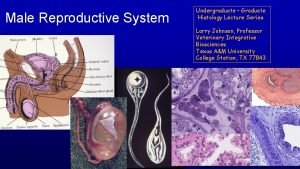
Male Reproductive System Organs of Male Reproduction Gonads


















































- Slides: 122

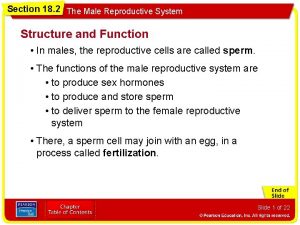
Male Reproductive System

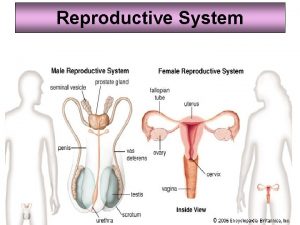
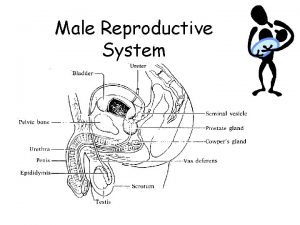
• Organs of Male Reproduction – Gonads (Testes) • produce gametes (sperm) • secrete the sex steroid hormones
• Organs of Male Reproduction – Ducts (reproductive tract) • Store Sperm • Transport sperm
• Organs of Male Reproduction – Accessory Organs • Secrete substances that support sperm
• Organs of Male Reproduction –External genitalia • Penis • scrotum
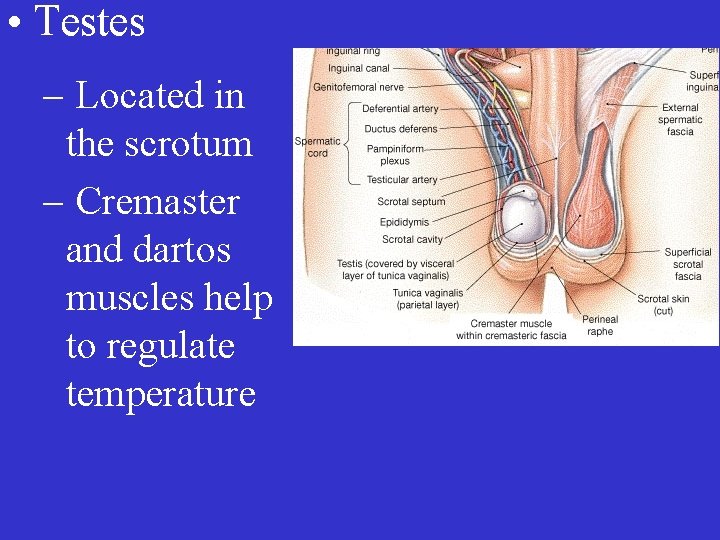
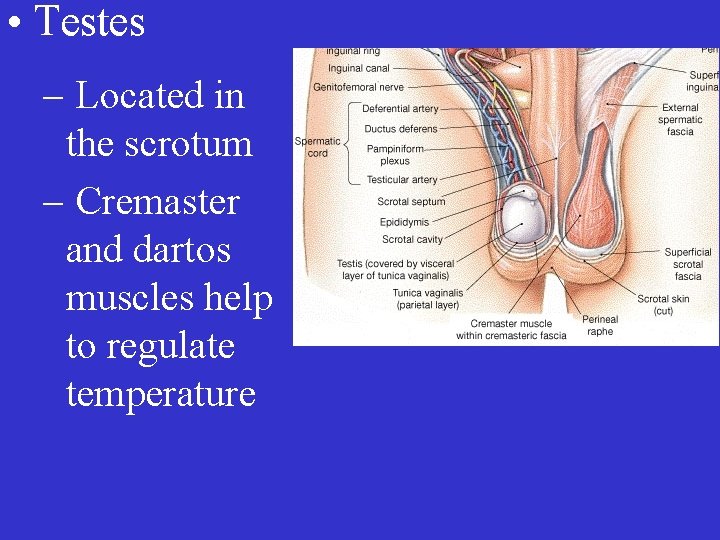
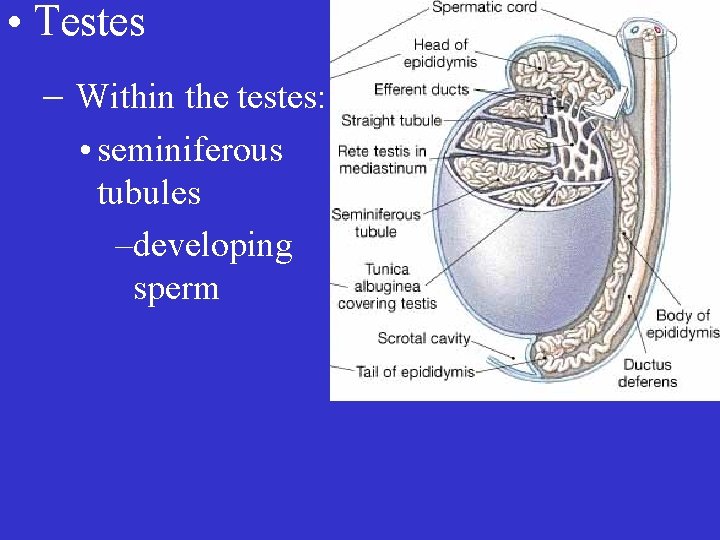
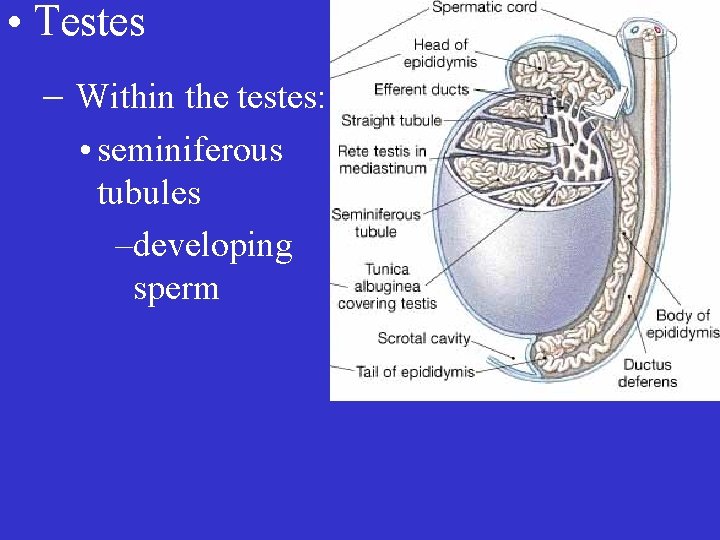
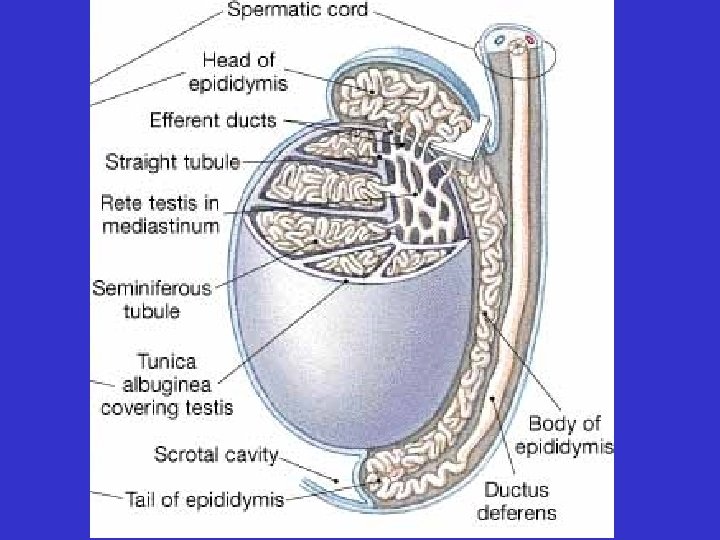
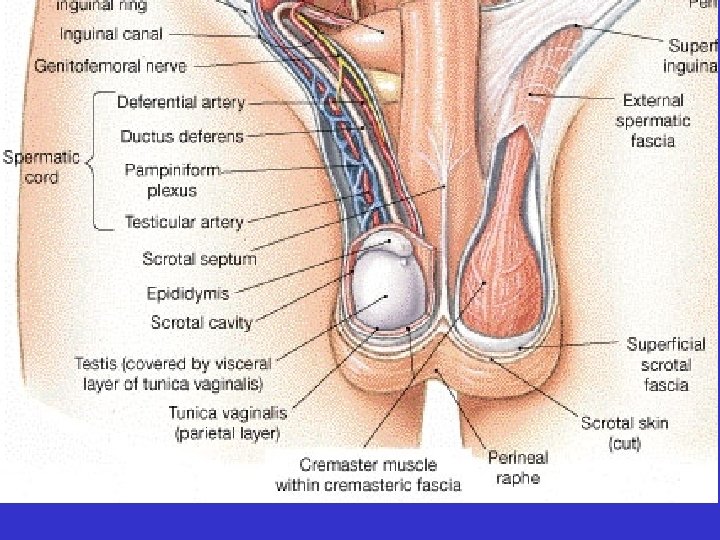
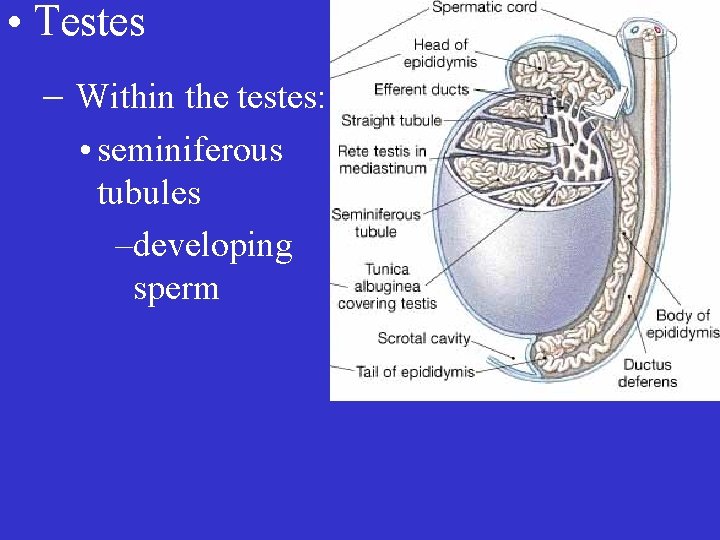
• Testes – Located in the scrotum – Cremaster and dartos muscles help to regulate temperature
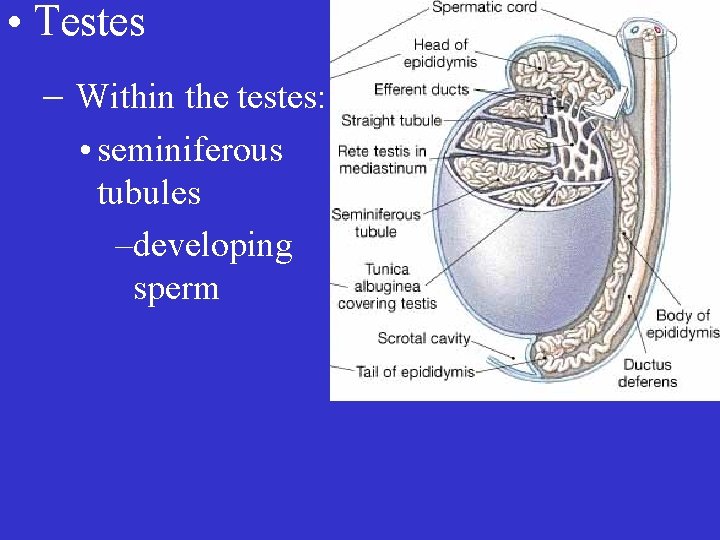
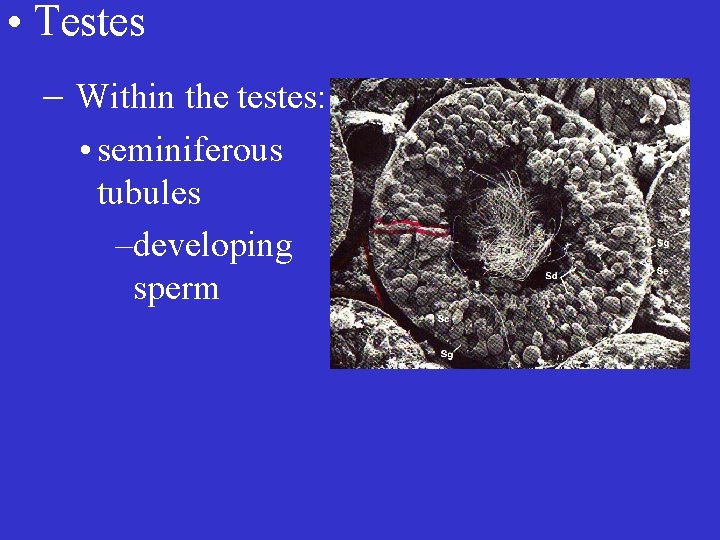
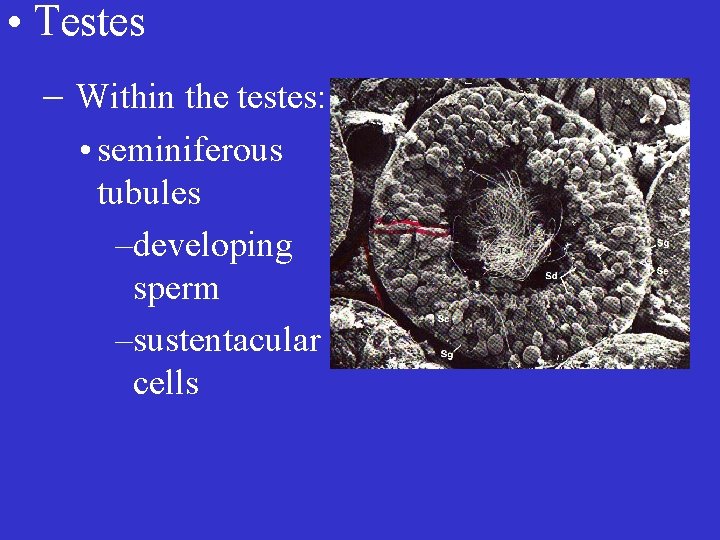
• Testes – Within the testes: • seminiferous tubules –developing sperm
• Testes – Within the testes: • seminiferous tubules –developing sperm
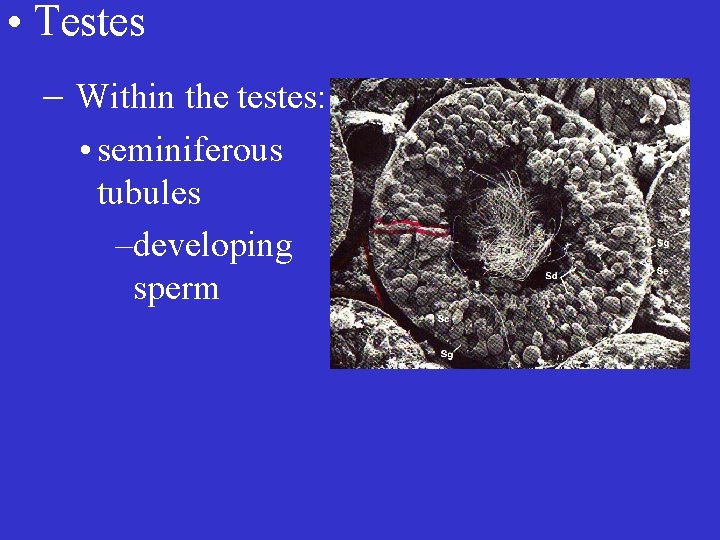
• Testes – Within the testes: • seminiferous tubules –developing sperm
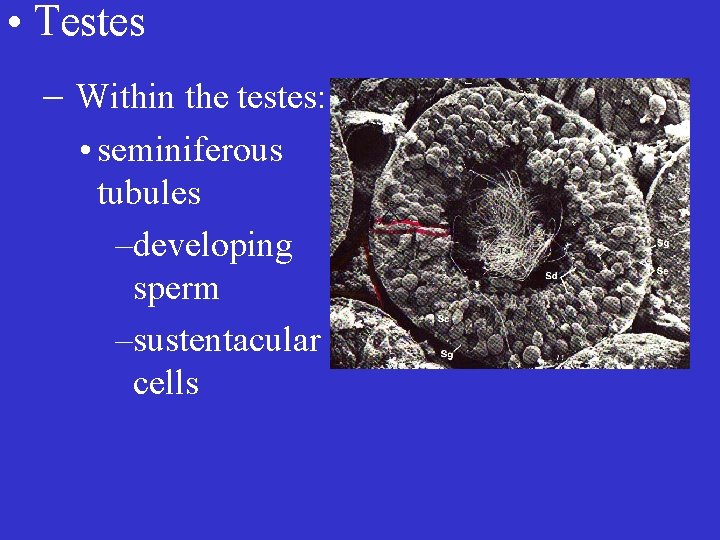
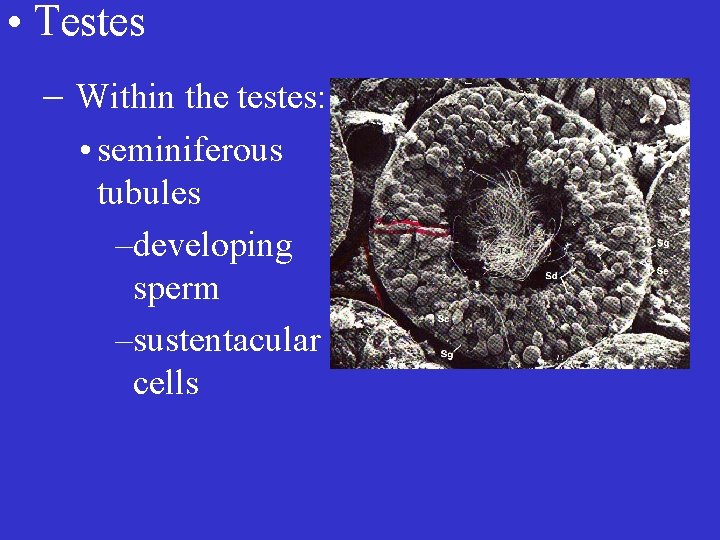
• Testes – Within the testes: • seminiferous tubules –developing sperm –sustentacular cells

