Reproductive System Explain the structure of the male


- Slides: 13
Reproductive System Explain the structure of the male reproductive system Analyze the function of the male reproductive system Explain the structure of the female reproductive system Analyze the function of the female reproductive system Discuss characteristics and treatment of common reproductive disorders
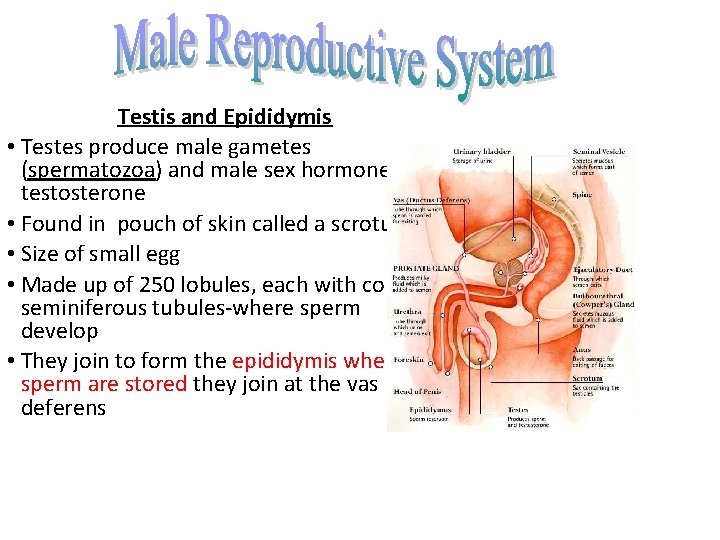
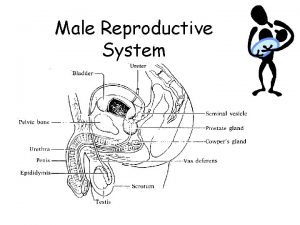
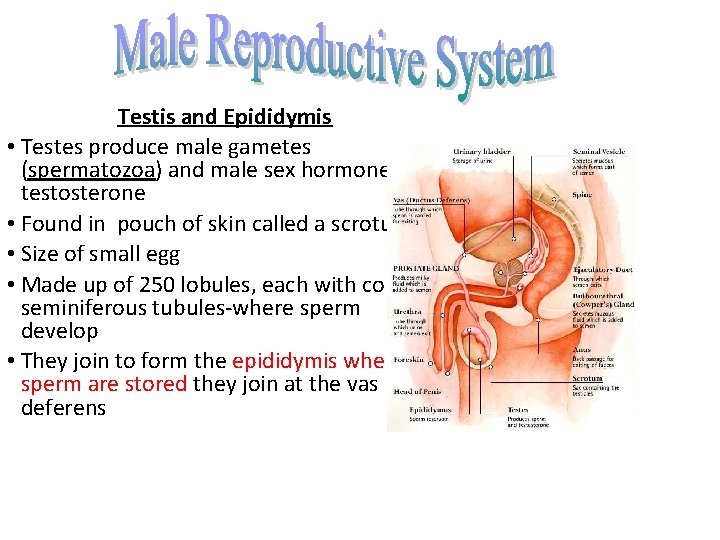
Testis and Epididymis • Testes produce male gametes (spermatozoa) and male sex hormonetestosterone • Found in pouch of skin called a scrotum • Size of small