Reproduction Testes male gonads Produce sperm Produce sex






















- Slides: 73
Reproduction

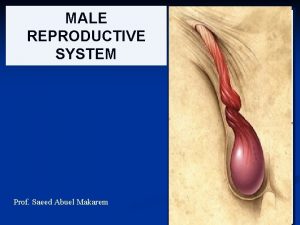
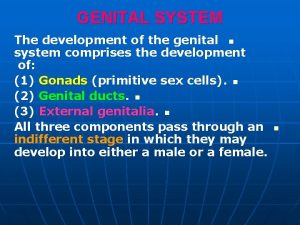
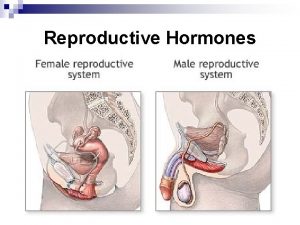
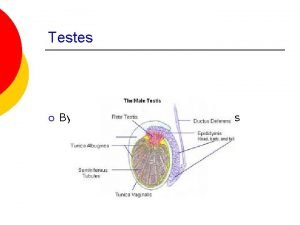
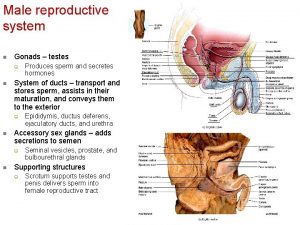
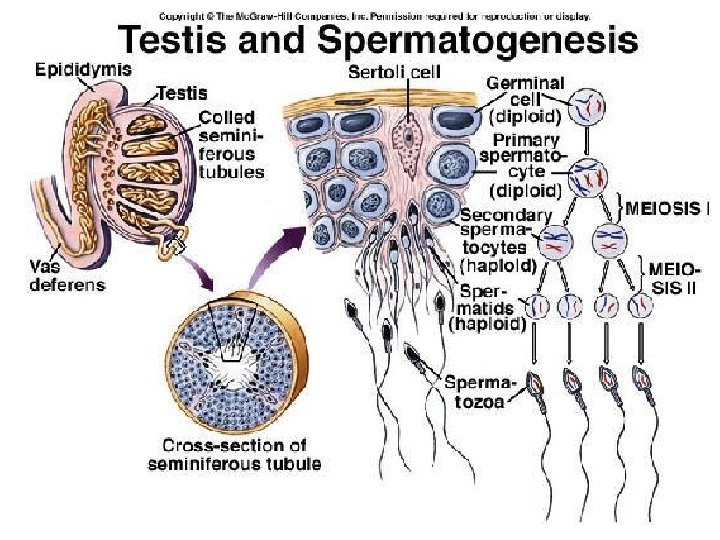
Testes (male gonads) -Produce sperm -Produce sex hormones -Found in a sac called the scrotum -Suspended outside of the body cavity for temperature reduction
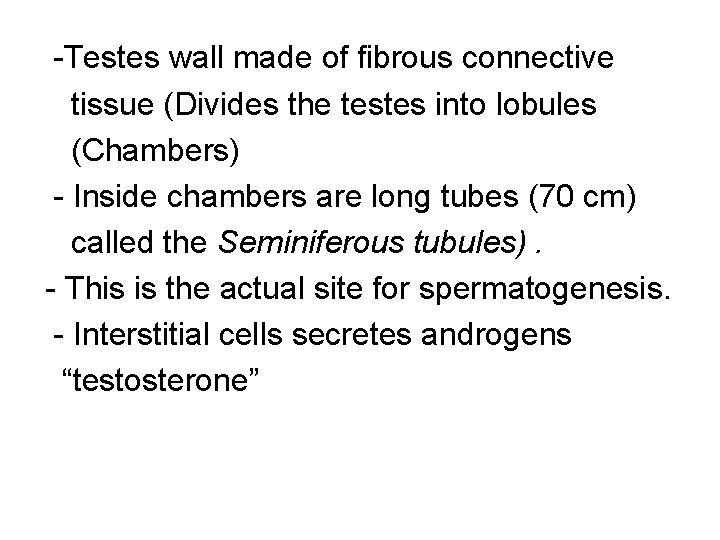
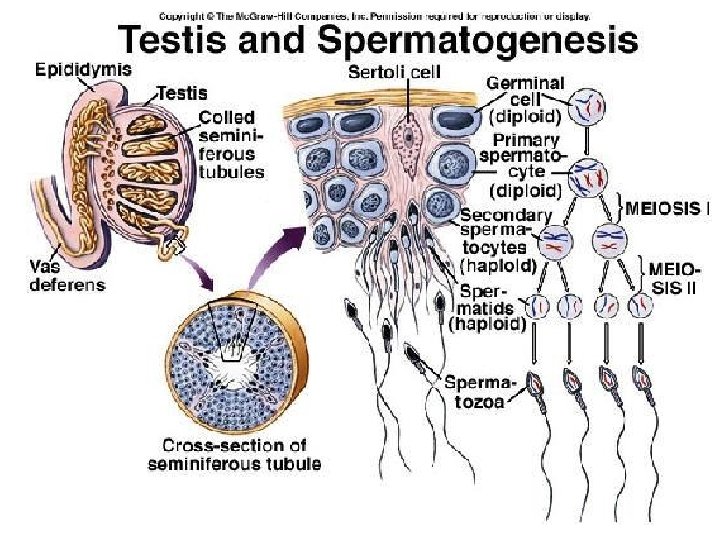
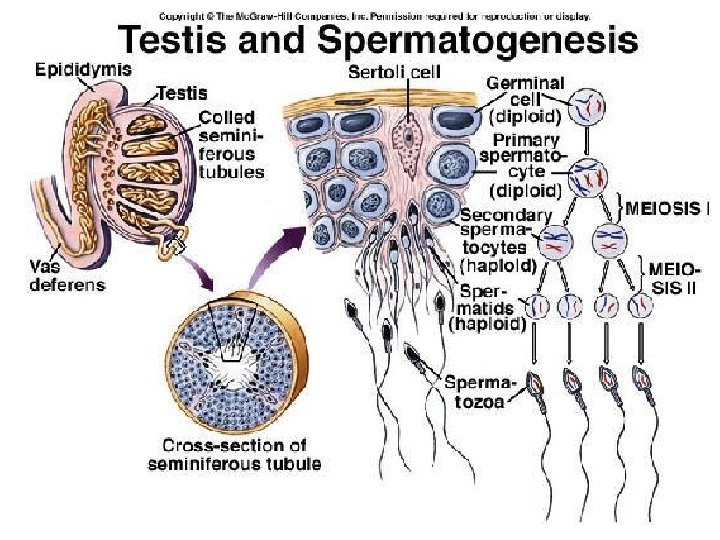
-Testes wall made of fibrous connective tissue (Divides the testes into lobules (Chambers) - Inside chambers are long tubes (70 cm) called the Seminiferous tubules). - This is the actual site for spermatogenesis. - Interstitial cells secretes androgens “testosterone”
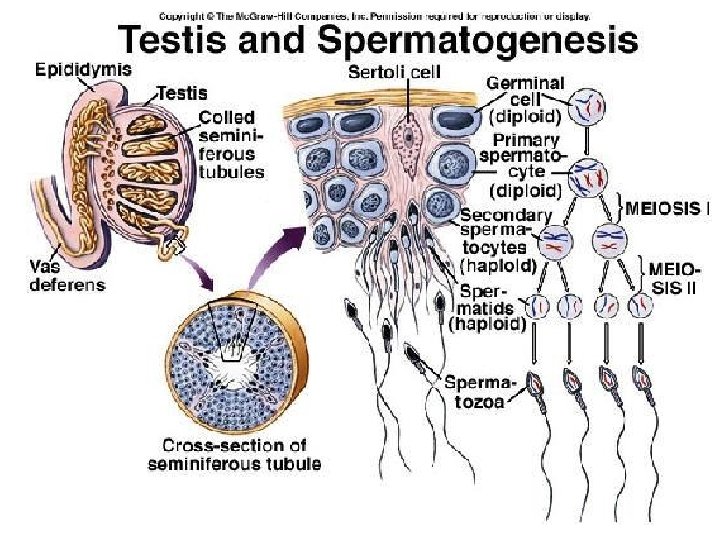