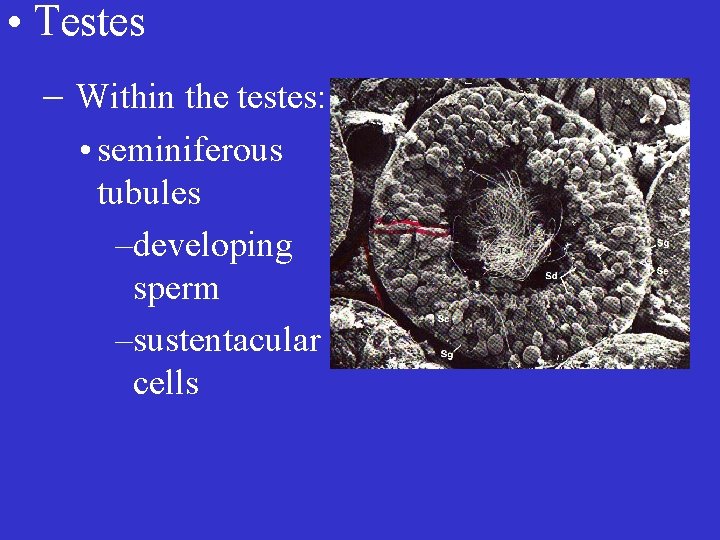
• Testes – Within the testes: • seminiferous tubules –developing sperm –sustentacular cells
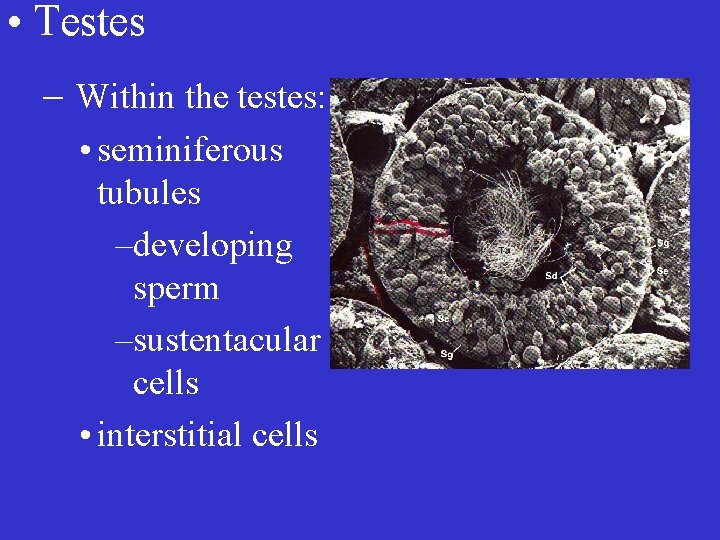
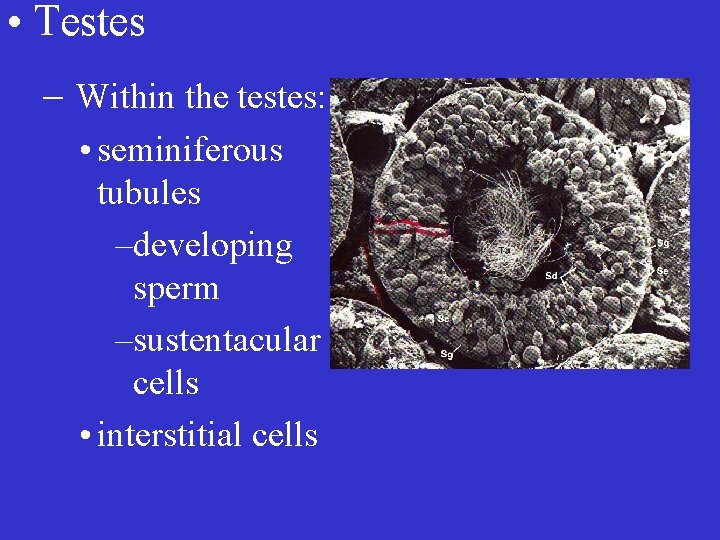
• Testes – Within the testes: • seminiferous tubules –developing sperm –sustentacular cells • interstitial cells


Spermatogenesis
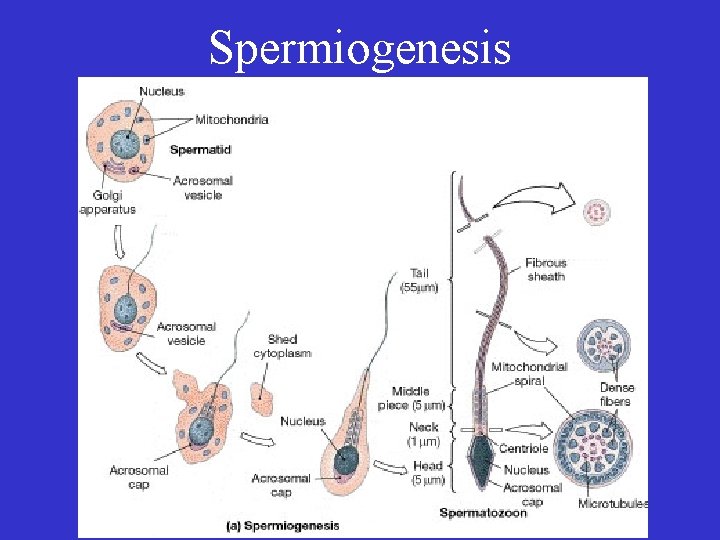
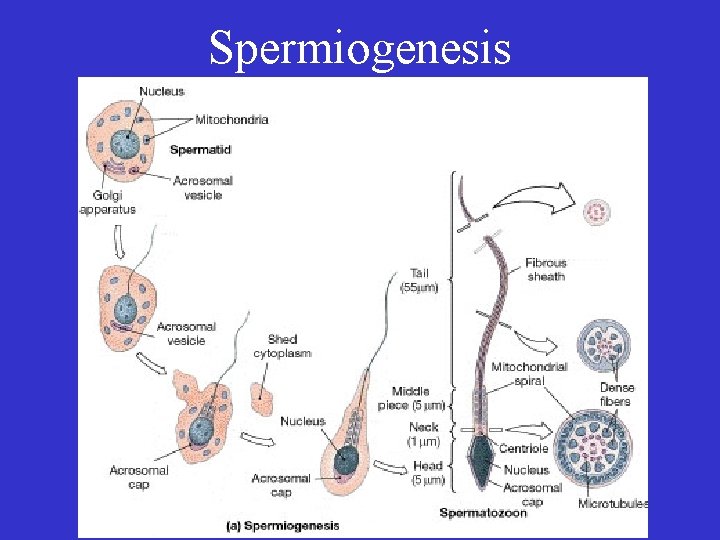
Spermiogenesis

Spermatogenesis


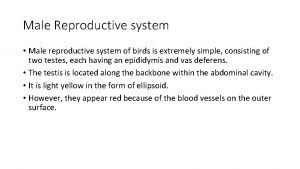
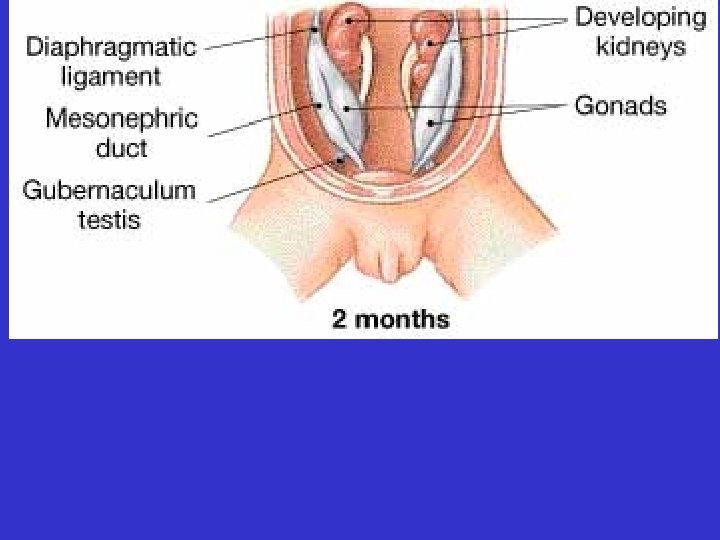
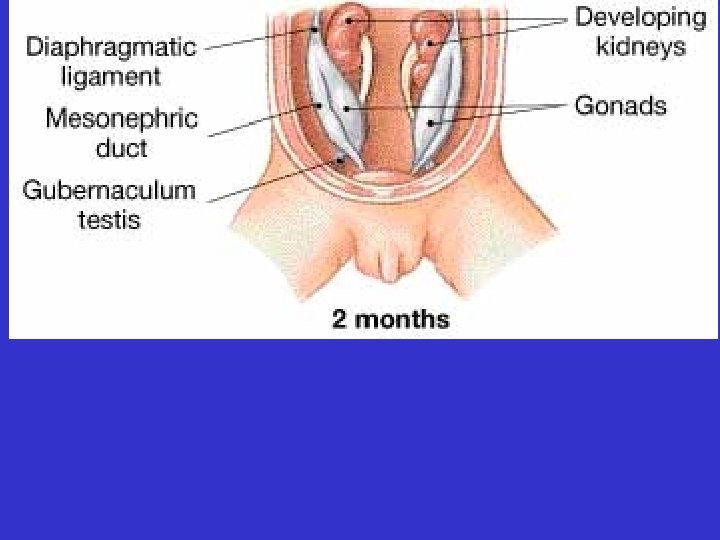
• The testes descend from the abdomen during fetal development





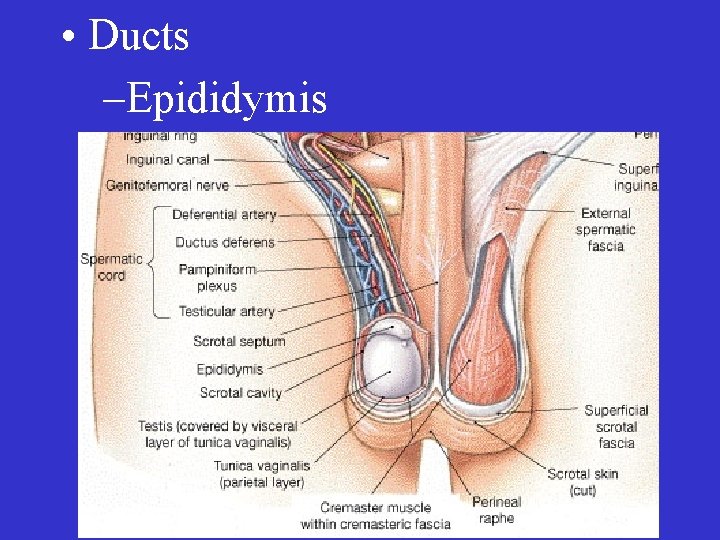
• Ducts
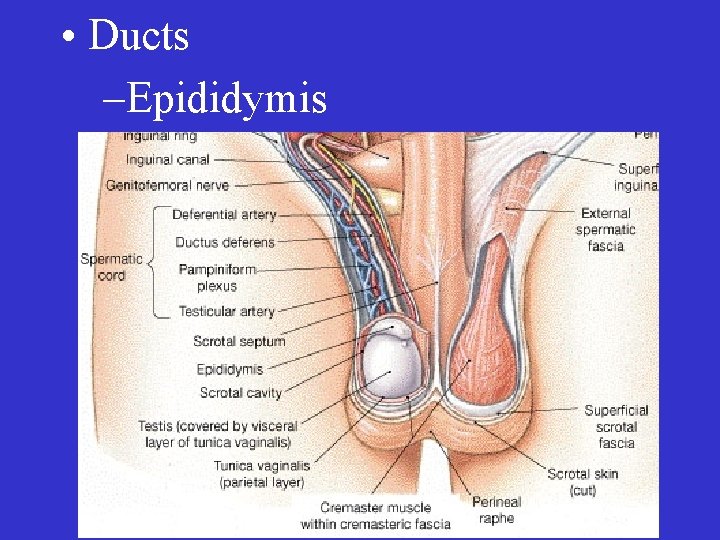
• Ducts –Epididymis

• Ducts –Epididymis
• Ducts –Epididymis – Vas deferens
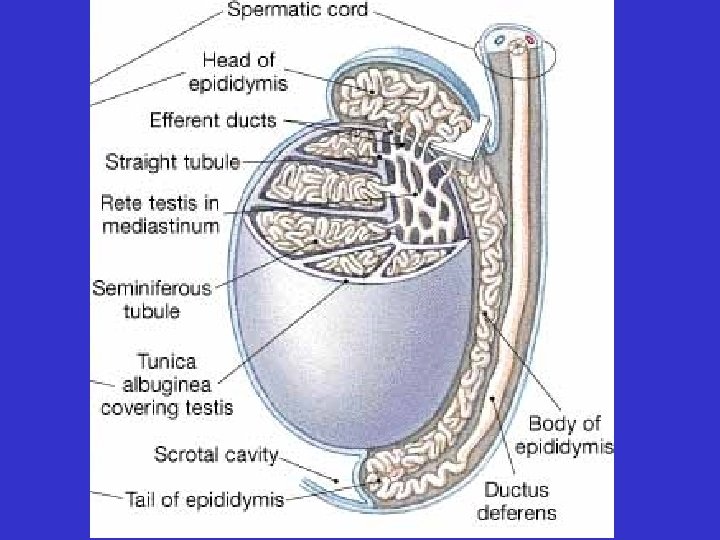

