Fundamentals of nursing PNU 145 Chapter 15 Nutrition









- Slides: 40
Fundamentals of nursing PNU 145 Chapter 15 Nutrition Cheryl Proffitt MSN, RN October, 2013.
Nutrition • Objectives • Define nutrition and malnutrition • List six components of basic nutrition • List at least five factors that influence nutritional needs • Discuss the purpose and components of the myplate food guidelines • Discuss three facts available on nutritional labels • Explain protein complementation • Identify four objective assessments for determining a person’s nutritional status • Discuss the purpose of a diet history
Objectives Cont’d • List five common problems that can be identified from a nutritional assessment • Plan nursing interventions fro resolving problems caused or affected by nutrition • List seven common hospital diets • Discuss four nursing responsibilities for meeting clients nutritional needs • Identify three facts a nurse must know about a client’s diet • Describe and demonstrate techniques fro feeding clients • Explain how to meet the nutritional needs of clients with visual impairments or dementia • Discuss at least three unique aspects of nutrition that apply to older adults.

Nutrition • Nutrition is the process by which the body uses food • Malnutrition is a condition resulting from a lack of proper nutrients in the diet. It is chronic inadequate nutrition
Who Is at Risk of Malnutrition • Malnutrition is common among people living in developing countries. Is lack of proper nutrients in the diet. Common amongst poor as well as affluent countries • In the U. S. : – Older adults who are socially isolated or living on fixed incomes – Homeless people – Children of economically deprived parents

