Audit on Adrenal Incidentalomas P Lang Ping Nam



- Slides: 28
Audit on Adrenal Incidentalomas P Lang Ping Nam, MSJ Wilson, A Reid, SR Aspinall Northumbria Healthcare NHS Foundation Trust
Contents • • Background Aims and Standard Measures Method Results – 1. Prevalence and comorbidities – 2. Radiological analysis – 3. Referral and outcomes • Interpretation • Summary
Background • Definition – Adrenal mass found on imaging conducted for another reason • Prevalence – 1. 65 - 4. 4% (1, 2) of Computed Tomography (CT) and >6% in autopsy series (3, 4)
Aims • Establish prevalence of adrenal incidentalomas in Northumbria Trust • Audit referral pathways, investigation protocols and end-point management • Compare to published guidelines
BAETS Guidelines 2003 (5) • Clinical evaluation to assess for evidence of hormone overproduction • Biochemical screening in all cases • Surgery if lesion is functioning, >3 cm or shows rapid increase in size • Surveillance by repeat CT if lesion <3 cm • Needle biopsy only if history of primary malignancy elsewhere with no other metastases
BMJ Best Practice Guidelines 2011 (6) • Clinical evaluation • Biochemical screening in all cases • Imaging with CT/magnetic resonance imaging (MRI) – If attenuation > 10 Hounsfield Units on unenhanced CT → contrast CT – If hormonally active → functional imaging • Surveillance imaging at 6 – 12 months and annual biochemical assessment for 4 years
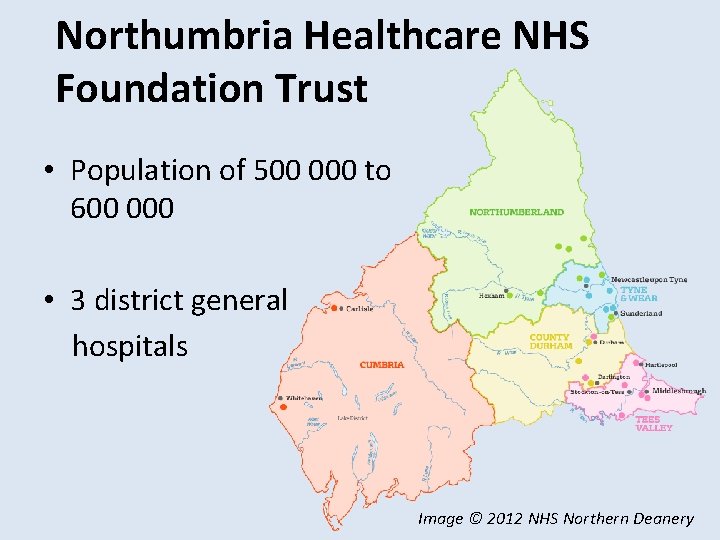
Northumbria Healthcare NHS Foundation Trust • Population of 500 000 to 600 000 • 3 district general hospitals Image © 2012 NHS Northern Deanery
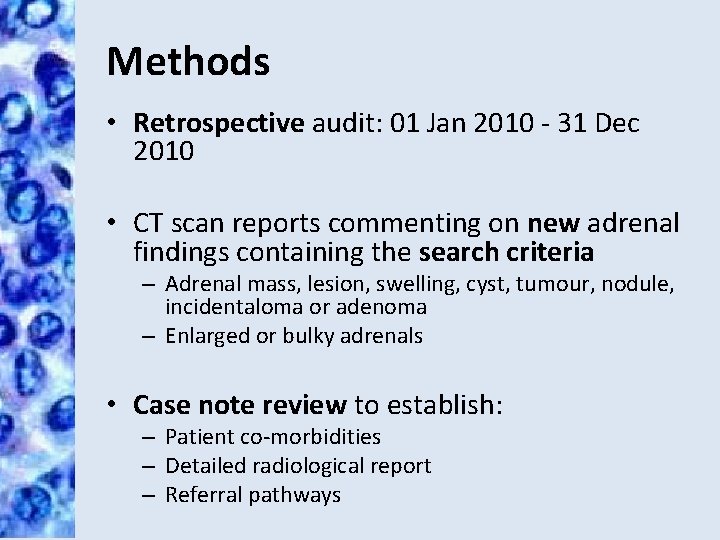
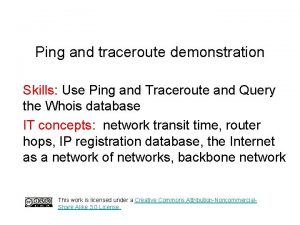
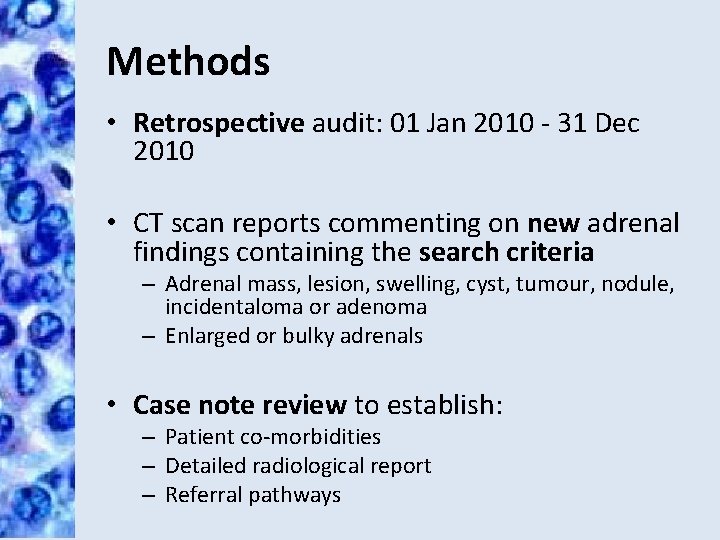