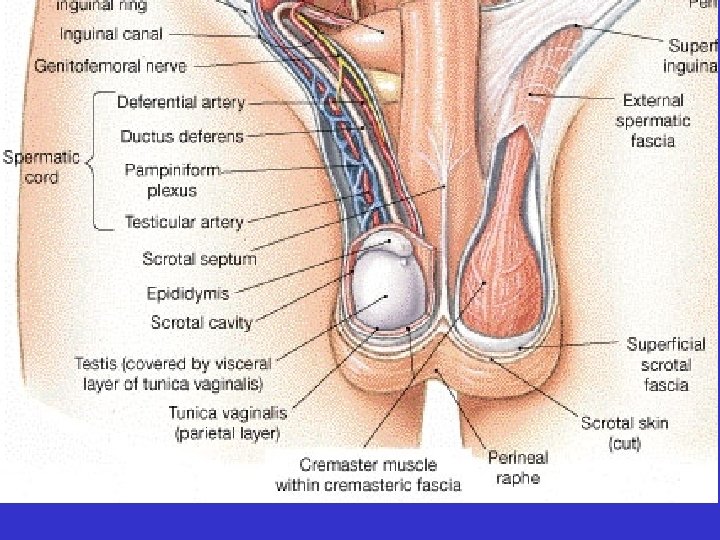






• Ducts –Epididymis – Vas deferens
• Ducts –Epididymis – Vas deferens – Ejaculatory duct


• Ducts –Epididymis – Vas deferens – Ejaculatory duct

• Ducts –Epididymis – Vas deferens – Ejaculatory duct – Urethra

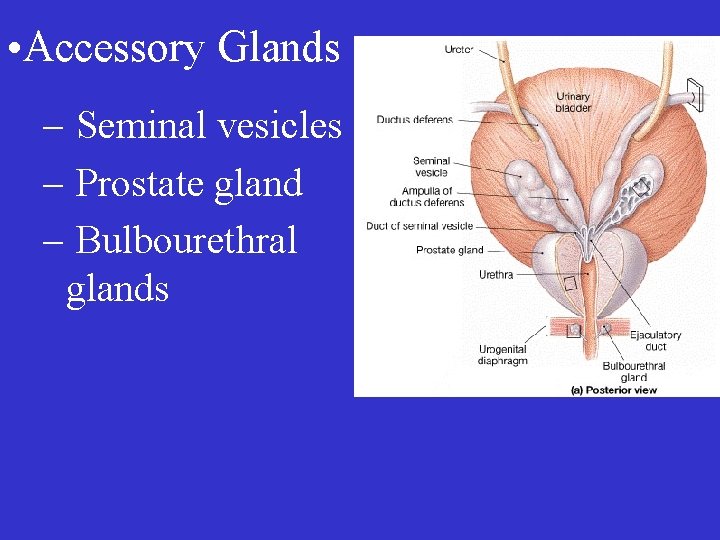
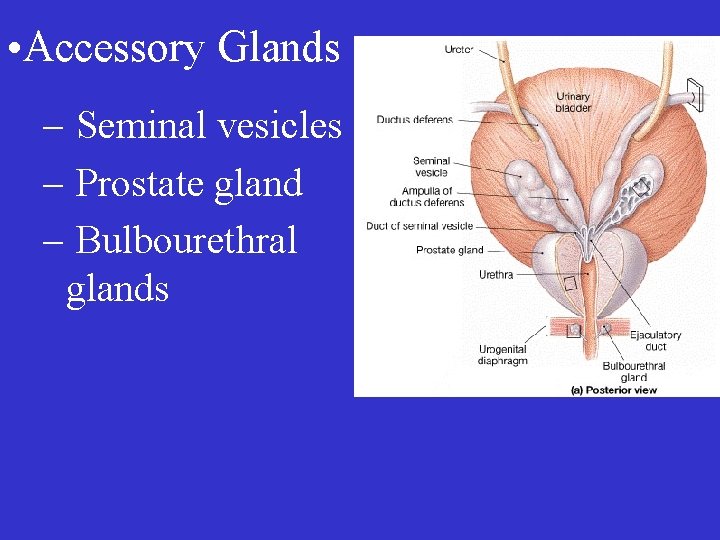
• Accessory Glands – Seminal vesicles – Prostate gland – Bulbourethral glands

• Semen
• Semen – sperm plus seminal fluid
• Semen – sperm plus seminal fluid – 20 -150 million sperm/ml
• Semen – sperm plus seminal fluid – 20 -150 million sperm/ml – includes prostaglandins,
• Semen – sperm plus seminal fluid – 20 -150 million sperm/ml – includes prostaglandins, bicarbonate,

• Semen – sperm plus seminal fluid – 20 -150 million sperm/ml – includes prostaglandins, bicarbonate, fructose,
• Semen – sperm plus seminal fluid – 20 -150 million sperm/ml – includes prostaglandins, bicarbonate, fructose, antibiotics,
• Semen – sperm plus seminal fluid – 20 -150 million sperm/ml – includes prostaglandins, bicarbonate, fructose, antibiotics, & enzymes that activate sperm
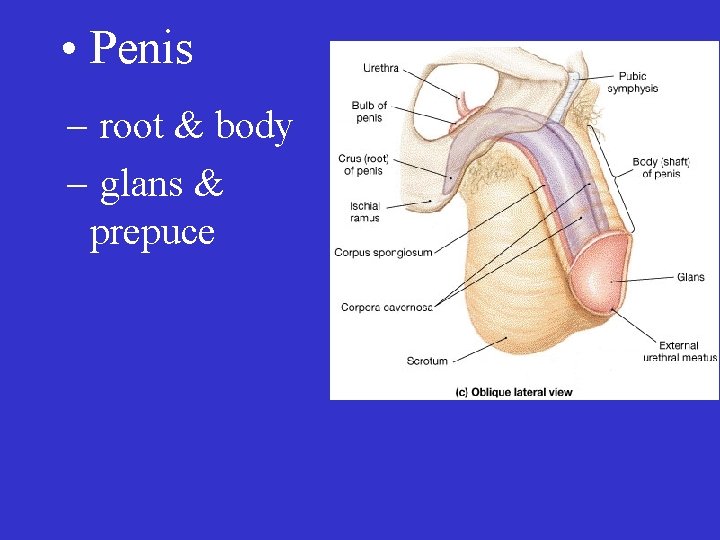
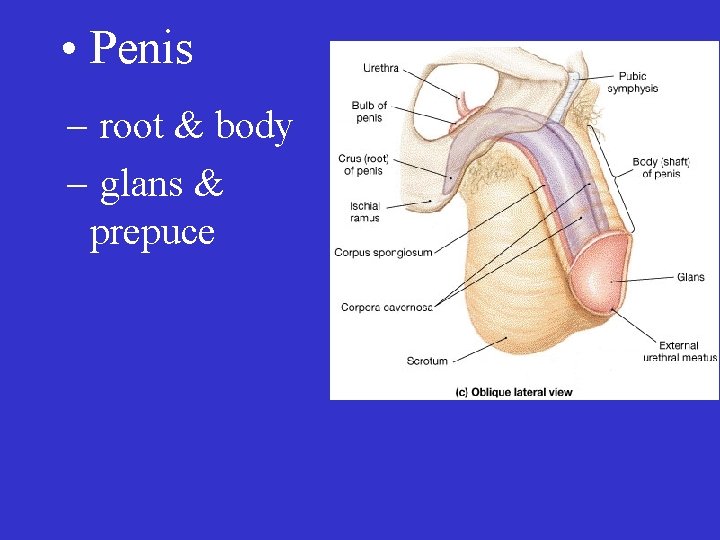
• Penis – root & body – glans & prepuce

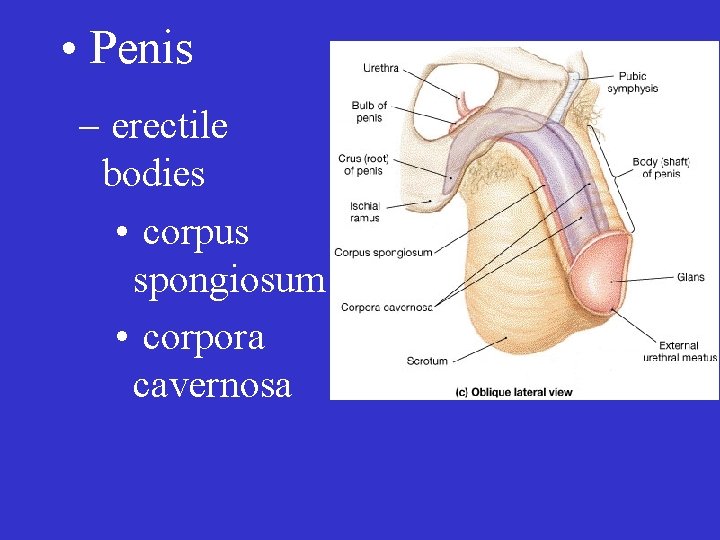
• Penis – erectile bodies • corpus spongiosum • coropora cavernosa
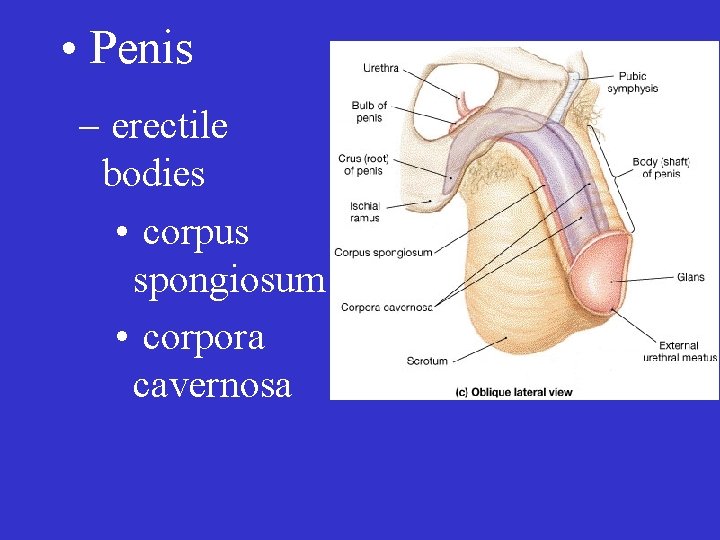
• Penis – erectile bodies • corpus spongiosum • corpora cavernosa


• Penis –erections under the control of parasympathetic stimulation – ejaculation: sympathetic
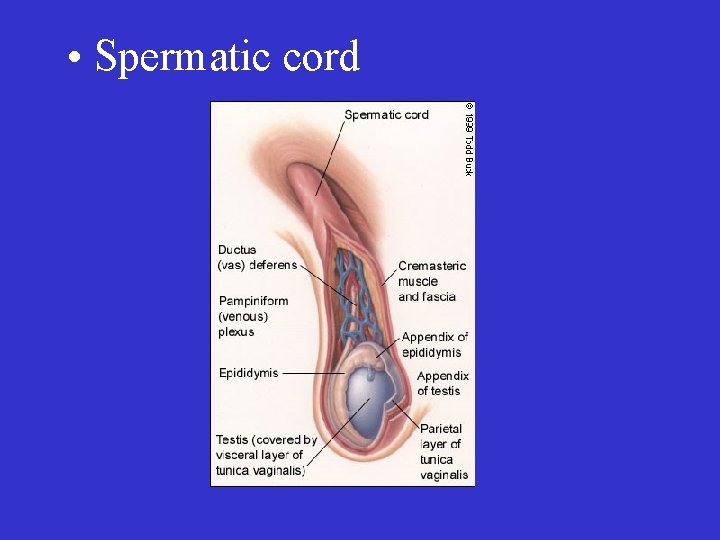
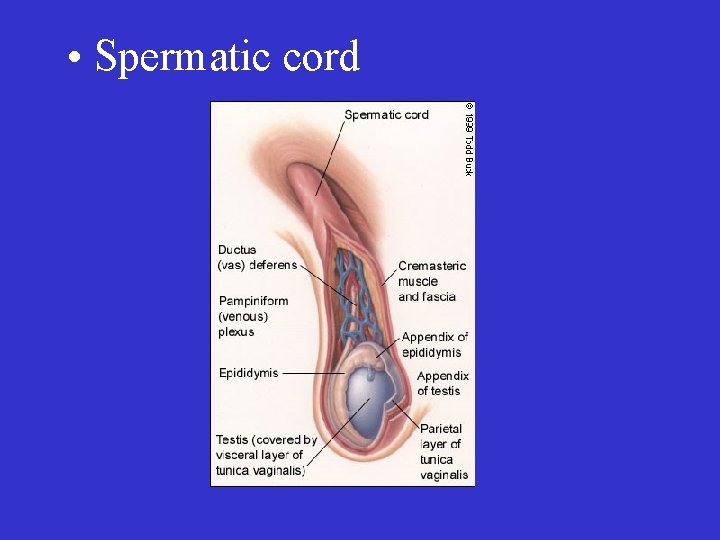
• Spermatic cord
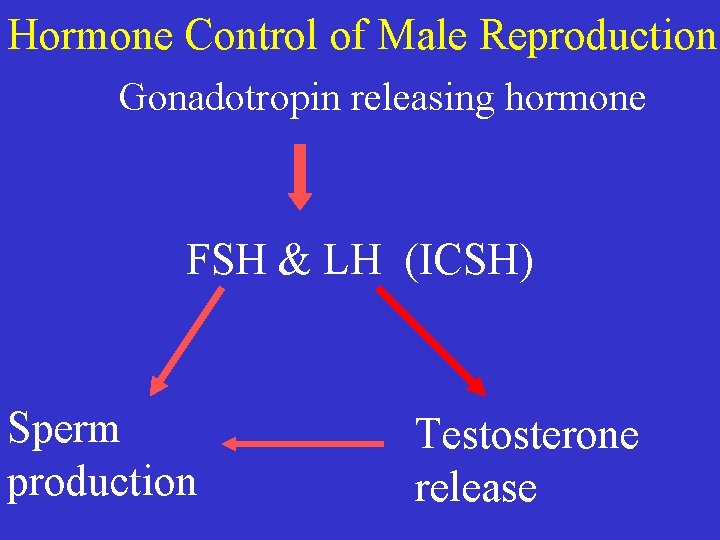
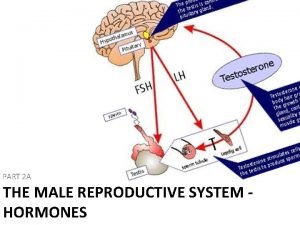
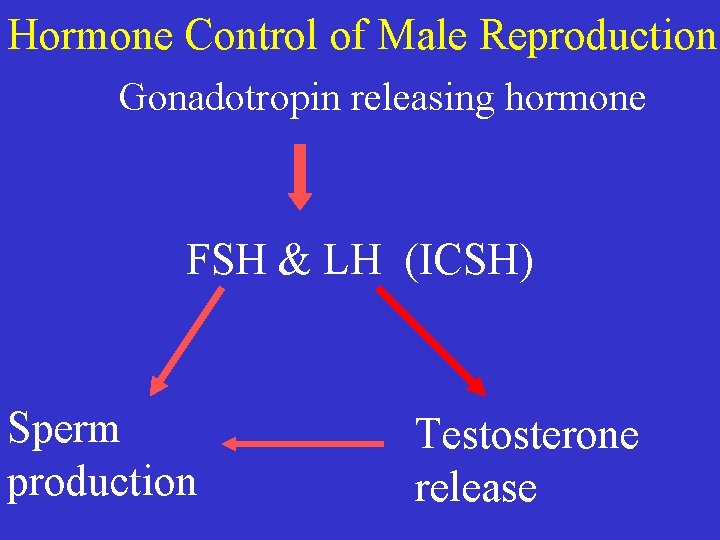
Hormone Control of Male Reproduction Gonadotropin releasing hormone FSH & LH (ICSH) Sperm production Testosterone release
• Other Functions of Testosterone – development, growth, & maintenance of male sex organs – bone and muscle growth – 2 o sex characteristics – aggression? – libido
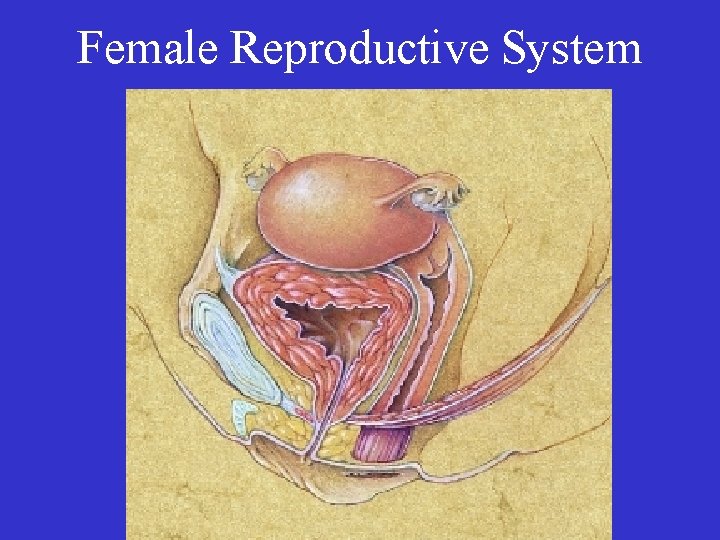
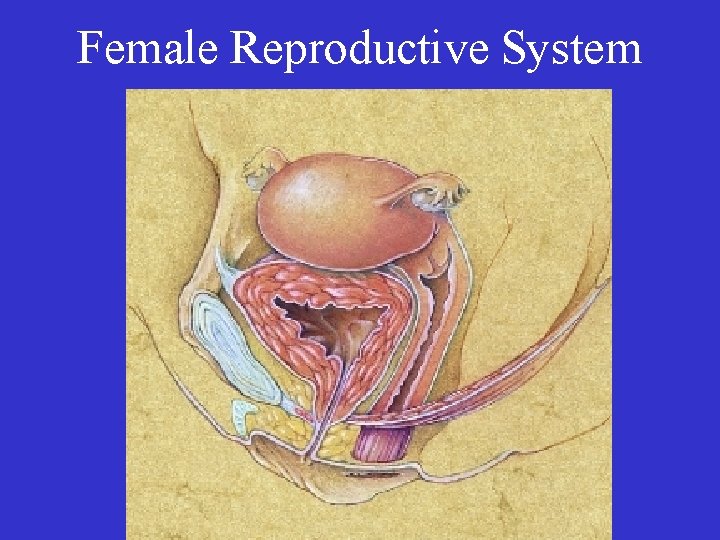
Female Reproductive System

