THE REPRODUCTIVE SYSTEM Primary Sex Organs Gonads are












- Slides: 39
THE REPRODUCTIVE SYSTEM
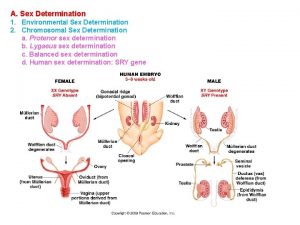
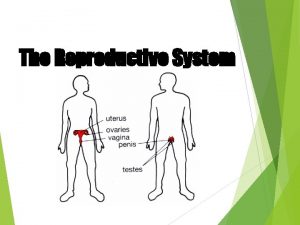
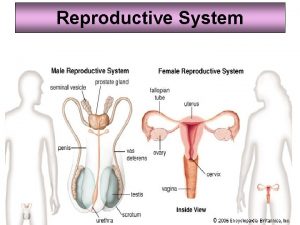
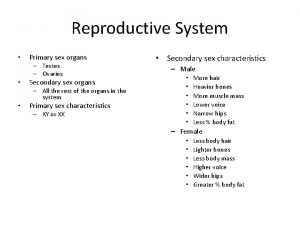
Primary Sex Organs � � Gonads are the primary sex organs of both male and female: �Testes – male gonads �Ovaries – female gonads Gonads secrete sex hormones and produce sex cells (gametes – egg or sperm)
Role of Reproduction � � � Reproductive role of male is to manufacture sperm and deliver it to the female reproductive tract. Reproductive role of female is to produce ova (eggs). Fertilization is the union of egg and sperm to form a zygote, which will develop into an embryo and later into a fetus.
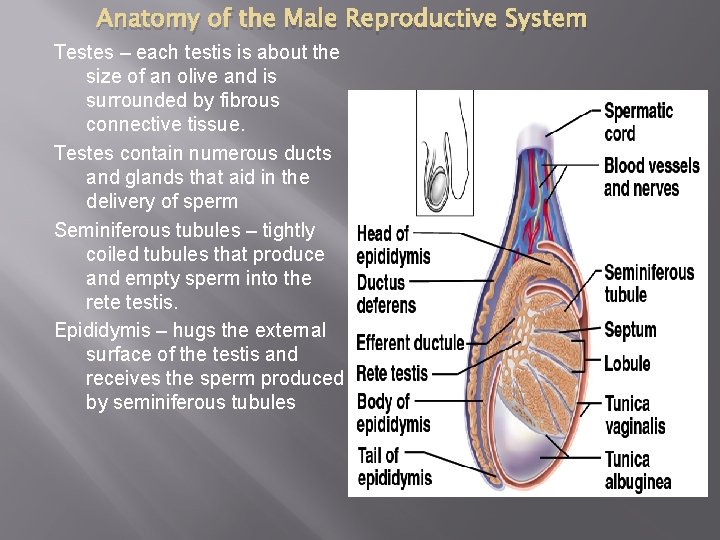
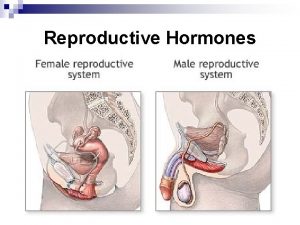
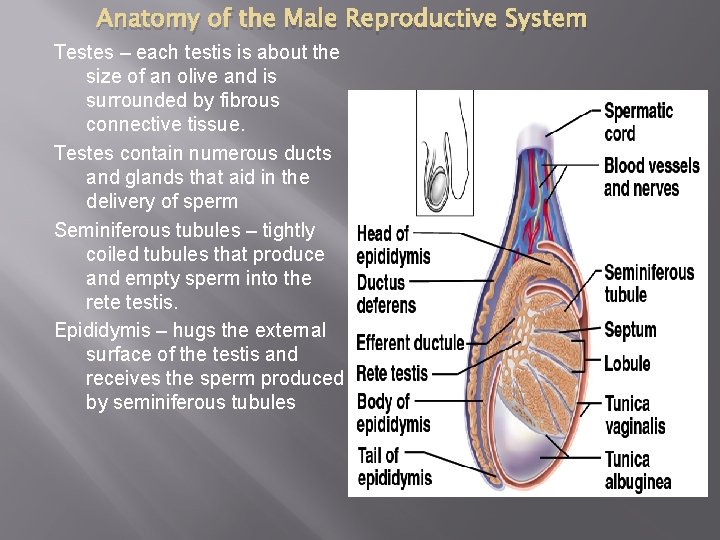
Anatomy of the Male Reproductive System Testes – each testis is about the size of an olive and is surrounded by fibrous connective tissue. Testes contain numerous ducts and glands that aid in the delivery of sperm Seminiferous tubules – tightly coiled tubules that produce and empty sperm into the rete testis. Epididymis – hugs the external surface of the testis and receives the sperm produced by seminiferous tubules

