Reproductive System Primary sex organs gonads testes and

- Slides: 74
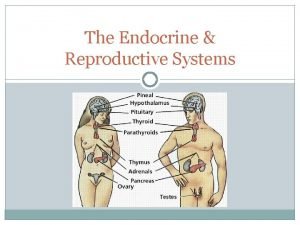
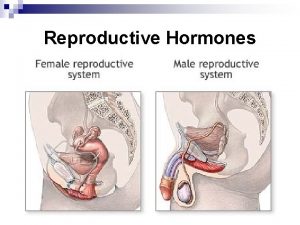
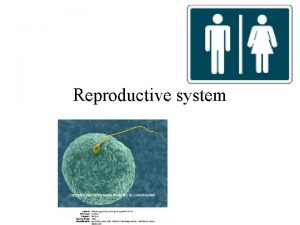
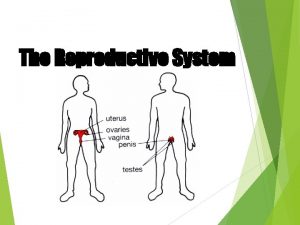
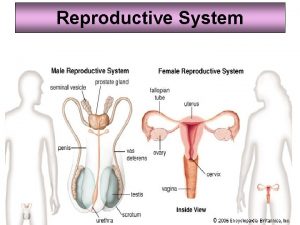
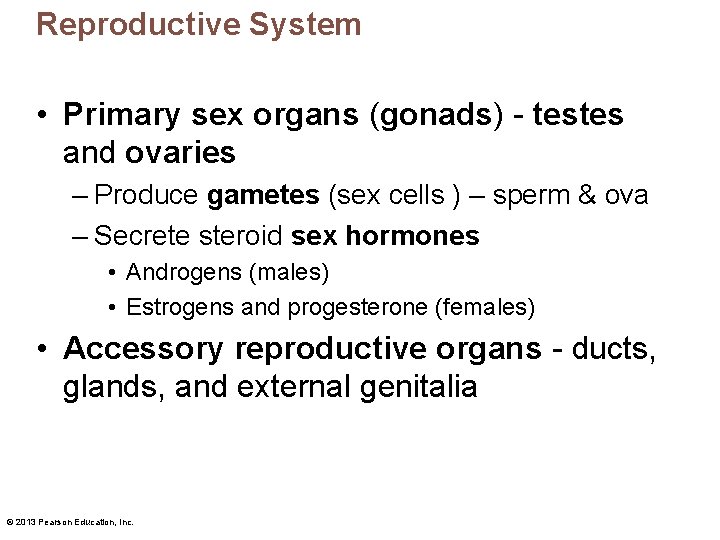
Reproductive System • Primary sex organs (gonads) - testes and ovaries – Produce gametes (sex cells ) – sperm & ova – Secrete steroid sex hormones • Androgens (males) • Estrogens and progesterone (females) • Accessory reproductive organs - ducts, glands, and external genitalia © 2013 Pearson Education, Inc.
Reproductive System • Sex hormones play roles in – Development and function of reproductive organs – Sexual behavior and drives – Growth and development of many other organs and tissues © 2013 Pearson Education, Inc.
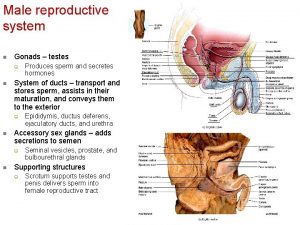
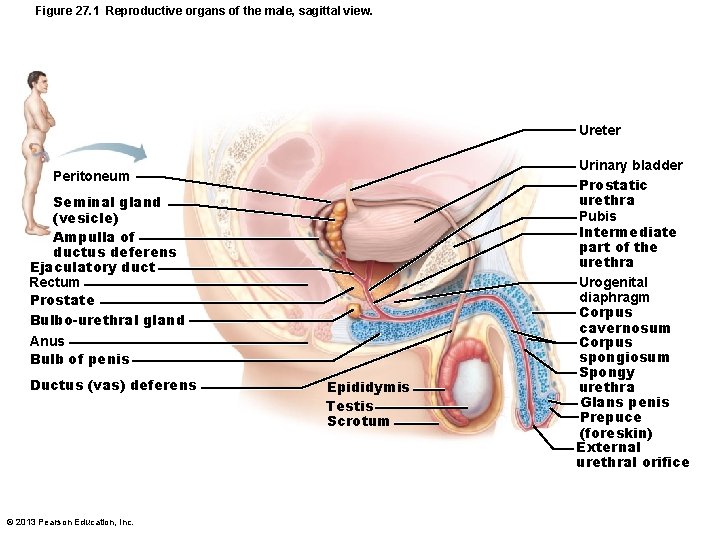
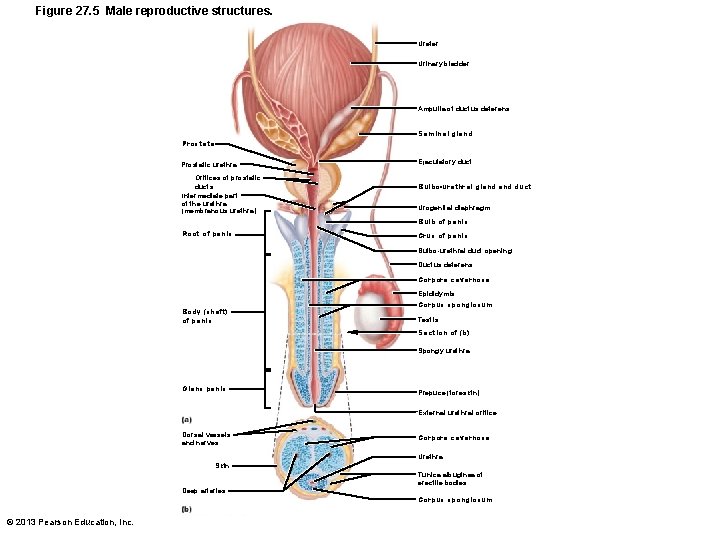
Male Reproductive System • Testes (within scrotum) produce sperm • Sperm delivered to exterior through system of ducts – Epididymis ductus deferens ejaculatory duct urethra © 2013 Pearson Education, Inc.
Male Reproductive System • Accessory sex glands – Seminal vesicles – Prostate – Bulbourethral glands – Empty secretions into ducts during ejaculation © 2013 Pearson Education, Inc.
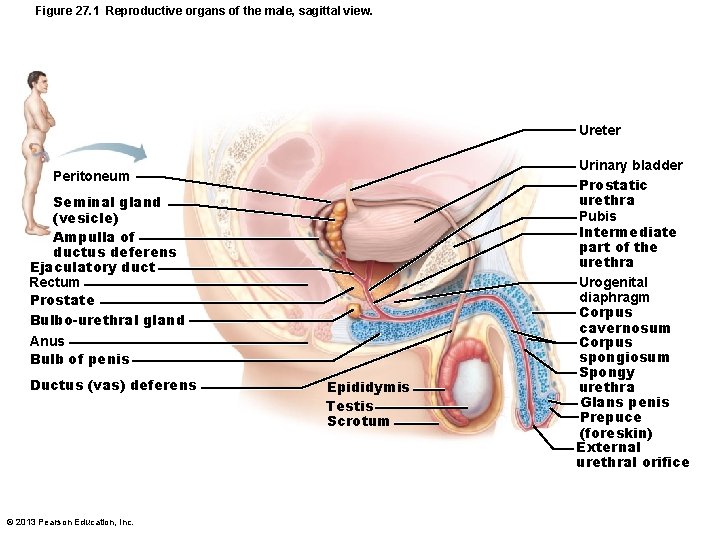
Figure 27. 1 Reproductive organs of the male, sagittal view. Ureter Peritoneum Seminal gland (vesicle) Ampulla of ductus deferens Ejaculatory duct Rectum Prostate Bulbo-urethral gland Anus Bulb of penis Ductus (vas) deferens © 2013 Pearson Education, Inc. Epididymis Testis Scrotum Urinary bladder Prostatic urethra Pubis Intermediate part of the urethra Urogenital diaphragm Corpus cavernosum Corpus spongiosum Spongy urethra Glans penis Prepuce (foreskin) External urethral orifice
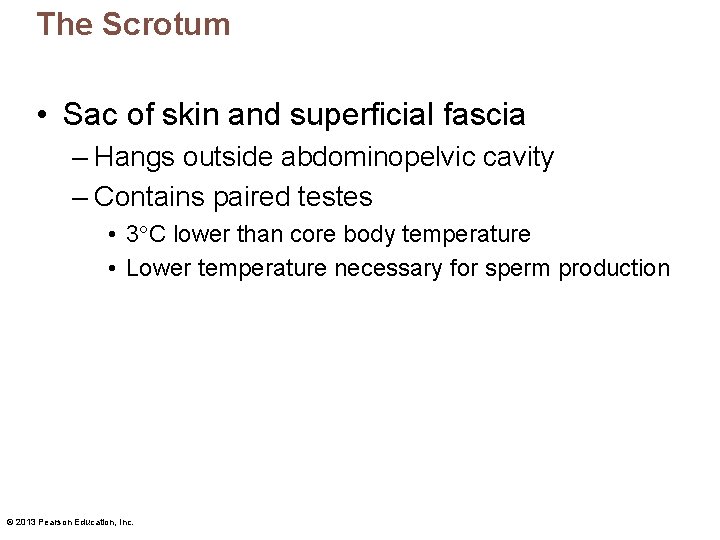
The Scrotum • Sac of skin and superficial fascia – Hangs outside abdominopelvic cavity – Contains paired testes • 3 C lower than core body temperature • Lower temperature necessary for sperm production © 2013 Pearson Education, Inc.
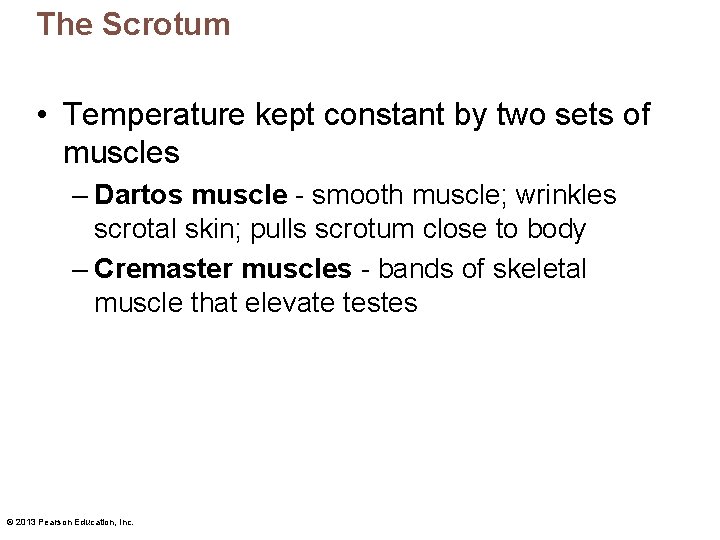
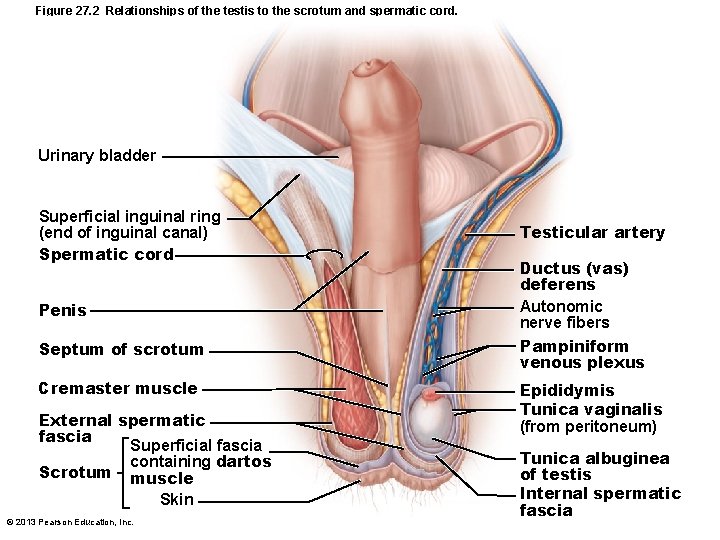
The Scrotum • Temperature kept constant by two sets of muscles – Dartos muscle - smooth muscle; wrinkles scrotal skin; pulls scrotum close to body – Cremaster muscles - bands of skeletal muscle that elevate testes © 2013 Pearson Education, Inc.