egg • Made up of 250 lobules, each with coiled seminiferous tubules-where sperm develop • They join to form the epididymis where sperm are stored they join at the vas deferens


Vas Deferens • Runs from epididymis to ejaculatory duct • Seminal vesicles connect to vas deferens secretion nourish sperm • Ejaculatory duct- connect vas deferens with urethra Scrotum Sac of skin that contains testes Descent of the testes • In embryo, testes formed in the abdomen • During last 3 months, migrate into scrotum Penis • Contains erectile tissue • End of penis covered by loose fitting skin –foreskin • Foreskin removed during circumcision
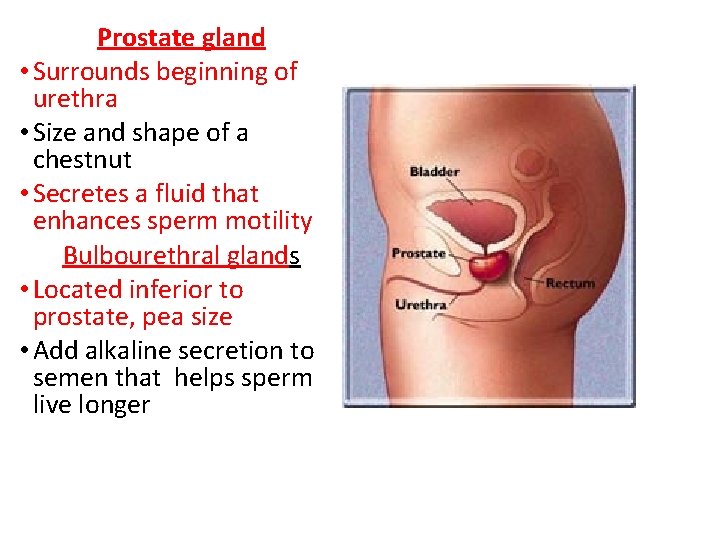
