Male Reproductive System Male Reproductive System The Scrotum

- Slides: 25
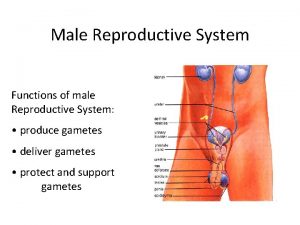
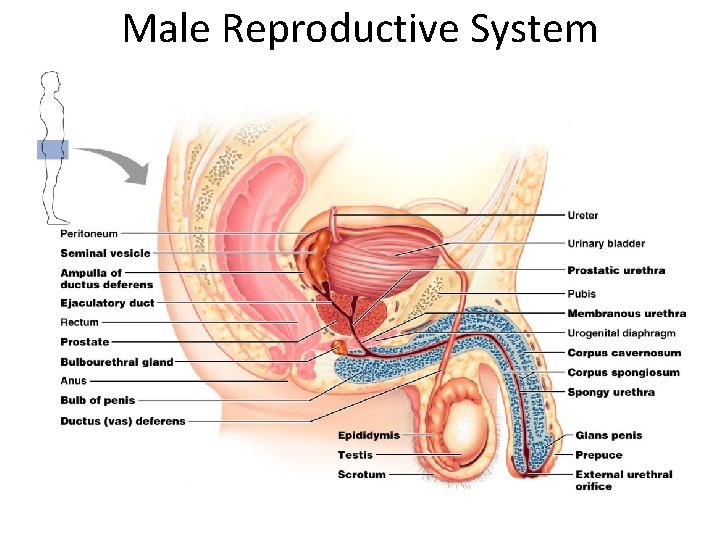
Male Reproductive System
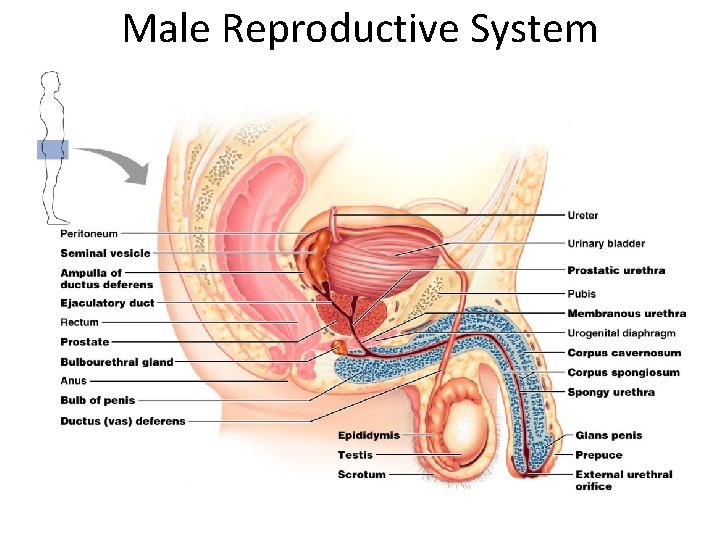
Male Reproductive System
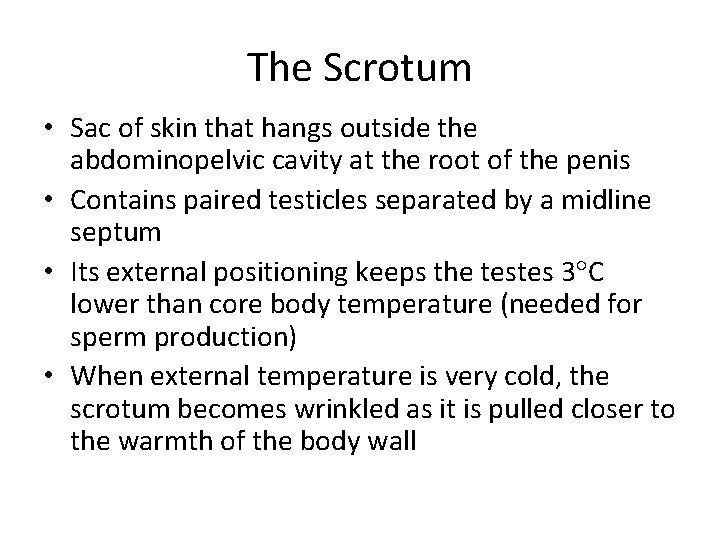
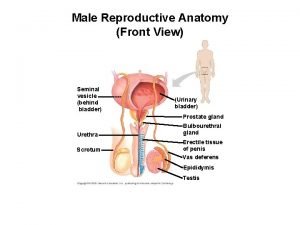
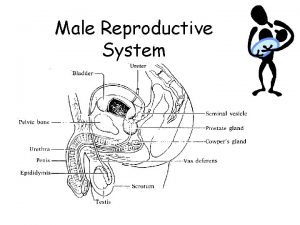
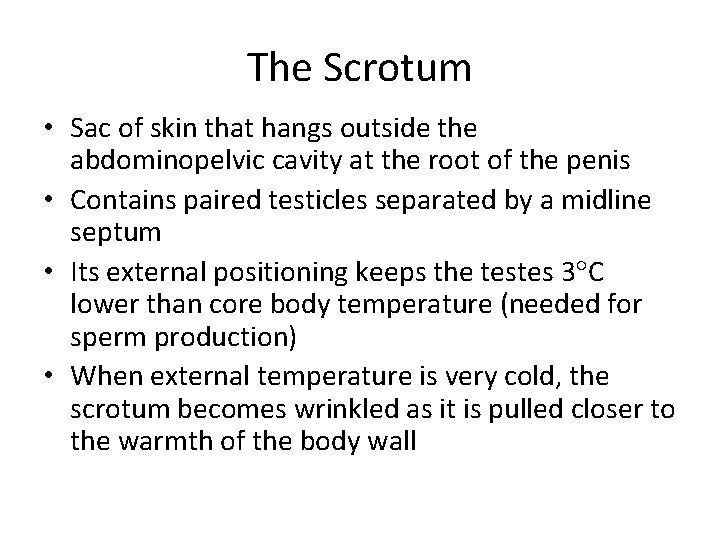
The Scrotum • Sac of skin that hangs outside the abdominopelvic cavity at the root of the penis • Contains paired testicles separated by a midline septum • Its external positioning keeps the testes 3 C lower than core body temperature (needed for sperm production) • When external temperature is very cold, the scrotum becomes wrinkled as it is pulled closer to the warmth of the body wall