Spermatogenesis –Sperm Development Sperms cells are derived from undifferentiated cells called SPERMATOGONIA (sing. Spermatogonium), which lie just on the outside wall of a tubule and divide mitotically (dividing into copies), always producing new spermatogonia.
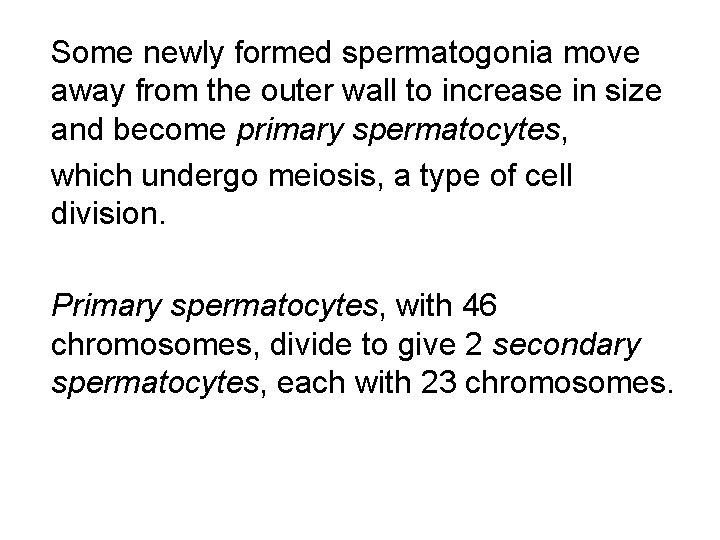
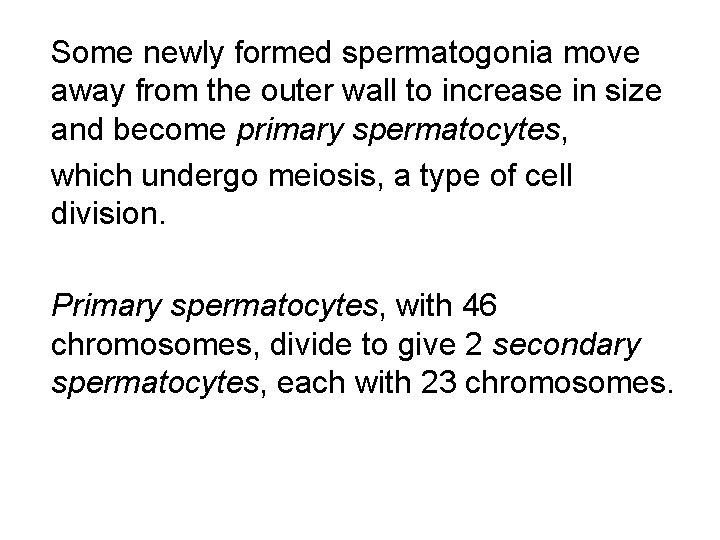
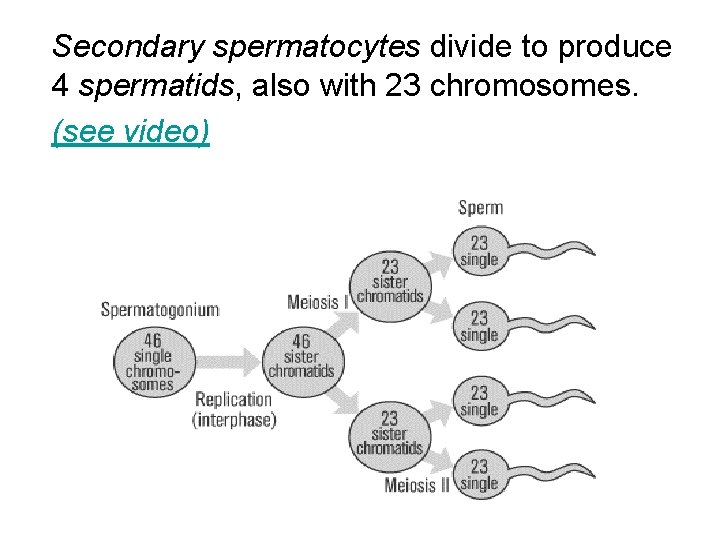
Some newly formed spermatogonia move away from the outer wall to increase in size and become primary spermatocytes, which undergo meiosis, a type of cell division. Primary spermatocytes, with 46 chromosomes, divide to give 2 secondary spermatocytes, each with 23 chromosomes.
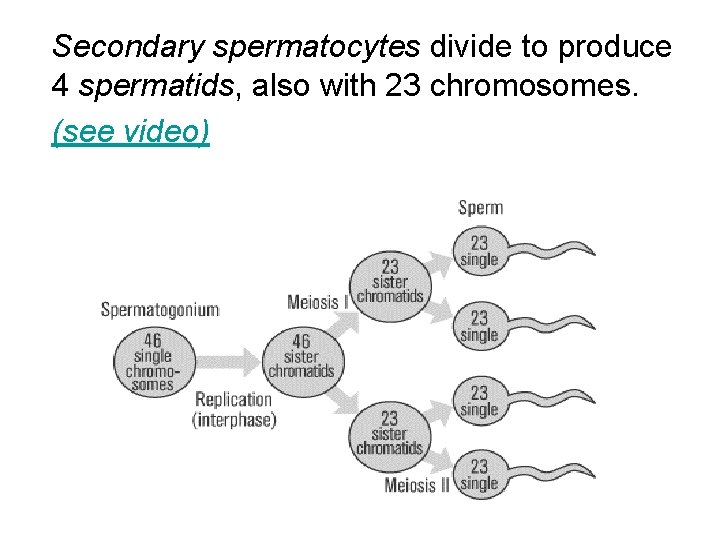
Secondary spermatocytes divide to produce 4 spermatids, also with 23 chromosomes. (see video)
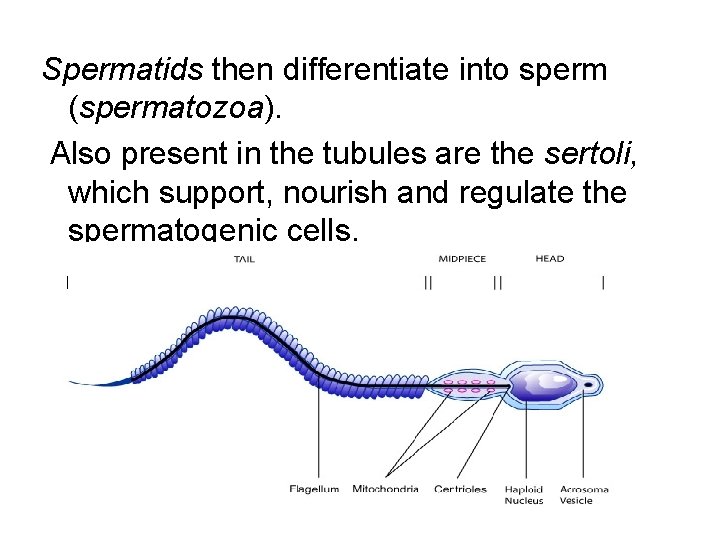
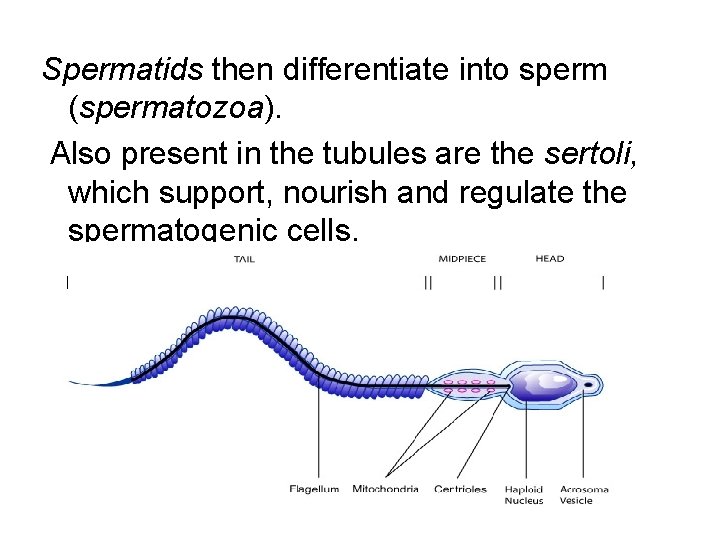
Spermatids then differentiate into sperm (spermatozoa). Also present in the tubules are the sertoli, which support, nourish and regulate the spermatogenic cells.

