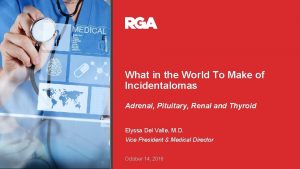
What in the World To Make of Incidentalomas
- Slides: 50
What in the World To Make of Incidentalomas Adrenal, Pituitary, Renal and Thyroid Elyssa Del Valle, M. D. Vice President & Medical Director October 14, 2016
2
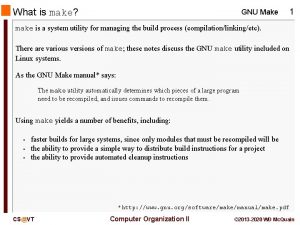
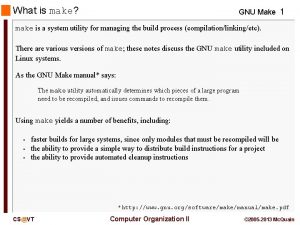
Terminology: Nodule, Lesion, Mass, Tumor § Nodule is a radiographic finding of a mass or lesion and does not in and of itself imply whether benign or malignant § Tumor is used to imply mass/lesion/nodule that has been removed or biopsied and confirmed as either benign, malignant or atypical § Point to this: If nodule has characteristics of a benign process by virtue of imaging and lab results, often it may not warrant biopsy/removal to assume a benign entity § If nodule has malignant characteristics on imaging, then it would necessitate biopsy to confirm malignant tumor via cytology evaluation 3
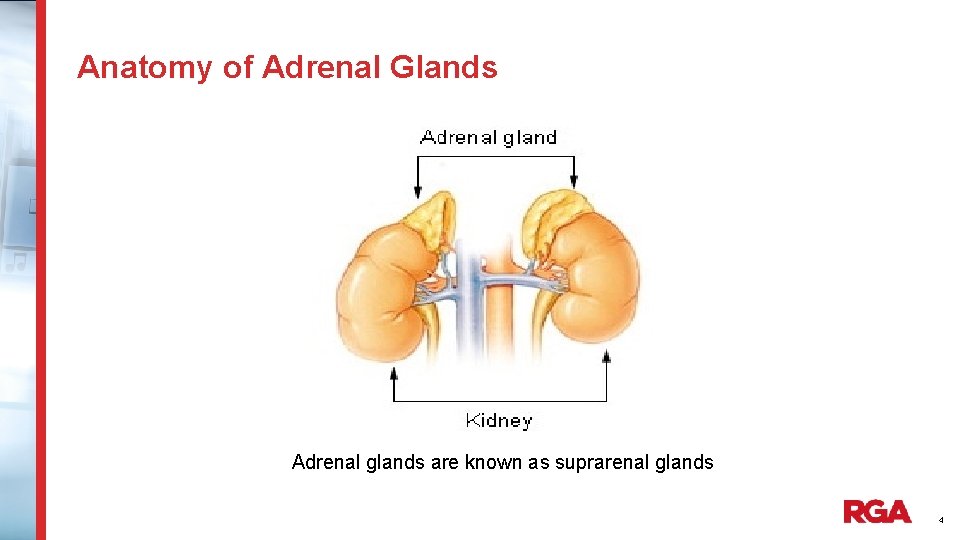
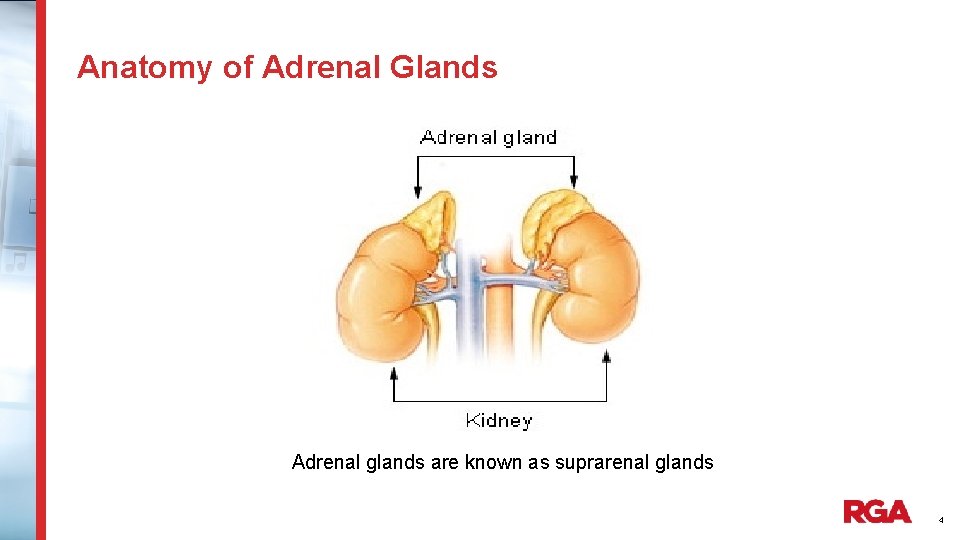
Anatomy of Adrenal Glands Adrenal glands are known as suprarenal glands 4
Adrenal Incidentaloma: Defintion § An adrenal mass, generally 1 cm or greater, that is discovered during a radiologic examination performed for indications other than an evaluation for adrenal disease § In other words, detection of an otherwise unsuspected adrenal mass on imaging 5
Prevalence of Adrenal Incidentalomas § Incidentalomas have become widespread since use of CT, MRI, resulting in the dilemma regarding their significance § Prevalence is 4. 4% on CT and MRI § Prevalence increases with increasing age § In those between 20 -29 yrs old, prevalence is 0. 2% § In those over 70 yrs of age, prevalence is 7% 6
Underwriting Risks of Adrenal Incidentalomas § Malignancy Risk Factors - Nodule > 4 cm - Multiple - Imaging characteristics - Growth on surveillance - Hormone Producing § Surgical Risks 7
What Next In Its Evaluation Must ask 3 specific questions: 1) Is the nodule/mass/lesion functioning or nonfunctioning? 2) Does it have radiographic features to suggest malignancy? 3) Does the person have a history of a previous malignancy? These questions are similarly raised for most glandular Incidentalomas 8
Why Ask These Questions Re: Adrenal Incidentaloma? § 80% are nonfunctioning adenomas § 5% have associated subclinical Cushing’s Syndrome § 5% pheochromocytoma § 1% hyperaldosteronism § < 5% are adrenocortical carcinoma § 2. 5% have metastatic disease § Remaining are benign cysts, ganglioneuromas, lipoma or myelolipomas 9