Who Is at Risk of Malnutrition (cont’d) • In the U. S. (cont’d): – Pregnant teenagers – People with substance abuse problems such as alcoholism – Clients with eating disorders, such as anorexia nervosa and bulimia nervosa
Basic Nutrients • All humans have basic nutritional needs- researchers recommend the following: • Calories: energy value of food • Proteins: building blocks of the body, composed of amino acids, builds and repairs cells • Carbohydrates: source of quick energy • Fats: concentrated energy source – Saturated fats: generally solid – Unsaturated fats: healthier form of fat

Basic Nutrients • Minerals: non-caloric substances that regulates chemical processes • Vitamins: normal growth, maintenance of health, and functioning of the body ØWater-soluble vitamins: eliminated with body fluids ØFat-soluble vitamins: stored in the body as reserves for future needs • Water: Necessary for life
Health Risks related to Fat and Cholesterol • Excess fat intake is related to heart disease, hypertension, diabetes, and some cancers. • The goal of the government is for at least 50% of people 2 years and older to consume no more than 29. 8%of their daily calories from fat • The American heart Association (AHA, 2010), indicates that consumption of trans fat ( fats that has been processed and hydrogen added), increases the risk for coronary heart disease.

Risks Associated With Cholesterol
Vitamins (Refer to Table 15 -3 in the textbook. )
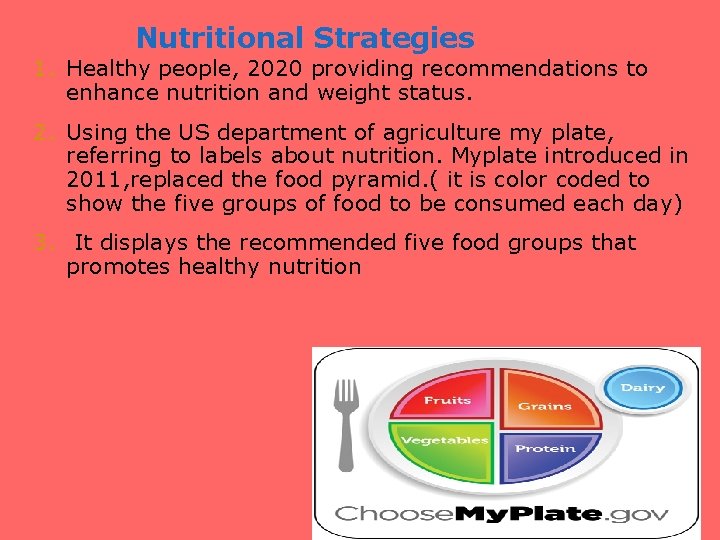
