Asthma and COPD Current Therapeutic Interventions and Future









- Slides: 93
, Asthma and COPD: Current Therapeutic Interventions and Future Treatment 39 th Annual Convention of the National Diamondback Pharmacy Alumni Council E. Watson Pharm. D.
Learning Objectives: upon completion of this lecture, the participants should be able to n n To compare and contrast the epidemiology, clinical and economic burden, and natural history of chronic obstructive pulmonary disease (COPD) and asthma Outline the pathophysiology, incidence, presentation, and diagnosis of COPD and asthma; Define the processes and exacerbation of COPD and asthma and the need for additional referral; (note the influence of HIV/ AIDS infection) Counsel patients about nonpharmacological options for optimizing control of their disease.
Learning Objectives: upon completion of this lecture, the participants should be able to n n n Review the new therapeutic options available for the treatment of COPD and asthma; Provide participants with the knowledge and skills (techniques) to properly administer medications used for the treatment of COPD and asthma; Provide participants with the tools to educate others in their practice and the patients who they serve to properly administer COPD/asthma medications.
Characteristics Asthma and COPD n n Both have a reduced rate of pulmonary airflow resulting from increased inflammation. Airway obstruction is usually reversible in patients with asthma COPD airway obstruction is not fully reversible. Either disease may develop acute exacerbations with increased inflammation of the airway and worsening airway obstruction causing reduced rate of pulmonary airflow.
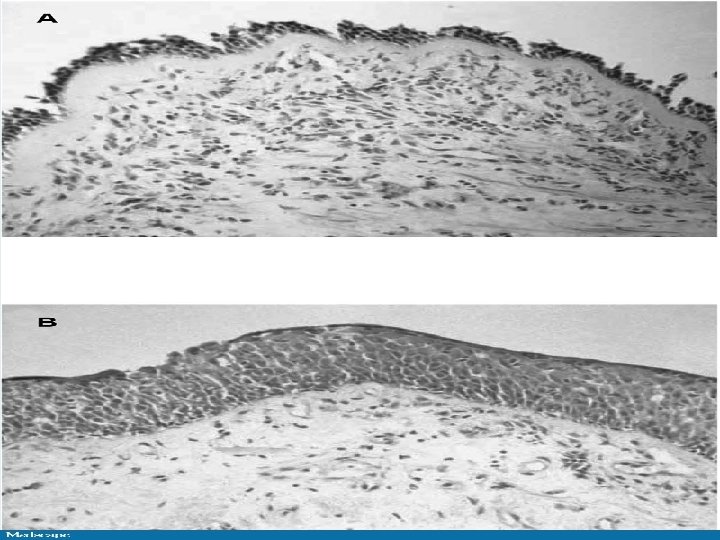
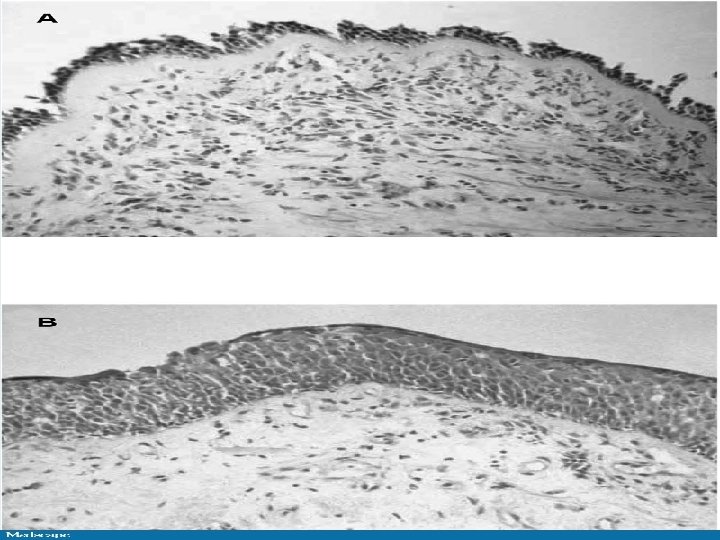
Airway mucosa (bronchial biopsy) from a patient with asthma, heavy smoker with COPD. n A, patient with asthma, showing loss of surface epithelium and early basement membrane thickening. n B, a heavy smoker with COPD with an FEV 1 of 40% predicted, showing epithelial squamous metaplasia. Remodeling in asthma and chronic obstructive lung disease. Am J Respir Crit Care Med. 2001; 164: S 28 -S 38.
Definition: National Heart, Lung and Blood institute (NHLBI) and WHO n n n COPD is a group of chronic respiratory disorders that lead to progressive tissue degeneration and obstruction in the airways and lungs that is not fully reversible. They are debilitating conditions that affect the individual’s ability to work and function independently. These include; Chronic bronchitis, asthmatic bronchitis and emphysema. May coexist. COPD may coexist with asthma.
Definition: GOLD COPD is a preventable and treatable disease with significant extra-pulmonary effects that may contribute to severity in individual patients. Its pulmonary component is characterized by airflow limitation that is non-reversible. The airflow resistance is normally progressive and is associated with an abnormal inflammatory response of the lung to noxious particles or gas. The GOLD definition does not use the term bronchitis or emphysema and excludes asthma (reversible air flow limitation)
Asthma n Asthma is a common chronic disorder of the airways that is complex and characterized by n variable and recurring symptoms, n airflow obstruction, n Bronchial hyperresponsiveness, n and an underlying inflammation
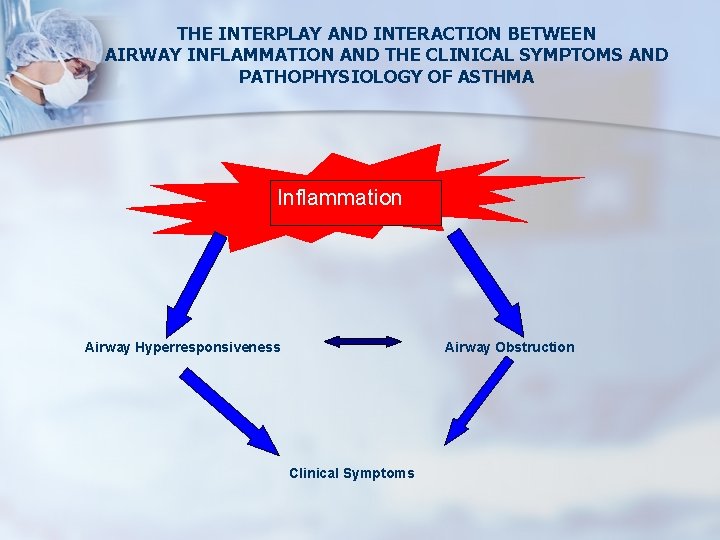
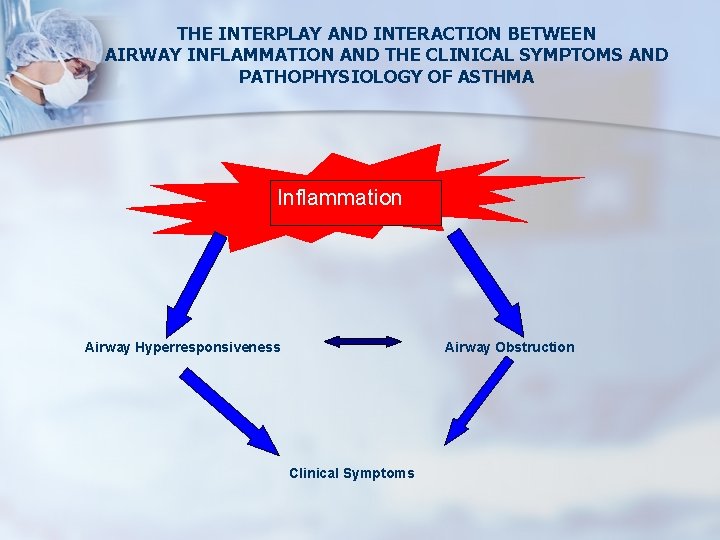
THE INTERPLAY AND INTERACTION BETWEEN AIRWAY INFLAMMATION AND THE CLINICAL SYMPTOMS AND PATHOPHYSIOLOGY OF ASTHMA Inflammation Airway Hyperresponsiveness Airway Obstruction Clinical Symptoms

Asthma Many cells and cellular elements play a role: in particular, n mast cells, n eosinophils, n T lymphocytes, n macrophages, n neutrophils, n and epithelial cells.
