Treatment Planning in FPD Dr Kaushal Kishor Agrawal





- Slides: 35

Treatment Planning in FPD Dr Kaushal Kishor Agrawal Assistant Professor Departmnent of Prosthodontics KGMU Lucknow
Types of Fixed Prosthodontic Treatment n - Conventional tooth supported fixed partial denture Utilizes an abutment tooth on each end or only one end (cantilever) of the edentulous space. - If abutment teeth are periodontally sound, the edentulous span is short and straight and the retainers are well designed and executed, the FPD can be expected to provide a long life and function for the pt. - there should be : - no gross soft tissue defect in the edentulous space - no dry mouth which can create a poor environment for FPD
n Resin bonded tooth supported fixed partial denture - conservative restoration reserved for use on defect free abutments to replace single missing tooth usually an incisor or premolar. - for molars – replaced only if muscles of mastication are not too well developed - abutments on both sides of edentulous space, preparation is shallow and restricted to enamel - useful in young pts who have immature teeth with large pulps - should be used with extreme care and may require additional resistance features (e. g. grooves) - Abutment Mobility has been shown to be a serious hazard in the successful use of this type of prosthesis.
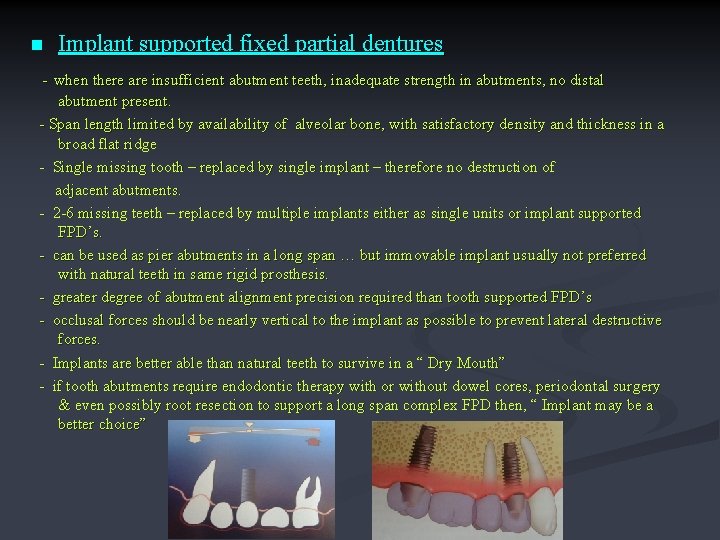
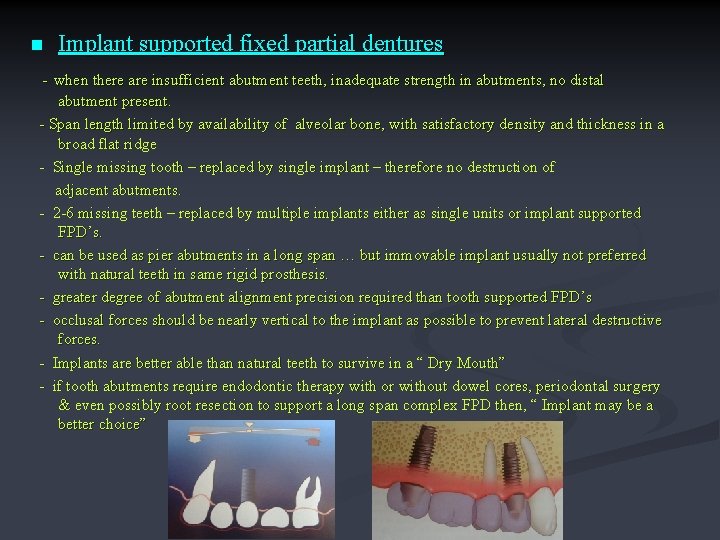
n Implant supported fixed partial dentures - when there are insufficient abutment teeth, inadequate strength in abutments, no distal abutment present. - Span length limited by availability of alveolar bone, with satisfactory density and thickness in a broad flat ridge - Single missing tooth – replaced by single implant – therefore no destruction of adjacent abutments. - 2 -6 missing teeth – replaced by multiple implants either as single units or implant supported FPD’s. - can be used as pier abutments in a long span … but immovable implant usually not preferred with natural teeth in same rigid prosthesis. - greater degree of abutment alignment precision required than tooth supported FPD’s - occlusal forces should be nearly vertical to the implant as possible to prevent lateral destructive forces. - Implants are better able than natural teeth to survive in a “ Dry Mouth” - if tooth abutments require endodontic therapy with or without dowel cores, periodontal surgery & even possibly root resection to support a long span complex FPD then, “ Implant may be a better choice”
Treatment Planning I - Identification of patients needs a) Correction of existing disease - By identification and reduction of the initiating factors and improvement of the resistive factors or Both b) Prevention of future disease - by evaluating the patients disease experience & knowing the prevalence of the disease in general population. Treatment should be proposed if future disease seems likely in the absence of such intervention. c) Restoration of Function – level of the function is assessed during examination and treatment may be proposed to correct impaired function (e. g. speech & mastication). d) Improvement of appearance – listen carefully to the patient’s views and if the appearance is far outside socially accepted values, the feasibility of corrective procedures should be brought to the patients attention. Long term dental health should not be compromised by unwise attempts to improve appearance and patients should always be made aware of the possible adverse consequences of treatment.
II- Available materials and techniques Clinician should understand the limitations of appropriate materials and procedures & this will help prevent experimental approach to treatment. a) Plastic materials (e. g. Am & Composite) b) Cast Metal – intracoronal restoration & extracoronal restoration c) Metal ceramic d) Resin Veneered e) Fiber-reinforced resin f) Complete ceramic g) Fixed partial denture h) Implant supported prosthesis i) Removable partial dentures
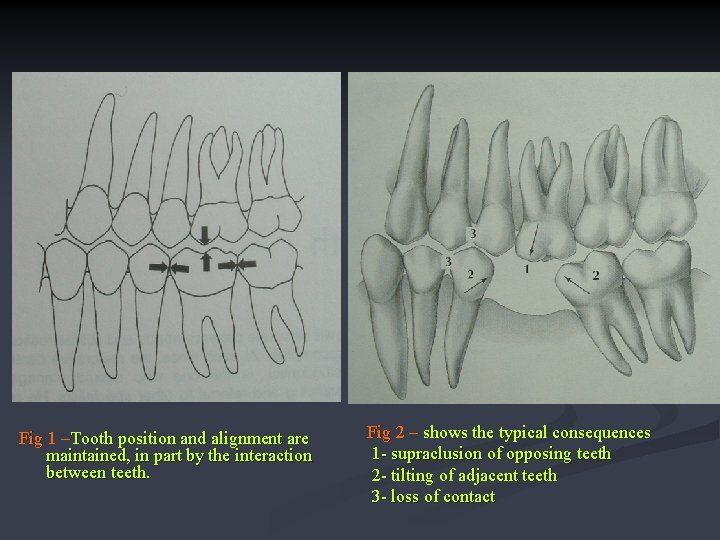
III-Treatment of tooth loss Causes- caries, pdl disease, trauma, neoplasm, congenitally absent a) Decision to remove a tooth – poor/hopeless teeth should be removed. A decision about replacing a missing tooth is best made at the time of its removal rather than months or years after the fact. b) Consequences of removal without replacement – - supraclusion/ supraeruption of opposing tooth/teeth. - tilting of the adjacent teeth - loss of proximal contact Extended treatment plans like orthodontic repositioning and additional cast restoration may be needed to compensate for the lack of treatment at the time of tooth removal
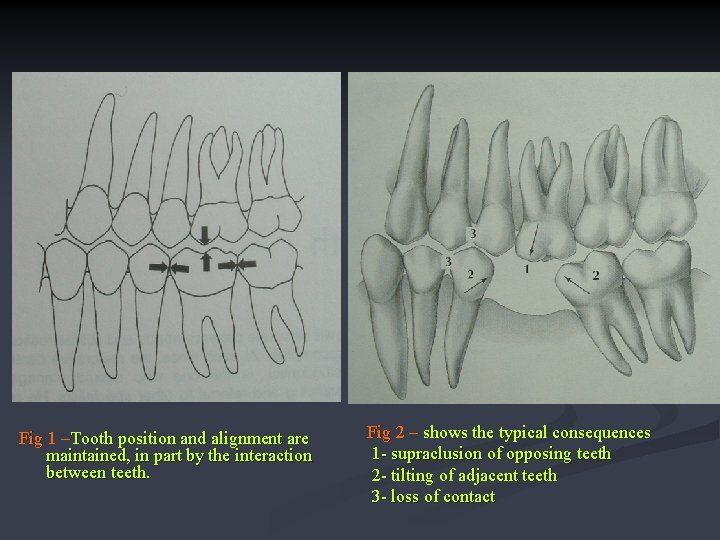
Fig 1 –Tooth position and alignment are maintained, in part by the interaction between teeth. Fig 2 – shows the typical consequences 1 - supraclusion of opposing teeth 2 - tilting of adjacent teeth 3 - loss of contact
IV-Selection of Abutment teeth/ Abutment Evaluation -Whenever possible an abutment should be a “VITAL TOOTH” -The forces that would normally be absorbed by the missing tooth, are transmitted through the pontic, connectors and retainers to the abutment teeth therefore the abutment teeth should be able to withstand the forces normally directed to the missing teeth in addition to those usually applied to the abutments. -An FPD should be designed as simply as possible A) REPLACEMENT OF SINGLE MISSING TOOTH Unless bone support has been weakened by pdl disease, a single missing tooth can almost always be replaced by a 3 unit FPD having one mesial and one distal abutment tooth. Factors to be considered i) Cantilever FPD - this is a potentially destructive design with the lever arm created by the pontic.