Nutritional Strategies 1. Healthy people, 2020 providing recommendations to enhance nutrition and weight status. 2. Using the US department of agriculture my plate, referring to labels about nutrition. Myplate introduced in 2011, replaced the food pyramid. ( it is color coded to show the five groups of food to be consumed each day) 3. It displays the recommended five food groups that promotes healthy nutrition
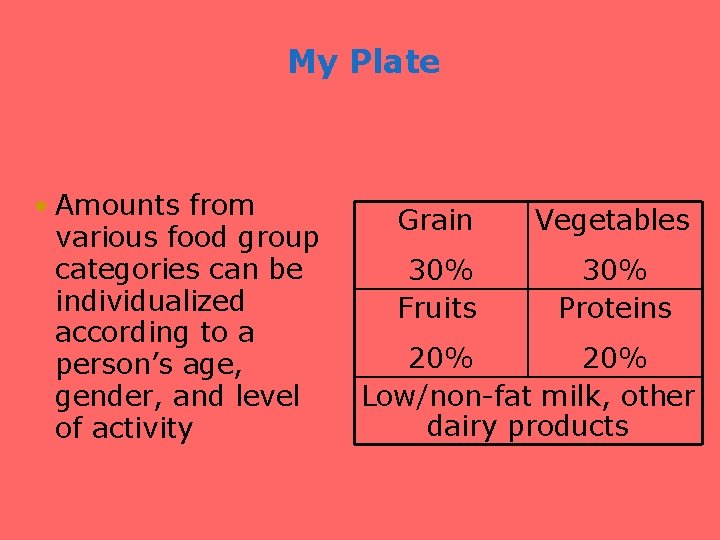
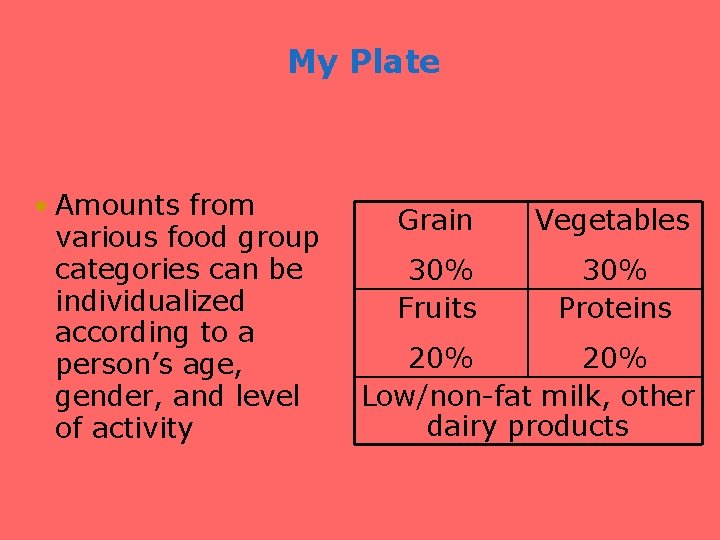
My Plate • Amounts from various food group categories can be individualized according to a person’s age, gender, and level of activity Grain Vegetables 30% Fruits 30% Proteins 20% Low/non-fat milk, other dairy products

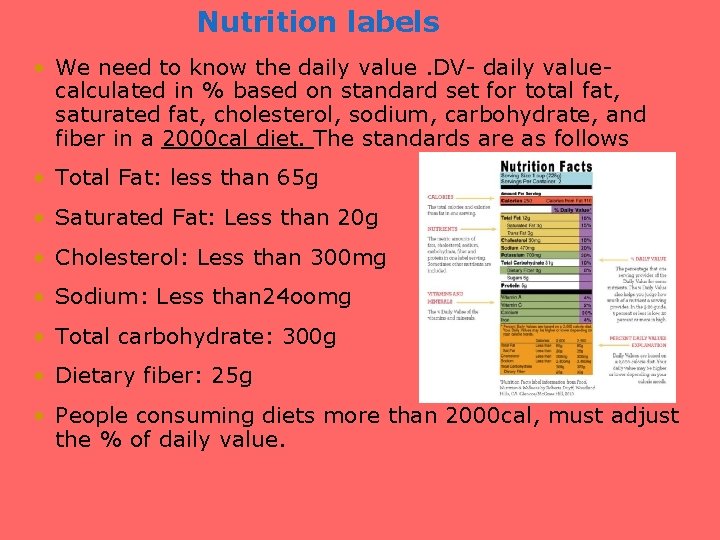
Nutritional Labels • Tells- Amount of each nutrient per serving, using household measurements e. x gm, mg • Must provide printed disease prevention guidelines
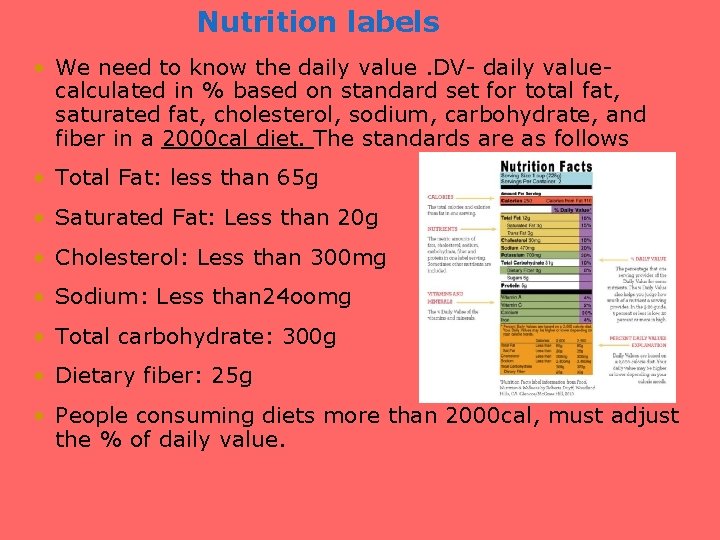
Nutrition labels • We need to know the daily value. DV- daily value- calculated in % based on standard set for total fat, saturated fat, cholesterol, sodium, carbohydrate, and fiber in a 2000 cal diet. The standards are as follows • Total Fat: less than 65 g • Saturated Fat: Less than 20 g • Cholesterol: Less than 300 mg • Sodium: Less than 24 oomg • Total carbohydrate: 300 g • Dietary fiber: 25 g • People consuming diets more than 2000 cal, must adjust the % of daily value.

Nutritional Labels (cont’d) • The federal Nutrition Labeling and Education Act states that companies should comply with standard definitions if they use health-related claims for, example low fat.
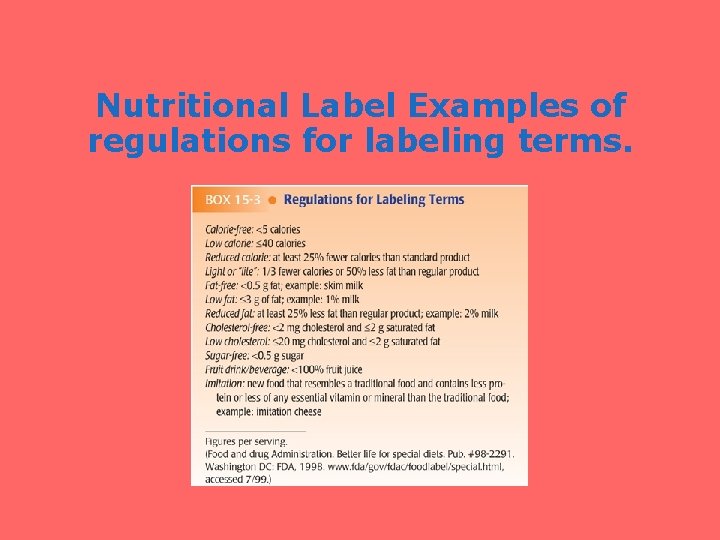
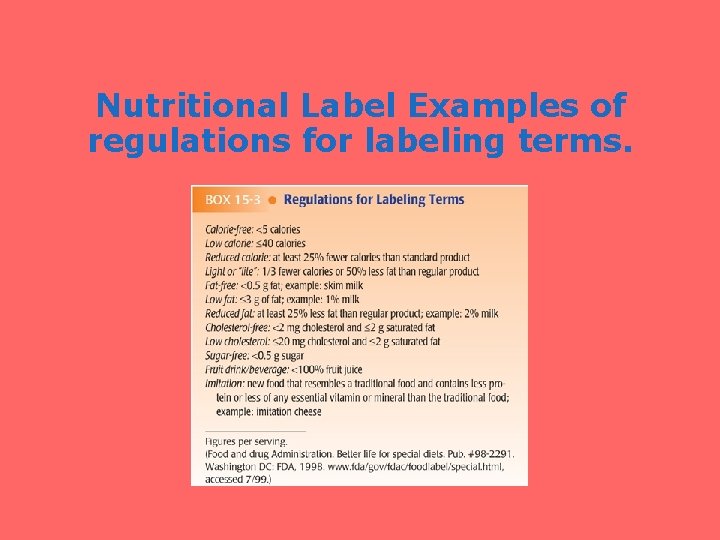
Nutritional Label Examples of regulations for labeling terms.