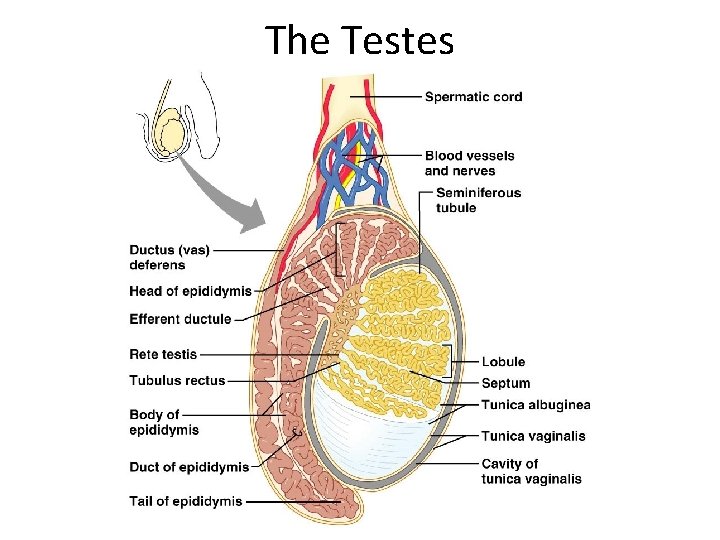
The Testes • Each testis is divided into 250 -300 lobules, each containing 1 -4 seminiferous tubules • Seminiferous tubules produce the sperm stimulated by FSH released by pituitary • Interstitial cells around the tubules produce androgens (testosterone) – stimulated by LH released by pituitary • Once the sperm are made, they continue to the epididymis
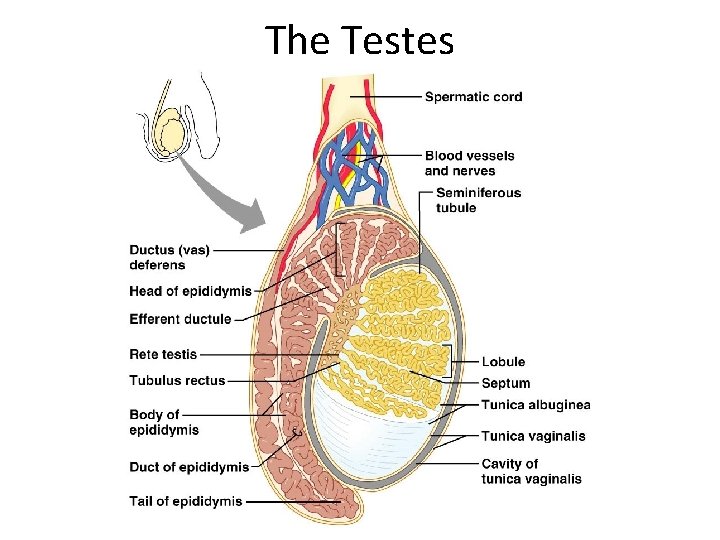
The Testes
The Epididymis • First part of male duct system • Provides a temporary storage site for the immature sperm cells – Trip through takes about 20 days – Sperm learn how to swim here! • When a male is sexually stimulated, the walls of the epididymis contract to propel sperm into the ductus deferens
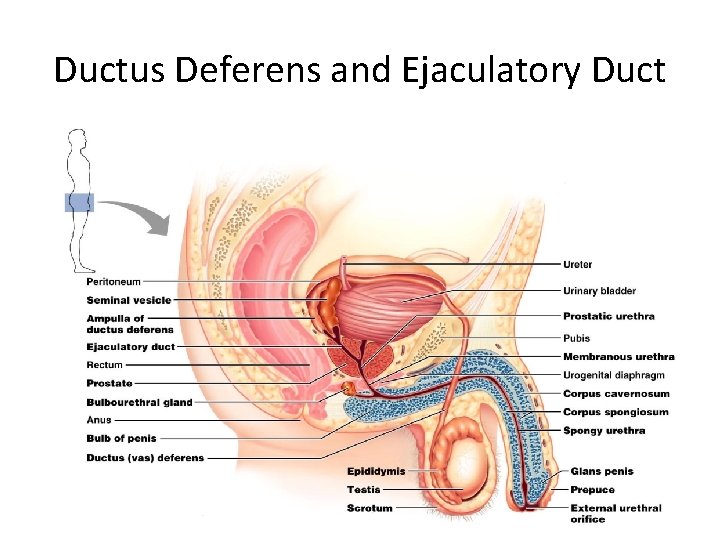
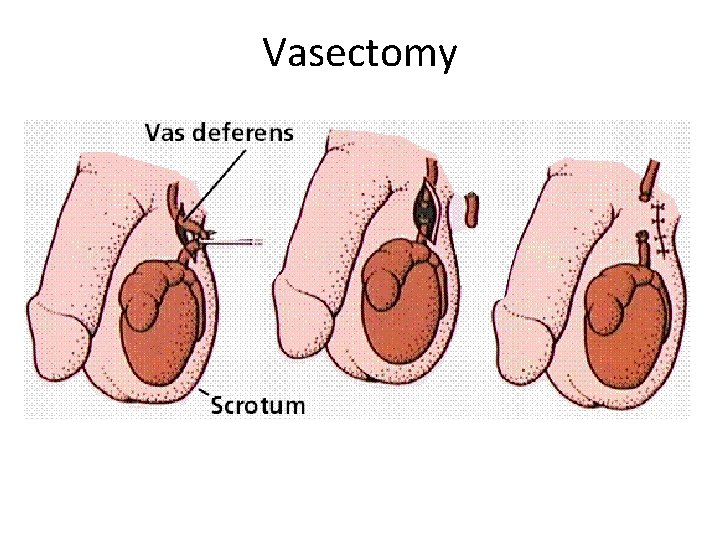
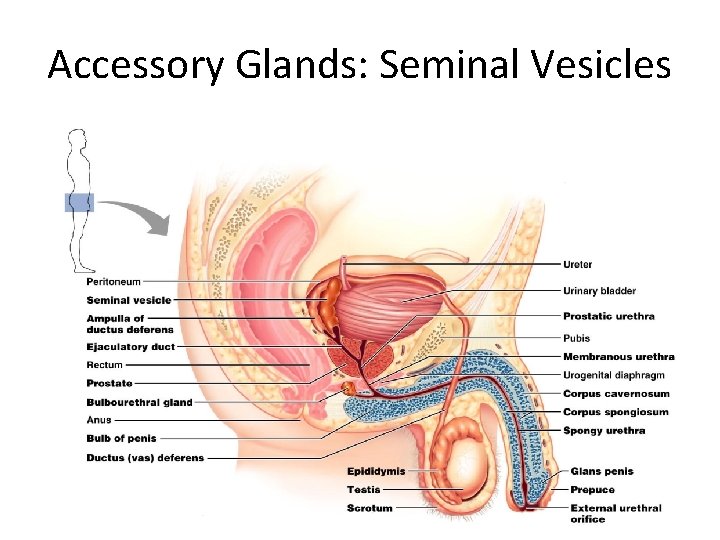
Ductus Deferens and Ejaculatory Duct • Propels sperm from the epididymis up into the pelvis, and back down to join up with the urethra • Also called the vas deferens • During an ejaculation, smooth muscles around the duct contract to create peristaltic waves that squeeze the sperm forward • Vasectomy – cutting and ligating the ductus deferens, which is a nearly 100% effective form of birth control
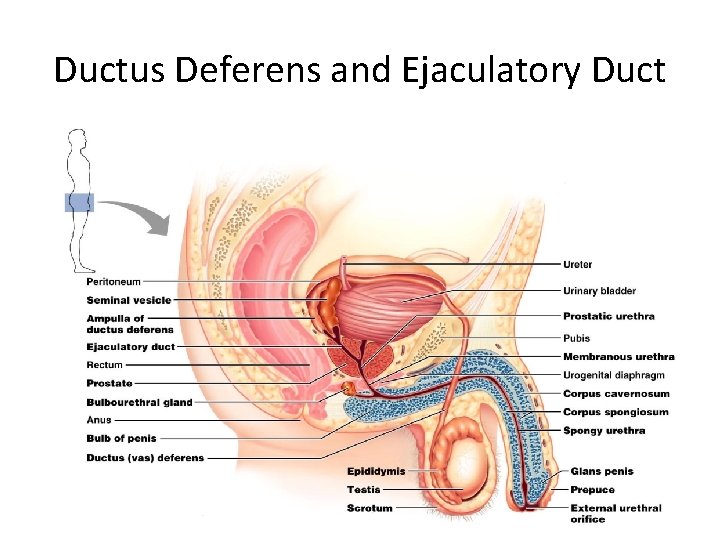
