Oncology PCMH Processes • • • Patient Engagement & Orientation Patient Navigation Shared Decision-Making Execution of Care coordination Symptom Management • Survivorship Care • Consistent & Coordinated Care Plans • Progress note templates integrated into software overlay “Assessment & Survivorship Care Plan” • Coordination agreements with primary care team (ACP PCMH-N) • Dissemination of information to all involved providers • Enhanced patient interaction with community support services Goals of therapy Not for redistribution. © 2013 Oncology Management Services, Consultants in Medical Oncology & Hematology
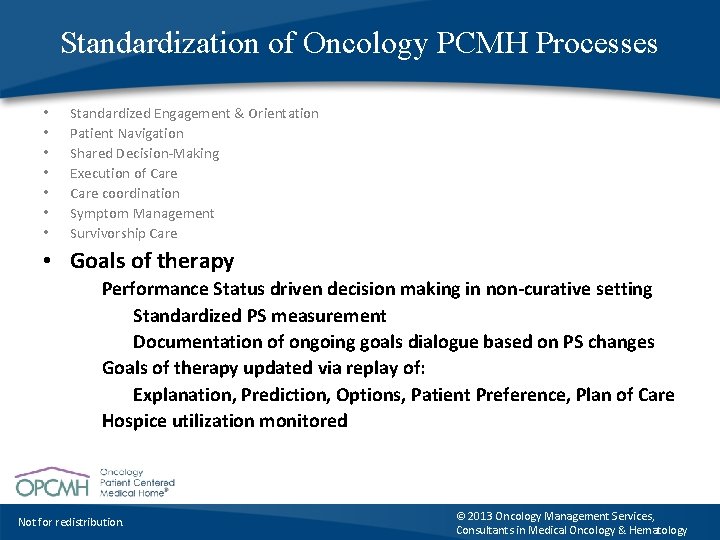
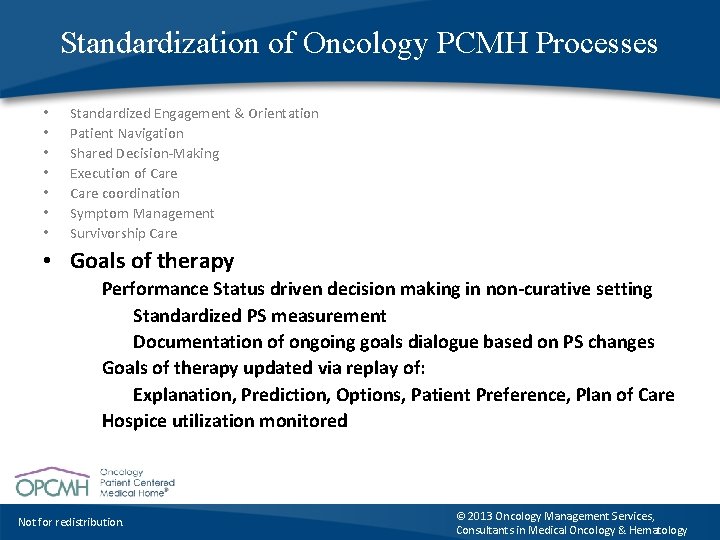
Standardization of Oncology PCMH Processes • • Standardized Engagement & Orientation Patient Navigation Shared Decision-Making Execution of Care coordination Symptom Management Survivorship Care • Goals of therapy Performance Status driven decision making in non-curative setting Standardized PS measurement Documentation of ongoing goals dialogue based on PS changes Goals of therapy updated via replay of: Explanation, Prediction, Options, Patient Preference, Plan of Care Hospice utilization monitored Not for redistribution. © 2013 Oncology Management Services, Consultants in Medical Oncology & Hematology
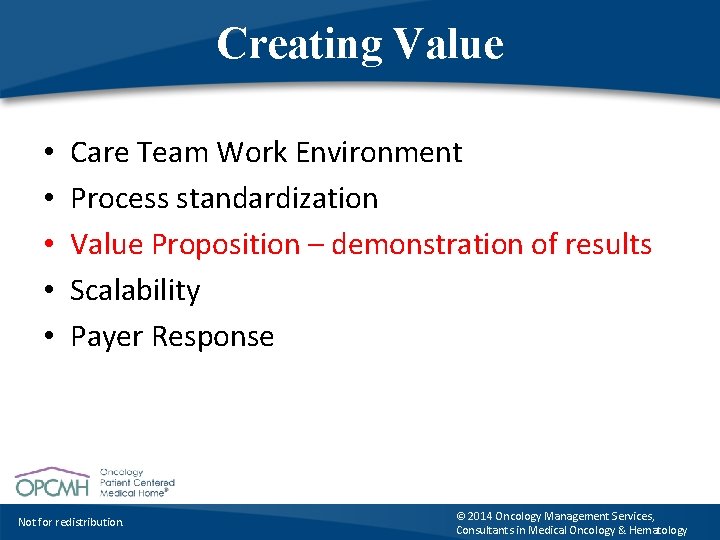
Creating Value • • • Care Team Work Environment Process standardization Value Proposition – demonstration of results Scalability Payer Response Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