Question 1: Functioning or Nonfunctioning § Adrenal glands produce a variety of hormones § Medulla or center produce catecholamines (epinephrine) § Cortex or outer portion produce steroids( cortisol androgen) and mineralocorticoids (aldosterone) § Thus in order to answer, need to assess for overproduction of these hormones 10
Functioning or Nonfunctioning: Hormone Evaluation § Subclinical Cushing’s: autonomous cortisol secretion who have no overt symptoms/signs of hypercortisolism • overnight dexamethasone suppression test • 24 hour urine for cortisol § Silent pheochromocytoma: in hypertensive individuals • 24 hour urine for metanephrines, catecholamines § Primary Aldosteronism: in hypertensive individuals • Potassium level and ratio of morning aldosterone to plasma renin activity § Sex hormone secreting tumor and congenital adrenal hyperplasia 11
Conditions Associated with Functional Adrenal Nodules § Cortisol secreting adenoma- obesity, IFG, DM, HLD, HTN § Pheochromocytoma – HTN, CVA -* (10% are malignant) § Aldosterone secreting adenoma- *HTN, Hypokalemia § Androgen secreting adenoma – virilization (hirsutism, cliteromegaly, deepening of voice, amenorrhea) has special concern for malignancy § Appropriate next step- Surgical removal and classification of tumor as benign or malignant - removal associated with resolution of conditions 12
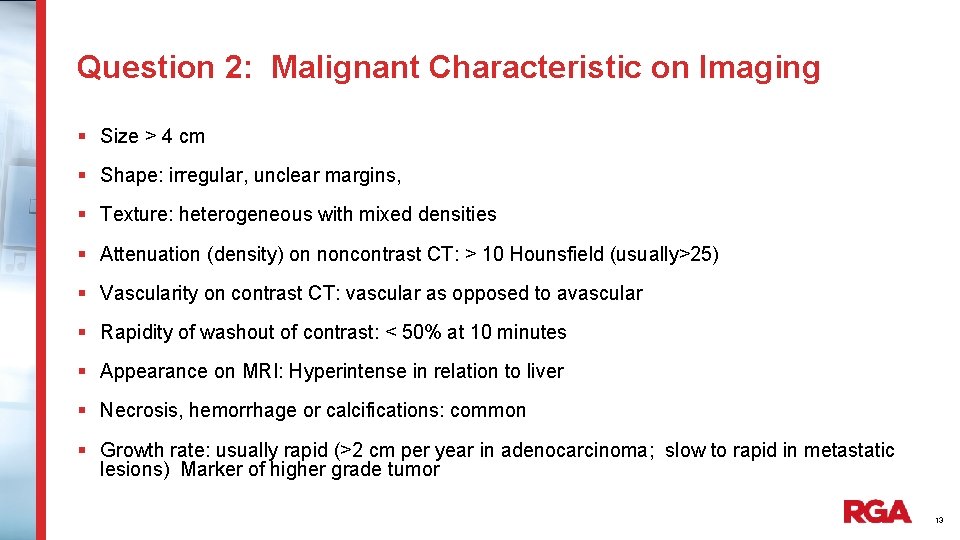
Question 2: Malignant Characteristic on Imaging § Size > 4 cm § Shape: irregular, unclear margins, § Texture: heterogeneous with mixed densities § Attenuation (density) on noncontrast CT: > 10 Hounsfield (usually>25) § Vascularity on contrast CT: vascular as opposed to avascular § Rapidity of washout of contrast: < 50% at 10 minutes § Appearance on MRI: Hyperintense in relation to liver § Necrosis, hemorrhage or calcifications: common § Growth rate: usually rapid (>2 cm per year in adenocarcinoma; slow to rapid in metastatic lesions) Marker of higher grade tumor 13
Question 3: Any History of Prior Malignancy § Metastasis is the cause in 50% who have history of malignancy § Cancers associated with metastasis to adrenals include: • • • Lung Kidney Colon Breast Esophagus Pancreas Liver Stomach Melanoma 14
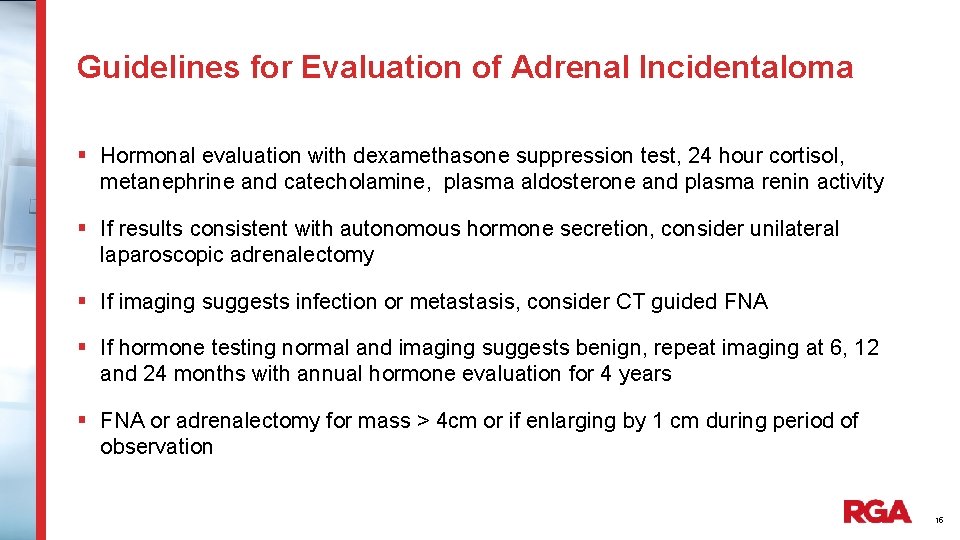
Guidelines for Evaluation of Adrenal Incidentaloma § Hormonal evaluation with dexamethasone suppression test, 24 hour cortisol, metanephrine and catecholamine, plasma aldosterone and plasma renin activity § If results consistent with autonomous hormone secretion, consider unilateral laparoscopic adrenalectomy § If imaging suggests infection or metastasis, consider CT guided FNA § If hormone testing normal and imaging suggests benign, repeat imaging at 6, 12 and 24 months with annual hormone evaluation for 4 years § FNA or adrenalectomy for mass > 4 cm or if enlarging by 1 cm during period of observation 15