Methods • Retrospective audit: 01 Jan 2010 - 31 Dec 2010 • CT scan reports commenting on new adrenal findings containing the search criteria – Adrenal mass, lesion, swelling, cyst, tumour, nodule, incidentaloma or adenoma – Enlarged or bulky adrenals • Case note review to establish: – Patient co-morbidities – Detailed radiological report – Referral pathways
Results
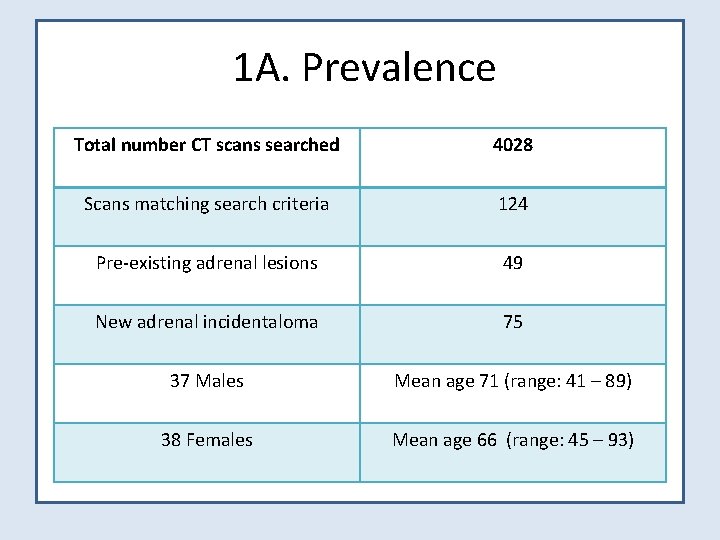
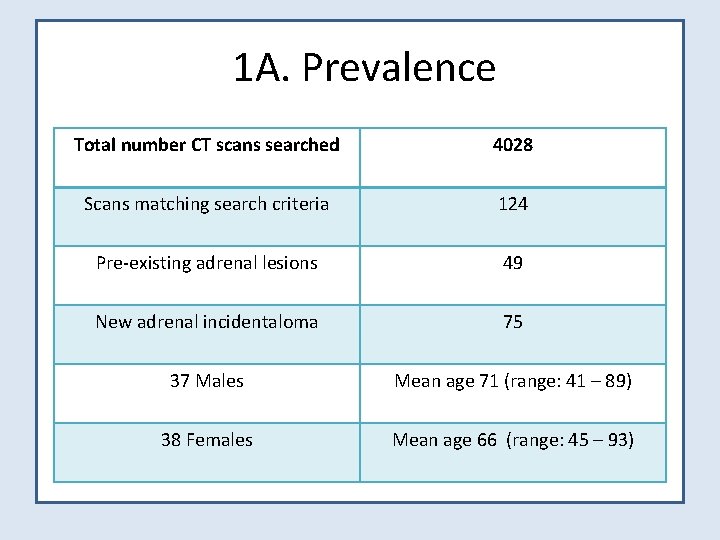
1 A. Prevalence Total number CT scans searched 4028 Scans matching search criteria 124 Pre-existing adrenal lesions 49 New adrenal incidentaloma 75 37 Males Mean age 71 (range: 41 – 89) 38 Females Mean age 66 (range: 45 – 93)

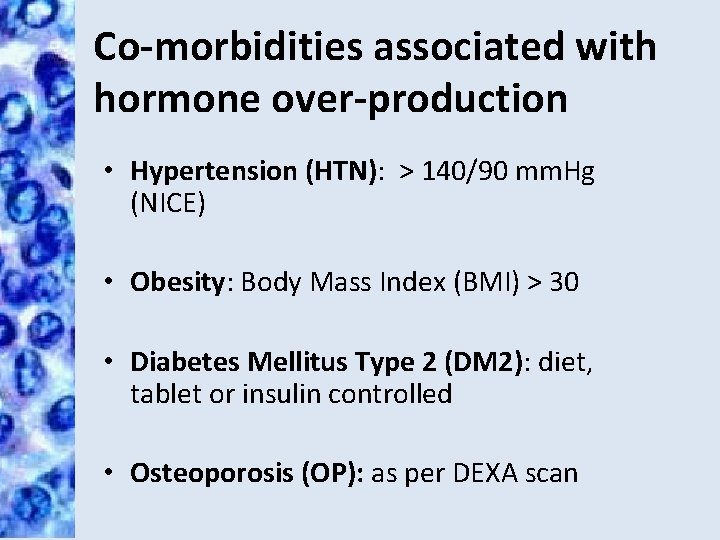
Co-morbidities associated with hormone over-production • Hypertension (HTN): > 140/90 mm. Hg (NICE) • Obesity: Body Mass Index (BMI) > 30 • Diabetes Mellitus Type 2 (DM 2): diet, tablet or insulin controlled • Osteoporosis (OP): as per DEXA scan