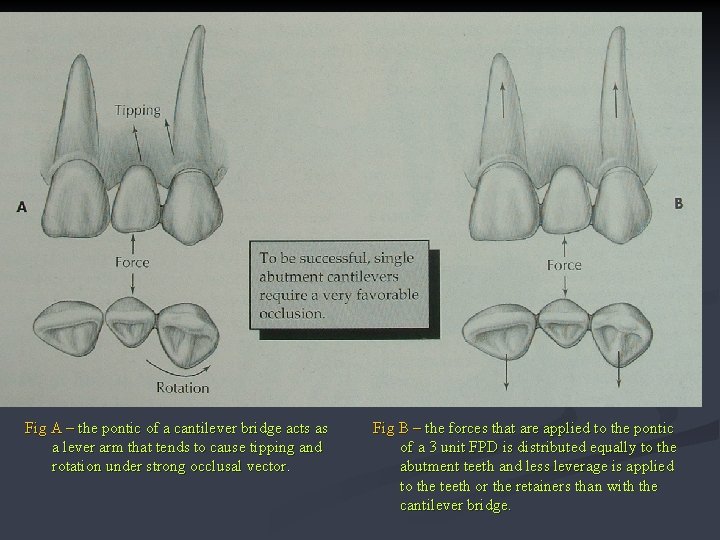
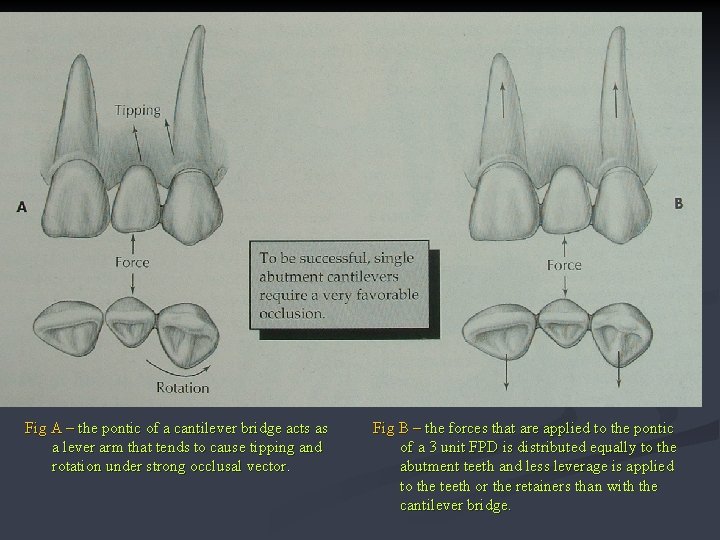
Fig A – the pontic of a cantilever bridge acts as a lever arm that tends to cause tipping and rotation under strong occlusal vector. Fig B – the forces that are applied to the pontic of a 3 unit FPD is distributed equally to the abutment teeth and less leverage is applied to the teeth or the retainers than with the cantilever bridge.
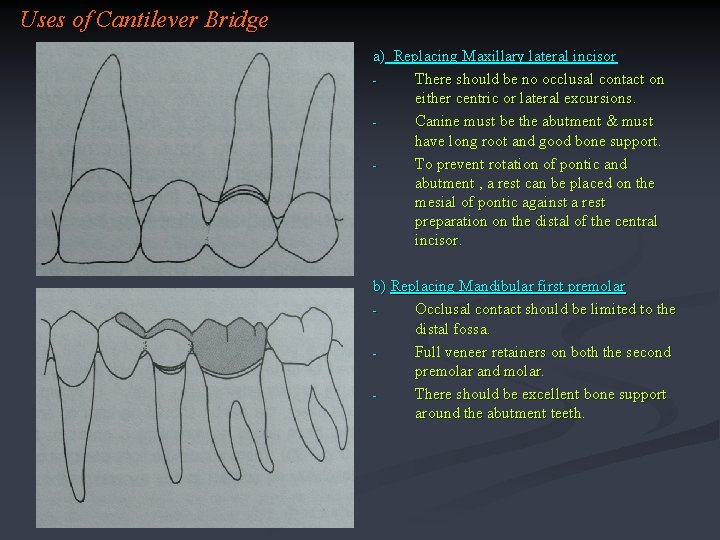
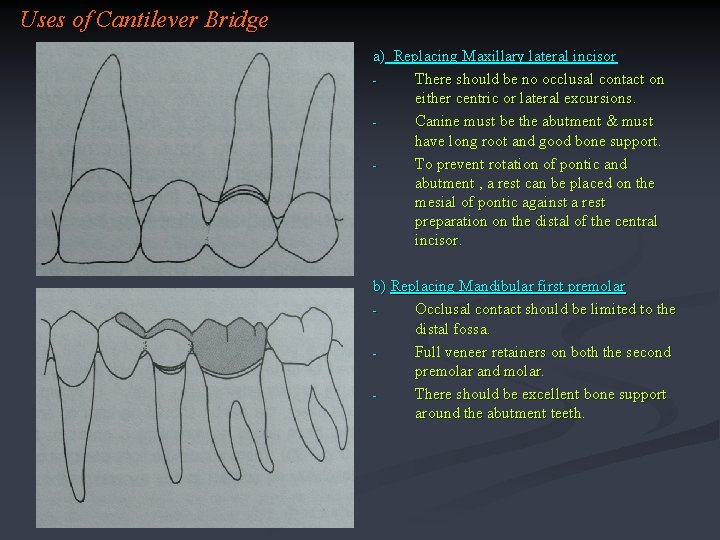
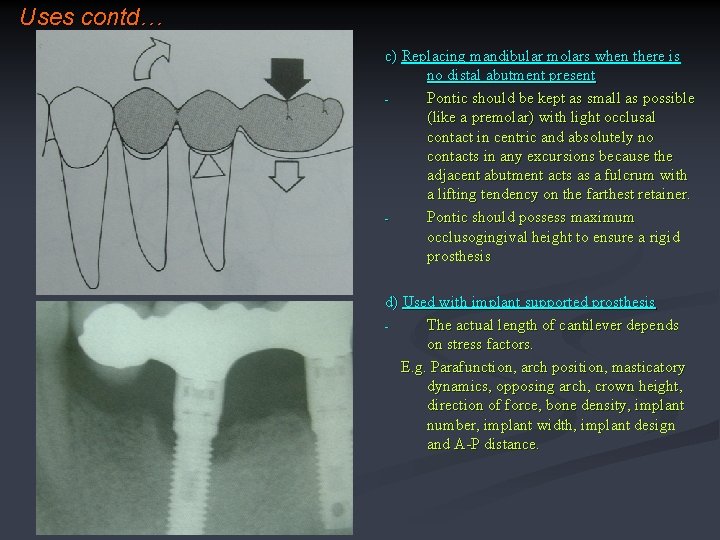
Uses of Cantilever Bridge a) Replacing Maxillary lateral incisor There should be no occlusal contact on either centric or lateral excursions. Canine must be the abutment & must have long root and good bone support. To prevent rotation of pontic and abutment , a rest can be placed on the mesial of pontic against a rest preparation on the distal of the central incisor. b) Replacing Mandibular first premolar Occlusal contact should be limited to the distal fossa. Full veneer retainers on both the second premolar and molar. There should be excellent bone support around the abutment teeth.