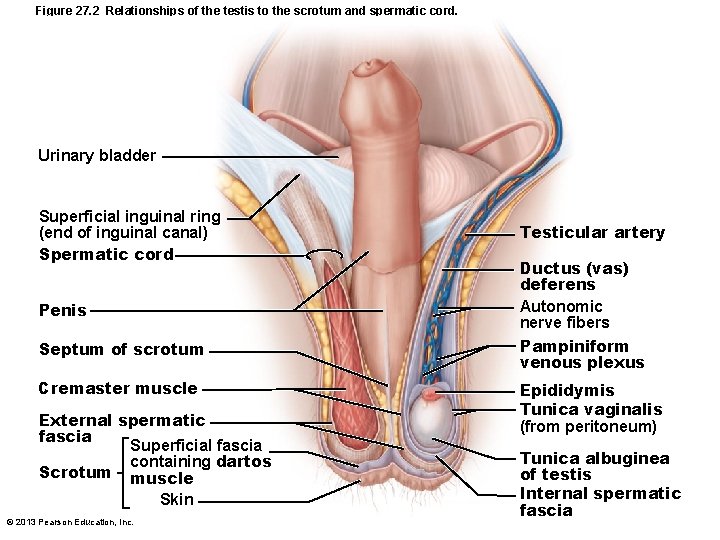
Figure 27. 2 Relationships of the testis to the scrotum and spermatic cord. Urinary bladder Superficial inguinal ring (end of inguinal canal) Spermatic cord Penis Septum of scrotum Cremaster muscle External spermatic fascia Superficial fascia containing dartos Scrotum muscle Skin © 2013 Pearson Education, Inc. Testicular artery Ductus (vas) deferens Autonomic nerve fibers Pampiniform venous plexus Epididymis Tunica vaginalis (from peritoneum) Tunica albuginea of testis Internal spermatic fascia
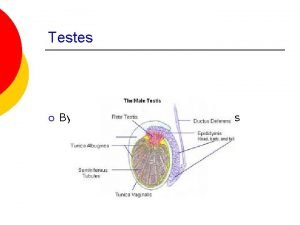
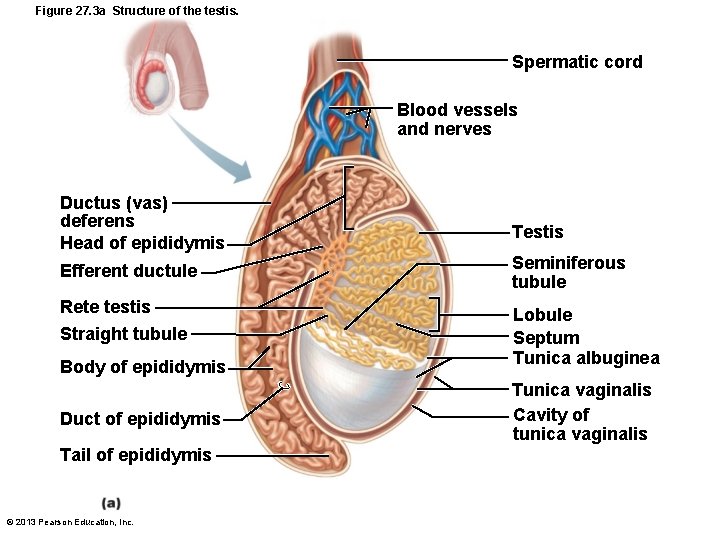
The Testes • Each surrounded by two tunics – Tunica vaginalis – outer layer derived from peritoneum – Tunica albuginea – inner layer; fibrous capsule • Septa divide testis into ~250 lobules, each containing 1– 4 seminiferous tubules site of sperm production © 2013 Pearson Education, Inc.
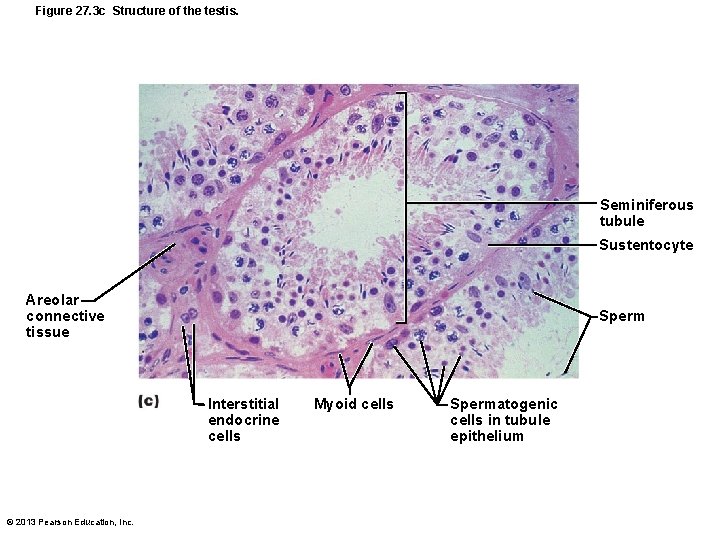
Seminiferous Tubules • Thick, stratified epithelium surrounding central fluid-containing lumen • Epithelium – Spheroid spermatogenic cells embedded in sustentocytes • Myoid cells surround each tubule – May squeeze sperm, testicular fluids out of testes • Tubules of each lobule form straight tubule © 2013 Pearson Education, Inc.
The Testes • Sperm conveyed from – Seminiferous tubules – Straight tubule – Rete testis – Efferent ductules – Epididymis © 2013 Pearson Education, Inc.
Seminiferous Tubules • Interstitial endocrine cells in soft tissue surrounding seminiferous tubules • Produce androgens, e. g. , testosterone – Secrete it into interstitial fluid © 2013 Pearson Education, Inc.
The Testes • Blood supply – Testicular arteries arise from abdominal aorta – Testicular veins arise from pampiniform venous plexus surrounding each testicular artery • Cooler; absorb heat from testicular arteries • Keep testes cool • Spermatic cord encloses nerve fibers, blood vessels, and lymphatics that supply testes © 2013 Pearson Education, Inc.
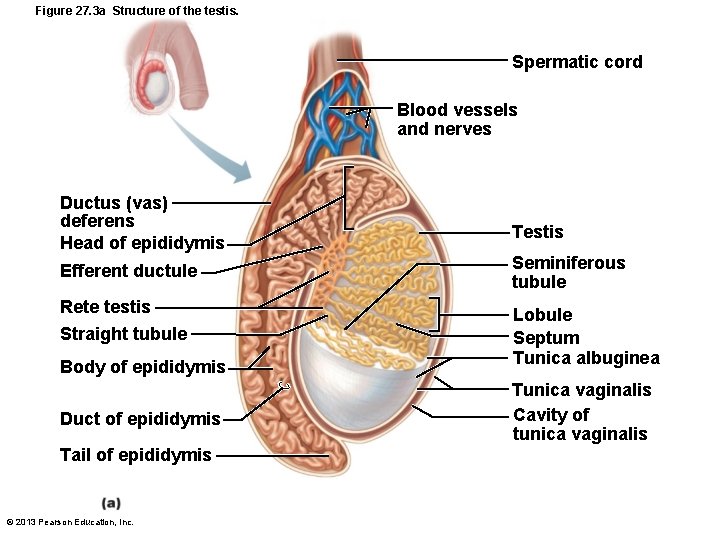
Figure 27. 3 a Structure of the testis. Spermatic cord Blood vessels and nerves Ductus (vas) deferens Head of epididymis Testis Efferent ductule Seminiferous tubule Rete testis Lobule Septum Tunica albuginea Straight tubule Body of epididymis Duct of epididymis Tail of epididymis © 2013 Pearson Education, Inc. Tunica vaginalis Cavity of tunica vaginalis
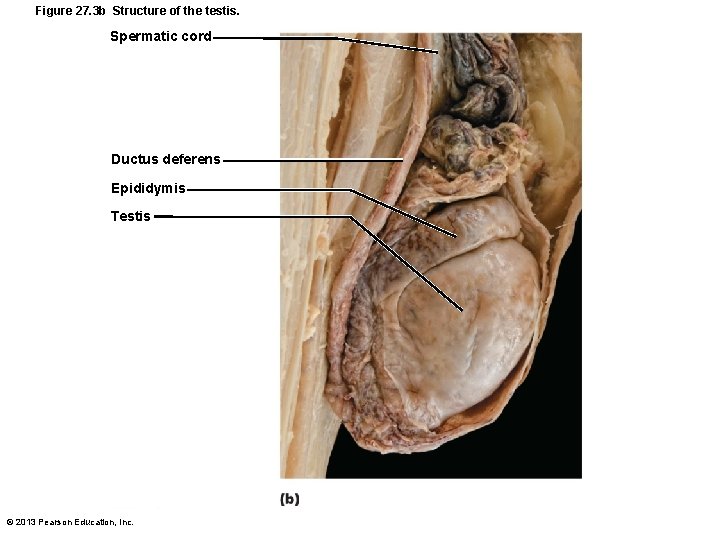
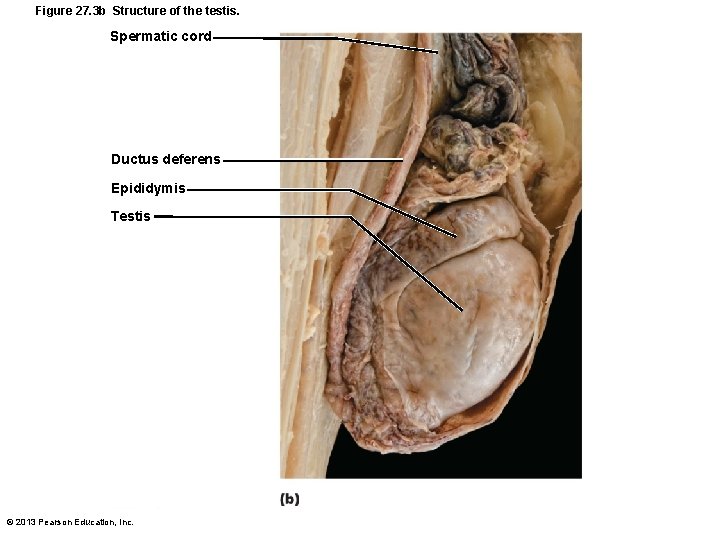
Figure 27. 3 b Structure of the testis. Spermatic cord Ductus deferens Epididymis Testis © 2013 Pearson Education, Inc.
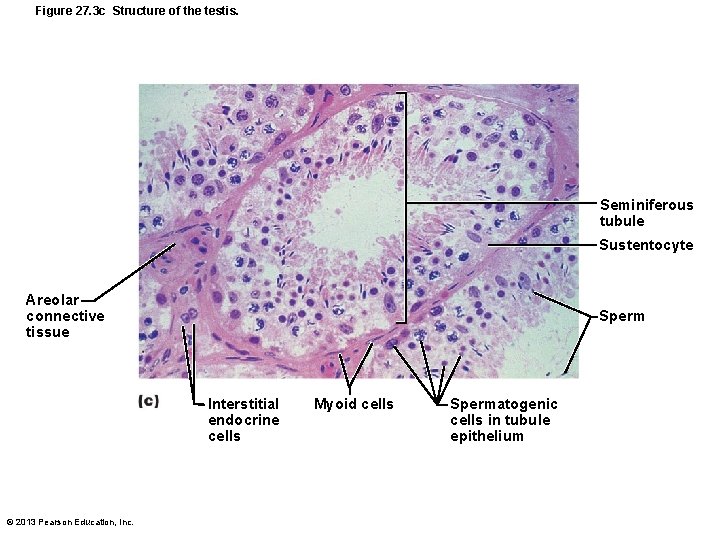
Figure 27. 3 c Structure of the testis. Seminiferous tubule Sustentocyte Areolar connective tissue Sperm Interstitial endocrine cells © 2013 Pearson Education, Inc. Myoid cells Spermatogenic cells in tubule epithelium
Homeostatic Imbalance • Testicular cancer – Rare; most common cancer in men 15 -35 – Cryptorchidism is risk factor – Sign – painless, solid mass in testis – 90% cured by surgical removal of testis and often radiation or chemotherapy © 2013 Pearson Education, Inc.
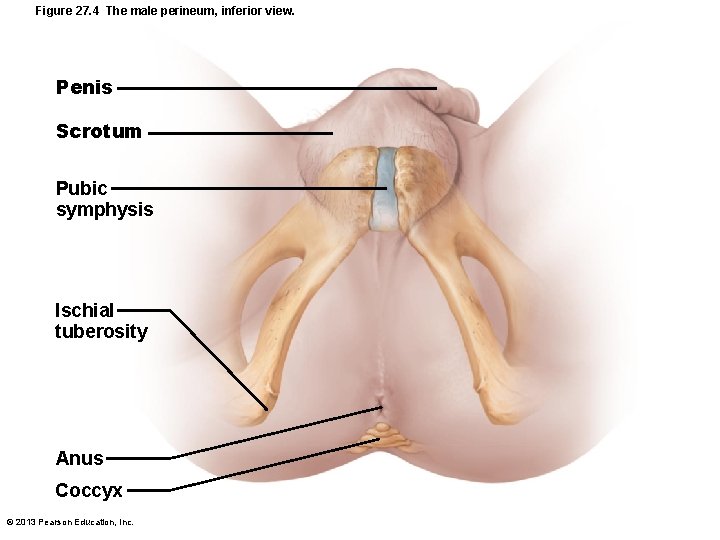
The Male Perineum • Diamond-shaped region between pubic symphysis, coccyx, and ischial tuberosities • Suspends scrotum; contains root of penis and anus © 2013 Pearson Education, Inc.