Epidemiology The rates for asthma prevalence have been consistently higher in children than in adults. n Asthma is more common in boys than in girls n Estimates from 2004 show that approximately 5. 1 million men (5%) and 9. 2 million women (8%) had asthma n
Epidemiology n n In 2006, an estimated 12. 1 million adults in the United States were diagnosed with COPD. The overall prevalence of COPD has been estimated at 24 million Higher among whites than blacks and males than among women; Rising rates of smoking have been accompanied by a rising prevalence of COPD.
Epidemiology n n Asthma is more prevalent than COPD, However, COPD imposes a heavier disease burden due to n n n greater number of hospitalizations, greater severity of exacerbations, uniform progression of the disease, and poorer overall prognosis. The estimated total cost of asthma in the United States in 2004 was $16. 1 billion Total cost of COPD was more than twice as high at $37. 2 billion
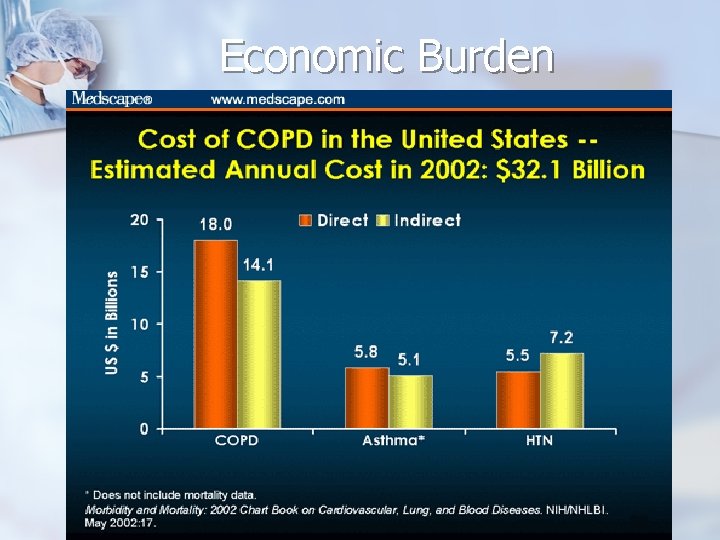
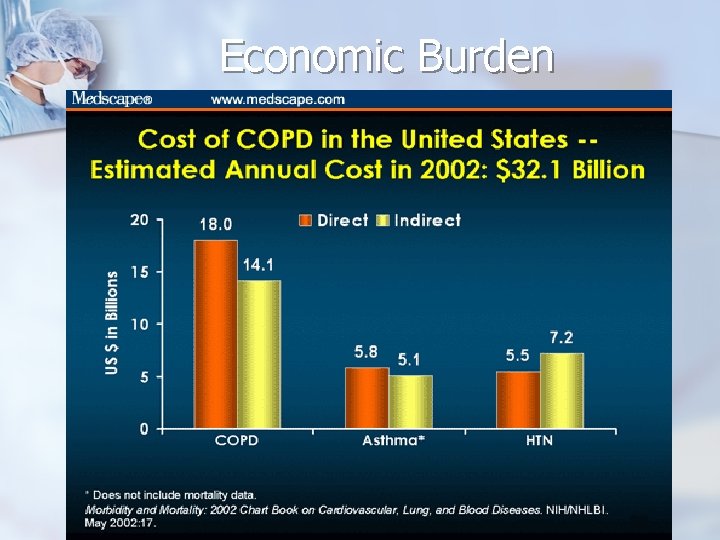
Economic Burden
Economic Burden Data from 2004 reveal that the costs have risen to $33. 72 billion in 2004. n Compared with costs of all chronic diseases in the US, which is about $470 billion, this is a big chunk of money spending on Asthma and COPD. n
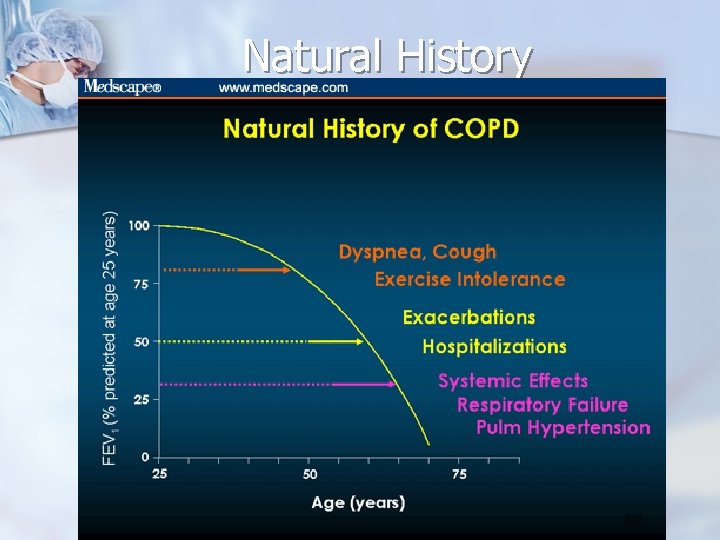
Natural History n n n Asthma is most often associated with onset during childhood, prior atopic reactions, and a family history of atopy or asthma In some cases, asthma symptoms diminish after childhood In contrast, COPD is essentially unknown in children and is rare in younger adults without a history of alpha 1 -antitrypsin deficiency. After age 40, however, the prevalence of COPD increases substantially with aging
Natural History COPD often coexists with cardiac disease, depression, and other chronic conditions. n Some of the coexisting conditions may be secondary to long-term tobacco exposure n Or may be part of the same inflammatory process that affects the lungs in COPD n
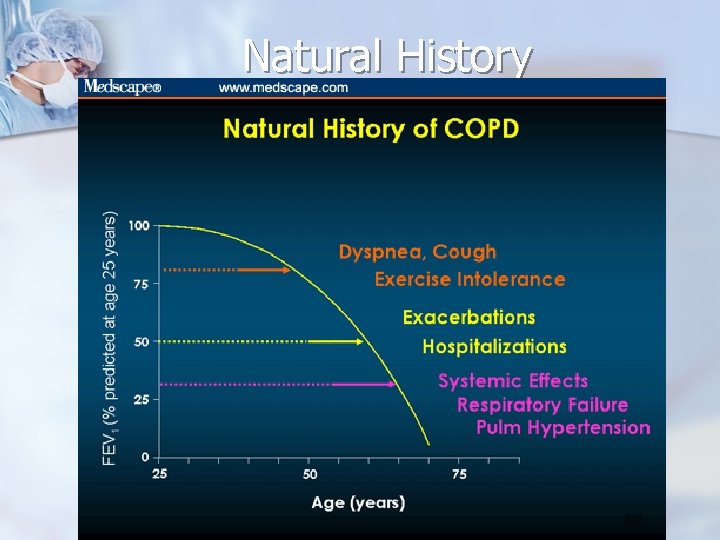
Natural History
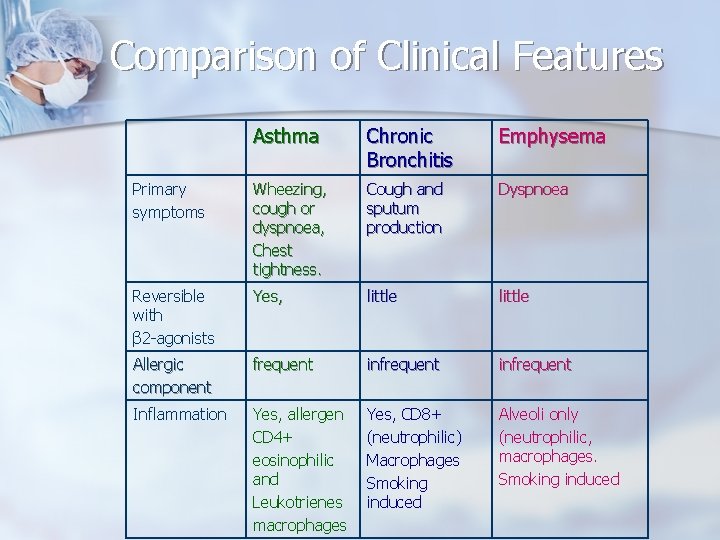
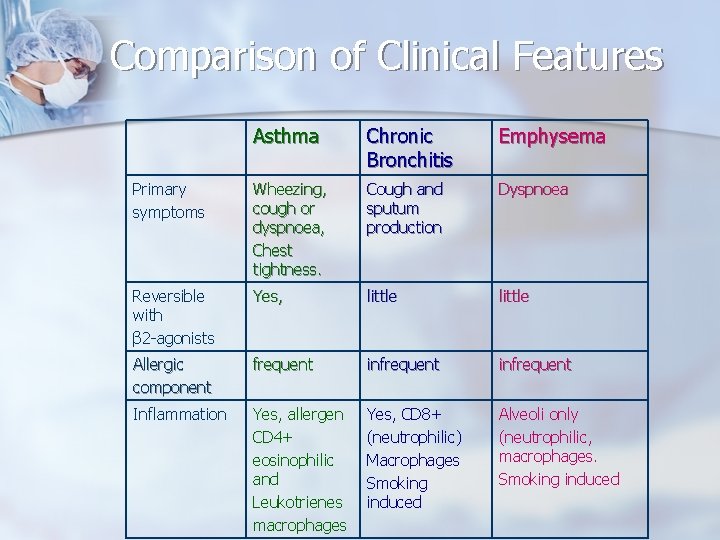
Comparison of Clinical Features Asthma Chronic Bronchitis Emphysema Primary symptoms Wheezing, cough or dyspnoea, Chest tightness. Cough and sputum production Dyspnoea Reversible with β 2 -agonists Yes, little Allergic component frequent infrequent Inflammation Yes, allergen CD 4+ eosinophilic and Leukotrienes macrophages Yes, CD 8+ (neutrophilic) Macrophages Smoking induced Alveoli only (neutrophilic, macrophages. Smoking induced
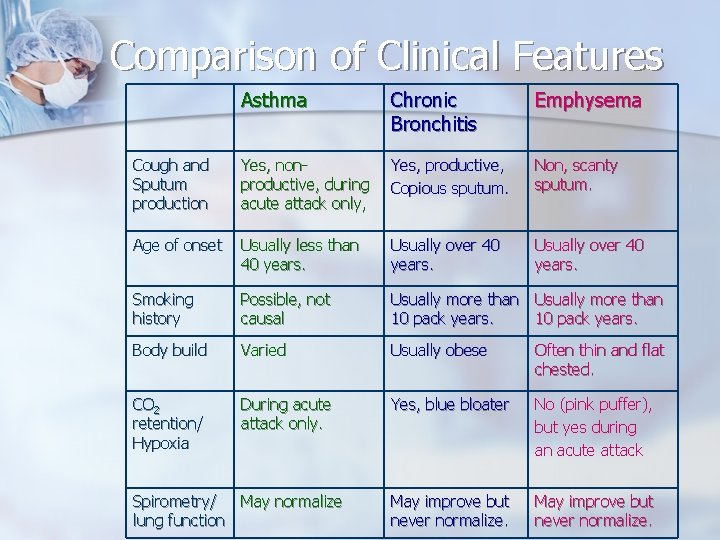
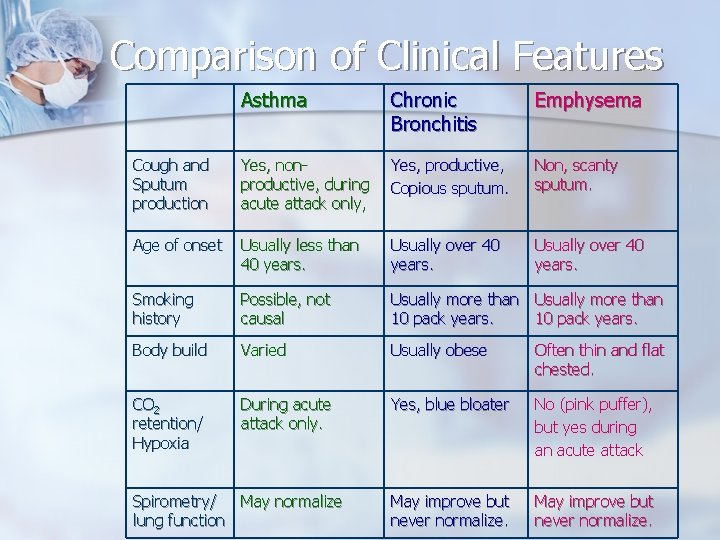
Comparison of Clinical Features Asthma Chronic Bronchitis Emphysema Cough and Sputum production Yes, nonproductive, during acute attack only, Yes, productive, Copious sputum. Non, scanty sputum. Age of onset Usually less than 40 years. Usually over 40 years. Smoking history Possible, not causal Usually more than 10 pack years. Body build Varied Usually obese Often thin and flat chested. CO 2 retention/ Hypoxia During acute attack only. Yes, blue bloater No (pink puffer), but yes during an acute attack May improve but never normalize. Spirometry/ May normalize lung function