Factors That Influence Nutritional Needs 1. Influence on eating Habits. 2. Vegetarianism Influence on Eating Habits: • Food preferences acquired during childhood • Established patterns for meals • Attitudes about nutrition, • Knowledge of nutrition • Income level, Time available for food preparation
Factors that Influence Nutritional Needs (cont’d) Influence on eating (Cont’d) • Number of people in the household • Access to food markets • Use of food for comfort, celebration, or symbolic reward • Satisfaction or dissatisfaction with body weight • Religious beliefs

Factors that Influence Nutritional Needs (cont’d) • Vegetarianism Ø Are people who restrict their consumption of animal food sources. Ø They modify their diet for religious or personal reasons Ø It is practiced in various forms an example is vegans ( (rely on plant sources for protein). Ø Semi-vegetarian exclude only red meat Ø Advantages of vegetarians: low incidence of colorectal cancer, fewer problems with obesity and diseases.

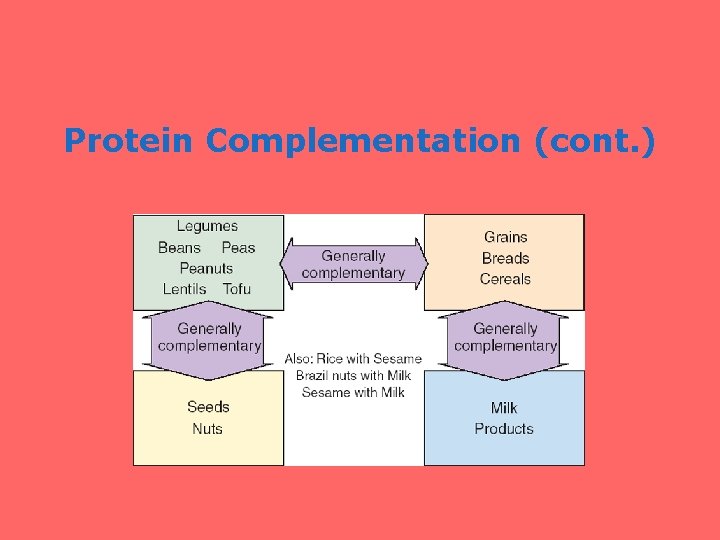
Protein Complementation • Protein complementation involves eating a variety of incomplete plant protein over the course of the day to provide adequate amounts and proportions of all the essential amino acids; found in animal sources • Examples: see next slide for guide
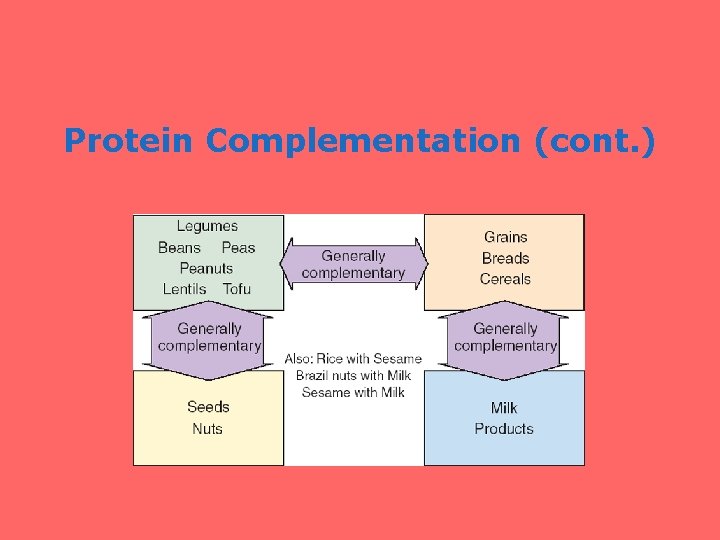
Protein Complementation (cont. )
Nutritional Status Assessment • Nurses identifies current or potential client problems associated with nutrition. • Nurses obtain subjective data by asking client focused questions on a diet history • Nurses obtain objective data using physical assessment techniques.