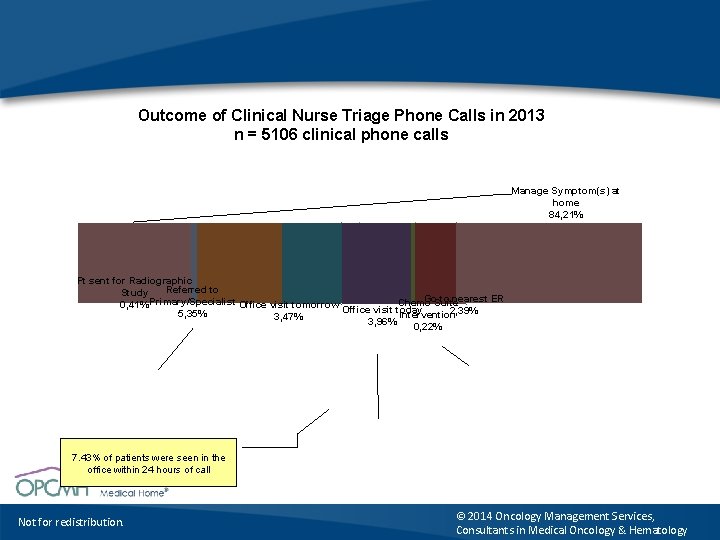
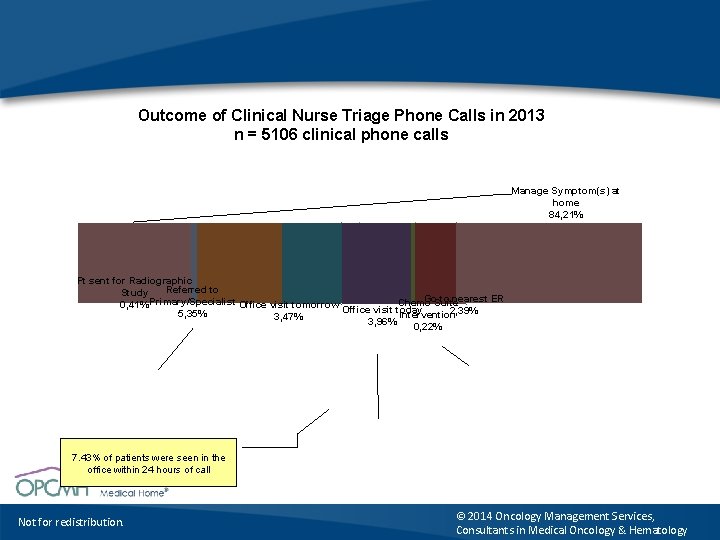
Outcome of Clinical Nurse Triage Phone Calls in 2013 n = 5106 clinical phone calls Manage Symptom(s) at home 84, 21% Pt sent for Radiographic Referred to Study Go. Suite to nearest ER Chemo 0, 41% Primary/Specialist Office visit tomorrow Office visit today 2, 39% 5, 35% Intervention 3, 47% 3, 96% 0, 22% 7. 43% of patients were seen in the office within 24 hours of call Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
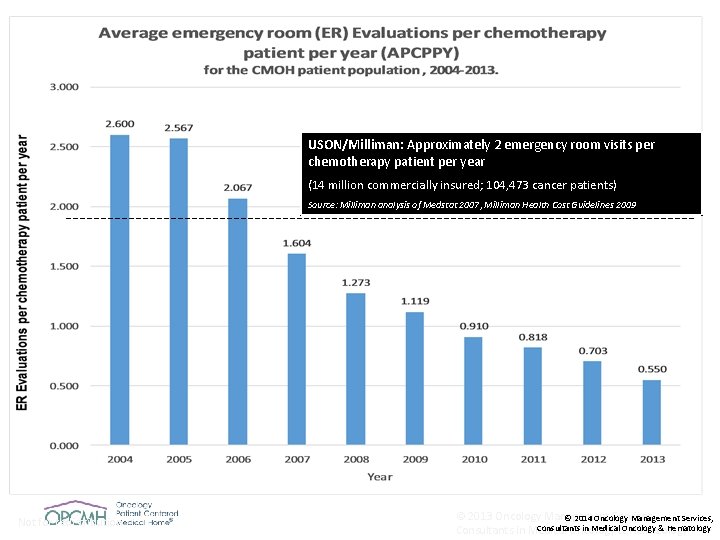
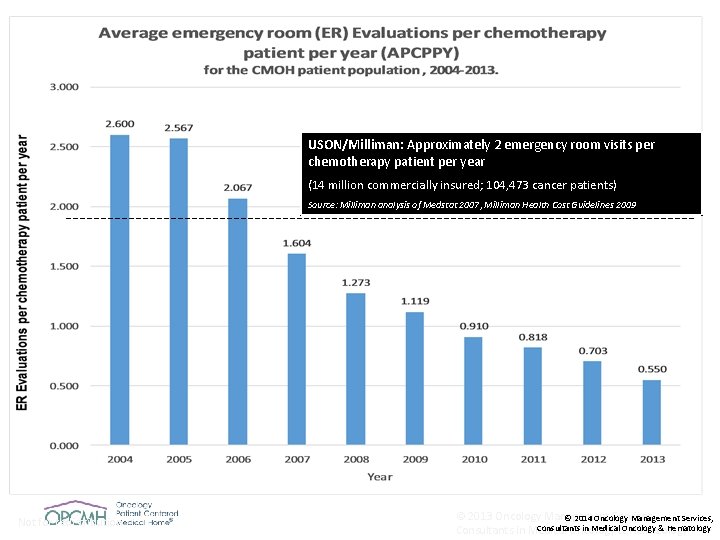
USON/Milliman: Approximately 2 emergency room visits per chemotherapy patient per year (14 million commercially insured; 104, 473 cancer patients) Source: Milliman analysis of Medstat 2007, Milliman Health Cost Guidelines 2009 Not for redistribution. © 2013 Oncology Management Services, © 2014 Oncology Management Services, Consultants in Medical&Oncology & Hematology Consultants in Medical Oncology Hematology
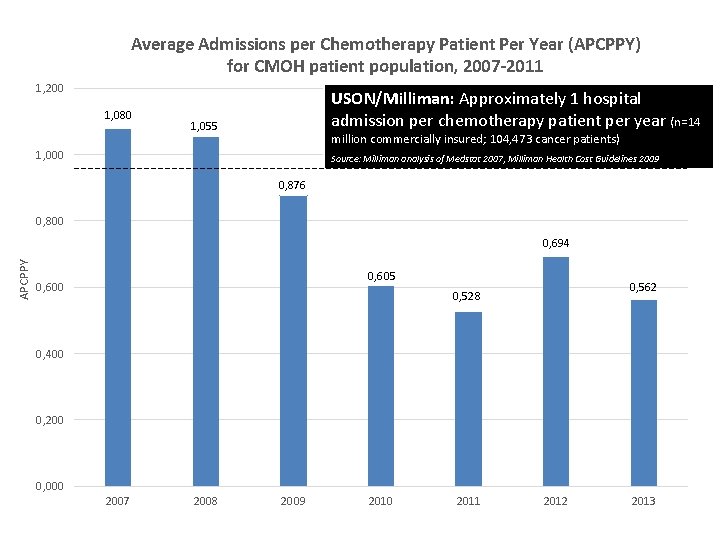
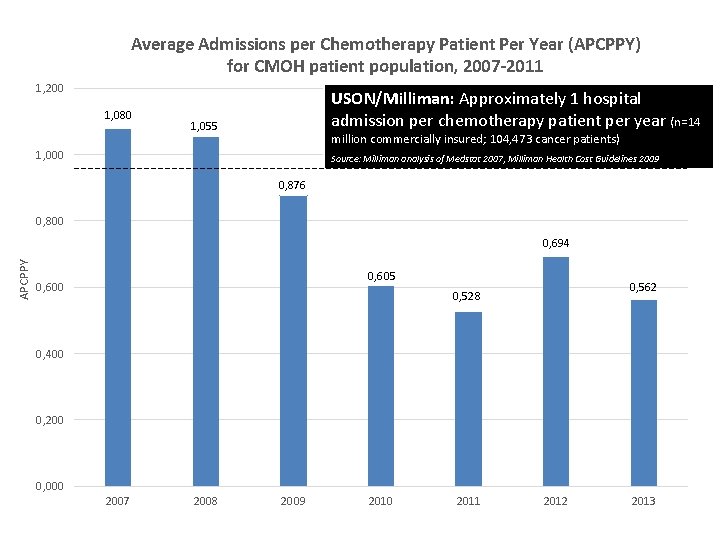
Average Admissions per Chemotherapy Patient Per Year (APCPPY) for CMOH patient population, 2007 -2011 1, 200 1, 080 USON/Milliman: Approximately 1 hospital admission per chemotherapy patient per year (n=14 1, 055 million commercially insured; 104, 473 cancer patients) 1, 000 Source: Milliman analysis of Medstat 2007, Milliman Health Cost Guidelines 2009 0, 876 0, 800 APCPPY 0, 694 0, 605 0, 600 0, 562 0, 528 0, 400 0, 200 0, 000 2007 2008 2009 2010 2011 2012 2013