Pathophysiology n Airway obstruction in asthma results from n bronchial smooth muscle constriction, n airway hyperreactivity to allergens and irritants, n inflammation accompanied by increased eosinophils and CD 4+ lymphocytes
Pathophysiology (EPR 3) n n n Report emphasizes variability in the pattern of inflammation, indicating phenotypic differences that may influence response to treatment. (cytokines and chemokines) Evidence is showing an expanding role of viral respiratory infections. Current therapy with anti-inflammatory agent does not appear to prevent progression of the underlying disease. (control symptoms, airway limitation, exacerbations)
Pathophysiology n Airway obstruction in COPD is associated with n n cellular damage and mucus hypersecretion; inflammation becomes more prominent in exacerbations of severe disease. Cellular damage is a progressive process initiated by inflammatory changes induced by smoking and other environmental toxins to pulmonary tissues. the cellular destruction and structural changes associated with COPD interfere with oxygenation and pulmonary circulation.
Pathophysiology n Emphysema is characterized by loss of lung elastic recoil and loss of alveolar structure resulting from inflammatory cell-mediated damage to bronchioles, alveolar ducts, and alveoli.
Pathophysiology n In chronic bronchitis, chronic cough and increased sputum production occur as a consequence of mucosal infiltration by inflammatory cells that lead to cellular damage to the airway mucosa.
Diagnosis Detailed medical history. n Physical examination n Spirometry can demonstrate obstruction and assess reversibility in patients older than 5 years of age. n
Diagnosis n n n Spirometry is the most commonly performed noninvasive test of lung function. Considered the most practical and reliable tool for establishing the presence and severity of obstructive airway diseases, including asthma and COPD. Standardized guidelines are available (eg, the American Thoracic Society/European Respiratory Society Standardization of Lung Function Testing
Diagnosis n n n Discussions have been added on the use of spirometry, especially in children, and on the criteria for reversibility. Information has been added on vocal cord dysfunction (VCD) and cough variant asthma as an alternative diagnosis. Reference has been added to updated information in another component on comorbid conditions that may complicate diagnosis and treatment of asthma n n n (e. g. , allergic bronchopulmonary aspergillosis (ABPA), obstructive sleep apnea (OSA), GERD).
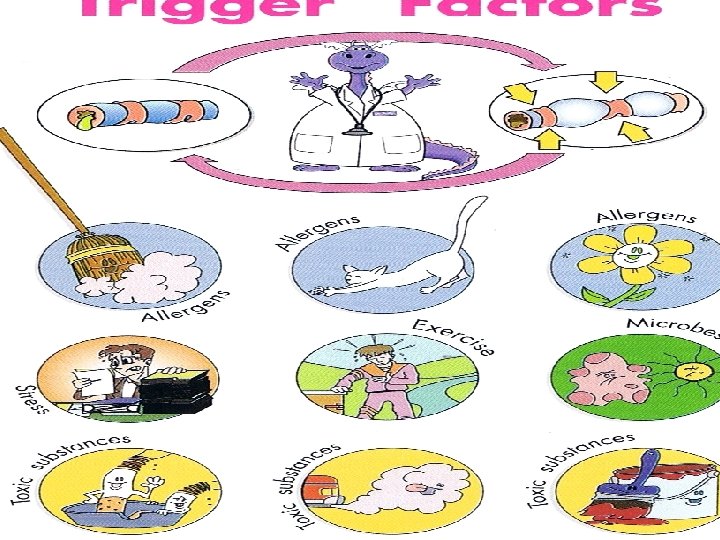
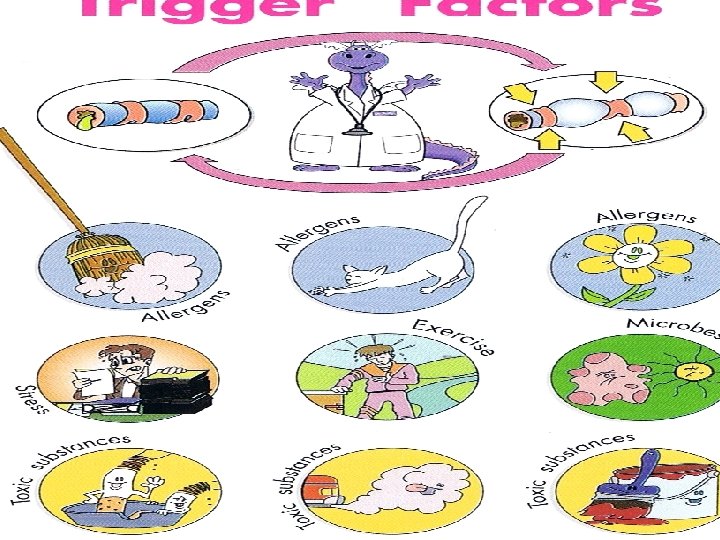
KEY SYMPTOM INDICATORS FOR CONSIDERING A DIAGNOSIS OF ASTHMA n Wheezing, (especially in children. ) n n History of Cough (worse particularly at night), n n Recurrent wheeze, difficulty in breathing, chest tightness Symptoms occur or worsen in the presence of, n n A lack of wheezing and a normal chest examination do not exclude asthma. Exercise, viral infection, Inhalant allergens (e. g. , animals with fur or hair, house-dust mites, mold, pollen), irritants (tobacco or wood smoke, airborne chemicals), Changes in weather, Strong emotional expression (laughing or crying hard), Stress, menstrual cycles Symptoms occur or worsen at night, awakening the patient.