Ductus Deferens and Ejaculatory Duct
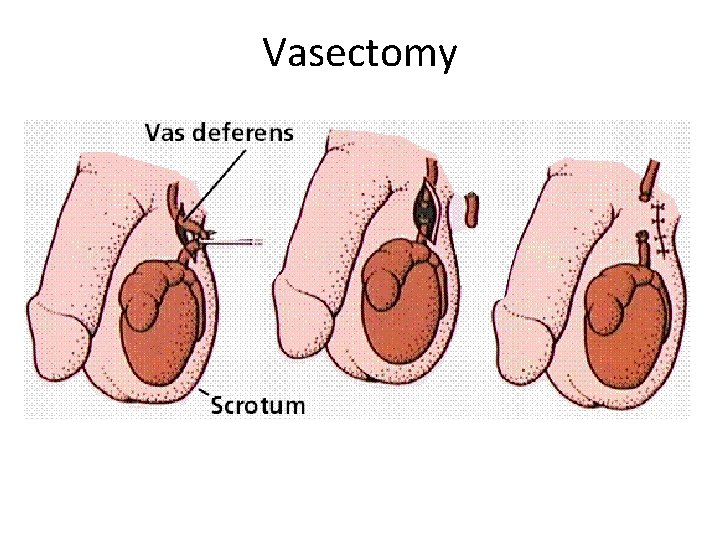
Vasectomy
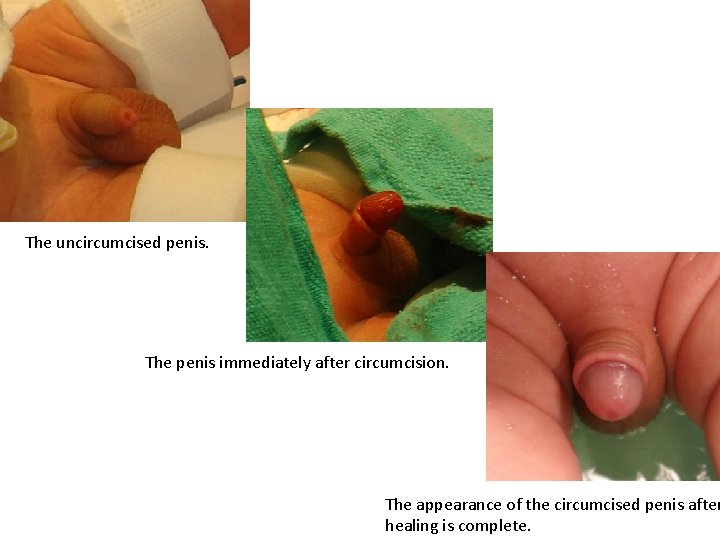
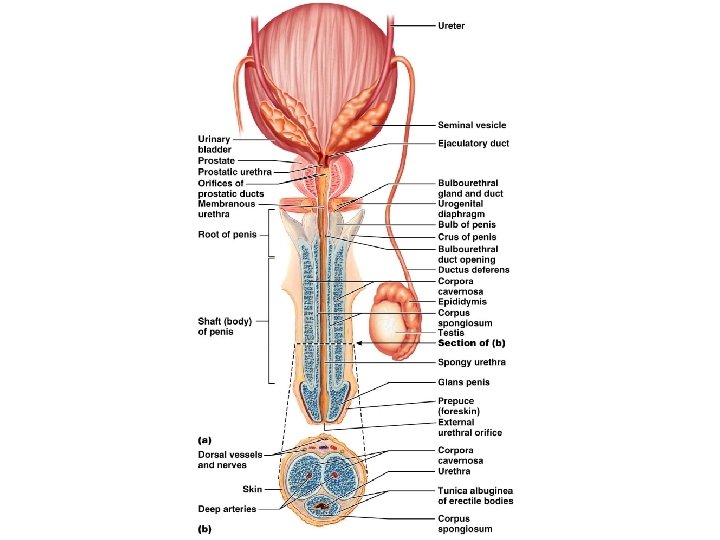
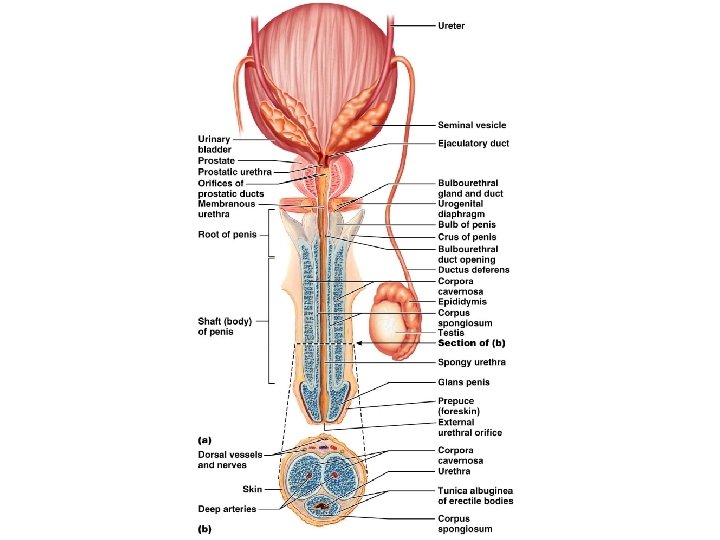
The Penis • A copulatory organ designed to deliver sperm into the female reproductive tract • Consists of an attached root and a free shaft that ends in the glans penis • Prepuce, or foreskin – cuff of skin covering the distal end of the penis – Circumcision – surgical removal of the foreskin after birth
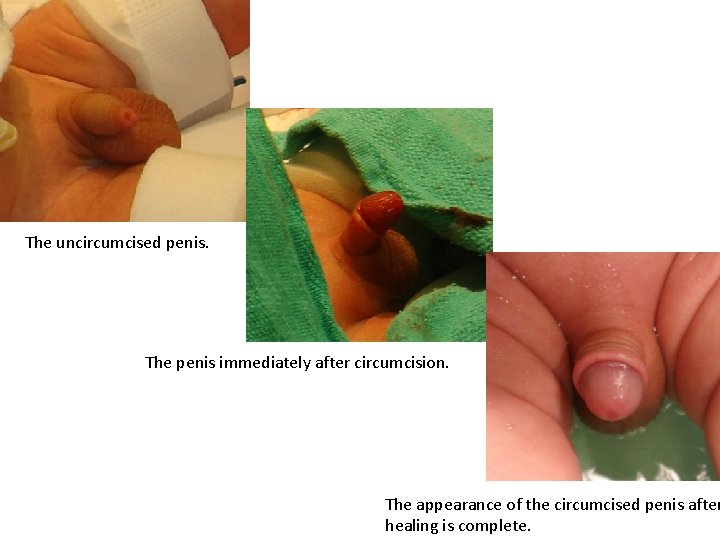
The uncircumcised penis. The penis immediately after circumcision. The appearance of the circumcised penis after healing is complete.