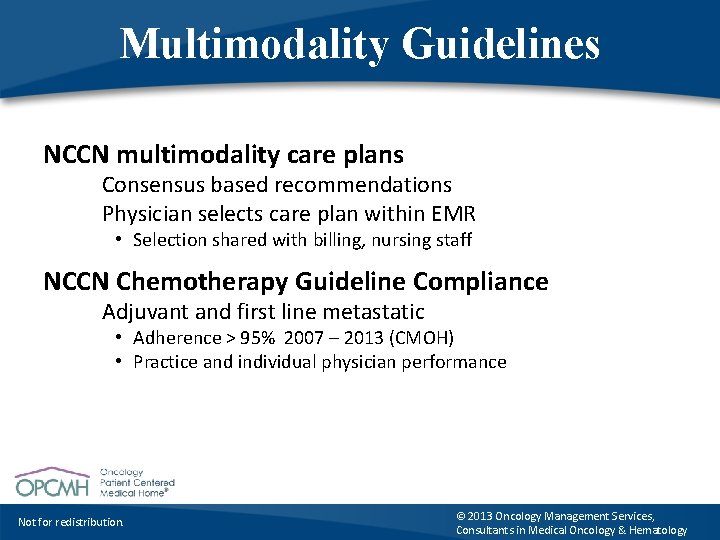
Multimodality Guidelines NCCN multimodality care plans Consensus based recommendations Physician selects care plan within EMR • Selection shared with billing, nursing staff NCCN Chemotherapy Guideline Compliance Adjuvant and first line metastatic • Adherence > 95% 2007 – 2013 (CMOH) • Practice and individual physician performance Not for redistribution. © 2013 Oncology Management Services, Consultants in Medical Oncology & Hematology
Oncology PCMH Palliative Care Concurrent delivery of palliative care • Comprehensive health assessment each visit • Symptoms: patient defined, RN/MA confirmed, physician accountable to respond • NCI graded and longitudinally viewed • Dynamic problem list of symptoms, co-morbid conditions Documentation of ongoing management Use of standardized approaches and instructions Patient view of documentation via portal Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
Oncology PCMH End of Life Care Performance Status Driven Decision-Making • PS: patient defined, RN/MA documentation, physicians accountable to respond PSAQ, ECOG grading (fixed), physician prompt • PS longitudinally viewed by patient and physician • Physician accountability Systems that monitor for changes in PS (ECOG 3) Documentation of rationale for continuation of therapy Transparency of discussion of goals Patient visibility of documentation via portal Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