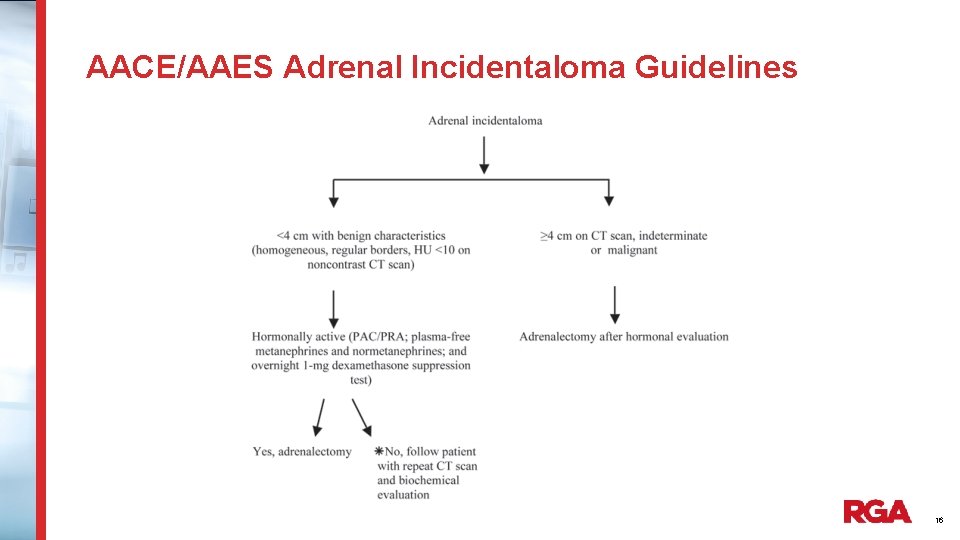
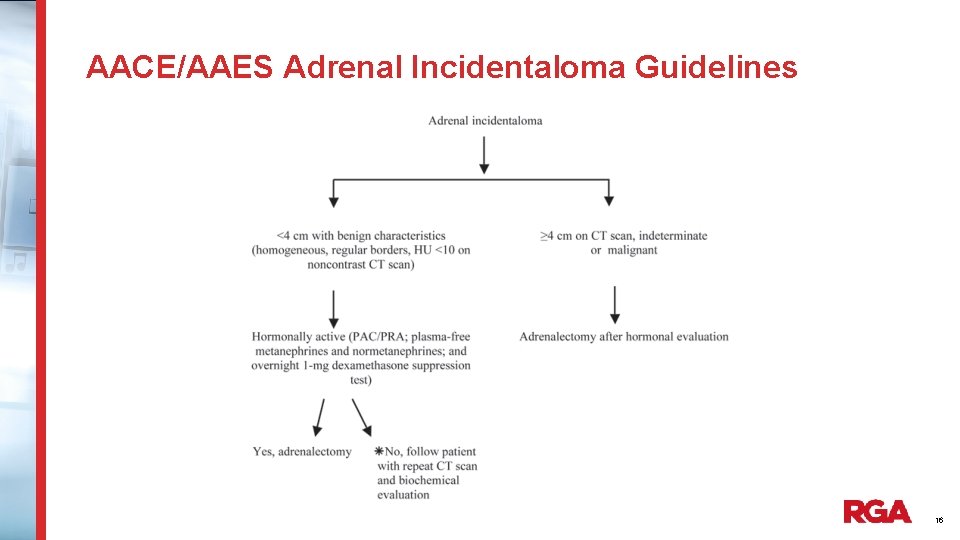
AACE/AAES Adrenal Incidentaloma Guidelines 16
Mortality and Morbidity of Adrenal Incidentaloma § Mortality related to local and metastatic spread if malignant § Mortality concerns for functional adenomas include DM, HTN, MI, CVA, Arrhythmia, CHF and Surgical Complications § Morbidity concerns for functional adenomas include DM, HTN, Post MI, CVA, Obesity, Osteoporosis, Arrhythmia, Virilization 17
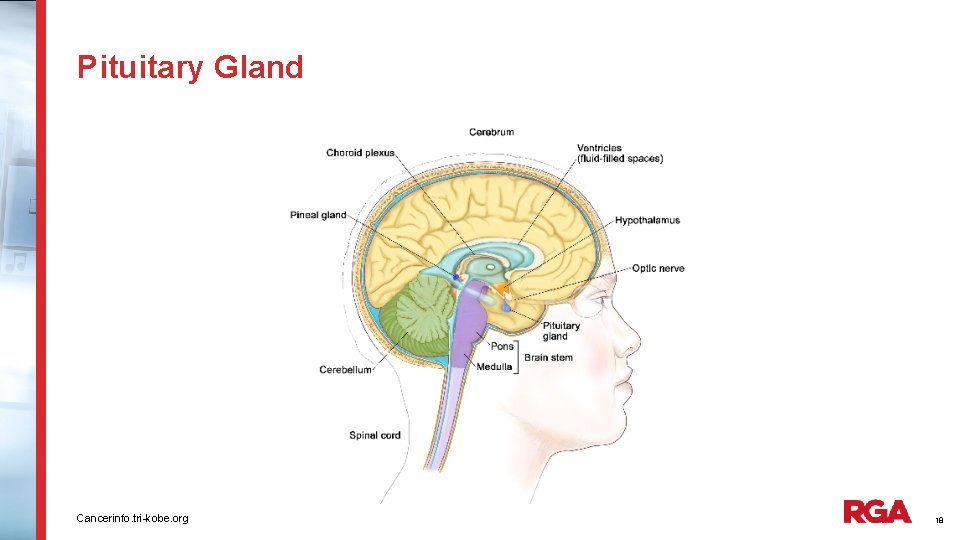
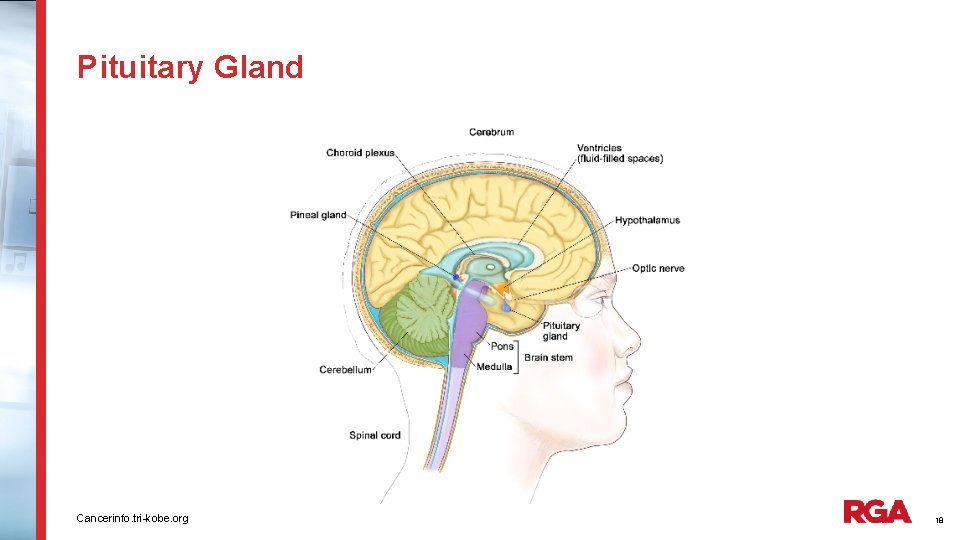
Pituitary Gland Cancerinfo. tri-kobe. org 18
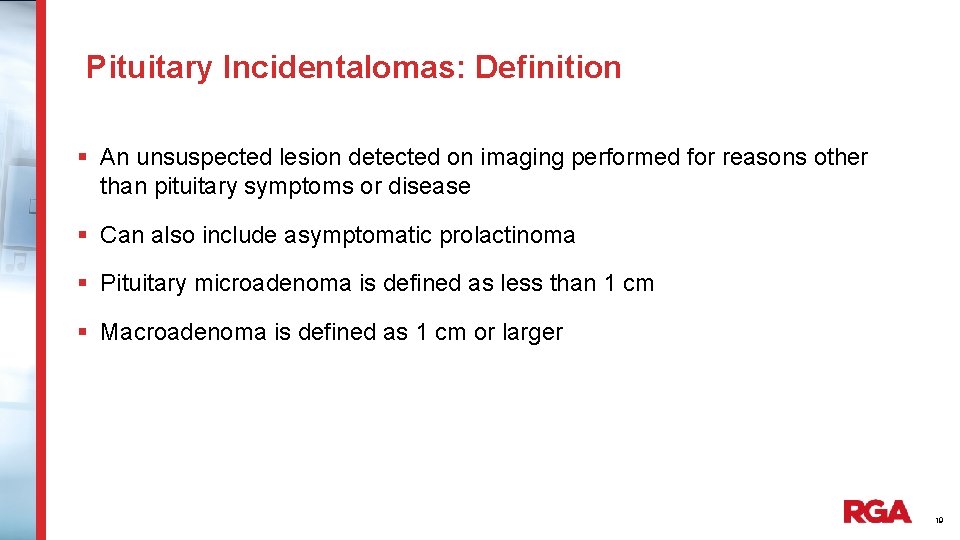
Pituitary Incidentalomas: Definition § An unsuspected lesion detected on imaging performed for reasons other than pituitary symptoms or disease § Can also include asymptomatic prolactinoma § Pituitary microadenoma is defined as less than 1 cm § Macroadenoma is defined as 1 cm or larger 19
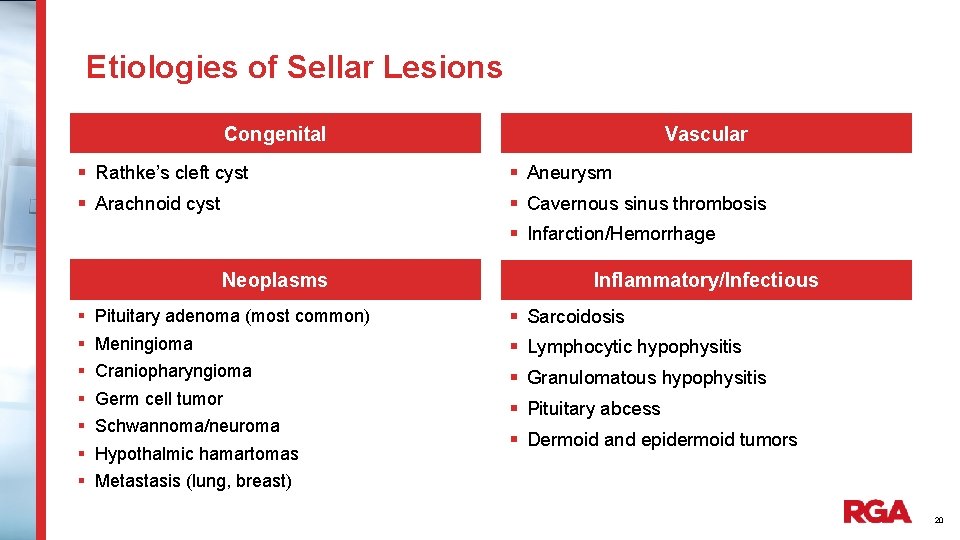
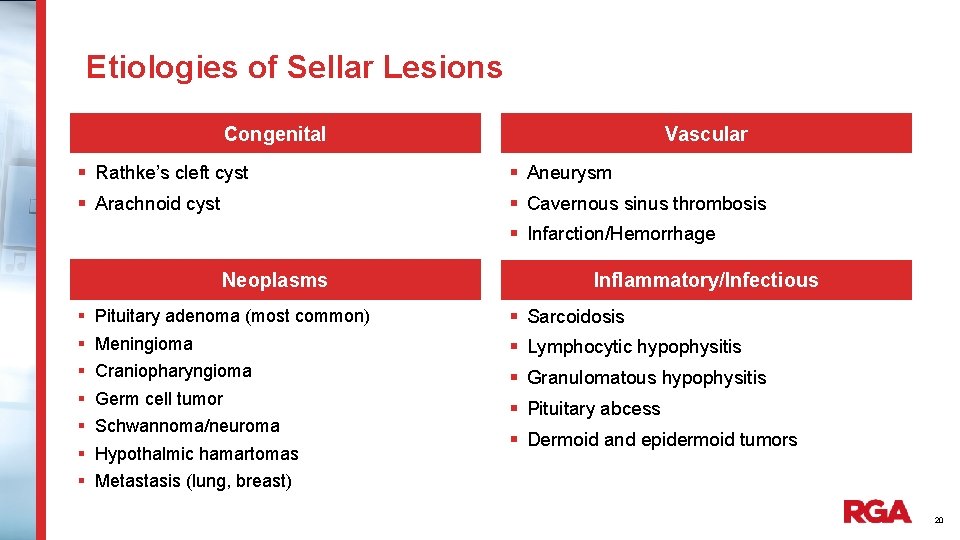
Etiologies of Sellar Lesions Congenital Vascular § Rathke’s cleft cyst § Aneurysm § Arachnoid cyst § Cavernous sinus thrombosis § Infarction/Hemorrhage Neoplasms § § § § Inflammatory/Infectious Pituitary adenoma (most common) § Sarcoidosis Meningioma § Lymphocytic hypophysitis Craniopharyngioma § Granulomatous hypophysitis Germ cell tumor Schwannoma/neuroma Hypothalmic hamartomas § Pituitary abcess § Dermoid and epidermoid tumors Metastasis (lung, breast) 20
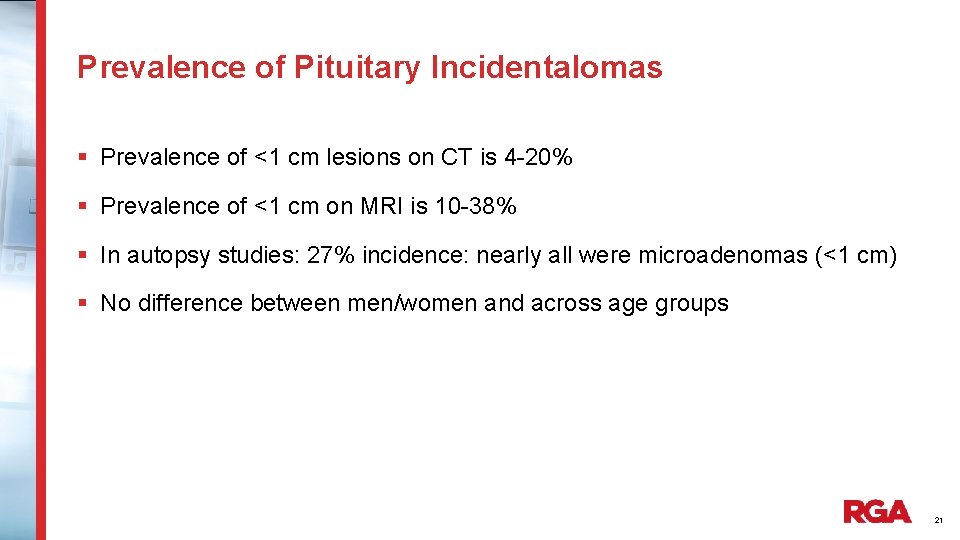
Prevalence of Pituitary Incidentalomas § Prevalence of <1 cm lesions on CT is 4 -20% § Prevalence of <1 cm on MRI is 10 -38% § In autopsy studies: 27% incidence: nearly all were microadenomas (<1 cm) § No difference between men/women and across age groups 21
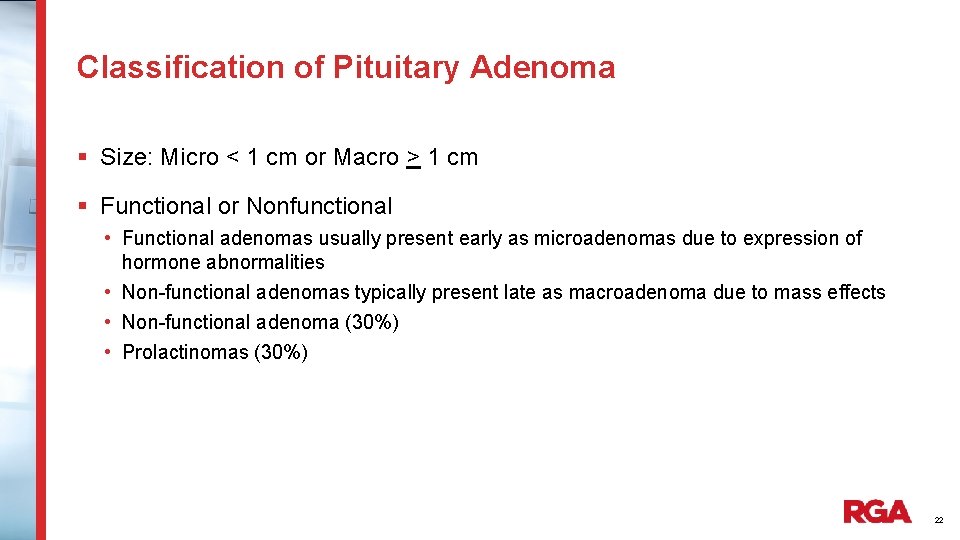
Classification of Pituitary Adenoma § Size: Micro < 1 cm or Macro > 1 cm § Functional or Nonfunctional • Functional adenomas usually present early as microadenomas due to expression of hormone abnormalities • Non-functional adenomas typically present late as macroadenoma due to mass effects • Non-functional adenoma (30%) • Prolactinomas (30%) 22
Clinical Course in Prospective Studies § Non-functioning sellar masses > 1 cm were 4 x likely to experience growth during follow up than those < 1 cm (incidence 12. 5 versus 3. 3 per 100 person-years, respectively) § This illustrates why there is less concern for non-functioning pituitary incidentalomas less than 0. 5 cm § This also illustrates why we may decline those that are > 1 cm if not surgically resected unless they prove stable in size for many years 23