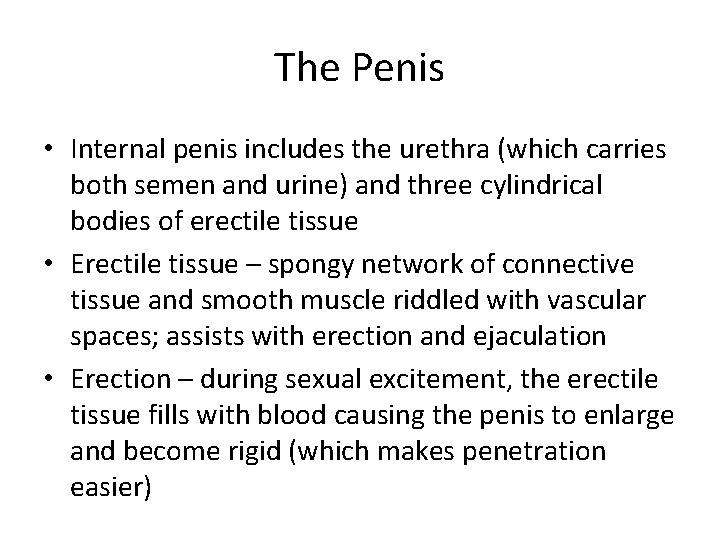
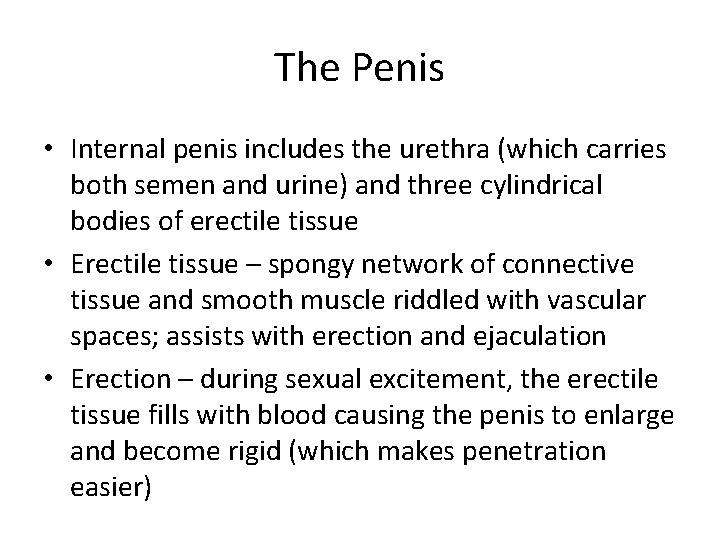
The Penis • Internal penis includes the urethra (which carries both semen and urine) and three cylindrical bodies of erectile tissue • Erectile tissue – spongy network of connective tissue and smooth muscle riddled with vascular spaces; assists with erection and ejaculation • Erection – during sexual excitement, the erectile tissue fills with blood causing the penis to enlarge and become rigid (which makes penetration easier)
The Penis
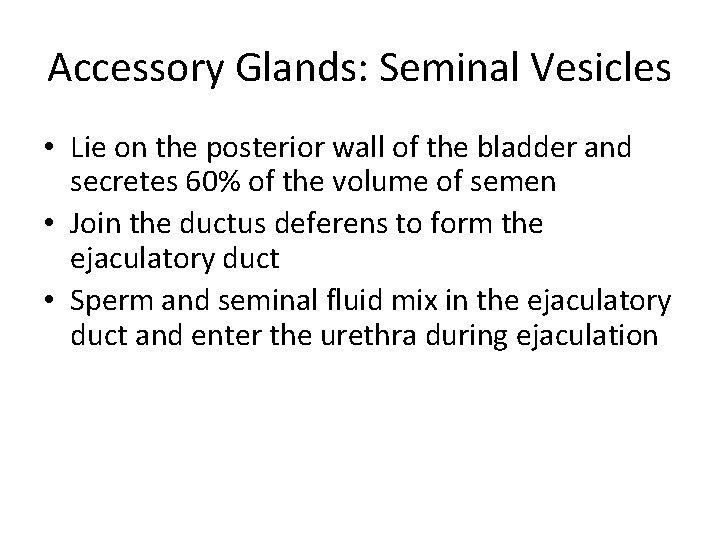
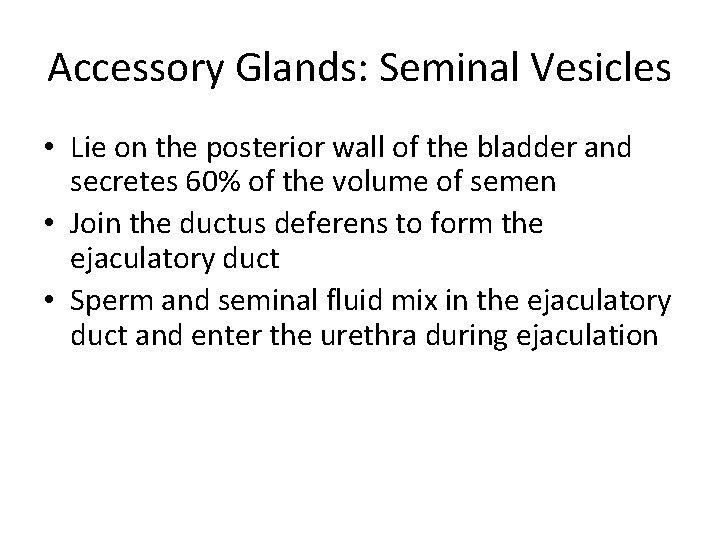
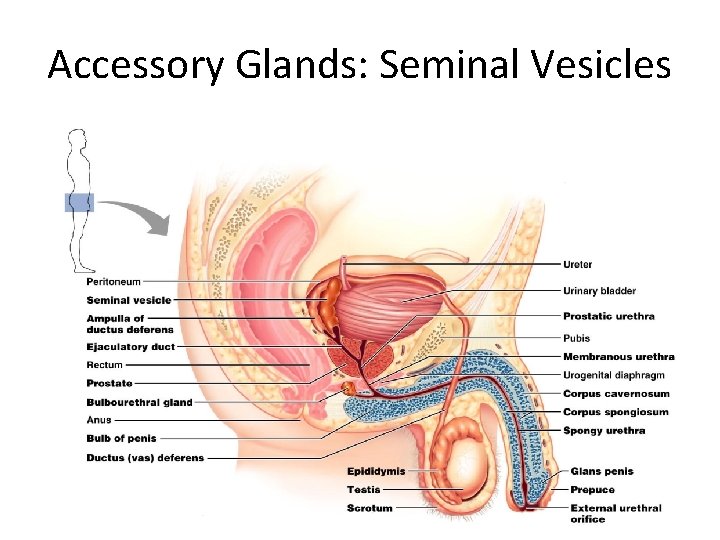
Accessory Glands: Seminal Vesicles • Lie on the posterior wall of the bladder and secretes 60% of the volume of semen • Join the ductus deferens to form the ejaculatory duct • Sperm and seminal fluid mix in the ejaculatory duct and enter the urethra during ejaculation
Accessory Glands: Seminal Vesicles
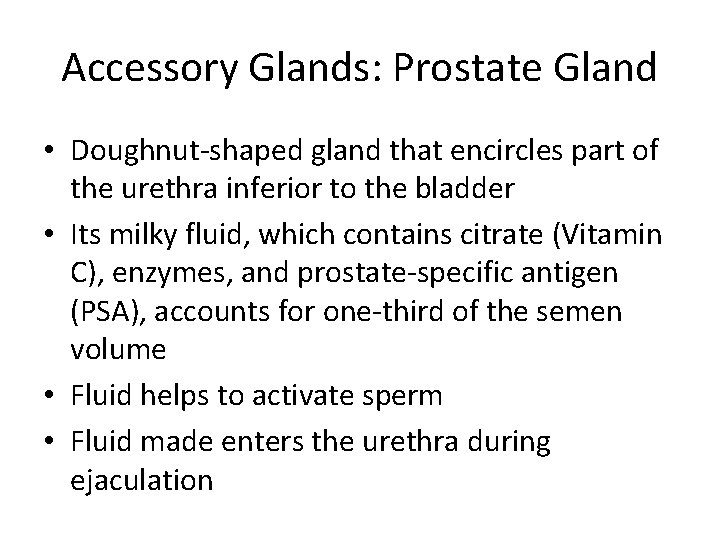
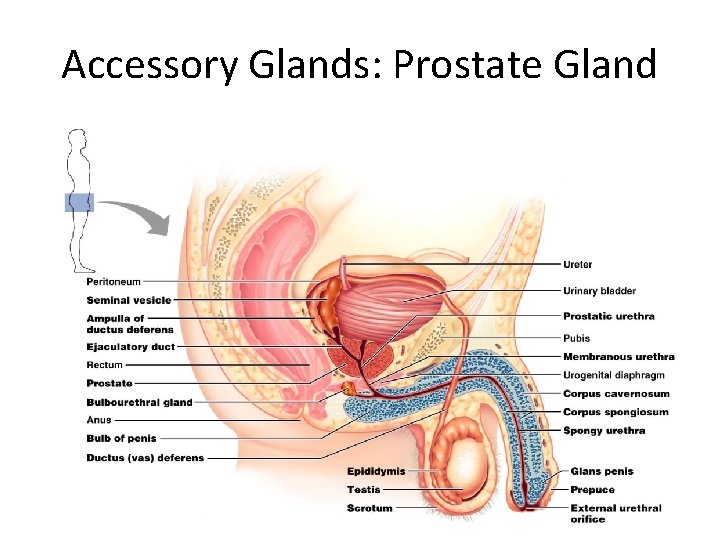
Accessory Glands: Prostate Gland • Doughnut-shaped gland that encircles part of the urethra inferior to the bladder • Its milky fluid, which contains citrate (Vitamin C), enzymes, and prostate-specific antigen (PSA), accounts for one-third of the semen volume • Fluid helps to activate sperm • Fluid made enters the urethra during ejaculation