Oncology PCMH Survivorship Care team: NP/PA + physician collaboration • • Survivorship care plan templates (ASCO) Clinical summary (toxicities, co-morbidities) Documentation of management of residual symptoms Treatment summary, genetic testing, family history Surveillance and screening activities, immunizations Community resource utilization Coordination of care arrangements in survivorship Responsibility matrix defined Primary PCMH, Oncology PCMH, Radiation and Surgical teams • Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
Oncology PCMH Transitions of Care Transition responsibility: facilitating hand-offs • Symptomatic patients with an apparent new malignancy from ER, Primary PCMH or specialist office • Oncology team drives efficiency, shortening timeline to diagnosis, symptom control and treatment • Symptom control = reduced unnecessary ER visits, admission • From oncology office to ER or inpatient admission • Transfer of information to accepting parties • Notification to Primary PCMH team • From acute care to outpatient or skilled care • Scheduling of all testing, consultation and follow-up visits • Notification to Primary PCMH team Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
Creating Value • • • Care Team Work Environment Process standardization Value Proposition Scalability Payer Response Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
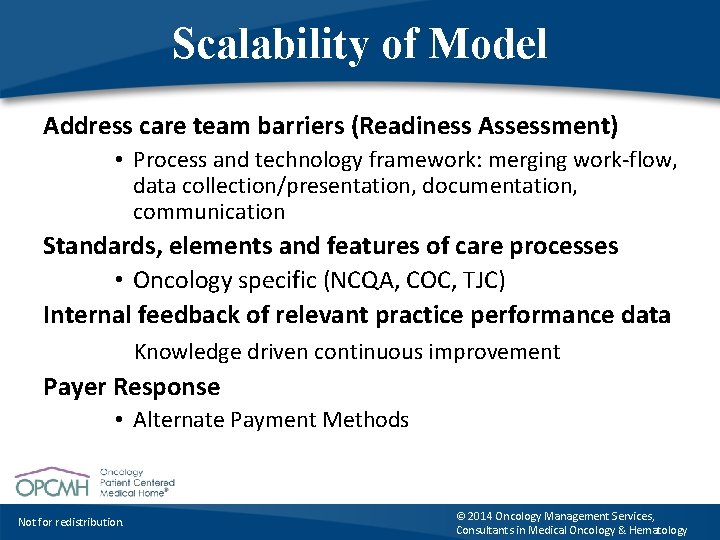
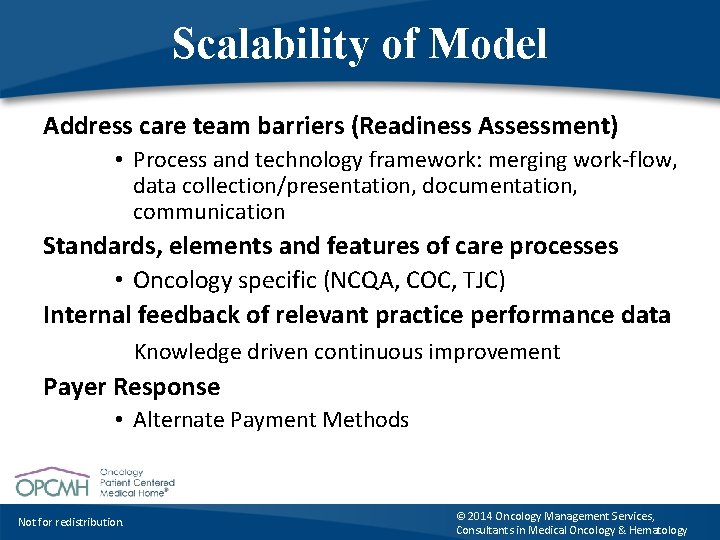
Scalability of Model Address care team barriers (Readiness Assessment) • Process and technology framework: merging work-flow, data collection/presentation, documentation, communication Standards, elements and features of care processes • Oncology specific (NCQA, COC, TJC) Internal feedback of relevant practice performance data Knowledge driven continuous improvement Payer Response • Alternate Payment Methods Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
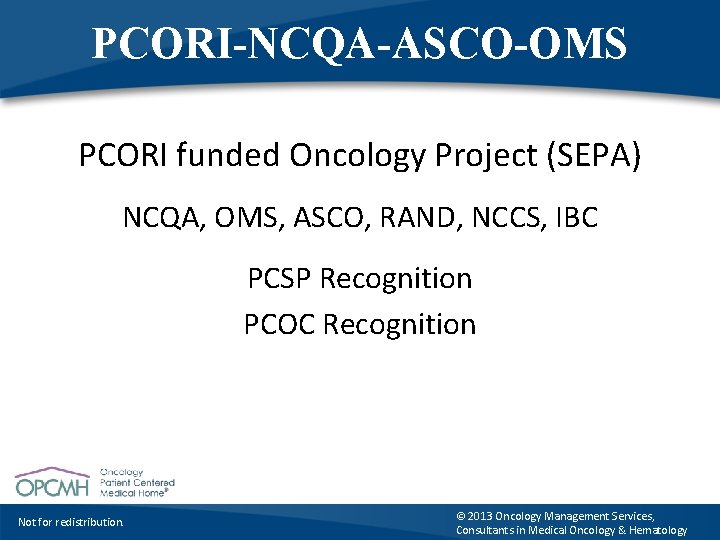
PCORI-NCQA-ASCO-OMS PCORI funded Oncology Project (SEPA) NCQA, OMS, ASCO, RAND, NCCS, IBC PCSP Recognition PCOC Recognition Not for redistribution. © 2013 Oncology Management Services, Consultants in Medical Oncology & Hematology
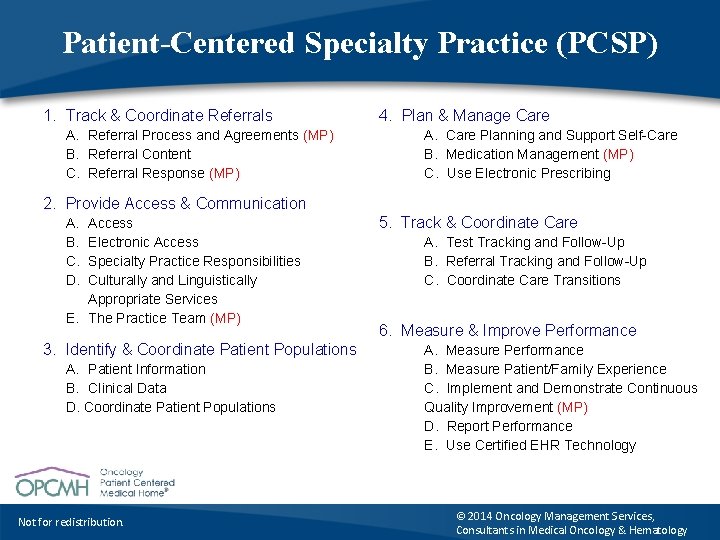
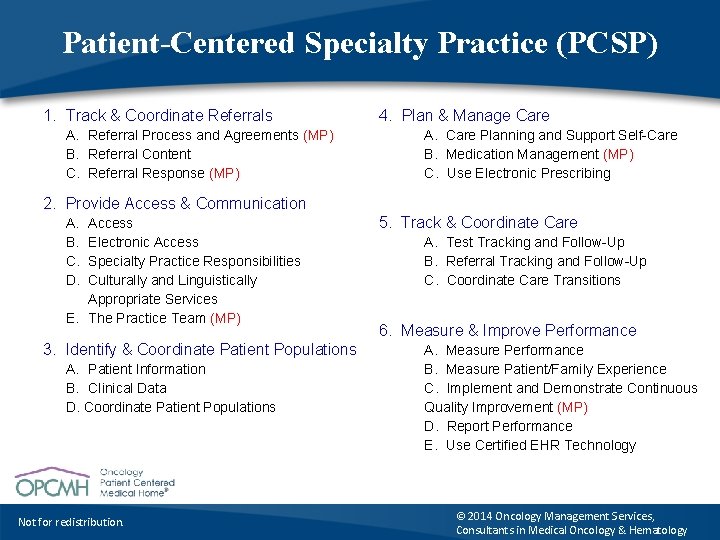
Patient-Centered Specialty Practice (PCSP) 1. Track & Coordinate Referrals A. Referral Process and Agreements (MP) B. Referral Content C. Referral Response (MP) 4. Plan & Manage Care A. Care Planning and Support Self-Care B. Medication Management (MP) C. Use Electronic Prescribing 2. Provide Access & Communication A. B. C. D. Access Electronic Access Specialty Practice Responsibilities Culturally and Linguistically Appropriate Services E. The Practice Team (MP) 3. Identify & Coordinate Patient Populations A. Patient Information B. Clinical Data D. Coordinate Patient Populations Not for redistribution. 