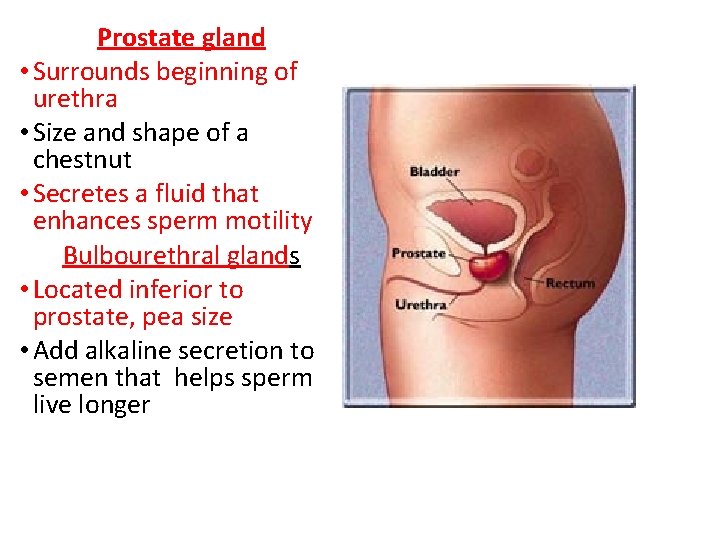
Prostate gland • Surrounds beginning of urethra • Size and shape of a chestnut • Secretes a fluid that enhances sperm motility Bulbourethral glands • Located inferior to prostate, pea size • Add alkaline secretion to semen that helps sperm live longer
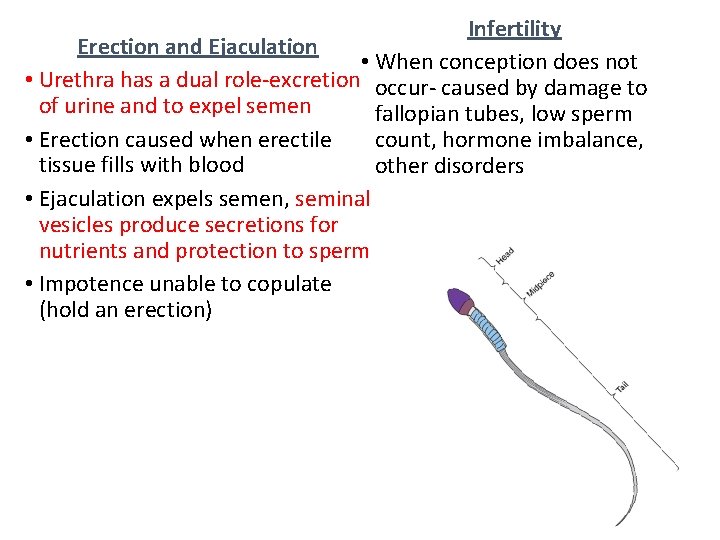
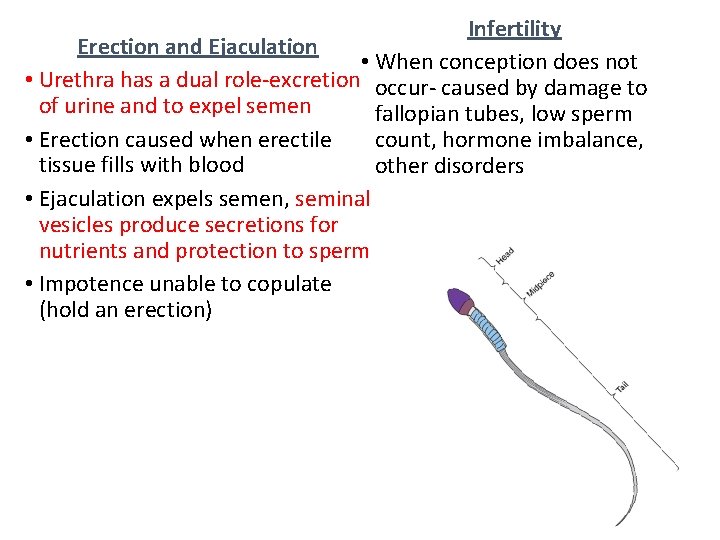
Infertility Erection and Ejaculation • When conception does not • Urethra has a dual role-excretion occur- caused by damage to of urine and to expel semen fallopian tubes, low sperm • Erection caused when erectile count, hormone imbalance, tissue fills with blood other