Objective Data Assessment • So how. • Physical assessment: assessment of physique and general well-being • Laboratory data: used in nutritional assessment. Cholesterol • Anthropometric data: are measurements for body size and composition, by measuring height and weight and calculating body-mass index (BMI)
BMI Cont’d • (BMI )Body mass index- provides numeric data to compare a person’s size in relation to established norms for the adult population- calculated using height and weight). (box 15 -4) • Mid-arm circumference: - helps to determine skeletal muscle mass • Triceps skinfold measurement: - additional data for estimating the amount of subcutaneous fat deposits. ( fig 15 -6) • Abdominal measurement: _ measurement of fatty
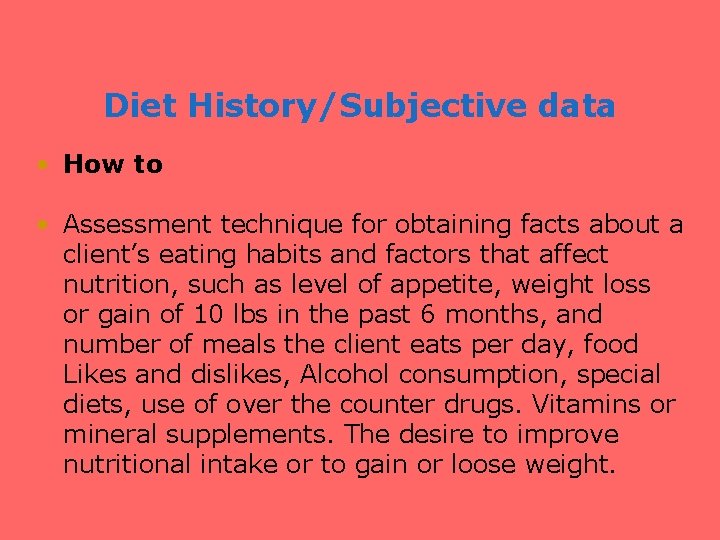
Diet History/Subjective data • How to • Assessment technique for obtaining facts about a client’s eating habits and factors that affect nutrition, such as level of appetite, weight loss or gain of 10 lbs in the past 6 months, and number of meals the client eats per day, food Likes and dislikes, Alcohol consumption, special diets, use of over the counter drugs. Vitamins or mineral supplements. The desire to improve nutritional intake or to gain or loose weight.