Duct System � � � Epididymis - a comma-shaped, highly coiled tube about 20 feet long that sits atop the superior part of the testis and receives the sperm produced by seminiferous tubules. Sperm mature and gain the ability to swim as they make their way through the epididymis (takes about 20 days) When sexually stimulated, walls of the epididymis contract to expel sperm into the vas deferens (ductus deferens)
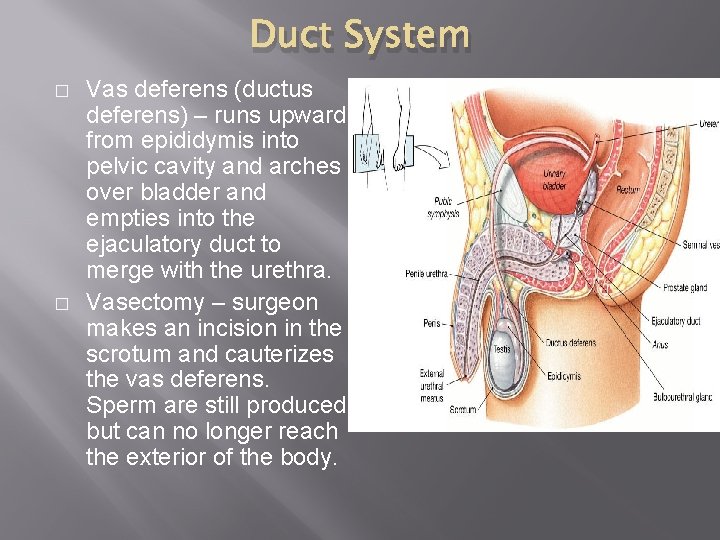
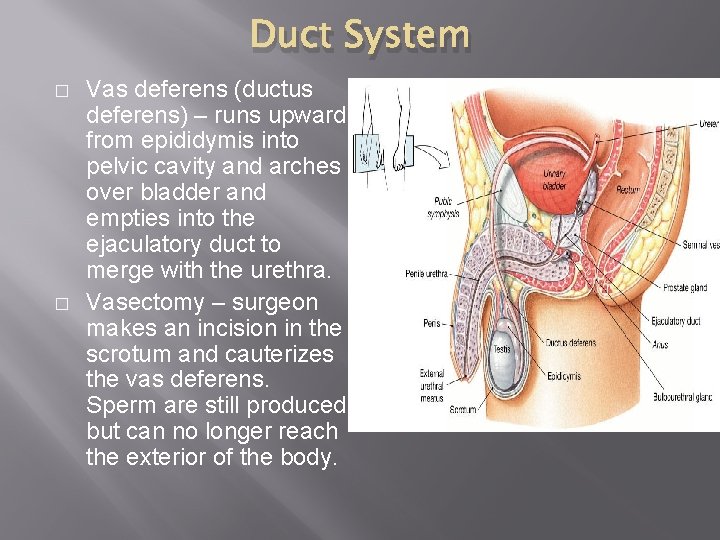
Duct System � � Vas deferens (ductus deferens) – runs upward from epididymis into pelvic cavity and arches over bladder and empties into the ejaculatory duct to merge with the urethra. Vasectomy – surgeon makes an incision in the scrotum and cauterizes the vas deferens. Sperm are still produced but can no longer reach the exterior of the body.
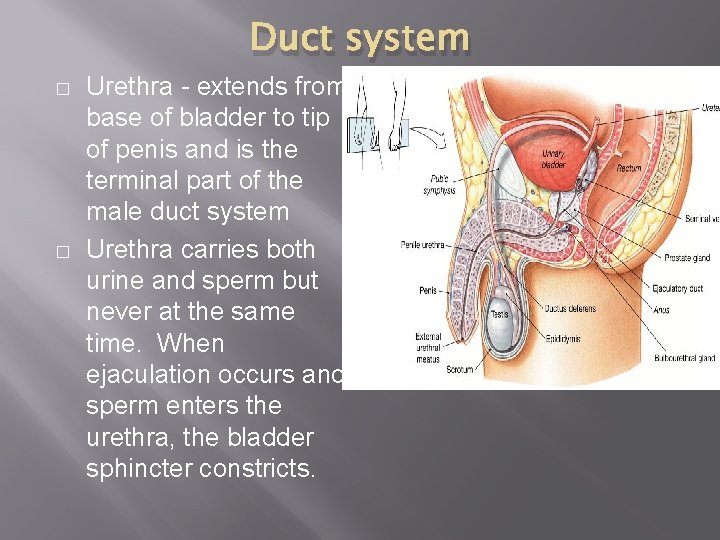
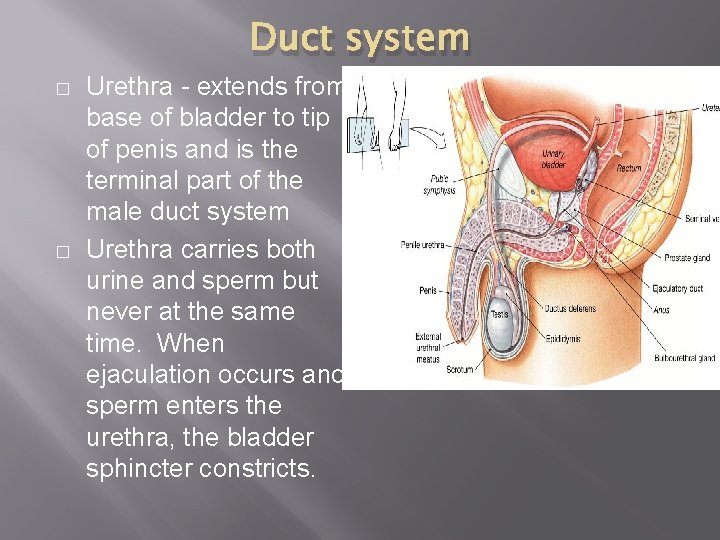
Duct system � � Urethra - extends from base of bladder to tip of penis and is the terminal part of the male duct system Urethra carries both urine and sperm but never at the same time. When ejaculation occurs and sperm enters the urethra, the bladder sphincter constricts.
Accessory Glands 1. Seminal Vesicles – located at base of bladder, produce most of the fluid volume of semen. Fluid is rich in fructose, vitamin C, and prostaglandins. The duct of each seminal vesicle joins that of the vas deferens on the same side to form the ejaculatory duct. (So sperm and seminal fluid enter the urethra together during ejaculation)