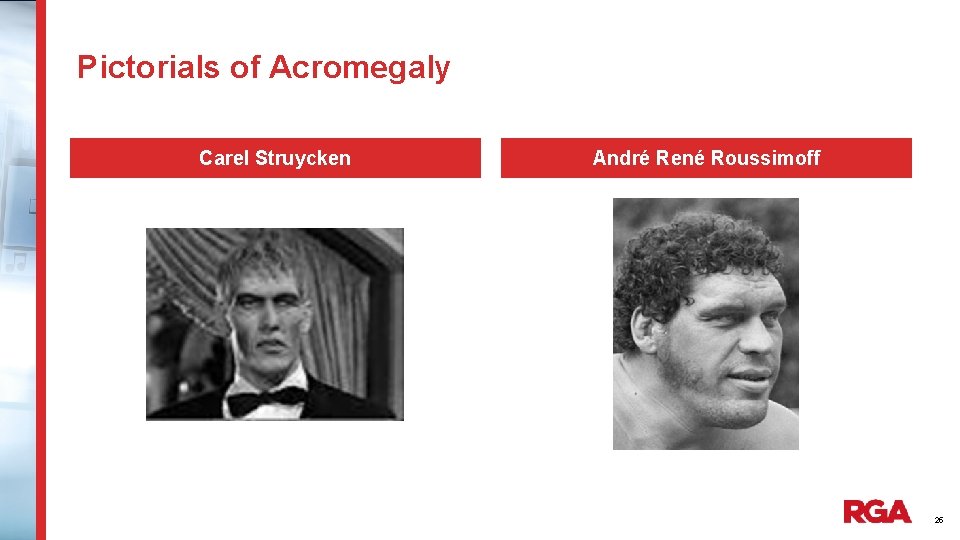
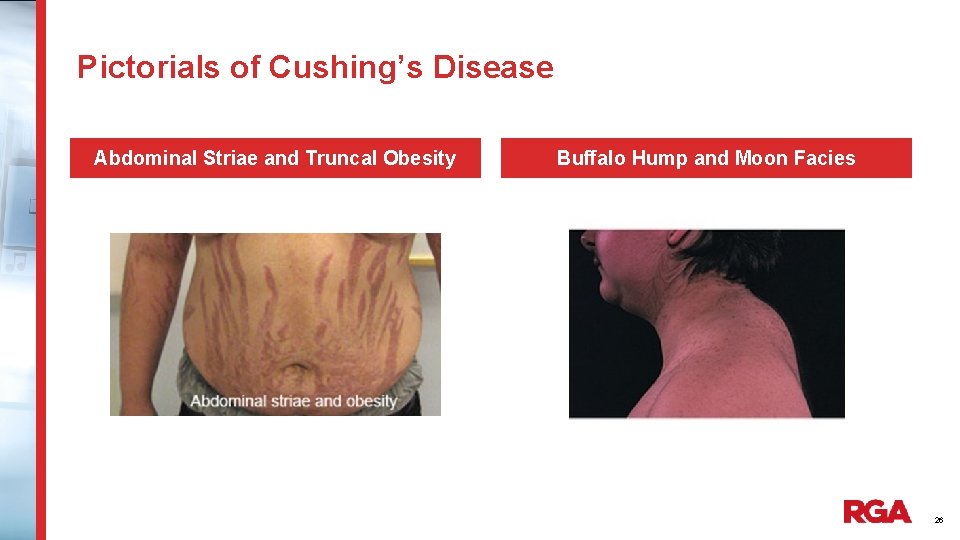
Symptoms Associated with Pituitary Adenomas § Mass effect: If large, can invade and compress structures outside sella and cause HA, double vision/diminished visual field and acuity and hydrocephalus § Hormonal effect: If large, can compress pituitary gland causing loss of one or more hormones ranging from LH/FSH deficiency, growth hormone deficiency, secondary hypothyroidism, adrenal insufficiency or even panhypopituitarism § Hormonally active adenomas can secrete one or more hormones resulting in hyperthyroidism, Cushing’s disease (cortisol excess), or acromegaly (growth hormone excess) or prolactinemia § If above symptoms not present when pituitary mass found, this would be deemed an incidentaloma 24
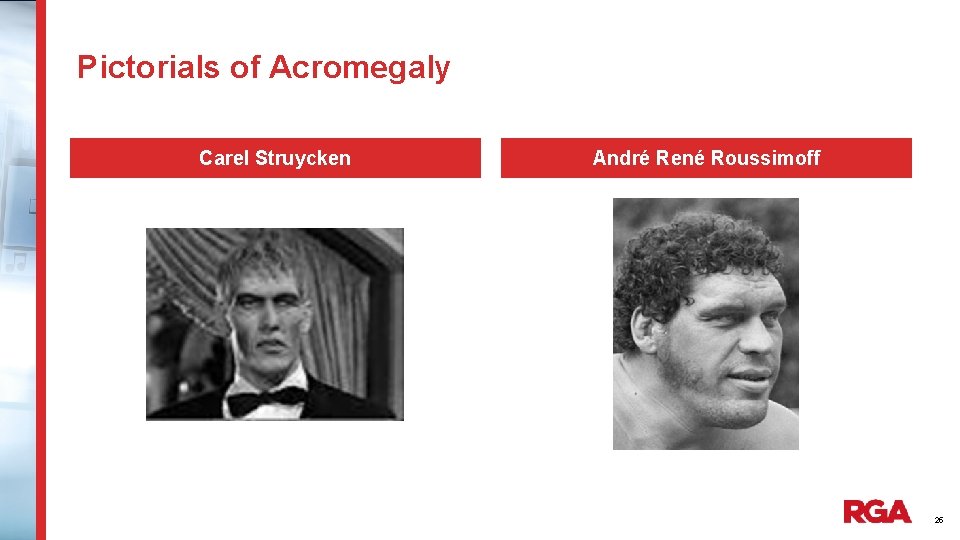
Pictorials of Acromegaly Carel Struycken André René Roussimoff 25
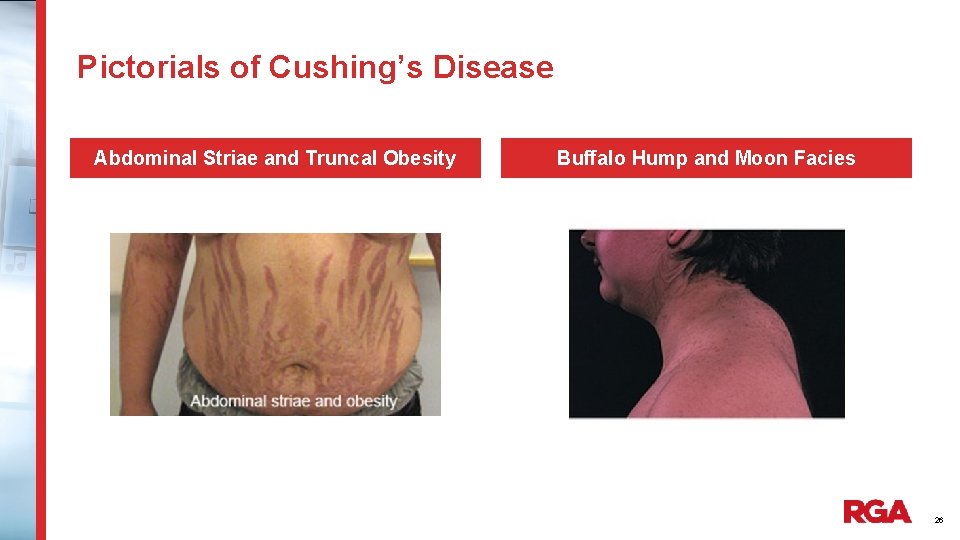
Pictorials of Cushing’s Disease Abdominal Striae and Truncal Obesity Buffalo Hump and Moon Facies 26
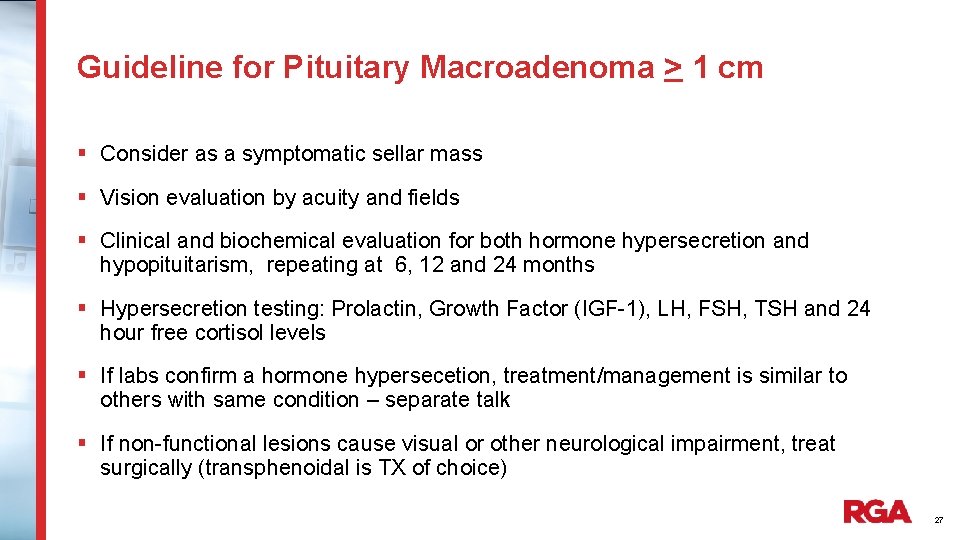
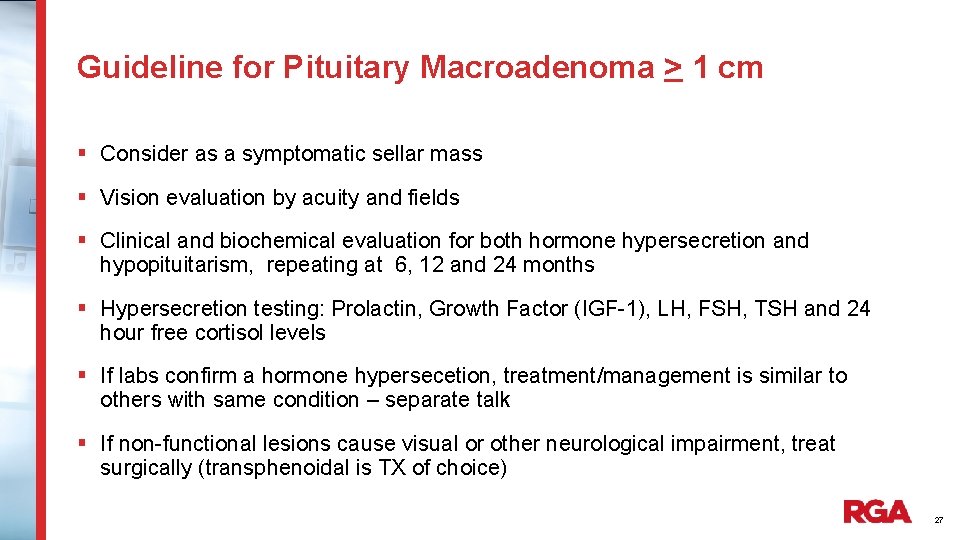
Guideline for Pituitary Macroadenoma > 1 cm § Consider as a symptomatic sellar mass § Vision evaluation by acuity and fields § Clinical and biochemical evaluation for both hormone hypersecretion and hypopituitarism, repeating at 6, 12 and 24 months § Hypersecretion testing: Prolactin, Growth Factor (IGF-1), LH, FSH, TSH and 24 hour free cortisol levels § If labs confirm a hormone hypersecetion, treatment/management is similar to others with same condition – separate talk § If non-functional lesions cause visual or other neurological impairment, treat surgically (transphenoidal is TX of choice) 27
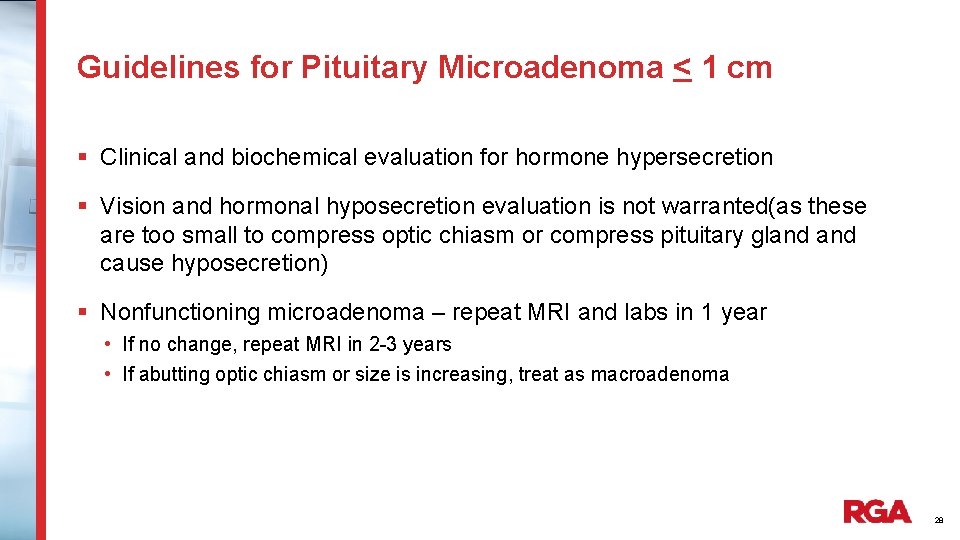
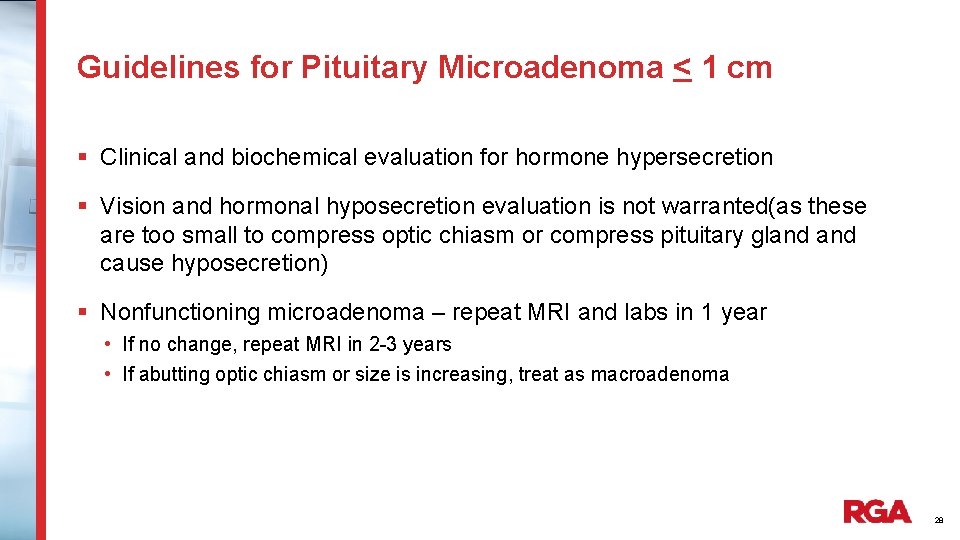
Guidelines for Pituitary Microadenoma < 1 cm § Clinical and biochemical evaluation for hormone hypersecretion § Vision and hormonal hyposecretion evaluation is not warranted(as these are too small to compress optic chiasm or compress pituitary gland cause hyposecretion) § Nonfunctioning microadenoma – repeat MRI and labs in 1 year • If no change, repeat MRI in 2 -3 years • If abutting optic chiasm or size is increasing, treat as macroadenoma 28
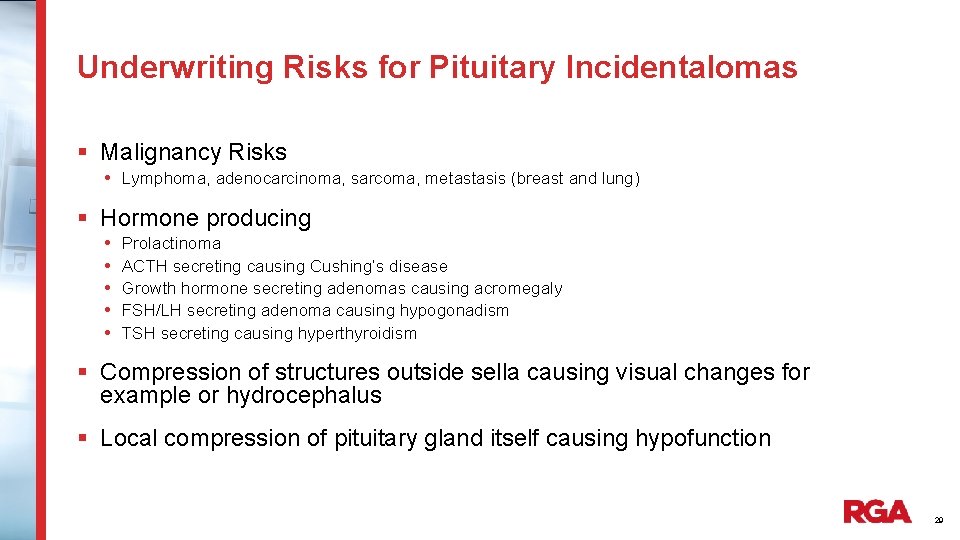
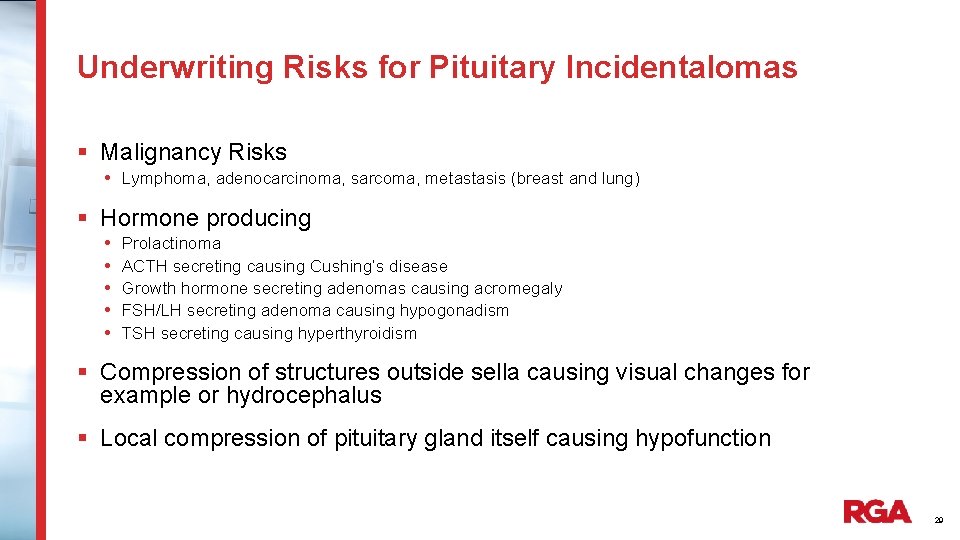