disorders • Ejaculation expels semen, seminal vesicles produce secretions for nutrients and protection to sperm • Impotence unable to copulate (hold an erection)
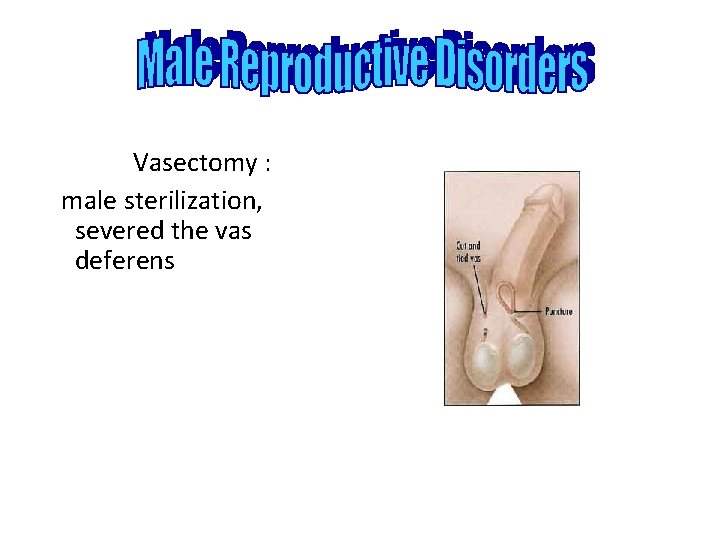
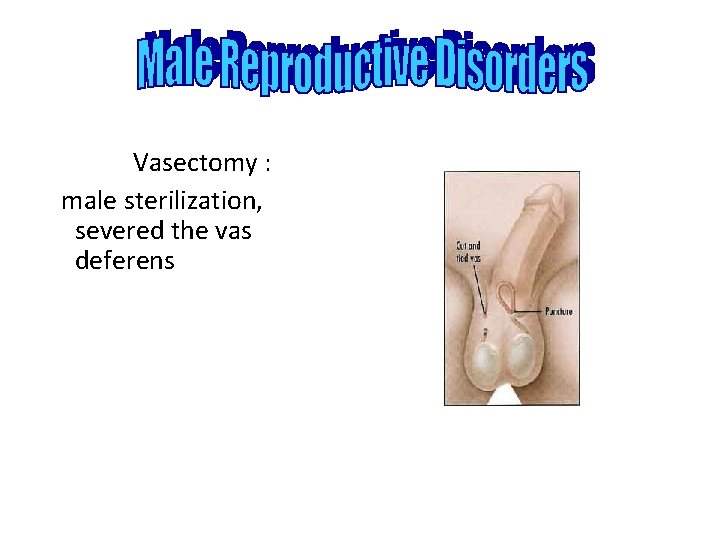
Vasectomy : male sterilization, severed the vas deferens
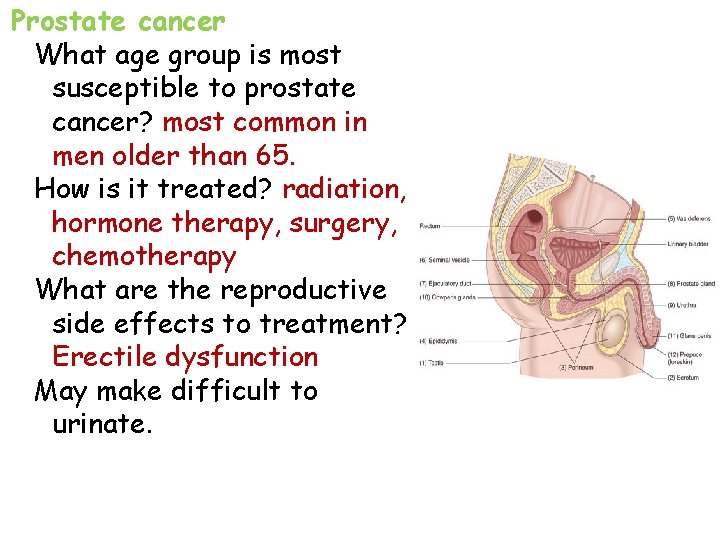
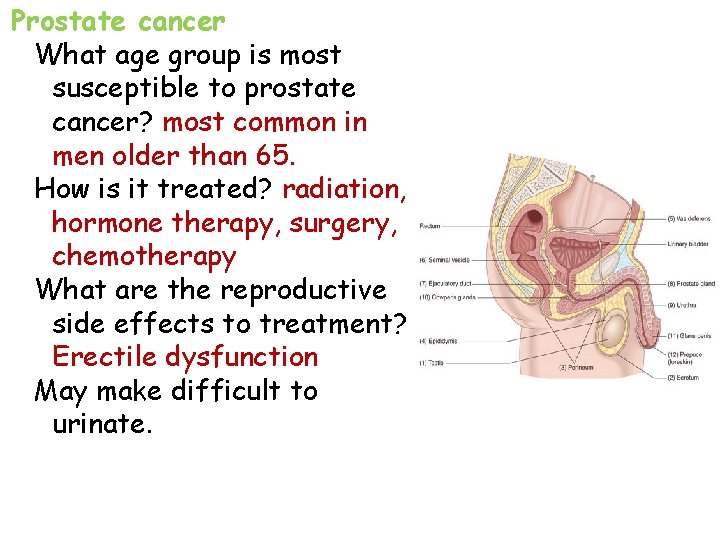
Prostate cancer What age group is most susceptible to prostate cancer? most common in men older than 65. How is it treated? radiation, hormone therapy, surgery, chemotherapy What are the reproductive side effects to treatment? Erectile dysfunction May make difficult to urinate.