Laboratory Test. n n n chest X-ray PFT ( assess pre and post bronchidilators) – decreased FEV 1 and FVC ABG – hypoxemia, hypercarbia and acidemia Hct/Hgb – erythrocytosis ECG-RVH Cultures
Classification of Asthma (Changes) n The key elements of assessment and monitoring are refined to include the separate, but related, concepts of n severity, n control, n responsiveness to treatment.
Classification of Asthma Classifying severity is emphasized for initiating therapy; n assessing control is emphasized for monitoring and adjusting therapy. n Asthma severity and control are defined in terms of two domains: n n impairment n risk
Classification of Asthma n n impairment —to emphasize the need to consider separately asthma’s effects on quality of life and functional capacity on an ongoing basis (i. e. , in the present) the risks asthma presents for adverse events in the future, n n n such as exacerbations and progressive loss of pulmonary function. These domains of asthma may respond differentially to treatment.
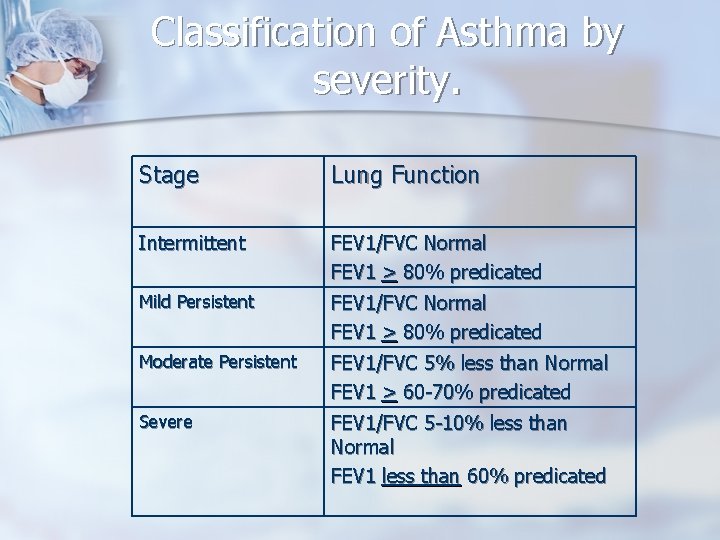
Classification of Asthma n n n The severity classification for asthma changed the category of mild intermittent to emphasize that even patients who have intermittent asthma can have severe exacerbations. A note of emphasis has also been added that acute exacerbations can be mild, moderate, or severe in any category of persistent asthma. A new emphasis on using FEV 1/FVC has been added for classifying severity in children because it may be a more sensitive measure than FEV 1.
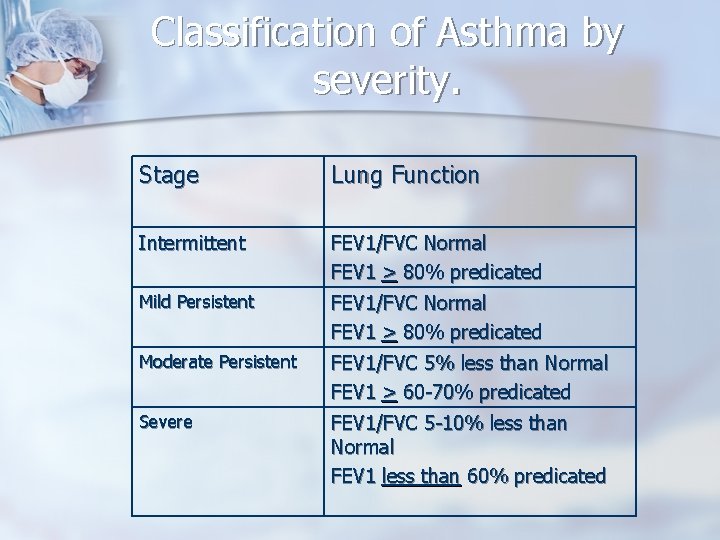
Classification of Asthma by severity. Stage Lung Function Intermittent FEV 1/FVC Normal FEV 1 > 80% predicated Mild Persistent FEV 1/FVC Normal FEV 1 > 80% predicated Moderate Persistent FEV 1/FVC 5% less than Normal FEV 1 > 60 -70% predicated Severe FEV 1/FVC 5 -10% less than Normal FEV 1 less than 60% predicated
New Classifications (GINA) Controlled n Partly Controlled n Uncontrolled This is due to the understanding that severity is also a factor of response to treatment. n
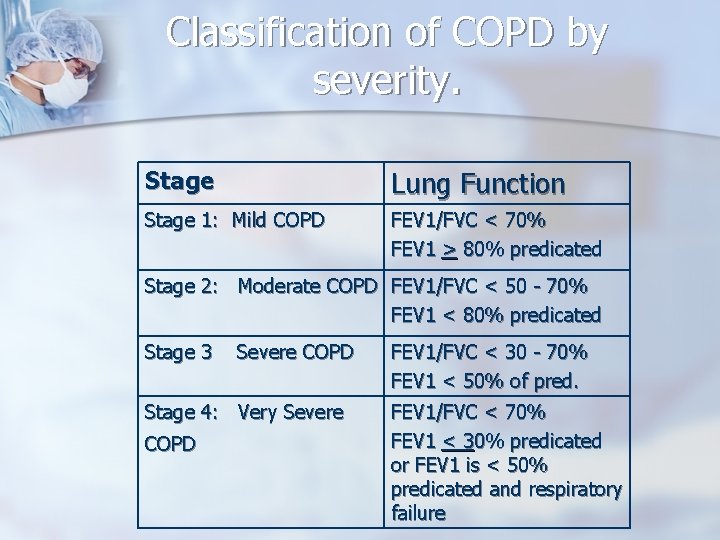
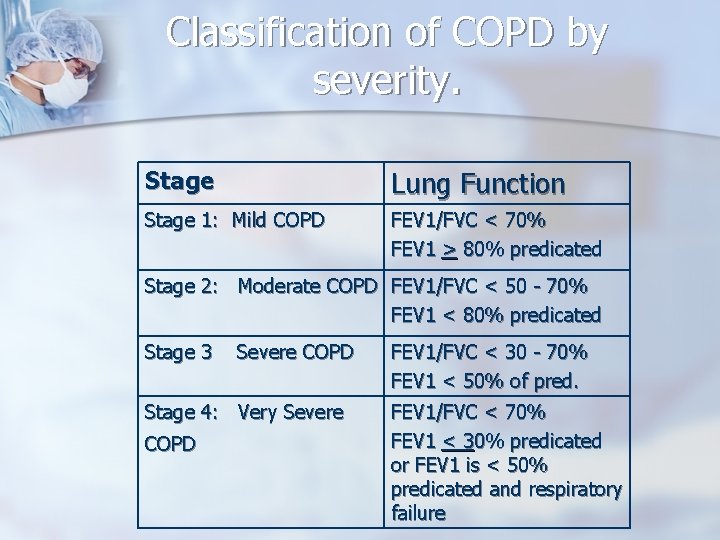
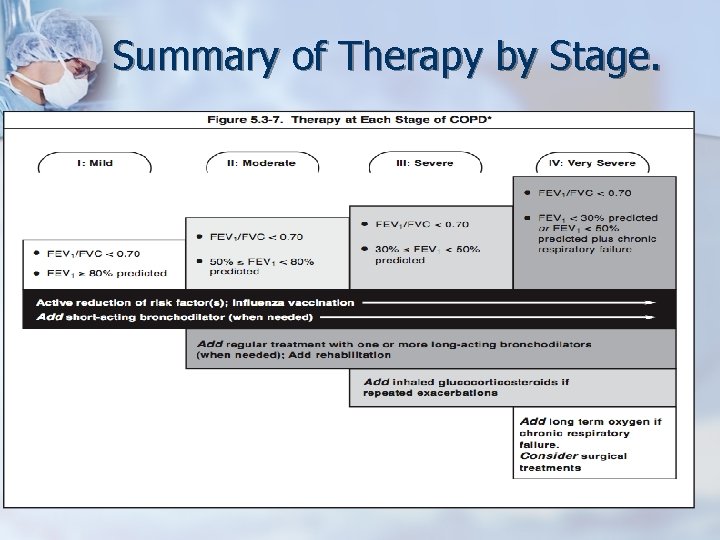
Classification of COPD by severity. Stage Lung Function Stage 1: Mild COPD FEV 1/FVC < 70% FEV 1 > 80% predicated Stage 2: Moderate COPD FEV 1/FVC < 50 - 70% FEV 1 < 80% predicated Stage 3 Severe COPD Stage 4: Very Severe COPD FEV 1/FVC < 30 - 70% FEV 1 < 50% of pred. FEV 1/FVC < 70% FEV 1 < 30% predicated or FEV 1 is < 50% predicated and respiratory failure
Factors Determining Severity of Chronic COPD. n n n n Severity of symptoms Severity of airway limitation Frequency and severity of exacerbations Presence of complications of COPD Presence of respiratory insufficiency Comorbidity General health status Number of medications needed to manage the disease
Process of exacerbation (Asthma) n n n Acute or subacute episodes of progressively worsening shortness of breath, cough, wheezing, and chest tightness—or some combination of these symptoms. Characterized by decreases in expiratory airflow. Can be measured. (spirometry or PEF). Can vary widely among individuals and within individuals, from very rare to frequent.