5. Track & Coordinate Care A. Test Tracking and Follow-Up B. Referral Tracking and Follow-Up C. Coordinate Care Transitions 6. Measure & Improve Performance A. Measure Performance B. Measure Patient/Family Experience C. Implement and Demonstrate Continuous Quality Improvement (MP) D. Report Performance E. Use Certified EHR Technology © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
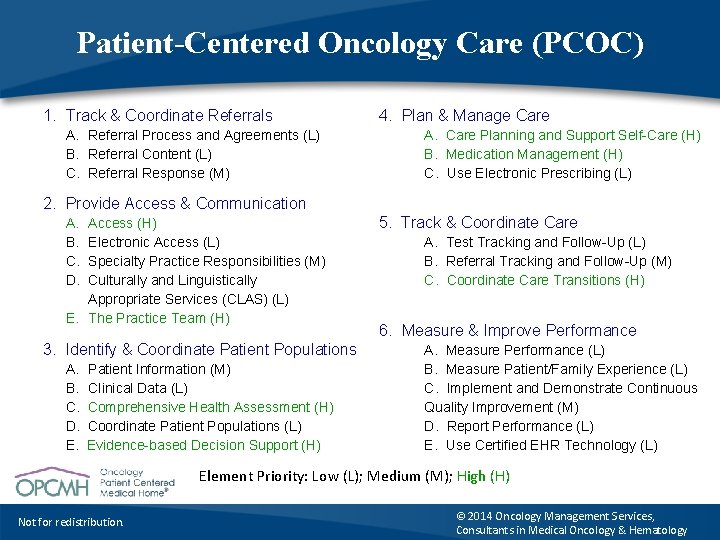
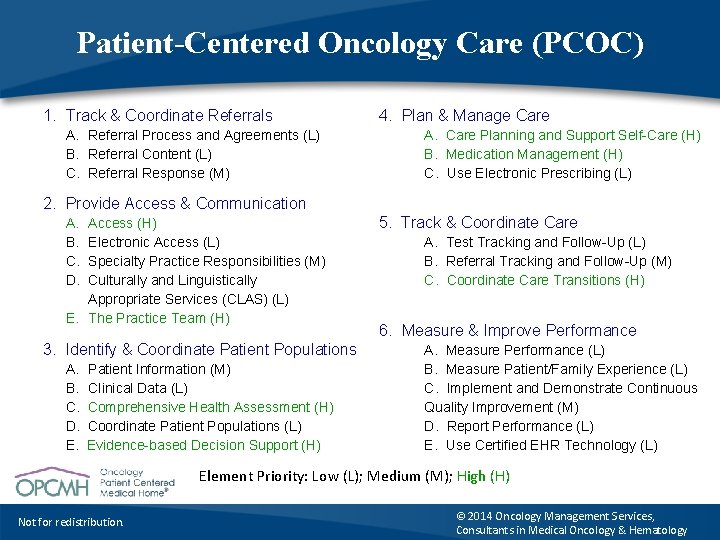
Patient-Centered Oncology Care (PCOC) 1. Track & Coordinate Referrals A. Referral Process and Agreements (L) B. Referral Content (L) C. Referral Response (M) 4. Plan & Manage Care A. Care Planning and Support Self-Care (H) B. Medication Management (H) C. Use Electronic Prescribing (L) 2. Provide Access & Communication A. B. C. D. Access (H) Electronic Access (L) Specialty Practice Responsibilities (M) Culturally and Linguistically Appropriate Services (CLAS) (L) E. The Practice Team (H) 3. Identify & Coordinate Patient Populations A. B. C. D. E. Patient Information (M) Clinical Data (L) Comprehensive Health Assessment (H) Coordinate Patient Populations (L) Evidence-based Decision Support (H) 5. Track & Coordinate Care A. Test Tracking and Follow-Up (L) B. Referral Tracking and Follow-Up (M) C. Coordinate Care Transitions (H) 6. Measure & Improve Performance A. Measure Performance (L) B. Measure Patient/Family