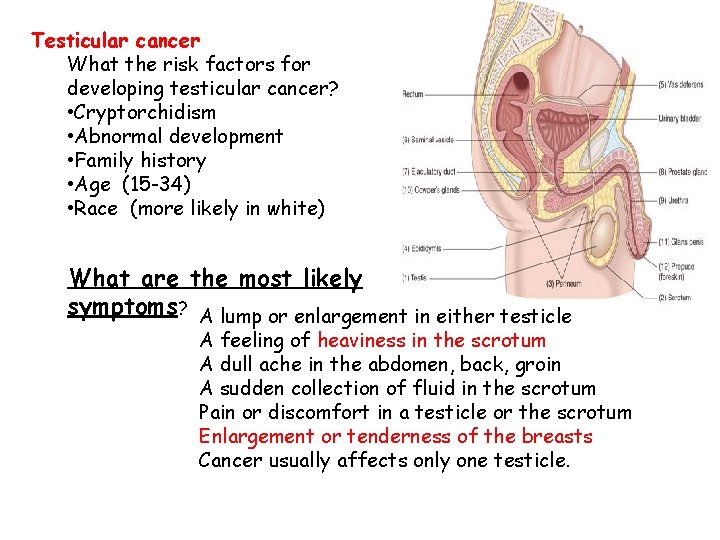
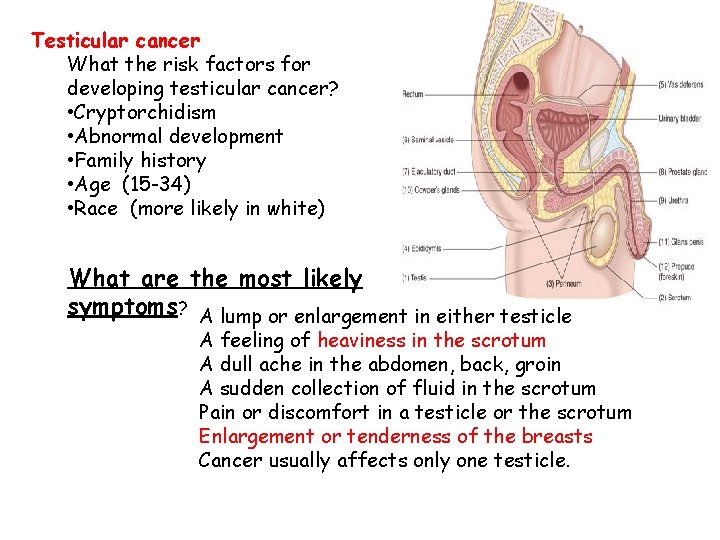
Testicular cancer What the risk factors for developing testicular cancer? • Cryptorchidism • Abnormal development • Family history • Age (15 -34) • Race (more likely in white) What are the most likely symptoms? A lump or enlargement in either testicle A feeling of heaviness in the scrotum A dull ache in the abdomen, back, groin A sudden collection of fluid in the scrotum Pain or discomfort in a testicle or the scrotum Enlargement or tenderness of the breasts Cancer usually affects only one testicle.
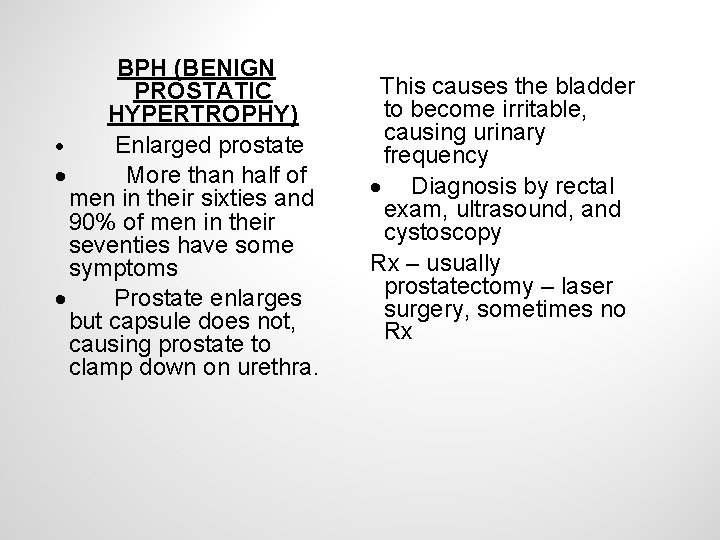
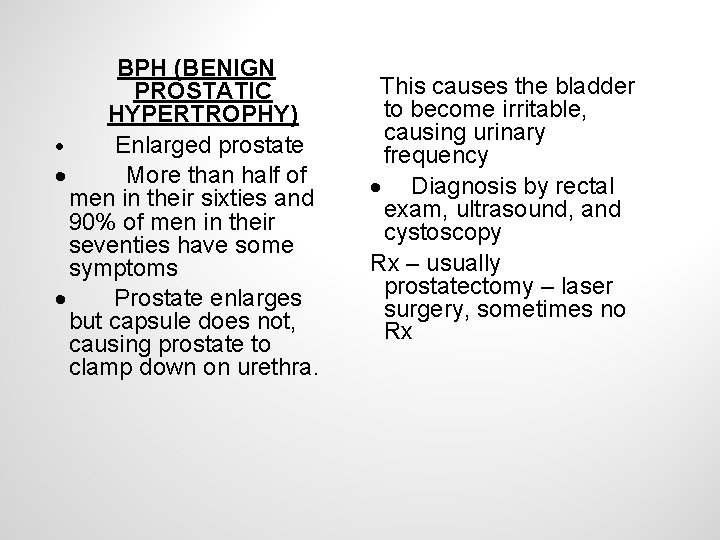
BPH (BENIGN PROSTATIC HYPERTROPHY) · Enlarged prostate · More than half of men in their sixties and 90% of men in their seventies have some symptoms · Prostate enlarges but capsule does not, causing prostate to clamp down on urethra. This causes the bladder to become irritable, causing urinary frequency · Diagnosis by rectal exam, ultrasound, and cystoscopy Rx – usually prostatectomy – laser surgery, sometimes no Rx
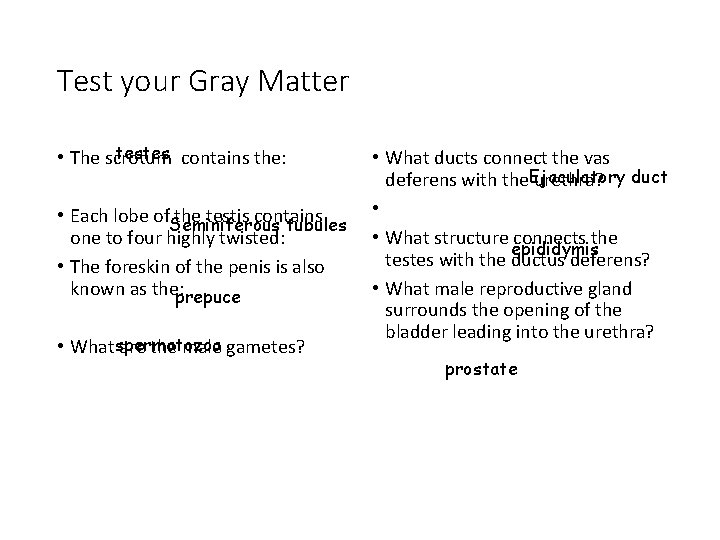
Test your Gray Matter testes contains the: • The scrotum • Each lobe of. Seminiferous the testis contains tubules one to four highly twisted: • The foreskin of the penis is also known as the: prepuce • Whatspermatozoa are the male gametes? • What ducts connect the vas deferens with the. Ejaculatory urethra? duct • • What structure connects the epididymis testes with the ductus deferens? • What male reproductive gland surrounds the opening of the bladder leading into the urethra? prostate