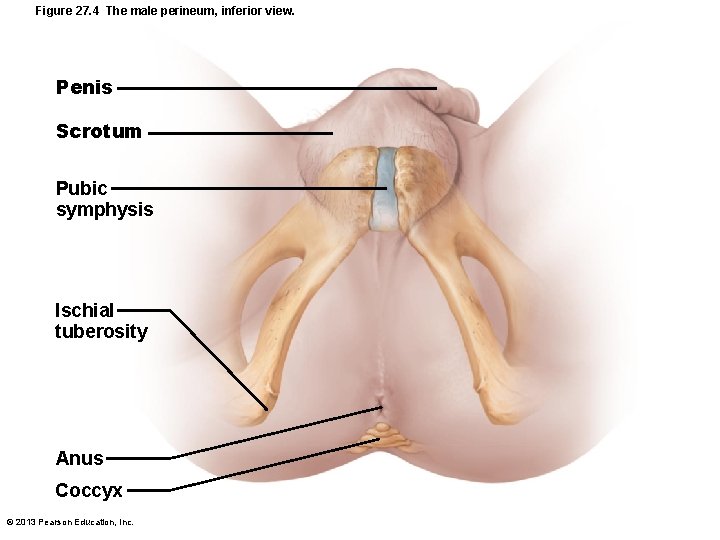
Figure 27. 4 The male perineum, inferior view. Penis Scrotum Pubic symphysis Ischial tuberosity Anus Coccyx © 2013 Pearson Education, Inc.
The Penis • External genitalia - scrotum and penis • Penis - male copulatory organ © 2013 Pearson Education, Inc.
The Penis • Penis consists of – Root and shaft that ends in glans penis – Prepuce, or foreskin—cuff of loose skin covering glans – Crura • Proximal ends of corpora cavernosa surrounded by ischiocavernosus muscle; anchors penis to pubic arch © 2013 Pearson Education, Inc.
Circumcision • Surgical removal of foreskin • 60% newborn boys in US circumcised – 15% in other parts of world – Some claim medically unnecessary – Studies show • 60% reduction in HIV risk • Reduced risk for other reproductive system infections © 2013 Pearson Education, Inc.
The Penis: Internally • Spongy urethra and three cylindrical bodies of erectile tissue (spongy network of connective tissue and smooth muscle with vascular spaces) – Corpus spongiosum - surrounds urethra and expands to form glans and bulb – Corpora cavernosa - paired dorsal erectile bodies • Erection - erectile tissue fills with blood, causing penis to enlarge and become rigid © 2013 Pearson Education, Inc.
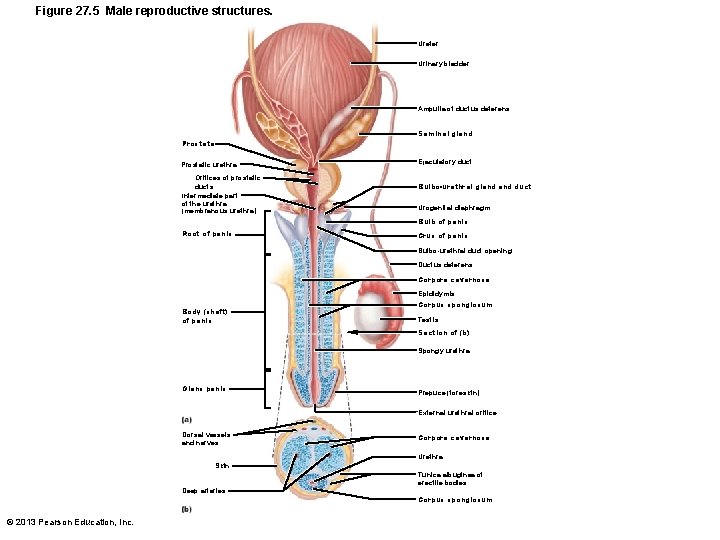
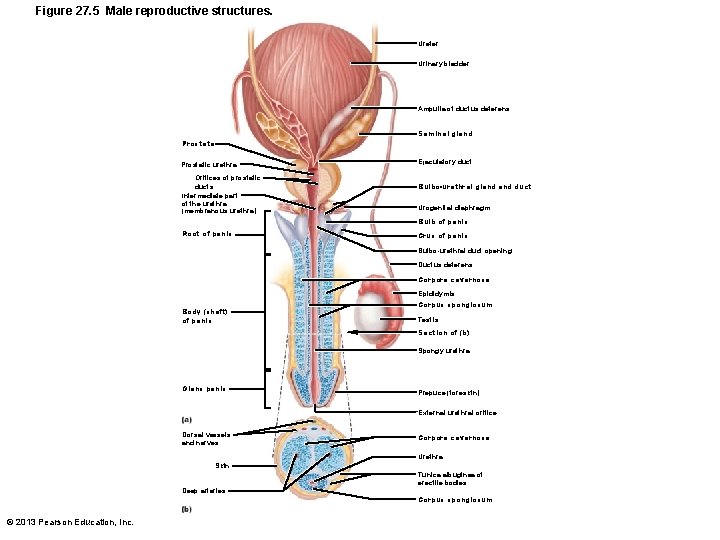
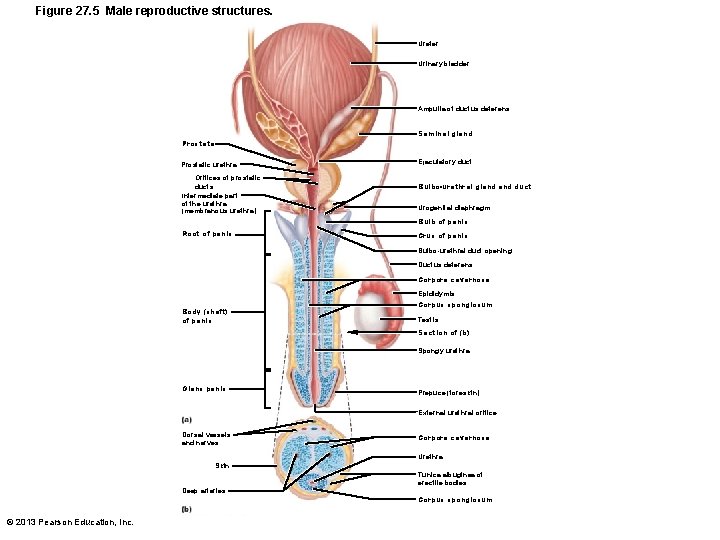
Figure 27. 5 Male reproductive structures. Ureter Urinary bladder Ampulla of ductus deferens Seminal gland Prostate Prostatic urethra Ejaculatory duct Orifices of prostatic ducts Intermediate part of the urethra (membranous urethra) Urogenital diaphragm Root of penis Crus of penis Bulbo-urethral gland duct Bulb of penis Bulbo-urethral duct opening Ductus deferens Corpora cavernosa Epididymis Body (shaft) of penis Corpus spongiosum Testis Section of (b) Spongy urethra Glans penis Prepuce (foreskin) External urethral orifice Dorsal vessels and nerves Corpora cavernosa Urethra Skin Tunica albuginea of erectile bodies Deep arteries © 2013 Pearson Education, Inc. Corpus spongiosum
The Male Duct System • Ducts carry sperm from testes to body exterior – Epididymis – Ductus deferens – Ejaculatory duct – Urethra © 2013 Pearson Education, Inc.
Epididymis • Head - contains efferent ductules; superior aspect of testis; body and tail on posterolateral area of testis • Duct of the epididymis ~ 6 m in length – Microvilli (stereocilia) absorb testicular fluid and pass nutrients to stored sperm • Nonmotile sperm enter, pass slowly through (~ 20 days), become motile; can be stored several months • During ejaculation epididymis contracts, expelling sperm into ductus deferens © 2013 Pearson Education, Inc.
Ductus Deferens and Ejaculatory Duct • Ductus deferens (vas deferens) ~ 45 cm – Passes through inguinal canal to pelvic cavity – Expands to form ampulla; joins duct of seminal vesicle to form ejaculatory duct • Smooth muscle in walls propels sperm from epididymis to urethra • Vasectomy - cutting and ligating ductus deferens; nearly 100% effective form of birth control © 2013 Pearson Education, Inc.
Urethra • Conveys both urine and semen (at different times) • Has three regions – Prostatic urethra – surrounded by prostate – Intermediate part of the urethra (membranous urethra) – in urogenital diaphragm – Spongy urethra – runs through penis; opens at external urethral orifice © 2013 Pearson Education, Inc.
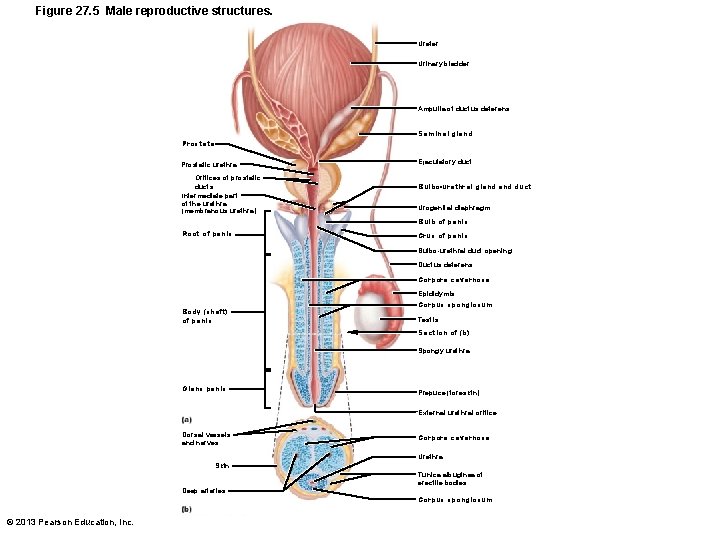
Figure 27. 5 Male reproductive structures. Ureter Urinary bladder Ampulla of ductus deferens Seminal gland Prostate Prostatic urethra Ejaculatory duct Orifices of prostatic ducts Intermediate part of the urethra (membranous urethra) Urogenital diaphragm Root of penis Crus of penis Bulbo-urethral gland duct Bulb of penis Bulbo-urethral duct opening Ductus deferens Corpora cavernosa Epididymis Body (shaft) of penis Corpus spongiosum Testis Section of (b) Spongy urethra Glans penis Prepuce (foreskin) External urethral orifice Dorsal vessels and nerves Corpora cavernosa Urethra Skin Tunica albuginea of erectile bodies Deep arteries © 2013 Pearson Education, Inc. Corpus spongiosum
The Male Accessory Glands • Paired seminal glands (seminal vesicles) • Paired bulbo-urethral glands • Prostate gland • Produce bulk of semen – Remainder - sperm from testes © 2013 Pearson Education, Inc.
Accessory Glands: Seminal Glands • On posterior bladder surface; smooth muscle contracts during ejaculation • Produces viscous alkaline seminal fluid – Fructose, citric acid, coagulating enzyme (vesiculase), and prostaglandins – Yellow pigment fluoresces with UV light – 70% volume of semen • Duct of seminal vesicle joins ductus deferens to form ejaculatory duct © 2013 Pearson Education, Inc.

Accessory Glands: Prostate • Encircles urethra inferior to bladder; size of peach pit; smooth muscle contracts during ejaculation • Secretes milky, slightly acid fluid – Contains citrate, enzymes, and prostatespecific antigen (PSA) – Role in sperm activation – Enters prostatic urethra during ejaculation • 1/3 semen volume © 2013 Pearson Education, Inc.
Prostate Disorders • Prostatitis – inflammatory disorders – Bacterial infection; acute and chronic; treated with antibiotics • Benign prostatic hyperplasia – May be age-related; distorts urethra; treated with surgery, microwaves, drugs, balloon compression, radio-frequency radiation © 2013 Pearson Education, Inc.
Prostate Disorders • Prostate cancer – Second most common cause of cancer death in males – Digital exam screening, PSA levels • Biopsy if abnormal – Treated with surgery and sometimes radiation; castration; drugs – In clinical trials - cryosurgery, chemotherapy, ultrasound, proton beam therapy © 2013 Pearson Education, Inc.
Accessory Glands: Bulbo-Urethral Glands (Cowper's Glands) • Pea-sized glands inferior to prostate • Produce thick, clear mucus during sexual arousal – Lubricates glans penis – Neutralizes traces of acidic urine in urethra © 2013 Pearson Education, Inc.