Process of exacerbation. Asthma n n The classification of severity focuses on the frequency of exacerbations Severity of disease does not necessarily correlate with the intensity. Can vary from mild to very severe and lifethreatening. Patients at any level of severity, even intermittent asthma, can have severe exacerbations.
Process of exacerbation. COPD n n Deterioration in lung function is correlated with the severity of the disease and the consequences. Airflow limitation is very important, Causes increased n n n dyspnea, deconditioning, decreased exercise tolerance, inactivity, deterioration in the health status. At the top of the list are exacerbations, which can actually worsen the outcome of COPD.

Components of Asthma and COPD Management. n n Assess and monitor disease Reduce risk factors (COPD) / Control environmental factors or comorbid conditions. Process of exacerbation. Manage stable Disease -Education -Non-pharmacologic -Pharmacologic Manage exacerbation
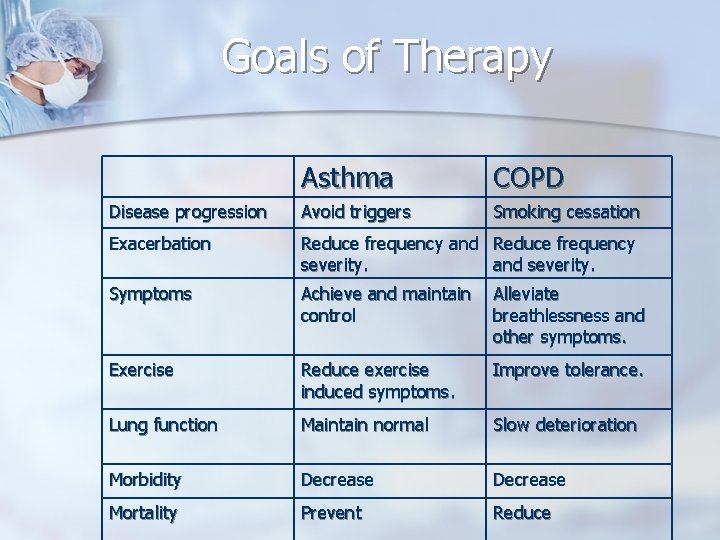
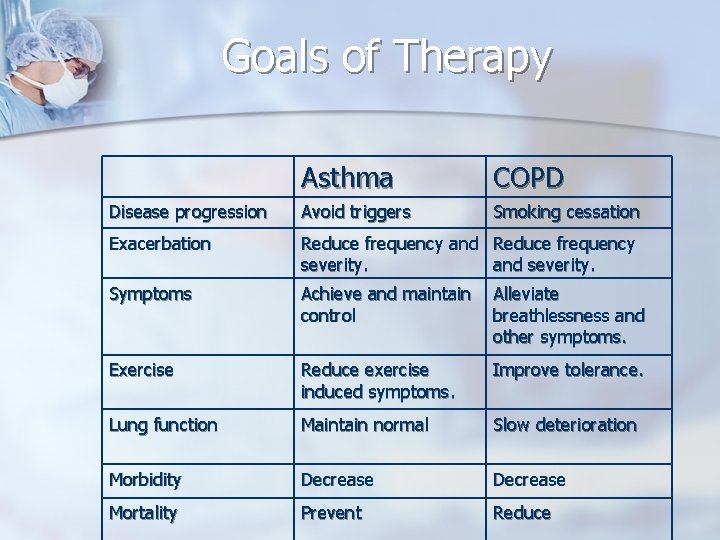
Goals of Therapy Asthma COPD Disease progression Avoid triggers Smoking cessation Exacerbation Reduce frequency and Reduce frequency severity. and severity. Symptoms Achieve and maintain control Alleviate breathlessness and other symptoms. Exercise Reduce exercise induced symptoms. Improve tolerance. Lung function Maintain normal Slow deterioration Morbidity Decrease Mortality Prevent Reduce
Goals of Therapy 2008 GINA guidelines stresses that the overall goal of therapy for Asthma is to achieve and maintain Clinical Control. n Also emphasizes that increase use of daily reliever medications indicate a deterioration. n
Non-Pharmacological Management. (NPT) Discontinue smoking n Chest Physiology n Breathing exercises n Rehabilitation n Preventative measures. n
Discontinue Smoking most effective strategy to reduce the risk of developing COPD and affect the long-term rate of decline in FEV 1. n Group therapy n Drugs (Chantrix; varenicline), nicotine replacement. n Hypnosis n
Chest Physiology Postural drainage n Chest percussion and vibration n Use if > 30 cc sputum/day n
Breathing Exercises Inspire slowly and expire through pursed lips n Inspiratory muscle training n Breathing retraining n
Rehabilitation Exercise reconditioning – increase endurance, exercise tolerance, maximal oxygen consumption n Energy conservation n Nutrition n Psychosocial management – anxiety, depression and problems with cognitive perceptual and motor activity; financial and social resources n
Preventative Measures n n n Vaccines – annual influenza vaccine. Protection rate is 60 -80 % Pneumococcal vaccine – recommended for patients with COPD, revaccination for patients>65 years if vaccination is >5 years Amantadine – efficacy is 50 -90% 100 mg bid for ages <65 mg. 100 mg/day for ages > 65 years. Useful in non-immunized but exposed patients
Pharmacological Management of Asthma (New) LABA should not be used as monotherapy. n Used in combination with ICS n Recent data indicate an increased risk of Asthma related deaths in a small group of individuals when LABA used alone. n
Pharmacological Management of Asthma (New) n n Of the adjunctive therapies available, LABA is the preferred therapy to combine with ICS in youths ≥ 12 years of age and adults (Evidence A). (EP 3) the beneficial effects of LABA in combination therapy for the great majority of patients who require more therapy than low-dose ICS alone to control asthma (i. e. , require step 3 care or higher) should be weighed against the increased risk of severe exacerbations, although uncommon, associated with the daily use.
Pharmacological Management of Asthma (New) n n In both the National Heart Lung and Blood Institute/National Asthma Education and Prevention Program and Global Initiative for Asthma guideline updates, ICSs are confirmed as the preferred therapy for asthma inflammation. Other considerations, such as allergic disease, adherence, and acceptability, should be considered when individualizing therapy.