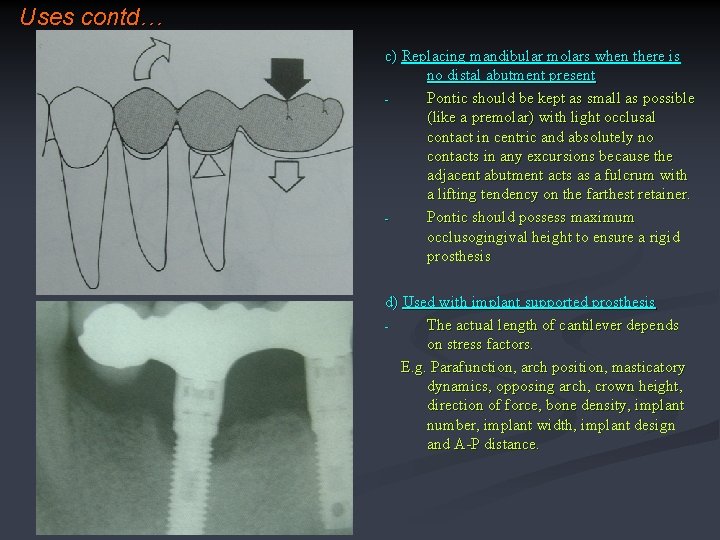
Uses contd… c) Replacing mandibular molars when there is no distal abutment present Pontic should be kept as small as possible (like a premolar) with light occlusal contact in centric and absolutely no contacts in any excursions because the adjacent abutment acts as a fulcrum with a lifting tendency on the farthest retainer. Pontic should possess maximum occlusogingival height to ensure a rigid prosthesis d) Used with implant supported prosthesis The actual length of cantilever depends on stress factors. E. g. Parafunction, arch position, masticatory dynamics, opposing arch, crown height, direction of force, bone density, implant number, implant width, implant design and A-P distance.
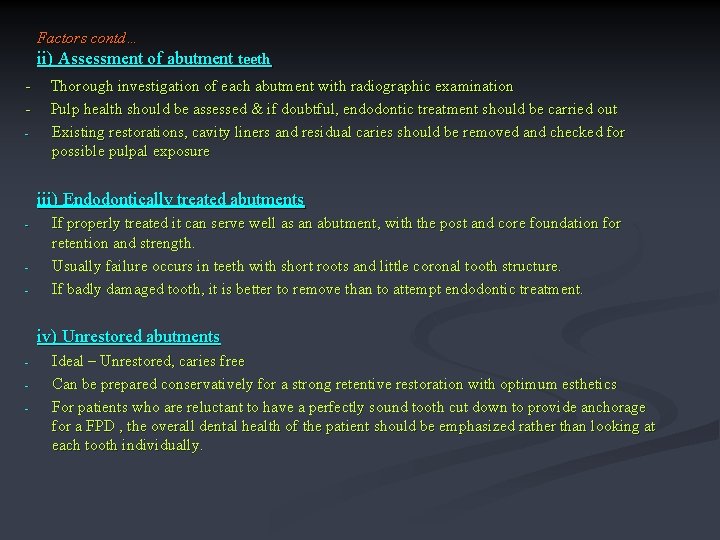
Factors contd… ii) Assessment of abutment teeth - Thorough investigation of each abutment with radiographic examination Pulp health should be assessed & if doubtful, endodontic treatment should be carried out Existing restorations, cavity liners and residual caries should be removed and checked for possible pulpal exposure iii) Endodontically treated abutments - If properly treated it can serve well as an abutment, with the post and core foundation for retention and strength. Usually failure occurs in teeth with short roots and little coronal tooth structure. If badly damaged tooth, it is better to remove than to attempt endodontic treatment. iv) Unrestored abutments - Ideal – Unrestored, caries free Can be prepared conservatively for a strong retentive restoration with optimum esthetics For patients who are reluctant to have a perfectly sound tooth cut down to provide anchorage for a FPD , the overall dental health of the patient should be emphasized rather than looking at each tooth individually.
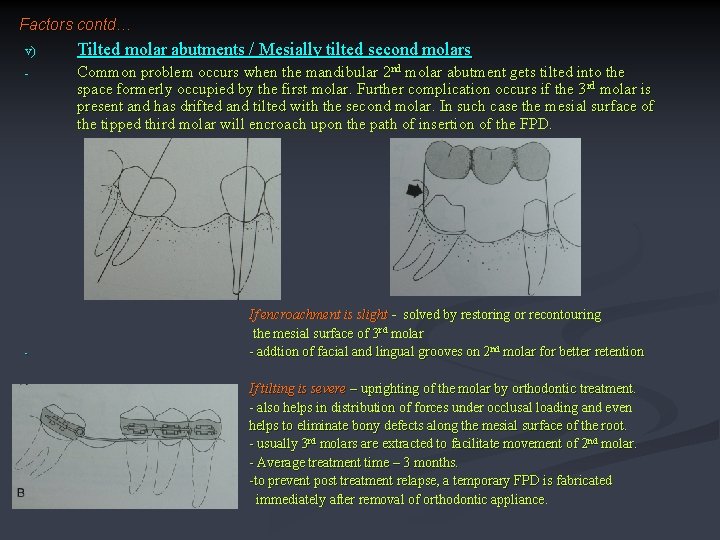
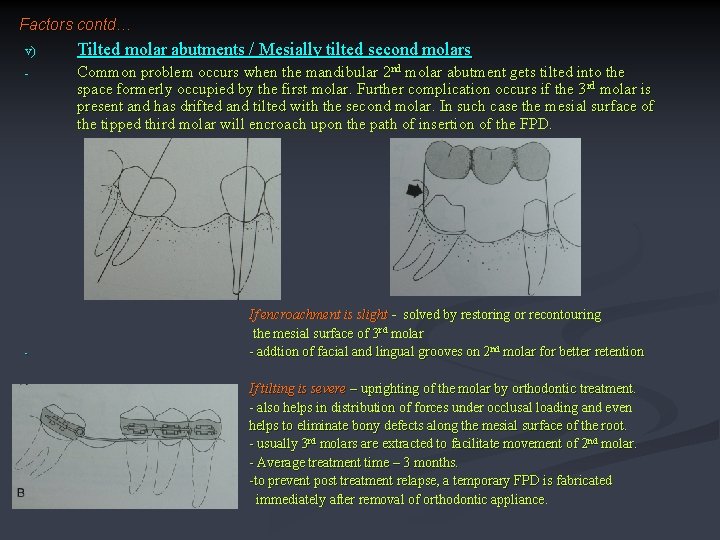
Factors contd… v) Tilted molar abutments / Mesially tilted second molars - Common problem occurs when the mandibular 2 nd molar abutment gets tilted into the space formerly occupied by the first molar. Further complication occurs if the 3 rd molar is present and has drifted and tilted with the second molar. In such case the mesial surface of the tipped third molar will encroach upon the path of insertion of the FPD. - If encroachment is slight - solved by restoring or recontouring the mesial surface of 3 rd molar - addtion of facial and lingual grooves on 2 nd molar for better retention If tilting is severe – uprighting of the molar by orthodontic treatment. - also helps in distribution of forces under occlusal loading and even helps to eliminate bony defects along the mesial surface of the root. - usually 3 rd molars are extracted to facilitate movement of 2 nd molar. - Average treatment time – 3 months. -to prevent post treatment relapse, a temporary FPD is fabricated immediately after removal of orthodontic appliance.