Accessory Glands 2. Prostate Gland - single gland that encircles the upper part of the urethra just below the bladder. Secretion is a milky fluid that helps to activate sperm. The prostate can be palpated by digital examination of rectum. � Almost every elderly man experiences enlargement (hypertrophy) of the prostate – this can strangle the urethra and make urination difficult
Accessory Glands 3. Bulbourethral Glands – pea-sized glands inferior to prostate gland; produce a thick, clear mucus that drains into urethra �This secretion is the first to pass down the urethra during sexual excitement cleanses urethra of acidic urine and acts as a lubricant during intercourse
Semen � � � Milky white mixture of sperm and accessory gland secretions Provides a transport medium and nutrients for sperm p. H = 7. 2 – 7. 6 which helps neutralize acidity of vagina 2 -5 ml in typical ejaculation which contains between 50 – 130 million sperm in each milliliter Sperm count lower than 20 million per ml = infertility
Male external genitalia 1. Scrotum - divided sac of skin that hangs outside abdominal cavity at the root of penis � Viable sperm cannot be produced at normal body temperature so scrotum hangs loosely outside of body and provides a temperature about 3 C lower than body temp. � Testes are pulled closer to body when external temperatures are very low.
Male external genitalia 2. Penis – designed to deliver sperm into female reproductive tract � shaft – makes up majority of penis � glans penis – enlarged tip of the shaft � prepuce (foreskin) – cuff of skin around proximal end of the glans penis (removed during circumcision) � erectile tissue – spongy tissue that fills with blood during sexual excitement causes penis to enlarge and become rigid (erection)