• Organs of Female Reproduction – Gonads (Ovaries)
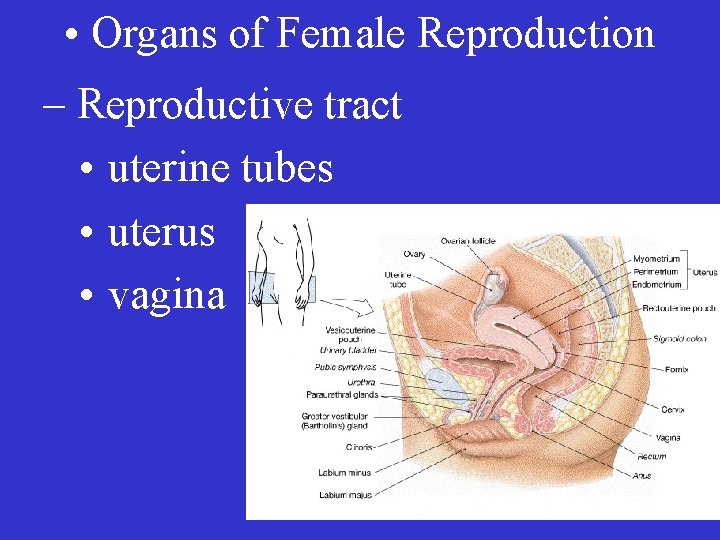
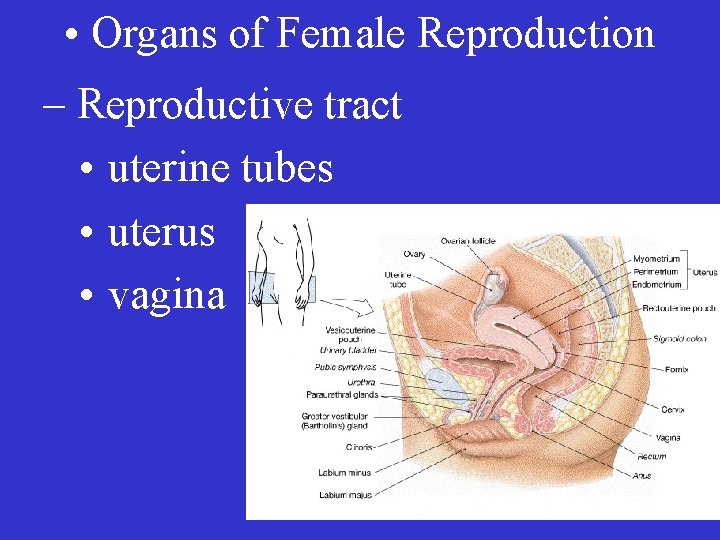
• Organs of Female Reproduction – Reproductive tract • uterine tubes • uterus • vagina
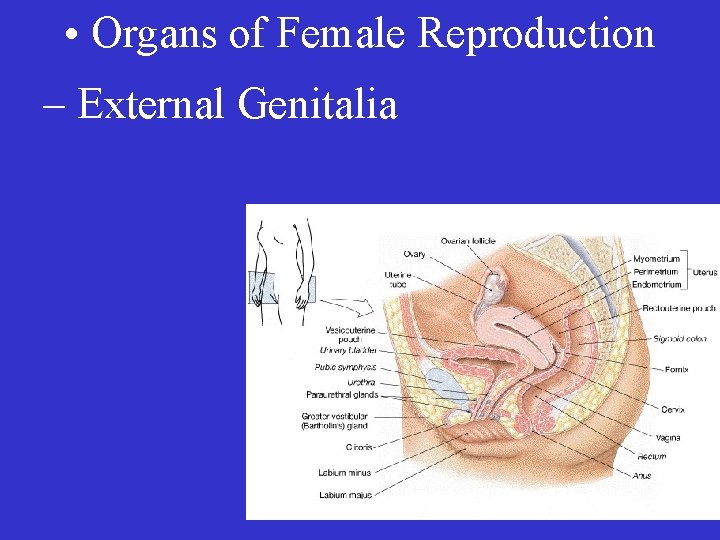
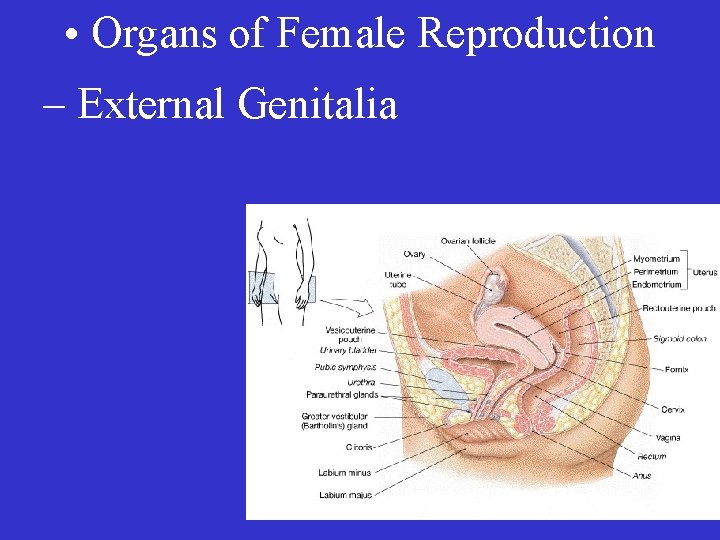
• Organs of Female Reproduction – External Genitalia
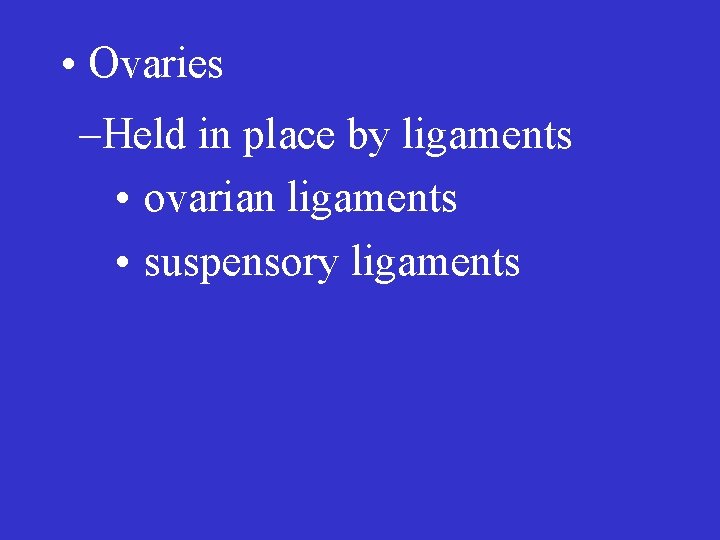
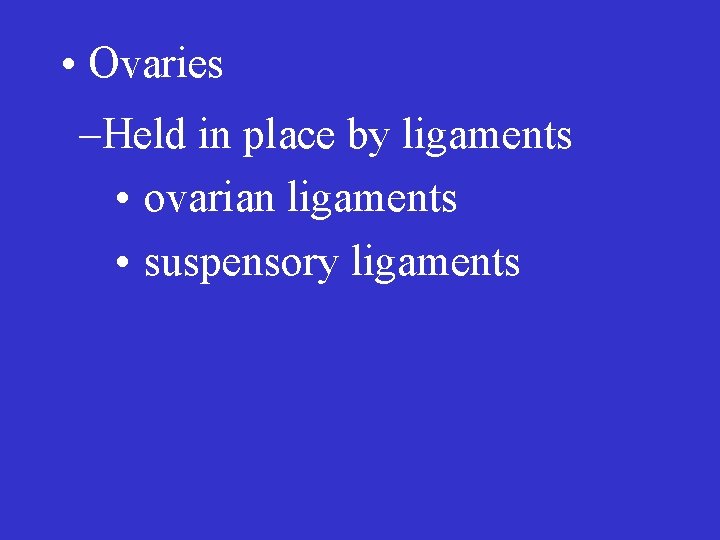
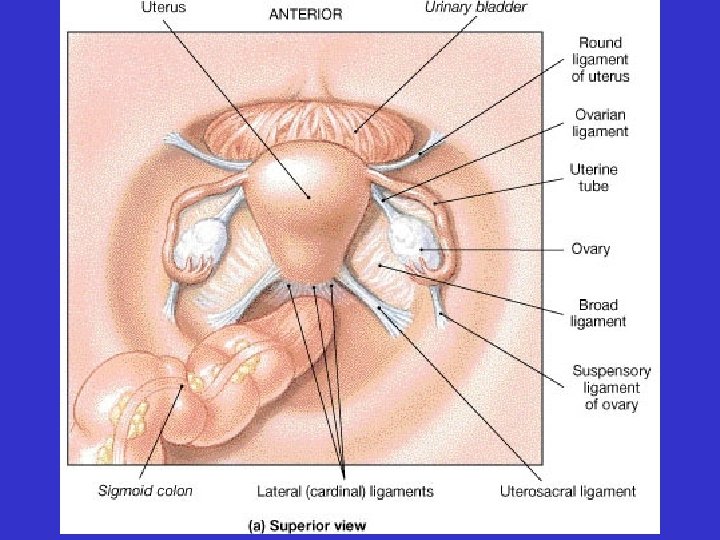
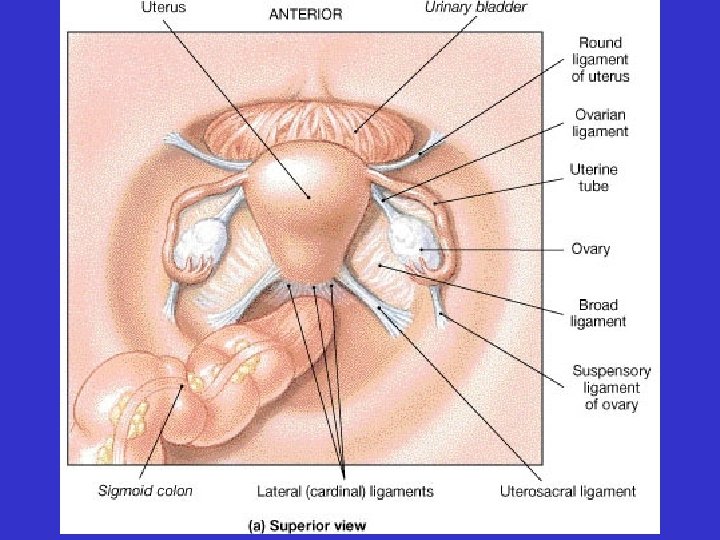
• Ovaries –Held in place by ligaments • ovarian ligaments • suspensory ligaments
• Ovaries – Produce gametes (ova) – Secrete the sex steroid hormones
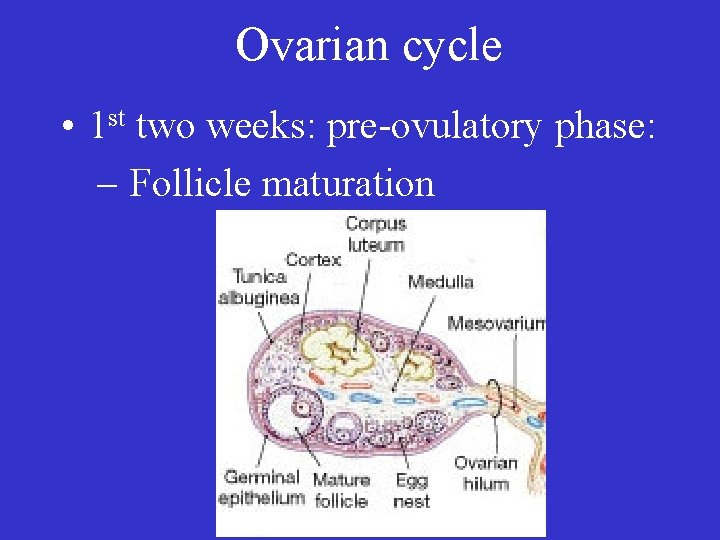
• Ovaries – Contain thousands of follicles – Each follicle contains one ovum