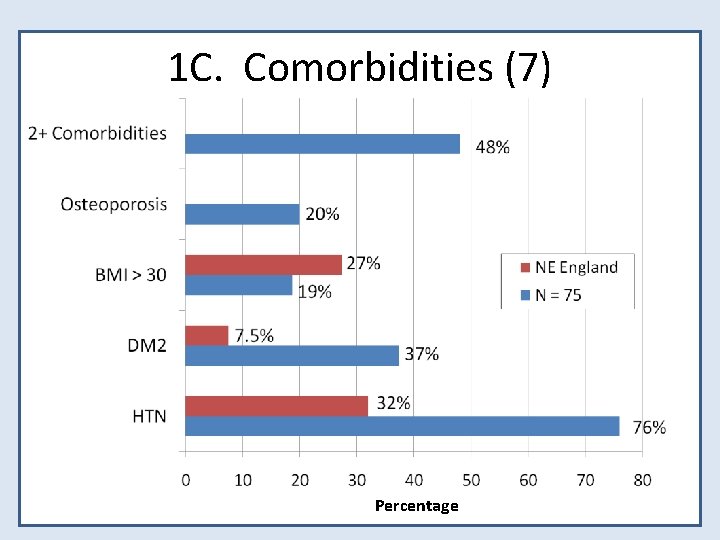
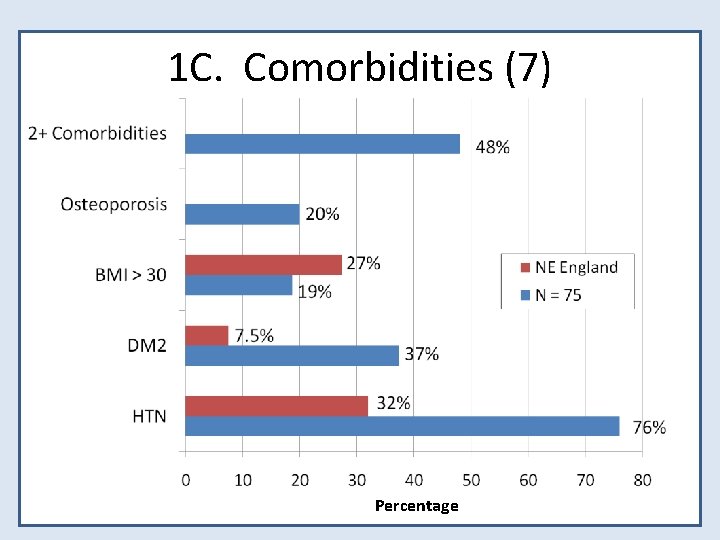
1 C. Comorbidities (7) Percentage
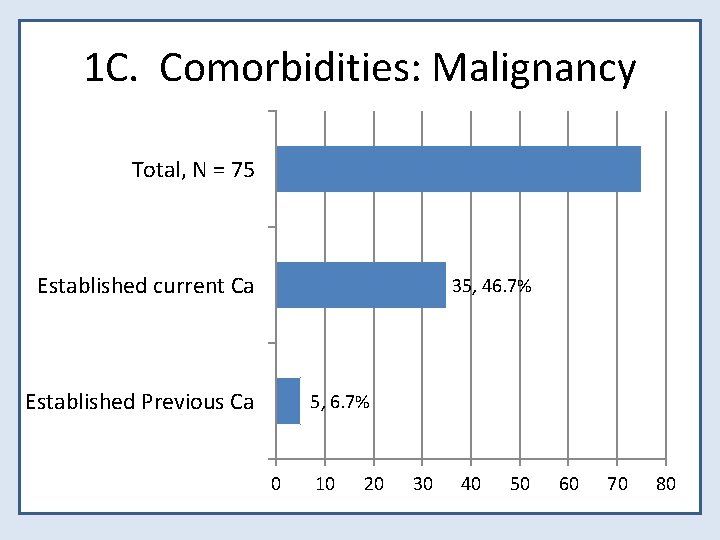
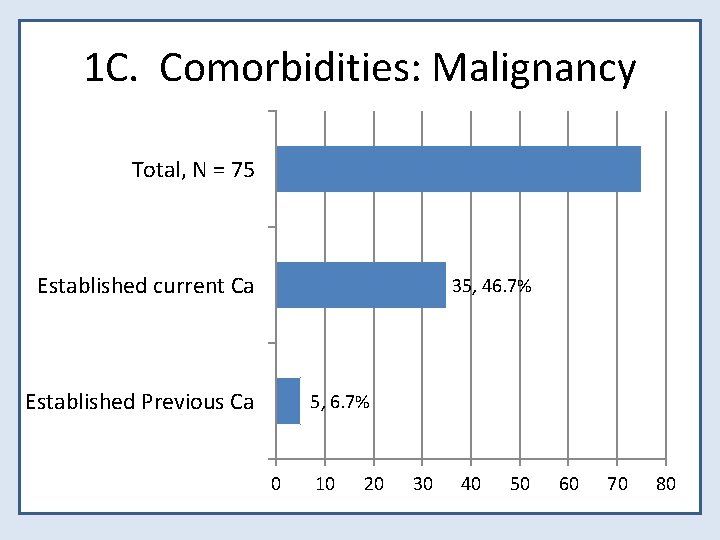
1 C. Comorbidities: Malignancy Total, N = 75 Established current Ca 35, 46. 7% Established Previous Ca 5, 6. 7% 0 10 20 30 40 50 60 70 80
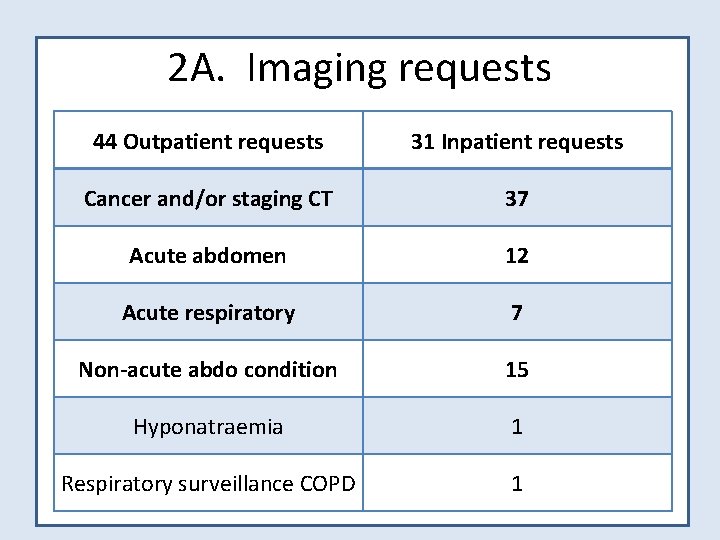
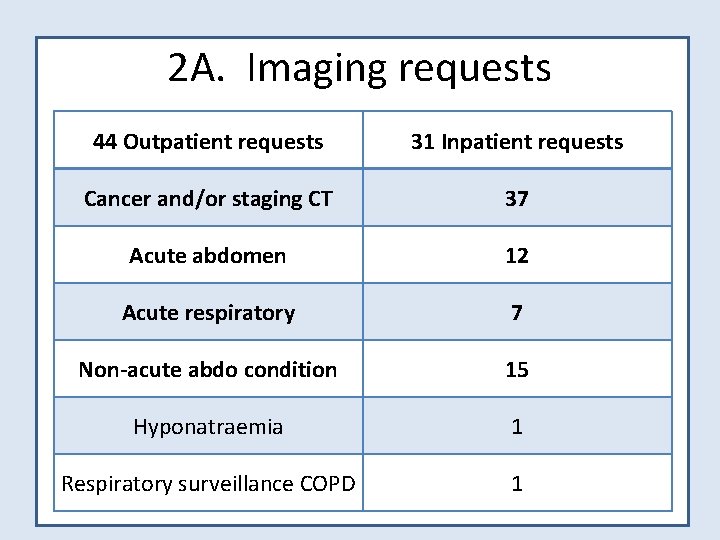
2 A. Imaging requests 44 Outpatient requests 31 Inpatient requests Cancer and/or staging CT 37 Acute abdomen 12 Acute respiratory 7 Non-acute abdo condition 15 Hyponatraemia 1 Respiratory surveillance COPD 1
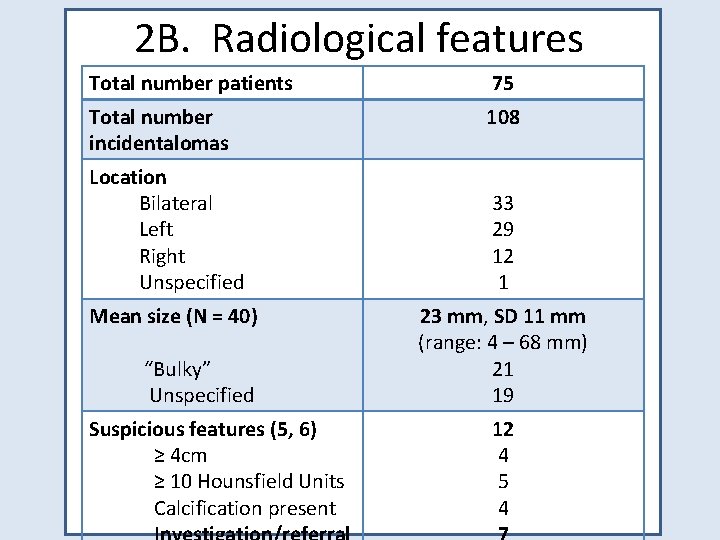
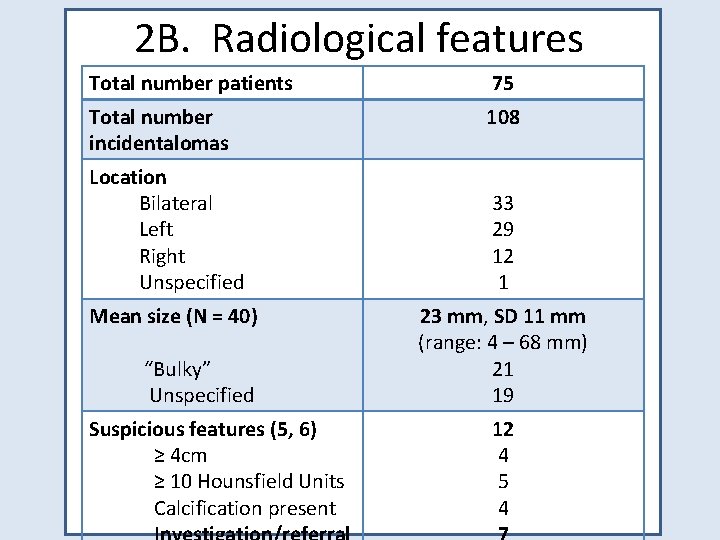
2 B. Radiological features Total number patients 75 Total number incidentalomas 108 Location Bilateral Left Right Unspecified Mean size (N = 40) “Bulky” Unspecified Suspicious features (5, 6) ≥ 4 cm ≥ 10 Hounsfield Units Calcification present 33 29 12 1 23 mm, SD 11 mm (range: 4 – 68 mm) 21 19 12 4 5 4