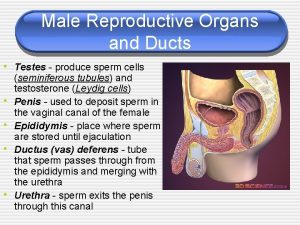
Epididymus -Stores sperm as they mature Seminal Vesicle -Contributes to seminal fluid Cowper’s Gland -Pea-sized organs that lie posterior to the prostate on either side of the urethra. -Contributes to seminal fluid

Prostate Gland -A single dough-nut shaped gland that surrounds the upper portion of the urethra just below the bladder.
- Older men can have their prostate become enlarged and urination becomes quite painful. (surgically fixed) - Helps produce seminal fluid
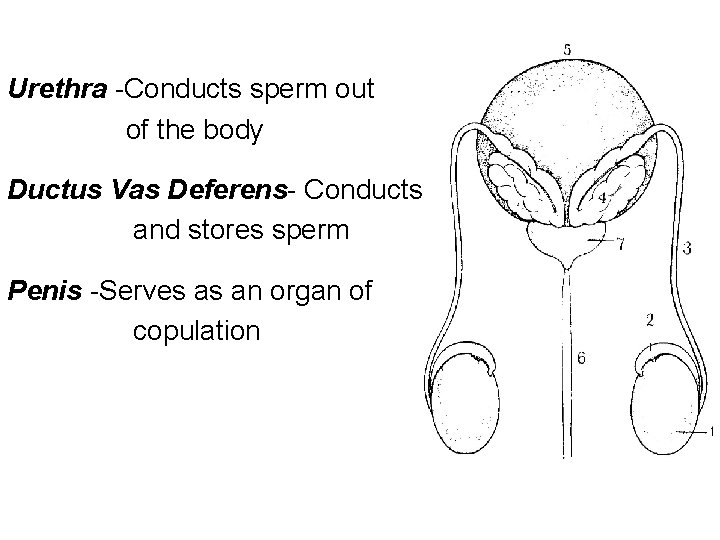
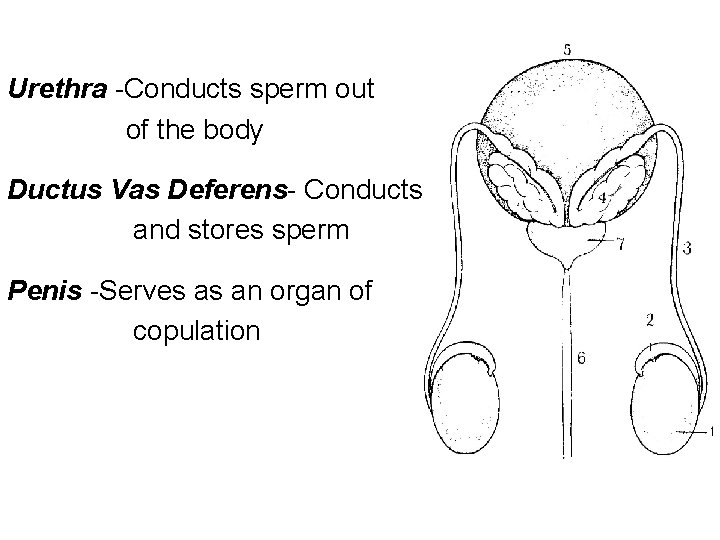
Urethra -Conducts sperm out of the body Ductus Vas Deferens- Conducts and stores sperm Penis -Serves as an organ of copulation

Path of Sperm 1. Formed in the seminiferous tubules of the testes 2. Mature and stored in the epididymus 3. Stored in the Vas Deferens 4. Enters the urethra just prior to ejaculation 5. Accessory glands (prostate, Cowper’s gland, and seminal vesicle) add secretions to semen. 6. Semen and sperm exit through the penis.
Seminal Fluid SOURCES: 1. Seminal Vesicle 2. Prostate Gland 3. Cowper’s Gland
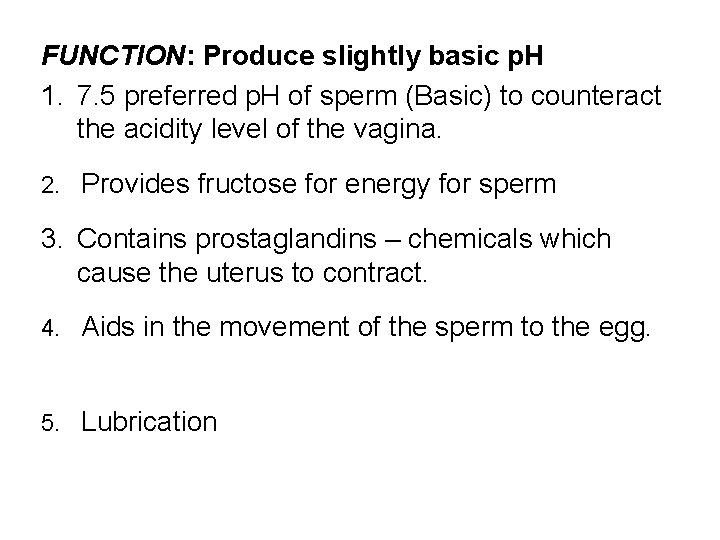
FUNCTION: Produce slightly basic p. H 1. 7. 5 preferred p. H of sperm (Basic) to counteract the acidity level of the vagina. 2. Provides fructose for energy for sperm 3. Contains prostaglandins – chemicals which cause the uterus to contract. 4. Aids in the movement of the sperm to the egg. 5. Lubrication
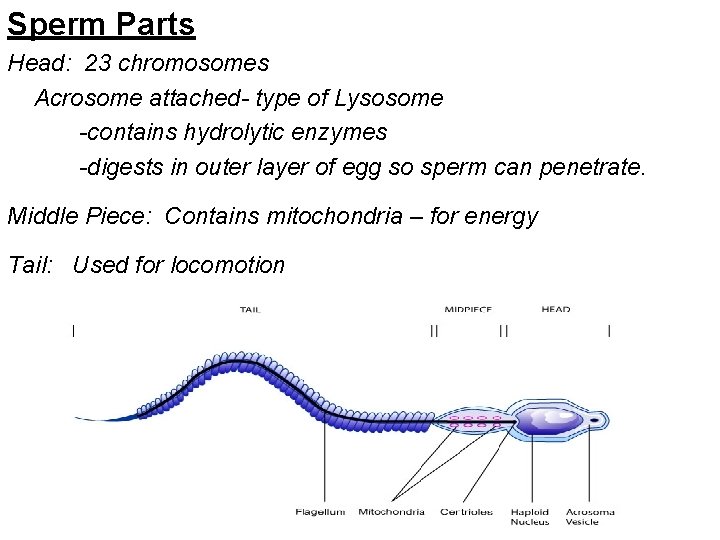
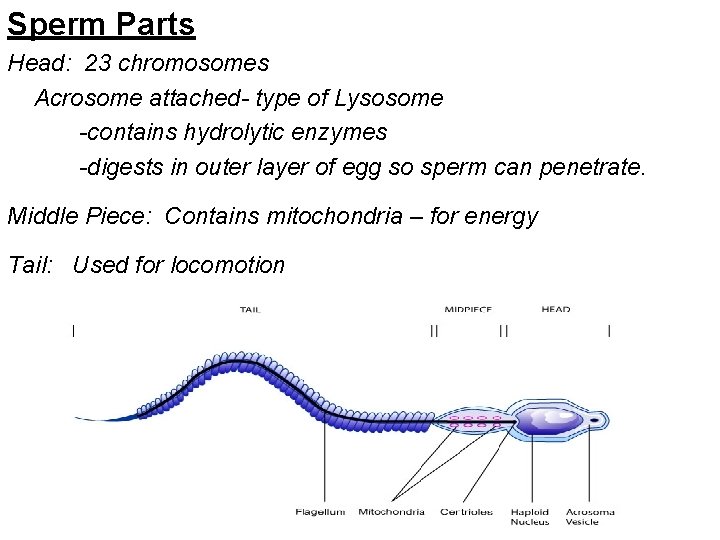
Sperm Parts Head: 23 chromosomes Acrosome attached- type of Lysosome -contains hydrolytic enzymes -digests in outer layer of egg so sperm can penetrate. Middle Piece: Contains mitochondria – for energy Tail: Used for locomotion
Function of Testosterone 1. Essential for development of primary sex organs. 2. Essential for the development of sperm -spermatogenic cells take up testosterone which stimulate their activity. 3. Increased testosterone concentration at puberty causes maturation of penis and testes.
4. Secondary Sex Characteristics -facial hair -larynx expands (voice changes) -armpit hair -Increase muscular strength -pubic hair -aggression -oil and sweat -sex drive glands secrete(=Stinky)