Pharmacological Management of Asthma (New) Immunomodulators are the only additive therapy other than LABA which demonstrates added efficacy to high dose ICS. n FDA 2007 update for anaphylaxis reaction with Omalizumab. n
Pharmacological Management of Asthma (New) n n A study suggests that children who have higher levels of eosinophilic/allergic airway inflammation (nitric oxide, Ig. E levels, total eosinophil levels) or low pulmonary function are more likely to respond favorably to ICS than to LTRA. Children who do not have these markers appeared to respond equally to treatment with ICS or LTRA (Szefler et al. 2005; Zeiger et al. 2006).
Pharmacological Management of Asthma (New) Leukotriene modifiers now have a more prominent role as controller medications, particularly in adults. n Monotherapy with cromones no longer an alternative to monotherapy with low dose ICS in adults. n
Pharmacological Management of Asthma (New) n Changes to eqipotent doses of ICS.
Pharmacological Management of Asthma (New) n Treatment organized into 5 steps.
Summary of recommendations for treatment of children under 5 years. Spacer + Budesonide dose 400 mcg or equivalent result in near maximum benefits. n Use of oral or inhaled intermittment glucocorticosteroid in children with viral induced wheezing remains controversial. n ICS Not recommended to prevent transient early wheezing. n
Summary of recommendations for treatment of children under 5 years. Leukotriene modifiers recommended to reduce viral induced wheezing in children age 2 -5 years with a history of intermittent asthma. n Rapid acting inhaled B 2 -agonist are the best bronchodilators and are recommended for treating acute asthma in children of all ages. n
Summary of recommendations for treatment of children under 5 years. If Low dose ICS does not achieve control, increasing the dose may be the best option. n Combination therapy, LABA, Leukotrine modifiers, theophylline in uncontrolled asthma has not been studied in children under 5 years. n
Pharmacological Management of COPD n n n n n Oxygen Anticholinergics Short acting Beta Agonists (SABA) Long Acting Beta Agonist (LABA) Combination therapy (CT) Theophylline Oral Steroids Inhaled steroids (IC) Antibiotics
TREATMENT CHANGES The use of inhaled corticosteroids (ICS) and long-acting beta 2 adrenergics (LABA) in fixed combination (ICS/LABA) was recently extended to COPD patients with a baseline FEV 1 50 -60% predicted, thus broadening the original guideline indications (GOLD 2006) that limited their use only to stages III and IV. n
TREATMENT CHANGES Combining bronchodilators of different pharmacological classes may improve efficacy and reduce side effects compared to increasing the dose of a single agent. n Continued support that there is no benefit to use of short acting bronchodilators on a regular basis. n
TREATMENT CHANGES Inhaled Anticholinergic + Sympathomimetic bronchdilators can achieve meaningful increases in lung function even in patients with moderate to severe COPD. n Long acting anticholinergics improve the effectiveness of pulmonary rehabilitation. n
TREATMENT CHANGES No difference in incidence of exacerbations were found between Tiotropium and combination therapy. n Some evidence that COPD patients who have not been treated with ICS, treatment with mucolytics such as carbocisteine may reduce exacerbations. n
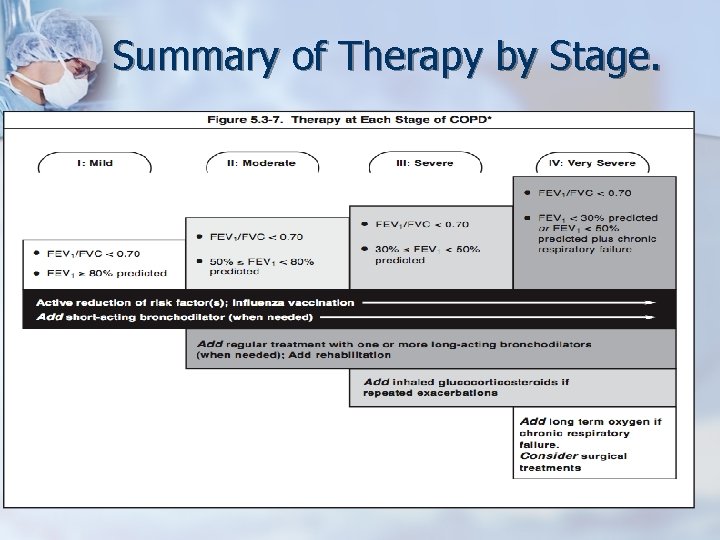
Summary of Therapy by Stage.
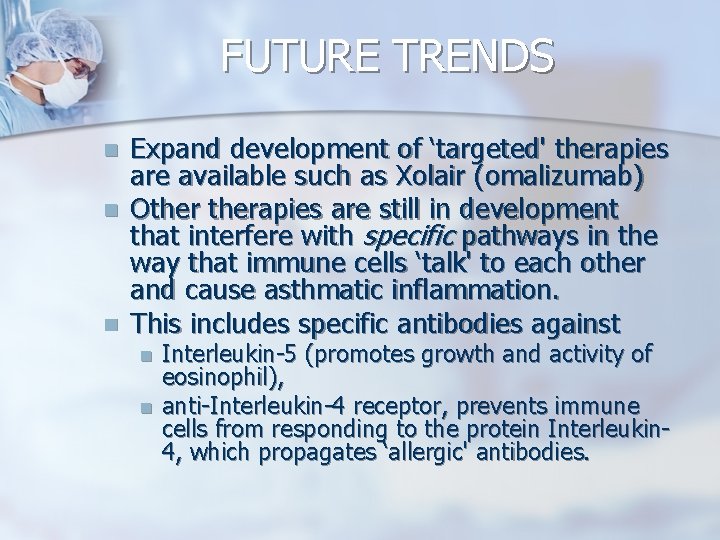
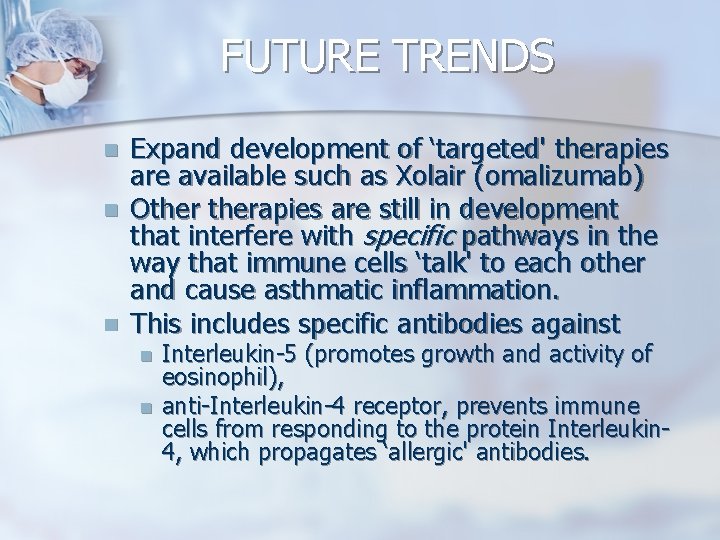
FUTURE TRENDS n n n Expand development of ‘targeted' therapies are available such as Xolair (omalizumab) Otherapies are still in development that interfere with specific pathways in the way that immune cells ‘talk' to each other and cause asthmatic inflammation. This includes specific antibodies against n n Interleukin-5 (promotes growth and activity of eosinophil), anti-Interleukin-4 receptor, prevents immune cells from responding to the protein Interleukin 4, which propagates ‘allergic' antibodies.