Underwriting Risks for Pituitary Incidentalomas § Malignancy Risks • Lymphoma, adenocarcinoma, sarcoma, metastasis (breast and lung) § Hormone producing • • • Prolactinoma ACTH secreting causing Cushing’s disease Growth hormone secreting adenomas causing acromegaly FSH/LH secreting adenoma causing hypogonadism TSH secreting causing hyperthyroidism § Compression of structures outside sella causing visual changes for example or hydrocephalus § Local compression of pituitary gland itself causing hypofunction 29
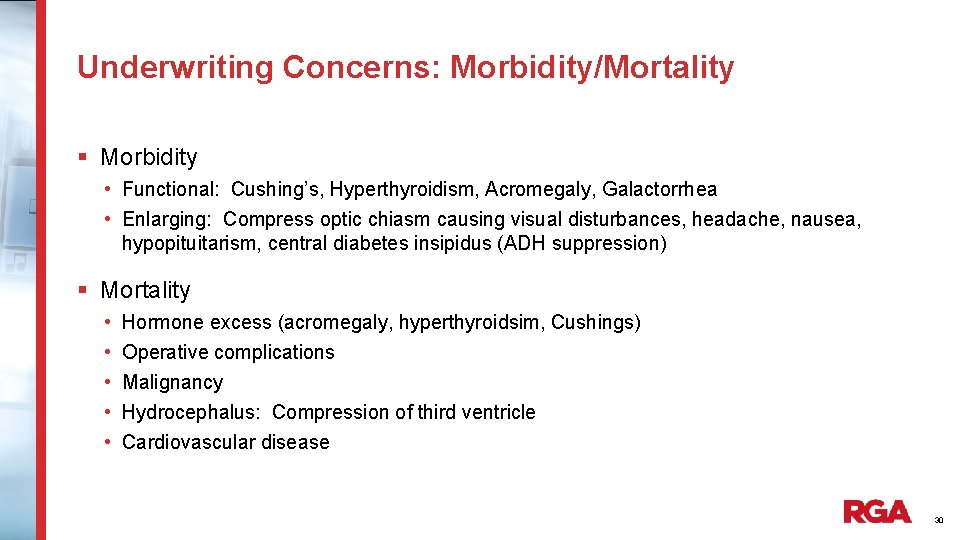
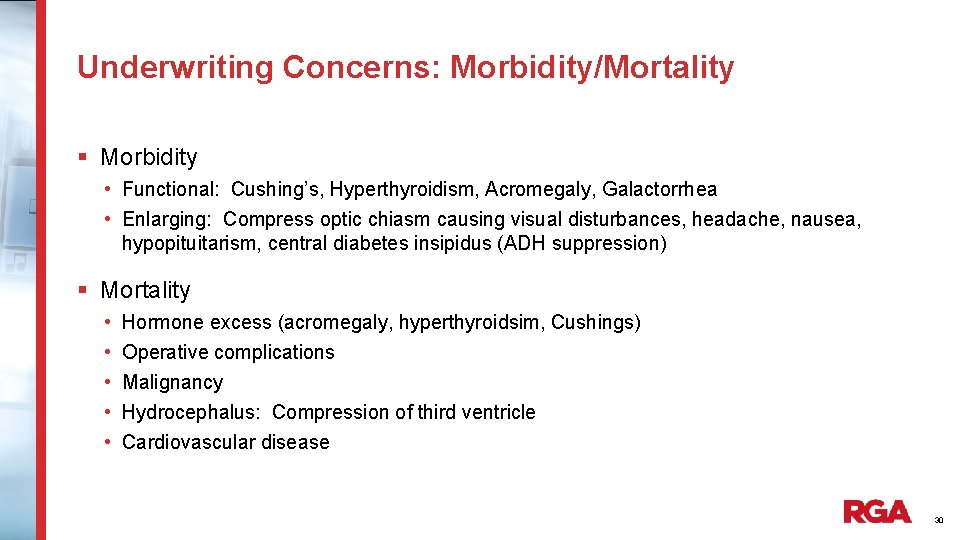
Underwriting Concerns: Morbidity/Mortality § Morbidity • Functional: Cushing’s, Hyperthyroidism, Acromegaly, Galactorrhea • Enlarging: Compress optic chiasm causing visual disturbances, headache, nausea, hypopituitarism, central diabetes insipidus (ADH suppression) § Mortality • • • Hormone excess (acromegaly, hyperthyroidsim, Cushings) Operative complications Malignancy Hydrocephalus: Compression of third ventricle Cardiovascular disease 30
Renal Incidentalomas 31
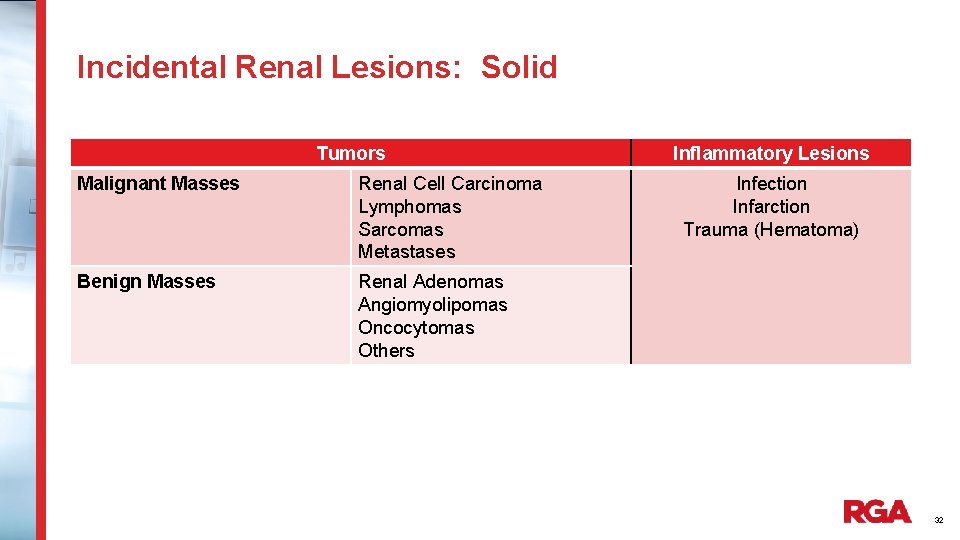
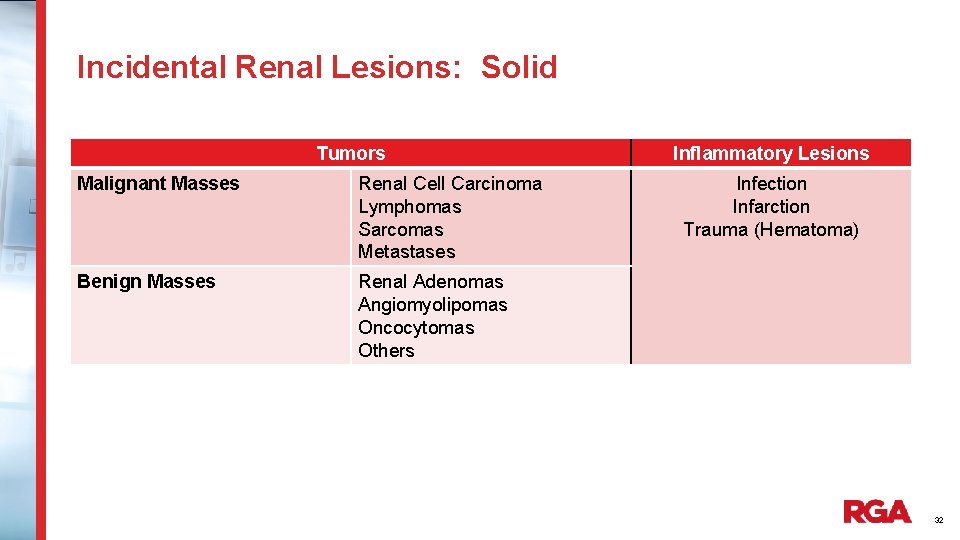
Incidental Renal Lesions: Solid Tumors Malignant Masses Renal Cell Carcinoma Lymphomas Sarcomas Metastases Benign Masses Renal Adenomas Angiomyolipomas Oncocytomas Others Inflammatory Lesions Infection Infarction Trauma (Hematoma) 32
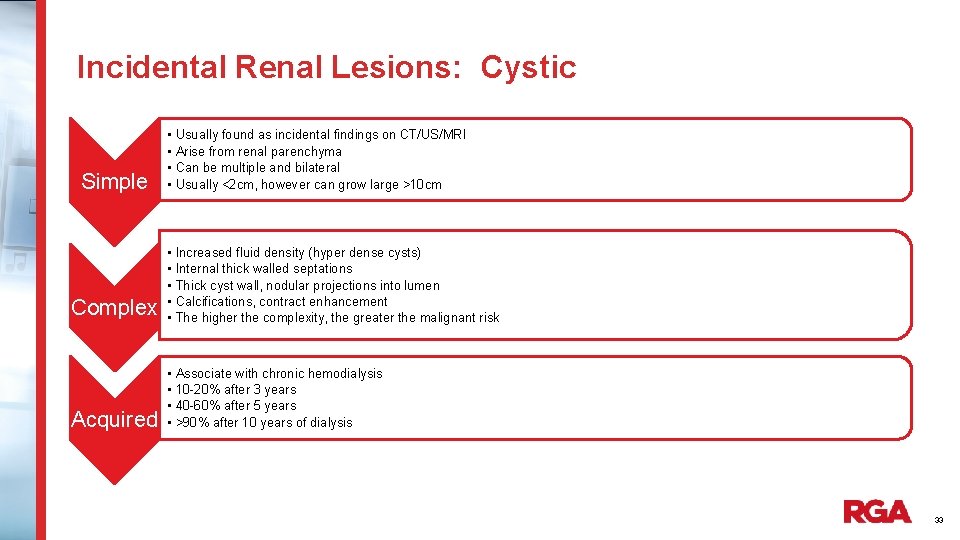
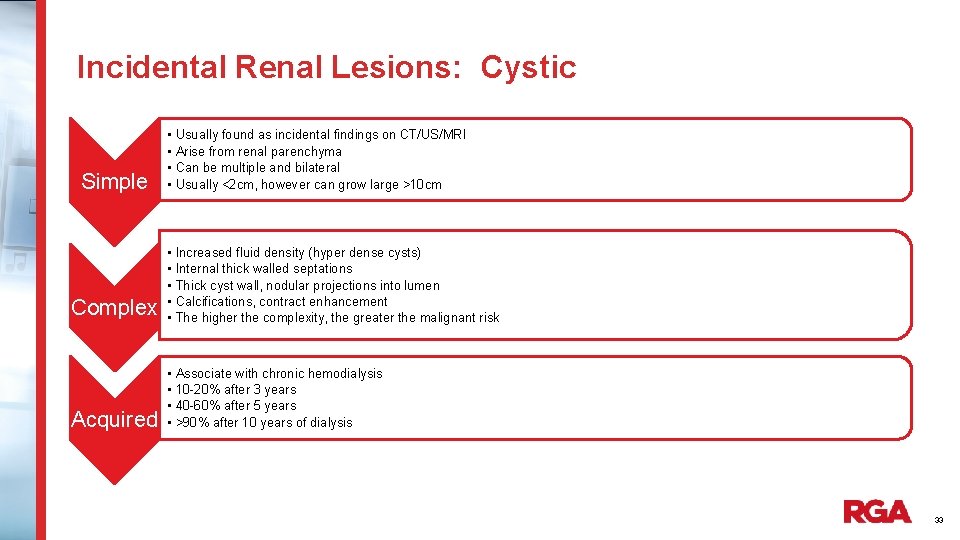
Incidental Renal Lesions: Cystic Simple • • Usually found as incidental findings on CT/US/MRI Arise from renal parenchyma Can be multiple and bilateral Usually <2 cm, however can grow large >10 cm Complex • • • Increased fluid density (hyper dense cysts) Internal thick walled septations Thick cyst wall, nodular projections into lumen Calcifications, contract enhancement The higher the complexity, the greater the malignant risk Acquired • • Associate with chronic hemodialysis 10 -20% after 3 years 40 -60% after 5 years >90% after 10 years of dialysis 33
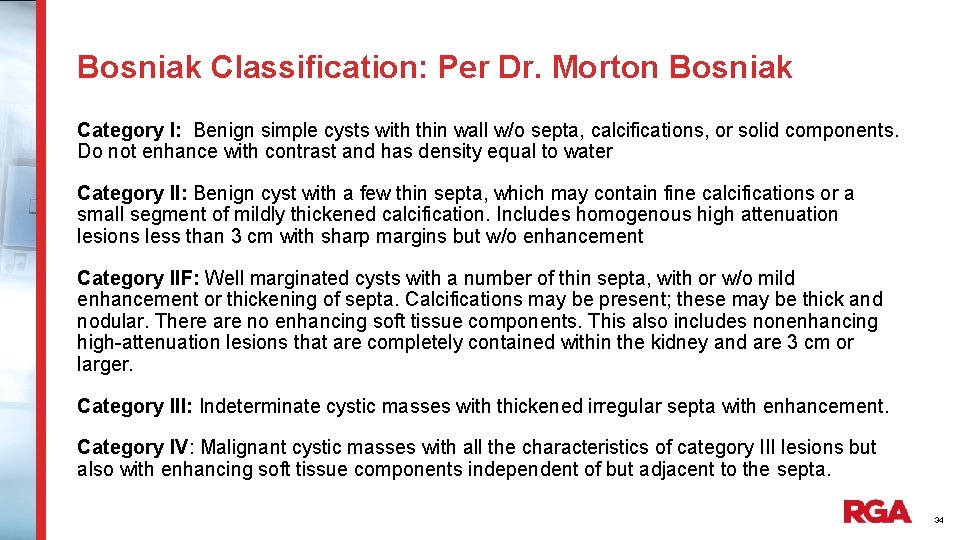
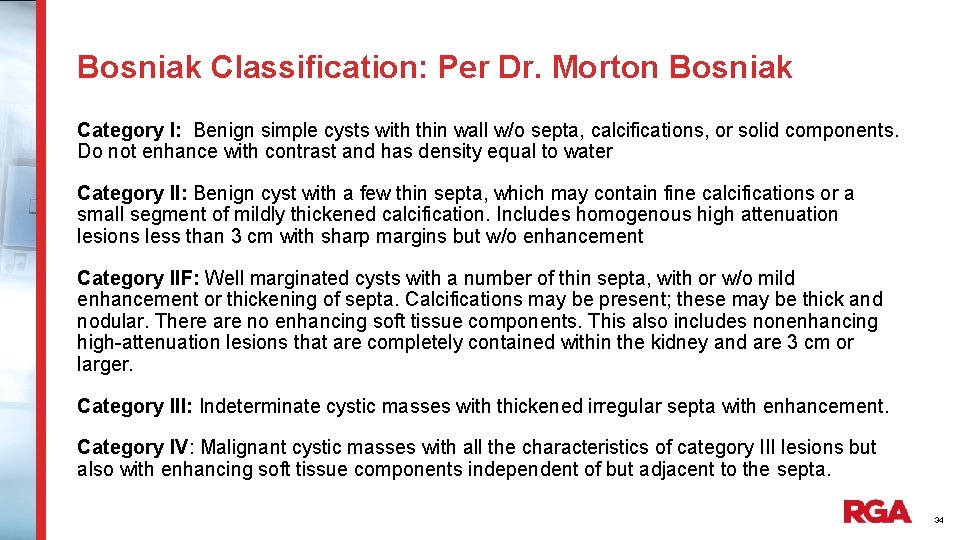
Bosniak Classification: Per Dr. Morton Bosniak Category I: Benign simple cysts with thin wall w/o septa, calcifications, or solid components. Do not enhance with contrast and has density equal to water Category II: Benign cyst with a few thin septa, which may contain fine calcifications or a small segment of mildly thickened calcification. Includes homogenous high attenuation lesions less than 3 cm with sharp margins but w/o enhancement Category IIF: Well marginated cysts with a number of thin septa, with or w/o mild enhancement or thickening of septa. Calcifications may be present; these may be thick and nodular. There are no enhancing soft tissue components. This also includes nonenhancing high-attenuation lesions that are completely contained within the kidney and are 3 cm or larger. Category III: Indeterminate cystic masses with thickened irregular septa with enhancement. Category IV: Malignant cystic masses with all the characteristics of category III lesions but also with enhancing soft tissue components independent of but adjacent to the septa. 34