The prostate gland is the size and shape of a: Chestnut or strawberry The external organs of the male reproductive system are the: Scrotum + penis The vas deferens begins in the: scrotum Sperm are produced in the: testes The male hormone produced by testosterone the testes is: Sperm are stored in the: epididymis Which of the following glands does not produce a secretion to transport sperm? Bartholin’s gland, Cowpers gland, Prostate gland, or Seminal vesicles What structure serves as a storage site for sperm and as the excretory duct of the testis? Vas deferens
 Male reproductive system in plant
Male reproductive system in plant Function of cervix
Function of cervix Reproductive hygiene
Reproductive hygiene Drawing of the male and female reproductive system
Drawing of the male and female reproductive system Anatomy of the reproductive system exercise 42
Anatomy of the reproductive system exercise 42 Male reproductive system lateral view
Male reproductive system lateral view Broad ligament
Broad ligament Female and male reproductive system
Female and male reproductive system Figure 16-1 male reproductive system
Figure 16-1 male reproductive system Reproductive physiology
Reproductive physiology Art-labeling activity: the male reproductive system, part 1
Art-labeling activity: the male reproductive system, part 1 Male reproductive system information
Male reproductive system information Where is sperm located
Where is sperm located Bull reproductive system parts and functions
Bull reproductive system parts and functions