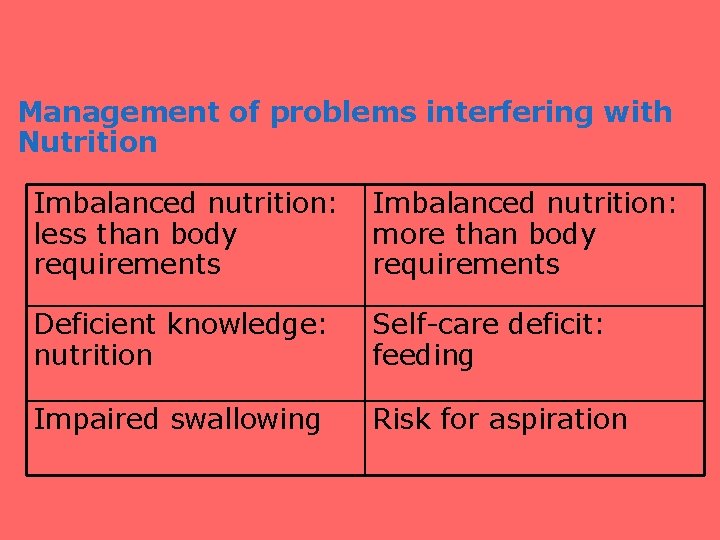
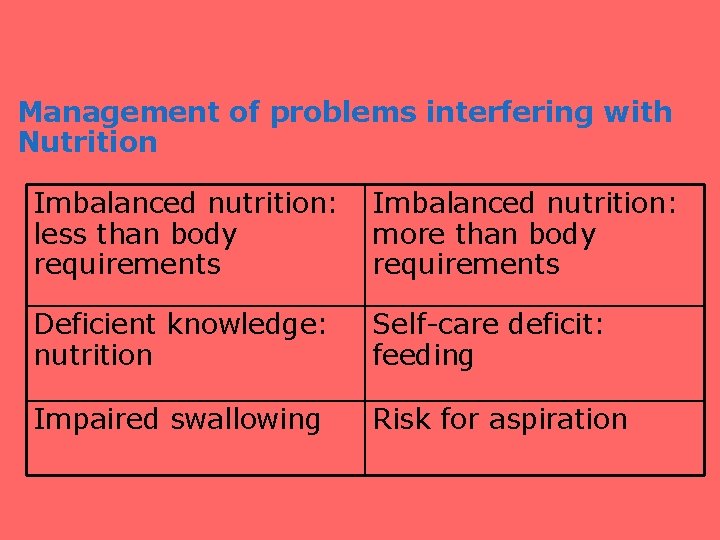
Management of problems interfering with Nutrition Imbalanced nutrition: less than body more than body requirements Deficient knowledge: nutrition Self-care deficit: feeding Impaired swallowing Risk for aspiration
Other Problems interfering with Nutritional • Obesity-A person’s BMI exceeds 30 or trifold measurement exceeds 15 mm. • Emaciation-Prolonged weight loss, or excessiveness leanness, or cachexia general wasting away of the body tissue. • Anorexia- Loss of appetite due to sickness • Nausea-usually preceeds vomiting. • Vomiting- Loss of stomach contents through the mouth.
Other Problems interfering with Nutritional ( Vomiting Cont’d) • Emesis- or vomitus ( substance vomited) • Retching- the act of vomiting without producing vomitus. • Regurgitation-bringing stomach contents to the throat and mouth without the effort of vomiting • Projectile vomiting- vomiting that occurs with great force, is associated with certain diseases.
Other Problems interfering with Nutritional • Stomach gas- results from swallowing air • Eructation- ( Belching) discharge of gas from stomach • Flatus – Gas formed in the intestine/ released from the rectum.
Hospital Diets • Common hospital Diets includes: • Regular or general: allows unrestricted food selections • Light or convalescent: differs from regular diet in preparation; typically omits fried, fatty, gas-forming, and raw foods and rich pastries

Hospital Diets (cont’d) • Soft: contains foods soft in texture; usually low in residue and readily digestible; provides fewer fruits, vegetables, or meats than a light diet • Mechanical soft: resembles a light diet but used for clients with chewing difficulties; provides cooked fruits and vegetables and ground meats
Hospital Diets (cont’d) • Full liquid: fruit and vegetable juices; creamed or blended soups; milk, ices, ice cream, gelatin, junket, custards; and cooked cereals • Clear liquid: water, clear broth, clear fruit juices, plain gelatin, tea, and coffee; may or may not include carbonated beverages • Special therapeutic: foods prepared to meet special needs, such as low in sodium, fat, or fiber • Health care agencies having a dietician
Management of Nutrition • Meal Trays: meals served at bedside or dining rooms or cafeterias • Feeding Assistance- assistance with eating, and for clients with dysphagia ( difficulty swallowing). Remain with the client throughout eating. Place client in sitting position. Encourage the client to eat slowly. Limit distracting stimuli. Give short, simple instructions to prompt the client to eat and swallow • Feeding a visually impaired client • Place towel across the clients chest, Arrange for finger foods, use dishes with rims.