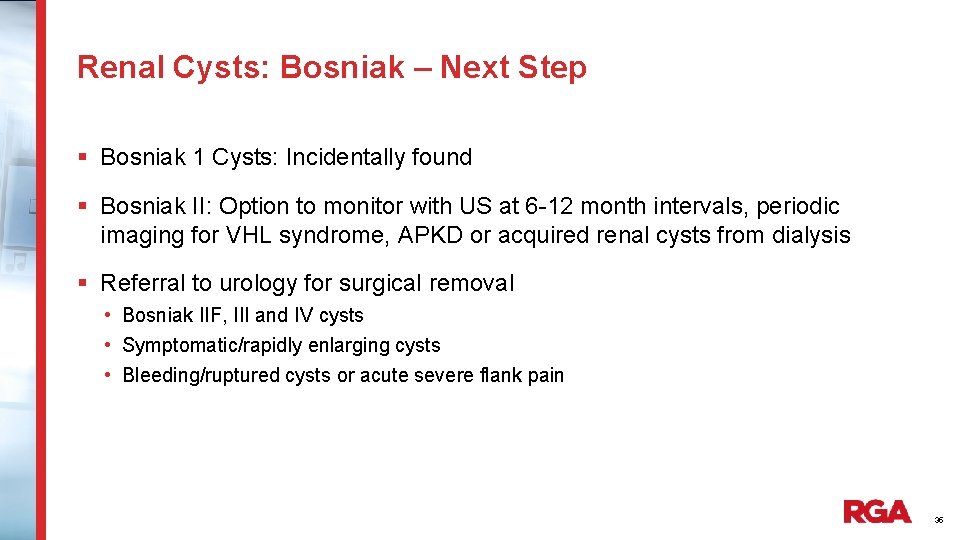
Renal Cysts: Bosniak – Next Step § Bosniak 1 Cysts: Incidentally found § Bosniak II: Option to monitor with US at 6 -12 month intervals, periodic imaging for VHL syndrome, APKD or acquired renal cysts from dialysis § Referral to urology for surgical removal • Bosniak IIF, III and IV cysts • Symptomatic/rapidly enlarging cysts • Bleeding/ruptured cysts or acute severe flank pain 35
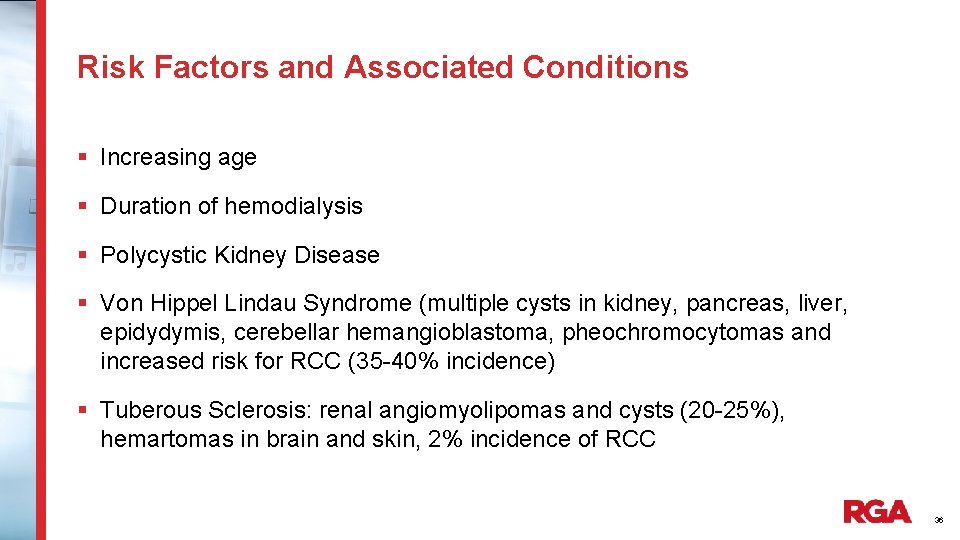
Risk Factors and Associated Conditions § Increasing age § Duration of hemodialysis § Polycystic Kidney Disease § Von Hippel Lindau Syndrome (multiple cysts in kidney, pancreas, liver, epidydymis, cerebellar hemangioblastoma, pheochromocytomas and increased risk for RCC (35 -40% incidence) § Tuberous Sclerosis: renal angiomyolipomas and cysts (20 -25%), hemartomas in brain and skin, 2% incidence of RCC 36
Natural Course and Epidemiology of Renal Cysts § Incidence increases with age: 0. 2% age 0 -18 20% age 20 -40 33% age 41 -60 § Most cysts grow slowly 3. 9 mm per year for age < 50 1. 8 mm per year for age > 50 Some involute and disappear over time 37
Underwriting Concerns for Risk of Malignancy Smoking Age > 60 History or suspected history of malignancy elsewhere Family history of hereditary syndromes such as Tuberous sclerosis or VHL Nodule size > 4 cm Nodule growth on serial imaging Multiple if not disease related CT imaging: solid, complex Bosniak 2 F, 3, 4, capsular invasion and/or enlarged lymph nodes Angiomyolipoma: Bilateral (80 -90% tuberous sclerosis) > 4 cm surgery 38
Underwriting Risks for Renal Incidentalomas § Incidence of Renal Cancer § 3% of renal incidentalomas grow and metastasize w/in 3 yrs of surveillance § Renal cell carcinoma with metastasis is incurable 39
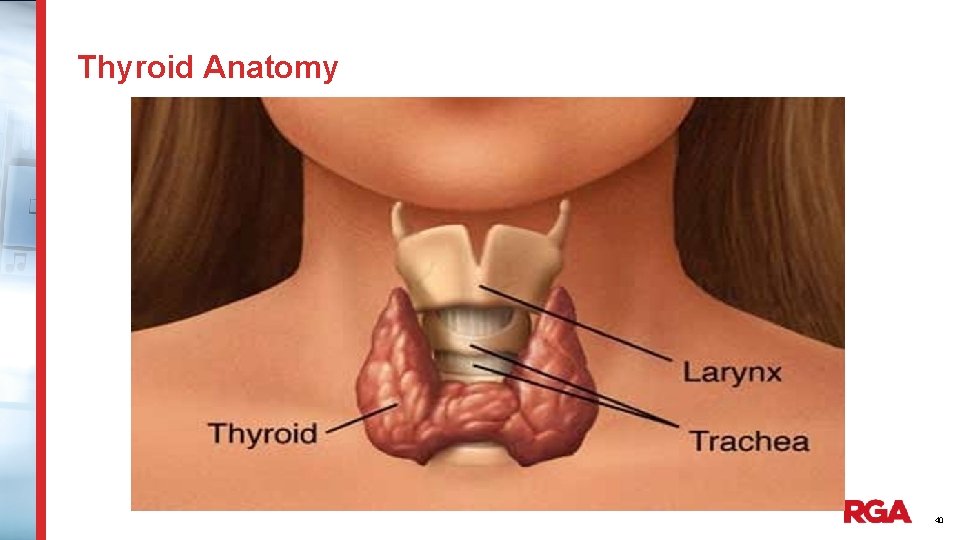
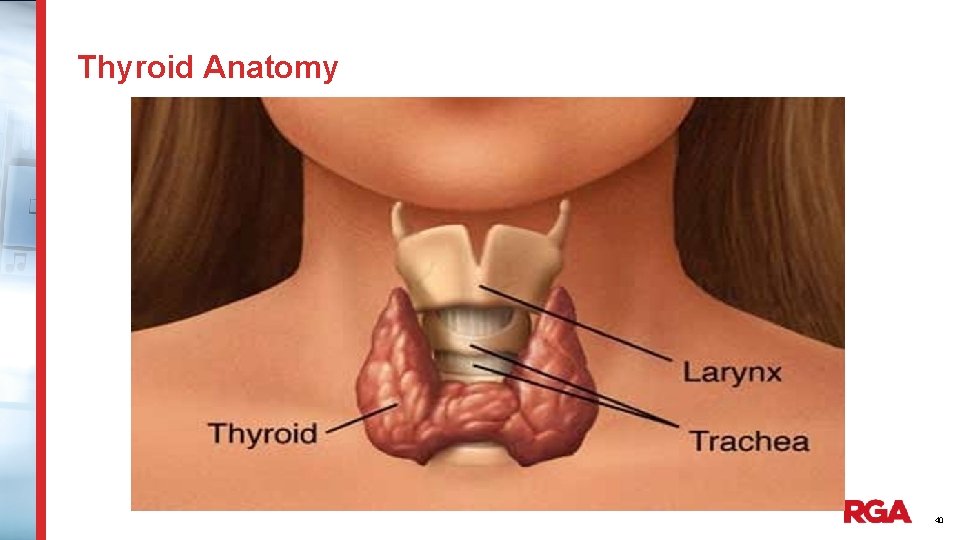
Thyroid Anatomy 40
Thyroid Incidentaloma Prevalence § Seen in 50% of autopsies § Screening thyroid ultrasounds will find thyroid nodules in 50% of those screened § Carotid ultrasounds will typically detect thyroid incidentalomas in 13% 41