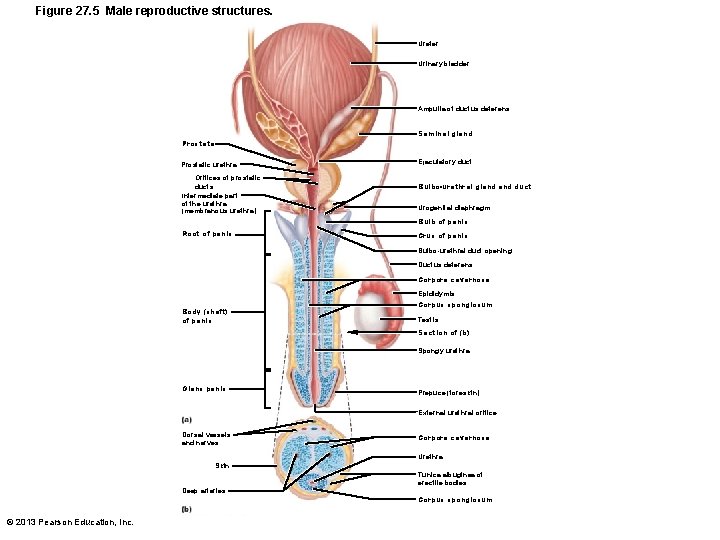
Figure 27. 5 Male reproductive structures. Ureter Urinary bladder Ampulla of ductus deferens Seminal gland Prostate Prostatic urethra Ejaculatory duct Orifices of prostatic ducts Intermediate part of the urethra (membranous urethra) Urogenital diaphragm Root of penis Crus of penis Bulbo-urethral gland duct Bulb of penis Bulbo-urethral duct opening Ductus deferens Corpora cavernosa Epididymis Body (shaft) of penis Corpus spongiosum Testis Section of (b) Spongy urethra Glans penis Prepuce (foreskin) External urethral orifice Dorsal vessels and nerves Corpora cavernosa Urethra Skin Tunica albuginea of erectile bodies Deep arteries © 2013 Pearson Education, Inc. Corpus spongiosum
Semen • Milky-white mixture of sperm and accessory gland secretions – 2– 5 ml semen ejaculated, contains 20– 150 million sperm/ml • Contains fructose for ATP production; protects and activates sperm; facilitates sperm movement • Alkaline neutralizes acidity of male urethra and female vagina enhanced motility © 2013 Pearson Education, Inc.
Semen Functions • Prostaglandins decrease viscosity of mucus in cervix; stimulate reverse peristalsis in uterus • Hormone relaxin, enzymes sperm motility • Contains ATP for energy • Suppresses female immune response • Antibacterial action • Clotting factors coagulate semen initially to prevent draining out; then liquefied by fibrinolysin sperm begin journey © 2013 Pearson Education, Inc.
Male Sexual Response • Erection – Arterioles normally constricted – Sexual excitement causes CNS activation of parasympathetic neurons – nitric oxide (NO) release local vascular smooth muscle relaxation – arterioles dilate corpora cavernosa expands, retards venous drainage – engorgement of erectile tissues with blood – enlargement and stiffening of penis © 2013 Pearson Education, Inc.
Erection • Initiated by sexual stimuli – Touch; mechanical stimulation of penis; erotic sights, sounds, and smells • Can be induced or inhibited by emotions or higher mental activity • Longitudinal and circular collagen fibers around penis prevent kinking/buckling of erect penis • Corpus spongiosum keeps urethra open © 2013 Pearson Education, Inc.
Male Sexual Response • Ejaculation – Propulsion of semen from male duct system – Sympathetic spinal reflex • Bladder sphincter muscle constricts, preventing expulsion of urine • Ducts and accessory glands contract and empty their contents • Bulbospongiosus muscles undergo rapid series of contractions expulsion of semen at ~ 500 cm/s (close to 11 mph) – Ejaculatory event – climax (orgasm) © 2013 Pearson Education, Inc.
Homeostatic Imbalance • Erectile dysfunction – Parasympathetic nerves of penis release too little NO – Causes – alcohol, drugs, hormones, blood vessel or nervous system problems, incompetent venous valves fail to retain blood in penis – New drugs (Viagra, Cialis) potentiate existing NO effects © 2013 Pearson Education, Inc.
Spermatogenesis • Sperm (spermatozoa) production in seminiferous tubules • Most body cells have 46 chromosomes diploid chromosomal number (2 n) – Two sets (23 pairs) of chromosomes • One maternal, one paternal – homologous chromosomes – Gametes have 23 chromosomes - haploid chromosomal number (n) • Only one member of homologous pair © 2013 Pearson Education, Inc.
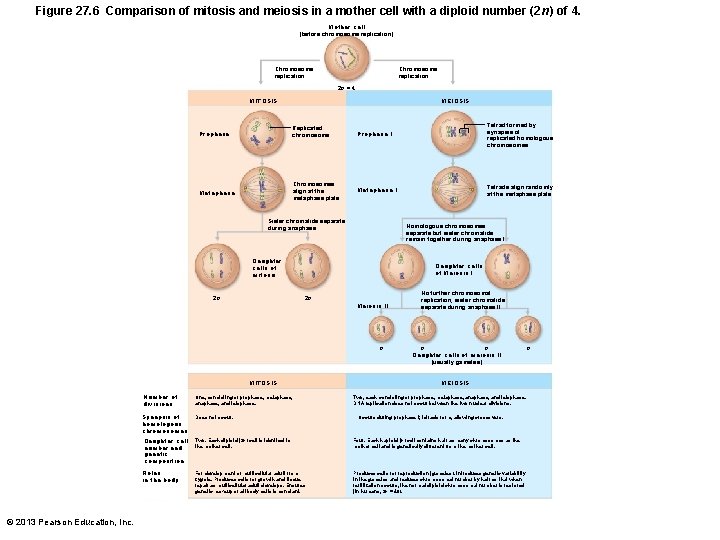
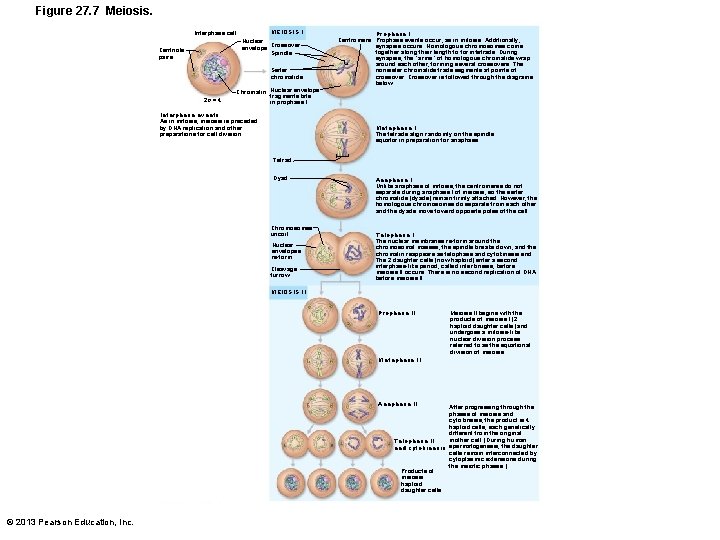
Meiosis • Gamete formation involves meiosis – Differs from mitosis – Two consecutive cell divisions (meiosis I and II); only one round of DNA replication • Produces four daughter cells • Functions of meiosis – Number of chromosomes halved (from 2 n to n) – Introduces genetic diversity © 2013 Pearson Education, Inc.
Meiosis • Random alignment of homologous pairs in meiosis I variability of gametes • Crossover variability of gametes • ~ No two gametes exactly alike • ~ All different from original mother cells © 2013 Pearson Education, Inc.
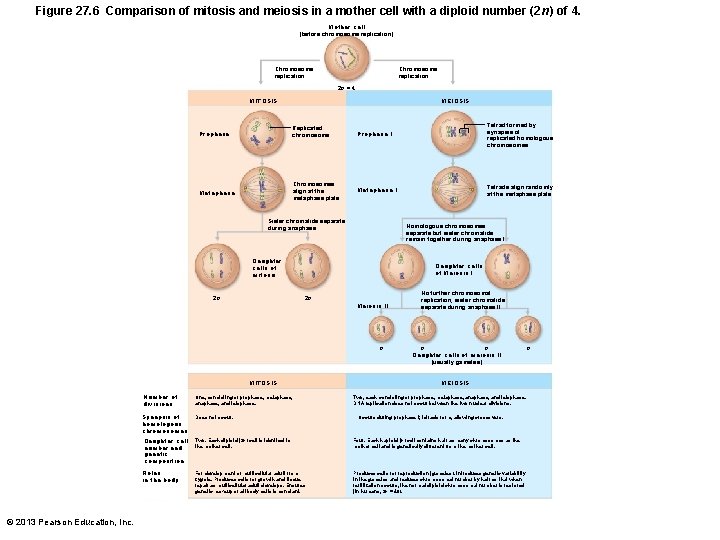
Figure 27. 6 Comparison of mitosis and meiosis in a mother cell with a diploid number (2 n) of 4. Mother cell (before chromosome replication) Chromosome replication 2 n = 4 MITOSIS MEIOSIS Prophase Replicated chromosome Prophase I Tetrad formed by synapsis of replicated homologous chromosomes Metaphase Chromosomes align at the metaphase plate Metaphase I Tetrads align randomly at the metaphase plate Sister chromatids separate during anaphase Homologous chromosomes separate but sister chromatids remain together during anaphase I Daughter cells of mitosis 2 n Daughter cells of Meiosis I 2 n Meiosis II n MITOSIS Number of divisions Synapsis of homologous chromosomes Daughter cell number and genetic composition Roles in the body © 2013 Pearson Education, Inc. One, consisting of prophase, metaphase, and telophase. Does not occur. No further chromosomal replication; sister chromatids separate during anaphase II n n Daughter cells of meiosis II (usually gametes) MEIOSIS Two, each consisting of prophase, metaphase, and telophase. DNA replication does not occur between the two nuclear divisions. Occurs during prophase I; tetrads form, allowing crossovers. Two. Each diploid (2 n) cell is identical to the mother cell. Four. Each haploid (n) cell contains half as many chromosomes as the mother cell and is genetically different from the mother cell. For development of multicellular adult from zygote. Produces cells for growth and tissue repair as multicellular adult develops. Ensures genetic makeup of all body cells is constant. Produces cells for reproduction (gametes). Introduces genetic variability in the gametes and reduces chromosomal number by half so that when fertilization occurs, the normal diploid chromosomal number is restored (in humans, 2 n = 46). n
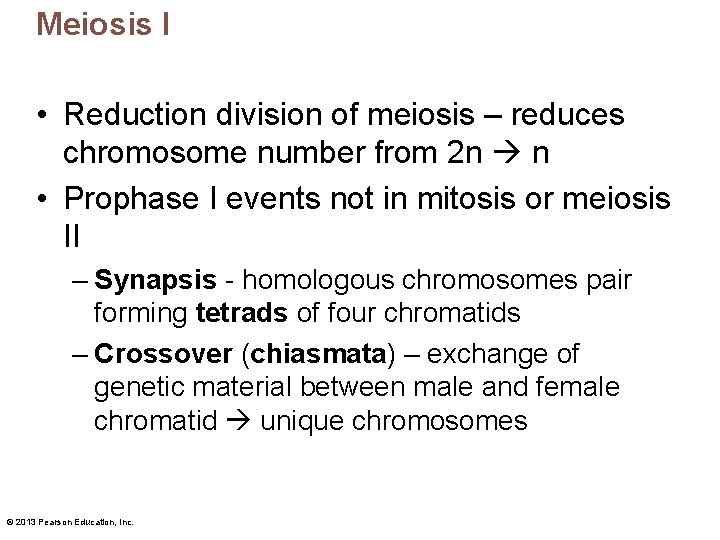
Meiosis I • Reduction division of meiosis – reduces chromosome number from 2 n n • Prophase I events not in mitosis or meiosis II – Synapsis - homologous chromosomes pair forming tetrads of four chromatids – Crossover (chiasmata) – exchange of genetic material between male and female chromatid unique chromosomes © 2013 Pearson Education, Inc.
Meiosis I • End of meiosis I each daughter cell – Two copies of one member of each homologous pair (either maternal or paternal); none of the other – Haploid chromosomal number; still-united sister chromatids one chromosome (twice amount DNA in each chromosome) © 2013 Pearson Education, Inc.
Meiosis II • Equational division of meiosis – Sister chromatids from meiosis I separated, one per cell • Like mitosis except no chromosome replication before begins © 2013 Pearson Education, Inc.
Meiosis PLAY Animation: Interphase PLAY Animation: Prophase I PLAY Animation: Metaphase I PLAY Animation: Anaphase I PLAY Animation: Telophase I PLAY Animation: Meiosis II © 2013 Pearson Education, Inc.