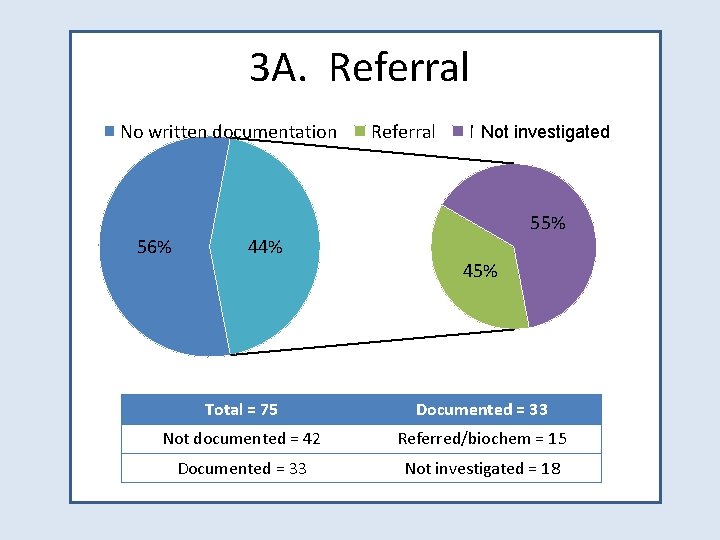
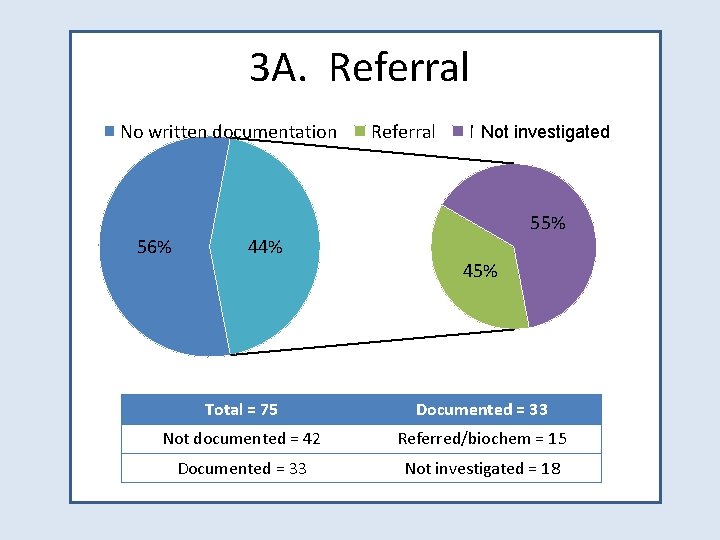
3 A. Referral No written documentation 56% 44% Referral Not investigated Not referred 55% 45% Total = 75 Documented = 33 Not documented = 42 Referred/biochem = 15 Documented = 33 Not investigated = 18
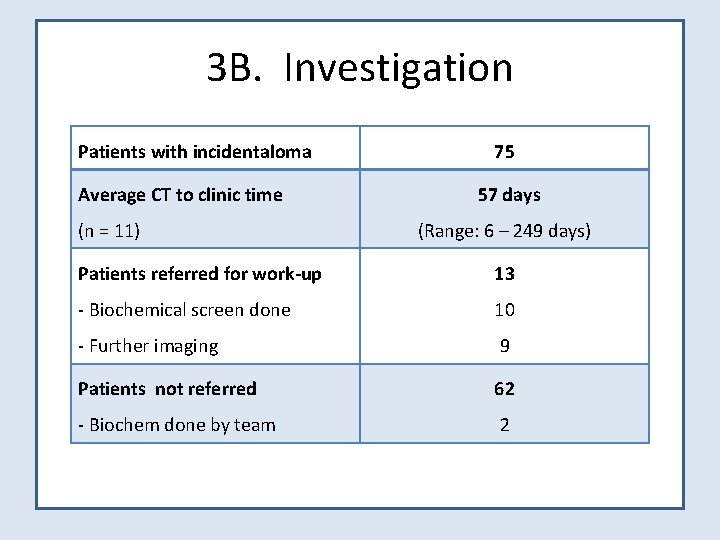
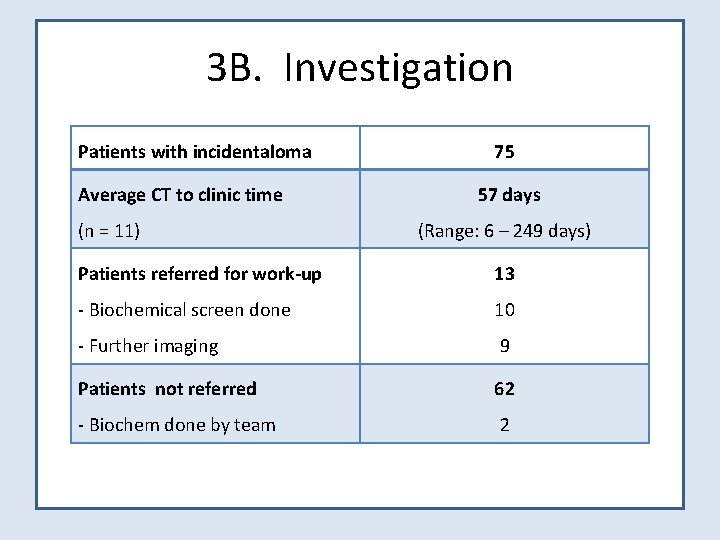
3 B. Investigation Patients with incidentaloma Average CT to clinic time (n = 11) 75 57 days (Range: 6 – 249 days) Patients referred for work-up 13 - Biochemical screen done 10 - Further imaging 9 Patients not referred 62 - Biochem done by team 2

3 C. Outcomes Patients referred for work-up Referred Did Not Attend 13 1 Reviewed in clinic - Surgery Phaeochromocytoma Cushing’s 12 3 1 2 - Metastates Received CT-guided FNA Presumed 4 1 3 - Surveillance Presumed benign Pit. Hyperprolactinaemia 5 4 1