Underwriting Risk of Malignancy within Thyroid Nodules § Strong family history of thyroid cancer § Personal or family history of MEN (Multiple Endocrine Neoplasm) or history of parathyroid tumor or pheochromocytoma § History of radiation treatment to neck area § Thyroid nodule described as hard, fixed, firm or causing tracheal deviation § Thyroid ultrasound shows irregular or micro lobulated border, taller than wide, marked hypoechoicity, spiculated, increased vascularity, indistinct borders, extension beyond the capsule or into the chest § Abnormal neck lymph nodes § Thyroid nodule greater > 2 cm 42
Underwriting Risk of Malignancy within Thyroid Nodule § Growth on surveillance imaging § Positive on PET scan § Cold on Thyroid scan § Hot nodules on thyroid scans are almost always benign and would rate as hyperthyroidism 43
Case 1 § Marianne is a 45 year old accountant applying for $1 million term life insurance and $3000/month disability policy with a 90 day EP to age 70 § On 5/10, she presented to Emergency room for right flank pain and found to have right kidney stone, which she eventually passed. The CT also revealed an incidental left 1. 5 cm adrenal nodule characterized as an adrenal adenoma. § On f/u, her PCP noted no personal or family history for malignancies. She had DM II controlled on 1000 mg of Metformin and well controlled HTN on HCTZ. 24 hour urine for cortisol was elevated. Dexamethasone suppression test was abnormal. Urine for metanephrines were normal as was aldosterone and renin activity. She underwent left adrenalectomy for functioning adrenal adenoma. Since surgery, DM is controlled with diet alone. What is the Risk Assessment? 44
Case 1 (Continued) § Adrenal Nodule: Biochemical (hormonal) testing abnormal § Favorable factors: • Benign adrenal unilateral disease • Treated with surgery with no complications • Improved glycemic control off medication § Unfavorable factors: none § Risk Assessment Life – Rate for DM only Disability-Rate as would for DM 45
Case 2 § Stuart a 28 year old pharmacist with chronic migraines was previously evaluated with brain MRI during his senior year in college when age 22. Brain MRI had revealed a 0. 7 cm pituitary mass. His neurologist did not opine headaches were related to this incidentaloma as visual field testing was normal as was hormone levels including TSH, prolactin, GH, ACTH, LH and FSH. § He was recently seen by his neurologist for follow up of migraines. Repeat MRI showed stable pituitary lesion when compared to previous study. No further follow up was recommended regarding the pituitary lesion. What is the Risk Assessment? 46
Case 2 (Continued) § Non functioning pituitary microadenoma § Favorable factors: • Microadenoma less than 1 cm • Nonfunctional • Stable repeat imaging 5 years later § Unfavorable factors: NONE § Risk Assessment Life – STD/Preferred as qualifies Disability - Rider 47