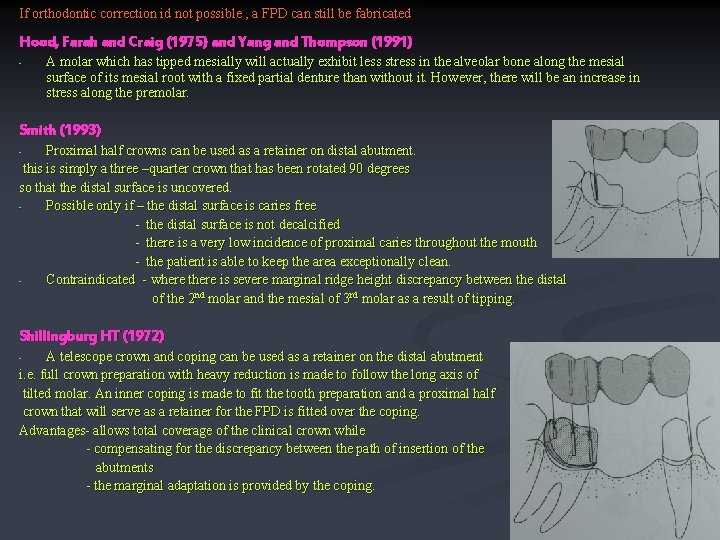
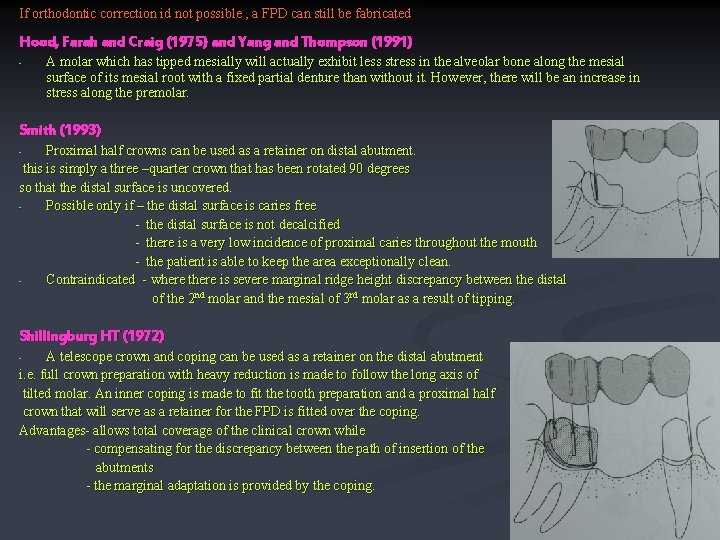
If orthodontic correction id not possible , a FPD can still be fabricated Hood, Farah and Craig (1975) and Yang and Thompson (1991) - A molar which has tipped mesially will actually exhibit less stress in the alveolar bone along the mesial surface of its mesial root with a fixed partial denture than without it. However, there will be an increase in stress along the premolar. Smith (1993) Proximal half crowns can be used as a retainer on distal abutment. this is simply a three –quarter crown that has been rotated 90 degrees so that the distal surface is uncovered. Possible only if – the distal surface is caries free - the distal surface is not decalcified - there is a very low incidence of proximal caries throughout the mouth - the patient is able to keep the area exceptionally clean. Contraindicated - where there is severe marginal ridge height discrepancy between the distal of the 2 nd molar and the mesial of 3 rd molar as a result of tipping. - Shillingburg HT (1972) A telescope crown and coping can be used as a retainer on the distal abutment i. e. full crown preparation with heavy reduction is made to follow the long axis of tilted molar. An inner coping is made to fit the tooth preparation and a proximal half crown that will serve as a retainer for the FPD is fitted over the coping. Advantages- allows total coverage of the clinical crown while - compensating for the discrepancy between the path of insertion of the abutments - the marginal adaptation is provided by the coping. -
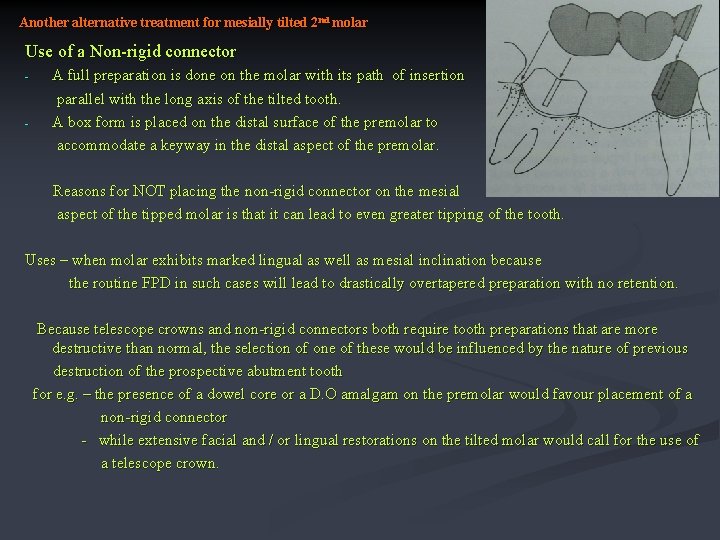
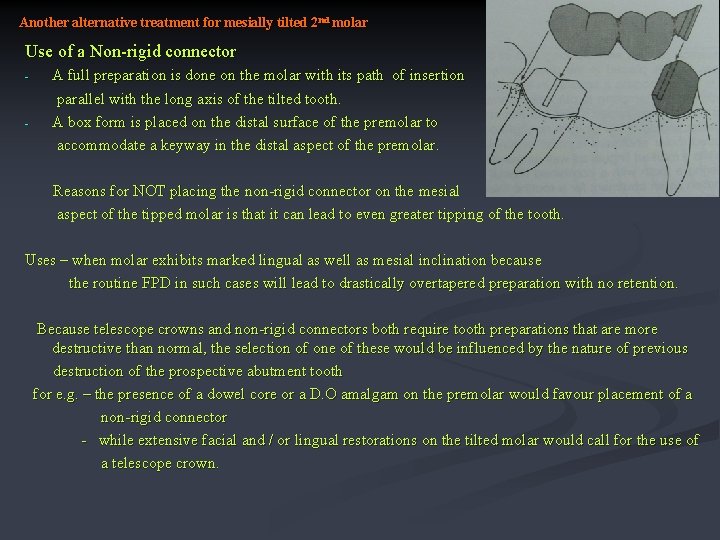
Another alternative treatment for mesially tilted 2 nd molar Use of a Non-rigid connector - - A full preparation is done on the molar with its path of insertion parallel with the long axis of the tilted tooth. A box form is placed on the distal surface of the premolar to accommodate a keyway in the distal aspect of the premolar. Reasons for NOT placing the non-rigid connector on the mesial aspect of the tipped molar is that it can lead to even greater tipping of the tooth. Uses – when molar exhibits marked lingual as well as mesial inclination because the routine FPD in such cases will lead to drastically overtapered preparation with no retention. Because telescope crowns and non-rigid connectors both require tooth preparations that are more destructive than normal, the selection of one of these would be influenced by the nature of previous destruction of the prospective abutment tooth for e. g. – the presence of a dowel core or a D. O amalgam on the premolar would favour placement of a non-rigid connector - while extensive facial and / or lingual restorations on the tilted molar would call for the use of a telescope crown.
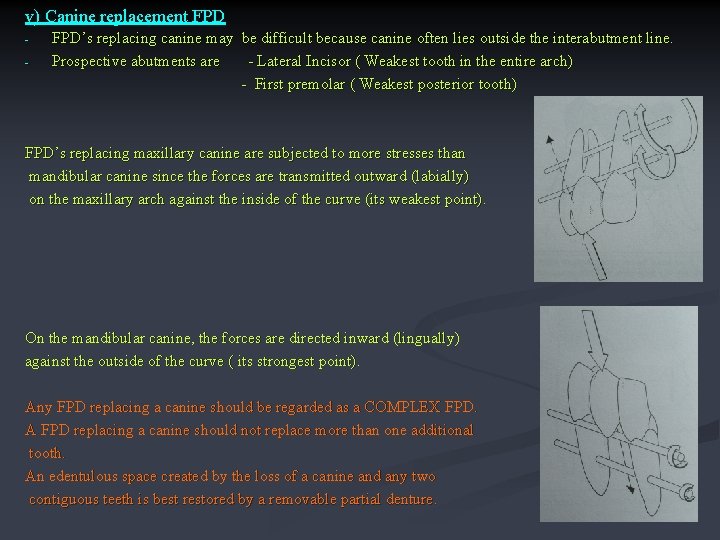
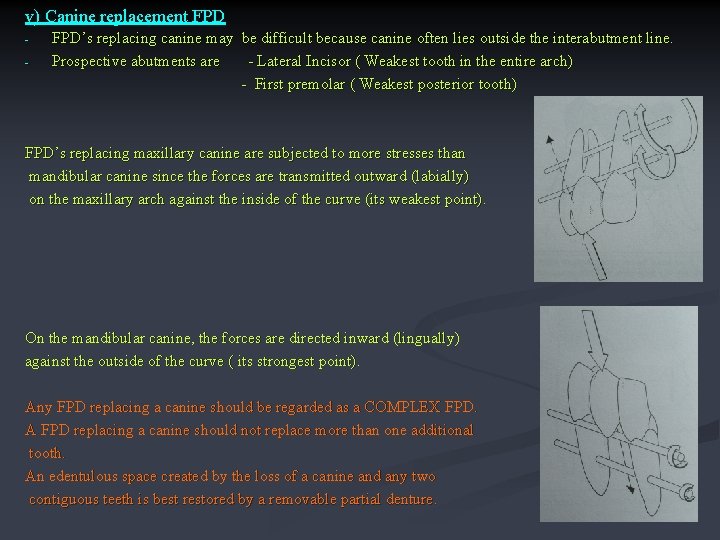
v) Canine replacement FPD - FPD’s replacing canine may be difficult because canine often lies outside the interabutment line. Prospective abutments are - Lateral Incisor ( Weakest tooth in the entire arch) - First premolar ( Weakest posterior tooth) FPD’s replacing maxillary canine are subjected to more stresses than mandibular canine since the forces are transmitted outward (labially) on the maxillary arch against the inside of the curve (its weakest point). On the mandibular canine, the forces are directed inward (lingually) against the outside of the curve ( its strongest point). Any FPD replacing a canine should be regarded as a COMPLEX FPD. A FPD replacing a canine should not replace more than one additional tooth. An edentulous space created by the loss of a canine and any two contiguous teeth is best restored by a removable partial denture.

B) REPLACEMENT OF SEVERAL MISSING TEETH FPD becomes more difficult when several teeth must be replaced, and underestimation of the problems involved in extensive prosthodontics can lead to failure. Factors to be considered i) Overloading of abutment teeth the ability of the abutment teeth to accept applied forces without drifting or becoming mobile must be estimated. The forces are particularly severe during parafunctional grinding and clenching and need to eliminate them becomes obvious. a) Direction of Forces. - a well fabricated FPD can distribute applied force in the most favorable way by directing them in the long axis of the abutment teeth. - The dislodging forces on a FPD retainer tend to act in a mesiodistal direction as opposes to the more common buccolingual direction of forces in a single restoration. - Preparations should be modified accordingly to produce greater resistance & structural durability - Multiple grooves, including some on the buccal and lingual surfaces are commonly employed for this purpose.