Hormonal Control of Testosterone -Hypothalamus releases Gn. RH (Gonadotropic releasing hormone) -Gn. RH causes anterior pituitary to release 2 gonadotropic hormones:
FSH (Follicle stimulating hormone) -promotes spermatogenesis in the seminiferous tubules LH (Leutenizing Hormone) -promotes production of testosterone in interstitial cells.
NEGATIVE FEEDBACK Increased testosterone concentration in the blood causes the anterior pituitary to make less LH, therefore less testosterone is produced. Decreased testosterone concentration in the blood causes the anterior pituitary to make more LH and therefore more testosterone is produced.
Increased concentration of stored sperm causes an increase in production of inhibin and decreases production of FSH, therefore production of sperm decreases. Decreased concentration of stored sperm causes a decrease in production of inhibin and more FSH, therefore more sperm is produced.
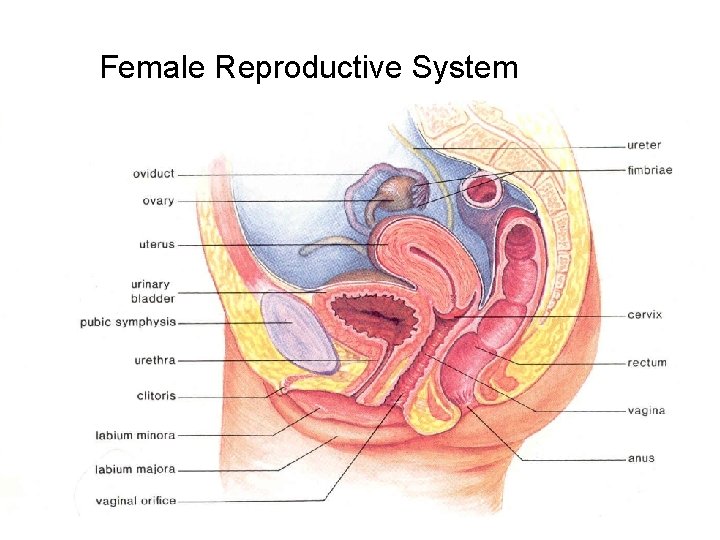
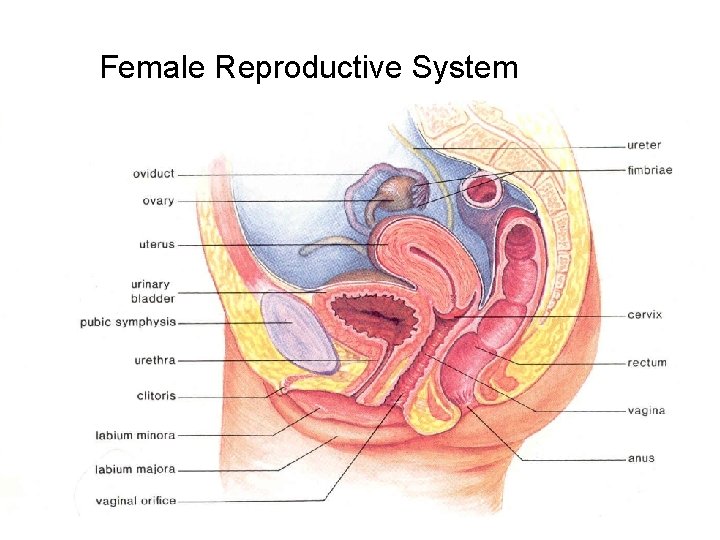
Female Reproductive System
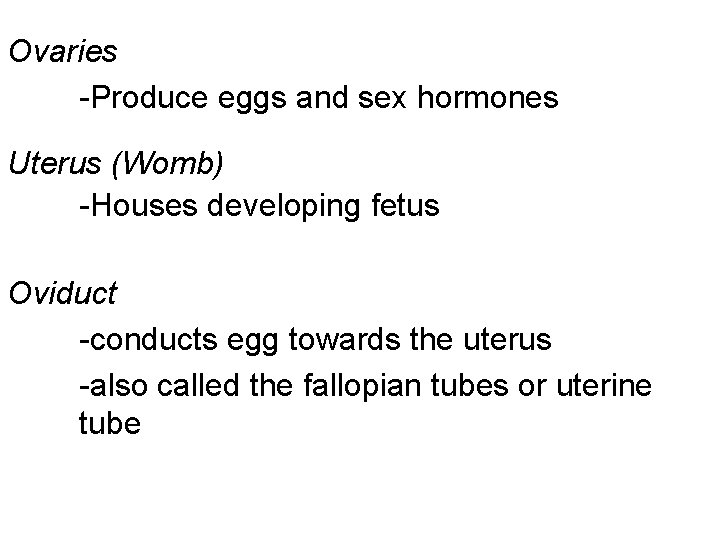
Ovaries -Produce eggs and sex hormones Uterus (Womb) -Houses developing fetus Oviduct -conducts egg towards the uterus -also called the fallopian tubes or uterine tube
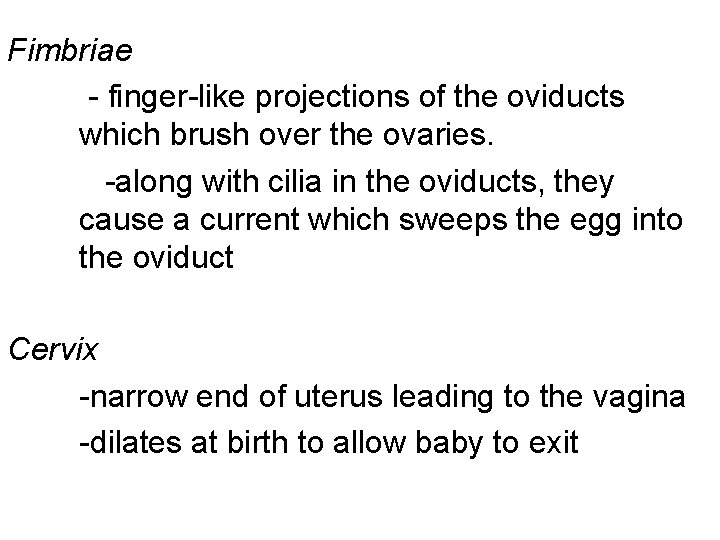
Fimbriae - finger-like projections of the oviducts which brush over the ovaries. -along with cilia in the oviducts, they cause a current which sweeps the egg into the oviduct Cervix -narrow end of uterus leading to the vagina -dilates at birth to allow baby to exit

Vagina -Receives penis during sexual intercourse and serves as a birth canal Clitoris -female sensory organ; homologous to the male penis -provides sensitivity during intercourse Labia major and Labia minor -protective folds of skin which surround and protect the clitoris and the openings of the vagina and urethra
Functions of Estrogen (Female Sex Hormone) 1. Stimulates growth of uterus and vagina at puberty 2. Egg maturation 3. Secondary Sex Characteristics: -armpit hair / pubic hair -fat distribution beneath skin -enlarged pelvic girdle (wider hips) -breast development (requires progesterone as well)