FUTURE TRENDS Research targeting understanding the early steps in the development of the immune system in asthma. n Research studies have shown that there is a link between the environment in which children grow up and the risk of developing asthma and allergies. n
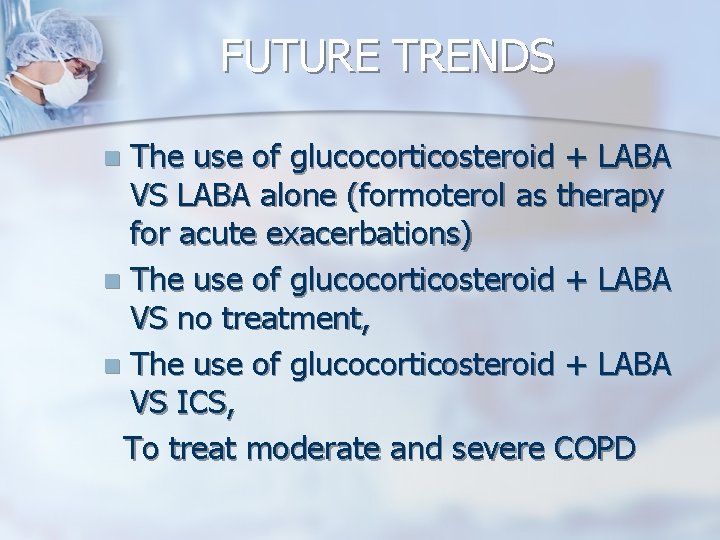
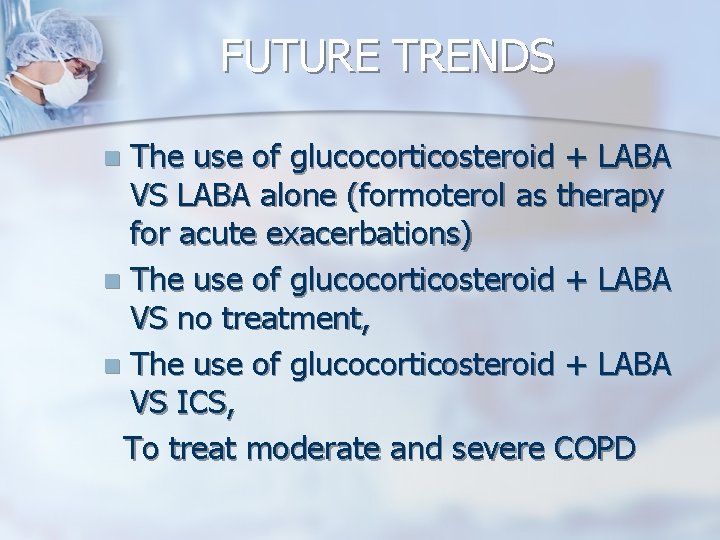
FUTURE TRENDS The use of glucocorticosteroid + LABA VS LABA alone (formoterol as therapy for acute exacerbations) n The use of glucocorticosteroid + LABA VS no treatment, n The use of glucocorticosteroid + LABA VS ICS, To treat moderate and severe COPD n
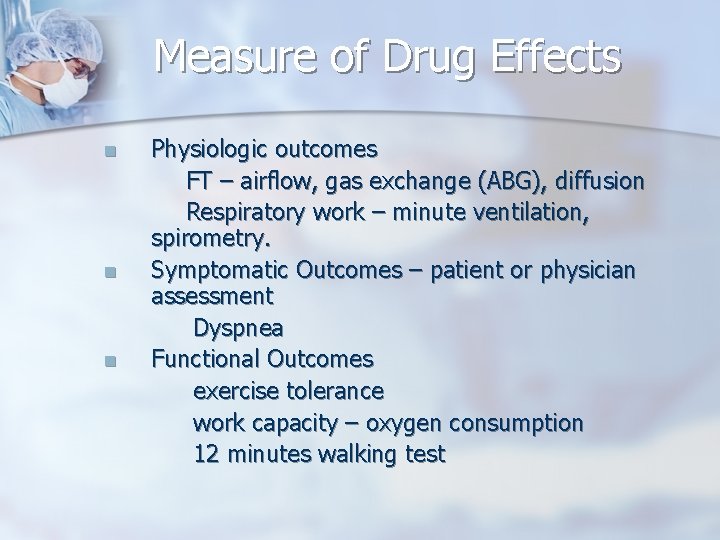
Measure of Drug Effects n n n Physiologic outcomes FT – airflow, gas exchange (ABG), diffusion Respiratory work – minute ventilation, spirometry. Symptomatic Outcomes – patient or physician assessment Dyspnea Functional Outcomes exercise tolerance work capacity – oxygen consumption 12 minutes walking test
Measure of Drug Effects Hospitalization n Other Considerations stability of disease and response to therapy. airflow changes are not always closely correlated with exercise capacity. n
Role of the Pharmacist in the management of COPD. n n n Pharmacist have a tremendous opportunity to identify patients at risk for Asthma/ COPD and to recommend for referral and assessment. Active promotion of activities aimed at smoking cessation is by far the most significant step a pharmacist can take. Patient education aimed at slowing the progress of the disease and improving compliance.
Role of the Pharmacist in the management of COPD. Too promote pharmacist/ patient interaction to empower the patient and improve patient self-management. n Assess and make recommendation for drug therapy based on most current guidelines and literature. n

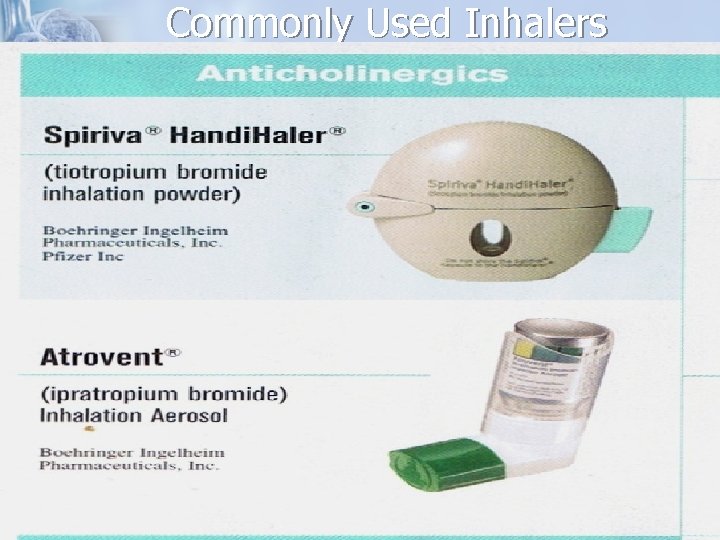
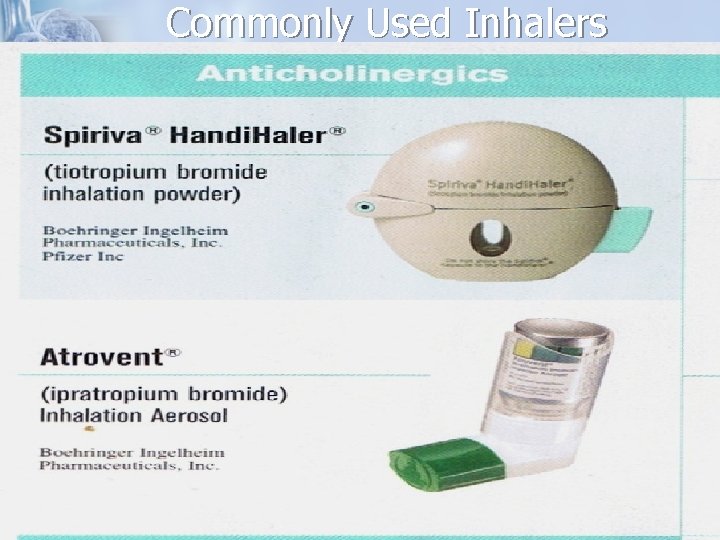
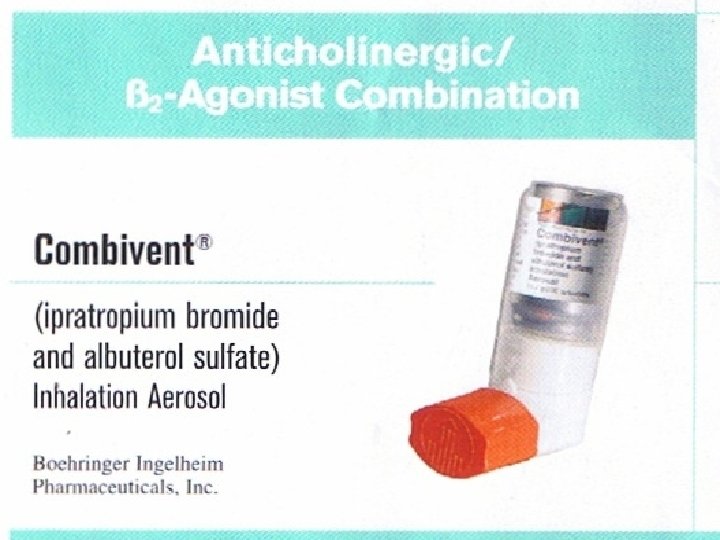
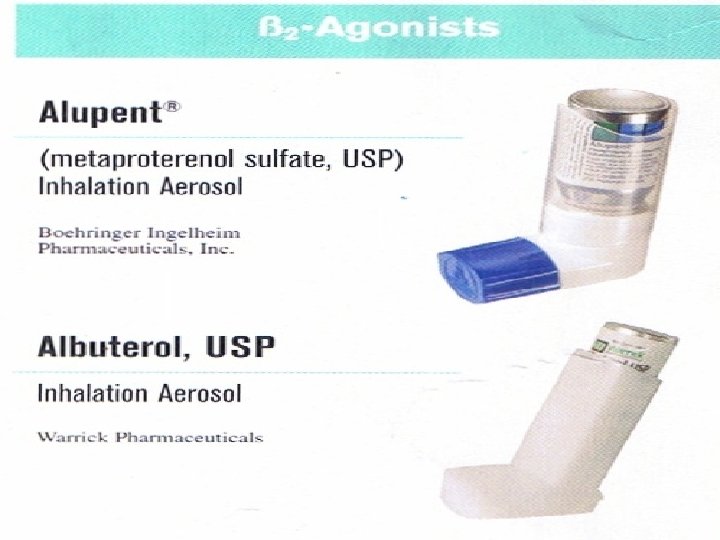
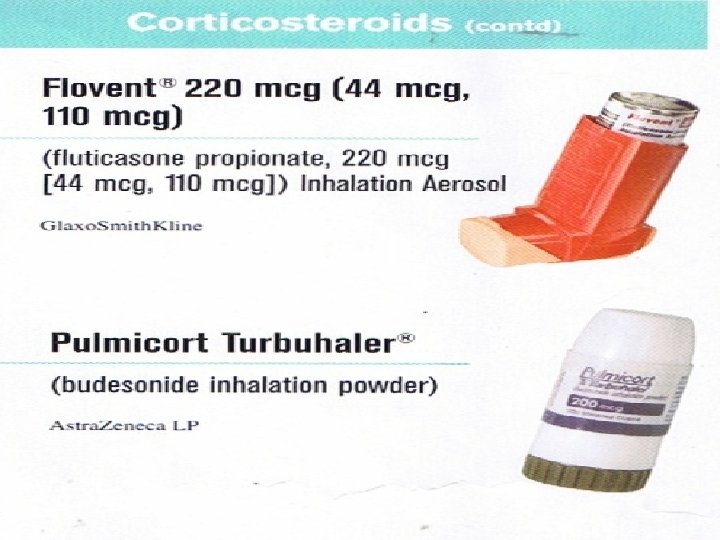
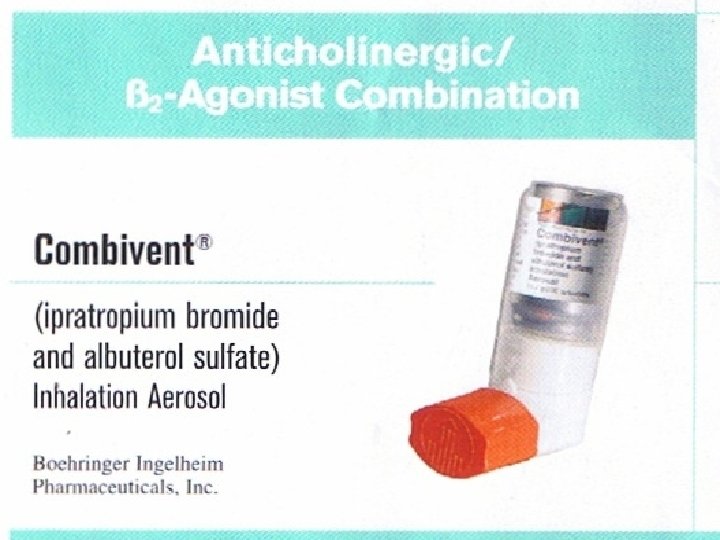
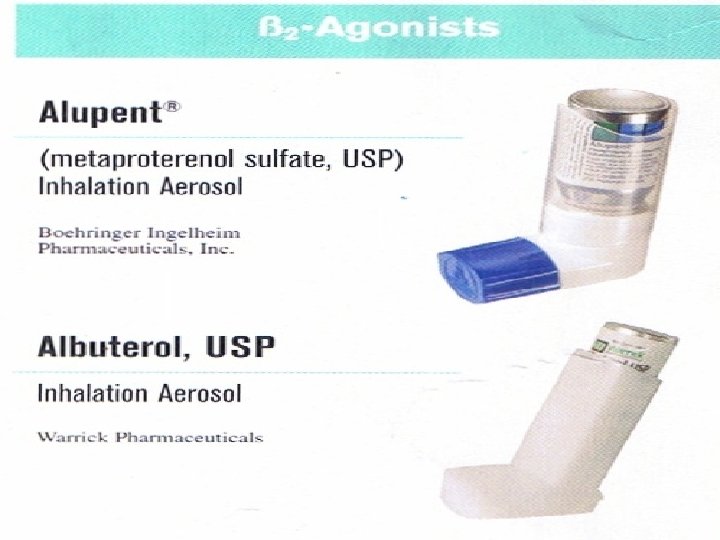
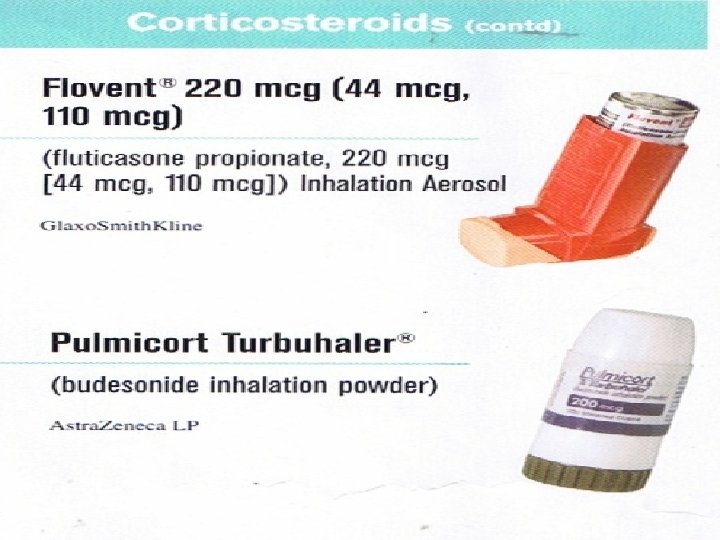
Commonly Used Inhalers





Take Home Points/ Summary. COPD is a preventable disease that can be managed to reduce exacerbations and improve QOL for patients. n It is a progressive generally irreversible inflammatory lung disease. n Smoking is the major risk factor worldwide. n