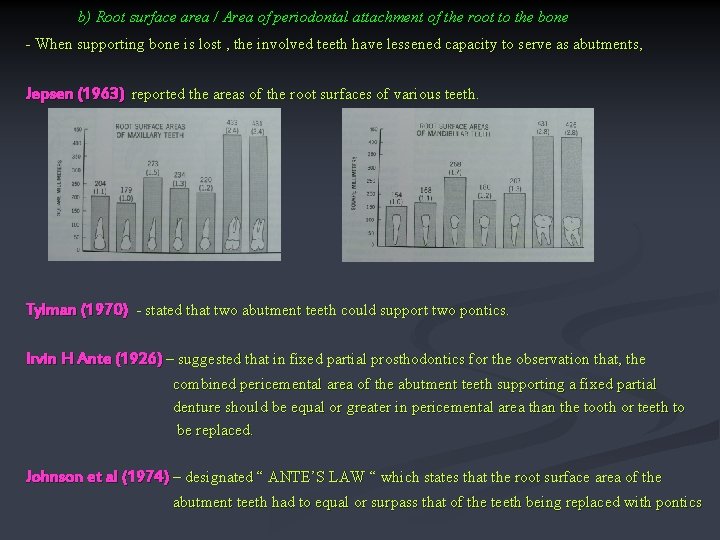
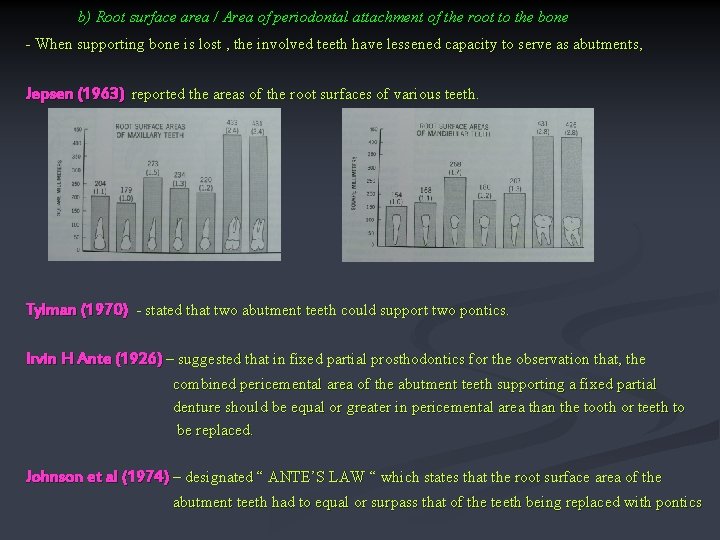
b) Root surface area / Area of periodontal attachment of the root to the bone - When supporting bone is lost , the involved teeth have lessened capacity to serve as abutments, Jepsen (1963) reported the areas of the root surfaces of various teeth. Tylman (1970) - stated that two abutment teeth could support two pontics. Irvin H Ante (1926) – suggested that in fixed partial prosthodontics for the observation that, the combined pericemental area of the abutment teeth supporting a fixed partial denture should be equal or greater in pericemental area than the tooth or teeth to be replaced. Johnson et al (1974) – designated “ ANTE’S LAW “ which states that the root surface area of the abutment teeth had to equal or surpass that of the teeth being replaced with pontics
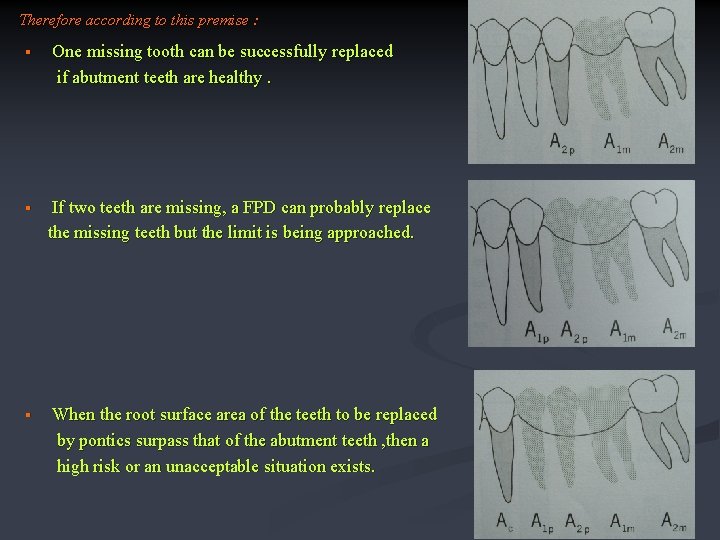
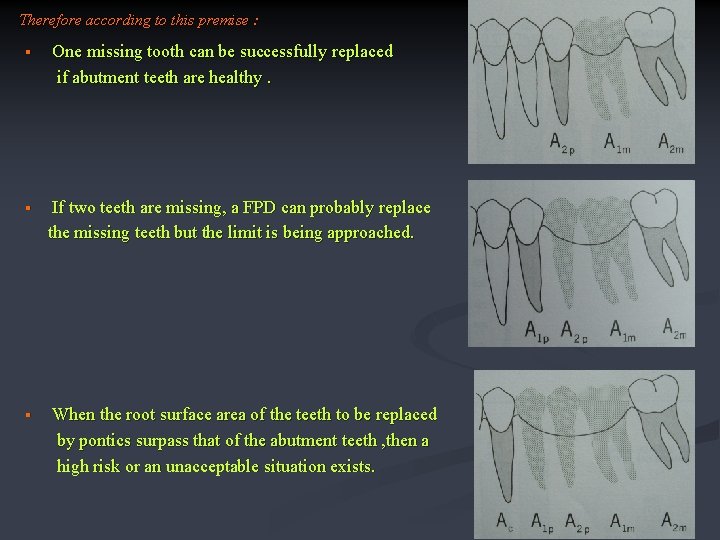
Therefore according to this premise : § § § One missing tooth can be successfully replaced if abutment teeth are healthy. If two teeth are missing, a FPD can probably replace the missing teeth but the limit is being approached. When the root surface area of the teeth to be replaced by pontics surpass that of the abutment teeth , then a high risk or an unacceptable situation exists.
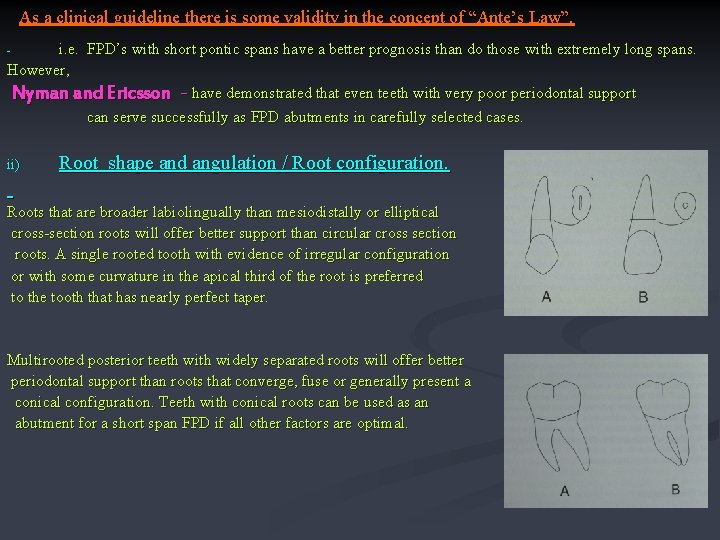
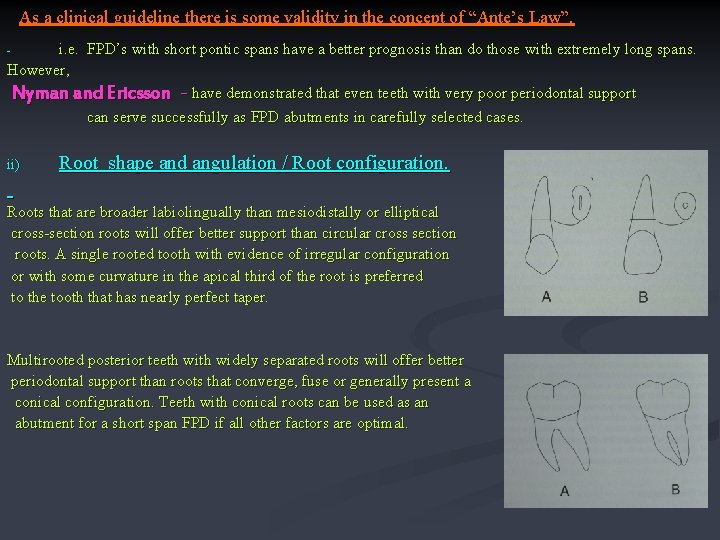
As a clinical guideline there is some validity in the concept of “Ante’s Law”. i. e. FPD’s with short pontic spans have a better prognosis than do those with extremely long spans. However, Nyman and Ericsson - have demonstrated that even teeth with very poor periodontal support can serve successfully as FPD abutments in carefully selected cases. - ii) Root shape and angulation / Root configuration. Roots that are broader labiolingually than mesiodistally or elliptical cross-section roots will offer better support than circular cross section roots. A single rooted tooth with evidence of irregular configuration or with some curvature in the apical third of the root is preferred to the tooth that has nearly perfect taper. Multirooted posterior teeth widely separated roots will offer better periodontal support than roots that converge, fuse or generally present a conical configuration. Teeth with conical roots can be used as an abutment for a short span FPD if all other factors are optimal.