Spermatogenesis – production of sperm � A man makes millions of sperm each day � There are 3 regions of a mature sperm: v Head – contains DNA v Midpiece – contain mitochondria ATP v Tail – means of propelling itself Acrosome – helmetlike structure anterior to head – breaks down and releases enzymes as sperm approaches egg. Enzymes help sperm penetrate egg �

Testosterone � � � Most important hormone of testes. Once puberty hits, testosterone is produced continuously for rest of life Rising levels of testosterone stimulate reproductive organs to develop to adult size, underlies sex drive and causes secondary sex characteristics to appear Deepening of voice Increased hair growth (facial, axillary, pubic) Skeletal muscles enlarge Bones thicken
Anatomy of the Female Reproductive System � � More complex role than of males. A female must be able to produce female gametes (ova) and nuture and protect a developing fetus for 9 months Ovaries – paired structures the size and shape of almonds � Many ovarian follicles, each of which consists of an immature egg or oocyte � Oocyte matures and is ejected from ovary in a event called ovulation

Female Duct System 1. Uterine Tubes (Fallopian Tubes) – receive the ovulated oocyte and provide a site of fertilization � Each fallopian tube is about 10 cm long and extends from an ovary to superior part of the uterus � There is no direct connection between fallopian tubes and ovary. The distal end of fallopian tube expands and has fingerlike projections which sweep oocyte into fallopian tube. � The journey to the uterus takes 3 -4 days and if viable for up to 24 hours after ovulation

Female Duct System 2. Uterus – located between bladder and rectum, the uterus is hollow that functions to receive, retain, an nourish a fertilized egg. � normally, about size of a pear � made up of body, fundus (superior rounded region), and cervix (outlet to the vagina) � 3 layers of mucosa line walls of uterus Endometrium – inner layer; provides soft place in which embryo to develop Myometrium – middle layer; contracts to force baby out during labor Perimetrium – outermost layer of uterus (deepest layer)

Female Duct System 3. Vagina – thin-walled tube 8 – 10 cm long; lies between the bladder and rectum and extends from cervix to exterior of body. provides a passageway for menstruation and for delivery of infant • female organ of copulation • Hymen – thin fold of mucosa that partially closes vaginal opening; very vascular and tends to bleed during first intercourse •