Case 3 § Sarah is a 55 year old engineer who is applying for a $2 million whole life policy as well as $5000/month disability policy/90 EP to age 65 § In January 2014, her PCP noted an asymptomatic right sided bruit and neck exam was otherwise normal as was remainder of complete physical exam. Carotid ultrasound was ordered revealing non hemodynamically significant plaque, however there was a 1. 5 cm right thyroid nodule described as isoechoic without irregular borders or increase in vascularity. Repeat thyroid ultrasound in January 2015 revealed no changes. § Sarah has no personal history of radiation or cancer and has no family history of cancer of any types. What is the Risk Assessment? 48
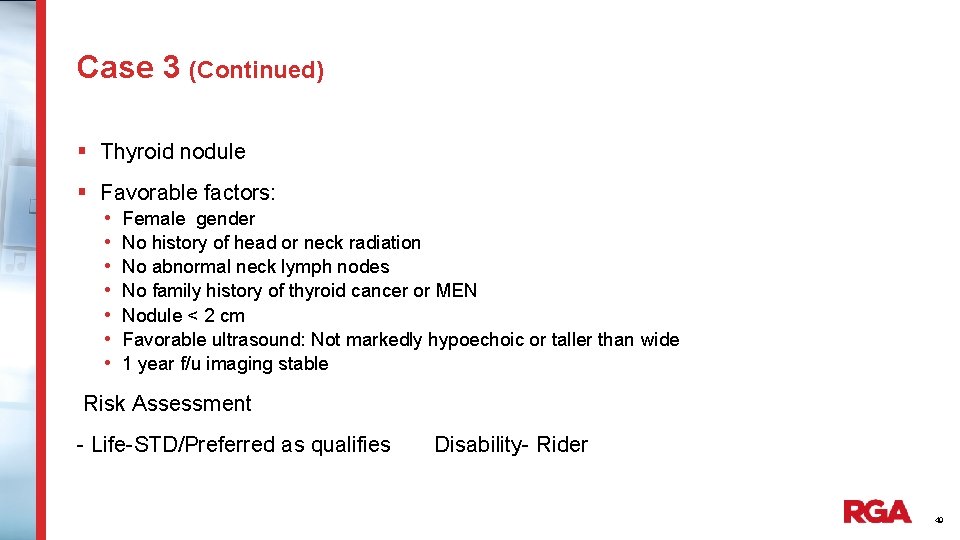
Case 3 (Continued) § Thyroid nodule § Favorable factors: • Female gender • No history of head or neck radiation • No abnormal neck lymph nodes • No family history of thyroid cancer or MEN • Nodule < 2 cm • Favorable ultrasound: Not markedly hypoechoic or taller than wide • 1 year f/u imaging stable Risk Assessment - Life-STD/Preferred as qualifies Disability- Rider 49
© 2016 RGA. All rights reserved. No part of this publication may be reproduced in any form without the prior permission of RGA. The information in this publication is for the exclusive, internal use of the recipient and may not be relied upon by any other party other than the recipient and its affiliates, or published, quoted or disseminated to any party other than the recipient without the prior written consent of RGA.
 Make the lie big keep it simple
Make the lie big keep it simple Go make a difference
Go make a difference Make the lie big make it simple
Make the lie big make it simple Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Thang điểm glasgow
Thang điểm glasgow Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công của trọng lực
Công của trọng lực Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thứ tự các dấu thăng giáng ở hóa biểu
Thứ tự các dấu thăng giáng ở hóa biểu Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là So nguyen to
So nguyen to Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Computers make the world smaller and smarter answers
Computers make the world smaller and smarter answers Money make the world go round meaning
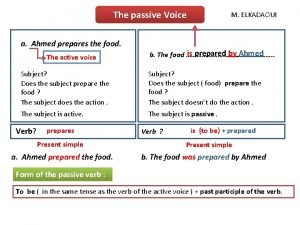
Money make the world go round meaning Make a chart on active and passive voice
Make a chart on active and passive voice Computers make the world smaller and smarter
Computers make the world smaller and smarter Love doesn't make the world go round
Love doesn't make the world go round Love doesn't make the world go round
Love doesn't make the world go round