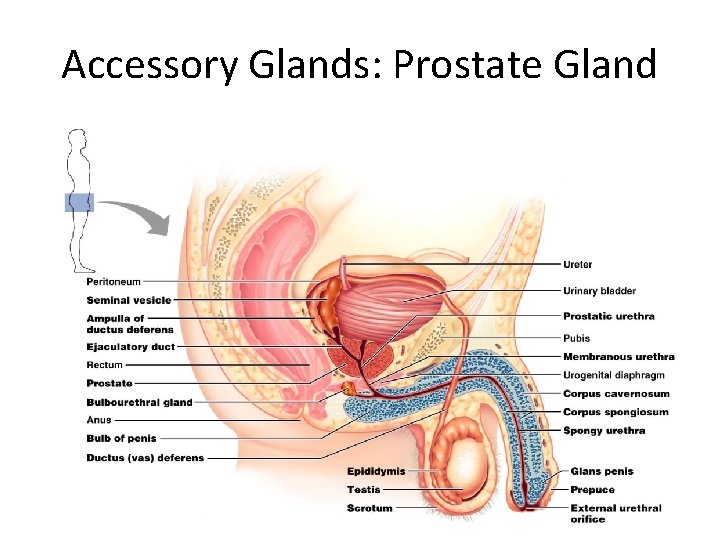
Accessory Glands: Prostate Gland
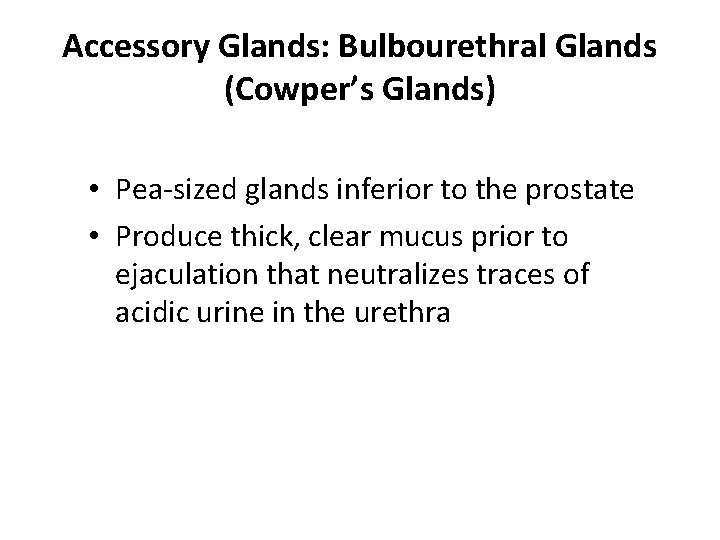
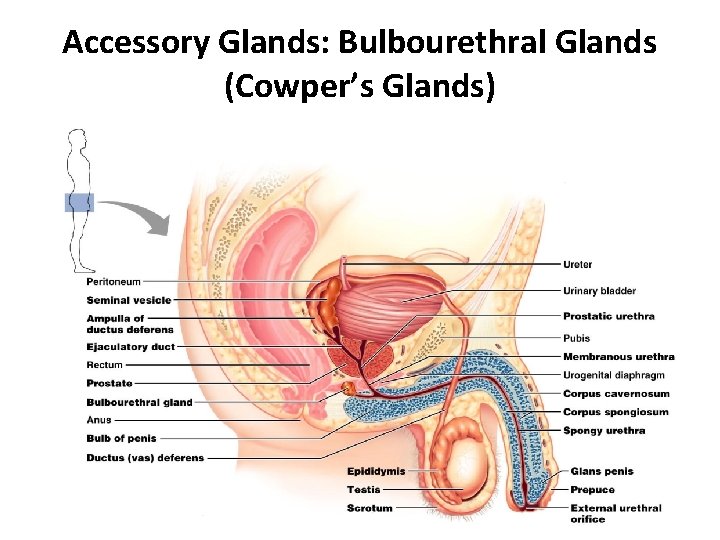
Accessory Glands: Bulbourethral Glands (Cowper’s Glands) • Pea-sized glands inferior to the prostate • Produce thick, clear mucus prior to ejaculation that neutralizes traces of acidic urine in the urethra
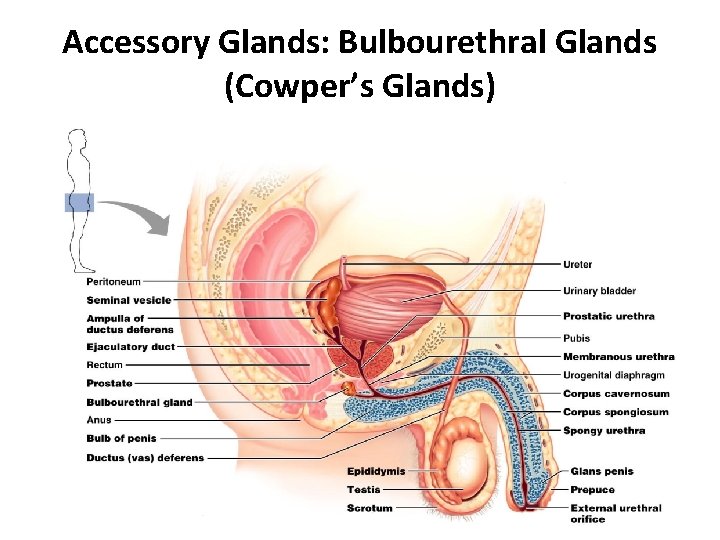
Accessory Glands: Bulbourethral Glands (Cowper’s Glands)
Semen • Milky white, sticky mixture of sperm and accessory gland secretions • Provides a transport medium and nutrients (fructose), protects and activates sperm, and facilitates their movement • Prostaglandins in semen: – Decrease the viscosity of mucus in the cervix – Stimulate reverse peristalsis in the uterus – Facilitate the movement of sperm through the female reproductive tract
Semen • Sperm are most active at neutral p. H, and can even die off at p. H of 4 and below! • However, vaginal p. H is normally 3. 5 -3. 9! • Seminal fluid and prostate gland fluid has a p. H of 7. 27. 6, which will help to neutralize out the vagina… but this doesn’t last forever! • p. H in vagina will drop back down to 4. 