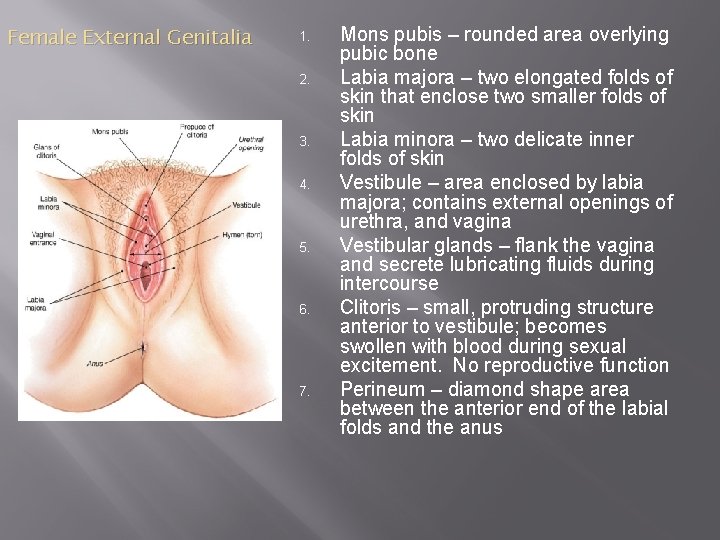
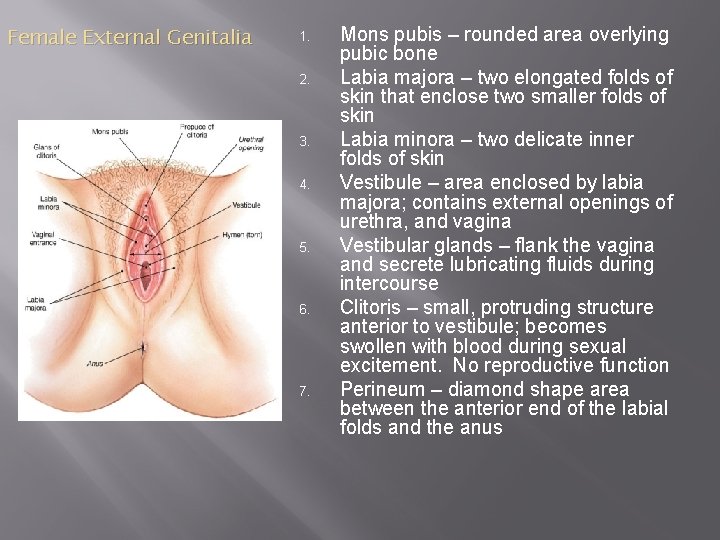
Female External Genitalia 1. 2. 3. 4. 5. 6. 7. Mons pubis – rounded area overlying pubic bone Labia majora – two elongated folds of skin that enclose two smaller folds of skin Labia minora – two delicate inner folds of skin Vestibule – area enclosed by labia majora; contains external openings of urethra, and vagina Vestibular glands – flank the vagina and secrete lubricating fluids during intercourse Clitoris – small, protruding structure anterior to vestibule; becomes swollen with blood during sexual excitement. No reproductive function Perineum – diamond shape area between the anterior end of the labial folds and the anus
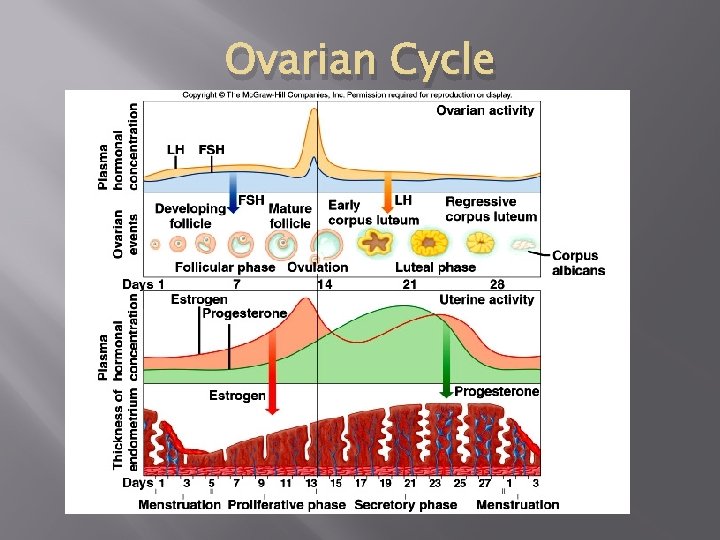
The Ovarian Cycle � � � At birth, the female has all the primary oocytes she will ever have (~ 2 million) They remain as primary oocytes until puberty hits (~ 10 -14 years) A mature egg develops and is released (ovulated) from one of the two ovaries about once every 28 days. If the egg is not fertilized, the endometrium of the uterus breaks down and is shed as menstrual fluid. Four stages to Ovarian Cycle:
1. Follicle Stage � � � At puberty, the anterior pituitary gland releases Follicle Stimulating Hormone (FSH) and a small number of primary follicles begin to mature each month – only one matures per month As this follicle grows, it fills with estrogen which stimulates the endometrium to thicken in preparation for implantation of an embryo should the egg be fertilized Follicle stage lasts for about 10 days
2. Ovulation Stage � � � Increasing estrogen levels cause the pituitary to stop secreting FSH and start secreting Luteinizing Hormone (LH) Around day 14 of the menstrual cycle, the combination of estrogen, FSH, LH in the blood stream stimulates the mature follicle to rupture and release a mature oocyte (egg cell) This event is called ovulation.

3. Corpus Luteum Stage � � � After ovulation, LH stimulates the cells of the ruptured follicle to divide and develop into a mass of reddish-yellow cells called the corpus luteum. Progesterone is secreted by the corpus luteum and helps to maintain the thickening of the endometrium (should fertilization occur). This stage lasts about 14 days.
4. Menstruation Stage � � � If fertilization does not take place, the corpus luteum breaks down which causes a decrease in progesterone levels. The lining of the endometrium becomes progressively thinner and eventually breaks down. The extra layers of the endometrium, the unfertilized egg, and blood that results when the endometrium pulls away from the uterus are discharged through the vagina. This menstruation stage begins around day 28 of the cycle and lasts 3 -7 days. While this is occurring, estrogen levels decrease and the anterior pituitary secretes FSH which stimulates the growth of a new follicle and the cycle begins again.