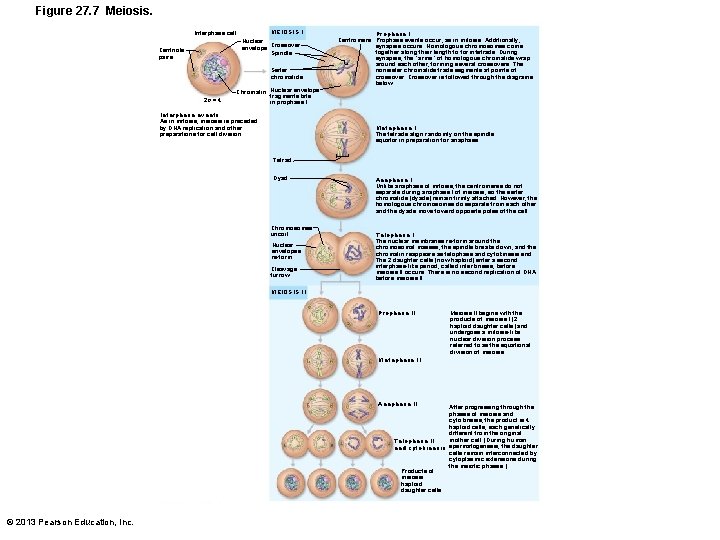
Figure 27. 7 Meiosis. MEIOSIS I Interphase cell Nuclear envelope Crossover Spindle Centriole pairs Sister chromatids 2 n = 4 Prophase I Centromere Prophase events occur, as in mitosis. Additionally, synapsis occurs: Homologous chromosomes come together along their length to form tetrads. During synapsis, the “arms” of homologous chromatids wrap around each other, forming several crossovers. The nonsister chromatids trade segments at points of crossover. Crossover is followed through the diagrams below. Chromatin Nuclear envelope fragments late in prophase I Interphase events As in mitosis, meiosis is preceded by DNA replication and other preparations for cell division. Metaphase I The tetrads align randomly on the spindle equator in preparation for anaphase. Tetrad Dyad Chromosomes uncoil Nuclear envelopes re-form Cleavage furrow Anaphase I Unlike anaphase of mitosis, the centromeres do not separate during anaphase I of meiosis, so the sister chromatids (dyads) remain firmly attached. However, the homologous chromosomes do separate from each other and the dyads move toward opposite poles of the cell. Telophase I The nuclear membranes re-form around the chromosomal masses, the spindle breaks down, and the chromatin reappears as telophase and cytokinesis end. The 2 daughter cells (now haploid) enter a second interphase-like period, called interkinesis, before meiosis II occurs. There is no second replication of DNA before meiosis II. MEIOSIS II Prophase II Meiosis II begins with the products of meiosis I (2 haploid daughter cells) and undergoes a mitosis-like nuclear division process referred to as the equational division of meiosis. Metaphase II Anaphase II After progressing through the phases of meiosis and cytokinesis, the product is 4 haploid cells, each genetically different from the original mother cell. (During human Telophase II and cytokinesis spermatogenesis, the daughter cells remain interconnected by cytoplasmic extensions during the meiotic phases. ) Products of meiosis: haploid daughter cells © 2013 Pearson Education, Inc.
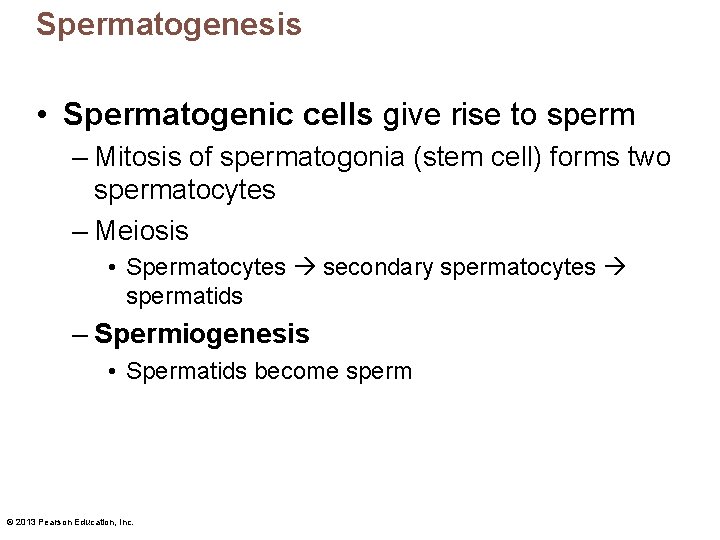
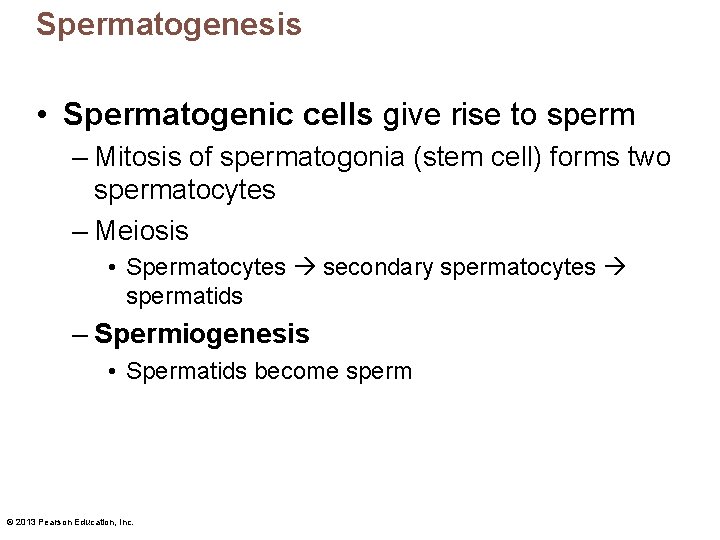
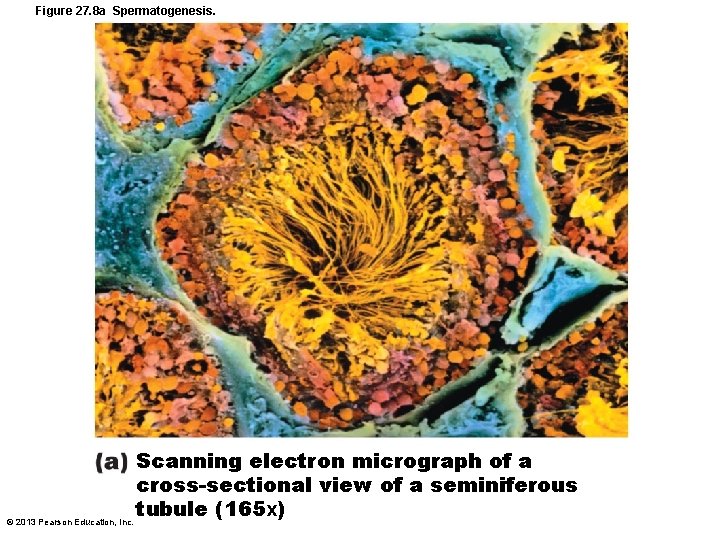
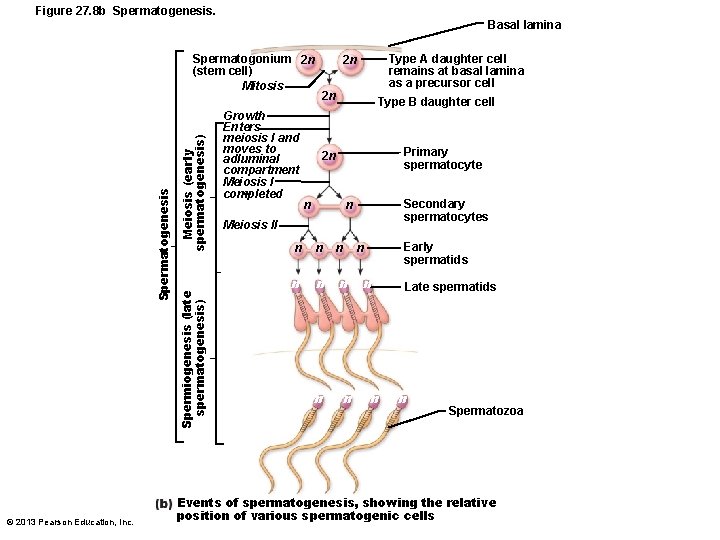
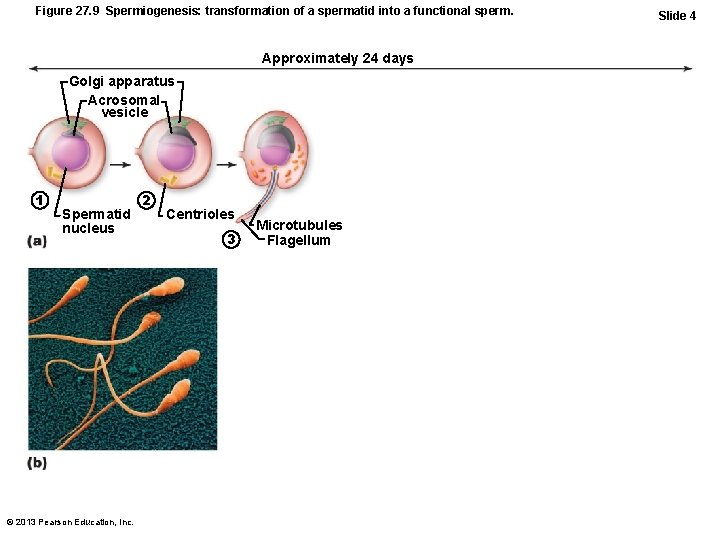
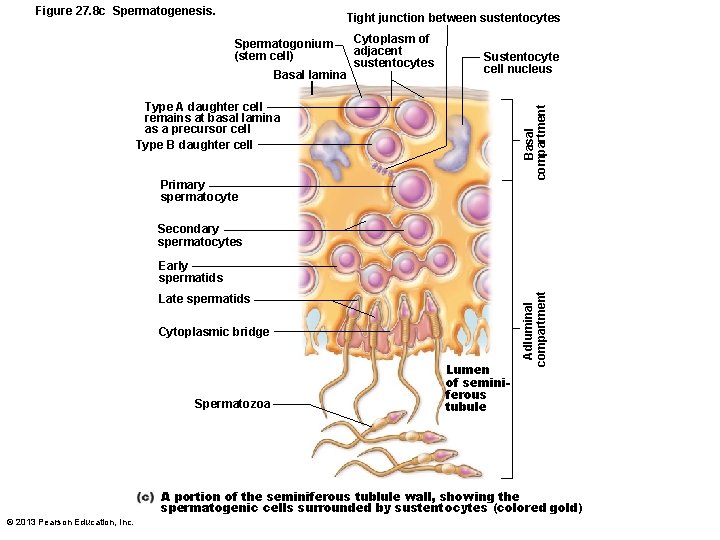
Spermatogenesis • Spermatogenic cells give rise to sperm – Mitosis of spermatogonia (stem cell) forms two spermatocytes – Meiosis • Spermatocytes secondary spermatocytes spermatids – Spermiogenesis • Spermatids become sperm © 2013 Pearson Education, Inc.
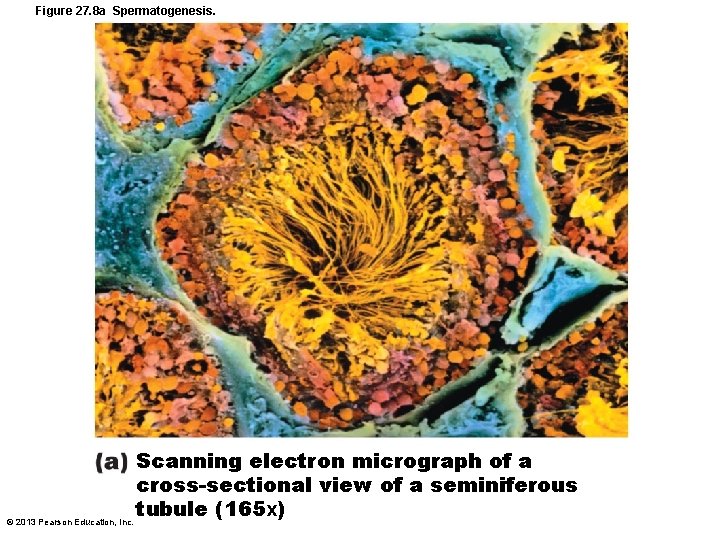
Figure 27. 8 a Spermatogenesis. Scanning electron micrograph of a cross-sectional view of a seminiferous tubule (165 x) © 2013 Pearson Education, Inc.
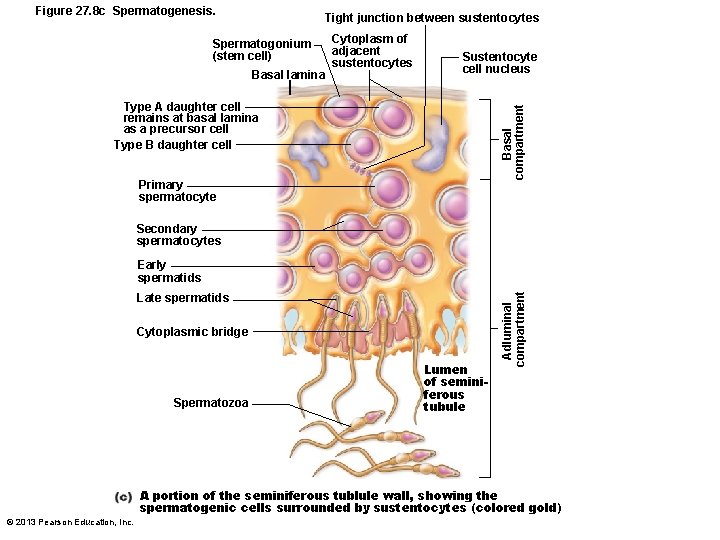
Figure 27. 8 c Spermatogenesis. Tight junction between sustentocytes Spermatogonium (stem cell) Basal lamina Cytoplasm of adjacent sustentocytes Sustentocyte cell nucleus Basal compartment Type A daughter cell remains at basal lamina as a precursor cell Type B daughter cell Primary spermatocyte Secondary spermatocytes Late spermatids Cytoplasmic bridge Spermatozoa Lumen of seminiferous tubule Adluminal compartment Early spermatids A portion of the seminiferous tublule wall, showing the spermatogenic cells surrounded by sustentocytes (colored gold) © 2013 Pearson Education, Inc.