0 within 8 hours – so the lifetime of sperm in the vaginal canal is 8 hours max; lifetime in the uterus and fallopian tubes is about 48 hours • Only 2 -5 m. L of semen are ejaculated, but it contains 50 -130 million sperm per m. L
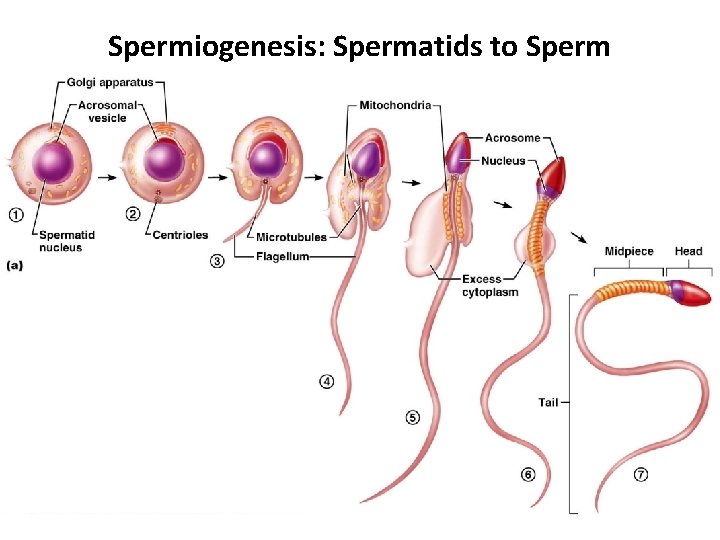
Sperm • Sperm have three major regions – Head – contains DNA and has a helmetlike acrosome containing hydrolytic enzymes that allow the sperm to penetrate and enter the egg – Midpiece – contains mitochondria spiraled around the tail filaments – Tail – a typical flagellum produced by a centriole
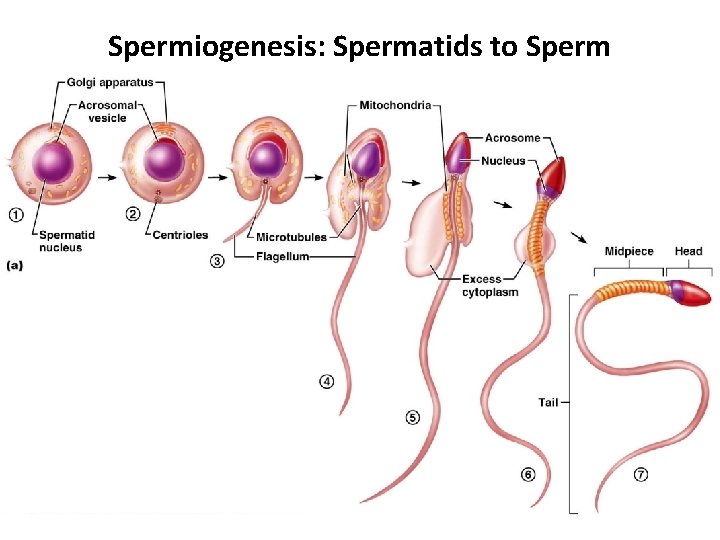
Spermiogenesis: Spermatids to Sperm

Secondary Male Characteristics • Deeper voice due to enlarged larynx • Increased hair growth over body, especially in axillary and pubic regions, as well as on face • Enlargement of skeletal muscles • Increased heaviness of bones • Long, narrow pelvis • All are due to testosterone levels
 Function of vagina
Function of vagina Male function
Male function Male and female reproductive system
Male and female reproductive system Exercise 42 anatomy of the reproductive system
Exercise 42 anatomy of the reproductive system Oogenesis diagram
Oogenesis diagram Female external reproductive system
Female external reproductive system Parts of male and female reproductive system
Parts of male and female reproductive system Male reproductive organ
Male reproductive organ Luteinizing hormone in male reproductive system
Luteinizing hormone in male reproductive system Male reproductive system in plants
Male reproductive system in plants Art-labeling activity: the male reproductive system, part 1
Art-labeling activity: the male reproductive system, part 1 Male reproductive system information
Male reproductive system information Where is semen stored
Where is semen stored Bull reproductive system parts and functions
Bull reproductive system parts and functions What does the prostate do
What does the prostate do Asexual reproduction
Asexual reproduction Function of male reproductive system
Function of male reproductive system Male fish reproductive system
Male fish reproductive system In pila fertilization is
In pila fertilization is Pig reproductive anatomy
Pig reproductive anatomy Female part of a flower
Female part of a flower Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Base of prostate gland
Base of prostate gland Chapter 20 reproduction and pregnancy
Chapter 20 reproduction and pregnancy Cow reproductive anatomy
Cow reproductive anatomy Pearson
Pearson