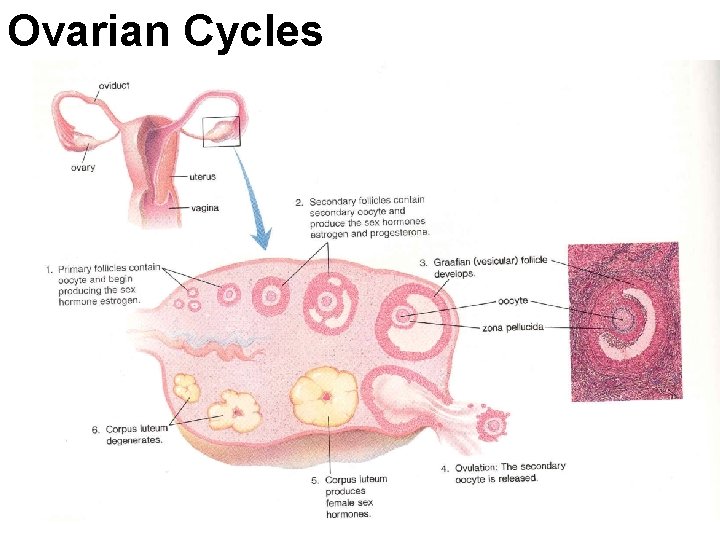
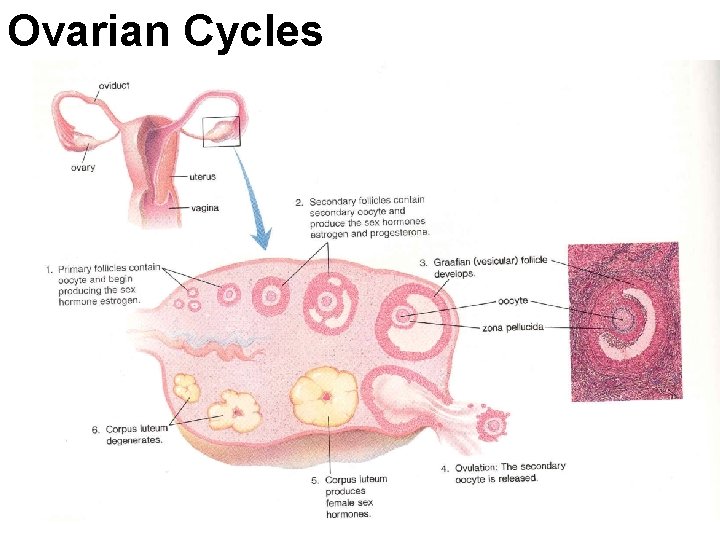
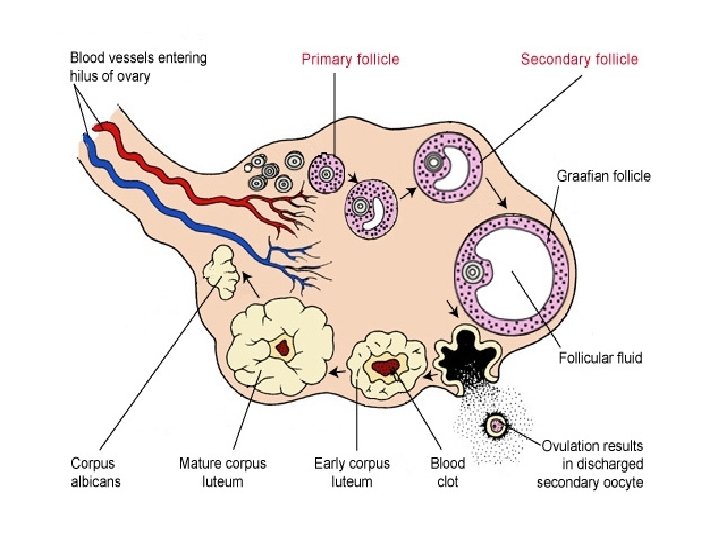
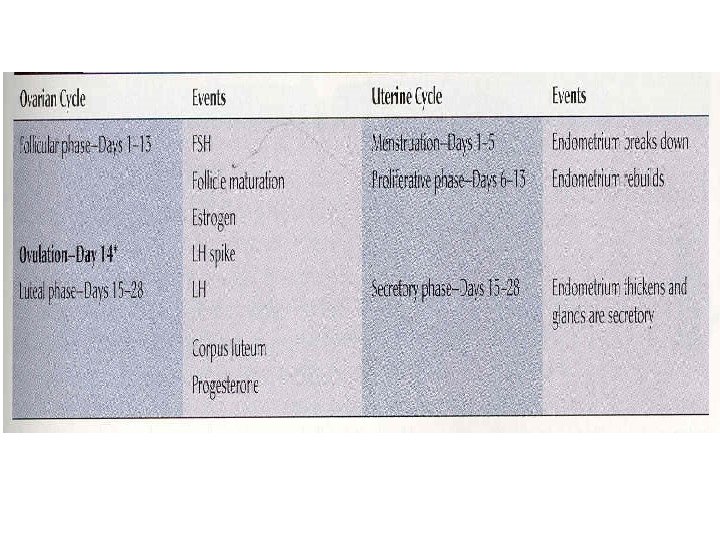
Ovarian Cycles