Mitosis of Spermatogonia • Spermatogenesis begins at puberty • Spermatogonia – Stem cells in contact with epithelial basal lamina – Each mitotic division one type A daughter cell and one type B daughter cell © 2013 Pearson Education, Inc.
Mitosis of Spermatogonia • Type A cells maintain germ cell line at basal lamina • Type B cells move toward lumen and develop into primary spermatocytes © 2013 Pearson Education, Inc.
Meiosis: Spermatocytes to Spermatids • Meiosis I – Primary spermatocyte (2 n) two secondary spermatocytes (n) • Meiosis II – Each secondary spermatocyte (n) two spermatids (n) – Spermatid – small, nonmotile cells close to lumen of tubule © 2013 Pearson Education, Inc.
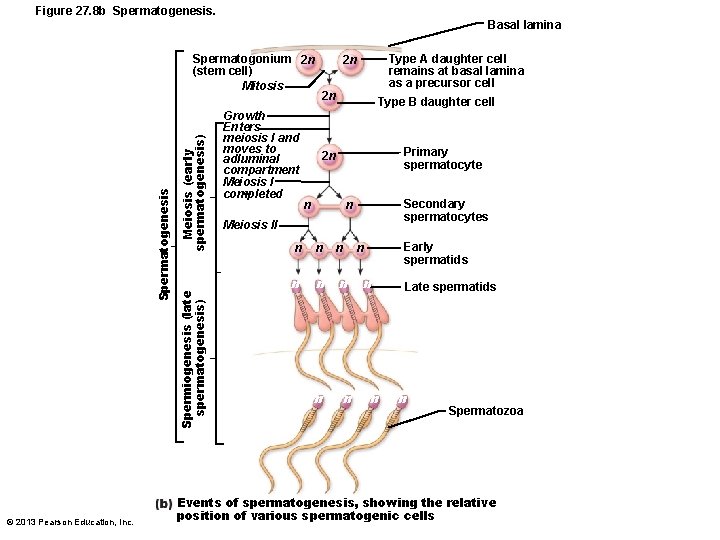
Figure 27. 8 b Spermatogenesis. Basal lamina © 2013 Pearson Education, Inc. Meiosis (early spermatogenesis) Spermiogenesis (late spermatogenesis) Spermatogenesis Spermatogonium 2 n (stem cell) Mitosis Growth Enters meiosis I and moves to adluminal compartment Meiosis I completed Type A daughter cell remains at basal lamina as a precursor cell 2 n 2 n Type B daughter cell Primary spermatocyte 2 n Secondary spermatocytes n n Meiosis ll n n n n Early spermatids n n n Late spermatids n Spermatozoa Events of spermatogenesis, showing the relative position of various spermatogenic cells
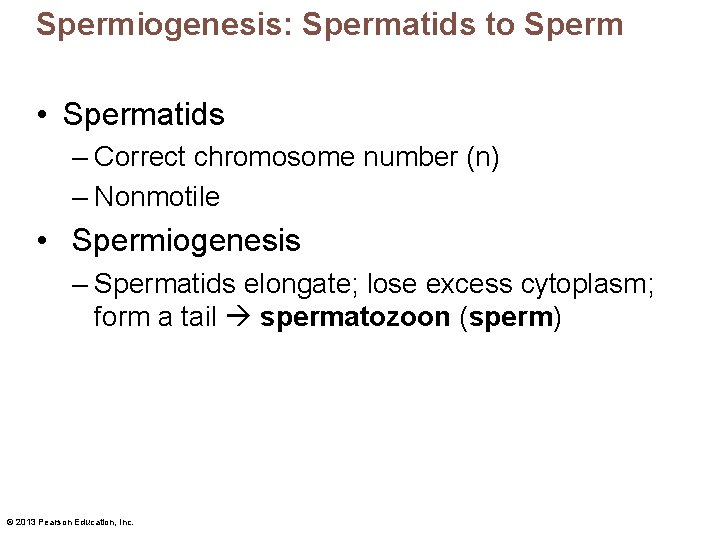
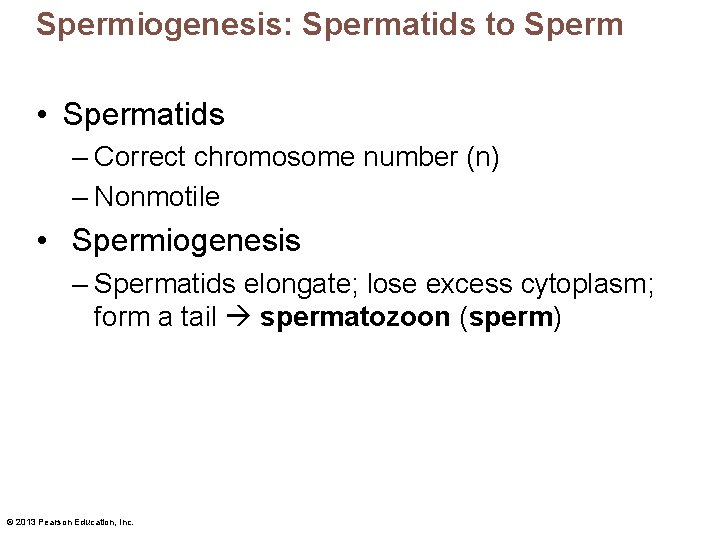
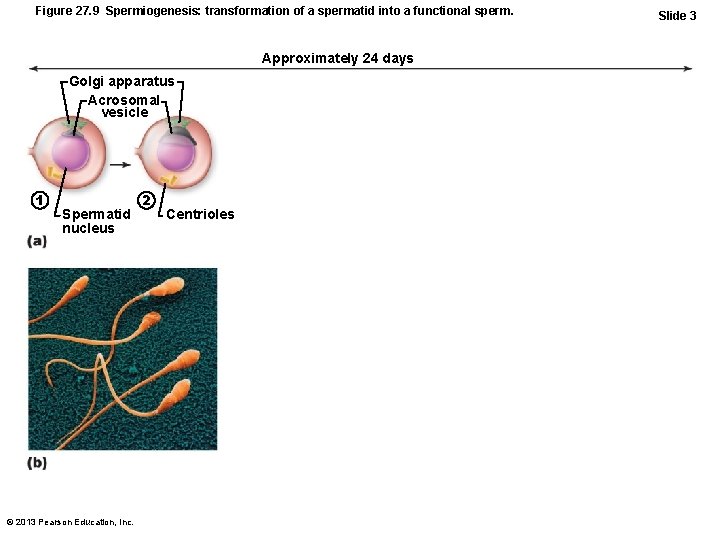
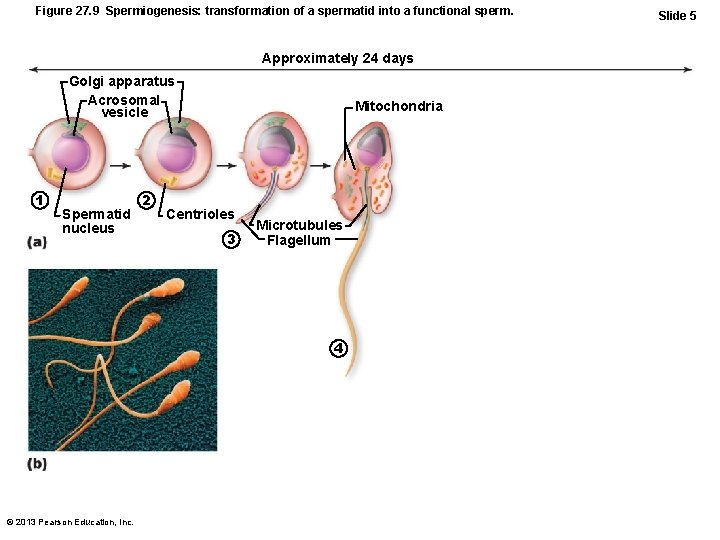
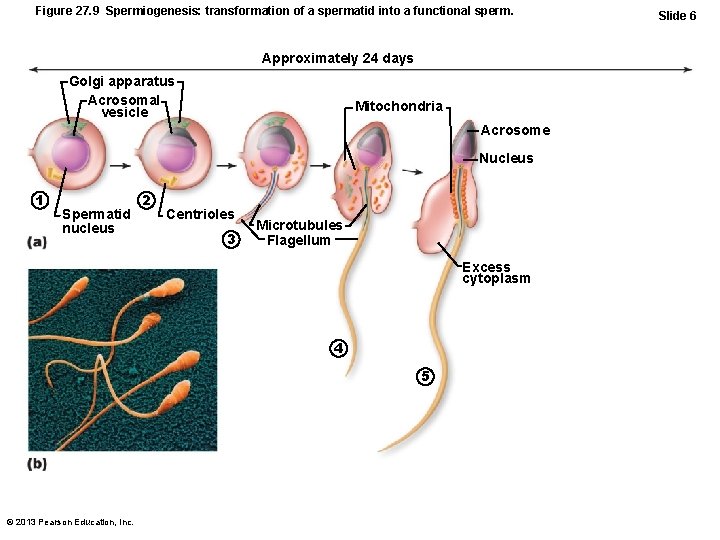
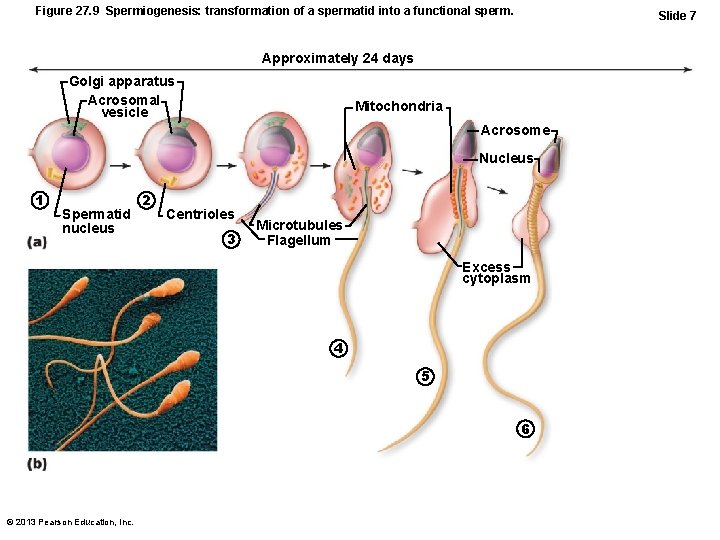
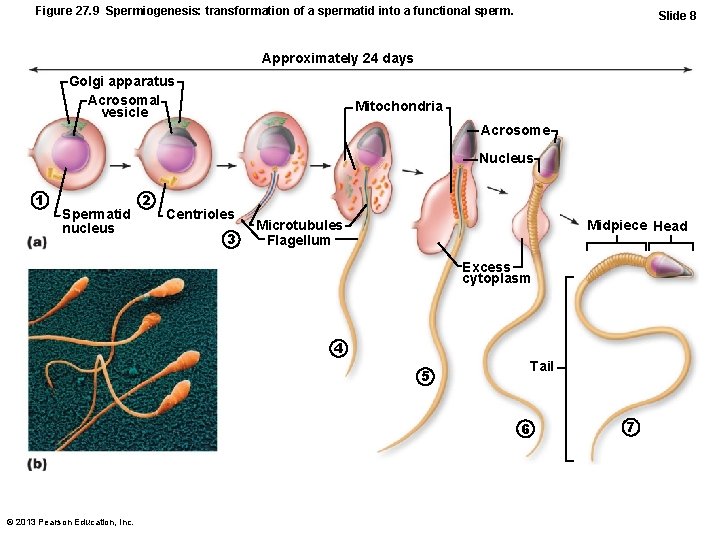
Spermiogenesis: Spermatids to Sperm • Spermatids – Correct chromosome number (n) – Nonmotile • Spermiogenesis – Spermatids elongate; lose excess cytoplasm; form a tail spermatozoon (sperm) © 2013 Pearson Education, Inc.