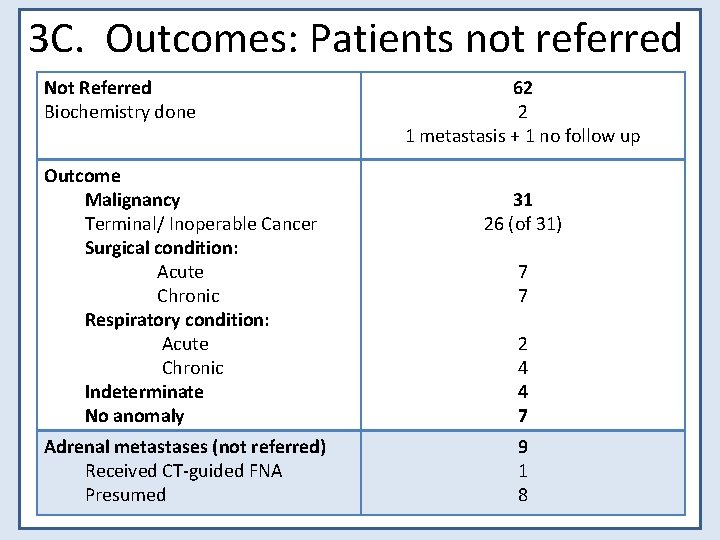
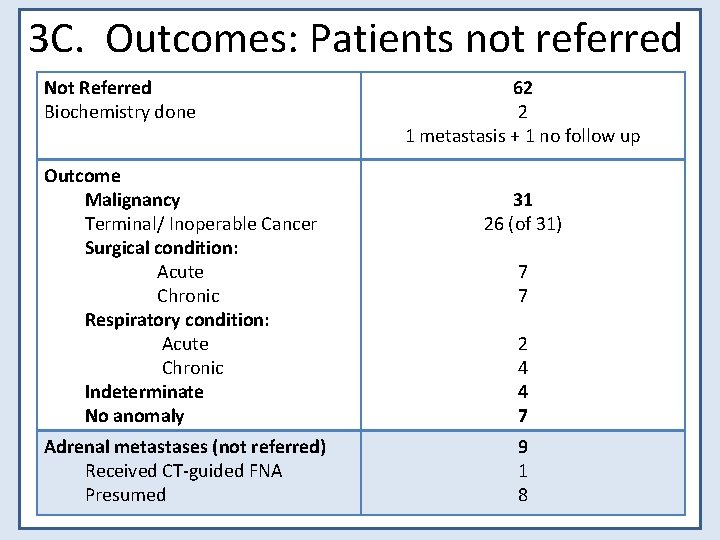
3 C. Outcomes: Patients not referred Not Referred Biochemistry done Outcome Malignancy Terminal/ Inoperable Cancer Surgical condition: Acute Chronic Respiratory condition: Acute Chronic Indeterminate No anomaly Adrenal metastases (not referred) Received CT-guided FNA Presumed 62 2 1 metastasis + 1 no follow up 31 26 (of 31) 7 7 2 4 4 7 9 1 8
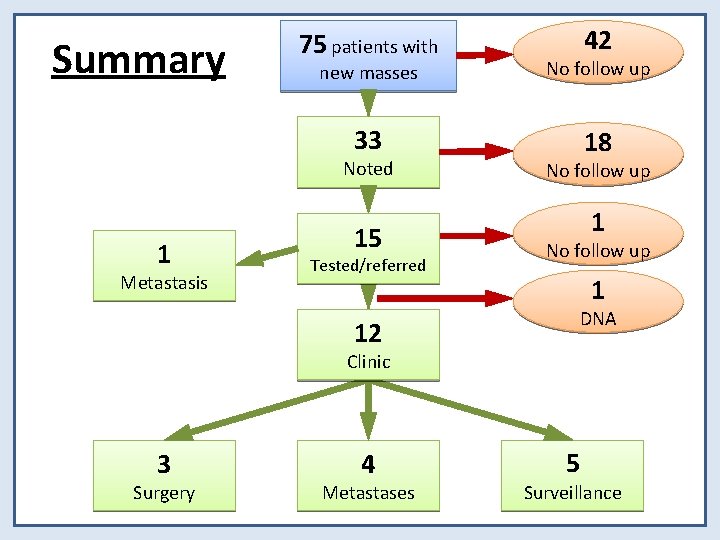
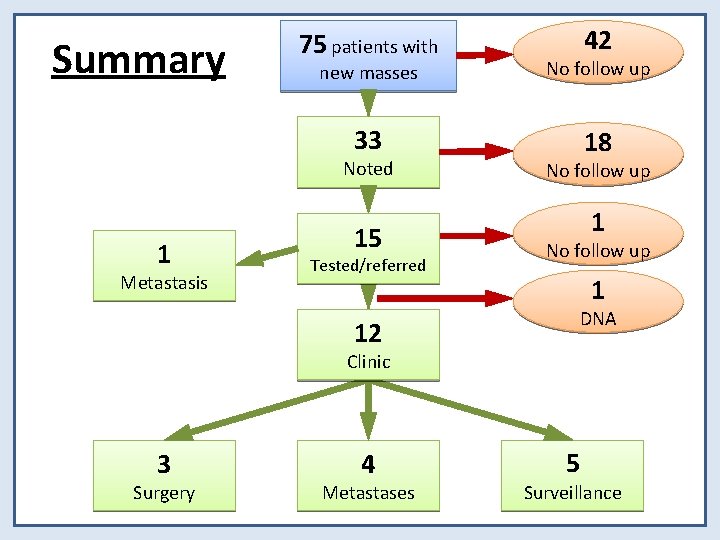
Summary 75 patients with new masses No follow up 33 18 Noted 1 Metastasis 42 15 Tested/referred No follow up 1 DNA 12 Clinic 3 Surgery 4 Metastases 5 Surveillance
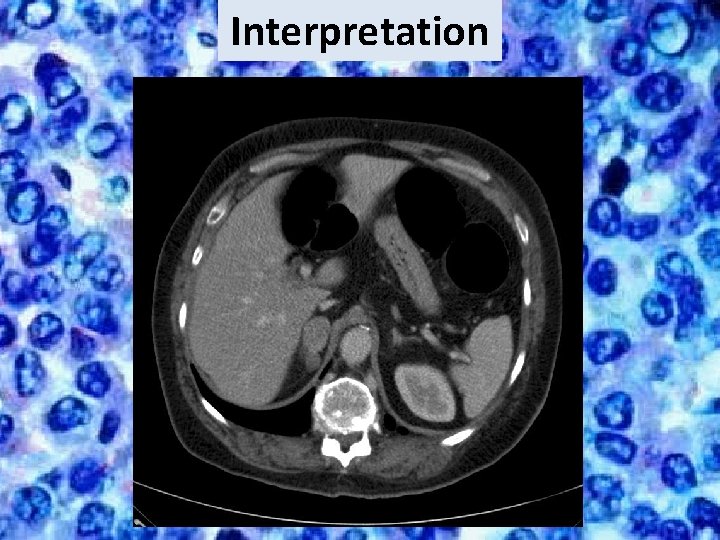
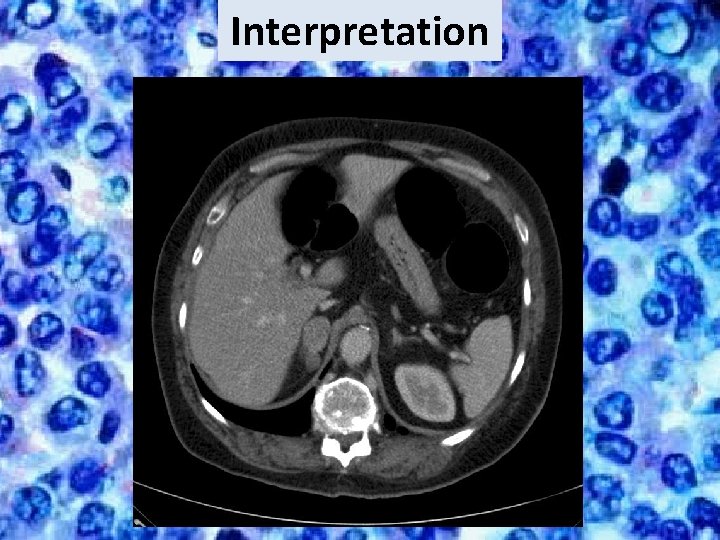
Interpretation
Discussion • Prevalence in this series (1. 9%) consistent with other published studies (1, 2) • National Guidelines are not being followed – Majority of incidentalomas (56%) were not commented upon in case notes – Only a minority (20%) had biochemical screening or referral for work-up • Investigative protocols in those referred comply with National Guidelines
Discussion • 3 of 12 (25%) incidentalomas worked up were functioning lesions – All surgically managed – Histology: 2 benign adrenal cortical adenomas, 1 phaeochromocytoma • 62 of 75 (83%) were not referred – 26 (42%) were diagnosed with metastatic/inoperable cancer – 36 (58%) did not have co-morbidities that would preclude incidentaloma work-up
Discussion • A high incidence of co-morbidities associated with hormone over-production • Are adrenal incidentalomas contributing to the high incidence of DM 2 (37% or x 5 regional value) and HTN (76% or x 2 regional value) observed?