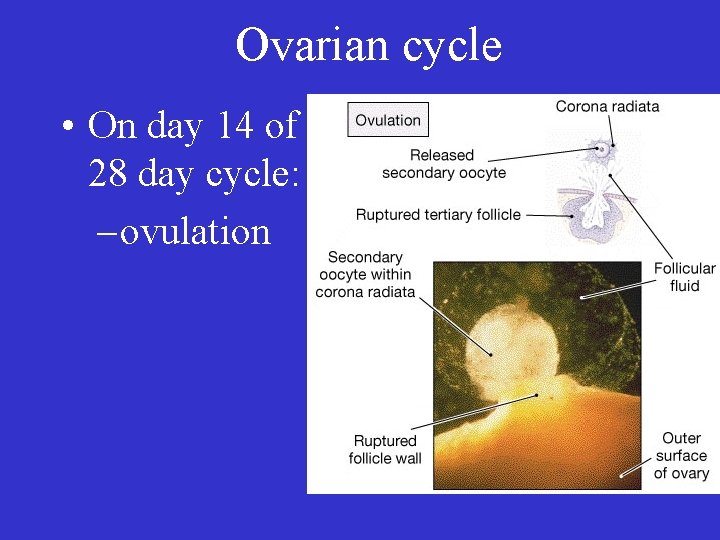
• Ovaries – each month one follicle matures – at ovulation: a mature follicle releases an ovum
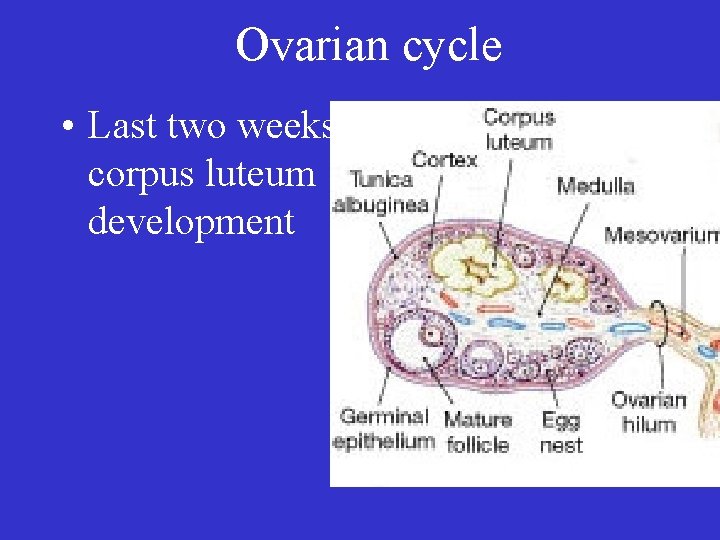
• Ovaries – hormones secreted include • estrogens • progestins (progesterone)
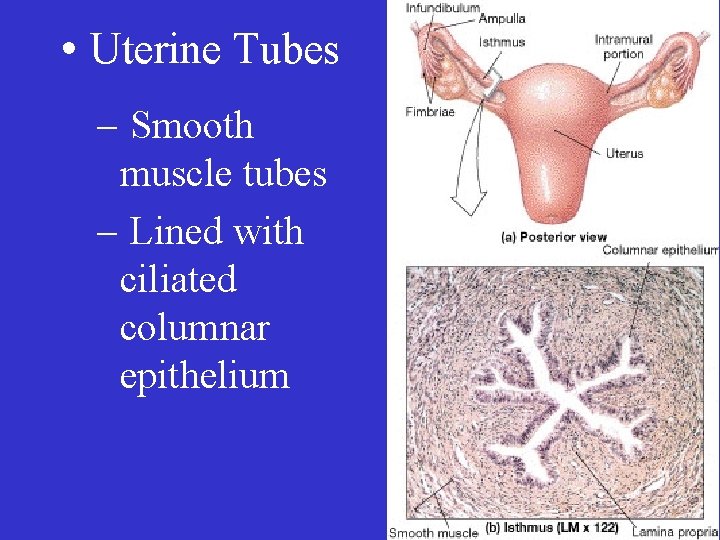
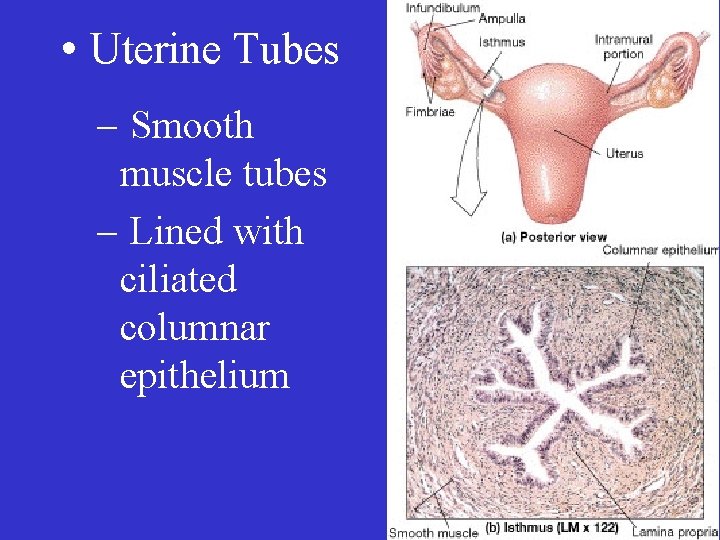
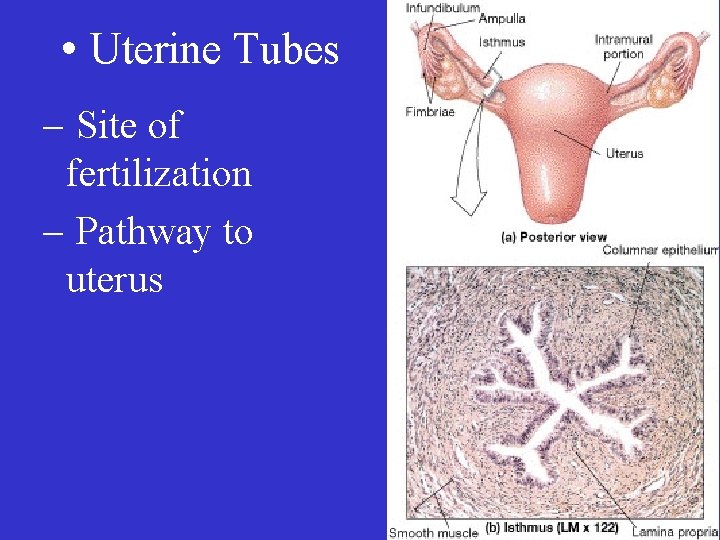
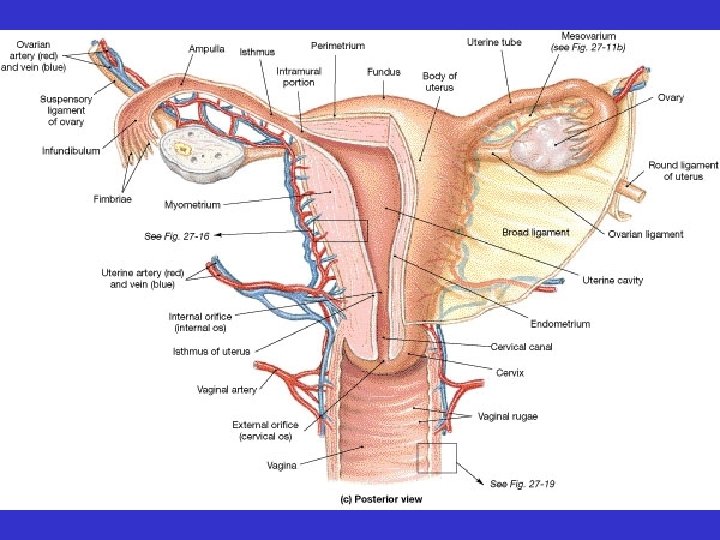
• Uterine Tubes – Smooth muscle tubes – Lined with ciliated columnar epithelium

• Uterine Tubes – Features: • infundibulum • frimbriae • ampulla
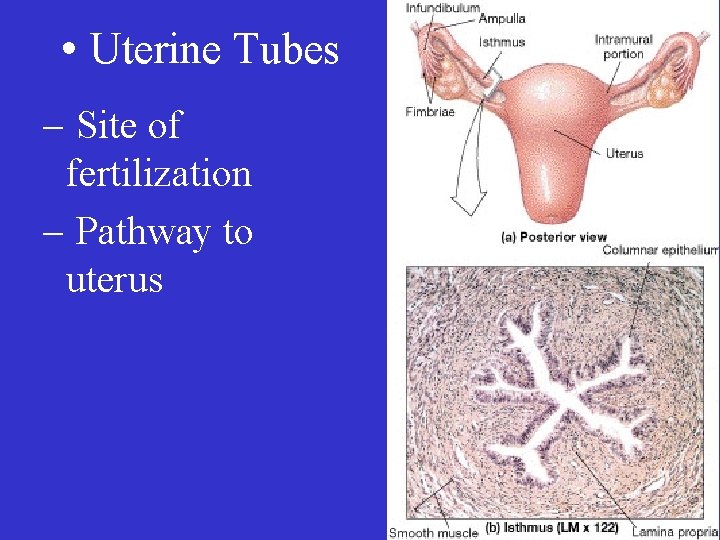
• Uterine Tubes – Site of fertilization – Pathway to uterus
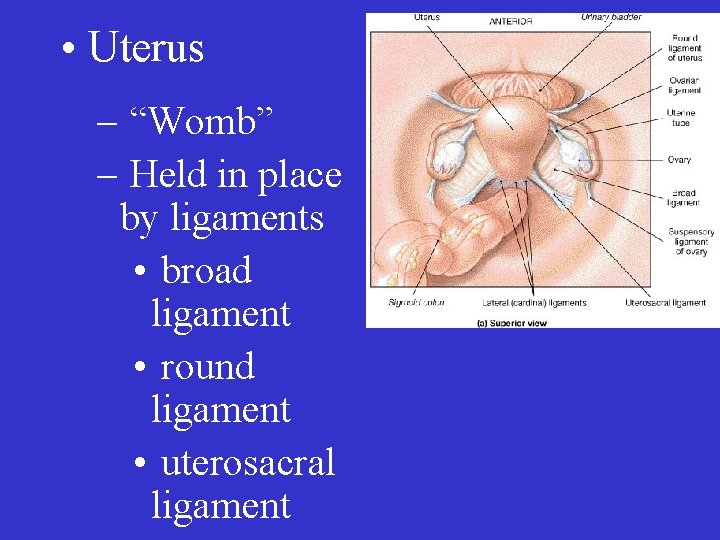
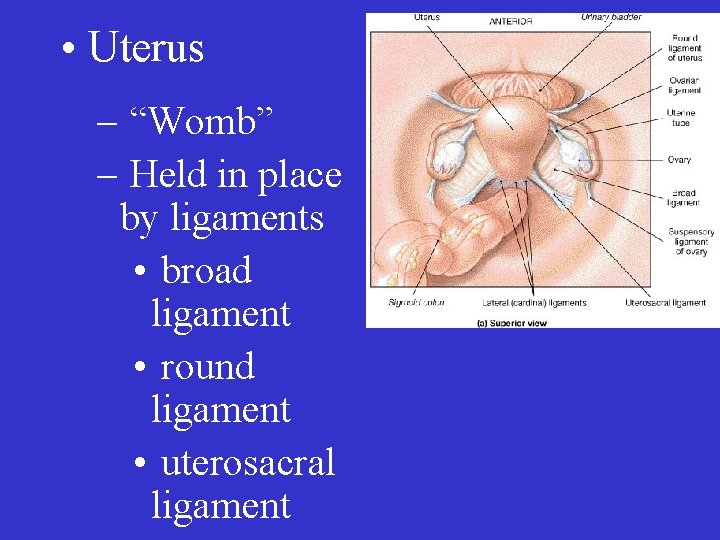
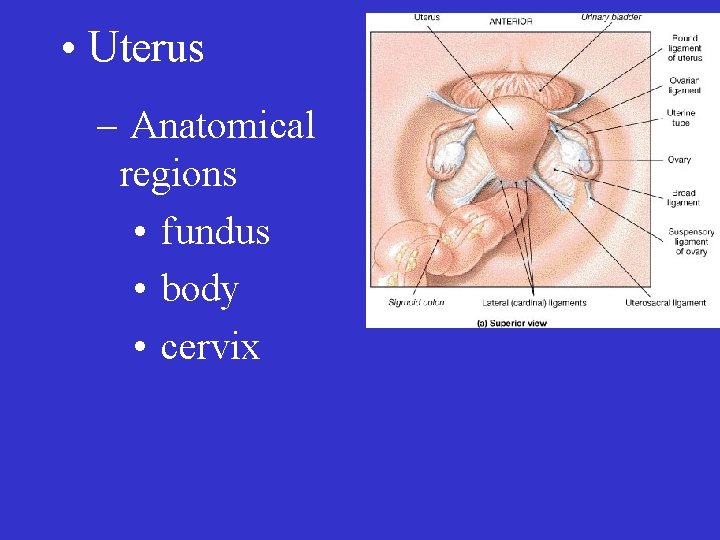
• Uterus – “Womb” – Held in place by ligaments • broad ligament • round ligament • uterosacral ligament

• Uterus – Site of • embryo implantation • embryo and fetal development • labor
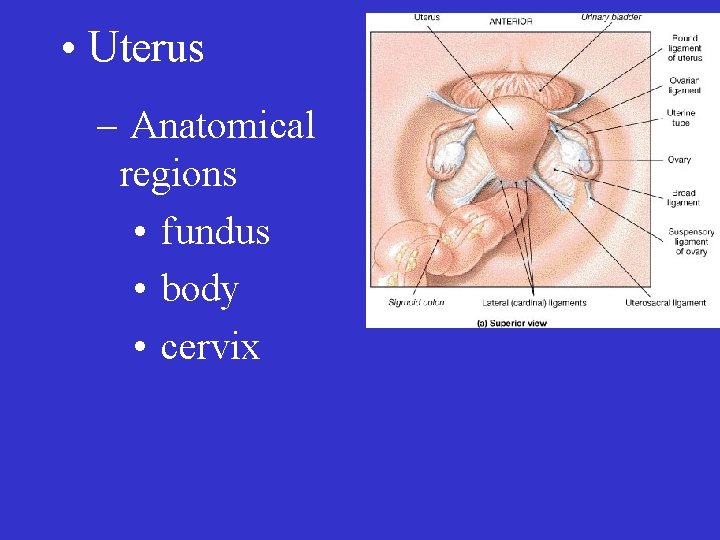
• Uterus – Anatomical regions • fundus • body • cervix
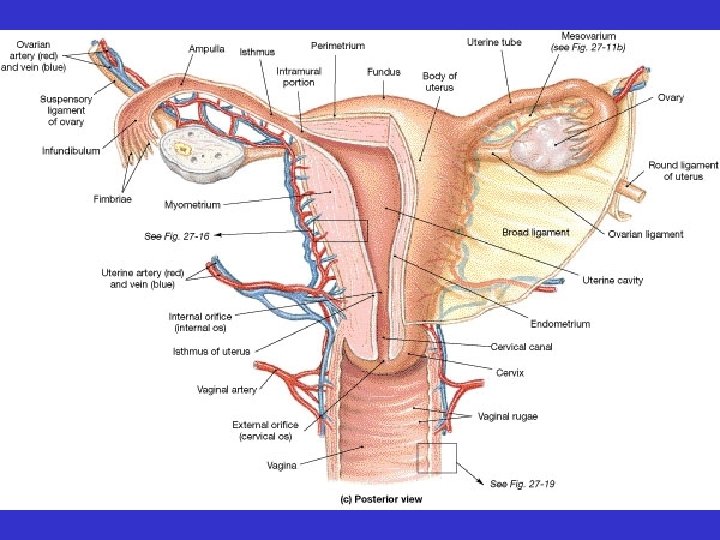
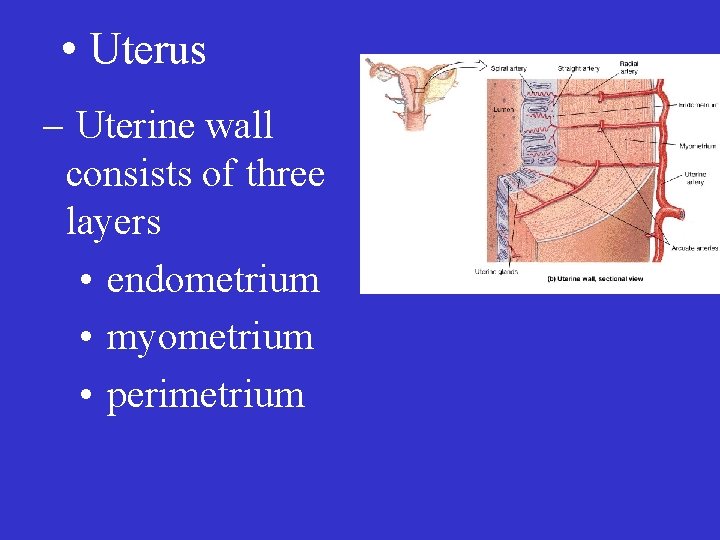
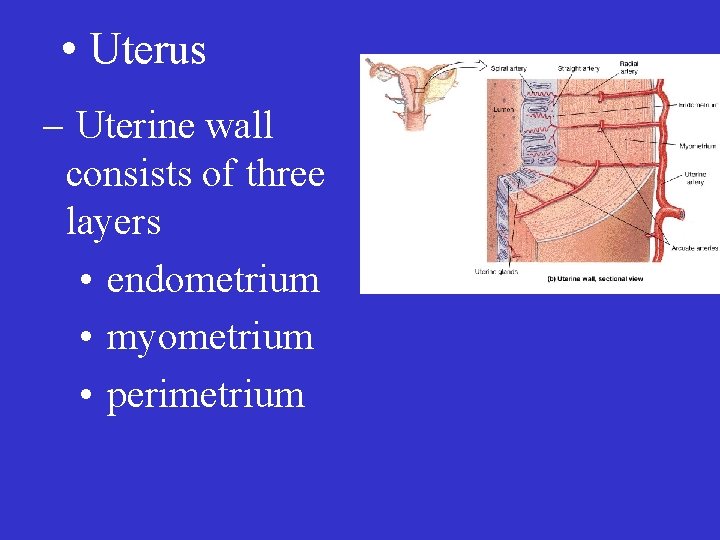
• Uterus – Uterine wall consists of three layers • endometrium • myometrium • perimetrium