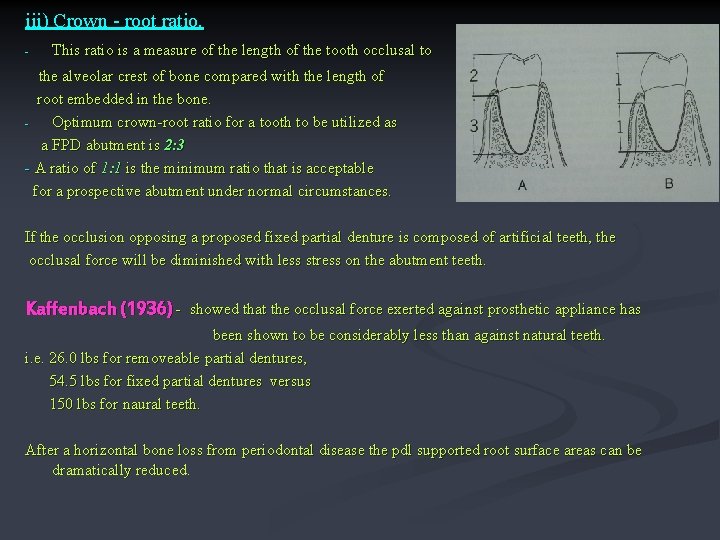
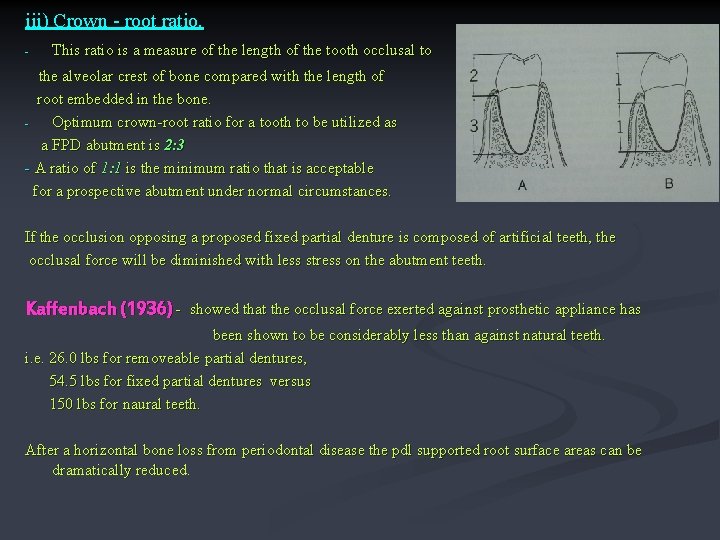
iii) Crown - root ratio. - This ratio is a measure of the length of the tooth occlusal to the alveolar crest of bone compared with the length of root embedded in the bone. Optimum crown-root ratio for a tooth to be utilized as a FPD abutment is 2: 3 - A ratio of 1: 1 is the minimum ratio that is acceptable for a prospective abutment under normal circumstances. If the occlusion opposing a proposed fixed partial denture is composed of artificial teeth, the occlusal force will be diminished with less stress on the abutment teeth. Kaffenbach (1936) - showed that the occlusal force exerted against prosthetic appliance has been shown to be considerably less than against natural teeth. i. e. 26. 0 lbs for removeable partial dentures, 54. 5 lbs for fixed partial dentures versus 150 lbs for naural teeth. After a horizontal bone loss from periodontal disease the pdl supported root surface areas can be dramatically reduced.
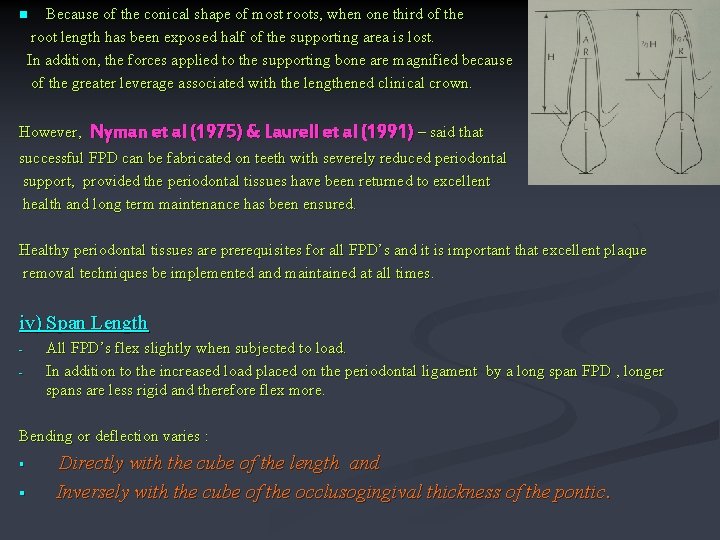
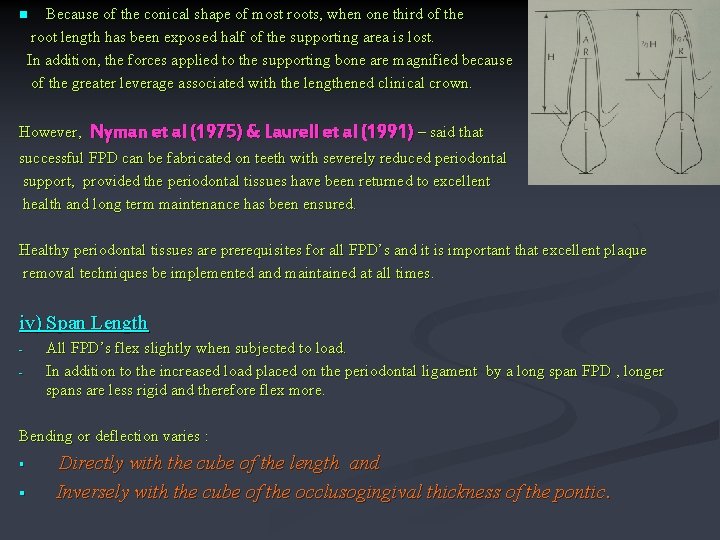
Because of the conical shape of most roots, when one third of the root length has been exposed half of the supporting area is lost. In addition, the forces applied to the supporting bone are magnified because of the greater leverage associated with the lengthened clinical crown. n However, Nyman et al (1975) & Laurell et al (1991) – said that successful FPD can be fabricated on teeth with severely reduced periodontal support, provided the periodontal tissues have been returned to excellent health and long term maintenance has been ensured. Healthy periodontal tissues are prerequisites for all FPD’s and it is important that excellent plaque removal techniques be implemented and maintained at all times. iv) Span Length - All FPD’s flex slightly when subjected to load. In addition to the increased load placed on the periodontal ligament by a long span FPD , longer spans are less rigid and therefore flex more. Bending or deflection varies : § § Directly with the cube of the length and Inversely with the cube of the occlusogingival thickness of the pontic.