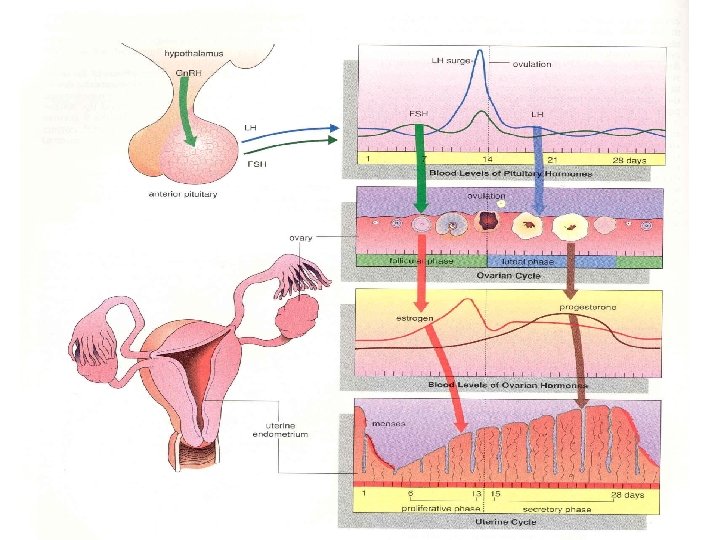
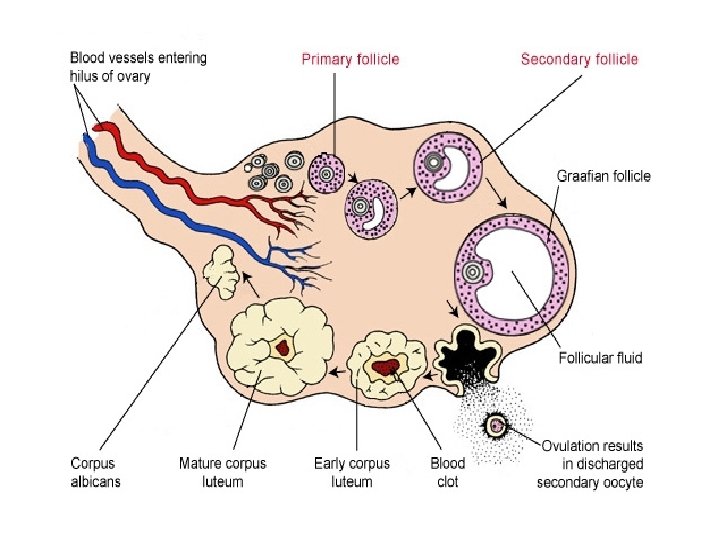
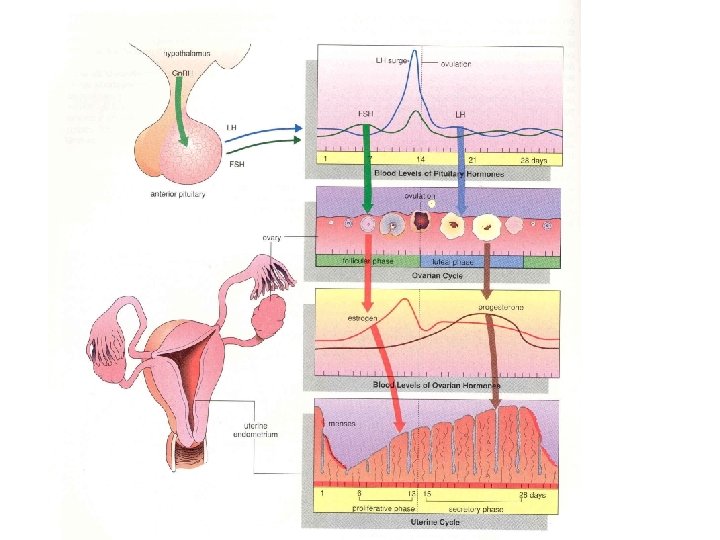
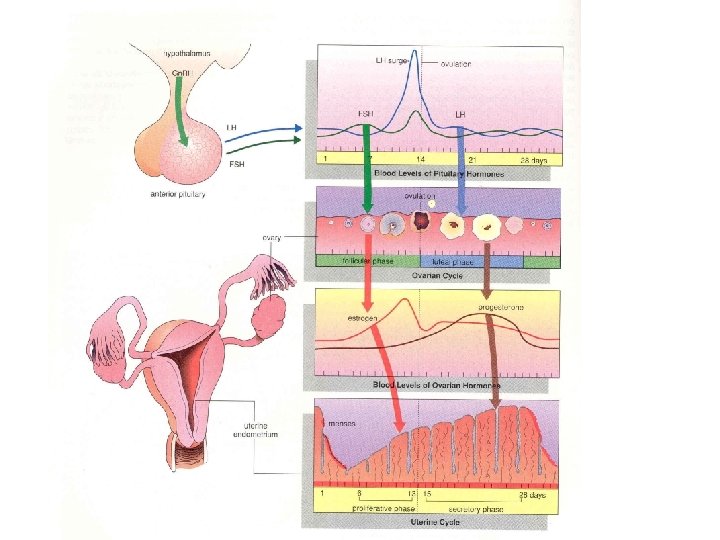
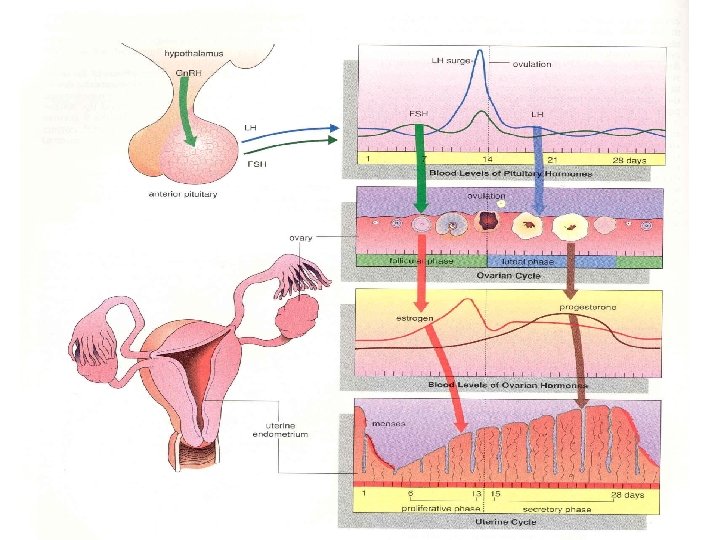
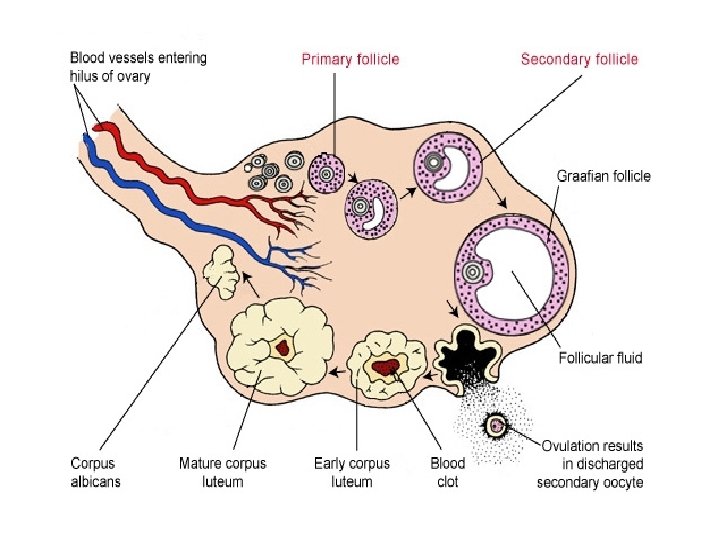
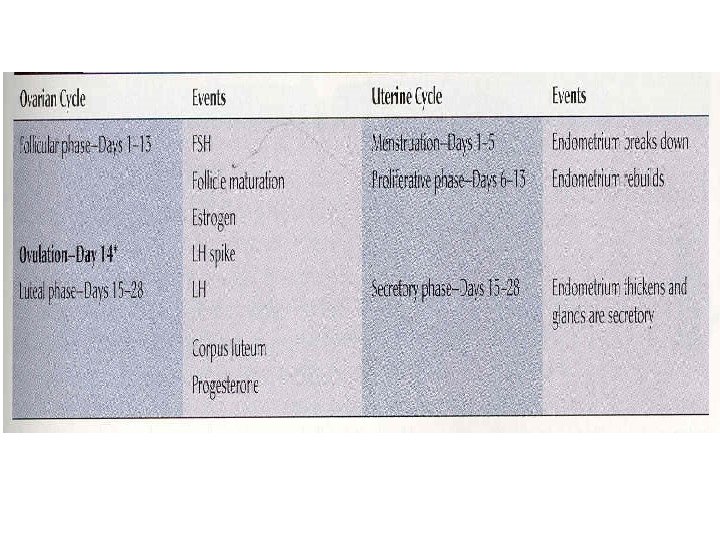
(see video) Day 1 – 13 Follicular Phase 1. Hypothalamus produces a Gn. RH to stimulate Anterior lobe of pituitary 2. FSH and LH stimulates ovary for follicle growth from pituitary gland
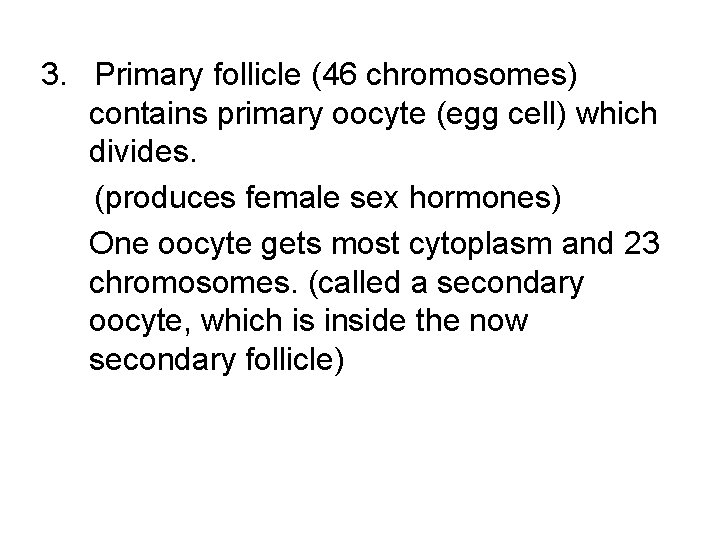
3. Primary follicle (46 chromosomes) contains primary oocyte (egg cell) which divides. (produces female sex hormones) One oocyte gets most cytoplasm and 23 chromosomes. (called a secondary oocyte, which is inside the now secondary follicle)

4. Other oocyte called the polar body disintegrates 5. The secondary follicle grows into a Grafian (vesicular) Follicle.

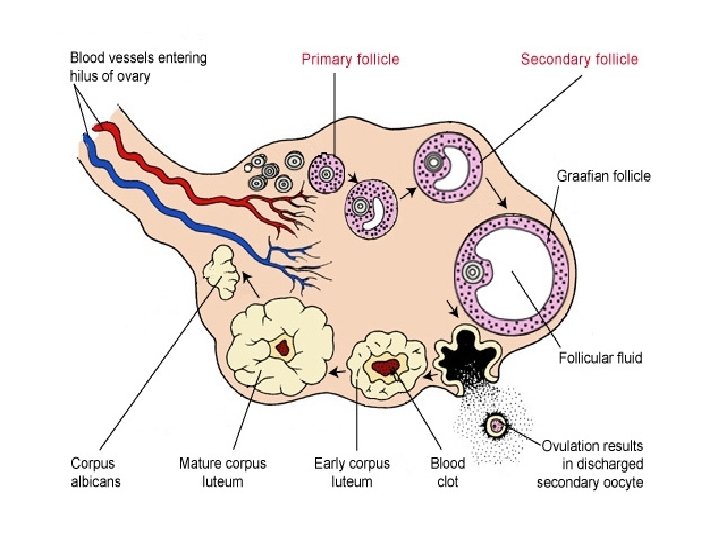
Day 14 Ovulation 6. Grafian Follicle bursts (ovulation) LH is at its highest and triggers ovulation