Experience (L) C. Implement and Demonstrate Continuous Quality Improvement (M) D. Report Performance (L) E. Use Certified EHR Technology (L) Element Priority: Low (L); Medium (M); High (H) Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
Creating Value • • • Care Team Work Environment Process standardization Value Proposition Scalability Payer Response Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
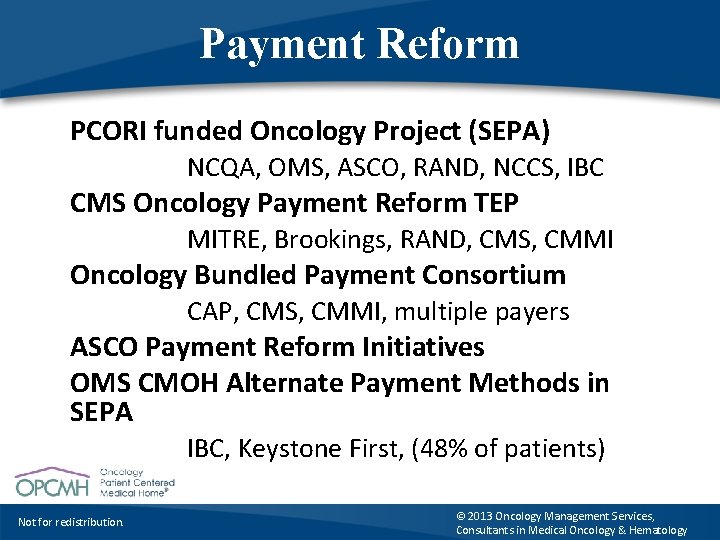
Payment Reform PCORI funded Oncology Project (SEPA) NCQA, OMS, ASCO, RAND, NCCS, IBC CMS Oncology Payment Reform TEP MITRE, Brookings, RAND, CMS, CMMI Oncology Bundled Payment Consortium CAP, CMS, CMMI, multiple payers ASCO Payment Reform Initiatives OMS CMOH Alternate Payment Methods in SEPA IBC, Keystone First, (48% of patients) Not for redistribution. © 2013 Oncology Management Services, Consultants in Medical Oncology & Hematology
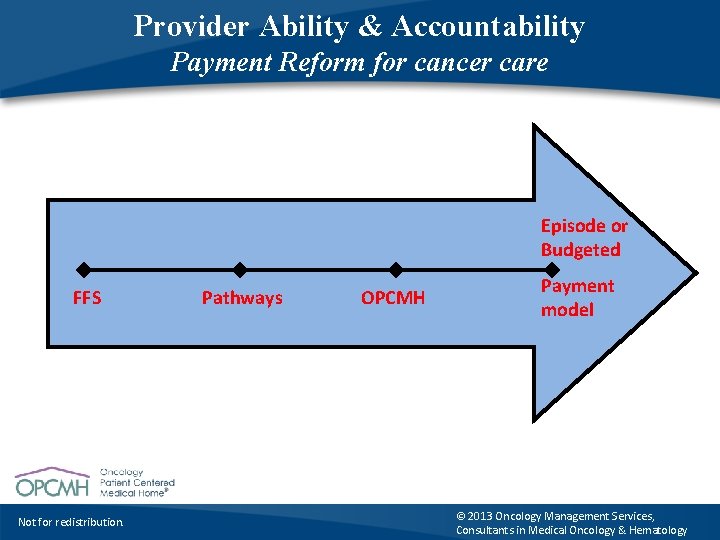
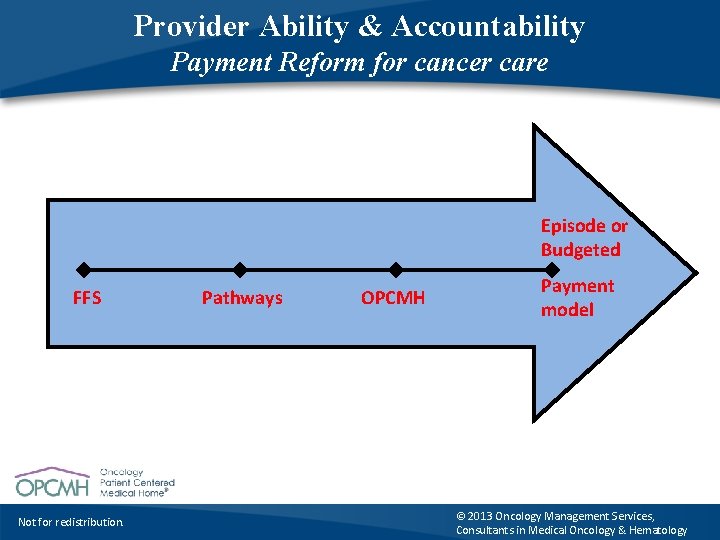
Provider Ability & Accountability Payment Reform for cancer care Episode or Budgeted FFS Not for redistribution. Pathways OPCMH Payment model © 2013 Oncology Management Services, Consultants in Medical Oncology & Hematology
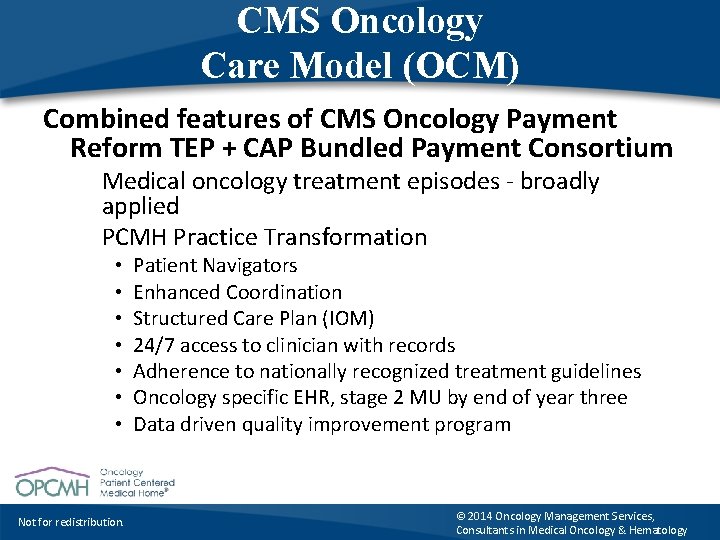
CMS Oncology Care Model (OCM) Combined features of CMS Oncology Payment Reform TEP + CAP Bundled Payment Consortium Medical oncology treatment episodes - broadly applied PCMH Practice Transformation • • Not for redistribution. Patient