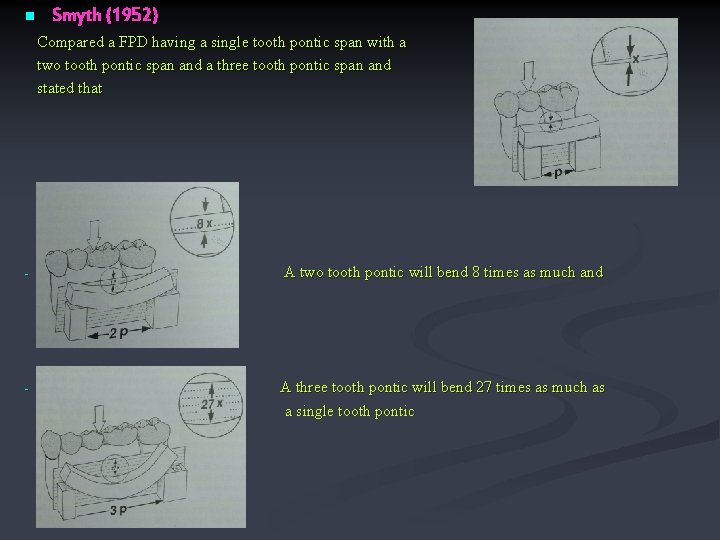
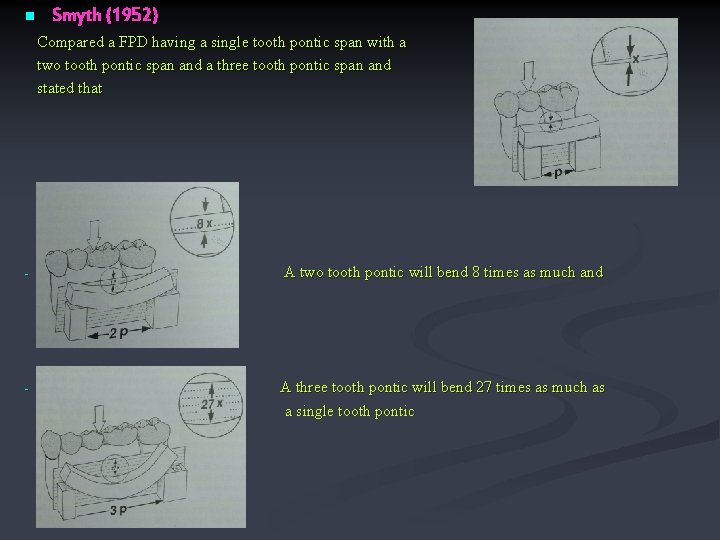
n Smyth (1952) Compared a FPD having a single tooth pontic span with a two tooth pontic span and a three tooth pontic span and stated that - A two tooth pontic will bend 8 times as much and - A three tooth pontic will bend 27 times as much as a single tooth pontic

A pontic with a given occluso-gingival dimension will bend 8 times as much if the pontic thickness is halved. - Therefore, a long span FPD on short mandibular teeth can have disappointing results. - Longer pontic spans also have the potential for producing more torquing forces on the FPD. To minimize flexing - select pontic design with greater occlusogingival direction - make bulky connectors to ensure optimum rigidity - if long span or unfavorable crown –root ratio then use double abutments. Criteria for double Abutments. Secondary abutments (remote from edentulous space) must have – as much root surface area and as favorable a crown root ratio as the primary abutment ( adjacent to the edentulous space). The retainers on secondary abutments must be at least as retentive as on primary abutments because when the pontic flexes tensile forces will be applied on the retainers on the secondary abutments. There must also be sufficient crown length and space between adjacent abutments to prevent impingement on the gingiva under the connector -

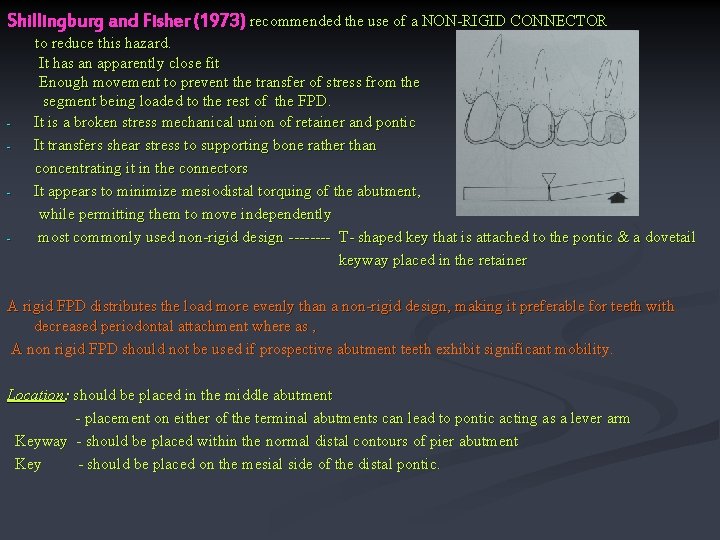
v) Pier Abutments An edentulous space can occur on both sides of a tooth creating a lone , free standing pier abutment. Shillingburg and Fisher (1973) – forces are transmitted to the terminal retainers as a result of the middle abutment acting as a fulcrum causing failure of the weaker retainer. However, photoelastic stress analysis and displacement measurement indicate that the prosthesis bends rather than rocks and Standlee & Caputo (1988) suggested that tension between the terminal retainers and their respective abutments rather than pier fulcrum, as the mechanism of failure. Because of the forces : - the retainers or the casting will get loosened Leakage will be caused around the margin leading to extensive caries. Since there are limits to increase a retainers capacity to withstand displacing forces, some means must be used to neutralize the effects of those factors.
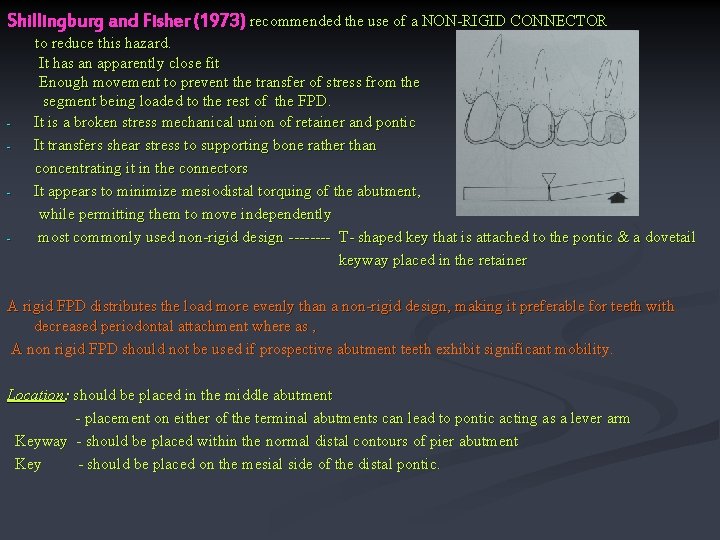
Shillingburg and Fisher (1973) recommended the use of a NON-RIGID CONNECTOR - - - to reduce this hazard. It has an apparently close fit Enough movement to prevent the transfer of stress from the segment being loaded to the rest of the FPD. It is a broken stress mechanical union of retainer and pontic It transfers shear stress to supporting bone rather than concentrating it in the connectors It appears to minimize mesiodistal torquing of the abutment, while permitting them to move independently most commonly used non-rigid design ---- T- shaped key that is attached to the pontic & a dovetail keyway placed in the retainer A rigid FPD distributes the load more evenly than a non-rigid design, making it preferable for teeth with decreased periodontal attachment where as , A non rigid FPD should not be used if prospective abutment teeth exhibit significant mobility. Location: should be placed in the middle abutment - placement on either of the terminal abutments can lead to pontic acting as a lever arm Keyway - should be placed within the normal distal contours of pier abutment Key - should be placed on the mesial side of the distal pontic.
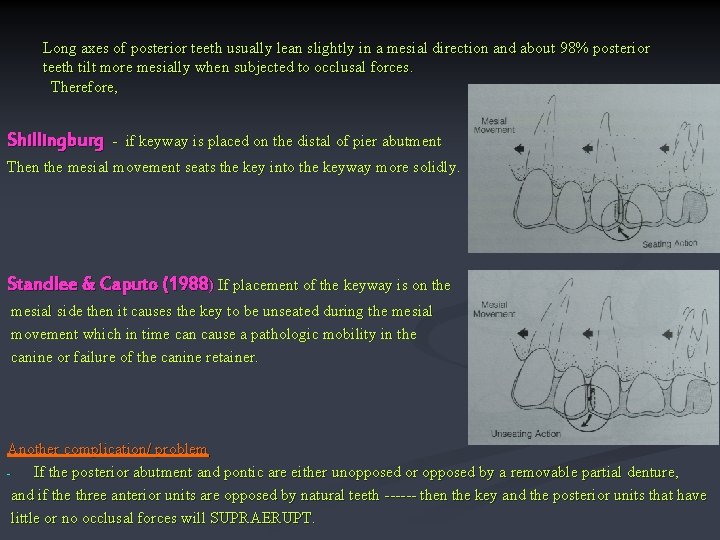
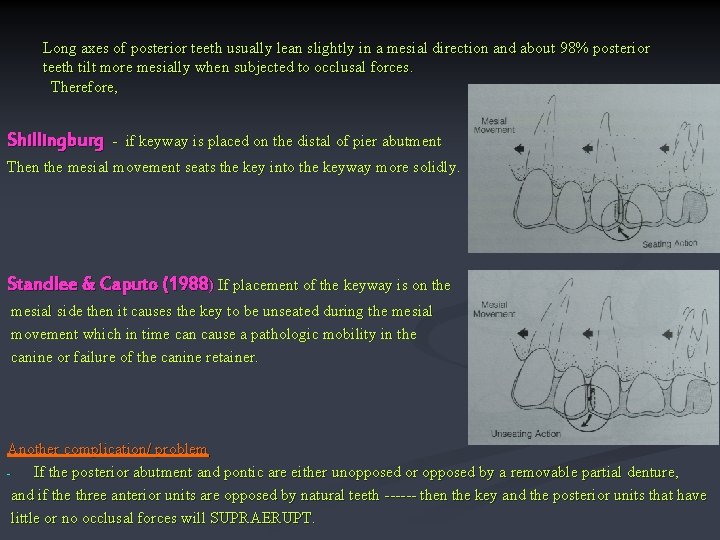
Long axes of posterior teeth usually lean slightly in a mesial direction and about 98% posterior teeth tilt more mesially when subjected to occlusal forces. Therefore, Shillingburg - if keyway is placed on the distal of pier abutment Then the mesial movement seats the key into the keyway more solidly. Standlee & Caputo (1988) If placement of the keyway is on the mesial side then it causes the key to be unseated during the mesial movement which in time can cause a pathologic mobility in the canine or failure of the canine retainer. Another complication/ problem If the posterior abutment and pontic are either unopposed or opposed by a removable partial denture, and if the three anterior units are opposed by natural teeth ------ then the key and the posterior units that have little or no occlusal forces will SUPRAERUPT.