Take Home Points/ Summary. n Asthma is a common chronic disorder of the airways that is complex and characterized by variable and recurring symptoms, airflow obstruction, Bronchial hyperresponsiveness, and an underlying inflammation.
Take Home Points/ Summary. n Spirometry can demonstrate obstruction and assess reversibility in patients older than 5 years of age.
References 1. 2. 3. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. National Heart Lung and Blood Institute, National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD; 2007. NIH Publication No. 07 -4051. Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007; 176: 532 -555. Global Initiative for Asthma. Global strategy for asthma management and prevention. Bethesda, MD: Nation al Heart, Lung, and Blood Institute; 2006. NIH Publication No. 02 -3659 American Thoracic Society/European Respiratory Society statement: standards for the diagnosis and management of individuals with alpha-1 antitrypsin deficiency. Am J Respir Crit Care Med. 2003; 168: 818 -900. American Lung Association. Trends in COPD (chronic bronchitis and emphysema): morbidity and mortality American Lung Association epidemiology & statistics unit research and program services; 2007. Global Initiative for Asthma. Pocket Guide for Asthma Management and Prevention. Available at: www. ginasthma. org/download. asp? int. Id=215 Mallia P, Contoli M, Caramori G, et al. Exacerbations of asthma and chronic obstructive pulmonary disease (COPD): focus on virus induced exacerbations Chang J, Mosenifar Z. Differentiating COPD from asthma in clinical practice. J Intensive Care Med. 2007; 22: 300 -309. Smiley, T. Single-Inhaler Maintenance And Reliever Therapy for Asthma Control: A primer for Pharmacist. Pharmacy Gateway. October 2006. Available at www. pharmacygateway. ca Smiley, T. The Pharmacist’s Role in Management of COPD: A Focus on the Canadian Thoracic Society COPD Recommendations 2007 update. Pharmacy Gateway. October 2006. Available at www. pharmacygateway. ca National Heart Lung and Blood Institute. Treatment of COPD and Asthma. Update 2006. Available at www. nlhep. org Leavitt BJ, Ross CS, Spence B, et al. Long-term survival of patients with chronic obstructive pulmonary disease undergoing coronary artery bypass surgery. Circulation. 2006 Jul 4; 114(1 Suppl): I 430 -4. ACC/AHA/ESC Practice Guidelines Circulation. 2006; 114: 700 -752