Navigators Enhanced Coordination Structured Care Plan (IOM) 24/7 access to clinician with records Adherence to nationally recognized treatment guidelines Oncology specific EHR, stage 2 MU by end of year three Data driven quality improvement program © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
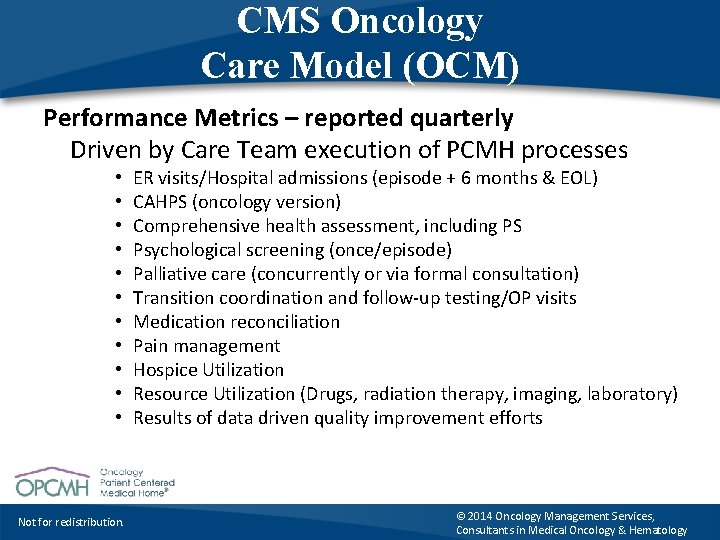
CMS Oncology Care Model (OCM) Performance Metrics – reported quarterly Driven by Care Team execution of PCMH processes • • • Not for redistribution. ER visits/Hospital admissions (episode + 6 months & EOL) CAHPS (oncology version) Comprehensive health assessment, including PS Psychological screening (once/episode) Palliative care (concurrently or via formal consultation) Transition coordination and follow-up testing/OP visits Medication reconciliation Pain management Hospice Utilization Resource Utilization (Drugs, radiation therapy, imaging, laboratory) Results of data driven quality improvement efforts © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology
Principles of PCMH-N Applied to Cancer Care PCMH standards + supportive technology applied to primary and specialty care enables a neighborhood of practices that deliver what Don Berwick called for in 2012: “…. an electronic line-of-sight contact with each other all day long, weaving a net of help and partnership with patients and families. ” Not for redistribution. © 2014 Oncology Management Services, Consultants in Medical Oncology & Hematology