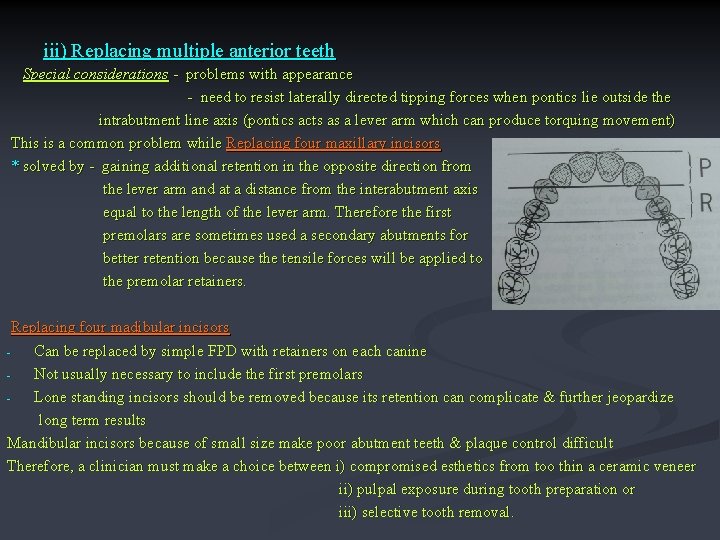
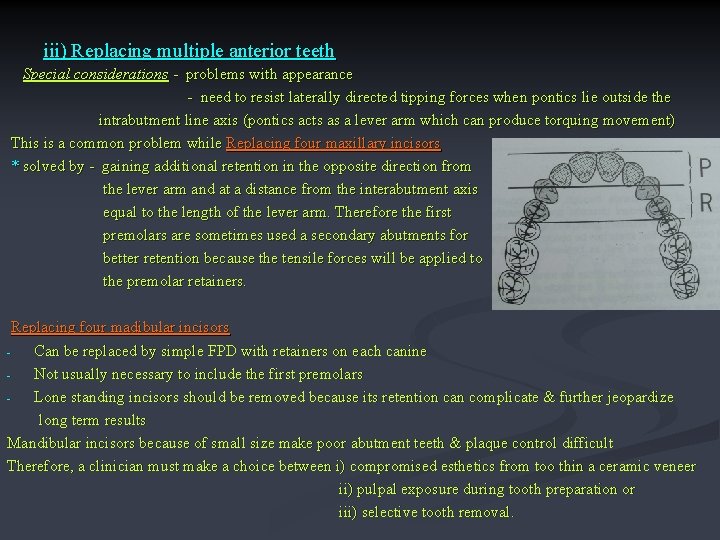
iii) Replacing multiple anterior teeth Special considerations - problems with appearance - need to resist laterally directed tipping forces when pontics lie outside the intrabutment line axis (pontics acts as a lever arm which can produce torquing movement) This is a common problem while Replacing four maxillary incisors * solved by - gaining additional retention in the opposite direction from the lever arm and at a distance from the interabutment axis equal to the length of the lever arm. Therefore the first premolars are sometimes used a secondary abutments for better retention because the tensile forces will be applied to the premolar retainers. Replacing four madibular incisors Can be replaced by simple FPD with retainers on each canine Not usually necessary to include the first premolars Lone standing incisors should be removed because its retention can complicate & further jeopardize long term results Mandibular incisors because of small size make poor abutment teeth & plaque control difficult Therefore, a clinician must make a choice between i) compromised esthetics from too thin a ceramic veneer ii) pulpal exposure during tooth preparation or iii) selective tooth removal.
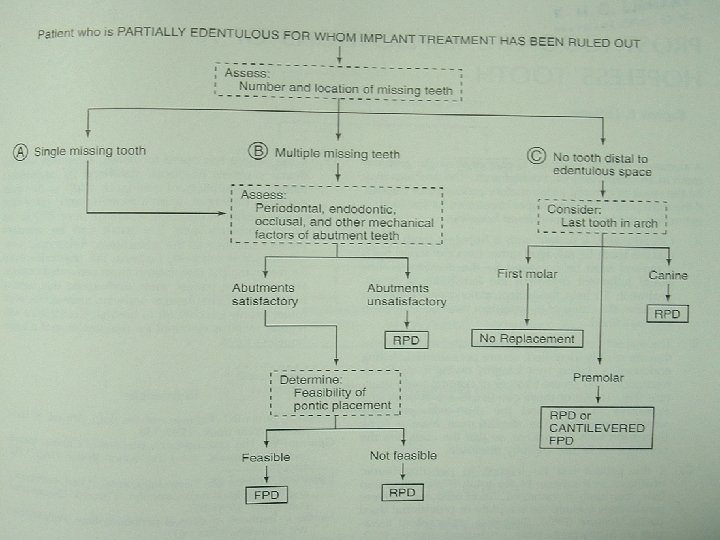
C) INDICATIONS FOR REMOVEABLE PARTIAL DENTURE Whenever possible edentulous spaces will should be restored with FPD than RPD, however under the following circumstances RPD is indicated. n Where vertical support from the edentulous ridge is needed. E. g. in the absence of a distal abutment. n Where resistance to lateral movement is needed from contra-lateral teeth and soft tissues. E. g. to ensure stability with a long edentulous space n When there is a considerable bone loss in the visible anterior region and an FPD would have an unacceptable appearance.
V) Sequence of treatment Includes : a) Treatment of symptoms Relief of discomfort accompanying acute conditions Urgent treatment of non-acute problems b) Stabilization of deteriorating factors Dental caries Periodontal disease c) Definitive therapy Oral surgery, Periodontics, Endodontics, Orthodontics, Fixed Prosthodontics – Occlusal adjustments - Anterior restorations - Posterior Restorations - Complex Prosthodontics d) Follow up specific program of follow up care & regular recall visits.
References 1) Contemporary Fixed Prosthodontics – Rosenstiel, Land & Fujimoto 2) Fundamentals of Fixed Prosthodontics – Shillingburg 3) A preliminary diagnostic and treatment protocol – J Bowley et al DCNA. July 1992, 36(3) 551 -567. 4) Decision making in Dental treatment planning – Hall, Roberts and La. Barre

THANK YOU !
 Crown root ratio
Crown root ratio Satyender kishor
Satyender kishor Rksk banner
Rksk banner Jyoti kaushal
Jyoti kaushal Rainu kaushal
Rainu kaushal Kaushal bharat help desk
Kaushal bharat help desk Surbhi kaushal
Surbhi kaushal Subodh agrawal
Subodh agrawal Ca rakesh agrawal
Ca rakesh agrawal Dr raj agrawal
Dr raj agrawal Vishwani agrawal
Vishwani agrawal Agrawal-kayal-saxena
Agrawal-kayal-saxena Ameeta agrawal
Ameeta agrawal Dr deepak agrawal
Dr deepak agrawal Biomedical waste management introduction
Biomedical waste management introduction Nikolay yakovets
Nikolay yakovets Divyakant agrawal
Divyakant agrawal Krati agrawal
Krati agrawal Anoop agrawal
Anoop agrawal Shankarlal agrawal science college salekasa
Shankarlal agrawal science college salekasa Dr shweta agrawal
Dr shweta agrawal Removable partial denture slideshare
Removable partial denture slideshare Phases of dental treatment planning
Phases of dental treatment planning Endodontic diagnosis and treatment planning
Endodontic diagnosis and treatment planning Case formulation and treatment plan example
Case formulation and treatment plan example Chapter 28 oral diagnosis and treatment planning
Chapter 28 oral diagnosis and treatment planning Cbt assessment example
Cbt assessment example Advantages and disadvantages of rpd
Advantages and disadvantages of rpd Oral diagnosis and treatment planning ppt
Oral diagnosis and treatment planning ppt Lip length classification
Lip length classification Fpd
Fpd Inlay wax pattern fabrication
Inlay wax pattern fabrication Types of fpd
Types of fpd Kennedy class 1 mod 2 rpd design
Kennedy class 1 mod 2 rpd design Spring cantilever bridge indication
Spring cantilever bridge indication Cementation in fpd
Cementation in fpd