Summary • Prevalence of adrenal incidentaloma in Northumbria is 1. 9% • National Guidelines for their management are not being followed as the majority were not investigated • Awareness of adrenal incidentalomas among clinicians needs to be raised
References 1) Price L, Munigoti S, Rees A (2011) Management of adrenal incidentaloma: are we getting it right? Endocrine Abstracts 25: 54 2) Bovio S, Cataldi A, Reimondo G, Sperone P, Novello S, Berruti A, Borasio P, Fava C, Dogliotti L, Scagliotti GV, Angeli A, Terzolo M (2006) Prevalence of adrenal incidentaloma in a contemporary computerized tomography series Journal of Endocrinological Investigation 29(4): 298302 3) Young WFJr (2007) The Incidentally Discovered Adrenal Mass New England Journal of Medicine 356: 601 -10 4) Kloos RT, Gross MD, Francis IR, Korobkin M, Shapiro B (1995) Incidentally Discovered Adrenal Masses Endocrine Reviews 16 (4): 46084 5) BAETS (2003) Guidelines for the Surgical Management of Endocrine Disease 6) BMJ Evidence Centre (2011) Assessment of incidental adrenal mass Best Practice 7) The Network of Public Health Observatories Northumberland Health Profile (2012); Modelled estimates of prevalence (2011) www. apho. org. uk • Image: Cybermedicine 2000 – Adrenal Neoplasm
 Chí tuyến nam nằm ở vĩ độ nào
Chí tuyến nam nằm ở vĩ độ nào Lịch sử hà nội từ năm 1802 đến năm 1918
Lịch sử hà nội từ năm 1802 đến năm 1918 Daj nam svima duha svog tekst
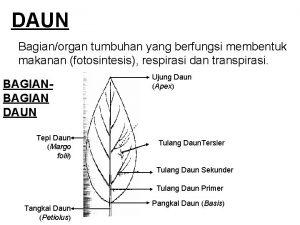
Daj nam svima duha svog tekst Bentuk daun acicular
Bentuk daun acicular Limitations of auditing
Limitations of auditing Audit informasi klinis adalah
Audit informasi klinis adalah Perbedaan prosedur audit top-down dengan bottom-up
Perbedaan prosedur audit top-down dengan bottom-up Janette loveys
Janette loveys Beda audit medis dan audit klinis
Beda audit medis dan audit klinis Auditor definition
Auditor definition Overall audit plan and audit program
Overall audit plan and audit program Penyelesaian audit dan tanggung jawab pasca audit
Penyelesaian audit dan tanggung jawab pasca audit Perbedaan audit konvensional dengan audit berbasis risiko
Perbedaan audit konvensional dengan audit berbasis risiko Perbedaan audit konvensional dengan audit berbasis risiko
Perbedaan audit konvensional dengan audit berbasis risiko Hubungan ekonomisasi efisiensi dan efektivitas
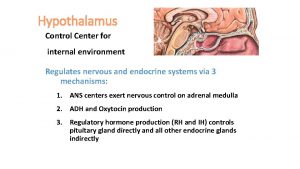
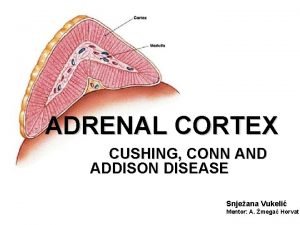
Hubungan ekonomisasi efisiensi dan efektivitas The adrenal medullae secrete
The adrenal medullae secrete Adrenal gland regions
Adrenal gland regions Adrenal medulla cortex
Adrenal medulla cortex Adrenal kriz acilci
Adrenal kriz acilci Hipotálamo-hipófise-adrenal
Hipotálamo-hipófise-adrenal Adrenal gland
Adrenal gland Conn vs addison
Conn vs addison Adrenal sympathetic pathway
Adrenal sympathetic pathway Site:slidetodoc.com
Site:slidetodoc.com Pak pandani
Pak pandani Hormonların çalışma mekanizması
Hormonların çalışma mekanizması Addison's disease vs cushing's syndrome
Addison's disease vs cushing's syndrome Relation of adrenal gland
Relation of adrenal gland Adrenal hormone pathway
Adrenal hormone pathway