Management of Nutrition • Feeding clients with dementia ( deteroriation of previous intellectual capacity) • Have the same staff help the client • Be consistent with the time and place for eating • Place the food try close to the client • Guide the hand food to the client’s mouth
Nursing Responsibilities • Ordering and canceling diets for clients • Serving and collecting meal trays • Helping clients to eat • Recording the percentage of food that clients eat
Older Adults • Evaluation of nutritional status in annual examinations or more frequently • Diminished senses of smell and taste; require fewer calories; nutritional supplements should be evaluated; if sedentary, teach benefits of exercise; oral and dental problems • Chronic conditions; food–drug interactions; poor intake due to ill fitted dentures, encourage adequate fluid intake.
Gerontological Considerations cont’d • Dysphagia among older adults often results from neurological conditions including stroke, esophageal disorders, or increased pressure from abdominal disorders.
References Timby, B. (2014). Fundamental nursing skills and concepts (11 th ed. ). Philadelphia, PA: Lippincott Williams & Wilkins. Google pictures. (2015, August 10). Retrieved from http: //www. google. com
 Nutrition fundamentals of nursing
Nutrition fundamentals of nursing Nutritional needs in fundamentals of nursing
Nutritional needs in fundamentals of nursing Outlook pnu
Outlook pnu Pnu point
Pnu point Pnu korea
Pnu korea Nursing chapter 1
Nursing chapter 1 Chapter 17 fundamentals of nursing
Chapter 17 fundamentals of nursing Back channeling nursing
Back channeling nursing Kataoka-yahiro and saylor's model
Kataoka-yahiro and saylor's model Fundamentals of nursing chapter 16
Fundamentals of nursing chapter 16 Hygiene fundamentals of nursing
Hygiene fundamentals of nursing Activity and exercise fundamentals of nursing
Activity and exercise fundamentals of nursing Procedure for admitting a patient
Procedure for admitting a patient Fundamentals of nursing craven
Fundamentals of nursing craven Sensory functioning fundamentals of nursing
Sensory functioning fundamentals of nursing Pain definition nursing
Pain definition nursing Ostonies
Ostonies Vitals include
Vitals include Fundamentals of nursing care concepts connections & skills
Fundamentals of nursing care concepts connections & skills Conclusion of positioning in nursing
Conclusion of positioning in nursing Bedpan placement
Bedpan placement Risk for aspiration nursing care plan
Risk for aspiration nursing care plan Psalm 76 tpt
Psalm 76 tpt Psalm 42 gnt
Psalm 42 gnt Pasal 145 kuhap
Pasal 145 kuhap Oehwg
Oehwg 5 4 145 lbs woman
5 4 145 lbs woman Jar 145
Jar 145 145 iq percentile
145 iq percentile Alanintransaminase højt
Alanintransaminase højt Lied 189 weerklank
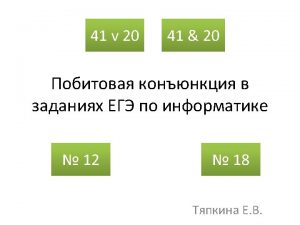
Lied 189 weerklank Cs 145
Cs 145 Gezang 145
Gezang 145 Gezang 145
Gezang 145 Ccr 145-8-3
Ccr 145-8-3 Ephesians 1:7-9
Ephesians 1:7-9 750 yüzlüğe yuvarlama
750 yüzlüğe yuvarlama Generel helbredsattest eksempel
Generel helbredsattest eksempel Math 145
Math 145 Supercade-suba (2) -avenida calle 145 no.103b-90
Supercade-suba (2) -avenida calle 145 no.103b-90 Réglementation part 145
Réglementation part 145