Day 15 – 28 Luteal Phase 7. The follicle has lost its oocyte (or “egg”) and forms into the Corpus Luteum. (LH causes the corpus luteum to form. ) -the corpus luteum secretes hormones -estrogen and progesterone (see video)
If pregnancy (fertilization) does not occur: Corpus Luteum breaks down (about 10 days) Cycle will repeat. If pregnancy does occur: Corpus luteum remains for 3 – 6 months and continues to produce hormones.
Uterine Cycle Day 1 – 5 Menstruation 1. Low levels of sex hormones (Corpus Luteum has just disintegrated) 2. Endometrium (lining of Uterus) breaks down

3. Cells of the endometrium, blood vessels, and blood are shedding from the uterus and exit the vagina. 4. A flow of blood (called menses) passes out of the vagina during a period called menstruation.
Day 6 – 13 Proliferative phase 1. Increase estrogen by the ovarian follicle causes the endometrium to rebuild. 2. Endometrium becomes thick and vascularized

Day 14 Ovulation occurs (release of the egg) Day 15 – 28 Secretory Phase 1. Increase level of progesterone by the corpeus luteum 2. Endometrium doubles in thickness 3. Glands produce mucous 4. Now prepared to receive embryo (see video)

If no pregnancy, the corpeus luteum degenerates, decrease in progesterone production occurs and the endometrium breaks down. Cycle continues.
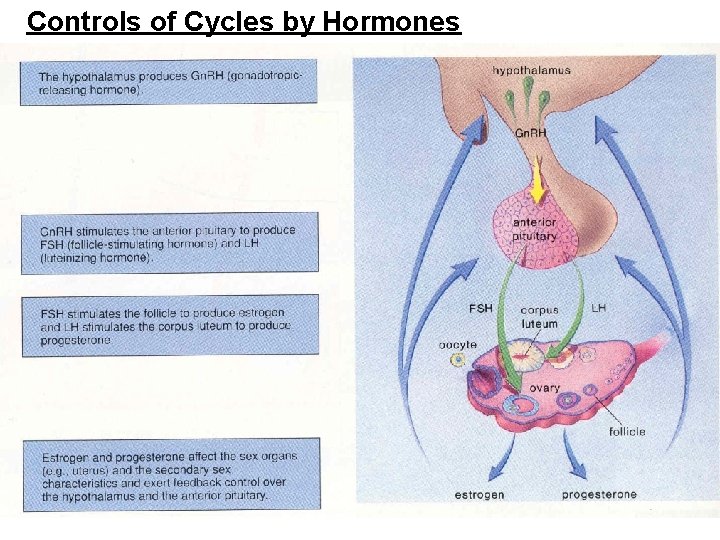
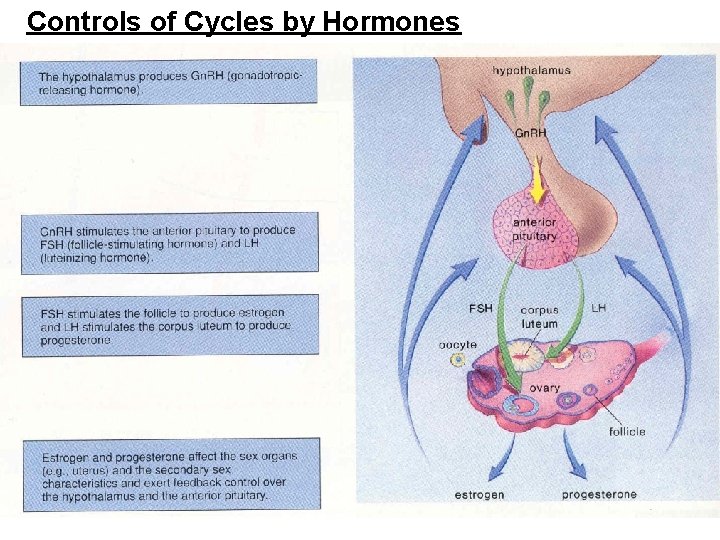
Controls of Cycles by Hormones

Hypothalamus secretes Gn. RH (gonadotropic releasing hormone) and causes the anterior pituitary to secrete FSH and LH FSH causes follicles to mature. Maturing follicles produce estrogen. Increase in estrogen concentration causes the anterior pituitary to stop producing FSH and LH(negative feedback)
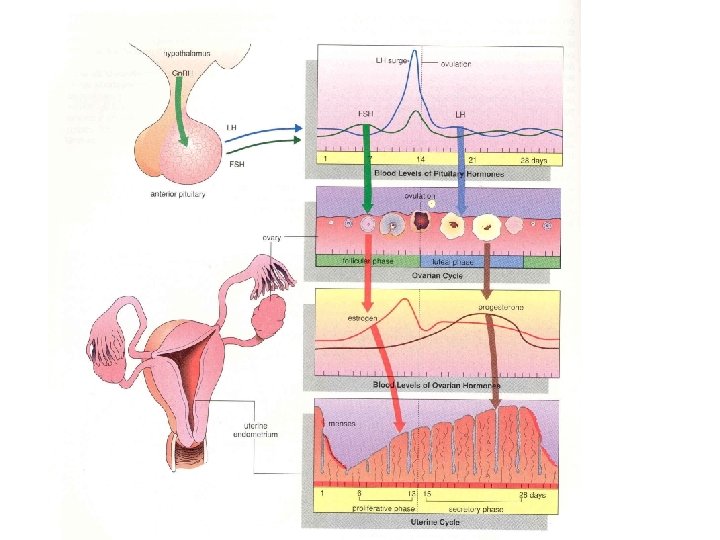
Around day 12, the increased levels of estrogen suddenly cause positive feedback on the anterior pituitary and stimulate the release of FSH and large amounts of LH. This surge of LH triggers ovulation. LH then triggers the remaining follicle cells to differentiate into the corpus luteum which secretes progesterone and some estrogen.


Estrogen promotes the thickening of the endometrium Progesterone stimulates the endometrium to mature and become secretory. These changes are to prepare for the possibility of fertilization, implantation and pregnancy.
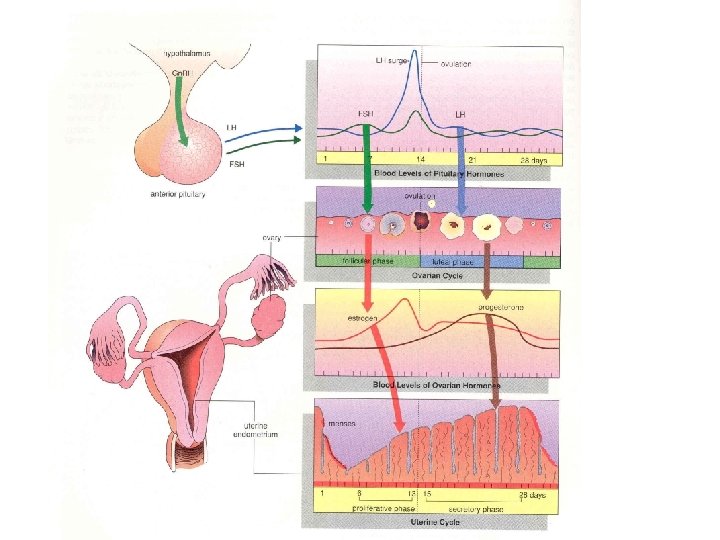
At the end of the cycle, if the egg has not been fertilized or implantation and pregnancy do not occur, the corpus luteum breaks down and stops releasing estrogen and progesterone. Without these hormones, the uterine lining (endometrium) breaks down and menstruation starts.