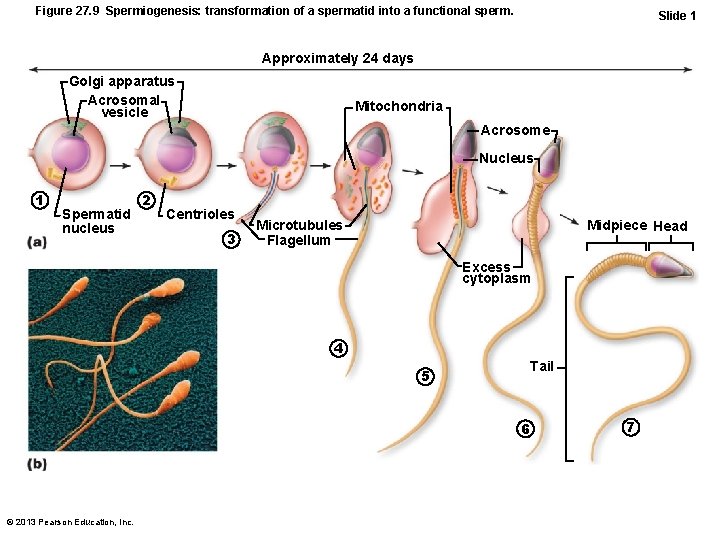
Figure 27. 9 Spermiogenesis: transformation of a spermatid into a functional sperm. Slide 1 Approximately 24 days Golgi apparatus Acrosomal vesicle Mitochondria Acrosome Nucleus 1 Spermatid nucleus 2 Centrioles 3 Microtubules Flagellum Midpiece Head Excess cytoplasm 4 Tail 5 6 © 2013 Pearson Education, Inc. 7
Figure 27. 9 Spermiogenesis: transformation of a spermatid into a functional sperm. Approximately 24 days Golgi apparatus Acrosomal vesicle 1 Spermatid nucleus © 2013 Pearson Education, Inc. Slide 2
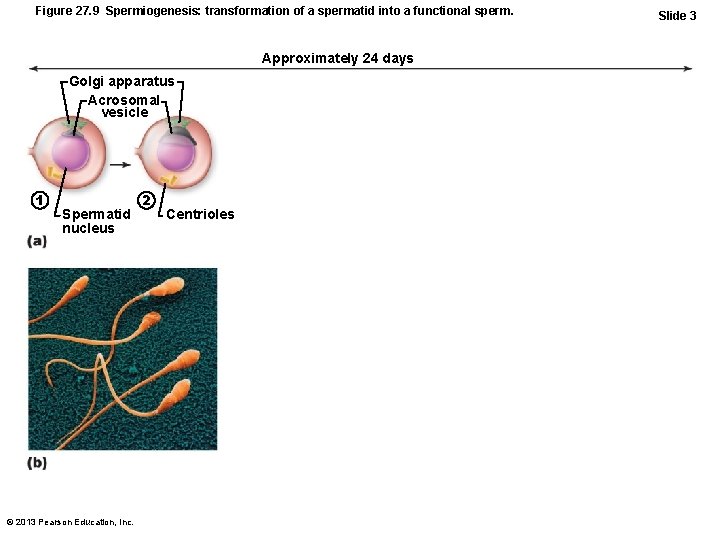
Figure 27. 9 Spermiogenesis: transformation of a spermatid into a functional sperm. Approximately 24 days Golgi apparatus Acrosomal vesicle 1 Spermatid nucleus © 2013 Pearson Education, Inc. 2 Centrioles Slide 3
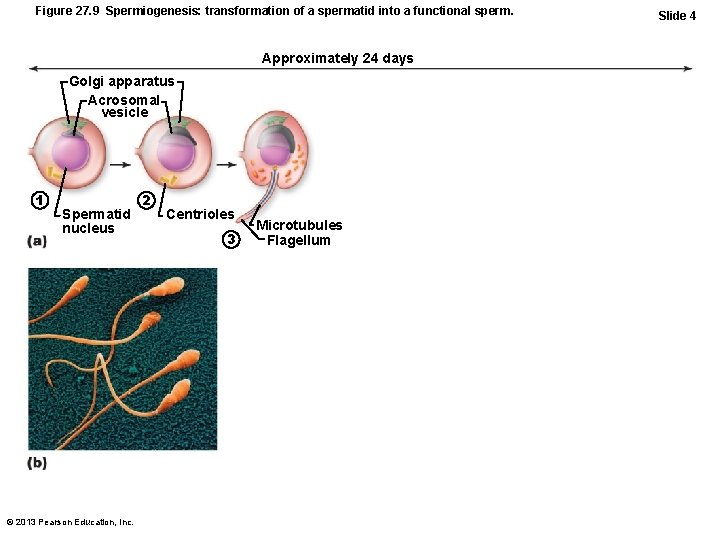
Figure 27. 9 Spermiogenesis: transformation of a spermatid into a functional sperm. Approximately 24 days Golgi apparatus Acrosomal vesicle 1 Spermatid nucleus © 2013 Pearson Education, Inc. 2 Centrioles 3 Microtubules Flagellum Slide 4
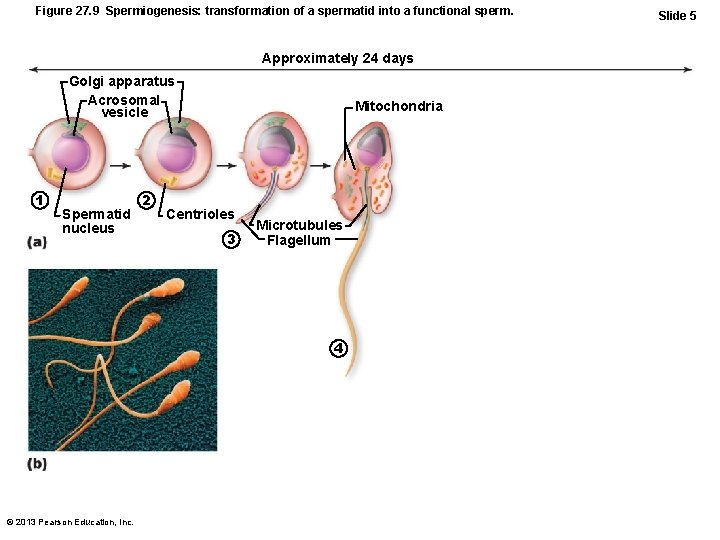
Figure 27. 9 Spermiogenesis: transformation of a spermatid into a functional sperm. Approximately 24 days Golgi apparatus Acrosomal vesicle 1 Spermatid nucleus 2 Mitochondria Centrioles 3 Microtubules Flagellum 4 © 2013 Pearson Education, Inc. Slide 5
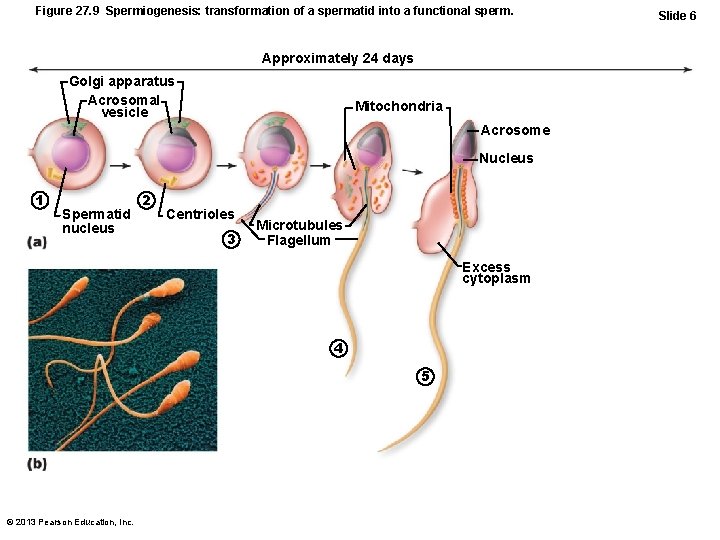
Figure 27. 9 Spermiogenesis: transformation of a spermatid into a functional sperm. Approximately 24 days Golgi apparatus Acrosomal vesicle Mitochondria Acrosome Nucleus 1 Spermatid nucleus 2 Centrioles 3 Microtubules Flagellum Excess cytoplasm 4 5 © 2013 Pearson Education, Inc. Slide 6
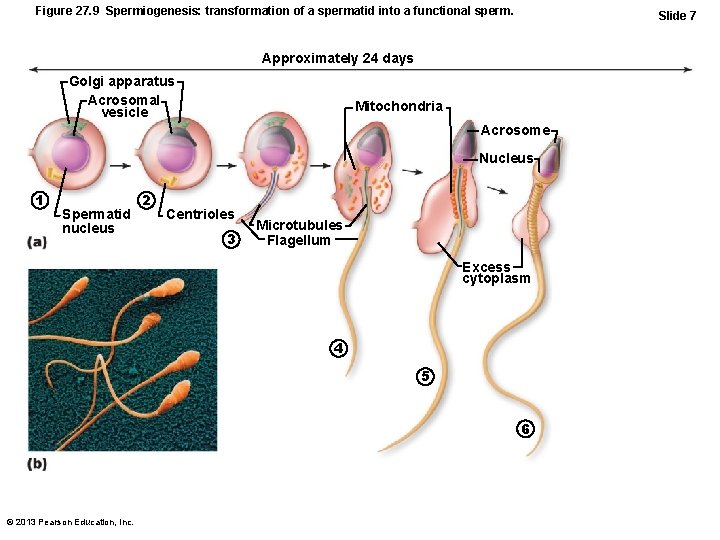
Figure 27. 9 Spermiogenesis: transformation of a spermatid into a functional sperm. Slide 7 Approximately 24 days Golgi apparatus Acrosomal vesicle Mitochondria Acrosome Nucleus 1 Spermatid nucleus 2 Centrioles 3 Microtubules Flagellum Excess cytoplasm 4 5 6 © 2013 Pearson Education, Inc.
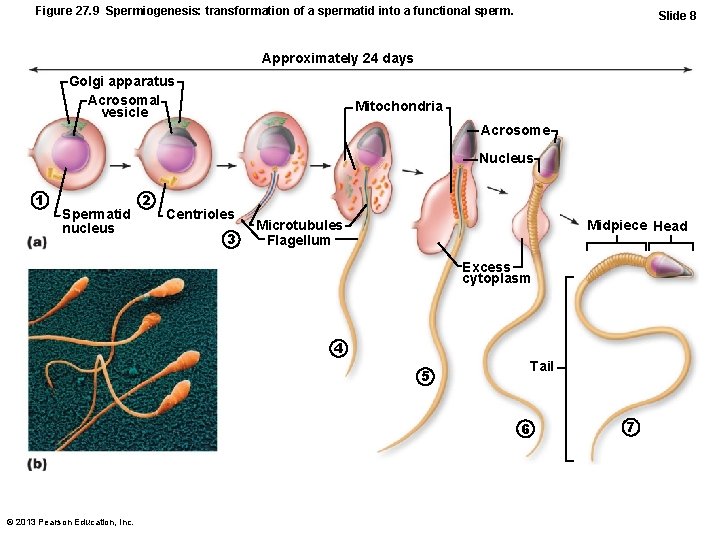
Figure 27. 9 Spermiogenesis: transformation of a spermatid into a functional sperm. Slide 8 Approximately 24 days Golgi apparatus Acrosomal vesicle Mitochondria Acrosome Nucleus 1 Spermatid nucleus 2 Centrioles 3 Microtubules Flagellum Midpiece Head Excess cytoplasm 4 Tail 5 6 © 2013 Pearson Education, Inc. 7
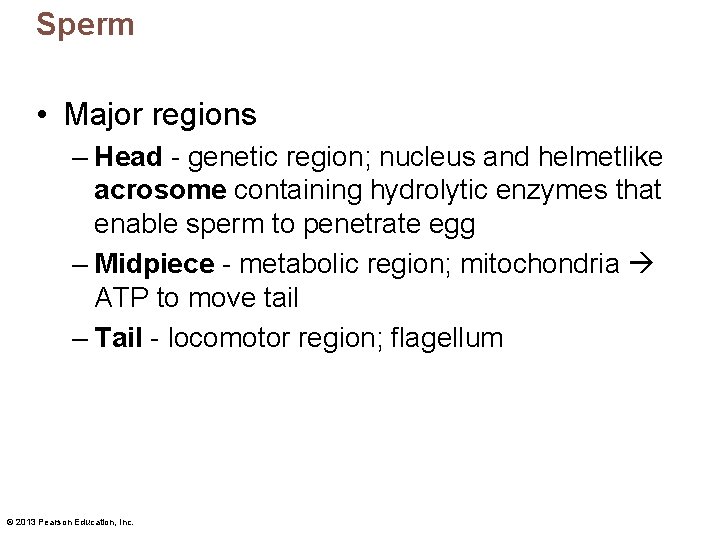
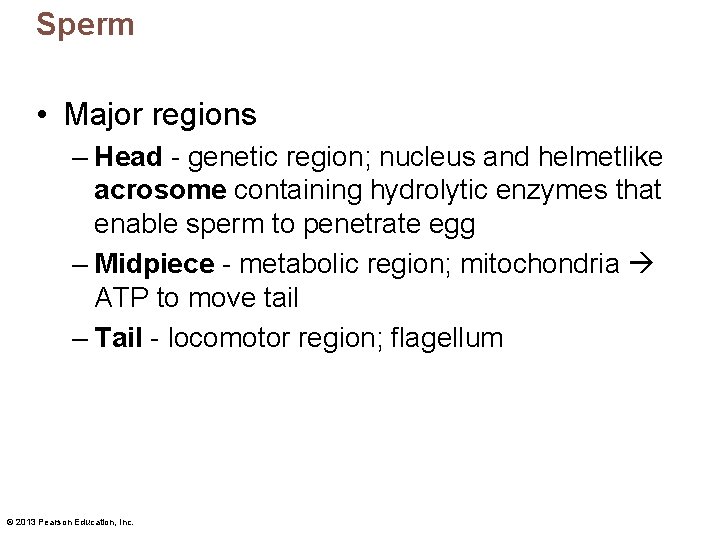
Sperm • Major regions – Head - genetic region; nucleus and helmetlike acrosome containing hydrolytic enzymes that enable sperm to penetrate egg – Midpiece - metabolic region; mitochondria ATP to move tail – Tail - locomotor region; flagellum © 2013 Pearson Education, Inc.