• Uterus – Endometrium divided into • functional zone • basilar zone

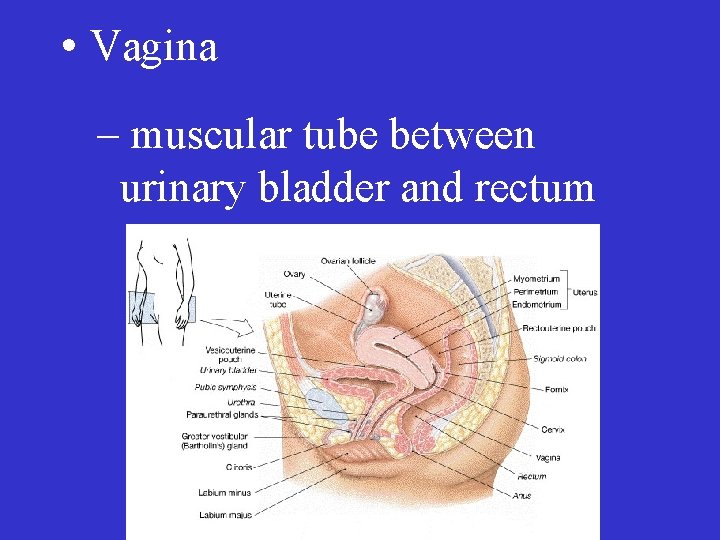
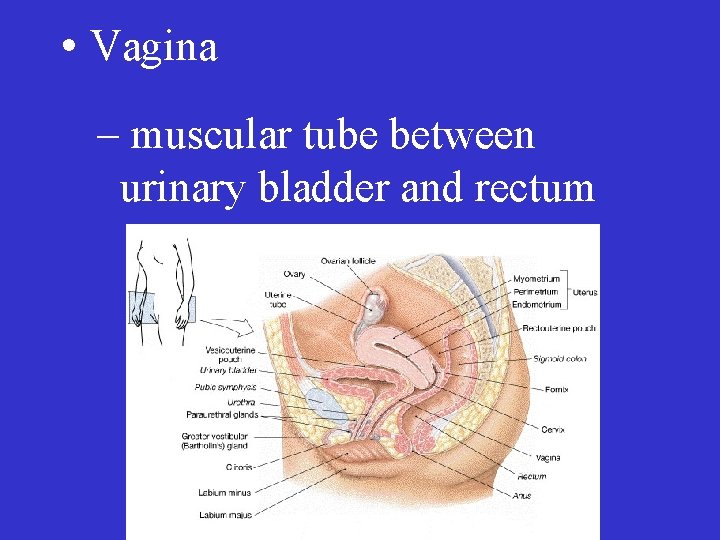
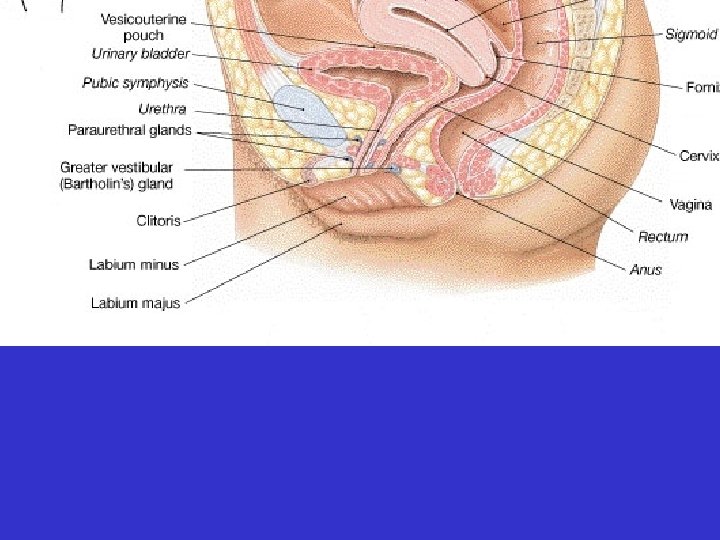
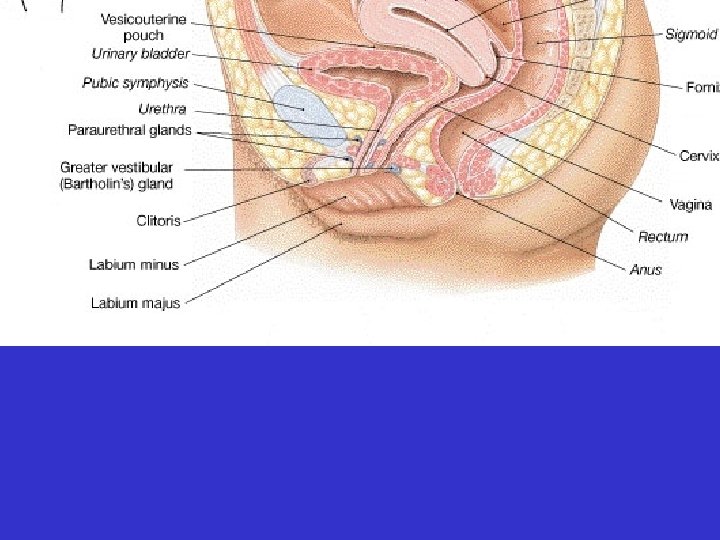
• Vagina – muscular tube between urinary bladder and rectum
• Vagina – pathway for sperm – pathway for menstrual flow – birth canal – vaginal opening may be partially covered by the hymen

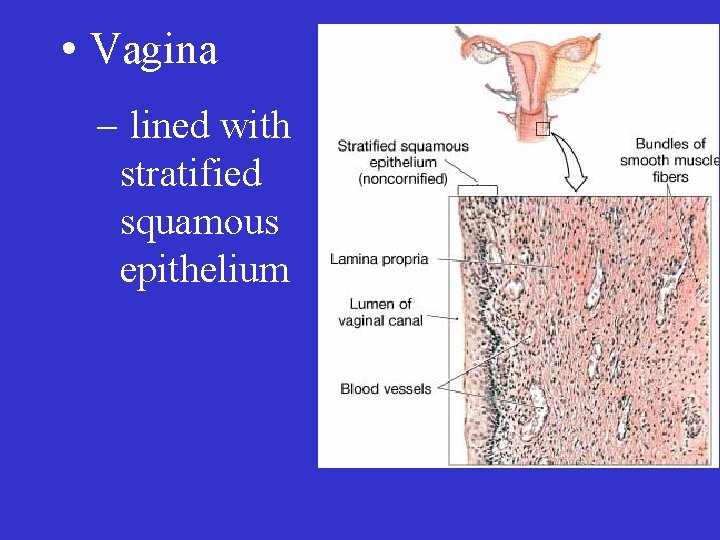
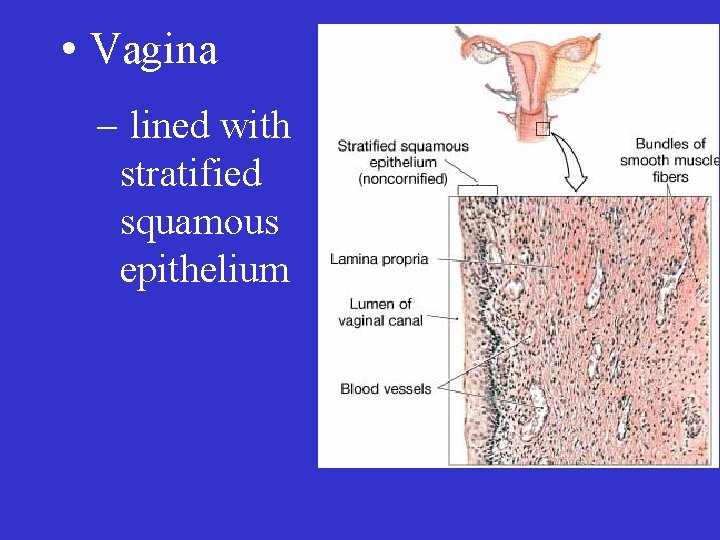
• Vagina – lined with stratified squamous epithelium
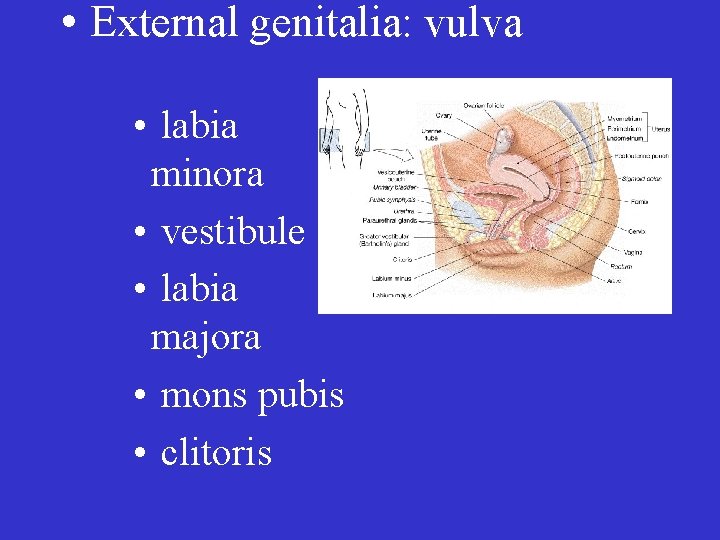
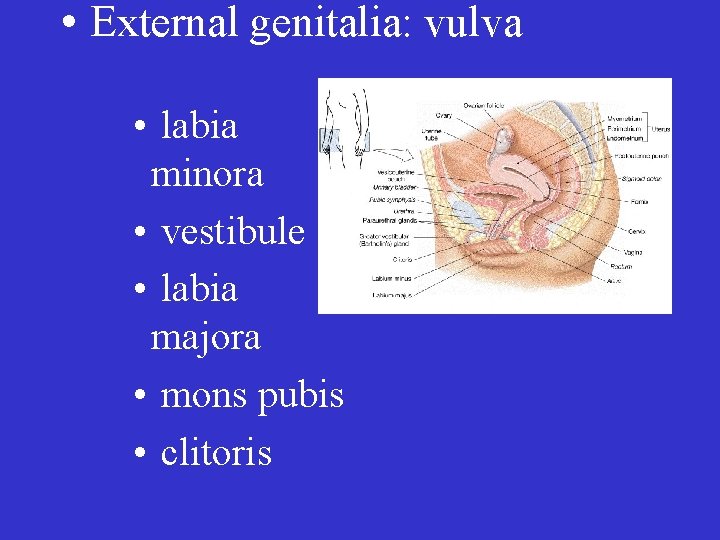
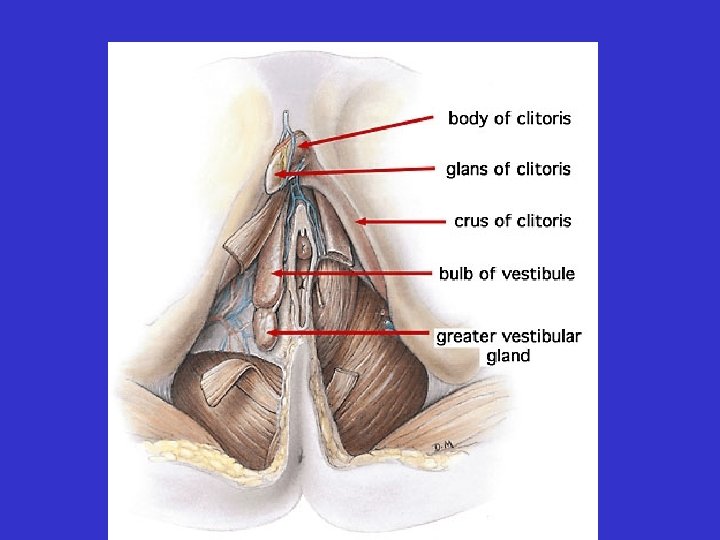
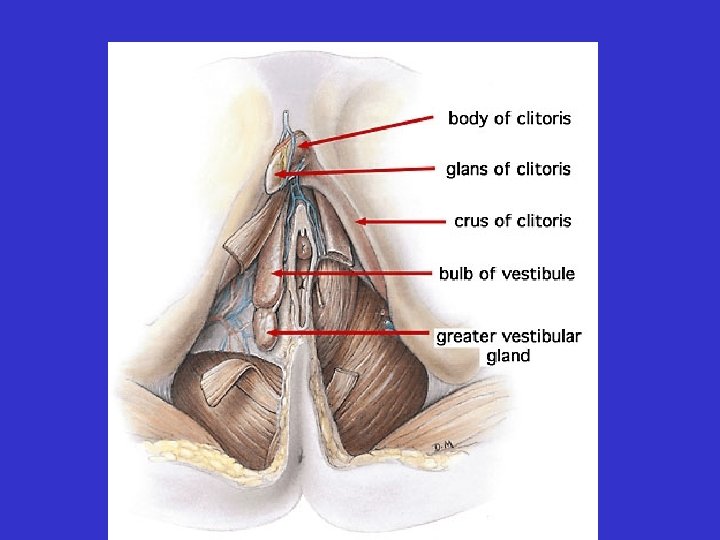
• External genitalia: vulva • labia minora • vestibule • labia majora • mons pubis • clitoris