Implantation Fertilization (sperm cell enters the oocyte) occurs in the oviduct. The joining of the two cells forms an embryo. Implantation of the embryo occurs in the uterus. Embryo embeds itself in the endometrium several days after fertilization. Pregnancy has now begun.


Implantation starts the production of the hormone HCG (Human Chorionic Gonadotropin) which prevents the corpus luteum from degenerating. It is found immediately in blood and a few days later in the urine. Ex. Pregnancy test. (About one week later)
HCG prevents the breakdown of the Corpus Luteum. The Corpus Luteum produces progesterone that keeps the endometrium from breaking down. FSH and LH production is inhibited which stops the egg from being released.
The placenta begins to develop from embryonic and maternal tissues after implantation. Placenta Contains both maternal and fetal tissue Area where gas and nutrients exchange occurs. No exchange of blood Diffusion of gases and wastes and nutrients occur over the cell layers
Placenta produces HCG, progesterone (prevents breakdown of the endometrium) and estrogen (keeps new egg from developing)
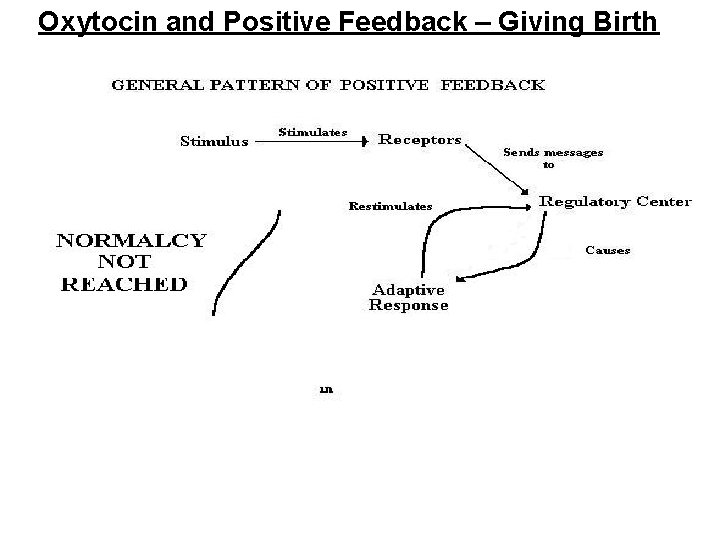
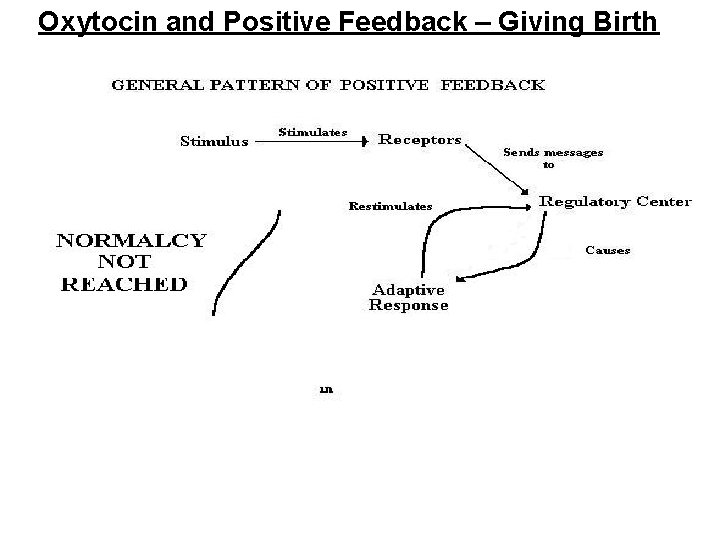
Oxytocin and Positive Feedback – Giving Birth
Oxytocin used to induce birth. Oxytocin causes uterine contractions, which in turn stimulate the release of more oxytocin. Positive feedback. Oxytocin also causes mammary glands to release milk. Lobules containing milk contract forcing milk into ducts which lead to the nipple.
 Sex sex sex
Sex sex sex Sex sex sex
Sex sex sex Snv sex
Snv sex Sex sex sex
Sex sex sex Sex sex sex
Sex sex sex Killer whale eating sea lion
Killer whale eating sea lion What hormone does the testes produce
What hormone does the testes produce Where is sperm stored in the male body
Where is sperm stored in the male body Mesovarium
Mesovarium Pathway of sperm in male reproductive system
Pathway of sperm in male reproductive system Hare lynx
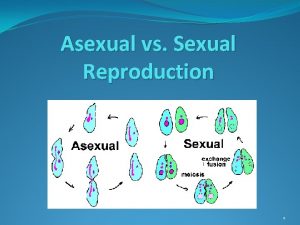
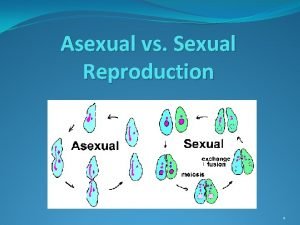
Hare lynx Asexual reproduction vs sexual reproduction venn diagram
Asexual reproduction vs sexual reproduction venn diagram The disadvantages of sexual reproduction
The disadvantages of sexual reproduction Primary sex organ of the male reproductive system? *
Primary sex organ of the male reproductive system? * Androgen insensitivity
Androgen insensitivity A combining form for the male sex cell is
A combining form for the male sex cell is Uncircumcised gentiles photos
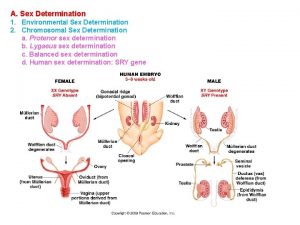
Uncircumcised gentiles photos Sex determination and sex linkage
Sex determination and sex linkage Once a sex offender always a sex offender
Once a sex offender always a sex offender X linked punnett square
X linked punnett square Heterogametic
Heterogametic Spermogensis
Spermogensis Testis and spermatogenesis
Testis and spermatogenesis Monads and gonads
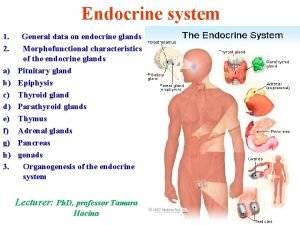
Monads and gonads Gonads
Gonads What is gonad
What is gonad Gonads
Gonads Steroids endocrine system
Steroids endocrine system What are gonads
What are gonads Lymphatic drainage of vulva
Lymphatic drainage of vulva Starfish mouth
Starfish mouth Gonads glands
Gonads glands Squid gonads
Squid gonads Projeção psicanálise
Projeção psicanálise Testes
Testes Testes
Testes Testes neuropsicopedagógicos pdf
Testes neuropsicopedagógicos pdf Spermatocyte
Spermatocyte Fertilization and implantation
Fertilization and implantation Testes psicométricos
Testes psicométricos Diploid
Diploid Cretinism
Cretinism Testes
Testes Spermatolysis adalah
Spermatolysis adalah Perch external anatomy
Perch external anatomy Cow male reproductive system
Cow male reproductive system Oogenesi
Oogenesi Frog lungs
Frog lungs Paula melo silva
Paula melo silva Spermatolysis adalah
Spermatolysis adalah Hormones testes
Hormones testes Tabela tukey
Tabela tukey Testicular function
Testicular function Drawing of the male and female reproductive system
Drawing of the male and female reproductive system Antebraçi
Antebraçi Mediastinum testis
Mediastinum testis Testes regressivos
Testes regressivos Requirements for natural selection
Requirements for natural selection Female reproductive system diseases
Female reproductive system diseases Gliserofosfokolin sperm
Gliserofosfokolin sperm A spermatocyte produces the following four sperm cells
A spermatocyte produces the following four sperm cells Wasting sperm
Wasting sperm Intervilozni prostor
Intervilozni prostor What adds sugary fluid to sperm
What adds sugary fluid to sperm Semen protein
Semen protein Sperm whale range map
Sperm whale range map What is the joining of egg and sperm called
What is the joining of egg and sperm called Sperm cell
Sperm cell Sperm nucleus
Sperm nucleus Spermatozoa in urine
Spermatozoa in urine Base represent totality
Base represent totality What is seminal vesicle in male reproductive system
What is seminal vesicle in male reproductive system Sperm analysis chart
Sperm analysis chart Where is sperm produced
Where is sperm produced