Estrogens � Cause appearance of secondary sex characteristics in females at puberty �Enlargement of the accessory organs of female reproductive system �Development of breasts �Axillary and pubic hair �Increased deposits of fats in hip and breast area �Widening of pelvis �Onset of menses (menstrual cycle)
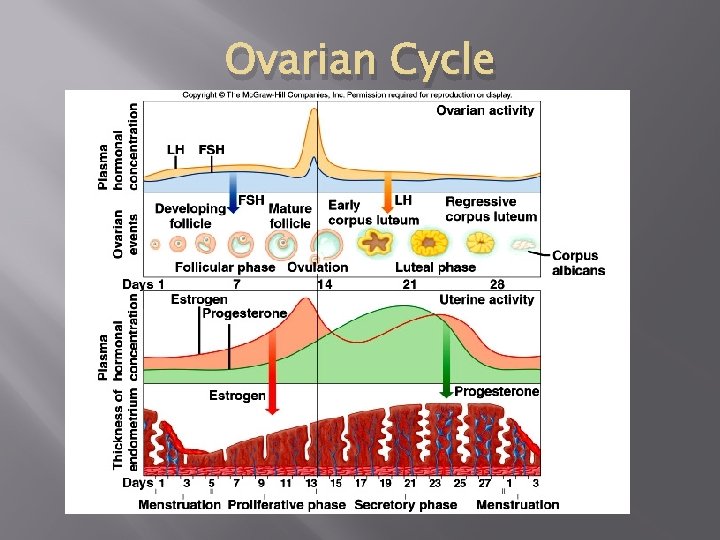
Ovarian Cycle

 Primary sex organ of the male reproductive system? *
Primary sex organ of the male reproductive system? * Antigentest åre
Antigentest åre Sex sex sex
Sex sex sex Sex sex sex
Sex sex sex Sex sex sex
Sex sex sex Sex sex sex
Sex sex sex Secondary sexual characters
Secondary sexual characters What is gonads
What is gonads Mucous membrane reproductive system
Mucous membrane reproductive system Female reproductive organs sagittal section
Female reproductive organs sagittal section Reproductive organs of the bull
Reproductive organs of the bull Male reproductive organs
Male reproductive organs Rabbit reproductive organs
Rabbit reproductive organs Sperm duct
Sperm duct Male reproductive system diagram
Male reproductive system diagram The female anatomy
The female anatomy Sex
Sex What is sex linkage in biology
What is sex linkage in biology Sex determination and sex linkage
Sex determination and sex linkage Once a sex offender always a sex offender
Once a sex offender always a sex offender Primary and secondary retroperitoneal organs
Primary and secondary retroperitoneal organs Posterior abdominal wall
Posterior abdominal wall What are gonads
What are gonads Squid diagram internal
Squid diagram internal What ate gonads
What ate gonads Ovary innervation
Ovary innervation Spermogensis
Spermogensis Monads and gonads
Monads and gonads Endocrine molecules
Endocrine molecules Gonads glands
Gonads glands Gonads
Gonads Gonads
Gonads Starfish
Starfish Figure of female reproductive system
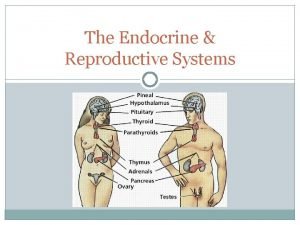
Figure of female reproductive system Endocrine system and reproductive system
Endocrine system and reproductive system Secondary sexual characteristic
Secondary sexual characteristic Sensory system organs
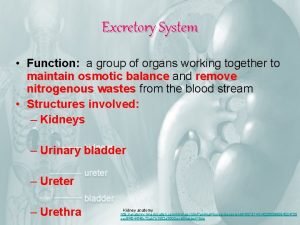
Sensory system organs Excretory system organs and functions
Excretory system organs and functions Accessory organ of the digestive system
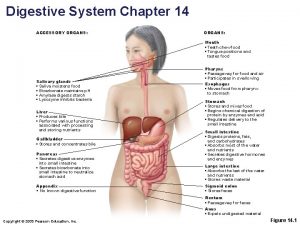
Accessory organ of the digestive system Accessory organs of the digestive system
Accessory organs of the digestive system