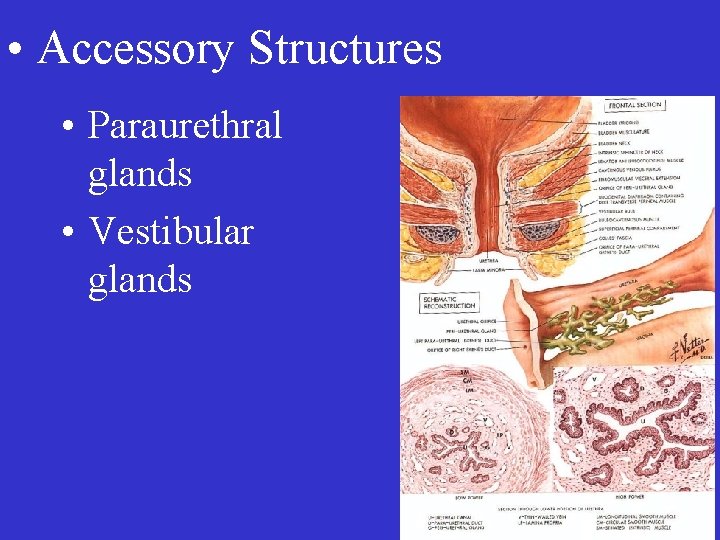
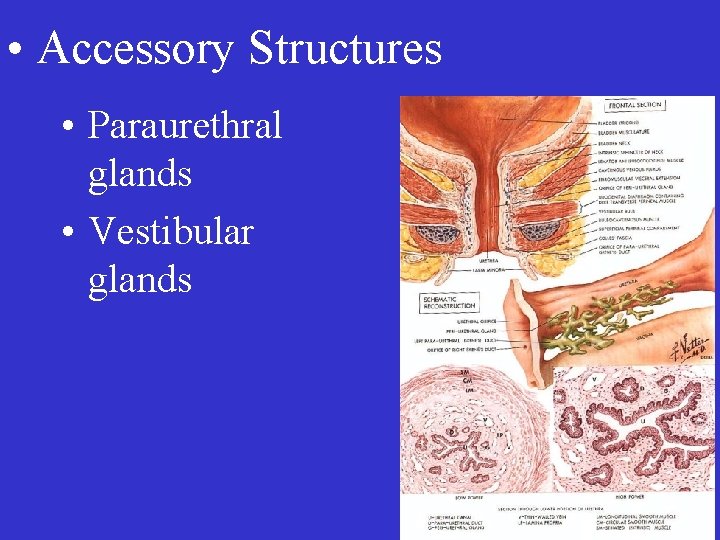
• Accessory Structures • Paraurethral glands • Vestibular glands
• Accessory Structures • Vestibular Bulb
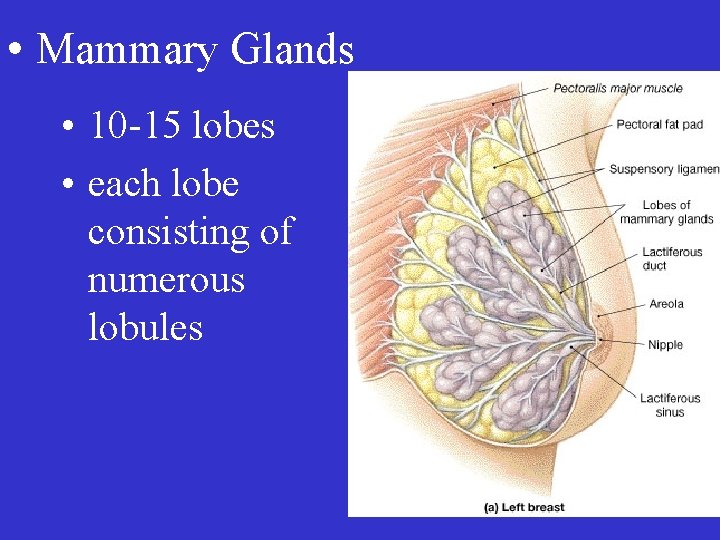
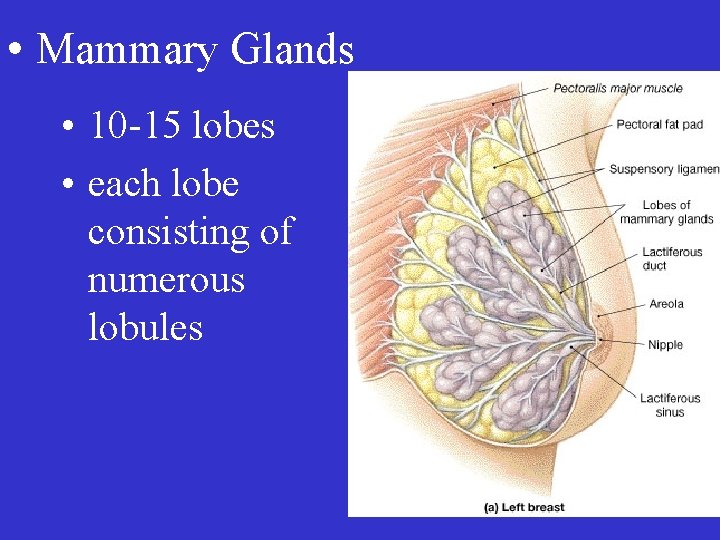
• Mammary Glands • 10 -15 lobes • each lobe consisting of numerous lobules
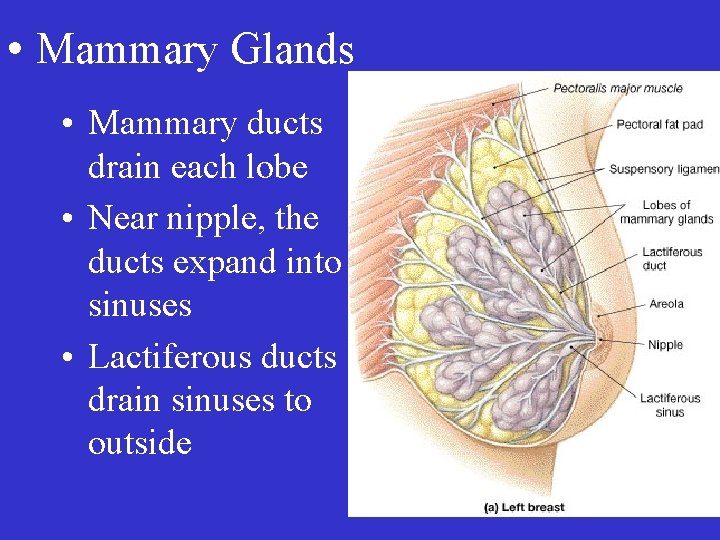
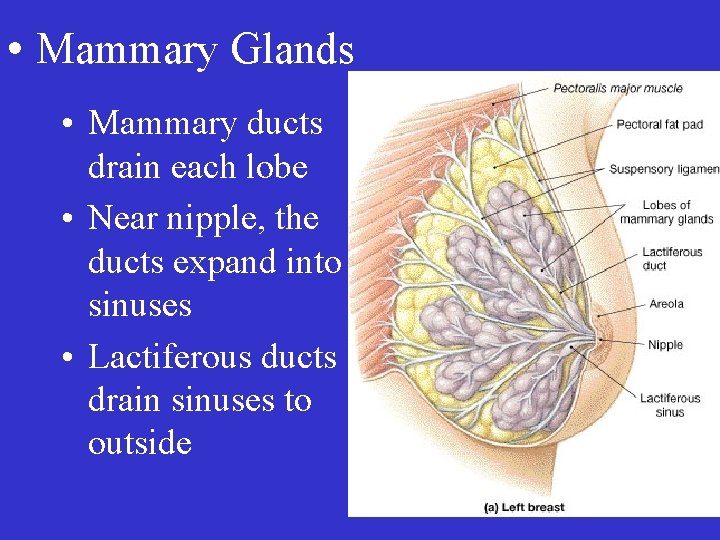
• Mammary Glands • Mammary ducts drain each lobe • Near nipple, the ducts expand into sinuses • Lactiferous ducts drain sinuses to outside

• Mammary Glands • Ducts and lobules associated with myoepithelial cells

• The breast is supported by numerous suspensory ligaments



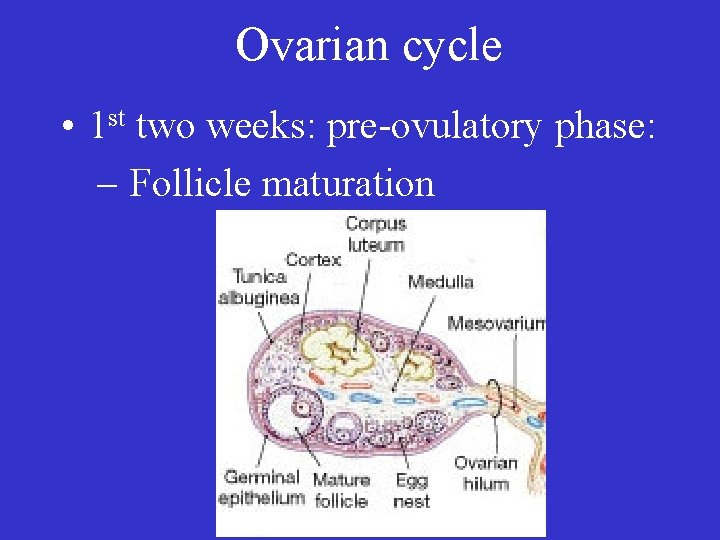
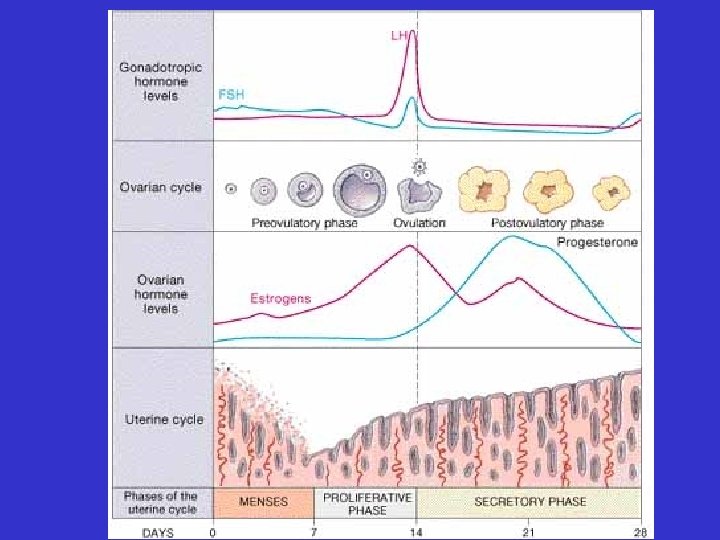
Ovarian cycle • 1 st two weeks: pre-ovulatory phase: – Follicle maturation

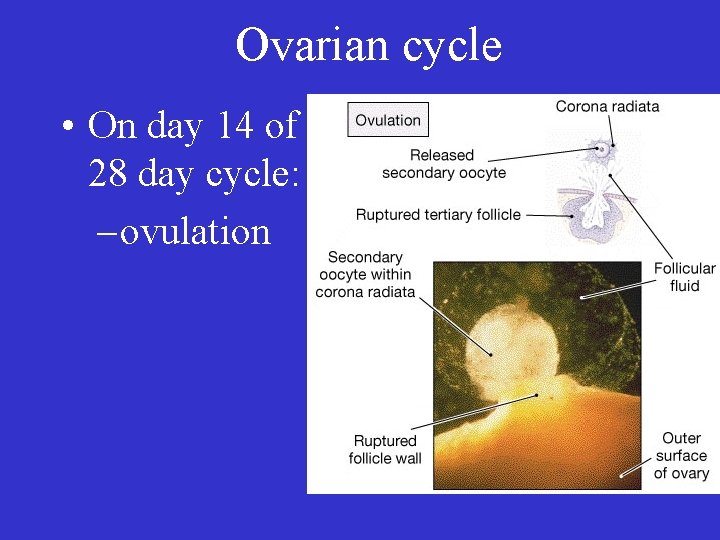
Ovarian cycle • On day 14 of a 28 day cycle: – ovulation

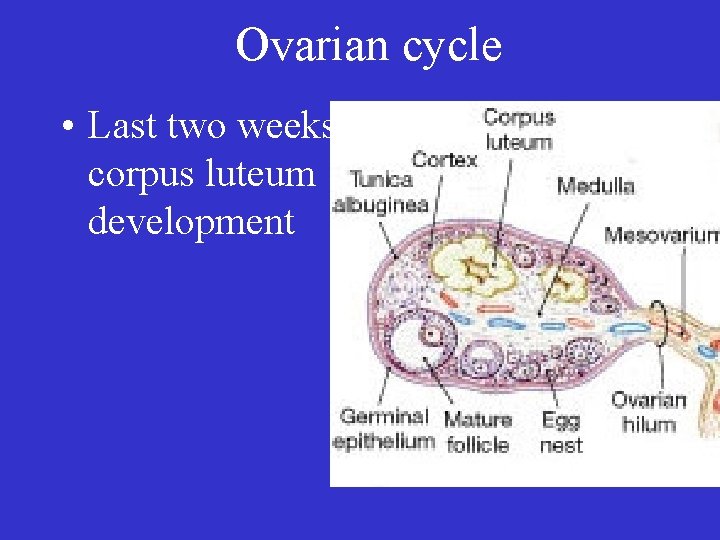
Ovarian cycle • Last two weeks: corpus luteum development
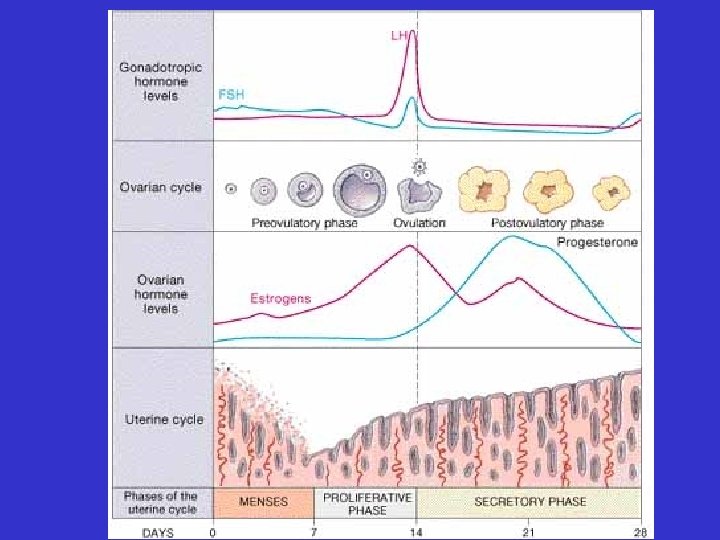
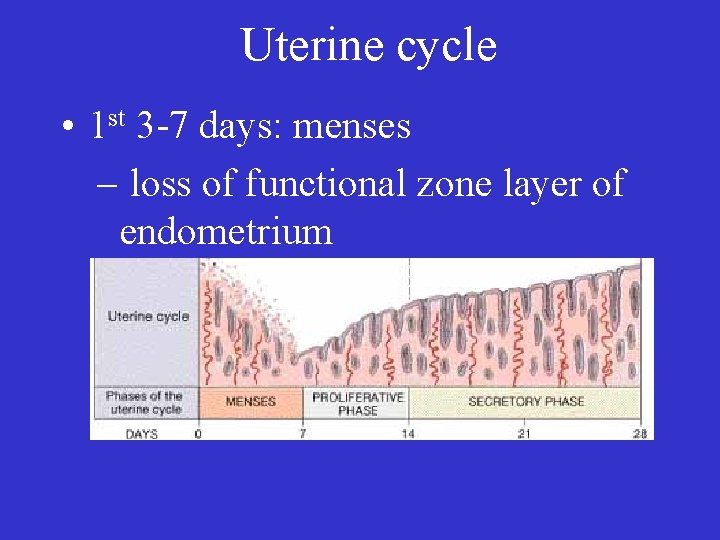
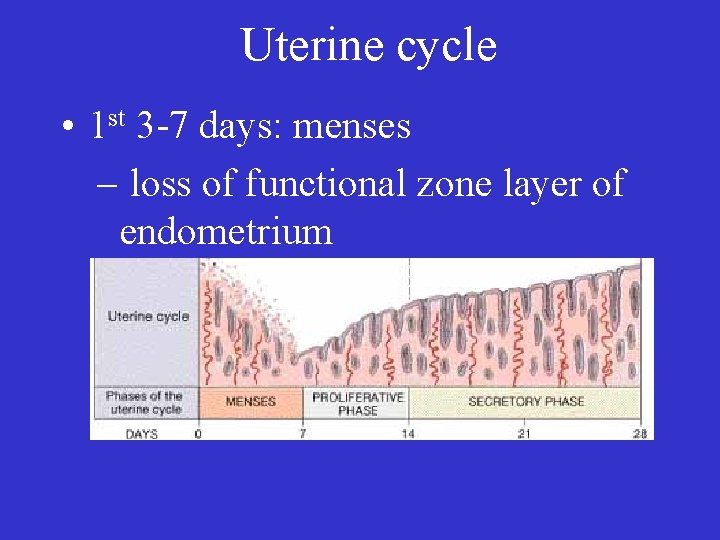
Uterine cycle • 1 st 3 -7 days: menses – loss of functional zone layer of endometrium