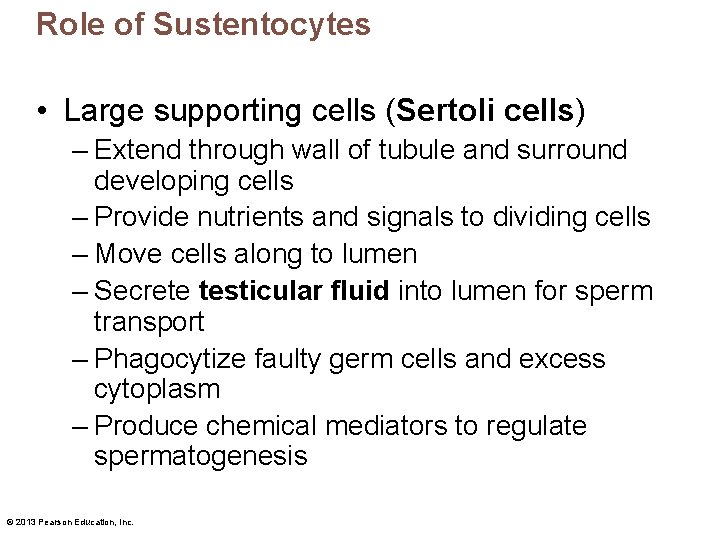
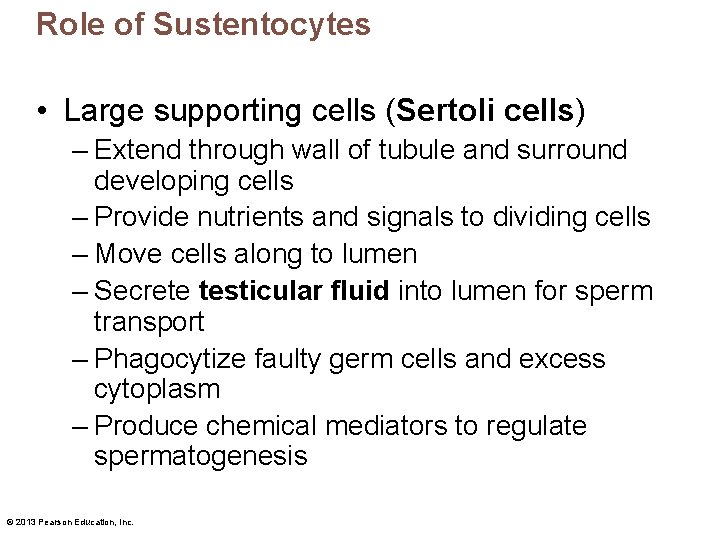
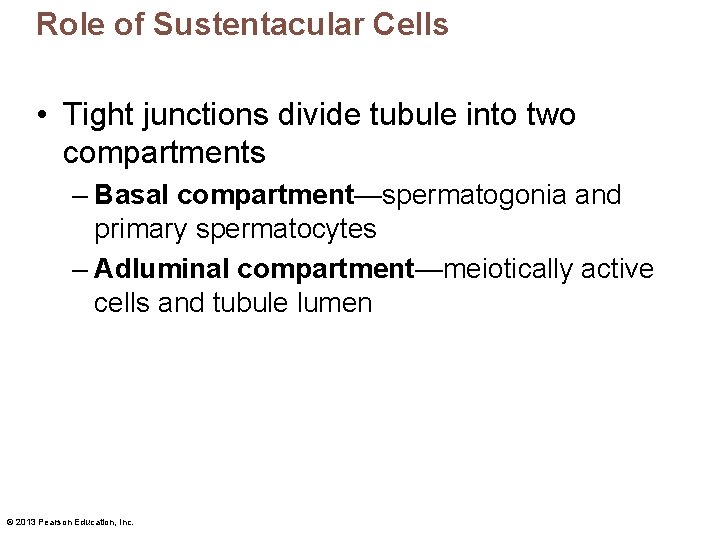
Role of Sustentocytes • Large supporting cells (Sertoli cells) – Extend through wall of tubule and surround developing cells – Provide nutrients and signals to dividing cells – Move cells along to lumen – Secrete testicular fluid into lumen for sperm transport – Phagocytize faulty germ cells and excess cytoplasm – Produce chemical mediators to regulate spermatogenesis © 2013 Pearson Education, Inc.
Role of Sustentacular Cells • Tight junctions divide tubule into two compartments – Basal compartment—spermatogonia and primary spermatocytes – Adluminal compartment—meiotically active cells and tubule lumen © 2013 Pearson Education, Inc.
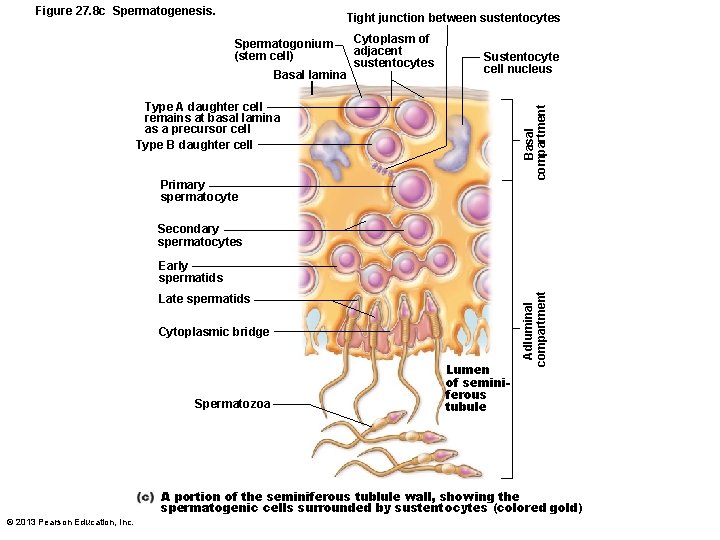
Figure 27. 8 c Spermatogenesis. Tight junction between sustentocytes Spermatogonium (stem cell) Basal lamina Cytoplasm of adjacent sustentocytes Sustentocyte cell nucleus Basal compartment Type A daughter cell remains at basal lamina as a precursor cell Type B daughter cell Primary spermatocyte Secondary spermatocytes Late spermatids Cytoplasmic bridge Spermatozoa Lumen of seminiferous tubule Adluminal compartment Early spermatids A portion of the seminiferous tublule wall, showing the spermatogenic cells surrounded by sustentocytes (colored gold) © 2013 Pearson Education, Inc.
Role of Sustentacular Cells • Tight junctions form blood-testis barrier – Prevents sperm antigens from escaping into blood activation of immune system – Important - sperm not formed until puberty, absent during immune system development, would not be recognized as "self" © 2013 Pearson Education, Inc.
Spermatogenesis • Takes 64 – 72 days if conditions hospitable • Pressure of testicular fluid pushes immotile sperm into epididymis motility and fertilizing power © 2013 Pearson Education, Inc.
Homeostatic Imbalance • Infertility – Gradual decline in male fertility past 50 years – Xenobiotics (alien molecules) may be cause • Environmental toxins, PVCs, phthalates, pesticides, herbicides, compounds with estrogenic effects, antibiotics, radiation, lead, marijuana – Also, lack of selenium, excessive alcohol, lack of specific Ca 2+ channel, anatomical obstructions, hormonal imbalances, oxidative stress, fevers, hot tubs © 2013 Pearson Education, Inc.
 Primary sex organ of the male reproductive system? *
Primary sex organ of the male reproductive system? * Sex sex sex
Sex sex sex Greenhouse sex
Greenhouse sex Sex sex sex
Sex sex sex Sex sex sex
Sex sex sex Secondary sexual characters
Secondary sexual characters Primary sex organs of the female *
Primary sex organs of the female * Definition of reproductive system
Definition of reproductive system Female reproductive organs sagittal section
Female reproductive organs sagittal section Reproductive organs of the bull
Reproductive organs of the bull Mesovariun
Mesovariun Sheep reproductive system
Sheep reproductive system Parts of and functions of female reproductive system
Parts of and functions of female reproductive system Produces a lubricating mucus that cleanses the urethra
Produces a lubricating mucus that cleanses the urethra Functions of the uterus
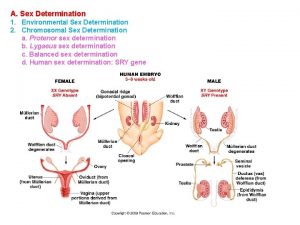
Functions of the uterus X linked recessive punnett square
X linked recessive punnett square What is sex linkage in biology
What is sex linkage in biology Sex determination and sex linkage
Sex determination and sex linkage Primary and secondary retroperitoneal organs
Primary and secondary retroperitoneal organs Posterior abdominal wall
Posterior abdominal wall Once a sex offender always a sex offender
Once a sex offender always a sex offender Monads and gonads
Monads and gonads Endocrine system and reproductive system
Endocrine system and reproductive system What is gonads
What is gonads External anatomy of squid
External anatomy of squid Parts of sperm
Parts of sperm Mesosalpinx
Mesosalpinx Path of sperm
Path of sperm Endocrine molecules
Endocrine molecules Pak pandani
Pak pandani Gonads
Gonads Gonads
Gonads Starfish aboral view
Starfish aboral view Ovarian duct
Ovarian duct What is the function of the excretory system
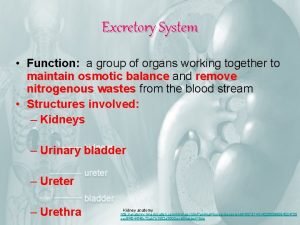
What is the function of the excretory system Accessory organ of the digestive system
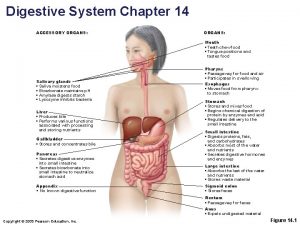
Accessory organ of the digestive system Accessory organs of the digestive system
Accessory organs of the digestive system Spleen function
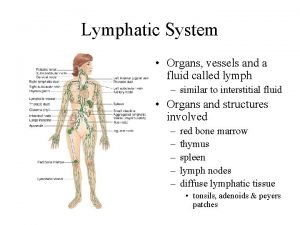
Spleen function Lymphatic system organs and functions
Lymphatic system organs and functions Primary sexual characteristics
Primary sexual characteristics Psicometria significado
Psicometria significado Frimbae
Frimbae Frog testis labeled
Frog testis labeled Testes neuropsicopedagógicos pdf
Testes neuropsicopedagógicos pdf Singkatan kata untuk test skrining kanker prostate adalah
Singkatan kata untuk test skrining kanker prostate adalah Anaorchidism adalah
Anaorchidism adalah Testes regressivos
Testes regressivos Fertilization and implantation
Fertilization and implantation Functions of testis
Functions of testis Testes post hoc
Testes post hoc Male gonad
Male gonad Testes
Testes Gonad
Gonad Testes
Testes What hormone does the testes produce
What hormone does the testes produce Testes gland
Testes gland Paula melo silva
Paula melo silva Ductnn
Ductnn Spermatocyte
Spermatocyte Perch testes
Perch testes History of biopsychology
History of biopsychology Etimiologia
Etimiologia Meiosis
Meiosis Frog lungs
Frog lungs Teste de neer
Teste de neer Sensory system organs
Sensory system organs Accessory organs of the digestive system
Accessory organs of the digestive system Lymphatic system organs
Lymphatic system organs Stratified squamous non-keratinized epithelium
Stratified squamous non-keratinized epithelium Organs of the sensory system
Organs of the sensory system Which organs are involved in respiratory system
Which organs are involved in respiratory system Respiratory system organs
Respiratory system organs Chapter 16 matching questions 1-5
Chapter 16 matching questions 1-5 Function of male reproductive system
Function of male reproductive system Parts of male and female reproductive system
Parts of male and female reproductive system