Uterine cycle • 2 nd week: proliferative phase – restoration of endometrial functional zone layer
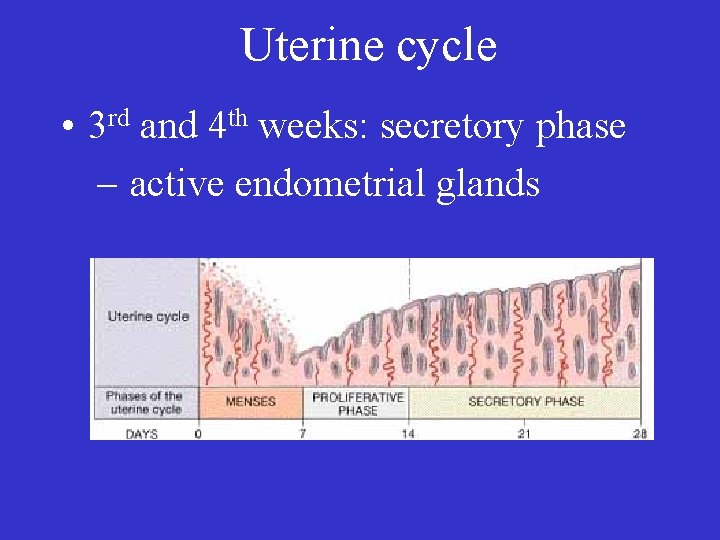
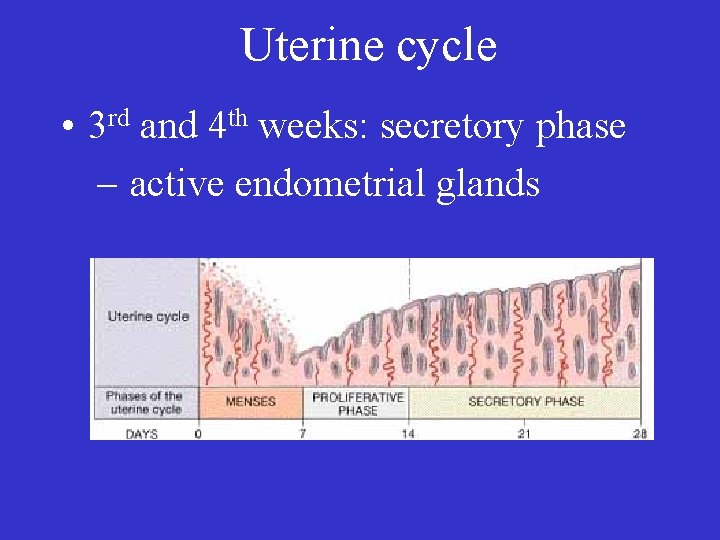
Uterine cycle • 3 rd and 4 th weeks: secretory phase – active endometrial glands
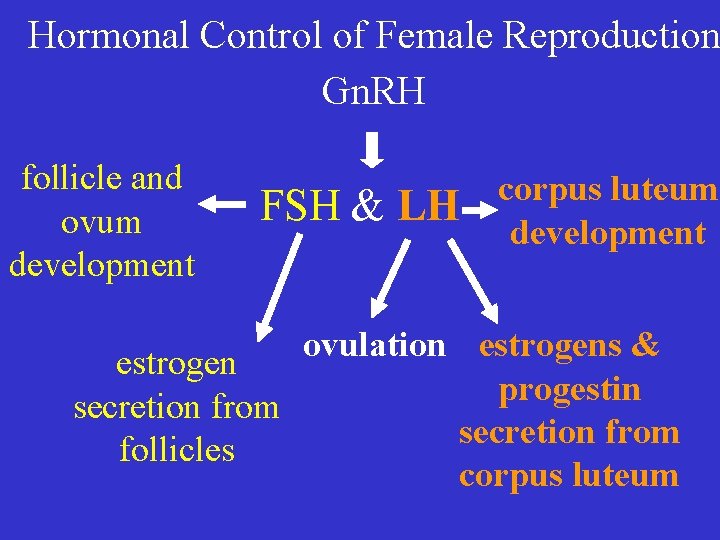
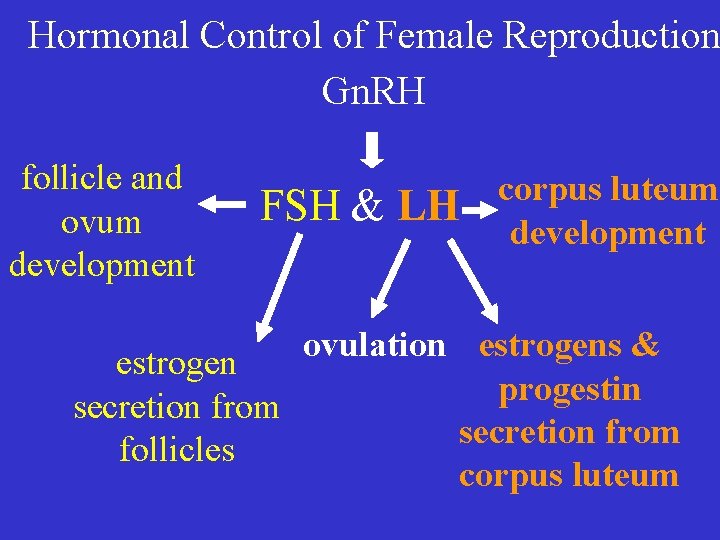
Hormonal Control of Female Reproduction Gn. RH follicle and ovum development FSH & LH corpus luteum development ovulation estrogens & estrogen progestin secretion from follicles corpus luteum
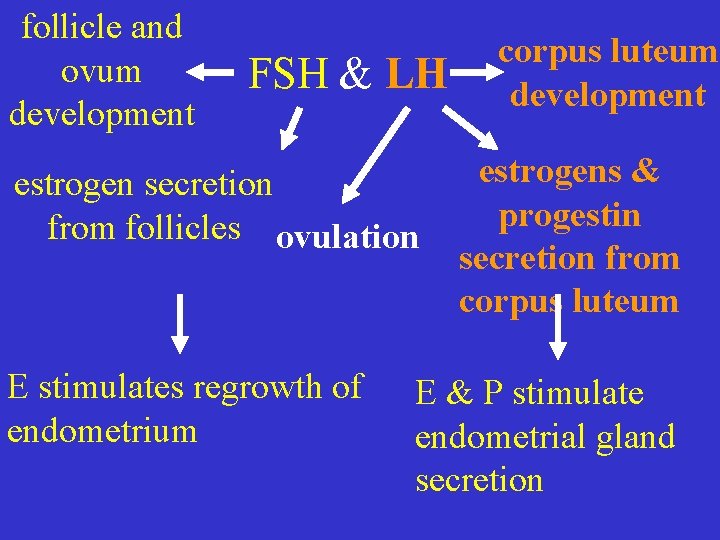
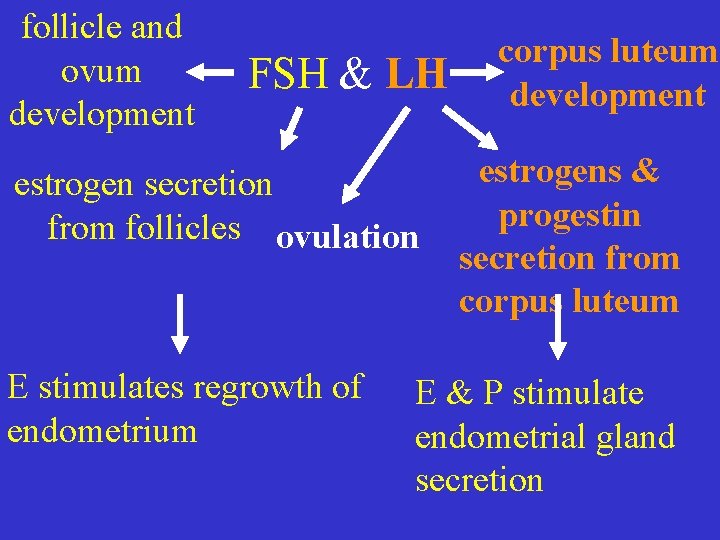
follicle and ovum development FSH & LH estrogen secretion from follicles ovulation E stimulates regrowth of endometrium corpus luteum development estrogens & progestin secretion from corpus luteum E & P stimulate endometrial gland secretion


• If (after two weeks) no pregnancy: – corpus luteum shuts down. – E & P secretion stops – endometrium loses hormonal support – menses begins
• If a successful fertilization occurs: – corpus luteum does not shut down. – E & P secretion continues – endometrium is maintained – pregnancy continues

• Why doesn’t the corpus luteum shut down if an early embryo is present?
• Other Functions of Estrogen – development, growth, & maintenance of female sex organs – bone and muscle growth – 2 o sex characteristics – libido
• General Function of Progestins – preparation of the body for pregnancy

Thank you ulnar nerve.
 Male reproductive organs
Male reproductive organs Uterus perimetrium
Uterus perimetrium Infindibulum
Infindibulum Reproductive organs of the bull
Reproductive organs of the bull Cows reproductive system
Cows reproductive system Function of reproductive organs
Function of reproductive organs Pearson education
Pearson education Women anatomy
Women anatomy Function of the vagina
Function of the vagina Male function
Male function Frog testis labeled
Frog testis labeled Exercise 42 review male reproductive system
Exercise 42 review male reproductive system Male reproductive system lateral view
Male reproductive system lateral view Function of fsh
Function of fsh Parts of male and female reproductive system
Parts of male and female reproductive system Reproductive physiology
Reproductive physiology Human reproductive system
Human reproductive system Art-labeling activity: the male reproductive system, part 1
Art-labeling activity: the male reproductive system, part 1 Male reproductive system information
Male reproductive system information Where is the sperm stored
Where is the sperm stored Bull reproductive system parts and functions
Bull reproductive system parts and functions Where is the prostate
Where is the prostate Male reproductive system plants
Male reproductive system plants Function of male reproductive system
Function of male reproductive system Is croaker a cartilaginous fish
Is croaker a cartilaginous fish In pila fertilization
In pila fertilization Urogenital papilla fetal pig
Urogenital papilla fetal pig Male plant reproductive system
Male plant reproductive system Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Base of prostate gland
Base of prostate gland Lesson 20.2 the male reproductive system
Lesson 20.2 the male reproductive system Pearson
Pearson Colon function in male reproductive system
Colon function in male reproductive system Figure 16-1 male reproductive system
Figure 16-1 male reproductive system Differences between male and female reproductive organ
Differences between male and female reproductive organ Male reproductive system labeled
Male reproductive system labeled Pathway of semen
Pathway of semen Drawing of the male and female reproductive system
Drawing of the male and female reproductive system Male plant reproductive system
Male plant reproductive system Reproductive system summary
Reproductive system summary Layers of scrotum anatomy
Layers of scrotum anatomy Penile urethra
Penile urethra Oogenesis diagram
Oogenesis diagram Path of male reproductive system
Path of male reproductive system Uterine orifice
Uterine orifice Basic animal reproduction crossword
Basic animal reproduction crossword Chapter 16 lesson 2 the male reproductive system
Chapter 16 lesson 2 the male reproductive system Figure 16-1 is a sagittal view of the male reproductive
Figure 16-1 is a sagittal view of the male reproductive Male reproductive system side view
Male reproductive system side view Reproductive system
Reproductive system Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Figure 16-2 is a longitudinal section of a testis
Figure 16-2 is a longitudinal section of a testis Folliculogenesis
Folliculogenesis Male reproductive system table
Male reproductive system table Male reproductive system
Male reproductive system Lesson 2 the male reproductive system
Lesson 2 the male reproductive system Cylindrical pendant organ located anterior to the scrotum
Cylindrical pendant organ located anterior to the scrotum What is reproductive system
What is reproductive system Prostatic utricle
Prostatic utricle Cylindrical pendant organ located anterior to the scrotum
Cylindrical pendant organ located anterior to the scrotum Male reproductive system
Male reproductive system Asexual reproduction cell division
Asexual reproduction cell division Asexualk
Asexualk Sexual asexual venn diagram
Sexual asexual venn diagram Glans penis
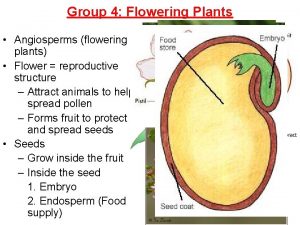
Glans penis Angiosperm with one seed leaf
Angiosperm with one seed leaf What is gonads
What is gonads Gonad of a squid
Gonad of a squid Gonads glands
Gonads glands What is gonads
What is gonads Ovary sympathetic innervation
Ovary sympathetic innervation Path of sperm
Path of sperm Monads and gonads
Monads and gonads Endocrine molecules
Endocrine molecules Thyroid
Thyroid Gonads
Gonads Define gametogenesis
Define gametogenesis Emerchandise
Emerchandise Female reproductive ducts
Female reproductive ducts Endocrine system and reproductive system
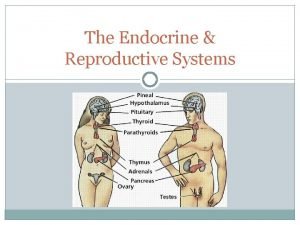
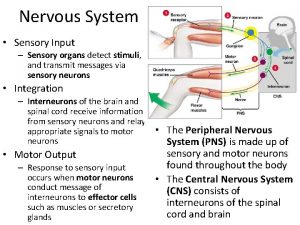
Endocrine system and reproductive system Sensory system organs
Sensory system organs What is the main function of the excretory system
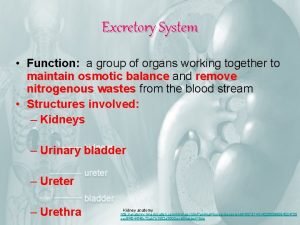
What is the main function of the excretory system Figure 14-1 digestive system
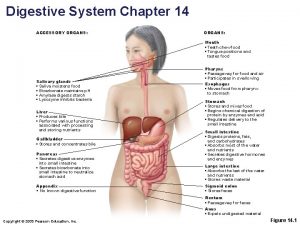
Figure 14-1 digestive system Accessory organs of the digestive system
Accessory organs of the digestive system Accessory organs
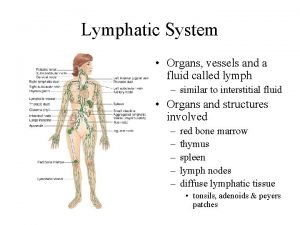
Accessory organs Lymph tissue fluid
Lymph tissue fluid Formation of lymph
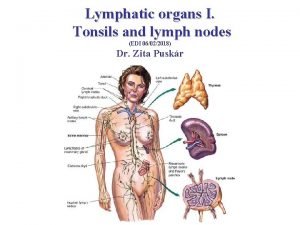
Formation of lymph Lingual tonsil
Lingual tonsil Lymphatic system organs and functions
Lymphatic system organs and functions Organs of the sensory system
Organs of the sensory system Which organs are involved in respiratory system
Which organs are involved in respiratory system Chapter 13 respiratory system
Chapter 13 respiratory system Chapter 16 matching questions 20-24
Chapter 16 matching questions 20-24 Female reproductive system with baby
Female reproductive system with baby The reproductive system chapter 16
The reproductive system chapter 16 Female anatomy diagram
Female anatomy diagram Female reproductive system pregnancy
Female reproductive system pregnancy Epidiymitis
Epidiymitis Reproductive system jeopardy
Reproductive system jeopardy Graham munson
Graham munson Poultry reproductive system
Poultry reproductive system Poultry reproductive system
Poultry reproductive system Unit 5 lesson 3 the female reproductive system
Unit 5 lesson 3 the female reproductive system Ovary diagram
Ovary diagram Female reproductive system functions
Female reproductive system functions Peristomium in earthworm
Peristomium in earthworm Claspers are structures involved in:
Claspers are structures involved in: How to care reproductive system
How to care reproductive system Chapter 21 reproductive system review questions
Chapter 21 reproductive system review questions Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 16 the reproductive system figure 16-2
Chapter 16 the reproductive system figure 16-2 Chapter 16 the reproductive system answer key
Chapter 16 the reproductive system answer key Medical terminology chapter 14 labeling exercises
Medical terminology chapter 14 labeling exercises Female cow reproductive system
Female cow reproductive system Reptilian reproductive system
Reptilian reproductive system Reproductive system objectives
Reproductive system objectives Picture of the urethra
Picture of the urethra Oogenesis
Oogenesis Puberty meaning
Puberty meaning Female reproductive system diagram
Female reproductive system diagram Lesson 3 the female reproductive system
Lesson 3 the female reproductive system Female reproductive system colour
Female reproductive system colour Female anatomy diagram
Female anatomy diagram